Key Point
Hemodialysis patients showed resilience in their ability to adapt to the new reality of their hemodialysis treatments.
COVID-19 was not associated with negative effects on patients' medical care.
Keywords: dialysis, COVID-19 pandemics, hemodialysis, patient experience, qualitative methods, Quebec, SARS-CoV-2
Visual Abstract
Abstract
Background
Hemodialysis patients have faced unique challenges during the COVID-19 pandemic. They face high risk of death if infected and have unavoidable exposure to others when they come to hospital three times weekly for their life-saving treatments. The objective of this study was to gain a better understanding of the scope and magnitude of the effects of the pandemic on the lived experience of patients receiving in-center hemodialysis.
Methods
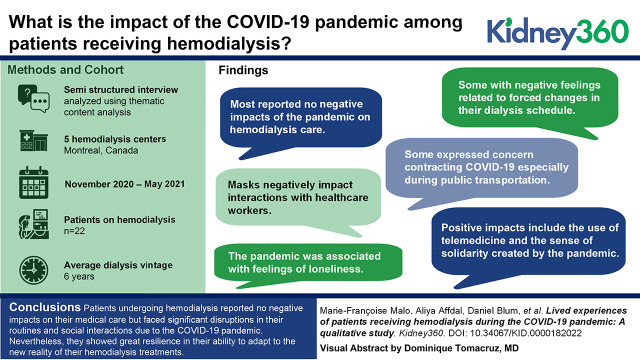
We conducted semi-structured interviews with 22 patients who were undergoing dialysis treatments in five hemodialysis centers in Montreal from November 2020 to May 2021. Interviews were transcribed and then analyzed using thematic content analysis.
Results
Most participants reported no negative effects of the COVID-19 pandemic on their hemodialysis care. Several patients had negative feelings related to forced changes in their dialysis schedules, and this was especially pronounced for indigenous patients in a shared living situation. Some patients were concerned about contracting COVID-19, especially during public transportation, whereas others expressed confidence that the physical distancing and screening measures implemented at the hospital would protect them and their loved ones. Some participants reported that masks negatively affected their interactions with health care workers, and for many others, the pandemic was associated with feelings of loneliness. Finally, some respondents reported some positive effects of the pandemic, including use of telemedicine and creating a sense of solidarity.
Conclusions
Patients undergoing hemodialysis reported no negative effects on their medical care but faced significant disruptions in their routines and social interactions due to the COVID-19 pandemic. Nevertheless, they showed great resilience in their ability to adapt to the new reality of their hemodialysis treatments. We also show that studies focused on understanding the lived experiences of indigenous patients and patients from different ethnic backgrounds are needed in order reduce inequities in care during public health emergencies.
Introduction
Patients receiving hemodialysis have been particularly vulnerable during the coronavirus disease 2019 (COVID-19) pandemic. Their impaired immunity and high burden of comorbid diseases put them at increased risk of death and severe complications from COVID-19 (1–6). To reduce transmission of COVID-19, public health agencies quickly mandated physical distancing and self-isolation measures (7). However, patients receiving in-center hemodialysis cannot self-isolate: uniquely, they must come to the center three times weekly for life-saving treatments, which can last several hours (8), resulting in unavoidable and regular exposure to health care workers (HCWs) and other patients. Many patients also use public transportation or ride share to get to the dialysis unit (9,10). Further, hemodialysis units are often crowded, making physical distancing difficult to achieve (11), increasing the probability of patients’ exposure to COVID-19.
In the Canadian province of Quebec, a public health emergency and a general lockdown were declared on March 13, 2020. During the first wave of COVID-19, Quebec was considered a hot spot, with the city of Montreal being particularly affected with very high rates of community transmission (12). Numerous protective measures were quickly implemented in dialysis units (11), such as symptom assessments before entering the treatment area, isolating suspected or confirmed cases, sanitizing, social distancing, and mandatory mask wearing (13). Infection rates approached 25% in patients receiving in-center hemodialysis in Montreal (11,14).
Patients’ experiential knowledge is key to improving their care (15,16). Very few studies have examined the experiences of in-center hemodialysis patients during the COVID-19 pandemic. The purpose of this study, which is part of a larger study documenting the effect of COVID-19 hemodialysis clinics in Quebec (17,18), was to gather hemodialysis patients’ perspectives and experiences after the first wave of COVID-19 infections. A better understanding of the scope and magnitude of the disruptions faced by hemodialysis patients during the pandemic would help to inform interventions during public health emergencies.
Materials and Methods
This exploratory study relied on semistructured interviews with dialysis patients. We used the consolidated criteria for reporting qualitative research checklist (19). Recruitment and interviews were carried out between November 2020 and May 2021 during the second and third waves of COVID-19 infections in Quebec. Convenience and purposive sampling (20) were used to recruit hemodialysis patients from five hemodialysis centers in the Montreal area. Purposive sampling consisted in recruiting participants with varying sociodemographic characteristics (age, sex, type of work, ethnic origin, etc.) (20). Patients were recruited by a local coordinator at each site and were referred to the research team. Participants received $30 as compensation for their participation.
Interviews were conducted in English or French over the telephone (9) or by videoconference (13). Two different experienced interviewers (A.A. and F.B.) carried out the interviews; they had no involvement with the care provided in the dialysis units, nor were they in any way connected with the participants. The interviews lasted between 20 and 78 minutes and were digitally recorded and transcribed. The Centre hospitalier de l’Université de Montréal Research Ethics Board approved the study (CE 20.065, MP-02-2021-9006), and all participants provided informed consent. The interview transcripts were sent for approval to the participants we were able to reach.
Themes covered during the interviews were outlined in an interview guide with open-ended questions that are summarized in Table 1. The interview guide was developed by the research team and pretested by a patient partner. The interview guide was modified as new topics emerged from the interviews (20,21).
Table 1.
Themes addressed during the qualitative interviews
| Themes |
|---|
| Overall experience of hemodialysis care during the pandemic |
| Mode of transportation to the dialysis unit |
| Fears and concerns related to the pandemic |
| Interaction between health care workers and patients |
| Recommendations |
| Effect of the pandemic on mental health and feelings of loneliness |
Patients were identified by self-identified gender. We used a qualitative descriptive approach to describe hemodialysis patients’ experiences during the COVID-19 pandemic (22–24). The goal of this pragmatic approach is to stay close to the data and provide a comprehensive summary of the topic studied (23), using thematic and content analysis (21,24). The latest version of NVivo (QSR International) was used to facilitate the analysis. All members of the research team developed the coding frame. M.F.M. coded the interviews, and no new codes were created after the 12th interview. The number of participants allowed for data saturation (25). A.A. coded 32% of the raw data, with the rate of coding agreement assessed at 88%, and disagreements were discussed. Coded quotes were then organized by theme and subtheme.
Results
Participants’ Characteristics
Over the study period, 39 patients were approached, 32 agreed to participate, and 22 were interviewed. Two patients declined after being contacted, three declined because of personal and health issues, and five could not be reached. Participants were 13 men and nine women, with a mean age of 60 years (Table 2). They had spent an average of 6 years in dialysis, and ten were listed for a transplant. Fourteen identified as White, and four patients were members of Indigenous communities (Table 2).
Table 2.
Participants’ characteristics
| Characteristics | N=22, n (%) |
|---|---|
| Sex | |
| Men/women | 13 (59)/9 (41) |
| Age, yr, (mean±SD) | 60.5±16.7 (range 30–90) |
| Ethnic group | |
| White | 14 (64) |
| Indigenous | 4 (18) |
| Other | 4 (18) |
| Hemodialysis center | |
| Center 1 | 5 (23) |
| Center 2 | 6 (27) |
| Center 3 | 4 (18) |
| Center 4 | 4 (18) |
| Center 5 | 3 (14) |
| Employment status | |
| Retired | 12 (55) |
| Unemployed | 7 (32) |
| Employed full time/part time | 2 (9) |
| Student | 1 (4) |
| Level of education | |
| Elementary | 3 (14) |
| High school | 10 (45) |
| Technical school or college | 5 (23) |
| University | 4 (18) |
| Annual family income, $ | |
| <30,000 | 9 (41) |
| 30,000–99,999 | 6 (27) |
| >100,000 | 1 (4.5) |
| No income | 1 (4.5) |
| Preferred not to answer | 5 (22) |
| Marital status | |
| Married/civil union | 14 (64) |
| Single | 5 (23) |
| Widowed | 2 (9) |
| Separated/divorced | 1 (4) |
| Number of years on dialysis, mean±SD | 6.0±6.2 (range 1–27) |
| Listed for a kidney transplant | 10 (45) |
| Tested for COVID-19a | 22 (100) |
| Number of times tested for COVID-19 (range 2–25), mean±SD | 8±6.8 |
COVID-19, coronavirus disease 2019.
Four patients mentioned during the interviews that they were positive for COVID-19.
Qualitative Interviews
The themes identified during the interviews are presented in Table 3 with interview excerpts.
Table 3.
Themes addressed during the qualitative interviews
| Themes and Interview Excerpts | N =22 |
|---|---|
| Effects of the COVID-19 pandemic on hemodialysis care and routine | |
Effect on hemodialysis care
|
14 |
Change in their routine
|
4 |
Change in their routine regarding their mode of transportation
|
9 |
Switching from in-center dialysis to home hemodialysis
|
8 |
| Effect of COVID-19 infection risk and mitigation measures | |
Concerns related to their own infection risk
|
13 |
|
Risk management in the hemodialysis unit Appropriate measures
|
16 |
Mixed feelings
|
4 |
Prohibition of visitors
|
9 |
Fear of infecting their loved ones
|
13 |
| Effect of COVID-19 pandemic on relationships | |
Interactions with health care workers
|
11 |
COVID-19 pandemic and isolation from loved ones
|
16 |
COVID-19, coronavirus disease 2019.
Effects of the COVID-19 Pandemic on Hemodialysis Care and Routine
The majority of patients mentioned that the protective measures and changes implemented at the start of the pandemic “didn’t really affect the treatments themselves” (P19, woman).
However, one significant effect was the changes in their routine related to infection prevention and control measures. Four patients had to change dialysis units, two of whom were from Indigenous communities: “we don’t have a dialysis clinic … And before the COVID, they went to different dialysis clinics … So, they were all different, different areas where they went, but ever since the COVID happened, we have, we’ve all been placed at the same time, at the same hospital” (P14, man). Some patients mentioned having difficulty coping with a modification of their dialysis schedule: “I was doing in the morning. I was liking the mornings, so I don’t really like it in the evenings doing my hemodialysis because I cannot sleep well when I go home” (P15, man). The other changes were requested by patients who felt safer in another unit or who had to change after being infected by COVID-19.
Another change reported was the modification in their transportation to the unit. Two participants stopped using public transit because they feared being infected: “Since March or April, I’ve been getting there myself by car, and I make sure to be in the outdoor parking lot to avoid being in the elevators” (P10, man).
Although switching from in-center to home hemodialysis would limit exposure to COVID-19 in the hospital, no participants had considered it: “I prefer going to the hospital even if we’re in the middle of a COVID-19 pandemic than doing this at home” (P22, man).
Effect of COVID-19 Infection Risk and Mitigation Measures
Concerns Related to Their Own Infection Risk.
Patients expressed different attitudes about the risk of being infected with COVID-19. Some stated that they were “not afraid of the COVID” (P15, man). One patient had a fatalistic attitude about being infected: “If I have to catch it, it’s because the good Lord wanted it this way” (P14, woman). On the other hand, some patients reported being afraid of dying of COVID-19. Others were more concerned than afraid: “I was, I wouldn’t say afraid, I wasn’t in fear, but I was, you know, uneasy that I may catch the coronavirus” (P4, man). The idea of going to the hospital multiple times a week and being infected in their unit seemed to concern some patients, especially those who “knew a person that got the COVID while at the hospital, […], so that […], added a little bit more paranoia” (P10, man).
Effect of Infection Control and Prevention Measures in the Hemodialysis Unit.
In order to prevent COVID-19 infection within dialysis units, strict infection prevention and control measures were rapidly implemented. These included wearing masks, physical distancing when possible, use of plexiglass between stations, and screening questionnaires with regular nasopharyngeal swabbing at each treatment (11). Despite those onerous measures, most patients reported being satisfied, believing that “these measures are good” (P15, woman) and being “very enthusiastic about what’s happening in that unit” (P08, man). They also had good words for HCWs in their units and their ability to adapt.
On the other hand, some patients did criticize measures in their unit, which some felt were inconsistent: “…wearing the mask and washing the hands is adequate … everybody touches the same scale, everybody uses the same washroom, everyone uses the same waiting room, so I don’t think that’s very effective. Yes, we’re using the same pen to write our weights, we’re touching the scale to weigh ourselves, how is that helping?” (P20, woman).
The prohibition of visitors was also well accepted by most patients. That said, it appeared to affect elderly patients from indigenous communities disproportionately who could no longer communicate with HCWs due to the language barrier, which previously their visitors helped to bridge: “When the COVID first happened, they were not allowed to bring their escorts and there was this lady, she only speaks her native tongue, and there was no translator for her … when you are elderly and you can’t speak the language that they’re using to communicate you with at the dialysis, it’s kind of scary for her” (P10, man).
Finally, some patients mentioned the positive effect of health measures on their social lives and on the hospital, and they hoped it will last well beyond the pandemic because “it’s good for newer generations. It’s showing young people … some good, hygienic habits to maintain” (P7, woman).
Fears of Infecting Their Loved Ones.
Several patients reported fears of infecting their families and putting them at risk. Some decided to “stay away from them” (P13, woman). Patients from indigenous communities feared for their communities once allowed to return to their remote villages and took the decision to not “see anybody” (P13, woman). The health measures implemented by dialysis units and the government overall helped to reduce patients’ stress and were viewed by patients as a way to protect themselves and their families. They were also willing to take every step necessary to minimize their risk of exposure while “avoiding situations that were higher risk” (P7, man).
Effect of COVID-19 on Relationships
Interactions with HCWs.
Patients who had been in hemodialysis for a long time reported that the HCWs, particularly doctors, were more distant than before and that they would “do everything they can to avoid being closer” (P3, man). Patients also had fewer interactions with HCWs and would “chat less and less” (P1, man), and masks prevented patients from seeing HCWs’ nonverbal expressions. Other patients, mostly women, mentioned that physical distancing had an effect on their relationships with HCWs, and that they found it “a little bit hurtful” (P19, woman). On a more positive note, telephone appointments “have been very welcome” (P4, man).
COVID-19 Pandemic and Isolation from Loved Ones.
Patients reported “feeling down sometimes” (P11, man) during the COVID-19 pandemic and missed interactions with family members and friends. “It gets depressing sometimes. But there have been times where I have cried in my room missing my family” (P14, woman). Social media was used as a way to cope with isolation from their loved ones. Some would even “see each other every day through FaceTime” (P17, man). Other participants accepted this distance, inevitable in the context, affirming: “What we’re hoping is that we all get through it and be able to give each other hugs later” (P11, man). The feeling of loneliness and isolation was reported more often by women than men. Despite that, others mentioned that the pandemic fostered a sense of solidarity and support and that “in terms of helping each other, going to help neighbors, making something to eat then bringing it next door … stopped to think that everything is a given” (P18, woman).
Discussion
Our study documents hemodialysis patients’ lived experiences during the COVID-19 pandemic in the Canadian province of Quebec, which was particularly affected by COVID-19 in the first and second waves of the pandemic (26). Fortunately, the pandemic did not appear to alter patients’ experiences related to their hemodialysis care. However, patients were profoundly affected by changes to their overall routine, which included changes in their mode of transportation to and from the unit due to fear of contracting COVID-19, transfers to another unit, and imposed changes to their schedules. These two last factors particularly affected the four indigenous patients we interviewed. These patients were originally from northern remote regions in Quebec, and despite already being in a shared living situation in Montreal from before the pandemic began, all patients in this shared living situation were cohered to receive their dialysis treatments together after the pandemic began. Although most patients were fearful of contracting COVID-19 and were appreciative of the implemented infection prevention and control measures that they felt would protect them and their loved ones, some felt the measures made them distant from their HCWs and experienced isolation from loved ones. Interestingly, patients who were in hemodialysis the longest were least affected by the changes as a result of the pandemic. Hemodialysis patients demonstrate exceptional resilience, and it may be that more time spent in hemodialysis increases this resilience.
There are a few other studies in this field. Similar to our results, Sousa et al. (27) reported that some patients found adherence to protective measures as a coping strategy that helped them to accept changes in their routine. Patients also reported that COVID-19 led to a decrease in physical activity, difficulty complying with dietary and fluid recommendations, and the need to consult a nephrologist, all of which were not mentioned in our participants’ interviews.
Another US study surveyed 49 in-center hemodialysis patients to determine the effect of the COVID-19 pandemic on their psychological health (10). Their participants were moderately to extremely worried about leaving their homes for dialysis treatment, and like in our study, patients feared getting infected in the unit or during their transport to hemodialysis. As in our study, switching to home dialysis therapy was not an option for the majority. The desire to continue to go to the unit could be further attributed to the importance of their routine and also the desire to break the mandatory COVID-19 isolation. In a survey conducted in Ireland, participants reported changes in their interactions with medical staff (23).
Both women and men reported feeling lonely and isolated from their loved ones, but women seemed to be more affected than men. This difference could potentially be explained by a social desirability bias, where men are less prone to discuss psychological issues (28). Participants in our study did not report a major effect on their mental health and increased suicidal ideation. This differs from studies that have shown increased psychological distress and anxiety in different countries and among the Quebec population (29–32). In the dialysis population, the effects of the pandemic on mental health vary across studies. In the US study mentioned above, participants reported feeling lonely, and some developed depressive symptoms (10). Another study showed that the mental health of dialysis patients appeared unaffected by the pandemic (33). The authors hypothesized that dialysis patients are used to adapting to various difficulties because of their disease and dialysis treatment and have therefore developed coping mechanisms that could help them face the challenges associated with a pandemic (33). The need for dialysis patients to report to the hospital three times weekly could have possibly contributed to easing their feelings of loneliness and isolation in that study (33). This could well be the case for patients interviewed in our study, who, despite social isolation and distance from their HCWs, felt a strong sense of belonging to a community. Another study had similar findings where patients looked forward to their dialysis treatment for social interactions, even if these were limited (34).
We recognize our study’s limitations. We were only able to interview patients receiving dialysis treatment in an urban region predominantly affected by the first and second waves of the COVID-19 pandemic. Most of our patients were White and spoke French or English, and thus the results do not reflect the reality of dialysis patients from other ethnic backgrounds. Our ability to draw definitive conclusions regarding the experience of indigenous patients is also limited and requires further study. Finally, the majority of our patients were married or in civil unions, which may have lessened the effect of the pandemic on their mental health.
Some recommendations can be made on the basis of our results in order to improve patient care during a pandemic or other public health emergency. First, as demonstrated in our study, hemodialysis patients seem very attached to their care routine. Maintaining this routine should accordingly be of the outmost importance, in order to minimize patients’ stress in times of uncertainty. If this is not possible, any disruptions should be communicated rapidly with the reasons, and eliminated as soon as feasible. Second, our findings show that dialysis, for patients, is not only a place of care but also a place of life. Effective communication with HCWs should be prioritized, and efforts should be made to encourage safe social contacts with other patients and HCWs when desired. Third, even if our study did not show dire mental health consequences for patients during the COVID-19 pandemic, these results should not be generalized because mental health is personal to each individual. Units should put protocols in place to monitor patients’ mental health over time. Fourth, special attention should be paid during health emergencies to marginalized populations such as indigenous communities in order to prevent and mitigate inequities in care.
In conclusion, the aim of this study was to report the experiences of in-center dialysis patients in an urban area heavily affected by the COVID-19 pandemic. The patients interviewed showed resilience and an ability to adapt to uncertainty. Patients were willing to adhere to measures to protect themselves and their loved ones but expressed opinions on how the disruptions to their lives could be minimized, including improving their interactions with health care. These results highlight the importance of considering patients’ perspectives in the implementation of protective measures in case of a pandemic or health emergency. Further studies are also needed to understand the experiences and responses of indigenous patients and patients from different ethnic backgrounds better in order to reduce inequities in care.
Disclosures
A. Affdal reports being Scientific Director for the Canadian Journal of Bioethics. W. Beaubien-Souligny reports honoraria from Baxter. D. Blum reports honoraria from AstraZeneca and Otsuka. M.-C. Fortin reports being a member of the ethics committee of Transplant Quebec, the Collège des médecins du Québec, and the Canadian Society of Transplantation and being a member of different committees of the Canadian Blood Services. A.-C. Nadeau-Fredette reports a current scholarship from Fonds de la recherche du Québec en Santé (FRQS). R.S. Suri reports the honoraria from Amgen and Otskuka and an advisory or leadership role for the Canadian Institutes of Health Research Institute of Circulatory and Respiratory Health and the Canadian Society of Nephrology. M. Vasilevsky reports ownership interest in the Bank of America, Birchcliff Energy Ltd., Brookfield Infrastructure Partners, CCL Industries, Inc., CAE, Inc., Canadian National Railway, Cenovus Energy, Eli Lilly, Enbridge, Inc., Inovio Pharmaceuticals, Microsoft, Parkland Corp., Precigen, Inc., Sirius XM Holdings, Stellantis N.V., Teck Resources Ltd., Toronto Dominion Bank, West Fraser Timber Co. Ltd., and Yamana Gold, Inc.; and research funding from CIHR via Sunnybrooke Research Institute and GSK/PPD Investigator Services. All remaining authors have nothing to disclose.
Funding
This research project was funded by an operating grant 447760 (COVID-19 Rapid Research Funding Opportunity) from the Canadian Institutes of Health Research.
Acknowledgments
We would like to thank all of the participants in this study.
Author Contributions
A. Affdal, F. Ballesteros Gallego, M.-L. Caron, M.-F. Malo, A.-C. Nadeau-Fredette, N. Rios, and M. Vasilevsky were responsible for the investigation; A. Affdal, F. Ballesteros Gallego, W. Beaubien-Souligny, M.-F. Malo, A.-C. Nadeau-Fredette, and R.S. Suri reviewed and edited the manuscript; A. Affdal, F. Ballesteros Gallego, M.-C. Fortin, and M.-F. Malo were responsible for the formal analysis; W. Beaubien-Souligny, M.-C. Fortin, A.-C. Nadeau-Fredette, and R.S. Suri were responsible for conceptualization; W. Beaubien-Souligny, A.-C. Nadeau-Fredette, and R.S. Suri were responsible for funding acquisition; D. Blum, M.-L. Caron, N. Rios, and M. Vasilevsky were responsible for data curation; M.-C. Fortin was responsible for the methodology; M.-C. Fortin and M.-F. Malo wrote the original draft of the manuscript; and N. Rios was responsible for project administration.
References
- 1.Syed-Ahmed M, Narayanan M: Immune dysfunction and risk of infection in chronic kidney disease. Adv Chronic Kidney Dis 26: 8–15, 2019 [DOI] [PubMed] [Google Scholar]
- 2.Webster AC, Nagler EV, Morton RL, Masson P: Chronic kidney disease. Lancet 389: 1238–1252, 2017 [DOI] [PubMed] [Google Scholar]
- 3.Haarhaus M, Santos C, Haase M, Mota Veiga P, Lucas C, Macario F: Risk prediction of COVID-19 incidence and mortality in a large multi-national hemodialysis cohort: Implications for management of the pandemic in outpatient hemodialysis settings. Clin Kidney J 14: 805–813, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bell S, Campbell J, McDonald J, O’Neill M, Watters C, Buck K, Cousland Z, Findlay M, Lone NI, Metcalfe W, Methven S, Peel R, Almond A, Sanu V, Spalding E, Thomson PC, Mark PB, Traynor JP; Scottish Renal Registry : COVID-19 in patients undergoing chronic kidney replacement therapy and kidney transplant recipients in Scotland: Findings and experience from the Scottish renal registry. BMC Nephrol 21: 419, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Creput C, Fumeron C, Toledano D, Diaconita M, Izzedine H: COVID-19 in patients undergoing hemodialysis: Prevalence and asymptomatic screening during a period of high community prevalence in a large paris center. Kidney Med 2: 716–723.e1, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alfano G, Ferrari A, Magistroni R, Fontana F, Cappelli G, Basile C: The frail world of haemodialysis patients in the COVID-19 pandemic era: A systematic scoping review. J Nephrol 34: 1387–1403, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akbarialiabad H, Kavousi S, Ghahramani A, Bastani B, Ghahramani N: COVID-19 and maintenance hemodialysis: A systematic scoping review of practice guidelines. BMC Nephrol 21: 470, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rombolà G, Brunini F: COVID-19 and dialysis: Why we should be worried. J Nephrol 33: 401–403, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiner DE, Watnick SG: Hemodialysis and COVID-19: An Achilles’ heel in the pandemic health care response in the United States. Kidney Med 2: 227–230, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee J, Steel J, Roumelioti ME, Erickson S, Myaskovsky L, Yabes JG, Rollman BL, Weisbord S, Unruh M, Jhamb M: Psychosocial impact of COVID-19 pandemic on patients with end-stage kidney disease on hemodialysis. Kidney360 1: 1390–1397, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beaubien-Souligny W, Nadeau-Fredette AC, Nguyen MN, Rios N, Caron ML, Tom A, Suri Md RS; Quebec Renal Network COVID-19 Study Investigators : Infection control measures to prevent outbreaks of COVID-19 in Quebec hemodialysis units: A cross-sectional survey. CMAJ Open 9: E1232–E1241, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gouvernement du Québec : Data on COVID-19 in Quebec. Available at: https://www.quebec.ca/en/health/health-issues/a-z/2019-coronavirus/situation-coronavirus-in-quebec. Accessed September 23, 2021
- 13.Institut National de Santé Publique : COVID-19: Infection Prevention and Control Measures for Hemodialysis Units. Available at: https://www.inspq.qc.ca/en/publications/2980-infection-prevention-control-measures-hemodialysis-units-covid19. Accessed September 23, 2021
- 14.Canadian Broadcasting Corporation : Cancer, dialysis patients infected as COVID-19 sweeps through Montreal’s Sacré-Coeur hospital. Available at: https://www.cbc.ca/news/canada/montreal/sacr%C3%A9-c%C5%93ur-de-montr%C3%A9al-hospital-montreal-covid-19-1.5540492. Accessed September 24, 2021
- 15.Coulter A: Engaging Patients in Healthcare, Maidenhead, United Kingdom, Open University Press, 2011 [Google Scholar]
- 16.Caron-Flinterman JF, Broerse JEW, Bunders JF: The experiential knowledge of patients: A new resource for biomedical research? Soc Sci Med 60: 2575–2584, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Beaudet M, Ravensbergen L, DeWeese J, Beaubien-Souligny W, Nadeau-Fredette AC, Rios N, Caron ML, Suri RS, El-Geneidy A: Accessing hemodialysis clinics during the COVID-19 pandemic. Transp Res Interdiscip Perspect 13: 100533, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goupil R, Benlarbi M, Beaubien-Souligny W, Nadeau-Fredette AC, Chatterjee D, Goyette G, Gunaratnam L, Lamarche C, Tom A, Finzi A, Suri RS; Réseau Rénal Québécois (Quebec Renal Network) COVID-19 Study Investigators : Short-term antibody response after 1 dose of BNT162b2 vaccine in patients receiving hemodialysis. CMAJ 193: E793–E800, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tong A, Sainsbury P, Craig J: Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care 19: 349–357, 2007 [DOI] [PubMed] [Google Scholar]
- 20.Green J, Thorogood N: Qualitative Methods for Health Research, 3rd Ed., London, UK, SAGE, 2014 [Google Scholar]
- 21.Miles MB, Huberman MA: Qualitative Data Analysis: A Source Book of New Methods, 1st Ed., Newbury Park, CA, SAGE, 1984 [Google Scholar]
- 22.Sandelowski M: What’s in a name? Qualitative description revisited. Res Nurs Health 33: 77–84, 2010 [DOI] [PubMed] [Google Scholar]
- 23.Sandelowski M: Whatever happened to qualitative description? Res Nurs Health 23: 334–340, 2000 [DOI] [PubMed] [Google Scholar]
- 24.Green J, Thorogood N: Beginning Data Analysis. In: Qualitative Methods for Health Research, London, Sage, 2018, pp 249–284 [Google Scholar]
- 25.Lessard-Hébert M, Goyette G, Boutin G: La recherche qualitative: Fondements et pratiques, Montreal, Canada, Éditions nouvelles, 1995 [Google Scholar]
- 26.Institut national de santé publique du Québec : Données COVID-19 au Québec. Available at: https://www.inspq.qc.ca/covid-19/donnees. Accessed March 24, 2022
- 27.Sousa H, Frontini R, Ribeiro O, Paúl C, Costa E, Amado L, Miranda V, Ribeiro F, Figueiredo D: Caring for patients with end-stage renal disease during COVID-19 lockdown: What (additional) challenges to family caregivers? Scand J Caring Sci 36: 215–224, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kelly CA, Soler-Hampejsek E, Mensch BS, Hewett PC: Social desirability bias in sexual behavior reporting: Evidence from an interview mode experiment in rural Malawi. Int Perspect Sex Reprod Health 39: 14–21, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Généreux M, Schluter PJ, Landaverde E, Hung KK, Wong CS, Mok CPY, Blouin-Genest G, O’Sullivan T, David MD, Carignan ME, Champagne-Poirier O, Pignard-Cheynel N, Salerno S, Lits G, d’Haenens L, Coninck D, Matthys K, Champagne E, Burlone N, Qadar Z, Herbosa T, Ribeiro-Alves G, Law R, Murray V, Chan EYY, Roy M: The evolution in anxiety and depression with the progression of the pandemic in adult populations from eight countries and four continents. Int J Environ Res Public Health 18: 4845, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Institut national de santé publique du Québec : COVID-19—Sondages sur les attitudes et comportements des adultes québécois. Pandémie, bien-être émotionnel et santé mentale. Available at: https://www.inspq.qc.ca/covid-19/sondages-attitudes-comportements-quebecois/sante-mentale-janvier-2021. Accessed October 5, 2021
- 31.Hwang TJ, Rabheru K, Peisah C, Reichman W, Ikeda M: Loneliness and social isolation during the COVID-19 pandemic. Int Psychogeriatr 32: 1217–1220, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu B: Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Glob Health Res Policy 5: 27, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bonenkamp AA, Druiventak TA, van Eck van der Sluijs A, van Ittersum FJ, van Jaarsveld BC, Abrahams AC; DOMESTICO study group : The impact of COVID-19 on the mental health of dialysis patients. J Nephrol 34: 337–344, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Antoun J, Brown DJ, Jones DJW, Sangala NC, Lewis RJ, Shepherd AI, McNarry MA, Mackintosh KA, Mason L, Corbett J, Saynor ZL: Understanding the impact of initial COVID-19 restrictions on physical activity, wellbeing and quality of life in shielding adults with end-stage renal disease in the United Kingdom dialysing at home versus in-centre and their experiences with telemedicine. Int J Environ Res Public Health 18: 3144, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]