Abstract
Background
In recent years, efforts have been made to implement virtual reality (VR) to support the delivery of poststroke upper extremity motor rehabilitation exercises. Therefore, it is important to review and analyze the existing research evidence of its effectiveness.
Objective
Through a systematic review and meta-analysis of randomized controlled trials, this study examined the effectiveness of using VR-supported exercise therapy for upper extremity motor rehabilitation in patients with stroke.
Methods
This study followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The CINAHL Plus, MEDLINE, Web of Science, Embase, and Cochrane Library databases were searched on December 31, 2021. Changes in outcomes related to impairments in upper extremity functions and structures, activity limitations, and participation restrictions in life situations from baseline to after intervention, after intervention to follow-up assessment, and baseline to follow-up assessment were examined. Standardized mean differences (SMDs) were calculated using a random-effects model. Subgroup analyses were performed to determine whether the differences in treatment outcomes depended on age, stroke recovery stage, VR program type, therapy delivery format, similarities in intervention duration between study groups, intervention duration in VR groups, and trial length.
Results
A total of 42 publications representing 43 trials (aggregated sample size=1893) were analyzed. Compared with the control groups that used either conventional therapy or no therapy, the intervention groups that used VR to support exercise therapy showed significant improvements in upper extremity motor function (Fugl-Meyer Assessment-Upper Extremity; SMD 0.45, 95% CI 0.21-0.68; P<.001), range of motion (goniometer; SMD 1.01, 95% CI 0.50-1.52; P<.001), muscle strength (Manual Muscle Testing; SMD 0.79, 95% CI 0.28-1.30; P=.002), and independence in day-to-day activities (Functional Independence Measure; SMD 0.23, 95% CI 0.06-0.40; P=.01, and modified Rankin Scale; SMD 0.57, 95% CI 0.01-1.12; P=.046). Significant subgroup differences were observed in hand dexterity (Box and Block Test), spasticity (Ashworth Scale or modified Ashworth Scale), arm and hand motor ability (Wolf Motor Function Test and Manual Function Test), hand motor ability (Jebsen Hand Function Test), and quality of life (Stroke Impact Scale). There was no evidence that the benefits of VR-supported exercise therapy were maintained after the intervention ended.
Conclusions
VR-supported upper extremity exercise therapy can be effective in improving motor rehabilitation results. Our review showed that of the 12 rehabilitation outcomes examined during the course of VR-based therapy, significant improvements were detected in 2 (upper extremity motor function and range of motion), and both significant and nonsignificant improvements were observed in another 2 (muscle strength and independence in day-to-day activities), depending on the measurement tools or methods used.
Trial Registration
PROSPERO CRD42021256826; https://tinyurl.com/2uarftbh
Keywords: virtual reality, stroke, rehabilitation, upper extremity, meta-analysis
Introduction
Upper extremity motor impairment after stroke significantly impedes the performance of daily activities and affects patients’ quality of life [1-6]. A major health goal for these patients is to recover their motor function and regain independence. Upper extremity therapeutic exercises are the main approach used to achieve this goal [7].
The physical therapist–led, face-to-face approach to delivering therapeutic exercises has been a common practice, but it can be costly and inconvenient owing to professional and institutional resource requirements. Therefore, alternative delivery protocols that leverage technology have been developed. In particular, the application of virtual reality (VR) technology in poststroke therapeutic exercise delivery has received considerable attention in recent years [8-11].
Although previous studies have reported the application of VR to deliver therapeutic exercise, a greater understanding of its effectiveness in poststroke functioning and health improvement is also required. Such knowledge can be acquired by reviewing the existing literature. Despite some reviews that have examined the effectiveness of using VR for upper extremity motor rehabilitation [12-17], there have been several new studies published in recent years; therefore, an updated review of the existing evidence is warranted. Moreover, previous reviews [12,16,17] have categorized study outcomes into three levels: (1) impairments in body functions (ie, problems with the physiological function of body systems) and structures (eg, extremities), (2) activity limitations (ie, difficulties in executing activities), and (3) restrictions on participation in life situations (ie, difficulties in involvement in life situations), according to the International Classification of Functioning, Disability, and Health Framework [18]. However, some study outcomes that have previously been grouped at the same level may not actually measure the same construct. For example, hand dexterity (as measured by the Box and Block Test [BBT]), and independence in day-to-day activities (as measured by the Functional Independence Measure [FIM]) have both been categorized as activity limitations, but are, in fact, 2 different types of outcomes. Therefore, it may not be appropriate to group the 2 measures together. Moreover, several recent reviews have mainly analyzed a small number of common outcomes [19-21], such as upper extremity motor function (as measured by the Fugl-Meyer Assessment-Upper Extremity [FMA-UE]) and hand dexterity (BBT), whereas relatively less attention has been paid to other outcomes (eg, range of motion [ROM] and muscle strength as measured by Manual Muscle Testing [MMT]), which may also be important for evaluating the effects of VR-supported exercise therapy on upper extremity motor recovery. Furthermore, previous reviews [15,16] performed subgroup analyses to demonstrate the effects of several moderating factors (eg, the stage of stroke recovery, the type of VR program, and the intervention duration) on the association between VR-supported exercise therapy and relevant study outcomes. However, similar to the aforementioned issues, the moderating effects on individual outcomes could not be accurately determined because outcomes that were actually related to different aspects were inappropriately grouped into the same category (eg, grouping grip strength and ROM into one category).
In view of the aforementioned limitations of previous reviews, we conducted this systematic review and meta-analysis to provide more evidence for the effectiveness of VR-supported exercise therapy for upper extremity motor rehabilitation in patients with stroke, particularly relating to outcomes in impairment of upper extremity functions and structures, activity limitations, and participation restrictions in life situations. In addition, we attempted to examine additional factors (eg, therapy delivery format) for their moderating effects on these 3 outcome categories.
Methods
This review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement and its associated checklist (Multimedia Appendix 1) [22] and was registered with PROSPERO (CRD42021256826).
Search Strategy
A literature search was performed on December 31, 2021, using the following databases: CINAHL Plus via EBSCO (from 1937 to present), MEDLINE via Ovid (from 1946 to present), Web of Science (from 1956 to present), Embase via Ovid (from 1974 to present), and the Cochrane Library (no date restriction). Medical Subject Headings and free-text search terms related to stroke, VR, upper extremity, and rehabilitation were used. Details of the search are presented in Multimedia Appendix 2.
Inclusion and Exclusion Criteria
Studies were included if (1) they were randomized controlled trials examining the effectiveness of VR-supported exercise therapy for upper extremity motor rehabilitation; (2) the intervention groups used either VR-supported exercise therapy alone or in combination with conventional therapy and the control groups used either conventional therapy alone or no therapy; (3) they examined adult patients with stroke (aged >18 years); (4) they assessed outcomes related to impairments in upper extremity functions or structures, activity limitations, and participation restrictions in life situations; and (5) they were written in English and published in peer-reviewed journals. Studies were excluded if (1) they did not focus on motor rehabilitation only for the upper extremities, as the independent effects of VR-supported exercise therapy on the upper extremities may be difficult to identify in combined studies; (2) they did not report mean and SD values for the changes in outcomes for effect size calculations; (3) the data could not be imputed based on the information available in the publication; (4) the data could not be obtained within 1 month of contacting the corresponding authors; or (5) they were review studies, case reports, or abstracts.
Study Selection
After removing duplicate publications from the search results, 2 authors (JC and TC) independently screened the titles and abstracts of the remaining publications and excluded those that were deemed irrelevant. The full texts of the potentially relevant publications were further reviewed to determine their eligibility for inclusion. The reference lists of the included articles and relevant review articles were manually searched to identify additional studies. Agreement between the authors on inclusion and exclusion decisions was assessed using the κ statistic, with κ values from 0.40 to 0.59, 0.60 to 0.74, and ≥0.75 considered as fair, good, and excellent agreement, respectively [23]. Any disagreements were resolved through discussions between the authors until a consensus was reached.
Data Extraction
JC and TC used a standardized form to independently extract data related to the characteristics of the trial, the attributes of the participants, the details of the intervention and control conditions, the outcomes examined in each trial, and the mean and SD values for changes in outcomes (ie, changes from baseline to after intervention, changes from after intervention to follow-up assessment, and changes from baseline to follow-up assessment). Data from the final follow-up assessment were used for the trials with multiple follow-up assessments. Any disagreements regarding data extraction were resolved through discussion between the authors until a consensus was reached.
Assessment of Risk of Bias
The risk of bias in the included trials was independently assessed by JC and TC using the Cochrane Collaboration tool [24]. The following aspects were assessed: random sequence generation; allocation concealment; blinding of participants and health care providers; blinding of outcome assessors; incomplete outcome data; selective reporting; and other sources of bias, including significant differences between study groups at baseline and different intervention durations between study groups.
Data Analysis
Outcomes were included in the meta-analysis if they were reported in at least 2 trials. For data from follow-up assessments, outcomes were included in the meta-analysis if they were reported in at least 2 follow-up assessments. We pooled the data across trials using random-effects models and calculated the standardized mean difference (SMD) for each outcome. Positive (or negative) SMDs indicated that the results favored the intervention (or control) condition. Unreported SDs were imputed according to the guidelines provided in the Cochrane Handbook for Systematic Reviews of Interventions [24]. Outliers in the meta-analysis were identified using studentized residuals (>3 in absolute value) and leave-one-out sensitivity analyses [25]. Heterogeneity across trials was assessed using Cochran Q test and I2 statistics (25%, 50%, and 75% were considered low, moderate, and high levels of heterogeneity, respectively) [26]. Egger regression test was used to measure the possibility of publication bias, with 2-tailed P values of <.05 indicating potential publication bias [27]. Comprehensive Meta-Analysis (version 3.0) was used to perform the meta-analysis.
Subgroup analysis was performed to investigate the factors that may moderate the effects of at least 1 trial in each subgroup. The following moderating factors were examined: age (below the median value of the participants’ ages vs equal to or above the median value of the participants’ ages), stage of recovery (subacute vs chronic stroke) [28], type of VR program (specialized programs designed for rehabilitation vs commercial games) [7], therapy delivery format (VR-supported exercise therapy alone compared with a control condition vs VR-supported exercise therapy+conventional therapy compared with a control condition), similarity of the intervention duration between the study groups (same intervention duration in both VR and control groups vs longer intervention duration in VR groups), intervention duration in VR groups (≤15 hours vs >15 hours) [15], and length of the trial (≤1 month vs >1 month and ≤2 months vs >2 months).
Assessment of Quality of Evidence
The quality of evidence for each outcome was assessed using the Grading of Recommendations Assessment, Development, and Evaluation approach [29]. For each outcome, the quality of evidence was downgraded from high by one level for each serious issue found in the domains of risk of bias, inconsistency, indirectness, imprecision, and publication bias.
Results
Study Selection Process
Figure 1 illustrates the study selection process. A total of 42 studies were identified as being eligible [8-10,30-68]. A study [52] had 2 groups of participants: individuals with subacute stroke and individuals with chronic stroke. Therefore, the study was divided into 2 trials (ie, Miclaus et al (1) [52] and Miclaus et al (2) [52]) for analysis. Altogether, 42 studies representing 43 trials (aggregated sample size=961 [intervention groups] and 932 [control groups]) were included in the final analysis. The agreement between the 2 authors on the inclusion and exclusion decisions was good at both the title and abstract screening (κ=0.64) and full-text reading steps (κ=0.61).
Figure 1.
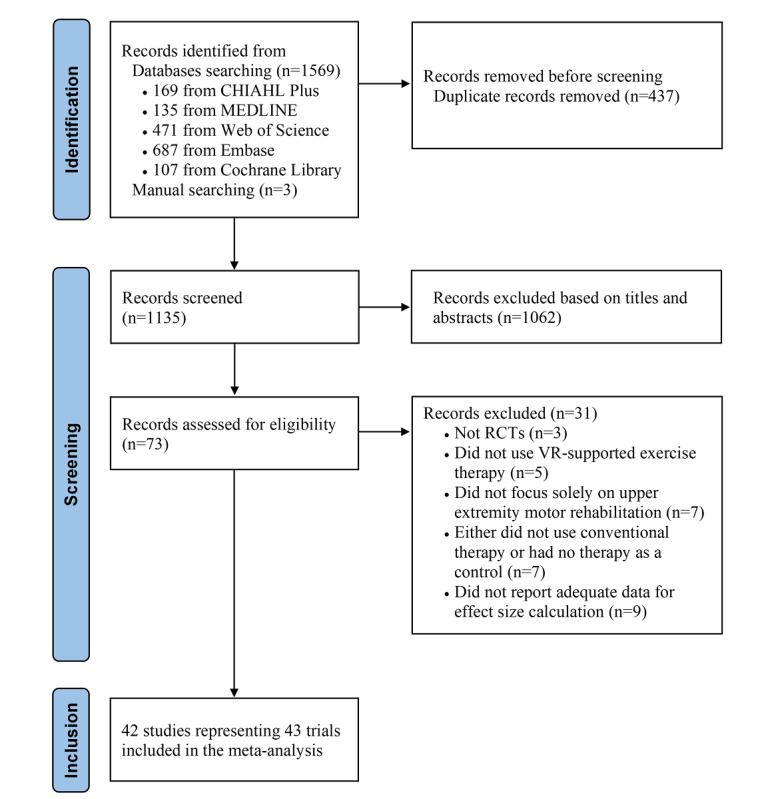
Study selection process. RCT: randomized controlled trial; VR: virtual reality.
Characteristics of the Included Trials
Table 1 summarizes the characteristics of the 43 included trials. Multimedia Appendix 3 [8-10,30-68] presents the characteristics of the participants and the study groups in each trial. Multimedia Appendix 4 [8-10,30-68] describes the outcome of each trial.
Table 1.
Summary of trial characteristics (N=43).
| Characteristics | Values | |
| Publication year | ||
|
|
2011 and before, n (%) | 3 (7) [43,55,56] |
|
|
2012-2016, n (%) | 17 (40) [10,37,38,42,44-48,50,51,57-60,64,66] |
|
|
2017-2021, n (%) | 23 (53) [8,9,30-36,39-41,49,52-54,61-63,65,67,68] |
|
|
Value, median (IQR) | 2017 (2014-2019) |
| Trial location, n (%) | ||
|
|
Asia | 25 (58) [31,32,34-37,39-41,44,46-50,54,57-60,62,63,65,66,68] |
|
|
Europe | 11 (26) [9,30,38,42,43,45,52,55,56,61] |
|
|
North America | 2 (5) [53,64] |
|
|
Oceania | 1 (2) [51] |
|
|
Africa | 1 (2) [67] |
|
|
South America | 1 (2) [33] |
|
|
Multiple locations | 2 (5) [8,10] |
| Sample size, median (range) | 33 (11-235) | |
| Participant age (years), median (range) | 60.36 (49.64-74.07)a | |
| Males (%), median (range) | 61.04 (36.36-86.00)b | |
| Ischemic stroke (%), median (range) | 70.83 (38.46-100)c | |
| Stroke recovery stage, n (%) | ||
|
|
Subacute stroke (≤6 months) | 22 (51) [8-10,30,31,34,36,37,41-44,46,49,52,57,59,61-63,65,68] |
|
|
Chronic stroke (>6 months) | 20 (47) [32,33,35,38-40,45,47,48,50-56,58,60,64,67] |
|
|
No adequate information was provided | 1 (2) [66] |
| Type of VRd program, n (%) | ||
|
|
Specialized program designed for rehabilitation | 27 (63) [8,9,34,35,38,40-43,45,46,48,50,52-58,61,63-66,68] |
|
|
Commercial game | 16 (37) [10,30-33,36,37,39,44,47,49,51,59,60,62,67] |
| Therapy delivery format, n (%) | ||
|
|
VR-supported exercise therapy alone compared with no therapy | 2 (5) [33,61] |
|
|
VR-supported exercise therapy alone compared with conventional therapy | 13 (30) [8,30,34,37,38,45,48,50,51,55,56,59,64] |
|
|
VR-supported exercise therapy+conventional therapy compared with conventional therapy | 28 (65) [9,10,31,32,35,36,39-44,46,47,49,52-54,57,58,60,62,63,65-68] |
| VR-supported exercise therapy delivery frequency, n (%) | ||
|
|
2 to 3 times per week | 11 (25) [38-40,45,47-49,53,59,60,67] |
|
|
>3 times per week | 27 (63) [8,9,30-37,41-44,46,51,52,54-56,61-63,65,66,68] |
|
|
No adequate information was provided | 5 (12) [10,50,57,58,64] |
| Duration of each VR-supported exercise therapy session, n (%) | ||
|
|
20 to 45 minutes per session | 23 (54) [30-32,34,37-41,45-50,53,54,57,58,60,63,67,68] |
|
|
>45 and ≤75 minutes per session | 16 (37) [9,10,33,35,42-44,51,52,55,56,59,62,65,66] |
|
|
No adequate information was provided | 4 (9) [8,36,61,64] |
| Intervention duration for VR groups, n (%) | ||
|
|
≤15 hours | 15 (35) [8,33,34,37,38,41,45,48,50-52,57,63,64] |
|
|
>15 hours | 23 (53) [9,30-32,35,39,42-44,46,47,49,54-56,58-62,65,66,68] |
|
|
No adequate information was provided | 5 (12) [10,36,40,53,67] |
| Trial length, n (%) | ||
|
|
2 weeks to 1 month | 31 (72) [8-10,31,33-38,41-44,46,50-58,62-66,68] |
|
|
>1 and ≤2 months | 10 (23) [30,32,39,45,47-49,60,61,67] |
|
|
>2 and ≤3 months | 2 (5) [40,59] |
| Time point of the final follow-up assessment after the end of intervention, n (%) | ||
|
|
1 month | 8 (19) [10,41,45,50,53-55,58] |
|
|
1.5 months | 1 (2) [38] |
|
|
3 months | 3 (7) [8,40,44] |
|
|
6 months | 2 (5) [30,51] |
|
|
No follow-up assessment | 29 (67) [9,31-37,39,42,43,46-49,52,56,57,59-68] |
aAnjum et al [34], Miclaus et al (1) [52], and Miclaus et al (2) [52] did not report the participants’ mean age.
bAnjum et al [34] did not report the number or ratio of male participants in their study.
cAin et al [32], Anjum et al [34], Crosbie et al [38], Ersoy and Iyigun [39], Jo et al [66], Levin et al [50], Mokhtar et al [67], Park et al [65], Shin et al [57], Standen et al [61], Xie et al [63], and Zondervan et al [64] did not report the participants’ stroke types.
dVR: virtual reality.
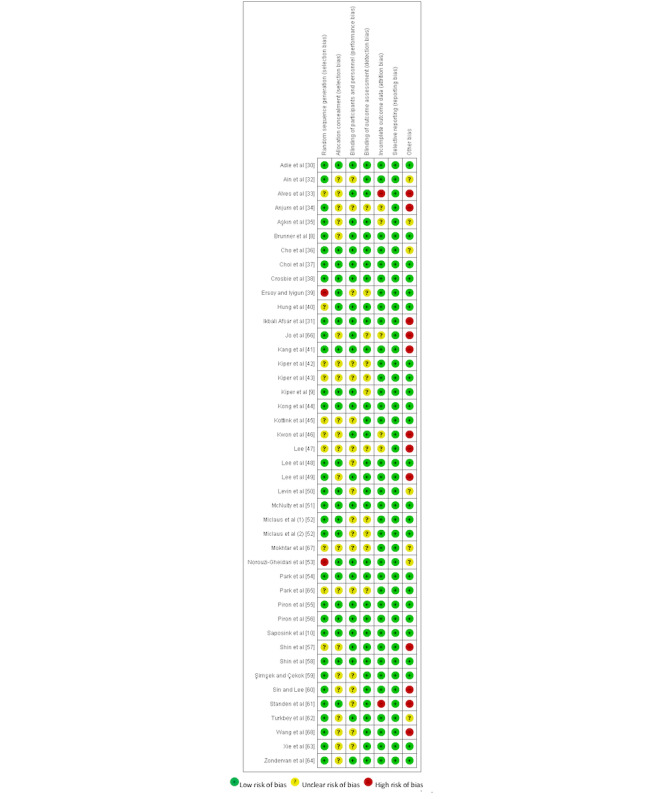
Risk of Bias
Figure 2 [8-10,30-68] shows the results of the risk of bias assessment for all 43 trials. Random sequence generation was assessed as adequate in 72% (31/43) of the trials. Allocation concealment was assessed as adequate in 51% (22/43) of the trials. Blinding of the participants or health care providers was reported in 58% (25/43) of the trials, and blinding of the outcome assessors was reported in 74% (32/43) of the trials. We assessed 84% (36/43) of the trials as free of bias in terms of incomplete outcome data. All the trials were assessed as having a low risk of reporting bias. Of the trials, 56% (24/43) had a low risk of bias in terms of significant differences between study groups at baseline or different intervention durations between study groups.
Figure 2.
Meta-analysis of the Effects of VR-Supported Exercise Therapy
Table 2 presents the results of the meta-analyses and the assessments of heterogeneity, publication bias, and quality of evidence. Forest plots for each outcome are presented in Multimedia Appendix 5 (Figures S1-S20 [8-10,30-68]).
Table 2.
Meta-analyses and assessments of heterogeneity, publication bias, and quality of evidence.
| Outcomes | Tools or methods used to assess the outcomes | Number of trials analyzed and number of participants involved | Standardized mean difference (95% CI) | Between-group difference, P value | Heterogeneity | Egger test, P value | Quality of evidence | |||||
|
|
|
|
|
|
Cochrane Q test | P value | I2 (%) |
|
|
|||
| Impairments in upper extremity functions and structures | ||||||||||||
|
|
(1) Upper extremity motor function | Fugl-Meyer Assessment-Upper Extremity | 28 [9,31-33,35-37,40-46,48,50-58, 60,63,65]; NVRa group=526, Ncontrol group=509 | 0.45 (0.21 to 0.68) |
<.001 | 83.72 | <.001 | 68 | .33 | Moderateb | ||
|
|
(1) Upper extremity motor function (after one outlier removedc) | Fugl-Meyer Assessment-Upper Extremity | 27 [9,31-33,35-37,40-46,48,50-58, 60,63,65]; NVR group=502, Ncontrol group=487 | 0.35 (0.19 to 0.50) |
<.001 | 35.23 | .11 | 26 | .84 | High | ||
|
|
(2) Grip strength | Dynamometer | 6 [10,36,37,41,65,67]; NVR group=157, Ncontrol group=155 | −0.002 (−0.30 to 0.30) |
.99 | 7.41 | .19 | 32 | .23 | Moderated | ||
|
|
(3) Spasticity | Ashworth Scale or modified Ashworth Scale | 6 [35,43,47,52,55]; NVR group=109, Ncontrol group=111 | 0.09 (−0.28 to 0.47) |
.63 | 8.68 | .12 | 42 | .35 | Moderated | ||
|
|
(4) Range of motion | Goniometer | 4 [52,54,60]; NVR group=56, Ncontrol group=56 | 1.01 (0.50 to 1.52) |
<.001 | 4.65 | .20 | 35 | .99 | Lowd | ||
|
|
(5) Stroke recovery stage | Brunnstrom stages of stroke recovery for upper extremity | 2 [35,62]; NVR group=28, Ncontrol group=29 | 0.26 (−0.26 to 0.79) |
.32 | 0.27 | .61 | 0 | N/Ae | Lowd | ||
|
|
(6) Muscle strength | Manual Muscle Testing | 3 [47,52]; NVR group=33, Ncontrol group=33 | 0.79 (0.28 to 1.30) |
.002 | 2.03 | .36 | 1 | .73 | Lowd | ||
|
|
(6) Muscle strength | Motricity Index | 2 [35,38]; NVR group=27, Ncontrol group=29 | 0.09 (−0.43 to 0.62) |
.73 | 0.88 | .35 | 0 | N/A | Lowd | ||
| Activity limitations | ||||||||||||
|
|
(7) Independence in day-to-day activities | Functional Independence Measure | 13 [8-10,31,42-44,47,52,56,59,62]; NVR group=406, Ncontrol group=395 | 0.23 (0.06 to 0.40) |
.01 | 16.01 | .19 | 25 | .03 | High | ||
|
|
(7) Independence in day-to-day activities | Barthel Index or modified Barthel Index | 11 [10,34,36,37,41,46,48,54,57,65,67]; NVR group=224, Ncontrol group=221 | 0.20 (−0.16 to 0.55) |
.28 | 30.54 | .001 | 67 | .59 | Moderateb | ||
|
|
(7) Independence in day-to-day activities | Modified Rankin Scale | 2 [52]; NVR group=26, Ncontrol group=26 | 0.57 (0.01 to 1.12) |
.046 | 0.55 | .46 | 0 | N/A | Lowd | ||
|
|
(8) Hand dexterity | Box and Block Test | 13 [8,10,31,32,35,37,41,48,51,53,60,62,64]; NVR group=297, Ncontrol group=286 | 0.26 (−0.08 to 0.60) |
.13 | 42.63 | <.001 | 72 | .33 | Moderateb | ||
|
|
(9) Arm and hand motor ability | Action Research Arm Test | 6 [8,30,38,44,45,64]; NVR group=238, Ncontrol group=238 | −0.03 (−0.21 to 0.15) |
.76 | 2.08 | .84 | 0 | .22 | High | ||
|
|
(9) Arm and hand motor ability | Wolf Motor Function Test task completion time | 9 [10,40,50,51,54,61,62,66,68]; NVR group=174, Ncontrol group=170 | 0.15 (−0.06 to 0.37) |
.16 | 7.19 | .52 | 0 | .28 | Moderated | ||
|
|
(9) Arm and hand motor ability | Wolf Motor Function Test task performance score | 7 [39,40,50,54,62,66,68]; NVR group=93, Ncontrol group=91 | 0.36 (−0.07 to 0.79) |
.10 | 11.97 | .06 | 50 | .28 | Lowd,f | ||
|
|
(9) Arm and hand motor ability | Manual Function Test | 4 [37,46,48,49]; NVR group=51, Ncontrol group=51 | 0.20 (−0.37 to 0.78) |
.49 | 6.28 | .10 | 52 | .70 | Lowd,f | ||
|
|
(10) Hand motor ability | Jebsen Hand Function Test | 4 [36,41,58,65]; NVR group=70, Ncontrol group=67 | 0.90 (−0.42 to 2.22) |
.18 | 36.25 | <.001 | 92 | .65 | Very lowb,d | ||
| Participation restrictions in life situations | ||||||||||||
|
|
(11) Quality of life | Stroke Impact Scale total score | 3 [30,53,54]; NVR group=138, Ncontrol group=140 | 0.13 (−0.41 to 0.66) |
.65 | 4.26 | .12 | 53 | .12 | Very lowd,f | ||
|
|
(11) Quality of life | Stroke Impact Scale hand function score | 2 [10,44]; NVR group=104, Ncontrol group=105 | −0.04 (−0.31 to 0.23) |
.78 | 0.89 | .35 | 0 | N/A | Lowd | ||
|
|
(12) Upper extremity use in daily life | Motor Activity Log quality of movement score | 6 [40,50,51,53,61,64]; NVR group=71, Ncontrol group=68 | 0.50 (−0.05 to 1.05) |
.08 | 11.78 | .04 | 58 | .31 | Lowd,f | ||
|
|
(12) Upper extremity use in daily life | Motor Activity Log amount of use score | 5 [40,50,53,61,64]; NVR group=50, Ncontrol group=48 | 0.27 (−0.13 to 0.67) |
.18 | 3.36 | .50 | 0 | .91 | Moderated | ||
aVR: virtual reality.
bDowngraded owing to a high level of heterogeneity.
cShin et al [58] was removed.
dDowngraded owing to an inadequate sample size.
eN/A: not applicable.
fDowngraded owing to a moderate level of heterogeneity.
Effects on Outcomes Related to Impairments in Upper Extremity Functions and Structures
Compared with the control condition, the use of VR-supported exercise therapy was associated with significant improvements in upper extremity motor function (FMA-UE; SMD 0.45, 95% CI 0.21-0.68; P<.001 or SMD 0.35, 95% CI 0.19-0.50; P<.001 after outlier [58] removal), upper extremity ROM (goniometer; SMD 1.01, 95% CI 0.50-1.52; P<.001), and upper extremity muscle strength (MMT; SMD 0.79, 95% CI 0.28-1.30; P=.002).
No significant improvements were observed in grip strength (dynamometer), spasticity (ie, involuntary muscle contraction, stiffening, and tightening upon the movement of body parts; Ashworth Scale [AS] or Modified AS [mAS]), upper extremity stroke recovery stage (Brunnstrom Stages of Stroke Recovery for Upper Extremity), and upper extremity muscle strength (Motricity Index).
Effects on Outcomes Related to Activity Limitation
Compared with the control condition, the use of VR-supported exercise therapy was associated with significant improvements in independence in day-to-day activities (FIM; SMD 0.23, 95% CI 0.06-0.40; P=.01 and modified Rankin Scale scores; SMD 0.57, 95% CI 0.01-1.12; P=.046). However, no significant association was observed with the Barthel Index or modified Barthel Index.
No significant improvements were detected in hand dexterity (BBT), arm and hand motor ability (Action Research Arm Test [ARAT], Wolf Motor Function Test [WMFT], and Manual Function Test [MFT]), and hand motor ability (Jebsen Hand Function Test [JHFT]).
Effects on Outcomes Related to Participation Restrictions in Life Situations
No significant improvements were detected in quality of life (Stroke Impact Scale [SIS]) or upper extremity use in daily life (Motor Activity Log).
Subgroup Analyses
Overview
The subgroup analyses for outcomes examined in at least 10 trials are presented in this paper (Tables 3-6). For outcomes that were examined in <10 trials, the subgroup analyses are presented in Multimedia Appendix 6 (Tables S1-S16 [8-10,30-68]).
Table 3.
Subgroup analyses of upper extremity motor function as assessed by the Fugl-Meyer Assessment-Upper Extremity.
| Moderating factors | Number of trials analyzed and number of participants involved | Standardized mean difference (95% CI) | Between-group difference, P value | Subgroup difference, P value | |||||
| Age (years) | |||||||||
|
|
Younger (<60.36) | 14 [32,33,35,40,41,44,46,50,51,53,54,57,58,63]; NVRa group=222, Ncontrol group=213 | 0.54 (0.09 to 1.00) | .02 | .43 | ||||
|
|
Older (≥60.36) | 12 [9,31,36,37,42,43,45,48,55,56,60,65]; NVR group=278, Ncontrol group=270 | 0.35 (0.18 to 0.52) | <.001 | .43 | ||||
| Stroke recovery stage | |||||||||
|
|
Subacute stroke | 13 [9,31,36,37,41-44,46,52,57,63,65]; NVR group=273, Ncontrol group=266 | 0.27 (0.04 to 0.50) | .02 | .16 | ||||
|
|
Chronic stroke | 15 [32,33,35,40,45,48,50-56,58,60]; NVR group=253, Ncontrol group=243 | 0.60 (0.21 to 1.00) | .003 | .16 | ||||
| Type of VR program used | |||||||||
|
|
Specialized program designed for rehabilitation | 20 [9,35,40-43,45,46,48,50,52-58,63,65]; NVR group=371, Ncontrol group=364 | 0.44 (0.15 to 0.74) | .003 | .90 | ||||
|
|
Commercial game | 8 [31-33,36,37,44,51,60]; NVR group=155, Ncontrol group=145 | 0.47 (0.10 to 0.85) | .01 | .90 | ||||
| Therapy delivery format | |||||||||
|
|
VR-supported exercise therapy alone compared with no therapy | 1 [33]; NVR group=17, Ncontrol group=10 | 1.10 (0.27 to 1.94) | .01 | .12 | ||||
|
|
VR-supported exercise therapy alone compared with conventional therapy | 7 [37,45,48,50,51,55,56]; NVR group=103, Ncontrol group=100 | 0.25 (−0.03 to 0.53) | .08 | .12 | ||||
|
|
VR-supported exercise therapy+conventional therapy compared with conventional therapy | 20 [9,31,32,35,36,40-44,46,52-54,57,58,60,63,65]; NVR group=406, Ncontrol group=399 | 0.50 (0.20 to 0.81) | .001 | .12 | ||||
| Similarity of intervention duration between groups | |||||||||
|
|
Same intervention duration in both VR and control groups | 21 [9,32,37,40-46,48,50-52,54-56,58,63,65]; NVR group=424, Ncontrol group=418 | 0.44 (0.16 to 0.73) | .002 | .14 | ||||
|
|
Longer intervention duration in VR groups | 4 [31,33,57,60]; NVR group=63, Ncontrol group=50 | 0.81 (0.42 to 1.20) | <.001 | .14 | ||||
| Intervention duration in VR groups (hours) | |||||||||
|
|
≤15 | 11 [33,37,41,45,48,50-52,57,63]; NVR group=128, Ncontrol group=119 | 0.37 (0.05 to 0.69) | .02 | .43 | ||||
|
|
>15 | 14 [9,31,32,35,42-44,46,54-56,58,60,65]; NVR group=360, Ncontrol group=353 | 0.56 (0.21 to 0.91) | .002 | .43 | ||||
| Trial length | |||||||||
|
|
2 weeks to 1 month | 23 [9,31,33,35-37,41-44,46,50-58,63,65]; NVR group=445, Ncontrol group=428 | 0.43 (0.16 to 0.69) | .002 | .47 | ||||
|
|
>1 and ≤2 months | 4 [32,45,48,60]; NVR group=64, Ncontrol group=65 | 0.68 (0.18 to 1.18) | .01 | .47 | ||||
|
|
>2 and ≤3 months | 1 [40]; NVR group=17, Ncontrol group=16 | 0.16 (−0.53 to 0.84) | .65 | .47 | ||||
aVR: virtual reality.
Significant subgroup differences were observed in the following outcomes: hand dexterity (BBT), spasticity (AS or mAS), arm and hand motor ability (WMFT task performance score and MFT), hand motor ability (JHFT), and quality of life (SIS total score). The details of this process are presented in the following sections.
Table 5.
Subgroup analyses of independence in day-to-day activities as assessed by the Functional Independence Measure.
| Moderating factors | Number of trials analyzed and number of participants involved | Standardized mean difference (95% CI) | Between-group difference, P value | Subgroup difference, P value | |
| Age (years) | |||||
|
|
Younger (<60.36) | 2 [44,59]; NVRa group=53, Ncontrol group=57 | 0.36 (−0.54 to 1.26) | .44 | .70 |
|
|
Older (≥60.36) | 9 [8-10,31,42,43,47,56,62]; NVR group=327, Ncontrol group=312 | 0.18 (0.02 to 0.33) | .03 | .70 |
| Stroke recovery stage | |||||
|
|
Subacute stroke | 10 [8-10,31,42-44,52,59,62]; NVR group=352, Ncontrol group=344 | 0.26 (0.05 to 0.47) | .02 | .79 |
|
|
Chronic stroke | 3 [47,52,56]; NVR group=54, Ncontrol group=51 | 0.20 (−0.19 to 0.58) | .31 | .79 |
| Type of VR program used | |||||
|
|
Specialized program designed for rehabilitation | 7 [8,9,42,43,52,56]; NVR group=246, Ncontrol group=236 | 0.28 (0.06 to 0.51) | .02 | .58 |
|
|
Commercial game | 6 [10,31,44,47,59,62]; NVR group=160, Ncontrol group=159 | 0.18 (−0.10 to 0.46) | .21 | .58 |
| Therapy delivery format | |||||
|
|
VR-supported exercise therapy alone compared with conventional therapy | 3 [8,56,59]; NVR group=109, Ncontrol group=103 | 0.27 (−0.18 to 0.73) | .23 | .86 |
|
|
VR-supported exercise therapy+conventional therapy compared with conventional therapy | 10 [9,10,31,42-44,47,52,62]; NVR group=297, Ncontrol group=292 | 0.23 (0.04 to 0.42) | .02 | .86 |
| Similarity of intervention duration between groups | |||||
|
|
Same intervention duration in both VR and control groups | 11 [8-10,42-44,52,56,59,62]; NVR group=380, Ncontrol group=372 | 0.25 (0.05 to 0.44) | .01 | .96 |
|
|
Longer intervention duration in VR groups | 2 [31,47]; NVR group=26, Ncontrol group=23 | 0.23 (−0.34 to 0.79) | .43 | .96 |
| Intervention duration in VR groups (hours) | |||||
|
|
≤15 | 3 [8,52]; NVR group=88, Ncontrol group=84 | 0.47 (−0.24 to 1.17) | .20 | .62 |
|
|
>15 | 9 [9,31,42-44,47,56,59,62]; NVR group=247, Ncontrol group=241 | 0.28 (0.10 to 0.46) | .002 | .62 |
| Trial length | |||||
|
|
2 weeks to 1 month | 11 [8-10,31,42-44,52,56,62]; NVR group=379, Ncontrol group=366 | 0.19 (0.02 to 0.35) | .03 | .14 |
|
|
>1 and ≤2 months | 1 [47]; NVR group=7, Ncontrol group=7 | 0.32 (−0.74 to 1.37) | .56 | .14 |
|
|
>2 and ≤3 months | 1 [59]; NVR group=20, Ncontrol group=22 | 0.84 (0.21 to 1.47) | .01 | .14 |
aVR: virtual reality.
Table 6.
Subgroup analyses of independence in day-to-day activities as assessed by the Barthel Index or modified Barthel Index.
| Moderating factors | Number of trials analyzed and number of participants involved | Standardized mean difference (95% CI) | Between-group difference, P value | Subgroup difference, P value | |||||
| Age (years) | |||||||||
|
|
Younger (<60.36) | 6 [34,41,46,54,57,67]; NVRa group=96, Ncontrol group=94 | 0.38 (−0.24 to 1.00) | .23 | .33 | ||||
|
|
Older (≥60.36) | 5 [10,36,37,48,65]; NVR group=128, Ncontrol group=127 | 0.04 (−0.25 to 0.33) | .80 | .33 | ||||
| Stroke recovery stage | |||||||||
|
|
Subacute stroke | 8 [10,34,36,37,41,46,57,65]; NVR group=169, Ncontrol group=165 | 0.19 (−0.22 to 0.60) | .36 | .97 | ||||
|
|
Chronic stroke | 3 [48,54,67]; NVR group=55, Ncontrol group=56 | 0.17 (−0.73 to 1.08) | .71 | .97 | ||||
| Type of VR program | |||||||||
|
|
Specialized program designed for rehabilitation | 7 [34,41,46,48,54,57,65]; NVR group=101, Ncontrol group=99 | 0.18 (−0.36 to 0.72) | .52 | .93 | ||||
|
|
Commercial game | 4 [10,36,37,67]; NVR group=123, Ncontrol group=122 | 0.21 (−0.31 to 0.74) | .43 | .93 | ||||
| Therapy delivery format | |||||||||
|
|
VR-supported exercise therapy alone compared with conventional therapy | 3 [34,37,48]; NVR group=43, Ncontrol group=43 | 0.23 (−1.04 to 1.49) | .73 | .96 | ||||
|
|
VR-supported exercise therapy+conventional therapy compared with conventional therapy | 8 [10,36,41,46,54,57,65,67]; NVR group=181, Ncontrol group=178 | 0.19 (−0.15 to 0.52) | .27 | .96 | ||||
| Similarity of intervention duration between groups | |||||||||
|
|
Same intervention duration in both VR and control groups | 7 [10,34,37,41,48,54,65]; NVR group=160, Ncontrol group=159 | 0.10 (−0.38 to 0.58) | .69 | .72 | ||||
|
|
Longer intervention duration in VR groups | 2 [46,57]; NVR group=22, Ncontrol group=20 | 0.24 (−0.37 to 0.85) | .45 | .72 | ||||
| Intervention duration in VR groups (hours) | |||||||||
|
|
≤15 | 5 [34,37,41,48,57]; NVR group=64, Ncontrol group=61 | 0.06 (−0.80 to 0.91) | .90 | .69 | ||||
|
|
>15 | 3 [46,54,65]; NVR group=47, Ncontrol group=48 | 0.25 (−0.16 to 0.66) | .23 | .69 | ||||
| Trial length | |||||||||
|
|
2 weeks to 1 month | 9 [10,34,36,37,41,46,54,57,65]; NVR group=181, Ncontrol group=178 | 0.17 (−0.20 to 0.54) | .37 | .91 | ||||
|
|
>1 and ≤2 months | 2 [48,67]; NVR group=43, Ncontrol group=43 | 0.26 (−1.15 to 1.66) | .72 | .91 | ||||
aVR: virtual reality.
Age
Older patients (SMD 0.47, 95% CI 0.01-0.92; P=.05) showed greater improvements in arm and hand motor ability (MFT) than younger patients (SMD −0.52, 95% CI −1.30 to 0.26; P=.19); the difference between the groups was significant (P=.03; Table S10 in Multimedia Appendix 6).
Moreover, younger patients (SMD 0.49, 95% CI −0.11 to 1.10; P=.11) showed greater improvements in quality of life (SIS total score) than older patients (SMD −0.20, 95% CI −0.46 to 0.06; P=.13), and the difference between the groups was significant (P=.04; Table S13 in Multimedia Appendix 6).
Stroke Recovery Stage
Patients with subacute stroke (SMD 1.13, 95% CI 0.50-1.76; P<.001) showed greater improvements in arm and hand motor ability (WMFT task performance score) than those with chronic stroke (SMD −0.07, 95% CI −0.44 to 0.31; P=.72), and the difference between the groups was significant (P=.001; Table S9 in Multimedia Appendix 6).
In addition, patients with chronic stroke (SMD 3.12, 95% CI 2.26-3.98; P<.001) showed greater improvements in hand motor ability (JHFT) than patients with subacute stroke (SMD 0.25, 95% CI −0.16 to 0.67; P=.24); the difference between the groups was significant (P<.001; Table S11 in Multimedia Appendix 6).
Moreover, patients with chronic stroke (SMD 0.49, 95% CI −0.11 to 1.10; P=.11) showed greater improvements in quality of life (SIS total score) than patients with subacute stroke (SMD −0.20, 95% CI −0.46 to 0.06; P=.13), and the difference between the groups was significant (P=.04; Table S13 in Multimedia Appendix 6).
Type of VR Program Used
The use of specialized programs designed for rehabilitation (SMD 0.49, 95% CI −0.11 to 1.10; P=.11) showed greater improvements in quality of life (SIS total score) than those using commercial games (SMD −0.20, 95% CI −0.46 to 0.06; P=.13); the difference between the groups was significant (P=.04; Table S13 in Multimedia Appendix 6).
Therapy Delivery Format
The use of a combination of VR-supported exercise therapy and conventional therapy (SMD 0.52, 95% CI −0.01 to 1.05; P=.052) was associated with greater improvements in hand dexterity (BBT) than the use of VR-supported exercise therapy alone (SMD −0.08, 95% CI −0.34 to 0.18; P=.56); the subgroup difference was significant (P=.046; Table 4).
Table 4.
Subgroup analyses of hand dexterity as assessed by the Box and Block Test.
| Moderating factors | Number of trials analyzed and number of participants involved | Standardized mean difference (95% CI) | Between-group difference, P value | Subgroup difference, P value | |
| Age (years) | |||||
|
|
Younger (<60.36) | 6 [32,35,41,51,53,64]; NVRa group=94, Ncontrol group=93 | 0.12 (−0.38 to 0.62) | .64 | .47 |
|
|
Older (≥60.36) | 7 [8,10,31,37,48,60,62]; NVR group=203, Ncontrol group=193 | 0.38 (−0.11 to 0.87) | .13 | .47 |
| Stroke recovery stage | |||||
|
|
Subacute stroke | 6 [8,10,31,37,41,62]; NVR group=184, Ncontrol group=174 | 0.11 (−0.27 to 0.48) | .58 | .44 |
|
|
Chronic stroke | 7 [32,35,48,51,53,60,64]; NVR group=113, Ncontrol group=112 | 0.38 (−0.20 to 0.95) | .20 | .44 |
| Type of VR program | |||||
|
|
Specialized program designed for rehabilitation | 6 [8,35,41,48,53,64]; NVR group=123, Ncontrol group=119 | −0.03 (−0.28 to 0.22) | .81 | .09 |
|
|
Commercial game | 7 [10,31,32,37,51,60,62]; NVR group=174, Ncontrol group=167 | 0.54 (−0.06 to 1.14) | .08 | .09 |
| Therapy delivery format | |||||
|
|
VR-supported exercise therapy alone compared with conventional therapy | 5 [8,37,48,51,64]; NVR group=115, Ncontrol group=109 | −0.08 (−0.34 to 0.18) | .56 | .046 |
|
|
VR-supported exercise therapy+conventional therapy compared with conventional therapy | 8 [10,31,32,35,41,53,60,62]; NVR group=182, Ncontrol group=177 | 0.52 (−0.01 to 1.05) | .052 | .046 |
| Similarity of intervention duration between groups | |||||
|
|
Same intervention duration in both VR and control groups | 9 [8,10,32,37,41,48,51,62,64]; NVR group=233, Ncontrol group=224 | 0.07 (−0.25 to 0.40) | .66 | .002 |
|
|
Longer intervention duration in VR groups | 2 [31,60]; NVR group=37, Ncontrol group=33 | 1.34 (0.61 to 2.07) | <.001 | .002 |
| Intervention duration in VR groups (hours) | |||||
|
|
≤15 | 6 [8,37,41,48,51,64]; NVR group=127, Ncontrol group=120 | −0.10 (−0.35 to 0.15) | .45 | <.001 |
|
|
>15 | 5 [31,32,35,60,62]; NVR group=90, Ncontrol group=87 | 0.92 (0.35 to 1.49) | .002 | <.001 |
| Trial length | |||||
|
|
2 weeks to 1 month | 10 [8,10,31,35,37,41,51,53,62,64]; NVR group=241, Ncontrol group=231 | 0.02 (−0.22 to 0.26) | .84 | .049 |
|
|
>1 and ≤2 months | 3 [32,48,60]; NVR group=56, Ncontrol group=55 | 0.97 (0.06 to 1.89) | .04 | .049 |
aVR: virtual reality.
Moreover, those using a combination of VR-supported exercise therapy and conventional therapy (SMD 0.49, 95% CI −0.11 to 1.10; P=.11) showed greater improvements in quality of life (SIS total score) than those using VR-supported exercise therapy alone (SMD −0.20, 95% CI −0.46 to 0.06; P=.13), and the difference between the groups was significant (P=.04; Table S13 in Multimedia Appendix 6).
Similarity of Intervention Duration Between Groups
Longer intervention durations for the VR groups (SMD 1.34, 95% CI 0.61-2.07; P<.001) were associated with greater improvements in hand dexterity (BBT) than equal intervention durations between the groups (SMD 0.07, 95% CI −0.25 to 0.40; P=.66); the subgroup difference was significant (P=.002; Table 4).
In addition, longer intervention durations for the VR groups (SMD 0.96, 95% CI 0.36-1.57; P=.002) resulted in greater improvements in arm and hand motor ability (WMFT task performance score) than equal intervention durations between the groups (SMD 0.06, 95% CI −0.29 to 0.41; P=.72), and the subgroup difference was significant (P=.01; Table S9 in Multimedia Appendix 6).
Intervention Duration in VR Groups
The results revealed that receiving >15 hours of VR intervention (SMD 0.92, 95% CI 0.35-1.49; P=.002) was associated with significant improvements in hand dexterity (BBT) compared with receiving ≤15 hours of VR intervention (SMD −0.10, 95% CI −0.35 to 0.15; P=.45); a significant subgroup difference was observed (P<.001; Table 4).
Moreover, receiving >15 hours of VR intervention (SMD 0.33, 95% CI 0.02-0.63; P=.04) was associated with a significant decrease in spasticity (AS or mAS) compared with receiving ≤15 hours of VR intervention (SMD −0.50, 95% CI −1.14 to 0.14; P=.13); the subgroup difference was significant (P=.02; Table S2 in Multimedia Appendix 6).
Trial Length
Receiving VR-supported exercise therapy for >1 month (SMD 0.97, 95% CI 0.06-1.89; P=.04) was associated with greater improvements in hand dexterity (BBT) than receiving VR-supported exercise therapy for <1 month (SMD 0.02, 95% CI −0.22 to 0.26; P=.84); the difference between the groups was significant (P=.049; Table 4).
Furthermore, those who experienced trial lengths of 2 weeks to 1 month (SMD 0.49, 95% CI −0.11 to 1.10; P=.11) showed greater improvements in quality of life (SIS total score) than those for whom trial lengths were >1 month (SMD −0.20, 95% CI −0.46 to 0.06; P=.13), and the difference between the groups was significant (P=.04; Table S13 in Multimedia Appendix 6).
Meta-analysis of the Effects of VR-Supported Exercise Therapy in the Follow-up Assessments
The results of the meta-analyses of outcomes that were examined in the follow-up assessment are presented in Table 7 (from after intervention to follow-up assessment) and Table 8 (from baseline to follow-up assessment). Multimedia Appendix 5 (Figures S21-S44) shows the associated forest plots. Significant improvements (SMD 0.26, 95% CI 0.00-0.51; P=.049) in arm and hand motor ability (WMFT task completion time) from baseline to follow-up assessments were observed (Table 8). No statistically significant heterogeneity was observed across trials. No publication bias was observed in the analysis.
Table 7.
Meta-analyses of outcomes examined in the follow-up assessments (from after intervention to follow-up assessments).
| Outcomes | Tools or methods used to assess the outcomes | Number of trials analyzed and number of participants involved | Standardized mean difference (95% CI) | Between-group difference, P value | Heterogeneity | Egger test, P value | ||||
|
|
|
|
|
|
Cochran Q test | P value | I2 (%) |
|
||
| Impairments in upper extremity functions and structures | ||||||||||
|
|
Upper extremity motor function | Fugl-Meyer Assessment-Upper Extremity | 10 [40,41,44,45,50,51,53-55,58]; NVRa group=160, Ncontrol group=160 | 0.00 (−0.22 to 0.22) |
.99 | 2.66 | .98 | 0 | .91 | |
| Activity limitations | ||||||||||
|
|
Independence in day-to-day activities | Functional Independence Measure | 3 [8,10,44]; NVR group=166, Ncontrol group=163 | −0.05 (−0.27 to 0.17) |
.64 | 0.04 | .98 | 0 | .43 | |
|
|
Independence in day-to-day activities | Barthel Index or modified Barthel Index | 3 [10,41,54]; NVR group=95, Ncontrol group=94 | −0.02 (−0.31 to 0.26) |
.87 | 1.87 | .39 | 0 | .32 | |
|
|
Arm and hand motor ability | Action Research Arm Test | 5 [8,30,38,44,45]; NVR group=229, Ncontrol group=230 | 0.10 (−0.08 to 0.29) |
.27 | 1.87 | .76 | 0 | .56 | |
|
|
Arm and hand motor ability | Wolf Motor Function Test task completion time | 5 [10,40,50,51,54]; NVR group=127, Ncontrol group=125 | 0.01 (−0.30 to 0.32) |
.95 | 5.07 | .28 | 21 | .10 | |
|
|
Arm and hand motor ability | Wolf Motor Function Test task performance score | 2 [50,54]; NVR group=18, Ncontrol group=19 | −0.24 (−0.88 to 0.41) |
.47 | 0.17 | .68 | 0 | N/Ab | |
|
|
Hand dexterity | Box and Block Test | 5 [8,10,41,51,53]; NVR group=175, Ncontrol group=168 | 0.13 (−0.09 to 0.34) |
.25 | 1.70 | .79 | 0 | .54 | |
|
|
Hand motor ability |
Jebsen Hand Function Test | 2 [41,58]; NVR group=36, Ncontrol group=33 | 0.17 (−0.30 to 0.65) |
.48 | 0.38 | .54 | 0 | N/A | |
| Participation restrictions in life situations | ||||||||||
|
|
Quality of life | Stroke Impact Scale total score | 3 [30,53,54]; NVR group=138, Ncontrol group=140 | 0.14 (−0.10 to 0.37) |
.25 | 1.48 | .48 | 0 | .31 | |
|
|
Quality of life | Stroke Impact Scale hand function score | 2 [10,44]; NVR group=104, Ncontrol group=105 | −0.19 (−0.46 to 0.08) |
.17 | 0.17 | .68 | 0 | N/A | |
|
|
Upper extremity use in daily life | Motor Activity Log quality of movement score | 4 [40,50,51,53]; NVR group=53, Ncontrol group=51 | −0.17 (−0.64 to 0.30) |
.48 | 4.11 | .25 | 27 | .53 | |
|
|
Upper extremity use in daily life | Motor Activity Log amount of use score | 3 [40,50,53]; NVR group=32, Ncontrol group=31 | 0.06 (−0.43 to 0.56) |
.80 | 0.42 | .81 | 0 | .47 | |
aVR: virtual reality.
bN/A: not applicable.
Table 8.
Meta-analyses of outcomes examined in the follow-up assessments (from baseline to follow-up assessments).
| Outcomes | Tools or methods used to assess the outcomes | Number of trials analyzed and number of participants involved | Standardized mean difference (95% CI) | Between-group difference, P value | Heterogeneity | Egger test, P value | ||||||||||||
|
|
|
|
|
|
Cochran Q test | P value | I2 (%) |
|
||||||||||
| Impairments in upper extremity functions and structures | ||||||||||||||||||
|
|
Upper extremity motor function | Fugl-Meyer Assessment-Upper Extremity | 10 [40,41,44,45,50,51,53-55,58]; NVRa group=160, Ncontrol group=160 | 0.48 (−0.15 to 1.11) | .13 | 62.37 | <.001 | 86 | .35 | |||||||||
| Activity limitations | ||||||||||||||||||
|
|
In Independence in day-to-day activities | Functional Independence Measure | 3 [8,10,44]; NVR group=166, Ncontrol group=163 | −0.05 (−0.27 to 0.16) | .63 | 0.39 | .82 | 0 | .56 | |||||||||
|
|
Independence in day-to-day activities | Barthel Index or modified Barthel Index | 3 [10,41,54]; NVR group=95, Ncontrol group=94 | −0.02 (−0.30 to 0.27) | .90 | 0.53 | .77 | 0 | .54 | |||||||||
|
|
Arm and hand motor ability | Action Research Arm Test | 5 [8,30,38,44,45]; NVR group=229, Ncontrol group=230 | 0.03 (−0.15 to 0.22) | .71 | 1.16 | .89 | 0 | .62 | |||||||||
|
|
Arm and hand motor ability | Wolf Motor Function Test task completion time | 5 [10,40,50,51,54]; NVR group=127, Ncontrol group=125 | 0.26 (0.00 to 0.51) | .049 | 4.10 | .39 | 2 | .74 | |||||||||
|
|
Arm and hand motor ability | Wolf Motor Function Test task performance score | 2 [50,54]; NVR group=18, Ncontrol group=19 | −0.32 (−0.98 to 0.34) | .34 | 1.01 | .32 | 1 | N/Ab | |||||||||
|
|
Hand dexterity | Box and Block Test | 5 [8,10,41,51,53]; NVR group=175, Ncontrol group=168 | 0.05 (−0.16 to 0.26) | .66 | 2.34 | .67 | 0 | .62 | |||||||||
|
|
Hand motor ability |
Jebsen Hand Function Test | 2 [41,58]; NVR group=36, Ncontrol group=33 | 1.81 (−0.85 to 4.46) | .18 | 19.57 | <.001 | 95 | N/A | |||||||||
| Participation restrictions in life situations | ||||||||||||||||||
|
|
Quality of life | Stroke Impact Scale total score | 3 [30,53,54]; NVR group=138, Ncontrol group=140 | 0.05 (−0.19 to 0.28) | .70 | 0.88 | .64 | 0 | .09 | |||||||||
|
|
Quality of life | Stroke Impact Scale hand function score | 2 [10,44]; NVR group=104, Ncontrol group=105 | −0.25 (−0.52 to 0.02) | .07 | 0.18 | .67 | 0 | N/A | |||||||||
|
|
Upper extremity use in daily life | Motor Activity Log quality of movement score | 4 [40,50,51,53]; NVR group=53, Ncontrol group=51 | 0.17 (−0.21 to 0.56) | .38 | 1.11 | .77 | 0 | .85 | |||||||||
|
|
Upper extremity use in daily life | Motor Activity Log amount of use score | 3 [40,50,53]; NVR group=32, Ncontrol group=31 | 0.12 (−0.38 to 0.61) | .64 | 0.54 | .76 | 0 | .83 | |||||||||
aVR: virtual reality.
bN/A: not applicable.
Discussion
Principal Findings
This study included meta-analysis of 43 eligible trials to assess the effects of VR-supported exercise therapy on upper extremity motor rehabilitation in patients following stroke. A total of 12 outcomes regarding impairments in upper extremity functions and structures, activity limitations, and participation restrictions in life situations were examined using 17 tools or methods, with several outcomes examined using different measurement tools or methods. Overall, compared with the use of either conventional therapy or no therapy (ie, control), the use of VR-supported exercise therapy alone or in combination with conventional therapy (ie, intervention) significantly improved 2 outcomes—upper extremity motor function (FMA-UE) and upper extremity ROM (goniometer). Both significant and nonsignificant improvements were observed in another 2 outcomes, depending on the methods used to measure them: muscle strength (significant when measured by MMT) and independence in day-to-day activities (significant when measured by FIM and modified Rankin Scale). However, as for the other 8 outcomes, the use of VR-supported exercise therapy did not significantly reduce spasticity (AS or mAS) or improve grip strength (dynamometer), upper extremity stroke recovery (Brunnstrom Stages of Stroke Recovery for Upper Extremity), hand dexterity (BBT), arm and hand motor ability (ARAT, WMFT, and MFT), hand motor ability (JHFT), quality of life (SIS), and upper extremity use in daily life (Motor Activity Log).
High-quality evidence was available only for upper extremity motor function (FMA-UE), arm and hand motor ability (ARAT), and independence in day-to-day activities (FIM). In the following sections, we discuss possible explanations for these findings using high-quality evidence. For findings with very low to moderate quality of evidence, further investigation is required before generalizations can be made.
Effects on Upper Extremity Motor Function (FMA-UE)
Our findings contribute further evidence to the literature, showing that VR-supported exercise therapy is effective in improving motor function, especially gross motor function. One possible explanation for our findings is that VR promotes motor learning. First, VR can promote access to therapeutic exercises; it can be used to simulate real-life environments, which allows for real-time interactions and provides a means for individuals to practice therapeutic tasks that may not be feasible to perform in the real world because of resource limitations or safety concerns [69]. Second, virtual environments can provide visual, auditory, or haptic feedback that can facilitate motor skill learning. Such feedback can inform individuals of their success or failure in performing therapeutic tasks [7,69]. Individuals can then make adjustments during tasks. Linking positive feedback to improved or successful therapeutic task performance can also motivate and encourage individuals to engage in rehabilitation therapy [69,70]. Third, VR allows repetitive and intensive therapeutic exercises. Intensive practice can facilitate contraction of muscles involved in exercise and promote muscle coordination [47,71]. At the nervous system level, a large amount of practice can strengthen the connections among neurons and induce reorganization in regions of the cerebral cortex corresponding to the affected extremity, thus improving motor function [69]. Fourth, various types of gaming features can be incorporated in VR-supported exercise therapy protocols, which can be useful for increasing individuals’ motivation to perform therapeutic tasks [8,72-75]. For instance, games can set rewards (eg, credits), the pursuit and experience of which motivates users to perform specific behaviors [72]. As another example, games can have different levels of difficulties to meet the needs of different users. Providing appropriate levels of challenges to users can help them avoid boredom or frustration with therapy. Enhanced motivation has been associated with better concentration on therapeutic tasks, higher training intensity, and adherence to therapy [37,69,76].
Effects on Arm and Hand Motor Ability (ARAT)
Our study showed that VR-supported exercise therapy did not have any positive impact on fine motor function improvement (ARAT). The possible explanation for our finding is as follows. In VR-supported exercise therapy, there is a need for interaction with virtual objects, which requires the use of input devices. In most of the reviewed VR-supported exercise therapies, the input devices used were handheld controllers, which required individuals to apply only gross motor skills to hold and move the controllers for interaction (eg, [30,44]). Consequently, fine movements could hardly be involved, and training in them could hardly be achieved. Thus, no significant improvement in fine motor function was observed. This finding suggests that VR systems that use input mechanisms that would facilitate fine motor movements, such as Leap Motion or gloves with sensors [41,63], may be more suitable for supporting fine movement exercises.
Effects on Independence in Day-to-day Activities (FIM)
FIM measures independence in self-care, sphincter control, transfer, locomotion, communication, and social cognition in daily life [77]. Our findings suggest that VR-supported exercise therapy can improve independence in performing such day-to-day activities, which require good upper extremity function. For example, self-care activities, such as eating, bathing, and dressing, usually involve the use of both sides of the upper extremities. Another example is that changing positions from lying down to sitting up may involve the use of the affected upper extremity to support the upper body. As mentioned in the previous section, VR-supported exercise therapy can help improve upper extremity motor function (FMA-UE), enabling patients to participate more actively in the abovementioned day-to-day activities and requiring less assistance from health care providers or caregivers after receiving VR-supported exercise therapy.
Subgroup Analysis of the Effects of VR-Supported Exercise Therapy
We found that the use of VR-supported exercise therapy in combination with conventional therapy, longer VR-supported exercise therapy interventions (ie, >15 hours), and longer trial lengths of VR-supported exercise therapy (ie, >1 and ≤2 months) could improve hand dexterity (BBT), possibly because VR-supported exercise therapy offers longer durations of therapy. Increasing the duration of therapy has been shown to be associated with better motor recovery outcomes [4,7,69,78,79]. It should be noted, however, that motor recovery outcomes are not only determined by the duration of therapy but also by other factors, such as the number of repetitions of the therapeutic tasks, the duration of each training session, the number of sessions, and the frequency of training [7]. More information regarding the details of VR-supported exercise therapy is needed for further analysis before proposing recommendations for the best levels of practice.
Except for the subgroup analyses of hand dexterity (BBT), the number of trials (<10) and participants included in the subgroup analyses for the other outcomes was quite small, implying that these analyses were less likely to produce confirmatory conclusions [24,80]. Further clinical trials are needed to examine the impact of these moderating factors on the effectiveness of VR-supported exercise therapy.
Effects of VR-Supported Exercise Therapy During Follow-up Assessments
The benefits of VR-supported exercise therapy were not maintained after withdrawing from the technology. However, because we did not have any details on the rehabilitation therapy or exercises that the participants received during the follow-up periods in any of the trials, we could not explore the factors that may have influenced the long-term effects of VR-supported exercise therapy on these outcomes.
Implications for Research
The conclusions of this review have several implications for future studies. First, several trials had small sample sizes (10 trials examined <20 participants) and likely had insufficient statistical power to detect significant changes in the outcomes. Studies with small sample sizes also bear the risk of being less likely to be published [81-83]. Therefore, larger sample sizes are suggested to reduce the risk of failing to detect significant changes and face publication bias. Second, the positive effects of VR-supported exercise therapy were not maintained after withdrawing the technology. However, poststroke rehabilitation and recovery is a long-term, even lifelong, process, and more research is required to determine how best to maintain the long-term effects of VR-supported exercise therapy. Third, most of the VR systems used in the included trials were nonimmersive (eg, Nintendo Wii); the effectiveness of immersive VR-based (eg, head-mounted display) interventions remains relatively less known and should be further examined, as the degree of immersion may influence user experience and the effectiveness of VR-based interventions [84-87].
Implications for Practice
Our review has several practical implications. First, VR-based interventions can be incorporated into therapeutic exercises for motor function training and day-to-day activity training in patients following stroke. Commercial games (eg, Nintendo Wii Sports) appear to be a good option because of their high availability in the market and relatively low prices [62]. Using commercially available games would enable researchers to avoid the costs (eg, time and resources) of designing and developing new games. However, it should be noted that commercial games are typically intended to be played by healthy users and therefore may not meet the heterogeneous needs of patients with impairments [7,88]. For example, commercial games may provide exercises for the overall arm but not for specific joints. To better fulfill the heterogeneous needs of patients and meet specific therapeutic goals, specialized VR programs that allow therapists to customize therapeutic aspects, such as feedback type and difficulty level, based on each patient’s condition must be designed [7,69]. Second, patients with stroke are commonly older people [89] who may face difficulties in learning new technologies owing to age-related declines in physical or cognitive functions and other psychological factors (eg, technology anxiety) [90-93]. Therefore, the usability of VR-based interventions must be assessed and improved to provide a user-friendly interface, match the patients’ abilities and preferences, and ultimately promote patients’ experiences with and acceptance of VR-based interventions, because the acceptance of technology is an essential prerequisite for the successful implementation of technology-based health care interventions [94-107]. Third, as older patients may have limited experience with VR technology [91], the provision of appropriate assistance and guidance is necessary to support patients in learning to use VR input devices and interact with virtual environments.
Limitations
This review has some limitations. First, several study outcomes displayed only a small degree of responsiveness [108-111]; thus, changes in such outcomes may have gone undetected. Second, the risk assessment indicated a low quality of evidence for several outcomes (eg, upper extremity ROM). Therefore, the results related to these study outcomes should be interpreted with caution. Third, the number of trials and participants examined was quite small for several subgroup analyses (eg, Tables S4 and S5 in Multimedia Appendix 6), implying that the findings need to be interpreted cautiously. Fourth, moderate to high levels of heterogeneity were observed in the meta-analysis, which could not be explained by the moderating factors examined and indicated the presence of other moderating factors that require further investigation. Fifth, detection of publication bias suggests that the findings should be interpreted with caution.
Conclusions
This systematic review and meta-analysis provided evidence for the effects of VR-supported exercise therapy on outcomes related to impairments in upper extremity functions and structures, activity limitations, and participation restrictions in life situations. A total of 12 outcomes were examined, some of which were measured using various tools or methods. Of the 12 outcomes, significant improvements were detected in 2, and both significant and nonsignificant improvements were observed in another 2, depending on the measurement tools or methods used. The findings with high-quality evidence suggest that, compared with the use of either conventional therapy or no therapy, VR-supported exercise therapy could effectively improve upper extremity gross motor function (FMA-UE) and independence in daily life (FIM), at least during therapy, but it did not improve fine motor function (ARAT). For findings with low-quality evidence, more research is required before drawing confirmatory conclusions. Future studies should examine how the benefits of VR-supported exercise therapy can be maintained over time.
Acknowledgments
The authors are grateful for the support from Dr Zhenzhen Xie and Dr Yong Zhou for their suggestions and clinical advice.
This review was supported by the Seed Fund for Basic Research (project number 201811159012) at the University of Hong Kong. The funder had no role in the study design, data extraction process, data analysis, result interpretation, or manuscript preparation.
Abbreviations
- ARAT
Action Research Arm Test
- AS
Ashworth Scale
- BBT
Box and Block Test
- FIM
Functional Independence Measure
- FMA-UE
Fugl-Meyer Assessment-Upper Extremity
- JHFT
Jebsen Hand Function Test
- mAS
Modified Ashworth Scale
- MFT
Manual Function Test
- MMT
Manual Muscle Testing
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- ROM
range of motion
- SIS
Stroke Impact Scale
- SMD
standardized mean difference
- VR
virtual reality
- WMFT
Wolf Motor Function Test
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist.
Details of the search.
Details of the characteristics of the included trials.
Outcomes examined in the included trials.
Forest plots of the meta-analyses.
Results of subgroup analyses.
Footnotes
Authors' Contributions: JC and CKO designed the study. JC and TC conducted data screening and data extraction. JC performed data analysis and drafted the manuscript. CKO and TC reviewed and significantly revised the manuscript.
Conflicts of Interest: None declared.
References
- 1.Johnson W, Onuma O, Owolabi M, Sachdev S. Stroke: a global response is needed. Bull World Health Organ. 2016 Sep 01;94(9):634–A. doi: 10.2471/BLT.16.181636. http://europepmc.org/abstract/MED/27708464 .BLT.16.181636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campbell BC, Khatri P. Stroke. Lancet. 2020 Jul 11;396(10244):129–42. doi: 10.1016/S0140-6736(20)31179-X.S0140-6736(20)31179-X [DOI] [PubMed] [Google Scholar]
- 3.GBD 2016 Lifetime Risk of Stroke Collaborators. Feigin VL, Nguyen G, Cercy K, Johnson CO, Alam T, Parmar PG, Abajobir AA, Abate KH, Abd-Allah F, Abejie AN, Abyu GY, Ademi Z, Agarwal G, Ahmed MB, Akinyemi RO, Al-Raddadi R, Aminde LN, Amlie-Lefond C, Ansari H, Asayesh H, Asgedom SW, Atey TM, Ayele HT, Banach M, Banerjee A, Barac A, Barker-Collo SL, Bärnighausen T, Barregard L, Basu S, Bedi N, Behzadifar M, Béjot Y, Bennett DA, Bensenor IM, Berhe DF, Boneya DJ, Brainin M, Campos-Nonato IR, Caso V, Castañeda-Orjuela CA, Rivas JC, Catalá-López F, Christensen H, Criqui MH, Damasceno A, Dandona L, Dandona R, Davletov K, de Courten B, deVeber G, Dokova K, Edessa D, Endres M, Faraon EJ, Farvid MS, Fischer F, Foreman K, Forouzanfar MH, Gall SL, Gebrehiwot TT, Geleijnse JM, Gillum RF, Giroud M, Goulart AC, Gupta R, Gupta R, Hachinski V, Hamadeh RR, Hankey GJ, Hareri HA, Havmoeller R, Hay SI, Hegazy MI, Hibstu DT, James SL, Jeemon P, John D, Jonas JB, Jóźwiak J, Kalani R, Kandel A, Kasaeian A, Kengne AP, Khader YS, Khan AR, Khang YH, Khubchandani J, Kim D, Kim YJ, Kivimaki M, Kokubo Y, Kolte D, Kopec JA, Kosen S, Kravchenko M, Krishnamurthi R, Kumar GA, Lafranconi A, Lavados PM, Legesse Y, Li Y, Liang X, Lo WD, Lorkowski S, Lotufo PA, Loy CT, Mackay MT, Abd El Razek HM, Mahdavi M, Majeed A, Malekzadeh R, Malta DC, Mamun AA, Mantovani LG, Martins SC, Mate KK, Mazidi M, Mehata S, Meier T, Melaku YA, Mendoza W, Mensah GA, Meretoja A, Mezgebe HB, Miazgowski T, Miller TR, Ibrahim NM, Mohammed S, Mokdad AH, Moosazadeh M, Moran AE, Musa KI, Negoi RI, Nguyen M, Nguyen QL, Nguyen TH, Tran TT, Nguyen TT, Anggraini Ningrum DN, Norrving B, Noubiap JJ, O’Donnell MJ, Olagunju AT, Onuma OK, Owolabi MO, Parsaeian M, Patton GC, Piradov M, Pletcher MA, Pourmalek F, Prakash V, Qorbani M, Rahman M, Rahman MA, Rai RK, Ranta A, Rawaf D, Rawaf S, Renzaho AM, Robinson SR, Sahathevan R, Sahebkar A, Salomon JA, Santalucia P, Santos IS, Sartorius B, Schutte AE, Sepanlou SG, Shafieesabet A, Shaikh MA, Shamsizadeh M, Sheth KN, Sisay M, Shin KJ, Shiue I, Silva DA, Sobngwi E, Soljak M, Sorensen RJ, Sposato LA, Stranges S, Suliankatchi RA, Tabarés-Seisdedos R, Tanne D, Nguyen CT, Thakur JS, Thrift AG, Tirschwell DL, Topor-Madry R, Tran BX, Nguyen LT, Truelsen T, Tsilimparis N, Tyrovolas S, Ukwaja KN, Uthman OA, Varakin Y, Vasankari T, Venketasubramanian N, Vlassov VV, Wang W, Werdecker A, Wolfe AD, Xu G, Yano Y, Yonemoto N, Yu C, Zaidi Z, El Sayed Zaki M, Zhou M, Ziaeian B, Zipkin B, Vos T, Naghavi M, Murray CJ, Roth GA. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med. 2018 Dec 20;379(25):2429–37. doi: 10.1056/NEJMoa1804492. http://europepmc.org/abstract/MED/30575491 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet. 2011 May 14;377(9778):1693–702. doi: 10.1016/S0140-6736(11)60325-5.S0140-6736(11)60325-5 [DOI] [PubMed] [Google Scholar]
- 5.Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. Lancet Neurol. 2009 Aug;8(8):741–54. doi: 10.1016/S1474-4422(09)70150-4.S1474-4422(09)70150-4 [DOI] [PubMed] [Google Scholar]
- 6.Mayo NE, Wood-Dauphinee S, Côté R, Durcan L, Carlton J. Activity, participation, and quality of life 6 months poststroke. Arch Phys Med Rehabil. 2002 Aug;83(8):1035–42. doi: 10.1053/apmr.2002.33984.S0003-9993(02)00025-4 [DOI] [PubMed] [Google Scholar]
- 7.Levin MF, Demers M. Motor learning in neurological rehabilitation. Disabil Rehabil. 2021 Nov 20;43(24):3445–53. doi: 10.1080/09638288.2020.1752317. [DOI] [PubMed] [Google Scholar]
- 8.Brunner I, Skouen JS, Hofstad H, Aßmus J, Becker F, Sanders AM, Pallesen H, Qvist Kristensen L, Michielsen M, Thijs L, Verheyden G. Virtual reality training for upper extremity in subacute stroke (VIRTUES): a multicenter RCT. Neurology. 2017 Dec 12;89(24):2413–21. doi: 10.1212/WNL.0000000000004744.WNL.0000000000004744 [DOI] [PubMed] [Google Scholar]
- 9.Kiper P, Szczudlik A, Agostini M, Opara J, Nowobilski R, Ventura L, Tonin P, Turolla A. Virtual reality for upper limb rehabilitation in subacute and chronic stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2018 May;99(5):834–42.e4. doi: 10.1016/j.apmr.2018.01.023.S0003-9993(18)30099-6 [DOI] [PubMed] [Google Scholar]
- 10.Saposnik G, Cohen LG, Mamdani M, Pooyania S, Ploughman M, Cheung D, Shaw J, Hall J, Nord P, Dukelow S, Nilanont Y, De Los Rios F, Olmos L, Levin M, Teasell R, Cohen A, Thorpe K, Laupacis A, Bayley M, Stroke Outcomes Research Canada Efficacy and safety of non-immersive virtual reality exercising in stroke rehabilitation (EVREST): a randomised, multicentre, single-blind, controlled trial. Lancet Neurol. 2016 Sep;15(10):1019–27. doi: 10.1016/S1474-4422(16)30121-1. http://europepmc.org/abstract/MED/27365261 .S1474-4422(16)30121-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee HY, Kim YL, Lee SM. Effects of virtual reality-based training and task-oriented training on balance performance in stroke patients. J Phys Ther Sci. 2015 Jun;27(6):1883–8. doi: 10.1589/jpts.27.1883. http://europepmc.org/abstract/MED/26180341 .jpts-2015-016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lohse KR, Hilderman CG, Cheung KL, Tatla S, Van der Loos HF. Virtual reality therapy for adults post-stroke: a systematic review and meta-analysis exploring virtual environments and commercial games in therapy. PLoS One. 2014 Mar 28;9(3):e93318. doi: 10.1371/journal.pone.0093318. https://dx.plos.org/10.1371/journal.pone.0093318 .PONE-D-14-02313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saposnik G, Levin M, Outcome Research Canada (SORCan) Working Group Virtual reality in stroke rehabilitation: a meta-analysis and implications for clinicians. Stroke. 2011 May;42(5):1380–6. doi: 10.1161/STROKEAHA.110.605451.STROKEAHA.110.605451 [DOI] [PubMed] [Google Scholar]
- 14.Henderson A, Korner-Bitensky N, Levin M. Virtual reality in stroke rehabilitation: a systematic review of its effectiveness for upper limb motor recovery. Top Stroke Rehabil. 2007;14(2):52–61. doi: 10.1310/tsr1402-52.R477437HG74GW833 [DOI] [PubMed] [Google Scholar]
- 15.Laver KE, Lange B, George S, Deutsch JE, Saposnik G, Crotty M. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev. 2017 Nov 20;11(11):CD008349. doi: 10.1002/14651858.CD008349.pub4. http://europepmc.org/abstract/MED/29156493 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aminov A, Rogers JM, Middleton S, Caeyenberghs K, Wilson PH. What do randomized controlled trials say about virtual rehabilitation in stroke? A systematic literature review and meta-analysis of upper-limb and cognitive outcomes. J Neuroeng Rehabil. 2018 Mar 27;15:29. doi: 10.1186/s12984-018-0370-2. https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-018-0370-2 .10.1186/s12984-018-0370-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Palma GC, Freitas TB, Bonuzzi GM, Soares MA, Leite PH, Mazzini NA, Almeida MR, Pompeu JE, Torriani-Pasin C. Effects of virtual reality for stroke individuals based on the International Classification of Functioning and Health: a systematic review. Top Stroke Rehabil. 2017 May;24(4):269–78. doi: 10.1080/10749357.2016.1250373. [DOI] [PubMed] [Google Scholar]
- 18.ICF beginner's guide: towards a common language for functioning, disability and health. World Health Organization. 2002. Jan 1, [2022-01-03]. https://www.who.int/publications/m/item/icf-beginner-s-guide-towards-a-common-language-for-functioning-disability-and-health .
- 19.Domínguez-Téllez P, Moral-Muñoz JA, Salazar A, Casado-Fernández E, Lucena-Antón D. Game-based virtual reality interventions to improve upper limb motor function and quality of life after stroke: systematic review and meta-analysis. Games Health J. 2020 Mar;9(1):1–10. doi: 10.1089/g4h.2019.0043. [DOI] [PubMed] [Google Scholar]
- 20.Karamians R, Proffitt R, Kline D, Gauthier LV. Effectiveness of virtual reality- and gaming-based interventions for upper extremity rehabilitation poststroke: a meta-analysis. Arch Phys Med Rehabil. 2020 May;101(5):885–96. doi: 10.1016/j.apmr.2019.10.195.S0003-9993(19)31438-8 [DOI] [PubMed] [Google Scholar]
- 21.Mekbib DB, Han J, Zhang L, Fang S, Jiang H, Zhu J, Roe AW, Xu D. Virtual reality therapy for upper limb rehabilitation in patients with stroke: a meta-analysis of randomized clinical trials. Brain Inj. 2020 Mar 20;34(4):456–65. doi: 10.1080/02699052.2020.1725126. [DOI] [PubMed] [Google Scholar]
- 22.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71. doi: 10.1136/bmj.n71. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=33782057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Orwin R. Evaluating coding decisions. In: Cooper H, Hedges LV, editors. The Handbook of Research Synthesis. New York, NY, USA: Russell Sage Foundation; 1994. pp. 139–62. [Google Scholar]
- 24.Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021) London, UK: Cochrane; 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Viechtbauer W, Cheung MW. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010 Apr;1(2):112–25. doi: 10.1002/jrsm.11. [DOI] [PubMed] [Google Scholar]
- 26.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003 Sep 06;327(7414):557–60. doi: 10.1136/bmj.327.7414.557. http://europepmc.org/abstract/MED/12958120 .327/7414/557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997 Sep 13;315(7109):629–34. doi: 10.1136/bmj.315.7109.629. http://europepmc.org/abstract/MED/9310563 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernhardt J, Hayward KS, Kwakkel G, Ward NS, Wolf SL, Borschmann K, Krakauer JW, Boyd LA, Carmichael ST, Corbett D, Cramer SC. Agreed definitions and a shared vision for new standards in stroke recovery research: the Stroke Recovery and Rehabilitation Roundtable taskforce. Int J Stroke. 2017 Jul;12(5):444–50. doi: 10.1177/1747493017711816. [DOI] [PubMed] [Google Scholar]
- 29.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ, GRADE Working Group GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008 Apr 26;336(7650):924–6. doi: 10.1136/bmj.39489.470347.AD. http://europepmc.org/abstract/MED/18436948 .336/7650/924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adie K, Schofield C, Berrow M, Wingham J, Humfryes J, Pritchard C, James M, Allison R. Does the use of Nintendo Wii Sports TM improve arm function? Trial of Wii TM in stroke: a randomized controlled trial and economics analysis. Clin Rehabil. 2017 Mar;31(2):173–85. doi: 10.1177/0269215516637893.0269215516637893 [DOI] [PubMed] [Google Scholar]
- 31.Ikbali Afsar S, Mirzayev I, Umit Yemisci O, Cosar Saracgil SN. Virtual reality in upper extremity rehabilitation of stroke patients: a randomized controlled trial. J Stroke Cerebrovasc Dis. 2018 Dec;27(12):3473–8. doi: 10.1016/j.jstrokecerebrovasdis.2018.08.007.S1052-3057(18)30449-X [DOI] [PubMed] [Google Scholar]
- 32.Ain QU, Khan S, Ilyas S, Yaseen A, Tariq I, Liu T, Wang J. Additional effects of Xbox Kinect training on upper limb function in chronic stroke patients: a randomized control trial. Healthcare. 2021 Feb 24;9(3):242. doi: 10.3390/healthcare9030242. https://www.mdpi.com/resolver?pii=healthcare9030242 .healthcare9030242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alves SS, Ocamoto GN, de Camargo PS, Santos AT, Terra AM. Effects of virtual reality and motor imagery techniques using Fugl Meyer Assessment scale in post-stroke patients. Int J Ther Rehabil. 2018 Nov 02;25(11):587–96. doi: 10.12968/ijtr.2018.25.11.587. [DOI] [Google Scholar]
- 34.Anjum AF, Jawwad G, Khokhar A, Sadiq N, Masud R, Khalid AM. Effect of “Wii-habilitation” and constraint induced movement therapy on improving quality of life in stroke survivors. RMJ. 2021;46(1):220–3. [Google Scholar]
- 35.Aşkın A, Atar E, Koçyiğit H, Tosun A. Effects of Kinect-based virtual reality game training on upper extremity motor recovery in chronic stroke. Somatosens Mot Res. 2018 Mar;35(1):25–32. doi: 10.1080/08990220.2018.1444599. [DOI] [PubMed] [Google Scholar]
- 36.Cho HY, Song E, Moon JH, Hahm SC. Effects of virtual reality based therapeutic exercise on the upper extremity function and activities of daily living in patients with acute stroke: a pilot randomized controlled trial. Med Leg Update. 2021 Mar 19;21(2):676–82. doi: 10.37506/mlu.v21i2.2761. [DOI] [Google Scholar]
- 37.Choi JH, Han EY, Kim BR, Kim SM, Im SH, Lee SY, Hyun CW. Effectiveness of commercial gaming-based virtual reality movement therapy on functional recovery of upper extremity in subacute stroke patients. Ann Rehabil Med. 2014 Aug;38(4):485–93. doi: 10.5535/arm.2014.38.4.485. http://e-arm.org/journal/view.php?doi=10.5535/arm.2014.38.4.485 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Crosbie JH, Lennon S, McGoldrick MC, McNeill MD, McDonough SM. Virtual reality in the rehabilitation of the arm after hemiplegic stroke: a randomized controlled pilot study. Clin Rehabil. 2012 Sep;26(9):798–806. doi: 10.1177/0269215511434575.0269215511434575 [DOI] [PubMed] [Google Scholar]
- 39.Ersoy C, Iyigun G. Boxing training in patients with stroke causes improvement of upper extremity, balance, and cognitive functions but should it be applied as virtual or real? Top Stroke Rehabil. 2021 Mar;28(2):112–26. doi: 10.1080/10749357.2020.1783918. [DOI] [PubMed] [Google Scholar]
- 40.Hung JW, Chou CX, Chang YJ, Wu CY, Chang KC, Wu WC, Howell S. Comparison of Kinect2Scratch game-based training and therapist-based training for the improvement of upper extremity functions of patients with chronic stroke: a randomized controlled single-blinded trial. Eur J Phys Rehabil Med. 2019 Oct;55(5):542–50. doi: 10.23736/S1973-9087.19.05598-9. https://www.minervamedica.it/index2.t?show=R33Y2019N05A0542 .S1973-9087.19.05598-9 [DOI] [PubMed] [Google Scholar]
- 41.Kang MG, Yun SJ, Lee SY, Oh BM, Lee HH, Lee SU, Seo HG. Effects of upper-extremity rehabilitation using smart glove in patients with subacute stroke: results of a prematurely terminated multicenter randomized controlled trial. Front Neurol. 2020 Nov 9;11:580393. doi: 10.3389/fneur.2020.580393. doi: 10.3389/fneur.2020.580393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kiper P, Agostini M, Luque-Moreno C, Tonin P, Turolla A. Reinforced feedback in virtual environment for rehabilitation of upper extremity dysfunction after stroke: preliminary data from a randomized controlled trial. Biomed Res Int. 2014;2014:752128. doi: 10.1155/2014/752128. doi: 10.1155/2014/752128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kiper P, Piron L, Turolla A, Stożek J, Tonin P. The effectiveness of reinforced feedback in virtual environment in the first 12 months after stroke. Neurol Neurochir Pol. 2011;45(5):436–44. doi: 10.1016/s0028-3843(14)60311-x.S0028-3843(14)60311-X [DOI] [PubMed] [Google Scholar]
- 44.Kong KH, Loh YJ, Thia E, Chai A, Ng CY, Soh YM, Toh S, Tjan SY. Efficacy of a virtual reality commercial gaming device in upper limb recovery after stroke: a randomized, controlled study. Top Stroke Rehabil. 2016 Oct;23(5):333–40. doi: 10.1080/10749357.2016.1139796. [DOI] [PubMed] [Google Scholar]
- 45.Kottink AI, Prange GB, Krabben T, Rietman JS, Buurke JH. Gaming and conventional exercises for improvement of arm function after stroke: a randomized controlled pilot study. Games Health J. 2014 Jun;3(3):184–91. doi: 10.1089/g4h.2014.0026. [DOI] [PubMed] [Google Scholar]
- 46.Kwon JS, Park MJ, Yoon IJ, Park SH. Effects of virtual reality on upper extremity function and activities of daily living performance in acute stroke: a double-blind randomized clinical trial. NeuroRehabilitation. 2012;31(4):379–85. doi: 10.3233/NRE-2012-00807.47K9607337H4N4WX [DOI] [PubMed] [Google Scholar]
- 47.Lee G. Effects of training using video games on the muscle strength, muscle tone, and activities of daily living of chronic stroke patients. J Phys Ther Sci. 2013 May;25(5):595–7. doi: 10.1589/jpts.25.595. http://europepmc.org/abstract/MED/24259810 .jpts-2012-396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lee M, Son J, Kim J, Pyun SB, Eun SD, Yoon BC. Comparison of individualized virtual reality- and group-based rehabilitation in older adults with chronic stroke in community settings: a pilot randomized controlled trial. Eur J Integr Med. 2016 Oct;8(5):738–46. doi: 10.1016/j.eujim.2016.08.166. [DOI] [Google Scholar]
- 49.Lee MM, Lee KJ, Song CH. Game-based virtual reality canoe paddling training to improve postural balance and upper extremity function: a preliminary randomized controlled study of 30 patients with subacute stroke. Med Sci Monit. 2018 Apr 27;24:2590–8. doi: 10.12659/MSM.906451. https://www.medscimonit.com/download/index/idArt/906451 .906451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Levin MF, Snir O, Liebermann DG, Weingarden H, Weiss PL. Virtual reality versus conventional treatment of reaching ability in chronic stroke: clinical feasibility study. Neurol Ther. 2012 Aug 24;1:3. doi: 10.1007/s40120-012-0003-9. http://europepmc.org/abstract/MED/26000209 .3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McNulty PA, Thompson-Butel AG, Faux SG, Lin G, Katrak PH, Harris LR, Shiner CT. The efficacy of Wii-based Movement Therapy for upper limb rehabilitation in the chronic poststroke period: a randomized controlled trial. Int J Stroke. 2015 Dec;10(8):1253–60. doi: 10.1111/ijs.12594. [DOI] [PubMed] [Google Scholar]
- 52.Miclaus R, Roman N, Caloian S, Mitoiu B, Suciu O, Onofrei RR, Pavel E, Neculau A. Non-immersive virtual reality for post-stroke upper extremity rehabilitation: a small cohort randomized trial. Brain Sci. 2020 Sep 21;10(9):655. doi: 10.3390/brainsci10090655. https://www.mdpi.com/resolver?pii=brainsci10090655 .brainsci10090655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Norouzi-Gheidari N, Hernandez A, Archambault PS, Higgins J, Poissant L, Kairy D. Feasibility, safety and efficacy of a virtual reality exergame system to supplement upper extremity rehabilitation post-stroke: a pilot randomized clinical trial and proof of principle. Int J Environ Res Public Health. 2019 Dec 23;17(1):113. doi: 10.3390/ijerph17010113. https://www.mdpi.com/resolver?pii=ijerph17010113 .ijerph17010113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Park M, Ko MH, Oh SW, Lee JY, Ham Y, Yi H, Choi Y, Ha D, Shin JH. Effects of virtual reality-based planar motion exercises on upper extremity function, range of motion, and health-related quality of life: a multicenter, single-blinded, randomized, controlled pilot study. J Neuroeng Rehabil. 2019 Oct 24;16:122. doi: 10.1186/s12984-019-0595-8. https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-019-0595-8 .10.1186/s12984-019-0595-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Piron L, Turolla A, Agostini M, Zucconi C, Cortese F, Zampolini M, Zannini M, Dam M, Ventura L, Battauz M, Tonin P. Exercises for paretic upper limb after stroke: a combined virtual-reality and telemedicine approach. J Rehabil Med. 2009 Nov;41(12):1016–20. doi: 10.2340/16501977-0459. https://www.medicaljournals.se/jrm/content/abstract/10.2340/16501977-0459 . [DOI] [PubMed] [Google Scholar]
- 56.Piron L, Turolla A, Agostini M, Zucconi CS, Ventura L, Tonin P, Dam M. Motor learning principles for rehabilitation: a pilot randomized controlled study in poststroke patients. Neurorehabil Neural Repair. 2010;24(6):501–8. doi: 10.1177/1545968310362672.24/6/501 [DOI] [PubMed] [Google Scholar]
- 57.Shin JH, Ryu H, Jang SH. A task-specific interactive game-based virtual reality rehabilitation system for patients with stroke: a usability test and two clinical experiments. J Neuroeng Rehabil. 2014 Mar 06;11:32. doi: 10.1186/1743-0003-11-32. https://jneuroengrehab.biomedcentral.com/articles/10.1186/1743-0003-11-32 .1743-0003-11-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shin JH, Kim MY, Lee JY, Jeon YJ, Kim S, Lee S, Seo B, Choi Y. Effects of virtual reality-based rehabilitation on distal upper extremity function and health-related quality of life: a single-blinded, randomized controlled trial. J Neuroeng Rehabil. 2016 Feb 24;13:17. doi: 10.1186/s12984-016-0125-x. https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-016-0125-x .10.1186/s12984-016-0125-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Şimşek TT, Çekok K. The effects of Nintendo Wii(TM)-based balance and upper extremity training on activities of daily living and quality of life in patients with sub-acute stroke: a randomized controlled study. Int J Neurosci. 2016 Dec;126(12):1061–70. doi: 10.3109/00207454.2015.1115993. [DOI] [PubMed] [Google Scholar]
- 60.Sin H, Lee G. Additional virtual reality training using Xbox Kinect in stroke survivors with hemiplegia. Am J Phys Med Rehabil. 2013 Oct;92(10):871–80. doi: 10.1097/PHM.0b013e3182a38e40.00002060-201310000-00004 [DOI] [PubMed] [Google Scholar]
- 61.Standen PJ, Threapleton K, Richardson A, Connell L, Brown DJ, Battersby S, Platts F, Burton A. A low cost virtual reality system for home based rehabilitation of the arm following stroke: a randomised controlled feasibility trial. Clin Rehabil. 2017 Mar;31(3):340–50. doi: 10.1177/0269215516640320. https://journals.sagepub.com/doi/10.1177/0269215516640320?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .0269215516640320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Türkbey TA, Kutlay S, Gök H. Clinical feasibility of Xbox KinectTM training for stroke rehabilitation: a single-blind randomized controlled pilot study. J Rehabil Med. 2017 Jan 19;49(1):22–9. doi: 10.2340/16501977-2183. https://www.medicaljournals.se/jrm/content/abstract/10.2340/16501977-2183 . [DOI] [PubMed] [Google Scholar]
- 63.Xie H, Zhang H, Liang H, Fan H, Zhou J, Ambrose Lo WL, Li L. A novel glasses-free virtual reality rehabilitation system on improving upper limb motor function among patients with stroke: a feasibility pilot study. Med Novel Technol Devices. 2021 Sep;11:100069. doi: 10.1016/j.medntd.2021.100069. [DOI] [Google Scholar]
- 64.Zondervan DK, Friedman N, Chang E, Zhao X, Augsburger R, Reinkensmeyer DJ, Cramer SC. Home-based hand rehabilitation after chronic stroke: randomized, controlled single-blind trial comparing the MusicGlove with a conventional exercise program. J Rehabil Res Dev. 2016;53(4):457–72. doi: 10.1682/JRRD.2015.04.0057. https://www.rehab.research.va.gov/jour/2016/534/pdf/JRRD-2015-04-0057.pdf .JRRD-2015-04-0057 [DOI] [PubMed] [Google Scholar]
- 65.Park YS, An CS, Lim CG. Effects of a rehabilitation program using a wearable device on the upper limb function, performance of activities of daily living, and rehabilitation participation in patients with acute stroke. Int J Environ Res Public Health. 2021 May 21;18(11):5524. doi: 10.3390/ijerph18115524. https://www.mdpi.com/resolver?pii=ijerph18115524 .ijerph18115524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jo K, Yu J, Jung J. Effects of virtual reality-based rehabilitation on upper extremity function and visual perception in stroke patients: a randomized control trial. J Phys Ther Sci. 2012;24(11):1205–8. doi: 10.1589/jpts.24.1205. [DOI] [Google Scholar]
- 67.Mokhtar MM, Atteya M, Rawash M. Virtual reality Xbox 360 Kinect training for stroke patients with hemiplegia. Biosci Res. 2019;16(1):672–6. [Google Scholar]
- 68.Wang ZR, Wang P, Xing L, Mei LP, Zhao J, Zhang T. Leap Motion-based virtual reality training for improving motor functional recovery of upper limbs and neural reorganization in subacute stroke patients. Neural Regen Res. 2017 Nov;12(11):1823–31. doi: 10.4103/1673-5374.219043. http://www.nrronline.org/article.asp?issn=1673-5374;year=2017;volume=12;issue=11;spage=1823;epage=1831;aulast=Wang .NeuralRegenRes_2017_12_11_1823_219043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Levac DE, Sveistrup H. Motor learning and virtual reality. In: Weiss PL, Keshner EA, Levin MF, editors. Virtual Reality for Physical and Motor Rehabilitation. New York, NY, USA: Springer; 2014. pp. 25–46. [Google Scholar]
- 70.Holden MK. Virtual environments for motor rehabilitation: review. Cyberpsychol Behav. 2005 Jun;8(3):187–211. doi: 10.1089/cpb.2005.8.187. [DOI] [PubMed] [Google Scholar]
- 71.Carr JH, Shepherd RB. Chapter 1 - Brain reorganization, the rehabilitation environment, measuring outcomes. In: Carr JH, Shepherd RB, editors. Stroke Rehabilitation: Guidelines for Exercise and Training to Optimize Motor Skill. Oxford, UK: Butterworth-Heinemann; 2003. pp. 3–31. [Google Scholar]
- 72.Lohse K, Shirzad N, Verster A, Hodges N, Van der Loos HF. Video games and rehabilitation: using design principles to enhance engagement in physical therapy. J Neurol Phys Ther. 2013 Dec;37(4):166–75. doi: 10.1097/NPT.0000000000000017.01253086-201312000-00004 [DOI] [PubMed] [Google Scholar]
- 73.Lewis GN, Woods C, Rosie JA, McPherson KM. Virtual reality games for rehabilitation of people with stroke: perspectives from the users. Disabil Rehabil Assist Technol. 2011;6(5):453–63. doi: 10.3109/17483107.2011.574310. [DOI] [PubMed] [Google Scholar]
- 74.Cheung KL, Tunik E, Adamovich SV, Boyd LA. Neuroplasticity and virtual reality. In: Weiss PL, Keshner EA, Levin MF, editors. Virtual Reality for Physical and Motor Rehabilitation. New York, NY, USA: Springer; 2014. pp. 5–24. [Google Scholar]
- 75.Wong RS, Yu EY, Wong TW, Fung CS, Choi CS, Or CK, Liu KS, Wong CK, Ip P, Lam CL. Development and pilot evaluation of a mobile app on parent-child exercises to improve physical activity and psychosocial outcomes of Hong Kong Chinese children. BMC Public Health. 2020 Oct 14;20(1):1544. doi: 10.1186/s12889-020-09655-9. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-09655-9 .10.1186/s12889-020-09655-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rohrbach N, Chicklis E, Levac DE. What is the impact of user affect on motor learning in virtual environments after stroke? A scoping review. J Neuroeng Rehabil. 2019 Jun 27;16(1):79. doi: 10.1186/s12984-019-0546-4. https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-019-0546-4 .10.1186/s12984-019-0546-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kidd D, Stewart G, Baldry J, Johnson J, Rossiter D, Petruckevitch A, Thompson AJ. The Functional Independence Measure: a comparative validity and reliability study. Disabil Rehabil. 1995 Jan;17(1):10–4. doi: 10.3109/09638289509166622. [DOI] [PubMed] [Google Scholar]
- 78.Veerbeek JM, van Wegen E, van Peppen R, van der Wees PJ, Hendriks E, Rietberg M, Kwakkel G. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS One. 2014 Feb 4;9(2):e87987. doi: 10.1371/journal.pone.0087987. https://dx.plos.org/10.1371/journal.pone.0087987 .PONE-D-13-44188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kwakkel G, van Peppen R, Wagenaar RC, Wood Dauphinee S, Richards C, Ashburn A, Miller K, Lincoln N, Partridge C, Wellwood I, Langhorne P. Effects of augmented exercise therapy time after stroke: a meta-analysis. Stroke. 2004 Nov;35(11):2529–39. doi: 10.1161/01.STR.0000143153.76460.7d.01.STR.0000143153.76460.7d [DOI] [PubMed] [Google Scholar]
- 80.Richardson M, Garner P, Donegan S. Interpretation of subgroup analyses in systematic reviews: a tutorial. Clin Epidemiol Glob Health. 2019 Jun 01;7(2):192–8. doi: 10.1016/j.cegh.2018.05.005. [DOI] [Google Scholar]
- 81.Moher D, Dulberg CS, Wells GA. Statistical power, sample size, and their reporting in randomized controlled trials. JAMA. 1994 Jul 13;272(2):122–4. [PubMed] [Google Scholar]
- 82.Lin L. Bias caused by sampling error in meta-analysis with small sample sizes. PLoS One. 2018 Sep 13;13(9):e0204056. doi: 10.1371/journal.pone.0204056. https://dx.plos.org/10.1371/journal.pone.0204056 .PONE-D-18-14403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Macaskill P, Walter SD, Irwig L. A comparison of methods to detect publication bias in meta-analysis. Stat Med. 2001 Mar 28;20(4):641–54. doi: 10.1002/sim.698. [DOI] [PubMed] [Google Scholar]
- 84.Gorini A, Capideville CS, De Leo G, Mantovani F, Riva G. The role of immersion and narrative in mediated presence: the virtual hospital experience. Cyberpsychol Behav Soc Netw. 2011 Mar;14(3):99–105. doi: 10.1089/cyber.2010.0100. [DOI] [PubMed] [Google Scholar]
- 85.Shahrbanian S, Ma X, Aghaei N, Korner-Bitensky N, Moshiri K, Simmonds MJ. Use of virtual reality (immersive vs. non immersive) for pain management in children and adults: a systematic review of evidence from randomized controlled trials. Eur J Exp Biol. 2012;2(5):1408–22. https://www.researchgate.net/publication/315740184_Use_of_virtual_reality_immersive_vs_non_immersive_for_pain_management_in_children_and_adults_A_systematic_review_of_evidence_from_randomized_controlled_trials . [Google Scholar]
- 86.Chen J, Xie Z, Kalun Or C. Head-mounted display virtual reality in disease treatment: a systematic review and meta-analysis. Proc Hum Factors Ergon Soc Annu Meet. 2020;64(1):1388–9. doi: 10.1177/1071181320641331. [DOI] [Google Scholar]
- 87.Chen J, Xie Z, Or C. Effectiveness of immersive virtual reality-supported interventions for patients with disorders or impairments: a systematic review and meta-analysis. Health Technol. 2021 Jul 16;11:811–33. doi: 10.1007/s12553-021-00561-7. [DOI] [Google Scholar]
- 88.Barrett N, Swain I, Gatzidis C, Mecheraoui C. The use and effect of video game design theory in the creation of game-based systems for upper limb stroke rehabilitation. J Rehabil Assist Technol Eng. 2016 May 9;3:1–16. doi: 10.1177/2055668316643644. https://journals.sagepub.com/doi/10.1177/2055668316643644?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .10.1177_2055668316643644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hall MJ, Levant S, DeFrances CJ. Hospitalization for stroke in U.S. hospitals, 1989-2009. NCHS Data Brief. 2012 May;(95):1–8. https://www.cdc.gov/nchs/data/databriefs/db95.pdf . [PubMed] [Google Scholar]
- 90.Deng Z, Mo X, Liu S. Comparison of the middle-aged and older users' adoption of mobile health services in China. Int J Med Inform. 2014 Mar;83(3):210–24. doi: 10.1016/j.ijmedinf.2013.12.002.S1386-5056(13)00249-9 [DOI] [PubMed] [Google Scholar]
- 91.Chen J, Or C. Assessing the use of immersive virtual reality, mouse and touchscreen in pointing and dragging-and-dropping tasks among young, middle-aged and older adults. Appl Ergon. 2017 Nov;65:437–48. doi: 10.1016/j.apergo.2017.03.013.S0003-6870(17)30072-8 [DOI] [PubMed] [Google Scholar]
- 92.Ng HC, Tao D, Or CK. Age differences in computer input device use: a comparison of touchscreen, trackball, and mouse. Proceedings of the 2013 World Conference on Information Systems and Technologies; WorldCIST '13; March 27-30, 2013; Algarve, Portugal. 2013. pp. 1015–24. [DOI] [Google Scholar]
- 93.Or CK, Valdez RS, Casper GR, Carayon P, Burke LJ, Brennan PF, Karsh BT. Human factors and ergonomics in home care: current concerns and future considerations for health information technology. Work. 2009;33(2):201–9. doi: 10.3233/WOR-2009-0867. http://europepmc.org/abstract/MED/19713630 .J64614388R473752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chen T, Or CK, Chen J. Effects of technology-supported exercise programs on the knee pain, physical function, and quality of life of individuals with knee osteoarthritis and/or chronic knee pain: a systematic review and meta-analysis of randomized controlled trials. J Am Med Inform Assoc. 2021 Feb 15;28(2):414–23. doi: 10.1093/jamia/ocaa282. http://europepmc.org/abstract/MED/33236109 .6000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Or C, Tao D. Usability study of a computer-based self-management system for older adults with chronic diseases. JMIR Res Protoc. 2012 Nov 08;1(2):e13. doi: 10.2196/resprot.2184. https://www.researchprotocols.org/2012/2/e13/ v1i2e13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yan M, Or C. A 12-week pilot study of acceptance of a computer-based chronic disease self-monitoring system among patients with type 2 diabetes mellitus and/or hypertension. Health Informatics J. 2019 Sep;25(3):828–43. doi: 10.1177/1460458217724580. https://journals.sagepub.com/doi/10.1177/1460458217724580?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 97.Xie Z, Liu K, Or C, Chen J, Yan M, Wang H. An examination of the socio-demographic correlates of patient adherence to self-management behaviors and the mediating roles of health attitudes and self-efficacy among patients with coexisting type 2 diabetes and hypertension. BMC Public Health. 2020 Aug 12;20:1227. doi: 10.1186/s12889-020-09274-4. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-09274-4 .10.1186/s12889-020-09274-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cheung DS, Or CK, So MK, Tiwari A. Usability testing of a smartphone application for delivering Qigong training. J Med Syst. 2018 Sep 05;42(10):191. doi: 10.1007/s10916-018-1048-9.10.1007/s10916-018-1048-9 [DOI] [PubMed] [Google Scholar]
- 99.Liu K, Or CK, So M, Cheung B, Chan B, Tiwari A, Tan J. A longitudinal examination of tablet self-management technology acceptance by patients with chronic diseases: integrating perceived hand function, perceived visual function, and perceived home space adequacy with the TAM and TPB. Appl Ergon. 2022 Apr;100:103667. doi: 10.1016/j.apergo.2021.103667.S0003-6870(21)00314-8 [DOI] [PubMed] [Google Scholar]
- 100.Or CK, Karsh BT, Severtson DJ, Burke LJ, Brown RL, Brennan PF. Factors affecting home care patients' acceptance of a Web-based interactive self-management technology. J Am Med Inform Assoc. 2011;18(1):51–9. doi: 10.1136/jamia.2010.007336. http://europepmc.org/abstract/MED/21131605 .jamia.2010.007336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chen T, Or CK. Development and pilot test of a machine learning-based knee exercise system with video demonstration, real-time feedback, and exercise performance score. Proc Hum Factors Ergon Soc Annu Meet. 2021 Nov 12;65(1):1519–23. doi: 10.1177/1071181321651109. [DOI] [Google Scholar]
- 102.Xie Z, Kalun Or C. Acceptance of mHealth by elderly adults: a path analysis. Proc Hum Factors Ergon Soc Annu Meet. 2021 Feb 09;64(1):755–9. doi: 10.1177/1071181320641174. [DOI] [Google Scholar]
- 103.Chen T, Kalun Or C, Chen J. A systematic review and meta-analysis of randomized controlled trials to evaluate technology-supported exercise programs for knee health. Proc Hum Factors Ergon Soc Annu Meet. 2021 Feb 09;64(1):639–40. doi: 10.1177/1071181320641145. [DOI] [Google Scholar]
- 104.Karsh BT, Holden RJ, Or CK. Human factors and ergonomics of health information technology implementation. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2nd ed. Boca Raton, FL, USA: CRC Press; 2011. pp. 249–64. [Google Scholar]
- 105.Or CK, Holden RJ, Valdez R. Human factors engineering and user-centered design for mobile health technology: enhancing effectiveness, efficiency, and satisfaction. Human-Automation Interaction: Mobile Computing. 2022 (forthcoming) [Google Scholar]
- 106.Or CK, Liu K, So MK, Cheung B, Yam LY, Tiwari A, Lau YF, Lau T, Hui PS, Cheng HC, Tan J, Cheung MT. Improving self-care in patients with coexisting type 2 diabetes and hypertension by technological surrogate nursing: randomized controlled trial. J Med Internet Res. 2020 Mar 27;22(3):e16769. doi: 10.2196/16769. https://www.jmir.org/2020/3/e16769/ v22i3e16769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Or CK, Karsh BT. A systematic review of patient acceptance of consumer health information technology. J Am Med Inform Assoc. 2009;16(4):550–60. doi: 10.1197/jamia.M2888. http://europepmc.org/abstract/MED/19390112 .M2888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hsieh YW, Wu CY, Lin KC, Chang YF, Chen CL, Liu JS. Responsiveness and validity of three outcome measures of motor function after stroke rehabilitation. Stroke. 2009 Apr;40(4):1386–91. doi: 10.1161/STROKEAHA.108.530584.STROKEAHA.108.530584 [DOI] [PubMed] [Google Scholar]
- 109.Sears ED, Chung KC. Validity and responsiveness of the Jebsen-Taylor Hand Function Test. J Hand Surg Am. 2010 Jan;35(1):30–7. doi: 10.1016/j.jhsa.2009.09.008. http://europepmc.org/abstract/MED/19954898 .S0363-5023(09)00758-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Schepers VP, Ketelaar M, Visser-Meily JM, Dekker J, Lindeman E. Responsiveness of functional health status measures frequently used in stroke research. Disabil Rehabil. 2006 Sep 15;28(17):1035–40. doi: 10.1080/09638280500494694.L25166538657XQN0 [DOI] [PubMed] [Google Scholar]
- 111.Santisteban L, Térémetz M, Bleton JP, Baron JC, Maier MA, Lindberg PG. Upper limb outcome measures used in stroke rehabilitation studies: a systematic literature review. PLoS One. 2016 May 6;11(5):e0154792. doi: 10.1371/journal.pone.0154792. https://dx.plos.org/10.1371/journal.pone.0154792 .PONE-D-15-54915 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist.
Details of the search.
Details of the characteristics of the included trials.
Outcomes examined in the included trials.
Forest plots of the meta-analyses.
Results of subgroup analyses.


