Supplemental Digital Content is Available in the Text.
Key Words: triangular osteosynthesis, lumbopelvic fixation, sacral fracture, pelvic ring
Summary:
Triangular osteosynthesis is a technique used to stabilize posterior pelvic ring injuries. Conventional triangular fixation can be problematic for several reasons, including the need for advanced skill sets to place instrumentation, difficulty with pelvic reduction and placing the connecting construct, and prominent instrumentation. The purpose of this study is 2-fold: (1) to describe in detail a technique for lumbopelvic fixation using implants that are easy to connect, allow distraction for complex lumbosacral displacements, and are placed in a location minimizing soft tissue prominence and (2) to present our initial case series using this technique. We present a retrospective review of 18 consecutively treated patients with this technique. Inclusion criteria were patients with complete disruption through the sacrum or sacroiliac joint from blunt trauma (OTA/AO type C injuries). Outcomes included pelvic reduction/malreduction, wound healing, and complications. Fourteen patients underwent unilateral fixation (81%), and 4 patients underwent bilateral fixation (19%). All patients (18 of the 18) had a well-reduced pelvis after fixation. No patient (0%) required a return trip to the operating room for loss of reduction/malreduction, wound breakdown, or implant failure. This study presents an updated technique for a low-profile triangular osteosynthesis construct with straightforward application for unstable posterior pelvic ring injuries. This technique does not require rod bending, results in a consistently more recessed iliac screw and connecting rod, and can be used in a wide variety of unstable posterior pelvic ring injuries, including comminuted sacral fractures, L5/S1 facet fractures, and vertical shear injuries.
INTRODUCTION
Sacral fractures are often a component of pelvic ring injuries. Many are due to lower-energy lateral compression injuries (OTA/AO type A) and are considered stable sacral fractures. Others are caused by higher-energy mechanisms in lateral compression, anterior-posterior compression, vertical shear, or combined mechanisms with displacement (OTA/AO type B and type C injuries) and are considered unstable.1,2 These are associated with significant mortality and morbidity.3–5 After initial resuscitation, operative fixation of these injuries can be accomplished with various types of posterior fixation (eg, iliosacral/transsacral screws, transiliac plates, transiliac rod fixation, and lumbopelvic fixation)6–9 and anterior fixation {plates, external fixation, rami screws, or anterior subcutaneous pelvic fixation [internal fixator (INFIX)]}.
Triangular osteosynthesis was described by Schildhauer et al10 and consists of a unilateral lumbopelvic pedicle (P) screw construct combined with horizontal fixation using iliosacral/transsacral screws or a transiliac plate. This construct has been reported in biomechanical studies to have sufficient rigidity to enable early weight-bearing.11,12 The forces during ambulation with triangular fixation are transmitted directly from the lumbar spine into the ilium, which decreases force through the injured sacrum or sacroiliac (SI) joint.13 Indications for its use include comminuted sacral fractures with displacement, L5/S1 facet fractures, and vertical instability (either through the sacrum or through the SI joint). Triangular osteosynthesis can be used to help reduce complete posterior pelvic injuries of the SI joint or sacrum and supplement their fixation.14,15
Traditional triangular osteosynthesis is problematic for 3 reasons:
Owing to the difficult angles created in triangular osteosynthesis, the implants needed for connection between the L5 P screw and the iliac screw may require offset clamps, rod bending, or the use of polyaxial screws, which limit the reduction capability of the construct.
It is a relatively invasive procedure associated with wound healing disturbance rates as high as 26%.16,17 This is due to the prominence of the instrumentation in an area where soft tissue coverage is limited, and pressure is abundant when lying flat on one's back.
Occasionally, Schanz pins and a femoral distractor are needed to reduce displaced sacral U fractures, and the pins must be replaced with P screws after the reduction is secure to definitively stabilize the injury.
After using multiple different instrumentation systems for lumbopelvic/triangular fixation, we started using a system that uses Schanz pins and connectors that we had been using for thoraco-lumbar fractures (USS Fracture, Depuy Synthes, Johnson & Johnson). This system provided implants that could be inserted without offset clamps or the need for rod bending. The monoaxial P Schanz screws were also able to be used for reduction maneuvers without the use of other adjuncts such as traction pins or femoral distractors.
The purpose of this study is 2-fold: first, to describe in detail a technique for easier placement of lumbopelvic fixation that can be used for reduction of complex lumbosacral displacements and can be placed in a location to minimize soft tissue prominence and second, to present a case series of 18 consecutively treated patients with this technique and assess their reduction on postoperative radiographs. Outcomes included pelvic reduction, healing, and complications. Several case examples are also provided.
TECHNIQUE DESCRIPTION
Patient Positioning
The patient is placed in the prone position with a Kambin frame attachment on an OSI radiolucent table (Mizuho, Union City, CA) for sacral fractures or the spinal frame for the Jackson table (Mizuho) if hyperextension of the sacrum is desired for the reduction of a U-type or H-type sacral fracture. Before any incisions, fluoroscopy is used to ensure that adequate inlet/outlet, iliac oblique, and obturator outlet/inlet views are possible.
Approach
An approximately 6-cm lateral Wiltse incision is made from L5-S2 with exposure down to the posterior bony elements of L5 and S1. If both sides are involved, incisions are made bilaterally. The muscles are split and do not need to be elevated off the bone.
L5 Pedicle Screw Insertion
A perfect posterior-anterior (PA) image of the L5 vertebra is made with the C-arm when the superior end plate (SE) is flat to the coronal plane [Fig. 1A-(SE)] and the spinous process (SP) sits in the midline [Fig. 1A-(SP)] between the 2 Ps [Fig. 1A-(P)]. The Ps are equidistant from the SP, indicating a perfect PA image without any rotation. Start by drilling at the 3-o'clock position on the right P or the 9-o'clock position on the left P with a 3.2-mm drill bit. Fluoroscopy is used to place a 6 × 150-mm Schanz pin into the L5 P and vertebral body. This is checked with PA and lateral images during insertion (Figs. 1B, C).
FIGURE 1.
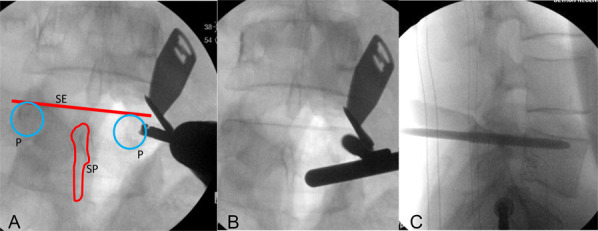
L5 P screw insertion—a perfect PA image of the L5 vertebra is made when the SE is flat to the coronal plane and the SP sits in the midline between the 2 P. The Ps are equidistant from the SP, indicating a perfect PA image without any rotation (A). Start by drilling at the 3-o'clock position on the right P or the 9-o'clock position on the left P with a 3.2-mm drill bit. Fluoroscopy is used to place a 6 × 150-mm Schanz pin into the L5 P and vertebral body. This is checked with PA and lateral images during insertion (B, C).
Iliac Screw Insertion
Next, another Schanz pin (6–8 mm in diameter, 150 mm in length, 55 mm in thread length) is placed from the sacrum, across the SI joint, and into the ilium. The starting point for the triangular osteosynthesis in this technique is not at the posterior superior iliac spine (PSIS) when used for sacral fractures. It is on the sacrum recessed into a dip on the posterolateral aspect of S1, as described by Arlet et al.18 First, the obturator outlet oblique view is used to visualize the starting point on the medial teardrop (Fig. 2A). The obturator inlet view confirms the angle of insertion in the axial plane and that the screw is in fact within the LC2 bony corridor as it crosses the SI joint (Figs. 2B, C). Finally, an iliac oblique view is used to ensure that the screw is above the sciatic notch (Fig. 2D). Final construct anterior-posterior (AP) and lateral fluoroscopic images can be seen in Figures 3A–D.
FIGURE 2.
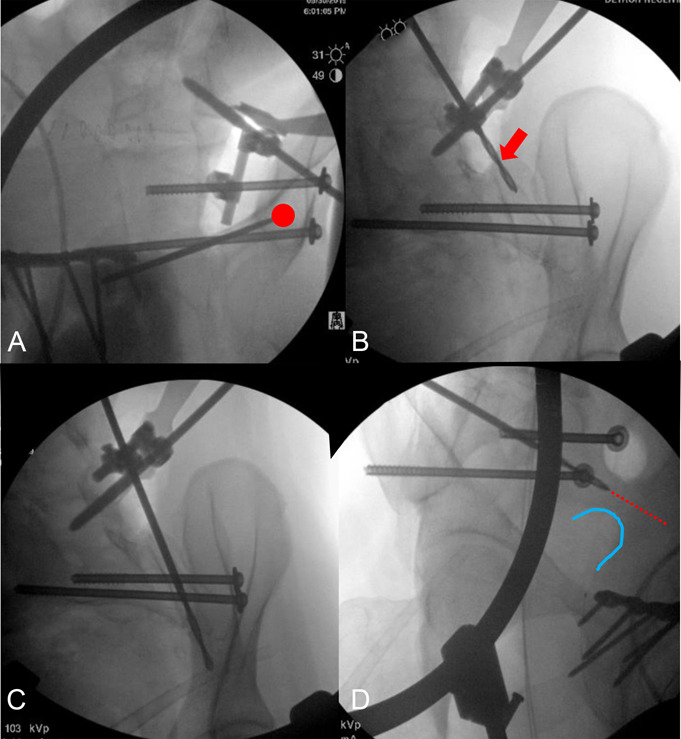
For the iliac screw, the starting point is just slightly medial in the teardrop on the obturator outlet view (A, red circle) and still on the sacral side of the SI joint on the inlet view (B, red arrow). The drill is passed across the SI joint (C) in a trajectory above the sciatic notch (red line over blue outline of sciatic notch) on the iliac oblique view (D).
FIGURE 3.
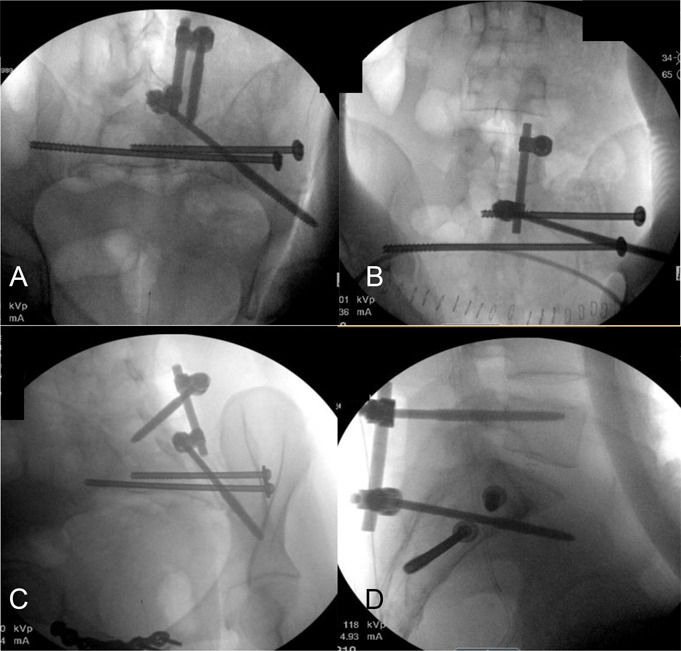
Final construct with inlet (A), outlet (B), iliac oblique (C), and lateral (D) views on fluoroscopy.
Connecting the Schanz Pins
Once in place, the L5 P Schanz pin and the iliac Schanz pin should make approximately a 45-degree angle with one another in the axial plane (Fig. 4A), and one should attempt to insert them parallel in the sagittal plane or close to parallel (Fig. 3D). The USS fracture connectors are then placed onto the pins, and a straight 6-mm spinal rod is then inserted, connecting the 2 pins (100 mm–150 mm in length) (Fig. 4B). As the USS connecting nuts are slid down the Schanz pins, they will align with each other when placed in opposite directions. The spinal rods should not require any bending and can be placed directly through the connecting nuts. The construct can then be distracted as needed (these injuries are usually superiorly displaced fractures of the hemipelvis) to reduce the hemipelvis to the stable sacral segment and tightened (Fig. 4C). The Schanz pins are then cut flush with the connecting heads, and the incision is closed (Fig. 4D). The final construct is a low-profile, triangular osteosynthesis that uses straight connecting rods for easier fixation compared with traditional lumbopelvic fixation techniques. The lower starting point of the Schanz pin on the sacrum is what eliminates the prominence of instrumentation that one finds when starting at the PSIS (this requires recession of the instrumentation into the PSIS). In bilateral cases, this technique is performed on both sides, and a cross-link can be used to increase stiffness. When reducing SI joints, one must start the iliac Schanz pin on the iliac side of the SI joint, but it can still be started below the crest to prevent prominence. Transsacral or SI screws are added to complete the construct and are inserted in the usual manner.
FIGURE 4.
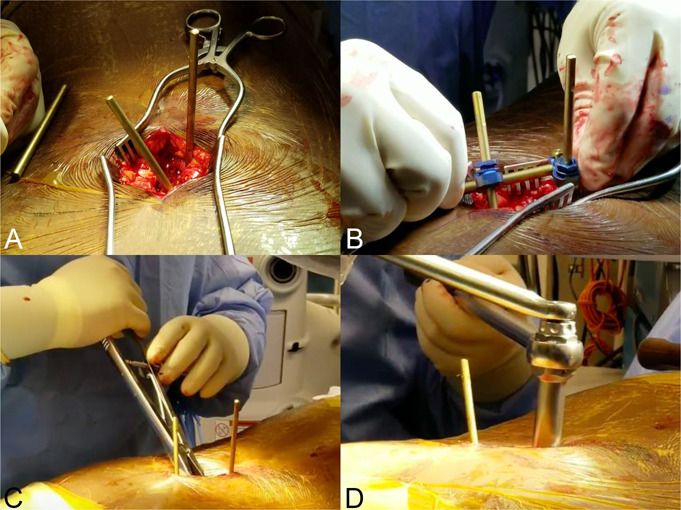
Posterior mini-open incision with L5 (top pin) and SI Schanz pins (bottom pin) in place. Note the Schanz pins are at approximately a 45-degree angle with one another in the axial plane (A). Placement of straight connecting rod between both pins (B). Tightening of construct to restore lumbosacral lordosis (C). Final cutting in situ of Schanz pins flush to connecting nut (D).
Postoperative Protocol
Patients are made toe-touch weight-bearing on the side of complete posterior pelvic ring disruption with progressive weight-bearing as tolerated and weight-bearing as tolerated on the contralateral side. Patients with bilateral complete disruption of the posterior pelvic ring are made weight-bearing for transfers and advanced to weight-bearing as tolerated over the next 2–3 weeks. Removal of the posterior instrumentation can be performed at 6 months postoperatively.
CASE SERIES
Methods
An institutional review board–approved retrospective study was performed on 18 consecutive patients who underwent triangular osteosynthesis for a sacral fracture/pelvic ring injury. In 14 patients, the technique was used to supplement an adequately reduced comminuted sacral fracture already stabilized with iliosacral/transsacral screws. In 4 patients, the technique was used as part of the initial reduction maneuver, including 2 sacral U fractures with kyphosis, one bilateral vertical shear SI joint dislocation, and one bilateral L5/S1 facet fracture extension. We included only patients with a complete disruption through either the sacrum or SI joint from blunt trauma (OTA/AO type C injuries). Select patients' preoperative and postoperative radiographs and preoperative and postoperative computed tomography slices of the posterior pelvic ring injury and subsequent reduction can be seen here (see Figures, Supplemental Digital Content 1, http://links.lww.com/JOT/B604). Postoperative pelvic reduction was measured on radiographs by the modified Keshishyan index19 and superior migration of the hemipelvis on the Bonesetter APP (https://detroitbonesetter.com/user/login, Detroit, Michigan) (see Figure, Supplemental Digital Content 2, http://links.lww.com/JOT/B605). Superior migration was measured on patients with unilateral vertical shear injury as the distance from the top of the iliac crest to a line parallel to the SE of L5 on preoperative AP radiographs. The percentage correction of the vertical shear achieved postoperatively was calculated as the ratio between the differences in the preoperative and postoperative distances of the iliac crest to the SE of L5 of each hemipelvis. This was calculated only on patients with unilateral vertical shear injuries (10 of the 18). The pelvic deformity index percentage correction was calculated using the method described by Vaidya et al20 and was calculated in all patients.
Results
Fourteen patients underwent unilateral fixation (81%), and 4 patients underwent bilateral fixation (19%). Each patient's injury pattern, fixation method, and OTA/AO classification is summarized (see Table, Supplemental Digital Content 3, http://links.lww.com/JOT/B606). In patients with a unilateral vertical shear injury (10 of the 18 patients), the percentage correction compared with the contralateral stable hemipelvis was on average 60.4% ± 39.6%. The average pelvic deformity percentage correction using the modified Keshishyan index was 74.2% ± 14.7%. A list of all patients' pelvic deformity indices, hemipelvis displacement, and their percentage correction is summarized (see Table, Supplemental Digital Content 4, http://links.lww.com/JOT/B607). No patient (0%) required a return trip to the operating room for loss of reduction, malreduction, wound breakdown, or implant failure. Four patients (22%) did experience urological injury at the time of initial injury, 2 of whom had extraperitoneal bladder rupture (one requiring surgical repair), one had a urethral injury not requiring surgery, and one had a scrotal degloving injury requiring surgical debridement and repair. In addition, 2 patients (11%) had postoperative suture abscesses after removal of the lumbopelvic instrumentation; however, these did not require additional trips to the operating room and resolved on their own with local dressing changes and a brief course of oral antibiotic therapy. All patients had at least 1 year of follow-up.
Case Examples
Three case examples displaying the use of the USS fracture system (DePuy Synthes, Johnson & Johnson) for triangular osteosynthesis in different injury patterns are presented further:
Case 1: APC3 Injury with Unilateral Sacral Fracture [OTA/AO 61C1.3(d)]
The first case is a 31- year-old man who experienced a motor vehicle accident. He first underwent pubic symphysis plating and placement of S1 iliosacral and S2 transsacral percutaneous screws. In a second surgery, he underwent right-sided lumbopelvic fixation (Fig. 5).
FIGURE 5.
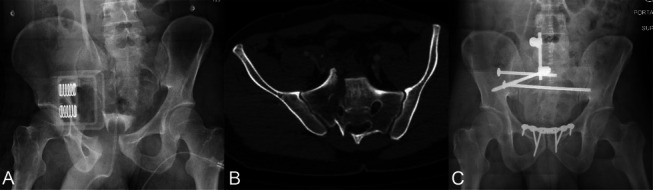
Example case 1, unilateral transforaminal comminuted sacral fracture—patient 6—AP pelvis in ED showing pelvic binder in place, which is stabilizing an APC3 type pelvis injury. There is a Denis type 2 vertical sacral fracture through the sacral foramen with vertical shear (A). Axial cut on computed tomography pelvis (bone window) showing an unstable fracture through the R sacral neuroforamen with external rotation of the R hemipelvis (B). Postoperative AP pelvis demonstrating a superior pubic symphysis plate, right side S1 iliosacral screw, right side S2 transsacral screw, and right side lumbopelvic fixation (C). This patient did not have implant removal during our follow-up period. ED, emergency department.
Case 2: Right-Sided Sacral Fracture with Extension into L5-S1 Facet and Contralateral Pubic Rami Fractures [OTA/AO 61C3.1(c)]
The second case is a 60--year-old woman who was crushed by a falling object at the hardware store. She first underwent anterior pelvic fixation with INFIX before undergoing right-sided triangular osteosynthesis. Her sacral fracture and posterior pelvic ring were unstable due to fracture extension into the L5-S1 facet (see Figure, Supplemental Digital Content 1B, http://links.lww.com/JOT/B604).
Case 3: Bilateral Superior Sacroiliac Joint Fracture Dislocations with Bilateral Pubic Rami Fractures [OTA/AO 61C3.1(j)]
The third case is a 27- year-old woman with additional left hip dislocation without acetabulum fracture after a motor vehicle accident. She first underwent bilateral lumbopelvic fixation to reduce her bilateral SI joints before undergoing iliosacral and transsacral screw placement and INFIX. Posterior instrumentation was removed at 12 months (see Figure, Supplemental Digital Content 1D, http://links.lww.com/JOT/B604).
DISCUSSION
Triangular osteosynthesis was first described in the literature by Schildhauer et al in 2006 for use as an adjunct to fixation in unstable posterior pelvic ring injuries. Their construct consisted of P screws into L4 and L5 connected by a contoured spinal rod to an iliac screw that began at the PSIS.10 The use of a low-profile lumbopelvic construct that crosses the SI joint was previously described by Arlet et al18 in the setting of neuromuscular scoliosis using maximum width fixation. Maximum width instrumentation consists of four 7 mm screws that form a W on the top-down view of the pelvis. Two screws each travel from the right and left outer iliac wings medially across the SI joint into the body of S1. The other 2 screws each traverse the right and left SI joints in the opposite direction with their starting point in a recessed spot on the posterolateral surface of S1 just medial to the PSIS and travel laterally into the body of the ilium. This is the same starting point that is used in the technique described in this study. Shah et al also described a technique that crosses the SI joint; however, they used a starting point at S2 that crosses the SI joint. In addition, they used polyaxial P screws that do not allow for direct reduction maneuvers and require adjuncts such as femoral distractors.21 To the knowledge of the authors, this deeper starting point on the sacrum at S1 that crosses the SI joint using monoaxial P Schanz screws has not been described for triangular osteosynthesis. This technique consistently results in the iliac Schanz pin ending in a position that does not require rod bending to connect it to the L5 P Schanz pin, and it places the entirety of the construct deeper within the body. Wound healing complications occur in up to 26% of patients with traditional fixation,16 and this new position hopefully mitigates this complication.
Other studies have shown that minimally invasive triangular osteosynthesis (MITO) can result in better wound healing outcomes.21–23 Many of these studies focused on the use of MITO for U-shaped and H-shaped sacral fractures and lumbopelvic dissociation type injuries. MITO may improve wound healing outcomes when compared with traditional triangular osteosynthesis; however, both techniques still have starting points on the ilium and are more superficial than the recessed sacral starting point described in this study. In addition, MITO necessitates that k-wires be swapped out for iliac screws,23 whereas our technique uses Schanz screws initially and does not require screw substitution. Our technique also makes it possible to reduce the fracture using the Schanz pins as joysticks rather than using adjunct reduction maneuvers or materials such as bilateral femoral traction pins to aid in sacral reduction.21
There are other treatment options for unstable posterior pelvic injuries besides lumbopelvic fixation. These include transiliac bars, posterior plate and screw constructs, horizontal iliac P screw constructs, and transiliac-transsacral screws. Transiliac bars travel between the ilia, posterior to the sacrum, and have been shown to offer greater stability than iliosacral or transsacral screws alone.24 Multiple authors have described plate and screw constructs for unstable sacral fractures, and these can be placed open or percutaneously, and they can span the ilia horizontally, cross the SI joint, or be placed vertically on the dorsal sacrum.25–29 Posterior iliac P screw constructs have been described to treat pathologic fractures of the sacrum and, when combined with iliosacral or transsacral screws, have similar strength compared with traditional posterior pelvic fixation.14 Finally, the strength of double S1 transiliac-transsacral screw fixation has been tested against triangular osteosynthesis in cadaveric biomechanical studies for transforaminal sacral fractures.12 The authors showed similar translational and rotational stiffness, suggesting this as an alternative posterior pelvic fixation; however, this technique has no reduction capabilities. All fixation strategies have their own indications, strengths, and weaknesses, and it is up to the treating surgeon to decide which technique to use given each clinical scenario.
This study was performed to describe an improvement on the technique of lumbopelvic fixation. Many surgeons had experienced implant choices that were cumbersome to connect the P screws to the iliac screws. The fixation remained prominent in an area that is prone to pressure and often leads to wound breakdown. Reduction maneuvers were best accomplished with a femoral distractor, and Schanz pins then replaced with P screw constructs as the definitive fixation. The technique described in this study solves all these issues with a simple implant connection, an easy reduction with a straight rod and distractor, and more low-profile instrumentation that is less likely to result in wound breakdown. Our methods are relevant because we have performed this technique consistently on a series of 18 consecutive patients with good success, no wound breakdowns or infections, and reductions that have persisted to union at least 1 year postoperatively. The limitations of this study are that these injuries are not common, so we have performed only 18 cases. Other limitations include those inherent to a retrospective case series and that the cases presented were performed by a single surgeon from a single level I trauma center.
CONCLUSION
This study presents an updated technique for a low-profile triangular osteosynthesis construct with easier application for unstable posterior pelvic ring injuries. This technique does not require rod bending and results in a consistently more recessed iliac screw and connecting rod. This technique can be used in a wide variety of unstable injuries, including comminuted sacral fractures, L5/S1 facet fractures, posterior pelvic vertical shear injuries, and SI joint fracture dislocations. This construct is biomechanically superior to iliosacral or transiliac screws alone.
Supplementary Material
Footnotes
The authors report no conflict of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jorthotrauma.com).
Contributor Information
Ryan Bray, Email: rcbray33@gmail.com.
Rahul Vaidya, Email: rahvaidya2012@gmail.com.
REFERENCES
- 1.Dalal SA, Burgess AR, Siegel JH, et al. Pelvic fracture in multiple trauma: classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J Trauma. 1989;29:981–1000; discussion 1000–1002. [PubMed] [Google Scholar]
- 2.Meinberg EG, Agel J, Roberts CS, et al. Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018;32(suppl 1):S1–S170. [DOI] [PubMed] [Google Scholar]
- 3.Latenser BA, Gentilello LM, Tarver AA, et al. Improved outcome with early fixation of skeletally unstable pelvic fractures. J Trauma. 1991;31:28–31. [DOI] [PubMed] [Google Scholar]
- 4.Lykomitros VA, Papavasiliou KA, Alzeer ZM, et al. Management of traumatic sacral fractures: a retrospective case-series study and review of the literature. Injury. 2010;41:266–272. [DOI] [PubMed] [Google Scholar]
- 5.Park YS, Baek SW, Kim HS, et al. Management of sacral fractures associated with spinal or pelvic ring injury. J Trauma Acute Care Surg. 2012;73:239–242. [DOI] [PubMed] [Google Scholar]
- 6.Nork SE, Jones CB, Harding SP, et al. Percutaneous stabilization of U-shaped sacral fractures using iliosacral screws: technique and early results. J Orthop Trauma. 2001;15:238–246. [DOI] [PubMed] [Google Scholar]
- 7.Griffin DR, Starr AJ, Reinert CM, et al. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: does posterior injury pattern predict fixation failure? J Orthop Trauma. 2006;20(1 suppl):S30–S36; discussion S36. [PubMed] [Google Scholar]
- 8.Suzuki T, Hak DJ, Ziran BH, et al. Outcome and complications of posterior transiliac plating for vertically unstable sacral fractures. Injury. 2009;40:405–409. [DOI] [PubMed] [Google Scholar]
- 9.Jones CB, Sietsema DL, Hoffmann MF. Can lumbopelvic fixation salvage unstable complex sacral fractures? Clin Orthop Relat Res. 2012;470:2132–2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schildhauer TA, Josten CH, Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing. J Orthop Trauma. 2006;20(1 suppl):S44–S51. [PubMed] [Google Scholar]
- 11.Schildhauer TA, Ledoux WR, Chapman JR, et al. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma. 2003;17:22–31. [DOI] [PubMed] [Google Scholar]
- 12.Min KS, Zamorano DP, Wahba GM, et al. Comparison of two-transsacral-screw fixation versus triangular osteosynthesis for transforaminal sacral fractures. Orthopedics. 2014;37:e754–e760. [DOI] [PubMed] [Google Scholar]
- 13.Hoffmann MF, Dudda M, Schildhauer TA. Unilaterale trianguläre lumbopelvine Stabilisierung: indikationen und Technik [in German]. Der Unfallchirurg. 2013;116:985–990. [DOI] [PubMed] [Google Scholar]
- 14.Vigdorchik JM, Jin X, Sethi A, et al. A biomechanical study of standard posterior pelvic ring fixation versus a posterior pedicle screw construct. Injury. 2015;46:1491–1496. [DOI] [PubMed] [Google Scholar]
- 15.Sagi HC. Technical aspects and recommended treatment algorithms in triangular osteosynthesis and spinopelvic fixation for vertical shear transforaminal sacral fractures. J Orthop Trauma. 2009;23:354–360. [DOI] [PubMed] [Google Scholar]
- 16.Tan GQ, He JL, Fu BS, et al. Lumbopelvic fixation for multiplanar sacral fractures with spinopelvic instability. Injury. 2012;43:1318–1325. [DOI] [PubMed] [Google Scholar]
- 17.Bellabarba C, Schildhauer TA, Vaccaro AR, et al. Complications associated with surgical stabilization of high-grade sacral fracture dislocations with spino-pelvic instability. Spine (Phila Pa 1976). 2006;31(11 suppl):S80–S88; discussion S104. [DOI] [PubMed] [Google Scholar]
- 18.Arlet V, Marchesi D, Papin P, et al. The “MW” sacropelvic construct: an enhanced fixation of the lumbosacral junction in neuromuscular pelvic obliquity. Eur Spine J. 1999;8:229–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lefaivre KA, Blachut PA, Starr AJ, et al. Radiographic displacement in pelvic ring disruption: reliability of 3 previously described measurement techniques. J Orthop Trauma. 2014;28:160–166. [DOI] [PubMed] [Google Scholar]
- 20.Vaidya R, Oliphant BW, Hudson I, et al. Sequential reduction and fixation for windswept pelvic ring injuries (LC3) corrects the deformity until healed. Int Orthop. 2013;37:1555–1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shah DS, Bates T, Fowler J, et al. Minimally invasive lumbopelvic fixation for unstable U-type sacral fractures. Cureus. 2019;11:e5621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams SK, Quinnan SM. Percutaneous lumbopelvic fixation for reduction and stabilization of sacral fractures with spinopelvic dissociation patterns. J Orthop Trauma. 2016;30:e318–e324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kanezaki S, Miyazaki M, Notani N, et al. Minimally invasive triangular osteosynthesis for highly unstable sacral fractures: technical notes and preliminary clinical outcomes. Medicine (Baltimore). 2019;98:e16004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gorczyca JT, Varga E, Woodside T, et al. The strength of iliosacral lag screws and transiliac bars in the fixation of vertically unstable pelvic injuries with sacral fractures. Injury. 1996;27:561–564. [DOI] [PubMed] [Google Scholar]
- 25.Pohlemann T, Gänsslen A, Tscherne H. Die sakrumfraktur [in German]. Unfallchirurg. 2000;103:769–786. [DOI] [PubMed] [Google Scholar]
- 26.Krappinger D, Larndorfer R, Struve P, et al. Minimally invasive transiliac plate osteosynthesis for type C injuries of the pelvic ring: a clinical and radiological follow-up. J Orthop Trauma. 2007;21:595–602. [DOI] [PubMed] [Google Scholar]
- 27.Albert MJ, Miller ME, MacNaughton M, et al. Posterior pelvic fixation using a transiliac 4.5-mm reconstruction plate: a clinical and biomechanical study. J Orthop Trauma. 1993;7:226–232. [DOI] [PubMed] [Google Scholar]
- 28.Hao T, Changwei Y, Qiulin Z. Treatment of posterior pelvic ring injuries with minimally invasive percutaneous plate osteosynthesis. Int Orthop. 2009;33:1435–1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Acklin YP, Marco G, Sommer C. Double locking plate fixation of sacral fractures in unstable pelvic ring C-type injuries. Oper Orthop Traumatol. 2015;27:74–79. Erratum in: Oper Orthop Traumatol. 2015;27:34. [DOI] [PubMed] [Google Scholar]


