Abstract
Background:
Although studies have reported variation in out-of-hospital cardiac arrest (OHCA) survival by geographic location, little is known about variation in OHCA survival at the level of Emergency Medical Service (EMS) agencies – which may have modifiable practices, unlike counties and regions. We quantified the variation in OHCA survival across EMS agencies and explored whether variation in two specific EMS resuscitation practices were associated with survival to hospital admission.
Methods:
Within the Cardiac Arrest Registry to Enhance Survival, a prospective registry representing approximately 51% of the U.S. population, we identified 258,342 OHCAs from 764 EMS agencies with ≥10 OHCA cases annually during 2015–2019. Using hierarchical logistic regression, risk-standardized rates of survival to hospital admission were computed for each EMS agency. We quantified inter-agency variation in survival with median odds ratios (MOR) and assessed the association of two resuscitation practices (EMS response time and the proportion of OHCAs with termination of resuscitation [TOR] without meeting futility criteria) with EMS agency survival rates to hospital admission.
Results:
Across 764 EMS agencies comprising 258,342 OHCAs, the median risk-standardized rate of survival to hospital admission was 27.3% (interquartile range, 24.5%−30.1%; range: 16.0–45.6%). The adjusted MOR was 1.35 (95% CI: 1.32–1.39), denoting that the odds of survival of two patients with identical covariates varied by 35% at two randomly selected EMS agencies. EMS agencies in the lowest quartile of risk-standardized survival had longer EMS response times when compared to the highest quartile (12.0 ± 3.4 minutes vs. 9.0 ± 2.6 minutes, P<0.001), and a higher proportion of OHCAs with TOR without meeting futility criteria (27.9% ± 16.1% vs. 18.9% ± 11.4%, P<0.001).
Conclusions:
Survival after OHCA varies widely across EMS agencies. EMS response times and TOR practices were associated with agency-level rates of survival to hospital admission, suggesting potentially modifiable practices which can improve OHCA survival.
Keywords: Cardiac arrest, Survival, Outcomes, Variation
INTRODUCTION
Over 350,000 out-of-hospital cardiac arrests (OHCA) occur annually in the United States, and nearly all are assessed by emergency medical service (EMS) personnel.1 Survival rates after OHCA remain low, with less than 23% surviving to hospital admission and 10% surviving to hospital discharge.2,3 Although some studies have reported variation in OHCA survival by county4 and geographic region,5 little is known about variation in OHCA survival at the level of the EMS agency. Variation in OHCA survival across EMS agencies is critical to understand as resuscitation practices are potentially modifiable at this level whereas they are ill-defined at the level of counties or regions since these geographical entities are typically served by multiple EMS agencies.
For instance, practice patterns on whether to terminate resuscitations in the field may vary widely across EMS agencies and influence EMS agency rates of OHCA survival. Given the poor prognosis associated with OHCA, guidelines have been developed to support decisions for termination of resuscitation (TOR) when the likelihood of survival to discharge is less than 1% and continuing resuscitation is considered futile.6–8 These guidelines suggest that TOR be considered due to futility when all four of the following advanced life support (ALS) criteria are met: unwitnessed OHCA, no provision of bystander cardiopulmonary resuscitation (CPR) prior to EMS arrival, no shock delivered during resuscitation (i.e., non-shockable rhythm), and no return of spontaneous circulation (ROSC) prior to transport.7,9 However, TOR decisions are made for a number of patients not meeting all four futility criteria. Currently, it is unknown whether EMS agencies vary in termination rates for patients who do not meet criteria for futility and potential variation in this practice could affect EMS-level rates of OHCA survival. A second potential factor influencing variation in OHCA survival across EMS agencies is response time – defined as the time from initial activation of 911 for an OHCA to EMS arrival. Given that the majority of OHCA victims do not receive bystander CPR prior to EMS arrival and that the quality of bystander CPR may be suboptimal, differential response times among EMS agencies may also account for variation in OHCA survival at the EMS agency level.
To address these gaps in knowledge, within the national Cardiac Arrest Registry to Enhance Survival (CARES), we quantified the variation in OHCA survival to hospital admission across EMS agencies. We also examined whether EMS agencies varied in response times and rates of TOR in patients not meeting futility criteria, and whether these resuscitation practices are associated with EMS agency-level rates of OHCA survival to hospital admission. A finding that significant variation in survival exists should motivate regional strategies to identify best practices to improve the quality of EMS care.
METHODS
Data Source and Study Design
The data that support the findings of this study are available from the corresponding author on request and approval by the CARES registry. CARES is a prospective, multicenter registry of patients with OHCA in the U.S, with a catchment area of over 161 million residents, representing approximately 51% of the U.S. population. Established by the Centers for Disease Control and Emory University, the design of the registry has been previously described.10,11 Briefly, all patients with a confirmed OHCA and for whom resuscitation is attempted are identified and followed by EMS agencies. Data are collected from three sources: 9-1-1 dispatch (public safety answering point) centers, EMS agencies, and receiving hospitals. Standardized international Utstein definitions are used for uniformity in clinical variables and outcomes across EMS agencies.12 A CARES analyst reviews records for completeness and accuracy.11 The study was approved by Saint Luke’s Hospital’s institutional review board, which waived the requirement for informed consent as the study involved deidentified data.
Study Population
In this study, we were interested in evaluating all cases of non-traumatic OHCA between 2015 and 2019, during which 377,475 cases from 1449 EMS agencies were initially identified (Figure 1). We excluded 10,356 OHCAs in those under 18 years of age to focus on adults, and 57,024 OHCAs which occurred in nursing facilities, medical clinics, transport centers or hospitals. We also excluded 2021 OHCAs due to electrocution or drowning, 40,821 OHCAs witnessed by EMS, and 8350 OHCAs from EMS agencies with fewer than 10 cases annually over 2 or more years (or those with fewer than 20 cases if the EMS agency had only one year of CARES participation). Additionally, 561 OHCAs were excluded for missing survival data. The final study cohort comprised 258,342 OHCAs from 764 EMS agencies.
Figure 1. Definition of Study Cohort.
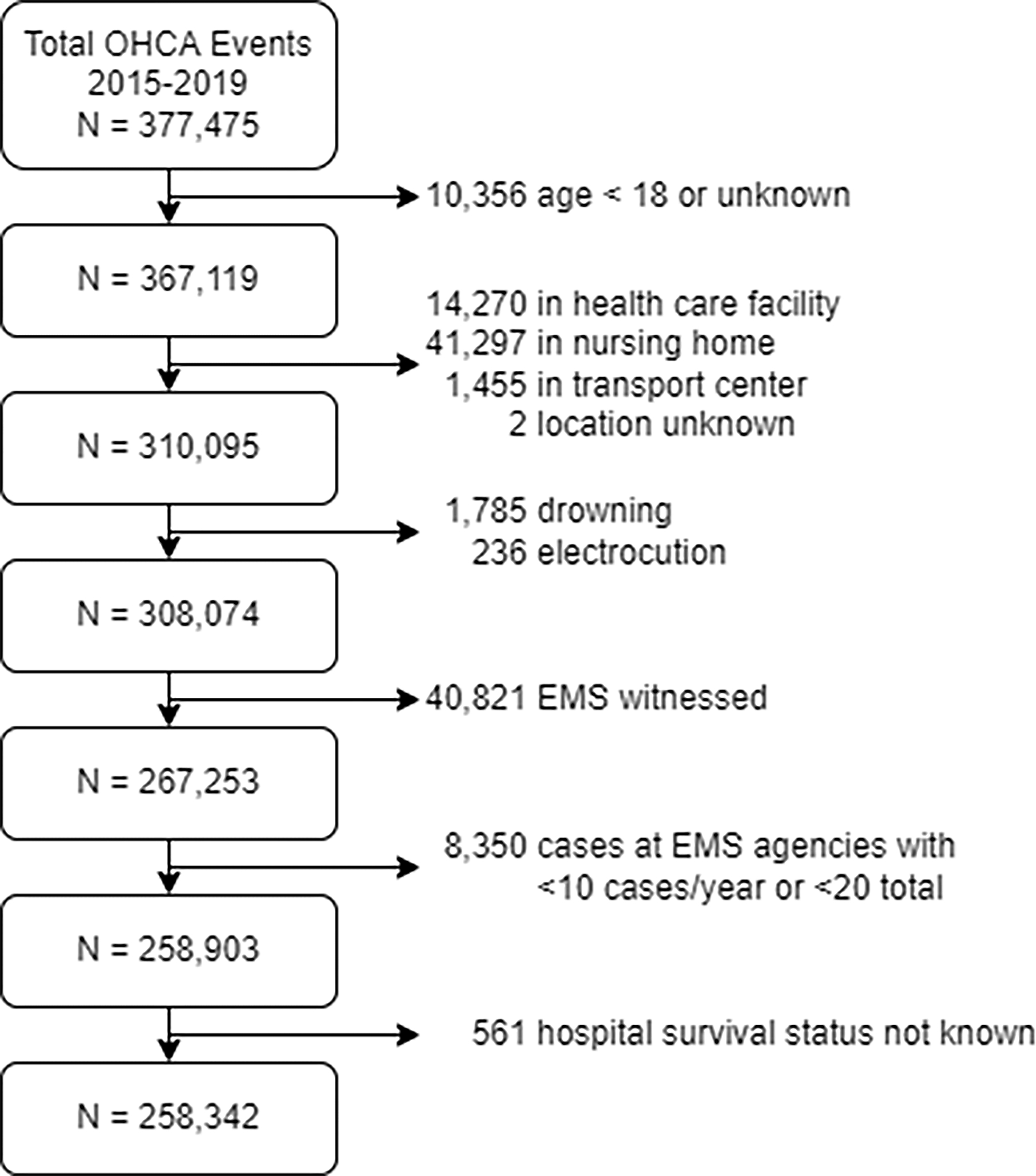
Consort diagram. Abbreviations: EMS, emergency medical services; OHCA, out-of-hospital cardiac arrest.
Study Outcome and Resuscitation Practices
The primary outcome was survival to hospital admission. Among all OHCAs at each EMS agency, we also examined two resuscitation practices: 1) the mean EMS response time, defined as the time from 911 dispatch to EMS arrival on scene, and 2) the proportion of patients with TOR despite not meeting all four ALS criteria for futility (unwitnessed OHCA, no bystander CPR, no shock delivered due to non-shockable OHCA rhythm, and no ROSC). As a sensitivity analysis, we also evaluated the latter using the 3-variable Universal TOR criteria (unwitnessed OHCA, no shock delivered, and no ROSC).
Statistical Analysis
For each EMS agency, we calculated risk-standardized rates of survival to hospital admission. We constructed a multivariable hierarchical logistic regression model for the outcome of survival to hospital admission, including patient and cardiac arrest variables as fixed effects and EMS agency as a random effect to account for clustering of patients at the agency level.13,14 This model adjusted for demographics (age, sex, race), location of arrest (home, commercial workplace, public location, recreational facility, or other), whether the arrest was witnessed, initial cardiac arrest rhythm (asystole, pulseless electrical activity, unknown unshockable rhythm, unknown shockable rhythm, ventricular fibrillation and ventricular tachycardia), etiology of cardiac arrest (presumed cardiac, respiratory, drug overdose, and other), and whether bystander CPR was administered prior to EMS personnel arrival. Model discrimination was assessed with the c-statistic and was 0.73, suggesting good discrimination. Using the estimates from the model, risk-standardized rates of survival to hospital admission were calculated using methodology analogous to that used by the Center for Medicare and Medicaid Services for risk-standardized measures.15,16 EMS agencies were then categorized into quartiles based on their risk-standardized rates of survival to hospital admission, and site and patient characteristics were summarized descriptively by quartile.
We next examined variation in site performance, graphically and quantitatively, using median odds ratio (MOR) to quantify the extent of variability in rates of survival to hospital admission across EMS agencies. The MOR represents the median relative difference in odds that two patients with identical model covariates would survive to hospital admission at one randomly selected EMS agency in the study cohort vs. another EMS agency.
Additionally, we examined site-level rates for each of the two EMS agency resuscitation practices (EMS response time and ALS TOR without meeting futility criteria), across the EMS agency quartiles of survival. To determine whether these resuscitation practices were associated with variation in rates of survival to hospital admission among EMS agencies, we first summarized practice rates descriptively across quartiles of risk-standardized survival. Next, each resuscitation practice was added as a site-level variable in the hierarchaical model described above, to assess whether each resuscitation practice was significantly associated with variation in OHCA survival across EMS agencies. We also examined for an interaction between each of the two resuscitation practices and urbanicity of the EMS agency (categorized as urban areas [≥50,000 residents], urban clusters [2500 to 49,999 residents], and rural areas [<2500 residents] by the U.S. Census Bureau.17
Finally, we evaluated the relationship between EMS agency rates of survival to hospital admission and favorable neurological survival to confirm the robustness of our findings. Hierarchical logistic regression models for the outcome of favorable neurological survival (as defined by Cerebral Performance Category scores of 1 or 2 for those surviving to hospital discharge) were constructed in similar fashion as in our primary analysis, except for also adjusting for receipt of targeted temperature management. Spearman’s coefficient then assessed the correlation between EMS agency risk-standardized rates of survival to hospital admission and favorable neurological survival.
The rate of missingness for patient-level variables was <1%, except for EMS response times. Overall, 56 (7%) of EMS agencies did not report response times. Therefore, we first fit models only on those agencies with available response times, and then another model was fit to include all agencies (with a dummy variable for whether or not response times were reported). Results were virtually identical with both approaches, therefore, we reported estimates from the latter model.
All analyses were evaluated at a 2-sided significance level of 0.05 and performed with SAS 9.4 (SAS Institute, Cary, NC) and R version 3.6.3.11
RESULTS
Of 258,342 persons with OHCA, mean age was 62.2 years (standard deviation: 17.0 years) and 36.1% were female (Table 1). Nearly half (49.5%) of patients were of White race, 21.2% were of Black race, and 29.3% were of other or unknown race. Overall, 85.0% were of presumed cardiac etiology, 82.3% occurred at home, and 44.0% were witnessed by a bystander. Nearly four in five OHCAs were due to an initial rhythm that was non-shockable, and bystander CPR was performed in 39.2% of OHCAs. At the patient level, the mean EMS response time was 10.1 ± 14.3 minutes, and sustained ROSC was achieved in 30.6% of patients. Overall, 70,752 (27.4%) patients survived to hospital admission, 97,584 (37.8%) had TOR in the field, and 90,006 (34.8%) were transported but did not survive to hospital admission. Of 97,584 who had TOR in the field, 53,925 (55.3%) had TOR without meeting all four ALS futility criteria.
Table 1.
Baseline Characteristics of Patients
| Total N = 258,342 | |
|---|---|
|
| |
| Age, years | |
| Mean ± SD | 62.2 ± 17.0 |
| Median (IQR) | 63.0 (52.0, 75.0) |
|
| |
| Sex | |
| Female | 93,254 (36.1%) |
| Male | 165,077 (63.9%) |
| Missing | 11 |
|
| |
| Race | |
| White | 127,853 (49.5%) |
| Black | 54,849 (21.2%) |
| Other | 23,698 (9.2%) |
| Unknown | 51,942 (20.1%) |
|
| |
| Location of Arrest | |
| Home/Residence | 212,612 (82.3%) |
| Industrial Place | 1407 (0.5%) |
| Place of Recreation | 4185 (1.6%) |
| Public/Commercial Building | 23,050 (8.9%) |
| Street/Highway | 16,193 (6.3%) |
| Other | 895 (0.3%) |
|
| |
| Witness Status | |
| Bystander Witnessed | 113,696 (44.0%) |
| Unwitnessed | 144,640 (56.0%) |
| Missing | 6 |
|
| |
| Presumed Etiology of Cardiac Arrest | |
| Cardiac | 219,540 (85.0%) |
| Respiratory | 18,065 (7.0%) |
| Drug Overdose | 13,291 (5.1%) |
| Hemorrhage/Exsanguination | 1116 (0.4%) |
| Other | 6330 (2.5%) |
|
| |
| Bystander CPR Status | |
| Bystander CPR | 101,172 (39.2%) |
| No Bystander CPR | 157,116 (60.8%) |
| Missing | 54 |
|
| |
| First Monitored Rhythm | |
| Asystole | 133,164 (51.6%) |
| Idioventricular/PEA | 46,456 (18.0%) |
| Unknown Unshockable Rhythm | 24,629 (9.5%) |
| Unknown Shockable Rhythm | 12,364 (4.8%) |
| Ventricular Fibrillation | 39,252 (15.2%) |
| Ventricular Tachycardia | 2454 (0.9%) |
| Missing | 23 |
| EMS Response Time from 911 Call (minutes) | |
| Mean ± SD | 10.1 ± 14.3 |
| Median (IQR) | 8.8 (6.6, 11.8) |
| Missing | 65,348 |
|
| |
| TOR | 97,584 (37.8%) |
|
| |
| TOR Without Meeting Futility Criteria | |
| *ALS (4-variable) TOR criteria | 53,925 (20.9%) |
| Universal (3-variable) TOR criteria | 31,149 (12.1%) |
| Missing | 28 |
The 4-variable ALS TOR criteria was the main TOR variable in the primary analysis.
Abbreviations: ALS, advanced life support; CPR, cardiopulmonary resuscitation; EMS, emergency medical service; IQR, interquartile range; SD, standard deviation; PEA, pulseless electrical activity; TOR, termination of resuscitation
The 764 EMS agencies in the study cohort were distributed throughout the U.S. as follows: 154 (20.2%) in the Northeast, 171 (22.4%) in the South, 193 (25.3%) in the Midwest, and 246 (32.2%) in the West. The hierarchical model to derive risk-standardized rates of survvial to hospital admission is reported in Supplementary Appendix Figure S1. Across EMS agencies in the study cohort, the median risk-standardized rate of survival to hospital admission was 27.3% (IQR, 24.5% – 30.2%; range, 16.0% – 45.6%) (Figure 2). EMS agenices by quartiles of risk-standardized survival are described in Table 2. EMS agencies in the lowest quartile (quartile 1) of risk-standardized survival had a mean EMS reponse time of 12.0 ± 3.4 minutes, whereas those in quartiles 2, 3, and the highest quartile (quartile 4) of risk-standardized survival had mean EMS arrival times of 10.1 ± 3.0 minutes, 9.6 minutes ± 2.8 minutes, and 9.0 ± 2.6 minutes, respectively. The mean proportion of OHCA cases with ALS TOR in the field without meeting futility critera was 27.9% ± 16.1% in the lowest quartile of risk-standardized survival, 21.9% ± 13.6% in quartile 2, 21.0% ± 13.1% in quartile 3, and 18.9% ± 11.4% in the highest quartile of risk-standardized survival. EMS agency rates of risk-standardized survival by their response times and rates of ALS TOR without futility criteria are shown as scatterplots in Figures 3 and 4.
Figure 2. Distribution of EMS Agency Rates of Risk-Standardized Survival to Hospital Admission for OHCA.
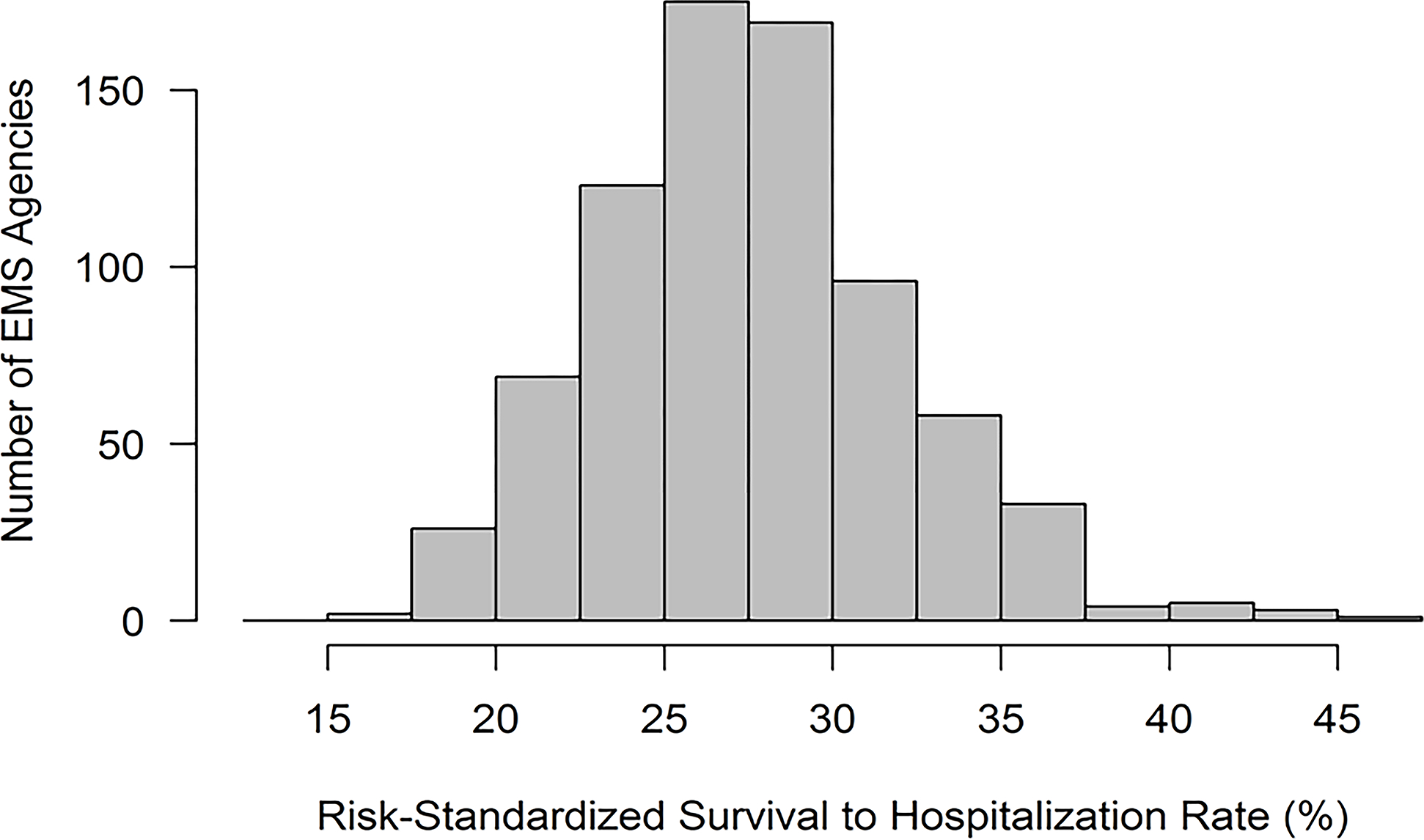
Histogram of EMS-level risk-standardized survival to hospital admission. Abbreviations: EMS, emergency medical services; OHCA, out-of-hospital cardiac arrest.
Table 2. EMS Characteristics and Practices Across Quartiles of Risk-Standardized Survival.
EMS agencies were categorized by quartiles of risk-standardized rates of survival to hospital admission for OHCA. Rates for favorable neurological survival and the two resuscitation practices are summarized for each quartile.
| RISK-STANDARDIZED RATES OF SURVIVAL TO HOSPITAL ADMISSION | |||||
|---|---|---|---|---|---|
| Total | Quartile 1 | Quartile 2 | Quartile 3 | Quartile 4 | |
| (16.0% to 45.6%) | (16.0% to 24.4%) | (24.5% to 27.2%) | (27.3% to 30.1%) | (30.2% to 45.6%) | |
| N = 764 | n = 191 | n = 191 | n = 191 | n = 191 | |
|
| |||||
| Number of OHCA cases | |||||
| Mean ± SD | 338.1 ± 663.3 | 211.6 ± 382.7 | 281.2 ± 496.1 | 321.2 ± 660.8 | 538.6 ± 936.8 |
| Median (IQR) | 124.5 (59.0, 289.5) | 95.0 (56.0, 200.0) | 102.0 (47.0, 274.0) | 111.0 (58.0, 284.0) | 181.0 (89.0, 564.0) |
| Favorable neurological survival | |||||
| Mean ± SD | 8.8 ± 4.8 | 5.7 ± 3.0 | 8.1 ± 4.1 | 10.1 ± 4.7 | 11.4 ± 5.2 |
| Median (IQR) | 8.4 (5.3, 11.4) | 5.3 (3.6, 8.0) | 7.9 (5.1, 10.4) | 9.4 (6.7, 12.8) | 11.0 (7.4, 14.7) |
|
| |||||
| EMS PRACTICES | |||||
|
| |||||
| Mean EMS Response Time, mins | |||||
| Mean ± SD | 10.2 ± 3.2 | 12.0 ± 3.4 | 10.1 ± 3.0 | 9.6 ± 2.8 | 9.0 ± 2.6 |
| Median (IQR) | 9.6 (8.1, 11.5) | 11.5 (9.7, 13.7) | 9.8 (8.2, 11.3) | 9.3 (8.1, 10.7) | 8.7 (7.5, 10.0) |
| Missing | 56 | 10 | 19 | 14 | 13 |
| *ALS TOR definition without meeting futility criteria, % | |||||
| Mean ± SD | 22.4 ± 14.0 | 27.9 ± 16.1 | 21.9 ± 13.6 | 21.0 ± 13.1 | 18.9 ± 11.4 |
| Median (IQR) | 21.8 (11.1, 32.4) | 29.1 (14.6, 38.9) | 21.3 (9.9, 32.4) | 19.1 (10.8, 30.8) | 19.3 (9.4, 28.1) |
| Universal TOR definition without meeting futility criteria, % | |||||
| Mean ± SD | 13.7 ± 10.0 | 18.2 ± 12.0 | 13.7 ± 9.7 | 12.6 ± 9.1 | 10.2 ± 7.1 |
| Median (IQR) | 12.6 (5.5, 19.7) | 18.4 (9.2, 26.5) | 12.7 (4.7, 20.5) | 11.6 (5.2, 19.0) | 9.6 (3.7, 15.3) |
The 4-variable ALS TOR criteria was the main TOR variable in the primary analysis.
Abbreviations: ALS, advanced life support; EMS, emergency medical service; IQR, interquartile range; SD, standard deviation; TOR, termination of resuscitation
Figure 3. Mean EMS Response Time and EMS Agency Rate of Survival to Hospital Admission.
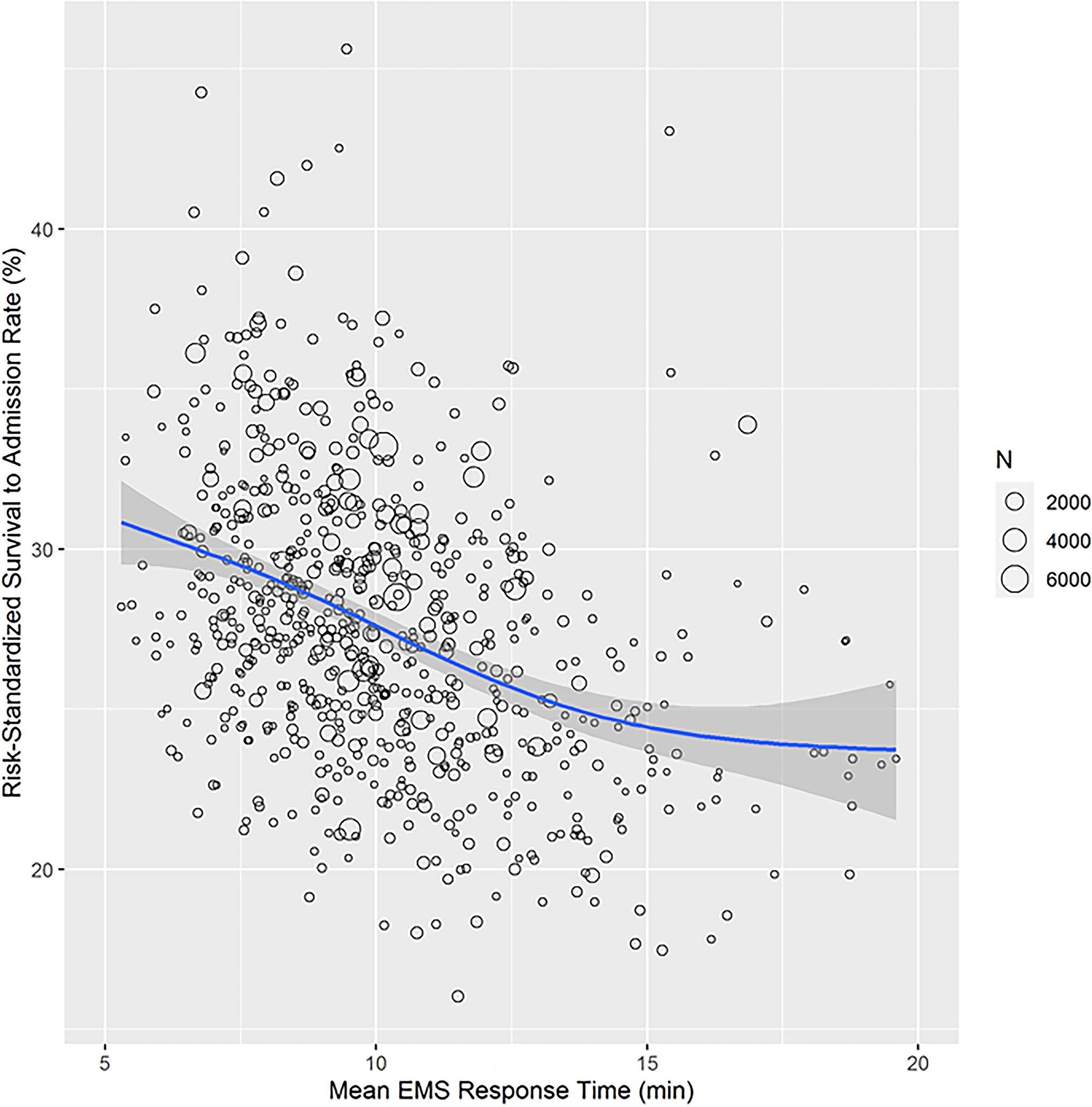
In this scatterplot, each dot represents a unique EMS agency, and the size of the dot is weighted based on the number of OHCA cases at that EMS agency. The blue line is the average EMS agency rate of OHCA survival for a given mean EMS arrival time, and the shaded region is the 95% confidence interval. EMS agency rates of survival to hospital admission are risk-standardized. Abbreviations: EMS, emergency medical services; OHCA, out-of-hospital cardiac arrest.
Figure 4. EMS Agency Rate of TOR Without Meeting Futility Criteria and Rate of Survival to Hospital Admission.
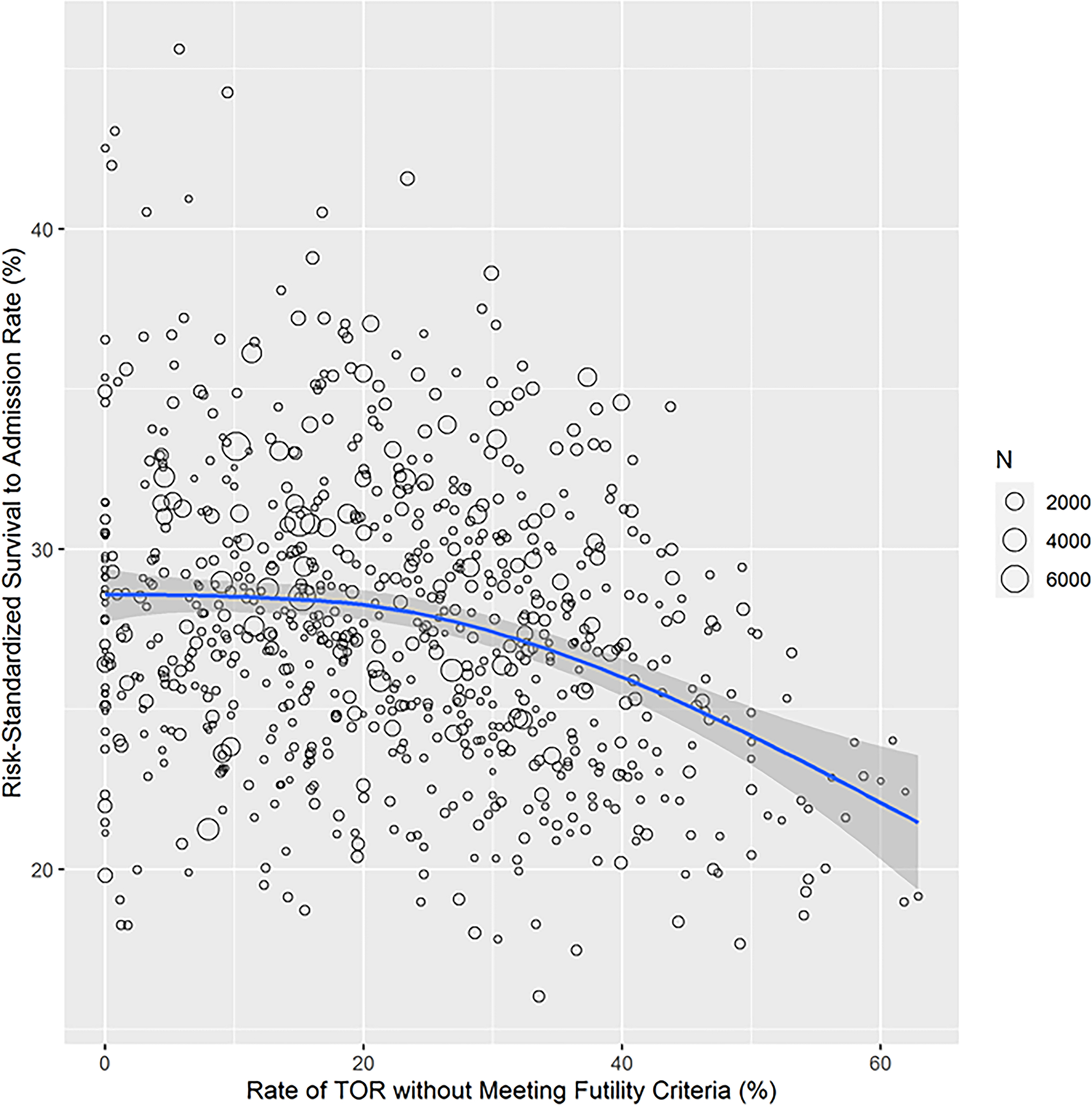
In this scatterplot, each dot represents a unique EMS agency, and the size of the dot is weighted based on the number of OHCA cases at that EMS agency. The blue line is the average EMS agency rate of OHCA survival for a given rate of TOR without meeting futility criteria. The shaded region is the 95% confidence interval. EMS agency rates of survival to hospital admission are risk-standardized. Abbreviations: EMS, emergency medical services; OHCA, out-of-hospital cardiac arrest; TOR, termination of resuscitation.
After adjustment for patient characteristics, there was significant variation in EMS agency rates of survival to hospital admission for OHCA. The MOR was 1.35 (95% CI: 1.32, 1.39), which suggests that the odds of survival of two patients with identical covariates varied by 35% at one randomly selected EMS agency vs. another. Both EMS agency response times and ALS TOR rates among patients not meeting futility criteria were each (P<0.001) associated with site-level rates of survival to hospital admission. Sensitivity analyses using the 3-variable Universal TOR futility criteria demonstrated a similar association between EMS agency rates of TOR without meeting futility criteria and survival to hospital admission, with P<0.001 (see Table 2). Also, there was no interaction between an EMS agency’s urbanicity with EMS response time or ALS TOR rates without meeting futility criteria for the outcome of survival to hospital admission (P for interactions of 0.35 and 0.33, respectively), suggesting that the associations between these two EMS practices and survival were similar in urban areas, urban clusters, and rural areas. Finally, we confirmed that there was a high correlation between EMS agency risk-standardized rates of survival to hospital admission and favorable neurological survival (Spearman’s coefficient = 0.81), highlighting the robustnes of our focus on survival to hospital admission (see also Table 2).
DISCUSSION
Within a large national registry representing a catchment area of approximately 51% of the U.S. population, we found that rates of survival to hospital admission for OHCA varied substantially across EMS agencies. Although the median risk-standardized rate of survival to hospital admission for OHCA was 27.3%, survival rates ranged widely from 16.0% to 45.6%. We also found that two resuscitation practices were associated with EMS agency rates of OHCA survival. Collectively, our study suggests that significant variation in OHCA survival exists at the EMS agency level and may be, in part, due to modifiable resuscitation practices at the EMS agency level.
Although variability in OHCA survival has been previously described at the level of counties and geographical regions,4,5 these units are typically not modifiable and are often served by multiple EMS agencies. One study using data from CARES previously described county-level variation in rates of survival to hospital discharge for OHCA, which ranged from 3.4% to 22.0%. Within the Resuscitation Outcomes Consortium, others have found that unadjusted rates of survival for OHCA varied widely from 3.0% to 16.3% across 10 geographical regions in the U.S. To our knowledge, this study is the first to describe variation in OHCA survival at the EMS agency level—the core reporting unit of the CARES registry. Our work extends the prior literature as it examined variation in rates of survival to hospital admission for OHCA—the outcome within the locus of control of EMS agencies, focused the evaluation of survival variation at the level of the EMS agency (which is potentially modifiable) instead of a geographical unit (which typically is not modifiable), and quantified the extent of this variation with the MOR.
The initial TOR rules for futility were developed to assist EMS agency providers in making difficult decisions about cessation of resuscitative efforts. While there are reasons to declare TOR when not all futility criteria are met (e.g., witnessed arrest but no ROSC after 60 minutes of CPR), we would expect that these scenarios should occur at relatively similar frequencies across EMS agencies. In fact, we found that EMS agencies with the lowest risk-standardized rates of survival to hospital admission had a ~48% higher rate of declaring TOR without meeting ALS futility criteria, as compared with those with the highest rates of risk-standardized survival (27.9% vs. 18.9%). This relationship was similar using the 3-variable Universal TOR criteria. These findings suggest that reducing rates of TOR without meeting futility criteria has the potential to improve rates of OHCA survival at EMS agencies in the lowest quartile of OHCA survival and could be explored as an EMS agency performance measure if more granular information on TOR decisions were to be collected.
In similar fashion, EMS response times were substantially longer for EMS agencies in the lowest quartile of OHCA survival, and there was an inverse graded relationship between EMS response times and OHCA survival between 7 and 15 minutes—the time range for most EMS agencies (see Figure 3). Previous studies have similarly reported the association between EMS response time and survival;18,19 however, our work confirms and extends this historical relationship as it is a more contemporary report involving a larger cohort of both patients and EMS agencies. Although delays could also be partly structural in nature (e.g., traffic patterns in a city), we did not find an interaction between an EMS agency’s urbanicity and response times.
Our study should be interpreted in the context of the following limitations. First, although we demonstrated that rates of survival to hospital admission varied significantly between two randomly selected EMS agencies, the factors which underlie this variation remain poorly defined. In CARES, resuscitation practices and protocols among EMS agencies are not routinely collected, precluding our ability to evaluate other site-level measures associated with rates of survival to hospital admission for OHCA. Second, patient comorbidities are not captured within CARES, given that most patients die before hospital admission making this information impractical to collect. It is possible that some of the unexplained variation may also reflect differences in patient case-mix across EMS agencies, even as we were able to adjust for age, demographics, and cardiac arrest factors. Third, the reasons for TOR in those without meeting futility criteria are not collected in CARES and deserve further study to better understand variation in this practice across EMS agencies as it was associated with site-level rates of survival. Finally, our analyses were conducted among EMS agencies within CARES and our findings may not be generalizable to all EMS agencies within the U.S.
In conclusion, we found that survival after OHCA varies widely across EMS agencies. Certain EMS agency resuscitation factors such as EMS response times and TOR practices were associated with agency-level rates of survival to hospital admission, suggesting potentially modifiable practices which can improve OHCA rates of survival.
Supplementary Material
What Is Known
Over 350,000 out-of-hospital cardiac arrests (OHCA) occur annually in the United States, and nearly all are assessed by EMS personnel.
There is substantial variability in survival rates for OHCA by county and geographic region, but the extent to which OHCA survival varies by EMS agency is unknown.
What The Study Adds
Rates of cardiac arrest survival to hospital admission varied widely at the level of EMS agencies (range 16% to 46%)—with the odds of survival for a patient with an OHCA varying by 34% between two randomly selected EMS agencies.
We found that EMS agencies with the highest survival rates for OHCA had the fastest response times and lowest rates of termination of resuscitation in the field for patients not meeting futility criteria.
Our studies suggest that certain modifiable EMS agency practices may distinguish EMS agencies which excel at OHCA survival.
SOURCES OF FUNDING:
Dr. Raul Angel Garcia is supported by the National Heart, Lung and Blood Institutes of Health under Award Number T32HL110837. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
NON-STANDARD ABBREVIATIONS AND ACRONYMS:
- CARES
Cardiac Arrest Registry Enhancing Survival
- CPR
cardiopulmonary resuscitation
- EMS
Emergency Medical Services
- MOR
median odds ratio
- OHCA
out-of-hospital cardiac arrest
- ROSC
return of spontaneous circulation
- TOR
termination of resuscitation
Footnotes
DISCLOSURES: None of the authors have any conflicts of interest or disclosures to report.
SUPPLEMENTAL MATERIALS: Figure S1.
REFERENCES
- 1.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, et al. Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation. 2019;139:e56–e528. doi: doi: 10.1161/CIR.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 2.Yan S, Gan Y, Jiang N, Wang R, Chen Y, Luo Z, Zong Q, Chen S, Lv C. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Critical care (London, England). 2020;24:61. doi: 10.1186/s13054-020-2773-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan Paul S, McNally B, Tang F, Kellermann A. Recent Trends in Survival From Out-of-Hospital Cardiac Arrest in the United States. Circulation. 2014;130:1876–1882. doi: 10.1161/CIRCULATIONAHA.114.009711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Girotra S, van Diepen S, Nallamothu BK, Carrel M, Vellano K, Anderson ML, McNally B, Abella BS, Sasson C, Chan PS, et al. Regional Variation in Out-of-Hospital Cardiac Arrest Survival in the United States. Circulation. 2016;133:2159–2168. doi: 10.1161/CIRCULATIONAHA.115.018175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morrison LJ, Verbeek PR, Vermeulen MJ, Kiss A, Allan KS, Nesbitt L, Stiell I. Derivation and evaluation of a termination of resuscitation clinical prediction rule for advanced life support providers. Resuscitation. 2007;74:266–275. doi: 10.1016/j.resuscitation.2007.01.009 [DOI] [PubMed] [Google Scholar]
- 7.Panchal Ashish R, Bartos Jason A, Cabañas José G, Donnino Michael W, Drennan Ian R, Hirsch Karen G, Kudenchuk Peter J, Kurz Michael C, Lavonas Eric J, Morley Peter T, et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S366–S468. doi: 10.1161/CIR.0000000000000916 [DOI] [PubMed] [Google Scholar]
- 8.Schneiderman LJ. Defining Medical Futility and Improving Medical Care. Journal of bioethical inquiry. 2011;8:123–131. doi: 10.1007/s11673-011-9293-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Termination of resuscitation in nontraumatic cardiopulmonary arrest. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2011;15:542. doi: 10.3109/10903127.2011.598621 [DOI] [PubMed] [Google Scholar]
- 10.McNally B, Stokes A, Crouch A, Kellermann AL. CARES: Cardiac Arrest Registry to Enhance Survival. Annals of emergency medicine. 2009;54:674–683.e672. doi: 10.1016/j.annemergmed.2009.03.018 [DOI] [PubMed] [Google Scholar]
- 11.McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, Sasson C, Crouch A, Perez AB, Merritt R, et al. Out-of-hospital cardiac arrest surveillance --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005--December 31, 2010. Morbidity and mortality weekly report Surveillance summaries (Washington, DC : 2002). 2011;60:1–19. [PubMed] [Google Scholar]
- 12.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D’Este K, Finn J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004;110:3385–3397. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein H, Browne W, Rasbash J. Partitioning variation in multilevel models. Understanding Statistics. 2002;1:223–232. [Google Scholar]
- 14.Goldstein H Multilevel Statistical Models. 3rd ed. London, UK: Arnold Publishers; 2003. [Google Scholar]
- 15.Normand S-LT, Glickman ME, Gatsonis CA. Statistical Methods for Profiling Providers of Medical Care: Issues and Applications. Journal of the American Statistical Association. 1997;92:803–814. doi: 10.1080/01621459.1997.10474036 [DOI] [Google Scholar]
- 16.Ash AS FS, Louis TA, Normand SL, Stukel TA, Utts J. Statistical issues in assessing hospital performance: Commissioned by the Committee of Presidents of Statistical Societies. https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/downloads/statistical-issues-in-assessing-hospital-performance.pdf. 2012.
- 17.U.S. Census Bureau. 2010 Census urban and rural classification and urban area criteria. https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural/2010-urban-rural.html. 2010.
- 18.Holmén J, Herlitz J, Ricksten SE, Strömsöe A, Hagberg E, Axelsson C, Rawshani A. Shortening Ambulance Response Time Increases Survival in Out-of-Hospital Cardiac Arrest. Journal of the American Heart Association. 2020;9:e017048. doi: 10.1161/JAHA.120.017048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keeffe C, Nicholl J, Turner J, Goodacre S. Role of ambulance response times in the survival of patients with out-of-hospital cardiac arrest. Emergency Medicine Journal. 2011;28:703. doi: 10.1136/emj.2009.086363 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


