Abstract
Background
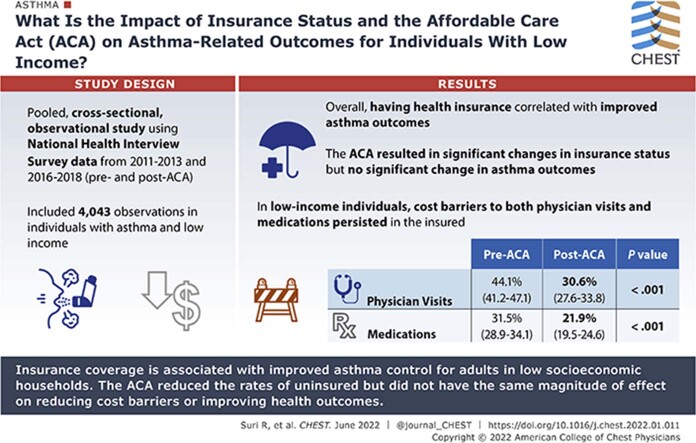
Asthma disproportionately affects individuals with lower income. High uninsured rates are a potential driver for this disparity. Previous studies have not examined the effect of the Affordable Care Act (ACA) on asthma-related outcomes for individuals with low income.
Research Question
What is the impact of insurance status and the ACA on asthma outcomes for adults 18 to 64 years of age in households with low-income status?
Study Design and Methods
This study was a pooled cross-sectional observational study using National Health Interview Survey data from 2011 through 2013 and 2016 through 2018. Individuals 18 to 64 years of age with a history of asthma and low income were included. Survey-weighted regression modeling and mediation analysis was used to explore the relationship of insurance status and asthma control. Univariate and multivariate survey-weighted regression modeling then was used to evaluate the correlation of the ACA and asthma outcomes.
Results
We identified 4,043 individual observations. Having health insurance was correlated with improved asthma outcomes (OR, 1.25). This relationship was completely mediated by cost barriers to medications and physician visits. Although the ACA resulted in significant changes in insurance status (OR, 2.4), no statistically significant change was found in asthma outcomes. Furthermore, cost barriers to both medications and physician visits persisted in the insured population, 20.7% and 30.0%, respectively.
Interpretation
Insurance coverage is associated with improved asthma control for adults 18 to 64 years from households with low socioeconomic status. The ACA reduced the rates of uninsured, but did not have the same magnitude of effect on reducing cost barriers. The persistence of cost barriers may explain in part the lack of population-level improvement in asthma control.
Key Words: Affordable Care Act, asthma outcomes
Abbreviations: ACA, Affordable Care Act; FPL, federal poverty level; KHB, Karlson, Bernt, and Holm; NHIS, National Health Interview Survey
Graphical Abstract
FOR EDITORIAL COMMENT, SEE PAGE 1429
Take-home Points.
Study Question: For individuals with low income, does insurance status improve asthma outcomes, and what effect has the Affordable Care Act (ACA) had on asthma control?
Results: Having insurance is associated with improved asthma outcomes, but this did not translate to a statistically significant population-level improvement in asthma outcomes during the period after ACA implementation.
Interpretation: Persistent cost barriers and underinsurance for individuals with low income may explain the lack of population-level improvement for asthma in the period after ACA implementation, despite improvements in uninsured rates.
Asthma affects 8% of the adult population in the United States and accounts for 9.8 million office visits annually.1 Prior studies found that asthma disproportionately impacts individuals with lower socioeconomic status, resulting in an increased risk of treatment failure and asthma exacerbations.2 Additionally, adults with asthma have demonstrated higher odds of experiencing an exacerbation because of interruptions in health-care coverage, no insurance, or public insurance defined as Medicaid and Medicare.3, 4, 5 In fact, individuals without insurance more commonly delay or forgo filling asthma medications and also self-adjust dosing to ration supply.6 Furthermore, biologic medications, which are newer and effective, but more costly, are prescribed predominantly to individuals with higher income and commercial insurance.7 Therefore, insurance status and the associated financial barriers limiting access to medications and physician visits are potential drivers for the increased disease burden in lower socioeconomic groups.
The Affordable Care Act (ACA) expanded Medicaid up to 138% of the federal poverty level (FPL) with the hopes of improving health outcomes by decreasing uninsured rates and subsequently reducing the individual’s financial burden. However, the Supreme Court rendered this expansion optional, leaving it up to individual states to decide the outcome of this provision. Despite the ruling, subsequent studies demonstrated effectiveness in the overall policy, with a reduction in individuals without insurance and increase in Medicaid enrollees.8, 9, 10, 11, 12, 13, 14, 15, 16 Medicaid expansion resulted in 13.1 million new Medicaid enrollees in states that voluntarily expanded and 1.69 million new enrollees for states that did not expand Medicaid.17 It is postulated that previously eligible individuals in nonexpansion states realized their eligibility and therefore increased enrollment.17,18
In addition to the expansion of Medicaid, the ACA established an insurance marketplace that offered private health insurance with an income-based tax-credit subsidy for individuals between 100% and 400% of the FPL. The policy also included regulations to ban discrimination based on pre-existing conditions and to ban annual or lifetime benefit limits. Of the total decrease in individuals without insurance, 40% is attributed to the insurance marketplace.18
Ultimately, this increased insurance coverage improved an individual’s ability to pay for health care.8,19 Fewer people are delaying medications and physician visits because of cost, and catastrophic fees occur less frequently.9, 10, 11, 12, 13, 14 For individuals with asthma, data from the Behavioral Risk Factor Surveillance System demonstrated a trend toward decreased inability to pay for medications and physician visits.20 This translated into a 15% increase in respiratory and allergy medications in states that expanded Medicaid.21,22 Interestingly, states with higher cost-sharing models through drug co-pays experienced a smaller increase in prescription medications.22
Disease-specific outcome measurements have been more difficult to assess given the complexity of contributing factors and short follow-up periods. However, a linked survey and administrative data study demonstrated a mortality benefit for individuals with low income after Medicaid expansion.16 Furthermore, other studies have demonstrated improvement in HIV identification and viral suppression, lower incidence of ruptured appendicitis, and better hypertension control.15,23,24To our knowledge, no studies have evaluated outcome measurements for asthma.
This study sought to add to the literature by evaluating the effect of insurance status on asthma control, specifically for the low-income adult population 18 to 64 years of age. Furthermore, it evaluated factors that mediate the association of insurance status and asthma outcomes. Finally, the study aimed to evaluate the effect of the ACA on insurance status, cost barriers, and asthma control.
Study Design and Methods
This is a pooled cross-sectional observational study using National Health Interview Survey (NHIS) data from 2011 through 2013 (before ACA implementation) and from 2016 through 2018 (after ACA implementation). The years 2014 and 2015 were treated as a washout period. A total of 29 states expanded Medicaid by 2015.25 It is important to note that five states and the District of Columbia began expanding Medicaid to different degrees before 2014.26 Additionally, two states expanded Medicaid in 2016.25
The NHIS is a cross-sectional in-person household interview survey. The number of participants sampled ranged from 72,831 in 2018 to 108,131 in 2012. The response rate ranged from 64.2% in 2018 to 82% in 2011. This dataset excludes individuals in correctional facilities and long-term care as well as US nationals living abroad or families with all adults who are active-duty military.27
We excluded individuals younger than 18 years and older than 65 years to focus the analysis on nonelderly adults who were most likely to benefit from the policy. Of the remaining population, we selected sample adults who identified as currently having asthma, as defined by the question, “Do you still have asthma?” Nonsample adults were not asked asthma-specific questions. Ideally, the studied population would include only those at < 138% of the FPL to limit the analysis to those eligible for Medicaid expansion. Based on the cutoffs available in the public-use NHIS dataset, individuals at < 149% of the FPL were selected for this analysis. Of the total sample, 1.38% were defined in a larger category of 100% to 199% of the federal poverty level. Additionally, 4.85% were categorized as “undefinable” or “unknown.” For these subsets, imputed family income and family size were used to identify those at less than the 138% threshold.28
The independent variable was defined as having any health insurance coverage at the time of the survey, and the dependent variable was defined as having asthma control. Direct measures of asthma control such as daily symptom burden are not available. Therefore, we used indirect measures of asthma control as defined by the American Thoracic Society and European Respiratory Society.29 Individuals with asthma were asked if they had an asthma attack or episode in the previous 12 months, visited the ED for asthma in the previous 12 months, or required hospitalization for asthma in the previous 12 months. Answering “no” to all three questions was defined as having asthma control.
The study’s conceptual model did not posit any direct relationship between insurance status and asthma control. Instead, we hypothesized that the effect of insurance on asthma control was mediated fully by cost barriers to medications and physician visits. Cost barriers to medications were defined as needing but unable to afford prescription medicine in the previous 12 months. Similarly, cost barriers to physician visits were defined as needing but unable to afford medical care, follow-up care, or specialist care in the previous 12 months. Confounders include sex, age, race or ethnicity, education level, smoking status, routine influenza vaccine, and having an established relationship with a physician. Race or ethnicity was defined as White, Black, Hispanic, and other. Other included American Indian or Alaskan Native, Asian, multiracial, or race group not releasable. Education level was defined as high school or less, some college, or Bachelor’s degree or higher. Potential confounders such as genetics, environmental factors, and other public health interventions are not included in the dataset.
Survey-weighted data were used for this analysis. A descriptive analysis was performed for uncontrolled and controlled asthma. A design-corrected F test was performed to evaluate differences between the two groups. The next analysis used the Karlson, Bernt, and Holm (KHB) model to test the hypothesis that cost barriers to physicians or medications are mediators in the relationship of insurance status and asthma outcomes.30,31 Given the nonlinear regression models, the KHB method was used to allow comparison of the regression coefficients before and after the addition of potential mediators to the model.
A set of nested survey-weighted logistic regression models was built to assess the relationship between insurance status and asthma control. The first model included demographic variables and confounders. The second and third models included the hypothesized mediators of cost barriers to physician visits and medications in a stepwise fashion.
The next set of analyses evaluated the periods before and after ACA implementation. The approach used was similar to intention-to-treat analysis in that all states were given the opportunity to expand Medicaid, but not all chose to do so. The public-use NHIS dataset did not allow for specifications based on states. For the analysis, we identified a comparative group of sample adults at > 400% of the FPL who were 18 to 64 years of age with a concurrent diagnosis of asthma. Descriptive characteristics were obtained using survey-weighted data with a design-corrected F test. We further explored the association of ACA implementation on insurance status and cost barriers to physician visits and medications. An adjusted Wald test using the suest command was used to evaluate for different magnitudes of effect by ACA implementation.
A survey-weighted logistic regression model then was used to evaluate the association of ACA implementation on asthma outcomes. Before ACA implementation was defined as 2011 through 2013, and after ACA implementation was defined as 2016 through 2018. Sex, age, race or ethnicity, and education level were confounders in this analysis. A subsequent model incorporated individuals at > 400% of the FPL to evaluate if the interaction of high income and ACA implementation revealed a different association with asthma outcomes.
Stata version 15 software (StataCorp) was used for the analysis. This study was based on de-identified publicly available data and was considered exempt from human subject review.
Results
The 6 years of NHIS data resulted in 562,658 individual observations. After selecting for a population with low income, 18 to 64 years of age, sample adults currently with asthma, and dropping individuals with any missing data (2.91%), the final sample size was 4,043 individual observations. The comparative group of individuals at > 400% of the FPL with all other similar characteristics had 1.82% missing data and a final sample size of 3,512 observations.
Survey-weighted descriptive analysis of controlled and uncontrolled asthma for individuals with low income is depicted in Table 1. A larger proportion of individuals with controlled asthma was younger than among those with uncontrolled asthma. The controlled asthma group included a lower percentage of female patients and a lower percentage of cost barriers to physician or medication access compared with the uncontrolled asthma group. The controlled asthma group showed a trend toward having more insurance, although this did not reach statistical significance with a P value of .11. No difference was found regarding race or ethnicity and education level. In further survey-weighted descriptive analysis not depicted in Table 1, of those individuals with cost barriers to either medications or physician visits, asthma control was 39.8% compared with 52.7% without any cost barriers.
Table 1.
Descriptive Analysis by Asthma Control Status
| Variable | Uncontrolled Asthma | Controlled Asthma | Total Population | P Valuea |
|---|---|---|---|---|
| Age, y | < .001 | |||
| 18-29 | 27.21 (24.74-29.84) | 39.5 (36.53-42.55) | 32.98 (30.96-35.08) | |
| 30-39 | 17.79 (15.82-19.94) | 16.8 (14.77-19.05) | 17.33 (15.88-18.88) | |
| 40-49 | 19.6 (17.39-22.02) | 15.85 (13.77-18.18) | 17.84 (16.28-19.52) | |
| 50-64 | 35.4 (32.87-38.01) | 27.85 (25.22-30.64) | 31.85 (30.02-33.75) | |
| Sex | < .001 | |||
| Female | 72.54 (69.90-75.03) | 61.69 (58.71-64.58) | 67.44 (65.40-69.42) | |
| Race or ethnicity | .469 | |||
| White | 52.13 (49.13-55.11) | 49.71 (46.51-52.92) | 50.99 (48.69-53.29) | |
| Black | 23.37 (20.83-26.11) | 23.35 (20.80-26.11) | 23.36 (21.42-25.43) | |
| Hispanic | 17.24 (15.01-19.73) | 18.06 (15.51-20.93) | 17.63 (15.87-19.54) | |
| Otherb | 7.26 (5.95-8.83) | 8.87 (7.17-10.92) | 8.02 (6.90-9.30) | |
| Education | .408 | |||
| High school or less | 56.12 (53.27-58.93) | 58.87 (55.80-61.88) | 57.41 (55.30-59.49) | |
| Some college | 35.67 (32.99-38.43) | 33.18 (30.36-36.12) | 34.5 (32.532-36.54) | |
| Bachelor’s degree or more | 8.22 (6.83-9.85) | 7.95 (6.42-9.81) | 8.09 (7.04-9.29) | |
| Insurance status | .11 | |||
| Uninsured | 20.69 (18.49-23.08) | 18.21 (15.97-20.69) | 19.53 (17.83-21.36) | |
| Cost barriers to seeing physician | < .001 | |||
| Delayed care | 42.23 (39.42-45.08) | 32.11 (29.30-35.05) | 37.47 (35.33-39.66) | |
| Cost barriers to medications | < .001 | |||
| Cost barrier | 33.20 (30.62-35.88) | 19.54 (17.28-22.01) | 26.78 (24.95-28.69) | |
| Having a usual place of care | .629 | |||
| No usual place | 14.07 (12.06-16.35) | 14.83 (12.83-17.07) | 14.43 (13.01-15.96) | |
| Smoking status | .482 | |||
| Current smoker, % | 34.81 (32.32-37.39) | 33.48 (30.78-36.28) | 34.19 (32.33-36.09) | |
| Flu vaccine | .445 | |||
| No vaccine | 60.01 (57.20-62.76) | 61.61 (58.65-64.50) | 60.76 (58.77-62.72) |
Data are survey weighted and presented as percentage (95% CI), unless otherwise indicated.
Design-corrected F test to compare groups.
Includes American Indian or Alaskan Native, Asian, multiracial, or race group not releasable.
The relationship between insurance status and asthma control is believed to be mediated through reducing cost barriers to physician visits and medications. This hypothesis was tested with the KHB model. Cost barriers to physicians and medications both independently demonstrated significant mediation, resulting in a nonsignificant relationship between insurance status and asthma control.
Although 51.7% of individuals with low income without insurance reported having medication-related cost barriers, only 20.7% of individuals with low income with insurance reported having these issues. Similarly, a difference in cost barriers to physician visits from 68.3% to 30.0% was reported. When combining both metrics for cost barriers, 72.3% of individuals with low income without insurance reported cost barriers compared with 37.6% for those with insurance.
Model 1 of the multiple logistic regression analysis showed higher odds for asthma control when having insurance coverage (Table 2). The second model added cost barriers for physician visits, which showed an associated OR of 1.45 for asthma control. The third model showed that when all else was equal, not having a cost barrier to medication was associated with an increased odds for asthma control (OR, 1.93). Cost barrier to physicians was removed in this model because of concern of collinearity. As expected, based on the KHB model, adding mediators for cost barriers to physicians and medications removes the association of insurance status and asthma control.
Table 2.
Survey-Weighted Logistic Regression Model for Asthma Control With OR (95% CI)
| Variable | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Unweighted sample size, No. | 4,046 | 4,046 | 4,043 |
| Sex | |||
| Male | Reference | … | … |
| Female | 0.64a (0.54-0.77) | 0.65a (0.54-0.77) | 0.66a (0.55-0.79) |
| Age | |||
| Age | 0.98a (0.98-0.99) | 0.98a (0.98-0.99) | 0.98a (0.98-0.99) |
| Race or ethnicity | |||
| White | Reference | … | … |
| Black | 1.03 (0.83-1.3) | 1.00 (0.81-1.2) | 1.02 (0.83-1.3) |
| Hispanic | 1.11 (0.86-1.4) | 1.09 (0.83-1.4) | 1.10 (0.84-1.4) |
| Otherb | 1.16 (0.85-1.6) | 1.14 (0.83-1.5) | 1.11 (0.81-1.5) |
| Education | |||
| High school or less | Reference | … | … |
| Some college | 0.88 (0.73-1.1) | 0.89 (0.74-1.1) | 0.89 (0.74-1.1) |
| Bachelor’s degree or more | 0.95 (0.68-1.3) | 0.98 (0.71-1.4) | 0.93 (0.67-1.3) |
| Smoking status | |||
| Current smoker | Reference | … | … |
| Nonsmoker | 1.01 (0.85-1.2) | 0.98 (0.82-1.2) | 0.97 (0.82-1.2) |
| Having a usual place of care | |||
| No | Reference | … | … |
| Yes | 1.04 (0.79-1.4) | 1.01 (0.76-1.3) | 1.04 (0.78-1.4) |
| Flu vaccine | |||
| No | Reference | … | … |
| Yes | 0.99 (0.82-1.2) | 0.99 (0.82-1.2) | 1.00 (0.83-1.2) |
| Insurance status | |||
| Uninsured | Reference | … | … |
| Insured | 1.25c (1.0-1.6) | 1.09 (0.86-1.4) | 1.02 (0.80-1.3) |
| Cost barrier to physician | |||
| Yes | Reference | … | … |
| No | … | 1.45a (1.2-1.7) | … |
| Cost barrier to medications | |||
| Yes | Reference | … | … |
| No | … | … | 1.93a (1.6-2.3) |
Data are presented as OR (95% CI), unless otherwise indicated.
P ≤ .005.
Includes American Indian or Alaskan Native, Asian, multiracial, or race group not releasable.
P ≤ .05.
Before and after ACA implementation survey-weighted descriptive analysis is shown in Table 3. A significant decrease was found in the uninsured population for individuals with both low and high income, although the magnitude of change is different, –13.2% vs –2%. A significant decrease in cost barriers for physician visits and medications was seen only for individuals with low income. Interestingly, only high-income individuals showed statistically significant improvement in asthma outcomes, with asthma control improving from 53% to 57.1% (P = .046).
Table 3.
Descriptive Analysis by Period Before Implementation (2011-2013) and After Implementation (2016-2018) of the ACA for Individuals With Both Low and High Income
| Variable | Low Income |
High Income |
||||
|---|---|---|---|---|---|---|
| Before ACA Implementation | After ACA Implementation | P Valuea | Before ACA Implementation | After ACA Implementation | P Valuea | |
| Uninsured | 26.0 (23.5-28.7) | 12.8 (10.7-15.2) | < .001 | 4.8 (3.7-6.2) | 2.8 (2.0-3.8) | .01 |
| Cost barrier to physician | 44.1 (41.2-47.1) | 30.6 (27.6-33.8) | < .001 | 13.6 (11.7-15.6) | 14.3 (12.4-16.4) | .65 |
| Cost barrier to medications | 31.5 (28.9-34.1) | 21.9 (19.5-24.6) | < .001 | 6.4 (5.1-8.0) | 6.9 (5.5-8.5) | .66 |
| Asthma control | 45.4 (42.8-48.0) | 48.6 (45.3-52.0) | .13 | 53.0 (50.0-55.9) | 57.1 (54.2-60.0) | .05 |
Data are survey weighted and presented as percentage (95% CI), unless otherwise indicated. ACA = Affordable Care Act.
Design-corrected F test to compare groups.
Table 4 shows the univariate analysis of ACA implementation for low-income individuals and its association with insurance status and two mediators of cost barriers. The period after ACA implementation showed a meaningful increase in being insured (OR, 2.4). More precisely, the uninsured rate decreased from 26.0% to 12.8% after ACA implementation. The association of period after ACA implementation and no cost barrier to physicians or medications, although statistically significant, was of a lower magnitude (OR, 1.79 and 1.63, respectively). An adjusted Wald test using the suest command confirmed the difference in association of the ACA on insurance status compared with reducing cost barriers to both physicians and medications.
Table 4.
Univariate Logistic Regression of Period After ACA Implementation Compared With Reference Group of Period Before ACA Implementation on Insurance Status and Cost Barriers to Physicians and Medications
| Variable | OR | P Value |
|---|---|---|
| Having insurance | 2.40 | < .001 |
| No cost barrier to physicians | 1.79 | < .001 |
| No cost barrier to medications | 1.63 | < .001 |
Adjusted Wald test using suest command revealed a significant difference in effect of ACA implementation on insurance status vs physician cost barrier (P = .03) and medication cost barrier (P = .004). No difference was found in effect of ACA implementation on physician cost barrier vs medication cost barrier. ACA = Affordable Care Act.
Table 5 presents results of multivariate logistic regressions of asthma control before and after ACA implementation. The period after ACA implementation was associated with higher odds (OR, 1.16) of improved asthma control compared with the period before Medicaid expansion. This was not statistically significant, with a P value of .09. A second model incorporated individuals with high income as a comparative group. No difference was found between the two groups regarding the correlation of asthma control before and after the implementation of the ACA.
Table 5.
Multivariate Logistic Regression Model of Period After ACA Implementation Compared With Reference Group of Period Before ACA Implementation on Asthma Control
| Variable | Model 1 |
Model 2 |
||
|---|---|---|---|---|
| β Coefficient | P Value | β Coefficient | P Value | |
| Sex | ||||
| Male | Reference | Reference | ||
| Female | –0.44 (–0.62 to –0.27) | < .001 | –0.37 (–0.50 to –0.24) | < .001 |
| Age | –0.02 (–0.02 to –0.01) | < .001 | –0.01 (–0.01 to –0.01) | < .001 |
| Race or ethnicity | ||||
| White | Reference | Reference | ||
| Black | 0.05 (–0.16 to 0.26) | .63 | 0.05 (–0.13 to 0.23) | .56 |
| Hispanic | 0.07 (–0.18 to 0.33) | .58 | –0.03 (–0.25 to 0.20) | .82 |
| Othera | 0.16 (–0.14 to 0.46) | .31 | 0.17 (–0.05 to 0.39) | .12 |
| Education | ||||
| High school or less | Reference | Reference | ||
| Some college | –0.15 (–0.33 to 0.03) | .10 | –0.02 (–0.16 to 0.13) | .81 |
| Bachelor’s degree or more | –0.05 (–0.37 to 0.27) | .74 | –0.07 (–0.24 to 0.10) | .41 |
| Affordable Care Act implementation | ||||
| Before | Reference | Reference | ||
| After | 0.15 (–0.02 to 0.32) | .09 | 0.14 (–0.03 to 0.31) | .11 |
| Income | ||||
| Low | … | … | Reference | |
| High | … | … | 0.34 (0.20-0.56) | < .001 |
| After implementation × high income | … | … | 0.03 (–0.20 to 0.27) | .781 |
ACA = Affordable Care Act.
Includes American Indian or Alaskan Native, Asian, multiracial, or race group not releasable.
Discussion
Although prior studies evaluated the effect of insurance status on asthma control regardless of income, this study sought to elucidate this association for the low-income adult population 18 to 64 years of age. Furthermore, this study evaluated the association of ACA implementation on insurance status, asthma control, and the proposed mediators of these associations for low-income individuals.
This study showed several significant findings. For individuals between 18 and 64 years of age and of lower income status, having health insurance showed a significant correlation with improved asthma outcomes. This is consistent with prior studies that demonstrated the significance of insurance coverage in the general population.3, 4, 5,32, 33, 34 This analysis differs from prior literature in that it focused on a financially vulnerable population—and the association was maintained.
Second, we found that despite this association of having insurance and improved asthma outcomes, ACA implementation did not demonstrate a statistically significant association for improved asthma control. However, with an OR of 1.16 (β = 0.15), the magnitude of observed clinical difference may be clinically relevant. This analysis was performed as an intention-to-treat analysis for the country because it included states that both expanded and did not expand Medicaid. By the end of 2018, 31 states and the District of Columbia had expanded Medicaid. With 19 states not expanding, the potential correlation may have been dampened. Since the end of the inclusion period of 2018 for this study, an additional six states have expanded Medicaid.25
A third significant finding of our study is that the relationship of insurance and asthma outcomes is mediated strongly through decreasing cost barriers to physician visits and medications. Despite this mediation, cost barriers to both physicians and medications persisted for individuals with low income, despite having insurance. Cost barriers to medications remained for 20.7% of the insured low-income population, whereas cost barriers to physicians remained at 30.0%. The ACA showed a population effect on insurance status. However, it did not have the same degree of effect on removing cost barriers to physicians or medications.
The findings of our study have several important policy implications. The persistent cost barriers despite having insurance offer a potential explanation for the lack of statistically significant population-level association of asthma control in the period after ACA implementation. Despite higher rates of insurance, individuals remained underinsured with a significant cost burden. This is consistent with the findings of Magge et al,35 who described a prevalence of 34.5% of underinsurance for low-income individuals. In their analysis, underinsured status was defined as expenditures of > 5% of household income or delaying medical care or prescriptions because of cost. Our analysis was unable to calculate expenditures as a percentage of household income, but it did incorporate cost barriers to physician visits and medications. With the narrower definition, 37.6% of insured low-income adults 18 to 64 years of age with asthma were underinsured.
The negative impacts of being underinsured are compounded by the higher co-pays for brand-name medications. This could contribute to the cost barriers for medications, despite having insurance. In the United States, options are limited for generic inhalers for asthma. Fluticasone plus salmeterol and albuterol became among of the first generic asthma medications in 2019 and 2020, respectively.36,37 Both of these occurred after the inclusion period of this analysis. Additionally, Ghosh et al22 showed significant price elasticity for respiratory and allergy medications within this population. They demonstrated change in medication use resulting from co-pays as either part of a price sharing model or the result of brand name medications. Negotiation of drug prices at a national level may be necessary to reduce the cost barrier for medications. This is especially important for a disease like asthma that has a disproportionate burden on individuals with lower socioeconomic status, has significant price elasticity, and for which only a few options for generic medications exist.
Cost-sharing models for health insurance are a tool used to rein in costs and reduce overuse of health-care services.38 However, a detrimental effect of this same policy is the creation of barriers for necessary access to care and treatment, which leads to underinsurance. Further analysis is needed to optimize the balance of cost-sharing on the spectrum of overuse and the creation of barriers that hinder access to physician visits and medications. This balance may lie at a different point for those with high income vs low income.
Our findings must be interpreted in the context of our study design. The cross-sectional design resulting in lack of longitudinal follow-up and the observational study design limit the causal inference one can draw. NHIS data are self-reported data that are subject to recall bias, which can influence the categorization of controlled vs uncontrolled asthma. Furthermore, the outcome variable of asthma control is evaluated using indirect measures of exacerbations in an all-or-nothing format and does not capture, for example, improvement in the number of exacerbations. Additionally, this analysis does not account for measures of direct asthma control, which is defined by daily symptom burden.29
The inclusion criteria do not include citizenship status; therefore, we cannot be sure that every individual is a candidate for Medicaid expansion. Additionally, the insurance status question asks only about having insurance at the time of the survey, and does not comment on having insurance all year. As prior studies have demonstrated, interruptions in care can impact asthma control negatively.3 By potentially including individuals with coverage interruptions, the association between insurance status and asthma control could be reduced. Louisiana and Montana both expanded Medicaid during the years 2016 through 2018.25 For these states, some preimplementation period is included in the postimplementation category.
The NHIS dataset also is unable to capture data on environmental factors and genetics, which may confound the results. Finally, ACA implementation occurred at the same time as an economic recovery. Isolating the effects of the ACA is not possible with this study design.
Interpretation
For individuals with low income who are 18 to 64 years of age, insurance coverage is associated with improved asthma control. This effect is mediated by decreased cost barriers to physician visits and medication access. The ACA resulted in a significant decrease in the uninsured population. However, the policy did not have the same magnitude of effect on reducing cost barriers. The continued issue of cost barriers and underinsurance may explain the lack of population-level improvement in asthma control.
Acknowledgments
Author contributions: R. S., J. M., and J. N. conceived and designed the study. R. S. analyzed and interpreted the data. R. S., J. M., M. I., and J. N. wrote and edited the manuscript.
Financial/nonfinancial disclosures: None declared.
Footnotes
FUNDING/SUPPORT: The authors have reported to CHEST that no funding was received for this study.
References
- 1.Centers for Disease Control and Prevention Asthma. 2021. Centers for Disease Control and Prevention website. cdc.gov/nchs/fastats/asthma.htm
- 2.Cardet J.C., Louisias M., King T.S., et al. Income is an independent risk factor for worse asthma outcomes. J Allergy Clin Immunol. 2019;141(2):754–760. doi: 10.1016/j.jaci.2017.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Markovitz B.P., Andresen E.M. Lack of insurance coverage and urgent care use for asthma: a retrospective cohort study. BMC Public Health. 2006;6:1–6. doi: 10.1186/1471-2458-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hasegawa K., Stoll S.J., Ahn J., Kysia R.F., Sullivan A.F., Camargo C.A. Association of insurance status with severity and management in ED patients with asthma exacerbation. West J Emerg Med. 2016;17(1):22–27. doi: 10.5811/westjem.2015.11.28715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hasegawa K., Sullivan A.F., Tovar Hirashima E., et al. A multicenter observational study of US adults with acute asthma: who are the frequent users of the emergency department? J Allergy Clin Immunol Pract. 2014;2(6):733–740.e3. doi: 10.1016/j.jaip.2014.06.012. [DOI] [PubMed] [Google Scholar]
- 6.Stevens D., Sharma K., Kesten S. Insurance status and patient behavior with asthma medications. J Asthma. 2003;40(7):789–793. doi: 10.1081/jas-120023570. [DOI] [PubMed] [Google Scholar]
- 7.Inselman J., Jeffery M.M., Maddux J.T., Shah N.D., Rank M.A. Trends and disparities in asthma biologic use in the United States. J Allergy Clin Immunol Pr. 2020;8(2):549–554. doi: 10.1016/j.jaip.2019.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barakat M.T., Mithal A., Huang R.J., et al. Affordable Care Act and healthcare delivery: a comparison of California and Florida hospitals and emergency departments. PLoS One. 2017;12(8):1–12. doi: 10.1371/journal.pone.0182346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carrie F., Sommers B.D. Effect of Medicaid expansion on health insurance coverage and access to care among adults with depression. Psychiatr Serv. 2018;69(11):1146–1152. doi: 10.1176/appi.ps.201800181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cawley J., Soni A., Simon K. Third year of survey data shows continuing benefits of Medicaid expansions for low-income childless adults in the U.S. J Gen Intern Med. 2018;33(9):1495–1497. doi: 10.1007/s11606-018-4537-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee H., Porell F.W. The effect of the Affordable Care Act Medicaid expansion on disparities in access to care and health status. Med Care Res Rev. 2020;77(5):461–473. doi: 10.1177/1077558718808709. [DOI] [PubMed] [Google Scholar]
- 12.Kobayashi L.C., Altindag O., Truskinovsky Y., Berkman L.F. Effects of the Affordable Care Act Medicaid expansion on subjective well-being in the US adult population, 2010–2016. Am J Public Health. 2019;109(9):1236–1242. doi: 10.2105/AJPH.2019.305164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller S., Wherry L.R. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. 2017;376(10):947–956. doi: 10.1056/NEJMsa1612890. [DOI] [PubMed] [Google Scholar]
- 14.Sommers B.D., Blendon R.J., Orav E.J., Epstein A.M. Changes in utilization and health among low-income adults after medicaid expansion or expanded private insurance. JAMA Intern Med. 2016;176(10):1501–1509. doi: 10.1001/jamainternmed.2016.4419. [DOI] [PubMed] [Google Scholar]
- 15.Zogg C.K., Scott J.W., Bhulani N., et al. Impact of Affordable Care Act insurance expansion on pre-hospital access to care: changes in adult perforated appendix admission rates after Medicaid expansion and the dependent coverage provision. J Am Coll Surg. 2019;228(1):29–43.e1. doi: 10.1016/j.jamcollsurg.2018.09.022. [DOI] [PubMed] [Google Scholar]
- 16.Miller S., Norman J., Wherry L.R. Medicaid and mortality: new evidence from linked survey and administrative data. Q J Econ. 2021;136(3):1783–1829. [Google Scholar]
- 17.Advaned Medical Reviews Medicaid expansion and managed care organizations explained. https://www.admere.com/amr-blog/medicaid-expansion-and-managed-care-organizations-explained Advaned Medical Reviews website.
- 18.Frean M., Gruber J., Sommers B.D. Premium subsidies, the mandate, and Medicaid expansion: coverage effects of the Affordable Care Act. J Health Econ. 2017;53:72–86. doi: 10.1016/j.jhealeco.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 19.Glied S, Chakraborty O, Russo T. How Medicaid expansion affected out-of-pocket health care spending for low-income families. Issue Brief (Commonw Fund). 2017;2017:1-9. [PubMed]
- 20.Hsu J., Qin X., Mirabelli M.C., Dana Flanders W. Medicaid expansion, health insurance coverage, and cost barriers to care among low-income adults with asthma: the Adult Asthma Call-Back Survey. J Asthma. 2020;0(0):1–10. doi: 10.1080/02770903.2020.1804577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahendraratnam N., Dusetzina S.B., Farley J.F. Prescription drug utilization and reimbursement increased following state medicaid expansion in 2014. J Manag Care Spec Pharm. 2017;23(3):355–363. doi: 10.18553/jmcp.2017.23.3.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ghosh A., Simon K., Sommers B.D. The effect of health insurance on prescription drug use among low-income adults: evidence from recent Medicaid expansions. J Health Econ. 2019;63:64–80. doi: 10.1016/j.jhealeco.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 23.Adamson B., Lipira L., Katz A.B. The impact of ACA and Medicaid expansion on progress toward UNAIDS 90-90-90 goals. Curr HIV/AIDS Rep. 2019;16:105–112. doi: 10.1007/s11904-019-00429-6. [DOI] [PubMed] [Google Scholar]
- 24.Mazurenko B.O., Balio C.P., Agarwal R., Carroll A.E., Menachemi N. The effects of Medicaid expansion under the ACA: a systematic review. Health Aff. 2018;37(6):944–950. doi: 10.1377/hlthaff.2017.1491. [DOI] [PubMed] [Google Scholar]
- 25.Kaiser Family Foundation Status of state Medicaid expansion decision: interactive map. 2021. https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/ Kaiser Family Foundation website.
- 26.Golberstein E., Gonzales G., Sommers B.D. California’s early ACA expansion increased coverage and reduced out-of-pocket spending for the state’s low-income population. Health Aff. 2015;34(10):1688–1694. doi: 10.1377/hlthaff.2015.0290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blewett L.A., Rivera Drew J.A., King M.L., Williams K.C.W. IPUMS health survey: National Health Interview Survey, version 6.4. Integrated Public Use Microdata Series. 2019. http://www.nhis.ipums.org National Health Interview Survey website.
- 28.Division of Health Interview Statistics, National Center for Health Statistics. Multiple imputation of family income and personal earnings in the National Health Interview Survey: methods and examples. 2018. Accessed December 1, 2021. https://www.cdc.gov/nchs/data/nhis/tecdoc17.pdf.
- 29.Reddel H.K., Taylor D.R., Bateman E.D., et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations—standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009;180(1):59–99. doi: 10.1164/rccm.200801-060ST. [DOI] [PubMed] [Google Scholar]
- 30.Karlson K.B., Holm A., Breen R. Comparing regression coefficients between same-sample nested models using logit and probit: a new method. Sociol Methodol. 2012;42(1):286–313. [Google Scholar]
- 31.Linden A., Karlson K.B. Using mediation analysis to identify causal mechanisms in disease management interventions. Heal Serv Outcomes Res Methodol. 2013;13(2-4):86–108. [Google Scholar]
- 32.Bloomberg G.R., Trinkaus K.M., Fisher E.B., Musick J.R., Strunk R.C. Hospital readmissions for childhood asthma: a 10-year metropolitan study. Am J Respir Crit Care Med. 2003;167(8):1068–1076. doi: 10.1164/rccm.2201015. [DOI] [PubMed] [Google Scholar]
- 33.Gushue C., Miller R., Sheikh S., et al. Gaps in health insurance coverage and emergency department use among children with asthma. J Asthma. 2019;56(10):1070–1078. doi: 10.1080/02770903.2018.1523929. [DOI] [PubMed] [Google Scholar]
- 34.Ferris T.G., Crain E.F., Oken E., Wang L., Clark S., Camargo C.A. Insurance and quality of care for children with acute asthma. Ambul Pediatr. 2001;1(5):267–274. doi: 10.1367/1539-4409(2001)001<0267:iaqocf>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 35.Magge H., Cabral H.J., Kazis L.E., Sommers B.D. Prevalence and predictors of underinsurance among low-income adults. J Gen Intern Med. 2013;28(9):1136–1142. doi: 10.1007/s11606-013-2354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.United States Food and Drug Administration FDA approves first generic Advair Diskus. 2019. https://www.fda.gov/news-events/press-announcements/fda-approves-first-generic-advair-diskus United States Food and Drug Administration website.
- 37.United States Food and Drug Administration FDA approves first generic of a commonly used albuterol inhaler to treat and prevent bronchospasm. 2020. United States Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-approves-first-generic-commonly-used-albuterol-inhaler-treat-and-prevent-bronchospasm
- 38.Stadhouders N., Kruse F., Tanke M., Koolman X., Jeurissen P. Effective healthcare cost-containment policies: a systematic review. Health Policy (New York) 2019;123(1):71–79. doi: 10.1016/j.healthpol.2018.10.015. [DOI] [PubMed] [Google Scholar]