Abstract
Background/Setting:
In San Francisco, HIV viral suppression is 71% among housed individuals, but only 20% among unhoused individuals. We conducted a discrete choice experiment (DCE) at a San Francisco public HIV clinic to evaluate care preferences among people living with HIV (PLH) experiencing homelessness/unstable housing during the COVID-19 pandemic.
Methods:
From July-November 2020, we conducted a DCE among PLH experiencing homelessness/unstable housing who accessed care through a) an incentivized, drop-in program (“POP-UP”) or b) traditional primary care. We investigated five program features: single provider vs team of providers; visit incentives ($0, $10, $20); location (current site vs current+additional site); drop-in vs scheduled visits; in-person only vs optional telehealth visits; and navigator assistance. We estimated relative preferences using mixed-effects logistic regression and conducted latent class analysis to evaluate preference heterogeneity.
Results:
We enrolled 115 PLH experiencing homelessness/unstable housing, 40% of whom lived outdoors. The strongest preferences were for the same provider (β=0.94, 95%CI 0.48–1.41), visit incentives (β=0.56 per $5; 95%CI 0.47–0.66), and drop-in visits (β=0.47, 95%CI 0.12–0.82). Telehealth was not preferred. Latent class analysis revealed two distinct groups: 78 (68%) preferred a flexible care model; while 37 (32%) preferred a single provider.
Conclusion:
We identified heterogeneous care preferences among PLH experiencing homelessness/unstable housing during the COVID pandemic, with two-thirds preferring greater flexibility and one-third preferring provider continuity. Telehealth was not preferred, even with navigator facilitation. Including patient choice in service delivery design can improve care engagement, particularly for marginalized populations, and is an essential tool for ending the HIV epidemic.
Keywords: HIV, Homeless Persons, Care Engagement, Discrete Choice Experiment, COVID-19, Patient Preference
Introduction
People with HIV experiencing homelessness or unstable housing (PWH-HUH) face individual and structural barriers to care and have lower rates of viral suppression compared to those who are housed.1 Only 20% of PWH in San Francisco experiencing homelessness were virally suppressed in 2020, compared to 71% of those who were housed.2 Innovative care models are needed to address the unique care needs and improve viral suppression of this vulnerable population.1,3,4
Understanding patient preferences is important for designing effective models of care, especially for vulnerable populations. We previously conducted a discrete choice experiment (DCE) that demonstrated PWH-HUH strongly preferred having a personal relationship with and drop-in access to their care team.5 These findings informed the POP-UP program at Ward 86, a public HIV clinic in San Francisco, which provides drop-in, incentivized comprehensive HIV primary care and has demonstrated success in improving care engagement and viral suppression among PWH-HUH.3
During the COVID-19 pandemic, PWH-HUH have faced compounding medical and socioeconomic challenges.6 Public health ordinances lowered capacity for in-person medical and behavioral health services while accelerating telehealth adoption.7–9 In addition, the pandemic impacted access to housing10 and harm reduction resources for substance use.11,12 Patients also reported difficulties engaging with telehealth.13–15 At Ward 86, PWH-HUH who engage with traditional primary care had a higher odds of unsuppressed viral loads after as compared to before the city’s COVID-related shelter-in-place ordinance in March 2020.16
By identifying patient preferences for characteristics of healthcare that are most desirable, DCEs can facilitate design of more patient-centered healthcare services, ultimately translating to greater engagement.17–19 Our prior DCE was conducted before COVID-19. We conducted a new DCE to evaluate preferences for HIV primary care engagement for PWH-HUH during the COVID-19 pandemic, with specific interest in understanding preferences for increased flexibility of care, including telehealth and interventions to facilitate telehealth for patients without phones. Patients with marginal housing were particularly affected by shelter-in-place orders, making this new DCE critical to understanding unique barriers faced by marginalized patient populations during COVID-19 and ensuring that the “patient voice” is front and center in healthcare design.
Methods
Study setting and population
The DCE was conducted between July and November 2020 at Ward 86 where approximately a third of patients experience homelessness or unstable housing.20 Homelessness or unstable housing is defined as living outdoors, in a shelter, couch-surfing, or temporary housing. Patients were eligible for this study if they were PWH experiencing homelessness/unstable housing and were either in the POP-UP program or participated in traditional primary care at Ward 86. Ward 86 patients are eligible for the POP-UP program if they meet the following criteria on enrollment: 1) current unsuppressed HIV RNA (≥200 copies/mL) or reported discontinuation of ART for ≥1 month; 2) currently homeless or unstably housed; 3) missed ≥1 primary care visit in the past 12 months; 4) ≥2 Ward 86 drop in visits in the past 12 months. In order to compare the two groups, patients in traditional primary care had to have an unsuppressed viral load or report being off antiretroviral therapy (ART) for >1 month in the prior 12 months.
We recruited patients during routine clinic visits and during outreach visits to shelter-in-place hotels, which were set up by the city in April 2020 to provide temporary housing for people experiencing homelessness who are at increased risk for severe COVID-19 disease.21 Those expressing interest in the DCE met with research staff in a private location at Ward 86, or at their shelter-in-place hotel. Patients were excluded from study participation if not fluent in English or Spanish. Housing status and ART adherence were collected via self-report and HIV viral loads were assessed via electronic chart review. Patients received a $20 grocery store gift card for their participation.
The University of California, San Francisco Institutional Review Board approved our study protocol. We obtained informed consent from each participant after explaining the possible risks and benefits of the study.
DCE attribute selection
We identified program features previously reported to increase HIV care engagement among people experiencing homelessness, care models encouraged by public health orders during COVID-19 (e.g. telehealth), and interventions for improving care flexibility. Though telehealth was adopted across many health systems during the pandemic, there were concerns that telehealth would not be accessible to many people experiencing homelessness/unstable housing,15 leading to worsening HIV viral suppression among this group.16 Given the growing reliance on telehealth during the pandemic, and the fact that patient preferences for telehealth among PWH-HUH are unknown, we evaluated preferences for in-person visits only, in-person visits with optional access to phone visits, and in-person visits with optional access to video visits. A systematic review identified that patient navigation may improve retention in care and viral suppression.22 To explore preferences for navigation and possible interactions with telehealth, we included navigator assistance among attributes. A previous DCE found that participants preferred having providers who “know them as a person.”5 To better understand preferences for provider continuity and trade-offs between this feature and other program features, we asked participants to select between single vs. group of providers, defined as seeing the “same provider” or a “small group of providers who work together for my care.” To evaluate preferences for flexibility in care location, we included the option of accessing care with the Ward 86 care team at a second site. The attribute included the current location of the POP-UP program (“a clinic visit with my team at Ward 86”) or the option to have “a clinic visit with my team at either Ward 86 or a location in the Tenderloin,” which is a neighborhood of San Francisco that has over 1,500 PWH23 and a high prevalence of homelessness.24 Finally, we included drop-in vs scheduled visits and incentives, which are known to be preferred among this population based on findings from a prior DCE,5 to understand trade-offs between these preferred attributes and other newly included attributes.
DCE design
The final DCE included six attributes, with 2–3 response levels per attribute. All response levels included pictorial examples to improve understanding and ease the cognitive task of comparing two clinics with multiple attributes (see Figure 1, Supplemental Digital Content 1). We presented respondents with 12 choice tasks to minimize cognitive and time burden and maximize design efficiency.25 Each choice task presented respondents with two clinic models that differed by one or more attribute. The respondent was then asked for their clinic preference: “Do you prefer Clinic A, Clinic B, or would you rather not go to either one?” The final DCE design was statistically efficient because it was balanced (each attribute level appears with the same frequency) and orthogonal (each pair of levels appeared with the same frequency across all pairs of attributes within the design).26 The DCE was translated into English and Spanish. We pilot tested the DCE design with five patients and based on this, we modified the size for readability and refined how we explained the survey to ensure comprehension.
Figure 1.
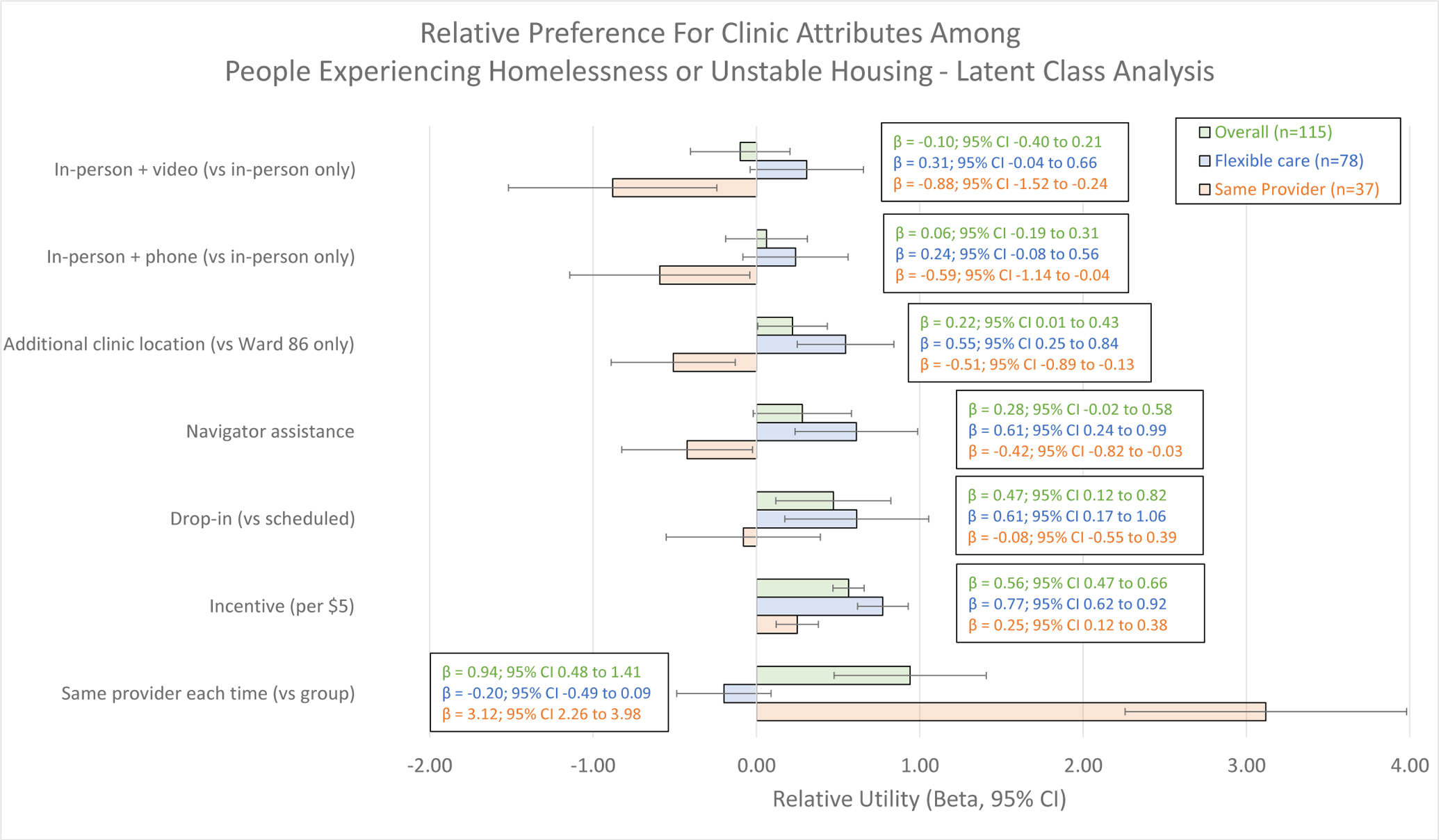
Relative preference for clinic features, by latent class grouping among individuals living with HIV and receiving care at the San Francisco public HIV clinic during the COVID-19 pandemic (N=115).
Sample size
We calculated a minimum required sample size of approximately 63 respondents per arm using the formula “n ≥ 500c/ta,” where ‘n’ is the number of participants, ‘t’ is the number of choice tasks, ‘a’ is the number of options per choice task, and ‘c’ is largest number of levels for any attribute.27
Data collection
We used electronic tablets to administer the DCE and a survey collecting information on demographics, technology use, and substance use. After locating a private setting and obtaining consent, research staff displayed the DCE attributes, explained each level, and confirmed understanding before proceeding to an example choice task. Research staff answered clarifying questions before starting the DCE, then read each clinic option aloud as they pointed to the corresponding picture for each attribute.
Analysis
We performed a mixed-effects logistic regression to estimate the relative preferences among attributes and their levels, which presents the relative mean preference weight and standard deviations in the sample.28 We conducted a latent class analysis to identify respondent groups with similar choice patterns and repeated the utility analysis stratified by latent class groupings. We selected two latent class groupings based on the small sample size in our study. We conducted Pearson’s chi-squared tests and Student’s t-test to investigate demographic differences between the two groups. Analyses were conducted in Stata Version 16; DCE analyses were conducted in Lighthouse Studio Version 9.6.1 (Sawtooth Software, Provo, Utah, USA).
Results
We screened 840 people, of whom 146 were eligible and 117 enrolled in this study (Supplemental Digital Content 2). We excluded two surveys due to incomplete data, resulting in 115 responses included in our analysis (Table 1). Of the 115, 59 were enrolled in POP-UP and 56 were in traditional primary care. The median age was 44 years, 78% identified as cisgender men, 11% identified as transgender women, 50% were White, 26% were Black, and 34% were Hispanic/Latino/a. Forty-six (40%) reported living outdoors in the 3 months prior to their survey date and the majority (54%) reported daily methamphetamine use. Three-quarters (76%) currently owned a phone and 56% reported having a phone lost or stolen in the prior 6 months.
Table 1.
Participant characteristics among individuals living with HIV and receiving care at the San Francisco public HIV clinic during the COVID-19 pandemic, by preference phenotype according to latent class group (N=115).
| Characteristic | Total Sample N = 115 n (%) |
Flexible Care n = 78 n (%) |
One Provider n = 37 n (%) |
P-value |
|---|---|---|---|---|
| Current Care Model | <0.01 | |||
| POP-UP | 59 (51%) | 49 (63%) | 10 (27%) | |
| Traditional Primary Care | 56 (49%) | 29 (37%) | 27 (73%) | |
| Recruitment Site | ||||
| Routine Clinic Visit | 106 (92%) | 74 (94%) | 32 (86%) | |
| Shelter-In-Place Outreach | 9 (8%) | 4 (6%) | 5 (14%) | |
| Age | 0.24 | |||
| Median [IQR] | 44 [35–53] | 41 [35–53] | 47 [40–51] | |
| Gender | 0.65 | |||
| Cisgender men | 90 (78%) | 60 (77%) | 30 (81%) | |
| Cisgender women | 7 (6%) | 6 (8%) | 1 (3%) | |
| Transgender women | 13 (11%) | 8 (10%) | 5 (14%) | |
| Nonbinary/Fluid | 5 (4%) | 4 (5%) | 1 (3%) | |
| Race | 0.68 | |||
| American Indian/Alaska Native | 6 (5%) | 3 (4%) | 3 (8%) | |
| Asian/Pacific Islander | 2 (2%) | 2 (2%) | 0 | |
| Black | 30 (26%) | 21 (27%) | 9 (24%) | |
| White | 58 (50%) | 41 (52%) | 16 (43%) | |
| Multi-Racial | 16 (14%) | 10 (13%) | 6 (16%) | |
| Other | 3 (2%) | 1 (1%) | 2 (5%) | |
| Ethnicity | <0.01 | |||
| Hispanic/Latino/a | 39 (34%) | 18 (23%) | 21 (57%) | |
| Not Hispanic/Latino/a | 76 (66%) | 60 (77%) | 16 (43%) | |
| Substance Use † | ||||
| Methamphetamines | 62 (54%) | 44 (56%) | 18 (50%) | 0.44 |
| Alcohol | 14 (12%) | 9 (12%) | 5 (14%) | 0.76 |
| Opioids | 10 (9%) | 6 (8%) | 4 (11%) | 0.58 |
| Cocaine | 3 (3%) | 2 (3%) | 1 (3%) | 0.97 |
| Housing Type ‡ | ||||
| Outdoors § | 46 (40%) | 37 (47%) | 9 (27%) | 0.02 |
| Shelter/emergency housing | 13 (11%) | 10 (13%) | 3 (8%) | 0.46 |
| Institution: rehab, jail, hospital | 29 (25%) | 21 (27%) | 8 (22%) | 0.54 |
| Couch-surfing | 32 (28%) | 23 (29%) | 9 (24%) | 0.56 |
| Temporary SRO | 61 (53%) | 42 (54%) | 19 (51%) | 0.80 |
| Long-term housing ¶ | 16 (14%) | 12 (15%) | 4 (11%) | 0.51 |
| Time Since Last Stable Housing | 0.21 | |||
| Less than 6 months | 9 (8%) | 4 (5%) | 5 (14%) | |
| Less than 12 months ago | 14 (12%) | 8 (10%) | 6 (16%) | |
| Within last 5 years | 45 (40%) | 29 (37%) | 16 (43%) | |
| Within last 10 years | 22 (19%) | 17 (22%) | 5 (14%) | |
| More than 10 years ago | 25 (22%) | 20 (26%) | 5 (14%) | |
| Phone Ownership | <0.01 | |||
| Yes | 88 (76%) | 53 (68%) | 35 (95%) | |
| No | 27 (24%) | 25 (32%) | 2 (5%) | |
| Phone Lost/Stolen in last 6 months | <0.01 | |||
| Yes | 64 (56%) | 51 (65%) | 13 (35%) | |
| Frequency: Median [IQR] | 2 [1–3] | 2 [1–3] | 1 [1–2] | 0.94 |
| No | 51 (44%) | 27 (35%) | 24 (65%) |
Able to select multiple substances. Defined as reporting daily or almost daily use. Chi-squared analysis conducted with each substance type between latent class groups.
Able to select multiple housing types. Defined as spending any time in the listed spaces during the last three months. Chi-squared analysis conducted with each housing type between latent class groups.
Defined as reporting being street homeless, living in a car/bus/van/RV, or a non-residential commercial space, storage unit, or abandoned building in the three months prior to survey.
Defined as a long-term SRO residence or rent/own an apartment.
Overall, the strongest preferences were for seeing the same provider at every clinic visit (β=0.94, 95% CI: 0.48–1.41), receiving financial incentives for clinic visits (β=0.56 per $5 increase; 95% CI: 0.47–0.66), and having the option for no appointment/drop-in visits (β=0.47, 95% CI: 0.12–0.82) (Figure 1). Added telephone visits (β = 0.06, 95% CI: −0.19–0.31) or video (telehealth) visits (β = −0.10, 95% CI: −0.40–0.21) were not preferred. There were no significant interactions observed between attributes.
Our latent class analysis revealed two subgroups with distinct preferences (Figure 1). Approximately two-thirds of respondents (n=78, 68%) preferred attribute levels which increased care flexibility, such as including an additional clinic location (β = 0.55, 95% CI: 0.25–0.84), having navigator assistance (β=0.61, 95% CI 0.24–0.99), and drop-in visits (β=0.61, 95% CI 0.17–1.06). The other one-third (n=37, 32%) of respondents preferred seeing the same provider every time (β=3.12, 95% CI 2.26–3.98). Both groups preferred clinic visit incentives (flexible care group β=0.77, 95% CI 0.62 to 0.92; single provider group β=0.25, 95% CI 0.12 to 0.38). The flexible care group had a higher proportion of people ages 25–39 (46% vs 22%), living outdoors (47% vs 27%), experiencing homelessness or unstable housing for >5 years (48% vs 28%), less current phone ownership (68% vs 95%), and greater phone turnover in the previous six months (65% vs 35%) (Table 1). Conversely, the single provider group had a higher proportion of people over the age of 40 (77% vs 52%) and who reported Hispanic/Latino/a ethnicity (57% vs 23%).
Discussion
People with HIV with marginal housing receiving care during the COVID-19 pandemic expressed heterogeneous clinic model preferences, with two-thirds preferring additional service flexibility in where to receive care and one-third preferring the same provider to provide care. These findings highlight the importance of eliciting patient preferences and incorporating care model flexibility to tailor to a range of preferences. This process allows for patient-centered care at all times, including during the pandemic.29,30
Patient preference evaluation is a powerful way to design more patient-centered health services. Among PLH experiencing homelessness or unstable housing in San Francisco, only 20% were virally suppressed at any point during 2020; therefore, current healthcare services are not meeting minimal HIV care needs for at least 80% of this population.2 Novel interventions are needed, yet different patients will need, and prefer, different types of services. Identifying preference heterogeneity offers an opportunity to optimize service offerings to maximize engagement with preferred services for the greatest number of patients – a concept others have termed ‘mosaic effectiveness’.31
Within the POP-UP care model, a low barrier care program established at Ward 86, we have applied these findings of desiring care at other sites by forming a partnership with the San Francisco HIV Homeless Outreach and Mobile Engagement (HHOME) program.32 This allows us to offer interested patients the option of accessing care at both Ward 86 and the HHOME care site with close coordination of care across teams. For patients who benefit from the POP-UP model of care but who prefer provider continuity, we now offer patient-provider cohorting within POP-UP and encourage patients to drop in on weekdays when their specific provider is in clinic. Because care models generally cannot accommodate both full provider continuity and full flexibility (drop in any day and at multiple sites), tailoring to patient preference by allowing people to choose the model that works best for them is critical to ensuring patient-centeredness and optimizing care engagement.
Heterogeneous preferences for trade-offs between flexibility, relationship-oriented care, and other aspects of care delivery also have relevance beyond HIV primary care. A recent qualitative study identified heterogeneous preferences for substance treatment services that are stand-alone vs integrated with primary health care among people with an opioid use disorder.33 Reasons for these preferences were diverse and included preferences for greater convenience and an individualized approach when receiving treatment from their primary care provider versus the value of anonymity and perceived greater quality of services from non-integrated treatment. Other studies have evaluated patient preferences and trade-offs regarding convenience versus depersonalization of telehealth services for cancer care.34 In these and other settings, soliciting patient preferences and offering choice between different service offerings is an important step toward building more patient-centered healthcare.35
Although previous studies conducted among people experiencing homelessness have found a range of technology access and use,13,14 there are no studies to date exploring the acceptability of telehealth among PWH-HUH. We found that the option of adding phone or video visits to available in-person care was not preferred, even when facilitated by a navigator to address technology access issues and during a respiratory virus pandemic. While there was a societal shift to telehealth during the pandemic, our findings highlight the importance of offering in-person visits for persons experiencing homelessness with chronic health conditions during the pandemic.
Our findings have limitations. First, DCEs only measure stated preferences and not actual behaviors; however, patient preferences as indicated in DCE’s predict health-related behaviors and uptake of preferred health services.18 Second, our findings are not representative of all PWH-HUH. Despite having the ability to administer the DCE in English and Spanish, we did not identify any eligible Spanish-speaking patients to enroll in our study. In addition, we only surveyed patients who presented to clinic or were contacted at shelter-in-place hotels during the pandemic. This may have biased our sample toward individuals with fewer barriers to receiving services. For example, the proportion of patients who prefer a flexible model (i.e., those who were younger, unstably housed and less likely to have a working phone) may be substantially higher than two-thirds, and effects may be even stronger than those reported here. Given our study was conducted during the COVID-19 pandemic, generalizability of our findings beyond this time may be limited.
Conclusions
Our findings highlight the importance of in-person incentivized care for PLH experiencing homelessness/unstable housing, with the option to choose between provider continuity and service flexibility during the COVID-19 pandemic. Service models for public HIV clinics that incorporate these care preferences during COVID-19 may improve care engagement and reduce the disparity in viral suppression for people living with HIV experiencing homelessness or unstable housing.
Supplementary Material
Supplemental Digital Content 1. Discrete choice experiment attributes and levels.pdf
Supplemental Digital Content 2. Recruitment flow diagram.pdf
Supplemental Digital Content 3. Additional participant characteristics.pdf
Acknowledgements
We would like to acknowledge the POP-UP team at Ward 86 including Jon Oskarsson, Mary Shiels, Helen Lin, Elizabeth Lynch, Jackelyn Kelley, Janet Grochowski, Yennifer Breganza-Lopez, Ayesha Appa, and John Friend.
Conflicts of Interest and Source of Funding
We have no conflict of interest, financial or otherwise, to disclose. The ‘Ward 86’ HIV program in the Division of HIV, ID and Global Medicine received an unrestricted investigator-initiated grant from the Gilead Foundation to support implementation and evaluation of the ‘POP-UP’ program, a clinical program for people with HIV experiencing homelessness or unstable housing (Grant # IN-US-985-5691). Gilead had no role in the interpretation or presentation of these results. This research was also supported by an Ending the HIV Epidemic Supplemental grant from the National Institutes of Health to the UCSF-Gladstone Center for AIDS Research P30 AI027763 (M.G.) and a U.S. National Institute of Allergy and Infectious Diseases (NIAID) training grant 5T32AI060530-13 (M.D.H.).
List of abbreviations
- ART
anti-retroviral therapy
- COVID-19
SARS-CoV-2 disease
- DCE
discrete choice experiment
- PWH-HUH
People living with HIV experiencing homelessness or unstable housing
References
- 1.Clemenzi-Allen AA, Hickey M, Conte M, et al. Improving Care Outcomes for PLWH Experiencing Homelessness and Unstable Housing: a Synthetic Review of Clinic-Based Strategies. Curr HIV/AIDS Rep. 2020;17(3):259–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Colfax G, Aragon T, Enanoria W, Hsu L. HIV Epidemiology: Annual Report, 2019. September 2020. 2020.
- 3.Imbert E, Hickey MD, Clemenzi-Allen A, et al. Evaluation of the POP-UP programme: a multicomponent model of care for people living with HIV with homelessness or unstable housing. AIDS. 2021;35(8):1241–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riley ED, Vittinghoff E, Koss CA, et al. Housing First: Unsuppressed Viral Load Among Women Living with HIV in San Francisco. AIDS and behavior. 2019;23(9):2326–2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Conte M, Eshun-Wilson I, Geng E, et al. Brief Report: Understanding Preferences for HIV Care Among Patients Experiencing Homelessness or Unstable Housing: A Discrete Choice Experiment. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2020;85(4):444–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okonkwo NE, Aguwa UT, Jang M, et al. COVID-19 and the US response: accelerating health inequities. BMJ evidence-based medicine. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colfax GN. Order of the Health Officer No. C19–07s (Directing All Individuals Living in the County to Stay Safer at Their Place of Residence) 2021.
- 8.Colfax GN. Order of the Health Officer No. C19–08s (Moratorium on Routine Medical Appointments and Elective Surgery, Encouraging Remote Appointments) 2020.
- 9.Bhaskar S, Bradley S, Chattu VK, et al. Telemedicine Across the Globe-Position Paper From the COVID-19 Pandemic Health System Resilience PROGRAM (REPROGRAM) International Consortium (Part 1). Front Public Health. 2020;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imbert E, Kinley PM, Scarborough A, et al. Coronavirus Disease 2019 Outbreak in a San Francisco Homeless Shelter. Clinical Infectious Diseases. 2020(ciaa1071). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peavy KM, Darnton J, Grekin P, et al. Rapid Implementation of Service Delivery Changes to Mitigate COVID-19 and Maintain Access to Methadone Among Persons with and at High-Risk for HIV in an Opioid Treatment Program. AIDS Behav. 2020:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glick SN, Prohaska SM, LaKosky PA, Juarez AM, Corcorran MA, Des Jarlais DC. The Impact of COVID-19 on Syringe Services Programs in the United States. AIDS Behav. 2020:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McInnes DK, Sawh L, Petrakis BA, et al. The Potential for Health-Related Uses of Mobile Phones and Internet with Homeless Veterans: Results from a Multisite Survey. Telemedicine and e-Health. 2014;20(9):801–809. [DOI] [PubMed] [Google Scholar]
- 14.Rhoades H, Wenzel SL, Rice E, Winetrobe H, Henwood B. No digital divide? Technology use among homeless adults. Journal of Social Distress and Homelessness. 2017;26(1):73–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hickey MD, Sergi F, Zhang K, et al. Pragmatic randomized trial of a pre-visit intervention to improve the quality of telemedicine visits for vulnerable patients living with HIV. Journal of Telemedicine and Telecare. 2020:1357633X20976036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spinelli MA, Hickey MD, Glidden DV, et al. Viral suppression rates in a safety-net HIV clinic in San Francisco destabilized during COVID-19. AIDS. 2020;34(15):2328–2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zanolini A, Sikombe K, Sikazwe I, et al. Understanding preferences for HIV care and treatment in Zambia: Evidence from a discrete choice experiment among patients who have been lost to follow-up. PLoS medicine. 2018;15(8):e1002636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quaife M, Terris-Prestholt F, Di Tanna GL, Vickerman P. How well do discrete choice experiments predict health choices? A systematic review and meta-analysis of external validity. Eur J Health Econ. 2018;19(8):1053–1066. [DOI] [PubMed] [Google Scholar]
- 19.de Bekker-Grob EW, Donkers B, Bliemer MCJ, Veldwijk J, Swait JD. Can healthcare choice be predicted using stated preference data? Soc Sci Med. 2020;246:112736. [DOI] [PubMed] [Google Scholar]
- 20.Clemenzi-Allen A, Geng E, Christopoulos K, et al. Degree of Housing Instability Shows Independent “Dose-Response” With Virologic Suppression Rates Among People Living With Human Immunodeficiency Virus. Open Forum Infectious Diseases. 2018;5(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.San Francisco’s COVID-19 Response [press release]. 2021.
- 22.Mizuno Y, Higa DH, Leighton CA, Roland KB, Deluca JB, Koenig LJ. Is HIV patient navigation associated with HIV care continuum outcomes? AIDS. 2018;32(17):2557–2571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Colfax GN, Enanoria W, Hsu L. HIV Epidemiology Annual Report. 2020.
- 24.Breed L San Francisco releases Tenderloin Neighborhood Safety Assessment and Plan for COVID-19 | San Francisco. 2020.
- 25.Bridges JFP, Hauber AB, Marshall D, et al. Conjoint analysis applications in health--a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–413. [DOI] [PubMed] [Google Scholar]
- 26.Reed Johnson F, Lancsar E, Marshall D, et al. Constructing Experimental Designs for Discrete-Choice Experiments: Report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value in Health. 2013;16(1):3–13. [DOI] [PubMed] [Google Scholar]
- 27.Orme BK. Getting Started with Conjoint Analysis: Strategies for Product Design and Pricing Research. 1st edition ed. Madison, Wis: Research Publishers, LLC; 2005. [Google Scholar]
- 28.Hauber AB, González JM, Groothuis-Oudshoorn CGM, et al. Statistical Methods for the Analysis of Discrete Choice Experiments: A Report of the ISPOR Conjoint Analysis Good Research Practices Task Force. Value Health. 2016;19(4):300–315. [DOI] [PubMed] [Google Scholar]
- 29.Jego M, Abcaya J, Ștefan D-E, Calvet-Montredon C, Gentile S. Improving Health Care Management in Primary Care for Homeless People: A Literature Review. International Journal of Environmental Research and Public Health. 2018;15(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kertesz SG, Holt CL, Steward JL, et al. Comparing Homeless Persons’ Care Experiences in Tailored Versus Nontailored Primary Care Programs. Am J Public Health. 2013;103(Suppl 2):S331–S339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glidden DV, Mehrotra ML, Dunn DT, Geng EH. Mosaic effectiveness: measuring the impact of novel PrEP methods. The lancet HIV. 2019;6(11):e800–e806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Borne D, Tryon J, Rajabiun S, Fox J, de Groot A, Gunhouse-Vigil K. Mobile Multidisciplinary HIV Medical Care for Hard-to-Reach Individuals Experiencing Homelessness in San Francisco. American Journal of Public Health. 2018;108(S7):S528–S530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saunders EC, Moore SK, Walsh O, et al. “It’s way more than just writing a prescription”: A qualitative study of preferences for integrated versus non-integrated treatment models among individuals with opioid use disorder. Addiction Science & Clinical Practice. 2021;16(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cox A, Lucas G, Marcu A, et al. Cancer Survivors’ Experience With Telehealth: A Systematic Review and Thematic Synthesis. Journal of Medical Internet Research. 2017;19(1):e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Medical care research and review: MCRR. 2013;70(4):351–379. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. Discrete choice experiment attributes and levels.pdf
Supplemental Digital Content 2. Recruitment flow diagram.pdf
Supplemental Digital Content 3. Additional participant characteristics.pdf


