Abstract
The gut microbiome has been implicated in the pathogenesis of inflammatory bowel disease (IBD). Studies suggest that the IBD gut microbiome is less diverse than that of the unaffected population, a phenomenon often referred to as dysbiosis. However, these studies have heavily focused on bacteria, while other intestinal microorganisms—fungi, protozoa, and bacteriophages—have been neglected. Of the nonbacterial microbes that have been studied in relation to IBD, most are thought to be pathogens, although there is evidence that some of these species may instead be harmless commensals. In this review, we discuss the nonbacterial gut microbiome of IBD, highlighting the current biases, limitations, and outstanding questions that can be addressed with high-throughput DNA sequencing methods. Further, we highlight the importance of studying nonbacterial microorganisms alongside bacteria for a comprehensive view of the whole IBD biome and to provide a more precise definition of dysbiosis in patients. With the rise in popularity of microbiome-altering therapies for the treatment of IBD, such as fecal microbiota transplantation, it is important that we address these knowledge gaps to ensure safe and effective treatment of patients.
Keywords: inflammatory bowel disease (IBD), microbiome, fungi, protozoa, bacteriophage
Introduction
Inflammatory bowel disease (IBD) is an umbrella diagnosis for a group of chronic inflammatory disorders of the gastrointestinal tract; the 2 most commonly diagnosed forms are ulcerative colitis (UC) and Crohn’s disease (CD).1 IBDs are multifactorial diseases that arise from complex interactions between genetic, environmental, and microbial factors.2-4 Among the microbial factors, the gut microbiome (Box 1) has been implicated in the disease.5,6 Patients with IBD generally have gut microbiomes that are less diverse in species and function compared with unaffected individuals,6,7 a microbial signature often referred to as dysbiosis.8 Research has not arrived at a consensus on the role of dysbiosis in IBD—whether it is a causal factor in IBD development, a perpetuating factor, or simply a result of the disease or lifestyle changes in response to the disease.9,10
Box 1. Definitions of terms.
Microbiota
A collection of microbes, including prokaryotes (bacteria and archaea), eukaryotes (microbial parasites and fungi), and viruses, found in a specified environment.23 The term is often used as a shortened replacement for bacterial microbiota, which may cause confusion if not explicitly stated.
Microbiome
The combined microbiota, their genes and gene products, and their surrounding microenvironment.23,24 Like microbiota, this term is often confusingly used to describe only bacterial populations. However, by default, it denotes the wider population of microbial types (prokaryotes, eukaryotes, and viruses), their genes, and environment.
Amplicon Sequencing
Sometimes referred to as metabarcoding, this high-throughput sequencing method can be used to survey the prokaryotic microbiome community by targeting the bacterial or archaeal 16S ribosomal RNA gene or to survey the eukaryotic community by targeting 18S and ITS (ITS1 and ITS2) ribosomal RNA genes.
Shotgun Sequencing
A high-throughput sequencing method in which the DNA of a sample is fragmented and sequenced at random. When used to explore the microbiome, it is often referred to as metagenomic sequencing.25 Instead of targeting a small proportion of the total genes in a sample like amplicon sequencing, shotgun sequencing captures random fragments of any DNA in the sample, including both host and microbial DNA.
Mycobiome
Like microbiome, this term includes the fungal community in a specified environment, and its genetic and environmental information. It is synonymous with fungal microbiome.
Protozoa
Unicellular eukaryotic microbes often referred to as parasites in the context of human health.
Virus
A nonliving biological entity that infects cells in order to persist and replicate. Viruses are divided into 2 coarse groupings: those that infect bacteria are termed bacteriophages (shortened to phages), and those that infect eukaryotic cells, including host cells and microbial eukaryotes, known simply as viruses.
Virome
A term for all viral DNA in a specified environment.
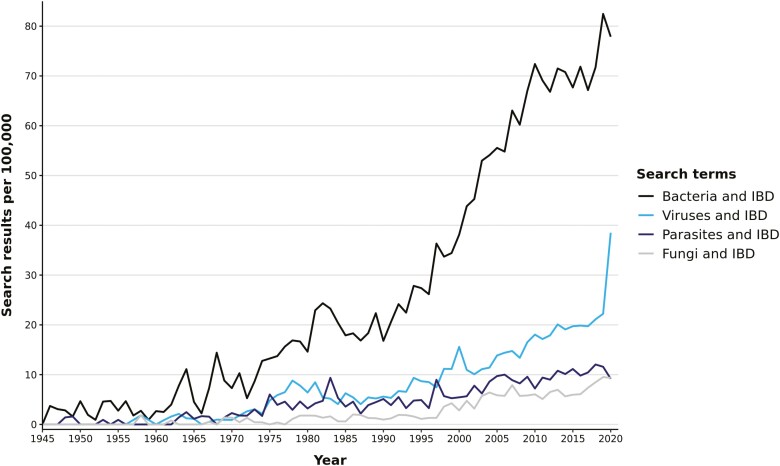
Bacteria are easily identified in gut microbiome studies due to their abundance and have become the focal point of most IBD research (Figure 1), to the exclusion of other intestinal microorganisms such as fungi, protozoa, and bacteriophages.11,12 This myopic investigation of the microbiome has caused the usage of terminology to shift to a point of imprecision and opaqueness; the terms microbiota and microbiome are often used to denote only the bacterial portion of a microbial community.13-15 This usage becomes increasingly ambiguous when researchers describe IBD patients with dysbiosis, yet only the bacterial microbiome has been investigated.9,16,17 Currently, nonbacterial microorganisms are mainly associated with pathogenicity.12 Despite this, many are found in the gastrointestinal tracts of healthy individuals, and there is still conflicting evidence on whether these species have direct and consistent proinflammatory effects.6,12,18-21 There is even evidence to suggest that the absence of some nonbacterial species is associated with disease.22 In this review, we seek to address this knowledge gap by discussing what is known of nonbacterial gut microorganisms, namely fungi, protozoa, and viruses, in IBD. We draw attention to new high-throughput sequencing methods used to study these microbes to develop a more comprehensive understanding of the gut microbiome in IBD.
Figure 1.
Search results of citations featuring microbial types and inflammatory bowel disease (IBD) on PubMed from 1945 to 2020. The total number of search results for bacteria and IBD (15 354) outnumbers results on IBD and viruses (4570), parasites (2314), and fungi (1516). Search conducted on November 1, 2021. Figure generated with PubMed by year (https://esperr.github.io/pubmed-by-year/).
Gut Fungi in IBD
Are gut fungi pathogenic or protective?
Fungi are found on every skin and mucosal surface of the human body,26,27 with the skin, vagina, oral cavity, small intestine, and large intestine harboring the highest abundance and diversity of fungal species. Most of these species are yeasts such as Candida, Malassezia, and Saccharomyces,27,28 and these species have been associated with IBD.12,29 Elevated levels of anti-S. cerevisiae antibodies have been found in IBD patients,30,31 and these antibodies have been associated with an early risk for surgery in CD patients,32 and used to help differentiate33 and predict the development of CD and UC.34 Higher abundances of Candida species, particularly C. albicans, have been found in CD patients and their first-degree relatives, and in a mouse model of colitis.35,36 This has sparked the hypothesis that intestinal inflammation leads to a compromised mucosal barrier that allows C. albicans and potentially other opportunistic bacteria and fungi to proliferate and/or penetrate the mucosal barrier, thus driving interaction with the host immune system.37 Additionally, this fungal-induced inflammation may be exacerbated in IBD patients with inherited genetic mutations in antifungal immune genes (eg, DECTIN-1, Card9).38
However, there is also evidence that Candida and Saccharomyces are not exclusively pathogenic. For example, the presence of Candida species had an alleviating effect in a mouse model of acute colitis39 and S. cerevisiae has been shown to have an attenuating effect on Escherichia coli–induced mouse colitis,40 suggesting that fungi may have a protective effect against IBD. Another species, S. boulardii, also had an attenuating effect in mice with carcinogenic colitis, a condition that can develop from IBD.41,42 The protective effect of S. boulardii has been trialed in CD patients with mixed success rates.43,44 Thus, there is evidence that some fungi may be beneficial in IBD, but inconsistent findings exemplify the complexity of fungi-host interactions. Fungal species may have a spectrum of effects that depend on multiple factors related to an individual’s physiology and microbiome.11 These complexities cannot be gleaned from single-species interrogations, and instead, methods examining the whole microbial community are now being favored.
Insights into gut fungi in IBD from high-throughput sequencing
Initial studies on fungi were limited to species that could be isolated and cultured, wherein researchers characterized a cultured species by sequencing its genome, or generating antibodies to its cellular components.27 This limitation historically biased the reporting of microbes to only culturable species. This may be one of the reasons why Candida and Saccharomyces are most often reported in IBD research, as many species from these genera are readily isolated, cultured, and identified.45,46 Bacterial research previously suffered from similar limitations, and high-throughput DNA sequencing technologies, such as amplicon sequencing and shotgun sequencing, were developed to help overcome these challenges.25 A major advantage of these methods is that they can indiscriminately capture DNA from several fungal taxonomic groups directly from a sample, without the tedious requirement of culturing each fungal species.47 They can also capture DNA from unculturable fungal species in samples dominated by bacterial and human DNA, and thus may give a more representative depiction of the fungal community of a sample.11
With the rise of high-throughput sequencing, the past 10 years have seen a steady increase in studies of the human fungal microbiome, known as the mycobiome.11 The 2 most common sampling types for surveying the mycobiome are fecal samples, either in the form of whole stool or swab, and mucosal biopsies. Fecal samples are used as a proxy for the intestinal microbiome due to the invasiveness of acquiring biopsies,47 although it is expected that the microbiome composition of these 2 sample types will somewhat differ.48 It is now apparent that the gut mycobiome can include species from several dozen genera of fungi (eg, Alternaria, Aspergillus, Candida, Cladosporium, Cryptococcus, Debaryomyces, Fusarium, Galactomyces, Malassezia, Penicillium, Pichia, Rhodotorula, Saccharomyces, Trichosporon), dominated by yeast species from the family Saccharomycetaceae.49-52 Gut mycobiomes differ between individuals and seem to be more temporally variable than gut bacterial microbiomes.49,51 Several mycobiome studies indicate that our intestinal mycobiome, like the bacterial microbiome, differs due to environmental factors such as mode of delivery during birth, age, diet, and geographical location.53-56
High-throughput sequencing approaches have revealed that the gut mycobiome differs in IBD patients, a microbial signature sometimes referred to as fungal dysbiosis (Table 1). Amplicon sequencing studies of colonic biopsies have shown that adult CD patients have a higher number of fungal species compared with UC patients and unaffected control subjects,57 whereas adults with active UC have fewer species and less abundant mycobiomes in both colonic biopsies58 and stool.52 CD patients in flare also have a higher fungal load in both inflamed and uninflamed mucosa than CD patients in remission and healthy individuals.59 Both CD and UC patients also have an altered abundance of different yeast species, namely C. tropicalis in stool of CD patients,60D. hansenii in inflamed mucosa of CD patients,61Aspergillus in colonic biopsies from UC patients,58 and an increase in C. albicans and decrease in both M. sympodialis and S. cerevisiae in stool from a cohort of CD and UC patients in flare.52 The fact that some yeasts are more abundant in IBD patients has been incorporated into the hypothesis that IBD may be caused or perpetuated by an overgrowth of opportunistic intestinal fungi.12,29,37 These fungi may achieve this through interkingdom interactions, such as the biofilm formed between C. tropicalis and the bacterial species E. coli and S. marcescens, which induces the expression of pathogenic fungal hyphae.60 Other fungal species may be able to exert their pathogenicity without the help of bacteria. For example, D. hansenii was shown to preferentially localize to inflamed mucosa in colonic tissue isolated from biopsy-injured mice and ileal tissue isolated from CD patients.61D. hansenii prevented repair of colonic mucosa in the absence of bacteria, which was established using gnotobiotic mice.
Table 1.
Current insights from high-throughput sequencing of the nonbacterial microbiome in IBD
| Study | Study Population(s) | Microbiome Sample(s) and Methods | Key Findings |
|---|---|---|---|
| Fungi | |||
| 57 | Active CD (n = 31), active UC (n = 26), non-IBD intestinal inflammation (n = 15), healthy individuals (n = 32) | 18S rRNA–based amplification, denaturing gradient gel electrophoresis, and clone library analysis of stool and biopsies from inflamed colon | ↑ fungal species in active CD biopsies compared with active UC and control subjects |
| 62 | Pediatric IBD (26 CD, 4 UC, and 2 indeterminate colitis), healthy adult and pediatric control subjects (n = 90) | ITS1 sequencing of stool | ↓ fungal diversity (Shannon index) in IBD |
| ↑ abundance of Cyberlindnera jadinii and C. parapsilosis and ↓ abundance of Cladosporium cladosporioides in IBD | |||
| 63 | Pediatric active CD (n = 90), healthy pediatric control subjects (n = 26) | Shotgun whole metagenome sequencing of stool | ↑ abundance of C. jadinii, S. cerevisiae, Clavispora lusitaniae, C. albicans, and Kluyveromyces marxianus in active CD, which decreased following 8 weeks of exclusive enteral nutrition |
| 60 | Active and inactive CD (n = 20), CD relatives (n = 28), unrelated healthy individuals (n = 21) | ITS1, ITS2, and 16S rRNA sequencing of stool | ↑ abundance of C. tropicalis in CD patients, positively correlated with Serratia marcescens and Escherichia coli |
| 59 | Active CD (n = 16), inactive CD (n = 7), healthy individuals (n = 10) | ITS2 rRNA sequencing of ileo-colonic biopsies with quantitative PCR | ↑ fungal load of both inflamed and inflamed mucosa in active CD compared with inactive CD and healthy control subjects |
| 58 | Active UC (n = 14), healthy individuals (n = 15) | 18S and ITS2 rRNA sequencing of biopsies from inflamed colon; quantitative PCR of 18S rRNA for fungal load | ↓ fungal species count and abundance in active UC |
| ↑ abundance of Aspergillus in active UC | |||
| 52 | Active CD and UC patients (n = 106), inactive CD and UC patients (n = 129), healthy individuals (n = 38) | ITS2 rRNA sequencing of stool | ↑ abundance of C. albicans and ↓ abundance of S. cerevisiae and Malassezia sympodialis in active IBD compared with remission |
| ↓ fungal species count in UC | |||
| 64 | PSC patients with IBD in remission (n = 27), PSC patients without IBD (n = 22), IBD patients in remission without PSC (n = 33), and healthy individuals (n = 30) | ITS2 and 16S sequencing of stool | No difference in fungal diversity (Shannon and Chao1 indices) between IBD remission and healthy individuals |
| ↑ fungal diversity (Shannon) index in PSC compared with IBD remission | |||
| 61 | Mice injured by colonic biopsies and treated with antibiotics to impair healing, control mice injured but not treated with antibiotics | Quantitative PCR of ITS of murine mucosal wounds and patient ileal biopsies | ↑ Debaryomyces hansenii abundance in mucosal wounds of antibiotic-treated mice compared with control subjects |
| Patients with active CD (n = 7) and healthy individuals (n = 10) | ↑ D. hansenii abundance in inflamed mucosa of CD patients compared with uninflamed mucosa in same patients | ||
| 65 | Patients with 3-month remission of UC (n = 31), and ileal or ileocolonic CD (n = 34), patients with active CD (n = 55), UC relatives (n = 29), CD relatives (n = 29), healthy unrelated individuals (n = 28) | Quantitative PCR of ITS2 and 16S rRNA of stool, random forest predictive modelling | ↑ fungal load in relapsed CD compared with patients who remained in remission |
| ↑ fungal load in relapsed UC compared with UC remission, CD remission, and CD relapsed | |||
| Fungal and bacterial load combined with clinical markers (C-reactive protein and fecal calprotectin) and demographic data distinguished UC from CD and could predict relapse | |||
| Protozoa | |||
| 66 | Active and inactive CD and UC patients (n = 100), healthy individuals (n = 96) | Culture and PCR of stool | ↓ Blastocystis and Dientamoeba fragilis prevalence in active CD and UC than inactive |
| ↓ Blastocystis prevalence in both active and inactive IBD than control subjects | |||
| 67 | Patients with active CD (n = 76) and UC (n = 31), healthy individuals (n = 616) | 18S rRNA sequencing of stool | ↓ Blastocystis prevalence in IBD |
| Viruses | |||
| 68 | Patients with active (n = 10) and inactive (n = 1) ileocolonic CD, healthy individuals (n = 8) | 454 pyrosequencing of stool | ↓ virome diversity (Shannon index) in CD |
| 69 | Pediatric patients with CD (n = 6), and healthy individuals (n = 6) | 454 pyrosequencing of ileal and colonic biopsies, and gut washes | ↑ abundances of viral species in CD, Caudovirales most abundant |
| 63 | Pediatric active CD (n = 90), healthy pediatric control subjects (n = 26) | Shotgun whole metagenome sequencing of stool | No difference in bacteriophage species between groups |
| 70 | Patients with CD (n = 18), UC (n = 42), healthy individuals (n = 12) | 454 pyrosequencing of stool | ↑ abundances of Caudovirales bacteriophage species in CD and UC |
| 71 | Patients with new-onset active CD (n = 12), healthy individuals (n = 12) | 454 pyrosequencing of colonic biopsies | ↑ viral species in active CD |
| 72 | C57BL6/J Rag1-/- mice with colitis induced by injection of CD4+ CD45RBHigh T cells (n = 3) and control mice injected with saline (n = 3) | Shotgun whole metagenome sequencing of stool | ↑ abundances of Caudovirales bacteriophages species in murine colitis |
Abbreviations: CD, Crohn’s disease; IBD, inflammatory bowel disease; PCR, polymerase chain reaction; PSC, primary sclerosing cholangitis; rRNA, ribosomal RNA; UC, ulcerative colitis.
Because the mycobiome shows a marked alteration in IBD, it has the potential to be used as a diagnostic tool. For example, the fecal mycobiome was used to discriminate between CD and UC by combining fungal load with bacterial load, clinical biomarkers (fecal calprotectin and C-reactive protein), and demographic data (age, gender, BMI, and smoking habit) in a random forest predictive model.65 The fecal mycobiome also differs in patients experiencing a flare52,65 compared with patients in remission who may have gut mycobiomes that more closely resemble a healthy mycobiome,64,65 and was better able to predict relapse in CD and UC patients when fungal load was incorporated into the predictive model described previously. Therefore, the fecal mycobiome may be a minimally invasive diagnostic tool for predicting IBD subtype and relapse.
Mycobiome shifts also exist in pediatric IBD patients (Table 1). Pediatric patients showed a reduction in overall gut fungal diversity and an increase in Cyberlindnera jadinii and C. parapsilosis in stool samples compared with healthy adult and pediatric control subjects.62 In one of the few shotgun sequencing studies of the IBD mycobiome, pediatric patients with active CD undergoing a formula diet (exclusive enteral nutrition) or anti-tumor necrosis factor therapy also had elevated C. jadinii, as well as elevated S. cerevisiae, Clavispora lusitaniae, C. albicans, and Kluyveromyces marxianus at baseline compared with healthy pediatric control subjects.63 This elevation in yeast species subsequently decreased following 8 weeks of nutrition therapy, suggesting that diet is an effective modifier of the mycobiome in patients.
It is clear that differences exist between the IBD mycobiome and unaffected individuals. However, a lack of research and studies incorporating different populations, sample types, and methods existing studies means that it is still too early to ascertain clear trends (Table 1). Research thus far suggests that the IBD mycobiome varies between CD and UC,52,57,65 between patients in remission and in flare,52,64,65 and between sites of inflamed mucosa and adjacent uninflamed tissue.61 Therefore, it is important that we continue to have different disease subtypes and disease states represented in future IBD mycobiome datasets. Longitudinal sampling will also help uncover whether compositional changes are a cause or effect of flare.73
Limitations and future directions of gut mycobiome research
Preliminary work shows that the IBD mycobiome differs from unaffected individuals, though inconsistencies in findings and, more importantly, an overall lack of research means that much work is still needed in this area. Fungi remain underexplored in sequence-based approaches, likely due to the low abundance of fungal DNA relative to bacterial DNA in gut microbiome samples.51,65 It has been hypothesized that the ratio of fungal to bacterial cells changes throughout the gastrointestinal tract and that parts of the upper gastrointestinal tract (stomach and duodenum) have a higher ratio of fungi to bacteria than lower parts (jejunum, ileum, and colon).11,74 The proportional influence of fungi may thus differ considerably throughout the gastrointestinal tract, and further research is needed to understand such differences in interactions. The anatomical variation in fungal interactions might indeed be one reason that we see an anatomical restriction in where CD and UC occur in individuals, and in the diseases themselves.
Owing to the low abundance of fungi in intestinal microbiome samples, deep sequencing is required to capture the fungal genomic component of these samples, which can be costly and time-consuming.11 There are, however, methods to mitigate this difficulty. Samples can be enriched for fungal DNA prior to sequencing via several options of protocols and kits, to reduce the sequencing effort required to capture fungal DNA.47,75 Additionally, computational tools have been developed that specifically recognize fungal DNA sequences. There are now several bioinformatic pipelines available to recover and taxonomically assign fungal DNA from amplicon data (eg, RiboTagger)76 and shotgun data (eg, FindFungi, EukRep, HumanMycobiomeScan, EukDetect).77-80
High-throughput sequencing methods for studying the mycobiome can circumvent some of the limitations of previous technologies, but they also suffer from their own limitations. Though amplicon sequencing is a useful method for determining fungal abundances and coarse phylogenetic groupings, the approach does not always yield good resolution to the species level, or even to the genus level, and is generally less sensitive than 16S sequencing for bacteria.27,81 Shotgun sequencing is more sensitive than amplicon sequencing; however, it is more expensive and computationally intensive. Because shotgun sequencing indiscriminately captures all the DNA in a sample, human DNA contamination is common and must be dealt with in the laboratory and computationally.82 Another disadvantage of amplicon sequencing is that it does not allow for direct functional inference, as only ribosomal genes are sequenced with this method, and function is inferred with predictive tools.83 Shotgun sequencing can recover partial or whole microbial genomes, so it enables direct functional inference. This method is additionally advantageous because one can profile both the bacterial and fungal portions of the microbiome in a single effort.
There are also limitations that affect both amplicon and shotgun sequencing. Gene and genome references available for fungi in databases are still biased toward already cultured organisms.27 This is important to consider for both amplicon and shotgun studies wherein yeasts are still frequently reported over other fungi. Because fewer fungal species from the gastrointestinal tract have been cultured than bacteria, even less is known of their metabolic functions, and so predictive tools can be unreliable. Reference databases used to assign taxonomy to fungi also contain thousands of unannotated and incorrectly annotated sequences.81 Fortunately, tools that facilitate de novo assembly of fungal genomes are available to characterize the fraction of the mycobiome that is both unculturable and lacking reference genomes, such as a recent pipeline used to identify novel fungal genomes from premature infants,84 and EukCC, a tool to estimate the quality of eukaryotic genome assembly.85 With these tools, reference databases for fungi are expanding faster than ever before. Researchers can now retrospectively mine metagenomic data for fungal DNA, and this can similarly be done for IBD cohorts. New metagenomic approaches such as these are critically important to answer remaining questions regarding the role of the mycobiome in IBD: Is there a characteristic mycobiome signature of IBD or its subtypes? Is there a tipping point at which yeasts such as Candida become more abundant and, potentially, proinflammatory? Which fungal and bacterial species or strains are involved in this process? Is an increase in these species a cause or a result of IBD?
Gut Protozoa in IBD
Gut protozoa: Falsely villainized?
Intestinal parasites are typically known for causing dysenteric infections.86 These parasites have gradually been depleted with industrial-associated lifestyle factors such as improved sanitation, hygiene, and health care.87,88 However, an industrialized lifestyle has also been associated with the rise in incidences of IBD,89,90 and some hypothesize that exposure to certain intestinal parasites may be beneficial for maintaining a healthy and diverse microbiome.90-92 Macroparasites, namely helminths, and their purified antigens have been used to treat IBD in mice93-95 and in controversial human trials with some success.96-99 Protozoa have received far less attention in relation to IBD, although there are several protozoan species that are able to commensally colonize and reside in the human intestine.18
Blastocystis species and Dientamoeba fragilis are the most common protozoa found in human stool and are primarily transmitted through the fecal-oral route.100,101 The prevalence of Blastocystis species in human stool ranges from 1% to 50% in developed nations and is generally >30% in developing nations.67,101,102 Similarly, the prevalence of D. fragilis varies greatly between regions of the world, with a higher prevalence in developing regions.103,104Blastocystis and D. fragilis are often blamed for causing gastroenteritis-like symptoms, although they have been found in both symptomatic and asymptomatic individuals and their pathogenicity is thus still debated.18 More recently, largescale controlled cohorts have not found an association between Blastocystis, D. fragilis, and gastroenteritis.105-107 Rather, these protozoa were found to be more abundant in healthy individuals108 and were are also associated with increased gut bacterial diversity.51 These findings suggest that Blastocystis and D. fragilis may not be parasitic, but rather enteric commensals. In fact, the name “parasite” may be a misnomer for these species. This hypothesis is also supported in IBD patients, wherein both Blastocystis and D. fragilis have been found more frequently in unaffected individuals and UC patients with inactive disease than in UC and CD patients with active disease.22,66,67 Whether the lower prevalence of Blastocystis in patients was a cause or effect of the disease was not addressed in these studies, but we should consider if these protozoa are a hallmark of a healthy gut, and whether administering antibiotics when they are found may be causing harm.
Limitations and future directions of gut protozoa research
The study of intestinal protozoa has experienced similar biases to fungal research—some species have been heavily studied whereas others are scarcely discussed (Table 1). There is an evident ascertainment bias toward the reporting of culturable parasites, and very little is known about unculturable protozoan members of the human gut microbiome.109 For example, Blastocystis species, though anerobic, can be readily cultured and they are commonly detected with microscopy following in vitro culture from stool.101,110 However, microscopic detection of Blastocystis subtypes in stool is less sensitive than sequencing methods, particularly when they are present in low abundances.111 Capturing protozoan DNA can be achieved with 18S amplicon sequencing, and there are parasite-specific 18S primers that can capture DNA from several taxonomic groups.112 Though as stated previously, this method is rarely sensitive enough for robust species-level resolution.109 Shotgun sequencing can bypass some of the limitations of amplicon sequencing, but it is similarly limited by the low proportion of protozoa in the intestinal microbiome.51 Thus, deep sequencing, even deeper than required to detect fungi, is necessary to capture enough protozoan DNA for species identifications. It is therefore critical that samples are enriched for eukaryotic cells prior to sequencing. Fortunately, decreases in the cost of sequencing, enrichment for eukaryotic DNA, and improvements to computational methods and reference databases may soon help to provide insights into protozoa in IBD.
Gut Bacteriophages in IBD
Bacteriophages: contributors to the IBD gut microbiome
An assortment of viral particles exists in the gastrointestinal environment of many animals, including humans.21,113 Viruses of the gut microbiome include 2 major types: those that infect eukaryotic cells (eg, human cells) and phages that infect bacteria. While both types have been detected in the human gut,114 phages comprise most of the viral species present in the gut. Phages can transfer genetic content, such as antibiotic resistance genes, between bacterial cells,114,115 and cause rapid destruction of bacterial cells upon infection during the lytic cycle. Therefore, these viruses can regulate population levels of resident bacteria114 and should be recognized as able contributors to microbiome composition shifts, such as those seen in IBD.116
The gut virome in IBD studies
The gut virome is an emerging area of study in IBD research, and to date, the field contains only a handful of studies (Table 1). One small study of stool samples from CD patients (n = 11) and unaffected control subjects (n = 8) found that virome and bacterial diversity in stool samples was lower in the patients.68 Conversely, in another study, colonic biopsies of 12 CD patients had more viral species compared with the 12 control subjects.71 This same study also found that the sample type and patient from which the sample originated had a greater impact on virome composition than the disease state, suggesting high inter-individual variation in virome composition. Bacterial composition was contrastingly less variable within groups and was instead more affected by the disease state. Other studies suggest that Caudovirales phages, a grouping of over 350 double-stranded DNA viral species,117 may be more abundant in murine colitis, in pediatric CD, and in adults patients with CD and UC.69,70,72 However, not all studies have recapitulated this finding.63 Given that virome research is newly emerging, discrepant findings between these studies may be largely influenced by methodological biases (discussed subsequently), in addition to confounding influences between cohorts.
Current limitations and future directions of virome research
Identifying and classifying viral DNA in microbial samples remains challenging.118 As they have incredibly high diversity, tiny gene content, and acquire new mutations rapidly, viral species are not easily assigned to closely related species. There is also no gene common to all viruses that can be used as a viral identity marker, and thus, sequencing viral DNA cannot be achieved with a targeted amplicon-like sequencing method.113 Additionally, viral DNA makes up a small proportion of the total DNA in a microbiome sample.119 Culturing viruses is equally challenging. Viruses cannot make their own energy because they are parasitic and rely on host cells for resources, so these hosts must be identified and cultured as well. As many microbes of the gastrointestinal tract cannot be cultured, it is difficult to culture their associated viruses.68
Embarking on a metagenomic study of the virome may seem like a daunting task, but there are some methodological strategies that can assist in managing the challenge. Prior to sequencing, viral particles can be isolated and purified from a microbiome sample by size selection via centrifugation, filtering (0.2- to 0.45-µm filters), and particle precipitation with polyethylene glycol.120 Newer computational tools can also reduce the difficulty of studying the human virome, such as METAVIR, an online resource for annotating virus genes from metagenomic data,121 and VIP and VirFinder, which provide pipelines to map, filter, and identify viruses from metagenomic sequences.122,123 There are also several databases to identify viral genes (eg, National Center for Biotechnology Information viral genomes resource, IMG/VR, and ACLAME).124-126 Future gut virome studies can incorporate tools like these, following viral protein enrichment127 or host DNA depletion, and high-throughput sequencing of patient microbiome samples.118
Fecal Microbiota Transplantation and the Neglected Microbiome
Given the observed link between the gut microbiome and IBD, researchers and clinicians have turned to microbiome-based therapies such as fecal microbiota transplantation (FMT) to treat the disease.128-130 FMT initially received attention for its high efficacy in treating Clostridioides difficile infections,131 and is a procedure that involves the transfer of stool or its microbial derivatives from a healthy donor to a patient, by means of enema, oral capsule, or nasogastric tube.132 This therapy is presumed to work by restoring a patient’s microbiome to a healthy state.133 FMT is an attractive alternative to other standard therapies, such as immunosuppressants, biologics, or surgery, as successful engraftment of FMT offers the prospect of long-term symptom amelioration without the side effects of other treatment options. So far, FMT for IBD has seen moderate successes and low adverse events in UC patients.134-136 The average rate of clinical remission achieved sits below 50% which is on par with many other IBD therapies, though this number varies depending on factors such as FMT type, mode of administration, donor type (related vs unrelated), IBD subtype, and geographic location.134,135
FMT success rates may also differ because the microbial composition of donor stools used in FMT is still poorly described.9 Further, we have only successfully characterized a fraction of the total gut microbiome, leaving many species yet to be described.137 It is therefore critical to include all microbial types in microbiome analyses of FMT studies to provide a more precise depiction of the biological material each patient receives. This might allow for better discrimination between effective and ineffective donor and recipient microbiome samples. Currently, prospective donor samples are screened for agents previously regarded as putative pathogens, such as Blastocystis and D. fragilis,138 and donors who are positive for these protozoa may be ruled out.139 As we have previously discussed, the growing body of literature would suggest that these protozoa are innocuous colonizers of the human gut and may in fact indicate a healthy microbiome. For example, one study did not find different outcomes between C. difficile patients receiving FMT that was positive and negative for Blastocystis.140 Donor-derived viruses may also be an important factor for FMT efficacy. One study found that C. difficile patients who received donor stool with a higher content of Caudovirales phages were more likely to respond positively to their transplants.141 Thus, further work on gut fungi, protozoa, and bacteriophages is required to reduce the likelihood of discounting commensal species in microbiome-based therapies.
Conclusions and Future Directions
Exploring the ill-defined, nonbacterial microbiome through high-throughput methods is the next logical step toward understanding the link between the gut microbiome and IBD. To this end, it is important that sequencing and computational methods for analyzing eukaryotes and viruses are accessible to clinicians, and that we continue to foster multidisciplinary collaborations to translate bioinformatic results to clinical diagnostics.47 Future research should incorporate data from nonbacterial organisms with extensive patient information, such as disease state and lifestyle factors, to disentangle the interplay between microbial and host factors.11,116,142 Last, IBD microbiome research, as in many other fields, will benefit from statistical modelling to disentangle relationships between eukaryotes, prokaryotes, viruses, and host genomic data.143 As interest in the gut microbiome and microbiome-based therapies continues to rise, studying these relationships will ensure greater precision of diagnostics and treatments for IBD patients.
Acknowledgments
We thank Bastien Llamas and the Thesis Writing Group at the Australian Centre for Ancient DNA for providing edits and feedback on the manuscript. The references for this Review were identified using PubMed and Web of Science with Boolean search terms for bacteria (“bacter∗”), viruses (“virus∗ OR viral OR virome∗ OR bacteriophage∗ OR phage∗”), parasites (“parasit∗ OR protoz∗ OR helminth∗ OR protist∗”), and fungi (“fung∗ OR mycobio∗ OR yeast∗”) combined with the search terms for IBD (“IBD OR Crohn’s OR ulcerative colitis OR inflammatory bowel”). The results were narrowed to articles and reviews published in English. The final reference list was chosen for its novelty and relevance to the scope of this Review topic.
Contributor Information
Gina L Guzzo, School of Biological Sciences, University of Adelaide, Adelaide, South Australia, Australia.
Jane M Andrews, Inflammatory Bowel Disease Service, Department of Gastroenterology and Hepatology, Royal Adelaide Hospital and School of Medicine, Faculty of Health Sciences, University of Adelaide, Adelaide, South Australia, Australia.
Laura S Weyrich, School of Biological Sciences, University of Adelaide, Adelaide, South Australia, Australia; Department of Anthropology and Huck Institutes of the Life Sciences, Pennsylvania State University, State College, PA, USA.
Author Contributions
G.L.G. wrote and conducted the research for the manuscript. L.S.W. and J.M.A. provided substantial discussion and editing of the manuscript.
Support By
None to disclose.
Conflicts of Interest
The authors declare no competing interests.
REFERENCES
- 1. Podolsky DK. Inflammatory bowel disease (1). N Engl J Med. 1991;325:928-937. [DOI] [PubMed] [Google Scholar]
- 2. Ho SM, Lewis JD, Mayer EA, et al. Challenges in IBD research: environmental triggers. Inflamm Bowel Dis. 2019;25:S13-S23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Khor B, Gardet A, Xavier RJ.. Genetics and pathogenesis of inflammatory bowel disease. Nature. 2011;474:307-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Loddo I, Romano C.. Inflammatory bowel disease: genetics, epigenetics, and pathogenesis. Front Immunol. 2015;6:551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schirmer M, Garner A, Vlamakis H, Xavier RJ.. Microbial genes and pathways in inflammatory bowel disease. Nat Rev Microbiol. 2019;17:497-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zuo T, Ng SC.. The gut microbiota in the pathogenesis and therapeutics of inflammatory bowel disease. Front Microbiol. 2018;9:2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Clemente JC, Ursell LK, Parfrey LW, Knight R.. The impact of the gut microbiota on human health: an integrative view. Cell. 2012;148:1258-1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hooks KB, O’Malley MA.. Dysbiosis and its discontents. MBio 2017;8:e01492-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khan I, Ullah N, Zha L, et al. Alteration of gut microbiota in inflammatory bowel disease (IBD): cause or consequence? IBD treatment targeting the gut microbiome. Pathogens 2019;8:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ni J, Wu GD, Albenberg L, Tomov VT.. Gut microbiota and IBD: causation or correlation? Nat Rev Gastroenterol Hepatol. 2017;14:573-584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Richard ML, Sokol H.. The gut mycobiota: insights into analysis, environmental interactions and role in gastrointestinal diseases. Nat Rev Gastroenterol Hepatol. 2019;16:331-345. [DOI] [PubMed] [Google Scholar]
- 12. Sartor RB, Wu GD.. Roles for intestinal bacteria, viruses, and fungi in pathogenesis of inflammatory bowel diseases and therapeutic approaches. Gastroenterology 2017;152:327-339.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Clooney AG, Eckenberger J, Laserna-Mendieta E, et al. Ranking microbiome variance in inflammatory bowel disease: a large longitudinal intercontinental study. Gut. 2021;70:499-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ryan FJ, Ahern AM, Fitzgerald RS, et al. Colonic microbiota is associated with inflammation and host epigenomic alterations in inflammatory bowel disease. Nat Commun. 2020;11:1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vich Vila A, Imhann F, Collij V, et al. Gut microbiota composition and functional changes in inflammatory bowel disease and irritable bowel syndrome. Sci Transl Med. 2018;10:eaap8914. [DOI] [PubMed] [Google Scholar]
- 16. DeGruttola AK, Low D, Mizoguchi A, Mizoguchi E.. Current understanding of dysbiosis in disease in human and animal models. Inflamm Bowel Dis. 2016;22:1137-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fritsch J, Garces L, Quintero MA, et al. Low-fat, high-fiber diet reduces markers of inflammation and dysbiosis and improves quality of life in patients with ulcerative colitis. Clin Gastroenterol Hepatol. 2021;19:1189-1199.e30. [DOI] [PubMed] [Google Scholar]
- 18. Chabé M, Lokmer A, Ségurel L.. Gut protozoa: friends or foes of the human gut microbiota? Trends Parasitol. 2017;33:925-934. [DOI] [PubMed] [Google Scholar]
- 19. Fritsch J, Abreu MT.. Candida in IBD: friend or foe? Cell Host Microbe. 2020;27:689-691. [DOI] [PubMed] [Google Scholar]
- 20. Lukeš J, Stensvold CR, Jirků-Pomajbíková K, Wegener Parfrey L.. Are human intestinal eukaryotes beneficial or commensals? PLoS Pathog. 2015;11:e1005039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Virgin HW. The virome in mammalian physiology and disease. Cell. 2014;157:142-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rossen NG, Bart A, Verhaar N, et al. Low prevalence of Blastocystis sp. in active ulcerative colitis patients. European Soc Clin Microbiol. 2015;34:1039-1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Marchesi JR, Ravel J.. The vocabulary of microbiome research: a proposal. Microbiome. 2015;3:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Turnbaugh PJ, Ley RE, Hamady M, et al. The human microbiome project. Nature. 2007;449:804-810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Riesenfeld CS, Schloss PD, Handelsman J.. Metagenomics: genomic analysis of microbial communities. Annu Rev Genet. 2004;38:525-552. [DOI] [PubMed] [Google Scholar]
- 26. Parfrey LW, Walters WA, Lauber CL, et al. Communities of microbial eukaryotes in the mammalian gut within the context of environmental eukaryotic diversity. Front Microbiol. 2014;5:298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Underhill DM, Iliev ID.. The mycobiota: interactions between commensal fungi and the host immune system. Nat Rev Immunol. 2014;14:405-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Findley K, Oh J, Yang J, et al.; NIH Intramural Sequencing Center Comparative Sequencing Program. Topographic diversity of fungal and bacterial communities in human skin. Nature. 2013;498:367-370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Miyoshi J, Sofia MA, Pierre JF.. The evidence for fungus in Crohn’s disease pathogenesis. Clin J Gastroenterol. 2018;11:449-456. [DOI] [PubMed] [Google Scholar]
- 30. Main J, McKenzie H, Yeaman GR, et al. Antibody to Saccharomyces cerevisiae (bakers’ yeast) in Crohn’s disease. BMJ. 1988;297:1105-1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Quinton JF, Sendid B, Reumaux D, et al. Anti-Saccharomyces cerevisiae mannan antibodies combined with antineutrophil cytoplasmic autoantibodies in inflammatory bowel disease: prevalence and diagnostic role. Gut. 1998;42:788-791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Forcione DG, Rosen MJ, Kisiel JB, Sands BE.. Anti-Saccharomyces cerevisiae antibody (ASCA) positivity is associated with increased risk for early surgery in Crohn’s disease. Gut. 2004;53:1117-1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Reese GE, Constantinides VA, Simillis C, et al. Diagnostic precision of anti-Saccharomyces cerevisiae antibodies and perinuclear antineutrophil cytoplasmic antibodies in inflammatory bowel disease. Am J Gastroenterol. 2006;101:2410-2422. [DOI] [PubMed] [Google Scholar]
- 34. van Schaik FD, Oldenburg B, Hart AR, et al. Serological markers predict inflammatory bowel disease years before the diagnosis. Gut. 2013;62:683-688. [DOI] [PubMed] [Google Scholar]
- 35. Standaert-Vitse A, Sendid B, Joossens M, et al. Candida albicans colonization and ASCA in familial Crohn’s disease. Am J Gastroenterol. 2009;104:1745-1753. [DOI] [PubMed] [Google Scholar]
- 36. Zwolinska-Wcislo M, Brzozowski T, Budak A, et al. Effect of Candida colonization on human ulcerative colitis and the healing of inflammatory changes of the colon in the experimental model of colitis ulcerosa. J Physiol Pharmacol. 2009;60:107-118. [PubMed] [Google Scholar]
- 37. Yan L, Yang C, Tang J.. Disruption of the intestinal mucosal barrier in Candida albicans infections. Microbiol Res. 2013;168:389-395. [DOI] [PubMed] [Google Scholar]
- 38. Richard ML, Lamas B, Liguori G, et al. Gut fungal microbiota: the Yin and Yang of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21:656-665. [DOI] [PubMed] [Google Scholar]
- 39. Qiu X, Zhang F, Yang X, et al. Changes in the composition of intestinal fungi and their role in mice with dextran sulfate sodium-induced colitis. Sci Rep. 2015;5:10416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sivignon A, de Vallée A, Barnich N, et al. Saccharomyces cerevisiae CNCM I-3856 prevents colitis induced by AIEC bacteria in the transgenic mouse model mimicking Crohn’s disease. Inflamm Bowel Dis. 2015;21:276-286. [DOI] [PubMed] [Google Scholar]
- 41. Herszenyi L, Miheller P, Tulassay Z.. Carcinogenesis in inflammatory bowel disease. Digest Dis. 2007;25:267-269. [DOI] [PubMed] [Google Scholar]
- 42. Wang C, Li W, Wang H, et al. Saccharomyces boulardii alleviates ulcerative colitis carcinogenesis in mice by reducing TNF-α and IL-6 levels and functions and by rebalancing intestinal microbiota. BMC Microbiol. 2019;19:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Bourreille A, Cadiot G, Le Dreau G, et al.; FLORABEST Study Group. Saccharomyces boulardii does not prevent relapse of Crohn’s disease. Clin Gastroenterol Hepatol. 2013;11:982-987. [DOI] [PubMed] [Google Scholar]
- 44. Garcia Vilela E, De Lourdes De Abreu Ferrari M, Oswaldo Da Gama Torres H, et al. Influence of Saccharomyces boulardii on the intestinal permeability of patients with Crohn’s disease in remission. Scand J Gastroenterol. 2008;43:842-848. [DOI] [PubMed] [Google Scholar]
- 45. Duina AA, Miller ME, Keeney JB.. Budding yeast for budding geneticists: a primer on the Saccharomyces cerevisiae model system. Genetics. 2014;197:33-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Graf B, Adam T, Zill E, Göbel UB.. Evaluation of the VITEK 2 system for rapid identification of yeasts and yeast-like organisms. J Clin Microbiol. 2000;38:1782-1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Allaband C, McDonald D, Vázquez-Baeza Y, et al. Microbiome 101: studying, analyzing, and interpreting gut microbiome data for clinicians. Clin Gastroenterol Hepatol. 2019;17:218-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Tang Q, Jin G, Wang G, et al. Current sampling methods for gut microbiota: a call for more precise devices. Front Cell Infect Microbiol. 2020;10:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hallen-Adams HE, Suhr MJ.. Fungi in the healthy human gastrointestinal tract. Virulence. 2017;8:352-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Limon JJ, Skalski JH, Underhill DM.. Commensal fungi in health and disease. Cell Host Microbe. 2017;22:156-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Nash AK, Auchtung TA, Wong MC, et al. The gut mycobiome of the Human Microbiome Project healthy cohort. Microbiome. 2017;5:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Sokol H, Leducq V, Aschard H, et al. Fungal microbiota dysbiosis in IBD. Gut. 2017;66:1039-1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bliss JM, Basavegowda KP, Watson WJ, et al. Vertical and horizontal transmission of Candida albicans in very low birth weight infants using DNA fingerprinting techniques. Pediatr Infect Dis J. 2008;27:231-235. [DOI] [PubMed] [Google Scholar]
- 54. David LA, Maurice CF, Carmody RN, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559-563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kabwe MH, Vikram S, Mulaudzi K, et al. The gut mycobiota of rural and urban individuals is shaped by geography. BMC Microbiol. 2020;20:257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Strati F, Di Paola M, Stefanini I, et al. Age and gender affect the composition of fungal population of the human gastrointestinal tract. Front Microbiol. 2016;7:1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ott SJ, Kühbacher T, Musfeldt M, et al. Fungi and inflammatory bowel diseases: Alterations of composition and diversity. Scand J Gastroenterol. 2008;43:831-841. [DOI] [PubMed] [Google Scholar]
- 58. Qiu X, Ma J, Jiao C, et al. Alterations in the mucosa-associated fungal microbiota in patients with ulcerative colitis. Oncotarget. 2017;8:107577-107588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Liguori G, Lamas B, Richard ML, et al. Fungal dysbiosis in mucosa-associated microbiota of Crohn’s disease patients. J Crohns Colitis. 2016;10:296-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Hoarau G, Mukherjee PK, Gower-Rousseau C, et al. Bacteriome and mycobiome interactions underscore microbial dysbiosis in familial Crohn’s disease. MBio 2016;7:e01250-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Jain U, Ver Heul AM, Xiong S, et al. Debaryomyces is enriched in Crohn’s disease intestinal tissue and impairs healing in mice. Science. 2021;371:1154-1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Chehoud C, Albenberg LG, Judge C, et al. Fungal signature in the gut microbiota of pediatric patients with inflammatory bowel disease. Inflamm Bowel Dis. 2015;21:1948-1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Lewis JD, Chen EZ, Baldassano RN, et al. Inflammation, antibiotics, and diet as environmental stressors of the gut microbiome in pediatric Crohn’s disease. Cell Host Microbe. 2015;18:489-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Lemoinne S, Kemgang A, Ben Belkacem K, et al.; Saint-Antoine IBD Network. Fungi participate in the dysbiosis of gut microbiota in patients with primary sclerosing cholangitis. Gut. 2020;69:92-102. [DOI] [PubMed] [Google Scholar]
- 65. Sarrabayrouse G, Elias A, Yáñez F, et al. Fungal and bacterial loads: noninvasive inflammatory bowel disease biomarkers for the clinical setting. mSystems 2021;6:e01277-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Petersen AM, Stensvold CR, Mirsepasi H, et al. Active ulcerative colitis associated with low prevalence of Blastocystis and Dientamoeba fragilis infection. Scand J Gastroenterol. 2013;48:638-639. [DOI] [PubMed] [Google Scholar]
- 67. Tito RY, Chaffron S, Caenepeel C, et al. Population-level analysis of Blastocystis subtype prevalence and variation in the human gut microbiota. Gut. 2019;68:1180-1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Pérez-Brocal V, García-López R, Vázquez-Castellanos JF, et al. Study of the viral and microbial communities associated with Crohn’s disease: a metagenomic approach. Clin Transl Gastroenterol. 2013;4:e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Wagner J, Maksimovic J, Farries G, et al. Bacteriophages in gut samples from pediatric Crohn’s disease patients: metagenomic analysis using 454 pyrosequencing. Inflamm Bowel Dis. 2013;19:1598-1608. [DOI] [PubMed] [Google Scholar]
- 70. Norman JM, Handley SA, Baldridge MT, et al. Disease-specific alterations in the enteric virome in inflammatory bowel disease. Cell. 2015;160:447-460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Pérez-Brocal V, García-López R, Nos P, et al. Metagenomic analysis of crohn’s disease patients identifies changes in the virome and microbiome related to disease status and therapy, and detects potential interactions and biomarkers. Inflamm Bowel Dis. 2015;21:2515-2532. [DOI] [PubMed] [Google Scholar]
- 72. Duerkop BA, Kleiner M, Paez-Espino D, et al. Murine colitis reveals a disease-associated bacteriophage community. Nat Microbiol. 2018;3:1023-1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Lane ER, Zisman TL, Suskind DL.. The microbiota in inflammatory bowel disease: current and therapeutic insights. J Inflamm Res. 2017;10:63-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Sender R, Fuchs S, Milo R.. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 2016;14:e1002533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Halwachs B, Madhusudhan N, Krause R, et al. Critical issues in mycobiota analysis. Front Microbiol. 2017;8:180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Xie C, Goi CL, Huson DH, et al. RiboTagger: fast and unbiased 16S/18S profiling using whole community shotgun metagenomic or metatranscriptome surveys. BMC Bioinformatics. 2016;17:508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Donovan PD, Gonzalez G, Higgins DG, et al. Identification of fungi in shotgun metagenomics datasets. PLoS One. 2018;13:e0192898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. West PT, Probst AJ, Grigoriev IV, et al. Genome-reconstruction for eukaryotes from complex natural microbial communities. Genome Res. 2018;28:569-580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Soverini M, Turroni S, Biagi E, et al. HumanMycobiomeScan: a new bioinformatics tool for the characterization of the fungal fraction in metagenomic samples. BMC Genom. 2019;20:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Lind AL, Pollard KS.. Accurate and sensitive detection of microbial eukaryotes from whole metagenome shotgun sequencing. Microbiome. 2021;9:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Kõljalg U, Nilsson RH, Abarenkov K, et al. Towards a unified paradigm for sequence-based identification of fungi. Mol Ecol. 2013;22:5271-5277. [DOI] [PubMed] [Google Scholar]
- 82. Quince C, Walker AW, Simpson JT, et al. Shotgun metagenomics, from sampling to analysis. Nat Biotechnol. 2017;35:833-844. [DOI] [PubMed] [Google Scholar]
- 83. Sharpton TJ. An introduction to the analysis of shotgun metagenomic data. Front Plant Sci. 2014;5:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Olm MR, West PT, Brooks B, et al. Genome-resolved metagenomics of eukaryotic populations during early colonization of premature infants and in hospital rooms. Microbiome. 2019;7:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Saary P, Mitchell AL, Finn RD.. Estimating the quality of eukaryotic genomes recovered from metagenomic analysis with EukCC. Genome Biol. 2020;21:244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Kucik CJ, Martin GL, Sortor BV.. Common intestinal parasites. Am Fam Physician. 2004;69:1161-1168. [PubMed] [Google Scholar]
- 87. Gizaw Z, Adane T, Azanaw J, et al. Childhood intestinal parasitic infection and sanitation predictors in rural Dembiya, northwest Ethiopia. Environ Health Prev Med. 2018;23:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Schmidlin T, Hürlimann E, Silué KD, et al. Effects of hygiene and defecation behavior on helminths and intestinal protozoa infections in Taabo, Côte d’Ivoire. PLoS One. 2013;8:e65722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 2018;390:2769-2778. [DOI] [PubMed] [Google Scholar]
- 90. Zuo T, Kamm MA, Colombel JF, Ng SC.. Urbanization and the gut microbiota in health and inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2018a;15:440-452. [DOI] [PubMed] [Google Scholar]
- 91. Bach JF. The hygiene hypothesis in autoimmunity: the role of pathogens and commensals. Nat Rev Immunol. 2018;18:105-120. [DOI] [PubMed] [Google Scholar]
- 92. Loke P, Lim YA.. Helminths and the microbiota: parts of the hygiene hypothesis. Parasite Immunol. 2015;37:314-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Cho MK, Lee CH, Yu HS.. Amelioration of intestinal colitis by macrophage migration inhibitory factor isolated from intestinal parasites through toll-like receptor 2. Parasite Immunol. 2011;33:265-275. [DOI] [PubMed] [Google Scholar]
- 94. Reyes JL, Lopes F, Leung G, et al. Treatment with cestode parasite antigens results in recruitment of CCR2+ myeloid cells, the adoptive transfer of which ameliorates colitis. Infect Immun. 2016;84:3471-3483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Smith P, Mangan NE, Walsh CM, et al. Infection with a helminth parasite prevents experimental colitis via a macrophage-mediated mechanism. J Immunol. 2007;178:4557-4566. [DOI] [PubMed] [Google Scholar]
- 96. Croese J, O’neil J, Masson J, et al. A proof of concept study establishing Necator americanus in Crohn’s patients and reservoir donors. Gut. 2006;55:136-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Fortun P, Shepherd V, Moroz V, et al. OC-004 effect of hookworm treatment on active Crohn’s disease. Gut 2010;59:A2. [Google Scholar]
- 98. Sandborn WJ, Elliott DE, Weinstock J, et al. Randomised clinical trial: the safety and tolerability of Trichuris suis ova in patients with Crohn’s disease. Aliment Pharmacol Ther. 2013;38:255-263. [DOI] [PubMed] [Google Scholar]
- 99. Summers RW, Elliott DE, Qadir K, et al. Trichuris suis seems to be safe and possibly effective in the treatment of inflammatory bowel disease. Am J Gastroenterol. 2003;98:2034-2041. [DOI] [PubMed] [Google Scholar]
- 100. Garcia LS. Dientamoeba fragilis, one of the neglected intestinal protozoa. J Clin Microbiol. 2016;54:2243-2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Wawrzyniak I, Poirier P, Viscogliosi E, et al. Blastocystis, an unrecognized parasite: an overview of pathogenesis and diagnosis. Ther Adv Infect Dis. 2013;1:167-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. El Safadi D, Gaayeb L, Meloni D, et al. Children of Senegal River Basin show the highest prevalence of Blastocystis sp. ever observed worldwide. BMC Infect Dis. 2014;14:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Cacciò SM. Molecular epidemiology of Dientamoeba fragilis. Acta Trop. 2018;184:73-77. [DOI] [PubMed] [Google Scholar]
- 104. Stark D, Roberts T, Marriott D, et al. Detection and transmission of Dientamoeba fragilis from environmental and household samples. Am J Trop Med Hyg. 2012;86:233-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Brands MR, Van de Vijver E, Haisma SM, et al. No association between abdominal pain and Dientamoeba in Dutch and Belgian children. Arch Dis Child. 2019;104:686-689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Holtman GA, Kranenberg JJ, Blanker MH, et al. Dientamoeba fragilis colonization is not associated with gastrointestinal symptoms in children at primary care level. Fam Pract. 2016;34:25-29. [DOI] [PubMed] [Google Scholar]
- 107. Jokelainen P, Hebbelstrup Jensen B, Andreassen BU, et al. Dientamoeba fragilis, a commensal in children in Danish day care centers. J Clin Microbiol. 2017;55:1707-1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Dullaert-de Boer M, Schuurs TA, Vermeer M, et al. Distribution and relevance of Dientamoeba fragilis and Blastocystis species in gastroenteritis: results from a case-control study. Eur J Clin Microbiol Infect Dis. 2019;39:197-203. [DOI] [PubMed] [Google Scholar]
- 109. Marzano V, Mancinelli L, Bracaglia G, et al. “Omic” investigations of protozoa and worms for a deeper understanding of the human gut “parasitome”. PLoS Negl Trop Dis. 2017;11:e0005916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Clark CG, Stensvold CR.. Blastocystis: isolation, xenic cultivation, and cryopreservation. Curr Protoc Microbiol. 2016;43:20a.21.21-20a.21.28. [DOI] [PubMed] [Google Scholar]
- 111. Roberts T, Barratt J, Harkness J, et al. Comparison of microscopy, culture, and conventional polymerase chain reaction for detection of Blastocystis sp. in clinical stool samples. Am J Trop Med Hyg. 2011;84:308-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Cannon MV, Bogale H, Rutt L, et al. A high-throughput sequencing assay to comprehensively detect and characterize unicellular eukaryotes and helminths from biological and environmental samples. Microbiome 2018;6:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Zhang YZ, Shi M, Holmes EC.. Using metagenomics to characterize an expanding virosphere. Cell. 2018;172:1168-1172. [DOI] [PubMed] [Google Scholar]
- 114. Carding SR, Davis N, Hoyles L.. Review article: the human intestinal virome in health and disease. Aliment Pharmacol Ther. 2017;46:800-815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Gregory AC, Zablocki O, Zayed AA, et al. The gut virome database reveals age-dependent patterns of virome diversity in the human gut. Cell Host Microbe. 2020;28:724-740.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Mukhopadhya I, Segal JP, Carding SR, et al. The gut virome: the ‘missing link’ between gut bacteria and host immunity? Therap Adv Gastroenterol. 2019;12:1756284819836620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Lavigne R, Molineux IJ, Kropinski AM.. Order—caudovirales. In: King AMQ, Adams MJ, Carstens EB, Lefkowitz EJ, eds. Virus Taxonomy. San Diego: Elsevier; 2012:39-45. [Google Scholar]
- 118. Dutilh BE, Reyes A, Hall RJ, Whiteson KL.. Editorial: virus discovery by metagenomics: the (im)possibilities. Front Microbiol. 2017;8:1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Qin J, Li R, Raes J, et al.; MetaHIT Consortium. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464:59-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Kleiner M, Hooper LV, Duerkop BA.. Evaluation of methods to purify virus-like particles for metagenomic sequencing of intestinal viromes. BMC Genomics. 2015;16:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Roux S, Tournayre J, Mahul A, et al. Metavir 2: new tools for viral metagenome comparison and assembled virome analysis. BMC Bioinformatics. 2014;15:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Li Y, Wang H, Nie K, et al. VIP: an integrated pipeline for metagenomics of virus identification and discovery. Sci Rep. 2016;6:23774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Ren J, Ahlgren NA, Lu YY, et al. VirFinder: a novel k-mer based tool for identifying viral sequences from assembled metagenomic data. Microbiome. 2017;5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Brister JR, Ako-Adjei D, Bao Y, Blinkova O.. NCBI viral genomes resource. Nucleic Acids Res. 2015;43:D571-D577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Paez-Espino D, Chen IA, Palaniappan K, et al. IMG/VR: a database of cultured and uncultured DNA Viruses and retroviruses. Nucleic Acids Res. 2017;45:D457-D465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Leplae R, Hebrant A, Wodak SJ, Toussaint A.. ACLAME: a CLAssification of Mobile genetic Elements. Nucleic Acids Res. 2004;32:D45-D49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Metsky HC, Siddle KJ, Gladden-Young A, et al.; Viral Hemorrhagic Fever Consortium. Capturing sequence diversity in metagenomes with comprehensive and scalable probe design. Nat Biotechnol. 2019;37:160-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Levine A, Wine E, Assa A, et al. Crohn’s disease exclusion diet plus partial enteral nutrition induces sustained remission in a randomized controlled trial. Gastroenterology 2019;157:440-450.e8. [DOI] [PubMed] [Google Scholar]
- 129. Sales-Campos H, Soares SC, Oliveira CJF.. An introduction of the role of probiotics in human infections and autoimmune diseases. Crit Rev Microbiol. 2019;45:413-432. [DOI] [PubMed] [Google Scholar]
- 130. Singh RK, Chang HW, Yan D, et al. Influence of diet on the gut microbiome and implications for human health. J Transl Med. 2017;15:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Kassam Z, Lee CH, Yuan Y, Hunt RH.. Fecal microbiota transplantation for Clostridium difficile infection: systematic review and meta-analysis. Am J Gastroenterol. 2013;108:500-508. [DOI] [PubMed] [Google Scholar]
- 132. Ramai D, Zakhia K, Fields PJ, et al. Fecal microbiota transplantation (FMT) with colonoscopy is superior to enema and nasogastric tube while comparable to capsule for the treatment of recurrent clostridioides difficile infection: a systematic review and meta-analysis. Digest Dis Sci. 2021;66:369-380. [DOI] [PubMed] [Google Scholar]
- 133. Sadowsky MJ, Khoruts A.. Faecal microbiota transplantation is promising but not a panacea. Nat Microbiol. 2016;1:16015. [DOI] [PubMed] [Google Scholar]
- 134. Caldeira LdF, Borba HH, Tonin FS, et al. Fecal microbiota transplantation in inflammatory bowel disease patients: a systematic review and meta-analysis. PLoS One. 2020;15:e0238910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Costello SP, Soo W, Bryant RV, et al. Systematic review with meta-analysis: faecal microbiota transplantation for the induction of remission for active ulcerative colitis. Aliment Pharmacol Ther. 2017;46:213-224. [DOI] [PubMed] [Google Scholar]
- 136. Lopez J, Grinspan A.. Fecal microbiota transplantation for inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2016;12:374-379. [PMC free article] [PubMed] [Google Scholar]
- 137. Thomas AM, Segata N.. Multiple levels of the unknown in microbiome research. BMC Biol. 2019;17:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Terveer EM, van Beurden YH, Goorhuis A, et al. How to: establish and run a stool bank. Clin Microbiol Infect. 2017;23:924-930. [DOI] [PubMed] [Google Scholar]
- 139. Costello SP, Hughes PA, Waters O, et al. Effect of fecal microbiota transplantation on 8-week remission in patients with ulcerative colitis: a randomized clinical trial. JAMA. 2019;321:156-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Terveer EM, van Gool T, Ooijevaar RE, et al.; Netherlands Donor Feces Bank (NDFB) Study Group. Human transmission of blastocystis by fecal microbiota transplantation without development of gastrointestinal symptoms in recipients. Clin Infect Dis. 2020;2630-2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Zuo T, Wong SH, Lam K, et al. Bacteriophage transfer during faecal microbiota transplantation in Clostridium difficile infection is associated with treatment outcome. Gut. 2018;67:634-643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Laforest-Lapointe I, Arrieta MC.. Microbial eukaryotes: a missing link in gut microbiome studies. mSystems 2018;3:e00201-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Marcos-Zambrano LJ, Karaduzovic-Hadziabdic K, Loncar Turukalo T, et al. Applications of machine learning in human microbiome studies: a review on feature selection, biomarker identification, disease prediction and treatment. Front Microbiol. 2021;12:634511. [DOI] [PMC free article] [PubMed] [Google Scholar]