Abstract
Purpose of review
To assess the current challenges regarding liver diseases, including the burden of disease, access to care, screening, and treatment needs in Latin America.
Recent findings
Latin America is a region with a rich multicultural heritage and important socioeconomic differences. The burden of liver diseases is high and mainly determined by a high level of alcohol intake and the surge of risk factors associated with NAFLD (i.e., sedentary lifestyles, broader access to highly processed foods, obesity, and type 2 diabetes mellitus). Hepatotropic viruses also play a role in the development of chronic liver diseases, although their comparative frequency has been decreasing over the last decades. There are important disparities in access to screening and treatment for liver diseases in Latin America, which are reflected in low access to critical treatments such as direct-acting antiviral agents and drugs to treat hepatocellular carcinoma. Also, important barriers to liver transplantation are present in multiple countries, including a low deceased donors’ rate and a lack of availability in several countries (especially in Central America). Our region also has disadvantages in research and education in liver diseases, which limits regional academic development and improvement in quality of care of liver diseases.
Summary
In order to tackle an increasing health burden due to liver diseases, Latin America urgently needs tailored interventions aiming to control the main risk factors for these disorders through the establishment of effective public health policies. Also, development of liver transplantation programs and improvement of medical education and research capabilities as well as extensive collaboration between all stakeholders are keys to address the liver disease agenda in the region.
Keywords: Public policy, Cirrhosis, Alcohol, Alcohol-associated hepatitis, ALD, Alcohol use disorders, Steatosis, Fatty liver disease
Introduction
Latin America comprises around 20 countries that account for more than 8% of the worldwide population [1]. The region is characterized by important social, cultural, ethnic, and economic differences, which determine significant variabilities in the burden of both infectious and non-transmittable liver diseases [2]. The gross domestic product (GDP) is one of the main economic indicators, and Latin America shows a substantial variability between nations (Table 1). For example, on the one hand, several countries have a GDP lower than USD 2500 per capita, including Haiti, Nicaragua, and Honduras [1]. On the other hand, countries like Costa Rica, Panama, Chile, and Uruguay have a GDP higher than USD 12,000 per capita [1]. Even with the low economic development of some Latin American countries, a recent analysis including 11 nations demonstrated that individuals in absolute poverty dropped from 1 in 3 in 2006 to 1 in 5 by 2019, while income inequality declined substantially over the same period of time [3]. In the same line, life expectancy and access to both drinking water and the Internet improved during this period [3]. Consequently, the differences mentioned above make Latin America a unique region in cultural heritage but determine disparities in health outcomes.
Table 1.
Main sociodemographic characteristics and development of liver transplantation in Latin America. Data was obtained from the World Bank Database and the International registry in organ donation and transplantation (IRODaT)
| Country | Population in 2019 | GDP+ | Gini index* | Life expectancy from birth (years)* | Deceased donors' rate* | DDLT rate* | LDLT rate* |
|---|---|---|---|---|---|---|---|
| Argentina | 44,938,712 | 8441.9 | 42.9 | 76 | 19.6 | 10.7 | 0.9 |
| Bolivia | 11,513,102 | 3143.1 | 41.6 | 71 | 0.4 | 0 | 0.8 |
| Brazil | 211,049,519 | 6796.8 | 53.4 | 75 | 18.1 | 10 | 0.8 |
| Chile | 18,952,035 | 13,231.7 | 44.4 | 80 | 10.4 | 8.1 | 1.1 |
| Colombia | 50,339,443 | 5332.8 | 51.3 | 77 | 8.4 | 5.3 | 1.1 |
| Costa Rica | 5,047,561 | 12,076.8 | 48.2 | 80 | 6.6 | 3.8 | 0 |
| Cuba | 11,333,484 | 9099.7 | N/A | 79 | 12 | 0.9 | 0.09 |
| Dominican Republic | 10,738,957 | 7268.2 | 41.9 | 74 | 2.2 | 0.5 | 0 |
| Ecuador | 17,373,657 | 5600.4 | 45.7 | 77 | 7.8 | 1.6 | 0 |
| El Salvador | 6,453,550 | 3798.6 | 38.8 | 73 | 0 | 0 | 0 |
| Guatemala | 16,604,026 | 4603.3 | N/A | 74 | 0.4 | 0 | 0 |
| Haiti | 11,263,079 | 1176.8 | 41.1 | 63 | 0 | 0 | 0 |
| Honduras | 9,746,115 | 2405.7 | 48.2 | 75 | 0 | 0 | 0 |
| Mexico | 127,575,529 | 8346.7 | 45.4 | 75 | 4.5 | 1.7 | 0.1 |
| Nicaragua | 6,545,503 | 1905.3 | N/A | 74 | 0.3 | 0 | 0 |
| Panama | 4,246,440 | 12,269.1 | 49.8 | 78 | 4.3 | 2.1 | 0 |
| Paraguay | 7,044,639 | 4949.8 | 45.7 | 74 | 0.3 | 0.3 | 0 |
| Peru | 32,510,462 | 6126.9 | 41.5 | 76 | 2.3 | 1.4 | 0.2 |
| Uruguay | 3,461,731 | 15,438.4 | 39.7 | 78 | 22.9 | 7 | 0.6 |
| Venezuela | 28,515,829 | N/A | N/A | 72 | 0 | 0 | 0 |
Abbreviations: DDLT deceased donor liver transplantation, GDP gross domestic product, LDLT Living donor liver transplantation
*Updated to 2019
+Updated to 2020
Information about the epidemiology of liver diseases in Latin America is scarce. At present, chronic liver disease represents one of the main burden of disease, and most of the cases in developed countries are explained by alcohol misuse and non-alcoholic fatty liver disease (NAFLD), also called metabolic dysfunction-associated fatty liver disease (MAFLD) [4, 5]. Other relevant etiologies are the hepatotropic viruses, especially in low-income countries with a high prevalence of hepatitis B virus (HBV) and hepatitis C virus (HCV) infection, affecting individuals of any age and generating a substantial cost in disability-adjusted life-years (DALYs) [6]. In this context, a proper characterization of epidemiology and healthcare resources in the region represents an opportunity to improve public health through prevention, surveillance, treatments, and education. These opportunities are well described in the literature and validated in several regions worldwide [7, 8]. The present review explores the current challenges that Latin American countries face regarding liver diseases, including the burden of disease, access to care, screening, and treatment needs.
The burden of liver diseases in Latin America
Latin America has 626 million people, who make up 58% of the continent’s population. However, epidemiological data on liver diseases in this region is limited or absent for some countries. As in other parts of the world, non-communicable diseases are the leading cause of mortality in the area, ranging from 62% in Costa Rica to 84% in Chile [9]. Of note, alcohol misuse and, in some countries, gastrointestinal diseases and cirrhosis are among the leading ten causes of DALYs [10]. For example, digestive diseases account for 15.8% of all diseases in Chile, where bile ducts and gallbladder disorders (4.2%), alcohol dependence (3.4%), and cirrhosis (3.3%) are the leading causes [11]. The estimated mortality rate due to cirrhosis in Latin America was 19.9 per 100,000 habitants in 2016 [12]. Unfortunately, the impact of liver disease in Latin America is significant and has increased throughout the entire region during recent years (Fig. 1). Indeed, the prevalence of compensated cirrhosis over the last 30 years increased by 33.2%, while decompensated cirrhosis increased by 54.8% [13].
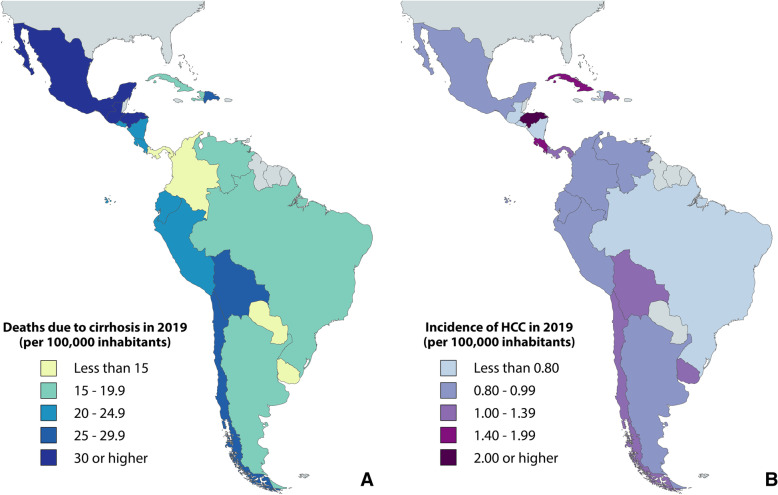
Fig. 1.
Impact of liver disease in terms of (A) deaths due to cirrhosis and (B) incidence of hepatocellular carcinoma (HCC). Data was obtained from the Global Burden of Disease database.
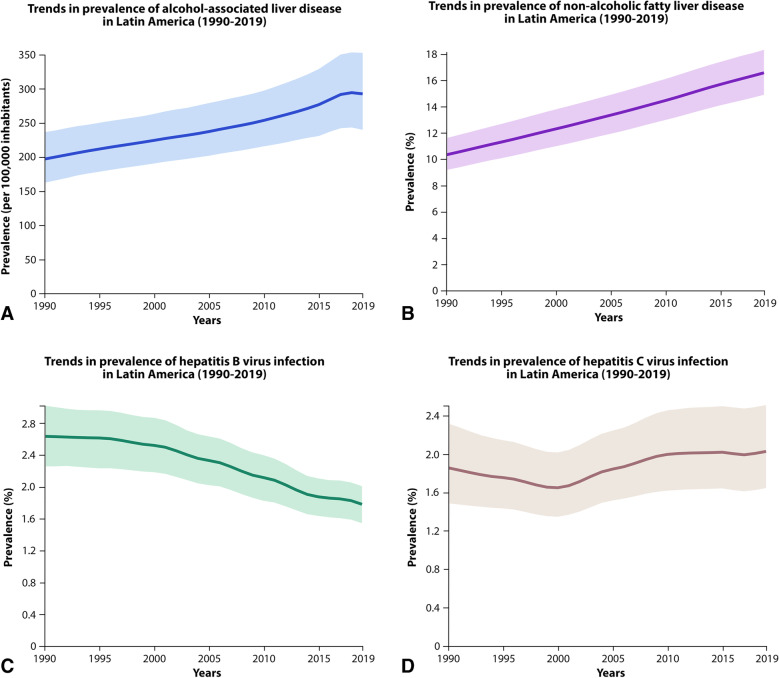
Excessive alcohol consumption causes a significant public health problem with devastating consequences, including alcohol-associated liver disease (ALD) and alcohol-associated hepatitis [14–16]. This is an important cause of chronic liver disease in Latin America and is the leading cause of cirrhosis in Argentina, Brazil, Chile, Mexico, and Peru [17]. In fact, the alcohol-attributable fraction of cirrhosis was around 53% [18]. Despite several efforts and public policies, the prevalence of ALD has been increasing during the last decades (Fig. 2A). Thus, the estimated number of deaths from ALD in Latin America was about 54,000 in 2017 [19], and the age-standardized death rate attributable to alcohol was 24 per 100,000 inhabitants in 2015 [18].
Fig. 2.
Trends in the main causes of chronic liver disease in Latin America between 1990 and 2019: (A) alcohol-related liver disease; (B) non-alcoholic fatty liver disease; (C) hepatitis B virus infection; (D) hepatitis C virus infection. Data was obtained from the Global Burden of Disease database.
NAFLD has an estimated global prevalence rate of 25% worldwide, and its prevalence is more significant and estimated at 31% in the Latin American population [20]. The prevalence of non-alcoholic steatohepatitis (NASH) increased more than any other cause of cirrhosis, and 8–11% of deaths due to cirrhosis were caused by NASH [13]. Few studies reported the NAFLD prevalence from Brazil (35.2%), Chile (23%), Mexico (17%), and Colombia (26.6%). Still, primary data from other Latin American countries are scarce, and most of the studies were performed more than a decade ago [20, 21]. Thus, it is likely that the current NAFLD prevalence is higher in Latin America. Of note, examination of epidemiological figures for obesity and diabetes as indirect estimates of NAFLD prevalence in the region suggest that NAFLD prevalence likely increased in the last decade; however, updated studies are needed (Fig. 2B) [22]. The prevalence of obesity in Latin America is significant, and some countries rank among the most affected worldwide [23]. Epidemiological trends for diabetes are also worrisome, with a very high prevalence in Chile and Mexico (8.6% and 13.5%, respectively) [24].
HBV, HCV, and hepatitis delta virus (HDV) infections generate relevant health problems in Latin America. In 2013, the estimated prevalence of HBV chronic infection ranged between 7 and 12 million people [25]. Different transmission routes have been observed among patients from Central and South America, with a higher prevalence between 20 and 40 years old. Evidence supports horizontal transmission as the most common route of infection in adults. Globally, Latin America is a region of intermediately high endemicity of HBV; however, this is dependent on the geographical location, as prevalence is highly variable with areas of low endemicity and others that have high endemicity (such as the Amazon basin region, including northern Brazil, Colombia, Peru, and Venezuela, as well as northwestern Argentina, Haiti, and the Dominican Republic) (Fig. 2C) [26, 27]. Counter to this, the HCV prevalence (estimated by anti-HCV) is low, reaching an overall prevalence of 1.5%, and roughly 70% of cases are due to genotype 1 [28]. Some areas, such as Chile, can have a prevalence as low as 0.2–0.5%, while other regions such as northeast Brazil have a slightly higher prevalence estimated at 1.7–3.4% (Fig. 2D) [29, 30].
The reports of HDV prevalence are scarce in Latin America. Notably, the infection is not restricted to risk groups, and it has been associated mostly with acute liver failure (ALF). In areas of northern Brazil, in the western Amazon region, many acute and chronic infections have been reported, where severe epidemics of HDV have affected this population, rapidly evolving to cirrhosis or death [31, 32]. A recent systematic review including 31 studies demonstrated that HDV prevalence among hepatitis B virus carriers was 22.37% in South America [33]. However, there was a substantial decline in HDV prevalence during the last decades.
Likewise, few epidemiological reports exist on autoimmune hepatitis (AIH) and other autoimmune liver diseases in Latin America. A recent Chilean cohort study demonstrated that AIH constitutes a frequent cause of liver transplantation (LT), with a prevalence of 13% in adult candidates [34]. In addition, a Peruvian study determined that between 4 and 6% of adult, LT in this country are secondary to AIH [35], while in Argentina, it corresponds to the second most common cause of ALF (25% of the cases) [36].
Risk factors for liver diseases in Latin America
Multiple factors are associated with liver diseases, especially those related to ALD, NAFLD, and the pathogenesis of cirrhosis. Notably, the high prevalence of liver diseases in Latin America is influenced by genetic factors, the elevated prevalence of obesity and metabolic syndrome, and environmental factors such as diet, low exercise, and excessive alcohol intake.
Genetic factors
Several genes have been identified to be associated with liver disease. Particularly, Patatin-like phospholipase domain-containing protein (PNPLA3) nonsynonymous gene variant (rs738409 c.444 C > G p.I148M) is the most studied genetic polymorphism shown to be robustly associated with steatosis, steatohepatitis, and fibrosis in patients with NAFLD [37]. Interestingly, a high prevalence of p.I148M has been observed in the general population in Latin America. An allelic frequency of the high-risk allele G of 59% in the general population has been reported in Chile, whereas in Argentina, the GG genotype of PNPLA3 rs738409 was present in 63.7% of individuals [38, 39]. In ALD, genetic factors are also associated with the onset and progression of the disease. For example, genetic polymorphisms among Amerindian populations in Mexico would increase the predisposition and severity of ALD [40, 41], similar to what was observed in the USA in the Hispanic ancestry population [42, 43]. The PNPLA3 polymorphisms, which are highly prevalent in the general Latin American population, would also play a vital role in ALD. Subjects carrying PNPLA3 have an increased risk of ALD and progression to cirrhosis and hepatocellular carcinoma (HCC) [44, 45]. A higher risk has been observed in subjects with the GG genotype than in the CC genotype (which had the four-fold risk of having ALD) [46]. Also, the TM6SF2 and MBOAT7 genes, related to lipid metabolic processes, confer risk for severe ALD [47, 48]. The TM6SF2, like PNPLA3, would have a role in the modulation of hepatic fat accumulation, fibrosis, and HCC development [49]. On the other hand, the MBOAT7 polymorphism is mainly associated with the generation of fibrosis [50].
Obesity, overweight, and metabolic syndrome
The increasing prevalence of obesity and overweight, known risk factors for liver diseases, in Latin America poses a major public health challenge to the region [51]. In recent years, the prevalence of obesity in Latin America has been increasing faster than in the rest of the world, being more critical in people of low socioeconomic status [52]. Currently, the prevalence of obesity in Latin America is among the highest globally. This situation is more complex in children and adolescents, where one in five is overweight or obese [52]. The transition from a predominantly underweight population to one that is overweight and obese has been remarkably rapid in Latin America; this has been associated with changes in food systems and living environments characterized by greater availability, accessibility, and affordability of ultra-processed foods, as well as an increase in sedentary lifestyle [53]. The countries with the highest prevalence of obesity are Mexico (20.6% in men, 32.7% in women), Chile (22% in men, 30.3% in women), Costa Rica (15.4% in men, 28.8% in women), and Uruguay (23.3% in men, 25.4% in women) [23]. Metabolic syndrome is another relevant risk factor for liver diseases that exhibit high prevalence rates (between 25 and 37%) in Latin America [54, 55]. The recent Cardiovascular Risk Factor Multiple Evaluation in Latin America (CARMELA) study found a global prevalence of metabolic syndrome of 21% [56]. The most affected cities were Mexico City (27%), Barquisimeto (26%), Santiago (21%), and Bogota (20%), and the cities with the lowest prevalence were Lima (18%), Buenos Aires (17%), and Quito (14%) [56]. Physical inactivity plays a fundamental role as a contributor to obesity and overweight and is highly prevalent in the region. Latin America corresponds to the area with the highest sedentary lifestyles globally, with a prevalence rate of insufficient physical activity of 32% [57]. This situation is also problematic in teenagers since only 15% of adolescents are physically active [58].
Alcohol consumption
It is critical to consider the role of alcohol consumption in this region as a predominant risk factor for liver disease. In Latin America, the harmful consumption of alcohol represents a significant health, social, and economic burden. More than 50% of people ≥ 15 years of age are current drinkers, and this prevalence has increased in recent years and is the leading cause responsible for almost 60% of cirrhosis. The estimated per capita consumption in Latin America was 6.84 L of pure alcohol in 2016, which was higher than the average consumption worldwide [12]. Men have a higher prevalence of alcohol use disorder (AUD) than women (8% vs. 2%, respectively), a phenomenon that is similar to other regions [4, 12]. In addition, low and lower-middle-income countries have the highest AUD prevalence, even with lesser alcohol consumption than countries with higher income [59, 60].
Incidence and mortality of hepatocellular carcinoma
Hepatocellular carcinoma (HCC) accounts for 85% of primary liver cancers worldwide, being the sixth most commonly diagnosed cancer and the third leading cause of cancer death in 2020, with 830,000 deaths, of which 4.6% occurred in Latin America (Fig. 1B) [61]. Both incidence and mortality are twice as high in men as in women [62]. The mortality due to HCC across the region ranges from less than 2.8 to more than 6.3 per 100,000 inhabitants, similar to other parts of the world. The ratio between incidence and mortality is close to 1, confirming the high lethality of HCC in the region. In fact, HCC is the leading cause of death due to cancer in Guatemala [61]. Most cases are diagnosed before age 50, with devastating consequences in DALYs [63].
The most frequent causes of HCC in Latin America are HCV and ALD [63]. However, HBV is the leading cause in Brazil and Peru (38% and 34%, respectively). An Argentinean cohort study demonstrated that HCV was the main etiology of HCC between 2009 and 2016. However, at the end of the study period, an increase in NASH as the etiology of HCC was seen up to 6 times. These results show a trend and projection of an increase in HCC due to NAFLD, similar to that described in North America [62, 64].
Several studies in HCC consistently report a high proportion of advanced stages at the moment of diagnosis (20–41%) [63]. Also, a substantial number of cases are diagnosed outside of surveillance programs. Indeed, data obtained from a South American retrospective cohort that included 14 centers in six countries showed that only 47% of HCC cases were carried out through surveillance programs. The latter is relevant since incidental diagnosis (outside the context of HCC screening) is associated with increased mortality compared to those diagnosed via surveillance [63].
Acute liver failure in Latin America: a critical situation
ALF is an entity characterized by severe acute or subacute temporary liver damage in patients without a prior history of chronic liver disease, with high associated morbidity and mortality. The most common manifestations of ALF are hepatic encephalopathy and prolonged coagulation time, as a manifestation of severe liver dysfunction. ALF is caused by various etiologies such as viral infections, autoimmunity, drug-induced liver injury (DILI), acute vascular liver disease, or pregnancy-related diseases.
There is limited information available regarding the etiologies of ALF in Latin America. A Brazilian retrospective study including candidates from 12 centers showed that 325 (5.4%) patients were secondary to ALF (2006–2015). Among the main etiologies in adults, 34% were cryptogenic, 26% DILI, 18% AIH, 8% HBV, 6% Wilson’s disease, 4% Hepatitis A virus (HAV), 1% acetaminophen overdose, and 1% acute fatty liver of pregnancy. Regarding DILI, the most frequent drugs related were anti-tuberculosis regimens with isoniazid, rifampin, and pyrazinamide (21%), non-steroidal anti-inflammatory drugs (21%), antibiotics (19%), along with other reports with phenytoin, venlafaxine, and propylthiouracil, among others [65]. In Argentina, a registry-based retrospective study carried out between 1998 and 2016 and including 363 adult patients transplanted due to ALF showed that the main etiology was cryptogenic in 103 cases (28.3%), followed by AIH (25%), HBV (17%), non-acetaminophen DILI (14%), and HAV 1.1% [36].
Acute-on-chronic liver failure (ACLF) is an important cause of admission and mortality. In Chile, a preliminary retrospective cohort study included 334 patients between 2017 and 2019 [66]. Patients with ACLF were younger and had higher MELD-Na and APACHE II on admission vs. decompensated cirrhotics without ACLF. In this cohort, the most common triggers were infections (42.4%), gastrointestinal bleeding (23.2%), and alcohol (31.3%), and the leading organ failures were kidney (60.2%) and brain (49.3%). The cumulative survival at 180 days was 58.3% in ACLF (p = 0.004), with significantly higher mortality in ACLF grade 2 and ACLF grade 3 when compared with patients without ACLF (HR 2.3 and 2.99, respectively; p < 0.05). Also, the risk of mortality or transplantation was higher in ACLF grade 2 and ACLF-3 than patients without ACLF (HR 2.19 and 4.61, respectively; p < 0.05) [66].
Socioeconomic differences, healthcare access, and treatments among Latin American countries
There are significant wealth disparities between countries, while some countries reach high positions on the gross domestic product (GDP) or the Human development index rankings; others place at the bottom of those rankings [1, 67]. Overall, Latin America has increased healthcare expenditure from 7.2% GDP in 2012 to 8% GDP in 2018 [1]. However, the current health expenditure as a percentage of GDP ranges from 11.2% (Cuba) to 3.5% (Venezuela) and is lower than the Organization for Economic Cooperation and Development (OECD) average (12.4%)[1].
During the last three decades, several Latin American countries have implemented social and health sector reforms to achieve universal healthcare access and coverage and address social inequities. Unfortunately, the disparities persist across Latin American countries, and health systems are still deeply fragmented [68–70]. Consequently, healthcare access is still limited by several factors, such as educational level, rural status, or ethnicity [71]. Also, high out-of-pocket expenditure and financial vulnerability and delay in new technologies incorporation are still challenging to be overcome [72, 73]. Access to advanced treatments is a particular issue for liver disease care. Recent progress in HCC and viral hepatitis care may not be available to a significant proportion of patients who live in deprived or rural areas [74, 75]. For example, in the GIDEON study, fewer patients with HCC from Latin America received TACE before sorafenib initiation versus the global cohort [75, 76]. Also, Latin American countries have some differences in sorafenib cost, but almost all (except for Brazil) pay higher prices than high-income European countries [77]. There are some opportunities to cope with these issues: cost-effectiveness analyses and health technology assessment, collective negotiation, and the use of generics and biosimilars through the flexibility of patent laws [78]. Lastly, the recent COVID-19 pandemic is a new threat for Latin America structurally stressed health systems. The impact in liver disease control, such as direct-acting antiviral and HCC screening coverages, is still forthcoming.
Liver transplantation in Latin America
Despite major economic limitations in Latin America and the lack of effective immunosuppressive drugs, the first LT was performed in 1968 in Brazil and 1969 in Chile [79]. In recent years, medical knowledge and surgical expertise have improved LT outcomes in Latin America, reaching a post-LT survival comparable to other regions of the world. For example, a Chilean nationwide cohort exhibited a 1-year post-LT survival of 84% [34]. Also, an Argentinean study showed that 1-month post-LT survival rates improved from 70 to 82% in the last 20 years, with a consistently associated reduction in wait-list mortality from 27 to 19% [36]. Furthermore, a Peruvian study demonstrated a 5-year survival after LT was 90.9%, while the 5-year graft survival was 95.5% [80]. However, differences among countries could be due to indication of LT, the severity of the liver disease before LT, and under-recording of deaths. The cause for LT follows the same trend in Latin America as in other western countries. For example, NAFLD-related cirrhosis is a growing indication for LT. In fact, it actually constitutes the main etiology of LT in Chile [34]. NAFLD-related cirrhosis was also the third etiology of underlying disease in HCC candidates for LT [81]. At the same time, the percentage of LT for HCV has declined in the last decades due to the extended use of effective antiviral regimens [82].
There are important barriers to donation, enhanced by inadequate financial and legislative support [83]. Regrettably, the donor rate is extremely low in most Latin American countries compared to Europe or North America, and there are dramatic differences between countries in the region (Table 1). For example, Argentina and Brazil perform more than 10 LT per million of the population (PMP) while countries like Venezuela, Dominican Republic, Paraguay, and Bolivia have around 0.2–0.4 PMP [84]. Moreover, LT is not routinely performed in six countries of Central America, including Guatemala, Trinidad y Tobago, Honduras, Nicaragua, El Salvador, and Haiti (Table) [85]. The main consequence of the low donor rate is the excessive dropout (progression or death) on the waitlist, which remains high despite the income level. For example, the dropout among Chilean candidates is 37.6% in adults and 22.1% in the pediatric population [34, 86].
An equitable allocation of donated organs to patients who need them the most on the waiting list is crucial. Initially, the liver allocation policy in most countries of Latin America was based on a patient’s location of care and time on the waiting list [83]. However, the social and political requests for a better allocation system, focusing on the severity of underlying liver disease, led to the implementation of an allocation policy based on the model for end-stage liver disease (MELD) score in countries like Brazil, Argentina, Mexico, and Chile [85]. Unfortunately, this new policy has not changed the waiting list mortality [34, 87]. Many important legal issues must be modified or implemented to address the problem [88], for example, brain death diagnosis criteria, the type of consent for retrieval, restrictions for living unrelated donation to avoid donor manipulation, medical criteria for allocation, and a clear prohibition of organ commercialization. One important advancement has been creating a presumed donor law wherein patients must explicitly opt-out of being organ donors [85]. However, cultural attitudes and beliefs in these countries, different organ donation legislation and the lack of a robust donor and overall health care organizational structure in Latin America are impediments to transplantation as a whole [89–91].
Unmet needs in liver diseases and future perspectives
A transversal limitation in LA is poor healthcare access and appropriate treatment. The lack of laws and resources limits the access to the improvements to therapy, research, education, and continuous medical training, limiting the ability to expand knowledge and generate data promoting a constant improvement of medical care [63]. Thus, the most critical barriers to decreasing the burden of liver diseases include lack of well-structured screening programs, absence of early identification of the population at risk of liver diseases (such as those with chronic HBV or HCV infection), ineffective application of routine HCC surveillance throughout the region, the lack of a robust and integrated health care system to treat and follow-up patients, and poor access in rural areas [63, 92]. For example, in a study including most countries from South America, only 54% of patients diagnosed with HCC were under surveillance [93]. Moreover, adherence to clinical guideline recommendations can be as low as 62%, and 41.2% of patients with HCV have not received direct-acting antiviral agents [94, 95].
As ALD is the main cause of cirrhosis in LA, excessive alcohol consumption should be actively sought to limit and regulated [14, 96]. A recent ecological study showed that the establishment of public health policies on alcohol consumption in LA is extremely heterogeneous; however, a higher number of public policies was associated with lower mortality due to ALD and AUD prevalence [12]. Interestingly, higher mortality of alcohol-related health consequences has been described in low-income countries, despite a lower alcohol consumption than countries with a higher income [97]. Therefore, it is especially relevant to implement robust and tailored measures to address alcohol misuse and its consequences [18, 60]. In addition, there are no specific public health policies on NAFLD in the Americas, which is similar to the situation of other world regions [98]. Thus, it is important to promote public health policies and raise awareness of the main risk factors for liver disease in Latin America [51, 60].
The lack of LT programs in many parts of the region generates important disparities in the management of advanced liver diseases. This point is critical since most cirrhotic patients may be undertreated due to the lack of LT availability. As the rate of LT carried out per million people is mainly correlated with the GDP, none of the Latin American countries classified as lower middle income (Honduras, Nicaragua, Guatemala, and Bolivia) can maintain LT programs [99]. This could be partially addressed through a higher allocation of resources and advanced training opportunities for healthcare teams.
Among proposed solutions, it is essential to perform well‐designed prevalence studies and reliable registries to better understand the prevalence of liver diseases in every Latin American country [100]. Secondly, better screening methods should be implemented to the population with well‐known risk factors [101]. Moreover, pharmaceutical companies should allow low‐ and middle‐income countries to access new treatments at lower costs or generic versions of the same [100]. Also, implementing measures that have proved to be effective in reducing alcohol consumption such as restricting easy access to alcohol, advertising, and specific pricing regulations are also recommended [18]. Finally, improving medical education and clinical research through better government funding and regional and international collaborations would predictably impact care of liver diseases in the region [51, 102].
Conclusions
Latin America is a multicultural region with important differences in socioeconomic status and healthcare access. Alcohol misuse and HBV infection were important causes of liver disease. However, sedentary lifestyles, broader access to highly processed foods, and a sustained increase in the prevalence of obesity and type 2 diabetes mellitus in the region have determined a shift, with NAFLD becoming a leading cause of chronic liver disease, especially in developed countries. Socioeconomic differences and inequities greatly influence the development, quality, and access to screening and treatment for liver diseases. Strong efforts and public policies should be encouraged to decrease the burden of liver diseases in LA.
Abbreviations
- ACLF
Acute-on-chronic liver failure
- ALD
Alcohol-associated liver disease
- ALF
Acute liver failure
- AUD
Alcohol use disorder
- DALYs
Disability-adjusted life-years
- DILI
Drug-induced liver injury
- GDP
Gross domestic product
- HBV
Hepatitis B virus
- HCV
Hepatitis C virus
- HDV
Hepatitis delta virus
- HCC
Hepatocellular carcinoma
- LT
Liver transplantation
- MAFLD
Metabolic dysfunction-associated fatty liver disease
- NAFLD
Non-alcoholic fatty liver disease
- NASH
Non-alcoholic steatohepatitis
- PHP
Public health policies
- PNPLA3
Patatin-like phospholipase domain-containing 3
- US
United States
- USD
United States Dollars
- WHO
World Health Organization
Author contribution
Authors confirm contribution to the article as follows:
Luis Antonio Díaz: Conceptualization, writing (review), and editing, supervision.
Gustavo Ayares: Writing—review and editing.
Jorge Arnold: Writing—review and editing.
Francisco Idalsoaga: Writing—review and editing.
Oscar Corsi: Writing—review and editing.
Marco Arrese: Review and editing.
Juan Pablo Arab: Conceptualization, writing (review), and editing, supervision.
Funding
Juan Pablo Arab and Marco Arrese receive support from the Chilean government through the Fondo Nacional de Desarrollo Científico y Tecnológico (FONDECYT 1200227 to JPA and 1191145 to MA) and the Agencia Nacional de Investigación y desarrollo (ANID) through ANID ACE 210009 grant. Additionally, this project has received funding from the European Union’s Horizon 2020 Research and Innovation Program under grant agreement no. 825510.
Compliance with Ethical Standards
Human and animal rights and informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of interest
Luis Antonio Díaz declares that he has no conflict of interest.
Gustavo Ayares declares that he has no conflict of interest.
Jorge Arnold declares that he has no conflict of interest.
Francisco Idalsoaga declares that he has no conflict of interest.
Oscar Corsi declares that he has no conflict of interest.
Marco Arrese declares that he has no conflict of interest.
Juan Pablo Arab declares that he has no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Bank Open Data. [cited 2022 Feb 21]; Available from: https://data.worldbank.org
- 2.Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70:151–171. doi: 10.1016/j.jhep.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 3.OECD. How’s Life in Latin America? Measuring well-being for policy making: Measuring well-being for policy making. OECD Publishing; 2021.
- 4.GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392:1015–1035. [DOI] [PMC free article] [PubMed]
- 5.Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73:202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 6.Holmes KK, Bertozzi S, Bloom BR, Jha P. Disease Control Priorities, Third Edition: Major Infectious Diseases. World Bank Publications; 2017:6. [PubMed]
- 7.Lazarus JV, Mark HE, Anstee QM, Arab JP, Batterham RL, Castera L, et al. Advancing the global public health agenda for NAFLD: a consensus statement. Nat Rev Gastroenterol Hepatol. 2021. Available from: 10.1038/s41575-021-00523-4 [DOI] [PubMed]
- 8.Yeoman AD. Novel Approaches to Detect Significant Liver Disease in the General Population. Clin Liver Dis. 2021;18:99–103. doi: 10.1002/cld.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Noncommunicable diseases country profiles 2018. World Health Organization. 2018.
- 10.GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. [DOI] [PMC free article] [PubMed]
- 11.Gómez Dantés H, Castro MV, Franco-Marina F, Bedregal P, Rodríguez García J, Espinoza A, et al. Burden of disease in Latin America. Salud Publica Mex. 2011;53(Suppl 2):s72–s77. [PubMed] [Google Scholar]
- 12.Díaz LA, Idalsoaga F, Fuentes-López E, Márquez-Lomas A, Ramírez CA, Roblero JP, et al. Impact of public health policies on alcohol-associated liver disease in Latin America: An ecological multi-national study. Hepatology. 2021. Available from: 10.1002/hep.32016 [DOI] [PubMed]
- 13.GBD 2017 Cirrhosis Collaborators. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5:245–266. [DOI] [PMC free article] [PubMed]
- 14.Arab JP, Roblero JP, Altamirano J, Bessone F, Chaves Araujo R, Higuera-De la Tijera F, et al. Alcohol-related liver disease: Clinical practice guidelines by the Latin American Association for the Study of the Liver (ALEH). Ann Hepatol. 2019;18:518–535. [DOI] [PubMed]
- 15.Arab JP, Díaz LA, Baeza N, Idalsoaga F, Fuentes-López E, Arnold J, et al. Identification of optimal therapeutic window for steroid use in severe alcohol-associated hepatitis: A worldwide study. J Hepatol. 2021;75:1026–1033. doi: 10.1016/j.jhep.2021.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meza V, Arnold J, Díaz LA, Ayala Valverde M, Idalsoaga F, Ayares G, et al. Alcohol Consumption: Medical Implications, the Liver and Beyond. Alcohol Alcohol. 2022. Available from: 10.1093/alcalc/agac013 [DOI] [PubMed]
- 17.World Health Organization. Global Status Report on Alcohol and Health 2018. World Health Organization. 2019.
- 18.Arab JP, Bataller R, Roblero JP. Are We Really Taking Care of Alcohol-Related Liver Disease in Latin America? Clin Liver Dis. 2020;16:91–95. doi: 10.1002/cld.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manthey J, Shield KD, Rylett M, Hasan OSM, Probst C, Rehm J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: a modelling study. Lancet. 2019;393:2493–2502. doi: 10.1016/S0140-6736(18)32744-2. [DOI] [PubMed] [Google Scholar]
- 20.Younossi Z, Tacke F, Arrese M, Chander Sharma B, Mostafa I, Bugianesi E, et al. Global Perspectives on Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis. Hepatology. 2019;69:2672–2682. doi: 10.1002/hep.30251. [DOI] [PubMed] [Google Scholar]
- 21.Pinto Marques Souza de Oliveira C, Pinchemel Cotrim H, Arrese M. Nonalcoholic Fatty Liver Disease Risk Factors in Latin American Populations: Current Scenario and Perspectives. Clin Liver Dis. 2019;13:39–42. [DOI] [PMC free article] [PubMed]
- 22.López-Velázquez JA, Silva-Vidal KV, Ponciano-Rodríguez G, Chávez-Tapia NC, Arrese M, Uribe M, et al. The prevalence of nonalcoholic fatty liver disease in the Americas. Ann Hepatol. 2014;13:166–178. doi: 10.1016/S1665-2681(19)30879-8. [DOI] [PubMed] [Google Scholar]
- 23.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gallardo-Rincón H, Cantoral A, Arrieta A, Espinal C, Magnus MH, Palacios C, et al. Review: Type 2 diabetes in Latin America and the Caribbean: Regional and country comparison on prevalence, trends, costs and expanded prevention. Prim Care Diabetes. 2021;15:352–359. doi: 10.1016/j.pcd.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 25.Alvarado-Mora MV, Rebello Pinho JR. Epidemiological update of hepatitis B, C and delta in Latin America. Antivir Ther. 2013;18. Available from: 10.3851/imp2595 [DOI] [PubMed]
- 26.Te HS, Jensen DM. Epidemiology of hepatitis B and C viruses: a global overview. Clin Liver Dis. 2010;14(1–21):vii. doi: 10.1016/j.cld.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 27.Tanaka J. Hepatitis A shifting epidemiology in Latin America. Vaccine. 2000;18(Suppl 1):S57–60. doi: 10.1016/S0264-410X(99)00466-1. [DOI] [PubMed] [Google Scholar]
- 28.Szabo SM, Bibby M, Yuan Y, Donato BMK, Jiménez-Mendez R, Castañeda-Hernández G, et al. The epidemiologic burden of hepatitis C virus infection in Latin America. Ann Hepatol. 2012;11:623–635. doi: 10.1016/S1665-2681(19)31435-8. [DOI] [PubMed] [Google Scholar]
- 29.Kershenobich D, Razavi HA, Sánchez-Avila JF, Bessone F, Coelho HS, Dagher L, et al. Trends and projections of hepatitis C virus epidemiology in Latin America. Liver Int. 2011;31(Suppl 2):18–29. doi: 10.1111/j.1478-3231.2011.02538.x. [DOI] [PubMed] [Google Scholar]
- 30.Lavanchy D. Evolving epidemiology of hepatitis C virus. Clin Microbiol Infect. 2011;17:107–115. doi: 10.1111/j.1469-0691.2010.03432.x. [DOI] [PubMed] [Google Scholar]
- 31.Bensabath G, Hadler SC, Soares MC, Fields H, Dias LB, Popper H, et al. Hepatitis delta virus infection and Labrea hepatitis. Prevalence and role in fulminant hepatitis in the Amazon Basin. JAMA. 1987;258:479–483. [DOI] [PubMed]
- 32.da Fonseca JCF. Hepatitis D. Rev Soc Bras Med Trop. 2002;35:181–190. doi: 10.1590/S0037-86822002000200009. [DOI] [PubMed] [Google Scholar]
- 33.Scarponi CF de O, Silva RDN da, Souza Filho JA de, Guerra MRL, Pedrosa MAF, Mol MPG. Hepatitis Delta Prevalence in South America: A Systematic Review and Meta-Analysis. Rev Soc Bras Med Trop. 2019;52:e20180289. [DOI] [PubMed]
- 34.Díaz LA, Norero B, Lara B, Robles C, Elgueta S, Humeres R, et al. Prioritization for liver transplantation using the MELD score in Chile: Inequities generated by MELD exceptions.: A collaboration between the Chilean Liver Transplant Programs, the Public Health Institute and the National Transplant Coordinator. Ann Hepatol. 2019;18:325–330. [DOI] [PubMed]
- 35.Padilla M, Mayorga R, Carrasco F, Bedregal T, Bobadilla F, Rondón C, et al. Liver transplantation for autoimmune hepatitis in Peru: outcomes and recurrence. Ann Hepatol. 2012;11:222–227. doi: 10.1016/S1665-2681(19)31027-0. [DOI] [PubMed] [Google Scholar]
- 36.Mendizabal M, Tagliafichi V, Rubinstein F, Rojas P, Marciano S, Yantorno S, et al. Liver transplantation in adults with acute liver failure: Outcomes from the Argentinean Transplant Registry. Ann Hepatol. 2019;18:338–344. doi: 10.1016/j.aohep.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 37.Sookoian S, Pirola CJ. Meta-analysis of the influence of I148M variant of patatin-like phospholipase domain containing 3 gene (PNPLA3) on the susceptibility and histological severity of nonalcoholic fatty liver disease. Hepatology. 2011;53:1883–1894. doi: 10.1002/hep.24283. [DOI] [PubMed] [Google Scholar]
- 38.Pontoriero AC, Trinks J, Hulaniuk ML, Caputo M, Fortuny L, Pratx LB, et al. Influence of ethnicity on the distribution of genetic polymorphisms associated with risk of chronic liver disease in South American populations. BMC Genet. 2015;16:93. doi: 10.1186/s12863-015-0255-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arrese M, Arab JP, Riquelme A, Benítez CE, Barrera F, Soza A, et al. High prevalence of PNPLA3 rs738409 (I148M) polymorphism in Chilean latino population and its association to non-alcoholic fatty liver disease risk and histological disease severity. 2015;Available from: http://repositorio.uchile.cl/handle/2250/137175
- 40.García-Bañuelos J, Panduro A, Gordillo-Bastidas D, Gordillo-Bastidas E, Muñoz-Valle JF, Gurrola-Díaz CM, et al. Genetic polymorphisms of genes coding to alcohol-metabolizing enzymes in western Mexicans: association of CYP2E1*c2/CYP2E1*5B allele with cirrhosis and liver function. Alcohol Clin Exp Res. 2012;36:425–431. doi: 10.1111/j.1530-0277.2011.01617.x. [DOI] [PubMed] [Google Scholar]
- 41.Roman S, Zepeda-Carrillo EA, Moreno-Luna LE, Panduro A. Alcoholism and liver disease in Mexico: genetic and environmental factors. World J Gastroenterol. 2013;19:7972–7982. doi: 10.3748/wjg.v19.i44.7972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carrion AF, Ghanta R, Carrasquillo O, Martin P. Chronic liver disease in the Hispanic population of the United States. Clin Gastroenterol Hepatol. 2011;9:834–41; quiz e109–10. [DOI] [PMC free article] [PubMed]
- 43.Levy R, Catana AM, Durbin-Johnson B, Halsted CH, Medici V. Ethnic differences in presentation and severity of alcoholic liver disease. Alcohol Clin Exp Res. 2015;39:566–574. doi: 10.1111/acer.12660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stickel F, Buch S, Lau K, Meyer zu Schwabedissen H, Berg T, Ridinger M, et al. Genetic variation in the PNPLA3 gene is associated with alcoholic liver injury in caucasians. Hepatology. 2011;53:86–95. [DOI] [PubMed]
- 45.Trépo E, Gustot T, Degré D, Lemmers A, Verset L, Demetter P, et al. Common polymorphism in the PNPLA3/adiponutrin gene confers higher risk of cirrhosis and liver damage in alcoholic liver disease. J Hepatol. 2011;55:906–912. doi: 10.1016/j.jhep.2011.01.028. [DOI] [PubMed] [Google Scholar]
- 46.Chamorro A-J, Torres J-L, Mirón-Canelo J-A, González-Sarmiento R, Laso F-J, Marcos M. Systematic review with meta-analysis: the I148M variant of patatin-like phospholipase domain-containing 3 gene (PNPLA3) is significantly associated with alcoholic liver cirrhosis. Aliment Pharmacol Ther. 2014;40:571–581. doi: 10.1111/apt.12890. [DOI] [PubMed] [Google Scholar]
- 47.Buch S, Stickel F, Trépo E, Way M, Herrmann A, Nischalke HD, et al. A genome-wide association study confirms PNPLA3 and identifies TM6SF2 and MBOAT7 as risk loci for alcohol-related cirrhosis. Nat Genet. 2015;47:1443–1448. doi: 10.1038/ng.3417. [DOI] [PubMed] [Google Scholar]
- 48.Tang S, Zhang J, Mei T-T, Guo H-Q, Wei X-H, Zhang W-Y, et al. Association of TM6SF2 rs58542926 T/C gene polymorphism with hepatocellular carcinoma: a meta-analysis. BMC Cancer. 2019;19:1128. doi: 10.1186/s12885-019-6173-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stickel F, Buch S, Nischalke HD, Weiss KH, Gotthardt D, Fischer J, et al. Genetic variants in PNPLA3 and TM6SF2 predispose to the development of hepatocellular carcinoma in individuals with alcohol-related cirrhosis. Am J Gastroenterol. 2018;113:1475–1483. doi: 10.1038/s41395-018-0041-8. [DOI] [PubMed] [Google Scholar]
- 50.Krawczyk M, Rau M, Schattenberg JM, Bantel H, Pathil A, Demir M, et al. Combined effects of the PNPLA3 rs738409, TM6SF2 rs58542926, and MBOAT7 rs641738 variants on NAFLD severity: a multicenter biopsy-based study. J Lipid Res. 2017;58:247–255. doi: 10.1194/jlr.P067454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Arab JP, Díaz LA, Dirchwolf M, Mark H, Lazarus JV, Vaughan E, et al. NAFLD: Challenges and opportunities to address the public health challenge in Latin America. Ann Hepatol. 2021;24:100359. doi: 10.1016/j.aohep.2021.100359. [DOI] [PubMed] [Google Scholar]
- 52.Halpern B, Louzada ML da C, Aschner P, Gerchman F, Brajkovich I, Faria-Neto JR, et al. Obesity and COVID-19 in Latin America: A tragedy of two pandemics-Official document of the Latin American Federation of Obesity Societies. Obes Rev. 2021;22:e13165. [DOI] [PMC free article] [PubMed]
- 53.Cominato L, Di Biagio GF, Lellis D, Franco RR, Mancini MC, de Melo ME. Obesity Prevention: Strategies and Challenges in Latin America. Curr Obes Rep. 2018;7:97–104. doi: 10.1007/s13679-018-0311-1. [DOI] [PubMed] [Google Scholar]
- 54.Cuevas A, Alvarez V, Carrasco F. Epidemic of metabolic syndrome in Latin America. Curr Opin Endocrinol Diabetes Obes. 2011;18:134–138. doi: 10.1097/MED.0b013e3283449167. [DOI] [PubMed] [Google Scholar]
- 55.Márquez-Sandoval F, Macedo-Ojeda G, Viramontes-Hörner D, FernándezBallart JD, Salas Salvadó J, Vizmanos B. The prevalence of metabolic syndrome in Latin America: a systematic review. Public Health Nutr. 2011;14:1702–1713. doi: 10.1017/S1368980010003320. [DOI] [PubMed] [Google Scholar]
- 56.Escobedo J, Schargrodsky H, Champagne B, Silva H, Boissonnet CP, Vinueza R, et al. Prevalence of the metabolic syndrome in Latin America and its association with sub-clinical carotid atherosclerosis: the CARMELA cross sectional study. Cardiovasc Diabetol. 2009;8:52. doi: 10.1186/1475-2840-8-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6:e1077–e1086. doi: 10.1016/S2214-109X(18)30357-7. [DOI] [PubMed] [Google Scholar]
- 58.Aguilar-Farias N, Martino-Fuentealba P, Carcamo-Oyarzun J, Cortinez-O’Ryan A, Cristi-Montero C, Von Oetinger A, et al. A regional vision of physical activity, sedentary behaviour and physical education in adolescents from Latin America and the Caribbean: results from 26 countries. Int J Epidemiol. 2018;47:976–986. [DOI] [PubMed]
- 59.The Global Burden of Disease: Generating Evidence, Guiding Policy – Latin America and Caribbean Regional Edition. Institute for Health Metrics and Evaluation. 2014. Cited 2022 Feb 20. Available from: https://www.healthdata.org/policy-report/global-burden-disease-generating-evidence-guiding-policy-%E2%80%93-latin-america-and-caribbean
- 60.Díaz LA, Roblero JP, Bataller R, Arab JP. Alcohol-Related Liver Disease in Latin America: Local Solutions for a Global Problem. Clin Liver Dis. 2020;16:187–190. doi: 10.1002/cld.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 62.Piñero F, Pages J, Marciano S, Fernández N, Silva J, Anders M, et al. Fatty liver disease, an emerging etiology of hepatocellular carcinoma in Argentina. World J Hepatol. 2018;10:41–50. doi: 10.4254/wjh.v10.i1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Piñero F, Poniachik J, Ridruejo E, Silva M. Hepatocellular carcinoma in Latin America: Diagnosis and treatment challenges. World J Gastroenterol. 2018;24:4224–4229. doi: 10.3748/wjg.v24.i37.4224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Valery PC, Laversanne M, Clark PJ, Petrick JL, McGlynn KA, Bray F. Projections of primary liver cancer to 2030 in 30 countries worldwide. Hepatology. 2018;67:600–611. doi: 10.1002/hep.29498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Santos G, Figueira ERR, D’Albuquerque LAC, Lisboa PB, de Almeida MD, Filgueira NA, et al. Evaluation of drug-induced liver injury as etiology for acute liver failure in Brazil. Ann Hepatol. 2021;23:100310. doi: 10.1016/j.aohep.2021.100310. [DOI] [PubMed] [Google Scholar]
- 66.Idalsoaga F, Valenzuela F, Díaz Luis A, Manzur F, Meza V, Sotomayor J, et al. O-7 Prevalence, characterization and survival of acute-on-chronic liver failure in A Chilean University Hospital. Ann Hepatol. 2021;24:100494. doi: 10.1016/j.aohep.2021.100494. [DOI] [Google Scholar]
- 67.Programme UND, United Nations Development Programme. Human Development Report 2019. Human Dev Re. 2019;Available from: 10.18356/838f78fd-en
- 68.Atun R, de Andrade LOM, Almeida G, Cotlear D, Dmytraczenko T, Frenz P, et al. Health-system reform and universal health coverage in Latin America. Lancet. 2015;385:1230–1247. doi: 10.1016/S0140-6736(14)61646-9. [DOI] [PubMed] [Google Scholar]
- 69.Andrade LOM de, de Andrade LOM, Filho AP, Solar O, Rígoli F, de Salazar LM, et al. Social determinants of health, universal health coverage, and sustainable development: case studies from Latin American countries. The Lancet. 2015;385:1343–1351. Available from: 10.1016/s0140-6736(14)61494-x [DOI] [PubMed]
- 70.Organisation for Economic Co-operation and Development, World Health Organization. Health at a glance: Latin America and the Caribbean 2020. Paris Cedex, France: Organization for Economic Co-operation and Development (OECD); 2020.
- 71.Ruano AL, Rodríguez D, Rossi PG, Maceira D. Understanding inequities in health and health systems in Latin America and the Caribbean: a thematic series. Int J Equity Health. 2021;20:94. doi: 10.1186/s12939-021-01426-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Báscolo E, Houghton N, Del Riego A. Types of health systems reforms in Latin America and results in health access and coverageLógica da transformação dos sistemas de saúde na América Latina e resultados no acesso e cobertura de saúde. Rev Panam Salud Publica. 2018;42:e126. doi: 10.26633/RPSP.2018.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gilardino RE, Valanzasca P, Rifkin SB. Has Latin America achieved universal health coverage yet? Lessons from four countries. Arch Public Health. 2022;80:38. doi: 10.1186/s13690-022-00793-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vorobioff JD, Contreras F, Tanno F, Hernández L, Bessone F, Colombato L, et al. A Latin American survey on demographic aspects of hospitalized, decompensated cirrhotic patients and the resources for their management. Ann Hepatol. 2020;19:396–403. doi: 10.1016/j.aohep.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 75.Roman S. Occult Hepatitis B and Other Unexplored Risk Factors for Hepatocellular Carcinoma in Latin America. Ann Hepatol. 2018;17:541–543. doi: 10.5604/01.3001.0012.0914. [DOI] [PubMed] [Google Scholar]
- 76.de Guevara LL, Dagher L, Arruda VM, Nakajima K, Kudo M. Sorafenib treatment by Child-Pugh score in Latin American patients with hepatocellular carcinoma. Future Oncol. 2020;16:2511–2520. doi: 10.2217/fon-2020-0323. [DOI] [PubMed] [Google Scholar]
- 77.Moye-Holz D, Vogler S. Comparison of Prices and Affordability of Cancer Medicines in 16 Countries in Europe and Latin America. Appl Health Econ Health Policy. 2022;20:67–77. doi: 10.1007/s40258-021-00670-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ruiz R, Strasser-Weippl K, Touya D, Herrero Vincent C, Hernandez-Blanquisett A, St Louis J, et al. Improving access to high-cost cancer drugs in Latin America: Much to be done. Cancer. 2017;123:1313–1323. doi: 10.1002/cncr.30549. [DOI] [PubMed] [Google Scholar]
- 79.Feier F, Antunes E, D’Agostino D, Varela-Fascinetto G, Jarufe N, Patillo JC, et al. Pediatric liver transplantation in Latin America: Where do we stand? Pediatr Transplant. 2016;20:408–416. doi: 10.1111/petr.12679. [DOI] [PubMed] [Google Scholar]
- 80.Mantilla Cruzatti O, Chaman Ortiz JC, Rondon Leyva CF, Padilla Machaca M, Rivera Romani J, Cardenas RB. Liver transplant and hepatocellular carcinoma in Peru: outcome after 15 years in the transplant department of the Guillermo Almenara Hospital - EsSalud. Rev Gastroenterol Peru. 2018;38:234–241. [PubMed] [Google Scholar]
- 81.Piñero F, TisiBaña M, de Ataide EC, Hoyos Duque S, Marciano S, Varón A, et al. Liver transplantation for hepatocellular carcinoma: evaluation of the alpha-fetoprotein model in a multicenter cohort from Latin America. Liver Int. 2016;36:1657–1667. doi: 10.1111/liv.13159. [DOI] [PubMed] [Google Scholar]
- 82.Arab JP, Dirchwolf M, Álvares-da-Silva MR, Barrera F, Benítez C, Castellanos-Fernandez M, et al. Latin American Association for the study of the liver (ALEH) practice guidance for the diagnosis and treatment of non-alcoholic fatty liver disease. Ann Hepatol. 2020;19:674–690. doi: 10.1016/j.aohep.2020.09.006. [DOI] [PubMed] [Google Scholar]
- 83.Piñero F, Costa P, Boteon YL, Duque SH, Marciano S, Anders M, et al. A changing etiologic scenario in liver transplantation for hepatocellular carcinoma in a multicenter cohort study from Latin America. Clin Res Hepatol Gastroenterol. 2018;42:443–452. doi: 10.1016/j.clinre.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 84.Gómez MP, Irazábal MM, Jr, Manyalich M. INTERNATIONAL REGISTRY IN ORGAN DONATION AND TRANSPLANTATION (IRODAT)–2019 WORLDWIDE DATA. Transplantation. 2020;104:S272. doi: 10.1097/01.tp.0000699864.69759.d7. [DOI] [Google Scholar]
- 85.Contreras AG, McCormack L, Andraus W, de Souza M Fernandes E, Latin America Liver Transplantation Group. Current status of liver transplantation in Latin America. Int. J. Surg. 2020;82S:14–21. [DOI] [PubMed]
- 86.Díaz LA, López M, Sin P, Wolff R, González G, Muñoz MP, et al. [Current situation of pediatric liver transplantation in Chile. Inequities associated with the MELD/PELD prioritization system]. Rev Med Chil. 2020;148:1261–1270. [DOI] [PubMed]
- 87.McCormack L, Gadano A, Lendoire J, Imventarza O, Andriani O, Gil O, et al. Model for end-stage liver disease-based allocation system for liver transplantation in Argentina: does it work outside the United States? HPB. 2010;12:456–464. doi: 10.1111/j.1477-2574.2010.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Salinas Nova M-A, Rojas Meneses Á, Restrepo Gutierrez J-C. Liver Transplant in Colombia. Liver Transpl. 2019;25:658–663. doi: 10.1002/lt.25427. [DOI] [PubMed] [Google Scholar]
- 89.Siegel JT, Alvaro EM, Hohman ZP, Maurer D. “Can you spare an organ?”: exploring Hispanic Americans’ willingness to discuss living organ donation with loved ones. Health Commun. 2011;26:754–764. doi: 10.1080/10410236.2011.566831. [DOI] [PubMed] [Google Scholar]
- 90.Mokdad AA, Lopez AD, Shahraz S, Lozano R, Mokdad AH, Stanaway J, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 2014;12:145. doi: 10.1186/s12916-014-0145-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Purcell LN, Charles AG. An invited commentary on “Status of liver transplantation in Latin America” - Current status of liver transplantation in Latin America: Cost, culture and consequences. Int J Surg. 2020;78:85. doi: 10.1016/j.ijsu.2020.04.045. [DOI] [PubMed] [Google Scholar]
- 92.Curioso WH. Building capacity and training for digital health: Challenges and opportunities in Latin America. J Med Internet Res. 2019;21:e16513. doi: 10.2196/16513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fassio E, Díaz S, Santa C, Reig ME, Martínez Artola Y, Alves de Mattos A, et al. Etiology of hepatocellular carcinoma in Latin America: a prospective, multicenter, international study. Ann Hepatol. 2010;9:63–69. [PubMed]
- 94.Gashin L, Tapper E, Babalola A, Lai K-C, Miksad R, Malik R, et al. Determinants and outcomes of adherence to recommendations from a multidisciplinary tumour conference for hepatocellular carcinoma. HPB. 2014;16:1009–1015. doi: 10.1111/hpb.12280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Viola L, Marciano S, Colombato L, Coelho H, Cheinquer H, Bugarin G, et al. HEPLA: A multicenter study on demographic and disease characteristics of patients with hepatitis C in Latin America. Ann Hepatol. 2020;19:161–165. doi: 10.1016/j.aohep.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 96.Ayares G, Idalsoaga F, Díaz LA, Arnold J, Arab JP. Current Medical Treatment for Alcohol-Associated Liver Disease. J Clin Exp Hepatol. 2022. Available from: https://www.sciencedirect.com/science/article/pii/S0973688322000226 [DOI] [PMC free article] [PubMed]
- 97.Roblero JP, Díaz LA, Arab JP, Roblero P, Bataller R. Socioeconomic inequalities in the incidence of alcohol-related liver disease in the Latin American context. Lancet Reg Health Eur. 2021;10:100229. doi: 10.1016/j.lanepe.2021.100229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Díaz LA, Fuentes-López E, Ayares G, Idalsoaga F, Arnold J, Márquez-Lomas A, et al. The establishment of public health policies and the burden of non-alcoholic fatty liver disease in the Americas. Lancet Gastroenterol Hepatol. 2022 [Accepted] [DOI] [PubMed]
- 99.Andraus W. Barriers and Limitations to Access to Liver Transplantation in Latin America. Clin Liver Dis. 2019;13:36–38. doi: 10.1002/cld.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Roblero JP, Arab JP, Mezzano G, Mendizabal M. Hepatitis C Virus Infection: What Are We Currently Doing in Latin America About WHO’s Proposals for 2030? Clin Liver Dis. 2021;18:72–75. doi: 10.1002/cld.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.FitzSimons D, Hendrickx G, Hallauer J, Larson H, Lavanchy D, Lodewyckx I, et al. Innovative sources for funding of viral hepatitis prevention and treatment in low- and middle-income countries: a roundtable meeting report. Hepatol Med Policy. 2016;1:16. doi: 10.1186/s41124-016-0022-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Mendizabal M, Silva MO. Developing multicenter consortia in liver disease in Latin America: Challenges and opportunities. Liver Transpl. 2017;23:1210–1215. doi: 10.1002/lt.24793. [DOI] [PubMed] [Google Scholar]