Abstract
Introduction
Chronic pain conditions are a leading cause of disease and disability. They are associated with symptoms such as fatigue, sleep and mood disturbances. Minimal evidence is available to support effective treatments and alternatives treatment approaches are called for. Photobiomodulation therapy has been highlighted as one promising option. A whole-body therapy device (NovoTHOR) has recently been developed with a number of potential advantages for people with chronic pain. Research is needed to consider the feasibility of this device.
Methods and analysis
A single-centre single-armed (no placebo group) feasibility study with an embedded qualitative component will be conducted. The intervention will comprise 18 treatments over 6 weeks, with 6-month follow-up, in the whole-body photobiomodulation device. A non-probability sample of 20 adult participants with a clinician diagnosis of chronic axial pain, polyarthralgia, myofascial pain or widespread pain will be recruited (self-referral and clinician referral). Outcome measures will focus on acceptability of trial processes with a view to guiding a definitive randomised controlled trial. Analyses will use descriptive statistics for quantitative aspects. The qualitative element will be assessed by means of a participant-reported experience questionnaire postintervention and semistructured audio-recorded interviews at three stages; preintervention, midintervention and postintervention. The latter will be transcribed verbatim and a reflexive thematic analysis will be used to identify emerging themes. Exploratory outcomes (participant-reported and performance-based measures) will be analysed according to data distribution.
Ethics and dissemination
The study has received ethical approval from the Leicester Central Research and Ethics Committee. Findings will be disseminated via local chronic pain groups, public register update, submission for presentation at scientific meetings and open-access peer-reviewed journals, and via academic social networks.
Trial registration number
Keywords: pain management, rheumatology, musculoskeletal disorders
Strengths and limitations of this study.
This is the first study investigating this novel therapy in this population.
Methods utilised are rigorous and informed with patient and public involvement.
This is a feasibility trial focusing on acceptability of trial intervention and processes.
A small sample size will be selected to identify important parameter estimates.
A single arm trial is proposed and does not include an active or inactive control group such as a placebo intervention for comparison.
Introduction
The International Association for the Study of Pain define pain as ‘an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage’.1 When pain becomes chronic it is persistent or recurrent, lasting longer than 3 months.2 It is a multidimensional phenomenon and prognosis is heavily influenced by a diverse array of psychosocial variables including distress levels, coping mechanisms and contextual factors.3 According to the 11th edition of International Classification of Diseases classification, there are two broad groups: (1) ‘chronic primary pain’ which includes conditions such as non-specific low back pain and fibromyalgia (FM), that is, those conditions where the cause is not known; and (2) ‘chronic secondary pain’ which encompasses cancer-related pain, neuropathic pain, visceral pain, post-traumatic and postsurgical pain, headache and orofacial pain, and musculoskeletal pain. This revised taxonomy allows for recognition of chronic pain as a health condition in its own right.4
Chronic pain carries with it a profound impact on both individuals and society. Internationally, it is the leading cause of disability and disease burden.5 6 Research suggests a mean prevalence of 30% globally,7 with estimates of 13%–50% in the UK.5 Across Europe, chronic pain incurs a cost of €200 billion per annum.7
There is no known effective treatment for chronic primary pain conditions like FM, likely owing to their complex nature.8 It is commonplace for affected individuals to try a multitude of therapies, often accompanied with side effects despite evidence of limited benefit.9 10 The most recent National Institute for Health and Care Excellence (NICE) guidance regarding chronic pain management advises against use of the many commonly instituted pain medications.11 The paucity of strong recommendations in international guidelines12–14 highlights a need for exploring other therapeutic methods and modalities. NICE has called for further treatment options to be made available to these patients,15 and have identified photobiomodulation (PBM) therapy as demonstrating positive effects on pain and quality of life, describing it to be a promising therapy and recommending further research in the area.12
PBM is a safe and non-invasive low energy light (red and near infrared) therapy that is absorbed by endogenous chromophores to induce cellular changes.16–18 Focused PBM has demonstrated positive results when treating a multitude of acute and chronic pain conditions.19–32 The therapy has received recent recognition from national and international healthcare governing bodies in treatment of cancer-related painful oral mucositis.16 It is traditionally delivered by a trained therapist using a small probe applied to specific painful areas; as such, sessions can take up to 90 min in widespread pain conditions such as FM. Recent studies have called for larger probes and stipulated that novel delivery devices would be advantageous.19 33
The development of whole-body devices has allowed participants themselves to operate the device. For example, the NovoTHOR (figure 1) device delivers the treatment to the whole-body in 20 min or less and requiring no specialist skills to deliver the treatment, appearing less labour intensive and time-consuming. Whole-body PBM therapy is a novel mode of treatment with the potential to address multiple aetiological mechanisms in patients experiencing chronic and diffuse pain. Co-existing features commonly include cognitive and emotional impairment and evidence is emerging that PBM therapy can aid in the treatment of these ailments.34
Figure 1.
NovoTHOR. Reprinted with permission.
We will explore the use of whole-body PBM therapy as a treatment option for chronic widespread pain. To the best of our knowledge, this is the first study using this device in this population. We suggest commencing with a feasibility study to assess acceptability of the therapy and study procedures in our population, with a view to designing a definitive RCT. We want to see if there is a potential to reduce pain and pain-related comorbidities by treating the whole body, rather than localised PBM therapy.
Aim and objectives
Aim
To undertake a feasibility study of whole-body PBM in the management of chronic pain.
Objectives
To determine study procedures with a view to guiding a definitive randomised controlled trial (RCT), specifically:
To determine whether eligibility criteria is either too open or too restrictive by estimating eligibility and recruitment rates.
To investigate acceptability of the trial device and treatment schedule (including perceptions, values and opinions).
To assess the acceptability of outcome measures, including user-friendliness of questionnaires.
To investigate the feasibility (and factors influencing this) of the outcome measures as methods to measure efficacy of the interventions within a definitive trial.
To assess refusal rates and barriers to uptake.
To assess trial retention rates including completion of therapy (6 weeks) and trial follow-up (6 months).
-
To assess potential effectiveness of whole-body PBM therapy using a combination of patient-reported and performance-based outcomes printervention and postintervention.
To synthesise data to inform the sample size of a definitive trial.
-
To assess participants’ perceptions and experience:
Regarding their condition.
Regarding the trial device and processes.
Regarding future randomisation, blinding and placebo therapy.
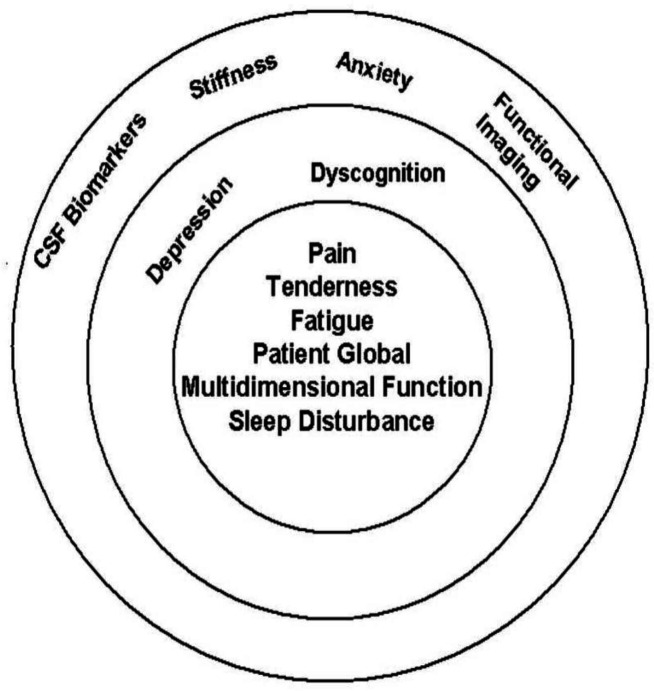
Figure 2.
OMERACT hierarchy of domains. Reprinted with permission. The innermost circle contains the core set of domains to be assessed in all clinical trials of FM. The second concentric circle includes the outer core set of domains to be assessed in some but not all FM trials. The outermost circle includes the domains on the research agenda that may or may not be included in FM trials.35 FM, fibromyalgia.
Methods and analysis
The following is laid out in accordance with the Consolidated Standards of Reporting Trials (CONSORT) extension to pilot and feasibility trials guidance.36
Trial design
A feasibility study designed as a single-centre and single-armed trial with embedded qualitative component. The following trial procedures are reported in accordance with SPIRIT-PRO extension.37
Trial setting
This study will be conducted at Sandwell and West Birmingham (SWB) NHS Trust, West Midlands. The NovoTHOR PBM therapy device will be installed in a designated space at the Clinical Research Facility, Sandwell General Hospital.
Recruitment
Potentially eligible participants will be recruited from two sources:
Self-referral/registration of interest of SWB-registered patients to a designated research telephone and email. This will be possible via a trial recruitment poster that will be displayed in pain and rheumatology clinic areas and pain procedures areas.
SWB-registered patients identified in pain clinics and procedure lists by the patient’s usual pain doctor who is not involved in the research trial.
Trust interpreters and ‘Language Line’ will be utilised to ensure a representative sample of non-English speaking participants are recruited. Participant Information Sheets (PIS) will be translated into the five most commonly spoken languages at the Trust; Punjabi, Urdu, Polish, Romanian and Bengali.
Eligibility criteria
The following criteria are in keeping with several other studies looking at PBM therapy in chronic pain.38–42
Inclusion criteria
-
Currently diagnosed or receiving treatment for a widespread chronic pain condition, including but not limited to:
Axial pain of any origin
Polyathralgia of any origin
Myofascial pain of any origin
A diagnosis of chronic widespread pain or FM
Able to provide informed written consent
≥18 years
Able to commit time to the trial treatment schedule of 6 weeks
Score as low or moderate risk on the COVID-19 risk stratification tool— applicable for the duration of the pandemic.
Exclusion criteria
Pregnancy
Severe skin diseases (eg, skin cancer, severe eczema, dermatitis or psoriasis)
Body weight≥136 kg, as per manufacturer instructions.
Uncontrolled comorbidities (eg, uncontrolled diabetes defined as HbA1c>69 mmol/mol, decompensated heart failure, major psychiatric disturbance such as acute psychosis or suicidal ideation).
Use of systemic corticosteroid therapy including oral prednisolone or corticosteroid injections within the preceding 6 months as recommended by the manufacturer; steroids are thought to inhibit the anti-inflammatory effect of PBM therapy.43
Known active malignancy
Inability to enter the NovoTHOR device or lie flat for 20 min (either due to physical reasons or other for example, claustrophobia).
Patients speaking a language for which an interpreter cannot be sought (namely Oromo, Tigranian, Amharic and Greek. Interpreters for all other languages at the Sponsor Trust can be sought)
Intervention
In order that the intervention can be replicated when building on future research, we have utilised the template for intervention description and replication checklist44 (table 1). NovoTHOR dosage parameters are exhibited in table 2.
Table 1.
Template for intervention description and replication checklist
| Brief name |
|
| Why |
|
| What |
|
| Who provided |
|
| How |
|
| Where |
|
| When and how much |
|
| Tailoring |
|
| Modifications |
|
| How well |
|
PBM, photobiomodulation; SWB, Sandwell and West Birmingham.
Table 2.
NovoTHOR parameters
| NovoTHOR XL parameters | Unit | |
| Wavelengths of red and near-infrared LEDs 50:50 ratio | 660 850 |
nm nm |
| Number of LEDs | 2400 | |
| Power emitted per LED | 0.289 | W |
| Beam area per LED (at the lens/skin contact surface) | 12.0 | cm2 |
| Total power emitted | 694 | W |
| Total area of NovoTHOR emitting surfaces | 26 740 | cm2 |
| Treatment time | 1200 | s |
| Continuous wave (not pulsed) | CW | |
| Irradiance | 0.028 | W/cm2 |
| Fluence | 33.6 | J/cm2 |
LEDs, light-emitting diodes.
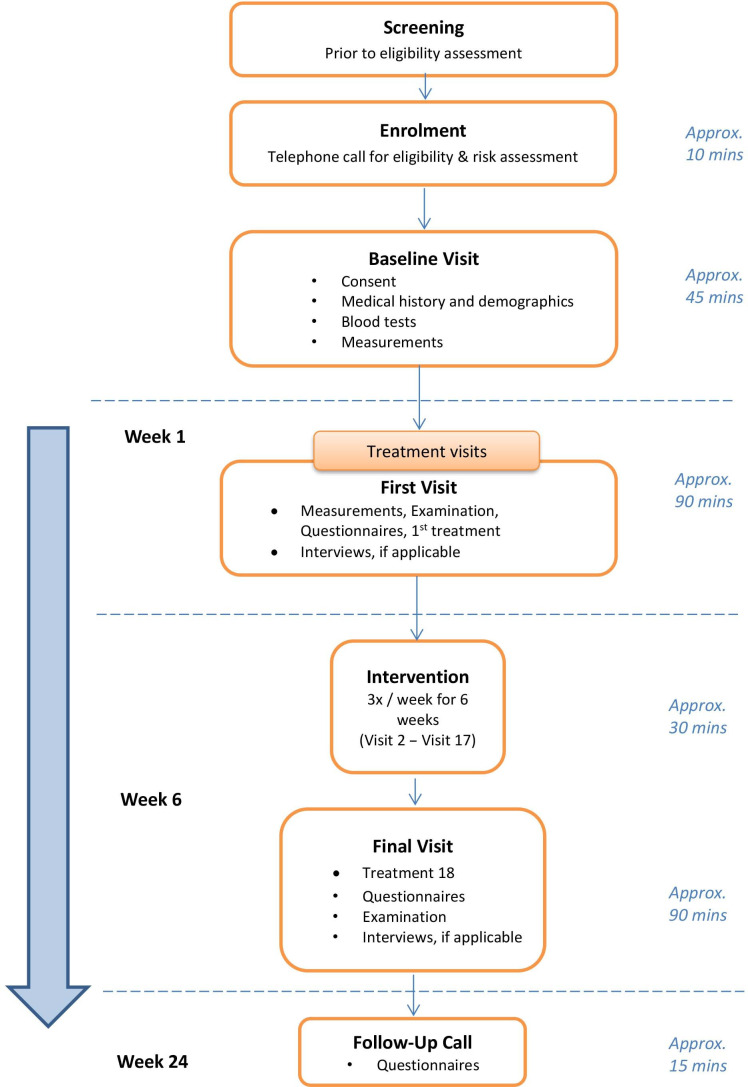
Study duration
We envisage the recruitment period should take approximately 3–6 months. Follow-up data will be collected at 6 months. This study schedule is depicted in table 3 and figure 3, including an overview of events at each study visit—in keeping with SPIRIT-PRO (SPIRIT, Standard Protocol Items: Recommendations for Interventional Trials) Extension guidance.37
Table 3.
Outline of study flow
| Procedures | Telephone call | Baseline visit | First visit | Visit 2–visit 17 | Final visit | 6-month telephone Follow-up |
| Eligibility | x | |||||
| Assessment | ||||||
| Informed consent | x | |||||
| Blood tests | ||||||
| Full blood count | ||||||
| Urea and electrolytes | ||||||
| Liver function tests | x | |||||
| HbA1c (if diabetic) | ||||||
| Demographics | ||||||
| Age | ||||||
| Gender | ||||||
| Marital status | ||||||
| Employment status | ||||||
| Educational level | x | |||||
| Ethnicity | ||||||
| Medical history | ||||||
| Duration of chronic pain symptoms | ||||||
| Comorbidities | ||||||
| Medications | x | x | ||||
| Measurements | ||||||
| Height | ||||||
| Weight | x | x | ||||
| BMI | ||||||
| Blood pressure | ||||||
| Heart rate | ||||||
| Oxygen saturations | ||||||
| Participant-reported outcome measures* | ||||||
| Brief pain inventory | x | x | ||||
| Widespread pain index/ symptom | x | x | ||||
| Severity score | ||||||
| Fatigue severity scale | x | x | ||||
| Jenkins sleep questionnaire | x | x | ||||
| Patient global impression of change | x | x | ||||
| Revised fibromyalgia impact questionnaire | x | x | x | |||
| Hospital anxiety and depression scale | x | x | ||||
| Performance-based outcome measures† | ||||||
| Tender point count | ||||||
| Stroop test | x | x | ||||
| Treatment | x | x | x | |||
| Weekly Numerical Rating Scale (NRS)—applicable for preceding week | x | x | ||||
| Participant-reported experience measure (online supplemental file 1) | x | |||||
| Audio-recorded qualitative interviews (online supplemental file 2 for topic guide) | x | x | x | |||
Figure 3.
CONSORT study flow diagram. CONSORT, Consolidated Standards of Reporting Trials.
bmjopen-2021-060058supp001.pdf (1.5MB, pdf)
bmjopen-2021-060058supp002.pdf (162.9KB, pdf)
Sample size
The trial will continue until 20 participants are recruited and complete 6 weeks of whole-body PBM therapy. CONSORT guidelines for feasibility studies require a primary evaluation that focuses on descriptive analysis of feasibility/process outcomes (eg, recruitment, adherence and treatment fidelity).36 In order to gauge our sample size, we took data from a 2019 meta-analysis on focused PBM therapy in fibromyalgia,45 as best proxy of the widespread chronic pain and included all of the symptoms under observation in this study. Our chosen sample size takes into account the study population’s number of visits at our clinics, objectives of the study and recommendations for the sample size calculations in pilot and feasibility trials by Moore et al46 Lancaster and Thabane,47 Lewis et al48 as well as the ‘rules of thumb’ for feasibility trials as set out by Kieser and Wassmer.49
Sample size for the qualitative component will be guided by the concept of information power.50 Information power uses specific principles which will guide numbers including the sample specificity, the aim of the study, the use of established theory, quality of dialogue and analysis strategy. We will seek to establish data saturation of themes.51 Considering past research52 looking at experiences of an intervention, we will attempt to interview all participants.
Data collection methods
Eligibility criteria will be explored by means of analysing eligibility rates (objective 1). Acceptability will be assessed quantitatively in terms of refusal and retention rates (objectives 5 and 6). Qualitative interviews and patient-reported experience questionnaires will help guide the qualitative aspect of acceptability and practicability of the device (objective 2), treatment schedule (objective 2), trial design and appropriateness of outcome measures (objectives 3 and 4). The eligibility rates, recruitment rates, refusal rates and retention rates will be measured and expressed in proportions. The results will guide design and methods of the future definitive RCT.
A combination of patient-reported (table 4) and performance-based (table 5) measures will be employed (objectives 7–9). The following patient-reported outcome measures have all demonstrated reliability and validity in the assessment of pain conditions.53–61 Additionally, these tools are recognised as the recommended standardised assessment tools for FM domains by an international consortium of experts in the field (2012).62 Out of the following seven questionnaires, five are less than a single page. The remaining two are less than three pages. All encompass simple tick box answers. Participants will complete paper questionnaires in the clinic room. For non-English speaking participants, an interpreter will be present. After testing with layperson representatives, it is estimated that the time taken to complete all outcome measures will be less than 20 min. Not all questionnaires will be asked each time (see brief tool description in table 4 for further information regarding individual questionnaires).
Table 4.
Patient-reported outcome measures
| OMERACT domain | Assessment tool | Brief tool description (taken into account when considering participant burden) |
| Core domains | ||
| Pain | Brief Pain Inventory Short Form (BPI-SF) | Time to complete: 3 min Number of administrations: 2 (first visit, final visit) Description: 12×11-point NRS |
| Widespread Pain Index (WPI) and Symptom Severity Score (SSS) | Time to complete: 4 min Number of administrations: 2 (first visit, final visit) Description: required to tick pain sites (0–19); three questions on symptom severity, 0=no problem, 3=severe; three questions on other symptoms, 0=no problem, 1=problem |
|
| Fatigue | Fatigue Severity Scale (FSS) | Time to complete: 1.5 min Number of administrations: 2 (first visit, final visit) Description: 9×7-point Likert scale; 1=strongly disagree, 7=strongly agree |
| Sleep disturbance | Jenkins Sleep Questionnaire (JSQ) | Time to complete: 1 min Number of administrations: 2 (first visit, final visit) Description: 4×6-point questions; 0=not at all, 5=22–28 days |
| Patient Global | Patient Global Impression of Change (PGIC) | Time to complete: 1 min Number of administrations: 2 (final visit, follow-up telephone call) Description: 2 questions; first: change post-treatment, 0=no change, 7=considerable improvement. Second: 11-point NRS, 0=much better, 10=much worse. |
| Multidimensional function | Revised Fibromyalgia Impact Questionnaire (FIQR)* | Time to complete: 3.5 min Number of administrations: 3 (first visit, final visit, follow-up telephone call) Description: 21×11—point numerical rating scale (NRS); 0=no difficulty, 10=very difficult; total maximal score=100 |
| Peripheral domains | ||
| Anxiety | HADS-A Subsection of Hospital Anxiety and Depression Scale assessment |
Time to complete: 1 min Number of administrations: 2 (first visit, final visit) Description: 7×4-point questions, ‘not at all’ → ‘most of the time’ |
| Depression | HADS-D Subsection of Hospital Anxiety and Depression Scale assessment |
Time to complete: 1 min Number of administrations: 2 (first visit, final visit) Description: 7×4-point questions, ‘not at all’ → ‘most of the time’ |
| Stiffness | – | Time to complete: N/A (subsection of FIQR) Number of administrations: 3 (first visit, final visit, follow-up telephone call) |
| Dyscognition | – | Time to complete: N/A (subsection of FIQR) Number of administrations: 3 (first visit, final visit, follow-up telephone call) |
Total completion time: 16 min.
*The rationale for inclusion of FM questionnaires is fourfold; (1) a proportion of participants included in the study will have widespread pain symptoms secondary to FM, (2) multifaceted subjective scores, encompassing all aspects of chronic pain in a comprehensive manner, (3) FM is the best proxy for widespread chronic pain symptoms, (4) the FIQR can be utilised for any chronic condition—when it is known as Symptom Impact Questionnaire or SIQR.
FM, fibromyalgia; N/A, not applicable; NRS, Numerical Rating Scale.
Table 5.
Performance-based outcome measures
| OMERACT domain | Assessment tool | Brief tool description (taken into account when considering participant burden) |
| Core domains | ||
| Tenderness | Tender point count using a dolorimeter set to apply 4 kg/cm2 of pressure—18 tender points as described by American College of Rheumatology | Time to complete: 2 min Number of administrations: 2 (first visit, final visit) The Manual Tender Point Survey/Fibromyalgia Intensity Score (MTPS/FIS) method will be used where the participant rates pain severity on application of the dolorimeter at each tender point on a verbal NRS. NRS≥2 is required to count a tender point as positive. A tender point about the size of a penny, located in clusters in soft tissues around the neck, chest, shoulders, elbows, hips and knees. These 18 specific tender points were identified by the American College of Rheumatology in 1990,71 and are often painful in FM patients. For a tender spot to be considered positive, the participant will experience temporary pain when a small amount of pressure is applied to the specific area. Positive tender points are no longer required to make a diagnosis of FM, but clinicians may still choose to examine these areas in routine practice to strengthen the probability of diagnosis and/or monitor response to treatment. Reliability and reproducibility will be ensured with the use of a dolorimeter set to apply a prespecified pressure at each of the tender points. Pain with 4 kg/cm2 pressure or less (taken to be equivalent to application of digital pressure until the pulp of the thumb nail becomes white) is considered to be a positive tender point.72 |
| Peripheral domains | ||
| Dyscognition | Stroop Test (to assess inhibitory control and processing speed) | Time to complete: 1 min Number of administrations: 2 (first visit, final visit) This is a computer-based test. A series of colours are spelt out on the screen; blue, red, yellow, green. Each time the word appears, it is presented in a different colour; blue, red, yellow or green. The participant must select the correct colour of the word. This is a timed task for 60 s. If the answer is selected incorrectly, the next word will appear. The test is scored by number of correct answers in this time period. No marks are lost for incorrect answers. |
Total completion time: 3 min.
FM, fibromyalgia; NRS, Numerical Rating Scale.
Data management
All data manipulation will be consistent with the Office for National Statistics recommendations as stated in the ‘Review of the Dissemination of Health Statistics: Confidentiality Guidance’, 2006.63 Compliance with the UK General Data Protection Regulation 201864 will be demonstrated throughout. Once enrolled, the participant will be allocated a unique study number—data will be pseudoanonymised by this coding method. The database that contains participant identifiable data will be separate to the research data. Only study numbers will be used for recording research data. The study delegation log with outlined duties will be kept, as well as a standard operating procedure (SOP) for device operation. All research records will be archived as per the Trust Research and Development (R&D) Archiving SOP and the end of study will be reported to the HRA and the Research Ethics Committee.
Quantitative data analysis
The primary feasibility outcome data (objectives 2–4) will be summarised using descriptive statistics, including narrative descriptions. Primary statistical analyses will be non-parametric, but if the data distribution allows, we will use also parametric statistics. Categorical data will be presented as frequencies and percentages, while continuous data will be presented as means, SD, median, mode and IQR, depending on the data distribution. Data will be assessed for normality both visually and with Shapiro-Wilk test. Recruitment, participation and retention rates (objectives 1, 5 and 6) will be reported and presented in a CONSORT flow diagram.
Both patient-reported and performance-based outcomes will be analysed (objective 7). Estimates of effect will be reported as 95% CI without p values, and will be used to generate CIs for a future RCT (objective 8). Table 6 provides a summary for the intended utilisation of statistical tests according to the type of data produced. Data will be analysed using SPSS or an equivalent statistical package.
Table 6.
Data analysis
| Data type | Statistical test |
| Normally distributed continuous variables for example, FIQR | Student’s paired t test |
| Non-parametric ordinal data for example, tender point count | Wilcoxon signed-rank test (will be used to compare pretreatment and post-treatment scores) |
| Categorical data for example, marital and employment status | Fisher’s exact test |
| Paired continuous data for example, comparison of mean scores pretreatment and post-treatment | Student’s paired t test |
| Subgroup analysis for example, gender and ethnicity comparisons | One-way analysis of variance |
| Non-parametric data (if assumptions of normality not met) | Wilcoxon signed-rank test Mann-Whitney test Kruskal-Wallis analysis |
FIQR, Fibromyalgia Impact Questionnaire.
Qualitative data analysis
A reflexive thematic analysis65 will be undertaken within six stages. Two independent researchers will examine the first five interviews in order to establish agreed focus and initial thematic content from open coding, initially participant by participant to maintain uniqueness. These two reviewers will then discuss and identify common themes across participants. All further stages will be undertaken by the lead researcher where supervising authors will act as a critical friend. The lead researcher will present a defendable case to the steering group for the later stages. For the purpose of the study, this analysis will be undertaken separately and inductively (objective 9). Depending on study results, the analysis will be presented separately as themes, or integrated at the stage of presentation to explain quantitative results if possible.
Data monitoring
Simple mean imputation for missing data will be employed where applicable.66 Additionally, missing data will be reported with reasons given where possible in order to assess the feasibility of methodology. This will be valuable when informing outcome measures for the definitive trial.
Risk assessment
A summary of hazard and risks will be kept in the Investigator Site File. There are exemptions for certain expected events relating to chronic pain patients and/or treatment that do not need reporting (other than in the Case Report Form). For this population, these include: flare ups or pain and increase in medication dosages, increased unscheduled healthcare usage including GP and Emergency Department visits for a flare, time off work/college/University due to flare. In addition, recognised minor expected side effects such as sensations of localised warmth and tingling will not be recorded as adverse events. See table 7 for definitions and action plan.
Table 7.
Event definitions and action plan
| Adverse events (AE) |
|
| Serious adverse events (SAE) |
|
| Adverse device events and serious adverse device events |
|
Auditing
The R&D department of SWB Trust are the trial Sponsor. The Trial Steering Committee will meet at allocated trial points including prior to recruitment, or if AEs occur. The trial committee comprised academics from the University of Birmingham (AS and NRH) and a chronic pain patient representative who is not a participant in the trial (NG). They will meet at least 6 monthly or more frequently if required.
Patient Public Involvement (PPI)
We have followed the NIHR INVOLVE collaborative guidance described in the ‘UK Standards for Public Involvement in Research’ (2019)67 and have utilised the GRIPP2 short form template68 when gaining PPI with regard to our aims and methods. Patients have been central towards the development of our methodology, particularly in relation to symptom domains to be investigated.
The proposed research has been designed in conjunction with patients diagnosed with FM at SWB Trust, as a predominant example of a chronic pain population experiencing symptoms of widespread pain. Patients have been involved in decision-making from the start. We have been informally liaising with approximately 30 patients over 12 months, including the use a focus group. One patient has taken on the role of liaison member—checking over detailed aspects of the trial design, PIS, user-friendliness of questionnaires and will participate in the Trial Steering Committee.
Limitations of this study
There are some limitations to this study. There is no control or placebo group and the sample size is not powered; hence, efficacy of the trial intervention cannot be established. For this reason, participants are able to continue to receive their usual care (with the exception of steroids) which has the potential to introduce bias. There is a possibility of treatment being non-uniform between participants in that they can receive treatment without the lid being fully close if they were to feel claustrophobic. For the purposes of this feasibility trial, this will be noted and be used to help guide study procedures for a definitive RCT.
Ethics and dissemination
Ethical considerations
The study has Leicester Central Research Ethics Committee (21/EM/0231) and Health Research Authority (project ID 278452) approvals, granted on 13 October 2021. Local approval was obtained from SWB NHS Trust Research and Development department (20PAIN01). Recruitment of participants will be consecutive. Each participant will receive written study information and be required to provide written inform consent before any study procedure is undertaken.
Protocol amendments
Protocol amendments will be communicated with relevant parties such as the trial investigators, Sponsor, university, trial registries, and if required, trial participants.
Dissemination policy
Findings of the trial will be widely disseminated to patients, healthcare professionals, commissioners and the general public. Research findings will be published within 1 year of the study’s completion, and the results section in the public register to which the study is registered will be updated, as per best practice guidance.69 Participants’ involvement in the trial will be acknowledged by providing them with a summary of the findings. The importance of this has been confirmed by our patients following discussions at focus groups.
We wish to disseminate findings in a user-friendly way which is accessible to multiple audiences. Our patient public involvement members will play a key role here. There are specific focus groups at our Trust, such as Pain Management Programmes. In particular, our patient liaison representative has regular access to community chronic pain groups. We will make our results locally available to both patients and staff via the Trust Intranet, and nationally via Pain Charity websites such as Fibromyalgia Action UK. Subsequent to TSC approvals, findings will be submitted for presentation at local, national and international meetings (regional Pain Consultant Forums, British Pain Society, International Association for the Study of Pain). Data will be submitted to international peer-reviewed scientific journals (eg, PlosOne, British Journal of Pain, European Journal of Pain, Pain Medicine). We recognise that use of social media and academic social networks (eg, LinkedIn, Twitter) are becoming widely used dissemination tools,70 which we intend to use to ensure our research is visible.
Supplementary Material
Acknowledgments
The authors thank Boki Savelyich, Gina Dutton and Dr Santhana Kannan for their valuable comments on protocol drafts, and the Patient Public Involvement Group for their input towards the trial design.
Footnotes
Twitter: @HeneghanNicola, @Andy_Soundy
Contributors: Conceptualisation, BF and AR; methodology, BF, AS and NRH; validation, AS and NRH, writing—original draft preparation, BF and AR; writing—review and editing, AS and NRH; supervision, AS and NRH. All authors have read and agreed to the published version of the protocol manuscript.
Funding: This work was supported by THOR who are loaning the device free of charge. SWB Trust Charitable funds have provided a donation (Fund 0125) under their ‘Innovation’ Scheme.
Competing interests: THOR are providing in-kind sponsorship. They are not providing any other funding or sponsorship. They will not have the final decision over study design, conduct, access to data set, analyses, interpretation of data, manuscript writing or results dissemination.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Raja SN, Carr DB, Cohen M, et al. The revised international association for the study of pain definition of pain: concepts, challenges, and compromises. Pain 2020;161:1976–82. 10.1097/j.pain.0000000000001939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Treede R-D, Rief W, Barke A, et al. A classification of chronic pain for ICD-11. Pain 2015;156:1003–7. 10.1097/j.pain.0000000000000160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meints SM, Edwards RR. Evaluating psychosocial contributions to chronic pain outcomes. Prog Neuropsychopharmacol Biol Psychiatry 2018;87:168–82. 10.1016/j.pnpbp.2018.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Treede R-D, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the International classification of diseases (ICD-11). Pain 2019;160:19–27. 10.1097/j.pain.0000000000001384 [DOI] [PubMed] [Google Scholar]
- 5.Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth 2019;123:e273–83. 10.1016/j.bja.2019.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet 2020;396:1204–22. 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Metwally A, Shaikh Q, Aldiab A, et al. The prevalence of chronic pain and its associated factors among Saudi Al-Kharj population; a cross sectional study. BMC Musculoskelet Disord 2019;20:177. 10.1186/s12891-019-2555-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kia S, Choy E. Update on treatment guideline in fibromyalgia syndrome with focus on pharmacology. Biomedicines 2017;5:20. 10.3390/biomedicines5020020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taylor R, Pergolizzi JV, Puenpatom RA, et al. Economic implications of potential drug–drug interactions in chronic pain patients. Expert Rev Pharmacoeconomics Outcomes Res 2013;13:725–34. [DOI] [PubMed] [Google Scholar]
- 10.Kisselev SB, Moskvin SV. The use of laser therapy for patients with fibromyalgia: a critical literary review. J Lasers Med Sci 2019;10:12–20. 10.15171/jlms.2019.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institute for Health and Care Excellence . Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain NICE guideline [NG193], 2021. Available: https://www.nice.org.uk/guidance/ng193 [Accessed 24 May 2021]. [PubMed]
- 12.Taulaniemi A, Kankaanpää M, Rinne M, et al. Fear-avoidance beliefs are associated with exercise adherence: secondary analysis of a randomised controlled trial (RCT) among female healthcare workers with recurrent low back pain. BMC Sports Sci Med Rehabil 2020;12:28. 10.1186/s13102-020-00177-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mc Veigh JG, Lucas A, Hurley DA, et al. Patients’ perceptions of exercise therapy in the treatment of fibromyalgia syndrome: a survey. Musculoskeletal Care 2003;1:98–107. 10.1002/msc.45 [DOI] [PubMed] [Google Scholar]
- 14.Jack K, McLean SM, Moffett JK, et al. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Ther 2010;15:220–8. 10.1016/j.math.2009.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Institute for Health and Care Excellence . Commonly used treatments for chronic pain can do more harm than good and should not be used, says NICE in draft guidance, 2020. Available: https://www.nice.org.uk/news/article/commonly-used-treatments-for-chronic-pain-can-do-more-harm-than-good-and-should-not-be-used-says-nice-in-draft-guidance [Accessed 2 Aug 2021].
- 16.National Institute for Health and Care Excellence . Low-level laser therapy for preventing or treating oral mucositis caused by radiotherapy or chemotherapy (Interventional procedures guidance [IPG615]), 2018. Available: https://www.nice.org.uk/guidance/ipg615 [Accessed 18 Jul 2020].
- 17.Chung H, Dai T, Sharma SK, et al. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng 2012;40:516–33. 10.1007/s10439-011-0454-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Farivar S, Malekshahabi T, Shiari R. Biological effects of low level laser therapy. J Lasers Med Sci 2014;5:58–62. [PMC free article] [PubMed] [Google Scholar]
- 19.Clijsen R, Brunner A, Barbero M, et al. Effects of low-level laser therapy on pain in patients with musculoskeletal disorders: a systematic review and meta-analysis. Eur J Phys Rehabil Med 2017;53:603–10. 10.23736/S1973-9087.17.04432-X [DOI] [PubMed] [Google Scholar]
- 20.International Association for the Study of Pain . Myofascial pain [fact sheet] (revised 2017), 2010. Available: https://s3.amazonaws.com/rdcmsiasp/files/production/public/Content/ContentFolders/GlobalYearAgainstPain2/20092010MusculoskeletalPain/14.%20Myofascial%20Pain%20Fact%20Sheet%20Revised%202017.pdf [Accessed 5 Jul 2020].
- 21.Chow RT, Johnson MI, Lopes-Martins RAB, et al. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet 2009;374:1897–908. 10.1016/S0140-6736(09)61522-1 [DOI] [PubMed] [Google Scholar]
- 22.Haldeman S, Carroll L, Cassidy JD, et al. The bone and joint decade 2000–2010 Task force on neck pain and its associated disorders. Spine 2008;33:S5–7. 10.1097/BRS.0b013e3181643f40 [DOI] [PubMed] [Google Scholar]
- 23.Maia MLdeM, Bonjardim LR, Quintans JdeSS, et al. Effect of low-level laser therapy on pain levels in patients with temporomandibular disorders: a systematic review. J Appl Oral Sci 2012;20:594–602. 10.1590/s1678-77572012000600002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bisset L, Coombes B, Vicenzino B. Tennis elbow. BMJ Clin Evid 2011;2011:1117. [PMC free article] [PubMed] [Google Scholar]
- 25.Favejee MM, Huisstede BMA, Koes BW. Frozen shoulder: the effectiveness of conservative and surgical interventions-systematic review. Br J Sports Med 2011;45:49–56. 10.1136/bjsm.2010.071431 [DOI] [PubMed] [Google Scholar]
- 26.Glazov G, Yelland M, Emery J. Low-level laser therapy for chronic non-specific low back pain: a meta-analysis of randomised controlled trials. Acupunct Med 2016;34:328–41. 10.1136/acupmed-2015-011036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of physicians. Ann Intern Med 2017;166:514–30. 10.7326/M16-2367 [DOI] [PubMed] [Google Scholar]
- 28.Rayegani SM, Raeissadat SA, Heidari S, et al. Safety and effectiveness of low-level laser therapy in patients with knee osteoarthritis: a systematic review and meta-analysis. J Lasers Med Sci 2017;8:S12–19. 10.15171/jlms.2017.s3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deana NF, Zaror C, Sandoval P, et al. Effectiveness of low-level laser therapy in reducing orthodontic pain: a systematic review and meta-analysis. Pain Res Manag 2017;2017:8560652. 10.1155/2017/8560652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Andrade ALM, Bossini PS, Parizotto NA. Use of low level laser therapy to control neuropathic pain: a systematic review. J Photochem Photobiol B 2016;164:36–42. 10.1016/j.jphotobiol.2016.08.025 [DOI] [PubMed] [Google Scholar]
- 31.Huisstede BM, Hoogvliet P, Franke TP, et al. Carpal tunnel syndrome: effectiveness of physical therapy and Electrophysical modalities. An updated systematic review of randomized controlled trials. Arch Phys Med Rehabil 2018;99:1623–34. 10.1016/j.apmr.2017.08.482 [DOI] [PubMed] [Google Scholar]
- 32.Carcia CR, Martin RL, Houck J, et al. Achilles pain, stiffness, and muscle power deficits: Achilles tendinitis. J Orthop Sports Phys Ther 2010;40:A1–26. 10.2519/jospt.2010.0305 [DOI] [PubMed] [Google Scholar]
- 33.Zadik Y, Arany PR, Fregnani ER, et al. Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer 2019;27:3969–39. 10.1007/s00520-019-04890-2 [DOI] [PubMed] [Google Scholar]
- 34.Gonzalez-Lima F, Barrett DW. Augmentation of cognitive brain functions with transcranial lasers. Front Syst Neurosci 2014;8:36. 10.3389/fnsys.2014.00036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mease P, Arnold LM, Choy EH, et al. Fibromyalgia syndrome module at OMERACT 9: domain construct. J Rheumatol 2009;36:2318–29. 10.3899/jrheum.090367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355:i5239. 10.1136/bmj.i5239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Calvert M, King M, Mercieca-Bebber R, et al. SPIRIT-PRO Extension explanation and elaboration: guidelines for inclusion of patient-reported outcomes in protocols of clinical trials. BMJ Open 2021;11:e045105. 10.1136/bmjopen-2020-045105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ruaro JA, Fréz AR, Ruaro MB, et al. Low-level laser therapy to treat fibromyalgia. Lasers Med Sci 2014;29:1815–9. 10.1007/s10103-014-1566-8 [DOI] [PubMed] [Google Scholar]
- 39.Gür A, Karakoc M, Nas K, et al. Effects of low power laser and low dose amitriptyline therapy on clinical symptoms and quality of life in fibromyalgia: a single-blind, placebo-controlled trial. Rheumatol Int 2002;22:188–93. 10.1007/s00296-002-0221-z [DOI] [PubMed] [Google Scholar]
- 40.Tomazoni SS, Costa LdaCM, Guimarães LdeS, et al. Effects of photobiomodulation therapy in patients with chronic non-specific low back pain: protocol for a randomised placebo-controlled trial. BMJ Open 2017;7:e017202. 10.1136/bmjopen-2017-017202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.de Carvalho PdeTC, Leal-Junior ECP, Alves ACA, et al. Effect of low-level laser therapy on pain, quality of life and sleep in patients with fibromyalgia: study protocol for a double-blinded randomized controlled trial. Trials 2012;13:221. 10.1186/1745-6215-13-221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.da Silva MM, Albertini R, de Tarso Camillo de Carvalho P, et al. Randomized, blinded, controlled trial on effectiveness of photobiomodulation therapy and exercise training in the fibromyalgia treatment. Lasers Med Sci 2018;33:343–51. 10.1007/s10103-017-2388-2 [DOI] [PubMed] [Google Scholar]
- 43.Lopes-Martins RAB, Albertini R, Lopes-Martins PSL. Steroids block the anti-inflammatory effects of low level laser therapy. In: Hamblin MR, Waynant RW, Anders J, eds. Mechanisms for low-light therapy, 2006: 98–103. [Google Scholar]
- 44.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 45.Yeh S-W, Hong C-H, Shih M-C, et al. Low-level laser therapy for fibromyalgia: a systematic review and meta-analysis. Pain Physician 2019;22:241–54. [PubMed] [Google Scholar]
- 46.Moore CG, Carter RE, Nietert PJ, et al. Recommendations for planning pilot studies in clinical and translational research. Clin Transl Sci 2011;4:332–7. 10.1111/j.1752-8062.2011.00347.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lancaster GA, Thabane L. Guidelines for reporting non-randomised pilot and feasibility studies. Pilot Feasibility Stud 2019;5:114. 10.1186/s40814-019-0499-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lewis M, Bromley K, Sutton CJ, et al. Determining sample size for progression criteria for pragmatic pilot RCTs: the hypothesis test strikes back! Pilot Feasibility Stud 2021;7:40. 10.1186/s40814-021-00770-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kieser M, Wassmer G. On the use of the upper confidence limit for the variance from a pilot sample for sample size determination. Biometrics 1996;38:941–9. 10.1002/bimj.4710380806 [DOI] [Google Scholar]
- 50.Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res 2016;26:1753–60. 10.1177/1049732315617444 [DOI] [PubMed] [Google Scholar]
- 51.Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 2018;52:1893–907. 10.1007/s11135-017-0574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Soundy A, Lee RT, Kingstone T, et al. Experiences of healing therapy in patients with irritable bowel syndrome and inflammatory bowel disease. BMC Complement Altern Med 2015;15:106. 10.1186/s12906-015-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mendoza T, Mayne T, Rublee D, et al. Reliability and validity of a modified brief pain inventory short form in patients with osteoarthritis. Eur J Pain 2006;10:353–61. 10.1016/j.ejpain.2005.06.002 [DOI] [PubMed] [Google Scholar]
- 54.Galvez-Sánchez CM, de la Coba P, Duschek S, et al. Reliability, factor structure and predictive validity of the widespread pain index and symptom severity scales of the 2010 American College of rheumatology criteria of fibromyalgia. J Clin Med 2020;9:2460. 10.3390/jcm9082460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Takasaki H, Treleaven J. Construct validity and test-retest reliability of the fatigue severity scale in people with chronic neck pain. Arch Phys Med Rehabil 2013;94:1328–34. 10.1016/j.apmr.2012.12.013 [DOI] [PubMed] [Google Scholar]
- 56.Duruoz MT, Ulutatar F, Ozturk EC, et al. Assessment of the validity and reliability of the Jenkins sleep scale in ankylosing spondylitis. Int J Rheum Dis 2019;22:275–9. 10.1111/1756-185X.13447 [DOI] [PubMed] [Google Scholar]
- 57.et alBaranidharan G, Williams A, Wilson S. 2019 outcome measures. 1st edn, faculty of pain medicine of the Royal College of Anaesthetists. Available: https://www.britishpainsociety.org/static/uploads/resources/files/Outcome_Measures_January_2019.pdf [Accessed 6 Aug 2021].
- 58.Chang K-V, Hung C-H, Sun W-Z, et al. Evaluating soreness symptoms of fibromyalgia: establishment and validation of the revised fibromyalgia impact questionnaire with integration of soreness assessment. J Formos Med Assoc 2020;119:1211–8. 10.1016/j.jfma.2019.10.018 [DOI] [PubMed] [Google Scholar]
- 59.Jensen OK, Callesen J, Nielsen MG, et al. Reproducibility of tender point examination in chronic low back pain patients as measured by intrarater and inter-rater reliability and agreement: a validation study. BMJ Open 2013;3:e002532. 10.1136/bmjopen-2012-002532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bell T, Trost Z, Buelow MT, et al. Meta-analysis of cognitive performance in fibromyalgia. J Clin Exp Neuropsychol 2018;40:698–714. 10.1080/13803395.2017.1422699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Din NC, Meng ECT. Computerized Stroop tests: a review. J Psychol Psychother 2019;9:1. [Google Scholar]
- 62.Sim J, Lewis M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol 2012;65:301–8. 10.1016/j.jclinepi.2011.07.011 [DOI] [PubMed] [Google Scholar]
- 63.Office for National Statistics . Review of the dissemination of health statistics: confidentiality guidance 2006 [online]. Available: https://www.ons.gov.uk/file?uri=/methodology/methodologytopicsandstatisticalconcepts/disclosurecontrol/healthstatistics/confidentialityguidanctcm77181864.pdf [Accessed 2 Jul 2021].
- 64.Data Protection Act . Data protection act 2018 [online], 2018. Available: https://www.gov.uk/government/collections/data-protection-act-2018 [Accessed 15 Jul 2021].
- 65.Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health 2019;11:589–97. 10.1080/2159676X.2019.1628806 [DOI] [Google Scholar]
- 66.Jakobsen JC, Gluud C, Wetterslev J, et al. When and how should multiple imputation be used for handling missing data in randomised clinical trials – a practical guide with flowcharts. BMC Med Res Methodol 2017;17. 10.1186/s12874-017-0442-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.UK Standards for Public Involvement . Better public involvement for better health and social care research, 2019. Available: https://www.invo.org.uk/wp-content/uploads/2019/11/UK-standards-for-public-involvement-v6.pdf [Accessed 5 Mar 2020].
- 68.Staniszewska S, Brett J, Simera I, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ 2017;358:j3453. 10.1136/bmj.j3453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Health Research Authority . Publication and dissemination of research findings [online], 2021. Available: https://www.hra.nhs.uk/planning-and-improving-research/best-practice/publication-and-dissemination-research-findings/ [Accessed 2nd Aug 2021].
- 70.Ross-Hellauer T, Tennant JP, Banelytė V, et al. Ten simple rules for innovative dissemination of research. PLoS Comput Biol 2020;16:e1007704. 10.1371/journal.pcbi.1007704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wolfe F, Smythe HA, Yunus MB. The American College of rheumatology 1990 criteria for the classification of fibromyalgia. Report of the multicenter criteria Committee. Arthritis Rheum 1990;33:160–72. 10.1002/art.1780330203 [DOI] [PubMed] [Google Scholar]
- 72.Tastekin N, Uzunca K, Sut N, et al. Discriminative value of tender points in fibromyalgia syndrome. Pain Med 2010;11:466–71. 10.1111/j.1526-4637.2009.00784.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-060058supp001.pdf (1.5MB, pdf)
bmjopen-2021-060058supp002.pdf (162.9KB, pdf)