Abstract
During the COVID-19 pandemic, reductions in heart failure (HF) hospitalizations have been widely reported, and there is an urgent need to understand how HF care has been reorganized in countries with different infection levels, vaccination rates and healthcare services. The OPTIMIZE Heart Failure Care program has a global network of investigators in 42 countries, with first-hand experience of the impact of the pandemic on HF management in different care settings. The national coordinators were surveyed to assess: 1) the challenges of the COVID-19 pandemic for continuity of HF care, from both a hospital and patient perspective; 2) the organizational changes enacted to ensure continued HF care; and 3) lessons learned for the future of HF care. Contributions were obtained from 37 national coordinators in 29 countries. We summarize their input, highlighting the issues raised and using the example of three very different settings (Italy, Brazil, and Taiwan) to illustrate the similarities and differences across the OPTIMIZE program.
Keywords: Heart failure, COVID-19, Pandemic, Continuity of care, Telemedicine
Graphical abstract
1. Introduction
During the COVID-19 pandemic, reductions in heart failure (HF) hospitalizations have been widely reported [[1], [2], [3], [4], [5]], with early evidence of worse long-term outcomes for those who are admitted [6]. Additionally, since the first reports of cases of COVID-19 in December 2019 [7], considerable progress has been made in understanding how patients with HF and COVID-19 should be managed [[8], [9], [10], [11], [12], [13], [14]]. However, as the COVID-19 pandemic moves only slowly towards an endemic situation, and with variable rates of vaccination globally, there is an urgent need to understand and learn from how HF specialists have reorganized HF care in countries with different infection levels, vaccination rates and healthcare services.
The OPTIMIZE Heart Failure Care program (http://www.optimize-hf.com) was initiated in 2013 to help improve outcomes following HF hospitalization through inexpensive initiatives promoting prescription of appropriate drug therapies, patient education and engagement, and post-discharge planning [15]. It includes best practice clinical protocols for local adaptation, pre- and post-discharge checklists, and ‘My HF Passport’, a printed and smartphone application to improve patient understanding of HF and encourage involvement in care and treatment adherence. It has a global network of investigators in 42 countries, with first-hand experience of the impact of the pandemic on HF management in different care settings. In view of this valuable resource, the OPTIMIZE Heart Failure Care working group decided to carry out an opportunistic survey of the national coordinators to assess: 1) the challenges of the COVID-19 pandemic for continuity of HF care, from both a hospital and patient perspective; 2) the organizational changes enacted to ensure continued HF care; and 3) lessons learned for the future of HF care. We report the results of this survey, highlighting the issues raised and using the example of three very different settings (Italy, Brazil, and Taiwan) to illustrate the similarities and differences across the OPTIMIZE program.
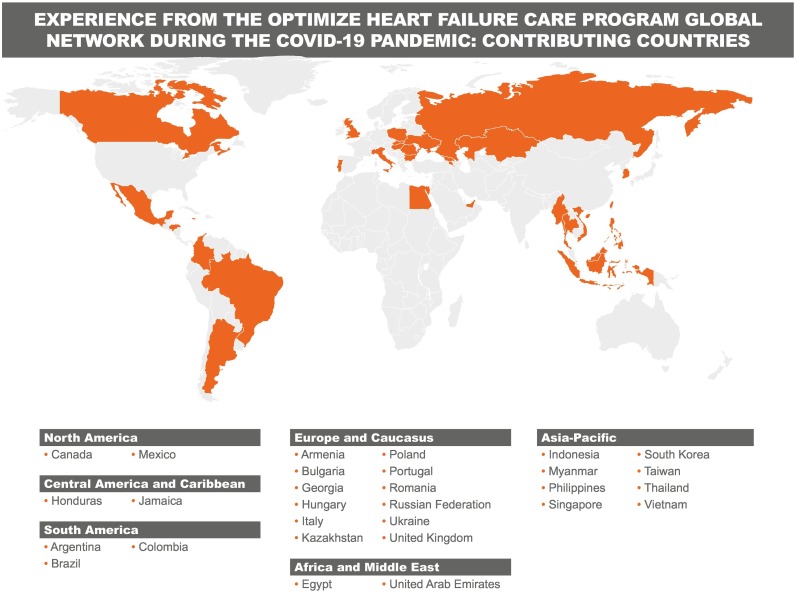
In August 2021, invitations to participate in the survey were sent to 72 OPTIMIZE national coordinators in 42 countries. This paper is based on the contributions received from 37 national coordinators in 29 countries (Fig. 1 ). These included contributions from countries with some of the highest rates of COVID-19 cases in the world, such as Brazil, Argentina, Colombia and Italy, and others with much lower reported case numbers including Egypt and Taiwan (see Fig. 2 for daily new confirmed COVID-19 cases in Italy, Brazil, and Taiwan between February 1, 2020 and January 15, 2022). The responses therefore reflect a very diverse range of disruption from COVID-19-related infection, vaccination rates, and healthcare systems.
Fig. 1.
Experience from the OPTIMIZE Heart Failure Care program global network during the COVID-19 pandemic: contributing countries.
2. Challenges of the COVID-19 pandemic for the continuity of HF care
From the hospital perspective, widespread and often sudden closure of elective and outpatient services, the conversion of cardiology wards and HF units to COVID-19 wards, reallocation of cardiologists and other healthcare professionals in the HF team to care for patients with COVID-19, and reduced multidisciplinary working were reported from across the OPTIMIZE network (Table 1 ).
Table 1.
Common challenges for HF care during the COVID-19 pandemic.
| Clinical challenges | Patient challenges | Logistical challenges |
|---|---|---|
|
|
|
A decrease in emergency HF admissions was commonly reported by OPTIMIZE contributors, along with reduced outpatient activity, and fewer referrals to cardiac rehabilitation units. OPTIMIZE clinicians at a University hospital's HF clinic in Thailand observed a 16% reduction in the number of outpatient visits and a 22% decline in the number of hospitalizations during the peak of the pandemic, although there were no restrictions on hospitalizations for symptomatic patients; in addition, HF readmission rates were significantly lower than in the pre-COVID period (2.5% vs. 8.7%) [16]. In countries with high COVID-19 rates and already limited HF services, the reallocation of staff and facilities to care of patients with COVID-19 was particularly problematic. In Mexico, for instance, during the first pandemic wave, 80% of the hospitals were converted receive COVID patients and a higher proportion of the healthcare staff was reallocated.
The management of patients with HF who required emergency admission for COVID-19 posed particular challenges. In Armenia, clinicians involved in the OPTIMIZE program reported that patients with comorbid HF and/or diabetes mellitus accounted for almost half of all hospitalizations in COVID structures. Among COVID-19 survivors included in a multicenter registry in seven post-Soviet states in the OPTIMIZE network, one of the leading risk factors for mortality within 3 months after hospitalization was NYHA class II-IV HF, which was associated with a 5-fold increased risk of death [17].
In a survey of 48 clinicians involved in the OPTIMIZE program in Colombia (which has one of the highest rates of COVID-19 cases in South America and had a seven-month lockdown in 2020), loss of follow-up of patients with HF during this period was the biggest problem for the majority of hospitals. Twenty-three per cent of the hospitals reported that when their patients did return for follow-up, they were sicker, with more advanced disease. In Portugal, where there had been over 1 million cases of COVID-19 by November 2021, OPTIMIZE investigators reported that patients with decompensated HF (who would previously have been admitted to Internal Medicine and Cardiology departments) were instead admitted to COVID or general wards and cared for by non-specialist teams. In Romania, which has had over 1.7 million cases with a resurgence in cases in recent months, participating OPTIMIZE clinicians reported that there has been a significant reduction in all HF-related procedures such as implanted cardioverter defibrillator devices (ICDs)/cardiac resynchronization therapy (CRT) and left ventricular assist devices (LVADs) or heart transplants. In Myanmar, where the number of patients with rheumatic heart disease remains high, OPTIMIZE participants said cardiac surgical theaters were closed and patients with HF who were waiting for valve replacement surgery experienced a worsening of their condition leading to increased mortality.
In Egypt, OPTIMIZE investigators reported that one of the serious problems was the misdiagnosis of patients with HF as patients infected with COVID-19. Patients presenting with shortness of breath were assumed to have COVID-19 until proved otherwise. Misdiagnosis or late diagnosis of HF was reported as having serious consequences, with inappropriate treatment of patients with anticoagulants, steroids and antiviral and immune-suppressive agents leading to hemorrhage and serious infections.
From the patient perspective, there has been a global reluctance to attend face-to-face consultations and physical examinations even when these were available, and lockdowns, social isolation and transportation problems have added to difficulties of accessing HF care. In some countries, patients were advised to stay at home, even if ill, and to avoid contact with the healthcare system. In Portugal, for example, OPTIMIZE survey respondents explained this meant that patients with new or decompensated HF often presented late to the Emergency Room, sometimes through other services, and consequently were more ill and had worse outcomes. Data published from a Lisbon HF unit involved in OPTIMIZE showed that inpatient mortality and six-month readmission and mortality rates were all higher for patients with HF between September and December 2020 than in the same period in 2019 [18].
The barriers to accessing services reported by OPTIMIZE coordinators (created by both patient fear of going to a hospital and not wishing to burden already busy healthcare facilities, and by HF services and staff being redeployed) have resulted in widespread reduction in demand for medical care for HF. For example, OPTIMIZE HF specialists in Georgia – a country with over 750,000 cases of COVID-19 and only 26% of the population vaccinated by November 2021 – have seen a 40% reduction in HF hospitalizations of and a 75% fall in outpatient visits during each wave of infection.
Owing to lost earnings, particularly in countries with limited or no social safety nets, some patients had difficulties paying for medications, with consequent lower adherence to HF therapy.
3. Organizational changes reported to help ensure continuity of HF care (Fig. 2)
Fig. 2.
Strategies for continued of HF care.
OPTIMIZE program investigators reported extensive introduction of telemedicine to reduce the need for in-person consultations for patients with HF (via online platforms, video consultations, phone, text, WhatsApp™, etc.), and prescriptions and test results sent by email or via smartphone applications. There was increased patient involvement in self-reporting changes in symptoms and physiological measurements, and in treatment adherence. In Colombia, OPTIMIZE coordinators reported that 85% of hospitals surveyed were using telemedicine to reach out to patients with HF, compared with almost none before the pandemic. OPTIMIZE participants in Poland reported a survey of 36 medical centers conducted in June 2020 which indicated that 30 centers offered teleconsultations, while only 2 centers were able to maintain in-person visits [19]. In Canada, OPTIMIZE investigators reported the advantages of a more patient-centered approach to virtual and digital care in a country so geographically large that many patients can only access specialized care by plane or long road trips, which can be particularly challenging in winter. Experience was gained on remote patient assessment using smartphone applications and uptitration of medications, particularly those with less impact on blood pressure.
In Singapore, after one month of the pandemic, OPTIMIZE coordinators observed that many patients were not coming back for follow-up. Telephone and video consultations were set up not only for HF but for all cardiology and patients. Although remote consultations are now offered as a standard of care, they account for less than 10% of all consultations and the uptake is variable among physicians. During the peak of the pandemic, most patients opted to delay their appointments and had their medications delivered via courier. As the rehabilitation center is closed, rehabilitation is performed using tablets via a virtual platform.
OPTIMIZE participants in Portugal reported that, thanks to restructuring during the peak COVID-19 period from April to June 2020, they were able to treat the same number of outpatients in HF clinics as in the same period in 2019, albeit using teleconsultations to triage the need for face-to-face review [20]. Patients were contacted by telephone and only seen if they presented with signs or symptoms of decompensation. Data for April to June 2020 showed that 204 consultations were carried out (144 by telephone) compared to 136 in the same period in 2019. There were 113 visits to the day hospital for the administration of intravenous therapy, compared with 100 in 2019.
The widely reported ‘techceleration’ triggered by the pandemic – with rapid adoption of more digital solutions for healthcare needs – had some benefits for patients with HF. In Thailand, OPTIMIZE coordinators reported that a telemedicine program was found to be effective in achieving target doses of guideline-directed medical therapy [16]. In Poland, clinicians in the OPTIMIZE network reported that, for those with a cardiac implantable electronic device such as an ICD or CRT, follow-up was largely shifted to remote device checks, with no harmful effect on device safety [21]. Despite the 16.8% reduction in follow-up visits for patients with ICDs/CRTs in the first two months of the pandemic (March to May 2020) compared to the previous year, the rate of appropriate ICD interventions remained similar for the two time periods (5.1% vs. 4.4%; P = 0.43) and there were significantly fewer inappropriate ICD interventions (1.0% vs. 1.6%; P = 0.03). The proportion of ICD/CRT technical dysfunctions was comparable (3.5% vs. 2.65%; P = 0.7).
Virtual consultations have proved generally popular with HF patients. OPTIMIZE coordinators working at a HF unit in Buenos Aires, Argentina, reported that 90% of patients who responded to a satisfaction survey strongly agreed that virtual consultations were easy to take part in and all strongly agreed or agreed that their health problem could be resolved through such consultations [22].
In some countries, but not all, OPTIMIZE investigators reported that physicians and patients received information technology (IT) training to support this rapid shift to more digital communication, including remote patient monitoring and remote rehabilitation. Even so, many of the clinicians reported that they had found the telemedicine approach time consuming, with frequent technical or Internet access issues. From a clinical perspective, limited options for physical examinations were considered a significant drawback.
3.1. The experience in Italy
Italy was one of the first countries to be affected by COVID-19, with the first reported case on January 31, 2020. By November 2021, nearly 5 million cases had been reported and 72% of the population had been fully vaccinated. In a report by the Italian Superior Health Institute (ISHI) on a sample of 6713 people who died from COVID-19, the most frequent preexisting diseases were cardiovascular (27.9% ischemic heart disease, 24.3% atrial fibrillation, 15.9% heart failure, 11.6% hypertension and 11.6% previous stroke).
During the first phase of COVID-19, 54 hospitals participated in a multicenter, observational, nationwide survey on admissions to Italian cardiac care units during March 12–19, 2020 compared to the same period in 2019 [23]. Only 82 patients were hospitalized for HF during the 2020 week, compared with 154 during the equivalent week in 2019 (47% reduction, P = 0.005). The mean age of patients with HF remained 73 years, and the reduction was the same in both men and women. Fear of COVID-19 at hospitals appears to have discouraged patients from calling emergency services during the first wave of infection, particularly as media coverage suggested that COVID-19 was largely spread among hospitalized patients and healthcare personnel due to the lack of personal protection equipment. In addition, emergency services were largely focused on COVID-19 at that time.
As in many countries, the Italian national health system has been under greater pressure during the pandemic than at any time in its history. As a result of cuts in healthcare expenditure during the last decade, there was already substantial inequality of service across the country, and a policy imperative during the pandemic to ensure that hospital services were not overwhelmed.
Cardiologists in training have expressed concerns about the negative impact of the pandemic on their education [24], and this was also widely reported by OPTIMIZE investigators. Postponement of most elective procedures, reduction in non-emergency outpatient care and limited participation of trainees in procedures may have negatively affected clinical training during the pandemic. Replacement of in-person lectures with webinars and the temporary closure of core research laboratories will also have had an impact. Concerns were expressed that during the pandemic there were reduced opportunities for professional growth, resulting in an educational and skills gap that is unlikely to be filled during the rest of a training program.
3.2. The experience in Brazil
After the first case of COVID-19 was reported in Brazil in February 2020, the initial peak occurred in the Summer of 2020. The rapid spread of the SARS-CoV-2 gamma variant in early 2021 led to sustained high levels and one of the highest case numbers worldwide (approximately 22 million, about 9.5% of the population, by November 2021). After a slow start to vaccination (in January 2021), 63% of the population were fully vaccinated by November 2021.
OPTIMIZE Investigators from one center in the State of Rio de Janeiro reported that while HF units were not converted into COVID wards, there was an approximately 50% reduction in multidisciplinary team (MDT) staff. Many patients were reluctant to have face-to-face consultations and about half of patients refused to attend even when offered an appointment. Outpatient intravenous infusions (iron, diuretics and inotropes) were also reduced. There was a significant reduction in the number of HF hospitalizations and some patients died at home. Those who were hospitalized had more advanced disease and more severe volume overload.
HF consultations moved to phone or WhatsApp™ (video or voice), and some patients received prescriptions by email or by WhatsApp™. Clinicians were able to order tests, prescriptions, certificates and reports via online resources provided by the Federal Council of Medicine. Patients without Internet access received phone messages. Those undergoing rehabilitation were helped by MDT phone calls and videos, and MDT staff also made phone calls to find missing patients. Virtual consultations took longer than face-to-face consultations as patients took time to understand what they were being told. However, clinicians were able to offer a broader range of visual resources through these virtual consultations than with standard consultations.
The OPTIMIZE investigators reported that the majority of patients understood instructions about their care, but those with only elementary school education found it more difficult to cope and developed more complications. Some patients stopped all medications due to reduced income after job losses, and these individuals tended to have a poor prognosis. Some medication adjustments organized remotely were ineffective, leading to worsening of HF and the need for hospitalization. It was reported that virtual consultations were most suitable for stable patients with less severe HF and were not effective in those with advanced disease.
3.3. The experience in Taiwan
With approximately 16,500 cases of COVID-19 by November 2021, Taiwan has one of the lower rates of infection worldwide, and 38% of the population have been fully vaccinated. This situation, with the policy aim of ‘COVID free’ is in marked contrast to Italy and Brazil, discussed above, where the policy aim was to limit the healthcare impact of COVID infection.
As HF has been identified as the most common critical complication during exacerbations of COVID-19 in Taiwan, rapid viral screening before initial evaluation of HF was made mandatory, but this was reported as causing delays in acute HF management. Additionally, although patients were advised to visit hospital if their symptoms worsened, many patients hesitated due to coronavirus anxiety. As heart transplantation was generally prohibited during the COVID-19 outbreak, some patients with advanced HF have received a left ventricular assist device instead.
The OPTIMIZE investigators reported professional society activity to produce a Consensus Statement for the management of HF during the COVID-19 pandemic, drawn up by the Taiwanese Society of Cardiology, that included a recommendation to continue pharmacological therapy for HF [12]. To monitor patients' progress, a HF case manager contacts patients by telephone and patients (and caregivers) were instructed to measure vital signs, body weight, and assess fluid status every day. These data were transmitted to hospital via smart phone. Instead of scheduled outpatient visits, virtual visits with smart phones enabled physicians to evaluate patients and complete electronic medical records remotely. Prescriptions were sent by post to patients, so they could obtain medications at their local pharmacy without the traditional need to attend a hospital pharmacy. The costs of these procedures were covered by the National Health Insurance, so patients did not need to pay extra. Patients with HF were advised to stay at home during the COVID-19 pandemic and to take home-based exercise, although virtual rehabilitation was generally not available in most hospitals due to technical difficulties.
4. Lessons learnt for the future of HF care including recommendations for action
Investigators in the global OPTIMIZE network have reported major limitations on hospital-based care for patients with HF during the COVID-19 pandemic, with accompanying deterioration in morbidity and mortality. This is supported by evidence from the literature that hospital cardiovascular care changed dramatically during the pandemic, not only for HF but also for acute myocardial infarction [25]. In a report from the University Health Network, Toronto, Canada, emergency presentations with acute decompensated HF (ADHF) from March 1 to April 19, 2020, were 43.5% lower than in the same time period in 2019 (p = 0.002), and ADHF hospitalizations were down by 39.3% (p = 0.009) [2]. UK data reported by the National Institute for Cardiovascular Outcomes Research (NICOR) showed that in April 2020, there was a 66% reduction in the number of hospital admissions for HF compared to the average for January/April 2019 [26]. Unlike data for acute myocardial infarction, there was no noticeable upturn in HF admissions by mid-May 2020. The effects of the pandemic have been demonstrated not only on HF hospitalization but also on guideline-directed medical therapy for HF. Data from Italian Medicines Agency (AIFA) monitoring registries showed that from March to December 2020 the initiation of new patients with HF on sacubitril/valsartan decreased by nearly 40%, with prescriptions dropping to levels seen in 2018 [27]. There was a slight increase in prescriptions after the lockdown measures were lifted, but prescriptions remained below the pre-lockdown levels.
Emerging from this experience is the need for a new ‘blended’ model of care which replaces many (but not necessarily all) outpatient appointments with virtual consultations and telemonitoring, while retaining the option of rapid hospitalization for patients with worsening signs and symptoms (Table 2 ). Such a model needs to be flexible and responsive to sudden changes in circumstances as countries move, often with little warning, from a stable situation to exponentially rising levels of infection. It also needs to accommodate MDT working through good communication between hospital and community-based services so that the benefits of this type of coordinated approach achieved over many years of developments in HF care are not lost.
Table 2.
Summary of lessons learned and recommendations for change.
| Clinical | Patient | Logistical |
|---|---|---|
|
|
|
Telemedicine has been widely implemented in all healthcare settings, with some considerable success, but lack of ‘smart’ equipment, poor Internet coverage or access, and inadequate IT training – for both clinicians and patients – can discourage users and limit applications. Major investment is needed in many countries to ensure coverage across a large geographic area, and regulatory and reimbursement issues will have to be addressed in order to integrate necessary technologies into healthcare delivery. It must also be accepted that, for some patients with HF, telemedicine is not a substitute for all in-person specialist consultations, particularly where there is a need for physical examination, investigations, or the need to discuss complex issues, especially in advanced disease. Any telemedicine program must therefore include clear pathways back into hospital-based care for those with signs of HF deterioration that cannot be managed remotely. Many investigators also mentioned the need to develop rapport with their patients, but once this had been developed, then remote consultation could provide a very useful and convenient way of interacting with many patients.
Guidelines for the management of HF and the optimization of HF care delivery that reflect the COVID-19 era has been published [[9], [10], [11], [12], [13], [14],[28], [29], [30], [31]]. Adherence to this type of guidance will be important as we move into a phase where SARS-CoV-2 infection becomes endemic. It emphasizes the importance of rigorous COVID-19 testing for patients prior to admission and isolation of infected individuals for whom there is no alternative to hospitalization for deteriorating HF. Many members of the OPTIMIZE network have highlighted the benefits of the program during the pandemic in helping clinicians and patients to remain focused on key guideline-based treatment recommendations and to reduce the need for unplanned hospital visits and rehospitalizations.
OPTIMIZE investigators agreed that it is essential that patients and their families remain empowered and involved in their own management and care. In the Philippines, a ‘Getting back on track in HF care’ initiative has been started within the OPTIMIZE program to support virtual visits and encourage clinicians to teach patients about self-monitoring. In Indonesia, a user-friendly app is in development to help patients with self-monitoring, and a virtual patient group is planned to help patients become familiar with virtual consultations. Virtual education may not be easy, but we need to adapt to the new reality.
The impact of disrupted medicines supply chains and job losses arising from the pandemic on patients' ability to access, pay for and adhere to medication was raised as a concern by many OPTIMIZE investigators. This is another area which needs to be considered carefully as we move out of the pandemic and its knock-on economic consequences.
Because the current report focuses on the impact of the COVID-19 pandemic in the early phase where the alpha and beta variants were the main SARS-CoV-2 variants, it may not reflect the very recent period of the COVID-19 pandemic: the further mutation of the SARS-CoV-2 has led to higher infectivity but also to less virulence. Along with the higher rate of full vaccination in various countries, this will modify the impact of the COVID-19 pandemic on HF management.
Funding
The OPTIMIZE Heart Failure Care program is funded by Servier, which provided support for writing assistance and the organization of working group meetings.
CRediT authorship contribution statement
Martin R. Cowie: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing, Visualization. Ricardo Mourilhe-Rocha: Conceptualization, Methodology, Investigation, Writing – review & editing. Hung-Yu Chang: Conceptualization, Methodology, Investigation, Writing – review & editing. Maurizio Volterrani: Conceptualization, Methodology, Investigation, Writing – review & editing. Ha Ngoc Ban: Conceptualization, Methodology, Investigation, Writing – review & editing. Denilson Campos de Albuquerque: Conceptualization, Methodology, Investigation, Writing – review & editing. Edward Chung: Conceptualization, Methodology, Investigation, Writing – review & editing. Cândida Fonseca: Conceptualization, Methodology, Investigation, Writing – review & editing. Yuri Lopatin: Conceptualization, Methodology, Investigation, Writing – review & editing. José Antonio Magaña Serrano: Conceptualization, Methodology, Investigation, Writing – review & editing. Lilyana Mircheva: Conceptualization, Methodology, Investigation, Writing – review & editing. Gustavo Adolfo Moncada-Paz: Conceptualization, Methodology, Investigation, Writing – review & editing. Zurab Pagava: Conceptualization, Methodology, Investigation, Writing – review & editing. Eugenio B. Reyes: Conceptualization, Methodology, Investigation, Writing – review & editing. Clara Saldarriaga: Conceptualization, Methodology, Investigation, Writing – review & editing. Pedro Schwartzmann: Conceptualization, Methodology, Investigation, Writing – review & editing. David Sim Kheng Leng: Conceptualization, Methodology, Investigation, Writing – review & editing. Marcelo Trivi: Conceptualization, Methodology, Investigation, Writing – review & editing. Yoto Trifonov Yotov: Conceptualization, Methodology, Investigation, Writing – review & editing. Shelley Zieroth: Conceptualization, Methodology, Investigation, Writing – review & editing.
Declaration of competing interest
MRC reports consultancy fees from Servier, AstraZeneca, Medtronic, Abbott, Philips, and Roche Diagnostics. RMR has received consultancy fees and speaker honoraria from Servier, AstraZeneca, Boehringer Ingelheim, Bayer and Novartis. CF has received consultancy fees, grants and speaker honoraria from AstraZeneca, Bayer, Bial, Boehringer Ingelheim, Novartis, Roche, Sanofi, Servier and Vifor Pharma. YL has received consulting and speaker fees from Boehringer Ingelheim, Servier, MSD, and Novartis. EBR has received consulting fees from E. Merck, Pfizer, Innogen, Servier, and Torrent, speaker fees from AstraZeneca, Corbridge, Servier, Pfizer, E. Merck, Novartis, Innogen, and Boehringer Ingelheim, and research grants from Novartis and Corbridge. CS has received speaker honoraria from Servier, AstraZeneca, Boehringer Ingelheim, Novartis, Medtronic, Bayer and Merck, consulting fees from Servier, Bayer, AstraZeneca, Merck and Novartis, and honoraria as a principal investigator from Bayer, Novartis, and Merck. PS has received honoraria from Servier, Novartis, Bayer, AstraZeneca and Boehringer Ingelheim. SZ has received research grant support or served on advisory boards for Abbott, Akcea, AstraZeneca, Amgen, Alnylam, Bayer, Boehringer Ingelheim, Eli Lilly, Merck, Novartis, Otsuka, Pfizer, Servier, and Vifor, she has speaker engagements Amgen, AstraZeneca, Bayer, Boehringer-Ingelheim, Eli-Lilly, Novartis, Novo Nordisk, Servier, and Vifor, and she serves on a clinical trial steering committee or as a national lead for studies sponsored by AstraZeneca, Bayer, Boehringer Ingelheim, Merck and Novartis. HYC, MV, HNB, DCDA, EC, JAMS, LM, GAMP, ZP, DSKL, MT, and YTY have no competing interests to declare.
Acknowledgments
We gratefully acknowledge the contributions of the following OPTIMIZE Heart Failure Care program coordinators who provided input for this article:
Wael AlMahmeed (United Arab Emirates), Ha Ngoc Ban (Vietnam), Denilson Campos de Albuquerque (Brazil), Hung-Yu Chang (Taiwan), Anna I. Chesnikova (Russian Federation), Ovidiu Chioncel (Romania), Dong-Ju Choi (South Korea), Edward Chung (Jamaica), Martin R. Cowie (UK), Cândida Fonseca (Portugal), Mahmoud Hassanein (Egypt), Hamlet G. Hayrapetyan (Armenia), Małgorzata Lelonek (Poland), Przemysław Leszek (Poland), Yuri Lopatin (Russian Federation) José Antonio Magaña Serrano (Mexico), Lilyana Mircheva (Bulgaria), Gustavo Adolfo Moncada-Paz (Honduras), Ricardo Mourilhe-Rocha (Brazil), Noémi Nyolczas (Hungary), Zurab Pagava (Georgia), Jin Joo Park (South Korea), Arintaya Phrommintikul (Thailand), Rarsari Soerarso Pratikto (Indonesia), Amina G. Rakisheva (Kazakhstan), Eugenio B. Reyes (Philippines), Clara Saldarriaga (Colombia), Mohamed Ayman Saleh (Egypt), Pedro Schwartzmann (Brazil), David Sim Kheng Leng (Singapore), Hamayak Sisakian (Armenia), Marcelo Trivi (Argentina), Maurizio Volterrani (Italy), Leonid G. Voronkov (Ukraine), Kyaw Soe Win (Myanmar), Yoto Trifonov Yotov (Bulgaria), Shelley Zieroth (Canada).
The organization of working group meetings and the collection of input from national coordinators was supported by MedEd Global Solutions. Writing assistance was provided by Jenny Bryan.
Footnotes
All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
OPTIMIZE Heart Failure Care program coordinators who provided input for this article are listed in the acknowledgments.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcard.2022.06.022.
Appendix A. Supplementary data
Daily new confirmed COVID-19 cases in Italy, Brazil, and Taiwan (February 1, 2020 – January 15, 2022)
References
- 1.Cannatà A., Bromage D.I., Rind I.A., Gregorio C., Bannister C., Albarjas M., et al. Temporal trends in decompensated heart failure and outcomes during COVID-19: a multisite report from heart failure referral centres in London. Eur. J. Heart Fail. 2020;22:2219–2224. doi: 10.1002/ejhf.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frankfurter C., Buchan T.A., Kobulnik J., Lee D.S., Luk A., McDonald M., et al. Reduced rate of hospital presentations for heart failure during the COVID-19 pandemic in Toronto, Canada. Can. J. Cardiol. 2020;36:1680–1684. doi: 10.1016/j.cjca.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burgos L.M., Diez M., Villalba L., Miranda R.M., Belardi J. [Impact of the COVID-19 pandemic on heart failure hospitalizations] [Article in Spanish] Medicina (B Aires) 2020;80:315–316. [PubMed] [Google Scholar]
- 4.Hall M.E., Vaduganathan M., Khan M.S., Papadimitriou L., Long R.C., Hernandez G.A., et al. Reductions in heart failure hospitalizations during the COVID-19 pandemic. J. Card. Fail. 2020;26:462–463. doi: 10.1016/j.cardfail.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morishita T., Takada D., Shin J.-h., Higuchi T., Kunisawa S., Fushimi K., et al. Effects of the COVID-19 pandemic on heart failure hospitalizations in Japan: interrupted time series analysis. ESC Heart Fail. 2021 doi: 10.1002/ehf2.13744. Dec 16 [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ta Anyu A., Badawy L., Cannata A., Bromage D.I., Rind I.A., Albarjas M., et al. Long-term outcomes after heart failure hospitalization during the COVID-19 pandemic: a multisite report from heart failure referral centers in London. ESC Heart Fail. 2021;8:4701–4704. doi: 10.1002/ehf2.13579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou P., Yang X.-L., Wang X.-G., Hu B., Zhang L., Zhang W., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cigarroa-López J.A., Magaña-Serrano J.A., Álvarez-Sangabriel A., Ruíz-Ruíz V., Chávez-Mendoza A., Méndez-Ortíz A., et al. [Recommendations for the care of patients with heart failure and COVID-19] [Article in Spanish] Arch. Cardiol. Mex. 2020;90:26–32. doi: 10.24875/ACM.M20000060. [DOI] [PubMed] [Google Scholar]
- 9.Torres Navas A., Rivera Toquica A., García Peña Á.A., Arias C.A., Saldarriaga Giraldo C.I., Gómez López E.A., et al. [Evaluation and treatment of heart failure during the COVID-19 pandemic: executive summary. Recommendations from the section on heart failure, transplantation and pulmonary hypertension of the Columbian Association of Cardiology and Cardiovascular Surgery.] [Article in Spanish] Rev. Cardiol. Colomb. 2020;27 [Google Scholar]
- 10.DeFilippis E.M., Reza N., Donald E., Givertz M.M., Lindenfeld J., Jessup M. Considerations for heart failure care during the COVID-19 pandemic. JACC Heart Fail. 2020;8:681–691. doi: 10.1016/j.jchf.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang Y., Coats A.J.S., Zheng Z., Adamo M., Ambrosio G., Anker S.D., et al. Management of heart failure patients with COVID-19: a joint position paper of the Chinese heart failure Association & National Heart Failure Committee and the heart failure Association of the European Society of cardiology. Eur. J. Heart Fail. 2020;22:941–956. doi: 10.1002/ejhf.1915. [DOI] [PubMed] [Google Scholar]
- 12.Lin K.C., Wang C.C., Huang W.C., Hwang J.J. Considerations when managing heart failure during the COVID-19 pandemic – consensus from the Taiwan Society of Cardiology. Acta Cardiol. Sin. 2021;37:125–129. doi: 10.6515/ACS.202103_37(2).20200916A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Task Force for the management of COVID-19 of the European Society of Cardiology European Society of Cardiology guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: part 1—epidemiology, pathophysiology, and diagnosis. Eur. Heart J. 2022;43:1033–1058. doi: 10.1093/eurheartj/ehab696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Task Force for the management of COVID-19 of the European Society of Cardiology ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: part 2—care pathways, treatment, and follow-up. Eur. Heart J. 2022;43:1059–1103. doi: 10.1093/eurheartj/ehab697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cowie M.R., Lopatin Y.M., Saldarriaga C., Fonseca C., Sim D., Magaña J.A., et al. The optimize heart failure care program: initial lessons from global implementation. Int. J. Cardiol. 2017;236:340–344. doi: 10.1016/j.ijcard.2017.02.033. [DOI] [PubMed] [Google Scholar]
- 16.Puwanant S., Sinphurmsukskul S., Krailak L., Nakaviroj P., Boonbumrong N., Siwamogsatham S., et al. The impact of the coronavirus disease and tele-heart failure clinic on cardiovascular mortality and heart failure hospitalization in ambulatory patients with heart failure. PLoS One. 2021;16 doi: 10.1371/journal.pone.0249043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arutyunov G.P., Tarlovskaya Е.I., Arutyunov A.G., Belenkov Y.N., Konradi A.O., Lopatin Y.M., et al. Clinical features of post-COVID-19 period. Results of the international register “Dynamic analysis of comorbidities in SARS-CoV-2 survivors (AKTIV SARS-CoV-2)”. Data from 6-month follow-up. Russian J. Cardiol. 2021;26:4708. doi: 10.15829/1560-4071-2021-4708. [DOI] [Google Scholar]
- 18.Correia M.J., Guerreiro R., Chaves J., Madeira D., Eça R., Monteiro M., et al. Presented at the 26th Portuguese National Congress on Internal Medicine, Braga, Portugal, May 21–24. 2020. Healthcare access for the chronically ill during the COVID-19 pandemic – the example of heart failure. [Google Scholar]
- 19.Lelonek M., Książczyk M., Pawlak A., Gąsior M., Rozentryt P., Nessler J. Heart failure management in Polish medical centers during the coronavirus disease 2019 pandemic: results of a survey. Kardiol. Pol. 2020;78:1035–1038. doi: 10.33963/KP.15584. [DOI] [PubMed] [Google Scholar]
- 20.Guerreiro R., Correia M.J., Chaves J., Madeira D., Eça R., Monteiro M., et al. Presented at the 26th Portuguese National Congress on Internal Medicine, Braga, Portugal, May 21–24. 2020. Reorganization of a heart failure clinic due to the COVID-19 pandemic. [Google Scholar]
- 21.Tajstra M., Wojtaszczyk A., Sterliński M., Świerżyńska E., Szumowski Ł., Tomasiuk M., et al. Patients with heart failure and an implanted cardioverter-defibrillator during the coronavirus disease 2019 pandemic: insights from a multicenter registry in Poland. Kardiol. Pol. 2021;79:562–565. doi: 10.33963/KP.15918. [DOI] [PubMed] [Google Scholar]
- 22.Burgos L.M., Benzadón M., Candiello A., Cabral M.H., Conde D., Alberto de Lima A., et al. Telehealth in heart failure care during COVID-19 pandemic lockdown in Argentina. Int. J. Heart Fail. 2020;2:247–253. doi: 10.36628/ijhf.2020.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.De Rosa S., Spaccarotella C., Basso C., Calabrò M.P., Curcio A., Filardi P.P., et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Strangio A., Leo I., Spaccarotella C.A.M., Barillà F., Basso C., Calabrò M.P., et al. Effects of the COVID-19 pandemic on the formation of fellows in training in cardiology. J. Cardiovasc. Med. (Hagerstown) 2021;22:711–715. doi: 10.2459/jcm.0000000000001185. [DOI] [PubMed] [Google Scholar]
- 25.Sofi F., Dinu M., Reboldi G., Stracci F., Pedretti R.F.E., Valente S., et al. Worldwide differences of hospitalization for ST-segment elevation myocardial infarction during COVID-19: a systematic review and meta-analysis. Int. J. Cardiol. 2022;347:89–96. doi: 10.1016/j.ijcard.2021.10.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Institute for Cardiovascular Outcomes Research (NICOR) COVID-19 Report Rapid Cardiovascular Data: We Need it Now (and in the Future) September 2020. https://www.nicor.org.uk/covid-19-and-nicor/nicor-covid-19-report/ Available at.
- 27.Rosano G.M.C., Celant S., Olimpieri P.P., Colatrella A., Onder G., Di Lenarda A., et al. Impact of the COVID-19 pandemic on prescription of sacubitril/valsartan in Italy. Eur. J. Heart Fail. 2022 doi: 10.1002/ejhf.2490. Mar 18 [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Virani S.A., Clarke B., Ducharme A., Ezekowitz J.A., Heckman G.A., McDonald M., et al. Optimizing access to heart failure care in Canada during the COVID-19 pandemic. Can. J. Cardiol. 2020;36:1148–1151. doi: 10.1016/j.cjca.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roifman I., Arora R.C., Bewick D., Chow C.-M., Clarke B., Cowan S., et al. Cardiovascular care delivery during the second wave of COVID-19 in Canada. Can. J. Cardiol. 2021;37:790–793. doi: 10.1016/j.cjca.2020.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gorodeski E.Z., Goyal P., Cox Z.L., Thibodeau J.T., Reay R.E., Rasmusson K., et al. Virtual visits for care of patients with heart failure in the era of COVID-19: a statement from the Heart Failure Society of America. J. Card. Fail. 2020;26:448–456. doi: 10.1016/j.cardfail.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Silva-Cardoso J., González Juanatey J.R., Comin-Colet J., Sousa J.M., Cavalheiro A., Moreira E. The future of telemedicine in the management of heart failure patients. Card Fail. Rev. 2021;7 doi: 10.15420/cfr.2020.32. e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Daily new confirmed COVID-19 cases in Italy, Brazil, and Taiwan (February 1, 2020 – January 15, 2022)