Abstract
Hesitancy to receive the COVID-19 vaccine among healthcare workers (HCWs) in low-resource settings, such as the Democratic Republic of the Congo (DRC), is a major global health challenge. This study identifies changes in willingness to receive vaccination among 588 HCWs in the DRC and reported influences on COVID-19 vaccination intentions. Up to 25 repeated measures were collected from participants between August 2020 to August 2021. Among the overall cohort, between August 2020 and mid-March 2021, the proportion of HCWs in each period of data collection reporting COVID-19 vaccine hesitancy ranged from 8.6% (95% CI: 5.97, 11.24) to 24.3% (95% CI: 20.12, 28.55). By early April 2021, the proportion reporting hesitancy more than doubled (52.0%; 95% CI: 46.22, 57.83). While hesitancy in the cohort began to decline by late-June 2021, 22.6% (95% CI: 18.05, 27.18) respondents indicated hesitancy in late-August 2021 which remains greater than the proportion of hesitancy at any time prior to early-March 2021. Patterns in reported influences on COVID-19 vaccination were varied with the proportion reporting some influences (e.g., no serious side effects, country of vaccine production) remaining stable throughout the year and other factors (e.g., recommendation of Ministry of Health, ease of vaccination) falling in popularity among respondents. Agreement that the national vaccination schedule should be followed apart from the COVID-19 vaccine remained high among respondents throughout the study period. This study shows that, among a cohort of HCWs in the DRC who have likely been influenced by regional, national, and global factors, COVID-19 vaccine hesitancy has fluctuated during the pandemic and should not be treated as a static factor. Additional research to determine which factors most influence HCWs’ willingness to receive the COVID-19 vaccine offers opportunities to reduce vaccine hesitancy among this important population through tailored public health messaging.
Keywords: Vaccine hesitancy, COVID-19 vaccine, Healthcare worker
1. Introduction
Vaccine hesitancy is a global health threat and major challenge to successful control of COVID-19 transmission [1], [2], [3]. The World Health Organization Strategic Advisory Group of Experts (SAGE) on vaccination has adapted the term “vaccine hesitancy” to refer to a delay in accepting or refusing vaccination despite the availability of immunization services [4]. A review of vaccine hesitancy studies in 33 different countries conducted in 2020 found that COVID-19 vaccine acceptance among the general population was about 70% or greater in most of the countries studied [2]. However, the lowest vaccine acceptance rates, between 23.6% and 58.9%, were generally reported in Africa, the Middle East, and several European countries including Russia. The Africa Centers for Disease Control and Prevention (CDC) published that across a 15-country study, the Democratic Republic of the Congo (DRC) had the lowest reported willingness to accept a COVID-19 vaccine with about 59% Congolese respondents willing to receive vaccination [5].
The previously mentioned review [2] found only eight studies of COVID-19 vaccine hesitancy among healthcare workers (HCWs) with the lowest levels of acceptance among HCWs in the DRC (27.7%) [6]. HCWs are a critical population for vaccination not only in terms of preventing COVID-19 transmission to vulnerable populations and reducing frontline worker shortages [7], but also as promoters of vaccination [8], [9], [10]. HCWs who are vaccinated or are willing to receive vaccinations are consistently found to be more likely to recommend vaccination to patients [11], [12], [13], [14].
The DRC continues to struggle with routine immunization uptake due to an underfinanced healthcare system, lack of access to and availability of vaccines, and a need for stronger HCW training and community based-surveillance [15], [16], [17]. During the COVID-19 pandemic specifically, issues such as disbelief in the existence of COVID-19 and a distrust in the vaccine among HCWs have emerged [18]. Four cross-sectional studies have investigated willingness to receive the COVID-19 vaccine in the DRC. The first was conducted among HCWs working at 23 Congolese hospitals in three different provinces between March 20th and April 30th of 2020 [6]. Less than one-third (27.7%) of the 613 participants reported that they would get the COVID-19 vaccine if it were available to them. The second study was conducted using an online questionnaire a few months later between August 24th and September 8th of 2020 [18]. Among 4,160 respondents from 17 provinces across the DRC, 55.9% reported they would be willing to be vaccinated for COVID-19. As previously discussed, an Africa CDC study found that 59% of 1,007 Congolese respondents reported willingness to receive a COVID-19 vaccine with substantial variation by region (85% willingness in Kasai Occidental compared to 38% in Equateur). Face-to-face data collection for this study occurred between late September and mid-October 2020 [5]. The most recent study was conducted between January and March 2021 and also utilized an online survey tool [19]. While this study did not directly ask participants whether they would be vaccinated if offered, two-thirds (66.5%) of the 11,971 respondents from nine different provinces reported a fear that the vaccine did not prevent COVID-19.
In their cross-sectional analysis, Nzaji et al. [6] reported that among Congolese HCW study participants, being male, a doctor, and having a positive attitude towards COVID-19 were associated with intention to receive the COVID-19 vaccine. Within a general population sample, Ditekemena et al. [18] reported that Congolese individuals working in healthcare, in a lower income group, and who deny the existence of COVID-19 were more likely to report COVID-19 vaccine hesitation. Willingness to receive vaccination is, however, likely to fluctuate over time. Several models of vaccination behavior have been proposed typically focusing on risk perception of disease, environmental factors related to convenience of vaccine access, and confidence in the efficacy of vaccines [4], [8]. The context of vaccination against COVID-19 is further complicated by global discussions of politics, misinformation, trust in vaccine development processes, and social responsibility [3], [8].
Public opinion and attention regarding COVID-19 are largely influenced by media coverage [20], [21], [22]. During the past year, major developments in the COVID-19 pandemic have been frequent from pathogen identification to national lockdowns to vaccine development and rollout and recently, the emergence of the Delta and Omicron variants. Research findings that predominant narratives in the media and perceived social norms are also highly influential on vaccination uptake [3], [8], [23], [24], [25], [26] support the hypothesis that COVID-19 vaccine hesitancy has not been static among HCWs, particularly in the DRC, during the pandemic. For example, major events of interest include more than 1.7 million doses of COVID-19 vaccine (AstraZeneca/COVIDSHEILD) arriving in the DRC on March 2, 2021 [27]. At this time, the AstraZeneca COVID-19 vaccine was the only COVID-19 vaccine available in DRC as shipments of Pfizer-BioNTech, Moderna, Janssen (Johnson and Johnson), and Sinovac vaccine did not arrive to the country until September 2021 [28], [29]. On March 11, 2021, several European countries with the support of the European Medicines Agency (EMA) paused vaccinations with the AstraZeneca COVID-19 vaccine due to reports regarding a rare but serious blood clotting side effect [30]. Vaccine rollout in the DRC was delayed until April 19, 2021 to heed any findings from the EMA investigations on vaccine side effects [31] . During this time, rumors circulated on social media, television, and radio about the quality of the vaccine and when the vaccine would be available and to whom [32]. Before the end of June 2021, when all vaccine received in DRC was due to expire, 1.3 million doses were reallocated to nearby countries in Africa. According to the Our World in Data COVID-19 vaccination dataset [33], only 1,710,177 individuals in the DRC are fully vaccinated against COVID-19 (1.85% of the population) as of June 5, 2022.
The current study extends upon previous research conducted in the DRC by collecting measures longitudinally within a HCW cohort throughout the COVID-19 pandemic. Between August 2020 and August 2021, Congolese HCWs in our cohort were consistently monitored for changes in knowledge, attitudes, and practices regarding COVID-19 prevention, occupational and community exposures, and possible incidence of primary SARS-CoV-2 infection. This analysis aims to provide a thorough outlook on vaccine hesitancy and self-identified influences on COVID-19 vaccination decision-making among a sample of HCWs in the DRC.
2. Methods
2.1. Study design and sample participants
A cohort of HCWs, 18 years and older from four locations in DRC (Kinshasa, Beni, Kikwit, Mbandaka), were enrolled for a longitudinal study that began data collection in August 2020 (starting in epidemiological (epi) week 33; [34]). Participants were selected from a larger cohort of participants enrolled by our team in a study entitled: “Epidemiology, Immunopathology Immunogenetics and Sequelae of Ebola Virus and other Viral Hemorrhagic Fever Infections,” which has been on-going since 2016. HCWs working at randomly selected facilities located in Kinshasa, Kikwit, and Mbandaka were all invited to participate in this original study. However, in Beni, HCWs who had received the Ebola vaccine were specifically targeted. Therefore, only health facilities with confirmed Ebola patients were chosen due to the ring vaccination strategy [35] and HCWs in Beni working at those facilities who had received the Ebola vaccine (i.e., rVSVΔG-ZEBOV-GP Ebola vaccine) were eligible to participate in the study. During this initial study, 1,871 participants consented to future contact for additional studies during the informed consent process and participants for the current study were randomly selected for participation among this pool.
A calculated sample of 653 potential participants contacted was estimated to have more than 80% power to detect a 20% difference in the proportion of participants willing to take a COVID-19 vaccine based on a previous publication [36], and included a non-response/refusal rate of 25%. Thus, we randomly contacted 677 HCWs from the four sites (213 Kinshasa, 232 Kikwit, 112 Mbandaka, and 120 Beni) of the original cohort to meet the minimum calculated sample size. Among these, 81 refused participation and 8 individuals consented but never completed the baseline questionnaire or were missing basic demographic information (e.g., age, place of living, gender). Among 9,457 responses collected across the study, 176 (1.9%) specific participant responses were excluded from the analysis due to errors in subject identification and 58 (0.6%) responses were excluded due to missing data on outcomes of interest (i.e., vaccine hesitancy and influences on vaccination).
2.2. Study procedures
Prior to enrollment, study interviewers were trained on study procedures and on conducting phone-based interviews including obtaining verbal consent. Participants verbally consented to participate and were contacted twice a month to complete follow up questionnaires. Study interviewers administered questionnaires over the phone using electronic questionnaires in Open Data Kit (ODK) Collect [37]. Data collection for a two-part baseline questionnaire began on August 11, 2020 (epi week 33) and follow up began in mid-September 2020 (epi week 38). Follow up data collection typically occurred from a Monday to the following Tuesday of the next week. Baseline phone calls took between 1 and 1.5 h to complete and follow up calls took between 10 and 20 min to complete. Forms and questionnaires were written in English, translated into French and local languages (Lingala and Swahili), and translated back into English to ensure quality of translation. Subjects were assigned unique codes to link to their repeated measures.
2.3. Variables of interest
Hesitancy to COVID-19 vaccination was dichotomized from a 5-point scale. Based on previous publications [38], we defined vaccine hesitant as responding “strongly disagree”, “disagree”, or “neutral” to the question, “If a vaccine [for COVID-19] was recommended for me, I would get it.” Responses of “strongly agree” or “agree” were treated as not hesitant to COVID-19 vaccination. Participants were also asked a series of yes or no questions regarding their influences on their decision to receive the COVID-19 vaccine (e.g., “If a COVID-19 vaccine is made available in my country, my decision of whether or not to get vaccinated would depend on recommendation from my family doctor.”) Additionally, respondents were asked whether they agreed with the statement, “Apart from COVID-19, I think everyone should be vaccinated according to the national vaccination schedule.” Responses of “No” or “Prefer not to say/don’t know” were considered as generally vaccine hesitant.
Demographic variables of interest in this analysis included original recruitment location (Kinshasa, Beni, Kikwit, Mbandaka), age, gender, and level of education. Age in years was dichotomized as younger than 55 years old and 55 or older to capture the current age cutoff in DRC vaccination policy and additional risk of severe COVID-19 infection [27], [39]. Educational attainment was collapsed into less than high school or high school degree, some college or Associate degree, and Bachelor’s or advanced degree. Whether the subject self-identified as having a chronic disease was also included in analyses to capture underlying health risk. Participants were asked “Do you have a chronic disease (including chronic lung disease, diabetes, cardiovascular disease, chronic renal or liver disease) or are otherwise immunocompromised?”.
2.4. Statistical analysis
Participants’ responses throughout the study were linked using a unique identification code. Time was operationalized using epi weeks, a standard measure of each week throughout the calendar year in which the week begins on Sunday and ends on Saturday [34]. Since data collection typically occurred at the beginning of a week (i.e., Monday) to the middle of the following week, the epi weeks were grouped such that dates of data collection fell within the corresponding two epi weeks. There was no data collection in epi weeks 52 and 53 (2020) or 1 and 2 (2021) due to the winter holidays. The proportion of HCWs in each epi week interval reporting hesitancy vaccination was plotted across time. Similarly, the proportion of HCWs reporting various influences on their decision to receive the COVID-19 vaccine was plotted across time. COVID-19 vaccine hesitancy was additionally plotted over time within levels of key demographic variables. Line graphs include error bars with +/- 2 standard error (95% confidence interval) to display the uncertainty of the proportion in each epi week interval [40]. Relative positioning of error bars should not be interpreted as a measure of significance.
2.5. Ethical
Institutional review board approval was obtained from the University of California, Los Angeles (IRB#20–001321) as well as the Kinshasa School of Public Health at the University of Kinshasa (ESP/CE/118/2020), which served as the local ethics committee. During phone calls, participants provided an oral consent to participate. Original cohorts were enrolled under ethics approvals: UCLA IRB #16–001346/KSPH IRB: ESP/CE/022/2017.
3. Results
HCW respondents included in this analysis (n = 588) contributed a total of 9,223 responses on key outcomes (i.e., vaccine hesitancy and influences on vaccination) across 25 questionnaires. Data utilized in this analysis were collected between August 11, 2020 and August 25, 2021. On average, each participant contributed 15.7 responses (SD: 6.48, median: 17.0, IQR: 9.5, mode: 21.0). About one-third (34.0%) of participants were originally recruited in Kikwit, 29.8% in Kinshasa, 19.7% in Beni, and 16.5% in Mbandaka (Table 1 ). The average age among the respondents was 43.0 years old with 17.5% of the cohort being 55 years old or older. Over half (55.1%) of the participants are male and nearly two-thirds (63.6%) reported having some college education or an Associate degree. Nearly one in twelve HCWs (7.8%) self-identified as having a chronic disease or otherwise being immunocompromised.
Table 1.
Sample characteristics of a cohort of 588 healthcare workers (HCWs) in Kinshasa, Kikwit, Mbandaka, and Beni in the Democratic Republic of the Congo, August 2020 to August 2021.
| N = 588 | |
|---|---|
| Location, n (%) | |
| Kinshasa | 175 (29.8) |
| Kikwit | 200 (34.0) |
| Mbandaka | 97 (16.5) |
| Beni | 116 (19.7) |
| Age (in years) | |
| Mean (SD) | 43.0 |
| Median [Min, Max] | 42.0 [20.0, 81.0] |
| Age relative to 55 years, n (%) | |
| <55 | 485 (82.5) |
| 55+ | 103 (17.5) |
| Gender, n (%) | |
| Female | 264 (44.9) |
| Male | 324 (55.1) |
| Education, n (%) | |
| Less than HS/HS graduate | 93 (15.8) |
| Some college/Associate degree | 374 (63.6) |
| Bachelor’s/Advanced degree | 120 (20.4) |
| Missing | 1 (0.2%) |
| Chronic disease or immunocompromised, n (%) | |
| Yes | 46 (7.8) |
| No | 542 (92.2) |
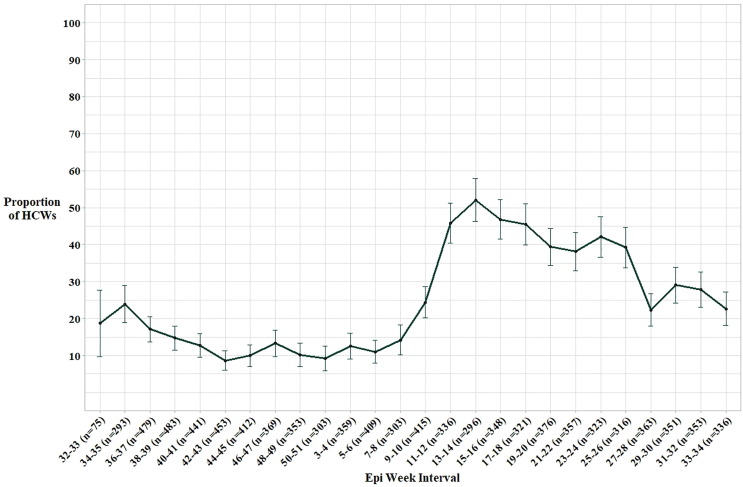
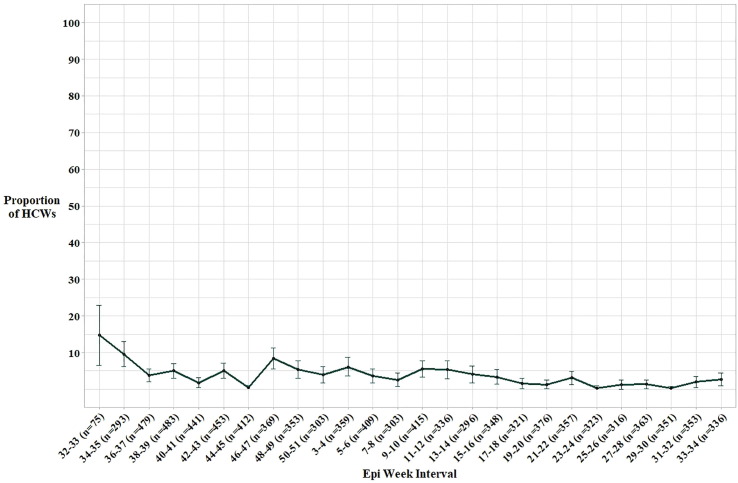
Between August 2020 and mid-March 2021 [epi weeks 33 (2020)-10 (2021)], the proportion of HCW respondents reporting COVID-19 vaccine hesitancy in a particular epi week interval did not rise above 24.3% (95% CI: 20.12, 28.55; Fig. 1 and Supplementary Material Table 1). However, in the following weeks of 2021 (March 14th to March 27th, epi weeks 11–12) the proportion of hesitant respondents nearly doubled to 45.8% (95% CI: 40.40, 51.27). Between mid-March and late-June (epi weeks 11–26), hesitancy among the cohort ranged from 38.1% (95% CI: 32.95, 43.24) to 52.0% (95% CI: 46.22, 57.83). By late-August 2021 (epi weeks 33–34), vaccine hesitancy among the respondents had decreased to 22.6% (95% CI: 18.05, 27.18).
Fig. 1.
Proportion of HCWs reporting COVID-19 vaccine hesitancy overall with 95% confidence interval error bars, Democratic Republic of the Congo, August 2020 to August 2021 (n=588).
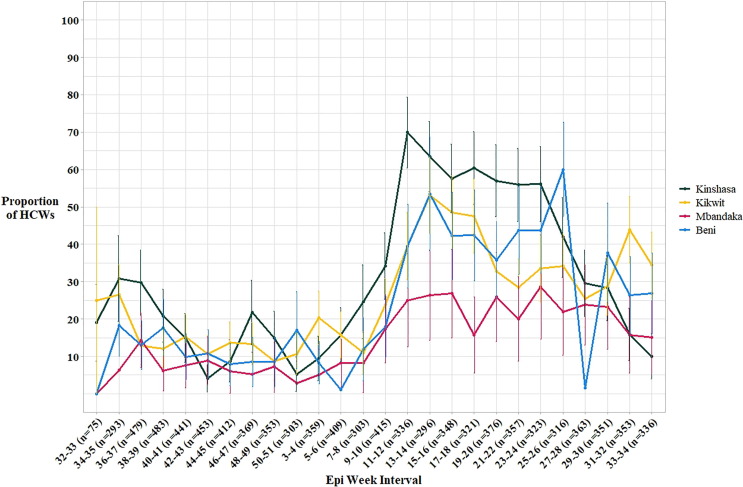
In our sample, COVID-19 vaccine hesitancy levels among HCW respondents from different localities were similar from early August 2020 to mid-March 2021 (epi weeks 33–10; Fig. 2 and Supplementary Material Table 2). Differences in hesitancy between localities became stark after mid-March 2021 (epi week 11). Respondents from Kinshasa emerged as tending to have greater levels of hesitancy while Mbandaka had lower hesitancy compared to the other regions during this time. Between March 14th and March 27th of 2021 (epi weeks 11–12), 69.9% (95% CI: 60.38, 79.41) of HCW respondents from Kinshasa reported vaccine hesitancy compared to 25.0% (95% CI: 12.50, 37.50) from Mbandaka. From mid-March to late-August 2021 (epi weeks 11–34), the proportion of HCWs from Mbandaka reporting vaccine hesitancy remained relatively stable with between about 15–30% of respondents reporting hesitancy in each two-week period. Levels of hesitancy among participants from Kikwit and Beni were more variable following mid-March (epi week 11), with proportions of hesitant HCWs typically ranging between about 25% and 55% and no clear patterns emerging. Vaccine hesitancy among HCWs from Kinshasa dramatically decreased between mid-June and late-August 2021 (epi weeks 25–34). Specifically, 10.0% (95% CI: 4.00, 16.00) of HCW respondents from Kinshasa in late-August 2021 (epi weeks 33–34) reported hesitancy compared to 56.1% (95% CI: 46.10, 66.15) of respondents in mid-June (epi weeks 23–24).
Fig. 2.
Proportion of HCWs reporting COVID-19 vaccine hesitancy by location with 95% confidence interval error bars, Democratic Republic of the Congo, August 2020 to August 2021 (n=588).
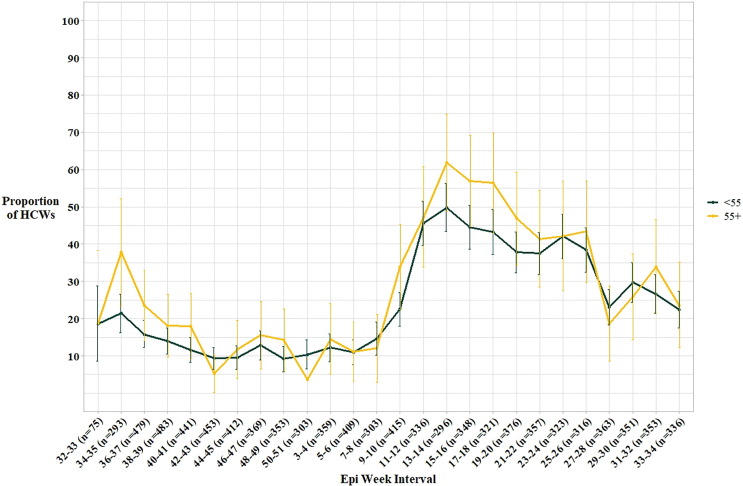
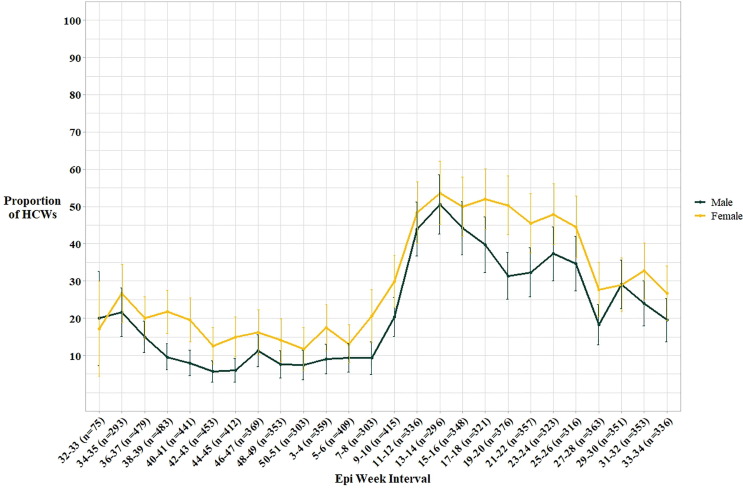
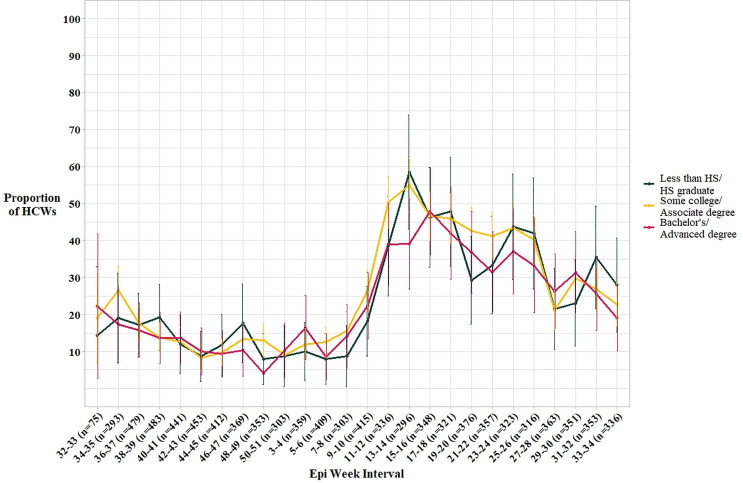
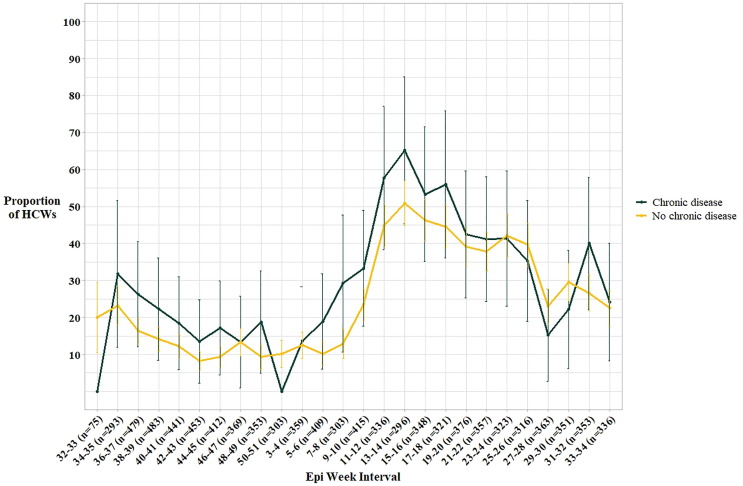
In our study, patterns of COVID-19 vaccine hesitancy did not appear to differ considerably based on age relative to 55 years old (Fig. 3 and Supplementary Material Table 3). Alternatively, a larger proportion of female HCWs reported hesitancy than male HCW respondents in almost every epi week interval of the study (Fig. 4 and Supplementary Material Table 4). Both male and female participants followed a similar trend of reported hesitancy throughout the beginning of the observation period to mid-March 2021 [epi weeks 33 (2020)-10 (2021)]. From mid-March to late-June 2021 (epi weeks 11–26), the proportion of hesitant female HCW respondents remained around 50%, but hesitancy among male HCWs appeared to decrease. Over half of female respondents (50.3%, 95% CI: 42.38, 58.24) reported hesitancy between May 3rd and 16th (epi weeks 19–20) compared to 31.3% (95% CI: 25.04, 37.63) of males. Respondents within the three education levels had similar levels of hesitancy throughout the observation period and followed the pattern of a substantial increase in reported hesitancy in mid-March 2021 followed by a gradual decrease hesitancy by late-August 2021 (Fig. 5 and Supplementary Material Table 5). In most epi week intervals, a greater proportion of participants with chronic disease reported COVID-19 vaccine hesitancy compared to those without chronic disease (Fig. 6 and Supplementary Material Table 6). However, both groups followed a similar pattern in reported vaccine hesitancy over time and the difference between the groups was never greater than 20.0% which occurred in the first week of data collection when no respondents identifying as having chronic disease (n = 5) reported vaccine hesitancy.
Fig. 3.
Proportion of HCWs reporting COVID-19 vaccine hesitancy by age above or below 55 with 95% confidence interval error bars, Democratic Republic of the Congo, August 2020 to August 2021 (n=588).
Fig. 4.
Proportion of HCWs reporting COVID-19 vaccine hesitancy by gender with 95% confidence interval error bars, Democratic Republic of the Congo, August 2020 to August 2021 (n=588).
Fig. 5.
Proportion of HCWs reporting COVID-19 vaccine hesitancy by education level with 95% confidence interval error bars, Democratic Republic of the Congo, August 2020 to August 2021 (n=588).
Fig. 6.
Proportion of HCWs reporting COVID-19 vaccine hesitancy by chronic disease status with 95% confidence interval error bars, Democratic Republic of the Congo, August 2020 to August 2021 (n=588).
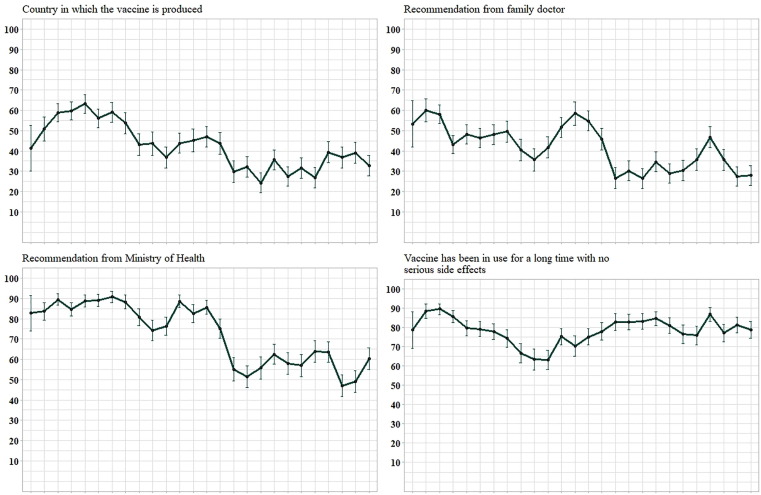
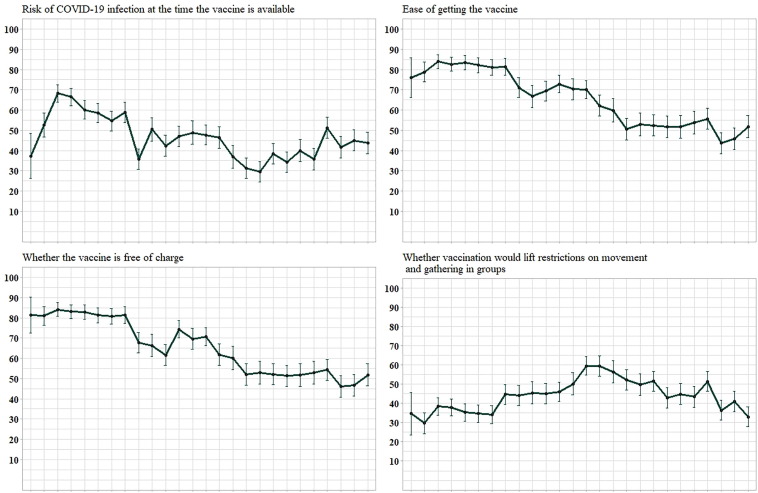
Several influences on HCWs’ COVID-19 vaccination decision followed similar reporting patterns throughout the follow up period (Fig. 7, Fig. 8 and Supplementary Material Table 7). The proportion of respondents considering the country in which the vaccine is produced, recommendation from a family doctor, the risk of COVID-19 infection, and whether vaccination would lift restrictions never rose above 68.3% throughout the study. Prior to late-March 2021 (epi weeks 11–12), a large majority of HCW respondents, between 74.3% (95% CI: 69.23, 79.28) and 90.8% (95% CI: 87.93, 93.63), reported being influenced by the recommendation of the Ministry of Health. However, by late-August 2021 (epi weeks 33–34), only 60.4% (95% CI: 55.08, 65.75) of participants responded that they would consider the recommendation of the Ministry of Health when deciding to get the COVID-19 vaccine. Whether the vaccine had been in use for a long time with no serious side effects remained a popular influence among respondents throughout the year. About 90% (88.4; 95% CI: 84.65, 92.14) of respondents endorsed this influence on their vaccination decision in late-August 2020 (epi weeks 34–35) compared to 78.9 % (95% CI: 74.41, 83.32) in late-August 2021 (epi weeks 33–34). The proportion of respondents considering ease of getting the vaccine and whether it is free of charge decreased gradually during the study. Between 66.3% (95% CI: 60.91, 71.77) and 84.1% (95% CI: 80.80, 87.47) of respondents reported these two influences each epi week interval in 2020 but by late-August 2021 (epi weeks 33–34), only about half (51.8%; 95% CI: 46.33, 57.24) of the HCW respondents reported considering ease and cost of getting the vaccine in their decision to get vaccinated against COVID-19.
Fig. 7.
Proportion of HCWs reporting influences on COVID-19 vaccination, Democratic Republic of the Congo, August 2020 to August 2021 (n=588)Note. Axes for plots are the same as axes in Figures 2-7. 95% confidence interval error bars included.
Fig. 8.
Proportion of HCWs reporting influences on COVID-19 vaccination, Democratic Republic of the Congo, August 2020 to August 2021 (n=588) – Continued Note. Axes for plots are the same as axes in Figures 2-8. 95% confidence interval error bars included.
Disagreement with the statement that, apart from the COVID-19 vaccine, the national vaccination schedule in DRC should be followed was consistently low among respondents throughout the study. After the first week of data collection, the proportion of respondents reporting disagreement with national vaccination schedule adherence ranged from 0.3% (95% CI: 0.00, 0.85) in late-July 2021 (epi weeks 29–30) to 9.6% (95% CI: 6.12, 12.99) in late-August 2020 [(epi weeks 34–35); Fig. 9 and Supplementary Material Table 8].
Fig. 9.
Proportion of HCWs reporting general vaccine hesitancy overall with 95% confidence interval error bars, Democratic Republic of the Congo, August 2020 to August 2021 (n=588).
4. Discussion
Overall, among our cohort of HCW respondents, there was a dramatic increase in COVID-19 vaccine hesitancy around mid-March 2021 (epi weeks 11–12) followed by a gradual decrease between late-March and late-August 2021. Despite smaller proportions of respondents reporting hesitancy to receive the COVID-19 vaccine in recent weeks, the level of hesitancy is still generally greater than that observed among the cohort between August 2020 and early-March 2021. Mid-March 2021 emerges in the pattern of hesitancy among almost all subgroups investigated as an inflection point when the proportion of participants reporting COVID-19 vaccine hesitancy rose dramatically. Only among HCW respondents from Mbandaka was the increase in reported hesitancy relatively small compared to participants from other locations. The timing of this rise in hesitancy among the respondents in our HCW cohort coincided with the initial COVID-19 vaccine delivery to the DRC as well as a halt of vaccinations with this same vaccine, AstraZeneca, in the EU due to the reporting of rare but serious side effects [27], [30]. The Ministry of Health in the DRC delayed its vaccination campaign due to news of these side effects during this time as well [31].
Of note, the dramatic decrease in COVID-19 vaccine hesitancy reported by respondents beginning in late-June 2021 coincided with the third wave of COVID-19 infection in the DRC. The highest level of COVID-19 transmission in the DRC during the study follow up period occurred on June 20, 2021 with 3.99 individuals infected per million people [33]. Between late-May and late-July 2021, the proportion of the total population in the DRC who had received at least one dose of the COVID-19 vaccine increased from 0.03% to 0.08%. We speculate that with the increased transmission and burden of COVID-19 in the DRC during this time, HCWs might have felt more susceptible to disease and as a result, more willing to receive vaccination. Importantly, support for following the national vaccination schedule, apart from the COVID-19 vaccine, remained high throughout the study indicating that general attitudes towards routine vaccination among this cohort of HCWs were possibly little affected by the events of the pandemic.
Although the exact reasons for the disparity in hesitancy between localities needs to be further investigated, contextual differences between these localities should be considered. Kinshasa is the capital city and the province with the largest population in the DRC – nearly 15 million people [41]. North Kivu (Beni) is also considered an urban province and has struggled with security issues and on-going civil conflict over the past two decades. Kwilu Province (Kikwit) and Equateur Province (Mbandaka) are both more rural provinces [42]. Kinshasa most consistently performs better than Kwilu, Equateur, and North Kivu Provinces on general health indicators such as childhood vaccination coverage and nutrition, access to proper drinking water, and child mortality [42], [43] which is expected as the capital of the country and hub for national activities, including product distribution and centralization of policies. Nzaji et al. [6] and Ditekemena et al. [18], speculate that the speed at which misinformation spreads through social media, television, radio, and newspapers could have contributed to the differences in hesitancy observed between regions of the DRC. Cities with low access to these media outlets are less likely to be exposed to circulating misinformation about the vaccine while cities with greater access might be likely to be more exposed. Internet, television, radio, and print media are more accessible in Kinshasa than any other city in the DRC [42].
Specifically, the stark difference between the higher levels of reported hesitancy to the COVID-19 vaccine among respondents from Kinshasa compared to lower hesitancy observed among those from Mbandaka might be due to differing experiences with other infectious disease outbreaks, such as Ebola. Kikwit (Kwilu Province), Mbandaka (Equateur Province), and Beni (North Kivu Province) were sites of previous Ebola outbreaks in 1995, 2018, 2018–2020, respectively, while Kinshasa has never experienced an Ebola outbreak [44]. During data collection for this study, both Mbandaka (2020) and Beni (2021) experienced additional Ebola outbreaks. The vast majority of COVID-19 burden in terms of reported cases, hospitalizations, and deaths in the DRC have occurred in Kinshasa [15], [45]. On the other hand, Mbandaka has maintained a low prevalence of COVID-19 diagnoses throughout the pandemic but experienced an Ebola outbreak between June and November 2020 during our study follow up [46]. The 2018 Ebola outbreak in Mbandaka was the first outbreak in which the novel Ebola vaccine (i.e., rVSVΔG-ZEBOV-GP Ebola vaccine) was implemented [47]. HCWs in our cohort from Mbandaka likely have firsthand experience with implementation of a relatively new vaccine as a focus of the Ebola outbreak responses in both 2018 and again in 2020. Specifically, 48.5% of the HCWs from Mbandaka included in this cohort received vaccination with the rVSVΔG-ZEBOV-GP Ebola vaccine prior to licensure [unpublished data]. Knowledge and involvement in the rollout and subsequent successes of the Ebola vaccine might lead HCWs from Mbandaka to find the novel COVID-19 vaccine more acceptable. However, the same result was not observed among our Beni respondents, all of whom received the rVSVΔG-ZEBOV-GP Ebola vaccine as a part of enrollment in the original cohort as previously discussed.
When considering future COVID-19 vaccination, the issue most consistently reported by the most respondents throughout the study was whether the COVID-19 vaccine has been in use for a prolonged period with no serious side effects. Interestingly, the proportion of participants reporting this consideration each epi week interval did not noticeably fluctuate when some EU members announced a halt in AstraZeneca vaccination, the only vaccine available in the DRC at the time, due to rare but serious blood clot concerns in mid-March 2021. Considering the recommendation of the Ministry of Health when deciding whether to get the COVID-19 vaccine was reported by a large majority of the HCW respondents until around mid-March 2021. Although speculative, this observed decrease in consideration among the HCW respondents could be related to the Ministry of Health’s decision to delay launching its vaccination campaign for a month after vaccine had arrived in the DRC [31]. Considerations for the ease of getting the vaccine as well as whether the vaccine would be free decreased among the cohort over the study year, but the proportion of participants reporting any other considerations did not appear to increase over time indicating the possibility that other influences not captured by this study, such as social norms or perceptions of population-level benefits [8], [23], [48], may be at play in more recent weeks.
The findings of this study should be interpreted in light of its limitations. This study presents patterns of vaccine hesitancy and vaccination influences over time among a cohort that is composed of HCWs enrolled through sampling in health facilities participating in a previous Ebola related study. The results presented do not control for the influence of any other factors, such as risk perception, COVID-19 exposure, or experience with other novel vaccines, or for the longitudinal nature of these data. Our cohort was ascertained using a previous study cohort of which a proportion of HCWs were selected based on their experience with a novel Ebola vaccine. Therefore, our cohort might not be representative of all HCWs in the DRC and, specifically, overrepresent HCWs that are receptive to a novel vaccine as an outbreak response tool. Importantly, within the overall cohort of 588 HCWs, a varying number participated in each questionnaire (average response rate: 61.6%, range: 49.7–89.1%). Although intention to receive the COVID-19 vaccine is presented by demographic groups, the distribution of covariates among the respondents differs between epi week intervals making comparison between groups potentially misleading. Thus, the patterns of vaccine intentions and vaccination considerations should not be a source of conclusions regarding the causes of differences between subgroups or general patterns over time but rather of hypothesis generation. These patterns do not imply causality of any specific events or other influences on the outcomes of interest but rather present the patterns of hesitancy and vaccination considerations over time as they were self-reported by our cohort. While the general pattern that mid-March 2021 appears to be an inflection point for COVID-19 vaccine hesitancy, the specific cause for this observed increase in hesitancy is undetermined. Likely, a combination of factors related to global, national, and local news as well as individual knowledge, attitudes, and perceptions influenced the cohorts’ responses. Further, errors in recording unique identifiers of participants required observations to be dropped from analysis.
To the authors’ knowledge, this is the first longitudinal study to measure vaccine hesitancy and influences among a HCW cohort in the DRC over time. This study adds to previous cross-sectional research [5], [6], [18], [19] by providing a more comprehensive understanding of hesitancy to vaccination among HCWs from different regions throughout the COVID-19 pandemic. A similar study conducted in Australia [49] observed different patterns of COVID-19 vaccine hesitancy over time compared to the present study supporting the hypothesis that vaccine hesitancy is likely highly setting dependent. Further, knowledge of what Congolese HCWs consider in their decision to receive vaccination is critical to the success of vaccine campaigns. Observing these outcomes over time not only provides an update on vaccine attitudes among an important population for controlling COVID-19, but also stimulates hypothesis generation of how and why these attitudes may have changed and, in the case of vaccination apart from COVID-19, not changed during the pandemic.
These findings generally support a fluctuation in vaccine hesitancy and considerations for future vaccination among HCWs in the DRC. It is vital for public health leaders in the DRC promoting COVID-19 prevention through vaccination to be aware of current measures of vaccine hesitancy and related attitudes rather than relying on outdated data that may not be specific to the target population for increased vaccination. Ongoing surveillance of COVID-19 vaccination sentiments at a regional-level and among key demographic groups will facilitate more tailored and effective COVID-19 vaccine promotion messages. Future research should focus on determining the strongest influences on vaccine hesitancy among HCWs in the DRC. Factors such as regional, clinical, and personal experiences, social influences, and knowledge, attitudes, and practice towards COVID-19 prevention, as well as demographics should be considered to determine their impact on vaccine hesitancy [8], [23], [50]. Future studies should also collect qualitative data related to current influences on HCWs’ vaccination decisions to better tailor nuanced health communication campaigns to increase vaccination uptake. Further, understanding the patterns of vaccination influences over time and what impacts these patterns will be important in crafting communication messages that have the intended affect during future health campaigns.
5. Conclusion
Combatting COVID-19 vaccine hesitancy among HCWs in the DRC is more vital than ever as the country is experiencing a rise in COVID-19 cases and as the highly contagious Delta variant becomes more prevalent [15], [51]. Vaccination remains the best strategy to combat and control the spread of disease from SARS-CoV-2 [52]. Encouragingly, support for following general vaccination guidance, apart from COVID-19, did not appear to diminish during the pandemic among this cohort. Previous studies have reported COVID-19 vaccine hesitancy at specific points in time, while this study shows that hesitancy among a cohort of HCWs in the DRC might not be static over time and should be explored as a dynamic variable. Willingness to receive the COVID-19 vaccine likely fluctuates within this important population and these changes are likely influenced by a variety of factors including national and global events, media messaging, and social pressures. Thus, with proper and positive public health messaging there is an opportunity to increase the willingness of HCWs to receive the COVID-19 vaccine when offered.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
We would like to thank our dedicated staff interviewers and participants for their time in completing these surveys throughout the year.
Funding
This work was supported in part by the Shaffer Family Foundation and Faucett Catalyst Fund. The funding source was not involved in study design, analysis, or the writing of this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2022.06.077.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.73rd World Health Assembly. COVID-19 response. 2020. WHA73.1. Geneva, Switzerland.
- 2.Sallam M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines. 2021;2(9):160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wiysonge C.S., Ndwandwe D., Ryan J., Jaca A., Batouré O., Anya B.-P., et al. Vaccine hesitancy in the era of COVID-19: could lessons from the past help in divining the future? Hum Vaccin Immunother. 2022;18(1):1–3. doi: 10.1080/21645515.2021.1893062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacDonald N.E. SAGE working group on vaccine hesitancy. vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;34(33):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 5.Africa Centres for Disease Control and Prevention. COVID 19 vaccine perceptions: A 15 country study. 2021. Addis Ababa, Ethiopia. https://africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/.
- 6.Nzaji M., Ngombe L., Mwamba G., Banza Ndala D., Miema J., Lungoyo C., et al. Acceptability of vaccination against COVID-19 among healthcare workers in the democratic republic of the Congo. Pragmat Obs Res. 2020;11):103–9 doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gostin L.O., Salmon D.A., Larson H.J. Mandating COVID-19 vaccines. JAMA. 2021;6(325):532–533. doi: 10.1001/jama.2020.26553. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization Behavioural considerations for acceptance and uptake of COVID-19 vaccines: WHO technical advisory group on behavioural insights and sciences for health. Meeting report. October 2020;15:2020. [Google Scholar]
- 9.Smith L.E., Amlôt R., Weinman J., Yiend J., Rubin G.J. A systematic review of factors affecting vaccine uptake in young children. Vaccine. 2017;45(35):6059–6069. doi: 10.1016/j.vaccine.2017.09.046. [DOI] [PubMed] [Google Scholar]
- 10.Yeung M.P.S., Lam F.L.Y., Coker R. Factors associated with the uptake of seasonal influenza vaccination in adults: a systematic review. J Public Health. 2016;4(38):746–753. doi: 10.1093/pubmed/fdv194. [DOI] [PubMed] [Google Scholar]
- 11.Paterson P., Meurice F., Stanberry L.R., Glismann S., Rosenthal S.L., Larson H.J. Vaccine hesitancy and healthcare providers. Vaccine. 2016;52(34):6700–6706. doi: 10.1016/j.vaccine.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 12.Zhang J., While A.E., Norman I.J. Nurses' knowledge and risk perception towards seasonal influenza and vaccination and their vaccination behaviours: a cross-sectional survey. Int J Nurs Stud. 2011;10(48):1281–1289. doi: 10.1016/j.ijnurstu.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 13.Makwe C.C., Anorlu R.I. Knowledge of and attitude toward human papillomavirus infection and vaccines among female nurses at a tertiary hospital in Nigeria. Int. J Womens Health. 2011;3:313–317. doi: 10.2147/IJWH.S22792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee C., Saskin R., McArthur M., McGeer A. Beliefs and practices of Ontario midwives about influenza immunization. Vaccine. 2005;13(23):1574–1578. doi: 10.1016/j.vaccine.2004.09.024. [DOI] [PubMed] [Google Scholar]
- 15.UNICEF. Democratic Republic of the Congo: Humanitarian situation report no.6. 2021. https://reliefweb.int/sites/reliefweb.int/files/resources/UNICEF%20Democratic%20Republic%20of%20Congo%20Humanitarian%20Situation%20Report%20No.%206%20-%20January-June%202021.pdf.
- 16.Ferrinho P., Dramé M. Barriers to immunization coverage in DRC: an analysis of the GAVI-Alliance cash-based support. Ann Trop Med Public Health. 2013;4(6):401. [Google Scholar]
- 17.PATH. Immunization in the Democratic Republic of the Congo: Landscape analysis and policy recommendations. 2016. Seattle, WA. https://path.azureedge.net/media/documents/APP_drc_landscape_rpt.pdf.
- 18.Ditekemena J.D., Nkamba D.M., Mutwadi A., Mavoko H.M., Siewe Fodjo J.N., Luhata C., et al. COVID-19 vaccine acceptance in the Democratic Republic of Congo: a cross-sectional survey. Vaccines. 2021;9(2):153. doi: 10.3390/vaccines9020153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nkodila A., Lukanu P., Mbendi C., Tebeu P., Saba J., Kabangi Tukadila H., et al. Perception of the congolese population on Covid-19 vaccination: cross sectional survey of online. Int J Vaccines Vaccination. 2021;1(6):12–19. [Google Scholar]
- 20.Chadwick A, Kaiser J, Vaccari C, Freeman D, Lambe S, Loe BS, et al. Online social endorsement and Covid-19 vaccine hesitancy in the United Kingdom. Soc Media Soc. 2021; 2(7):1-17.
- 21.Sousa-Pinto B., Anto A., Czarlewski W., Anto J.M., Fonseca J.A., Bousquet J. Assessment of the impact of media coverage on COVID-19–related Google trends data: Infodemiology study. J Med Internet Res. 2020;8(22) doi: 10.2196/19611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gozzi N., Tizzani M., Starnini M., Ciulla F., Paolotti D., Panisson A., et al. Collective response to media coverage of the COVID-19 pandemic on Reddit and Wikipedia: mixed-methods analysis. J Med Internet Res. 2020;22(10) doi: 10.2196/21597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Betsch C., Schmid P., Heinemeier D., Korn L., Holtmann C., Böhm R., et al. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE. 2018;13(12) doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewandowsky S., Ecker U.K.H., Seifert C.M., Schwarz N., Cook J. Misinformation and its correction: continued influence and successful debiasing. Psychol Sci Public Interest. 2012;3(13):106–131. doi: 10.1177/1529100612451018. [DOI] [PubMed] [Google Scholar]
- 25.Bruine de Bruin W., Parker A.M., Galesic M., Vardavas R. Reports of social circles' and own vaccination behavior: a national longitudinal survey. Health Psychol. 2019;11(38):975–983. doi: 10.1037/hea0000771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Loomba S., de Figueiredo A., Piatek S.J., de Graaf K., Larson H.J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. 2021;3(5):337–348. doi: 10.1038/s41562-021-01056-1. [DOI] [PubMed] [Google Scholar]
- 27.UNICEF. More than 1.7 million COVID-19 vaccines arrive in the Democratic Republic of Congo. 2021. New York, NY. https://www.unicef.org/press-releases/more-17-million-covid-19-vaccines-arrive-democratic-republic-congo.
- 28.UNICEF. Second shipment of Pfizer vaccines against COVID-19 reach Kinshasa. 2021. Kinshasa, DRC. https://www.unicef.org/drcongo/en/press-release/second-shipment-pfizer-vaccines.
- 29.UNICEF. 400,000 doses of Sinovac vaccine dontated by the Chinese government strengthen the fight against COVID-19 in DRC. 2021. Kinshasa, DRC. https://www.unicef.org/drcongo/en/press-releases/400000-doses-sinovac-vaccine-dontated-chinese-government.
- 30.European Medicines Agency. COVID-19 vaccine AstraZeneca: PRAC investigating cases of thromboembolic events - vaccine’s benefits currently still outweigh risks - Update. 2021. Amsterdam, Netherlands. https://www.ema.europa.eu/en/news/covid-19-vaccine-astrazeneca-prac-investigating-cases-thromboembolic-events-vaccines-benefits.
- 31.Ross A, Holland H. Congo begins COVID-19 vaccinations after delay over safety concerns. Reuters. 2021. Kinshasa, Democratic Republic of Congo. https://www.reuters.com/business/healthcare-pharmaceuticals/congo-begins-covid-19-vaccinations-after-delay-over-safety-concerns-2021-04-19/.
- 32.Roxby P. Covid: DR Congo in race against time to vaccinate people. BBC. 2021. London, England. https://www.bbc.com/news/health-57028747.
- 33.Mathieu E., Ritchie H., Ortiz-Ospina E., Roser M., Hasell J., Appel C., et al. A global database of COVID-19 vaccinations. Nat. Hum Behav. 2021:1–7. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Epi weeks ending log 2020-2021. 2020. https://ndc.services.cdc.gov/wp-content/uploads/2020.pdf.
- 35.World Health Organization. Ebola vaccination begins in North Kivu. 2018. Geneva, Switzerland. https://www.who.int/news/item/08-08-2018-ebola-vaccination-begins-in-north-kivu.
- 36.Ditekemena J.D., Nkamba D.M., Muhindo H.M., Siewe J.N.F., Luhata C., Van den Bergh R., et al. Factors associated with adherence to COVID-19 prevention measures in the Democratic Republic of the Congo (DRC): results of an online survey. BMJ Open. 2021;1(11) doi: 10.1136/bmjopen-2020-043356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hartung C, Lerer A, Anokwa Y, Tseng C, Brunette W, Borriello G. Open data kit: Tools to build information services for developing regions. Proceedings of the 4th ACM/IEEE International Conference on Information and Communication Technologies and Development. London, United Kingdom: Association for Computing Machinery; 2010. p. Article 18.
- 38.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;2(27):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization. WHO SAGE roadmap for prioritizing uses of COVID-19 vaccines in the context of limited supply. 2021. Geneva, Switzerland. https://www.who.int/publications/i/item/who-sage-roadmap-for-prioritizing-uses-of-covid-19-vaccines-in-the-context-of-limited-supply.
- 40.Krzywinski M., Altman N. Error bars: The meaning of error bars is often misinterpreted, as is the statistical significance of their overlap. Nat Methods. 2013;10(10):921–923. doi: 10.1038/nmeth.2659. [DOI] [PubMed] [Google Scholar]
- 41.United Nations DoEaSA, Population Division,. World urbanization prospects: The 2018 revision 2019. ST/ESA/SER.A/420. New York, NY. https://population.un.org/wup/Publications/Files/WUP2018-Report.pdf.
- 42.Institut National de la Statistique. Enquête par grappes à indicateurs multiples, 2017-2018, rapport de résultats de l’enquête. 2019. Kinshasa, DRC. https://mics-surveys-prod.s3.amazonaws.com/MICS6/West%20and%20Central%20Africa/Congo%2C%20Democratic%20Republic%20of%20the/2017-2018/Survey%20findings/Congo%2C%20Democratic%20Republic%20of%20the%2C%202017-18%20MICS%20SFR_French.pdf.
- 43.UNICEF. Maternal and newborn health disparities: Democratic Republic of the Congo. 2018. New York, NY. https://data.unicef.org/resources/maternal-newborn-health-disparities-country-profiles/.
- 44.Centers for Disease Control and Prevention. History of Ebola outbreaks. Ebola (Ebola Virus Disease). 2021. Atlanta, GA. https://www.cdc.gov/vhf/ebola/history/chronology.html.
- 45.UNICEF. Democratic Republic of the Congo: COVID-19 situation report no.18. 2021. https://reliefweb.int/sites/reliefweb.int/files/resources/UNICEF%20DRC_COVID-19_Situation%20Report%2318.pdf.
- 46.World Health Organization. 11th Ebola outbreak in the Democratic Republic of the Congo declared over. 2020. Kinshasa, Democratic Republic of the Congo. https://www.afro.who.int/news/11th-ebola-outbreak-democratic-republic-congo-declared-over.
- 47.GAVI. From biodefence to the DRC: How the Ebola vaccine became one of the fastest vaccines to license in history. 2021. Geneva, Switzerland. https://www.gavi.org/vaccineswork/biodefence-drc-how-ebola-vaccine-became-one-fastest-vaccines-license-history.
- 48.Solís Arce J.S., Warren S.S., Meriggi N.F., Scacco A., McMurry N., Voors M., et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021;8(27):1385–1394. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alley S.J., Stanton R., Browne M., To Q.G., Khalesi S., Williams S.L., et al. As the pandemic progresses, how does willingness to vaccinate against COVID-19 evolve? Int J Environ Res Public Health. 2021;2(18):797. doi: 10.3390/ijerph18020797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Simas C., Larson H.J. Overcoming vaccine hesitancy in low-income and middle-income regions. Nat Rev Dis Primers. 2021;1(7):41. doi: 10.1038/s41572-021-00279-w. [DOI] [PubMed] [Google Scholar]
- 51.World Health Organization. Rife COVID-19 variants fuel Africa’s surging wave. 2021. Brazzaville, Republic of the Congo. https://www.afro.who.int/news/rife-covid-19-variants-fuel-africas-surging-wave.
- 52.Grannis S, Rowley E, Ong T, Stenehjem E, Klein N, DeSilva M, et al. Interim estimates of COVID-19 vaccine effectiveness against COVID-19–associated emergency department or urgent care clinic encounters and hospitalizations among adults during SARS-CoV-2 B.1.617.2 (Delta) variant predominance — Nine states, June–Augut 2021. . MMWR. 2021. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.