Abstract
In the context of accelerated aging of the population worldwide, frailty has emerged as one of the main risk factors that can lead to loss of self-sufficiency in older people. This syndrome is defined as a reduced state of physiological reserve and functional capacity. The main diagnostic tools for frailty are based on scales that show deficits compared to their clinical application, such as the Fried frailty phenotype, among others. In this context, it is important to have one or more biomarkers with clinical applicability that can objectively and precisely determine the degree or risk of frailty in older people. The objective of this review was to analyze the biomarkers associated with frailty, classified according to the pathophysiological components of this syndrome (inflammation, coagulation, antioxidants, and liver function, among others). The evidence demonstrates that biomarkers associated with inflammation, oxidative stress, skeletal/cardiac muscle function, and platelet function represent the most promising markers of frailty due to their pathophysiological association with this syndrome. To a lesser extent but with the possibility of greater innovation, biomarkers associated with growth factors, vitamins, amino acids, and miRNAs represent alternatives as markers of this geriatric syndrome. Likewise, the incorporation of artificial intelligence represents an interesting approach to strengthening the diagnosis of frailty by biomarkers.
Keywords: frailty, aging, biomarkers, older people, diagnosis
1. Introduction
The world’s population is aging rapidly [1]. Twelve percent of the world’s population is 60 years old or older, and by mid-century, this population could reach 21.5% [2]. During this same period, the population aged ≥ 80 years would increase from 1.7% to 4.5% [2]. According to the World Health Organization (WHO), healthy aging is a process of development and maintenance of functional capacity that allows well-being in old age [3]. Concerning this, frailty emerges as one of the main risk factors that can lead older people to lose self-sufficiency, diminishing their quality of life and health [4]. Frailty is defined as a clinically recognizable state in which older people’s ability to cope with everyday stressors is compromised by an increased vulnerability, which is caused by reduced physiological reserve and decline in multiple physiological systems, all of the above associated with age [5]. The importance of frailty lies in the fact that frail older people have a higher risk of premature death, in addition to numerous adverse health outcomes, such as falls, fractures, dementia, disability, impaired quality of life, and excessive use of state health resources [6,7,8,9,10,11,12,13,14]. In this sense, the WHO developed the ICOPE guide (Integrated Care for Older People) with the aim of promoting, improving, or maintaining both the intrinsic and functional capacity of older persons to achieve healthy aging, being a key point in the prevention of frailty and a correct diagnosis through tools and/or biomarkers [15,16,17].
There are currently several scales to determine frailty in older people, within which the Fried frailty phenotype is positioned as a standard of physical frailty [18]. Other commonly used tools are the Rockwood Frailty Index, the Edmonton Frail Scale (EFS), and the Clinical Frailty Scale, which consists of simple questions and measurements for older people, such as weight, height, and walking speed, but the questions seem to impose greater complications since they are a more subjective measurement that will depend on the respondent’s self-appreciation and also, to a certain extent, influence how they feel emotionally at the time of the evaluation [19,20,21,22]. Likewise, there are various phenotypic determinants of the multidimensional construct of frailty (e.g., hepatic frailty, oral frailty, nutritional frailty, among others), that complicate its correct diagnosis [23,24,25]. In this context, different investigations indicate that the development of one or several biomarkers to detect frailty may be a more objective and precise way of evaluating both the initial state of the person and the progression of frailty over time, supporting the diagnosis, prognosis, and therapeutic decisions [26,27].
To date, different potential biomarkers of frailty have been reported, associated with the pathophysiological components of frailty, highlighting markers associated with increased inflammation, sarcopenia, nutritional deficit, and different hematological and biochemical parameters [28,29]. Based on the above, the main objective of this work was to describe the main biomarkers associated with frailty and to evaluate their possible usefulness for the early diagnosis of frailty in older people.
2. Methodology
We analyzed all original articles available in the mainly scientific databases (PubMed/Medline, Scopus, Web of Science, and SciELO), published until May 2022, with no date limitations and fulfilling the following inclusion criteria: (1) full text in English or Spanish; (2) original or review articles; (3) measurement of blood biomarkers; (4) frail patients (5) aging or older patients. When determining which articles to include, we analyzed the title and abstract and the full text of articles that fulfilled the inclusion criteria. The search terms employed were “frailty”, “biomarker” and “aging” or “older people”. Each article was evaluated by an independent reviewer, and any discrepancy was resolved by a second reviewer.
3. Diagnosis of Frailty: Main Diagnostic Tools and Their Deficiencies
Among all of the definitions of frailty, the frailty phenotype of Fried is the most used [30]. The Fried frailty phenotype evaluates five components to define frailty, which are: involuntary weight loss, weakness, reduction in walking speed, low physical activity, and fatigue [18]. This phenotype has recently been defined as the standard only for physical frailty, not considering intrinsic characteristics of frailty and being little applicable in the geriatric clinical area [31]. This is because this phenotype leaves out different areas affected by frailty, such as the nervous system and cognitive status, among others, in addition to not including psychosocial components [31,32]. On the other hand, the Frailty Index or Clinical Frailty Scale is based on a model of cumulative deficit that is defended by Mitnitski and Rockwood using the Canadian Study of Health and Aging [19]. Unlike the Fried frailty phenotype, this cumulative deficit approach describes frailty as a state that is caused by poor health throughout life, and the more deficits people have in their health, the more likely they are to develop frailty [30]. Despite its potential for clinical use, this tool presents a long list of deficit assessments, which is not very workable in geriatric practice, and its implementation in the health care area is not practical since it combines several domains [33,34]. The physical frailty phenotype and multidomain frailty index differ in that the physical frailty phenotype considers disability and comorbidities as a result of frailty, whereas in the multidimensional frailty model, these may be components of the model [35].
On the other hand, there is also the Edmonton Frail Scale (EFS), which was developed at the University of Alberta in the Canadian city of Edmonton by Rolfson and collaborators [20]. The EFS is a multidimensional frailty assessment tool designed to assist in the assessment and detection of frail older patients in primary health care [36]. This consists of 11 questions in 9 different domains, which are cognition, functional performance, general health status, functional independence, social support, pharmacological condition, nutritional aspect, mental condition, and continence [37,38]. Like the two previous tools, the EFS has deficiencies due to the subjectivity in some of its items and its limited usefulness in clinical implementation [14].
The presented evidence indicates that these scales, commonly used in research, are difficult to implement in clinical practice, for which it is necessary to have one or a set of biomarkers that can help predict the risk of frailty in time so that appropriate prevention or intervention measures can be implemented to reduce the risk or degree of frailty [39].
4. Blood Biomarkers Associated with Frailty
Age-associated changes in multiple physiological systems play a key role in the development of frailty, especially the neuromuscular, neuroendocrine, and immune systems, leading to compromise the physiological homeostasis [40,41]. The frailty phenotype includes sarcopenia, anorexia, osteoporosis, fatigue, risk of falling, poor physical health, and cognitive impairment, among other negative characteristics [40,41]. Just as frailty can be determined through different scales, the discovery of potential biomarkers of frailty is also important, which is evidenced in the multiple studies that analyzed inflammatory, hematological, and metabolic biomarkers, among others [42].
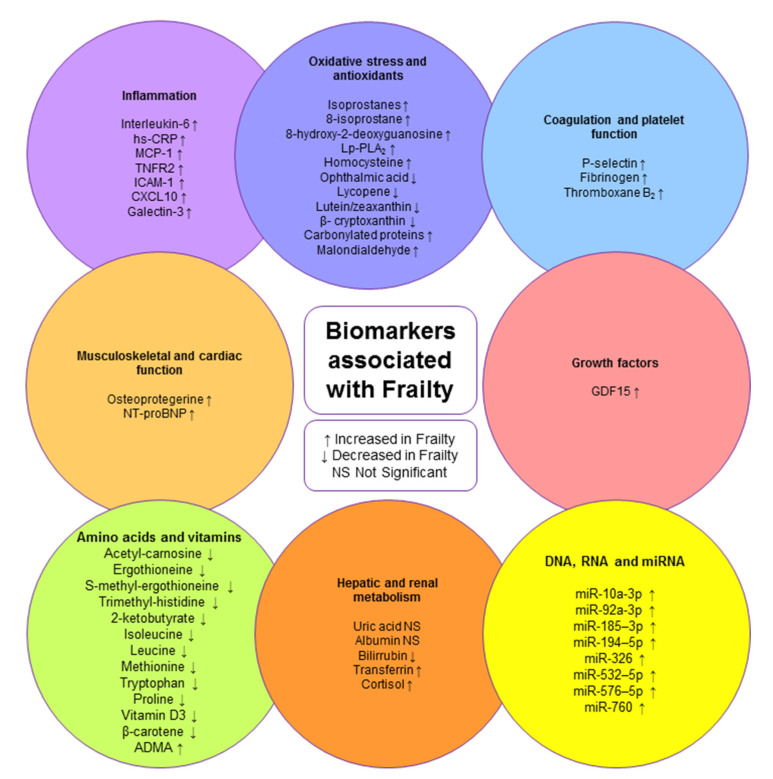
Next, the biomarkers associated with frailty and inflammation, antioxidants and oxidative stress, coagulation and platelet function, growth factors, skeletal and cardiac muscle function, amino acids and vitamins, hepatic and renal metabolism, and miRNA will be described (Figure 1).
Figure 1.
Biomarkers associated with frailty.
4.1. Biomarkers Associated with Inflammation
Aging has been associated with changes in the immune system and inflammation level, where in the latter an increase in blood or serum concentrations of acute-phase proteins can be observed, such as C-reactive protein and pro-inflammatory cytokines [43,44,45,46]. Among the inflammation markers, it is possible to mention the pro-inflammatory cytokine interleukin-6 (IL-6), which contributes to host defense through stimulation of the acute-phase response, hematopoiesis, and immune reactions [47,48]. In a study evaluating the relationship between frailty and biomarkers of inflammation in older people undergoing surgical procedures (n = 137), high levels of IL-6 were found in frail patients; previous studies also established a relationship between slower walking speed and higher levels of IL-6, as well as reduced physical function [49,50]. In clinical practice, the high-sensitivity C-reactive protein (hs-CRP) biomarker is very useful for detecting vascular inflammation, and also low-grade inflammation [51,52]. A study of 1478 elderly people (70 to 84 years old) with the objective of evaluating the relationship between frailty and the biomarker of inflammation hs-CRP indicated that higher levels of hs-CRP were observed in frail older people (4.2 mg/L) [28]. The significant association of hs-CRP with frailty observed in this study is consistent with evidence of sustained systemic inflammation in frail patients [28,53,54,55].
In a study carried out in participants aged ≥60 years and classified into three groups, frail, n = 142; pre-frail, n = 864; and non-frail, n = 913, the relationship between frailty and inflammation was evaluated, determining the levels of three biomarkers: monocyte chemoattractant protein-1 (MCP-1), tumor necrosis factor receptor 2 (TNFR2), and intercellular adhesion molecule 1 (ICAM-1). The median results obtained for the MCP-1 biomarker were 415 pg/mL (frail), 384 pg/mL (pre-frail), and 364 pg/mL (non-frail), underlining an increase in the levels of MCP-1 in the frail group [50]. MCP-1 is known to be an important chemokine for macrophage recruitment and is produced by a variety of cell types, either constitutively or after induction by oxidative stress, cytokines, or growth factors [56,57]. In the same study, the results for TNFR2 (median) were 3151 pg/mL for frail individuals, 2669 pg/mL for pre-frail individuals, and 2385 pg/mL for non-frail individuals [50]. Tumor necrosis factor α (TNF-α) is a cytokine that participates in systemic inflammation, having two receptors, TNFR1 and TNFR2, and by binding to these, it can activate pro-apoptotic or anti-apoptotic signaling [58,59]. TNFR2 is a surface receptor that regulates cell survival and proliferation [60]. ICAM-1, a 90-kDa member of the immunoglobulin superfamily, was also analyzed in this group. It is essential for the firm arrest and transmigration of leukocytes out of blood vessels and into fabrics, is present in atherosclerotic lesions, and is involved in their progression [61]. The results (median) were 307 ng/mL for the frail, 293 ng/mL for the pre-frail, and 270 ng/mL for the non-frail; it was possible to observe that the frail elderly had higher values compared to the group of non-frail older people [50].
Other chemokines that are abundantly secreted by immune and non-immune cells in response to an inflammatory stimulus are IFN-γ-inducible protein 10 (CXCL-10), TNF-α, and interleukin 1 beta (IL-1β) [62,63]; these are involved in the pathogenesis of various inflammatory diseases and are also potent chemoattractants for Th1 lymphocytes and natural killer (NK) cells [64,65]. In a study conducted in a group of 32 participants (frail group, n = 16; non-frail group, n = 16) to assess the relationship between frailty and inflammation, the CXCL-10 biomarker was found to be increased in frailty, which suggests the possibility that the activation of inflammation in frailty is probably mediated by Th1 lymphocytes [66].
It is also possible to mention another marker of inflammation, galectin-3, a β-galactoside binding lectin widely expressed in immune, epithelial, and endothelial cells and sensory neurons that plays an important role in the exacerbation of autoimmune/inflammatory diseases, malignant cardiac fibrosis, and the progression of heart failure [67,68,69,70]. In a study carried out in a group of 54 frail and 74 non-frail persons, the relationship between frailty and inflammation was evaluated, and it was observed that galectin-3 was increased in the frail group, for which the authors suggested that galectin-3 upregulation was associated with the development of heart failure and could interfere with mechanisms of premature senescence, accelerated aging and development of frailty [71].
The descriptions of all of the above-mentioned biomarkers are presented in Table 1.
Table 1.
Biomarkers associated with inflammation.
| BIOMARKER | SAMPLE | CUT VALUES (FRAIL—NOT FRAIL) | FRAILTY SCALE | COUNTRY | YEAR | GROUP DESCRIPTION |
REFERENCE |
|---|---|---|---|---|---|---|---|
| Interleukin-6 (pg/L) | Serum | Median 11.08 interquartile range: 5.04–13.63 (Frail) Median 4.11 interquartile range: 2.83–5.84 (Not Frail) |
Fried | Norway | 2010 | Transversal study Group of 137 patients, median age 80 years |
Rønning, B. et al., 2010 [49] |
| Hs-CRP (mg/L) | Serum | 4.2 (Frail) 3.1 (Not Frail) |
Fried | China | 2016 | Transversal study Group of 1478 participants, 70–84 years old |
Zhu, Y. et al. (2016) [28] |
| MCP-1 (pg/mL) | Plasma | Median and interquartile range: 415 (345–501) (Frail) 384 (324–462) (Pre-frail) 364 (301–441) (Not Frail) |
Fried | United States | 2016 | Group of people over 60 years of age, divided into 3 groups: n = 142 frail, n = 864 pre-frail, n = 913 not frail | Liu, C.K. et al. (2016) [50] |
| TNFR2 (pg/mL) | Plasma | Median and interquartile range: 3151 (2506–4447) (Frail) 2669 (2149–3443) (Pre-frail) 2385 (1963–2877) (Not Frail) |
Fried | United States | 2016 | Group of people over 60 years of age, divided into 3 groups: n = 142 frail, n = 864 pre-frail, n = 913 not frail | Liu, C.K. et al. (2016) [50] |
| ICAM-1 (ng/mL) | Plasma | Median and interquartile range: 307 (250–381) (Frail) 293 (244–359) (Pre-frail) 270 (233–334) (Not Frail) |
Fried | United States | 2016 | Group of people over 60 years of age, divided into 3 groups: n = 142 frail, n = 864 pre-frail, n = 913 not frail | Liu, C.K. et al. (2016) [50] |
| CXCL10 | Whole blood | Increased in frailty | Fried | United States | 2009 | Group of 32 people, 16 frail and 16 not frail, average age of 83 years, 87.5% women | Qu et al. (2009) [66] |
| Galectin-3 (ng/mL) | Serum | 34.4 ± 19.3 (Frail). 14.3 ± 7.6 (Not Frail). Increased in frailty |
Clinical Frailty Scale (CFS) | Italy | 2020 | Group of 54 frail persons and 74 not frail persons, age frail 70.5 ± 5.4 years, age not frail 68.2 ± 4.2 years | Komici et al. (2020) [71] |
4.2. Biomarkers Associated with Oxidative Stress and Antioxidants
Free radicals are highly reactive atoms or molecules that have one or more unpaired electrons in their outer shell, while the terms reactive oxygen species (ROS) and nitrogen species (RNS) refer to radicals derived from oxygen and nitrogen [72,73].
Isoprostanes, osteoprotegerin, and lipoprotein-associated phospholipase A2 (Lp-PLA2), a well-described biomarker of increased oxidative stress, were evaluated in the Framingham Offspring Study (≥60 years, three groups classified by Fried frailty phenotype: frail, n = 142; pre-frail, n = 864; non-frail, n = 913), and the results show that increased levels of isoprostanes and Lp-PLA2 were associated with higher odds of frailty, while high levels of osteoprotegerin were associated with slower walking speed [50].
Isoprostanes are prostaglandin-like compounds formed in vivo by free radical-initiated non-enzymatic peroxidation of arachidonic acid [74]. For the Framingham study, the median results obtained were 11.5 mg/L for the frail, 10.2 mg/L for the pre-frail, and 9.5 mg/L for the non-frail, with higher values found in the frail elderly [50]. 8-Isoprostane is a marker of the eicosanoid family, produced non-enzymatically by successive oxidations in membrane phospholipids [75]. In a study that included 58 participants ≥65 years (n = 29 frail, n = 29 non-frail), high plasmatic levels of 8-isoprostane were observed in the frail group (frail group: 69.5 pg/mL, interquartile range: 64.0–96.7 pg/mL) (control group: 51.3 pg/mL, interquartile range: 38.2–72.2 pg/mL); however, it extensive studies are still necessary to help establish a better relationship between these [76].
On the other hand, it is also important to mention that 8-hydroxy-2-deoxyguanosine (8-OHdG), which is generated after the repair of DNA damage mediated by reactive oxygen species, is one of the biomarkers of the most widely recognized oxidative DNA damage [77]. A study conducted in Japan, which included a group of 140 outpatients with probable Alzheimer’s disease, showed evidence of significant differences in 8-OHdG between frailty states: frail, 5.39 ± 2.23; pre-frail, 5.44 ± 2.70; and non-frail, 3.90 ± 1.67 [78]. In addition, the authors pointed out that both 8-OHdG and 8-isoprostane levels were indicative of oxidative damage of DNA and lipids associated with the progression of frailty in patients with Alzheimer’s disease [78].
Lp-PLA2 is a member enzyme of the 50 kDa phospholipase A₂ family that hydrolyzes oxidized phospholipids and is mainly associated with low-density lipoprotein (LDL), participating in oxidative modification of the vascular wall that can promote vascular inflammation and development of atherosclerotic plaque [79,80,81]. In the Framingham study described above, the median results obtained for Lp-PLA2 were 210 ng/mL (Frail),199 ng/mL (Pre-frail), and 199 ng/mL (Non-frail), with higher values in frail older people, which was also associated with a slower walking speed [50]. This relationship could be explained by previous studies, where murine models have shown that changes in Lp-PLA2 levels affect muscle contractility and resistance [82].
In a study carried out in a group of 1211 elderly people from the Toledo Study of Healthy Aging, the authors evaluated the relationship between frailty and oxidative stress, and in the group of frail people, they found a positive correlation between homocysteine levels, frailty, and the components of the fatigue score [83]. These findings are consistent with another study suggesting that inflammation could be the key mechanism in the pathophysiology of frailty [84]. Regarding homocysteine, high levels of this biomarker are related to inflammation and vitamin B deficiency, oxidative stress, mitochondrial dysfunction, and altered DNA methylation [85]. The above factors are also associated with cardiovascular diseases, disability, and a high risk of death [83].
In a study conducted to evaluate the relationship between frailty and oxidative stress in a group of 19 participants, of which 9 were diagnosed as frail and 10 as non-frail according to the Edmonton Frail Scale (EFS), a significant decrease in the plasmatic ophthalmic acid level was observed in the group of frail older people [86]. An important point about this biomarker is that it is one of the most abundant antioxidants in cells [87]. Ophthalmic acid (l-γ-glutamyl-l-α-amino butyryl glycine) is an analog of glutathione in which cysteine is replaced by l-α-aminobutyrate; since it is released from the liver into the bloodstream, its increase in blood has been proposed as an indicator of hepatic glutathione depletion [88].
The redox balance is altered in frail elderly people, showing that natural antioxidants that can be incorporated into the diet, such as lycopene, lutein/zeaxanthin, and β-cryptoxanthin, can be affected. This fact was observed in the FRALOMIC study, which was composed of 1450 people over 65 years of age [39]. Lycopene is a phytochemical found mainly in tomatoes and has been associated with anticancer, antidiabetic, antioxidant, cardioprotective, anti-inflammatory, hepatoprotective, neuroprotective, and other biological effects [89,90]. Lutein/zeaxanthin are two fat-soluble antioxidants that are the main components of macular pigment, a compound concentrated in the macular region of the retina that is responsible for the vision of fine features [91]. β-cryptoxanthin, a carotenoid commonly found in fruits, blood, and tissues, is an antioxidant and protects organs and tissues from oxidative damage; however, its main function is as a precursor of vitamin A [92,93]. The levels of lycopene (non-frail: 0.40 µmol/L, pre-frail: 0.36 µmol/L, frail: 0.29 µmol/L), lutein/zeaxanthin (non-frail: 0.36 µmol/L, pre-frail: 0.33 µmol/L, frail: 0.27 µmol/L) and β-cryptoxanthin (non-frail: 0.22 µmol/L, pre-frail: 0.21 µmol/L, frail: 0.16 µmol/L) were found to be significant decreased in the frail group, where the β-cryptoxanthin level was the lowest [29]. In this sense, the damage caused by oxidative stress represents a possible trigger for the genesis of the frailty syndrome, which can also be supported by the low levels of lycopene, lutein/zeaxanthin, and β-cryptoxanthin in plasm of frail patients. Continuing with the study of the FRAILOMIC group, the association between frailty and the marker carbonylated proteins in older people was studied [94]. This biomarker represents an irreversible form of protein modification, is relatively stable, and is called a biomarker of protein oxidation [95]. High levels of carbonylated proteins were observed in the frail group, compared to the pre-frail and non-frail groups (non-frail group: 0.26 nmol/mg, pre-frail group: 0.30 nmol/mg, frail group: 0.31 nmol/mg) [29]. With the data obtained, the researchers concluded that low concentrations of antioxidants and high concentrations of carbonylated proteins were associated with pre-frail and frail people over 65 years of age, thus suggesting that a diet high in these antioxidants could support frailty prevention [29].
Lipids are very sensitive to attack by oxidants, and to date, malondialdehyde (MDA), 4-hydroxy-2-nonenal, and F2-isoprostane have been the main biomarkers used for the evaluation of lipid peroxidation [96]. In the Toledo Study for Healthy Aging, in which 742 people were evaluated to assess the relationship between frailty and oxidative stress markers, increased levels of MDA were found in the frail group [97]. MDA is a final product of lipid peroxidation and is considered a biological marker of oxidative stress [98,99]. Therefore, according to a previous study, MDA is the marker that best shows the evolution of damage caused by lipid peroxidation, showing an exponential increase with age, which is associated with high systemic oxidative stress [100].
Based on the above, oxidative stress could contribute to a decline in muscle mass and function with the aging process, leading to weakness and slowness [101]. The descriptions of all of the above-mentioned biomarkers are presented in Table 2.
Table 2.
Biomarkers associated with oxidative stress and antioxidants.
| BIOMARKER | SAMPLE | CUT VALUES (FRAIL–NOT FRAIL) | FRAILTY SCALE | COUNTRY | YEAR | GROUP DESCRIPTION |
REFERENCE |
|---|---|---|---|---|---|---|---|
| Isoprostanes (mg/L) | Urine | Median and interquartile range: 11.5 (8.50–15.40) (Frail) 10.2 (7.60–14.30) (Pre-frail) 9.5 (7.1–12.8) (Not Frail) |
Fried | United States | 2016 | Group of people over 60 years of age, divided into 3 groups: n = 142 frail, n = 864 pre-frail, n = 913 not frail | Liu, C.K. et al. (2016) [50] |
| 8-isoprostane (pg/mL) | Plasma | Interquartile range: 64.0–96.7 (Frail) 38.2–72.2 (Not Frail) |
Fried | Chile | 2019 | Group of people over 65 years of age, divided into 2 groups: n = 29 frail, n = 29 not frail. | Arauna, D. et al. (2019) [76] |
| 8-hydroxy-2-deoxyguanosine (ng/mg Creatinine) | Urine | 5.39 ± 2.23 (Frail) 5.44 ± 2.70 (Pre-frail) 3.90 ± 1.67 (Not Frail) |
Fried | Japan | 2017 | Group of 140 outpatients with probable Alzheimer’s disease, 65 years and older | Namioka, N. et al. (2017) [78] |
| Lp-PLA2 mass (ng/mL) | Plasma | Median and interquartile range: 210 (183–237) (Frail) 199 (172–229) (Pre-frail) 199 (168–228) (Not Frail) |
Fried | United States | 2016 | Group of people over 60 years of age, divided into 3 groups: n = 142 frail, n = 864 pre-frail, n = 913 not frail | Liu, C.K. et al. (2016) [50] |
| Lp-PLA2 activity (nm/mL/min) | Plasma | Median and interquartile range: 139 (119–166) (Frail) 137 (115–160) (Pre-frail) 136 (114–159) (Not Frail) |
Fried | United States | 2016 | Group of people over 60 years of age, divided into 3 groups: n = 142 frail, n = 864 pre-frail, n = 913 not frail | Liu, C.K. et al. (2016) [50] |
| Homocysteine (µmol/L) | Serum | Increased in frail older people | Fried | Spain | 2020 | Study group of 1211 people, of which 515 were men (42.5%) and 696 were women (57.5%), whose ages were between 65 and 98 years | Alvarez-Sanchez n, (2020) [83] |
| Ophthalmic acid | Serum | Decreased in frailty | Edmonton Frail Scale (EFS) | Japan | 2020 | Group of 19 participants, mean age 84.2 ± 6.9 years, 7 men and 12 women, of which 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as not frail (age 80.5 ± 4.7 years) |
Kameda, M., et al. (2020) [86] |
| Lycopene (µmol/L) | Plasma | Decreased in frail older people | Fried | Germany | 2019 | Study group of 1450 people from the FRAILOMIC database, all over 65 years of age | Kochlik, B., (2019) [29] |
| Lutein/zeaxanthin (µmol/L) | Plasma | Decreased in frail older people | Fried | Germany | 2019 | Study group of 1450 people from the FRAILOMIC database, all over 65 years of age | Kochlik, B., (2019) [29] |
| β- cryptoxanthin (µmol/L) | Plasma | Decreased in frail older people | Fried | Germany | 2019 | Study group of 1450 people from the FRAILOMIC database, all over 65 years of age | Kochlik, B., (2019) [29] |
| Carbonylated proteins (nmol/mg) | Plasma | Increased in frail older people | Fried | Germany | 2019 | Study group of 1450 people from the FRAILOMIC database, all over 65 years of age | Kochlik, B., (2019) [29] |
| Malondialdehyde | Plasma | Increased in frail older people | Fried | Spain | 2014 | Group of 742 people from the Toledo Study for Healthy Aging, of which 309 were men and 433 were women | Ingles, M., (2014) [97] |
4.3. Biomarkers Associated with Coagulation and Platelet Function
Hemostasis stops bleeding at the site of vascular injury and maintains blood vessel integrity through clot formation, where this physiological process consists of interactions between endothelial cells, platelets, von Willebrand factor, and coagulation factors [102]. Some markers indicate when the platelet is activated, among which we can mention P-selectin (CD62P); some proteins participate in coagulation, such as fibrinogen and eicosanoids released by the activated platelet, such as thromboxane A2 [103,104,105].
In a study conducted on a group of people over 60 years of age, the cohort was divided into 3 groups: frail, n = 142; pre-frail, n = 864; non-frail, n = 913. This research aimed to evaluate the relationship between frailty and platelet function, observing that the median results for P-selectin in the group of frail and pre-frail people were greater than that in the non-frail group [50]. P-selectin belongs to the selectin family (CD62) and is a protein stored in the α-granules of platelets and the Weibel Palade bodies of endothelial cells [106].
A study carried out on elderly patients (≥65 years) from the retirement community of San Antonio (TX, USA) evaluated the relationship between frailty and coagulation, observing higher fibrinogen levels in the frail group [107]. Fibrinogen is a glycoprotein, synthesized in the liver, whose main function is to stop excessive bleeding and is associated with the thrombosis process [108,109]. In another study, where the relationship between frailty and platelet activation was evaluated (frail, n = 29; non-frail, n = 29), it was observed that the frail group had higher plasma levels of thromboxane B2 (TXB2) (69.5 pg/mL) compared to the non-frail group (51.3 pg/mL) [76]. Thromboxane B2 is a non-enzymatic derivative of thromboxane A2 (TXA2), the latter produced from arachidonic acid [76].
The previous results show that in the group of frail older people, the levels of P-selectin, fibrinogen, and thromboxane B2 were higher than in the group of non-frail older people, which is important to consider since frailty can cause the platelets in these people to be more activated with a higher risk of thrombosis, there being a clear relationship between platelet hyper-reactivity and the occurrence of thromboembolic events, and can contribute to cardiovascular comorbidities in old age [110,111]. Frailty is closely related to oxidative stress, which plays an important role in the mechanism of platelet activation; therefore, some researchers point out that significant changes in oxidative stress may be one of the main causes of a high platelet response in frail patients [112,113]. Descriptions of all of the above-mentioned biomarkers are presented in Table 3.
Table 3.
Biomarkers associated with coagulation and platelet function.
| BIOMARKER | SAMPLE | CUT VALUES (FRAIL—NOT FRAIL) | FRAILTY SCALE | COUNTRY | YEAR | GROUP DESCRIPTION |
REFERENCE |
|---|---|---|---|---|---|---|---|
| P-selectin (ng/mL) | Plasma | Median and interquartile range: 41 (32–51) (Frail) 41 (33–49) (Pre-frail) 39 (32–47) (Not Frail) |
Fried | United States | 2016 | Group of people over 60 years of age, divided into 3 groups: n = 142 frail, n = 864 pre-frail, n = 913 not frail | Liu, C.K. et al. (2016) [50] |
| Fibrinogen (g/L) | Plasma | 70.4 ± 17.5 (Frail) 40.6 ± 9.3 (Not Frail) |
Fried | United States | 2013 | Group of 65 people over 65 years old n = 12 frail n = 22 not frail |
Darvin, K. et al., 2013 [107] |
| Thromboxane B2 (ng/mL) | Plasma | Interquartile range: 64.0–96.7 (Frail) 38.1–72.2 (Not Frail) |
Fried | Chile | 2019 | Group of people over 65 years of age, divided into 2 groups: n = 29 frail, n = 29 not frail | Arauna, D. et al. (2019) [76] |
4.4. Biomarkers Associated with Growth Factors
A study of 58 participants (age 65 years or more) (frail group, n = 29; non-frail group, n = 29) evaluated the relationship between frailty and growth differentiation factor 15 (GDF-15) [76]. The evidence showed that the frail group presented higher levels in plasma (median: 2379 pg/mL) than the non-frail group (median: 1367 pg/mL) [76]. GDF15 is a member of the transforming growth factor-beta superfamily, widely distributed in mammalian tissues, and has been shown to play multiple roles in various pathologies, including inflammation, cancer, cardiovascular diseases, and obesity [114]. Being a stress-inducible cytokine, GDF-15 is upregulated by several proteins associated with stress and inflammation, such as IL-1β, TNF-α, IL-2, and macrophage colony-stimulating factor (MCSF-1), suggesting a complex tissue-specific regulation [115]. GDF-15 levels increase with age, which is why it has been proposed as a potential biomarker of aging and mitochondrial dysfunction [76,116]. In a previous study that evaluated older patients with chronic kidney disease, it was observed that there was a correlation between age and GDF-15 levels, which could serve as a precedent to evaluate the relationship between high levels of GDF-15 and frailty in extensive cohorts [117]. The description of this study is shown in Table 4.
Table 4.
Biomarkers associated with growth factors.
| BIOMARKER | SAMPLE | CUT VALUES (FRAIL—NOT FRAIL) | FRAILTY SCALE | COUNTRY | YEAR | GROUP DESCRIPTION |
REFERENCE |
|---|---|---|---|---|---|---|---|
| GDF15 | Plasma | Interquartile range: 1845–4121 (Frail) 1190–1747 (Not Frail) |
Fried | Chile | 2019 | Group of people over 65 years of age, divided into 2 groups: n = 29 frail, n = 29 not frail | Arauna, D. et al. (2019) [76] |
4.5. Biomarkers Associated with Musculoskeletal and Cardiac Function
The Framingham study described above also was to assess the relationship between frailty and musculoskeletal function, and the median results obtained for biomarker osteoprotegerin were 5.88 pm/L for the frail group, 5.13 pm/L for the pre-frail group, and 4.81 pm/L for the non-frail group, showing that it was higher in the frail group [50]. Concerning this, some authors report that acute secondary events due to fracture had an additive and independent effect by accentuating the differences between frailty groups, where the admitted patients with fractures had higher mean values of osteoprotegerin than patients without fractures [118]. Osteoprotegerin is a glycoprotein involved in bone remodeling that acts as a decoy receptor for receptor activator for nuclear factor κ B Ligand (RANKL), inhibiting bone resorption [119,120]. As mentioned, osteoprotegerin has been described as a biomarker of bone remodeling, but there is also evidence that it plays a role in cardiovascular diseases, contributing to atherosclerosis and being associated with peripheral arterial disease, where the latter has been associated with slower walking speeds [121,122,123].
NT-proBNP is an N-terminal pro-brain natriuretic peptide that is secreted by cardiac myocytes in response to ventricular and atrial wall stress, serving as a serum biomarker for the diagnosis of heart failure [124]. In a study carried out in a group of 54 frail participants and 74 non-frail participants, the relationship between frailty and cardiac function was evaluated, and the authors observed that NT-proBNP level was increased in the frail group [71]. In the same study, NT-proBNP emerged as an independent marker associated with frailty and has also been suggested as a useful biomarker in identifying frailty in patients with multiple myeloma [71,125]. In another study, it was observed that frail older people had more comorbidities, lower body mass index (BMI), and lower hemoglobin, and also had elevated levels of NT-proBNP along with more severe symptoms of chronic heart failure [126]. Descriptions of all of the above-mentioned biomarkers are presented in Table 5.
Table 5.
Biomarkers associated with musculoskeletal and cardiac function.
| BIOMARKER | SAMPLE | CUT VALUES (FRAIL—NOT FRAIL) | FRAILTY SCALE | COUNTRY | YEAR | GROUP DESCRIPTION |
REFERENCE |
|---|---|---|---|---|---|---|---|
| Osteoprotegerine (pm/L) | Plasma | Median and interquartile range: 5.88 (4.82–7.41) (Frail) 5.13 (4.23–6.13) (Pre-frail) 4.81 (4.01–5.59) (Not Frail) |
Fried | United States | 2016 | Group of people over 60 years of age, divided into 3 groups: n = 142 frail, n = 864 pre-frail, n = 913 not frail | Liu, C.K. et al. (2016) [50] |
| NT-proBNP (pg/mL) | Serum | 11,427.9 ± 21,803.4 (Frail). 1856.4 ± 3570.1 (Not Frail). Increased in frailty |
Clinical Frailty Scale (CFS) | Italy | 2020 | Group of 54 frail persons and 74 not frail persons, age frail 70.5 ± 5.4 years, age not frail 68.2 ± 4.2 years | Komici et al. (2020) [71] |
4.6. Biomarkers Associated with Amino Acids and Vitamins
An adequate protein diet is important in the elderly to maintain muscle mass, as well as support wound healing, skin integrity, immunity, and recovery from illness [127]. In addition, older people also need high protein intake to be able to compensate for high metabolism in conditions of inflammation and the decrease in anabolic capacity with aging [128]; in addition, decreased protein intake has been associated with sarcopenia and frailty [129,130]. Moreover, protein intake influences the production of IGF-1, an important trophic hormone with growth-promoting effects in almost all cells of the body, especially skeletal muscle, cartilage, and bone.
A study carried out in a group of 19 participants, of which 9 were diagnosed as frail and 10 as non-frail according to the Edmonton Frail Scale (EFS), assessed the relationship between frailty and the following amino acids: carnosine, ergothioneine, s-methyl-ergothioneine, trimethyl-histidine, 2-ketobutyrate, isoleucine, leucine, methionine, tryptophan, and proline; all of the aforementioned analytes were decreased in the frail group [86].
Relative to acetyl-carnosine, N-acetyl derivatives of histidine, such as carnosine, exist in mammalian cardiac and skeletal muscle, and the total concentration of these imidazoles can be within the measured range of L-carnosine in skeletal muscle (~10 mM) [131,132]. On the other hand, ergothioneine (ERG) is an unusual betaine thiohistidine amino acid that has potent antioxidant activities and also promotes neuronal stem cell differentiation [133,134,135,136]. As for trimethyl-histidine, it is formed by post-translational methylation of histidine residues in actin and myosin, and its plasma concentration and urinary excretion are sensitive markers of myofibrillar protein degradation [137,138]. On the other hand, the catabolism of threonine and methionine converges in 2-ketobutyrate, which was associated with cognitive impairment and low mobility, which are also associated with frailty in older people [139,140]. The amino acids isoleucine and leucine are branched-chain amino acids, which, together with methionine and tryptophan, are essential amino acids that cannot be synthesized in the human body, so they must be ingested in the diet [141,142,143,144,145,146]. Regarding these amino acids, leucine plays an important role in the regulation of protein metabolism [147], activating protein synthesis in the skeletal muscle by increasing phosphorylation of mammalian target of rapamycin (mTOR) [148], which is important to maintain muscle mass.
Finally, proline is necessary for the biosynthesis of collagen and other proline-containing proteins, so regulation of proline availability for collagen biosynthesis is essential to maintain tissue integrity [149]. The quality of the diet is inversely associated with the risk of developing frailty, and as it is a potentially modifiable factor, it can play an important role in frailty prevention [150,151,152].
A study conducted in the FRAILOMIC cohort evaluated the relationship between frailty and the levels of vitamin D and β-carotene [29]. Vitamin D exists in two forms: vitamin D2, which is obtained from UV radiation on the sterol of ergosterol-type yeasts and is found naturally in fungi exposed to the sun, while the influence of UVB light on the skin of humans synthesizes vitamin D3 [153]. Vitamin D acts as a steroid hormone and influences the bones, intestines, immune and cardiovascular systems, pancreas, muscles, brain, and the control of cell cycles [153]. β-carotene is a tetraterpenoid that in its structure includes 2 β-ionone rings; it is the most important source of non-preformed vitamin A [89]. Regarding these markers, both vitamin D and β-carotene levels were decreased in the frail group [29].
Finally, in a study carried out in a population of 1287 participants (frail group, n = 107; pre-frail group, n = 542; non-frail group, n = 638), the relationship between frailty and amino acid levels was evaluated, observing higher values for asymmetric dimethylarginine (ADMA) in the frail group [154]. ADMA is synthesized when arginine residues in proteins are methylated by the action of arginine methyltransferase, acting as an inhibitor of nitric oxide (NO) synthesis, reducing NO production, and this could lead to endothelial dysfunction and cardiovascular events [155,156,157]. As mentioned above, ADMA influences the reduction of NO production, leading to endothelial dysfunction and cardiovascular events. Descriptions of all of the above-mentioned biomarkers are presented in Table 6.
Table 6.
Biomarkers associated with amino acids and vitamins.
| BIOMARKER | SAMPLE | CUT VALUES (FRAIL—NOT FRAIL) | FRAILTY SCALE | COUNTRY | YEAR | GROUP DESCRIPTION |
REFERENCE |
|---|---|---|---|---|---|---|---|
| Acetyl-carnosine | Serum | Decreased in frailty | Edmonton Frail Scale (EFS) | Japan | 2020 | Group of 19 participants, mean age 84.2 ± 6.9 years, 7 men and 12 women, of which 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as not frail (age 80.5 ± 4.7 years) |
Kameda, M., et al. (2020) [86] |
| Ergothioneine | Serum | Decreased in frailty | Edmonton Frail Scale (EFS) | Japan | 2020 | Group of 19 participants, mean age 84.2 ± 6.9 years, 7 men and 12 women, of which 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as not frail (age 80.5 ± 4.7 years) |
Kameda, M., et al. (2020) [86] |
| S-methyl-ergothioneine | Serum | Decreased in frailty | Edmonton Frail Scale (EFS) | Japan | 2020 | Group of 19 participants, mean age 84.2 ± 6.9 years, 7 men and 12 women, of which 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as not frail (age 80.5 ± 4.7 years) |
Kameda, M., et al. (2020) [86] |
| Trimethyl-histidine | Serum | Decreased in frailty | Edmonton Frail Scale (EFS) |
Japan | 2020 | Group of 19 participants, mean age 84.2 ± 6.9 years, 7 men and 12 women, of which 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as not frail (age 80.5 ± 4.7 years) |
Kameda, M., et al. (2020) [86] |
| 2-ketobutyrate | Serum | Decreased in frailty | Edmonton Frail Scale (EFS) | Japan | 2020 | Group of 19 participants, mean age 84.2 ± 6.9 years, 7 men and 12 women, of which 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as not frail (age 80.5 ± 4.7 years) |
Kameda, M., et al. (2020) [86] |
| Isoleucine | Serum | Decreased in frailty | Edmonton Frail Scale (EFS) | Japan | 2020 | Group of 19 participants, mean age 84.2 ± 6.9 years, 7 men and 12 women, of which 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as not frail (age 80.5 ± 4.7 years) |
Kameda, M., et al. (2020) [86] |
| Leucine | Serum | Decreased in frailty | Edmonton Frail Scale (EFS) | Japan | 2020 | Group of 19 participants, mean age 84.2 ± 6.9 years, 7 men and 12 women, of which 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as not frail (age 80.5 ± 4.7 years) |
Kameda, M., et al. (2020) [86] |
| Methionine | Serum | Decreased in frailty | Edmonton Frail Scale (EFS) | Japan | 2020 | Group of 19 participants, mean age 84.2 ± 6.9 years, 7 men and 12 women, of which 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as not frail (age 80.5 ± 4.7 years) |
Kameda, M., et al. (2020) [86] |
| Tryptophan | Serum | Decreased in frailty | Edmonton Frail Scale (EFS) |
Japan | 2020 | Group of 19 participants, mean age 84.2 ± 6.9 years, 7 men and 12 women, of which 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as not frail (age 80.5 ± 4.7 years) |
Kameda, M., et al. (2020) [86] |
| Proline | Serum | Decreased in frailty | Edmonton Frail Scale (EFS) | Japan | 2020 | Group of 19 participants, mean age 84.2 ± 6.9 years, 7 men and 12 women, of which 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as not frail (age 80.5 ± 4.7 years) |
Kameda, M., et al. (2020) [86] |
| Vitamin D3 (nmol/L) | Plasma | Decreased in frail older people | Fried | Germany | 2019 | Study group of 1450 people from the FRAILOMIC database, all over 65 years of age | Kochlik, B., (2019) [29] |
| β-carotene (µmol/L) | Plasma | Decreased in frail older people | Fried | Germany | 2019 | Study group of 1450 people from the FRAILOMIC database, all over 65 years of age | Kochlik, B., (2019) [29] |
| ADMA | Plasma | Increased in frailty | Fried | Spain | 2014 | Group of 1287 people (552 men and 735 women), mean age of 74.4 years, of which 107 were frail, 542 pre-frail, and 638 not frail. In the group of frail people, ADMA presented higher values | Alonso-Bouzón, C. et al. (2014) [154] |
4.7. Biomarkers Associated with Hepatic and Renal Metabolism
A study carried out on a group of 140 patients with probable Alzheimer’s disease (age ≥65 years) evaluated the relationship between frailty and hepatic metabolism; patients underwent uric acid, albumin, and bilirubin analysis [78]. For uric acid and albumin biomarkers, no significant differences were found between the frail and other groups [78]. Decreased albumin values in clinical settings are associated with nutritional deterioration and inflammatory response associated with the disease, which could be the result of the aging process; however, more studies are still needed to establish this correlation with frailty [158].
On the other hand, in this same study, significant differences were found for bilirubin, with a lower level in the frail group (0.54 ± 0.18 mg/dL), compared to the pre-frail group (0.60 ± 0.21 mg/dL) and not frail (0.66 ± 0.22 mg/dL) [78]. In another study conducted on a group of 19 participants, where 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as non-frail (age 80.5 ± 4.7 years) according to the Edmonton Frail Scale (EFS), it was observed that the bilirubin level was decreased in the frail group, confirming the findings described in the above study [86]. Bilirubin is an end product of the catabolism of the heme group of hemoglobin present in senescent red blood cells [159]. The presented evidence suggests that low serum bilirubin levels could decrease antioxidant capacity, leading to several diseases associated with oxidative stress, and increased levels of oxidative stress and pro-inflammatory conditions in frail and pre-frail patients [112,160].
On the other hand, a previously mentioned study of elderly patients from the retirement community in San Antonio (Texas) also evaluated the relationship between frailty and liver metabolism, observing higher levels of transferrin (ng/mL) in the frail group [107]. Transferrin is a 76 kDa glycoprotein, produced mainly in the liver, and its function corresponds to the transport of iron. [161].
Finally, a study carried out in a group of 252 elderly people from Spain evaluated the relationship between frailty and renal metabolism, and the authors observed that the frail group present higher levels of cortisol than the pre-frail and non-frail groups, which could correlate with the decreased ability to cope with the stress that occurs in frail patients [162]. Cortisol is one of the major glucocorticoids synthesized in the fasciculate zone of the adrenal cortex; it plays an important role in regulating the body’s response to stress through the maintenance of homeostasis and regulation of water and salt balance, blood pressure, immune function and metabolism [163,164]. Descriptions of all of the above-mentioned biomarkers are presented in Table 7.
Table 7.
Biomarkers associated with hepatic and renal metabolism.
| BIOMARKER | SAMPLE | CUT VALUES (FRAIL—NOT FRAIL) | FRAILTY SCALE | COUNTRY | YEAR | GROUP DESCRIPTION |
REFERENCE |
|---|---|---|---|---|---|---|---|
| Uric acid (mg/dL) | Serum | 5.49 ± 1.29 (Frail) 5.00 ± 1.06 (Pre-frail) 5.25 ± 1.23 (Not Frail) |
Fried | Japan | 2017 | Group of 140 outpatients with probable Alzheimer’s disease, 65 years and older | Namioka, N. et al. (2017) [78] |
| Urate | Serum | Decreased in frailty | Edmonton Frail Scale (EFS) | Japan | 2020 | Group of 19 participants, mean age 84.2 ± 6.9 years, 7 men and 12 women, of which 9 were diagnosed as frail (age 88.2 ± 6.8 years) and 10 as not frail (age 80.5 ± 4.7 years) |
Kameda, M., et al. (2020) [86] |
| Albumin (g/dL) | Serum | 3.92 ± 0.31 (Frail) 3.96 ± 0.29 (Pre-frail) 4.06 ± 0.26 (Not Frail) |
Fried | Japan | 2017 | Group of 140 outpatients with probable Alzheimer’s disease, 65 years and older | Namioka, N. et al. (2017) [78] |
| Bilirubin (mg/dL) | Serum | 0.54 ± 0.18 (Frail) 0.60 ± 0.21 (Pre-frail) 0.66 ± 0.22 (Not frail) |
Fried | Japan | 2017 | Group of 140 outpatients with probable Alzheimer’s disease, 65 years and older | Namioka, N. et al. (2017) [78] |
| Transferrin (ng/mL) | Plasma | 58.3 ± 10.2 (Frail) 43.4 ± 11.4 (Not Frail) |
Fried | United States | 2013 | Group of 65 people over 65 years old, n = 12 frail n = 22 not frail |
Darvin, K. et al., 2013 [107] |
| Cortisol (µg/dL) | Serum | Increased in frail older people | Fried | Spain | 2019 | Study group of 252 elderly people (82 men and 170 women) from Spain, whose age range was 65–102 years | Marcos-Perez, D. (2019) [162] |
4.8. Biomarkers Associated with DNA, RNA, and miRNA
MicroRNAs (miRNAs) are a class of non-coding RNAs with a length of 22 nucleotides; they influence the expressions of their target mRNAs at post-transcriptional levels and have been used to detect genetic biomarkers of healthy aging and longevity [165,166]. On the other hand, it is also possible to find miRNA derived from exosomes in extracellular fluids that originate when the multivesicular bodies fuse with the plasma membrane [167]. These exosomes contain miRNA from the cells that gave rise to them, which can modulate protein production in recipient cells [168]. In a study of young people (23–35 years) and older people (≥65 years) classified as frail or robust according to Fried’s criteria [167], miRNAs derived from exosomes were analyzed, and the results show that eight miRNAs were uniquely enriched in frail patients: miR-10a-3p, miR-92a-3p, miR-185–3p, miR-194–5p, miR-326, miR-532–5p, miR-576–5p and miR-760 [167]. Regarding miR-10a-3p, it has been reported that it can regulate cholesterol metabolism in chondrocytes, while miR-92a-3p is expressed during chondrogenesis in human mesenchymal stem cells and differentially in osteoarthritis [169,170]. miR-185-3p has been identified as a tumor suppressor in colorectal cancer [171], whereas miR-194 is a specific miRNA in vertebrates that has a fundamental role in energy production, inflammatory inhibition, and neoplasms such as breast cancer, non-small cell lung cancer, and colorectal cancer [172,173,174]. On the other hand, miR-194-5p has been identified as a regulator of tumorigenesis, while recent studies have suggested that the downregulation of miR-326 serves as a tumor suppressor mechanism and plays a crucial role in carcinogenic cell growth [175,176]. miR-532-5p was reported to have a cancer-promoting effect in cutaneous melanoma [177]; while miR-576-5p enhances melanoma cell invasion in vitro, it is also upregulated in esophageal cancer, where it was found to be involved in cancer cell migration and invasion [178,179]. miR-760 has been reported to regulate the proliferation and apoptosis of a variety of cells, including pulmonary artery smooth muscle cells and colon and ovarian cancer cells [180].
All previously mentioned miRNAs were observed to be augmented in the frail group, representing novel biomarker candidates for frailty [167]. More research is required to determine if these miRNAs change before the development of frailty, which could help determine whether they should be considered as biomarkers for the early diagnosis of frailty. Descriptions of these biomarkers are provided in Table 8.
Table 8.
Biomarkers associated with DNA, RNA and miRNA.
| BIOMARKER | SAMPLE | CUT VALUES (FRAIL—NOT FRAIL) | FRAILTY SCALE | COUNTRY | YEAR | GROUP DESCRIPTION |
REFERENCE |
|---|---|---|---|---|---|---|---|
| miR-10a-3p | Plasma | Increased in frailty | Fried | United States | 2018 | Young people (ages 23–35 years) and people older than 65 years were recruited (the latter were classified as frail or not frail according to Fried’s criteria). | Ipson, B.R., et al. (2018) [167] |
| miR-92a-3p | Plasma | Increased in frailty | Fried | United States | 2018 | Young people (ages 23–35 years) and people older than 65 years were recruited (the latter were classified as frail or not frail according to Fried’s criteria) | Ipson, B.R., et al. (2018) [167] |
| miR-185–3p | Plasma | Increased in frailty | Fried | United States | 2018 | Young people (ages 23–35 years) and people older than 65 years were recruited (the latter were classified as frail or not frail according to Fried’s criteria) | Ipson, B.R., et al. (2018) [167] |
| miR-194–5p | Plasma | Increased in frailty | Fried | United States | 2018 | Young people (ages 23–35 years) and people older than 65 years were recruited (the latter were classified as frail or not frail according to Fried’s criteria) | Ipson, B.R., et al. (2018) [167] |
| miR-326 | Plasma | Increased in frailty | Fried | United States | 2018 | Young people (ages 23–35 years) and people older than 65 years were recruited (the latter were classified as frail or not frail according to Fried’s criteria) | Ipson, B.R., et al. (2018) [167] |
| miR-532–5p | Plasma | Increased in frailty | Fried | United States | 2018 | Young people (ages 23–35 years) and people older than 65 years were recruited (the latter were classified as frail or not frail according to Fried’s criteria) | Ipson, B.R., et al. (2018) [167] |
| miR-576–5p | Plasma | Increased in frailty | Fried | United States | 2018 | Young people (ages 23–35 years) and people older than 65 years were recruited (the latter were classified as frail or not frail according to Fried’s criteria) | Ipson, B.R., et al. (2018) [167] |
| miR-760 | Plasma | Increased in frailty | Fried | United States | 2018 | Young people (ages 23–35 years) and people older than 65 years were recruited (the latter were classified as frail or not frail according to Fried’s criteria) | Ipson, B.R., et al. (2018) [167] |
5. Outlook and Future Directions
Frailty has been assessed from a biophysical frailty phenotype approach as well as a cumulative deficit index model, both of which are reproducible and can predict important health outcomes, such as mortality, chronic diseases, and functional dependency [181,182]. Several biomarkers have been studied as possible candidates to determine frailty in older people; however, using them individually can be a limitation because these biomarkers are mostly considered markers of aging, for which alterations could be associated with this process regardless of whether or not they involve frailty [27,183]. Although many of the biomarkers mentioned are associated with frailty, none of them alone is sufficient for its diagnosis, but together they could improve the sensitivity and specificity of frailty detection, which is also consistent with the definition of frailty as a multidimensional syndrome caused by alterations in multiple biological systems [184]. This has been similarly observed in the relationship between diabetes mellitus and salivary biomarkers, when the incorporation of salivary amylase quantification could reflect improving glycemic control [185]. Communication and information technologies have been proposed in recent years as potential interventions to support older people who are affected by various clinical conditions that can impact their well-being [186]. The application of artificial intelligence (AI) technology offers a potential solution to improve the identification of frailty [187]. AI can be defined as a branch of computer science whose objective is to create systems or methods that analyze information and allow the management of complexity in a wide range of applications [188]. Previous studies suggest that the use of a predictive model based on machine learning could be useful to detect future frailty conditions, as well as the risk of hospital readmissions of these patients, using both clinical and socioeconomic variables that can generally be collected in centers for health care [189,190].
In the clinical environment, there is no standard measure of frailty, and it is necessary to have integral diagnostic tools that allow frailty to be predicted with consideration for the characteristics of each population and that can also be used by employing patient records that health centers maintain [190].
For this reason, there is a need for more research that will allow us to have validated biomarkers of frailty, which, together with some of the frailty scales currently available, can be used in all health centers to detect the risk of frailty, and in this way prevent this syndrome and its associated adverse health events.
6. Conclusions
There are several scales to diagnose frailty, among which the most used is the Fried phenotype, but there is still no validated biomarker that contributes to this diagnosis. Several studies have been carried out to evaluate biomarkers that may be altered when an elderly person is already frail or maintained robustly, but there are still no specific biomarkers that can help in the early diagnosis of frailty. The development of frailty in older people leads to a loss of self-worth and, therefore, they become dependent on the care provided by other persons. In addition, the risk of falls is also increased, and the development of other diseases can lead to the elderly person having to be hospitalized, with all the risks that this implies, which also decreases their life expectancy and quality of life. Being able to determine a biomarker that can detect frailty early would greatly contribute to improving the quality of life of the elderly and thus reduce the incidence of frailty, which is why it is important to continue with more studies that support the recent evidence.
The evidence presented in this review demonstrates that biomarkers associated with inflammation, oxidative stress, skeletal/cardiac muscle function, and platelet function represent promising markers of frailty due to their pathophysiological association with this syndrome. To a lesser extent but with the possibility of greater innovation, biomarkers associated with growth factors, vitamins, amino acids, and miRNAs represent alternatives as markers of this geriatric syndrome. Likewise, the use of AI and the incorporation of sociodemographic variables associated with frailty and available in the records of health centers represent interesting methodologies to strengthen the diagnosis of frailty through the aforementioned biomarkers.
Acknowledgments
All authors thanks to Interuniversity Center for Healthy Aging and FONDECYT (ANID).
Author Contributions
Conceptualization, M.S. and D.A.; methodology, E.F.; software, M.S.; validation, I.P., F.G. and C.A.; formal analysis, M.S.; investigation, M.S.; resources, E.F.; data curation, D.A.; writing—original draft preparation, M.S.; writing—review and editing, D.A., F.G., and C.A.; visualization, D.A.; supervision, E.F. and I.P.; project administration, I.P. and E.F.; funding acquisition, I.P. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by Interuniversity Center for Healthy Aging, Code RED211993, and ANID-FONDECYT N° 1211136.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Patel R., Khan I., Pennington M., Pitts N.B., Robertson C., Gallagher J.E. Protocol for A randomised feasibility trial comparing fluoride interventions to prevent dental decay in older people in care homes (FInCH trial) BMC Oral Health. 2021;21:302. doi: 10.1186/s12903-021-01650-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thumala D., Kennedy B.K., Calvo E., Gonzalez-Billault C., Zitko P., Lillo P., Villagra R., Ibáñez A., Assar R., Andrade M., et al. Aging and Health Policies in Chile: New Agendas for Research. Health Syst. Reform. 2017;3:253–260. doi: 10.1080/23288604.2017.1353844. [DOI] [PubMed] [Google Scholar]
- 3.Michel J.-P., Sadana R. “Healthy aging” concepts and measures. J. Am. Med. Dir. Assoc. 2017;18:460–464. doi: 10.1016/j.jamda.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Veronese N. Frailty as Cardiovascular Risk Factor (and Vice Versa) Adv. Exp. Med. Biol. 2020;1216:51–54. doi: 10.1007/978-3-030-33330-0_6. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization . WHO Clinical Consortium on Healthy Ageing: Topic Focus: Frailty and Intrinsic Capacity: Report of Consortium Meeting, 1–2 December 2016 in Geneva, Switzerland. World Health Organization; Geneva, Switzerland: 2017. [Google Scholar]
- 6.Kojima G. Frailty Defined by FRAIL Scale as a Predictor of Mortality: A Systematic Review and Meta-analysis. J. Am. Med. Dir. Assoc. 2018;19:480–483. doi: 10.1016/j.jamda.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 7.Kojima G. Frailty as a Predictor of Future Falls Among Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2015;16:1027–1033. doi: 10.1016/j.jamda.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 8.Kojima G. Frailty as a predictor of fractures among community-dwelling older people: A systematic review and meta-analysis. Bone. 2016;90:116–122. doi: 10.1016/j.bone.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 9.Kojima G., Taniguchi Y., Iliffe S., Walters K. Frailty as a Predictor of Alzheimer Disease, Vascular Dementia, and All Dementia Among Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2016;17:881–888. doi: 10.1016/j.jamda.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 10.Kojima G. Frailty as a predictor of disabilities among community-dwelling older people: A systematic review and meta-analysis. Disabil. Rehabil. 2017;39:1897–1908. doi: 10.1080/09638288.2016.1212282. [DOI] [PubMed] [Google Scholar]
- 11.Kojima G., Iliffe S., Jivraj S., Walters K. Association between frailty and quality of life among community-dwelling older people: A systematic review and meta-analysis. J. Epidemiol. Community Health. 2016;70:716–721. doi: 10.1136/jech-2015-206717. [DOI] [PubMed] [Google Scholar]
- 12.García-Nogueras I., Aranda-Reneo I., Peña-Longobardo L.M., Oliva-Moreno J., Abizanda P. Use of Health Resources and Healthcare Costs associated with Frailty: The FRADEA Study. J. Nutr. Health Aging. 2017;21:207–214. doi: 10.1007/s12603-016-0727-9. [DOI] [PubMed] [Google Scholar]
- 13.Gobbens R.J., Luijkx K.G., Wijnen-Sponselee M.T., Schols J.M. Toward a conceptual definition of frail community dwelling older people. Nurs. Outlook. 2010;58:76–86. doi: 10.1016/j.outlook.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 14.Lee H., Lee E., Jang I.Y. Frailty and Comprehensive Geriatric Assessment. J. Korean Med. Sci. 2020;35:e16. doi: 10.3346/jkms.2020.35.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Briggs A.M., Araujo de Carvalho I. Actions required to implement integrated care for older people in the community using the World Health Organization’s ICOPE approach: A global Delphi consensus study. PLoS ONE. 2018;13:e0205533. doi: 10.1371/journal.pone.0205533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Won C.W., Ha E., Jeong E., Kim M., Park J., Baek J.E., Kim S., Kim S.B., Roh J., Choi J.H., et al. World Health Organization Integrated Care for Older People (ICOPE) and the Integrated Care of Older Patients with Frailty in Primary Care (ICOOP_Frail) Study in Korea. Ann. Geriatr. Med. Res. 2021;25:10–16. doi: 10.4235/agmr.21.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rudnicka E., Napierała P., Podfigurna A., Męczekalski B., Smolarczyk R., Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020;139:6–11. doi: 10.1016/j.maturitas.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fried L.P., Tangen C.M., Walston J., Newman A.B., Hirsch C., Gottdiener J., Seeman T., Tracy R., Kop W.J., Burke G. Frailty in older adults evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001;56:M146–M157. doi: 10.1093/gerona/56.3.M146. [DOI] [PubMed] [Google Scholar]
- 19.Mitnitski A.B., Mogilner A.J., Rockwood K. Accumulation of deficits as a proxy measure of aging. Sci. World J. 2001;1:323–336. doi: 10.1100/tsw.2001.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aygör H.E., Fadıloğlu Ç., Şahin S., Aykar F.Ş., Akçiçek F. Validation of edmonton frail scale into elderly turkish population. Arch. Gerontol. Geriatr. 2018;76:133–137. doi: 10.1016/j.archger.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 21.García-García F.J., Carcaillon L., Fernandez-Tresguerres J., Alfaro A., Larrion J.L., Castillo C., Rodriguez-Mañas L. A New Operational Definition of Frailty: The Frailty Trait Scale. J. Am. Med. Dir. Assoc. 2014;15:371.e7–371.e13. doi: 10.1016/j.jamda.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 22.Navarro-Flores E., de Bengoa Vallejo R.B., Losa-Iglesias M.E., Palomo-López P., Calvo-Lobo C., López-López D., Martínez-Jiménez E.M., Romero-Morales C. The reliability, validity, and sensitivity of the Edmonton Frail Scale (EFS) in older adults with foot disorders. Aging. 2020;12:24623–24632. doi: 10.18632/aging.202140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zupo R., Castellana F., Donghia R., Lampignano L., Guerra V., De Pergola G., Lozupone M., Bortone I., De Nucci S., Tatoli R., et al. Liver frailty and all-cause mortality in the older participants of the Salus in Apulia Study. GeroScience. 2022;44:835–845. doi: 10.1007/s11357-021-00434-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zupo R., Castellana F., Bortone I., Griseta C., Sardone R., Lampignano L., Lozupone M., Solfrizzi V., Castellana M., Giannelli G., et al. Nutritional domains in frailty tools: Working towards an operational definition of nutritional frailty. Ageing Res. Rev. 2020;64:101148. doi: 10.1016/j.arr.2020.101148. [DOI] [PubMed] [Google Scholar]
- 25.Dibello V., Zupo R., Sardone R., Lozupone M., Castellana F., Dibello A., Daniele A., De Pergola G., Bortone I., Lampignano L., et al. Oral frailty and its determinants in older age: A systematic review. Lancet Healthy Longev. 2021;2:e507–e520. doi: 10.1016/S2666-7568(21)00143-4. [DOI] [PubMed] [Google Scholar]
- 26.Vatic M., von Haehling S., Ebner N. Inflammatory biomarkers of frailty. Exp. Gerontol. 2020;133:110858. doi: 10.1016/j.exger.2020.110858. [DOI] [PubMed] [Google Scholar]
- 27.Saedi A.A., Feehan J., Phu S., Duque G. Current and emerging biomarkers of frailty in the elderly. Clin. Interv. Aging. 2019;14:389–398. doi: 10.2147/CIA.S168687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhu Y., Liu Z., Wang Y., Wang Z., Shi J., Xie X., Jin L., Chu X., Wang X. C-reactive protein, frailty and overnight hospital admission in elderly individuals: A population-based study. Arch. Gerontol. Geriatr. 2016;64:1–5. doi: 10.1016/j.archger.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 29.Kochlik B., Stuetz W., Pérès K., Pilleron S., Féart C., García García F.J., Bandinelli S., Gomez-Cabrero D., Rodriguez-Mañas L., Grune T., et al. Associations of fat-soluble micronutrients and redox biomarkers with frailty status in the FRAILOMIC initiative. J. Cachexia Sarcopenia Muscle. 2019;10:1339–1346. doi: 10.1002/jcsm.12479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buta B.J., Walston J.D., Godino J.G., Park M., Kalyani R.R., Xue Q.L., Bandeen-Roche K., Varadhan R. Frailty assessment instruments: Systematic characterization of the uses and contexts of highly-cited instruments. Ageing Res. Rev. 2016;26:53–61. doi: 10.1016/j.arr.2015.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aubertin-Leheudre M., Woods A.J., Anton S., Cohen R., Pahor M. Frailty Clinical Phenotype: A Physical and Cognitive Point of View. Nestle Nutr. Inst. Workshop Ser. 2015;83:55–63. doi: 10.1159/000382061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abete P., Basile C., Bulli G., Curcio F., Liguori I., Della-Morte D., Gargiulo G., Langellotto A., Testa G., Galizia G., et al. The Italian version of the “frailty index” based on deficits in health: A validation study. Aging Clin. Exp. Res. 2017;29:913–926. doi: 10.1007/s40520-017-0793-9. [DOI] [PubMed] [Google Scholar]
- 33.Afilalo J. The Clinical Frailty Scale. Circulation. 2017;135:2025–2027. doi: 10.1161/CIRCULATIONAHA.116.025958. [DOI] [PubMed] [Google Scholar]
- 34.Moreno-Ariño M., Torrente Jiménez I., Cartanyà Gutiérrez A., Oliva Morera J.C., Comet R. Assessing the strengths and weaknesses of the Clinical Frailty Scale through correlation with a frailty index. Aging Clin. Exp. Res. 2020;32:2225–2232. doi: 10.1007/s40520-019-01450-w. [DOI] [PubMed] [Google Scholar]
- 35.Abellan van Kan G., Rolland Y., Houles M., Gillette-Guyonnet S., Soto M., Vellas B. The assessment of frailty in older adults. Clin. Geriatr. Med. 2010;26:275–286. doi: 10.1016/j.cger.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 36.Perna S., Francis M.D.A., Bologna C., Moncaglieri F., Riva A., Morazzoni P., Allegrini P., Isu A., Vigo B., Guerriero F., et al. Performance of Edmonton Frail Scale on frailty assessment: Its association with multi-dimensional geriatric conditions assessed with specific screening tools. BMC Geriatr. 2017;17:2. doi: 10.1186/s12877-016-0382-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.He Y., Li L.W., Hao Y., Sim E.Y., Ng K.L., Lee R., Lim M.S., Poopalalingam R., Abdullah H.R. Assessment of predictive validity and feasibility of Edmonton Frail Scale in identifying postoperative complications among elderly patients: A prospective observational study. Sci. Rep. 2020;10:14682. doi: 10.1038/s41598-020-71140-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rolfson D.B., Majumdar S.R., Tsuyuki R.T., Tahir A., Rockwood K. Validity and reliability of the Edmonton Frail Scale. Age Ageing. 2006;35:526–529. doi: 10.1093/ageing/afl041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Erusalimsky J.D., Grillari J., Grune T., Jansen-Duerr P., Lippi G., Sinclair A.J., Tegnér J., Viña J., Durrance-Bagale A., Miñambres R., et al. In Search of ‘Omics’-Based Biomarkers to Predict Risk of Frailty and Its Consequences in Older Individuals: The FRAILOMIC Initiative. Gerontology. 2016;62:182–190. doi: 10.1159/000435853. [DOI] [PubMed] [Google Scholar]
- 40.Clegg A., Young J. The frailty syndrome. Clin. Med. 2011;11:72–75. doi: 10.7861/clinmedicine.11-1-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Strandberg T.E., Pitkälä K.H. Frailty in elderly people. Lancet. 2007;369:1328–1329. doi: 10.1016/S0140-6736(07)60613-8. [DOI] [PubMed] [Google Scholar]
- 42.Picca A., Coelho-Junior H.J., Calvani R., Marzetti E., Vetrano D.L. Biomarkers shared by frailty and sarcopenia in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2022;73:101530. doi: 10.1016/j.arr.2021.101530. [DOI] [PubMed] [Google Scholar]
- 43.Atienza M., Ziontz J., Cantero J.L. Low-grade inflammation in the relationship between sleep disruption, dysfunctional adiposity, and cognitive decline in aging. Sleep Med. Rev. 2018;42:171–183. doi: 10.1016/j.smrv.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 44.Castro-Herrera V.M., Lown M., Fisk H.L., Owen-Jones E., Lau M., Lowe R., Hood K., Gillespie D., Hobbs F.D.R., Little P., et al. Relationships Between Age, Frailty, Length of Care Home Residence and Biomarkers of Immunity and Inflammation in Older Care Home Residents in the United Kingdom. Front. Aging. 2021;2:599084. doi: 10.3389/fragi.2021.599084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Calder P.C., Bosco N., Bourdet-Sicard R., Capuron L., Delzenne N., Doré J., Franceschi C., Lehtinen M.J., Recker T., Salvioli S., et al. Health relevance of the modification of low grade inflammation in ageing (inflammageing) and the role of nutrition. Ageing Res. Rev. 2017;40:95–119. doi: 10.1016/j.arr.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 46.Ventura M.T., Casciaro M., Gangemi S., Buquicchio R. Immunosenescence in aging: Between immune cells depletion and cytokines up-regulation. Clin. Mol. Allergy CMA. 2017;15:21. doi: 10.1186/s12948-017-0077-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Luo Y., Zheng S.G. Hall of Fame among Pro-inflammatory Cytokines: Interleukin-6 Gene and Its Transcriptional Regulation Mechanisms. Front. Immunol. 2016;7:604. doi: 10.3389/fimmu.2016.00604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tanaka T., Narazaki M., Kishimoto T. IL-6 in Inflammation, Immunity, and Disease. Cold Spring Harb. Perspect. Biol. 2014;6:a016295. doi: 10.1101/cshperspect.a016295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rønning B., Wyller T.B., Seljeflot I., Jordhøy M.S., Skovlund E., Nesbakken A., Kristjansson S.R. Frailty measures, inflammatory biomarkers and post-operative complications in older surgical patients. Age Ageing. 2010;39:758–761. doi: 10.1093/ageing/afq123. [DOI] [PubMed] [Google Scholar]
- 50.Liu C.K., Lyass A., Larson M.G., Massaro J.M., Wang N., D’Agostino R.B., Sr., Benjamin E.J., Murabito J.M. Biomarkers of oxidative stress are associated with frailty: The Framingham Offspring Study. Age. 2016;38:1. doi: 10.1007/s11357-015-9864-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Netea M.G., Balkwill F., Chonchol M., Cominelli F., Donath M.Y., Giamarellos-Bourboulis E.J., Golenbock D., Gresnigt M.S., Heneka M.T., Hoffman H.M., et al. A guiding map for inflammation. Nat. Immunol. 2017;18:826–831. doi: 10.1038/ni.3790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Musunuru K., Kral B.G., Blumenthal R.S., Fuster V., Campbell C.Y., Gluckman T.J., Lange R.A., Topol E.J., Willerson J.T., Desai M.Y., et al. The use of high-sensitivity assays for C-reactive protein in clinical practice. Nat. Clin. Pract. Cardiovasc. Med. 2008;5:621–635. doi: 10.1038/ncpcardio1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gale C.R., Baylis D., Cooper C., Sayer A.A. Inflammatory markers and incident frailty in men and women: The English Longitudinal Study of Ageing. AGE. 2013;35:2493–2501. doi: 10.1007/s11357-013-9528-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Puts M.T.E., Visser M., Twisk J.W.R., Deeg D.J.H., Lips P. Endocrine and inflammatory markers as predictors of frailty. Clin. Endocrinol. 2005;63:403–411. doi: 10.1111/j.1365-2265.2005.02355.x. [DOI] [PubMed] [Google Scholar]
- 55.Walston J., McBurnie M.A., Newman A., Tracy R.P., Kop W.J., Hirsch C.H., Gottdiener J., Fried L.P., Investigators f.t.C.H.S. Frailty and Activation of the Inflammation and Coagulation Systems With and Without Clinical Comorbidities: Results From the Cardiovascular Health Study. Arch. Intern. Med. 2002;162:2333–2341. doi: 10.1001/archinte.162.20.2333. [DOI] [PubMed] [Google Scholar]
- 56.Cranford T.L., Enos R.T., Velázquez K.T., McClellan J.L., Davis J.M., Singh U.P., Nagarkatti M., Nagarkatti P.S., Robinson C.M., Murphy E.A. Role of MCP-1 on inflammatory processes and metabolic dysfunction following high-fat feedings in the FVB/N strain. Int. J. Obes. 2016;40:844–851. doi: 10.1038/ijo.2015.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yadav A., Saini V., Arora S. MCP-1: Chemoattractant with a role beyond immunity: A review. Clin. Chim. Acta. 2010;411:1570–1579. doi: 10.1016/j.cca.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 58.Nan J., Hu H., Sun Y., Zhu L., Wang Y., Zhong Z., Zhao J., Zhang N., Wang Y., Wang Y., et al. TNFR2 Stimulation Promotes Mitochondrial Fusion via Stat3- and NF-kB–Dependent Activation of OPA1 Expression. Circ. Res. 2017;121:392–410. doi: 10.1161/CIRCRESAHA.117.311143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kastl L., Sauer S.W., Ruppert T., Beissbarth T., Becker M.S., Süss D., Krammer P.H., Gülow K. TNF-α mediates mitochondrial uncoupling and enhances ROS-dependent cell migration via NF-κB activation in liver cells. FEBS Lett. 2014;588:175–183. doi: 10.1016/j.febslet.2013.11.033. [DOI] [PubMed] [Google Scholar]
- 60.Chen X., Oppenheim J.J. Targeting TNFR2, an immune checkpoint stimulator and oncoprotein, is a promising treatment for cancer. Sci. Signal. 2017;10:eaal2328. doi: 10.1126/scisignal.aal2328. [DOI] [PubMed] [Google Scholar]
- 61.Lawson C., Wolf S. ICAM-1 signaling in endothelial cells. Pharmacol. Rep. 2009;61:22–32. doi: 10.1016/S1734-1140(09)70004-0. [DOI] [PubMed] [Google Scholar]
- 62.Liu M., Guo S., Hibbert J.M., Jain V., Singh N., Wilson N.O., Stiles J.K. CXCL10/IP-10 in infectious diseases pathogenesis and potential therapeutic implications. Cytokine Growth Factor Rev. 2011;22:121–130. doi: 10.1016/j.cytogfr.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lee E.Y., Lee Z.-H., Song Y.W. CXCL10 and autoimmune diseases. Autoimmun. Rev. 2009;8:379–383. doi: 10.1016/j.autrev.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 64.Zhao Q., Kim T., Pang J., Sun W., Yang X., Wang J., Song Y., Zhang H., Sun H., Rangan V., et al. A novel function of CXCL10 in mediating monocyte production of proinflammatory cytokines. J. Leukoc. Biol. 2017;102:1271–1280. doi: 10.1189/jlb.5A0717-302. [DOI] [PubMed] [Google Scholar]
- 65.Liu M., Guo S., Stiles J.K. The emerging role of CXCL10 in cancer (Review) Oncol. Lett. 2011;2:583–589. doi: 10.3892/ol.2011.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Qu T., Yang H., Walston J.D., Fedarko N.S., Leng S.X. Upregulated monocytic expression of CXC chemokine ligand 10 (CXCL-10) and its relationship with serum interleukin-6 levels in the syndrome of frailty. Cytokine. 2009;46:319–324. doi: 10.1016/j.cyto.2009.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Simovic Markovic B., Nikolic A., Gazdic M., Bojic S., Vucicevic L., Kosic M., Mitrovic S., Milosavljevic M., Besra G., Trajkovic V., et al. Galectin-3 Plays an Important Pro-inflammatory Role in the Induction Phase of Acute Colitis by Promoting Activation of NLRP3 Inflammasome and Production of IL-1β in Macrophages. J. Crohn’s Colitis. 2016;10:593–606. doi: 10.1093/ecco-jcc/jjw013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dong R., Zhang M., Hu Q., Zheng S., Soh A., Zheng Y., Yuan H. Galectin-3 as a novel biomarker for disease diagnosis and a target for therapy (Review) Int. J. Mol. Med. 2018;41:599–614. doi: 10.3892/ijmm.2017.3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lok D.J.A., Van Der Meer P., de la Porte P.W.B.-A., Lipsic E., Van Wijngaarden J., Hillege H.L., van Veldhuisen D.J. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: Data from the DEAL-HF study. Clin. Res. Cardiol. 2010;99:323–328. doi: 10.1007/s00392-010-0125-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sharma U.C., Pokharel S., Brakel T.J.v., Berlo J.H.v., Cleutjens J.P.M., Schroen B., André S., Crijns H.J.G.M., Gabius H.-J., Maessen J., et al. Galectin-3 Marks Activated Macrophages in Failure-Prone Hypertrophied Hearts and Contributes to Cardiac Dysfunction. Circulation. 2004;110:3121–3128. doi: 10.1161/01.CIR.0000147181.65298.4D. [DOI] [PubMed] [Google Scholar]
- 71.Komici K., Gnemmi I., Bencivenga L., Vitale D.F., Rengo G., Di Stefano A., Eleuteri E. Impact of Galectin-3 Circulating Levels on Frailty in Elderly Patients with Systolic Heart Failure. J. Clin. Med. 2020;9:2229. doi: 10.3390/jcm9072229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chandrasekaran A., Idelchik M., Melendez J.A. Redox control of senescence and age-related disease. Redox Biol. 2017;11:91–102. doi: 10.1016/j.redox.2016.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Powers S.K., Ji L.L., Kavazis A.N., Jackson M.J. Reactive oxygen species: Impact on skeletal muscle. Compr. Physiol. 2011;1:941–969. doi: 10.1002/cphy.c100054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Milne G.L., Yin H., Hardy K.D., Davies S.S., Roberts L.J. Isoprostane Generation and Function. Chem. Rev. 2011;111:5973–5996. doi: 10.1021/cr200160h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Montuschi P., Barnes P.J., Roberts L.J. Isoprostanes: Markers and mediators of oxidative stress. FASEB J. 2004;18:1791–1800. doi: 10.1096/fj.04-2330rev. [DOI] [PubMed] [Google Scholar]
- 76.Arauna D., García F., Rodríguez-Mañas L., Marrugat J., Sáez C., Alarcón M., Wehinger S., Espinosa-Parrilla Y., Palomo I., Fuentes E. Older adults with frailty syndrome present an altered platelet function and an increased level of circulating oxidative stress and mitochondrial dysfunction biomarker GDF-15. Free Radic. Biol. Med. 2020;149:64–71. doi: 10.1016/j.freeradbiomed.2020.01.007. [DOI] [PubMed] [Google Scholar]
- 77.Di Minno A., Turnu L., Porro B., Squellerio I., Cavalca V., Tremoli E., Di Minno MN D. 8-Hydroxy-2-Deoxyguanosine Levels and Cardiovascular Disease: A Systematic Review and Meta-Analysis of the Literature. Antioxid. Redox Signal. 2016;24:548–555. doi: 10.1089/ars.2015.6508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Namioka N., Hanyu H., Hirose D., Hatanaka H., Sato T., Shimizu S. Oxidative stress and inflammation are associated with physical frailty in patients with Alzheimer’s disease. Geriatr. Gerontol. Int. 2017;17:913–918. doi: 10.1111/ggi.12804. [DOI] [PubMed] [Google Scholar]
- 79.Dada N., Kim N.W., Wolfert R.L. Lp-PLA2: An emerging biomarker of coronary heart disease. Expert Rev. Mol. Diagn. 2002;2:17–22. doi: 10.1586/14737159.2.1.17. [DOI] [PubMed] [Google Scholar]
- 80.De Stefano A., Mannucci L., Tamburi F., Cardillo C., Schinzari F., Rovella V., Nisticò S., Bennardo L., Di Daniele N., Tesauro M. Lp-PLA(2), a new biomarker of vascular disorders in metabolic diseases. Int. J. Immunopathol. Pharmacol. 2019;33:2058738419827154. doi: 10.1177/2058738419827154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Stafforini D.M. Plasma PAF-AH (PLA2G7): Biochemical Properties, Association with LDLs and HDLs, and Regulation of Expression. Enzymes. 2015;38:71–93. doi: 10.1016/bs.enz.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 82.Gong M.C., Arbogast S., Guo Z., Mathenia J., Su W., Reid M.B. Calcium-independent phospholipase A2 modulates cytosolic oxidant activity and contractile function in murine skeletal muscle cells. J. Appl. Physiol. 2006;100:399–405. doi: 10.1152/japplphysiol.00873.2005. [DOI] [PubMed] [Google Scholar]
- 83.Álvarez-Sánchez N., Álvarez-Ríos A.I., Guerrero J.M., García-García F.J., Rodríguez-Mañas L., Cruz-Chamorro I., Lardone P.J., Carrillo-Vico A. Homocysteine and C-Reactive Protein Levels Are Associated With Frailty in Older Spaniards: The Toledo Study for Healthy Aging. J. Gerontology. Ser. A. 2020;75:1488–1494. doi: 10.1093/gerona/glz168. [DOI] [PubMed] [Google Scholar]
- 84.Clegg A., Young J., Iliffe S., Rikkert M.O., Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–762. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Depeint F., Bruce W.R., Shangari N., Mehta R., O’Brien P.J. Mitochondrial function and toxicity: Role of B vitamins on the one-carbon transfer pathways. Chem.-Biol. Interact. 2006;163:113–132. doi: 10.1016/j.cbi.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 86.Kameda M., Teruya T., Yanagida M., Kondoh H. Frailty markers comprise blood metabolites involved in antioxidation, cognition, and mobility. Proc. Natl. Acad. Sci. USA. 2020;117:9483–9489. doi: 10.1073/pnas.1920795117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Soga T., Baran R., Suematsu M., Ueno Y., Ikeda S., Sakurakawa T., Kakazu Y., Ishikawa T., Robert M., Nishioka T., et al. Differential metabolomics reveals ophthalmic acid as an oxidative stress biomarker indicating hepatic glutathione consumption. J. Biol. Chem. 2006;281:16768–16776. doi: 10.1074/jbc.M601876200. [DOI] [PubMed] [Google Scholar]
- 88.Orlowski M., Wilk S. Synthesis of ophthalmic acid in liver and kidney in vivo. Biochem. J. 1978;170:415–419. doi: 10.1042/bj1700415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bohn T., Desmarchelier C., El S.N., Keijer J., van Schothorst E., Rühl R., Borel P. β-Carotene in the human body: Metabolic bioactivation pathways – from digestion to tissue distribution and excretion. Proc. Nutr. Soc. 2019;78:68–87. doi: 10.1017/S0029665118002641. [DOI] [PubMed] [Google Scholar]
- 90.Imran M., Ghorat F., Ul-Haq I., Ur-Rehman H., Aslam F., Heydari M., Shariati M.A., Okuskhanova E., Yessimbekov Z., Thiruvengadam M., et al. Lycopene as a Natural Antioxidant Used to Prevent Human Health Disorders. Antioxidants. 2020;9:706. doi: 10.3390/antiox9080706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Eisenhauer B., Natoli S., Liew G., Flood V.M. Lutein and Zeaxanthin-Food Sources, Bioavailability and Dietary Variety in Age-Related Macular Degeneration Protection. Nutrients. 2017;9:120. doi: 10.3390/nu9020120. [DOI] [Google Scholar]
- 92.Burri B.J. Beta-cryptoxanthin as a source of vitamin A. J. Sci. Food Agric. 2015;95:1786–1794. doi: 10.1002/jsfa.6942. [DOI] [PubMed] [Google Scholar]
- 93.Turner T., Burri B.J., Jamil K.M., Jamil M. The effects of daily consumption of β-cryptoxanthin-rich tangerines and β-carotene-rich sweet potatoes on vitamin A and carotenoid concentrations in plasma and breast milk of Bangladeshi women with low vitamin A status in a randomized controlled trial. Am. J. Clin. Nutr. 2013;98:1200–1208. doi: 10.3945/ajcn.113.058180. [DOI] [PubMed] [Google Scholar]
- 94.Alvarado J.C., Fuentes-Santamaría V., Juiz J.M. Frailty Syndrome and Oxidative Stress as Possible Links Between Age-Related Hearing Loss and Alzheimer’s Disease. Front. Neurosci. 2022;15:816300. doi: 10.3389/fnins.2021.816300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Weber D., Davies M.J., Grune T. Determination of protein carbonyls in plasma, cell extracts, tissue homogenates, isolated proteins: Focus on sample preparation and derivatization conditions. Redox Biol. 2015;5:367–380. doi: 10.1016/j.redox.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mas-Bargues C., Escrivá C., Dromant M., Borrás C., Viña J. Lipid peroxidation as measured by chromatographic determination of malondialdehyde. Human plasma reference values in health and disease. Arch. Biochem. Biophys. 2021;709:108941. doi: 10.1016/j.abb.2021.108941. [DOI] [PubMed] [Google Scholar]
- 97.Ingles M., Gambini J., Carnicero J.A., Garcia-Garcia F.J., Rodriguez-Manas L., Olaso-Gonzalez G., Dromant M., Borras C., Vina J. Oxidative stress is related to frailty, not to age or sex, in a geriatric population: Lipid and protein oxidation as biomarkers of frailty. J. Am. Geriatr. Soc. 2014;62:1324–1328. doi: 10.1111/jgs.12876. [DOI] [PubMed] [Google Scholar]
- 98.El-Badry A.A.-M. Serum Malondialdehyde Levels as a Biomarker of Cellular Injury In Human Fascioliasis. J. Taibah Univ. Med. Sci. 2006;1:57–64. doi: 10.1016/S1658-3612(06)70008-7. [DOI] [Google Scholar]
- 99.Mao C., Yuan J.-Q., Lv Y.-B., Gao X., Yin Z.-X., Kraus V.B., Luo J.-S., Chei C.-L., Matchar D.B., Zeng Y., et al. Associations between superoxide dismutase, malondialdehyde and all-cause mortality in older adults: A community-based cohort study. BMC Geriatr. 2019;19:104. doi: 10.1186/s12877-019-1109-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gil P., Fariñas F., Casado A., López-Fernández E. Malondialdehyde: A Possible Marker of Ageing. Gerontology. 2002;48:209–214. doi: 10.1159/000058352. [DOI] [PubMed] [Google Scholar]
- 101.Wu I.C., Shiesh S.C., Kuo P.H., Lin X.Z. High oxidative stress is correlated with frailty in elderly chinese. J. Am. Geriatr. Soc. 2009;57:1666–1671. doi: 10.1111/j.1532-5415.2009.02392.x. [DOI] [PubMed] [Google Scholar]
- 102.Sang Y., Roest M., de Laat B., de Groot P.G., Huskens D. Interplay between platelets and coagulation. Blood Rev. 2021;46:100733. doi: 10.1016/j.blre.2020.100733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kattula S., Byrnes J.R., Wolberg A.S. Fibrinogen and Fibrin in Hemostasis and Thrombosis. Arterioscler. Thromb. Vasc. Biol. 2017;37:e13–e21. doi: 10.1161/ATVBAHA.117.308564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hegazy S., Elsabaawy M., Eltabakh M., Hammad R., Bedair H. CD62P (P-selectin) expression as a platelet activation marker in patients with liver cirrhosis with and without cholestasis. Clin. Exp. Hepatol. 2021;7:231–240. doi: 10.5114/ceh.2021.107566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Patrono C., Rocca B. Measurement of Thromboxane Biosynthesis in Health and Disease. Front. Pharmacol. 2019;10:1244. doi: 10.3389/fphar.2019.01244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Qi C., Wei B., Zhou W., Yang Y., Li B., Guo S., Li J., Ye J., Li J., Zhang Q., et al. P-selectin-mediated platelet adhesion promotes tumor growth. Oncotarget. 2015;6:6584–6596. doi: 10.18632/oncotarget.3164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Darvin K., Randolph A., Ovalles S., Halade D., Breeding L., Richardson A., Espinoza S.E. Plasma Protein Biomarkers of the Geriatric Syndrome of Frailty. J. Gerontol. Ser. A. 2013;69A:182–186. doi: 10.1093/gerona/glt183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lowe G.D.O., Rumley A., Mackie I.J. Plasma fibrinogen. Ann. Clin. Biochem. 2004;41:430–440. doi: 10.1258/0004563042466884. [DOI] [PubMed] [Google Scholar]
- 109.Li R., Shao H.-Y., Hao L.-B., Yu B.-Z., Qu P.-F., Zhou Y.-X., Chen J.-Y. Plasma Fibrinogen Exhibits Better Performance Than Plasma D-Dimer in the Diagnosis of Periprosthetic Joint Infection: A Multicenter Retrospective Study. JBJS. 2019;101:613–619. doi: 10.2106/JBJS.18.00624. [DOI] [PubMed] [Google Scholar]
- 110.Hernández B., Fuentes E., Palomo I., Alarcón M. Increased platelet function during frailty. Exp. Hematol. 2019;77:12–25.e12. doi: 10.1016/j.exphem.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 111.Faria A.V.S., Andrade S.S., Peppelenbosch M.P., Ferreira-Halder C.V., Fuhler G.M. Platelets in aging and cancer—“double-edged sword”. Cancer Metastasis Rev. 2020;39:1205–1221. doi: 10.1007/s10555-020-09926-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Soysal P., Isik A.T., Carvalho A.F., Fernandes B.S., Solmi M., Schofield P., Veronese N., Stubbs B. Oxidative stress and frailty: A systematic review and synthesis of the best evidence. Maturitas. 2017;99:66–72. doi: 10.1016/j.maturitas.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 113.Liu Y., Liu S., Wang K., Liu H. Association of Frailty With Antiplatelet Response Among Elderly Chinese Patients With Coronary Artery Disease Undergoing Percutaneous Coronary Intervention. Clin. Appl. Thromb./Hemost. 2020;26:1076029620915994. doi: 10.1177/1076029620915994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Unsicker K., Spittau B., Krieglstein K. The multiple facets of the TGF-β family cytokine growth/differentiation factor-15/macrophage inhibitory cytokine-1. Cytokine Growth Factor Rev. 2013;24:373–384. doi: 10.1016/j.cytogfr.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 115.Adela R., Banerjee S.K. GDF-15 as a Target and Biomarker for Diabetes and Cardiovascular Diseases: A Translational Prospective. J. Diabetes Res. 2015;2015:490842. doi: 10.1155/2015/490842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Liu H., Huang Y., Lyu Y., Dai W., Tong Y., Li Y. GDF15 as a biomarker of ageing. Exp. Gerontol. 2021;146:111228. doi: 10.1016/j.exger.2021.111228. [DOI] [PubMed] [Google Scholar]
- 117.Kim J.S., Kim S., Won C.W., Jeong K.H. Association between Plasma Levels of Growth Differentiation Factor-15 and Renal Function in the Elderly: Korean Frailty and Aging Cohort Study. Kidney Blood Press. Res. 2019;44:405–414. doi: 10.1159/000498959. [DOI] [PubMed] [Google Scholar]
- 118.Valentini A., Cianfarani M.A., Tarantino U., Di Daniele N., Bertoli A. Osteoprotegerin as a biomarker of geriatric frailty syndrome. Aging. 2019;11:4900–4909. doi: 10.18632/aging.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Pérez de Ciriza C., Lawrie A., Varo N. Osteoprotegerin in Cardiometabolic Disorders. Int. J. Endocrinol. 2015;2015:564934. doi: 10.1155/2015/564934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Muñoz-Torres M., Higuera López-Frías M.d.l., Fernández García D. Avances en el conocimiento de la biología del osteoclasto: El sistema osteoprotegerina-ligando del RANK. Med. Clínica. 2004;122:75–77. doi: 10.1016/S0025-7753(04)74146-9. [DOI] [PubMed] [Google Scholar]
- 121.Poulsen M.K., Nybo M., Dahl J., Hosbond S., Poulsen T.S., Johansen A., Høilund-Carlsen P.F., Beck-Nielsen H., Rasmussen L.M., Henriksen J.E. Plasma osteoprotegerin is related to carotid and peripheral arterial disease, but not to myocardial ischemia in type 2 diabetes mellitus. Cardiovasc. Diabetol. 2011;10:76. doi: 10.1186/1475-2840-10-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Montecucco F., Steffens S., Mach F. The immune response is involved in atherosclerotic plaque calcification: Could the RANKL/RANK/OPG system be a marker of plaque instability? Clin. Dev. Immunol. 2007;2007:75805. doi: 10.1155/2007/75805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.McDermott M.M., Liu K., Greenland P., Guralnik J.M., Criqui M.H., Chan C., Pearce W.H., Schneider J.R., Ferrucci L., Celic L., et al. Functional decline in peripheral arterial disease: Associations with the ankle brachial index and leg symptoms. Jama. 2004;292:453–461. doi: 10.1001/jama.292.4.453. [DOI] [PubMed] [Google Scholar]
- 124.Maisel A.S., Krishnaswamy P., Nowak R.M., McCord J., Hollander J.E., Duc P., Omland T., Storrow A.B., Abraham W.T., Wu A.H.B., et al. Rapid Measurement of B-Type Natriuretic Peptide in the Emergency Diagnosis of Heart Failure. N. Engl. J. Med. 2002;347:161–167. doi: 10.1056/NEJMoa020233. [DOI] [PubMed] [Google Scholar]
- 125.Milani P., Vincent Rajkumar S., Merlini G., Kumar S., Gertz M.A., Palladini G., Lacy M.Q., Buadi F.K., Hayman S.R., Leung N., et al. N-terminal fragment of the type-B natriuretic peptide (NT-proBNP) contributes to a simple new frailty score in patients with newly diagnosed multiple myeloma. Am. J. Hematol. 2016;91:1129–1134. doi: 10.1002/ajh.24532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sze S., Pellicori P., Zhang J., Weston J., Squire I., Clark A. Effect of frailty on treatment, hospitalisation and death in patients with chronic heart failure. Clin. Res. Cardiol. 2021;110:1249–1258. doi: 10.1007/s00392-020-01792-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Baum J.I., Kim I.-Y., Wolfe R.R. Protein Consumption and the Elderly: What Is the Optimal Level of Intake? Nutrients. 2016;8:359. doi: 10.3390/nu8060359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Paddon-Jones D., Rasmussen B.B. Dietary protein recommendations and the prevention of sarcopenia. Curr. Opin. Clin. Nutr. Metab. Care. 2009;12:86–90. doi: 10.1097/MCO.0b013e32831cef8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Clegg M.E., Williams E.A. Optimizing nutrition in older people. Maturitas. 2018;112:34–38. doi: 10.1016/j.maturitas.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 130.Richardson N.E., Konon E.N., Schuster H.S., Mitchell A.T., Boyle C., Rodgers A.C., Finke M., Haider L.R., Yu D., Flores V., et al. Lifelong restriction of dietary branched-chain amino acids has sex-specific benefits for frailty and lifespan in mice. Nat. Aging. 2021;1:73–86. doi: 10.1038/s43587-020-00006-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.O’Dowd J.J., Robins D.J., Miller D.J. Detection, characterisation, and quantification of carnosine and other histidyl derivatives in cardiac and skeletal muscle. Biochim. Biophys. Acta. 1988;967:241–249. doi: 10.1016/0304-4165(88)90015-3. [DOI] [PubMed] [Google Scholar]
- 132.Babizhayev M.A., Deyev A.I., Yermakova V.N., Semiletov Y.A., Davydova N.G., Kurysheva N.I., Zhukotskii A.V., Goldman I.M. N-Acetylcarnosine, a natural histidine-containing dipeptide, as a potent ophthalmic drug in treatment of human cataracts. Peptides. 2001;22:979–994. doi: 10.1016/S0196-9781(01)00407-7. [DOI] [PubMed] [Google Scholar]
- 133.Ishimoto T., Masuo Y., Kato Y., Nakamichi N. Ergothioneine-induced neuronal differentiation is mediated through activation of S6K1 and neurotrophin 4/5-TrkB signaling in murine neural stem cells. Cell. Signal. 2019;53:269–280. doi: 10.1016/j.cellsig.2018.10.012. [DOI] [PubMed] [Google Scholar]
- 134.López de Heredia M., Muñoz L., Carru C., Sotgia S., Zinellu A., Serra C., Llebaria A., Kato Y., Nunes V. S-Methyl-L-Ergothioneine to L-Ergothioneine Ratio in Urine Is a Marker of Cystine Lithiasis in a Cystinuria Mouse Model. Antioxidants. 2021;10:1424. doi: 10.3390/antiox10091424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Borodina I., Kenny L.C., McCarthy C.M., Paramasivan K., Pretorius E., Roberts T.J., van der Hoek S.A., Kell D.B. The biology of ergothioneine, an antioxidant nutraceutical. Nutr. Res. Rev. 2020;33:190–217. doi: 10.1017/S0954422419000301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Cheah I., Tang R., Yew T., Lim K., Halliwell B. Administration of Pure Ergothioneine to Healthy Human Subjects: Uptake, Metabolism, and Effects on Biomarkers of Oxidative Damage and Inflammation. Antioxid. Redox Signal. 2016;26 doi: 10.1089/ars.2016.6778. [DOI] [PubMed] [Google Scholar]
- 137.Holeček M. Histidine in Health and Disease: Metabolism, Physiological Importance, and Use as a Supplement. Nutrients. 2020;12:848. doi: 10.3390/nu12030848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Nagasawa T., Yoshizawa F., Nishizawa N. Plasma Nτ-Methylhistidine Concentration Is a Sensitive Index of Myofibrillar Protein Degradation during Starvation in Rats. Biosci. Biotechnol. Biochem. 1996;60:501–502. doi: 10.1271/bbb.60.501. [DOI] [PubMed] [Google Scholar]
- 139.Bui D., Ravasz D., Chinopoulos C. The Effect of 2-Ketobutyrate on Mitochondrial Substrate-Level Phosphorylation. Neurochem. Res. 2019;44:2301–2306. doi: 10.1007/s11064-019-02759-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ge M.L., Simonsick E.M., Dong B.R., Kasper J.D., Xue Q.L. Frailty, With or Without Cognitive Impairment, Is a Strong Predictor of Recurrent Falls in a US Population-Representative Sample of Older Adults. J. Gerontol. Ser. A. 2021;76:e354–e360. doi: 10.1093/gerona/glab083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Pályi G., editor. Biological Chirality. Academic Press; Cambridge, MA, USA: 2020. Chapter 2 - Stock-list of chiral biomolecules; pp. 15–83. [DOI] [Google Scholar]
- 142.Mero A. Leucine supplementation and intensive training. Sports Med. 1999;27:347–358. doi: 10.2165/00007256-199927060-00001. [DOI] [PubMed] [Google Scholar]
- 143.Gorissen S.H.M., Phillips S.M. Chapter 17 - Branched-Chain Amino Acids (Leucine, Isoleucine, and Valine) and Skeletal Muscle. In: Walrand S., editor. Nutrition and Skeletal Muscle. Academic Press; Cambridge, MA, USA: 2019. pp. 283–298. [DOI] [Google Scholar]
- 144.Harper A.E., Miller R.H., Block K.P. Branched-Chain Amino Acid Metabolism. Annu. Rev. Nutr. 1984;4:409–454. doi: 10.1146/annurev.nu.04.070184.002205. [DOI] [PubMed] [Google Scholar]
- 145.Martínez Y., Li X., Liu G., Bin P., Yan W., Más D., Valdivié M., Hu C.-A.A., Ren W., Yin Y. The role of methionine on metabolism, oxidative stress, and diseases. Amino Acids. 2017;49:2091–2098. doi: 10.1007/s00726-017-2494-2. [DOI] [PubMed] [Google Scholar]
- 146.Friedman M. Analysis, Nutrition, and Health Benefits of Tryptophan. Int. J. Tryptophan Res. 2018;11:1178646918802282. doi: 10.1177/1178646918802282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Cruz B., Oliveira A., Ventrucci G., Gomes-Marcondes M.C.C. A leucine-rich diet modulates the mTOR cell signalling pathway in the gastrocnemius muscle under different Walker-256 tumour growth conditions. BMC Cancer. 2019;19:349. doi: 10.1186/s12885-019-5448-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Mirza K.A., Pereira S.L., Voss A.C., Tisdale M.J. Comparison of the anticatabolic effects of leucine and Ca-β-hydroxy-β-methylbutyrate in experimental models of cancer cachexia. Nutrition. 2014;30:807–813. doi: 10.1016/j.nut.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 149.Albaugh V.L., Mukherjee K., Barbul A. Proline Precursors and Collagen Synthesis: Biochemical Challenges of Nutrient Supplementation and Wound Healing. J. Nutr. 2017;147:2011–2017. doi: 10.3945/jn.117.256404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Kelaiditi E., Guyonnet S., Cesari M. Is nutrition important to postpone frailty? Curr. Opin. Clin. Nutr. Metab. Care. 2015;18:37–42. doi: 10.1097/MCO.0000000000000129. [DOI] [PubMed] [Google Scholar]
- 151.Lorenzo-López L., Maseda A., de Labra C., Regueiro-Folgueira L., Rodríguez-Villamil J.L., Millán-Calenti J.C. Nutritional determinants of frailty in older adults: A systematic review. BMC Geriatr. 2017;17:108. doi: 10.1186/s12877-017-0496-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bartali B., Frongillo E.A., Bandinelli S., Lauretani F., Semba R.D., Fried L.P., Ferrucci L. Low nutrient intake is an essential component of frailty in older persons. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2006;61:589–593. doi: 10.1093/gerona/61.6.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Nair R., Maseeh A. Vitamin D: The “sunshine” vitamin. J. Pharmacol. Pharmacother. 2012;3:118–126. doi: 10.4103/0976-500x.95506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Alonso-Bouzon C., Carcaillon L., Garcia-Garcia F.J., Amor-Andres M.S., El Assar M., Rodriguez-Manas L. Association between endothelial dysfunction and frailty: The Toledo Study for Healthy Aging. Age. 2014;36:495–505. doi: 10.1007/s11357-013-9576-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Lee W., Lee H.J., Jang H.B., Kim H.-J., Ban H.-J., Kim K.Y., Nam M.S., Choi J.S., Lee K.-T., Cho S.B., et al. Asymmetric dimethylarginine (ADMA) is identified as a potential biomarker of insulin resistance in skeletal muscle. Sci. Rep. 2018;8:2133. doi: 10.1038/s41598-018-20549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.San Miguel A., San Miguel R., Martín Gil F.J. Dimetilarginina asimétrica (ADMA) en diferentes enfermedades. Rev. Lab. Clín. 2008;1:113–121. doi: 10.1016/j.labcli.2008.09.002. [DOI] [Google Scholar]
- 157.Sibal L., Agarwal S.C., Home P.D., Boger R.H. The Role of Asymmetric Dimethylarginine (ADMA) in Endothelial Dysfunction and Cardiovascular Disease. Curr. Cardiol. Rev. 2010;6:82–90. doi: 10.2174/157340310791162659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Yamamoto M., Adachi H., Enomoto M., Fukami A., Nakamura S., Nohara Y., Sakaue A., Morikawa N., Hamamura H., Toyomasu K., et al. Lower albumin levels are associated with frailty measures, trace elements, and an inflammation marker in a cross-sectional study in Tanushimaru. Environ. Health Prev. Med. 2021;26:25. doi: 10.1186/s12199-021-00946-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Vítek L. Bilirubin and atherosclerotic diseases. Physiol. Res. 2017;66:S11–S20. doi: 10.33549/physiolres.933581. [DOI] [PubMed] [Google Scholar]
- 160.Inoguchi T., Fukuhara S., Yamato M., Nakai M., Etoh T., Masakado M., Suehiro S., Umeda F., Yamauchi T. Serum bilirubin level is a strong predictor for disability in activities in daily living (ADL) in Japanese elderly patients with diabetes. Sci. Rep. 2019;9:7069. doi: 10.1038/s41598-019-43543-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kawabata H. Transferrin and transferrin receptors update. Free Radic. Biol. Med. 2019;133:46–54. doi: 10.1016/j.freeradbiomed.2018.06.037. [DOI] [PubMed] [Google Scholar]
- 162.Marcos-Pérez D., Sánchez-Flores M., Maseda A., Lorenzo-López L., Millán-Calenti J.C., Pásaro E., Laffon B., Valdiglesias V. Serum cortisol but not oxidative stress biomarkers are related to frailty: Results of a cross-sectional study in Spanish older adults. J. Toxicol. Environ. Health Part A. 2019;82:815–825. doi: 10.1080/15287394.2019.1654639. [DOI] [PubMed] [Google Scholar]
- 163.Katsu Y., Baker M.E. Subchapter 123D—Cortisol. In: Ando H., Ukena K., Nagata S., editors. Handbook of Hormones (Second Edition) Academic Press; San Diego, CA, USA: 2021. pp. 947–949. [DOI] [Google Scholar]
- 164.Gardner M.P., Lightman S., Sayer A.A., Cooper C., Cooper R., Deeg D., Ebrahim S., Gallacher J., Kivimaki M., Kumari M., et al. Dysregulation of the hypothalamic pituitary adrenal (HPA) axis and physical performance at older ages: An individual participant meta-analysis. Psychoneuroendocrinology. 2013;38:40–49. doi: 10.1016/j.psyneuen.2012.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Liu H., Yi X., Tu S., Cheng C., Luo J. Kaempferol promotes BMSC osteogenic differentiation and improves osteoporosis by downregulating miR-10a-3p and upregulating CXCL12. Mol. Cell. Endocrinol. 2021;520:111074. doi: 10.1016/j.mce.2020.111074. [DOI] [PubMed] [Google Scholar]
- 166.Smith-Vikos T., Liu Z., Parsons C., Gorospe M., Ferrucci L., Gill T.M., Slack F.J. A serum miRNA profile of human longevity: Findings from the Baltimore Longitudinal Study of Aging (BLSA) Aging. 2016;8:2971–2987. doi: 10.18632/aging.101106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Ipson B.R., Fletcher M.B., Espinoza S.E., Fisher A.L. Identifying Exosome-Derived MicroRNAs as Candidate Biomarkers of Frailty. J. Frailty Aging. 2018;7:100–103. doi: 10.14283/jfa.2017.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Valadi H., Ekström K., Bossios A., Sjöstrand M., Lee J.J., Lötvall J.O. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 169.Li X., Zhang L., Shi X., Liao T., Zhang N., Gao Y., Xing R., Wang P. MicroRNA-10a-3p Improves Cartilage Degeneration by Regulating CH25H-CYP7B1-RORα Mediated Cholesterol Metabolism in Knee Osteoarthritis Rats. Front. Pharmacol. 2021;12:690181. doi: 10.3389/fphar.2021.690181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Mao G., Zhang Z., Huang Z., Chen W., Huang G., Meng F., Zhang Z., Kang Y. MicroRNA-92a-3p regulates the expression of cartilage-specific genes by directly targeting histone deacetylase 2 in chondrogenesis and degradation. Osteoarthr. Cartil. 2017;25:521–532. doi: 10.1016/j.joca.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 171.Zhou C., Kong W., Ju T., Xie Q., Zhai L. MiR-185-3p mimic promotes the chemosensitivity of CRC cells via AQP5. Cancer Biol. Ther. 2020;21:790–798. doi: 10.1080/15384047.2020.1761238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Zhu X., Li D., Yu F., Jia C., Xie J., Ma Y., Fan S., Cai H., Luo Q., Lv Z., et al. miR-194 inhibits the proliferation, invasion, migration, and enhances the chemosensitivity of non-small cell lung cancer cells by targeting forkhead box A1 protein. Oncotarget. 2016;7:13139–13152. doi: 10.18632/oncotarget.7545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Yang F., Xiao Z., Zhang S. Knockdown of miR-194-5p inhibits cell proliferation, migration and invasion in breast cancer by regulating the Wnt/β-catenin signaling pathway. Int. J. Mol. Med. 2018;42:3355–3363. doi: 10.3892/ijmm.2018.3897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Chang H.Y., Ye S.P., Pan S.L., Kuo T.T., Liu B.C., Chen Y.L., Huang T.C. Overexpression of miR-194 Reverses HMGA2-driven Signatures in Colorectal Cancer. Theranostics. 2017;7:3889–3900. doi: 10.7150/thno.20041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Shi Y., Mao X., Cai M., Hu S., Lai X., Chen S., Jia X., Wang J., Lai S. miR-194-5p negatively regulates the proliferation and differentiation of rabbit skeletal muscle satellite cells. Mol. Cell. Biochem. 2021;476:425–433. doi: 10.1007/s11010-020-03918-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Liang X., Li Z., Men Q., Li Y., Li H., Chong T. miR-326 functions as a tumor suppressor in human prostatic carcinoma by targeting Mucin1. Biomed. Pharmacother. 2018;108:574–583. doi: 10.1016/j.biopha.2018.09.053. [DOI] [PubMed] [Google Scholar]
- 177.Kitago M., Martinez S.R., Nakamura T., Sim M.S., Hoon D.S. Regulation of RUNX3 tumor suppressor gene expression in cutaneous melanoma. Clin. Cancer Res. 2009;15:2988–2994. doi: 10.1158/1078-0432.CCR-08-3172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Kordaß T., Weber C.E.M., Eisel D., Pane A.A., Osen W., Eichmüller S.B. miR-193b and miR-30c-1(*) inhibit, whereas miR-576-5p enhances melanoma cell invasion in vitro. Oncotarget. 2018;9:32507–32522. doi: 10.18632/oncotarget.25986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Luo J., Liu L., Shen J., Zhou N., Feng Y., Zhang N., Sun Q., Zhu Y. miR-576-5p promotes epithelial-to-mesenchymal transition in colorectal cancer by targeting the Wnt5a-mediated Wnt/β-catenin signaling pathway. Mol. Med. Rep. 2021;23:94. doi: 10.3892/mmr.2020.11733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Tang X., Wang J., Zhou S., Zhou J., Jia G., Wang H., Xin C., Fu G., Zhang J. miR-760 regulates skeletal muscle proliferation in rheumatoid arthritis by targeting Myo18b. Mol. Med. Rep. 2019;20:4843–4854. doi: 10.3892/mmr.2019.10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Wou F., Conroy S. The frailty syndrome. Medicine. 2013;41:13–15. doi: 10.1016/j.mpmed.2012.10.004. [DOI] [Google Scholar]
- 182.Blodgett J., Theou O., Kirkland S., Andreou P., Rockwood K. Frailty in NHANES: Comparing the frailty index and phenotype. Arch. Gerontol. Geriatr. 2015;60:464–470. doi: 10.1016/j.archger.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 183.Mitnitski A., Collerton J., Martin-Ruiz C., Jagger C., von Zglinicki T., Rockwood K., Kirkwood T.B. Age-related frailty and its association with biological markers of ageing. BMC Med. 2015;13:161. doi: 10.1186/s12916-015-0400-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Mailliez A., Guilbaud A., Puisieux F., Dauchet L., Boulanger É. Circulating biomarkers characterizing physical frailty: CRP, hemoglobin, albumin, 25OHD and free testosterone as best biomarkers. Results of a meta-analysis. Exp. Gerontol. 2020;139:111014. doi: 10.1016/j.exger.2020.111014. [DOI] [PubMed] [Google Scholar]
- 185.Pérez-Ros P., Navarro-Flores E., Julián-Rochina I., Martínez-Arnau F.M., Cauli O. Changes in Salivary Amylase and Glucose in Diabetes: A Scoping Review. Diagnostics. 2021;11:453. doi: 10.3390/diagnostics11030453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Kouroubali A., Kondylakis H., Logothetidis F., Katehakis D.G. Developing an AI-Enabled Integrated Care Platform for Frailty. Healthcare. 2022;10:443. doi: 10.3390/healthcare10030443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Ambagtsheer R.C., Shafiabady N., Dent E., Seiboth C., Beilby J. The application of artificial intelligence (AI) techniques to identify frailty within a residential aged care administrative data set. Int. J. Med. Inform. 2020;136:104094. doi: 10.1016/j.ijmedinf.2020.104094. [DOI] [PubMed] [Google Scholar]
- 188.Contreras I., Vehi J. Artificial Intelligence for Diabetes Management and Decision Support: Literature Review. J. Med. Internet Res. 2018;20:e10775. doi: 10.2196/10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Mohanty S.D., Lekan D., McCoy T.P., Jenkins M., Manda P. Machine learning for predicting readmission risk among the frail: Explainable AI for healthcare. Patterns. 2022;3:100395. doi: 10.1016/j.patter.2021.100395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Tarekegn A., Ricceri F., Costa G., Ferracin E., Giacobini M. Predictive Modeling for Frailty Conditions in Elderly People: Machine Learning Approaches. JMIR Med. Inform. 2020;8:e16678. doi: 10.2196/16678. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.