Abstract
Migraine is prevalent, disabling, and peaks during people's peak productive years. The impact of migraine on people's professional lives, work productivity, and interpersonal relationships at work eventually affects everyone, has a significant detrimental effect on people with migraine, and a huge cost in terms of lost productivity. People with migraine want to work, so they do their best to work despite the varied migraine related and associated symptoms. Most of migraine-related productivity loss (89%) is due to presenteeism. People are less than half effective during a migraine attack due to the pain, migraine symptoms, attack unpredictability, migraine comorbidities, emotional impact, under-diagnosis and under-management, and the stigma. Migraine-related productivity loss may negatively affect people's career choice, job status and/or security, financial status, work relationships, mood, and confidence. Migraine is estimated to represent 16% of total US workforce presenteeism. Thankfully, there are ways to help support people with migraine in the workplace and increase their productivity such as: workplace migraine education programs, workplace migraine education and management programs, migraine-friendly work environment, migraine treatment optimization and advocacy. The example of the successful workplace migraine education and management program developed and run in collaboration between Fujitsu, the Japanase Headache Society, and the International Headache Society Global Patient Advocacy Coalition is discussed.
Keywords: Headache, Disability, Absenteeism, Presenteeism, Productivity, Stigma, Accommodation
Highlights
-
•
Migraine-related productivity loss is costly to people with migraine, to employers, and to everyone in one way or another.
-
•
Workplace migraine education and/or management programs and migraine-friendly environment help people with migraine at work.
-
•
Neurologists can help support their patients in the workplace and get involved in advocacy in many ways.
1. Introduction
“If you didn't have migraine, how would your life be different?” and “What are your expectations for this visit?” [1]. These questions help neurologists understand the many ways migraine impacts their patients' lives and help target the visit on what matters to the patients. Despite acute and/or preventive treatment, migraine negatively impacts the lives of 90% of people with migraine in many domains including work, cognitive function, and emotional health [1]. Migraine is the leading cause of disability in adults under age 50 years and the second leading cause of disability at all other ages in the world [2,3]. About one in four persons with migraine have moderate to severe disability ranging from 12% in Europe, 19% in Asia, 22% in South America, to 32.3% in North America [[4], [5], [6], [7]]. Migraine peaks during people's most productive years and as a result negatively affects their career and professional lives [1,8,9].
The aim of this review is to present the factors contributing to migraine-related disability, the personal and economic impact of migraine disability, and ways to support people with migraine in the workplace. This information will hopefully serve as a resource for neurologists when educating patients and letting them know they are not alone, coming up with a treatment plan such as acute therapies (medications or devices) to use at work and acute treatment to use at home or writing a letter to a supervisor to support a migraine-related reasonable accommodation, referring patients and/or companies to organizations and/or programs who can help, getting involved in the community and in advocacy efforts. Such information (e.g. economic burden of migraine-related productivity loss) helps put clinical care in a broader context. Addressing migraine-related productivity loss helps patients have a higher quality of life and employers be more successful, which helps the advocacy directed at employers and companies. Since the publication of the scoping review of workplace interventions and work factors associated with migraine-related productivity, there have been two main studies on migraine education and management programs in the workplace that are discussed in this review: one done at a pharmaceutical company in Switzerland, and one done at an information technology company in Japan [[10], [11], [12]].
1.1. Ways migraine negatively impacts work productivity (see Table 1)
Table 1.
Factors contributing to migraine-related decreased work productivity and ways to mitigate them.
| Factors contributing to migraine-related decreased work productivity | Ways to mitigate them |
|---|---|
| Migraine pain and symptoms |
|
| Unpredictability of attacks |
|
| Migraine comorbidities |
|
| Emotional impact of migraine |
|
| Under-diagnosis and under-management |
|
| Stigma |
|
People report being 46% effective when working during a migraine attack [13]. Patients ranked pain as the most disabling migraine attack symptom, followed by difficulty in thinking and worsening with mental effort, then photo- and phono-phobia, and last nausea [14].
Migraine can negatively impact work productivity even on non-headache days as 40% of people with migraine have interictal symptoms such as cognitive impairments (e.g. deficits in attention, executive function, processing speed, and memory) [15,16]. In addition to migraine-related cognitive dysfunction, cogniphobia may interfere with work productivity too [17].
The unpredictability of migraine attacks can be anxiety-provoking and makes it difficult for people with migraine to reliably plan their work. The fear of triggering another attack or having another attack may dissuade people with migraine from attending work meetings and outings [18]. The resulting social withdrawal may contribute to more severe symptoms [19].
Migraine comorbidities contribute to migraine-related decreased work productivity. Depression, depressive symptoms without fulfilling the criteria of a formal diagnosis, anxiety, anxiety symptoms without fulfilling the criteria of a formal diagnosis, sleep disorders, pain catastrophizing, and chronic pain are independently associated with work absenteeism and presenteeism and increased disability [[20], [21], [22], [23], [24], [25], [26], [27], [28], [29]].
Migraine remains underdiagnosed and undertreated [30,31]. Nearly three quarters of employees never consulted a doctor for migraine: 72% of employees in a survey of 2458 workers at an information technology firm in Japan and 74.7% of employees with migraine in a survey of 522 workers from 8 information technology companies in Korea [6,11]. And yet, about two third (65%) thought they could not manage their headaches by themselves [11]. In June 2018, Fujitsu, a large information technology company, conducted an in-house survey among Fujitsu employees in cooperation with the International Headache Society, World Health Organization (WHO), and Japanese Headache Society. The survey was designed to evaluate the impact of chronic headache disorders in the workplace [15]. Of the 2500 employees surveyed, 85% had experienced headache. Of those who experienced headache, 84% had never been treated.
The stigma against migraine is ubiquitous and interferes with the work productivity of people with migraine [[32], [33], [34]]. Perceived workplace difficulties are associated with a higher Migraine Disability Assessment (MIDAS) score [35]. Stigma comes from interactions with coworkers, family, friends, doctors, from institutions such as health insurance agencies and media, from the negative connotations of headache and migraine in our language, and from the ways migraine and other headache diseases are represented in language and imagery [[36], [37], [38]]. Stigma can also be internalized and lead to anxiety, fear, guilt, or shame regarding one's disease [36]. Stigma leads to discrimination, loss of status, loss of relationships, prejudice, presenteeism, and reduced pay [32,33,36]. There is more stigma against chronic migraine than other neurological diseases [32,[39], [40], [41]]. In a survey of almost 200,000 U.S. workers, only 22% of employers thought that migraine was a serious enough condition to justify an absence from work [42]. In a survey of a representative US sample of 2000 participants without migraine who knew at least one person with migraine, 32.4% thought that people with migraine exaggerated their symptoms, 35.5% answered that someone's migraine attacks were caused by their own unhealthy behavior(s), 39.1% answered that people with migraine hid their disease, 29% answered that people with migraine made things difficult for their coworkers and 31.1% answered that people use migraine as an excuse to get out of school or work commitments [43]. As a result of the stigma, more than half of workers who are absent because of headache do not disclose it is because of headache [44].
1.2. Personal impact of migraine-related decreased productivity
In the Migraine in the Workplace Survey advertised on the social media of the Migraine Association of Ireland in July and August 2021, migraine had a direct impact in the professional life of 82% of the 400 respondents due to a necessary change in career or career choice, having to work part time, decreased confidence, increased stress, increased anxiety, difficulty with time management and clarity of thought. About one in five (22%) of the 400 respondents had to change career due to migraine. When participants were asked to free text answer the question “What one change in your workplace do you feel would help you?,” the most common theme was awareness/understanding (30%) followed by supportive work environment (26%), and then flexibility (16%). Of those who wished for increased understanding of migraine in the workplace, 85% meant that their coworkers would understand that migraine is more than “just” a headache, 11% meant that their coworkers would be supportive, and 4% meant that their coworkers would understand how the environment may have an impact on migraine. Less than half (47%) of all respondents felt supported in their workplace. Their colleagues thought that migraine was “just” a headache, tolerated people with migraine rather than supported them, lacked understanding about how disabling migraine can be. Some reported that their immediate coworkers were supportive, but not management. Migraine-related productivity loss impacts work relationships, confidence, guilt, and fear of getting fired [4,15].
A vicious circle can settle: migraine disability and stigma hinder people with migraine from achieving their full occupational potential and hence may lead to a lower socioeconomic status, which in turns is associated with more life stressors, less medical care, and worse migraine [45,46].
1.3. Economic impact of migraine-related productivity loss
The significant economic impact of migraine-related productivity loss at work may be difficult to notice and quantify because 89% of it stems from presenteeism, i.e. working during a migraine attack and pushing through without being able to be as productive as usual due to migraine symptoms [47]. There is no standardized methods to measure presenteeism yet [10]. The cost of presenteeism to employers is estimated three to ten times more than absences [[47], [48], [49]]. In a four-year-long study of 7959 employees at a large US health care system across six locations, migraine was the second most costly condition in terms of presenteeism costing more than $2 million annually among 22 common health conditions (such as asthma, back pain, anxiety, stroke, heart disease, hypertension, metabolic diseases, cancer) after allergies. [50]. Extrapolating from those results, migraine is estimated to cause 16% of US workforce presenteeism with an estimated annual cost of $240 billion [50].
As headache frequency increases, migraine-related productivity loss increases. A study of 5916 employees at a car manufacturing factory in Turkey showed that workers with 10–14 headache days per month had on average 2 absences and 46 days with migraine-related impaired productivity per year compared to 3.5 days of absences and 87 days with decreased productivity for those with at least 15 days of headache per month [51]. In the American Migraine Prevalence and Prevention study, 29% of the 5997 participants with more than 10 headache days per month accounted for 49% of overall lost productive time [49].
In 2018, the migraine-related productivity loss to Fujitsu in terms of abstenteeism and presenteeism was estimated at 900 USD per year per employee with a headache disease. The cost was even higher for the employees with migraine (approximately 2300 USD). The total cost was estimated at 197 million USD per year for all employees, representing approximately 1% of the total annual salary paid to all employees.
1.4. Ways to support people with migraine in the workplace and help alleviate migraine-related productivity loss
1.4.1. Migraine education programs in the workplace
Migraine education programs in the workplace increased productivity by 29 to 36% in six prospective cohort studies in the USA. They decreased absences by 25%, decreased the number of days worked with a migraine attack by 32%, and increased productivity at work during a migraine attack by 10%, and decreased stigma [10,12,[52], [53], [54], [55], [56], [57], [58]]. Migraine education programs have three main goals: 1) raise awareness, provide education, and break down stigma, 2) increase migraine diagnosis, 3) support people with migraine in the workplace through education about treatment optimization and improvement of work relationships [59]. Without company-wide efforts to raise awareness to all the employees including those without migraine, there is a significant burden on people with migraine to do the “migraine talk,” and educate others on their disease, and risk discrimination or other negative consequences [60]. One way of mitigating the stigma against migraine is through rebranding of the disease via wide-spread public education, non-judgmental language and imagery, and advocacy [44]. It is helpful to become familiar with the local and global resources that can organize migraine education programs in the workplace for the companies patients work for.
1.4.2. Migraine education and management programs in the workplace
Five prospective cohort studies (two in the USA, one in Spain, one in Switzerland, and one in France) showed that migraine education and management programs in the workplace improve productivity by cutting absences in half, increasing productivity at work during a migraine attack by about 36 to 59%, and decreasing the costs of migraine-related productivity loss [10,11,52,[61], [62], [63], [64]]. There are 3 main steps to migraine education and management programs: 1) company-wide education campaign, 2) voluntary and anonymous migraine evaluation, 3) optional migraine management programs or referral offered to employees diagnosed with migraine [52]. The investment required for such programs varies based on the local health care system and coverage of medications offered, but they were shown to be cost-effective in studies so far. The Spanish Postal Service mailed a voluntary health survey to its employees [65]. Those who screened positive for migraine were offered to come to the occupational health services for an evaluation and migraine management by a Physician [65]. The Spanish Postal Service migraine education and management program in the reduced absences by 53%, increased productivity on days worked with migraine attack from 59% to 94.8%, which reduced the costs of migraine-related productivity loss by almost 90% [65]. A Swiss pharmaceutical company launched a program that started with company-wide migraine education via emails, info booths, lectures, newsletters, brochures [11]. Interested employees could choose to be medically evaluated for migraine [11]. Those who were found to have migraine were offered treatment and virtual coaching sessions for 6 months [11]. This program costed about $1000 to the employer per participant for 6 months, decreased absences by nearly 50%, increased productivity on migraine days at work (a reduction from 3.9 to 1.6 days per month with at least 50% reduced productivity at work due to migraine), which led to a total productivity benefit of 10.8 more workdays per year per employee, an almost 5 times positive return on investment [11]. Encourage patients to investigate their employee health resources to see if there are any programs in place to help with education and management of migraine in the workplace. In an anonymous web survey of 3342 patients, 43.71% of employees were aware of the occupational health service offered by their company [66].
1.4.3. Migraine-friendly workplace
Adaptations to the work environment and atmosphere, quantitative, emotional, and social work demands support people with migraine and may help decrease migraine-related productivity loss [10]. Job satisfaction, social support (especially from supervisor), positive work atmosphere, and autonomy are positively associated with productivity in workers with migraine [10,33,[67], [68], [69], [70]]. Migraine-friendly work environment such as natural lights, noise reduction, scent free areas, access to water and restroom, regular breaks, air quality are positively associated with productivity [10,68,71] [72,73]. High quantitative work demands (e.g. high workload, long work hours, inflexible schedule) are associated with decreased productivity [10,67,73,74]. To our knowledge, only one prospective study of two selected shift workers with formally diagnosed chronic refractory migraine assessed the impact of day and of night shifts on productivity for people with migraine, and found an association between night shifts and work absences [75]. Regarding social demands at work, a survey of 108 participants followed at a Headache Center in Serbia showed a positive association between MIDAS score and regular contact with at least 10 other people at work [76].
1.4.4. Advocacy
Health advocacy is an essential part of medicine [77]. It is “a proactive way of transforming ideas into actions and actions into meaningful reality.” It is an altruistic way to speak up for health equity. It stems from the recognition that health and wellness also depend on factors beyond the clinical context [77]. To support people with migraine and headache disorders in the workplace, advocacy efforts should be aimed at 1) education of the general public, employees, employers, general practitioners, occupational health physicians to increase understanding, decrease stigma, and optimize treatment while waiting to be seen by a headache specialist if needed 2) research to improve our understanding and management of the disease, 3) legislations to provide support for people in the workplace and support for people who are unable to work due to migraine or other headache disease, and 4) equitable access to headache care.
The recognition of the significant burden of headache diseases and the need to include patient advocates led to the first Global Patient Advocacy Summit in September 2017 [78]. Patients, health/neurological/pain/advocacy organizations, doctors, nurses, pharmaceutical manufacturers, scientists, and regulatory agency representatives from around the world discussed ways to address issues that are important for people with headache diseases [78]. The International Headache Society Global Patient Advocacy Coalition (IHS-GPAC) was created to “understand and promote the global, regional, and local interests of people with recurrent headache disorders” [78]. One of the priorities of the IHS-GPAC was to create a migraine at work fitness program to empower employees to seek treatment, reduce stigma, and ensure access to care [79].
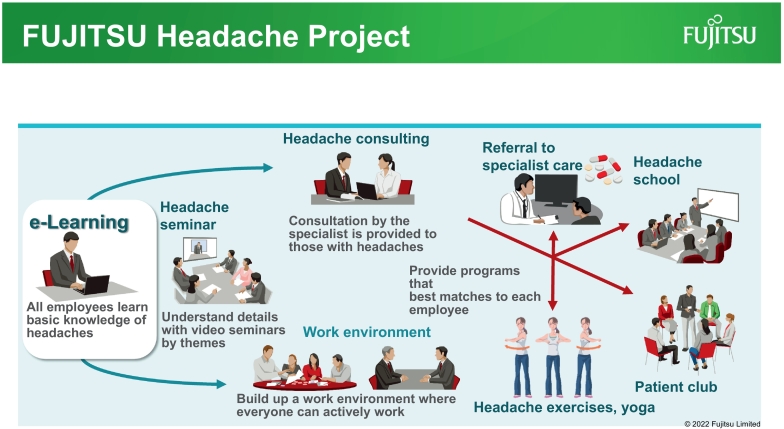
Fujitsu collaborated with the IHS-GPAC and Japanese Headache Society to launch the “FUJITSU Headache Project,” a headache education and management program in the workplace to improve quality of life and boost work productivity and aimed to create a workplace where people who have headache can work comfortably and with peace of mind. It is now globally available to all employees with a goal to reach approximately 80,000 Fujitsu Group employees in Japan. Fujitsu's efforts were recognized by the IHS-GPAC as a model case of corporate measures to support employees living with headache diseases (Fig. 1).
Fig. 1.
Overview of the FUJITSU Headache Project.
Some of the preliminary results were reported by Fujitsu at the press conference as follows [80].
1.4.4.1. e-Learning
Employees of Fujitsu and its group companies had access to the e-learning via the intranet for a month. Employees could take e-learning at any time, which took about one hour to complete. An invitation and reminder emails were sent to employees. As many as 73,432 employees (95%) completed the one-hour e-learning and responded to the questionnaires at the end of the learning. Of all the employees responded, 30.3% answered that e-learning program was “very useful” and 60.5% answered the program was “useful.” Nearly three quarters (72.5%) of the employees answered that their understanding and attitude toward migraine had changed. Before the e-learning less than half (46.8%) considered migraine a disease serious enough to cause problems in daily life, but after the e-learning more than two thirds (70.6%) of the participants considered migraine being a serious disease. More than three quarters (76.9%) of the participants responded that their attitude toward colleagues suffering from migraine will change.
1.4.4.2. Headache exercises
Participants were also instructed self-care approaches including the muscle stretching exercise to relieve tension-type headache and the trigger-point stretching at the neck (giving mild C2 stimulation) to help with chronic migraine prevention.
1.4.4.3. Headache consultation
Among 73,432 employees who completed e-learning, 376 (0.5%) were offered to receive a virtual personal headache consultation of 30 min by staff physicians on a first-come first-serve basis. The content of headache consultation varied according to individual patient needs. Patients with headache diseases wanted to know their headache diagnoses, medical treatment options, and nonpharmacological selfcare approaches to prevent migraine. One of the purposes of the virtual personal headache consultation program was to see the real-world situation of migraine at work and to evaluate any discrepancy from questionnaire study data. Consultation is continuing as a part of the service-program by the health promotion department staff.
About two third (67.3%) of the 376 employees who had a virtual personal headache consultation was advised to visit the headache clinic in person. More than half (56%) of those 376 employees went to the headache clinic and began receiving medical care for migraine with good outcomes. A typical example was a lady with chronic migraine whose work productivity was negatively affected by various migraine-related symptoms, yet she was very patient and hard-working. Since she has been receiving migraine treatment through the headache clinic, the impact of migraine on her functioning / quality of life decreased to 10 to 20% of the pretreatment. Her senior colleagues congratulated her success in regaining healthy work.
1.4.5. Disability
Unfortunately, despite current migraine treatment options, patient's best efforts, and neurologist's clinical and advocacy care, some people need to apply for either intermittent or permanent disability on the basis of migraine.
The disability legislations vary from country to country. To take the example of the US, migraine is recognized as a disability and people with migraine have the right to reasonable accommodations in the workplace according to the 2008 amendment of the Americans with Disabilities Act (ADA) [81,82]. Examples of reasonable accommodations for migraine include flexible schedule, ability to work from home when possible, scent-free environment, optimization of desk ergonomics or light sensitivity glasses [[82], [83], [84]].
If medical treatment optimization and reasonable accommodations are not sufficient, applying for the Family and Medical Leave Act (FMLA) can be considered. The FMLA provides up to 12 weeks of job-protected, intermittent unpaid leave during any one-year period for people with migraine currently employed by companies of at least 50 employees [82].
Unfortunately, some people need to apply for disability, which is practically, financially, and emotionally difficult. It may interfere with the patients' ability to get adequate medical care and go back to the workplace later. It is technically difficult to apply for social security disability insurance (SSDI) on the basis of migraine. Migraine contributed to 5.6% of the total annual US. disability burden between 1997 and 2004 but only 0.3% of all SSDI claimants [85]. The Headache on the Hill and Alliance for Headache Disorders Advocacy (AHDA) are working on trying to improve the SSDI application process for people with headache diseases, which is important for people in the US and may serve as a model and example of advocacy for other countries. Dr. Robert Shapiro created Headache on the Hill in the context of his American Academy of Neurology Palatucci Advocacy Leadership Forum in 2007. In addition to the constant work all year long from the team, physicians and patients meet with congressional representatives & staffers to advocate for equitable policies for people living with headache disorders one day a year, usually in February [85]. The AHDA was created in 2008 to help support the advocacy work of Headache on the Hill [85]. Applying for SSDI benefits occurs in several steps. During step 2, claimants need to prove that they have a severe “Medically Determinable Impairment” (MDI) (ie, a disease that prevents them from being able to work). However, a claimants' symptoms cannot be used as evidence for MDI, which would make it virtually impossible to establish an MDI on the basis of a primary headache disorder. Thanks to the advocacy efforts of the AHDA and the Headache on the Hill team, a Social Security Ruling (SSR) was issued in August 2019 to provide some guidance for step 2 of the SSDI application for claimants with headache disorders [86]. During step 3, SSDI claimants must compare their MDI to the impairments listed for their disease in the Social Security Administration (SSA) Listing of Impairments (“Blue Book”). Since no headache diseases are listed in the blue book, claimants with headache disorders have to compare their impairments to epilepsy [85,86]. Further AHDA and headache on the hill advocacy efforts led to a Freedom of Information Act (FOIA) Request in 2018 to request all SSA documents relevant to SSA refusal to include headache disorders in the Listing of Impairments, but all 1377 documents withheld “executive privilege” exemption, so now a federal law suit is under way [85]. It is important for doctors to have some knowledge regarding patients' rights in terms of reasonable accommodations, medical leave, and disability in their country to help educate and empower patients, support them and provide them with letters and/or other required documentations in their requests, provide them with resources that can help provide them with support and/or guidance, and maybe also get involved in advocacy.
2. Conclusion
Migraine is a leading cause of disability in the world, especially for people during their peak productive years in the workforce. Migraine disability is multifactorial; it comes from the pain and symptoms themselves, the unpredictability of the attacks, migraine comorbidities, the emotional impact of migraine, its underdiagnosis and undermanagement, and the pervasive stigma against migraine. Migraine-related productivity loss is extremely costly to people with migraine, to employers, and to everyone in one way or another. There are ways we can support people with migraine in the workplace such as migraine education programs in the workplace, employer sponsored migraine education and management/referral programs, migraine-friendly work environments, headache care access and treatment optimization, and advocacy.
CRediT authorship contribution statement
Olivia Begasse de Dhaem: Conceptualization, Writing – original draft, Writing – review & editing, Visualization. Fumihiko Sakai: Writing – original draft, Writing – review & editing, Visualization.
Declaration of Competing Interest
Olivia Begasse de Dhaem serves as an Executive Editor for the Pain Medicine Journal and as a consultant for Neurolytic Healthcare.
Fumihiko Sakai is consultant for Amgen, Lilly and Ohtsuka.
He received a grant with his team for the international research cooperation promotion project from the Japan Public Health Association, which supported the publication of a prior manuscript: Shimizu T, Sakai F, Miyake H, Sone T, Sato M, Tanabe S, et al. Disability, quality of life, productivity impairment and employer costs of migraine in the workplace. J Headache Pain. 2021 Apr 21;22 (1):29.
Both Olivia Begasse de Dhaem and Fumihiko Sakai are members of the Executive Committee of the International Headache Society Global Patient Advocacy Coalition (IHS-GPAC) for which they do not receive any funding.
This study was done independently of any company. The authors did not receive any compensation nor funding from corporate companies for this study. The authors did not receive any funding from Fujitsu. The results were obtained without influence from Fujitsu.
Contributor Information
Olivia Begasse de Dhaem, Email: begassededhaem@gmail.com.
Fumihiko Sakai, Email: fsakai@mist.dti.ne.jp.
References
- 1.Estave P.M., Beeghly S., Anderson R., Margol C., Shakir M., George G., et al. Learning the full impact of migraine through patient voices: A qualitative study. Headache. 2021;61(7):1004–1020. doi: 10.1111/head.14151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2016 headache collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the global burden of Disease study 2016. Lancet Neurol. 2018;17(11):954–976. doi: 10.1016/S1474-4422(18)30322-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steiner T.J., Stovner L.J., Vos T., Jensen R., Katsarava Z. Migraine is first cause of disability in under 50s: will health politicians now take notice? J Headache Pain. 2018;19(1):17. doi: 10.1186/s10194-018-0846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim B.K., Cho S.J., Kim C.S., Sakai F., Dodick D.W., Chu M.K. Disability and economic loss caused by headache among information Technology Workers in Korea. J Clin Neurol. 2021;17(4):546–557. doi: 10.3988/jcn.2021.17.4.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henry P., Auray J.P., Gaudin A.F., Dartigues J.F., Duru G., Lantéri-Minet M., et al. Prevalence and clinical characteristics of migraine in France. Neurology. 2002;59(2):232–237. doi: 10.1212/wnl.59.2.232. [DOI] [PubMed] [Google Scholar]
- 6.Lipton R.B., Manack Adams A., Buse D.C., Fanning K.M., Reed M.L. A comparison of the chronic migraine epidemiology and outcomes (CaMEO) study and American migraine prevalence and prevention (AMPP) study: demographics and headache-related disability. Headache. 2016;56(8):1280–1289. doi: 10.1111/head.12878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peres M.F.P., Queiroz L.P., Rocha-Filho P.S., Sarmento E.M., Katsarava Z., Steiner T.J. Migraine: a major debilitating chronic non-communicable disease in Brazil, evidence from two national surveys. J Headache Pain. 2019;20(1):85. doi: 10.1186/s10194-019-1036-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burch R.C., Buse D.C., Lipton R.B. Migraine: epidemiology, burden, and comorbidity. Neurol Clin. 2019;37(4):631–649. doi: 10.1016/j.ncl.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 9.Lipton R.B., Stewart W.F., von Korff M. Burden of migraine: societal costs and therapeutic opportunities. Neurology. 1997;48(3 Suppl 3):S4–S9. doi: 10.1212/wnl.48.3_suppl_3.4s. [DOI] [PubMed] [Google Scholar]
- 10.Begasse de Dhaem O., Gharedaghi M.H., Bain P., Hettie G., Loder E., Burch R. Identification of work accommodations and interventions associated with work productivity in adults with migraine: A scoping review. Cephalalgia. 2021;41(6):760–773. doi: 10.1177/0333102420977852. [DOI] [PubMed] [Google Scholar]
- 11.Schaetz L., Rimner T., Pathak P., Fang J., Chandrasekhar D., Mueller J., et al. Employee and employer benefits from a migraine management program: Disease outcomes and cost analysis. Headache. 2020;60(9):1947–1960. doi: 10.1111/head.13933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.IHS-GPAC Fujitsu Case Study Impact Report. 2021. [Google Scholar]
- 13.Gerth W.C., Carides G.W., Dasbach E.J., Visser W.H., Santanello N.C. The multinational impact of migraine symptoms on healthcare utilisation and work loss. Pharmacoeconomics. 2001;19(2):197–206. doi: 10.2165/00019053-200119020-00006. [DOI] [PubMed] [Google Scholar]
- 14.Gil-Gouveia R., Oliveira A.G., Martins I.P. The impact of cognitive symptoms on migraine attack-related disability. Cephalalgia. 2016;36(5):422–430. doi: 10.1177/0333102415604471. [DOI] [PubMed] [Google Scholar]
- 15.Shimizu T., Sakai F., Miyake H., Sone T., Sato M., Tanabe S., et al. Disability, quality of life, productivity impairment and employer costs of migraine in the workplace. J Headache Pain. 2021;22(1):29. doi: 10.1186/s10194-021-01243-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Begasse de Dhaem O., Robbins M.S. Cognitive impairment in primary and secondary headache disorders. Curr Pain Headache Rep. 2022;26(5):391–404. doi: 10.1007/s11916-022-01039-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seng E.K., Korey S.R., Klepper J.E. Development of the Cogniphobia scale for headache disorders (CS-HD): A pilot study. Psychol Assess. 2017;29(10):1296–1301. doi: 10.1037/pas0000432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peres M.F.P., Mercante J.P.P., Guendler V.Z., Corchs F., Bernik M.A., Zukerman E., et al. Cephalalgiaphobia: a possible specific phobia of illness. J Headache Pain. 2007;8(1):56–59. doi: 10.1007/s10194-007-0361-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kneipp S.M., Beeber L. Social withdrawal as a self-management behavior for migraine: implications for depression comorbidity among disadvantaged women. ANS Adv Nurs Sci. 2015;38(1):34–44. doi: 10.1097/ANS.0000000000000059. [DOI] [PubMed] [Google Scholar]
- 20.Minen M.T., Dhaem O.B.D., Diest A.K.V., Powers S., Schwedt T.J., Lipton R., et al. Migraine and its psychiatric comorbidities. J Neurol Neurosurg Psychiatry. 2016;87(7):741–749. doi: 10.1136/jnnp-2015-312233. [DOI] [PubMed] [Google Scholar]
- 21.Beck A., Crain A.L., Solberg L.I., Unützer J., Glasgow R.E., Maciosek M.V., et al. Severity of depression and magnitude of productivity loss. Ann Fam Med. 2011;9(4):305–311. doi: 10.1370/afm.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Plaisier I., Beekman A.T.F., de Graaf R., Smit J.H., van Dyck R., Penninx B.W.J.H. Work functioning in persons with depressive and anxiety disorders: the role of specific psychopathological characteristics. J Affect Disord. 2010;125(1–3):198–206. doi: 10.1016/j.jad.2010.01.072. [DOI] [PubMed] [Google Scholar]
- 23.Lagerveld S.E., Bültmann U., Franche R.L., van Dijk F.J.H., Vlasveld M.C., van der Feltz-Cornelis C.M., et al. Factors associated with work participation and work functioning in depressed workers: a systematic review. J Occup Rehabil. 2010;20(3):275–292. doi: 10.1007/s10926-009-9224-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hui S., kuen A, Grandner MA. Trouble sleeping associated with lower work performance and greater healthcare costs: longitudinal data from Kansas state employee wellness program. J Occup Environ Med. 2015;57(10):1031–1038. doi: 10.1097/JOM.0000000000000534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lantéri-Minet M., Radat F., Chautard M.H., Lucas C. Anxiety and depression associated with migraine: influence on migraine subjects’ disability and quality of life, and acute migraine management. Pain. 2005;118(3):319–326. doi: 10.1016/j.pain.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 26.Blumenfeld A.M., Varon S.F., Wilcox T.K., Buse D.C., Kawata A.K., Manack A., et al. Disability, HRQoL and resource use among chronic and episodic migraineurs: results from the international burden of migraine study (IBMS) Cephalalgia. 2011;31(3):301–315. doi: 10.1177/0333102410381145. [DOI] [PubMed] [Google Scholar]
- 27.Suvinen T.I., Ahlberg J., Rantala M., Nissinen M., Lindholm H., Könönen M., et al. Perceived stress, pain and work performance among non-patient working personnel with clinical signs of temporomandibular or neck pain. J Oral Rehabil. 2004;31(8):733–737. doi: 10.1111/j.1365-2842.2004.01312.x. [DOI] [PubMed] [Google Scholar]
- 28.Holroyd K., Drew J., Cottrell C., Romanek K., Heh V. Impaired functioning and quality of life in severe migraine: the role of catastrophizing and associated symptoms. Cephalalgia. 2007;27(10):1156–1165. doi: 10.1111/j.1468-2982.2007.01420.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seng E.K., Buse D.C., Klepper J.E., Mayson S.J., Grinberg A.S., Grosberg B.M., et al. Psychological factors associated with chronic migraine and severe migraine-related disability: an observational study in a tertiary headache center. Headache. 2017;57(4):593–604. doi: 10.1111/head.13021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lipton R.B., Stewart W.F., Simon D. Medical consultation for migraine: results from the American migraine study. Headache. 1998;38(2):87–96. doi: 10.1046/j.1526-4610.1998.3802087.x. [DOI] [PubMed] [Google Scholar]
- 31.Lipton R.B., Diamond S., Reed M., Diamond M.L., Stewart W.F. Migraine diagnosis and treatment: results from the American migraine study II. Headache. 2001;41(7):638–645. doi: 10.1046/j.1526-4610.2001.041007638.x. [DOI] [PubMed] [Google Scholar]
- 32.Young W.B., Park J.E., Tian I.X., Kempner J. The stigma of migraine. Preux PM, editor. PLoS ONE. 2013;8(1) doi: 10.1371/journal.pone.0054074. e54074-e54074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cottrell C.K., Drew J.B., Waller S.E., Holroyd K.A., Brose J.A., O’Donnell F.J. Perceptions and needs of patients with migraine. J Fam Pract. 2002;51(2):142–147. [PMC free article] [PubMed] [Google Scholar]
- 34.Shapiro R., Lipton R., Reiner P. EHMTI-0313. Factors influencing stigma towards persons with migraine. J Headache Pain. 2014;15(Suppl. 1):E36. [Google Scholar]
- 35.D’Amico D., Grazzi L., Curone M., Di Fiore P., Proietti Cecchini A., Leonardi M., et al. Difficulties in work activities and the pervasive effect over disability in patients with episodic and chronic migraine. Neurol Sci. 2015;36(Suppl. 1):9–11. doi: 10.1007/s10072-015-2130-4. [DOI] [PubMed] [Google Scholar]
- 36.Shapiro Robert. 2019. Migraine Stigma. HCNE Boston. (Boston) [Google Scholar]
- 37.Gvantseladze K., Do T.P., Hansen J.M., Shapiro R.E., Ashina M. The stereotypical image of a person with migraine according to mass media. Headache. 2020;60(7):1465–1471. doi: 10.1111/head.13846. [DOI] [PubMed] [Google Scholar]
- 38.Headache Disease and Migraine Disease Language and Image Guide [Internet] CHAMP; 2021. https://headachemigraine.org/headache-and-migraine-disease-language-and-image-guide/ [cited 2022 26]. Available from: [Google Scholar]
- 39.Rao D., Choi S.W., Victorson D., Bode R., Peterman A., Heinemann A., et al. Measuring stigma across neurological conditions: the development of the stigma scale for chronic illness (SSCI) Qual Life Res. 2009;18(5):585–595. doi: 10.1007/s11136-009-9475-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cella D., Lai J.S., Nowinski C.J., Victorson D., Peterman A., Miller D., et al. Neuro-QOL: brief measures of health-related quality of life for clinical research in neurology. Neurology. 2012;78(23):1860–1867. doi: 10.1212/WNL.0b013e318258f744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Best R.K., Arseniev-Koehler A. Stigma’s uneven decline [internet] SocArXiv. 2022 https://osf.io/preprints/socarxiv/7nm9x/ [cited 2022 May 30]. Available from: [Google Scholar]
- 42.Stewart W.F., Wood G.C., Razzaghi H., Reed M.L., Lipton R.B. Work impact of migraine headaches. J Occup Environ Med. 2008;50(7):736–745. doi: 10.1097/JOM.0b013e31818180cb. [DOI] [PubMed] [Google Scholar]
- 43.61st Annual Scientific Meeting American Headache Society® July 11–14 2019 Pennsylvania Convention Center Philadelphia, PA. Headache. The Journal of Head and Face Pain; 2019. pp. 1–208. 59(S1) [DOI] [PubMed] [Google Scholar]
- 44.Parikh S.K., Young W.B. Migraine: stigma in society. Curr Pain Headache Rep. 2019;23(1):8. doi: 10.1007/s11916-019-0743-7. [DOI] [PubMed] [Google Scholar]
- 45.Stewart W.F., Roy J., Lipton R.B. Migraine prevalence, socioeconomic status, and social causation. Neurology. 2013;81(11):948–955. doi: 10.1212/WNL.0b013e3182a43b32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peterlin B.L., Scher A.I. Migraine and the social selection vs causation hypotheses. Neurology. 2013;81(11):942–943. doi: 10.1212/WNL.0b013e3182a43ea7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goetzel R.Z., Long S.R., Ozminkowski R.J., Hawkins K., Wang S., Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting U.S. employers. J Occup Environ Med. 2004;46(4):398–412. doi: 10.1097/01.jom.0000121151.40413.bd. [DOI] [PubMed] [Google Scholar]
- 48.Hemp P. Presenteeism: at work—but out of it. Harv Bus Rev. 2004;82(10):49–58. (155) [PubMed] [Google Scholar]
- 49.Stewart W.F., Ricci J.A., Chee E., Morganstein D., Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290(18):2443–2454. doi: 10.1001/jama.290.18.2443. [DOI] [PubMed] [Google Scholar]
- 50.Allen D., Hines E.W., Pazdernik V., Konecny L.T., Breitenbach E. Four-year review of presenteeism data among employees of a large United States health care system: a retrospective prevalence study. Hum Resour Health. 2018;16(1):59. doi: 10.1186/s12960-018-0321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Selekler H.M., Gökmen G., Alvur T.M., Steiner T.J. Productivity losses attributable to headache, and their attempted recovery, in a heavy-manufacturing workforce in Turkey: implications for employers and politicians. J Headache Pain. 2015;16:96. doi: 10.1186/s10194-015-0579-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.de Dhaem Begasse. Migraines are a serious problem. Employers can help. [internet] Harv Bus Rev. 2021 https://hbr.org/2021/02/migraines-are-a-serious-problem-employers-can-help [cited 2021 Nov 12]. Available from: [Google Scholar]
- 53.Jutkowitz E., Nyman J.A., Michaud T.L., Abraham J.M., Dowd B. For what illnesses is a disease management program most effective? J Occup Environ Med. 2015;57(2):117–123. doi: 10.1097/JOM.0000000000000385. [DOI] [PubMed] [Google Scholar]
- 54.Page M.J., Paramore L.C., Doshi D., Rupnow M.F.T. Evaluation of resource utilization and cost burden before and after an employer-based migraine education program. J Occup Environ Med. 2009;51(2):213–220. doi: 10.1097/JOM.0b013e318192bcd1. [DOI] [PubMed] [Google Scholar]
- 55.Schneider W.J., Furth P.A., Blalock T.H., Sherrill T.A. A pilot study of a headache program in the workplace. The effect of education. J Occup Environ Med. 1999;41(3):202–209. doi: 10.1097/00043764-199903000-00010. [DOI] [PubMed] [Google Scholar]
- 56.Mannix L.K., Solomon G.D., Kippes C.M., Kunkel R.S. Impact of headache education program in the workplace. Neurology. 1999;53(4):868–871. doi: 10.1212/wnl.53.4.868. [DOI] [PubMed] [Google Scholar]
- 57.Burton W.N., Chen C.Y., Li X., McCluskey M., Erickson D., Schultz A.B. Evaluation of a workplace-based migraine education program. J Occup Environ Med. 2016;58(8):790–795. doi: 10.1097/JOM.0000000000000781. [DOI] [PubMed] [Google Scholar]
- 58.Landy S., Brookfield R., McGinnis J. Headache in the workplace: an evaluation of the impact of educational programming on employee disability. Headache Pain. 2003;14:156–160. [Google Scholar]
- 59.Lipton R.B., Bigal M.E. Ten lessons on the epidemiology of migraine. Headache. 2007;47(Suppl. 1):S2–S9. doi: 10.1111/j.1526-4610.2007.00671.x. [DOI] [PubMed] [Google Scholar]
- 60.Ganesh K., Lazar A. The work of workplace disclosure: invisible chronic conditions and opportunities for design. Proc ACM Hum Comput Interact. 2021 doi: 10.1145/3449147. (Apr;5:10.1145/3449147) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vicente-Herrero T., Burke T.A., Laínez M.J.A. The impact of a worksite migraine intervention program on work productivity, productivity costs, and non-workplace impairment among Spanish postal service employees from an employer perspective. Curr Med Res Opin. 2004;20(11):1805–1814. doi: 10.1185/030079904X10151. [DOI] [PubMed] [Google Scholar]
- 62.Parker C., Waltman N. Reducing the frequency and severity of migraine headaches in the workplace: implementing evidence-based interventions. Workplace Health Saf. 2012;60(1):12–18. doi: 10.1177/216507991206000103. [DOI] [PubMed] [Google Scholar]
- 63.Borok G., Hershoff D., Maurer R. PNL32 evaluation of the impact of an employee worksite disease management program for migraineurs on work productivity. Value Health. 2006;9:A89. [Google Scholar]
- 64.Lantéri-Minet M., Allain H., Nachit-Ouinekh F., Bentué-Ferrer D., Gilbert P., Schück S., et al. NOEMIE: an epidemiological study of migraine at work: results from 17 occupational health centres. Rev Neurol (Paris) 2004;160(10):928–934. doi: 10.1016/s0035-3787(04)71074-7. [DOI] [PubMed] [Google Scholar]
- 65.Vicente-Herrero M., Lainez M. Impacto de un programa de intervencion de la migrana en el medio laboral entre los trabajadores de correos. Medicina del Trabajo. 2006;15:12–22. [Google Scholar]
- 66.Vicente Herrero M.T., Iñiguez Ramírez, de la Torre M.V., Reinoso Barbero L., Ruiz de la Torre E. Preventive aspects for migraine and the workplace: A European survey. Arch Prev Riesgos Labor. 2021;24(1):20–33. doi: 10.12961/aprl.2021.24.01.03. [DOI] [PubMed] [Google Scholar]
- 67.van der Doef M.P., Schelvis R.M.C. Relations between psychosocial job characteristics and work ability in employees with chronic headaches. J Occup Rehabil. 2019;29(1):119–127. doi: 10.1007/s10926-018-9769-7. [DOI] [PubMed] [Google Scholar]
- 68.Scaratti C., Foitzek N., Grignani E., Leonardi M., Raggi A., Coenen M. The employment needs and the factors having a negative or positive impact on work of people with chronic diseases in Europe: the case of headache. Neurol Sci. 2018;39(Suppl. 1):121–123. doi: 10.1007/s10072-018-3376-4. [DOI] [PubMed] [Google Scholar]
- 69.Gerson L.W., Skipper J.K. Job status and expectations of exemptions from work due to illness. J Occup Med. 1973;15(8):633–634. [PubMed] [Google Scholar]
- 70.Berardelli I., Sarubbi S., Lamis D.A., Rogante E., Canzonetta V., Negro A., et al. Job satisfaction mediates the association between perceived disability and work productivity in migraine headache patients. Int J Environ Res Public Health. 2019;16(18):E3341. doi: 10.3390/ijerph16183341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Leonardi M., Raggi A., Ajovalasit D., Bussone G., D’Amico D. Functioning and disability in migraine. Disabil Rehabil. 2010;32(Suppl. 1):S23–S32. doi: 10.3109/09638288.2010.511687. [DOI] [PubMed] [Google Scholar]
- 72.Ávila C.C., Ayuso-Mateos J.L., Muñoz-Murillo A., Scaratti C., Coenen M., Vlachou A., et al. Identifying the employment needs of people with chronic health conditions in Europe. J Occup Environ Med. 2018;60(11):e618–e624. doi: 10.1097/JOM.0000000000001425. [DOI] [PubMed] [Google Scholar]
- 73.Raggi A., Covelli V., Guastafierro E., Leonardi M., Scaratti C., Grazzi L., et al. Validation of a self-reported instrument to assess work-related difficulties in patients with migraine: the HEADWORK questionnaire. J Headache Pain. 2018;19(1):85. doi: 10.1186/s10194-018-0914-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Leijten F.R.M., van den Heuvel S.G., Ybema J.F., Robroek S.J.W., Burdorf A. Do work factors modify the association between chronic health problems and sickness absence among older employees? Scand J Work Environ Health. 2013;39(5):477–485. doi: 10.5271/sjweh.3353. [DOI] [PubMed] [Google Scholar]
- 75.Sandoe C.H., Sasikumar S., Lay C., Lawler V. The impact of shift work on migraine: A case series and narrative review. Headache. 2019;59(9):1631–1640. doi: 10.1111/head.13622. [DOI] [PubMed] [Google Scholar]
- 76.Mitrovic A., Sretenovic A., Stanic A. Contribution of twenty-one epidemiological factors to migraine disability. J Neurol Sci. 2013;333:e489–e490. [Google Scholar]
- 77.Grisold W., Struhal W., Grisold T. Oxford University Press; 2019. Advocacy in Neurology. [Google Scholar]
- 78.Dodick D., Edvinsson L., Makino T., Grisold W., Sakai F., Jensen R., et al. Vancouver declaration on global headache patient advocacy 2018. Cephalalgia. 2018;38(13):1899–1909. doi: 10.1177/0333102418781644. [DOI] [PubMed] [Google Scholar]
- 79.Dodick D.W., Ashina M., Sakai F., Grisold W., Miyake H., Henscheid-Lorenz D., et al. Vancouver declaration II on global headache patient advocacy 2019. Cephalalgia. 2020;40(10):1017–1025. doi: 10.1177/0333102420921162. [DOI] [PubMed] [Google Scholar]
- 80.Fujitsu Honored by the International Headache Society - Global Patient Advocacy Coalition as a World Leader in Migraine Workplace Awareness, Education, and Employee Support Programs [Internet] Fujitsu Global; 2022. https://www.fujitsu.com/global/about/resources/news/press-releases/2022/0302-01.html Available from: [Google Scholar]
- 81.The Americans with Disabilities Act Amendments Act of 2008 | U.S. Equal Employment Opportunity Commission 2021. https://www.eeoc.gov/statutes/americans-disabilities-act-amendments-act-2008 Available from:
- 82.Shapiro R.E. Migraine and disability rights. CONTINUUM: lifelong learning. Neurology. 2012;18(4):900. doi: 10.1212/01.CON.0000418652.08268.9f. [DOI] [PubMed] [Google Scholar]
- 83.Daly M.C., Bound J. Worker adaptation and employer accommodation following the onset of a health impairment. J Gerontol B Psychol Sci Soc Sci. 1996;51(2):S53–S60. doi: 10.1093/geronb/51b.2.s53. [DOI] [PubMed] [Google Scholar]
- 84.Work at Home/Telework as a Reasonable Accommodation | U.S. Equal Employment Opportunity Commission. 2021. https://www.eeoc.gov/laws/guidance/work-hometelework-reasonable-accommodation Available from:
- 85.Shapiro R.E. What will it take to move the needle for headache disorders? An Advocacy Perspective Headache. 2020;60(9):2059–2077. doi: 10.1111/head.13913. [DOI] [PubMed] [Google Scholar]
- 86.Policy S Office of Medical. SSR 19-4p. 2022. https://www.ssa.gov/OP_Home/rulings/di/01/SSR2019-04-di-01.html Available from: