Abstract
The COVID-19 pandemic and its accompanying infection control measures introduced significant disruptions to the routines of many higher education students around the world. It also deprived them of in-person counselling services and social support. These changes have put students at a greater risk of developing mental illness. The objective of this review is to assess the prevalence of depressive symptoms, anxiety symptoms and sleep disturbances in higher education students during the pandemic. A systematic search of English and Chinese databases was conducted current to January 1st, 2021. The quality of included studies was evaluated using a modified Newcastle-Ottawa scale. Prevalence of depressive symptoms, anxiety symptoms and sleep disturbances were pooled using random-effects meta-analysis. Eighty-nine studies (n=1,441,828) were included. The pooled prevalence of depressive symptoms, anxiety symptoms, and sleep disturbances was 34%, 32% and 33%, respectively. The prevalence values differ based on geographical regions, diagnostic criteria, education level, undergraduate year of study, financial situation, living arrangements and gender. Overall, the prevalence of depressive symptoms and anxiety symptoms synthesized in this study was higher compared to pre-pandemic prevalence in similar populations. Evidently, mental health screening and intervention should be a top priority for universities and colleges during the pandemic.
Keywords: Depression, Anxiety, Sleep Disturbance, COVID-19, Pandemic, University, Student
1. Introduction
In December 2019, a series of acute, atypical respiratory diseases was identified in Wuhan, China. The illness was attributed to a novel coronavirus, the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), and the disease it causes was named the coronavirus disease 2019 (COVID-19) (Lotfi et al., 2020; Yuki et al., 2020; Zhai et al., 2020). This disease is highly infectious (Ryu et al., 2020); with a basic reproduction number (R0) of 3.28 (Liu et al., 2020), COVID-19 quickly spread to countries around the world. As a result, the World Health Organization (WHO) declared COVID-19 as a global pandemic on March 11th, 2020 (Shereen et al., 2020; World Health Organization, 2021). Since its discovery, there have been nearly 92 million confirmed cases and two million deaths in over 200 countries (Johns Hopkins University, 2021 COVID-19 Map).
With no effective treatment available for COVID-19, governments have since implemented various pandemic control measures, such as quarantine and social distancing guidelines, to control the spread of the pandemic (Sheikh et al., 2020). Some countries even enforced mandatory curfews during the early stages of the pandemic (Khatatbeh, 2020). Although these measures may help prevent the spread of SARS-CoV-2, they have inevitably led to the termination of social gatherings, closure of many small businesses (Fairlie, 2020), as well as increased prevalence of financial difficulties due to layoffs (Bartik et al., 2020) and medical expenses (Barnett et al., 2020). In the United States (US) alone, more than 20 million people filed for unemployment between the start of COVID-19 and mid-April of 2020 (Ettman et al., 2020). It is evident that the pandemic has introduced significant disruptions and stressors to the daily lives of the general public. As such, it is important to highlight the impact of the pandemic on mental health and psychological wellness, in addition to the physiological implications of COVID-19.
Previous studies investigating the effect of disasters on mental health have found that large-scale traumatic events that carry economic and social consequences are associated with an increased burden of mental illnesses in the affected populations (Goldmann and Galea, 2014). These correlations have remained true for this ongoing pandemic, as multiple studies had suggested that the prevalence of mental health disorders, such as depression and anxiety, has increased among the general population compared to pre-pandemic data (Ettman et al., 2020; Salari et al., 2020). For example, a cross-sectional study found that the prevalence of depression among US adults was 27.8% during the pandemic as compared to 8.5% before the pandemic (Ettman et al., 2020). These figures may be even higher in at-risk populations with additional stressors, as a previous review found the prevalence of depression to be as high as 45% in COVID-19 patients (J. Deng et al., 2020) and a survey found the prevalence of depression in front-line health care workers to be 50.4% in COVID-19 affected regions of China (J. Lai et al., 2020).
Apart from COVID-19 patients and health care workers, higher education students are another population that is particularly vulnerable to developing mental health disorders during this pandemic. Even under non-pandemic circumstances, university and college students can experience considerable anxiety and depression due to factors such as academic pressure and financial difficulties (Saleh et al., 2017). As shown in an international meta-analysis, the prevalence of depression among pre-pandemic university students worldwide was 30.6% (Ibrahim et al., 2013). This figure is substantially higher than the depression prevalence of 12.9% in the pre-pandemic, global population (Lim et al., 2018). As a direct result of the pandemic and its associated control measures, higher education students can expect to face worsened mental health challenges due to drastic deviations from their normal routines as they transition to an online learning environment. These challenges may be further exacerbated by social distancing guidelines, which deprive students of valuable in-person mental health resources and support services offered by their universities, as well as their family and friends. The resultant psychological distress may further develop into complications such as a decrease in self-esteem or self-efficacy (Saleh et al., 2017); if left unnoticed or untreated, these complications may potentially lead to severe consequences, such as suicidal ideations or other mental illnesses (Arria et al., 2009).
Despite the risk of increased prevalence of psychological disorders in higher education students, there is currently a lack of evidence synthesis regarding this topic. Therefore, we conducted a systematic review and meta-analysis to examine the prevalence of depressive symptoms, anxiety symptoms, and sleep disturbances in higher education students to better understand the impact of the COVID-19 pandemic on the mental health of this vulnerable population. We also aimed to identify possible risk factors that correlate with a higher prevalence of mental health issues in higher education students.
2. Methods
We conducted this systematic review and meta-analysis in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework (Moher et al., 2009) (see Table S1 for the PRISMA checklist) and followed recommendations from the Cochrane Handbook for Systematic Reviews of Interventions (Higgins and Green, 2008). This systematic review was prospectively registered on PROSPERO (Booth et al., 2012) (CRD42020192087).
2.1. Literature search
We searched the following databases from January 1st, 2020 to January 1st, 2021 for relevant studies: 1) MEDLINE, 2) EMBASE, 3) PubMed, 4) Web of Science, 5) Cumulative Index of Nursing and Allied Health Literature (CINAHL) and 6) APA PsycInfo. Moreover, we searched the following Chinese databases using a Chinese search strategy from January 1st, 2020 to January 1st, 2021: 1) Wanfang Data, 2) Wanfang Med Online, 3) China National Knowledge Infrastructure (CNKI), and 4) Chongqing VIP Information (CQVIP). The English and Chinese search strategies used for the database searches are appended in Table S2 and Table S3, respectively. In addition to the database searches, we hand-searched the reference sections of relevant reviews identified during the database search for relevant studies.
2.2. Eligibility criteria
Studies were included in the systematic review if they satisfied the following inclusion criteria: 1) sampled university or college students, including students enrolled in diploma, undergraduate/bachelor or graduate/doctorate studies in areas affected by COVID-19, and 2) reported the prevalence of depressive symptoms, anxiety symptoms and/or sleep disturbances. As medical and nursing students may be at greater risk for developing mental health issues from working in clinical environments and coming into close proximity with patients (Chandratre, 2020), we did not include studies that specifically sampled medical and nursing students to prevent possible overestimations of the overall prevalence. We also excluded studies that specifically defined students with known mental health disorders as their target populations.
We included all primary observational research studies, including longitudinal cohort, cross-sectional, and case-control studies with a sample size of ≥10 participants. We did not place limitations on the age or gender of the included students nor on the publications’ language or country of origin.
2.3. Study selection
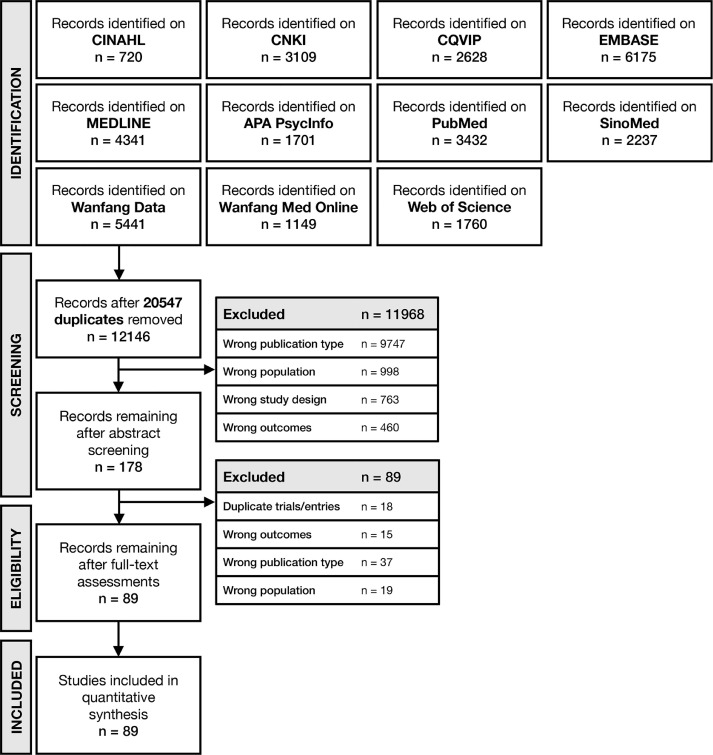
We screened titles and abstracts retrieved from the database search in duplicate using Rayyan (https://rayyan.qcri.org/) (Ouzzani et al., 2016). Articles deemed relevant by at least two reviewers, based on the above eligibility criteria, were entered into an in-duplicate full-text screening process. We recruited a senior author (JD) for arbitration when we encountered disagreements. Fig. 1 shows the PRISMA flow diagram of our study identification and selection processes (Liberati et al., 2009).
Fig. 1.
PRISMA flowchart for the identification and selection of observational studies.
Abbreviations: CINAHL Cumulative Index to Nursing and Allied Health Literature; CNKI Chinese National Knowledge Infrastructure; CQVIP Chongqing VIP Information.
2.4. Data extraction
We performed data extraction in duplicate using a standardized data extraction form developed a priori. The form included: 1) author names, 2) publication title, 3) publication date, 4) digital object identifier, 5) country of origin, 6) study design, 7) sample size, 8) demographic information of study participants, i.e., mean/median age, gender, study discipline and education level, 9) screening tools and cutoff values used for identifying the presence of depressive symptoms, anxiety symptoms and sleep disturbances, 10) prevalence of depressive symptoms, anxiety symptoms and/or sleep disturbances, and 11) relevant subgroup data. We made attempts to contact the principal investigators of studies with unclear or missing information to obtain relevant, unpublished data.
For longitudinal studies that reported the prevalence of depressive symptoms, anxiety symptoms and/or sleep disturbances at multiple time points, we only extracted the prevalence values at the earliest time point.
2.5. Quality assessment
We assessed the quality of our included studies using a modified version of the Newcastle-Ottawa Quality Assessment Scale adapted for cross-sectional studies (Modesti et al., 2016), which is similar in format to the scale used in previous meta-analyses (J. Deng et al., 2020; Pappa et al., 2020). The modified scale evaluated study quality based on five domains: 1) representativeness of the sample (the inclusion of all subjects or the use of random sampling), 2) sample size (justified using methods such as power analysis), 3) non-respondents (response rate is ≥80%), 4) valid measurement tools (appropriate screening tools used to evaluate depressive symptoms or anxiety symptoms), and 5) appropriate statistical analysis (appropriate and clearly described statistical tests). The total quality score ranged between 0 and 5; studies scoring ≥3 points were regarded as having a low risk of bias, while studies with <3 points were regarded as having a high risk of bias.
2.6. Statistical analysis
We conducted all statistical analyses using R 4.0.2 (https://www.r-project.org/). We performed random effect meta-analysis using the meta 4.12 library (https://cran.r-project.org/web/packages/meta/) (Fleiss, 1993). To avoid variance instability when the prevalence trends toward 0% or 100%, as well as to prevent confidence intervals (CIs) from extending beyond 0% and 100%, we transformed the prevalence values extracted from each study using the Freeman-Tukey double arcsine method for prevalence pooling (Barendregt et al., 2013). We then converted the results back to prevalence values with 95% CIs for ease of interpretation.
We used the Cochran's Q test, with a significance level of p<0.10, to assess the presence of heterogeneity as recommended by the Cochrane Handbook (Higgins et al., 2003). We then quantified heterogeneity using I2 statistics (Higgins et al., 2003; Higgins and Green, 2008). An I2 value ≥75% was considered to indicate serious heterogeneity, as recommended by the Cochrane Handbook (Higgins and Green, 2008).
2.7. Publication bias
We used funnel plots and Egger's regression tests to assess the presence of small study effects as an indication for publication bias (Egger et al., 1997; Higgins and Green, 2008).
2.8. Meta-regression
We performed meta-regression analyses to assess correlations between the pooled prevalence and study level covariates. We prospectively chose mean age and the date on which the study was conducted (expressed as the last day of the study duration as the number of months since January 1st, 2020) as our covariates of interest.
2.9. Subgroup analysis
As studies conducted before the pandemic have identified several factors that may impact mental health in higher education students, including gender (Ahern and Norris, 2011; Cruz et al., 2013; Shamsuddin et al., 2013), financial difficulties (Cooke et al., 2004; McCloud and Bann, 2019), level of social support (Alsubaie et al., 2019; Hefner and Eisenberg, 2009), education level (i.e., diploma vs. undergraduate vs. graduate) (Wyatt and Oswalt, 2013) and geographical regions (L. Gao et al., 2020; Lei et al., 2016; Sarokhani et al., 2013), we performed subgroup analyses by the following factors: 1) gender, 2) existence of financial difficulties, such as low income or poor financial backgrounds, 3) living alone vs. living with family and/or friends, 4) education level, and 5) by geographical region/country. In addition, we performed out-of-protocol subgroup analyses by years of undergraduate study, as undergraduate students made up a majority of our sample size.
We also performed subgroup analyses by different screening tools and cutoff values as well as validated vs. unvalidated screening tools to examine differences in prevalence values yielded by different screening tools.
2.10. Sensitivity analysis
We performed sensitivity analyses using the leave-one-out method. Studies were iteratively removed, one at a time, from the analysis, and the pooled prevalence and I2 of the remaining studies were calculated to identify single studies which severely affected the pooled prevalence or heterogeneity.
3. Results
3.1. Study characteristics
We included 89 studies (Amatori et al., 2020; Aslan et al., 2020; Aylie et al., 2020; Benham, 2020; Biber et al., 2020; Bourion-Bédès et al., 2021; Chang et al., 2020; Chen et al., 2020; Chi et al., 2020; B. Deng et al., 2020; C.-H. Deng et al., 2020; Dhar et al., 2020; Díaz-Jiménez et al., 2020; Ding and Hu, 2020; Dong, 2020; Dratva et al., 2020; Du et al., 2020; Essadek and Rabeyron, 2020; Fan and Yu, 2020a, 2020b; Fan et al., 2020; Fawaz and Samaha, 2020; Fu et al., 2021a; Gavurova et al., 2020; Ge et al., 2020; Ghazawy et al., 2020; Graupensperger et al., 2020; Gritsenko et al., 2020; Han et al., 2020; Islam et al., 2020; Jiang and Li, 2020; Ji et al., 2020; Khoshaim et al., 2020; A. Y.-K. Lai et al., 2020; Liang et al., 2020; Lian et al., 2020; Lin et al., 2020a; Lin and Xu, 2020; Liu, 2020; Li et al., 2020; L. Ma et al., 2020; Z. Ma et al., 2020a; Naser et al., 2020; Nurunnabi et al., 2020; Ozamiz-Etxebarria et al., 2020; Pavithra and Dheepak Sundar, 2020; Perz et al., 2020; Qiu et al., 2020; Ren et al., 2020; Rogowska et al., 2020a, 2020b; Rudenstine et al., 2020; Saddik et al., 2020; Salman et al., 2020; Sañudo et al., 2020; Sayeed et al., 2020; Scotta et al., 2020; Sundarasen et al., 2020; Tang et al., 2020; Tasnim et al., 2020; Thahir et al., 2020; Van Der Feltz-Cornelis et al., 2020; Verma, 2020; C. Wang et al., 2020a; Wang and Zhao, 2020a; S. Wang et al., 2020c; X. Wang et al., 2020; Wang, 2020; Y. Wang et al., 2020d; Z.-H. Wang et al., 2020a; Wathelet et al., 2020; B. B. Wu et al., 2020; T. H. Wu et al., 2020; Xiang et al., 2020; Xiao et al., 2020; Xia and Li, 2020; Xu and Li, 2020; X. J. Yang et al., 2020; Y. Y. Yang et al., 2020; Ye et al., 2020; Yi et al., 2020; Yue et al., 2020; B. Zhang et al., 2020; J. Zhang et al., 2020; L. L. Zhang et al., 2020; X. Y. Zhang et al., 2020; Y. Zhang et al., 2020; Zhao et al., 2020; Zhao, 2020) with 1,441,828 higher education students in our analysis (see Fig. 1). The characteristics of our included studies are tabulated in Table 1 . The median number of students with valid responses of the included studies was 1,172 (range 20 to 746,217), with a median male representation of 37.0% (range 9.9% to 67.2%). The median questionnaire response rate was 94.9% (range 1.2% to 100.0%).
Table 1.
Characteristics of Included Studies
| Study | Citation | Country | Study Design | Response Rate (%) | Sample Size (n) | Male (%) | Age (mean ± SD) | Screening Tools and Cutoff Values | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Depression | Anxiety | Sleep Disturbances | ||||||||
| 2020 Amatori | (Amatori et al., 2020) | Italy | Cross-Sectional | 64 | 159 | 58 | 23.0 ± 4.0 | PHQ-9 ≥ 5 | - | - |
| 2020 Aslan | (Aslan et al., 2020) | Turkey | Cross-Sectional | 3 | 358 | 42 | 23.0 | PHQ-8 ≥ 10 | GAD-7 ≥ 10 | - |
| 2020 Aylie | (Aylie et al., 2020) | Ethiopia | Cross-Sectional | 98 | 314 | 37 | 22.6 ± 2.8 | DASS-21D ≥ 10 | DASS-21A ≥ 8 | - |
| 2020 Benham | (Benham, 2020) | USA | Repeated Cross-Sectional | - | 450 (T1), 345 (T2) | 27 | 21.1 ± 4.4 (T1), 22.7 ± 6.0 (T2) | - | - | PSQI > 5 |
| 2020 Biber | (Biber et al., 2020) | USA | Cross-Sectional | 50 | 1640 | 39 | - | - | GAD-7 ≥ 5 | - |
| 2020 Bourion-Bédès | (Bourion-Bédès et al., 2021) | France | Cross-Sectional | - | 3936 | 29 | 21.7 ± 4.0 | - | GAD-7 ≥ 5 | - |
| 2020 Chang | (Chang et al., 2020) | China | Cross-Sectional | 91 | 3881 | 37 | 20a | PHQ-9 ≥ 5 | GAD-7 ≥ 5 | - |
| 2020 Chen | (Chen et al., 2020) | China | Cross-Sectional | 89 | 323489 | 40 | - | PHQ-9 ≥ 10 | - | - |
| 2020 Chi | (Chi et al., 2020) | China | Cross-Sectional | 96 | 2038 | 37 | 20.6 ± 1.9 | PHQ-9 ≥ 10 | SAS ≥ 50 | - |
| 2020 Deng A | (B. Deng et al., 2020b) | China | Cross-Sectional | 99 | 517 | 26 | - | - | SAS ≥ 50 | - |
| 2020 Deng B | (C.-H. Deng et al., 2020a) | China | Cross-Sectional | 96 | 1607 | 65 | - | DASS-21D ≥ 10 | DASS-21A ≥ 7 | - |
| 2020 Dhar | (Dhar et al., 2020) | Bangladesh | Cross-Sectional | - | 15543 | 67 | - | - | GAD-7 ≥ 5 | - |
| 2020 Díaz-Jiménez | (Díaz-Jiménez et al., 2020) | Spain | Cross-Sectional | 20 | 365 | 10 | 23.2 ± 6.2 | - | DASS-21A ≥ 8 | - |
| 2020 Ding | (Ding and Hu, 2020) | China | Cross-Sectional | 95 | 3055 | 46 | - | Custom Questionnaire | Custom Questionnaire | - |
| 2020 Dong | (Dong, 2020) | China | Cross-Sectional | 97 | 4085 | 23 | 18.9 ± 0.6 | SCL-90 (Depression Domain) ≥ 2 | SCL-90 (Anxiety Domain) ≥ 2 | - |
| 2020 Dratva | (Dratva et al., 2020) | Switzerland | Cross-Sectional | 18 | 2223 | 33 | 26.4 ± 5.6 | - | GAD-7 ≥ 10 | - |
| 2020 Du | (Du et al., 2020) | China, Ireland, Malaysia, Taiwan, South Korea, Netherlands, USA | Cross-Sectional | - | 2254 | 31 | 22.5 ± 5.5 | - | GAD-7 ≥ 10 | PSQI > 5 |
| 2020 Essadek | (Essadek and Rabeyron, 2020) | France | Cross-Sectional | 13 | 8004 | 33 | 21.7 | PHQ-9 ≥ 10 | GAD-7 ≥ 7 | - |
| 2020 Fan A | (Fan et al., 2020) | China | Cross-Sectional | 97 | 4148 | 27 | 20.6 ± 1.5 | - | SAS ≥ 50 | - |
| 2020 Fan B | (Fan and Yu, 2020a) | China | Cross-Sectional | 93 | 932 | 47 | - | - | - | PSQI > 7 |
| 2020 Fan C | (Fan and Yu, 2020b) | China | Longitudinal | - | 406 | - | - | - | SAS ≥ 50 | - |
| 2020 Fawaz | (Fawaz and Samaha, 2020) | Lebanon | Cross-Sectional | 84 | 520 | 39 | 21.0 ± 2.7 | DASS-21D ≥ 10 | DASS-21A ≥ 8 | - |
| 2020 Feltz-Cornelis | (Van Der Feltz-Cornelis et al., 2020) | UK | Cross-Sectional | 5 | 925 | 26 | 27.5 | PHQ-9 ≥ 10 | GAD-7 ≥ 10 | - |
| 2020 Fu | (Fu et al., 2021b) | China | Cross-Sectional | - | 89588 | 44 | - | - | GAD-7 ≥ 5 | - |
| 2020 Gavurova | (Gavurova et al., 2020) | Slovakia | Cross-Sectional | 84 | 1523 | 36 | - | PHQ-9 ≥ 5 | - | - |
| 2020 Ge | (Ge et al., 2020) | China | Cross-Sectional | 80 | 2009 | 49 | - | - | GAD-7 ≥ 7 | ISI > 14 |
| 2020 Ghazawy | (Ghazawy et al., 2020) | Egypt | Cross-Sectional | - | 1335 | 38 | - | DASS-21D ≥ 10 | DASS-21A ≥ 8 | - |
| 2020 Graupensperger | (Graupensperger et al., 2020) | USA | Cross-Sectional | 58 | 135 | 37 | 19.8 ± 1.4 | PROMIS-8D T-Score ≥ 55 | - | - |
| 2020 Gritsenko | (Gritsenko et al., 2020) | Russia, Belarus | Cross-Sectional | - | 939 | 19 | 21.8 ± 5.4 | FCV-19S | - | - |
| 2020 Han | (Han et al., 2020) | China | Cross-Sectional | 93 | 405 | 33 | - | DASS-21D ≥ 10 | DASS-21A ≥ 8 | - |
| 2020 Islam | (Islam et al., 2020) | Bangladesh | Cross-Sectional | 95 | 476 | 67 | - | PHQ-9 ≥ 5 | GAD-7 ≥ 5 | - |
| 2020 Ji | (Ji et al., 2020) | China | Cross-Sectional | 98 | 515 | 24 | - | - | - | PSQI ≥ 8 |
| 2020 Jiang | (Jiang and Li, 2020) | China | Cross-Sectional | 96 | 472 | 42 | - | - | SCL-90 (Anxiety Domain) ≥ 2 | - |
| 2020 Khoshaim | (Khoshaim et al., 2020) | Saudi Arabia | Cross-Sectional | 8 | 400 | 25 | - | - | SAS ≥ 45 | - |
| 2020 Lai | (A. Y.-K. Lai et al., 2020) | UK, USA | Cross-Sectional | - | 124 | 36 | - | - | - | ISI ≥ 15 |
| 2020 Li | (Li et al., 2020) | China | Cross-Sectional | 96 | 1000 | - | 21.8 ± 2.5 | - | SAS ≥ 50 | - |
| 2020 Lian | (Lian et al., 2020) | China | Cross-Sectional | 96 | 1437 | 55 | - | SCL-90 (Depression Domain) ≥ 2 | SCL-90 (Anxiety Domain) ≥ 2 | - |
| 2020 Liang | (Liang et al., 2020) | China | Cross-Sectional | 1 | 4164 | 52 | - | PHQ-9 ≥ 5 | - | - |
| 2020 Lin A | (Lin et al., 2020b) | China | Cross-Sectional | - | 625 | 35 | 20.2 ± 1.9 | CES-D ≥ 16 | - | - |
| 2020 Lin B | (Lin and Xu, 2020) | China | Cross-Sectional | 98 | 1297 | 44 | - | PHQ-9 ≥ 5 | GAD-7 ≥ 5 | - |
| 2020 Liu | (Liu, 2020) | China | Cross-Sectional | 96 | 191 | - | - | SCL-90 (Depression Domain) ≥ 2 | SCL-90 (Anxiety Domain) ≥ 2 | - |
| 2020 Ma A | (L. Ma et al., 2020) | China | Cross-Sectional | 97 | 516 | 53 | 20.8 ± 1.4 | SCL-90 (Depression Domain) ≥ 2 | SCL-90 (Anxiety Domain) ≥ 2 | - |
| 2020 Ma B | (Z. Ma et al., 2020b) | China | Cross-Sectional | 91 | 746217 | 44 | - | PHQ-9 ≥ 7 | GAD-7 ≥ 7 | - |
| 2020 Naser | (Naser et al., 2020) | Jordan | Cross-Sectional | - | 1165 | 46 | - | PHQ-9 ≥ 5 | GAD-7 ≥ 5 | - |
| 2020 Nurunnabi | (Nurunnabi et al., 2020) | China | Cross-Sectional | - | 559 | 40 | - | - | Custom Questionnaire | - |
| 2020 Ozamiz-Etxebarria | (Ozamiz-Etxebarria et al., 2020) | Spain | Longitudinal | 92 | 44 | 16 | 19.5 | - | GAD-7 ≥ 7 | - |
| 2020 Pavithra | (Pavithra and Dheepak Sundar, 2020) | India | Cross-Sectional | - | 396 | 46 | - | - | - | Custom Questionnaire |
| 2020 Perz | (Perz et al., 2020) | USA | Cross-Sectional | - | 237 | 27 | 30.3 ± 10.2 | - | GAD-7 ≥ 5 | - |
| 2020 Qiu | (Qiu et al., 2020) | China | Cross-Sectional | 98 | 1100 | 29 | - | - | GAD-7 ≥ 5 | - |
| 2020 Ren | (Ren et al., 2020) | China | Cross-Sectional | - | 4560 | 27 | 21.1 ± 1.4 | SDS ≥ 53 | - | - |
| 2020 Rogowska A | (Rogowska et al., 2020b) | Ukraine | Cross-Sectional | 98 | 1512 | 31 | - | PHQ-9 ≥ 10 | GAD-7 ≥ 10 | - |
| 2020 Rogowska B | (Rogowska et al., 2020a) | Poland | Cross-Sectional | 100 | 914 | 57 | 23.0 ± 2.6 | - | GAD-7 ≥ 10 | - |
| 2020 Rudenstine | (Rudenstine et al., 2020) | USA | Cross-Sectional | 62 | 1821 | 27 | -b | PHQ-9 ≥ 5 | GAD-7 ≥ 5 | - |
| 2020 Saddik | (Saddik et al., 2020) | UAE | Longitudinal | 93 | 1090 | 28 | 20.5 ± 2.3 | - | GAD-7 ≥ 10 | - |
| 2020 Salman | (Salman et al., 2020) | Pakistan | Cross-Sectional | - | 1134 | 30 | 21.7 ± 3.5 | PHQ-9 ≥ 10 | GAD-7 ≥ 10 | - |
| 2020 Sañudo | (Sañudo et al., 2020) | Spain | Cross-Sectional | 14 | 20 | 55 | 22.6 ± 3.4 | - | - | PSQI > 5 |
| 2020 Sayeed | (Sayeed et al., 2020) | Bangladesh | Cross-Sectional | - | 589 | 66 | - | DASS-21D ≥ 10 | DASS-21A ≥ 7 | - |
| 2020 Scotta | (Scotta et al., 2020) | Argentina | Cross-Sectional | - | 584 | 18 | 22.5 ± 6.3 | - | - | ISI ≥ 15 |
| 2020 Sundarasen | (Sundarasen et al., 2020) | Malaysia | Cross-Sectional | 93 | 983 | 34 | - | - | SAS ≥ 45 | - |
| 2020 Tang | (Tang et al., 2020) | China | Cross-Sectional | 69 | 2485 | 39 | 19.8 ± 1.6 | PHQ-9 ≥ 10 | - | - |
| 2020 Tasnim | (Tasnim et al., 2020) | Bangladesh | Cross-Sectional | 98 | 3331 | 59 | 21.4 ± 1.9 | DASS-21D > 14 | DASS-21A > 10 | Custom Questionnaire |
| 2020 Thahir | (Thahir et al., 2020) | Indonesia | Cross-Sectional | - | 1044 | 17 | 21.1 ± 2.4 | KADS-6 ≥ 6 | - | - |
| 2020 Verma | (Verma, 2020) | India | Cross-Sectional | - | 131 | 48 | - | PHQ-9 ≥ 5 | GAD-7 ≥ 5 | - |
| 2020 Wang A | (Wang, 2020) | China | Cross-Sectional | 100 | 3178 | 28 | - | - | HAM-A ≥ 7 | - |
| 2020 Wang B | (Wang and Zhao, 2020) | China | Cross-Sectional | 95 | 3611 | 40 | - | - | SAS ≥ 50 | - |
| 2020 Wang C | (Z.-H. Wang et al., 2020) | China | Cross-Sectional | 80 | 44447 | 45 | 21.0 ± 2.4 | CES-D ≥ 28 | SAS ≥ 50 | - |
| 2020 Wang D | (S. Wang et al., 2020c) | China | Cross-Sectional | - | 1365 | 40 | -c | - | SAS ≥ 50 | - |
| 2020 Wang E | (X. Wang et al., 2020) | China | Cross-Sectional | - | 3092 | 34 | - | - | GAD-7 ≥ 5 | SRSS ≥ 23 |
| 2020 Wang F | (C. Wang et al., 2020b) | China | Longitudinal | 31 | 1172 | 39 | - | - | SAS ≥ 50 | - |
| 2020 Wang G | (Y. Wang et al., 2020d) | China | Cross-Sectional | 89 | 3179 | 30 | - | PHQ-9 ≥ 5 | GAD-7 ≥ 5 | - |
| 2020 Wathelet | (Wathelet et al., 2020) | France | Cross-Sectional | 4 | 69054 | 28 | -d | BID-13 ≥ 16 | STAI ≥ 56 | - |
| 2020 Wu A | (B. B. Wu et al., 2020) | China | Cross-Sectional | 95 | 807 | 51 | - | SCL-90 (Depression Domain) ≥ 2 | SCL-90 (Anxiety Domain) ≥ 2 | - |
| 2020 Wu B | (T. H. Wu et al., 2020) | China | Cross-Sectional | - | 11787 | 43 | 20.5 ± 1.8 | - | GAD-7 ≥ 5 | - |
| 2020 Xia | (Xia and Li, 2020) | China | Cross-Sectional | 100 | 1186 | 17 | - | - | EAS ≥ 40 | - |
| 2020 Xiang | (Xiang et al., 2020) | China | Cross-Sectional | 60 | 1396 | 63 | 20.7 ± 1.8 | SDS ≥ 50 | SAS ≥ 50 | - |
| 2020 Xiao | (Xiao et al., 2020) | China | Cross-Sectional | 100 | 3966 | 40 | - | PHQ-9 ≥ 5 | - | - |
| 2020 Xu | (Xu and Li, 2020) | China | Cross-Sectional | 97 | 6891 | 31 | - | SDS ≥ 53 | SAS ≥ 50 | - |
| 2020 Yang A | (Y. Y. Yang et al., 2020) | China | Cross-Sectional | 93 | 1667 | 48 | 20.6 ± 2.0 | PQEEPH | PQEEPH | - |
| 2020 Yang B | (X. J. Yang et al., 2020) | China | Cross-Sectional | 94 | 4139 | 35 | - | PHQ-9 ≥ 5 | GAD-7 ≥ 5 | - |
| 2020 Ye | (Ye et al., 2020) | China | Cross-Sectional | 96 | 5532 | 56 | - | Custom Questionnaire | Custom Questionnaire | Custom Questionnaire |
| 2020 Yi | (Yi et al., 2020) | China | Cross-Sectional | 91 | 393 | 31 | 21.7 ± 0.9 | SDS ≥ 53 | SAS ≥ 50 | - |
| 2020 Yue | (Yue et al., 2020) | China | Cross-Sectional | 100 | 737 | 29 | - | - | Custom Questionnaire | - |
| 2020 Zhang A | (Y. Zhang et al., 2020) | China | Longitudinal | 100 | 66 | 38 | 20.7 ± 2.1 | DASS-21D ≥ 10 | DASS-21A ≥ 8 | PSQI > 5 |
| 2020 Zhang B | (L. L. Zhang et al., 2020) | China | Cross-Sectional | - | 7833 | 27 | 19.8 ± 1.9 | PHQ-9 ≥ 5 | GAD-7 ≥ 5 | - |
| 2020 Zhang C | (X. Y. Zhang et al., 2020) | China | Cross-Sectional | 97 | 1409 | 52 | - | SDS ≥ 53 | SAS ≥ 50 | - |
| 2020 Zhang D | (B. Zhang et al., 2020) | China | Repeated Cross-Sectional | 99 (T1), 98 (T2) | 2504 (T1), 2647 (T2) | 27 | - | - | Custom Questionnaire | Custom Questionnaire |
| 2020 Zhang E | (J. Zhang et al., 2020) | China | Cross-Sectional | 91 | 312 | 21 | 19.6 ± 2.0 | PHQ-9 ≥ 5 | - | - |
| 2020 Zhao A | (Zhao, 2020) | China | Cross-Sectional | - | 376 | 19 | - | Custom Questionnaire | Custom Questionnaire | - |
| 2020 Zhao B | (Zhao et al., 2020) | Korea, China, Japan | Cross-Sectional | 99 | 821 | 37 | 23.1 ± 4.8 | PHQ-9 ≥ 5 | - | - |
Cells containing “-“ indicate that the study author did not provide any relevant information for that column.
Abbreviations: USA United States of America, UAE United Arab Emirates, UK United Kingdom, SD standard deviation, PHQ-9 Patient Health Questionnaire-9, GAD-7 General Anxiety Disorder 7-item scale, SAS Zung Self-Rating Anxiety Scale, DASS-21D Depression Anxiety Stress Scales depression subscale, DASS-21A Depression Anxiety Stress Scales anxiety subscale, PSQI Pittsburgh Sleep Quality Index, ISI Insomnia Severity Index, PROMIS-8D Patient-Reported Outcomes Measurement Information System Depression-8, FCV-19S Fear of COVID-19 Scale, SCL-90 Symptom Checklist-90, HAM-A Hamilton Anxiety Rating Scale, CES-D Center for Epidemiologic Studies Depression Scale, EAS Existence of Anxiety Scale, PQEEPH Psychological Questionnaires for Emergent Events of Public Health, SRSS Self-Rating Scale of Sleep, KADS Kutcher Adolescent Depression Scale, BID-13 13-item Beck Depression Inventory, STAI State-Trait Anxiety Inventory, PHQ-8 Patient Health Questionnaire-8.
The interquartile range was 19-22.
The median age was 26.2 with a range of 18-77.
The age range was 18-28.
The median age was 20.0 with an interquartile range of 18-22.
Eighty-four studies (94.4%) were cross-sectional studies with two studies (2.2%) being repeated cross-sectional studies, while 5 studies (5.6%) were longitudinal studies. The majority of studies (51 studies, 57.3%) originated from China. Five studies (5.6%) originated from the United States of America (USA), 4 studies (4.5%) originated from Bangladesh, 3 studies (3.4%) originated from France, 3 studies (3.4%) originated from Spain, and 2 studies (2.2%) originated from India. We also included students from Jordan, Malaysia, Saudi Arabia, Italy, Ukraine, Lebanon, Indonesia, Poland, Turkey, United Arab Emirates (UAE), Argentina, Egypt, Pakistan, Ethiopia, Slovakia, Switzerland, and the United Kingdom (UK) with one study from each country. Lastly, there were 4 multinational studies that reported relevant data for students from Russia, Belarus, South Korea, China, Japan, Ireland, Malaysia, Taiwan, Netherlands, USA and UK.
3.2. Quality of included studies
The modified Newcastle-Ottawa quality score of the included studies is shown in Table 2 . The median quality score was 3 (range 1 to 5). Fifty-six studies (62.9%) were high quality studies with scores ≥3, while 33 studies were of low quality with scores <3. Major reasons for downgrading of quality ratings included the use of convenience sampling (instead of random sampling) and a lack of justification for target sample sizes (e.g. by using power calculations).
Table 2.
Quality ratings of included studies using the modified Newcastle-Ottawa Scale
| Study | Representativeness | Sample Size | Non-Respondents | Valid Measurement Tool | Valid Statistical Methods | Score |
|---|---|---|---|---|---|---|
| 2020 Amatori | * | * | 2 | |||
| 2020 Aslan | * | * | * | 3 | ||
| 2020 Aylie | * | * | * | * | * | 5 |
| 2020 Benham | * | * | 2 | |||
| 2020 Biber | * | * | 2 | |||
| 2020 Bourion-Bédès | * | * | 2 | |||
| 2020 Chang | * | * | * | 3 | ||
| 2020 Chen | * | * | * | 3 | ||
| 2020 Chi | * | * | * | 3 | ||
| 2020 Deng A | * | * | * | 3 | ||
| 2020 Deng B | * | * | * | 3 | ||
| 2020 Dhar | * | * | * | 3 | ||
| 2020 Díaz-Jiménez | * | * | 2 | |||
| 2020 Ding | * | * | * | 3 | ||
| 2020 Dong | * | * | * | 3 | ||
| 2020 Dratva | * | * | * | 3 | ||
| 2020 Du | * | * | 2 | |||
| 2020 Essadek | * | * | * | * | 4 | |
| 2020 Fan A | * | * | 2 | |||
| 2020 Fan B | * | * | 2 | |||
| 2020 Fan C | * | * | * | 3 | ||
| 2020 Fawaz | * | * | * | 3 | ||
| 2020 Feltz-Cornelis | * | * | * | 3 | ||
| 2020 Fu | * | * | 2 | |||
| 2020 Gavurova | * | * | * | 3 | ||
| 2020 Ge | * | * | * | 3 | ||
| 2020 Ghazawy | * | * | 2 | |||
| 2020 Graupensperger | * | * | * | * | 4 | |
| 2020 Gritsenko | * | * | * | 3 | ||
| 2020 Han | * | * | * | 3 | ||
| 2020 Islam | * | * | * | 3 | ||
| 2020 Ji | * | * | * | 3 | ||
| 2020 Jiang | * | * | * | 3 | ||
| 2020 Khoshaim | * | * | * | 3 | ||
| 2020 Lai | * | * | 2 | |||
| 2020 Li | * | * | * | * | 4 | |
| 2020 Lian | * | * | * | * | 4 | |
| 2020 Liang | * | * | 2 | |||
| 2020 Lin A | * | * | 2 | |||
| 2020 Lin B | * | * | * | 3 | ||
| 2020 Liu | * | * | 2 | |||
| 2020 Ma A | * | * | * | 3 | ||
| 2020 Ma B | * | * | * | * | 4 | |
| 2020 Naser | * | * | 2 | |||
| 2020 Nurunnabi | * | * | 2 | |||
| 2020 Ozamiz-Etxebarria | * | * | * | 3 | ||
| 2020 Pavithra | * | 1 | ||||
| 2020 Perz | * | * | 2 | |||
| 2020 Qiu | * | * | * | * | 4 | |
| 2020 Ren | * | * | * | 3 | ||
| 2020 Rogowska A | * | * | * | 3 | ||
| 2020 Rogowska B | * | * | * | 3 | ||
| 2020 Rudenstine | * | * | * | 3 | ||
| 2020 Saddik | * | * | * | * | 4 | |
| 2020 Salman | * | * | 2 | |||
| 2020 Sanudo | * | * | * | 3 | ||
| 2020 Sayeed | * | * | * | 3 | ||
| 2020 Scotta | * | * | 2 | |||
| 2020 Sundarasen | * | 1 | ||||
| 2020 Tang | * | * | * | 3 | ||
| 2020 Tasnim | * | * | 2 | |||
| 2020 Thahir | * | * | 2 | |||
| 2020 Verma | * | * | * | 3 | ||
| 2020 Wang A | * | * | 2 | |||
| 2020 Wang B | * | * | * | 3 | ||
| 2020 Wang C | * | * | * | 3 | ||
| 2020 Wang D | * | * | 2 | |||
| 2020 Wang E | * | * | 2 | |||
| 2020 Wang F | * | * | 2 | |||
| 2020 Wang G | * | * | * | 3 | ||
| 2020 Wathelet | * | * | 2 | |||
| 2020 Wu A | * | * | * | * | 4 | |
| 2020 Wu B | * | * | * | 3 | ||
| 2020 Xia | * | * | 2 | |||
| 2020 Xiang | * | * | 2 | |||
| 2020 Xiao | * | * | 2 | |||
| 2020 Xu | * | * | * | * | 4 | |
| 2020 Yang A | * | * | * | 3 | ||
| 2020 Yang B | * | * | * | 3 | ||
| 2020 Ye | * | * | * | 3 | ||
| 2020 Yi | * | * | 2 | |||
| 2020 Yue | * | * | 2 | |||
| 2020 Zhang A | * | * | * | * | 4 | |
| 2020 Zhang B | * | * | * | 3 | ||
| 2020 Zhang C | * | * | * | * | 4 | |
| 2020 Zhang D | * | * | * | 3 | ||
| 2020 Zhang E | * | * | * | 3 | ||
| 2020 Zhao A | * | * | * | 3 | ||
| 2020 Zhao B | * | * | * | 3 |
3.3. Prevalence of depressive symptoms
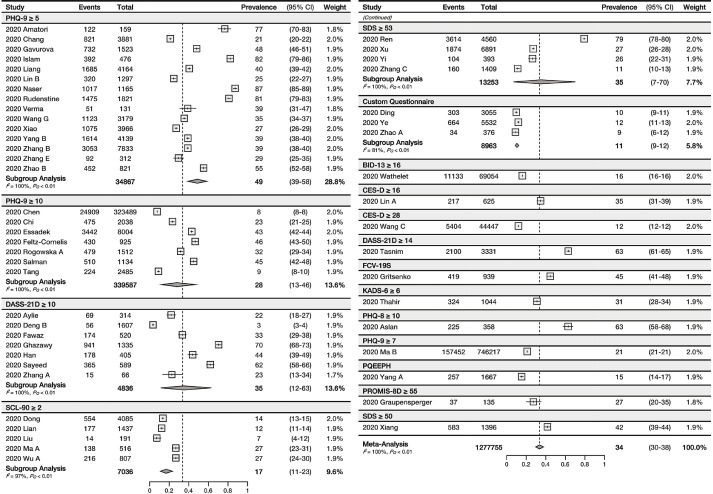
The pooled prevalence of depressive symptoms of 52 studies (n=1,277,755) was 34% (95% CI 30-38%). There was significant between-study heterogeneity (I2=100%, PQ<0.01).
3.4. Prevalence of anxiety symptoms
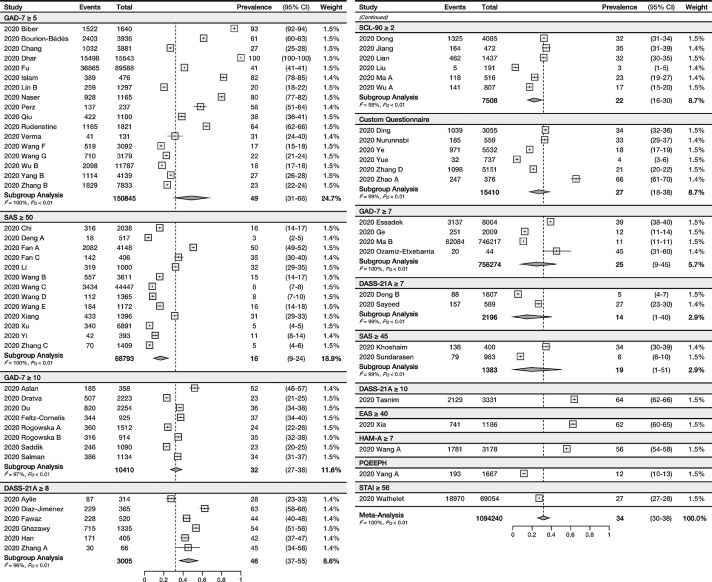
The pooled prevalence of anxiety symptoms of 69 studies (n=1,094,240) was 32% (95% CI 26-38%). There was significant between-study heterogeneity (I2=100%, PQ<0.01).
3.5. Prevalence of sleep disturbances
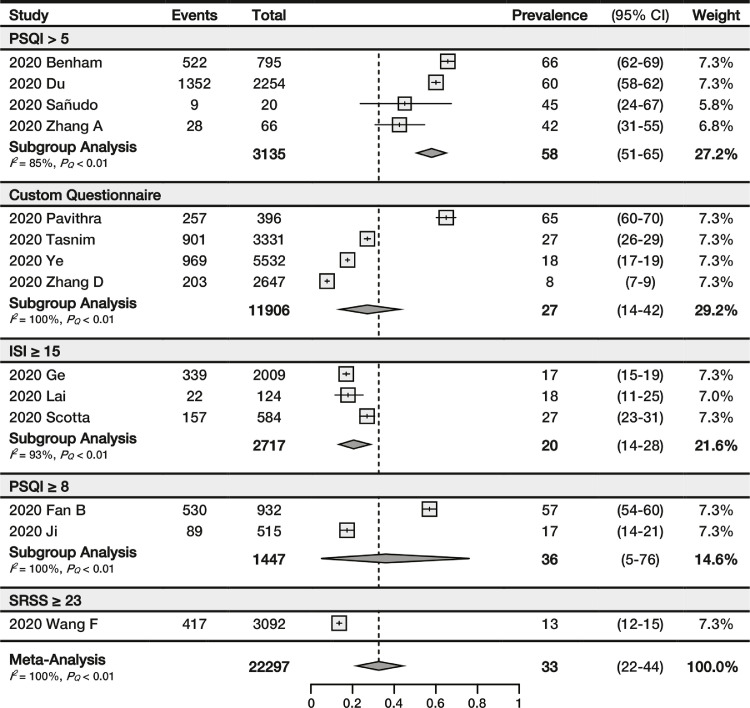
The prevalence of sleep disturbances was assessed in 14 studies (n=22,297) with a pooled prevalence of 33% (95% CI 22-44%). There was significant between-study heterogeneity (I2=100%, PQ<0.01).
3.6. Publication bias
There was no evidence of small study effects as an indication for publication bias in any of our study outcomes (Egger's test, p=0.42, p=0.46, p=0.45 for the prevalence of depressive symptoms, anxiety symptoms, and sleep disturbances, respectively; see Fig. S1).
3.7. Sensitivity analysis
The maximum effect of omitting a study on the pooled prevalence of depressive symptoms and pooled prevalence of anxiety symptoms was 1%, while the maximum effect was 3% for the pooled prevalence of sleep disturbances. Omitting single studies had no effect on the I2 value for any of our outcomes.
3.8. Meta-regression analysis
There were significant, positive correlations between study date and the pooled depressive symptoms and anxiety symptoms prevalences (p<0.01, β=0.06 [95% CI 0.02-0.09] for pooled depressive symptoms prevalence; p<0.01, β=0.04 [95% CI 0.02-0.07] for pooled anxiety symptoms prevalence). In addition, there was a significant, positive correlation between mean age and pooled depressive symptoms prevalence (p<0.01, β=0.07 [95% CI 0.02-0.12]). There were no other significant correlations observed in our meta-regression analyses.
3.9. Subgroup analysis
Results of the subgroup analysis of the prevalence of depressive symptoms, anxiety symptoms, and sleep disturbances by gender, financial situation, living arrangements, education level, undergraduate year of study, severity, and country is summarized and tabulated in Table 3 . Results of the subgroup analysis by screening tools and diagnostic criteria is listed in Fig. 2 - 4. Citations of studies included in each subgroup is listed in Table 4 .
Table 3.
Subgroup Analysis of Depression, Anxiety, and Sleep Disturbance Prevalence
| Depression | Anxiety | Sleep Disturbances | ||
|---|---|---|---|---|
| Gender | Male | 41%, 95% CI: 27-55% I2 = 100% |
37%, 95% CI: 21-53% I2 = 100% |
19%, 95% CI: 12-27% I2 = 72% |
| Female | 48%, 95% CI: 35-62% I2 = 100% |
44%, 95% CI: 34-55% I2 = 100% |
20%, 95% CI: 15-26% I2 = 74% |
|
| Financial Difficulties | Yes | 61%, 95% CI: 40-79% I2 = 100% |
49%, 95% CI: 25-73% I2 = 100% |
- |
| No | 49%, 95% CI: 39-60% I2 = 97% |
40%, 95% CI: 14-70% I2 = 100% |
- | |
| Living Alone | Yes | 52%, 95% CI: 28-76% I2 = 95% |
61%, 95% CI: 20-95% I2 = 100% |
- |
| No | 47%, 95% CI: 18-78% I2 = 99% |
44%, 95% CI: 15-77% I2 = 100% |
- | |
| Education Level | College | - | 6%, 95% CI: 2-11%a | - |
| Undergraduate | 32%, 95% CI: 22-44% I2 = 100% |
24%, 95% CI: 17-30% I2 = 100% |
30%, 95% CI: 18-44% I2 = 100% |
|
| Graduate | 25%, 95% CI: 0-73% I2 = 97% |
14%, 95% CI: 4-29% I2 = 98% |
20%, 95% CI 16-24%a | |
| Undergraduate Year of Study | Year 1 | 17%, 95% CI: 8-27% I2 = 99% |
19%, 95% CI: 12-27% I2 = 99% |
- |
| Year 2 | 21%, 95% CI: 9-35% I2 = 98% |
19%, 95% CI: 11-29% I2 = 99% |
- | |
| Year 3 | 24%, 95% CI: 12-38% I2 = 98% |
22%, 95% CI: 13-33% I2 = 99% |
- | |
| Year 4 | 29%, 95% CI: 15-45% I2 = 97% |
25%, 95% CI: 14-37% I2 = 97% |
- | |
| Severity | Mild | 23%, 95% CI: 21-26% I2 = 99% |
20%, 95% CI: 15-25% I2 = 100% |
- |
| Moderate | 13%, 95% CI: 8-19% I2 = 100% |
11%, 95% CI: 6-18% I2 = 100% |
- | |
| Severe | 8%, 95% CI: 5-12% I2 = 100% |
6%, 95% CI: 3-12% I2 = 100% |
- | |
| Country | China | 24%, 95% CI: 20-28% I2 = 100% |
23%, 95% CI: 18-28% I2 = 100% |
23%, 95% CI: 14-32% I2 = 99% |
| Bangladesh | 70%, 95% CI: 58-80% I2 = 98% |
73%, 95% CI: 31-99% I2 = 100% |
27%, 95% CI: 26-29%a | |
| France | 29%, 95% CI: 7-57% I2 = 100% |
42%, 95% CI: 26-60% I2 = 100% |
- | |
| USA | 55%, 95% CI: 8-97% I2 = 99% |
74%, 95% CI: 46-94% I2 = 100% |
66%, 95% CI: 62-69%a | |
| Russia | 53%, 95% CI: 49-57%a | - | - | |
| Belarus | 42%, 95% CI: 36-48%a | - | - | |
| Jordan | 87%, 95% CI: 85-89%a | 80%, 95% CI: 77-82%a | - | |
| Spain | - | 56%, 95% CI: 39-72% I2 = 79% |
45%, 95% CI: 24-67%a | |
| UAE | - | 23%, 95% CI: 20-25%a | - | |
| Pakistan | 45%, 95% CI: 42-48%a | 34%, 95% CI: 31-37%a | - | |
| Malaysia | - | 8%, 95% CI: 6-10%a | - | |
| India | 39%, 95% CI: 31-47%a | 31%, 95% CI: 24-40%a | 65%, 95% CI: 60-70%a | |
| Korea | 49%, 95% CI: 44-54%a | - | - | |
| Japan | 60%, 95% CI: 52-68%a | - | - | |
| Egypt | 70%, 95% CI: 68-73%a | 54%, 95% CI: 51-56%a | - | |
| Ethiopia | 22%, 95% CI: 18-27%a | 28%, 95% CI: 23-33%a | - | |
| Indonesia | 31%, 95% CI: 28-34%a | - | - | |
| Italy | 77%, 95% CI: 70-83%a | - | - | |
| Lebanon | 33%, 95% CI: 29-38%a | 44%, 95% CI: 40-48%a | - | |
| Slovakia | 72%, 95% CI: 69-74%a | - | - | |
| Turkey | 63%, 95% CI: 58-68%a | 52%, 95% CI: 46-57%a | - | |
| UK | 46%, 95% CI: 43-50%a | 37%, 95% CI: 34-40%a | - | |
| Ukraine | 32%, 95% CI: 29-34%a | 24%, 95% CI: 22-26%a | - | |
| Poland | - | 35%, 95% CI: 32-38%a | - | |
| Saudi Arabia | - | 34%, 95% CI: 30-39%a | - | |
| Switzerland | - | 23%, 95% CI: 21-25%a | - | |
| Argentina | - | - | 27%, 95% CI: 23-31%a | |
Cells containing “-“ indicate that no relevant subgroup analyses had been conducted.
Abbreviations: CI Confidence Interval, USA United States of America, UAE United Arab Emirates, UK United Kingdom
Only one study was included in this subgroup.
Fig. 2.
Forest plot for the pooling of depression prevalence. Studies were separated into subgroups based on the screening tool and cutoff values used for evaluating depression. The differences between subgroups were statistically significant (P<0.01).
Abbreviations: CI Confidence Interval; PHQ-9 Patient Health Questionnaire-9; DASS-21D Depression Anxiety Stress Scales, depression subscale; SCL-90 Symptom Checklist-90; SDS Zung Self-Rating Depression Scale; CES-D Center for Epidemiologic Studies Depression Scale; FCV-19S Fear of COVID-19 Scale; PQEEPH Psychological Questionnaires for Emergent Events of Public Health; PROMIS-8D Patient-Reported Outcomes Measurement Information System Depression-8, BID-13 13-item Beck Depression Inventory, KADS Kutcher Adolescent Depression Scale, PHQ-8 Patient Health Questionnaire-8
Fig. 4.
Forest plot for the pooling of sleep disturbances prevalence. Studies were separated into subgroups based on the screening tool and cutoff values used for evaluating sleep disturbances. The differences between subgroups were statistically significant (P<0.01).
Abbreviations: CI Confidence Interval; PSQI Pittsburgh Sleep Quality Index; ISI Insomnia Severity Index, SRSS Self-Rating Scale of Sleep.
Table 4.
Citation of Included Studies
Cells containing “-“ indicate that no relevant subgroup analyses had been conducted.
Abbreviations: NOS Modified Newcastle-Ottawa Scale
3.9.1. Screening tools for assessment of depressive symptoms
The results of the subgroup analysis by depressive symptoms screening tools and diagnostic criteria is listed in Fig. 2. The most commonly used diagnostic criteria was Patient Health Questionnaire-9 (PHQ-9)≥5 with a pooled prevalence of 49% based on 15 studies. Other commonly used criteria included PHQ-9≥10, which yielded a prevalence of 28% based on 7 studies; Depression Anxiety Stress Scales depression subscale (DASS-21D)≥10, which yielded a prevalence of 35% based on 7 studies; Symptom Checklist-90 (SCL-90) (depression domain)≥2, which yielded a prevalence of 17% based on 5 studies; and Zung Self-Rating Depression Scale (SDS)≥53, which yielded a prevalence of 35% based on 4 studies. There was no substantial reduction in heterogeneity for any of the subgroups. There were significant subgroup differences between different diagnostic criteria subgroups (p<0.01).
Forty-eight studies used validated screening tools and yielded a pooled depressive symptoms prevalence of 36% (95% CI 32-40%, I2=100%), which is similar to the overall pooled prevalence. Four studies used unvalidated, custom questionnaires. One of these studies (Y. Y. Yang et al., 2020) used the Psychological Questionnaire for Emergent Events of Public Health (PQEEPH) which was used in other mental health studies regarding COVID-19 (Duan et al., 2020; Qi et al., 2020), however we were not able to identify any relevant validation studies. Collectively, these four studies yielded a pooled depressive symptoms prevalence of 12% (95% CI 9-14%, I2=91%). There were significant subgroup differences between the prevalence estimates from validated versus unvalidated scales (p<0.01, see Fig. S2).
3.9.2. Screening tools for assessment of anxiety symptoms
For anxiety symptom screening tools (see Fig. 3 ), 17 studies used the criteria of General Anxiety Disorder-7 (GAD-7)≥5 and yielded a pooled prevalence of 49%. Other commonly used criteria include Zung Self-Rating Anxiety Scale (SAS)≥50, which yielded a prevalence of 16% based on 13 studies; GAD-7≥10, which yielded a prevalence of 32% based on 8 studies; SCL-90 (anxiety domain)≥2, which yielded a prevalence of 22% based on 6 studies; Depression Anxiety Stress Scales anxiety subscale (DASS-21A)≥8, which yielded a prevalence of 46% based on 6 studies; and GAD-7≥7, which yielded a prevalence of 25% based on 4 studies. There was no substantial reduction in heterogeneity for any of the subgroups. There were significant subgroup differences between different diagnostic criteria subgroups (p<0.01).
Fig. 3.
Forest plot for the pooling of anxiety prevalence. Studies were separated into subgroups based on the screening tool and cutoff values used for evaluating anxiety. The differences between subgroups were statistically significant (P<0.01).
Abbreviations: CI Confidence Interval; GAD-7 General Anxiety Disorder 7-item scale; SAS Zung Self-Rating Anxiety Scale; SCL-90 Symptom Checklist-90; DASS-21A Depression Anxiety Stress Scales, anxiety subscale; EAS Existence of Anxiety Scale; HAM-A Hamilton Anxiety Rating Scale; PQEEPH Psychological Questionnaires for Emergent Events of Public Health, STAI State-Trait Anxiety Inventory.
Sixty-one studies used validated screening tools and yielded a pooled anxiety symptoms prevalence of 32% (95% CI 26-39%, I2=100%), which is similar to the overall pooled prevalence. Eight studies used unvalidated, custom questionnaires, yielding a pooled prevalence of 29% (95% CI 19-41%). There were no significant subgroup differences between the two prevalence estimates (p=0.63, see Fig. S3).
3.9.3. Screening tools for assessment of sleep disturbances
The most commonly used criteria for evaluating sleep disturbances was Pittsburgh Sleep Quality Index (PSQI)>5, which yielded a pooled prevalence of 58% based on 4 studies, and Insomnia Severity Index (ISI)≥15, which yielded a pooled prevalence of 20% based on 3 studies. There were significant subgroup differences between different diagnostic criteria subgroups (p<0.01; see Fig. 4 ).
One study (conducted by Wang et al. (X. Wang et al., 2020)) used the Self-Rating Scale of Sleep (SRSS), which is a custom Chinese scale that have not been validated. Excluding the study by Wang et al. did not have a notable effect on the pooled prevalence (34%, according to the leave-one-out analysis).
3.9.4. Gender
Subgroup data by gender was reported by 17 studies for the prevalence of depressive symptoms, with a pooled prevalence of 48% for females and 41% for males (see Fig. S4). Twenty-two studies reported subgroup data by gender for the prevalence of anxiety symptoms, with a pooled prevalence of 44% for females and 37% for males (see Fig. S5). Four studies reported subgroup data by gender for the prevalence of sleep disturbances, with a pooled prevalence of 20% for females and 19% for males (see Fig. S6). There were no significant subgroup differences in any of the gender subgroups (P=0.45, 0.45, 0.82 for depressive symptoms, anxiety symptoms, and sleep disturbances, respectively).
3.9.5. Financial Situation
Four studies reported relevant subgroup data by financial situations for the prevalence of depressive symptoms with a pooled prevalence of 49% for students without financial difficulties and 61% for students with financial difficulties (see Fig. S7). Eight studies reported subgroup data for the prevalence of anxiety symptoms with a pooled prevalence of 40% for students without financial difficulties and 49% for students with financial difficulties (see Fig. S8). There were no significant subgroup differences in the aforementioned subgroup analyses (p=0.33 and p=0.64 for the prevalence of depressive symptoms and anxiety symptoms, respectively).
Only one study (Ge et al., 2020) reported subgroup data by students’ financial situation for the prevalence of sleep disturbances. Students with poor financial backgrounds had a reported prevalence of sleep disturbances of 19%, while students with high financial backgrounds had a reported prevalence of 16%.
3.9.6. Living Arrangement
Three studies reported relevant subgroup data by living arrangements for the prevalence of depressive symptoms with a pooled prevalence of 52% for students living alone and 47% for students living with family and/or friends (see Fig. S9). Six studies reported relevant subgroup data for the prevalence of anxiety symptoms with a pooled prevalence of 61% for students living alone and 44% for students living with family and/or friends (see Fig. S10). There were no significant subgroup differences in the aforementioned subgroup analyses (p=0.80 and p=0.55 for the prevalence of depressive symptoms and anxiety symptoms, respectively). No study reported subgroup data by students’ living arrangement for the prevalence of sleep disturbances.
3.9.7. Education Level
Twenty studies reported a pooled depressive symptoms prevalence of 25% for graduate students (see Fig. S11). For the prevalence of anxiety symptoms, 30 studies reported a pooled prevalence of 24% for undergraduate students, 4 studies reported a pooled prevalence of 14% for graduate students, while 1 study reported an anxiety symptoms prevalence of 6% for students enrolled in a diploma/college program (see Fig. S12). Eight studies reported a pooled prevalence of sleep disturbances of 30% for undergraduate students, and 1 study reported a sleep disturbance prevalence of 20% for graduate students (see Fig. S13). There were significant subgroup differences for the outcome of anxiety symptoms prevalence (p<0.01), however the subgroup difference was not significant for other outcomes (p=0.77 and p=0.13 for depressive symptoms and sleep disturbance prevalence, respectively).
3.9.8. Undergraduate Year of Study
Six studies reported subgroup data by undergraduate year of study for the prevalence of depressive symptoms. The pooled depressive symptoms prevalence was 17%, 21%. 24% and 29% for year 1, 2, 3, and 4 of undergraduate study, respectively (see Fig. S14). Thirteen studies reported relevant subgroup data for the prevalence of anxiety symptoms. The pooled anxiety symptoms prevalence was 19%, 19%, 22% and 25% for year 1, 2, 3, and 4 of undergraduate study, respectively (see Fig. S15). There were no significant subgroup differences in any of the aforementioned analyses (p=0.56 and p=0.83 for the prevalence of depressive symptoms and anxiety symptoms, respectively).
One study reported subgroup data by undergraduate year of study for the prevalence of sleep disturbances. The reported prevalence of sleep disturbances was 16%, 20%, 15%, and 19% for year 1, 2, 3, and 4 of undergraduate study, respectively.
3.9.9. Severity
Twenty-seven studies reported a pooled prevalence of 23%, 13%, and 8% for mild, moderate, and severe depressive symptoms, respectively (see Fig. S16). Thirty-three studies reported the pooled prevalence of mild, moderate, and severe anxiety symptoms to be 20%, 11%, and 7%, respectively. No study reported the prevalence of different severity of sleep disturbances (see Fig. S17).
3.9.10. Country
Thirty-two studies reported a pooled depressive symptoms prevalence of 24% from Chinese students. Three studies reported a pooled depressive symptoms prevalence of 70% for Bangladashi students, two studies reported a pooled depressive symptoms prevalence of 55% from American students, and two studies reported a pooled depressive symptoms prevalence of 29% for French students. No other country subgroups had more than one study for the prevalence of depressive symptoms (see Fig. S18); results from single-study subgroups can be found in Table 3.
Forty-two studies reported a pooled anxiety symptoms prevalence of 23% from Chinese students. Four studies reported a pooled anxiety symptoms prevalence of 73% for Bangladashi students, three studies reported a pooled prevalence of 74% for American students, three studies reported a pooled prevalence of 42% for French students, and two studies reported a pooled prevalence of 56% for Spanish students. No other country subgroups had more than one study for the prevalence of anxiety symptoms (see Fig. S19).
Seven studies reported a pooled sleep disturbance prevalence of 23% from Chinese students. There were no other country subgroups that had more than one study for the prevalence of sleep disturbances (see Fig. S20).
4. Discussion
This systematic review and meta-analysis provides the most up-to-date and comprehensive estimate of the prevalence of depressive symptoms, anxiety symptoms, and sleep disturbances in higher education students by pooling the data of 89 observational studies with a total of 1,441,828 students. The overall pooled prevalence of depressive symptoms, anxiety symptoms, and sleep disturbances among higher education students during the COVID-19 pandemic was determined to be 34%, 32%, and 33%, respectively.
4.1. Effect of geographical regions on prevalence
While our prevalence of depressive symptoms was not substantially greater compared to the pre-pandemic prevalence (30.6%) as reported in a previous meta-analysis conducted by Ibrahim et al. (Ibrahim et al., 2013), it must be noted that our study was largely based on data from Chinese students while Ibrahim et al.’s study contained mostly American, Canadian, and European students. This difference was likely due to the fact that the pandemic had a disproportionate impact on the Chinese population during the winter 2020 school year, while its impact on other student populations were not fully realized until the end of the school year. In many Asian countries, including China, mental illness and psychological disorders are commonly associated with distorted personality and moral defects (Liu et al., 2017; Parker et al., 2001; Subramaniam et al., 2017; Zhang et al., 2019); thus, students may be more reluctant to report symptoms of mental illness due to social stigma, leading to under-reporting (Guo et al., 2020; Sobowale et al., 2014). When comparing Ibraim et al.’s results with our subgroup data from non-Chinese countries, we observed substantially higher prevalence of depressive symptoms during the pandemic. For example, the prevalence of depressive symptoms in American students was found to be 55% in our study, which is substantially higher than the overall prevalence of 30.6% found in Ibrahim et al.’s study. Compared to other countries, the prevalence of depressive symptoms among Chinese higher education students (24%) was considerably lower (with the exception of Ethiopia, which reported a depressive symptoms prevalence of 22% based on 1 study). However, it still marks a substantial increase compared to results from a large-scale pre-pandemic observational study, which reported a depressive symptoms prevalence of 11.7% among Chinese university students (Chen et al., 2013).
Chinese students also reported a lower prevalence of anxiety symptoms compared to students from other countries at 23%, with the exception of Malaysian students (reported as 8% according to one study). Regardless, the prevalence of anxiety symptoms in Chinese students have surpassed the prevalence observed during the 2003 SARS epidemic, which was 9.5% based on data from three major universities in Beijing (Huang et al., 2003). The differences in the mental health of university students during COVID-19 compared to SARS is potentially due to the fact that COVID-19 cases are more prevalent—only 8,000 cumulative cases of SARS were reported in 2004 (World Health Organization, 2015), while over 46 million cases of COVID-19 have been reported thus far (Johns Hopkins University, 2021 COVID-19 Map). The popularity of social media and the spread of unverified online resources may have also contributed to the increased spread of misinformation (Cuan-Baltazar et al., 2020; Mian and Khan, 2020), leading to additional anxiety symptoms and stress compared to the SARS outbreak (J. Gao et al., 2020).
Overall, our results present a worrying trend of increased prevalence of mental health symptoms, i.e., depressive symptoms and anxiety symptoms, among higher education students during the COVID-19 pandemic. Additionally, our pooled prevalences may have been affected by an overrepresentation of Chinese students who might have under-reported symptoms of mental health symptoms. This study highlights the lack of mental health studies involving higher education students from non-Chinese countries and calls for further investigations into the mental health status of students from non-Chinese countries in order to provide a more comprehensive picture of the mental impact of COVID-19.
4.2. Effect of screening tools on prevalence
Our subgroup analyses showed that the screening tools and cutoff values used for assessing depressive symptoms, anxiety symptoms, and sleep disturbances had a significant impact on the resultant prevalence values. While a majority of the screening tool subgroups for the prevalence of depressive symptoms had similar pooled prevalences (e.g., 35%, 28%, and 35% for DASS-21D≥10, PHQ-9≥10, and SDS≥53, respectively), the PHQ-9 ≥5 subgroup yielded a substantially higher depressive symptoms prevalence compared to the other screening tool subgroups at 49%, while the SCL-90 subgroup reported a lower depressive symptoms prevalence at 17%. These observations were similar to those made in previous meta-analyses, which highlighted the finding that the depressive symptoms prevalence yielded by PHQ-9 ≥5 was approximately 30% higher compared to other screening tools (J. Deng et al., 2020). Future studies should consider using a higher cutoff value for PHQ-9, as previous studies have shown that using a cutoff value of 8-11 for PHQ-9 may increase the validity of the scale (Dunstan and Scott, 2019; Manea et al., 2012). In addition, the increased cutoff value will likely result in decreased prevalence of depressive symptoms as assessed using PHQ-9, potentially increasing agreement with results from other screening tools. Similarly, GAD-7 with a cutoff value of ≥5 yielded a substantially higher prevalence of anxiety symptoms compared to other anxiety scales. A cutoff of ≥10 may be more optimal in terms of balancing the scale's specificity and sensitivity (Johnson et al., 2019), as well as increasing agreement with other anxiety scales.
However, it must also be noted that there were substantial differences in the sample size of different screening tool subgroups that may have contributed to the differences in prevalence values. Subgroups with higher prevalences, such as the PHQ-9 ≥5 and GAD-7 ≥5 subgroups, included more studies and students compared to subgroups with lower prevalence estimates. Therefore, it is unclear whether the significant subgroup differences that we observed were valid. In addition, there was significant heterogeneity among the screening tool subgroups. This shows that results from individual studies in these subgroups are inconsistent, likely due to factors other than differences in screening tools and cutoff values. These factors should be considered when interpreting the results of our analysis. Addition of future studies may improve heterogeneity, increase the validity of the subgroup estimates, and reduce the observed subgroup differences (Richardson et al., 2019).
For the prevalence of sleep disturbances, the use of two different screening tools—PSQI and ISI—contributed to the significant subgroup differences that we observed. This finding was likely due to differences in the design of PSQI and ISI questionnaires. PSQI is generally preferred over ISI for assessing sleep disturbances as PSQI provides an overview of sleep quality by assessing multiple categories of sleep disturbances. In comparison, ISI is limited to insomnia and does not include items relevant to other forms of sleep disturbances (Smith and Wegener, 2003). This difference in measurement may explain the higher prevalence of sleep disturbances reported by the PSQI subgroups compared to the ISI subgroup, as ISI cannot assess as many forms of sleep disturbances as PSQI.
Several studies employed custom questionnaires or unvalidated Chinese questionnaires to assess the prevalence of mental health symptoms. The results reported by these studies must be interpreted with caution, as these studies did not publish their questionnaire items or did not report the reliability and validity of their screening tools. Future investigations should adopt validated scales with optimal cutoff values or online structured interviews to both increase the validity of their studies and the transparency of their methodology.
4.3. Interpretation of subgroup analyses and meta-regressions
We identified several factors that may have significant correlations with the prevalence of mental health symptoms in higher education students during the COVID-19 pandemic. First of all, the prevalence of depressive symptoms was found to be associated with the mean age of study participants. We speculated that this correlation may have been due to increased academic pressure in students of higher education levels (e.g., graduate students). Contrarily, we found that the prevalence of depressive symptoms in undergraduate students (32%) is higher compared to graduate students (25%); a similar trend exists for the prevalence of anxiety symptoms (24% versus 14%). This finding conflicts with results from a pre-pandemic meta-analysis, which found no significant differences between the depression prevalence of undergraduate and graduate students (Puthran et al., 2016). A cross-sectional study (Z.-H. Wang et al., 2020a), which was included in our analysis, suggested that this difference may be attributable to graduate students being more focused on their research work than the ongoing pandemic. We speculated that this difference may have also been due to differences in the ability to self-manage emotions between graduate and undergraduate students; graduate students may have developed better coping strategies compared to undergraduates, as graduate students typically have more experiences with stressful situations.
Within the undergraduate population (which constituted a considerable fraction of our study population), we found that the prevalence of depressive symptoms increased according to increasing undergraduate years. First-year undergraduate students, for example, had a depressive symptoms prevalence of 17% whereas fourth-year students had a depressive symptoms prevalence of 29%. This observation may explain the correlation we observed between mean age and the prevalence of depressive symptoms.
We also found correlations between the prevalences of depressive symptoms and anxiety symptoms and study date. In general, studies conducted during the later months of the pandemic (i.e., March and April) reported higher prevalence of depressive symptoms and anxiety symptoms compared to studies conducted in January and February. This difference suggests that the prevalence of depressive symptoms and anxiety symptoms may increase with time among higher education students, but this observation may also be attributable to the end-of-year examinations that typically take place during March and April in many institutions. Thus, future systematic reviews should examine whether this increasing trend continues into the new school year in September and October.
Similar to previous studies (Alsubaie et al., 2019; Cooke et al., 2004; Hefner and Eisenberg, 2009; McCloud and Bann, 2019), our findings demonstrate that financial situation, living arrangements (i.e., living alone vs. living with family and/or friends), and gender may have an impact on the prevalence of depressive symptoms and anxiety symptoms in higher education students during the ongoing pandemic. Students from poor financial backgrounds or had low income levels generally had higher prevalence of depressive symptoms and anxiety symptoms compared to students from advantaged financial backgrounds, while students who live alone had higher prevalence of depressive symptoms and anxiety symptoms compared to students living with family and/or friends. Additionally, female students were found to have higher prevalences of depressive symptoms and anxiety symptoms compared to male students. It must be noted that these findings were severely limited by low sample sizes and/or unbalanced covariate distribution. Furthermore, factors such as different screening tools may have confounded the subgroup analyses. As a result, we observed high uncertainties, large confidence intervals, and non-significant tests for subgroup differences (Richardson et al., 2019). These observations should be further investigated and corroborated in future studies with larger sample sizes and higher statistical powers.
4.4. Strengths and limitations
Since this systematic review and meta-analysis was conducted using data from the early stages of the pandemic, it has several notable limitations. First of all, we observed significant between-study heterogeneity that was not entirely accounted for by our subgroup analyses, sensitivity analyses, and meta-regressions. Secondly, our study participants were mostly made up of Chinese students, which severely limits the generalizability of our findings. Several Chinese studies may have also included the same population, as they were usually large-scale studies conducted within the same country. Lastly, there was a lack of data in our subgroup analyses resulting in unbalanced covariate distribution, as well high within-subgroup heterogeneity which reduced the effectiveness of our subgroup analyses.
Our study also has several strengths. Firstly, we did not detect signs of publication bias as shown by funnel plots and Egger's regression analyses. In addition, our results were not substantially impacted by our leave-one-out sensitivity analyses nor were they affected by the removal of studies using unvalidated screening tools. Lastly, a majority of our studies have a low risk of bias with high response rates, validated screening tools, and appropriate statistical methods.
4.5. Implications
To our knowledge, our study is the first knowledge synthesis project investigating the mental health effects of COVID-19 on higher education students. In response to the COVID-19 pandemic, many universities and colleges have suspended in-person lectures in favor of remote education. This shift has caused significant disruptions to the daily lives of many students, especially those living on campus and graduate students working to complete research projects or internships. For students who require counseling services offered by universities, this change may have deprived them of essential mental health screening and interventions needed to alleviate their psychological symptoms. These factors, combined with additional stressors such as quarantine and social distancing, have further disconnected students from their families and support systems (Zhai and Du, 2020). The increased prevalence of depressive symptoms and anxiety symptoms we observed during the pandemic may be attributed to a combination of disrupted academic routines, lack of in-person counselling, and physical and social isolation of university students.
Previous investigations into the mental health of students following traumatic events or natural disasters have suggested that the high prevalence of depressive symptoms and anxiety symptoms that we observed may be attributable to underlying psychological disorders, such as post-traumatic stress disorder (PTSD) or adjustment disorder (AD) (Li et al., 2021; Oh et al., 2019; Read et al., 2011). Adjustment disorder has been defined as a disproportionate, maladaptive response to a significant stressor, while PTSD is defined as a post-traumatic response characterized by re-experiencing traumatic events, avoidance of traumatic triggers, and heightened sense of current threat (Kazlauskas and Quero, 2020; Møller et al., 2020; World Health Organization, 2018). While our study did not directly evaluate the prevalence of suspected PTSD or AD, our observations of a prolonged mental health impact caused by the pandemic over a number of months is consistent with the possibility of a long-term underlying disorder such as PTSD and AD. These speculations need to be corroborated with future studies using specialized screening tools for assessing the severity of PTSD and AD symptomatology, such as the Adjustment Disorder–New Module 20 (ADNM-20) and the PTSD Symptom Scale (PSS) (Foa et al., 1993; Lorenz et al., 2016).
Given our findings, colleges and universities should implement long-term policies and programs to target the source of the students’ mental health issues. Despite pre-pandemic studies which showed that online learning may be just as effective as in-person lectures (Brockfeld et al., 2018; Paul and Jefferson, 2019; Porter et al., 2014), students may require time to adjust to this drastic shift in paradigm, especially within the context of the pandemic. The quality of pre-recorded videos for online course delivery, clarity in exam information, and regular online updates from universities/colleges are important factors which determine the students’ satisfaction with the institutional response to the COVID-19 pandemic (Browning et al., 2021). A previous letter to the editor by Zhai & Du also recommended that faculty members should offer virtual office hours for students to address academic concerns, while internship and research supervisors should implement alternative plans to make it easier for students to work and earn credits remotely (Zhai and Du, 2020).
Additionally, universities and colleges should continue to offer counseling services remotely via telephone- or Internet-based mental wellness programs (Brenes et al., 2015; Lattie et al., 2017, Lattie et al., 2019). Mental health interventions can be offered passively via information provision, or actively via automated or blended therapeutic interventions, such as wellness apps and mental health hotlines (Holmes et al., 2020). Providing students with virtual mindfulness or meditation sessions have also been shown to be effective in reducing anxiety and the sense of isolation during lockdown periods (Schlesselman et al., 2020). Our findings suggested that a majority of depressed or anxious students only experienced mild symptoms during the early stages of the pandemic. Therefore, timely and frequent mental health screening and interventions should be implemented to prevent these mild symptoms from progressing into more severe psychological disorders.
Funding sources/role of the funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The first and corresponding authors had full access to all data in the study and are solely responsible for the decision to submit for publication.
Financial disclosure
None.
Author Contributions (CRediT)
Jiawen Deng: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing - original draft, Writing - review & editing. Fangwen Zhou: Conceptualization, Data curation, Investigation, Resources, Validation, Writing - original draft, Writing - review & editing. Wenteng Hou: Data curation, Investigation, Writing - review & editing. Zachary Silver: Data curation, Investigation, Writing - review & editing. Chi Yi Wong: Data curation, Investigation, Writing - review & editing. Oswin Chang: Data curation, Investigation, Writing - review & editing. Anastasia Drakos: Data curation, Investigation, Writing - review & editing. Qi Kang Zuo: Data curation, Investigation, Writing - review & editing. Emma Huang: Data curation, Investigation, Writing - review & editing. All authors have given final approval for the final version of the manuscript to be submitted for publication.
Declaration of Competing Interests
The authors declare no conflict of interest.
Acknowledgements
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2021.113863.
Appendix. Supplementary materials
References
- Ahern N.R., Norris A.E. Examining factors that increase and decrease stress in adolescent community college students. J. Pediatr. Nurs. 2011;26:530–540. doi: 10.1016/j.pedn.2010.07.011. [DOI] [PubMed] [Google Scholar]
- Alsubaie M.M., Stain H.J., Webster L.A.D., Wadman R. The role of sources of social support on depression and quality of life for university students. Int. J. Adolesc. Youth. 2019;24:484–496. doi: 10.1080/02673843.2019.1568887. [DOI] [Google Scholar]
- Amatori S., Donati Zeppa S., Preti A., Gervasi M., Gobbi E., Ferrini F., Rocchi M.B.L., Baldari C., Perroni F., Piccoli G., Stocchi V., Sestili P., Sisti D. Dietary Habits and Psychological States during COVID-19 Home Isolation in Italian College Students: The Role of Physical Exercise. Nutrients. 2020;12 doi: 10.3390/nu12123660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria A.M., O'Grady K.E., Caldeira K.M., Vincent K.B., Wilcox H.C., Wish E.D. Suicide ideation among college students: a multivariate analysis. Arch. Suicide Res. 2009;13:230–246. doi: 10.1080/13811110903044351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aslan I., Ochnik D., Çınar O. Exploring Perceived Stress among Students in Turkey during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17238961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aylie N.S., Mekonen M.A., Mekuria R.M. The Psychological Impacts of COVID-19 Pandemic Among University Students in Bench-Sheko Zone, South-west Ethiopia: A Community-based Cross-sectional Study. Psychol. Res. Behav. Manag. 2020;13:813–821. doi: 10.2147/PRBM.S275593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barendregt J.J., Doi S.A., Lee Y.Y., Norman R.E., Vos T. Meta-analysis of prevalence. J. Epidemiol. Community Health. 2013;67:974–978. doi: 10.1136/jech-2013-203104. [DOI] [PubMed] [Google Scholar]
- Barnett M.L., Mehrotra A., Landon B.E. Covid-19 and the Upcoming Financial Crisis in Health Care. NEJM Catalyst Innovations in Care Delivery. 2020 doi: 10.1056/CAT.20.0153. [DOI] [Google Scholar]
- Bartik A.W., Bertrand M., Cullen Z., Glaeser E.L., Luca M., Stanton C. The impact of COVID-19 on small business outcomes and expectations. Proc. Natl. Acad. Sci. U. S. A. 2020;117:17656–17666. doi: 10.1073/pnas.2006991117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benham G. Stress and sleep in college students prior to and during the COVID-19 pandemic. Stress Health. 2020 doi: 10.1002/smi.3016. [DOI] [PubMed] [Google Scholar]
- Biber D.D., Melton B., Czech D.R. The impact of COVID-19 on college anxiety, optimism, gratitude, and course satisfaction. J Am. Coll. Health. 2020:1–6. doi: 10.1080/07448481.2020.1842424. [DOI] [PubMed] [Google Scholar]
- Booth A., Clarke M., Dooley G., Ghersi D., Moher D., Petticrew M., Stewart L. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Syst. Rev. 2012;1:2. doi: 10.1186/2046-4053-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourion-Bédès S., Tarquinio C., Batt M., Tarquinio P., Lebreuilly R., Sorsana C., Legrand K., Rousseau H., Baumann C. Psychological impact of the COVID-19 outbreak on students in a French region severely affected by the disease: results of the PIMS-CoV 19 study. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenes G.A., Danhauer S.C., Lyles M.F., Hogan P.E., Miller M.E. Telephone-Delivered Cognitive Behavioral Therapy and Telephone-Delivered Nondirective Supportive Therapy for Rural Older Adults With Generalized Anxiety Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2015;72:1012–1020. doi: 10.1001/jamapsychiatry.2015.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockfeld T., Müller B., de Laffolie J. Video versus live lecture courses: a comparative evaluation of lecture types and results. Med. Educ. Online. 2018;23 doi: 10.1080/10872981.2018.1555434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning M.H.E.M., Larson L.R., Sharaievska I., Rigolon A., McAnirlin O., Mullenbach L., Cloutier S., Vu T.M., Thomsen J., Reigner N., Metcalf E.C., D'Antonio A., Helbich M., Bratman G.N., Alvarez H.O. Psychological impacts from COVID-19 among university students: Risk factors across seven states in the United States. PLoS One. 2021;16 doi: 10.1371/journal.pone.0245327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandratre S. Medical Students and COVID-19: Challenges and Supportive Strategies. Journal of Medical Education and Curricular Development. 2020;7 doi: 10.1177/2382120520935059. 238212052093505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang J., Yuan Y., Wang D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Journal of Southern Medical University. 2020;40:171–176. doi: 10.12122/j.issn.1673-4254.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Wang L., Qiu X.H., Yang X.X., Qiao Z.X., Yang Y.J., Liang Y. Depression among Chinese university students: prevalence and socio-demographic correlates. PLoS One. 2013;8:e58379. doi: 10.1371/journal.pone.0058379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R.-N., Liang S.-W., Peng Y., Li X.-G., Chen J.-B., Tang S.-Y., Zhao J.-B. Mental health status and change in living rhythms among college students in China during the COVID-19 pandemic: A large-scale survey. J. Psychosom. Res. 2020;137 doi: 10.1016/j.jpsychores.2020.110219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi X., Becker B., Yu Q., Willeit P., Jiao C., Huang L., Hossain M.M., Grabovac I., Yeung A., Lin J., Veronese N., Wang J., Zhou X., Doig S.R., Liu X., Carvalho A.F., Yang L., Xiao T., Zou L., Fusar-Poli P., Solmi M. Prevalence and Psychosocial Correlates of Mental Health Outcomes Among Chinese College Students During the Coronavirus Disease (COVID-19) Pandemic. Front. Psychiatry. 2020;11:803. doi: 10.3389/fpsyt.2020.00803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke R., Barkham M., Audin K., Bradley M., Davy J. Student debt and its relation to student mental health. Journal of Further and Higher Education. 2004;28:53–66. doi: 10.1080/0309877032000161814. [DOI] [Google Scholar]
- Cruz S.Y., Fabián C., Pagán I., Ríos J.L., González A.M., Betancourt J., González M.J., Rivera-Soto W.T., Palacios C. Physical activity and its associations with sociodemographic characteristics, dietary patterns, and perceived academic stress in students attending college in Puerto Rico. P. R. Health Sci. J. 2013;32:44–50. [PubMed] [Google Scholar]
- Cuan-Baltazar J.Y., Muñoz-Perez M.J., Robledo-Vega C., Pérez-Zepeda M.F., Soto-Vega E. Misinformation of COVID-19 on the Internet: Infodemiology Study. JMIR Public Health Surveill. 2020;6:e18444. doi: 10.2196/18444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng C.-H., Wang J.-Q., Zhu L.-M., Liu H.-W., Guo Y., Peng X.-H., Shao J.-B., Xia W. Association of Web-Based Physical Education With Mental Health of College Students in Wuhan During the COVID-19 Outbreak: Cross-Sectional Survey Study. J. Med. Internet Res. 2020;22:e21301. doi: 10.2196/21301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng B., Ai Y.T., Hu H. Anxiety and influencing factors of undergraduates in Wuhan during the outbreak of coronavirus disease 2019. Medical Journal of Wuhan University. 2020;42(3):1–4. doi: 10.14188/j.1671-8852.2020.0357. [DOI] [Google Scholar]
- Deng J., Zhou F., Hou W., Silver Z., Wong C.Y., Chang O., Huang E., Zuo Q.K. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann. N. Y. Acad. Sci. 2020;1486(1) doi: 10.1111/nyas.14506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhar B.K., Ayittey F.K., Sarkar S.M. Impact of COVID-19 on Psychology among the University Students. Glob Chall. 2020 doi: 10.1002/gch2.202000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Díaz-Jiménez R.M., Ph.. Caravaca-Sánchez, F. Ph.., Martín-Cano M.C., Ph.. De la Fuente-Robles, Y.M. Ph.. Anxiety levels among social work students during the COVID-19 lockdown in Spain. Soc. Work Health Care. 2020;59:681–693. doi: 10.1080/00981389.2020.1859044. [DOI] [PubMed] [Google Scholar]
- Ding M.J., Hu C.F. [Study on the Influence of the Epidemic Situation of COVID-19 on the Psychological Behavior of College Students] Journal of Jiangsu Ocean University (Humanities & Social Sciences Edition) 2020;18:129–140. doi: 10.3969/j.issn.2096-8256.2020.02.016. [DOI] [Google Scholar]
- Dong X.L. Influence study of COVID-2019 on mental health of normal college students. Xin Li Yue Kan (PSY) 2020;15:37–39. doi: 10.19738/j.cnki.psy.2020.20.013. [DOI] [Google Scholar]
- Dratva J., Zysset A., Schlatter N., von Wyl A., Huber M., Volken T. Swiss University Students’ Risk Perception and General Anxiety during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17207433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan H., Yan L., Ding X., Gan Y., Kohn N., Wu J. Impact of the COVID-19 pandemic on mental health in the general Chinese population: Changes, predictors and psychosocial correlates. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du C., Zan M.C.H., Cho M.J., Fenton J.I., Hsiao P.Y., Hsiao R., Keaver L., Lai C.-C., Lee H., Ludy M.-J., Shen W., Swee W.C.S., Thrivikraman J., Tseng K.-W., Tseng W.-C., Tucker R.M. Increased Resilience Weakens the Relationship between Perceived Stress and Anxiety on Sleep Quality: A Moderated Mediation Analysis of Higher Education Students from 7 Countries. Clocks Sleep. 2020;2:334–353. doi: 10.3390/clockssleep2030025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunstan D.A., Scott N. Clarification of the cut-off score for Zung's self-rating depression scale. BMC Psychiatry. 2019;19:177. doi: 10.1186/s12888-019-2161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essadek A., Rabeyron T. Mental health of French students during the Covid-19 pandemic. J. Affect. Disord. 2020;277:392–393. doi: 10.1016/j.jad.2020.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairlie R. The impact of COVID-19 on small business owners: Evidence from the first 3 months after widespread social-distancing restrictions. J Econ Manag Strategy. 2020;19(4) doi: 10.1111/jems.12400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan J.Q., Yu J.J. Status quo of sleep quality and stress load of students from a college during the coronavirus disease 2019 pandemic. Journal of Environmental and Occupational Medicine. 2020;37:862–866. doi: 10.13213/j.cnki.jeom.2020.20131. [DOI] [Google Scholar]
- Fan J.Q., Yu J.J. Role of solution-focused intervention in improving mood of college students during the coronavirus disease 2019 pandemic - A study in a university of Hangzhou. Journal of Environmental and Occupational Medicine. 2020;37:858–866. doi: 10.13213/j.cnki.jeom.2020.20130. [DOI] [Google Scholar]
- Fan Y.H., Wang J.H., Jia X.L., Liu X.X., Song Y.L., Zhang L.L. The role of mental problem evaluation and intervention in university or college students kept at home due to serious Corona Virus Disease-2019 epidemic during high education. Pharmaceutical Care and Research. 2020;20:81–91. doi: 10.5428/pcar20200201. [DOI] [Google Scholar]
- Fawaz M., Samaha A. E-learning: Depression, anxiety, and stress symptomatology among Lebanese university students during COVID-19 quarantine. Nurs. Forum. 2020 doi: 10.1111/nuf.12521. [DOI] [PubMed] [Google Scholar]
- Fleiss J.L. The statistical basis of meta-analysis. Stat. Methods Med. Res. 1993;2:121–145. doi: 10.1177/096228029300200202. [DOI] [PubMed] [Google Scholar]
- Foa E.B., Riggs D.S., Dancu C.V., Rothbaum B.O. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J. Trauma. Stress. 1993;6:459–473. doi: 10.1002/jts.2490060405. [DOI] [Google Scholar]
- Fu W., Yan S., Zong Q., Anderson-Luxford D., Song X., Lv Z., Lv C. Mental health of college students during the COVID-19 epidemic in China. J. Affect. Disord. 2021;280:7–10. doi: 10.1016/j.jad.2020.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15 doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao L., Xie Y., Jia C., Wang W. Prevalence of depression among Chinese university students: a systematic review and meta-analysis. Sci. Rep. 2020;10:15897. doi: 10.1038/s41598-020-72998-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavurova B., Ivankova V., Rigelsky M. Relationships between Perceived Stress, Depression and Alcohol Use Disorders in University Students during the COVID-19 Pandemic: A Socio-Economic Dimension. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17238853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge F., Zhang D., Wu L., Mu H. Predicting Psychological State Among Chinese Undergraduate Students in the COVID-19 Epidemic: A Longitudinal Study Using a Machine Learning. Neuropsychiatr. Dis. Treat. 2020;16:2111–2118. doi: 10.2147/NDT.S262004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghazawy E.R., Ewis A.A., Mahfouz E.M., Khalil D.M., Arafa A., Mohammed Z., Mohammed E.-N.F., Hassan E.E., Abdel Hamid S., Ewis S.A., Mohammed A.E.-N.S. Psychological impacts of COVID-19 pandemic on the university students in Egypt. Health Promot. Int. 2020 doi: 10.1093/heapro/daaa147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldmann E., Galea S. Mental health consequences of disasters. Annu. Rev. Public Health. 2014;35:169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- Graupensperger S., Benson A.J., Kilmer J.R., Evans M.B. Social (Un)distancing: Teammate Interactions, Athletic Identity, and Mental Health of Student-Athletes During the COVID-19 Pandemic. J. Adolesc. Health. 2020;67:662–670. doi: 10.1016/j.jadohealth.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gritsenko V., Skugarevsky O., Konstantinov V., Khamenka N., Marinova T., Reznik A., Isralowitz R. COVID 19 Fear, Stress, Anxiety, and Substance Use Among Russian and Belarusian University Students. Int. J. Ment. Health Addict. 2020:1–7. doi: 10.1007/s11469-020-00330-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J., Meng D., Ma X., Zhu L., Yang L., Mu L. The impact of bedtime procrastination on depression symptoms in Chinese medical students. Sleep Breath. 2020;24:1247–1255. doi: 10.1007/s11325-020-02079-0. [DOI] [PubMed] [Google Scholar]
- Han T., Ma W.D., Gong H., Hu Y.C., Zhang Y., Zhang C.Y., Yao Z.H., Fan Y.J., Zheng Y., Wang C.X. Investigation and analysis of negative emotion among university students during home quarantine of COVID-19. Journal of Xi'an Jiaotong University (Medical Sciences) 2020:1–11. [Google Scholar]
- Hefner J., Eisenberg D. Social support and mental health among college students. Am. J. Orthopsychiatry. 2009;79:491–499. doi: 10.1037/a0016918. [DOI] [PubMed] [Google Scholar]
- Higgins J.P.T., Green S. Wiley; New Jersey: 2008. Cochrane Handbook for Systematic Reviews of Interventions. [Google Scholar]
- Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Silver Cohen, R. Everall, I. Ford, T. John, A. Kabir, T. King, K. Madan, I. Michie, S. Przybylski, A.K. Shafran, R. Sweeney, A. Worthman, C.M. Yardley, L. Cowan, K. Cope, C. Hotopf, M. Bullmore, E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Dang W., Liu Z. Psychosocial aspects in three universities during SARS epidemic in Beijing. Chinese Mental Health Journal. 2003;17:521–523. [Google Scholar]
- Ibrahim A.K., Kelly S.J., Adams C.E., Glazebrook C. A systematic review of studies of depression prevalence in university students. J. Psychiatr. Res. 2013;47:391–400. doi: 10.1016/j.jpsychires.2012.11.015. [DOI] [PubMed] [Google Scholar]
- Islam M.A., Barna S.D., Raihan H., Khan M.N.A., Hossain M.T. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: A web-based cross-sectional survey. PLoS One. 2020;15 doi: 10.1371/journal.pone.0238162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang R.C., Li A.M. Mental health status and its influencing factors of college students in Anhui province during the coronavirus disease 2019 pandemic. Journal of Environmental and Occupational Medicine. 2020;37:867–871. doi: 10.13213/j.cnki.jeom.2020.20171. [DOI] [Google Scholar]
- Ji K., Liu L., Wang P., Huang L.L., Xie D., Lu Y.J. Sleep quality and mental health of college students studying at home. Modern Preventive Medicine. 2020;47:3742–3763. [Google Scholar]
- Johns Hopkins University, 2021 COVID-19 Map [WWW Document]. Johns Hopkins Coronavirus Resource Center. URL https://coronavirus.jhu.edu/map.html (accessed 7.7.20).
- Johnson S.U., Ulvenes P.G., Øktedalen T., Hoffart A. Psychometric Properties of the General Anxiety Disorder 7-Item (GAD-7) Scale in a Heterogeneous Psychiatric Sample. Front. Psychol. 2019;10:1713. doi: 10.3389/fpsyg.2019.01713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazlauskas E., Quero S. Adjustment and coronavirus: How to prepare for COVID-19 pandemic-related adjustment disorder worldwide? Psychol. Trauma. 2020;12:S22–S24. doi: 10.1037/tra0000706. [DOI] [PubMed] [Google Scholar]
- Khatatbeh M. Efficacy of Nationwide Curfew to Encounter Spread of COVID-19: A Case From Jordan. Front Public Health. 2020;8:394. doi: 10.3389/fpubh.2020.00394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoshaim H.B., Al-Sukayt A., Chinna K., Nurunnabi M., Sundarasen S., Kamaludin K., Baloch G.M., Hossain S.F.A. Anxiety Level of University Students During COVID-19 in Saudi Arabia. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.579750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai A.Y.-K., Lee L., Wang M.-P., Feng Y., Lai T.T.-K., Ho L.-M., Lam V.S.-F., Ip M.S.-M., Lam T.-H. Mental Health Impacts of the COVID-19 Pandemic on International University Students, Related Stressors, and Coping Strategies. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.584240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lattie E.G., Duffecy J.L., Mohr D.C., Kashima K. Development and Evaluation of an Online Mental Health Program for Medical Students. Acad. Psychiatry. 2017;41:642–645. doi: 10.1007/s40596-017-0726-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lattie E.G., Kashima K., Duffecy J.L. An open trial of internet-based cognitive behavioral therapy for first year medical students. Internet Interv. 2019;18 doi: 10.1016/j.invent.2019.100279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei X.-Y., Xiao L.-M., Liu Y.-N., Li Y.-M. Prevalence of Depression among Chinese University Students: A Meta-Analysis. PLoS One. 2016;11 doi: 10.1371/journal.pone.0153454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang S.-W., Chen R.-N., Liu L.-L., Li X.-G., Chen J.-B., Tang S.-Y., Zhao J.-B. The Psychological Impact of the COVID-19 Epidemic on Guangdong College Students: The Difference Between Seeking and Not Seeking Psychological Help. Front. Psychol. 2020;11:2231. doi: 10.3389/fpsyg.2020.02231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lian X., Tan X., Zhang J.H. [Investigation of College Students’ Psychological Problems During the Novel Coronavirus Pneumonia Epidemic and Research on Intervention Countermeasures] J. Higher Educ. 2020:33–40. [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim G.Y., Tam W.W., Lu Y., Ho C.S., Zhang M.W., Ho R.C. Prevalence of Depression in the Community from 30 Countries between 1994 and 2014. Sci. Rep. 2018;8:2861. doi: 10.1038/s41598-018-21243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J., Guo T., Becker B., Yu Q., Chen S.-T., Brendon S., Hossain M.M., Cunha P.M., Soares F.C., Veronese N., Yu J.J., Grabovac I., Smith L., Yeung A., Zou L., Li H. Depression is Associated with Moderate-Intensity Physical Activity Among College Students During the COVID-19 Pandemic: Differs by Activity Level, Gender and Gender Role. Psychol. Res. Behav. Manag. 2020;13:1123–1134. doi: 10.2147/PRBM.S277435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin X.G., Xu J.Q. Influence of physical exercise on mental health of college students during the epidemic of COVID-19. Chinese Journal of School Health. 2020;41:1682–1687. doi: 10.16835/j.cnki.1000-9817.2020.11.023. [DOI] [Google Scholar]
- Liu F., Zhou N., Cao H., Fang X., Deng L., Chen W., Lin X., Liu L., Zhao H. Chinese college freshmen's mental health problems and their subsequent help-seeking behaviors: A cohort design (2005-2011) PLoS One. 2017;12 doi: 10.1371/journal.pone.0185531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N. [Analysis and counseling of college students’ mental health under the novel coronavirus pneumonia epidemic] Social Sciences Journal of Universities in Shanxi. 2020;32:33–36. doi: 10.16396/j.cnki.sxgxskxb.2020.08.008. [DOI] [Google Scholar]
- Liu Y., Gayle A.A., Wilder-Smith A., Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J. Travel Med. 2020;27 doi: 10.1093/jtm/taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Fu P., Fan C., Zhu M., Li M. COVID-19 Stress and Mental Health of Students in Locked-Down Colleges. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18020771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y.D., Wang J., Zhao S., Guo X.W. Study on anxiety factors of college students at home during COVID-19 epidemic. Xin Li Yue Kan (PSY) 2020;15:62–63. doi: 10.19738/j.cnki.psy.2020.20.023. [DOI] [Google Scholar]
- Lorenz L., Bachem R.C., Maercker A. The Adjustment Disorder–New Module 20 as a Screening Instrument: Cluster Analysis and Cut-off Values. Int. J. Occup. Environ. Med. 2016;7:215–220. doi: 10.15171/ijoem.2016.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotfi M., Hamblin M.R., Rezaei N. COVID-19: Transmission, prevention, and potential therapeutic opportunities. Clin. Chim. Acta. 2020;508:254–266. doi: 10.1016/j.cca.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L., Wang X., Liao Q.Y. Effect of stress events of COVID-19 on psychological health of college students. Health Research. 2020;40:257–260. doi: 10.3969/j.issn.1674-6449.2020.03.005. [DOI] [Google Scholar]
- Manea L., Gilbody S., McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. 2012;184:E191–E196. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Z., Zhao J., Li Y., Chen D., Wang T., Zhang Z., Chen Z., Yu Q., Jiang J., Fan F., Liu X. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020;29:e181. doi: 10.1017/S2045796020000931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCloud T., Bann D. Financial stress and mental health among higher education students in the UK up to 2018: rapid review of evidence. J. Epidemiol. Community Health. 2019;73:977–984. doi: 10.1136/jech-2019-212154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mian A., Khan S. Coronavirus: the spread of misinformation. BMC Med. 2020 doi: 10.1186/s12916-020-01556-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modesti P.A., Reboldi G., Cappuccio F.P., Agyemang C., Remuzzi G., Rapi S., Perruolo E., Parati G., ESH Working Group on CV Risk in Low Resource Settings Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. PLoS One. 2016;11 doi: 10.1371/journal.pone.0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Group PRISMA. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J. Clin. Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Møller L., Augsburger M., Elklit A., Søgaard U., Simonsen E. Traumatic experiences, ICD-11 PTSD, ICD-11 complex PTSD, and the overlap with ICD-10 diagnoses. Acta Psychiatr. Scand. 2020;141:421–431. doi: 10.1111/acps.13161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naser A.Y., Dahmash E.Z., Al-Rousan R., Alwafi H., Alrawashdeh H.M., Ghoul I., Abidine A., Bokhary M.A., Al-Hadithi H.T., Ali D., Abuthawabeh R., Abdelwahab G.M., Alhartani Y.J., Al Muhaisen H., Dagash A., Alyami H.S. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: A cross-sectional study. Brain Behav. 2020:e01730. doi: 10.1002/brb3.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurunnabi M., Hossain S.F.A.H., Chinna K., Sundarasen S., Khoshaim H.B., Kamaludin K., Baloch G.M., Sukayt A., Shan X. Coping strategies of students for anxiety during the COVID-19 pandemic in China: a cross-sectional study. F1000Res. 2020;9:1115. doi: 10.12688/f1000research.25557.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh J.K., Lee M.-S., Bae S.M., Kim E., Hwang J.-W., Chang H.Y., Lee J., Kim J., Lee C.-S., Park J., Bhang S.-Y. Psychiatric Symptoms and Clinical Diagnosis in High School Students Exposed to the Sewol Ferry Disaster. J. Korean Med. Sci. 2019;34:e38. doi: 10.3346/jkms.2019.34.e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozamiz-Etxebarria N., Santa María M.D., Munitis A.E., Gorrotxategi M.P. Reduction of COVID-19 Anxiety Levels Through Relaxation Techniques: A Study Carried Out in Northern Spain on a Sample of Young University Students. Front. Psychol. 2020;11:2038. doi: 10.3389/fpsyg.2020.02038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker G., Gladstone G., Chee K.T. Depression in the planet's largest ethnic group: the Chinese. Am. J. Psychiatry. 2001;158:857–864. doi: 10.1176/appi.ajp.158.6.857. [DOI] [PubMed] [Google Scholar]
- Paul J., Jefferson F. A Comparative Analysis of Student Performance in an Online vs. Face-to-Face Environmental Science Course From 2009 to 2016. Front. Comput. Sci. 2019;1:60. doi: 10.3389/fcomp.2019.00007. [DOI] [Google Scholar]
- Pavithra S., Dheepak Sundar M. Assessment Of Dry Eye Symptoms And Quality Of Sleep In Engineering Students During The Covid-19 Pandemic. International Journal of Research in Pharmaceutical Sciences. 2020;11:1202–1207. doi: 10.26452/ijrps.v11iSPL1.3593. [DOI] [Google Scholar]
- Perz C.A., Lang B.A., Harrington R. Validation of the Fear of COVID-19 Scale in a US College Sample. Int. J. Ment. Health Addict. 2020:1–11. doi: 10.1007/s11469-020-00356-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter A.L., Pitterle M.E., Hayney M.S. Comparison of online versus classroom delivery of an immunization elective course. Am. J. Pharm. Educ. 2014;78:96. doi: 10.5688/ajpe78596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puthran R., Zhang M.W.B., Tam W.W., Ho R.C. Prevalence of depression amongst medical students: a meta-analysis. Med. Educ. 2016;50:456–468. doi: 10.1111/medu.12962. [DOI] [PubMed] [Google Scholar]
- Qi M., Li X., Liu S., Li Y., Huang W. Impact of the COVID-19 epidemic on patterns of pregnant women's perception of threat and its relationship to mental state: A latent class analysis. PLoS One. 2020;15 doi: 10.1371/journal.pone.0239697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu Q.W., Zhang H.Y., Huang B., Chen X., Hao Y., Chen X.F., Wang S.Y., Dong X.M. Anxiety among college students during COVID-19 epidemic and its influencing factors. South China Journal of Preventive Medicine. 2020;46:372–375. doi: 10.12183/j.scjpm.2020.0372. [DOI] [Google Scholar]
- Read J.P., Ouimette P., White J., Colder C., Farrow S. Rates of Trauma Exposure and Posttraumatic Stress Disorder Among Newly Matriculated College Students. Psychol. Trauma. 2011;3:148–156. doi: 10.1037/a0021260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren S., Wang F., Li G.X., Hou W.J., Liu J.L., Hu B.C., Wei L.Q. Investigation on the status of influencing factors for depression and negative emotions of college students in Inner Mongolia during the prevalence of novel coronavirus pneumonia. Journal of Baotou Medical College. 2020;36:70–74. doi: 10.16833/j.cnki.jbmc.2020.08.020. [DOI] [Google Scholar]
- Richardson M., Garner P., Donegan S. Interpretation of subgroup analyses in systematic reviews: A tutorial. Clinical Epidemiology and Global Health. 2019;7:192–198. doi: 10.1016/j.cegh.2018.05.005. [DOI] [Google Scholar]
- Rogowska A.M., Kuśnierz C., Bokszczanin A. Examining Anxiety, Life Satisfaction, General Health, Stress and Coping Styles During COVID-19 Pandemic in Polish Sample of University Students. Psychol. Res. Behav. Manag. 2020;13:797–811. doi: 10.2147/PRBM.S266511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogowska A.M., Pavlova I., Kuśnierz C., Ochnik D., Bodnar I., Petrytsa P. Does Physical Activity Matter for the Mental Health of University Students during the COVID-19 Pandemic? J. Clin. Med. Res. 2020;9 doi: 10.3390/jcm9113494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudenstine S., McNeal K., Schulder T., Ettman C.K., Hernandez M., Gvozdieva K., Galea S. Depression and Anxiety During the COVID-19 Pandemic in an Urban, Low-Income Public University Sample. J. Trauma. Stress. 2020;16:195. doi: 10.1002/jts.22600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu S., Chun B.C. An interim review of the epidemiological characteristics of 2019 novel coronavirus. Epidemiol. Health. 2020;42 doi: 10.4178/epih.e2020006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saddik B., Hussein A., Sharif-Askari F.S., Kheder W., Temsah M.-H., Koutaich R.A., Haddad E.S., Al-Roub N.M., Marhoon F.A., Hamid Q., Halwani R. Increased Levels of Anxiety Among Medical and Non-Medical University Students During the COVID-19 Pandemic in the United Arab Emirates. Risk Manag. Healthc. Policy. 2020;13:2395–2406. doi: 10.2147/RMHP.S273333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global. Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleh D., Camart N., Romo L. Predictors of Stress in College Students. Front. Psychol. 2017;8:19. doi: 10.3389/fpsyg.2017.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salman M., Asif N., Mustafa Z.U., Khan T.M., Shehzadi N., Tahir H., Raza M.H., Khan M.T., Hussain K., Khan Y.H., Butt M.H., Mallhi T.H. Psychological Impairment and Coping Strategies during the COVID-19 Pandemic among Students in Pakistan: A Cross-Sectional Analysis. Disaster Med. Public Health Prep. 2020:1–22. doi: 10.1017/dmp.2020.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sañudo B., Fennell C., Sánchez-Oliver A.J. Objectively-Assessed Physical Activity, Sedentary Behavior, Smartphone Use, and Sleep Patterns Pre- and during-COVID-19 Quarantine in Young Adults from Spain. Sustain. Sci. Pract. Policy. 2020;12:5890. doi: 10.3390/su12155890. [DOI] [Google Scholar]
- Sarokhani D., Delpisheh A., Veisani Y., Sarokhani M.T., Manesh R.E., Sayehmiri K. Prevalence of Depression among University Students: A Systematic Review and Meta-Analysis Study. Depress. Res. Treat. 2013. 2013;373857 doi: 10.1155/2013/373857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayeed A., Satyajit K., Banna M.H., Hasan M.T., Begum M.R., Khan M.S.I. Mental health outcomes during the COVID-19 and perceptions towards the pandemic: Findings from a cross sectional study among Bangladeshi students. Child. Youth Serv. Rev. 2020;119 doi: 10.1016/j.childyouth.2020.105658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlesselman L.S., Cain J., DiVall M. Improving and Restoring the Well-being and Resilience of Pharmacy Students during a Pandemic. Am. J. Pharm. Educ. 2020;84:ajpe8144. doi: 10.5688/ajpe8144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scotta A.V., Cortez M.V., Miranda A.R. Insomnia is associated with worry, cognitive avoidance and low academic engagement in Argentinian university students during the COVID-19 social isolation. Psychol. Health Med. 2020:1–16. doi: 10.1080/13548506.2020.1869796. [DOI] [PubMed] [Google Scholar]
- Shamsuddin K., Fadzil F., Ismail W.S.W., Shah S.A., Omar K., Muhammad N.A., Jaffar A., Ismail A., Mahadevan R. Correlates of depression, anxiety and stress among Malaysian university students. Asian J. Psychiatr. 2013;6:318–323. doi: 10.1016/j.ajp.2013.01.014. [DOI] [PubMed] [Google Scholar]
- Sheikh A., Sheikh Z., Sheikh A. Novel approaches to estimate compliance with lockdown measures in the COVID-19 pandemic. J. Glob. Health. 2020;10 doi: 10.7189/jogh.10.010348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. J. Advert. Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith M.T., Wegener S.T. Measures of sleep: The Insomnia Severity Index, Medical Outcomes Study (MOS) Sleep Scale, Pittsburgh Sleep Diary (PSD), and Pittsburgh Sleep Quality Index (PSQI) Arthritis & Rheumatism. 2003;49:S184–S196. doi: 10.1002/art.11409. [DOI] [Google Scholar]
- Sobowale K., Zhou N., Fan J., Liu N., Sherer R. Depression and suicidal ideation in medical students in China: a call for wellness curricula. J. Int. Assoc. Med. Sci. Educ. 2014;5:31–36. doi: 10.5116/ijme.52e3.a465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramaniam M., Abdin E., Picco L., Pang S., Shafie S., Vaingankar J.A., Kwok K.W., Verma K., Chong S.A. Stigma towards people with mental disorders and its components - a perspective from multi-ethnic Singapore. Epidemiol. Psychiatr. Sci. 2017;26:371–382. doi: 10.1017/S2045796016000159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundarasen S., Chinna K., Kamaludin K., Nurunnabi M., Baloch G.M., Khoshaim H.B., Hossain S.F.A., Sukayt A. Psychological Impact of COVID-19 and Lockdown among University Students in Malaysia: Implications and Policy Recommendations. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17176206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., Chen S., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tasnim R., Islam M.S., Sujan M.S.H., Sikder M.T., Potenza M.N. Suicidal ideation among Bangladeshi university students early during the COVID-19 pandemic: Prevalence estimates and correlates. Child. Youth Serv. Rev. 2020;119 doi: 10.1016/j.childyouth.2020.105703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thahir A.I.A., Iqbal M., Maharani S.A., Syam A. The Emotional State and Physical Condition of Indonesian College Students: An Emerging Situation during the Coronavirus Disease-19 Crisis in Indonesia. Open Access Macedonian Journal of Medical Sciences. 2020;8:261–267. doi: 10.3889/oamjms.2020.5283. [DOI] [Google Scholar]
- Van Der Feltz-Cornelis C.M., Varley D., Allgar V.L., de Beurs E. Workplace Stress, Presenteeism, Absenteeism, and Resilience Amongst University Staff and Students in the COVID-19 Lockdown. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.588803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma K. The mental health impact of the COVID-19 epidemic on college students in India. Asian J. Psychiatr. 2020;53 doi: 10.1016/j.ajp.2020.102398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Zhao H. The Impact of COVID-19 on Anxiety in Chinese University Students. Front. Psychol. 2020;11:1168. doi: 10.3389/fpsyg.2020.01168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Zhao H., Zhang H. Chinese College Students Have Higher Anxiety in New Semester of Online Learning During COVID-19: A Machine Learning Approach. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.587413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Qin N., Zhang C., Hu C., Liu C.Y. An investigation of the awareness of COVID-19 epidemic and psychological behavior among college students. J. Qingdao Univ. 2020;56 doi: 10.11712/jms.2096-5532.2020.56.172. [DOI] [Google Scholar]
- Wang X., Chen H., Liu L., Liu Y., Zhang N., Sun Z., Lou Q., Ge W., Hu B., Li M. Anxiety and Sleep Problems of College Students During the Outbreak of COVID-19. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.588693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y. A Study on College Students’ Anxiety Levels and Influencing Factors During the Novel Coronavirus Prevention Period. J. Teach. Educ. 2020;7:76–83. doi: 10.13718/j.cnki.jsjy.2020.03.009. [DOI] [Google Scholar]
- Wang Y., Chen Q.H., Zhao H.P., Liu J. Survey and analysis of mental health status of college students in Wuhan during the post-COVID-19 pandemic. China Journal of Health Psychology. 2020 [Google Scholar]
- Wang Z.-H., Yang H.-L., Yang Y.-Q., Liu D., Li Z.-H., Zhang X.-R., Zhang Y.-J., Shen D., Chen P.-L., Song W.-Q., Wang X.-M., Wu X.-B., Yang X.-F., Mao C. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: A large cross-sectional study. J. Affect. Disord. 2020;275:188–193. doi: 10.1016/j.jad.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wathelet M., Duhem S., Vaiva G., Baubet T., Habran E., Veerapa E., Debien C., Molenda S., Horn M., Grandgenèvre P., Notredame C.-E., D'Hondt F. Factors Associated With Mental Health Disorders Among University Students in France Confined During the COVID-19 Pandemic. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.25591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2018. International classification of diseases for mortality and morbidity statistics (11th Revision) [WWW Document]. URL https://icd.who.int/en (accessed 2.16.21).
- World Health Organization, 2015. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003 [WWW Document]. URL https://www.who.int/csr/sars/country/table2004_04_21/en/ (accessed 7.7.20).
- World Health Organization, 2021 Coronavirus Disease (COVID-19) - events as they happen [WWW Document]. URL https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed 7.7.20).
- Wu B.B., Tao Z., Han X.L. Exploration and analysis of college students’ psychological health status during the epidemic situation: A case study of Shanghai University of Electric Power. Xin Li Yue Kan (PSY) 2020;15:43–44. doi: 10.19738/j.cnki.psy.2020.18.015. [DOI] [Google Scholar]
- Wu T.H., Zhang Y., Wang R.J., Wu X.Y., Tao S.M., Xu S.J., Tao F.B. Relationship between digital media use and anxiety in college students during the COVID-19 outbreak. Chinese Journal of School Health. 2020;41:1625–1628. doi: 10.16835/j.cnki.1000-9817.2020.11.007. [DOI] [Google Scholar]
- Wyatt T., Oswalt S.B. Comparing Mental Health Issues Among Undergraduate and Graduate Students. Am. J. Health Educ., Monograph Series No. 8T. 2013;44:96–107. doi: 10.1080/19325037.2013.764248. [DOI] [Google Scholar]
- Xiang M.-Q., Tan X.-M., Sun J., Yang H.-Y., Zhao X.-P., Liu L., Hou X.-H., Hu M. Relationship of Physical Activity With Anxiety and Depression Symptoms in Chinese College Students During the COVID-19 Outbreak. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.582436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H., Wang L.Y., Xiao C.C., Yan H. Analysis of psychological behavior of college students in Wuhan during the COVID-19 epidemic. Journal of Public Health and Preventative Medicine. 2020;31:14–18. doi: 10.3969/j.issn.1006-2483.2020.03.004. [DOI] [Google Scholar]
- Xia Y.Y., Li Y. A study on college students’ sense of security, existential anxiety and coping style. China Journal of Health Psychology. 2020:1–12. [Google Scholar]
- Xu W.Q., Li G.Y. Analysis of mental health status and differences of independent college students during the COVID-19. Xin Li Yue Kan (PSY) 2020;15:83–84. doi: 10.19738/j.cnki.psy.2020.19.032. [DOI] [Google Scholar]
- Yang X.J., Gao L., Zhang S.Y., Zhang L.G., Zhou S.J. Psychological status and its relationship with social support in college students during COVID-19 epidemic. Journal of Psychiatry. 2020;33:241–246. doi: 10.3969/j.issn.2095-9346.2020.04.001. [DOI] [Google Scholar]
- Yang Y.Y., Wang Y., Li S.X., Lei X.M., Yang Y.F. Psychological responses and related factors of college students in Shaan’ xi during COVID-19 outbreak. Chinese Journal of School Health. 2020;41:664–667. doi: 10.16835/j.cnki.1000-9817.2020.05.008. [DOI] [Google Scholar]
- Ye B.Q., Xu Y., Dong M. [Investigation and analysis of mental health status of post-2000s freshmen during the COVID-19 pandemic] Journal of Chongqing University of Technology (Social Science) 2020:1–10. [Google Scholar]
- Yi H., Peng Z., Zhang L.Q., Kong S.S. COVID-19 outbreak during the period of mental health survey of art students in Lingnan Teachers College. China Journal of Health Psychology. 2020:1–9. [Google Scholar]
- Yue X.H., Ding F.H., Shou L. [Research on the effect of art design as a psychological intervention of college students after the end of the novel coronavirus pneumonia epidemic] Literature Life. 2020:158–159. [Google Scholar]
- Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: A review. Clin. Immunol. 2020;215 doi: 10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai P., Ding Y., Wu X., Long J., Zhong Y., Li Y. The epidemiology, diagnosis and treatment of COVID-19. Int. J. Antimicrob. Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai Y., Du X. Addressing collegiate mental health amid COVID-19 pandemic. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.113003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang B., Ye Y., Jin J.M., Lin L.H. [Mental health status of college students in Fujian Province at different stages of the prevention and control of the novel coronavirus pneumonia epidemic] Chinese Journal of School Health. 2020;41:1896–1899. doi: 10.16835/j.cnki.1000-9817.2020.12.033. [DOI] [Google Scholar]
- Zhang J., Zeng J., Luo J.H., Zou X.Y., Gu J. Epidemiological survey of the COVID-19 epidemic-related knowledge, behaviors and psychology status among college students and their family members. Modern Preventive Medicine. 2020;47:3754–3758. [Google Scholar]
- Zhang L.L., Liu X., Guo S.S., Zhang Y.S., Liang W., Li K.Q., Ni Z.Y. 2019 novel coronavirus (2019-nCoV) associated mental health among medical students and non-medical students. China Journal of Health Psychology. 2020:1–7. [Google Scholar]
- Zhang X.Y., Sui X., Chang R.S. [Investigation of the relationship between social support, depression and anxiety during the novel coronavirus pneumonia epidemic - A study of higher education students] J. Liaoning Norm. Univ./Liaoning Shifan Daxue Xuebao. 2020;43:83–87. doi: 10.16216/j.cnki.lsxbwk.202005083. [DOI] [Google Scholar]
- Zhang Y., Zhang H., Ma X., Di Q. Mental Health Problems during the COVID-19 Pandemics and the Mitigation Effects of Exercise: A Longitudinal Study of College Students in China. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17103722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Sun K., Jatchavala C., Koh J., Chia Y., Bose J., Li Z., Tan W., Wang S., Chu W., Wang J., Tran B., Ho R. Overview of Stigma against Psychiatric Illnesses and Advancements of Anti-Stigma Activities in Six Asian Societies. Int. J. Environ. Res. Public Health. 2019;17 doi: 10.3390/ijerph17010280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao B., Kong F., Aung M.N., Yuasa M., Nam E.W. Novel Coronavirus (COVID-19) Knowledge, Precaution Practice, and Associated Depression Symptoms among University Students in Korea, China, and Japan. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17186671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao C.Z. A survey &study on college students’ mental health state and the education countermeasures during the Novel Coronavirus Pneumonia. Xin Li Yue Kan (PSY) 2020;15:1–3. doi: 10.19738/j.cnki.psy.2020.08.001. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.