Pancreatic cancer is among the most lethal of human malignancies and is projected to become the second leading cause of cancer-related mortality in the United States (US) by 20401. Among pancreatic cancer histologies, adenocarcinoma is the most common and has the lowest 5-year overall survival rate2. Though early-onset pancreatic cancer (EOPC, cancers diagnosed before age 50–55) accounts for only 5–12% of all pancreatic cancer cases3,4, several studies using Surveillance, Epidemiology and End Results (SEER) data have reported that the incidence of EOPC has been increasing in recent decades4–7. However, only two of these studies have examined differences in incidence trends across race/ethnicity5,7.
As the SEER program captures only 48% of the US population, there is a need to further evaluate sociodemographic patterns in pancreatic cancer incidence across a larger, more generalizable national sample. In this study, we utilized data from the North American Association of Central Cancer Registries (NAACCR)8, which provides nearly complete coverage of all US-based cancer registries, to compare incidence trends of EOPC and late-onset pancreatic cancer (LOPC) over multiple sex and race/ethnicity subgroups across the entire US population.
Using the 1995–2018 data from NAACCR, we identified and categorized all invasive pancreatic adenocarcinoma cases as EOPC (diagnosed age 0–54) or LOPC (diagnosed age 55+). We calculated annual age-adjusted incidence rates (AAIR) and average annual percent change (AAPC) in AAIRs for EOPC and LOPC for the entire cohort and by sex and race/ethnicity. Additional details of the methods can be found in the Supplemental Materials.
There were 713,622 (80,908 EOPC, 632,714 LOPC) incident cases of invasive pancreatic adenocarcinoma in the US from 1995–2018. The largest racial/ethnic group was non-Hispanic white (77.7%), followed by non-Hispanic black (11.9%), Hispanic (6.8%), and non-Hispanic Asian/Pacific Islander (2.8%). Compared to LOPC cases, individuals with EOPC were more likely to be male, less likely to be non-Hispanic white, and more likely to have advanced stage cancer at diagnosis and tumors in the tail of the pancreas (Table S1).
EOPC and LOPC incidence steadily increased over the study period, with the average annual percent change being twice as high for LOPC (AAPC 0.84, 95% CI 0.78–0.90) than EOPC (AAPC 0.40, 95% CI 0.24–0.57) (Figure 1A/B). For EOPC, the largest increases were observed in non-Hispanic whites (AAPC 0.58, 95% CI 0.41–0.75) and Hispanics (AAPC 0.46, 95% CI 0.13–0.79). Additionally, non-Hispanic blacks had a significant decreasing trend for EOPC (AAPC −0.23, 95% CI −0.45 to 0.00) (Figure 1A). In contrast, the AAIRs for LOPC were on a significant increasing trend for each individual race/ethnicity except for non-Hispanic Asian/Pacific Islanders (Figure 1B). For both EOPC and LOPC, AAIRs were highest in non-Hispanic blacks and lowest in non-Hispanic Asian/Pacific Islanders.
Figure 1.
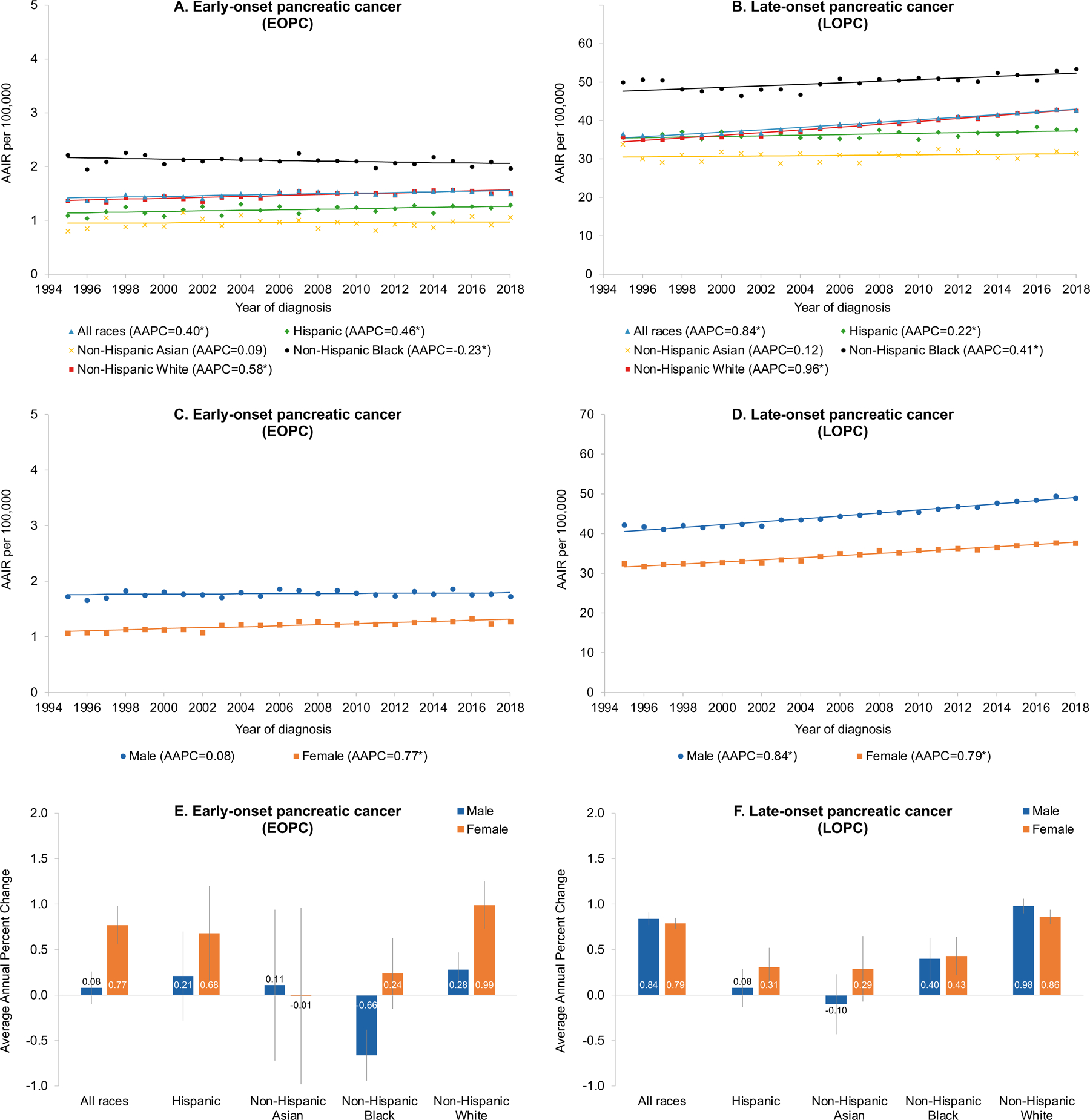
Panels A-B: Annual Age-Adjusted Incidence Rates (AAIRs) and Average Annual Percent Change (AAPC) of AAIRs by Race/ethnicity for (A) Early-Onset and (B) Late-Onset Invasive Pancreatic Cancer; Panels C-D: AAIRs and AAPCs of AAIRs by Sex for (C) Early-Onset and (D) Late-Onset Invasive Pancreatic Cancer; Panels E-F: AAPCs and 95% Confidence Intervals of AAIRs by Race/ethnicity and Sex for (E) Early-Onset and (F) Late-Onset Invasive Pancreatic Cancer
Footnote: For panels A-D, asterisk (*) indicates statistically significant average annual percent change (AAPC) in the AAIRs.
Incidence rates were also higher for males compared with females for both EOPC and LOPC (Figure 1C/D). However, only females had a significant increasing trend for EOPC (AAPC 0.77, 95% 0.56–0.98), while males (AAPC 0.84, 95% CI 0.77–0.91) and females (AAPC 0.79, 95% CI 0.72–0.85) had similar significant increasing trends for LOPC.
When evaluating the sex-specific AAIR trends by racial/ethnic subgroups, the increasing EOPC incidence for females was mainly driven by non-Hispanic whites (AAPC 0.99, 95% CI 0.73–1.25) and Hispanics (AAPC 0.68, 95% CI 0.17–1.20). Among males, non-Hispanic blacks had a significant decreasing EOPC incidence trend (AAPC −0.66, 95% CI −0.93 to −0.38), while non-Hispanic whites had a significant increasing trend (AAPC 0.28, 95% CI 0.09–0.47) (Figure 1E). For LOPC, the most rapid increases in incidence were observed among non-Hispanic whites (male: 0.98, 95% CI 0.90–1.06; female: 0.86, 95% CI 0.78–0.94) (Figure 1F).
The more rapid rise in EOPC incidence among females in our study is consistent with results from previous SEER-based analyses4,5,7. Indeed, a study using SEER data from 1973–2013 also observed the fastest increases in EOPC incidence among younger non-Hispanic white females5. It has been suggested that the accelerating EOPC incidence in young females could be due to histologic subtypes that are more common in females (e.g. cystic adenocarcinomas)5. This is congruent with our data, as the prevalence of cystic adenocarcinomas was also higher in females for EOPC compared with LOPC.
Surprisingly, we detected opposite trends for EOPC and LOPC incidence for non-Hispanic blacks, with the greatest decrease in EOPC incidence observed among black males. This negative trend was also detected in the aforementioned study using SEER data from 1973–2013, where the rates for black males aged 45–55 had a significant declining trend over time5.
The faster increases in EOPC incidence among non-Hispanic white and Hispanic females may be attributable to racial/ethnic differences in the prevalence and trends of pancreatic cancer risk factors. Data from the 2011–2018 National Health and Nutrition Examination Survey showed that Hispanics and non-Hispanic whites had significant increases in body mass index and waist circumference over time9. Higher rates of EOPC may also be explained by increases in the use of diagnostic imaging and earlier diagnosis, as supported by evidence showing increases in the rates of early stage10 and indolent tumor types5.
The major strength of our study is that NAACCR, which includes data from both the SEER program and the National Program of Cancer Registries, captures almost 100% of the US population8. This allowed us to delineate incidence trends for both EOPC and LOPC across multiple sex and racial/ethnic subgroups for the entire US population, making our results more generalizable compared to previous studies. However, we did not have data on risk factors (e.g. smoking, obesity) and thus could not account for these characteristics in our analyses. Nevertheless, our study still provides novel and important information for hypotheses generation and future directions in pancreatic cancer research.
In this study of 713,622 pancreatic adenocarcinoma cases in the US over two decades, we observed sex and racial/ethnic disparities in the incidence patterns for EOPC and LOPC. The more rapid increases in EOPC incidence for non-Hispanic white and Hispanic females indicate that these higher-risk populations might benefit from targeted surveillance and interventions. Future studies should seek to elucidate whether these differences across race/ethnicity are attributable to specific tumor characteristics, biomarkers, or other sociodemographic factors.
Supplementary Material
ACKNOWLEDGEMENTS
USC Pancreas Research Team: Chukwuemelie Okwo, Department of Population and Public Health Sciences, Keck School of Medicine of USC; Bo Han, Heinz-Josef Lenz, Department of Medicine, Keck School of Medicine of USC; Reginald Hill, Lawrence J. Ellison Institute of Transformative Medicine, Keck School of Medicine of USC.
The authors would like to extend their sincere appreciation to all cancer registry programs in the U.S. and to all cancer registrars whose hard work and dedication to data collection make cancer surveillance research like this possible. This work was supported by grants from the National Cancer Institute (NCI R01CA209798 to Veronica Wendy Setiawan and T32CA229110 and K99CA256525 to Brian Z. Huang).
Abbreviations:
- AAIR
age-adjusted incidence rate
- AAPC
average annual percent change
- CHIS
California Health Interview Survey
- EOPC
early-onset pancreatic cancer
- LOPC
late-onset pancreatic cancer
- NAACCR
North American Association of Central Cancer Registries
- SEER
Surveillance, Epidemiology and End Results
Footnotes
Disclosures: The authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Rahib L, et al. JAMA Netw Open 2021;4:e214708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fesinmeyer MD, et al. Cancer Epidemiol Biomarkers Prev 2005;14:1766–73. [DOI] [PubMed] [Google Scholar]
- 3.Ansari D, et al. Langenbecks Arch Surg 2019;404:565–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaddam S, et al. JAMA 2021;326:2075–2077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gordon-Dseagu VL, et al. Int J Epidemiol 2018;47:427–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramai D, Lanke G, et al. Pancreatology 2021;21:124–129. [DOI] [PubMed] [Google Scholar]
- 7.LaPelusa M, Shen C, et al. Cancers (Basel) 2022;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sherman R, et al. eds. North American Association of Central Cancer Registries, Inc.; 2021.
- 9.Liu B, et al. BMJ 2021;372:n365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blackford AL, et al. J Natl Cancer Inst 2020;112:1162–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


