Abstract
Two adolescent mental health fields — sleep and depression — have advanced largely in parallel until about four years ago. Although sleep problems have been thought to be a symptom of adolescent depression, emerging evidence suggests that sleep difficulties arise before depression does. In this Review, we describe how the combination of adolescent sleep biology and psychology uniquely predispose adolescents to develop depression. We describe multiple pathways and contributors, including a delayed circadian rhythm, restricted sleep duration and greater opportunity for repetitive negative thinking while waiting for sleep. We match each contributor with evidence-based sleep interventions, including bright light therapy, exogenous melatonin and cognitive-behaviour therapy techniques. Such treatments improve sleep and alleviate depression symptoms, highlighting the utility of sleep treatment for comorbid disorders experienced by adolescents.
Subject terms: Human behaviour, Sleep disorders, Psychology, Depression
Sleep problems are both a symptom and precursor of adolescent depression. In this Review, Gradisar et al. describe how the combination of adolescent sleep biology and psychology predisposes adolescents to develop depression, and describe interventions that improve sleep and depression symptoms in this population.
Introduction
Adolescents (from pubertal onset to 21 years of age) are the most chronically sleep-restricted subpopulation across human development1. Data from across the world suggest that adolescents sleep too late and too little2. Such meta-analytical and descriptive data show similar patterns of adolescent sleep in Western and Eastern societies3–5. Sleep onset for adolescents becomes later as they age (both on weekdays and weekends)3–5, a phenomenon not observed during any other decade in life1. A lack of morning commitments allows adolescents to potentially obtain optimal sleep duration (9.0–9.3 hours)6 on weekends. However, they are not afforded the same sleep opportunity on weekdays owing to the need to rise earlier than their natural wake time to attend school7. This restricted sleep opportunity is especially pronounced in countries that implement an early school start (for example, 7:30 am in the USA)7. Increases in sleep duration on school nights occurs when school start times are delayed8. Indeed, the quarantine associated with the COVID-19 pandemic eliminated the need for morning travel and therefore provided an extended sleep opportunity for adolescents, who showed increased sleep duration accordingly9–11. However, the return to in-person learning is accompanied by a return to restricted sleep for adolescents11. Although the American Academy of Pediatrics and the US Centers for Disease Control and Prevention have recommended delaying school start times to match adolescents’ natural tendency for delayed sleep timing, such policy changes have been largely unsuccessful — and are therefore not the solution12.
The rapid cascade of events that uniquely affect adolescent sleep begin around the beginning of high school and puberty13. This coincides with a period of increased risk for the onset of low mood and depression in adolescents14. Approximately 2.6% of adolescents experience a depressive disorder at any given time15, with the cumulative frequency of depression rising to 20% by the end of adolescence16. Female adolescents are twice as likely as male adolescents to experience depression16,17. Other risk factors include having a parent that has experienced depression18,19, exposure to stressful life events20,21 and experiencing bullying22. Experiencing depression in youth can have long-term negative impacts, including an increased risk of further episodes of depression as an adult23,24, and developing other mental health disorders25–27. Adolescence-onset depression has also been associated with educational underachievement, low income levels and unemployment28–30, and is a risk factor for suicidal behaviour31.
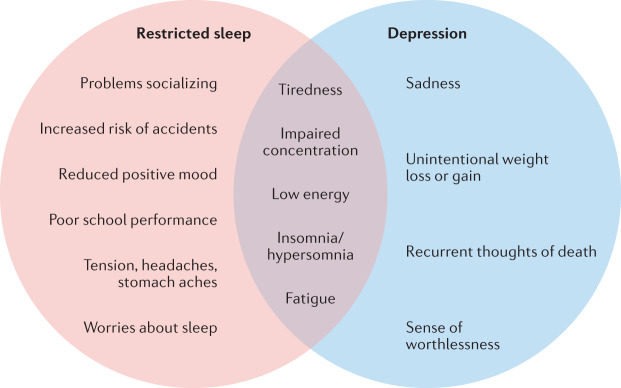
Depression is characterized by a diverse range of symptoms. From the nine symptom domains identified by the Diagnostic and Statistical Manual of Mental Disorders edition 5 (DSM-5; ref.32), more than 1,000 symptom combinations can be computed that meet the diagnostic criteria33. Little is known as to whether different combinations of symptoms at presentation are sufficient to form distinct subgroups34. One study suggests that there might be subtypes of depression that are primarily characterized by severity, with less severe groups (for example, fewer symptoms and lower risk) still presenting with high levels of somatic symptoms, such as sleep disturbance35. Among depressed adolescents, sleep problems (92%) are more frequently reported than low mood (84%)36. Indeed, there is overlap between symptoms of depression and those resulting from poor adolescent sleep (Fig. 1). However, rather than follow the notion that sleep problems are a symptom of depression, the scientific evidence suggests the reverse, especially during adolescence37.
Fig. 1. Unique and shared symptoms of restricted sleep and depression in adolescents.
Symptoms of restricted sleep, depression symptoms and common symptoms according to the DSM-5 (ref.32) and the International Classification of Sleep Disorders, 3rd edition (ICSD-3) (ref.81).
In this Review, we consider how adolescent sleep problems might contribute to the emergence of depression during this developmental stage. First, we describe the two main bioregulatory processes that drive sleep delay for adolescents: reduced sleep homeostatic pressure and delayed circadian timing. Next, we discuss how the consequences of these biological sleep characteristics — delayed sleep patterns, restricted sleep on school nights, and a long time taken to fall asleep at night — have biological and psychological implications for depression. Finally, we describe three evidence-based solutions that target the main contributing factors to adolescent sleep problems: bright light therapy, exogenous melatonin and cognitive-behaviour therapy. Although both insomnia and circadian rhythm disorders are present during adolescence38, the scientific literature and clinical trials are weighted towards circadian rhythm disorders. Thus, we focus on delayed sleep–wake phase disorder here.
Two-thirds of depressed adolescents have at least one comorbid disorder39. After sleep disorders, anxiety is the most common comorbid mental health problem in adolescents with depression36,40. Around 75% of adolescents with depression experience symptoms of anxiety41 and up to a quarter of depressed adolescents also meet diagnostic criteria for generalized anxiety disorder36,42. Although we focus on depression in this Review, we briefly summarize the interplay between sleep, depression and anxiety in Box 1.
Box 1 Anxiety, depression and sleep.
Poor adolescent sleep quality might be linked to the development of anxiety disorders178. From a neurobiological perspective, poor adolescent sleep is associated with reduced myelination of anterior white matter tracts and fronto-limbic connectivity, both of which are required to evaluate negative emotions156. In other words, when circadian shifts disrupt adolescent sleep, the brain has less opportunity to create connections in areas essential for processing emotions, and hence anxiety disorders are likely to develop156. The relationship between decreased sleep and increased anxiety disorders might be bidirectional, with poor sleep influencing daytime emotion regulation and hyperarousal delaying the onset of sleep. However, the evidence suggests that poor sleep is more likely to precede the development of anxiety175,178 than the other way around.
Decreased ability to process emotions due to impaired sleep could also contribute to depression175, especially considering shared psychological processes across anxiety, depression and sleep, such as negative cognitive biases, catastrophizing, rumination and worry175,179.
Biological, psychological and social mechanisms might interact to increase the risk of developing insomnia, anxiety or depression during adolescence (see the review in ref.175). The high comorbidity rate (between 10–50% in community samples179) between depression and anxiety in adolescence is therefore unsurprising.
Despite the triadic interplay of anxiety, depression and sleep, poor sleep often precedes these disorders175. Thus, early intervention of sleep difficulties may prevent future anxiety and/or depression175, and sleep intervention should be considered as a first approach for prevention and intervention.
The biology of adolescent sleep
The timing of when humans sleep is primarily governed by two distinct, yet inter-related, biological processes. Together, these form the ‘two-process model of sleep’43. Here, we describe these biological sleep processes, how they change over adolescent development, and how a late sleep onset may ensue.
Development of sleep homeostatic pressure
Human physiology strives for sleep–wake equilibrium. The sleep homeostatic process (also called process S43) depends on previous sleep and wake time. Sleep pressure progressively accumulates throughout wakefulness, and dissipates during sleep. Although the neuroanatomical locus of homeostatic regulation is not yet known, several biochemical factors, such as adenosine, have been shown to be involved44. The most prominent marker for the sleep homeostatic process is sleep electroencephalogram (EEG) slow-wave activity, which is defined as activity within the EEG frequency range of 0.75–4.5 Hz during non-rapid eye movement sleep. Slow-wave activity demonstrates dose-dependent increases in response to prolonged wakefulness45. That is, the greater the amount of time spent awake, the greater the slow-wave activity during sleep, indicating a homeostatic balance between wake and sleep.
The sleep homeostatic process evolves throughout the first two decades of life. Newborn infants have low tolerance for extended wakefulness. The development of an intrinsic bioregulatory process during infancy and young childhood enables multiple sleep periods throughout the 24-hour day to converge into a single, monophasic nocturnal sleep episode46. During adolescence, a further ‘developmental leap’ occurs. Slow-wave activity declines by approximately 40%, with the greatest reductions occurring at approximately 12.5 and 13.5 years of age for girls and boys, respectively47,48. This decline in slow-wave activity is associated with synaptic pruning. Some researchers suggest that diminished synaptic activity during wakefulness underlies the diminished need for sleep recuperation during adolescence. Thus, the lower slow-wave activity during adolescent (compared to childhood) sleep reflects a reduced need to recover from extended wakefulness49,50.
Furthermore, the accumulation of sleep pressure during wakefulness undergoes marked developmental changes during adolescence. In a seminal study51, post-pubertal adolescents showed reduced sleep pressure during sleep deprivation compared to pre-pubertal adolescents. This finding suggests that maturation during adolescence allows individuals to remain awake longer. Sleep propensity (the ability to transition from wakefulness to sleep) is lower in mature versus prepubertal adolescents following 14.5 hours, 16.5 hours and 18.5 hours of sustained wakefulness52. Similar patterns have been found in adolescent mice, whereby mature compared to younger individuals made fewer sleep attempts during a sleep deprivation paradigm53. Together, these findings index a growing physiological ability for extended wakefulness in adolescence, which might account for delayed bedtimes.
The rate at which sleep pressure builds during wakefulness decelerates in older adolescents. By contrast, the rate at which sleep pressure dissipates during sleep remains stable across adolescent development46,54. This stability suggests that the need for sleep does not substantially change throughout adolescence. Indeed, evidence from waking performance (for example, performance on a psychomotor vigilance task6,55), and from self-reports of sleepiness6 and mood56 assessed as a function of sleep duration, indicate an optimal sleep period of 9.0–9.3 hours per night across adolescence.
Two studies modelling the regulation of sleep homeostatic pressure during chronic sleep restriction (5 hours in bed over five or more nights) in older adolescents (15–17 years old) reveal an increase in slow-wave activity and decrease in slow wave energy (a combination of sleep intensity and duration measured via EEG) following chronic curtailed compared to adequate sleep opportunities5,57. These studies suggest that — like adults58 — adolescents do not adapt to continuous sleep loss, and sleep homeostasis remains operative during chronic sleep restriction. Thus, as adolescents mature, they are physiologically prepared to stay awake later. Yet they still require the same amount of sleep as at the onset of puberty, and do not physiologically adjust to chronic sleep loss.
Development of delayed circadian timing
The second biological process involved in regulating sleep is the 24-hour circadian rhythm (also called process C43,45,59). This bioregulatory mechanism interacts with, but is mostly independent of, prior wake time (homeostatic process2,60) in adolescents. The circadian process regulates sleep propensity during the approximately 24-hour day, with diurnal humans falling asleep at some time in the evening. Circadian rhythms can be measured biologically (for example, melatonin levels across the evening)61,62, physiologically (for example, body temperature measured continuously across more than 24 hours)63,64 and behaviourally (for example, reaction time measured at intervals across more than 24 hours)65.
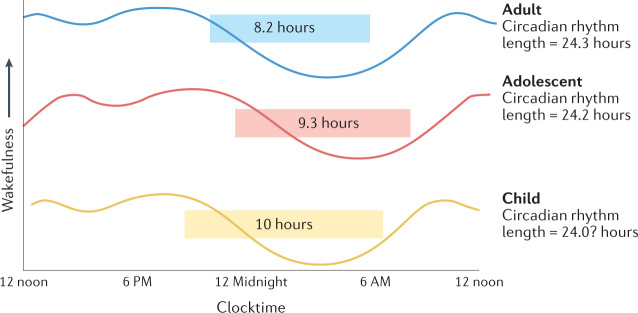
Although there are a number of biological clocks, the primary circadian clock resides in the suprachiasmatic nucleus in the anterior hypothalamus of the brain66. This master clock helps to regulate daily rhythms via photic input (that is, light and dark signals) from the retinas66. The daily oscillations of brain cell processes in the suprachiasmatic nucleus are not precisely 24 hours long. Thus, for most adolescents, the circadian cycle is slightly longer than 24 hours (on average, 24.2 hours)67–69. An adolescent’s circadian clock must therefore be reset each day to prevent sleep timing from drifting later and conflicting with school start times. External cues such as ambient light help to stabilize an adolescent’s sleep timing, and prevent a conflict between school start times and their natural wake time69,70.
Adolescents undergo drastic physiological alterations in the timing of their circadian rhythms and sleep patterns2,71. Relative to children, adolescent circadian rhythms are markedly delayed in their timing60 (Fig. 2). Thus, independent of sleep homeostatic pressure, adolescents have a strong tendency to stay up later than children do, owing to a delay in their circadian timing of sleep, and subsequently might experience delayed spontaneous morning arousal72,73. This circadian-driven evening arousal persists until about 20–21 years of age, and then begins to decline across young, middle and older adulthood1.
Fig. 2. Circadian rhythm and optimal sleep duration.
Circadian rhythm length, timing relative to clock time and optimal sleep duration (shaded boxes) for adolescents, children and adults. There are small differences in circadian rhythm length but significant differences in the timing of major peaks and troughs across development.
When circadian rhythms and sleep-wake patterns become delayed, adolescents have difficulty falling asleep at an earlier, more conventional time, analogous to sleep-onset insomnia74,75. Once asleep, adolescents have objectively and subjectively good-quality sleep76. However, owing to the combination of their delayed sleep onset and forced early awakenings to meet school commitments, their sleep becomes restricted across the 5-day school week71. This accumulation of insufficient sleep leads to daytime impairments (for example, low motivation and low mood) across the week77 and across school terms78. Although adolescents are afforded two consecutive days where no morning commitments might exist (that is, weekends), adolescents do not fully recover after two consecutive days of recovery sleep (as measured by tests of sustained attention)79. Moreover, sleeping in on weekends might exacerbate circadian delay in adolescents because they will lose the resetting benefits of morning bright light73,80. Weekend sleep-ins can therefore lead to further difficulty falling asleep on Sunday night and waking on Monday morning, resetting a weekly cycle80. When the delay in sleep timing becomes chronic and extremely late, such that it interferes with important aspects of the adolescent’s life (such as attending school), the adolescent might be diagnosed with a condition known as delayed sleep–wake phase disorder81.
Adolescent sleep and depression
The biological characteristics of adolescent sleep described above lead to sleep loss and delayed circadian timing, both of which have implications for depression. Moreover, the resulting inability to fall asleep has psychological consequences that might also contribute to adolescent depression. In this section, we discuss each of these factors and their contribution to adolescent depression.
Sleep loss and depression
Logical arguments have been provided for a bidirectional link between adolescent sleep and depression: poor sleep is a risk factor for depression, and depression leads to poor sleep82. However, a meta-analysis of prospective and experimental data suggests a greater tendency for poor sleep to lead to depression in adolescents than the other way around37. This meta-analysis also found that all longitudinal studies where sleep problems (specifically, sleep onset latency and wake after sleep onset) predicted depression used the gold standard measurement of sleep (polysomnography). By contrast, all studies that found that depression predicted later sleep problems used self-reports37. Because depressed adolescents might have negative perceptions of their sleep, the direction of effects from depression to sleep problems needs to be verified with objective sleep measures (such as polysomnography).
There is a longitudinal association between insufficient sleep and subsequent depressed mood in non-clinical groups of adolescents83. Analysis of the temporal relationship between sleep and next-day mood in clinical and non-clinical groups of adolescents showed that 9 hours of sleep per night was needed for optimal next-day mood56. The relationship between sleep duration and mood was U-shaped, with sleep durations longer and shorter than 9 hours associated with worse next-day depressed mood56. The impact of sleep loss was felt more keenly among adolescents experiencing clinically significant internalizing symptoms, who needed more sleep than adolescents below the clinical range56. This result suggests a differential vulnerability to the effects of sleep loss among adolescents, with those experiencing symptoms of psychopathology more at risk of experiencing insufficient sleep.
Insufficient sleep causally affects several risk factors for depression, including mood valence84–86. Multiple studies find large effects of insufficient sleep on the ability of adolescents to experience positive affective states, such as happiness, enthusiasm and excitement (for a review see ref.87). A meta-analytic review of 74 studies of 361,505 adolescents found that less sleep was associated with a 55% increase in the likelihood of emotional deficits87. A decrease in positive mood showed the largest effect, followed by increases in anger, depression, negative affect and anxiety.
Another mechanism by which sleep loss can lead to depression is through its effect on emotion regulation. Emotion regulation is a key transdiagnostic risk factor for a range of negative psychological sequelae88. Experimental studies have found that the ability of adolescents to regulate their emotions varies according to prior sleep84–86. A physiological mechanism may be at play: the limbic system, which is involved in emotion regulation, might be functionally affected by sleep loss. Thus, sleep loss affects the ability of adolescents to regulate emotions at a physiological level89.
Delayed circadian timing and depression
In addition to restricted sleep duration, the delayed sleep timing of adolescents also contributes to depression90. Studies investigating the association between circadian rhythm and depression have focused on biological, behavioural and social aspects. Biological markers, such as the timing of melatonin production, are more precise measures of circadian timing, followed by self-reported chronotype (a measure of actual sleep behaviour, that is, the midpoint of sleep calculated from adolescents’ reports of their sleep onset and wake times) and, finally, evening versus morning preference for daily activities (for example, their preference for when they choose to eat meals, study and exercise)90. When measured simultaneously, those who report an evening preference, delayed chronotype and show a delayed circadian phase also report more symptoms of depression91. Similarly, independent studies have found that adolescents and young adults with elevated symptoms of depression concurrently report delayed circadian timing92, later chronotype93 and a preference for evening activities94,95. Together, these studies suggest consistent links between different indicators of altered circadian timing and depression.
Beyond concurrent associations, longitudinal studies point to a reciprocal association between delayed circadian timing and symptoms of depression. Several studies have shown that adolescents who preferred evening activities were more likely to subsequently report depressive symptoms96–98, and one study found that depressed adolescents were more likely to subsequently develop an evening preference99. A bidirectional association between circadian timing and depression is not surprising, given that both share similar biological and psychological underpinnings that might maintain and exacerbate each other over time100.
Taken to the extreme, an adolescent with altered circadian timing would sleep during the day and be awake at night. But even much less dramatic alterations mean that an adolescent’s body clock is not synchronous with the environment and society, with consequences such as school tardiness, and missing morning classes or entire school days101. An adolescent who is asleep during the day will miss opportunities to be exposed to the circadian-rhythm-resetting properties of bright light73, to be physically active and to socialize with friends and family. Bright light, physical activity and connectedness with people are closely related to a positive mood102–104. A slight elevation of depressed mood has also been reported during holiday periods, when delayed sleep timing is more pronounced as adolescents stay up later and sleep in when not attending school105. Delaying sleep onset well into the night — when family and friends are asleep — might create a mental space for rumination106, which is a powerful risk factor for depression107. Indeed, people tend to ruminate more later in the day107,108. Thus, dyssynchronization with dark-and-light cycles and society is one possible explanation for the overlap between delayed circadian timing and depression.
Alterations in the regulation of hormones, body temperature, and neurotransmitter release might also explain deficits in mood regulation100. For example, there is evidence for lower melatonin amplitude in depressed individuals, which means that melatonin levels do not rise or decline sufficiently to regulate the alternation of sleepiness and wakefulness during the day and night109. Moreover, melatonin secretion might be delayed in adolescents or even unsynchronized with other circadian processes (such as cortisol levels and body temperature) that regulate the sleep–wake cycle (for a review, see ref.110). These alterations in circadian processes affect the sleep regulation and the daily variations in energy levels, alertness and mood typically seen in depression110. Therefore, both biological and psychosocial processes, or an interaction between the two, might explain why adolescents with altered circadian timing report higher rates of depression.
The psychological contribution of adolescent sleep to depression
The changes to bioregulatory sleep processes during adolescence can lead to many sleep difficulties111. The most common sleep problem is difficulty falling asleep, measured by sleep onset latency (the number of minutes from the sleep attempt to sleep onset)4. The majority of adolescents take more than 30 minutes to fall asleep112, which in adults would qualify as sleep-onset insomnia113. However, adolescents with depression take even longer to fall asleep compared to both anxious and non-depressed counterparts114. The amount of time spent awake before falling asleep predicts future depression in adolescents37.
Adolescents and their families are generally unaware that the combined effect of a delayed circadian rhythm and reduced sleep homeostatic pressure might result in a delayed sleep onset111. Instead, adolescents tend to choose a bedtime based on the best opportunity to gain sufficient sleep (9 h in bed), rather than based on their perceived level of sleepiness115. Consequently, adolescents attempt sleep at a time of near peak-circadian alertness101, and therefore experience difficulty falling asleep (that is, sleep onset latency greater than 30 minutes). One mechanism proposed to link the time taken to fall asleep and future depression are pre-sleep cognitions (the thoughts that occur before sleep onset)37.
Although pre-sleep cognitions also occur in adult insomnia116–118, two key distinctions make adolescent pre-sleep cognitions unique. First, as described above, adolescents’ pre-sleep cognitions occur during a period of arousal driven by the circadian peak of alertness101, rather than the constant hyperarousal observed in adults with insomnia116–118. Second, the content of pre-sleep cognitions differs between adults and adolescents. For example, ‘rehearsal and planning’ (that is, thinking about the past day, past experiences, next day, things to do, planning things and forthcoming events) is a common pre-sleep cognition theme for both adults with insomnia and adolescents diagnosed with delayed sleep–wake phase disorder119,120. However, for adolescents these rehearsal and planning pre-sleep cognitions are more likely to be related to their education and friendships119. Furthermore, adolescents report such pre-sleep cognitions on both school nights and weekends, despite shorter sleep latencies on weekends due to later bedtimes121. Although the immediate implications of pre-sleep cognitions are similar between adolescents and adults (a longer time taken to fall asleep), it is the content of such pre-sleep cognitions that differs between these developmental stages.
Adolescents with depression negatively interpret events and information122, and become fixated with negative self-perceptions (for example, describing themselves as “useless”, “unimportant” and “worthless”)123. Night-time ruminative thinking overlaps with and amplifies these depressogenic thoughts123. For example, detailed pre-sleep cognitions captured during focus group interviews with adolescents suggest that pre-sleep cognitions mirror typical negative thoughts reported during depression115. In another study, adolescents were surveyed about difficulty initiating sleep, repetitive negative thinking (specifically worry and rumination) and depression124. The results showed that repetitive negative thinking fully mediated the relationship between difficulty initiating sleep and depressed mood124. Although further replication and more empirical support for the role of specific pre-sleep cognitions is needed, the initial evidence suggests that increased sleep onset latency, and subsequent pre-sleep cognitions, probably play a part in the relationship between sleep disturbance and depression in adolescents. Future studies are also needed to confirm whether such processes occur when adolescents wake during the night for extended periods of time, as this phenomenon is relatively rare in this population (compared to a long sleep latency).
Adolescent sleep interventions
Given the prevalence of adolescent sleep difficulties and their maladaptive consequences, it is clear that interventions are necessary. In this section, we outline three evidence-based interventions to resolve sleep issues that are applicable to adolescents, and for which there is evidence for reductions in depression symptoms (Table 1).
Table 1.
Summary findings of key sleep intervention studies and meta-analyses
| Sleep treatment | Contributing factor targeted | Key paper(s) | Design | Sample | Key findings |
|---|---|---|---|---|---|
| Bright light therapy | Advances the timing of an adolescent’s delayed circadian rhythm; reduces sleep onset latency; reduces the opportunity for repetitive negative thinking | Richardson et al. (2018)129 | Randomized controlled trial | Clinical (n = 60) | Bright light therapy reduces adolescents’ sleep onset latency by about 50 minutes by 3-month follow-up |
| Richardson and Gradisar (2021)128 | Randomized controlled trial | Clinical (n = 63) | Bright light therapy decreased repetitive negative thinking (d = 0.39) and depression symptoms (d = 0.83) in adolescents at 3-month follow-up | ||
| Exogenous melatonin | Advances the timing of an adolescent’s delayed circadian rhythm; reduces sleep onset latency; reduces the opportunity for repetitive negative thinking. | Wei et al. (2020)150 | meta-analysis | Clinical (n = 387) | Compared to placebo, exogenous melatonin decreased sleep onset latency by 21 minutes in children and adolescents |
| Cognitive-behaviour therapy for insomnia (CBT-I) | Reduces sleep onset latency; reduces the opportunity for repetitive negative thinking | Bootzin and Stevens (2005)161 | Single-arm study | Clinical (n = 55) | Adolescents that completed treatment reduced sleep onset latency by 19 minutes, and reported significantly less worry |
| de Bruin et al. (2015)167 | Randomized controlled trial | Clinical (n = 116) | Adolescents provided with CBT-I via group or internet format reduced their sleep onset latency by 21 minutes and 29 minutes, respectively | ||
| Blake et al. (2017)159 | Meta-analysis | Clinical (n = 221) | Within-person meta-analysis found sleep onset latency decreased by 21 minutes and depression decreased (d = 1.22) | ||
| Mindfulness body scan | Reduces sleep onset latency; reduces the opportunity for repetitive negative thinking | Bartel et al. (2018)169 | Randomized controlled trial | School-based (n = 65) | Relative to control, listening to a 15-minute body scan at bedtime for 2 weeks reduced sleep onset latency by 8 minutes for adolescents with a baseline sleep onset latency greater than 30 minutes |
d is Cohen’s d, where small effect >0.20, moderate effect >0.50, large effect >0.80.
Bright light therapy
Light is one of the most potent time-givers for the human circadian system. Bright light exposure (around 5,000 lux) close to an adolescent’s natural wake time might advance the timing of their circadian rhythm125. Consequently, bright light therapy is usually used to treat a delayed circadian rhythm experienced by adolescents126. Bright light therapy involves post-awakening light exposure, usually via natural sunlight or bright-light-emitting devices (lamps or portable light glasses)127. Bed and wake times, and post-awakening light exposure, are then scheduled to become gradually earlier until the desired sleep timing is achieved. Bright light therapy effectively treats the symptoms of delayed sleep–wake phase disorder, including depression symptoms, experienced by adolescents101,128.
Bright light therapy alone129,130 or in combination with cognitive behavioural therapy101,131 improves a range of sleep parameters (advances sleep timing, shortens sleep onset latency and increases sleep duration) and daytime functioning (decreases sleepiness and fatigue and increases cognitive functioning)132,133 in adolescents with delayed sleep–wake phase disorder. Despite experimental evidence with adults that bright light should be more effective than dim light134, and short-wavelength light (for example, blue light) should be more effective than long-wavelength light (for example, red light)135, randomized controlled trials with adolescents have failed to replicate these effects129,130. These results suggest that evening light restriction and sleep scheduling might be important treatment components136. The addition of cognitive behavioural therapy to bright light therapy has been shown to provide benefits to adolescents beyond sleep improvements, such as decreased depression symptoms101,126,131.
Although the mechanism for linking bright light therapy to improved sleep outcomes is clear (light advances circadian timing and therefore advances sleep timing), the mechanisms for linking bright light to improvements in depression are less so. One possibility is that doses of bright light directly affect mood. A feasibility study found that 30 minutes of post-awakening light exposure improved depressive symptoms and sleep quality in moderately-to-severely depressed adolescents who were hospital inpatients137. Short-wavelength light (10,000 lux) administered via portable light glasses was just as effective at reducing depression symptoms as broad-spectrum white light (10,000 lux) administered via a light lamp137. It is possible that light therapy indirectly improves depressed mood via improvements in sleep. For example, reducing sleep onset latency and associated repetitive negative thinking138, or reducing the misalignment in biological circadian timing with one’s social timing, might mitigate depression symptoms90. Indeed, data from a clinical trial suggests that bright light therapy for adolescents diagnosed with delayed sleep–wake phase disorder reduces sleep onset difficulties, repetitive negative thinking (both sleep- and non-sleep-related) and depressed mood128.
Finally, in contrast to the depressogenic outcomes from chronic sleep loss over weeks and months described thus far, acute sleep deprivation over a short number of days (sometimes referred to as wake ‘therapy’) actually shows an anti-depressant effect139. The combined effect of bright light therapy and wake therapy has been explored in depressed adolescent inpatients. Results suggest that a combined approach is no more effective than bright light therapy alone139. Similarly, bright light therapy alone appears to be as effective as bright light therapy plus medication (fluoxetine) for adult depression (fluoxetine alone was no more effective than placebo)140. The effect of combined bright light therapy and medication has not yet been explored in adolescent populations.
Exogenous melatonin
Melatonin is a neurohormone that aids the onset of sleep141. Endogenous melotonin is naturally produced by the pineal gland in the absence of light in the evening, and is suppressed during the day with re-exposure to light, thereby following a 24-hour circadian rhythm142. Exogenous melatonin is taken as a dietary supplement to complement melatonin produced by the body143,144. As children develop into adolescents, their endogenous melatonin is produced later in the night, contributing to later sleep times145. To correct this delay, exogenous melatonin delivered in the evening can produce a ‘pulling’ effect such that a person’s circadian rhythm timing gradually becomes earlier127,146. The timing and dosage of exogenous melatonin administration is often individually tailored. However, exogenous melatonin is most effective when delivered in immediate-release form, at least 1–3 h before expected sleep onset, and in doses of up to 3 mg (refs143,147). Melatonin use can typically cease once the individual reaches their desired sleep time, and is therefore not a long-term treatment127.
The use of melatonin as a paediatric sleep treatment has increased in popularity over the past two decades146,148–152. Consequently, many studies have emerged investigating its efficacy. A systematic review of sleep treatments for children younger than 18 years old showed that exogenous melatonin significantly improved sleep latency, sleep duration and night-time awakenings across 19 randomized controlled trials148. Furthermore, a meta-analysis found that exogenous melatonin improved both sleep onset latency and total sleep time compared to placebo across seven trials with 387 children and adolescents150. Exogenous melatonin successfully advances circadian timing in adolescents with delayed circadian phase130,133,149. However, there have been other mixed findings. Some research suggests that exogenous melatonin improves sleep timing but not sleep onset latency147. Other studies have found improvements for sleep onset latency144,151, but not total sleep time144. On balance, the overall body of evidence suggests that exogenous melatonin is effective as a treatment for at least some sleep difficulties148,150.
Exogenous melatonin has the potential to improve symptoms of both sleeplessness and depression because it reduces time awake in bed (by shortening sleep latency)151, and phase-advances circadian rhythm timing130,133,147. Additionally, exogenous melatonin has shown efficacy in combination with other evidence-based treatments. For example, sleep interventions that combine bright light therapy with exogenous melatonin have shown improvements from baseline in sleep onset latency, total sleep time and circadian timing130. Furthermore, the benefits of combining exogenous melatonin and bright light therapy might be maintained longer compared to either treatment alone130. A combination of exogenous melatonin and bright light therapy might therefore be particularly effective at treating comorbid depression and sleep difficulties. Indeed, based on meta-analytic results a task force of sleep experts recommended exogenous melatonin to treat both sleep and comorbid psychiatric conditions in children and adolescents with delayed sleep–wake phase disorder126.
Contrary to the lay person’s beliefs, exogenous melatonin does not cause feelings of sleepiness in most adolescents and adults, and therefore is not akin to other sedative medications152. However, exogenous melatonin can have a sleep-inducing effect in addition to circadian benefits153 in children, leading to increased popularity for parents who wish to improve their children’s sleep. But, there is also controversy in the medical community about the use of melatonin146,149. Specifically, there is debate regarding the safety of melatonin use in paediatric populations143,154. Safety concerns stem largely from animal models suggesting that exogenous melatonin impairs reproduction and other physiological systems154. Opposing arguments are based on the fact that exogenous melatonin in paediatrics is generally safe, and is not associated with adverse side effects, even in long-term studies155. There is general agreement that more long-term studies with paediatric populations are needed to reach a consensus regarding safety155. Nonetheless, in adolescents exogenous melatonin is most often used to improve circadian timing and therefore is recommended for short-term use (a few weeks)147, not long-term use. Indeed, a meta-analysis of studies investigating short-term paediatric melatonin use revealed little to no difference in side effects in exogenous melatonin users compared to placebo150.
Cognitive and behavioural techniques
As previously discussed, a long sleep latency provides more opportunities for adolescents to worry and ruminate128. This is confirmed by a review of neuroimaging studies that suggested that sleep latency predicted future worry during adverse events156. Bright light therapy and/or exogenous melatonin can reduce this opportunity for repetitive negative thinking by advancing sleep onset. However, these interventions might not sufficiently reduce negative pre-sleep cognitions for some adolescents157. Furthermore, an adolescent’s long sleep latency might be due to other factors, such as insomnia, rather than delayed circadian rhythm alone. Cognitive and behavioural sleep interventions can simultaneously address these additional sleep issues and depression158. Indeed, a meta-analysis of cognitive-behavioural sleep interventions demonstrated clear subjective improvements to sleep (sleep duration, sleep latency, sleep efficiency and waking after sleep onset), objective improvements to sleep (sleep latency and efficiency) and decreased depression and anxiety symptoms159.
Cognitive behaviour therapy for insomnia (CBT-I) was originally developed for adults experiencing insomnia160. However, its potential for use in adolescents has been demonstrated over the past 15 years161,162. CBT-I targets both the adolescent’s sleep behaviours and cognitions. Behavioural techniques include calibrating an adolescent’s time in bed to reduce wakefulness in bed while ensuring sufficient opportunity for restorative sleep, and stimulus control therapy that increases the odds of falling asleep through associations with discrete stimuli (for example, lying down in bed)161. Relaxation training is also used to reduce physiological arousal, and sleep hygiene improves the adolescent’s bedroom environment (for example, a dark, quiet bedroom and comfortable bedding) and pre-sleep behaviours (for example, reducing stimulating activities before going to bed)161. Cognitive techniques address adolescents’ unhelpful thoughts when attempting sleep by critically evaluating them and generating alternative helpful thoughts161. CBT-I typically involves four to six sessions, and effectively decreases sleep latency following the intervention, although there is mixed evidence as to whether this improvement is maintained159,163. These combined cognitive and behavioural approaches for insomnia show promise for improving depression, as evidenced by meaningful declines in self-reported depression scores by the end of CBT-I159,164. Indeed, a meta-analysis found that treating adolescent sleep issues reduces depression symptoms165. Moreover, a pilot study in which adolescents presenting with insomnia and co-morbid anxiety, depression or pain were treated with CBT-I for six weeks found pre-to-post-treatment improvements in insomnia, depression and anxiety symptoms166.
Unlike bright light therapy and exogenous melatonin, CBT-I is not a singular treatment, and it might take longer to implement101. CBT-I is considered a ‘modular approach’ (that is, each behavioural and cognitive technique is considered a ‘module’), and we therefore have a limited understanding of which specific CBT-I techniques for adolescent sleep problems are more potent in improving sleep and depression167,168. Furthermore, the greater number of sessions needed to implement CBT-I (compared to bright light therapy and exogenous melatonin) means that it is a less cost-effective therapy for adolescents with sleep problems.
These issues have led some researchers to explore the effect of single stand-alone cognitive or behavioural techniques on adolescents’ sleep. For example, a randomized trial conducted in schools found that constructive worry (a cognitive technique where adolescents wrote down their worries and solutions before bed) did not influence sleep latency relative to a control condition169. By contrast, a mindfulness body scan technique at bedtime that aimed to focus thoughts on the present moment reduced the time taken to fall asleep by more than 50% for adolescents experiencing sleep-onset insomnia (that is, a sleep latency greater than 30 minutes)169. A mindfulness body scan, combined with instructions for good sleep hygiene (including a comfortable sleep environment, consistent bed and wake times, relaxing before bed and avoiding pre-bed stimulation), also decreased sleep latency in high-level junior tennis players during a tournament week170. Although not a standard behavioural technique for treating insomnia, one study found that restricting adolescents’ smartphone use before bed did not influence the time taken to fall asleep, but increased total sleep time by 19 minutes per night171. We can only infer that reducing sleep latency, or increasing total sleep time, would decrease depression symptoms, as these studies testing single therapeutic techniques did not simultaneously measure levels of depression.
Summary and future directions
The combination of developmental changes to the bioregulatory systems controlling sleeping and waking during adolescence provides unique pathways to depression. First, reduced sleep homeostatic pressure delays the onset of sleep in mature adolescents52. This delayed sleep onset restricts sleep opportunity on school nights, making it difficult for adolescents to achieve the optimal 9.3 hours of sleep. Empirical evidence shows that reductions in positive mood states occur following sleep loss, which in turn increases depression symptoms87. Second, there is a gradual delay in sleep timing (both sleep onset and offset) due to a delay in circadian rhythm timing across adolescent development71. Delayed circadian rhythm exacerbates delayed sleep onset, and is consistently associated with increased depression symptoms90. These biological underpinnings are unique to adolescent development, and cast doubt on models that posit that evening technology use is a cause for poor adolescent sleep172–174 (Box 2). The physiologically driven delay in sleep onset provides the opportunity for a third pathway to depression that is more psychological. More time between an adolescent’s bedtime and sleep onset increases the probability of experiencing negative pre-sleep cognitions124. This opportunity for repetitive negative thinking is linked to higher levels of depression in adolescents124.
Identifying these unique biological and psychological contributors that work in concert to produce delayed sleeping patterns is important because they can be matched to evidence-based techniques to reverse poor sleep and depressed mood. The gradual advance of bright light exposure in the morning (bright light therapy) and the gradual advance of evening exogenous melatonin can advance the timing of the circadian rhythm129,130,133. Doing so advances sleep onset to earlier in the evening, shortening sleep onset latency. These chronotherapies not only shorten adolescent sleep onset latency, but also decrease depressive symptomology via reduced negative pre-sleep cognitions when attempting sleep128. However, these treatments do not fully resolve sleep issues and depression symptoms. Thus, cognitive therapy techniques can be used to target residual sleep difficulties and depressed mood. Together, the clinical and meta-analytic evidence, and the cost-effectiveness of sleep interventions, suggest that they should be used in the first instance when adolescents experience co-morbid depression and sleep problems165.
An array of potential mechanisms link sleep and depression in adolescents175. Thus, further research is needed to explore the potential of bright light therapy for adolescent depression, given that only one study to date has tested multiple mechanistic pathways in the same sample126. Future research should also explore potential benefits of deploying interventions sequentially. For examples, it might be useful for adolescents who experience significant depression alongside sleep problems to start with exogenous melatonin treatment. Taking exogenous melatonin is less energy-intensive than other sleep interventions, which might increase the uptake of sleep interventions by adolescents who are fatigued by co-morbid depression and sleep problems. The adolescent might then be better able to engage in more energy-taxing interventions such as bright light therapy or concurrent cognitive behavioural therapy. However, this needs to be tested empirically.
Furthermore, we lack data that track the natural course and development of sleep problems due to evolving homeostatic and circadian changes over adolescent development. Longitudinal studies are needed to determine at what ages underlying biological sleep changes and depression symptoms occur. This will help to pinpoint when prevention studies for adolescent sleep problems — which are currently lacking176 — should be conducted. Future research is also needed to convert efficacy trials into broader effectiveness studies performed in health care, school and digital settings. The paediatric sleep literacy (that is, the sleep knowledge, practices and attitudes) of health professionals has much room for improvement177, suggesting that substantial efforts are needed to translate clinical research evidence to adolescent mental health practice. Given the worldwide prevalence of sleep problems, extrapolating this clinical evidence to a stepped-care model (for example, sleep prevention and intervention in high schools, intensive sleep interventions for adolescents on mental health service waiting lists, and accessible digital sleep interventions) for adolescents is needed.
Box 2 Evening technology use and adolescent sleep.
Multiple pathways connecting evening technology use and sleep in adolescents have been proposed172,173. First, technology use might increase arousal that delays the onset of sleep. Second, the blue light emitted from LED screens might promote alertness and delay sleep onset. Finally, according to the displacement hypothesis, adolescents might continue using technology past their usual sleep onset time and thereby restrict their sleep174.
Tests of the arousal mechanism usually compare conditions in which adolescents participate in highly interactive technology use before bed (for example, playing a violent videogame) versus engage with less interactive technology (for example, watching TV) or they compare small (50 minutes) versus moderate (150 minutes) periods of violent videogames before sleep. Differences in the time taken to fall asleep between conditions in these experiments have been minimal (mean differences <5 minutes)180–183.
Owing to a lack of support for the arousal mechanism, researchers turned towards testing the influence of blue light from LED screens. Methods for reducing these blue light emissions include wearing blue-light-blocking glasses184 and apps that decrease blue light emissions (for example, f.lux and Apple’s nightshift mode)185,186. Mean differences in the time taken to fall asleep between these blue light-reducing conditions and control are again minimal (mean differences <10 minutes)184–187.
By contrast, tests of the displacement hypothesis have yielded more substantial effects (for example, delaying bedtime by 1.5 hours)188. However, bedtime delays only occur when there is an interaction between personality characteristics (such as risk-taking, flow state, self-control and bedtime procrastination) and the type of technology consumed before sleep188–190. Although empirical support is more substantive for the bedtime displacement mechanism, the emerging evidence suggests that technology use does not influence all adolescents in the same way.
‘Social media and networking’ is a component in one of the most cited explanatory models of adolescent sleep2,71. However, a meta-analysis of all risk and protective factors for adolescent sleep identified in the published literature found no significant relationship between any form of technology (TVs, phones, internet and video gaming) and sleep onset latency (all weighted correlation coefficients r < 0.01)191. Overall, the influence of technology use on sleep was lower than other factors, including tobacco and alcohol use and family factors (such as parent-set bedtimes)191. Moreover, all factors combined explained only roughly a quarter of the variance in adolescents’ sleep duration191. Thus, the evidence to date casts doubt on the existence of a significant influence of evening technology use on adolescents’ sleep.
Instead, longitudinal studies suggest that an increase in poor sleep is followed by an increase in technology use192,193. Adolescents with sleep-onset difficulties report substantial negative pre-sleep cognitions119. When surveyed, the majority of adolescents report that using technological devices might aid in the onset of sleep194. This finding suggests that using evening technology might benefit adolescents. Specifically, using devices while waiting for sleep onset might be a form of cognitive distraction from negative pre-sleep cognitions195. Cross-sectional associations have been found between using social media to cope with negative feelings and sleep-onset difficulties in adolescents196. In the context of the abovementioned studies this finding could be interpreted as the use of evening technology as a coping mechanism for a delayed sleep onset.
Acknowledgements
The authors thank the hundreds of families who have participated in the authors’ and colleagues research, sharing their knowledge so that we could provide the reader with this Review.
Glossary
- Polysomnography
A comprehensive test used to diagnose sleep disorders that includes measures of brain waves, blood oxygen level, heart rate, breathing and eye and leg movements.
Author contributions
The authors contributed equally to all aspects of the article.
Peer review
Peer review information
Nature Reviews Psychology thanks Melynda Casement and the other, anonymous, reviewers for their contribution to the peer review of this work.
Competing interests
M.G. is the CEO of WINK Sleep Pty Ltd, and as such receives income from the sale of online courses for treating adolescent sleep problems. All other authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Roenneberg T, et al. A marker for the end of adolescence. Curr. Biol. 2004;14:R1038–R1039. doi: 10.1016/j.cub.2004.11.039. [DOI] [PubMed] [Google Scholar]
- 2.Carskadon MA. Sleep in adolescents: the perfect storm. Pediatr. Clin. North Am. 2011;58:637–647. doi: 10.1016/j.pcl.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gariepy G, et al. How are adolescents sleeping? Adolescent sleep patterns and sociodemographic differences in 24 European and North American countries. J. Adolesc. Health. 2020;66:S81–S88. doi: 10.1016/j.jadohealth.2020.03.013. [DOI] [PubMed] [Google Scholar]
- 4.Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. 2011;12:110–118. doi: 10.1016/j.sleep.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 5.Ong JL, Tandi J, Patanaik A, Lo JC, Chee MWL. Large-scale data from wearables reveal regional disparities in sleep patterns that persist across age and sex. Sci. Rep. 2019;9:3415. doi: 10.1038/s41598-019-40156-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Short MA, Weber N, Reynolds C, Coussens S, Carskadon MA. Estimating adolescent sleep need using dose-response modelling. Sleep. 2018;41:zsy011. doi: 10.1093/sleep/zsy011. [DOI] [PubMed] [Google Scholar]
- 7.Short MA, et al. A cross-cultural comparison of sleep duration between US and Australian adolescents: the effect of school start time, parent set bedtimes, and extracurricular load. Health Educ. Behav. 2013;40:323–330. doi: 10.1177/1090198112451266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bowers JM, Moyer A. Effects of school start time on students’ sleep duration, daytime sleepiness, and attendance: a meta-analysis. Sleep Health. 2017;3:423–431. doi: 10.1016/j.sleh.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 9.Becker SP, et al. Prospective examination of adolescent sleep paterrns and behaviors before and during COVID-19. Sleep. 2020;44:zsab054. doi: 10.1093/sleep/zsab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gruber R, Saha S, Somerville G, Boursier J, Wise MS. The impact of COVID-19 related school shutdown on sleep in adolescents: a natural experiment. Sleep Med. 2020;76:33–35. doi: 10.1016/j.sleep.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meltzer LJ, et al. COVID-19 instructional approaches (in-person, online, hybrid), school start times, and sleep in over 5,000 U.S. adolescents. Sleep. 2021;44:zsab180. doi: 10.1093/sleep/zsab180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barnes M, et al. Setting adolescents up for success: promoting a policy to delay high school start times. Sch. Health Policy. 2016;86:552–557. doi: 10.1111/josh.12405. [DOI] [PubMed] [Google Scholar]
- 13.Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16:258–262. doi: 10.1093/sleep/16.3.258. [DOI] [PubMed] [Google Scholar]
- 14.Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues Clin. Neurosci. 2009;11:7–20. doi: 10.31887/DCNS.2009.11.1/krmerikangas. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatr. 2015;56:345–365. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- 16.Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet. 2012;379:17–23. doi: 10.1016/S0140-6736(11)60871-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol. Rev. 2008;115:291–313. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]
- 18.Rice F, Harold G, Thapar A. The genetic aetiology of childhood depression: a review. J. Child Psychol. Psychiat. 2002;43:65–79. doi: 10.1111/1469-7610.00004. [DOI] [PubMed] [Google Scholar]
- 19.Tully EC, Iacono WG, McGue M. Ad adoption study of parental depression as an environmental liability for adolescent depression and childhood disruptive disorders. Am. J. Psychiat. 2008;165:1148–1154. doi: 10.1176/appi.ajp.2008.07091438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goodyer I, Wright C, Altham P. The friendships and recent life events of anxious and depressed school-age children. Br. J. Psychiat. 1990;156:689–698. doi: 10.1192/bjp.156.5.689. [DOI] [PubMed] [Google Scholar]
- 21.Pine DS, Cohen P, Johnson JG, Brook JS. Adolescent life events as predictors of adult depression. J. Affect. Dis. 2002;68:49–57. doi: 10.1016/S0165-0327(00)00331-1. [DOI] [PubMed] [Google Scholar]
- 22.Hawker DSJ, Boulton MJ. Twenty years’ research on peer victimization and psychosocial maladjustment: a meta-analytic review of cross-sectional studies. J. Child Psychol. Psychiat. 2000;41:441–455. doi: 10.1111/1469-7610.00629. [DOI] [PubMed] [Google Scholar]
- 23.Dunn V, Goodyer IM. Longitudinal investigation into childhood- and adolescent-onset depression: psychiatric outcome in early adulthood. Br. J. Psychiat. 2018;188:216–222. doi: 10.1192/bjp.188.3.216. [DOI] [PubMed] [Google Scholar]
- 24.Harrington, R., Dubicka, B. Natural history of mood disorders in children and adolescens. In The Depressed Child and Adolescent 2nd edn (ed. Goodyer, I. M.) (Cambridge Univ. Press, 2001).
- 25.Fergussin DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Arch. Gen. Psychiat. 2002;59:225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- 26.Halperin JM, Rucklidge JJ, Powers RL, Miller CJ, Newcorn JH. Childhood CBCL bipolar profile and adolescent/young adult personality disorders: a 9-year follow-up. J. Affect. Dis. 2011;130:155–161. doi: 10.1016/j.jad.2010.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rudolph KD, Klein DN. Exploring depressive personality traits in youth: origins, correlates, and developmental consequences. Dev. Psychopathol. 2009;21:1155–1180. doi: 10.1017/S0954579409990095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fergusson DM, Boden JM, Horwood LJ. Recurrence of major depression in adolescence and early adulthood and later mental health, educational and economic outcomes. Br. J. Psychiat. 2007;191:335–342. doi: 10.1192/bjp.bp.107.036079. [DOI] [PubMed] [Google Scholar]
- 29.Franko DL, Striegel-Moore RH, Thompson D, Schreiber GB, Daniels SR. Does adolescent depression predict obesity in black and white young adult women? Psychol. Med. 2005;35:1505–1532. doi: 10.1017/S0033291705005386. [DOI] [PubMed] [Google Scholar]
- 30.Gotlib IH, Lewinsohn PM, Seeley JR. Consequences of depression during adolescence: marital status and marital functioning in early adulthood. J. Abnorm. Psychol. 1998;107:686–690. doi: 10.1037/0021-843X.107.4.686. [DOI] [PubMed] [Google Scholar]
- 31.Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J. Child. Psychol. Psychiat. 2006;47:372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- 32.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
- 33.Fried EI. Problematic assumptions have slowed down depression research: why symptoms, not syndromes are the way forward. Front. Psychol. 2015;6:309. doi: 10.3389/fpsyg.2015.00309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goodyer IM, et al. Cognitive behavioural therapy and short-term psychoanalytical psychotherapy versus a brief psychsocial intervention in adolescents with unipolar major depressive disorder (IMPACT): a multicentre, pragmatic, observer-blind, randomised controlled superiority trial. Lancet Psychiat. 2017;4:109–119. doi: 10.1016/S2215-0366(16)30378-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Loades ME, et al. Depression symptom clusters in adolescents: a latent class analysis in a clinical sample. Psychother. Res. 2022 doi: 10.1080/10503307.2022.2030498. [DOI] [PubMed] [Google Scholar]
- 36.Orchard F, Pass L, Marshall T, Reynolds S. Clinical characteristics of adolescents referred for treatment of depressive disorders. Child. Adolesc. Ment. Health. 2017;22:61–68. doi: 10.1111/camh.12178. [DOI] [PubMed] [Google Scholar]
- 37.Lovato NL, Gradisar M. A meta-analysis and model of the relationship between sleep depression in adolescents: recommendations for future research and clinical practice. Sleep Med. Rev. 2014;18:521–529. doi: 10.1016/j.smrv.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 38.de Zambotti M, Goldstone A, Colrain IM, Baker FC. Insomnia disorder in adolescence: diagnosis, impact and treatment. Sleep Med. Rev. 2018;39:12–24. doi: 10.1016/j.smrv.2017.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ford T, Goodman R, Meltzer H. The British child and adolescent mental health survey 1999: the prevalence of DSM-IV disorders. J. Am. Acad. Child. Adolesc. Psychiat. 2003;42:1203–1211. doi: 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- 40.Angold A, Costello EJ, Erkanli A, Worthman CM. Pubertal changes in hormone levels and depression in girls. Psychol. Med. 1999;29:1043–1053. doi: 10.1017/S0033291799008946. [DOI] [PubMed] [Google Scholar]
- 41.Essau, C. A. & Chang, W. C. Epidemiology, comorbidity, and course of adolescent depression. In Treatments for Adolescent Depression: Theory and Practice (ed. Essau, C. A.) (Oxford Univ. Press, 2009).
- 42.Angold A, Costello EJ. Depressive comorbidity in children and adolescents: empirical, theoretical, and methodological issues. Am. J. Psychiat. 1993;150:1779–1791. doi: 10.1176/ajp.150.12.1779. [DOI] [PubMed] [Google Scholar]
- 43.Borbély AA. A two process model of sleep regulation. Hum. Neurobiol. 1982;1:195–204. [PubMed] [Google Scholar]
- 44.Greene RW, Bjorness TE, Suzuki A. The adenosine-mediated, neuronal-glial, homeostatic sleep response. Curr. Opin. Neurobiol. 2017;44:236–242. doi: 10.1016/j.conb.2017.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Borbély AA, Daan S, Wirz‐Justice A, Deboer T. The two‐process model of sleep regulation: a reappraisal. J. Sleep Res. 2016;25:131–143. doi: 10.1111/jsr.12371. [DOI] [PubMed] [Google Scholar]
- 46.Jenni OG, LeBourgeois MK. Understanding sleep–wake behavior and sleep disorders in children: the value of a model. Curr. Opin. Psychiat. 2006;19:282. doi: 10.1097/01.yco.0000218599.32969.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Campbell IG, Grimm KJ, de Bie E, Feinberg I. Sex, puberty, and the timing of sleep EEG measured adolescent brain maturation. Proc. Natl Acad. Sci. 2012;109:5740–5743. doi: 10.1073/pnas.1120860109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Feinberg I, Higgins LM, Khaw WY, Campbell IG. The adolescent decline of NREM delta, an indicator of brain maturation, is linked to age and sex but not to pubertal stage. Dev. Physiol. Pregn. 2006;291:R1724–R1729. doi: 10.1152/ajpregu.00293.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tononi G, Cirelli C. Sleep function and synaptic homeostasis. Sleep Med. Rev. 2006;10:49–62. doi: 10.1016/j.smrv.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 50.Fontanellaz-Castiglione CEG, Markovic A, Tarokh L. Sleep and the adolescent brain. Curr. Opin. Physiol. 2020;15:167–171. doi: 10.1016/j.cophys.2020.01.008. [DOI] [Google Scholar]
- 51.Jenni OG, Achermann P, Carskadon MA. Homeostatic sleep regulation in adolescents. Sleep. 2005;28:1446–1454. doi: 10.1093/sleep/28.11.1446. [DOI] [PubMed] [Google Scholar]
- 52.Taylor DJ, Jenni OG, Acebo C, Carskadon MA. Sleep tendency during extended wakefulness: insights into adolescent sleep regulation and behavior. J. Sleep Res. 2005;14:239–244. doi: 10.1111/j.1365-2869.2005.00467.x. [DOI] [PubMed] [Google Scholar]
- 53.Nelson AB, Faraguna U, Zoltan JT, Tononi G, Cirelli C. Sleep patterns and homeostatic mechanisms in adolescent mice. Brain Sci. 2013;3:318–343. doi: 10.3390/brainsci3010318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tarokh L, Carskadon MA, Achermann P. Dissipation of sleep pressure is stable across adolescence. Neuroscience. 2012;216:167–177. doi: 10.1016/j.neuroscience.2012.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lo JC, Ong JL, Leong RL, Gooley JJ, Chee MW. Cognitive performance, sleepiness, and mood in partially sleep deprived adolescents: the need for sleep study. Sleep. 2016;39:687–698. doi: 10.5665/sleep.5552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fuligni AJ, Bai S, Krull JL, Gonzales NA. Individual differences in optimum sleep for daily mood during adolescence. J. Clin. Child. Adolesc. Psychol. 2017;48:469–479. doi: 10.1080/15374416.2017.1357126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Skorucak J, et al. Homeostatic response to sleep restriction in adolescents. Sleep. 2021;44:zsab106. doi: 10.1093/sleep/zsab106. [DOI] [PubMed] [Google Scholar]
- 58.Skorucak J, et al. Response to chronic sleep restriction, extension, and subsequent total sleep deprivation in humans: adaptation or preserved sleep homeostasis? Sleep. 2018;41:zsy078. doi: 10.1093/sleep/zsy078. [DOI] [PubMed] [Google Scholar]
- 59.Achermann P. The two-process model of sleep regulation revisited. Aviat. Space Environ. Med. 2004;75:A37–A43. [PubMed] [Google Scholar]
- 60.Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep: implications for behavior. Ann. NY Acad. Sci. 2004;1021:276–291. doi: 10.1196/annals.1308.032. [DOI] [PubMed] [Google Scholar]
- 61.Crowley S, Acebo C, Fallone G, Carskadon M. Estimating dim light melatonin onset (DLMO) phase in adolescents using summer or school-year sleep/wake schedules. Sleep. 2006;29:1632. doi: 10.1093/sleep/29.12.1632. [DOI] [PubMed] [Google Scholar]
- 62.Micic, et al. Nocturnal melatonin profiles in patients with delayed sleep-wake phase disorder and control sleepers. J. Biol. Rhythms. 2015;30:437–448. doi: 10.1177/0748730415591753. [DOI] [PubMed] [Google Scholar]
- 63.Micic G, et al. The endogenous circadian temperature period length (tau) in delayed sleep phase disorder compared to good sleepers. J. Sleep. Res. 2013;22:617–624. doi: 10.1111/jsr.12072. [DOI] [PubMed] [Google Scholar]
- 64.Micic G, et al. Circadian melatonin and temperature taus in delayed sleep–wake phase disorder and non-24-h sleep–wake rhythm disorder patients: an ultradian constant routine study. J. Biol. Rhythm. 2016;31:387–405. doi: 10.1177/0748730416650069. [DOI] [PubMed] [Google Scholar]
- 65.Micic G, et al. Circadian tau difference and rhythm associations in delayed sleep-wake phase disorder and sighted non-24-h sleep-wake rhythm disorder. Sleep. 2021;44:zsaa132. doi: 10.1093/sleep/zsaa132. [DOI] [PubMed] [Google Scholar]
- 66.Reppert SM, Weaver DR. Molecular analysis of mammalian circadian rhythms. Ann. Rev. Physiol. 2001;63:647–676. doi: 10.1146/annurev.physiol.63.1.647. [DOI] [PubMed] [Google Scholar]
- 67.Burgess HJ, Eastman CI. Human tau in an ultradian light–dark cycle. J. Biol. Rhythm. 2008;23:374–376. doi: 10.1177/0748730408318592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Czeisler CA, et al. Stability, precision, and near-24-h period of the human circadian pacemaker. Science. 1999;284:2177–2181. doi: 10.1126/science.284.5423.2177. [DOI] [PubMed] [Google Scholar]
- 69.Duffy JF, Wright KP., Jr Entrainment of the human circadian system by light. J. Biol. Rhythms. 2005;20:326–338. doi: 10.1177/0748730405277983. [DOI] [PubMed] [Google Scholar]
- 70.Zeitzer JM, Dijk DJ, Kronauer RE, Brown EN, Czeisler CA. Sensitivity of the human circadian pacemaker to nocturnal light: melatonin phase resetting and suppression. J. Physiol. 2000;526:695–702. doi: 10.1111/j.1469-7793.2000.00695.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Crowley S, Wolfson A, Tarokh L, Carskadon M. An update on adolescent sleep: new evidence informing the perfect storm model. J. Adolesc. 2018;67:55–65. doi: 10.1016/j.adolescence.2018.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hagenauer MH, Perryman JI, Lee TM, Carskadon MA. Adolescent changes in the homeostatic and circadian regulation of sleep. Dev. Neurosci. 2009;31:276–284. doi: 10.1159/000216538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Crowley SJ, Carskadon MA. Modifications to weekend recovery sleep delay circadian phase in older adolescents. Chronobiol. Int. 2010;27:1469–1492. doi: 10.3109/07420528.2010.503293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dawson D, Lack L, Morris M. Phase resetting of the human circadian pacemaker with use of a single pulse of bright light. Chronobiol. Int. 1993;10:94–102. doi: 10.3109/07420529309059697. [DOI] [PubMed] [Google Scholar]
- 75.Strogatz SH, Kronauer ER, Czeisler C. Circadian pacemaker interferes with sleep onset at specific times each day: role in insomnia. Am. J. Physiol. 1987;253:R172–R178. doi: 10.1152/ajpregu.1987.253.1.R172. [DOI] [PubMed] [Google Scholar]
- 76.Saxvig I, et al. Objective measures of sleep and dim light melatonin onset in adolescents and young adults with delayed sleep phase disorder compared to healthy controls. J. Sleep Res. 2013;22:365–372. doi: 10.1111/jsr.12030. [DOI] [PubMed] [Google Scholar]
- 77.Owens JA, Belon K, Moss P. Impact of delaying school start time on adolescent sleep, mood, and behavior. Arch. Pediatr. Adolesc. Med. 2010;164:608–614. doi: 10.1001/archpediatrics.2010.96. [DOI] [PubMed] [Google Scholar]
- 78.Bei B, et al. Actigraphy-assessed sleep during school and vacation periods: a naturalistic study of restricted and extended sleep opportunities in adolescents. J. Sleep Res. 2014;23:107–117. doi: 10.1111/jsr.12080. [DOI] [PubMed] [Google Scholar]
- 79.Short MA, Chee MWL. Adolescent sleep restriction effects on cognition and mood. Prog. Brain Res. 2019;246:55–71. doi: 10.1016/bs.pbr.2019.02.008. [DOI] [PubMed] [Google Scholar]
- 80.Taylor A, Wright HR, Lack LC. Sleeping-in on the weekend delays circadian phase and increases sleepiness the following week. Sleep Biol. Rhythms. 2008;6:172–179. doi: 10.1111/j.1479-8425.2008.00356.x. [DOI] [Google Scholar]
- 81.American Academy of Sleep Medicine. The International Classification of Sleep Disorders: Diagnostic and Coding Manual 3rd edn (American Academy of Sleep Medicine, 2014).
- 82.Raniti MB, et al. Sleep duration and sleep quality: associations with depressive symptoms across adolescence. Behav. Sleep Med. 2017;15:198–215. doi: 10.1080/15402002.2015.1120198. [DOI] [PubMed] [Google Scholar]
- 83.Fredriksen K, Rhodes J, Reddy R, Way N. Sleepless in Chicago: tracking the effects of adolescent sleep loss during the middle school years. Child Dev. 2004;75:84–95. doi: 10.1111/j.1467-8624.2004.00655.x. [DOI] [PubMed] [Google Scholar]
- 84.Baum KT, et al. Sleep restriction worsens mood and emotion regulation in adolescents. J. Child. Psychol. Psychiat. 2014;55:180–190. doi: 10.1111/jcpp.12125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Vriend J, et al. Manipulating sleep duration alters emotional functioning and cognitive performance in children. J. Pediatr. Psychol. 2013;38:1058–1069. doi: 10.1093/jpepsy/jst033. [DOI] [PubMed] [Google Scholar]
- 86.Talbot LS, McGlinchey EL, Kaplan KA, Dahl RE, Harvey AG. Sleep deprivation in adolescents and adults: changes in affect. Emotion. 2010;10:831–841. doi: 10.1037/a0020138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Short MA, Booth SA, Omar O, Ostlundh L, Arora T. The relationship between sleep duration and mood in adolescents: a systematic review and meta-analysis. Sleep. Med. Rev. 2020;52:101311. doi: 10.1016/j.smrv.2020.101311. [DOI] [PubMed] [Google Scholar]
- 88.McLaughlin KA, Hatzenbuehler ML, Mennin DS, Nolen-Hoeksema S. Emotion dysregulation and adolescent psychopathology: a prospective study. Behav. Res. Ther. 2011;49:544–554. doi: 10.1016/j.brat.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Prehn-Kristensen A, et al. Sleep in children enhances preferentially emotional declarative but not procedural memories. J. Exp. Child. Psychol. 2009;104:132–139. doi: 10.1016/j.jecp.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 90.Bauducco S, Richardson C, Gradisar M. Chronotype, circadian rhythms and mood. Curr. Opin. Psychol. 2020;34:77–83. doi: 10.1016/j.copsyc.2019.09.002. [DOI] [PubMed] [Google Scholar]
- 91.Nguyen C, Murray G, Anderson S, Filipowicz A, Ingram KK. In vivo molecular chronotyping, circadian misalignment, and high rates of depression in young adults. J. Affect. Disord. 2019;250:425–431. doi: 10.1016/j.jad.2019.03.050. [DOI] [PubMed] [Google Scholar]
- 92.Dolsen MR, Harvey AG. Dim light melatonin onset and affect in adolescents with an evening circadian preference. J. Adolesc. Health. 2018;62:94–99. doi: 10.1016/j.jadohealth.2017.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chiu W-H, Yang HJ, Kuo P-H. Chronotype preference matters for depression in youth. Chronobiol. Int. 2017;34:933–941. doi: 10.1080/07420528.2017.1327441. [DOI] [PubMed] [Google Scholar]
- 94.Merikanto I, et al. Eveningness as a risk for behavioral problems in late adolescence. Chronobiol. Int. 2017;34:225–234. doi: 10.1080/07420528.2016.1267739. [DOI] [PubMed] [Google Scholar]
- 95.Koo DL, et al. Association between morningness–eveningness, sleep duration, weekend catch‐up sleep and depression among Korean high‐school students. J. Sleep Res. 2021;30:e13063. doi: 10.1111/jsr.13063. [DOI] [PubMed] [Google Scholar]
- 96.Haraden DA, Mullin BC, Hankin BL. The relationship between depression and chronotype: a longitudinal assessment during childhood and adolescence. Depress. Anxiety. 2017;34:967–976. doi: 10.1002/da.22682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Van den Berg JF, Kivelä L, Antypa N. Chronotype and depressive symptoms in students: an investigation of possible mechanisms. Chronobiol. Int. 2018;35:1248–1261. doi: 10.1080/07420528.2018.1470531. [DOI] [PubMed] [Google Scholar]
- 98.Vetter C, et al. Prospective study of chronotype and incident depression among middle-and older-aged women in the Nurses’ Health Study II. J. Psychiatr. Res. 2018;103:156–160. doi: 10.1016/j.jpsychires.2018.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Haraden DA, Mullin BC, Hankin BL. Internalizing symptoms and chronotype in youth: a longitudinal assessment of anxiety, depression and tripartite model. Psychiat. Res. 2019;272:797–805. doi: 10.1016/j.psychres.2018.12.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.McClung CA. How might circadian rhythms control mood? Let me count the ways. Biol. Psychiat. 2013;74:242–249. doi: 10.1016/j.biopsych.2013.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gradisar M, et al. Randomized controlled trial of cognitive-behavior therapy plus bright light therapy for adolescent delayed sleep phase disorder. Sleep. 2011;34:1671–1680. doi: 10.5665/sleep.1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Biddle SJ, Ciaccioni S, Thomas G, Vergeer I. Physical activity and mental health in children and adolescents: an updated review of reviews and an analysis of causality. Psychol. Sport Exerc. 2019;42:146–155. doi: 10.1016/j.psychsport.2018.08.011. [DOI] [Google Scholar]
- 103.Heinrich LM, Gullone E. The clinical significance of loneliness: a literature review. Clin. Psychol. Rev. 2006;26:695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 104.Stephenson KM, Schroder CM, Bertschy G, Bourgin P. Complex interaction of circadian and non-circadian effects of light on mood: shedding new light on an old story. Sleep Med. Rev. 2012;16:445–454. doi: 10.1016/j.smrv.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 105.Warner S, Murray G, Meyer D. Holiday and school-term sleep patterns of Australian adolescents. J. Adolesc. 2008;31:595–608. doi: 10.1016/j.adolescence.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 106.Antypa N, et al. Associations between chronotypes and psychological vulnerability factors of depression. Chronobiol. Int. 2017;34:1125–1135. doi: 10.1080/07420528.2017.1345932. [DOI] [PubMed] [Google Scholar]
- 107.Watkins ER, Roberts H. Reflecting on rumination: consequences, causes, mechanisms and treatment of rumination. Behav. Res. Ther. 2020;127:103573. doi: 10.1016/j.brat.2020.103573. [DOI] [PubMed] [Google Scholar]
- 108.Takano K, Tanno Y. Diurnal variation in rumination. Emotion. 2011;11:1046. doi: 10.1037/a0022757. [DOI] [PubMed] [Google Scholar]
- 109.Hühne A, Welsh DK, Landgraf D. Prospects for circadian treatment of mood disorders. Ann. Med. 2018;50:637–654. doi: 10.1080/07853890.2018.1530449. [DOI] [PubMed] [Google Scholar]
- 110.Hickie IB, Rogers NL. Novel melatonin-based therapies: potential advances in the treatment of major depression. Lancet. 2011;378:621–631. doi: 10.1016/S0140-6736(11)60095-0. [DOI] [PubMed] [Google Scholar]
- 111.Short MA, Gradisar M, Gill J, Camfferman D. Identifying adolescent sleep problems. PLoS ONE. 2013;8:e75031. doi: 10.1371/journal.pone.0075301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hysing M, Haugland S, Stormark KM, Bøe T, Siversten B. Sleep and school attendance in adolescence: results from a large population-based study. Scand. J. Pub. Health. 2014;43:2–9. doi: 10.1177/1403494814556647. [DOI] [PubMed] [Google Scholar]
- 113.Lichstein KL, Durrence HH, Taylor DJ, Bush AJ, Riedel BW. Quantitative criteria for insomnia. Behav. Res. Ther. 2003;41:427–445. doi: 10.1016/S0005-7967(02)00023-2. [DOI] [PubMed] [Google Scholar]
- 114.Orchard F, Gregory AM, Gradisar M, Reynolds S. Self-reported sleep patterns and quality amongst adolescents: cross-sectional and prospective associations with aniety and depression. J. Child. Psychol. Psychiat. 2020;61:1126–1137. doi: 10.1111/jcpp.13288. [DOI] [PubMed] [Google Scholar]
- 115.Jakobsson M, Sundin K, Högberg K, Josefsson K. “I want to sleep but I can’t”: adolescents’ lived experience of sleeping difficulties. J. Sch. Nurs. 2020 doi: 10.1177/1059840520966011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Espie CA. Understanding insomnia through cognitive modelling. Sleep Med. 2007;8:S3–S8. doi: 10.1016/S1389-9457(08)70002-9. [DOI] [PubMed] [Google Scholar]
- 117.Harvey AG. A cognitive model of insomnia. Behav. Res. Ther. 2002;40:869–893. doi: 10.1016/S0005-7967(01)00061-4. [DOI] [PubMed] [Google Scholar]
- 118.Lundh LG, Broman JE. Insomnia as an interaction between sleep-interfering and sleep-interpreting processes. J. Psychosom. Res. 2000;49:299–310. doi: 10.1016/S0022-3999(00)00150-1. [DOI] [PubMed] [Google Scholar]
- 119.Hiller RM, Lovato N, Gradisar M, Oliver M, Slater A. Trying to fall asleep while catastrophising: what sleep-disordered adolescents think and feel. Sleep Med. 2014;15:96–103. doi: 10.1016/j.sleep.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 120.Wicklow A, Espie CA. Intrusive thoughts and their relationship to actigraphic measurement of sleep: towards a cognitive model of insomnia. Behav. Res. Ther. 2000;38:679–693. doi: 10.1016/S0005-7967(99)00136-9. [DOI] [PubMed] [Google Scholar]
- 121.Saxvig I, et al. Circadian typology and implications for adolescent sleep health: results from a large, cross-sectional, school-based study. Sleep Med. 2021;83:63–70. doi: 10.1016/j.sleep.2021.04.020. [DOI] [PubMed] [Google Scholar]
- 122.Orchard F, Reynolds S. “It was all my fault”: negative interpretation bias in depressed adolescents. J. Abnorm. Child Psychol. 2016;44:991–998. doi: 10.1007/s10802-015-0092-x. [DOI] [PubMed] [Google Scholar]
- 123.Orchard F, Reynolds S. The combined influence of cognitions in adolescent depression: biases of interpretation, self-evaluation, and memory. Br. J. Clin. Psychol. 2018;57:420–435. doi: 10.1111/bjc.12184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Huang C, et al. The roles of repetitive negative thinking and perfectionism in explaining the relationship between sleep onset difficulties and depressed mood in adolescents. Sleep Health. 2020;6:166–171. doi: 10.1016/j.sleh.2019.09.008. [DOI] [PubMed] [Google Scholar]
- 125.Crowley S, Eastman C. Human adolescent phase response curves to bright white light. J. Biol. Rhythm. 2017;32:334–344. doi: 10.1177/0748730417713423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Auger RR, et al. Clinical practice guideline for the treatment of intrinsic circadian rhythm sleep–wake disorders: advanced sleep–wake phase disorder (ASWPD), delayed sleep–wake phase disorder (DSWPD), non-24-h sleep–wake rhythm disorder (N24SWD), and irregular sleep–wake rhythm disorder (ISWRD). An update for 2015: an American Academy of Sleep Medicine clinical practice guideline. J. Clin. Sleep Med. 2015;11:1199–1236. doi: 10.5664/jcsm.5100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Gradisar M, Smits M, Bjorvatn B. Assessment and treatment of delayed sleep phase disorder in adolescents: recent innovations and cautions. Sleep Med. Clin. 2014;9:199–210. doi: 10.1016/j.jsmc.2014.02.005. [DOI] [Google Scholar]
- 128.Richardson C, Gradisar M. Depressed mood and repetitive negative thinking in delayed sleep–wake phase disorder: treatment effects and a comparison with good sleepers. J. Sleep. Res. 2021;31:e13452. doi: 10.1111/jsr.13452. [DOI] [PubMed] [Google Scholar]
- 129.Richardson C, et al. A randomised controlled trial of bright light therapy and morning activity for adolescents and young adults with delayed sleep-wake phase disorder. Sleep. Med. 2018;45:114–123. doi: 10.1016/j.sleep.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 130.Saxvig I, et al. A randomized controlled trial with bright light and melatonin for delayed sleep phase disorder: effects on subjective and objective sleep. Chronobiol. Int. 2014;31:72–86. doi: 10.3109/07420528.2013.823200. [DOI] [PubMed] [Google Scholar]
- 131.Danielsson K, Jansson-Fröjmark M, Broman J-E, Markström A. Cognitive behavioral therapy as an adjunct treatment to light therapy for delayed sleep phase disorder in young adults: a randomized controlled feasibility study. Behav. Sleep Med. 2016;14:212–232. doi: 10.1080/15402002.2014.981817. [DOI] [PubMed] [Google Scholar]
- 132.Richardson C, et al. Cognitive performance in adolescents with delayed sleep-wake phase disorder: treatment effects and a comparison with good sleepers. J. Adolesc. 2018;65:72–84. doi: 10.1016/j.adolescence.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 133.Wilhelmsen-Langeland A, et al. A randomized controlled trial with bright light and melatonin for the treatment of delayed sleep phase disorder: effects on subjective and objective sleepiness and cognitive function. J. Biol. Rhythm. 2013;28:306–321. doi: 10.1177/0748730413500126. [DOI] [PubMed] [Google Scholar]
- 134.Rosenthal NE, et al. Phase-shifting effects of bright morning light as treatment for delayed sleep phase syndrome. Sleep. 1990;13:354–361. [PubMed] [Google Scholar]
- 135.Wright H, Lack L, Kennaway D. Differential effects of light wavelength in phase advancing the melatonin rhythm. J. Pineal Res. 2004;36:140–144. doi: 10.1046/j.1600-079X.2003.00108.x. [DOI] [PubMed] [Google Scholar]
- 136.Sharkey KM, Carskadon MA, Figueiro MG, Zhu Y, Rea MS. Effects of an advanced sleep schedule and morning short wavelength light exposure on circadian phase in young adults with late sleep schedules. Sleep. Med. 2011;12:685–692. doi: 10.1016/j.sleep.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kirschbaum-Lesch I, Gest S, Legenbauer T, Holtmann M. Feasibility and efficacy of bright light therapy in depressed adolescent inpatients. Z. Kinder Jugendpsychiatr. Psychother. 2018;46:a000603. doi: 10.1024/1422-4917/a000603. [DOI] [PubMed] [Google Scholar]
- 138.Danielsson N, Harvey A, MacDonald S, Jansson-Fröjmark M, Linton S. Sleep disturbance and depressive symptoms in adolescence: the role of catastrophic worry. J. Youth Adolesc. 2013;42:1223–1233. doi: 10.1007/s10964-012-9811-6. [DOI] [PubMed] [Google Scholar]
- 139.Gest S, et al. Chronotherapeutic treatments for depression in youth. Eur. Child. Adolesc. Psychiat. 2016;25:151–161. doi: 10.1007/s00787-015-0720-6. [DOI] [PubMed] [Google Scholar]
- 140.Lam R, et al. Efficacy of bright light treatment, fluoxetine, and the combination in patients with nonseasonal major depressive disorder: a randomized clinical trial. JAMA Psychiat. 2016;73:56–63. doi: 10.1001/jamapsychiatry.2015.2235. [DOI] [PubMed] [Google Scholar]
- 141.Gordon N. The therapeutics of melatonin: a paediatric perspective. Brain Dev. 2000;22:213–217. doi: 10.1016/S0387-7604(00)00120-0. [DOI] [PubMed] [Google Scholar]
- 142.Lewy AJ, Wehr TA, Goodwin FK, Newsome DA, Markey SP. Light suppresses melatonin secretion in humans. Science. 1980;210:1267–1269. doi: 10.1126/science.7434030. [DOI] [PubMed] [Google Scholar]
- 143.Bruni O, et al. Current role of melatonin in pediatric neurology: clinical recommendations. Eur. J. Paediatr. Neuro. 2015;19:122–133. doi: 10.1016/j.ejpn.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 144.Kayumov L, Brown G, Jindal R, Buttoo K, Shapiro CM. A randomized, double-blind, placebo-controlled crossover study of the effect of exogenous melatonin on delayed sleep phase syndrome. Psychosom. Med. 2001;63:40–48. doi: 10.1097/00006842-200101000-00005. [DOI] [PubMed] [Google Scholar]
- 145.Carskadon M, Wolfson A, Acebo C, Tzischinsky O, Seifer R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998;21:871–881. doi: 10.1093/sleep/21.8.871. [DOI] [PubMed] [Google Scholar]
- 146.Mindell JA, et al. Pharmacologic management of insomnia in children and adolescents: consensus statement. Pediatrics. 2006;117:e1223–e1232. doi: 10.1542/peds.2005-1693. [DOI] [PubMed] [Google Scholar]
- 147.Mundey K, Benloucif S, Harsanyi K, Dubocovich ML, Zee PC. Phase-dependent treatment of delayed sleep phase syndrome with melatonin. Sleep. 2005;28:1271–1278. doi: 10.1093/sleep/28.10.1271. [DOI] [PubMed] [Google Scholar]
- 148.McDonagh MS, Holmes R, Hsu F. Pharmacologic treatments for sleep disorders in children: a systematic review. J. Child. Neurol. 2019;34:237–247. doi: 10.1177/0883073818821030. [DOI] [PubMed] [Google Scholar]
- 149.Owens JA, Rosen CL, Mindell JA, Kirchner HL. Use of pharmacotherapy for insomnia in child psychiatry practice: a national survey. Sleep. Med. 2010;11:692–700. doi: 10.1016/j.sleep.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 150.Wei S, et al. Efficacy and safety of melatonin for sleep onset insomnia in children and adolescents: a meta-analysis of randomized controlled trials. Sleep. Med. 2020;68:1–8. doi: 10.1016/j.sleep.2019.02.017. [DOI] [PubMed] [Google Scholar]
- 151.Rahman SA, Kayumov L, Shapiro CM. Antidepressant action of melatonin in the treatment of delayed sleep phase syndrome. Sleep Med. 2010;11:131–136. doi: 10.1016/j.sleep.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 152.Jan JE, Freeman RD. Melatonin therapy for circadian rhythm sleep disorders in children with multiple disabilities: what have we learned in the last decade? Dev. Med. Child. Neurol. 2004;46:776–782. doi: 10.1111/j.1469-8749.2004.tb00999.x. [DOI] [PubMed] [Google Scholar]
- 153.van Geijlswijk IM, van der Heijden KB, Egberts ACG, Korzilius HP, Smits MG. Dose finding of melatonin for chronic idiopathic childhood sleep onset insomnia: an RCT. Psychopharmacology. 2010;212:379–391. doi: 10.1007/s00213-010-1962-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kennaway DJ. Potential safety issues in the use of the hormone melatonin in paediatrics. J. Paediatr. Child Health. 2015;51:584–589. doi: 10.1111/jpc.12840. [DOI] [PubMed] [Google Scholar]
- 155.Bruni O, et al. Paediatric use of melatonin (Author reply to DJ Kennaway) Eur. J. Paediatr. Neuro. 2015;19:491–493. doi: 10.1016/j.ejpn.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 156.Jamieson D, Shan Z, Lagopoulos J, Hermens DF. The role of adolescent sleep quality in the development of anxiety disorders: a neurobiologically-informed model. Sleep Med. Rev. 2021;59:101450. doi: 10.1016/j.smrv.2021.101450. [DOI] [PubMed] [Google Scholar]
- 157.Richardson C, et al. Cognitive “insomnia” processes in delayed sleep-wake phase disorder: do they exist and are they responsive to chronobiological treatment? J. Consult. Clin. Psychol. 2019;87:16–32. doi: 10.1037/ccp0000357. [DOI] [PubMed] [Google Scholar]
- 158.Blake M, Latham M, Blake L, Allen N. Adolescent sleep intervention research: current state and future directions. Curr. Dir. Psychol. Sci. 2019;28:475–482. doi: 10.1177/0963721419850169. [DOI] [Google Scholar]
- 159.Blake MJ, et al. Systematic review and meta-analysis of adolescent cognitive–behavioral sleep interventions. Clin. Child. Fam. Psychol. Rev. 2017;20:227–249. doi: 10.1007/s10567-017-0234-5. [DOI] [PubMed] [Google Scholar]
- 160.Harvey AG, Tang NKY. Cognitive behaviour therapy for insomnia: can we rest yet? Sleep Med. Rev. 2003;7:237–262. doi: 10.1053/smrv.2002.0266. [DOI] [PubMed] [Google Scholar]
- 161.Bootzin RR, Stevens SJ. Adolescents, substance abuse, and the treatment of insomnia and daytime sleepiness. Clin. Psychol. Rev. 2005;25:629–644. doi: 10.1016/j.cpr.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 162.Blake MJ, et al. A cognitive-behavioral and mindfulness-based group sleep intervention improves behavior problems in at-risk adolescents by improving perceived sleep quality. Behav. Res. Ther. 2017;99:147–156. doi: 10.1016/j.brat.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 163.Åslund L, Arnberg F, Kanstrup M, Lekander M. Cognitive and behavioral interventions to improve sleep in school-age children and adolescents: a systematic review and meta-analysis. J. Clin. Sleep. Med. 2018;14:1937–1947. doi: 10.5664/jcsm.7498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Chan NY, et al. A prevention program for insomnia in at-risk adolescents: a randomized controlled study. Pediatrics. 2021;147:e2020006833. doi: 10.1542/peds.2020-006833. [DOI] [PubMed] [Google Scholar]
- 165.Gee B, et al. The effect of non-pharmacological sleep interventions on depression symptoms: a meta-analysis of randomised controlled trials. Sleep Med. Rev. 2019;43:118–128. doi: 10.1016/j.smrv.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 166.Åslund L, Lekander M, Wicksell RK, Henje E, Jernelöv S. Cognitive-behavioral therapy for insomnia in adolescents with comorbid psychiatric disorders: a clinical pilot study. Clin. Child. Psychol. Psychiat. 2020;25:958–971. doi: 10.1177/1359104520929376. [DOI] [PubMed] [Google Scholar]
- 167.De Bruin UJ, Bögels SM, Oort FJ, Meijer AM. Efficacy of cognitive behavioral therapy for insomnia in adolescents: a randomized controlled trial with internet therapy, group therapy and a waiting list condition. Sleep. 2015;38:1913–1926. doi: 10.5665/sleep.5240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Gradisar M, Richardson C. CBT-I cannot rest until the sleepy teen can. Sleep. 2015;38:1841–1842. doi: 10.5665/sleep.5220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Bartel K, Huang C, Maddock B, Williamson P, Gradisar M. Brief school-based interventions to assist adolescents’ sleep-onset latency: comparing mindfulness and constructive worry versus controls. J. Sleep Res. 2018;27:e12668. doi: 10.1111/jsr.12668. [DOI] [PubMed] [Google Scholar]
- 170.Lever JR, Murphy AP, Duffield R, Fullagar HHK. A combined sleep hygiene and mindfulness intervention to improve sleep and well-being during high-performance youth tennis tournaments. Int. J. Sports Physiol. Perform. 2020;16:250–258. doi: 10.1123/ijspp.2019-1008. [DOI] [PubMed] [Google Scholar]
- 171.Bartel K, Scheeren R, Gradisar M. Altering adolescents’ prebedtime phone use to achieve better sleep health. Health Commun. 2019;34:456–462. doi: 10.1080/10410236.2017.1422099. [DOI] [PubMed] [Google Scholar]
- 172.Bartel, K. & Gradisar, M. New directions in the link between technology use and sleep in young people. In Sleep Disorders in Children (eds Nevšimalová, S. & Bruni, O.) (Springer, 2017).
- 173.Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: a review. Sleep. Med. 2010;11:735–742. doi: 10.1016/j.sleep.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 174.Van den Bulck J. The effects of media on sleep. Adolesc. Med. 2010;21:418–429. [PubMed] [Google Scholar]
- 175.Blake MJ, Trinder JA, Allen NB. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: implications for behavioral sleep interventions. Clin. Psychol. Rev. 2018;63:25–40. doi: 10.1016/j.cpr.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 176.Bauducco SV, Flink IK, Boersma K, Linton SJ. Preventing sleep deficit in adolescents: long-term effects of a quasi-experimental school-based intervention study. J. Sleep. Res. 2020;29:e12940. doi: 10.1111/jsr.12940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Richardson C, Ree M, Bucks RS, Gradisar M. Paediatric sleep literacy in Australian health professionals. Sleep. Med. 2021;81:327–335. doi: 10.1016/j.sleep.2021.02.035. [DOI] [PubMed] [Google Scholar]
- 178.Crowe K, Spiro-Levitt C. Sleep-related problems and pediatric anxiety disorders. Child. Adolesc. Psychiat. Clin. 2021;30:209–224. doi: 10.1016/j.chc.2020.09.004. [DOI] [PubMed] [Google Scholar]
- 179.Garber J, Weersing VR. Comorbidity of anxiety and depression in youth: implications for treatment and prevention. Clin. Psychol. 2010;17:293–306. doi: 10.1111/j.1468-2850.2010.01221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Higuchi S, Motohashi Y, Liu Y, Maeda A. Effects of playing a computer game using a bright display on presleep physiological variables, sleep latency, slow wave sleep and REM sleep. J. Sleep Res. 2005;14:267–273. doi: 10.1111/j.1365-2869.2005.00463.x. [DOI] [PubMed] [Google Scholar]
- 181.Ivarsson M, Anderson M, Åkerstedt T, Lindblad F. The effect of violent and nonviolent video games on heart rate variability, sleep, and emotions in adolescents with different violent gaming habits. Psychosom. Med. 2013;75:390–396. doi: 10.1097/PSY.0b013e3182906a4c. [DOI] [PubMed] [Google Scholar]
- 182.Weaver E, et al. The effect of presleep video-game playing on adolescent sleep. J. Clin. Sleep. Med. 2010;6:184–189. doi: 10.5664/jcsm.27769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.King DL, et al. The impact of prolonged violent video-gaming on adolescent sleep: an experimental study. J. Sleep. Res. 2013;22:137–143. doi: 10.1111/j.1365-2869.2012.01060.x. [DOI] [PubMed] [Google Scholar]
- 184.Van der Lely S, et al. Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. J. Adolesc. Health. 2015;56:113–119. doi: 10.1016/j.jadohealth.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 185.Heath, et al. Does one hour of bright or short-wavelength filtered tablet screenlight have a meaningful effect on adolescents’ pre-bedtime alertness, sleep and daytime functioning? Chronobiol. Int. 2014;31:496–505. doi: 10.3109/07420528.2013.872121. [DOI] [PubMed] [Google Scholar]
- 186.Duraccio KM, Zaugg KK, Blackburn RC, Jensen CD. Does iPhone night shift mitigate negative effects of smartphone use on sleep outcomes in emerging adults? Sleep Health. 2021;7:478–484. doi: 10.1016/j.sleh.2021.03.005. [DOI] [PubMed] [Google Scholar]
- 187.Knufinke M, Fittkau-Kock L, Møst EIS, Kompier MAJ, Nieuwenhuys A. Restricting short-wavelength light in the evening to improve sleep in recreational athletes — a pilot study. Eur. J. Sport. Sci. 2018;19:728–735. doi: 10.1080/17461391.2018.1544278. [DOI] [PubMed] [Google Scholar]
- 188.Smith, et al. Mechanisms influencing older adolescents’ bedtimes during videogaming: the roles of game difficulty and flow. Sleep Med. 2017;39:70–76. doi: 10.1016/j.sleep.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 189.Exelmans L, Van Den Bulck J. “Glued to the tube”: the interplay between self-control, evening television viewing, and bedtime procrastination. Commun. Res. 2017;48:594–616. doi: 10.1177/0093650216686877. [DOI] [Google Scholar]
- 190.Reynolds CM, et al. Adolescents who perceive fewer consequences of risk‐taking choose to switch off games later at night. Acta Paediatr. 2015;104:e222–e227. doi: 10.1111/apa.12935. [DOI] [PubMed] [Google Scholar]
- 191.Bartel K, Gradisar M, Williamson P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep. Med. Rev. 2015;21:72–85. doi: 10.1016/j.smrv.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 192.Tavernier R, Willoughby T. Sleep problems: predictor or outcome of media use among emerging adults at university? J. Sleep. Res. 2014;23:389–396. doi: 10.1111/jsr.12132. [DOI] [PubMed] [Google Scholar]
- 193.Richardson C, et al. A longitudinal investigation of sleep and technology use in early adolescence: does parental control of technology use protect adolescent sleep? Sleep Med. 2021;84:368–379. doi: 10.1016/j.sleep.2021.06.003. [DOI] [PubMed] [Google Scholar]
- 194.Eggermont S, van den Bulck J. Nodding off or switching off? The use of popular media as a sleep aid in secondary-school children. J. Paediatr. Child Health. 2006;42:428–433. doi: 10.1111/j.1440-1754.2006.00892.x. [DOI] [PubMed] [Google Scholar]
- 195.Jansson-Fröjmark M, Norell-Clarke A. The cognitive treatment components and therapies of cognitive behavioral therapy for insomnia: a systematic review. Sleep Med. Rev. 2018;42:19–36. doi: 10.1016/j.smrv.2018.05.001. [DOI] [PubMed] [Google Scholar]
- 196.Buda G, Lukoševičiūtė J, Šmigelskas K. Possible effects of social media use on adolescent health behaviors and perceptions. Psychol. Rep. 2020 doi: 10.1177/0033294120922481. [DOI] [PubMed] [Google Scholar]