Abstract
As medicine continues to advance, many individuals are living longer with injuries previously considered life threatening. These individuals often face numerous long-term physical and psychological sequelae associated with their injury that persist through the course of their lives. Recently, other injury populations have begun to think of their condition as “chronic”. Using data collected from the Burn Model System National Database, a framework for the reconsideration of burn injury as a chronic condition is proposed.
Seventy years ago, even moderate burn injuries presented considerable risk of death despite medical treatment [1]. Today, despite much improved mortality rates, the burn care community is still defining expected recovery and the long-term symptom complex of the burn survivor. To provide the optimum quality of care, it is necessary for clinicians, insurers, employers, as well as burn survivors and their families to better understand the breadth of symptoms after burns. While some symptoms are commonly reported, other more insidious symptoms occur that are not typically recognized as an outcome of burn injury [2]. Furthermore, many symptoms are described that do not have a well-defined pathophysiology related to the burn injury, such as fatigue, pain, itch, and cognitive impairments [3]. Other fields of medicine have recently advocated to describe specific injuries as chronic conditions, including traumatic brain injury [4]. Considering burn injury as a chronic condition provides a framework for the medical management of burn recovery that includes survivors’ long-term needs [5].
In 1993, the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) established the Burn Model System (BMS) to improve the lives burn survivors [6]. The BMS National Database is the largest collection of long-term outcomes data in the field of burns. This report reviews self-reported symptoms from the BMS database as an initial step toward delineating the persistent symptom complex that characterizes burns as a chronic condition [7]. Twenty-two binary review of systems questions administered at three follow up time points (6, 12, and 24 months after injury) were examined from August 2015 – August 2017. At all time points, the most prevalent physical sequela was paresthesia (defined as numbness in the burn scar). Most symptoms reported by participants persisted for the entire 2-year period after burns. Furthermore, over one-quarter of the population reported the following symptoms at all time points: numbness in hands and/or feet, joint pain, hot and cold intolerance, balance trouble, and memory difficulty. The frequencies of all symptoms are detailed in Fig. 1.
Fig. 1 –
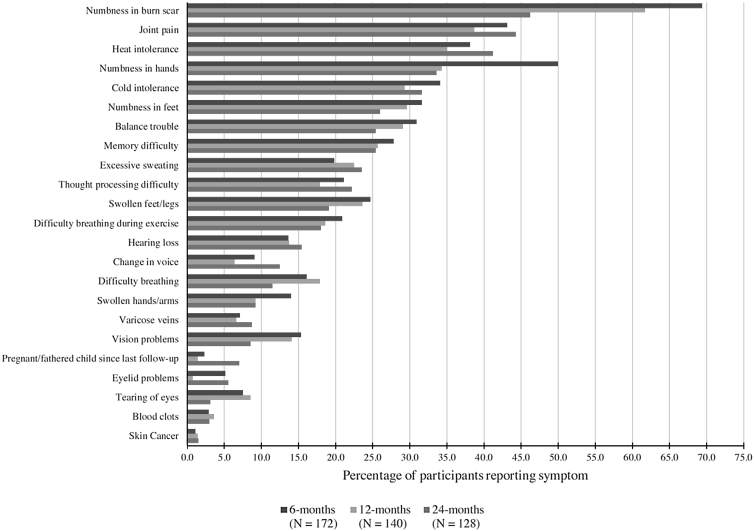
Percentage of Burn Model System Database participants reporting burn-related symptoms over time.
Previous studies in the burn survivor population corroborate the symptoms reported in the BMS Database. Recent literature notes a lack of effective treatments for numbness and paresthesias in areas affected by the burn [8]. Long term skin and musculoskeletal sequelae were corroborated in a cohort of burn survivors with severe burns at an average of 17 years after injury and findings of this study were reinforced with physical exam findings [9]. Recent research has demonstrated a physiologic link between thermoregulatory impairments and the lack of sweat glands exhibited in severe burns [10]. In regard to neurocognitive outcomes, researchers have documented impairments with autobiographical memory recall and ability to communicate memories efficiently [11]. In addition to the symptoms included in the BMS database, systematic reviews have identified the following persistent conditions: fatigue, sleep difficulty, tachycardia, chest pains, palpitations, hypertrophic scarring, dyschromia, altered skin texture/durability, renal insufficiency, kidney stones, incontinence, weight gain/loss, dissatisfaction with appearance, post-traumatic stress, depression, anxiety, itch, pain, grief, dysphagia, pulmonary embolism, constipation, change in appetite, contracture, and heterotopic ossification [12]. It is important to recognize both the debilitating nature and long-term complexity of these health problems. Fig. 2 illustrates the array of persistent symptoms identified from the BMS database as well as other publications. Due to the diversity and ongoing nature of symptoms and conditions experienced after a burn injury, it is critical to adequately represent the extent of burn sequelae.
Fig. 2 –
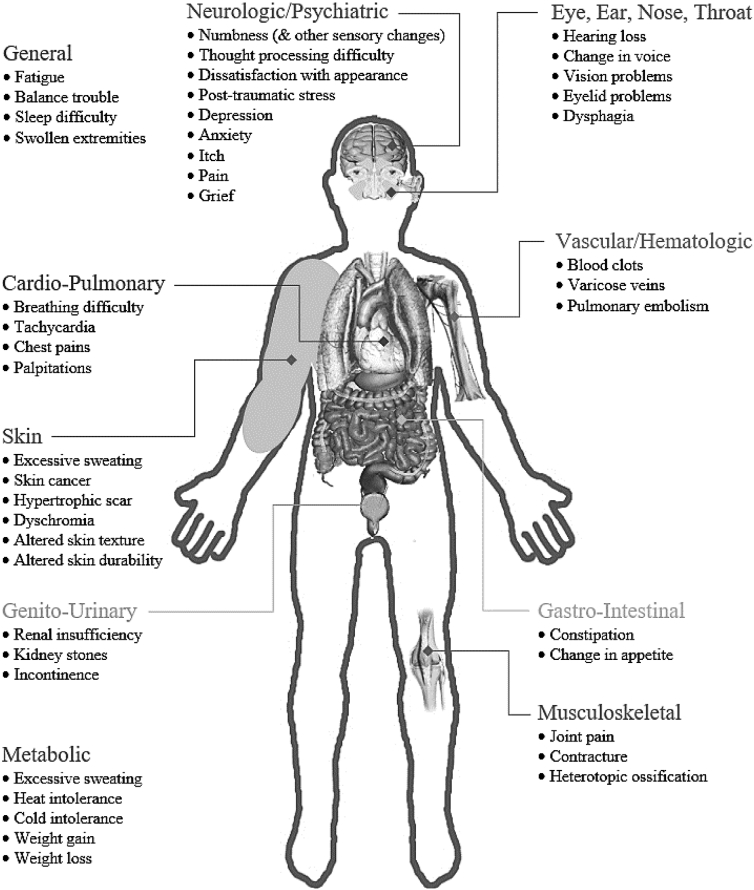
Potential long-term symptoms and other sequelae experienced by burn survivors.
Failure to identify burn injury as an acute condition that evolves into a chronic stage is an impediment to establishing a truly comprehensive system of care. Recognition of the chronic nature of burn symptoms will enable clinicians to address the significant, long-term, and degenerative aspects of the condition. The traumatic brain injury chronic condition literature provides evidence of improved quality of care through treatment of comorbid conditions and aging [4]. In burns, research highlights the interrelated nature of physical and psychosocial comorbidities, and that these complications changes over time [13]. The degenerative aspects of a burn injury manifest as an increased susceptibility to new comorbidities as well as worsening of preexisting comorbidities [14]. There are several benefits to reframing burn injury as a chronic condition. For one, the standardized collection of longitudinal outcome data would enable care providers to identify and target complications based on prevalence and risk assessment. Furthermore, applying a comprehensive system of preventative care has the potential dual benefit of improving wellness of the burn survivor population and reducing long-term medical expenses. To advance the quality of care for burn recovery it is necessary to more adequately define the long-term symptom complex and consider burn injury as chronic a condition.
Acknowledgements
The contents of this manuscript were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90DP0035 and 90DPBU0001). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this (insert type of publication; e.g., book, report, film) do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
Footnotes
Conflicts of interest
No authors have any conflicts of interest to disclose.
Contributor Information
B.M. Kelter, Department of Physical Medicine & Rehabilitation, Spaulding Rehabilitation Hospital, Harvard Medical School, Boston, MA, USA
R. Holavanahalli, Department of Physical Medicine and Rehabilitation, UT Southwestern Medical Center, Dallas, TX, USA
O.E. Suman, Department of Surgery, University of Texas Medical Branch and Shriners Hospitals for Children® - Galveston, Galveston, TX, USA
C.M. Ryan, Department of Surgery, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA; Shriners Hospitals for Children—Boston, Boston, MA, USA
J.C. Schneider, Department of Physical Medicine & Rehabilitation, Spaulding Rehabilitation Hospital, Harvard Medical School, Boston, MA, USA.
REFERENCES
- [1].Tompkins RG. Survival from burns in the new millennium: 70 years’ experience from a single institution. Ann Surg 2015;261(2):263–8, doi: 10.1097/SLA.0000000000000623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lawrence JW, Mason ST, Schomer K, Klein MB. Epidemiology and impact of scarring after burn injury: a systematic review of the literature. J Burn Care Res 2012;33 (1):136–46, doi: 10.1097/BCR.0b013e3182374452. [DOI] [PubMed] [Google Scholar]
- [3].Watson EJR, Nenadlová K, Clancy OH, Farag M, Nordin NA, Nilsen A, et al. Perioperative Research into Memory (PRiMe): cognitive impairment following a severe burn injury and critical care admission, part 1. Burns 2018;44(5):1167–78, doi: 10.1016/j.burns.2018.04.011. [DOI] [PubMed] [Google Scholar]
- [4].Corrigan JD, Hammond FM. Traumatic brain injury as a chronic health condition. Arch Phys Med Rehabil 2013;94(June (6)):1199–201, doi: 10.1016/j.apmr.2013.01.023. [DOI] [PubMed] [Google Scholar]
- [5].Rees S, Williams A. Promoting and supporting self-management for adults living in the community with physical chronic illness: a systematic review of the effectiveness and meaningfulness of the patient-practitioner encounter. JBI Libr Syst Rev 2009;7(13):492–582. [DOI] [PubMed] [Google Scholar]
- [6].Goverman J, Mathews K, Holavanahalli RK, Vardanian A, Herndon DN, Meyer WJ, et al. The National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: Twenty Years of Contributions to Clinical Service and Research. J Burn Care Res 2017;38(January/February (1)):e240–53, doi: 10.1097/BCR.0000000000000361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Schneider JC, Chen L, Simko LC, Warren KN, Nguyen BP, Thorpe CR, et al. Challenges to the standardization of burn data collection: a call for common data elements for burn care. J Burn Care Res 2018;39(February (2)):201–8, doi: 10.1097/BCR.0000000000000567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Xiao Y, Sun Y, Zhu B, Wang K, Liang P, Liu W, et al. Risk factors for hypertrophic burn scar pain, pruritus, and paresthesia development. Wound Repair Regen 2018;26(March (2)):172–81, doi: 10.1111/wrr.12637. [DOI] [PubMed] [Google Scholar]
- [9].Holavanahalli RK, Helm PA, Kowalske KJ. Long-term outcomes in patients surviving large burns: the musculoskeletal system. J Burn Care Res 2016;37(July-August (4)):243–54, doi: 10.1097/BCR.0000000000000257. [DOI] [PubMed] [Google Scholar]
- [10].Pearson J, Ganio MS, Schlader ZJ, Lucas RA, Gagnon D, Rivas E, et al. Post Junctional sudomotor and cutaneous vascular responses in noninjured skin following heat acclimation in burn survivors. J Burn Care Res 2017;38(January/February (1)): e284–92, doi: 10.1097/BCR.0000000000000372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Willebrand M, Norlund F, Kildal M, Gerdin B, Ekselius L, Andersson G. Cognitive distortions in recovered burn patients: the emotional Stroop task and autobiographical memory test. Burns 2002;28(5):465–71. [DOI] [PubMed] [Google Scholar]
- [12].Esselman PC, Thombs BD, Magyar-Russell G, Fauerbach JA. Burn rehabilitation: state of the science. Am J Phys Med Rehabil 2006;85:383–413, doi: 10.1097/01.phm.0000202095.51037.a3. [DOI] [PubMed] [Google Scholar]
- [13].McAleavey AA, Wyka K, Peskin M, Difede J. Physical, functional, and psychosocial recovery from burn injury are related and their relationship changes over time: a Burn Model System study. Burns 2018;44(June (4)):793–9, doi: 10.1016/j.burns.2017.12.011. [DOI] [PubMed] [Google Scholar]
- [14].van Beusekom I, Bakhshi-Raiez F, van der Schaaf M, Busschers WB, de Keizer NF, Dongelmans DA. ICU survivors have a substantial higher risk of developing new chronic conditions compared to a population-based control group. Crit Care Med 2019;47(March (3)):324–30, doi: 10.1097/CCM.0000000000003576. [DOI] [PubMed] [Google Scholar]


