Abstract
Objectives:
To determine the prevalence of alcohol use disorder and associated factors among residents of Dilla town, Gedeo zone, Southern Ethiopia, 2021.
Methods:
A community-based cross-sectional study was conducted among 666 randomly selected participants. Interview-assisted structured questionnaire was used to collect data, and alcohol use disorder identification test was employed to measure alcohol use disorder. The data were entered in to Epi info version 7 and exported in to SPSS version 25 for analysis. Both bivariate and multivariate binary logistic regression analysis were used to identify significant factors related with alcohol use disorder. In the multivariate model, variables with p value < 0.05 were considered as a statistical significant factor for the outcome variable. Finally, adjusted odds ratio with 95% confidence interval was computed to assess the strength of association.
Results:
The magnitude of alcohol used disorder during the past year was 30.6% (95% confidence interval: 25.5%–35.7%). Being male (adjusted odds ratio = 8.33, 95% confidence interval: (4.34, 15.98)), age of less than 33 years old (adjusted odds ratio = 1.78, 95% confidence interval: (1.06, 3.00)), current cigarette smoking (adjusted odds ratio = 2.49, 95% confidence interval: (1.42, 4.37)), current khat chewing (adjusted odds ratio = 6.23, 95% confidence interval: (3.8, 9.92)), high level of psychological distress (adjusted odds ratio = 7.69, 95% confidence interval: (4.16, 14.28)) and poor social support (adjusted odds ratio = 2.30, 95% confidence interval: (1.27, 4.18)) were significantly associated with alcohol use disorder.
Conclusion:
A large percentage of respondents in our sample had an alcohol use disorder. Alcohol use problems were linked to being men, under the age of 33 years old, current khat chewing, current cigarette smoking, a high level of psychological distress, and poor of social support. As a result, early screening, public health intervention programs and establishing appropriate referral linkages with mental health facilities are recommended.
Keywords: Alcohol, alcohol use disorder, associated factors, COVID-19, Ethiopia
Introduction
Alcohol is a psychoactive substance that is legal, culturally and socially acceptable, and commonly consumed in most nations throughout the world. 1 Alcohol use disorder (AUD) is a mental disorder defined by the negative consequences of frequent alcohol use, a pattern of compulsive alcohol use, and (occasionally) physiological dependence on alcohol (i.e. tolerance and/or withdrawal symptoms) 2 and identified by the Alcohol Use Disorders Identification Test (AUDIT), which is used as a screening instrument in primary care research, both in the general population and in hospital patients.3,4
Globally, around 2 billion people consume alcohol, with over 76 million people suffering from addiction. 5 According to a World Health Organization (WHO) report, alcohol consumption causes 3 million fatalities worldwide each year, as well as impairments and bad health for millions more individuals. Overall, hazardous alcohol use accounts for 5.1% of the global burden of disease, with males accounting for 7.1% and females accounting for 2.2% of the global burden of disease, respectively. 6
Until 10 August 2021, there were 285,413 cases, 4440 fatalities, and 264,798 recovery cases documented following the onset of the COVID-19 pandemic in Ethiopia 7 and with a negative significant impact on the day-to-day activities of individuals living throughout the country, as evidenced by a study conducted in similar settings with more than half of the population developing mild-to-severe psychological disturbances. 8
Many people are using substances during the COVID-19 epidemic, and alcohol is the most extensively utilized in most sections of the country. 9 Harmful alcohol consumption during the era of COVID-19 pandemic might be responsible for the different human rights violations, including physical and sexual abuse, bodily disease, including unwanted pregnancies, and death, 10 as well as a higher risk of death from all causes, including all diseases and medical conditions, and suicide, resulting in shorter life expectancy. 11 Furthermore, it increases the likelihood of developing bacterial and viral lung infections substantially (including COVID-19) 12 and a higher risk of HIV/AIDS transmission. 13
According to WHO, 14 the prevalence of AUD in the adult population ranges from 8.8% in Europe to 0.8% in the Eastern Mediterranean Region in 2018. It has been revealed that among COVID-19 patients hospitalized in England, 28.6% have a moderate degree of alcohol consumption, 15 in Australia, surveys indicated that 25%–52.7% of the sample had a risky pattern of alcohol usage during the COVID-19 pandemic,16,17 higher proportions of AUD were also discovered in China 18 and according to the studies, prolonged worrying (fear of contracting the COVID-19) leads to the development of anxiety disorders, as well as an increased risk of heavy alcohol use and the development of AUDs.19,20 According to the results of the Ethiopian Demographic and Health Survey (EDHS) in 2016, alcohol consumption among people aged 15–59 years old in Ethiopia was 46.64%. 21 A few community studies in Ethiopia found that the prevalence of AUDs ranged from 11.4% to 27% prior to the COVID-19 pandemic.22–25
The negative impacts of alcohol consumption can be seen in the short- and long-term repercussions on individuals and their families, as well as the entire society and property devastation. 26 The WHO 27 has set a goal of lowering hazardous alcohol usage by 10% by 2025. As a result, the government of Ethiopia has taken steps such as raising the price of each type of alcohol and limiting the amount of time each type of alcohol can be promoted on social media. 28 However, insufficient research has been conducted to demonstrate the efficiency of prevention initiatives and the consequences of COVID-19 pandemic on alcohol consumption.
To the best of our knowledge, there was no enough community-based studies targeted at assessing the prevalence of AUD and its related factors in several sections of the country, including the current research area during the era of COVID-19 pandemic. As a result, the purpose of this study was to assess the prevalence of AUD and its associated factors in Dilla town, Gedeo zone, southern Ethiopia in the past year preceding the data collection period. The outcomes of this study will be useful in determining the applicability of alcohol use prevention programs and identifying key contributing elements to the behavior. In addition, the findings are critical in order to make a positive impact on policymakers and to provide input for an evidence-based alcohol use issue intervention program. Moreover, the findings of this study could be utilized to connect individuals with AUDs to mental health facilities in the town at the time of the study, as well as to launch public health interventions to minimize AUDs through integration with various levels of health care services.
Methods and materials
Study area, period, and design
The study was conducted in Dilla administrative town, which is the capital of Gedeo zone of south nation nationality representative region (SNNRP) and 365 km away from Addis Ababa, the capital city of Ethiopia. The town has total population of 95,376 with 19,464 households and five kebeles (smallest administrative units in the town). There is one governmental hospital served as referral service for zone and for neighboring zones and two health centers with their satellite health posts. The hospital has psychiatric clinic providing both outpatient and in-patient services. Community-based cross-sectional survey was employed to conduct the study from 1 September to 2 October 2021.
Population
All residents of Dilla town with age of 18 and above years were considered as source population. Adult age 18 years and above who were available during the study period was the study population.
Eligibility criteria
Individuals of age 18 years and above in the household and permanently reside in the selected kebeles for 6 month and above were included. Individuals who are unable to communicate and severely ill were excluded from the study.
Sample size determination
The total sample size for the study was computed under the assumption of single population proportion formula considering 27% of AUD from previous study conducted in Ambo town, Ethiopia, 23 two-sided confidence interval (95% CI = 1.96), 5% of margin of error and 10% non-response rate. Bearing in mind of design effect of 2, the final sample size was 666.
Sampling technique and procedure
Multi-stage sampling technique was used to recruit 666 study participants. From a total of five kebeles, two kebeles were selected using simple random sampling techniques. To select individuals in the household systematic sampling technique was employed after selecting the first household randomly using lottery method. The sample size (666) was proportionally allocated to each selected kebeles proportional to their size of households, then ever 15th households were selected. In the case of more than one individual in a household lottery method was used to select one of them. When an eligible participant was not found at home, the interviewers returned to the household at various intervals, and if the interviewers were unable to locate an eligible participant, the household was marked as non-respondent.
Data collection tools and procedures
The data were collected using interview administered structured questionnaire developed by reviewing different previously published articles.23,29–31 The data collection tools were categorized into different sections namely; respondent’s socio-demographic characteristics, AUDIT questionnaires, K-10 questionnaires to asses’ psychological distress, social support scales used to determine the social support status of the respondents, the current and life time history of substance use of the respondents.
The WHO’s AUDIT questionnaire was used to screen AUDs.3,32 In primary-care studies, the AUDIT was found to be the best screening instrument for the complete range of alcohol problems, both in the general population and in specific institutional groups like hospital patients with sensitivity 94.1% and specificity of 91.7%.3,33 The AUDIT score is divided into four sections: the first three questions (1–3) evaluate the quantity and frequency of alcohol use (hazardous alcohol use); the second three questions (4–6) assess indicators of alcohol dependency; and the last four (7–10) investigate alcohol-related disorders (harmful alcohol use). Each question has a response category ranging from 0 to 4, with the first response scoring “0” never, “1” less than monthly, “2” monthly, “3” weekly, and “4” daily or practically daily. Question 9 and 10 contain only three possible answers and are scored as 0, 2, and 4. The AUDIT scores are totaled to produce an overall score ranging from 0 to 40.
In our study, the score was divided into four cut-off points: 0–7 implies low risk, 8–15 denotes risk/hazardous use, 16–19 denotes harmful use, and 20–40 denotes the possibility of alcohol dependency. Finally, we split our participants into two groups to get a binary outcome; those with an AUDIT score of ⩾8 (the cut-off point) were considered positive screening results (AUDs). The cut-off value of 8 for AUD has been confirmed across multiple nations,34–37 and previous Ethiopian research indicated that the internal consistency of AUDIT was outstanding (Cronbach’s = 0.90). 38 The internal consistency of AUDIT in this study was similarly excellent (Cronbach’s = 0.87).
The Kessler Psychological Distress Scale (K10) was used to determine the level of perceived psychological stress. 39 The K10 scale consists of 10 questions regarding emotional states, each with a 5-level response scale. The measure can be used as a brief screen to determine degrees of distresses, and the respondents’ scores were grouped as follows: 10–19 likely to be well; 20–24 likely to have a mild disorder; 25–29 likely to have a moderate disorder; and 30–50 likely to have a severe disorder. The scale has a good internal consistency of 0.93, sensitivity of 84.2%, and specificity of 77.8%. 40
The social support was measured with a three-item Oslo social support scale (OSSS-3) with a score range of 3 to 14. “Scores of 12–14 indicate strong support,” “scores of 9–11 indicate moderate social support,” and “scores of 3–8 indicate poor social support,”41,42 and the scale exhibited good internal consistency with a Cronbach’s alpha of 0.91. 43
The Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) version 2.0 was used to assess current and lifetime substance use of the respondents which was developed by WHO: 44 individuals noted with a recent 1 month history of any substance use were classified as current substance users, whereas those respondents with at least once lifetime exposure to any substance were classified as lifetime users, and the tools had 0.84 reliability and 0.97 test–retest reliability with Intraclass Correlation Coefficient (ICC) = 0.90.45,46
The data were collected by 4th year psychiatry students of dilla university after having 1 day of training about the objective of study, the study instruments, consent form, how to interview and follow the techniques of data collection procedure. Finally, data were collected through face-to-face interview after obtaining informed consent from the participants.
Statistical analysis
First the data were checked for completeness and consistence, and then it was coded. The coded data were entered in to epidemiological information (Epi info), software version 7 and exported to Statistical Package for Social Science (SPSS) version 25 for further statistical analysis. The results were expressed in terms of frequency (percentage) for categorical variable and means with standard deviation for continouse variables. Both bivariate and multivariate binary regression analysis was done to assess factors associated with AUD. Variables with p value < 0.25 in bivariate analysis were considered for multivariate binary logistic regression to control. In the multivariate model, variables with p value < 0.05 were considered as a statistical significant factor for the outcome variable. Finally, adjusted odds ratio (AOR) with 95% CI was computed to assess the strength of association.
Data quality control
Before the actual data collection pretest was conducted on 5% of the total sample size other than the selected kebeles, then correction on ambiguous items in the developed tools before the actual data collection. The written structured questionnaire was translated in to Amharic language and back to English by the selected Amharic and English language expert. At the end of the day of data collection, the collected data were checked by the selected group members for completeness.
Variables
The dependent variable in this study was AUD; whereas, the independent variables were socio-demographic and economic characteristics: age, sex, marital status, religion, educational status, monthly income of the household, family size, occupational status, psychosocial, and substance use characteristics: family history of substance use, current khat chewing, current cigarette smoking, life time history of cigarette smoking, life time history khat chewing, and psychological distress and social support.
Operational definitions
Khat: A moderately narcotic stimulant that is typically ingested by chewing the green leaf. 47
Result
Socio-demographic characteristics
The total number of participants in this study was 666, with a response rate of 100%. The mean (standard deviation (SD) age of the participants was 33.3 ± 11.3 years, with 56.4% of those under 33 years old. Around 466 (70%) of the 666 participants were men, 316 (47.4%) were married, 141 (21.2%) had attended primary education, 187 (28.1%) were merchants, 340 (51.1%) have a mean monthly income of more than 1539 Ethiopian birr (ETB) and 406 (61%) of the respondents had mean family size of ⩾5 (Table 1).
Table 1.
Socio-demographic characteristics among residents of Dilla town, Southern Ethiopia, 2021 (N = 666).
| Variables | Categories | Frequency | Percent (%) |
|---|---|---|---|
| Sex | Male | 466 | 70 |
| Female | 200 | 30 | |
| Mean age (years) | <33 | 376 | 56.4 |
| ⩾33 | 290 | 43.6 | |
| Marital status | Single | 282 | 42.3 |
| Married | 316 | 47.4 | |
| Divorced | 68 | 10.2 | |
| Educational status | Unable to read and write | 95 | 14.3 |
| Read and write | 215 | 32.3 | |
| Primary education | 141 | 21.2 | |
| Secondary | 98 | 14.7 | |
| College and above | 117 | 17.6 | |
| Occupational status | Government employer | 81 | 12.2 |
| Private worker | 186 | 27.9 | |
| Farmer | 84 | 12.6 | |
| Merchant | 187 | 28.1 | |
| Student | 128 | 19.2 | |
| Religion | Orthodox | 206 | 30.9 |
| Muslim | 204 | 30.6 | |
| Protestant | 220 | 33.0 | |
| Catholic | 36 | 5.4 | |
| Mean monthly income of the household (in Ethiopian birr (ETB) | < 1539 ETB | 326 | 48.9 |
| >= 1539ETB | 340 | 51.1 | |
| Mean family size (in number) | < 5 | 260 | 39 |
| ⩾ 5 | 406 | 61 |
Psychosocial and substance use characteristics
About 354 (53.2%) of the 666 participants had a family history of alcohol use, and 306 (45.9%) had a lifetime history of cigarette smoking. Furthermore, 262 (39.3%) and 218 (32.7%) were current smokers and khat chewers, respectively (Table 2).
Table 2.
Psychosocial and substance use characteristics among residents of Dilla town, Southern Ethiopia, 2021 (N = 666).
| Variables | Categories | Frequency | Percentage (%) |
|---|---|---|---|
| Family history of alcohol use | Yes | 354 | 53.2 |
| No | 321 | 46.8 | |
| Life time history of cigarette smoking | Yes | 306 | 45.9 |
| No | 360 | 54.1 | |
| Life time history khat chewing | Yes | 262 | 39.3 |
| No | 404 | 67.3 | |
| Current khat chewing | Yes | 218 | 32.7 |
| No | 448 | 60.7 | |
| Current cigarette smoking | Yes | 276 | 41.4 |
| No | 390 | 58.6 | |
| Social support | Poor | 282 | 42.3 |
| Moderate | 264 | 39.7 | |
| Strong | 120 | 18 |
Level of psychological distress
The participants’ level of perceived psychological stress was assessed. Out of the total 666 participants, 386 (58%) had a low level of psychological distress, 186 (27.9%) had a moderate level of psychological distress, and 94 (14.1%) had a high level of psychological distress (Figure 1).
Figure 1.
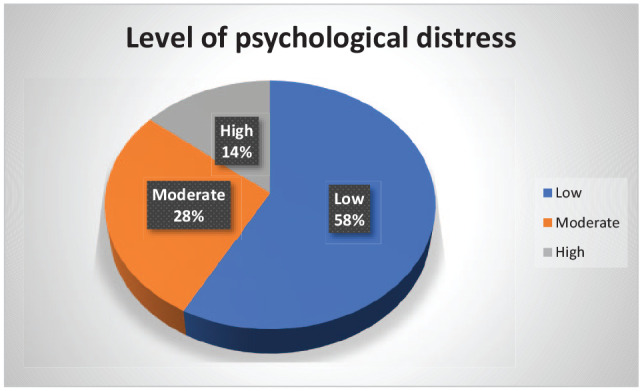
Level of psychological stress among residents of Dilla town, Southern Ethiopia, 2021 (N = 666).
Magnitude of AUD
The magnitude of AUD among 666 participants was assessed in this study. Based on their AUDIT score values, participants were divided into 462 (69.4%) who were not at risk, 132 (19.8%) who were at risk, 52 (7.8%) who were harmful, and 20 (3%) who were dependent. After reclassifying, 204 (30.6%; % CI: 25.5$–35.7%) of respondents had positive result for AUDIT, while 462 (69.4%; 95% CI: 64.3%–74.5%) of the respondents had negative result for AUDIT in the past year preceding the data collection period (Figure 2).
Figure 2.
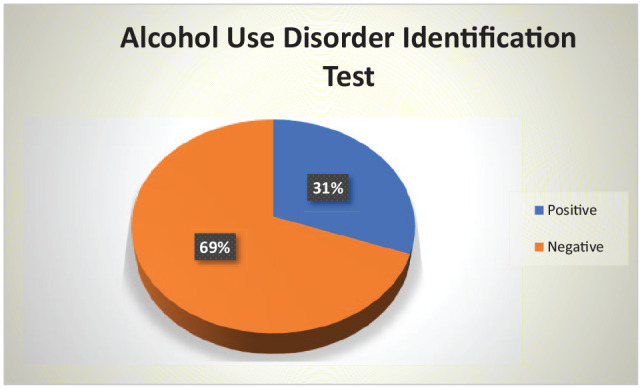
The proportion of alcohol use disorder identification test results among residents of Dilla town, GEDEO zone southern Ethiopia, 2021 (n = 666).
Factors associated with AUD
To determine the association between the independent variables with AUD identification test both bivariate and multivariate binary logistic regression analysis was carried out. In bivariate binary logistic regression analysis, factors which are significantly associated with AUD at p value of <0.25 were sex of the participants, age, marital status, occupational status, mean family size, life time history of cigarette smoking, current cigarette smoking, current khat chewing, level of psychological stress and social support candidate’s for multivariate binary logistic analysis.
Results from multivariate binary logistics analysis showed that male sex, younger age, current cigarette smoking, current khat chewing, level of psychological distress and social support were factors significantly associated with positive AUD identification test at p value of <0.05.
This study showed that the odds of positive result on AUDIT were 8.33 times higher among males than females (AOR = 8.33, 95% CI: (4.34, 15.98)). The odds of positive AUDIT were 1.78 times higher among participants with age groups of less than 33 years old as compared with those 33 years old and higher (AOR = 1.78,95% CI: (1.06, 3.00)). The odds of positive AUDIT were 2.49 times higher among current cigarette smoking than those with no history of current cigarette smoking (AOR = 2.49, 95% CI: (1.42, 4.37)). The odds of positive AUDIT were 6.23 times higher among current history of khat chewing than the participants with no current history of khat/khat (AOR = 6.23, 95% CI: (3.8, 9.92)).
The odds of positive AUDIT were 7.69 times higher among participants with severe psychological distress than participants with low level of psychological stress (AOR = 7.69, 95% CI: (4.16, 14.28)). The odds of positive AUDIT among participants with moderate level of psychological distress were 2.56 times higher than those with low level of psychological distress (AOR = 2.56, 95%CI: (1.35, 4.76)).
Moreover, the odds of positive AUDIT with participants who had poor social were 2.30 times higher than participants with good social support (AOR = 2.30, 95% CI: (1.27, 4.18)). Similarly, the odds of positive AUDIT with participants who had moderate social support were 2.38 times higher as compared with participants with good social support (AOR = 2.38, 95% CI: (1.29, 4.38); Table 3).
Table 3.
Factors associated with alcohol use disorder among residents of dilla town, southern Ethiopia, 2021(n = 666).
| Variables | Alcohol use disorder identification test | COR (95% CI) | p value | AOR (95% CI) | p value | |
|---|---|---|---|---|---|---|
| Positive (%) | Negative (%) | |||||
| Sex | 0.001 | |||||
| Male | 190 (93.1) | 276 (59.7) | 9.15 (5.15, 16.23) | 8.33 (4.34, 15.98) | 0.001** | |
| Female | 14 (6.9) | 186 (40.3) | 1 | 1 | ||
| Age (years) | 0.135 | |||||
| <33 | 124 (60.8) | 252 (54.5) | 1.29 (0.92, 1.81) | 1.78 (1.06, 3.00) | 0.029* | |
| ⩾33 | 80 (39.2) | 210 (45.5) | 1 | 1 | ||
| Marital status | 0.006 | |||||
| Single | 100 (49) | 182 (39.4) | 0.89 (0.51, 1.53) | 0.72 (0.33, 1.56) | 0.413 | |
| Married | 78 (38.2) | 238 (51.5) | 0.53 (0.30, 0.92) | 0.58 (0.29, 1.17) | 0.131 | |
| Divorced | 26 (12.7) | 42 (9.1) | 1 | 1 | ||
| Educational status | 0.286 | |||||
| Unable to read and write | 21 (10.3) | 74 (16.0) | 0.79 (0.42, 1.49) | |||
| Able to read and write | 73 (35.8) | 142 (30.7) | 1.43 (0.87, 2.35) | |||
| Primary school | 56 (27.5) | 85 (18.4) | 1.52 (0.96, 2.12) | |||
| Secondary school | 23 (11.3) | 75 (16.2) | 0.85 (0.46, 1.58) | |||
| College and above | 31 (15.1) | 86 (18.7) | 1 | |||
| Occupational status | 0.002 | |||||
| Government employee | 32 (15.7) | 49 (10.6) | 1.81 (0.99, 3.27) | 1.60 (0.75,3.43) | 0.228 | |
| Private employee | 72 (35.3) | 114 (24.7) | 1.75 (1.07, 2.85) | 1.37 (0.71, 2.63) | 0.341 | |
| Farmer | 15 (7.4) | 69 (14.9) | 0.60 (0.30, 1.19) | 0.61 (0.26, 1.41) | 0.248 | |
| Merchant | 51 (25.0) | 136 (29.4) | 1.04 (0.62, 1.72) | 0.75 (0.38, 1.48) | 0.408 | |
| Student | 34 (26.6) | 94 (20.3) | 1 | 1 | ||
| Mean family size(in number) | 0.014 | |||||
| <5 | 94 (46.1) | 166 (35.9) | 1.52 (1.09, 2.13) | 1.18 (0.77, 1.82) | 0.436 | |
| ⩾5 | 110 (53.9) | 296 (64.1) | 1 | 1 | ||
| Mean monthly income | 0.486 | |||||
| <1,539 ETB | 104 (51.0) | 222 (48.1) | 1.12 (0.81, 1.56) | |||
| ⩾1,539 ETB | 100 (49.0) | 240 (51.9) | 1 | |||
| Family history of alcohol use | 0.942 | |||||
| Yes | 108 (52.9) | 246 (53.2) | 1.01 (0.73, 1.40) | |||
| No | 96 (47.1) | 216 (46.8) | 1 | |||
| Life time history of cigarette smoking | 0.001 | |||||
| Yes | 142 (69.6) | 164 (35.5) | 4.16 (2.92, 5.93) | 1.44 (0.81, 2.58) | 0.213 | |
| No | 62 (30.4) | 298 (64.5) | 1 | 1 | ||
| Life time history of khat chewing | 0.619 | |||||
| Yes | 84 (41.2) | 178 (38.5) | 1.12 (0.80, 1.56) | |||
| No | 120 (58.8) | 284 (61.5) | 1 | |||
| Current cigarette smoking | 0.001 | |||||
| Yes | 134 (65.7) | 142 (30.7) | 4.31 (3.04, 6.12) | 2.49 (1.42, 4.37) | 0.010 ** | |
| No | 70 (34.3) | 320 (69.3) | 0.23 (0.16, 0.33) | 1 | ||
| Current khat chewing | 0.136 | |||||
| Yes | 139 (68.1) | 79 (17.1) | 10.37 (7.08, 15.18) | 6.23 (3.8, 9.92) | 0.005 ** | |
| No | 65 (31.9) | 383 (82.9) | 1 | 1 | ||
| Psychological stress | 0.001 | |||||
| High | 58 (28.4) | 36 (7.8) | 7.52 (4.61, 12.32) | 7.69 (4.16, 14.28) | 0.001 ** | |
| Moderate | 78 (32.8) | 108 (23.4) | 3.38 (2.28, 5.00) | 2.56 (1.35, 4.76) | 0.004 ** | |
| Low | 68 (33.3) | 318 (68.8) | 1 | 1 | ||
| Social support | 0.160 | |||||
| Poor | 92 (45.1) | 190 (41.1) | 1.59 (0.97, 2.59) | 2.30 (1.27, 4.18) | 0.006 ** | |
| Moderate | 84 (41.2) | 180 (39.0) | 1.53 (0.93, 2.52) | 2.38 (1.29, 4.38) | 0.005 ** | |
| Strong | 28 (13.7) | 92 (19.9) | 1 | 1 | ||
NB: COR: crude odds ratio; CI: confidence interval; AOR: adjusted odds ratio; ETB: Ethiopian birr; 1; Reference group; *p value < 0.05; **p value ≤ 0.01.
Discussion
The current COVID-19 pandemic 48 has a number of consequences, one of which is the possible impact on health behavior, including alcohol consumption. Therefore, the goal of this study was to determine the magnitude of AUD identification test and its associated factors. According to the findings, 30.6% (95% CI: 25.5%–35.7%) of residents of Dilla town screened positive for AUDIT in the past year preceding the data collection period. The findings are congruent with a previous Ethiopian study conducted in Ambo town (27%), 22 a study conducted in the United States among middle- and low-income adults revealed 35.3% of respondents screened positive for current AUD during the era of COVID-19 pandemics, 49 during the initial stages of the COVID-19 pandemic, approximately 30% of subjects in Poland consumed at-risk amounts of alcohol, 50 and 28% of conflict-affected males in the Republic of Georgia had at least harmful alcohol use, with an AUDIT score of ⩾8. 51
The finding was lower than that of a study conducted in Jimma, Ethiopia (38.9%), 3 a Nigerian study (48.1%), 42 the United States America 55.6%, 43 and an Indian study, in which 48.5% of alcohol users had an AUDIT score of 8 or higher. This might be explained by the COVID-19 pandemic crises are typically connected with unemployment and reduced working hours, resulting in lower income, which could lead to restricted resources and a drop in alcohol use and attributable disorders. In addition, the result could be attributed to the constraints on social engagements linked with drinking behavior.
Moreover, the magnitude of participants screened positive for AUDIT in this study is higher than studies conducted in Nepal (23.8%), 52 United States (13.9%), 53 Colombia (9%), 54 Brazil (7.9%), 55 Greece (3.1%), 56 Korea (7.5%), India (3.7%), 57 South Africa (3.9%), 58 Nigeria (24.7%), 59 Uganda (9.8%), 60 Kenya (6.7%) 61 Sodo zone, SNNPR (21%), 62 and south Gonder zone (23.7%), 29 Sodo district (13.9%), 24 and Agaro town (12.4%) 23 based on AUDIT cutoff value of ⩾8. This disparity could be attributed to differences in culture, lifestyle, drinking habits, research time, or population. It is also possible that this is related to the existence of undiagnosed and untreated AUD respondents in the study. In addition, one of the causes for the disparity could be the ease of access and accessibility of alcoholic beverages and during COVID-19 pandemics, people may stay at home. As a result, this period of isolation may result in an increase in alcohol dependence.
In this study, the odds of AUDs were higher among males than females. This finding was in line with previous studies conducted in Ethiopia,23,24,29,63 Indian, 57 Brazil, 55 Colombia, 54 United States, 53 and Kenya. 61 This could be because men consume more alcohol than women and cause more alcohol-related harm to themselves and others; societal restrictions on women’s alcohol use could lessen the risk of having positive AUDIT; or it could be because men have higher psychiatric co-morbidity. 54
Positive AUDIT were more common in people under the age of 33 years than in people over the age of 33 years because AUD is one of the leading causes of global disease, disability, and early mortality. 64 This evidence is backed up by a systematic review and meta-analysis study that linked positive AUDIT to a younger age group with a higher risk of mortality. 65 However, the findings differ markedly from those of previous research that have found that alcohol usage is lower among people under the age of 30.37,66,67 As a result, the findings point to the necessity for more comprehensive prevention and intervention initiatives in this age group.
The odds of positive AUDIT were higher among smokers as compared with non-smokers. This finding is consistent with research conducted in Brazil, 55 Nepal, 52 Colombia, 54 India, 57 Nigeria, 59 and other Ethiopian regions.23,63,68 Current khat chewing was found to be linked to positive AUDIT. When compared to non-khat chewers, respondents who chewed khat were six times more likely to have positive AUDIT. This result is consistent with prior Ethiopian research.68,69 The discovery could be explained by the fact that both khat and cigarettes have a similar mode of action with alcohol, in which one can enhance the rewarding impact of the other. 70 Another possibility is that, according to a study conducted in Jimma City, Ethiopia, khat chewing is closely associated to mental distress, 71 which leads to a problem with alcohol consumption. Furthermore, insomnia was linked to khat chewing, 72 and to combat this adverse effect, khat chewers drank excessive amounts of alcohol.
Positive result on AUDIT was shown to be more common among those with a high and moderate level of psychological distress compared to those with a low level of psychological distress. Previous Ethiopian research29,62,63 supports the findings. The result might be that during and after crises like the COVID-19 pandemic, greater psychological distress produced by a combination of financial hardships, social isolation, and uncertainty about the future might aggravate patterns of alcohol consumption and increase attributable harm and could be inferred as handling approaches for the disaster. 73
Furthermore, this study showed the odds of positive AUDIT were higher among participants with poor and moderate social support as compared to participants with high social support. A previous Ethiopian study 62 supports the finding. People who do not have many social connections or who do not have a lot of support from their friends and family are more likely to drink. At the completion of the survey, the community was given health education seminars on the problematic use of alcohol, as well as referral services.
Limitation of the study
One of the main limitation of this study was unable to relate AUDIT with the psychiatric disorders and the study could not cover some segments of the population (i.e, homeless individuals, prisoners, and most treated individuals) which may under or overestimate the prevalence of positive AUDIT. In addition, the AUDIT scores (cut off values) does not equate with the clinical AUD classification. Moreover, as the study being cross-sectional, unable to find causal association between AUDs and associated factors and social desirability bias; respondents who consume alcohol or other substances may under report or deny their use. Further research needed to address the long-term effects of COVID-19 on alcohol use and associated factors.
Conclusion
Significant proportions of residents of Dilla town had AUD. Being male, less than 33 years old, current khat chewing, current cigarette smoking, high and moderate level of psychological distress stress, poor and moderate social support were related with AUDs. Therefore, it is better to provide early detection and public health intervention services, and making AUD treatment available and accessible in the community, and its also recommend establishment of appropriate referral linkage with mental health institutions. Furthermore, the high prevalence of positive AUDIT in the community underscores the necessity for a strict alcohol policy that takes into account health and economic issues while also enforcing the law to prevent the harmful impact of problem drinking.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121221105031 for Alcohol use disorder and its associated factors among residents in Southern Ethiopia during the era of COVID-19 by Habtamu Endashaw Hareru, Abdene Weya Kaso, Berhanu Gidisa Debela, Lulu Abebe, Daniel Sisay W/tsadik, Reta Kassa Abebe and Chalachew Kassaw in SAGE Open Medicine
Acknowledgments
The authors would like to express their gratitude to Dilla University and the College of Health Science and Medicine for their cooperation in completing the study. Furthermore, they thank the graduating class of fourth-year psychiatry students for their support in data collecting, as well as to the participants for their willingness to engage in the study.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from institutional review board (IRB) of the Dilla University with ethics approval number of duirb/057/21-08.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical consideration: Ethical approval for this study was obtained from institutional review board (IRB) of Dilla University with ethics approval number of duirb/057/21-08. To maximize true response and reduce fear of respondent confidentiality disclosure, verbal/informed consent was obtained from each participant during the data collection period, and this method of obtaining consent was approved by the IRB of Dilla University. Participants’ right to refuse the participation will be kept. All study participants who were found to have AUD had a detailed assessment and appropriate intervention offered. Confidentiality of the respondents was maintained.
Informed consent: To maximize true response and reduce fear of respondent confidentiality disclosure, verbal/informed consent was obtained from each participant during the data collection period, and this method of obtaining consent was approved by the IRB of Dilla University.
Availability of the data: The raw data supporting the findings of this paper will be made available without restriction by the authors.
ORCID iDs: Habtamu Endashaw Hareru  https://orcid.org/0000-0002-0591-0893
https://orcid.org/0000-0002-0591-0893
Berhanu Gidisa Debela  https://orcid.org/0000-0002-1750-7356
https://orcid.org/0000-0002-1750-7356
Daniel Sisay W/tsadik  https://orcid.org/0000-0001-5734-3408
https://orcid.org/0000-0001-5734-3408
Supplemental material: Supplemental material for this article is available online.
References
- 1. Specka M, Kuhlmann T, Sawazki J, et al. Prevalence of Novel Psychoactive Substance (NPS) use in patients admitted to drug detoxification treatment. Front Psychiatry 2020; 11: 569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tarter RE, Vanyukov M. Alcoholism: a developmental disorder. In: Marlatt GA, VandenBos GR. (eds) Addictive behaviors: readings on etiology, prevention, and treatment. Washington, DC: American Psychological Association (APA), 1997, pp. 43–67. [Google Scholar]
- 3. Babor TF, Higgins-Biddle JC, Saunders JB, et al. The Alcohol Use Disorders Identification Test. Geneva: World Health Organization (WHO), 2001. [Google Scholar]
- 4. Hodgson R, Alwyn T, John B, et al. The FAST alcohol screening test. Alcohol Alcohol 2002; 37: 61–66. [DOI] [PubMed] [Google Scholar]
- 5. Peacock A, Leung J, Larney S, et al. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction 2018; 113: 1905–1926. [DOI] [PubMed] [Google Scholar]
- 6. World Health Organization (WHO). Alcohol. Geneva: WHO, 2018. [Google Scholar]
- 7. Federal Ministry of Health (FMoH). Covid-19 daily situational analysis. Addis Ababa: FMoH, 2021. [Google Scholar]
- 8. Kassaw C, Pandey D. The current mental health crisis of COVID-19 pandemic among communities living in Gedeo Zone Dilla, SNNP, Ethiopia, April 2020. J Psychosoc Rehabil Ment Health 2021; 8: 5–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gonçalves PD, Moura HF, Do Amaral RA, et al. Alcohol use and COVID-19: can we predict the impact of the pandemic on alcohol use based on the previous crises in the 21st century? A brief review. Front Psychiatry 2020; 11: 581113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wardell JD, Kempe T, Rapinda KK, et al. Drinking to cope during COVID-19 pandemic: the role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcohol Clin Exp Res 2020; 44: 2073–2083. [DOI] [PubMed] [Google Scholar]
- 11. Westman J, Wahlbeck K, Laursen TM, et al. Mortality and life expectancy of people with alcohol use disorder in Denmark, Finland and Sweden. Acta Psychiatr Scand 2015; 131: 297–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Testino G. Are patients with alcohol use disorders at increased risk for Covid-19 infection? Alcohol Alcohol 2020; 55: 344–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Egbe CO, Londani M, Parry CD, et al. Tobacco use and nicotine dependence among people living with HIV who drink heavily in South Africa: a cross-sectional baseline study. BMC Public Health 2019; 19: 1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization (WHO). Global status report on alcohol and health 2018. Geneva: WHO, 2019. [Google Scholar]
- 15. Hamer M, Kivimäki M, Gale CR, et al. Lifestyle risk factors for cardiovascular disease in relation to COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK. medRxiv. Epub ahead of print 13 May 2020. DOI: 10.1101/2020.05.09.20096438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Newby J, O’Moore K, Tang S, et al. Acute mental health responses during the COVID-19 pandemic in Australia. medRxiv. Epub ahead of print 8 May 2020. DOI: 10.1101/2020.05.03.20089961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stanton R, To QG, Khalesi S, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health 2020; 17: 4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ahmed MZ, Ahmed O, Aibao Z, et al. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatr 2020; 51: 102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lee SA. How much “Thinking” about COVID-19 is clinically dysfunctional? Brain Behav Immun 2020; 87: 97–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Overstreet C, Berenz EC, Kendler KS, et al. Predictors and mental health outcomes of potentially traumatic event exposure. Psychiatry Res 2017; 247: 296–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dessie BK. Poly substance use behavior among male population in Ethiopia: finding from the 2016 EDHS. In: Proceedings of the 31st EPHA annual conference, Addis Ababa, 15–17 March 2020. [Google Scholar]
- 22. Birhanu A, Mekuria M. Prevalence of alcohol use disorders and associated factors among Ambo Town Community, Central Ethiopia: a community based cross-sectional study. J Addict Res Ther 2019; 10: 389. [Google Scholar]
- 23. Bedaso A, Gobena M, Yigzaw N, et al. Determinants of alcohol use disorder among residents of Agaro town, Jimma, southwest, Ethiopia: a cross-sectional study. J Addict Res Ther 2019; 10: 377. [Google Scholar]
- 24. Zewdu S, Hanlon C, Fekadu A, et al. Treatment gap, help-seeking, stigma and magnitude of alcohol use disorder in rural Ethiopia. Subst Abuse Treat Pr 2019; 14: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mekonen T, Fekadu W, Chane T, et al. Problematic alcohol use among university students. Front Psychiatry 2017; 8: 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pirnia B, Dezhakam H, Pirnia K, et al. COVID-19 pandemic and addiction: current problems in Iran. Asian J Psychiatr 2020; 54: 102313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. World Health Organization (WHO). Global status report on alcohol and health 2014. Geneva: WHO, 2014. [Google Scholar]
- 28. Beyene N. Alcohol control policy in Ethiopia and implications for public health. J Public Health Policy 2019; 40: 423–435. [DOI] [PubMed] [Google Scholar]
- 29. Legas G, Asnakew S, Belete A, et al. Magnitude and correlates of alcohol use disorder in south Gondar zone, northwest Ethiopia: a community based cross-sectional study. PLoS One 2021; 16: e0257804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yitayih Y, Soboka M, Tesfaye E, et al. Trauma exposure and alcohol use disorder among prisoners in Jimma Zone correctional institution, Southwest Ethiopia: a cross-sectional study. BMC Res Notes 2019; 12: 748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sanchez-Ramirez DC, Franklin R, Voaklander D. Hazardous alcohol use in 2 countries: a comparison between Alberta, Canada and Queensland, Australia. J Prev Med Public Health 2017; 50: 311–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction 1993; 88: 791–804. [DOI] [PubMed] [Google Scholar]
- 33. World Health Organization (WHO). The alcohol use disorders identification test: guidelines for use in primary care. Geneva: WHO, 2001. [Google Scholar]
- 34. Morojele NK, Nkosi S, Kekwaletswe CT, et al. Utility of brief versions of the alcohol use disorders identification test (AUDIT) to identify excessive drinking among patients in HIV care in South Africa. J Stud Alcohol Drugs 2017; 78: 88–96. [DOI] [PubMed] [Google Scholar]
- 35. Blair AH, Pearce ME, Katamba A, et al. The alcohol use disorders identification test (AUDIT): exploring the factor structure and cutoff thresholds in a representative post-conflict population in northern Uganda. Alcohol Alcohol 2017; 52: 318–327. [DOI] [PubMed] [Google Scholar]
- 36. Pal HR, Jena R, Yadav D. Validation of the Alcohol Use Disorders Identification Test (AUDIT) in urban community outreach and de-addiction center samples in north India. J Stud Alcohol 2004; 65: 794–800. [DOI] [PubMed] [Google Scholar]
- 37. Nalwadda O, Rathod SD, Nakku J, et al. Alcohol use in a rural district in Uganda: findings from community-based and facility-based cross-sectional studies. Int J Ment Health Syst 2018; 12: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Habtamu E, Madoro D. Psychometric properties of Alcohol Use Disorder Identification Test screening tool among medical outpatients in Dilla University Referral Hospital, southern Ethiopia, 2020. SAGE Open Med. Epub ahead of print 15 February 2022. DOI: 10.1177/20503121221077568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Qamar K, Kiani MRB, Ayyub A, et al. Higher stress scores for female medical students measured by the Kessler Psychological Distress Scale (K10) in Pakistan. J Educ Eval Health Prof 2014; 11: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tesfaye M, Hanlon C, Wondimagegn D, et al. Detecting postnatal common mental disorders in Addis Ababa, Ethiopia: validation of the Edinburgh postnatal depression scale and Kessler scales. J Affect Disord 2010; 122: 102–108. [DOI] [PubMed] [Google Scholar]
- 41. Kocalevent R-D, Berg L, Beutel ME, et al. Social support in the general population: standardization of the Oslo social support scale (OSSS-3). BMC Psychol 2018; 6: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bøen H, Dalgard OS, Bjertness E. The importance of social support in the associations between psychological distress and somatic health problems and socio-economic factors among older adults living at home: a cross sectional study. BMC Geriatr 2012; 12: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Shumye S, Belayneh Z, Mengistu N. Health related quality of life and its correlates among people with depression attending outpatient department in Ethiopia: a cross sectional study. Health Qual Life Outcomes 2019; 17: 169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Humeniuk R, Henry-Edwards S, Ali R, et al.; World Health Organization. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): manual for use in primary care, 2010, https://www.who.int/publications/i/item/978924159938-2
- 45. Muhamad NA, Mihat O, Ramly R, et al. Translation, cross-cultural adaptation, reliability and validity of the Malay version of alcohol, smoking and substance involvement screening test (ASSIST) V3. 1. Health 2018; 10: 985–997. [Google Scholar]
- 46. WHO ASSIST Working Group. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction 2002; 97: 1183–1194. [DOI] [PubMed] [Google Scholar]
- 47. Haile D, Lakew Y. Khat chewing practice and associated factors among adults in Ethiopia: further analysis using the 2011 demographic and health survey. PLoS One 2015; 10: e0130460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. World Health Organization (WHO). World Health Organization Coronavirus Disease (COVID-19) Pandemic, https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 49. Tsai J, Elbogen EB, Huang M, et al. Psychological distress and alcohol use disorder during the COVID-19 era among middle- and low-income US adults. J Affect Disord 2021; 288: 41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chodkiewicz J, Talarowska M, Miniszewska J, et al. Alcohol consumption reported during the COVID-19 pandemic: the initial stage. Int J Environ Res Public Health 2020; 17: 4677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Roberts B, Murphy A, Chikovani I, et al. Individual and community level risk-factors for alcohol use disorder among conflict-affected persons in Georgia. PLoS One 2014; 9: e98299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Rathod SD, Luitel NP, Jordans MJD. Prevalence and correlates of alcohol use in a central Nepal district: secondary analysis of a population-based cross-sectional study. Glob Ment Health 2018; 5: e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry 2015; 72: 757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Rincon-Hoyos HG, Castillo A, Prada SI. Alcohol use disorders and psychiatric diseases in Colombia. Colomb Méd 2016; 47: 31–37. [PMC free article] [PubMed] [Google Scholar]
- 55. Mendoza-Sassi RA, Béria JU. Prevalence of alcohol use disorders and associated factors: a population-based study using AUDIT in Southern Brazil. Addiction 2003; 98: 799–804. [DOI] [PubMed] [Google Scholar]
- 56. Bellos S, Petrikis P, Malliori M, et al. Prevalence of alcohol use disorders and their association with sociodemographic determinants and depression/anxiety disorders in a representative sample of the Greek general population. Psychiatry J 2020; 2020: 4841050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ganesh Kumar S, Premarajan KC, Subitha L, et al. Prevalence and pattern of alcohol consumption using alcohol use disorders identification test (AUDIT) in rural Tamil Nadu, India. J Clin Diagn Res 2013; 7: 1637–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Peltzer K, Davids A, Njuho P. Alcohol use and problem drinking in South Africa: findings from a national population-based survey. Afr J Psychiatry 2011; 14: 30–37. [DOI] [PubMed] [Google Scholar]
- 59. Ani PN, Ngwu EK, Ani BU. Alcohol use disorders and associated factors among adults in rural communities in Enugu State, Nigeria: a cross-sectional survey. J Ethn Subst Abuse. Epub ahead of print 5 October 2020. DOI: 10.1080/15332640.2020.1824841. [DOI] [PubMed] [Google Scholar]
- 60. Kabwama SN, Ndyanabangi S, Mutungi G, et al. Alcohol use among adults in Uganda: findings from the countrywide non-communicable diseases risk factor cross-sectional survey. Glob Health Action 2016; 9: 31302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Pengpid S, Peltzer K. Alcohol use among adults in Kenya: results from the national non-communicable diseases risk factor survey, 2015. J Psychol Afr 2019; 29: 49–53. [Google Scholar]
- 62. Teferra S, Medhin G, Selamu M, et al. Hazardous alcohol use and associated factors in a rural Ethiopian district: a cross-sectional community survey. BMC Public Health 2016; 16: 218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Zenebe Y, Negash A, Feyissa G, et al. Alcohol use disorders and its associated factors among psychiatric outpatients in Jimma University Specialized Hospital, Southwest Ethiopia. J Alcohol Drug Depend 2015; 3: 3. [Google Scholar]
- 64. Rehm J, Mathers C, Popova S, et al. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 2009; 373: 2223–2233. [DOI] [PubMed] [Google Scholar]
- 65. Roerecke M, Rehm J. Alcohol use disorders and mortality: a systematic review and meta-analysis. Addiction 2013; 108: 1562–1578. [DOI] [PubMed] [Google Scholar]
- 66. Naamara W, Muhwezi WW. Factors associated with alcohol dependence among adult male clients in butabika hospital, Uganda. J Soc Work Pract Addict 2014; 14: 322–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Kullgren G, Alibusa S, Birabwa-Oketcho H. Problem drinking among patients attending primary healthcare units in Kampala, Uganda. Afr J Psychiatry 2009; 12: 52–58. [DOI] [PubMed] [Google Scholar]
- 68. Bultum JA, Yigzaw N, Demeke W, et al. Alcohol use disorder and associated factors among human immunodeficiency virus infected patients attending antiretroviral therapy clinic at Bishoftu General Hospital, Oromiya region, Ethiopia. PLoS One 2018; 13: e0189312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Soboka M, Tesfaye M, Feyissa GT, et al. Alcohol use disorders and associated factors among people living with HIV who are attending services in south west Ethiopia. BMC Res Notes 2014; 7: 828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Adams S. Psychopharmacology of tobacco and alcohol comorbidity: a review of current evidence. Curr Addict Rep 2017; 4: 25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Damena T, Mossie A, Tesfaye M. Khat chewing and mental distress: a community based study, in Jimma city, southwestern Ethiopia. Ethiop J Health Sci 2011; 21: 37–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Malaju MT, Asale GA. Association of Khat and alcohol use with HIV infection and age at first sexual initiation among youths visiting HIV testing and counseling centers in Gamo-Gofa Zone, South West Ethiopia. BMC Int Health Hum Rights 2013; 13: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Keyes KM, Hatzenbuehler ML, Hasin DS. Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors. Psychopharmacology 2011; 218: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121221105031 for Alcohol use disorder and its associated factors among residents in Southern Ethiopia during the era of COVID-19 by Habtamu Endashaw Hareru, Abdene Weya Kaso, Berhanu Gidisa Debela, Lulu Abebe, Daniel Sisay W/tsadik, Reta Kassa Abebe and Chalachew Kassaw in SAGE Open Medicine


