Abstract
Purpose
No study has assessed the titration success of CPAP therapy in patients with obesity hypoventilation syndrome (OHS) and an apnea-hypopnea index (AHI) <30 event/h. This study aimed to assess the titration success of CPAP therapy under polysomnography and subsequent short-term adherence (1 month) in patients with OHS and an AHI <30 event/h.
Methods
Consecutive OHS patients with an AHI <30 events/h between 2010 and 2019 were included (n=54). All OHS patients were first started on CPAP during the therapeutic sleep-study. If the therapeutic-study showed that the SpO2 remained < 90% for 20% of the total sleep time, a second therapeutic study was arranged with bi-level PAP (BPAP). Thirty patients agreed to participate in the 1-month follow-up adherence study. We applied the American-Thoracic-Society criteria for PAP adherence.
Results
The mean age was 54.8±14.6 years, and the mean BMI was 45.9±12.2 kg/m2. Successful titration on CPAP was attained in 36 (66.7%) patients, and 18 (33.3%) required BPAP. Patients who failed the CPAP trial had a significantly higher PaCO2 and bicarbonate, a more restrictive respiratory pattern on spirometry, and a significantly higher time with SpO2<90% (mins) during sleep. The only independent correlate of CPAP-titration success on the multivariable regression analysis was the desaturation index (OR: 1.33 [1.033–1.712]). More than 80% of the participants were using CPAP therapy after one-month with no differences in adherence between the CPAP and BPAP groups.
Conclusions
The current results suggest that CPAP therapy could be an acceptable alternative therapy to BPAP in patients with OHS without severe OSA.
Keywords: CPAP, bi-level positive airway pressure, compliance, obstructive sleep apnea, desaturation, titration
Introduction
Obesity hypoventilation syndrome (OHS) is an under-recognized disorder characterized by obesity (BMI>30kg/m2) and awake hypercapnia (PaCO2>45mmHg) and is usually accompanied by obstructive sleep apnea (OSA).1 OHS patients have a higher risk of cardiovascular and respiratory morbidity and mortality than eucapnic obese individuals and OSA patients.2,3 Additionally, they have higher healthcare utilization.4 Two phenotypes of OHS have been described, OHS with severe OSA and OHS without severe OSA, with an apnea-hypopnea index (AHI) of <30 events/h.5 OSA occurs in approximately 90% of OHS patients, and severe OSA in 73% of OHS patients.6 The pure hypoventilation phenotype occurs in 10–15% of patients.7
Positive airway pressure (PAP) therapy is the mainstay treatment for OHS; it aims to stabilize breathing and gas exchange during sleep. In a recent Official American Thoracic Society (ATS) Clinical Practice Guideline, the ATS recommended for stable ambulatory patients with OHS and concurrent severe OSA (AHI ≥30 events/h) to start therapy with continuous PAP (CPAP) as the first-line treatment before noninvasive ventilation (NIV), as the difference in the outcomes between CPAP and NIV was nonsignificant.8 However, for OHS patients with an AHI<30 events/h, the ATS practice guideline suggested that NIV might provide more benefits than CPAP, acknowledging the lack of studies to compare the two treatment modalities in this group; and indicating that there is less certainty of the superiority of NIV in OHS patients without concomitant severe OSA.8 Additionally, the recommendation was conditional due to a very low level of certainty in the evidence.8 Moreover, the ATS report indicated that further studies assessing the impact of different PAP modes in patients with OHS with mild/moderate OSA are needed.8 Though CPAP does not augment minute and alveolar ventilation; it may help to unload CO2 collected during airway narrowing during sleep.9
We have reported the long-term adherence to PAP therapy in ambulatory OHS patients with severe OSA;10 however, in general, limited studies have assessed adherence to PAP therapy in patients with OHS,10–14 and none has been done to assess the titration success of CPAP therapy and subsequent adherence in patients with OHS and an AHI <30 event/h. Currently, there is a lack of certainty on the clinical benefits of initiating CPAP treatment in OHS patients without severe OSA.8 Whether CPAP therapy has a good therapeutic effect in OHS patients with mild-moderate OSA remains unclear.15 As OHS patients with AHI<30 events/h may still have a significant proportion of obstructive events, CPAP may still benefit some patients with OHS in this group. Due to cost, availability, and logistic reasons, the practice in our sleep disorders center has been to start all patients with OHS on CPAP first and then shift them to BPAP if the CPAP titration trial fails. In addition, the ATS practice guidelines indicated that there are moderate cost inferences related to the choice of PAP mode of therapy, with NIV therapy being considerably more costly than CPAP.8,16 Further, NIV may necessitate more titration, preparation, and training expertise.8 Consequently, these factors may defer the provision of NIV compared to CPAP, especially in regions where the expertise required for more difficult NIV devices is inadequate.8
We hypothesized that CPAP titration improves sleep-related respiratory parameters in some OHS patients with an AHI <30 events/h during sleep. Therefore, this study aimed to assess the titration success of CPAP therapy under polysomnographic (PSG) monitoring and subsequent short-term adherence (1 month) in patients with OHS and an AHI <30 event/h.
Methods
Subjects
This prospective observational study was conducted at the University Sleep Disorders Center (USDC) at King Saud University Medical City at King Saud University, Riyadh, Saudi Arabia; this project is a part of a larger research project, with prospectively collected information, to evaluate OHS.10,17–19 Consecutive ambulatory, PAP-naïve, newly diagnosed OHS patients (>18 years), with an AHI <30 events/h in the period between January 2010 and December 2019 were invited to participate (n=60). Exclusion criteria were chronic illnesses that may result in hypercapnia or impact breathing, including chronic neurological, muscular, or pulmonary conditions, skeletal deformities, decompensated congestive heart failure, and use of drugs that depress the respiratory drive.
All participants underwent spirometry based on the task force guidelines by the American Thoracic Society/European Respiratory Society (ATS/ERS) using a Master Screen (Jaeger, Germany).20 Moreover, all participants had arterial blood analysis after 15 minutes of rest while awake, sitting, and at room-air employing a GEM® Premier™ 4000 analyzer (Instrumentation Laboratory, Lexington, MA). Daytime sleepiness was determined using the Epworth sleepiness scale (ESS).21 Comorbidities were identified based on clinical histories and medical records.
OHS Diagnosis
OHS was diagnosed according to the third edition of the International Classification of Sleep Disorders Manual (ICSD-3), including: 1) daytime hypercarbia (arterial PaCO2 >45 mm Hg), 2) BMI >30 kg/m2, and 3) excluding other disorders causing hypoventilation and daytime hypercarbia.22
Polysomnography
All participants had a standard diagnostic sleep study (Type 1).10,23 The following sleep parameters were recorded during the study, standard electroencephalogram, cardiogram, respiratory flow and efforts, pulse oximeter, and leg and chin electromyogram via Alice® diagnostic equipment (Philips, Respironics Inc., Murrysville, PA, USA). Sleep studies and respiratory events were scored manually according to the American Academy of Sleep Medicine (AASM) scoring criteria and rechecked by certified staff.23
Hypopneas were scored when there was a decrement in nasal pressure signal by ≥50% for ≥10 seconds, resulting in arousal or a ≥3% drop in SpO2 from the pre-event baseline. The desaturation index was calculated as the number of desaturations (fall in SpO2 of ≥3%) divided by total sleep time in hours. OSA severity was assessed using the AHI (the number of obstructive apneas and hypopneas per hour of sleep).
Attended PAP Therapy and Titration-Protocol
All included OHS patients were firstly started on CPAP during a therapeutic polysomnographic study. If the SpO2 remained continually less than 90% despite eliminating the obstructive events and flow limitation, CPAP pressure was increased by 2–3 cm H2O. The highest CPAP pressure that could be reached was 20 cm H2O.
At present, there is no consensus agreement on the Definition of “CPAP titration failure” in OHS patients.24,25 Some previous studies have labeled CPAP titration failure if the SpO2 remained less than 85–90% for 20% of the total sleep time.24,25 The ATS clinical practice guideline review indicated that previous studies had used the following definition of “CPAP failure” in stable OHS patients, the response to CPAP is observed over one night, and the failure to maintain SpO2 > 85–90% is deemed an indication of “CPAP failure,” which prompts a move to NIV.8,26–28 Therefore, we adopted the criterion of “SpO2 remained less than 85–90% for 20% of the total sleep time” during titration to define CPAP failure and arrange for a therapeutic night on BPAP.
Fixed pressure BPAP was used when CPAP failed. EPAP was increased to eliminate apneas, hypopneas, and upper airway narrowing.29 IPAP was increased to improve SpO2, aiming for a tidal volume of 8–10 ml/kg of ideal body weight. BPAP was initiated in the spontaneous mode, with a plan to add a backup rate if problems of ineffective triggering, central respiratory apneas, or a low respiratory rate developed.30
During BPAP titration, supplemental O2 was added when obstructive respiratory events were eliminated, and pressure support and respiratory rate were normalized, but the SpO2 remained < 90% for 5 minutes or more.31
Thirty patients agreed to participate in the 1-month follow-up study to assess PAP therapy adherence. The ATS criteria for positive airway pressure therapy adherence were used in this study.32 The ATS criteria defined “good adherence” to PAP as “using PAP therapy regularly for >4 h/night for >70% of the recorded time”; and “partial adherence” is defined as “using PAP therapy >2 h/night provided that PAP use is attended by subjective improvement in OHS-related symptoms such as quality of life”.32 If none of the above criteria is met, patients were deemed non-adherent.32 Adherence to PAP therapy was recorded via transferring “mask-on time tracking” information from PAP machines, which allowed the objective assessment of adherence to PAP therapy.33
Assessment of PAP Adherence
The follow-up and PAP therapy adherence assessment have been described in detail before.10 After attending an educational session (in the presence of a family member) with hands-on training, the PAP devices were provided to the patients.
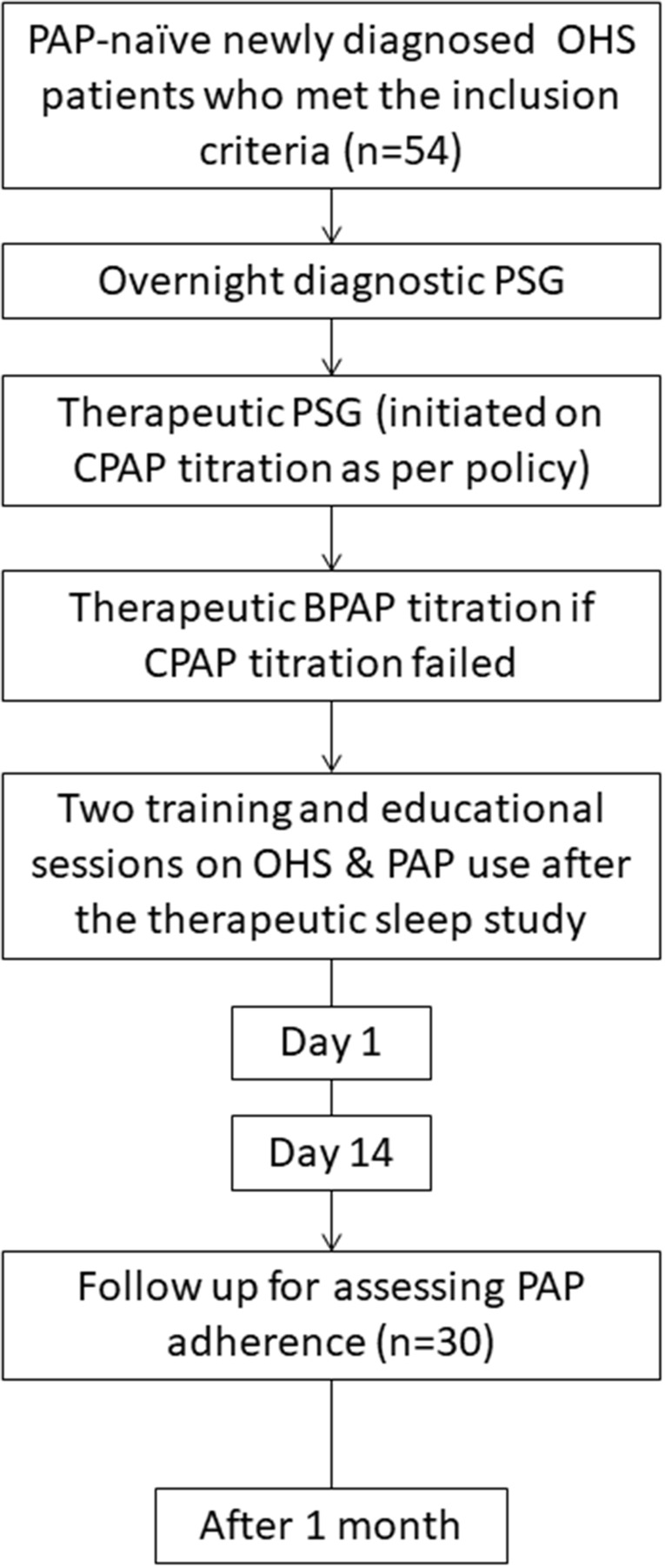
Figure 1 illustrates the study protocol; patients had two nights in the sleep disorders center; night-1: for diagnosis; and night-2: for CPAP therapy application and titration. If the CPAP titration trial failed, as defined above, a third night was arranged for BPAP titration. PAP titration was made within 2 weeks following the diagnostic night. After the therapeutic sleep study, patients underwent two hands-on training meetings on day 1 and day 14.
Figure 1.
A flowchart of the study group.
The study was concluded one month after initiating PAP therapy, and objective adherence was assessed.
During the study month after PAP therapy initiation, patients had direct, immediate access to medical and technical support by the treating team through phone contact during daytime working hours.
PAP therapy adherence was verified by downloading “mask-on time tracking” data from PAP devices. This method allowed the objective assessment of adherence to PAP therapy.33
Statistical Analysis
Data are displayed as numbers (%) or mean ± standard deviation (SD). The CPAP and BPAP groups were compared using the Chi-square test for binary (dichotomous) variables and the t-test for continuous variables. If the normality test failed, the Mann-Whitney U test was used. Additionally, a univariable logistic regression analysis was performed to identify factors associated with CPAP titration success during the therapeutic night, whereby one independent variable was analyzed at a time in the model. The following independent variables were run in the model, demographics, arterial blood gas parameters, sleep study variables, and comorbidities. Variables with significant p-values were run in the subsequent multivariable logistic regression analysis model. The correlation matrix calculated the multicollinearity between variables in the model, and no multicollinearity was found. Furthermore, the standard error in the model was utilized to reexamine multicollinearity. A p-value < 0.05 was accepted as statistically significant. The SPSS statistical software (version 23; Chicago, IL, USA) was used in the analysis.
Results
Sixty patients were diagnosed with OHS with an AHI <30 and met the inclusion criteria; 6 of them refused to use PAP (CPAP or BPAP) during titration. There was no difference between those six patients who refused PAP therapy and the remaining patients (n=54) regarding age, gender, BMI, comorbidities, AHI, mean nocturnal SpO2, baseline PaCO2, and PaO2.
The remaining 54 patients (41 women) completed the titration study. The mean age of the studied group was 54.8 ± 14.6 years (range: 40–74), and the mean BMI was 45.9 ± 12.2 kg/m2 (range: 40–56). Patient demographics and general characteristics are presented in Table 1. Successful titration on CPAP was attained in 36 (66.7%) patients, and 18 (33.3%) required BPAP spontaneous mode (none required the spontaneous-timed mode). The mean CPAP and BPAP pressures required at the end of the therapeutic studies were 11 ± 3.4 cmH2O and 14.8 ± 3.0/10.1 ± 2.5 cmH2O, respectively. Among patients who were switched to BPAP, only one patient required the addition of supplemental oxygen.
Table 1.
Demographic and General Information
| Variable Total (n=54) | Mean ± SD/n (%) |
|---|---|
| Age (Year) | 54.8 ± 14.6 |
| Body mass index (kg/m2) | 45.9 ± 11.2 |
| Epworth sleepiness scale | 8.7 ± 5.2 |
| PH | 7.4 ± 0.1 |
| PaCO2 (mmHg) | 53.9 ± 6.6 |
| PaO2 (mmHg) | 67.1 ± 17.5 |
| HCO3 (mmol/L) | 31.2 ± 8.4 |
| FEV1/FVC (%) | 85.3 ± 6.3 |
| FVC (% predicted) | 70.2 ± 21.4 |
| FEV1 (% predicted) | 73 ± 21.8 |
| Sex (Female) | 41 (75.9) |
| PSG findings | |
| Sleep efficiency (%) | 70.6 ± 18 |
| Stage N1 (%) | 8.8 ± 9.6 |
| Stage N2 (%) | 68.8 ± 18.2 |
| Stage N3 (%) | 9.1 ± 14.4 |
| Stage REM (%) | 12.8 ± 11.9 |
| Apnea hypopnea index (events/hr.) | 16.7 ± 7.8 |
| Central apnea index (events/hr.) | 0.04 ± 0.1 |
| Obstructive apnea index (events/hr.) | 0.6 ± 1.4 |
| Mixed apnea index (events/hr.) | 0.5 ± 3.6 |
| Hypopnea index (events/hr.) | 14.9 ± 7.6 |
| Desaturation index (desaturations/hr.) | 16.1 ± 15.4 |
| Time with SpO2 <90% (mins) | 35.4 ± 40.9 |
| Lowest recorded SpO2 (%) | 77.4 ± 12.8 |
| Mean nocturnal SpO2 (%) | 89.4 ± 10.5 |
| Arousal index (arousals/hr.) | 21.7 ± 10.9 |
| Comorbidities | |
| Hypertension | 37 (68.52 |
| Ischemic heart disease | 6 (11.1) |
| Diabetes mellitus | 29 (53.7) |
| Renal failure | 2 (3.7) |
| Compensated heart failure | 3 (5. 6) |
| Bronchial asthma | 19 (35.19) |
| Allergic rhinitis | 5 (9.26) |
| Hypothyroidism | 7 (12.96) |
| Hypercholesterolemia | 19 (35.2) |
Table 2 demonstrates a comparison between patients in whom CPAP titration was successful and patients who required a therapeutic study with BPAP. Patients in whom the CPAP trial failed and needed to be shifted to BPAP had a significantly higher PaCO2 level (49 ± 4.7 mmHg vs 63.7 ± 11.5 mmHg) and bicarbonate level (29.1 ± 2.4 mmol/L vs 35.1 ± 13.3 mmol/L). Additionally, they significantly had lower forced expiratory volume during the first second (FEV1) (% predicted) 76.1±19.3% vs 49.4±14.4%) and lower forced vital capacity (FVC) (% predicted) (79.4±19.5% vs 50.6±12.5%). With regards to the PSG findings, the group that needed to be shifted to BPAP during the therapeutic night had signs of more severe disease reflected by a significantly higher time with SpO2 <90% (mins), lower lowest recorded SpO2 (%), and mean nocturnal SpO2 (%), as shown in Table 2. However, the desaturation index was more in the CPAP group 24.1 ± 22.1/h vs 12.2 ± 8.5/h, p-value= 0.026).
Table 2.
Comparison Between Patients in Whom CPAP Was Successfully Titrated and Patients Who Were Shifted to BPAP
| Variable Total (n=54) | Mean ± SD/n (%) | P-Value | |
|---|---|---|---|
| CPAP (n=36) | BPAP (n=18) | ||
| Age (Year) | 53.4 ± 13.3 | 57.7 ± 16.9 | 0.307 |
| Body mass index (kg/m2) | 45.7 ± 11.6 | 46.1 ± 10.2 | 0.1 |
| Epworth sleepiness scale | 8.6 ± 5.3 | 8.9 ± 5.3 | 0.821 |
| PaCO2 (mmHg) | 49 ± 4.7 | 63.7 ± 11.5 | < 0.001 |
| PaO2 (mmHg) | 69.4 ± 17.7 | 62.5 ± 16.6 | 0.178 |
| HCO3 (mmol/L) | 29.1 ± 2.4 | 35.1 ± 13.3 | 0.006 |
| FEV1/FVC (%) | 85.4 ± 6.1 | 85 ± 7.5 | 0.875 |
| FVC (% predicted) | 76.1 ± 19.3 | 49.4 ± 14.4 | 0.001 |
| FEV1 (% predicted) | 79.4 ± 19.5 | 50.6 ± 12.5 | < 0.001 |
| Sex (Female) | 27 (75) | 14 (77.8) | 1.000 |
| Premenopausal | 9 (25) | 2 (11.1) | 0.429 |
| Comorbidities | |||
| Hypertension | 22 (61) | 15 (83.3) | 0.21 |
| Ischemic heart disease | 4 (11) | 2 (11.1) | 1.00 |
| Diabetes mellitus | 16 (44.4) | 13 (72.2) | 0.08 |
| Renal failure | 0 (0) | 2 (11.1) | 0.11 |
| Compensated heart failure | 2 (5.6) | 1 (5.6) | 1.00 |
| Bronchial asthma | 15 (41.7) | 4 (22.2) | 0.16 |
| Allergic rhinitis | 5 (13.9) | 0 (0) | 0.26 |
| Hypothyroidism | 6 (16.7) | 1 (5.6) | 0.40 |
| Hypercholesterolemia | 15 (41.7) | 4 (22.2) | 0.25 |
| Polysomnographic findings at baseline | |||
| Sleep efficiency (%) | 72.1 ± 16.5 | 67.6 ± 20.9 | 0.39 |
| Stage N1 (%) | 7.7 ± 5.6 | 11 ± 14.7 | 0.83 |
| Stage N2 (%) | 71.5 ± 17.1 | 63.4 ± 19.6 | 0.12 |
| Stage N3 (%) | 8.7 ± 15.1 | 9.8 ± 13.2 | 0.67 |
| Stage REM (%) | 11.9 ± 9.3 | 14.6 ± 16.2 | 0.52 |
| Apnea hypopnea index (events/hr) | 17.4 ± 7.8 | 15.3 ± 7.8 | 0.35 |
| Central apnea index (events/hr) | 0 ± 0.1 | 0 ± 0.1 | 0.946 |
| Obstructive apnea index (events/hr) | 0.6 ± 1.2 | 0.6 ± 1.7 | 0.577 |
| Mixed apnea index (events/hr) | 0.7 ± 4.4 | 0.1 ± 0.1 | 0.079 |
| Hypopnea index (events/hr) | 16.8 ± 7.6 | 14 ± 7.6 | 0.205 |
| Desaturation index (desaturations/hr) | 24.1 ± 22.1 | 12.2 ± 8.5 | 0.026 |
| Time with SpO2 <90% (mins) | 20.4 ± 34.2 | 65.4 ± 37.2 | < 0.001 |
| Lowest recorded SpO2 (%) | 81.1 ± 11.7 | 69.8 ± 11.8 | < 0.001 |
| Mean nocturnal SpO2 (%) | 91.8 ± 10.9 | 84.4 ± 7.7 | < 0.001 |
| Arousal index (arousals/hr) | 22.1 ± 9.9 | 21.5 ± 11.5 | 0.76 |
| Polysomnographic findings during successful titration | |||
| Sleep efficiency (%) | 76 ± 15.7 | 61.4 ± 22.3 | 0.01 |
| Stage N1 (%) | 7 ± 5.8 | 11.9 ± 14 | 0.49 |
| Stage N2 (%) | 65.5 ± 15.4 | 64.5 ± 18.2 | 0.649 |
| Stage N3 (%) | 6 ± 9.7 | 8.9 ± 12.1 | 0.59 |
| Stage REM (%) | 21.2 ± 11.4 | 14.1 ± 11 | 0.04 |
| Apnea hypopnea index (events/hr) | 5.9 ± 6.2 | 8.3 ± 7.3 | 0.216 |
| Central apnoea index (events/hr) | 0.4 ± 1.3 | 0.1 ± 0.2 | 0.732 |
| Obstructive apnoea index (events/hr) | 0.3 ± 1 | 0.3 ± 0.8 | 0.438 |
| Mixed apnoea index (events/hr) | 0.1 ± 0.2 | 0 ± 0.1 | 1.000 |
| Hypopnea index (events/hr) | 4.6 ± 4.5 | 7.9 ± 7 | 0.094 |
| Desaturation index (desaturations/hr) | 4.7 ± 4.8 | 4.9 ± 5 | 0.917 |
| Time with SpO2 <90% (mins) | 0.9 ± 2.1 | 15.7 ± 23.7 | 0.002 |
| Lowest recorded SpO2 (%) | 90.6 ± 3 | 81 ± 18.6 | 0.017 |
| Mean nocturnal SpO2 (%) | 95.7 ± 1.7 | 94.1 ± 2.7 | 0.015 |
| Arousal index (arousals/hr) | 12.8 ± 9.2 | 15.6 ± 14.3 | 0.868 |
| Required supplemental oxygen | – | 2 (11.1) | |
| PAP device pressure | |||
| PAP recommended pressure | 11 ± 3.4 | 14.8 ± 3/10.1 ± 2.5 | - |
Abbreviations: HCO3, bicarbonate; FEV1, forced expiratory volume in 1 sec; FVC, forced vital capacity; SPO2, percent saturation of oxygen in the blood; PAP, positive airway pressure.
Both groups (CPAP and BPAP) had major improvements in respiratory parameters during the therapeutic titration night (Table 2). However, two patients continued to desaturate while on BPAP during titration; therefore, supplemental oxygen was started.
Table 3 shows the univariate and multivariable regression analyses for the correlates of CPAP titration success during the therapeutic night. On the univariable regression analysis, the significant correlates were BMI (OR: 1.334 [1.065–1.672], p-value= 0.012), AHI (OR: 1.14 [1.001–1.299], p-value=0.049), and desaturation index (OR: 1.219 [1.015–1.464], p-value= 0.034). On the other hand, the only independent correlate on the multivariable regression analysis was the desaturation index (OR: 1.33 [1.033–1.712, p-value= 0.027].
Table 3.
Factors Associated with CPAP Titration Success During the Therapeutic Night. CPAP Acceptance Using Univariable and Multivariable Logistic Regression Analyses
| Variables in the Equation | p-value | OR [95% C.I.] | |
|---|---|---|---|
| Univariable Model | |||
| Age (Year) | 0.24 | 1.04 [0.97–1.12] | |
| Body mass index (kg/m2) | 0.012 | 1.334 [1.07–1.67] | |
| PaCO2 (mmHg) | 0.25 | 1.21 [0.87–1.68] | |
| HCO3 (mmol/L) | 0.14 | 1.39 [0.90–2.15] | |
| FVC (% predicted) | 0.99 | 1.00 [0.95–1.05] | |
| FEV1 (% predicted) | 0.91 | 0.99 [0.95–1.047] | |
| Apnea hypopnea index (events/hr) | 0.049 | 1.14 [1.001–1.30] | |
| Desaturation index (desaturations/hr) | 0.034 | 1.22 [1.02–1.46] | |
| Time with SpO2 <90% (mins) | 0.24 | 1.754 [0.69–4.43] | |
| Lowest recorded SpO2 (%) | 0.05 | 0.74 [0.55–1.003] | |
| Mean nocturnal SpO2 (%) | 0.10 | 0.71 [0.474–1.07] | |
| Sex (Female) | 0.23 | 3 [0.50–17.95] | |
| Diabetes mellitus | 0.54 | 1.667 [0.32–8.59] | |
| Hypertension | 0.08 | 4.72 [0.86–26.04] | |
| Multivariable logistic model (Forward Wald method)* | |||
| Desaturation index (desaturations/hr) | 0.027 | 1.33 [1.033–1.712] | |
Notes: *Multicollinearity: none. Overall accuracy: 80.6%, Sensitivity: 91.7%, Specificity: 42.9%, Area under the curve (ROC): 87.2%, Omnibus tests of model: p=0.002, Hosmer-Lemeshow goodness of fit: p=0.609, Nagelkerke R square: 42.2%.
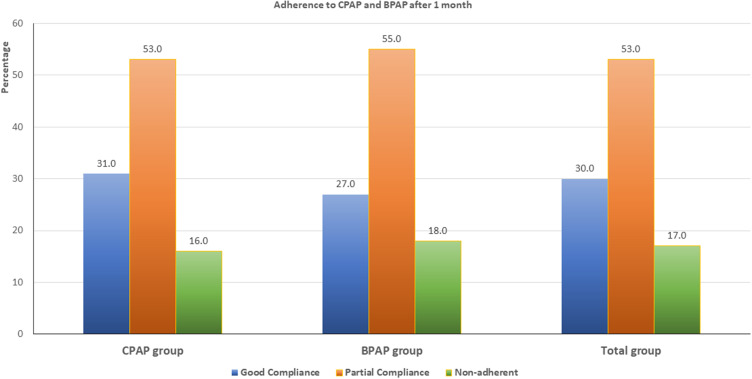
Thirty patients agreed to participate in the 1-month follow-up study, 19 in the CPAP group and 11 in the BPAP group. Figure 2 presents adherence to therapy in the whole group, CPAP group, and BPAP group. More than 80% of the participants were using PAP therapy after one month. In the CPAP group and BPAP group, good adherence was (31% vs 27%, p-value=1.0), partial adherence (53% vs 55%, p-value=0.9), and non-adherent (16% vs 18%, p-value=1.0). None of the CPAP group was shifted to BPAP during the study period. There was no difference in CPAP adherence between patients who required CPAP titration pressure > 15 cmH2O and < 15 cmH2O.
Figure 2.
Adherence to therapy in the whole group, CPAP group, and BPAP group after one month of initiating therapy.
PAP devices are usually replaced for patients after five years with new devices; however, as patients’ recruitment was between 2010 to 2019, and there is a possibility of advances in PAP devices technology, which may improve adherence, PAP therapy adherence was compared across the ten study years. No difference in adherence was detected between the different years.
During the one-month follow-up period, none of the patients was admitted to the hospital with respiratory failure.
Discussion
To our knowledge, no study has addressed the success of using CPAP as an acceptable alternative therapeutic option to NIV in OHS patients without severe OSA when NIV is not readily available. In this observational study, almost two-thirds of the studied patients had successful and acceptable CPAP titration, and most of the patients who participated in the follow-up continued to use their CPAP device after one month. The group that failed CPAP titration had more severe sleep-disordered breathing reflected by worse hypercapnia, more restriction of spirometry, and worse oxygenation during sleep. Switching this group of patients who failed CPAP titration to BPAP spared most of them the need to add supplemental oxygen (16 out of the 18 switched patients). A study by Schwartz et al reported better efficacy of BPAP than CPAP in OSA patients who have older age, higher BMI, and higher PaCO2.34 In the current study, the group that required BPAP had a higher PaCO2; on the other hand, the desaturation index was higher in the CPAP group. A higher desaturation index reflects intermittent hypoxemia and obstructive respiratory events responding to continuous PAP. As BPAP augments tidal volume and minute ventilation, it is more likely to rapidly wash out CO2, hence improving hypoxemia secondary to alveolar hypoventilation. Additionally, augmenting tidal volume during BPAP may further reduce atelectasis and improve lung mechanics, resulting in better oxygenation.35 Future studies should assess the feasibility of shifting this group of patients to CPAP therapy when eucapnia is achieved. Nevertheless, our current findings show that CPAP therapy can be an effective alternative in most OHS patients with mild to moderate OSA.
In OHS patients without severe OSA, previous case series had demonstrated that NIV therapy resulted in short-term stability.15,36 A randomized-controlled trial showed an improvement in parameters of respiratory failure in patients on NIV when compared to patients on lifestyle modifications.5 However, no study has addressed the success of CPAP titration and short-term adherence in this group of patients with OHS.
Whether CPAP is effective in patients with OHS accompanied by mild-moderate OSA is not known. Currently, most clinicians would initiate therapy in this group of OHS patients with BPAP (NIV), and consider shifting to CPAP therapy when eucapnia is attained.37 Our current results indicate that CPAP could be a starting alternative for some patients with OHS and mild-moderate OSA. The titration success rate and short-term adherence were good. The only independent correlate of CPAP titration success was the desaturation index, which reflects intermittent hypoxia and is a surrogate of OSA, suggesting that treating mild-moderate OSA may improve derangements in patients with OHS.38
Although CPAP does not directly provide ventilatory support, it has been proposed that CPAP enhances gas exchange by reducing upper airway resistance, improving lung mechanics, decreasing the work of breathing, and opening dependent atelectatic lung units.39 By removing upper airway narrowing, CPAP diminishes the cycle of low ventilation. CPAP therapy has been demonstrated to significantly improve hypercapnia in patients with sleep-disordered breathing who are adherent to treatment.26,40 The PSG findings demonstrated that all respiratory parameters had returned close to normal during successful titration.
The current findings are consistent with our recently published data in patients with OHS and severe OSA, where two-thirds of the patients achieved successful CPAP titration.10 The findings of this study may pave the way to large randomized controlled trials to assess the success of CPAP titration in OHS patients with mild to moderate OSA and precisely define the clinical and PSG characteristics of patients who are likely to have successful CPAP titration. Additionally, long-term studies are needed to assess the effect of CPAP therapy on arterial blood gas parameters, spirometric parameters, healthcare utilization, incident cerebrovascular and cardiovascular events, and mortality. Nevertheless, given the lower prevalence of this phenotype of OHS, it will be difficult to recruit an adequate sample for long-term clinical trials. Therefore, a collaborative international consortium is needed to recruit an adequate sample size.
More than 80% of the group were still using their CPAP device after one month, with no differences between the CPAP and BPAP groups. The currently presented data is comparable to the adherence rate after one month among OHS patients with severe OSA in a recent paper published by the same sleep disorders facility.10 Educational and support programs and close follow-up are necessary to enhance PAP therapy adherence among OHS patients.
Another finding of this study is the higher prevalence of OHS among women than men, which concurs with our previous reports,19,41 and the Spanish Pickwick trial, which showed that 56% of the participants were women.6 While OSA is more common in men; studies have reported contradictory data regarding gender differences in OHS.42–44 In our data, the higher prevalence of OHS in women, was mainly evident in postmenopause.19
Proposed theories to explain the higher prevalence of OHS among postmenopausal women included the withdrawal of female hormones, particularly progesterone, which has an important role in ventilation.45,46 Another theory to explain the higher prevalence in women included the higher prevalence of leptin resistance among obese women, which has been reported to be up to four times higher in obese women than obese men.47 Furthermore, clinical and subclinical hypothyroidism have been reported to be significantly higher in women than in men with OHS.19,41 Hypothyroidism is known to suppress the ventilatory response to hypercapnia,48 and hypoxia.49 Nonetheless, more research is needed to evaluate gender differences in OHS and the possible mechanisms.
The current study has strengths and limitations. Limitations include reporting data from one center. Hence, the results may not be generalized to other sleep disorders centers. Moreover, we did not collect data about physiological parameters at the end of the study and the follow-up period was short to demonstrate changes in the physiological parameters. Therefore, an extended study is warranted to clarify the long-term adherence of CPAP and BPAP in patients with OHS and mild/moderate OSA and the changes in physiological parameters. Moreover, the study sample is relatively small; however, it is difficult to recruit a large number of this phenotype of OHS due to a lower prevalence.5 The Pickwick Project Multicenter Group recruited only 98 patients of OHS without severe OSA over 8 years.5 Therefore, international multicenter collaboration is needed.
Strengths of the study include the fact that this is the first study to systematically assess the acceptance and success rate of CPAP titration in patients with OHS without severe OSA as an alternative to NIV, and the short-term adherence to therapy. The current study aims to send two messages: First, CPAP can be an alternative to NIV in OHS some patients without severe OSA, particularly in parts of the world where cost and lack of needed expertise are major problems. Second, based on the current findings, future multicenter RCTs can be conducted to evaluate CPAP success, long-term adherence, and changes in the physiological respiratory and cardiac parameters over time in both treatment modalities in OHS patients without severe OSA. In addition, the study may be helpful in the development of entire guidelines and comprehensive therapy in patients being comorbid with OHS and OSA.
In summary, this is the first study to systematically assess the utility of CPAP in patients with OHS without severe OSA. The current results suggest that CPAP therapy could be an acceptable alternative therapy in some patients with OHS without severe OSA when NIV therapy is not readily available. The acceptance rate, PSG titration parameters, and one-month adherence were good. Additionally, CPAP is easily available in most parts of the world and is cheaper and easier to apply than BPAP and other modes of NIV.50 Therefore, CPAP may be an adequate initial treatment for some stable ambulatory patients with OHS without severe OSA due to its relatively simple set-up, low cost, and efficacy. However, if sustained hypoxemia or alveolar hypoventilation continues in spite of eliminating obstructive events, patients should be shifted to BPAP therapy. Nevertheless, larger long-term studies are needed to confirm the current findings and characterize the patients who are likely to benefit from CPAP.
Acknowledgment
This study was supported by a research grant from the “Strategic Technologies Program of the National Plan for Sciences and Technology and Innovation in Saudi Arabia (08-MED511-02)”.
At this time, we keep in mind the coauthor Awad H. Olaish who passed before the publication of this work; we all miss you.
Data Availability
Data are available upon request. However, releasing data needs IRB approval.
Ethics Statement
The study protocol was approved by the Ethics Committee of the College of Medicine, King Saud University, and Medical City. All participants provided written informed consent. This study was performed according to the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors report no conflicts of interest in this work.
References
- 1.Piper AJ, BaHammam AS, Javaheri S. Obesity hypoventilation syndrome: choosing the appropriate treatment of a heterogeneous disorder. Sleep Med Clin. 2017;12(4):587–596. doi: 10.1016/j.jsmc.2017.07.008 [DOI] [PubMed] [Google Scholar]
- 2.Basoglu OK, Tasbakan MS. Comparison of clinical characteristics in patients with obesity hypoventilation syndrome and obese obstructive sleep apnea syndrome: a case-control study. Clin Respir J. 2014;8(2):167–174. doi: 10.1111/crj.12054 [DOI] [PubMed] [Google Scholar]
- 3.Castro-Anon O, Perez de Llano LA, De la Fuente Sanchez S, et al. Obesity-hypoventilation syndrome: increased risk of death over sleep apnea syndrome. PLoS One. 2015;10(2):e0117808. doi: 10.1371/journal.pone.0117808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berg G, Delaive K, Manfreda J, Walld R, Kryger MH. The use of health-care resources in obesity-hypoventilation syndrome. Chest. 2001;120(2):377–383. doi: 10.1378/chest.120.2.377 [DOI] [PubMed] [Google Scholar]
- 5.Masa JF, Benitez I, Sanchez-Quiroga MA, et al. Long-term noninvasive ventilation in obesity hypoventilation syndrome without severe OSA: the Pickwick randomized controlled trial. Chest. 2020;158(3):1176–1186. doi: 10.1016/j.chest.2020.03.068 [DOI] [PubMed] [Google Scholar]
- 6.Masa JF, Corral J, Alonso ML, et al. Efficacy of different treatment alternatives for obesity hypoventilation syndrome. Pickwick Study. Am J Respir Crit Care Med. 2015;192(1):86–95. doi: 10.1164/rccm.201410-1900OC [DOI] [PubMed] [Google Scholar]
- 7.Al Dabal L, Bahammam AS. Obesity hypoventilation syndrome. Ann Thorac Med. 2009;4(2):41–49. doi: 10.4103/1817-1737.49411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mokhlesi B, Masa JF, Brozek JL, et al. Evaluation and management of obesity hypoventilation syndrome. an official American thoracic society clinical practice guideline. Am J Respir Crit Care Med. 2019;200(3):e6–e24. doi: 10.1164/rccm.201905-1071ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berger KI, Ayappa I, Sorkin IB, Norman RG, Rapoport DM, Goldring RM. Postevent ventilation as a function of CO(2) load during respiratory events in obstructive sleep apnea. J Appl Physiol. 2002;93(3):917–924. doi: 10.1152/japplphysiol.01082.2001 [DOI] [PubMed] [Google Scholar]
- 10.Almeneessier AS, Aleissi S, Olaish AH, BaHammam AS. Long-term adherence to positive airway pressure therapy in Saudi ambulatory patients with obesity hypoventilation syndrome and severe obstructive sleep apnea: a one-year follow-up prospective observational study. Nat Sci Sleep. 2021;13:63–74. doi: 10.2147/NSS.S290349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Billings ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34(12):1653–1658. doi: 10.5665/sleep.1428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Means MK, Ulmer CS, Edinger JD. Ethnic differences in continuous positive airway pressure (CPAP) adherence in veterans with and without psychiatric disorders. Behav Sleep Med. 2010;8(4):260–273. doi: 10.1080/15402002.2010.509255 [DOI] [PubMed] [Google Scholar]
- 13.Mehrtash M, Bakker JP, Ayas N. Predictors of continuous positive airway pressure adherence in patients with obstructive sleep apnea. Lung. 2019;197(2):115–121. doi: 10.1007/s00408-018-00193-1 [DOI] [PubMed] [Google Scholar]
- 14.Scharf SM, Seiden L, DeMore J, Carter-Pokras O. Racial differences in clinical presentation of patients with sleep-disordered breathing. Sleep Breath. 2004;8(4):173–183. doi: 10.1055/s-2004-860894 [DOI] [PubMed] [Google Scholar]
- 15.Masa JF, Corral J, Caballero C, et al. Non-invasive ventilation in obesity hypoventilation syndrome without severe obstructive sleep apnoea. Thorax. 2016;71(10):899–906. doi: 10.1136/thoraxjnl-2016-208501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Masa JF, Mokhlesi B, Benitez I, et al. Long-term clinical effectiveness of continuous positive airway pressure therapy versus non-invasive ventilation therapy in patients with obesity hypoventilation syndrome: a multicentre, open-label, randomised controlled trial. Lancet. 2019;393(10182):1721–1732. doi: 10.1016/S0140-6736(18)32978-7 [DOI] [PubMed] [Google Scholar]
- 17.BaHammam AS. Prevalence, clinical characteristics, and predictors of obesity hypoventilation syndrome in a large sample of Saudi patients with obstructive sleep apnea. Saudi Med J. 2015;36(2):181–189. doi: 10.15537/smj.2015.2.9991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.BaHammam AS, Aleissi S, Olaish AH, Almeneessier AS, Jammah AA. Prevalence of hypothyroidism in a large sample of patients with obesity hypoventilation syndrome. Nat Sci Sleep. 2020;12:649–659. doi: 10.2147/NSS.S263959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.BaHammam AS, Pandi-Perumal SR, Piper A, et al. Gender differences in patients with obesity hypoventilation syndrome. J Sleep Res. 2016;25(4):445–453. doi: 10.1111/jsr.12400 [DOI] [PubMed] [Google Scholar]
- 20.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805 [DOI] [PubMed] [Google Scholar]
- 21.Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15(4):376–381. doi: 10.1093/sleep/15.4.376 [DOI] [PubMed] [Google Scholar]
- 22.American Academy of Sleep Medicine (AASM). International Classification of Sleep Disorders (ICSD). 3rd ed. Darien, IL: AASM; 2014. [Google Scholar]
- 23.Berry RB, Brooks R, Gamaldo CE, et al. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, version 2.1. Darien, Illinois: American Academy of Sleep Medicine; 2014. Available from: www.aasmnet.org. Accessed June 9, 2022. [Google Scholar]
- 24.Lastra AC, Masa JF, Mokhlesi B. CPAP titration failure is not equivalent to long-term CPAP treatment failure in patients with obesity hypoventilation syndrome: a case series. J Clin Sleep Med. 2020;16(11):1975–1981. doi: 10.5664/jcsm.8712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mokhlesi B. Positive airway pressure titration in obesity hypoventilation syndrome: continuous positive airway pressure or bilevel positive airway pressure. Chest. 2007;131(6):1624–1626. doi: 10.1378/chest.07-0384 [DOI] [PubMed] [Google Scholar]
- 26.Mokhlesi B, Tulaimat A, Evans AT, et al. Impact of adherence with positive airway pressure therapy on hypercapnia in obstructive sleep apnea. J Clin Sleep Med. 2006;2(1):57–62. doi: 10.5664/jcsm.26436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perez de Llano LA, Golpe R, Ortiz PM, et al. Short-term and long-term effects of nasal intermittent positive pressure ventilation in patients with obesity-hypoventilation syndrome. Chest. 2005;128(2):587–594. doi: 10.1378/chest.128.2.587 [DOI] [PubMed] [Google Scholar]
- 28.Storre JH, Seuthe B, Fiechter R, et al. Average volume-assured pressure support in obesity hypoventilation: a randomized crossover trial. Chest. 2006;130(3):815–821. doi: 10.1378/chest.130.3.815 [DOI] [PubMed] [Google Scholar]
- 29.Howard ME, Piper AJ, Stevens B, et al. A randomised controlled trial of CPAP versus non-invasive ventilation for initial treatment of obesity hypoventilation syndrome. Thorax. 2017;72(5):437–444. doi: 10.1136/thoraxjnl-2016-208559 [DOI] [PubMed] [Google Scholar]
- 30.Piper AJ. Positive airway pressure II: settings and outcomes. In: Tulaimat A, editor. Obesity Hypoventilation Syndrome. From Physiologic Principles to Clinical Practice. 1st ed. London, United Kingdom: Elsevier; 2020:187–2002. [Google Scholar]
- 31.Berry RB, Chediak A, Brown LK, et al. Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med. 2010;6(5):491–509. [PMC free article] [PubMed] [Google Scholar]
- 32.Schwab RJ, Badr SM, Epstein LJ, et al. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med. 2013;188(5):613–620. doi: 10.1164/rccm.201307-1282ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245–258. [PMC free article] [PubMed] [Google Scholar]
- 34.Schwartz SW, Rosas J, Iannacone MR, Foulis PR, Anderson WM. Correlates of a prescription for Bilevel positive airway pressure for treatment of obstructive sleep apnea among veterans. J Clin Sleep Med. 2013;9(4):327–335. doi: 10.5664/jcsm.2580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Heinemann F, Budweiser S, Dobroschke J, Pfeifer M. Non-invasive positive pressure ventilation improves lung volumes in the obesity hypoventilation syndrome. Respir Med. 2007;101(6):1229–1235. doi: 10.1016/j.rmed.2006.10.027 [DOI] [PubMed] [Google Scholar]
- 36.Redolfi S, Corda L, La Piana G, Spandrio S, Prometti P, Tantucci C. Long-term non-invasive ventilation increases chemosensitivity and leptin in obesity-hypoventilation syndrome. Respir Med. 2007;101(6):1191–1195. doi: 10.1016/j.rmed.2006.11.005 [DOI] [PubMed] [Google Scholar]
- 37.Murphy PB, Piper AJ, Hart N. Obesity hypoventilation syndrome: is less really more?. Lancet. 2019;393(10182):1674–1676. doi: 10.1016/S0140-6736(19)30248-X [DOI] [PubMed] [Google Scholar]
- 38.BaHammam A. Is apnea hypopnea index a good predictor for obesity hypoventilation syndrome in patients with obstructive sleep apnea?. Sleep Breath. 2007;11(3):201;author reply 203–204. doi: 10.1007/s11325-007-0121-2 [DOI] [PubMed] [Google Scholar]
- 39.Randerath W, Verbraecken J, Andreas S, et al. Definition, discrimination, diagnosis and treatment of central breathing disturbances during sleep. Eur Respir J. 2017;49(1):1. doi: 10.1183/13993003.00959-2016 [DOI] [PubMed] [Google Scholar]
- 40.Han F, Chen E, Wei H, He Q, Ding D, Strohl KP. Treatment effects on carbon dioxide retention in patients with obstructive sleep apnea-hypopnea syndrome. Chest. 2001;119(6):1814–1819. doi: 10.1378/chest.119.6.1814 [DOI] [PubMed] [Google Scholar]
- 41.BaHammam AS, Almeneessier AS. Is obesity hypoventilation Syndrome A postmenopausal disorder?. Open Respir Med J. 2019;13:51–54. doi: 10.2174/1874306401913010051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Palm A, Midgren B, Janson C, Lindberg E. Gender differences in patients starting long-term home mechanical ventilation due to obesity hypoventilation syndrome. Respir Med. 2016;110:73–78. doi: 10.1016/j.rmed.2015.11.010 [DOI] [PubMed] [Google Scholar]
- 43.Arish N, Mackay T, Frangulyan R, Riha RL. Sex differences in patients with obesity hypoventilation syndrome: do they really exist?. Health Sci Rep. 2022;5(1):e456. doi: 10.1002/hsr2.456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cunningham J, Hunter M, Budgeon C, et al. The prevalence and comorbidities of obstructive sleep apnea in middle-aged men and women: the Busselton Healthy Ageing Study. J Clin Sleep Med. 2021;17(10):2029–2039. doi: 10.5664/jcsm.9378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Javaheri S, Guerra LF. Effects of domperidone and medroxyprogesterone acetate on ventilation in man. Respir Physiol. 1990;81(3):359–370. doi: 10.1016/0034-5687(90)90116-G [DOI] [PubMed] [Google Scholar]
- 46.Saaresranta T, Polo O. Hormones and breathing. Chest. 2002;122(6):2165–2182. doi: 10.1378/chest.122.6.2165 [DOI] [PubMed] [Google Scholar]
- 47.Kapsimalis F, Kryger MH. Gender and obstructive sleep apnea syndrome, part 1: clinical features. Sleep. 2002;25(4):412–419. [PubMed] [Google Scholar]
- 48.Duranti R, Gheri RG, Gorini M, et al. Control of breathing in patients with severe hypothyroidism. Am J Med. 1993;95(1):29–37. doi: 10.1016/0002-9343(93)90229-I [DOI] [PubMed] [Google Scholar]
- 49.Zwillich CW, Pierson DJ, Hofeldt FD, Lufkin EG, Weil JV. Ventilatory control in myxedema and hypothyroidism. N Engl J Med. 1975;292(13):662–665. doi: 10.1056/NEJM197503272921302 [DOI] [PubMed] [Google Scholar]
- 50.Masa JF, Mokhlesi B, Benitez I, et al. Cost-effectiveness of positive airway pressure modalities in obesity hypoventilation syndrome with severe obstructive sleep apnoea. Thorax. 2020;75(6):459–467. doi: 10.1136/thoraxjnl-2019-213622 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon request. However, releasing data needs IRB approval.