Worldwide, there have already been about 20 million excess deaths during the coronavirus disease 2019 (COVID-19) pandemic (based on a recent estimate of 18 million during 2020–21), but only 6 million deaths have been individually attributed to COVID-19, suggesting 3-fold under-attribution.1,2 In Mexico the excess number of deaths during 2020–21 has been estimated as 0.8 million, but only 0.3 million deaths have been individually attributed to COVID-19, again suggesting substantial under-attribution. Within Mexico City, however, the attribution of causes of death may well have been much more reliable.
Obesity and obesity-related diseases are major risk factors for COVID-19 mortality. In the UK, where the Office for National Statistics registration of COVID-19 deaths has been reasonably accurate since May 2020, a study of 7 million adults reported that each 5-kg/m2 higher body mass index (BMI) above 23 kg/m2 was associated with a 28% higher risk of death from COVID-19, but the association appeared to be ‘J-shaped’.3 In Mexico, where the prevalences of overweight and obesity are among the highest in the world,4 a study of 50 000 adults attending hospital, who tested positive for SARS-Cov-2 using polymerase chain reaction, found that self-reported obesity (yes versus no) was associated with a 31% higher case-fatality rate; but the study did not have data on BMI and so could not assess the shape of the association of BMI with case-fatality.5 Using the Mexico City Prospective Study (MCPS) of adult mortality in the general population, we report the association between BMI and COVID-19 mortality throughout the full range from normal weight to morbidly obese, comparing this with similar analyses of mortality from all other causes combined.
The MCPS recruited 150 000 adults in 1998–2004, measured BMI and other factors and followed participants through the death registry for cause-specific mortality.6 Death registration in Mexico City is reliable, with almost all adult deaths certified medically.7 Deaths due to COVID-19 were defined as those with an International Classification of Diseases 10th revision (ICD-10) underlying cause U07.1 or U07.2. Among survivors aged <90 years on 1 January 2020, we used Cox regression to relate baseline BMI (which correlates strongly with BMI many years later8) to 2020 COVID-19 mortality. Associations with BMI were estimated across six categories (from normal to morbidly obese, excluding participants with BMI outside the range 18.5–60 kg/m2), adjusted for age, sex, residential district and highest educational level. (The few participants with missing data for BMI or any confounder were excluded.) Effects per 5-kg/m2 higher BMI were also reported, overall, by sex and by age (<70 vs ≥70 years on 1 January 2020). Analyses used SAS version 9.4 (SAS Institute) and R version 3.1.1 [www.r-project.org/]. Data were accurate as of May 2022.
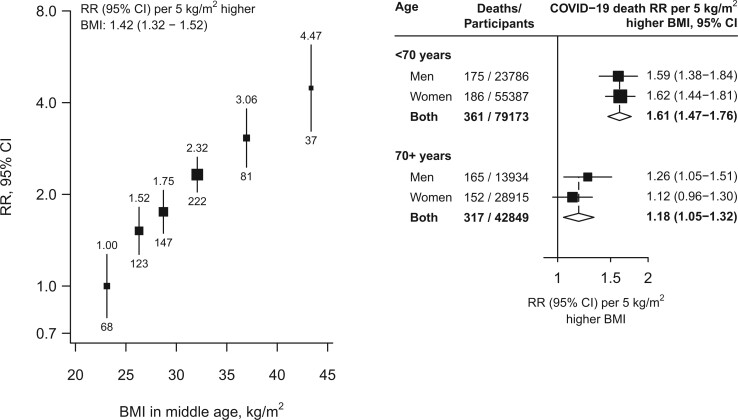
Among the 122 022 participants (37 720 men and 84 302 women) alive on 1 January 2020 [mean age 67 (SD 10) years, 65% under age 70], BMI at baseline was 28.1 (SD 4.0) kg/m2 in men and 29.6 (5.1) kg/m2 in women; 28% of men and 42% of women had a BMI >30 kg/m2 (Table 1). University or college education was more common in younger than older individuals and more common in men than women. During 2020, 678 died from COVID-19 and 1572 from other underlying causes. BMI was positively (and approximately log-linearly) associated with COVID-19 mortality, with no evidence of any threshold level below which lower BMI was not associated with lower risk (Figure 1). In the lowest BMI category, COVID-19 mortality among participants with BMI 22.5–25 kg/m2 (mean 24 kg/m2) was nearly twice that among those with BMI 18.5–22.5 kg/m2 (mean 21 kg/m2): mortality rate ratio (RR) 1.89, but with 95% confidence interval (CI) 1.01–3.53. Across the whole range, each 5-kg/m2 higher BMI was associated with 42% higher COVID-19 mortality (RR 1.42 per 5-kg/m2, 1.32–1.52). Comparing the top and bottom categories (BMI ≥40 versus <25 kg/m2, with means 43 kg/m2 and 23 kg/m2, respectively), there was about a 4-fold difference in COVID-19 mortality (RR 4.47, 2.98–6.70). The association was stronger in younger than older adults (RR per 5-kg/m2 higher BMI 1.61, 1.47–1.76, if age <70 years on 1 January 2020 versus 1.18, 1.05–1.32, if older) but, at any given age, was comparable in men and women. BMI was also strongly predictive of mortality from the aggregate of all other causes, with each 5-kg/m2 higher BMI associated with 32% higher mortality (RR 1.32, 1.26–1.39). In a sensitivity analysis restricted to the 348 deaths with an ICD-10 code of U07.1 (i.e. COVID-19 where the virus was confirmed by laboratory testing) the RR per 5 kg/m2 higher BMI was 1.36 (1.22–1.50).
Table 1 .
Characteristics of 122 022 individuals from the Mexico City Prospective Study aged <90 years on 1 January 2020
| Men |
Women |
|||
|---|---|---|---|---|
| <70 years(n = 23 786) | ≥70 years(n = 13 934) | <70 years(n = 55 387) | ≥70 years(n = 28 915) | |
| Age, years | 61 (5) | 78 (6) | 61 (5) | 78 (6) |
| Resident of Coyoacán | 10 040 (42%) | 6824 (49%) | 20 021 (36%) | 12 782 (44%) |
| University or college educated | 8212 (35%) | 2317 (17%) | 9535 (17%) | 1676 (6%) |
| Body mass index (kg/m²) at original study recruitment (1998–2004) | ||||
| Mean (SD) | 28.1 (4.1) | 28.1 (3.9) | 29.4 (5.1) | 30.0 (5.0) |
| ≥18.5 to <25 | 5191 (22%) | 3000 (22%) | 10 345 (19%) | 4278 (15%) |
| ≥25 to <30 | 11 783 (50%) | 7026 (50%) | 22 937 (41%) | 11 344 (39%) |
| ≥30 | 6812 (29%) | 3908 (28%) | 22 105 (40%) | 13 293 (46%) |
Numbers shown are mean (standard deviation) or n (%).
Figure 1.
Body mass index versus risk of death from COVID-19. In the left panel, estimates are adjusted for age, sex, education and district and in the right panel, the age- and sex-stratified results are adjusted for age, education and district. The areas of the squares are proportional to the amount of statistical information and the lines through them are the 95% confidence intervals. The numbers above each vertical line in the left panel show the death rate ratio for that group and the numbers below each vertical line give the number of COVID−19 deaths in that group. In the right panel, the diamonds are the information-weighted averages of the two results above them. BMI, body mass index; CI, confidence interval; RR, mortality rate ratio
Overweight (BMI 25–30 kg/m2) and obesity (BMI ≥30 kg/m2) affect more than one-third of the global adult population.9 Our findings highlight the importance of overweight in addition to obesity as a major modifiable risk factor for death from COVID-19. However, even during 2020 other causes of death accounted for more than twice as many deaths as COVID-19, so the absolute association of BMI with mortality was greater for the aggregate of those other causes than for COVID-19. Considering not only the pandemic but also other years, these other causes are the main way obesity reduces life expectancy. In addition, as overweight is much more common than morbid obesity, its population effects are more important.
Ethics approval
Approval for the study was given by the Mexican Ministry of Health, the Mexican National Council of Science and Technology (0595P-M) and the Central Oxford Research Ethics Committee (C99.260). All study participants provided written informed consent.
Data availability
We welcome requests from researchers who wish to access data from the Mexico City Prospective Study. If you are interested in obtaining data from the study for research purposes, or in collaborating with us on a specific research proposal, please visit our study website [https://www.ctsu.ox.ac.uk/research/prospective-blood-based-study-of-150-000-individuals-in-mexico] where you can download our Data and Sample Access Policy in either English or Spanish.
Author contributions
J.A-D., R.C., P.K-M., R.P. and R.T-C. established the cohort. J.A-D., P.K-M., R.R-R. and R.T-C. gathered the data. W.G.H., R.R-R. and R.W. linked, reviewed and/or adjudicated the death certificates. J.E., L.G.F. and R.W. developed the study design, did the analyses and wrote the first draft. All authors contributed to revision of the report and agreed to its publication. J.A-D. and J.R.E. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the analysis.
Funding
The Mexico City Prospective Study has received funding from the Mexican Health Ministry, the National Council of Science and Technology for Mexico, the Wellcome Trust, Cancer Research UK, British Heart Foundation and the UK Medical Research Council. W.G.H.. is supported by an MRC-Kidney Research UK Professor David Kerr Clinician Scientist Award. The funding sources had no role in the design, conduct or analysis of the study or the decision to submit the manuscript for publication.
Conflict of interest
None declared.
Contributor Information
Jesus Alegre-Díaz, School of Medicine, National Autonomous University of Mexico, Mexico City, Mexico.
Louisa G Friedrichs, MRC Population Health Research Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK; Clinical Trial Service Unit & Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK.
Raul Ramirez-Reyes, School of Medicine, National Autonomous University of Mexico, Mexico City, Mexico.
Rachel Wade, MRC Population Health Research Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK; Clinical Trial Service Unit & Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK.
Fiona Bragg, MRC Population Health Research Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK; Clinical Trial Service Unit & Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK.
William G Herrington, MRC Population Health Research Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK; Clinical Trial Service Unit & Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK.
Robert Clarke, Clinical Trial Service Unit & Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK.
Richard Peto, Clinical Trial Service Unit & Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK.
Rory Collins, Clinical Trial Service Unit & Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK.
Pablo Kuri-Morales, School of Medicine, National Autonomous University of Mexico, Mexico City, Mexico.
Jonathan R Emberson, MRC Population Health Research Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK; Clinical Trial Service Unit & Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK.
Roberto Tapia-Conyer, School of Medicine, National Autonomous University of Mexico, Mexico City, Mexico.
References
- 1. World Health Organization. Coronavirus (COVID-19) Dashboard. https://covid19.who.int/ (6th July 2022, date last accessed).
- 2. COVID-19 Excess Mortality Collaborators. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet 2022;399:1513–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gao M, Piernas C, Astbury NM et al. Associations between body-mass index and COVID-19 severity in 6.9 million people in England: a prospective, community-based, cohort study. Lancet Diabetes Endocrinol 2021;9:350–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ng M, Fleming T, Robinson M et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chiquete E, Alegre-Díaz J, Ochoa-Guzmán A et al. Ethnicity and other COVID-19 death risk factors in Mexico. Arch Med Sci 2022;18:711–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tapia-Conyer R, Kuri-Morales P, Alegre-Diaz J et al. Cohort Profile: The Mexico City Prospective Study. Int J Epidemiol 2006;35:243–92. [DOI] [PubMed] [Google Scholar]
- 7. Mikkelsen L, Phillips DE, AbouZahr C et al. A global assessment of civil registration and vital statistics systems: monitoring data quality and progress. Lancet 2015;386:1395–406. [DOI] [PubMed] [Google Scholar]
- 8. Gnatiuc L, Tapia-Conyer R, Wade R et al. Abdominal and gluteofemoral markers of adiposity and risk of vascular-metabolic mortality in a prospective study of 150 000 Mexican adults. Eur J Prev Cardiol 2022;29:730–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization. Obesity and Overweight Fact Sheet. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (6 July 2022, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
We welcome requests from researchers who wish to access data from the Mexico City Prospective Study. If you are interested in obtaining data from the study for research purposes, or in collaborating with us on a specific research proposal, please visit our study website [https://www.ctsu.ox.ac.uk/research/prospective-blood-based-study-of-150-000-individuals-in-mexico] where you can download our Data and Sample Access Policy in either English or Spanish.