Abstract
Background:
Despite their broad commitment to family-centred care, children’s hospitals and associated pediatric intensive care units (PICUs) restricted family presence during the COVID-19 pandemic. This study aimed to describe family presence policies and practices in Canadian PICUs from March to May 2020, and their evolution by August to December 2020.
Methods:
We conducted an environmental scan of family presence policies and restrictions in all 19 Canadian PICUs using 2 methods. We conducted a literature review of public-facing visitation policy documents in June 2020 using a standardized data extraction form. We also administered a cross-sectional survey of PICU leadership (managers and physician chiefs) between August and December 2020 by telephone or videoconferencing. We used inductive content analysis to code qualitative data, generating summative count data. We analyzed quantitative data descriptively.
Results:
As part of the literature search, we collected 2 (12%) PICU-specific, 14 (82%) pediatric-specific and 1 (6%) hospital-wide visitation policy documents from the early pandemic. One policy document provided guidance on all of the policy elements sought; the number of enabled caregivers was not included in the documents for 7 of 19 units (37%). All 19 Canadian PICUs were represented among the 24 survey respondents (15 physician chiefs and 9 operations or clinical managers). Before the COVID-19 pandemic, all units allowed the presence of 2 or more family members. Early in the pandemic, reported practices limited the number of adult caregivers for patients without SARS-CoV-2 infection to 1 (n = 21/24, 88%) or 2 (n = 3/24, 12%); all units prohibited siblings. Some centres restricted caregivers from switching bedside presence with one another (patients without SARS-CoV-2 infection: n = 16/23, 70%; patients with confirmed or suspected SARS-CoV-2 infection: n = 20/23, 87%); leaving their child’s PICU room (patients without SARS-CoV-2 infection: n = 1/24, 4%; patients with confirmed or suspected SARS-CoV-2 infection: n = 16/24, 67%); and joining in-person rounds (patients without SARS-CoV-2 infection: n = 9/22, 41%; patients with confirmed or suspected SARS-CoV-2 infection: n = 17/22, 77%). All respondents endorsed policy exceptions during end-of-life care. Some reported policies and practices were adapted over the study period.
Interpretation:
Early COVID-19–related family presence policies in Canadian PICUs varied among centres. Although some centres adapted policies and practices, this study revealed ongoing potential threats to family centred care at the mid-pandemic stage.
In response to the COVID-19 pandemic, hospitals worldwide implemented sweeping changes to visitation policies. Although the changes in pediatric facilities were less restrictive than in their adult counterparts, the impacts felt were still substantial.1–4 In children’s hospitals, the pediatric intensive care unit (PICU) is a frightening environment for children and parents; the risk of long-term morbidity is ever-present,5,6 and most deaths occur here.7
Recognizing that family members are central to a child’s experience of critical illness,8 Canadian children’s hospitals and their PICUs have traditionally advocated for and adopted a framework of family-centred care.9–14 Typical PICU practices include family participation in care, open visitation and unrestricted parental presence at the bedside.15,16 Restrictions to such practices were ethically justifiable at the outset of the COVID-19 pandemic,17,18 but they had the potential to create considerable harm.19–21
An examination of policy impacts during the COVID-19 pandemic requires an understanding of context. During the early months of the pandemic, Canadian adult intensive care units generally restricted all family presence.22 In the United States, children’s hospitals frequently limited presence to 1 (49%) or 2 (31%) caregivers.23 International surveys of restrictions during the pandemic described decreased family participation in rounds,24,25 restriction to 1 parent in 85% of neonatal intensive care units (NICUs)25 and access restricted to less than 24 hours a day for 0 to 2 family members in about half of reporting PICUs, with reports of limited in-hospital mobility and participation for caregivers who were allowed.24 Our own experiences of day-to-day PICU operations in Canada involved complex situations and decision-making that went beyond choosing how many caregivers could be enabled on the unit. A comprehensive exploration of the policies and practices related to family presence in Canadian children’s hospitals, both before and during the COVID-19 pandemic, was therefore warranted.
We designed this study to describe family presence policies and practices (including development, dissemination and variation) in Canadian PICUs during the first year of the COVID-19 pandemic.
Methods
Design
We conducted an environmental scan of family presence policies and practices in Canadian PICUs before the COVID-19 pandemic and in its early stages (March–May 2020), following the environmental scan process from the Canadian Agency for Drugs and Technologies in Health.26 We first performed a literature review of public-facing documents; then, because we found a paucity of information, we undertook a cross-sectional survey (August–December 2020) using a researcher-administered tool.
The study team included PICU clinicians (J.R.F., L.A.L., D.G.), an epidemiologist (J.A.S.), a research coordinator with qualitative experience (M.R.), a PICU leader (L.J.B.), a health care administrator (S.A.B.) and patient partners (C.S., M.W.). Patient partners were involved from inception, providing feedback on the study question and scope, survey instrument, data interpretation and manuscript drafts.
Setting
Across Canada, 19 administratively separate units in 8 provinces meet the Society of Critical Care Medicine definition of a PICU, including fellowship-trained pediatric intensivists as attending physicians.27 All units operate within a university-affiliated children’s hospital or children’s health program, serve as regional referral units and are well known in the pediatric community.28 Two hospitals have administratively separate cardiac and medical–surgical PICUs, and 4 provinces are served by more than 1 PICU. In 2 provinces and all 3 territories, physicians send patients out of province to regional referral centres.
Participants
For the survey, we purposively invited both the physician chief (also called the medical director, hereafter referred to as the “chief”) and the operations (or patient care) manager for all 19 Canadian PICUs, to examine response consistency and target a census of PICU practice. The manager is usually a registered nurse but may be any senior administrative member of the interprofessional team who is not a physician.
We identified participants through informal professional networks, hospital directories and personal communications. We recruited participants using an initial email invitation, followed by 1 telephone reminder and up to 3 email reminders. All participants received study information and consent documents by email and provided written or audiorecorded verbal informed consent before participation.
Data sources and collection
Literature search
J.R.F. collected public-facing policy and practice documents from early in the COVID-19 pandemic (March–May 2020) using Internet searches and a digital library of archived websites (web.archive.org). Searches included websites, historic websites and social media pages for each PICU, children’s hospital or children’s health program, and affiliated health authorities. We amalgamated documents that contained duplicative information.
J.R.F. and M.R. independently abstracted data using a standardized data extraction form designed by the research team that included the hospital name; the source and specificity of the policy information (PICU, children); the document type (website, poster, social media page, official policy, news release, other); the number and type of family members and visitors allowed; the timing of parental presence; practices related to parent and visitor switches (unnecessary, unrestricted, restricted times or frequencies, not allowed); any provision for policy exceptions; and in-hospital mobility (unrestricted, encouraged to remain in room, not allowed to leave, other).
Where we found no policies specific to the PICU, we extracted elements of hospital- or program-wide policies that referred to pediatric care. Discrepancies were resolved by consensus.
Survey
Based on team members’ clinical and administrative experience, we developed a survey to address perceived information deficits from the public-facing documents found during the literature search. The survey included the following domains: family presence policy and practice; pandemic policy creation and dissemination; personal protective equipment; patient care rounds (“rounds”); in-hospital mobility; and policy exceptions (Appendix 1, available at www.cmajopen.ca/content/10/3/E622/suppl/DC1).
Using the methods of Burns,29 we developed questions to address each domain through an iterative process of creation, team feedback and reduction or revision. We included closed- and open-ended questions to enable expanded description of policies and processes before the COVID-19 pandemic, early in the pandemic (March 2020) and the second half of 2020 (August–December, the time of survey administration). We pretested the survey with 5 professionals adjacent to our target population (Appendix 2, available at www.cmajopen.ca/content/10/3/E622/suppl/DC1).
Researchers (J.R.F., L.A.L.) practised administering the survey with 1 or 2 colleagues. The same authors then administered the survey via telephone or videoconference (Zoom), based on the participant’s preference, to enable clarification of questions and expansion on responses. We encouraged participants to look up answers and to have policies and relevant communications available during the survey. We filled out the data collection form as each interview progressed, audiorecorded responses to enable verification, sent participants their completed data collection form to verify their responses, and entered data into Excel (Microsoft) for analysis.
Data analysis
We conducted qualitative analysis of open-ended questions using a general inductive approach.30 J.R.F. read all responses, inductively coded the first 3 responses to each question, and then coded the remaining responses using the resulting framework, adding codes as needed. L.A.L. independently coded the data using the framework, providing suggestions for framework adjustments and resolving discrepancies through discussion. Responses for each code were totalled and summarized as count data.
We quantitatively summarized nominal-level data using frequencies and percentages; we used the actual number of respondents for each question as the denominator for all descriptive analyses. For questions that had chief–manager dyad responses, we calculated the percent agreement.
Ethics approval
The Research Ethics Board of IWK Health approved this study (REB No. 1025836).
Results
Of the 19 Canadian PICUs (Table 1), 5 were in 4 stand-alone children’s hospitals and 14 were in larger, mixed-population hospitals. Most PICUs were medical–surgical (n = 11, 58%), had 10 to 19 beds (n = 10, 53%) and admitted children from birth to age 18 years (n = 14, 74%).
Table 1:
Characteristics of Canadian PICUs (n = 19)*
| Characteristic | No. (%) |
|---|---|
| Hospital type | |
| Stand-alone children’s hospital | 5 (26) |
| Children’s health unit in a larger, mixed hospital | 11 (58) |
| Women and children’s hospital | 3 (16) |
| PICU type | |
| Medical–surgical | 11 (58) |
| Level 2 medical–surgical† | 2 (11) |
| Cardiac | 2 (11) |
| Mixed medical–surgical–cardiac | 6 (32) |
| No. of beds | |
| < 10 | 5 (26) |
| 10–19 | 10 (53) |
| ≥ 20 | 4 (21) |
| Ages admitted, yr | |
| Birth to 16 | 2 (11) |
| Birth to 17 | 3 (16) |
| Birth to 18 | 14 (74) |
Note: PICU = pediatric intensive care unit.
Information provided by respondents from each PICU.
Units providing single-organ support and short-term invasive mechanical ventilation only.
Literature search
We identified 20 prepandemic documents from 17 PICUs and analyzed 19 documents after amalgamation (10 PICU-specific, 8 hospital-based, 1 health authority–based; Appendix 3, available at www.cmajopen.ca/content/10/3/E622/suppl/DC1). We collected 22 early-pandemic documents from all 19 PICUs and analyzed 17 after amalgamation (11 hospital-based, 6 health authority–based). Two included PICU-specific rules; the rest addressed pediatrics or children’s health. Only 1 PICU provided documents that guided the public on all of the policy elements we sought to extract.
The most frequently reported element in the documents was whether minors or siblings were prohibited or allowed. For 7 of 19 units (37%, 6 documents), the number of support people permitted at the bedside was not provided. The ability of a second care provider to trade places as bedside care provider (i.e., switch) was reported for only 6 of 19 units (32%, 5 documents). Policy details by PICU are presented in Table 2.
Table 2:
Family presence policies early in the COVID-19 pandemic (March–May 2020) for all Canadian PICUs — results of literature search*
| Hospital, city, province | Policy information source | Document type(s) | No. of people at bedside | Switching practice to enable second parent or support† | Approach to minor-age siblings | Approach to other non-parent family and visitors‡ | Response to family or visitors with infectious symptoms or risk§ | In-hospital mobility¶ | |
|---|---|---|---|---|---|---|---|---|---|
| Patients without SARS-CoV-2 infection | Patients with confirmed or suspected SARS-CoV-2 infection | ||||||||
| Janeway Children’s Health and Rehabilitation Centre, St. John’s, Newfoundland and Labrador | Health authority | Website, social media | NS | NS | NS | Not allowed or only at end of life | Not allowed | NS | NS |
| IWK Health, Halifax, Nova Scotia | Hospital | Website | 1 | NS | NS | Not allowed or only at end of life | NS | Screened | NS |
| CHU de Québec–Université Laval, Québec City, Quebec | Hospital | Website | 1 | NS | NS | Not allowed or only at end of life | Not allowed | NS | NS |
| CIUSSS de l’Estrie–CHU Sherbrooke, Sherbrooke, Quebec | Health authority | Website | NS | NS | NS | NS | NS | Not allowed | NS |
| Montreal Children’s Hospital; Montréal, Quebec | Hospital | Website | 2 (strict) | NS | Unnecessary | Not allowed or only at end of life | Not allowed | NS | NS |
| CHU Sainte-Justine, Montréal, Quebec | Hospital | Website | 2 (strict) | NS | Unnecessary | Not allowed or only at end of life | Not allowed | Not allowed | NS |
| Kingston Health Sciences Centre, Kingston, Ontario | Hospital | Original policy, website | NS | NS | NS | Not allowed or only at end of life | Not allowed | Screened | NS |
| Children’s Hospital of Eastern Ontario, Ottawa, Ontario | Hospital | Website | 2 (strict) | NS | Restricted times or frequencies | Not allowed or only at end of life | Not allowed | Screened | NS |
| The Hospital for Sick Children, cardiac, Toronto, Ontario | Hospital | Website | 1 | NS | NS | Not allowed or only at end of life | Not allowed | Screened | NS |
| The Hospital for Sick Children, medical–surgical, Toronto, Ontario | Hospital | Website | 1 | NS | NS | Not allowed or only at end of life | Not allowed | Screened | NS |
| McMaster Children’s Hospital, Hamilton, Ontario | Hospital | Website | NS | 1 | NS | NS | NS | NS | NS |
| Children’s Hospital–London Health Sciences Centre, London, Ontario | Hospital | News release | 1 | NS | NS | Not allowed or only at end of life | Not allowed | Not allowed | NS |
| Children’s Hospital–Health Sciences Centre, Winnipeg, Manitoba | Hospital | Website | 1 | NS | NS | At manager’s discretion | NS | NS | NS |
| Jim Pattison Children’s Hospital, Saskatoon, Saskatchewan | Health authority | Original policy, website, news release, poster | 1 | 1 | Not allowed | Not allowed or only at end of life | Not allowed | Not allowed | Not allowed to leave PICU room |
| Stollery Children’s Hospital, cardiac, Edmonton, Alberta | Health authority | Original policy, website | NS | NS | NS | Not allowed or only at end of life | NS | Not allowed | NS |
| Stollery Children’s Hospital, medical–surgical, Edmonton, Alberta | Health authority | Original policy, website | NS | NS | NS | Not allowed or only at end of life | NS | Not allowed | NS |
| Alberta Children’s Hospital, Calgary, Alberta | Health authority | Original policy, website | NS | NS | NS | Not allowed or only at end of life | NS | Not allowed | NS |
| BC Children’s Hospital, Vancouver, British Columbia | Hospital | Website | 2 (strict) | NS | Unnecessary | Not allowed or only at end of life | NS | Screened | NS |
| Victoria General Hospital, Victoria, British Columbia | Health authority | Website | 1 | 1 | Restricted times or frequencies | Not allowed or only at end of life | NS | Not allowed | NS |
| No. not specified (%) | – | – | 7 (37) | 16 (84) | 13 (68) | 2 (11) | 9 (47) | 5 (26) | 18 (95) |
Note: NS = not specified, PICU = pediatric intensive care unit.
For full data, see Appendix 4, available at www.cmajopen.ca/content/10/3/E622/suppl/DC1.
Abstracted and abbreviated from publicly accessible documents.
Refers to a PICU or hospital practice in which the number at the bedside is limited to enable 1 caregiver to leave and be replaced by a different caregiver. In this table, switches were designated as “unnecessary” if both parents or 2 caregivers could be present at the same time.
Including siblings over age 18 years.
Including respiratory infectious symptoms or suspected SARS-CoV-2. ”Screened” indicates that family members were screened for infection, without indication of the action taken if a visitor screened positive.
Refers to whether caregivers were allowed to leave the PICU room and move around the hospital for any reason, including accessing basic needs.
Survey
From the 19 Canadian PICUs, 15 of 19 chiefs (79%) and 9 of 19 managers (47%) agreed to participate, for a total of 24 respondents. For 5 of 19 units (26%), both the chief and the manager responded within 2 weeks of one another.
Pandemic policy creation and dissemination
Most respondents perceived that pandemic family presence policies were designed at the hospital level (n = 15, 79%); 9 (47%) perceived that policies aligned with provincial requirements. Two hospitals followed regionally generated policies (e.g., health zone, municipality) but enabled adaptation for pediatric units. PICU-specific policies were consistent with those of the hospital in 17 of 19 units (89%) and were designed by PICU leadership in 2 of 19 (11%).
Most PICU leaders did not perceive that they were consulted for hospital (n = 19, 79%) or PICU (n = 17, 71%) policies. Four respondents (17%) from 4 institutions perceived that families were consulted during the design and implementation of children’s hospital policies, and 2 respondents (8%) from 2 institutions perceived that families were consulted for PICU-specific policies.
PICU leaders received policy information via leadership meetings (n = 11, 46%), emails (n = 11, 46%), direct communication from hospital leadership (n = 5, 21%), direct involvement in the decision-making process (n = 4, 17%) or a combination of these. However, 2 respondents (8%) reported learning about policies through media, websites or word of mouth. Communication to newly admitted families usually occurred through posters, letters and websites (n = 15, 63%); the PICU bedside nurse (n = 14, 58%); and the point of first contact (e.g., emergency department or transport teams; n = 8, 33%).
Policy elements
Table 3 describes respondents’ perceptions related to family presence policy elements. All respondents said that before the COVID-19 pandemic, family presence was enabled at all times, although 6 policies (25%) enabled only 1 parent for sleep, 2 (8%) did not allow family members to sleep at the bedside and 3 (13%) asked family members to leave for rounds and handover discussions about children who were not their own. All units enabled the presence of nonfamily visitors, although often through switching (n = 18, 75%).
Table 3:
PICU family presence policies — survey responses (n = 24)*
| Family presence policy | No. (%) of respondents | ||||
|---|---|---|---|---|---|
|
| |||||
| Before the pandemic | March 2020 | August–December 2020 | |||
|
|
|
||||
| Patients without SARS-CoV-2 infection | Patients with confirmed or suspected SARS-CoV-2 infection | Patients without SARS-CoV-2 infection | Patients with confirmed or suspected SARS-CoV-2 infection | ||
| Shared policies between PICU and all pediatric care areas | |||||
|
| |||||
| Yes | 11 (46) | 20 (83) | |||
|
| |||||
| No | 7 (29) | 3 (13) | |||
|
| |||||
| Unsure | 6 (25) | 1 (4) | |||
|
| |||||
| Agreement, no. of pairs (% agreement)† | 2 (50) | 5 (100) | |||
|
| |||||
| No. of support people at bedside | |||||
|
| |||||
| 1 | 0 (0) | 21 (88) | 23 (96) | 5 (21) | 12 (50) |
|
| |||||
| 2 (strict) | 8 (33) | 3 (13) | 1 (4) | 19 (79) | 12 (50) |
|
| |||||
| 2 (flexible) | 11 (46) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
| |||||
| Unlimited | 5 (21) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
| |||||
| Agreement, no. of pairs (% agreement)‡ | 5 (0) | 5 (80) | 5 (100) | 5 (100) | 5 (60) |
|
| |||||
| Switches to enable other parent’s presence§ | |||||
|
| |||||
| Unnecessary (multiple visitors permitted) | 24 (100) | 3 (13) | 1 (4) | 19 (79) | 12 (50) |
|
| |||||
| Not allowed | 0 (0) | 7 (30) | 13 (57) | 0 (0) | 3 (13) |
|
| |||||
| Any time | 0 (0) | 4 (17) | 2 (9) | 1 (4) | 2 (8) |
|
| |||||
| Restricted times or frequencies | 0 (0) | 9 (39) | 7 (30) | 4 (17) | 7 (29) |
|
| |||||
| Agreement, no. of pairs (% agreement)‡ | 5 (100) | 4 (50) | 4 (75) | 5 (100) | 5 (40) |
|
| |||||
| Timing of parental presence | |||||
|
| |||||
| 24/7 | 13 (54) | 19 (79) | 22 (92) | 20 (83) | 23 (96) |
|
| |||||
| Parents always allowed, but only 1 may stay if sleeping | 6 (25) | 2 (8) | 1 (4) | 2 (8) | 1 (4) |
|
| |||||
| Parents must leave overnight | 2 (8) | 1 (4) | 1 (4) | 0 (0) | 0 (0) |
|
| |||||
| Parents must leave during rounds or handover | 3 (13) | 2 (8) | 0 (0) | 2 (8) | 0 (0) |
|
| |||||
| Agreement, no. of pairs (% agreement)‡ | 5 (80) | 4 (80) | 5 (100) | 5 (80) | 5 (100) |
|
| |||||
| Nonparent family members and visitors may switch into bedside¶ | |||||
|
| |||||
| Unnecessary (family and visitors unlimited) | 6 (25) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
| |||||
| Not allowed | 0 (0) | 23 (96) | 23 (96) | 15 (65) | 19 (83) |
|
| |||||
| Any time | 12 (50) | 0 (0) | 0 (0) | 3 (13) | 0 (0) |
|
| |||||
| Restricted times or frequencies | 6 (25) | 1 (4) | 1 (4) | 5 (22) | 4 (17) |
|
| |||||
| Agreement, no. of pairs (% agreement)‡ | 5 (60) | 5 (100) | 5 (100) | 4 (50) | 4 (50) |
|
| |||||
| Sibling presence | |||||
|
| |||||
| Unrestricted | 12 (50) | 0 (0) | 0 (0) | 1 (4) | 0 (0) |
|
| |||||
| Not allowed, or only at end of life | 1 (4) | 24 (100) | 24 (100) | 17 (71) | 23 (96) |
|
| |||||
| With restrictions (e.g., time, duration, age) | 9 (38) | 0 (0) | 0 (0) | 6 (25) | 1 (4) |
|
| |||||
| At RN discretion | 2 (8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
| |||||
| Agreement, no. of pairs (% agreement)‡ | 5 (80) | 5 (100) | 5 (100) | 5 (100) | 5 (100) |
Note: PICU = pediatric intensive care unit, RN = registered nurse.
Unless otherwise indicated.
Physician chief and operations manager pairs from the same unit who did not indicate “unsure.”
Physician chief and operations manager pairs from the same unit for which both provided an answer to the given variable.
Early pandemic: n = 23.
Mid-pandemic: n = 23.
Early in the COVID-19 pandemic, all units enabled 1 to 2 caregivers at the bedside, but presence was limited to family-designated, hospital-approved individuals. One unit did not allow family presence overnight. Most respondents (n = 16, 67%) noted that the number of support people permitted had increased by the time of the survey. All 5 respondents who had indicated that their units allowed unlimited family presence before the pandemic allowed 2 caregivers for patients without SARS-CoV-2 infection by the time of the survey. Three of the 8 respondents who reported strict limitations to 2 at the bedside before the COVID-19 pandemic indicated ongoing restrictions to 1 family member at the time of the survey.
Practices
Non-policy practices are presented in Table 4. Before the COVID-19 pandemic, patient care rounds were always at the bedside and included active family participation. Early in the pandemic, family participation changed for patients without SARS-CoV-2 infection (n = 9/22, 41%; 66% chief–manager agreement) and patients with confirmed or suspected SARS-CoV-2 infection (n = 17/22, 77%; 33% chief–manager agreement). Although practices evolved during the pandemic, 7 of 21 (33%) respondents reported that families of patients with confirmed or suspected SARS-CoV-2 infection still were not participating in rounds by mid-pandemic (66% chief–manager agreement).
Table 4:
PICU family presence practices — survey responses (n = 24)*
| Family presence practice | No. (%) of respondents | ||||
|---|---|---|---|---|---|
|
| |||||
| Before the pandemic | March 2020 | August–December 2020 | |||
|
|
|
||||
| Patients without SARS-CoV-2 infection | Patients with confirmed or suspected SARS-CoV-2 infection | Patients without SARS-CoV-2 infection | Patients with confirmed or suspected SARS-CoV-2 infection | ||
| Rounds practices† | |||||
|
| |||||
| In-person | 24 (100) | 13 (59) | 5 (23) | 21 (95) | 7 (33) |
|
| |||||
| Virtual or telephone | 0 (0) | 5 (23) | 8 (36) | 1 (5) | 7 (33) |
|
| |||||
| Nonparticipation | 0 (0) | 4 (18) | 9 (41) | 0 (0) | 7 (33) |
|
| |||||
| Agreement, no. of pairs (% agreement)‡ | 5 (100) | 3 (66) | 3 (33) | 4 (100) | 3 (66) |
|
| |||||
| Rounds location§ | |||||
|
| |||||
| Adjacent to room (e.g., bedside) | 24 (100) | 17 (74) | 16 (70) | 22 (100) | 21 (100) |
|
| |||||
| Distant location (e.g., conference room) | 0 (0) | 6 (26) | 7 (30) | 0 (0) | 0 (0) |
|
| |||||
| Agreement, no. of pairs (% agreement)‡ | 5 (100) | 4 (100) | 4 (75) | 4 (75) | 3(100) |
|
| |||||
| Ability to leave PICU room¶ | |||||
|
| |||||
| Unrestricted | 24 (100) | 17 (71) | 0 (0) | – | – |
|
| |||||
| Not allowed to leave | 0 (0) | 0 (0) | 7 (29) | – | – |
|
| |||||
| Restricted: toilet | 0 (0) | 1 (4) | 11 (46) | – | – |
|
| |||||
| Restricted: stress/procedures | 0 (0) | 0 (0) | 4 (17) | – | – |
|
| |||||
| Restricted: eating | 0 (0) | 0 (0) | 2 (8) | – | – |
|
| |||||
| Encouraged not to leave room, not mandated | 0 (0) | 6 (25) | 3 (13) | – | – |
|
| |||||
| Agreement, no. of pairs (% agreement)‡ | 5 (100) | 5 (100) | 5 (80) | – | – |
|
| |||||
| Ability to leave hospital¶ | |||||
|
| |||||
| Unrestricted | 24 (100) | 21 (88) | 3 (13) | – | – |
|
| |||||
| Restricted frequency (e.g., once per shift, once per day) | 0 (0) | 0 (0) | 4 (17) | – | – |
|
| |||||
| Restricted: smoking | 0 (0) | 1 (4) | 5 (21) | – | – |
|
| |||||
| Restricted: switches | 0 (0) | 2 (8) | 7 (29) | – | – |
|
| |||||
| Never | 0 (0) | 1 (4) | 8 (33) | – | – |
|
| |||||
| Agreement, no. of pairs (% agreement)‡ | 5 (100) | 5 (80) | 5 (60) | – | – |
Note: PICU = pediatric intensive care unit.
Unless otherwise indicated.
Early pandemic: n = 22; mid-pandemic: n = 22 respondents for patients who tested negative for SARS-CoV-2, n = 21 for patients with confirmed or suspected SARS-CoV-2 infection.
Physician chief and operations manager pairs from the same unit for which both provided an answer to the given variable.
Early pandemic: n = 23; mid-pandemic: n = 22 for patients who tested negative for SARS-CoV-2; n = 21 for patients with confirmed or suspected SARS-CoV-2 infection.
Respondents could indicate more than 1 reason for leaving (e.g., toilet, eating, switches and smoking).
Family members — particularly families of patients with confirmed or suspected SARS-CoV-2 infection — experienced restrictions in their ability to leave their PICU room or the hospital. Mobility restrictions resulted in novel problems for caregivers, including the following: having to use a commode in patient rooms or a designated “COVID-19” bathroom; being unable to leave for cigarette breaks, leading to nicotine withdrawal, aggression to staff, and hospital provision of nicotine patches; a lack of sleeping provisions, necessitating sleep in chairs; barriers to obtaining food, resulting in hospital-supplied meals, delivery orders picked up by bedside staff, and lack of access to culturally appropriate options; and being unable to leave the patient room during traumatic events.
Policy exceptions
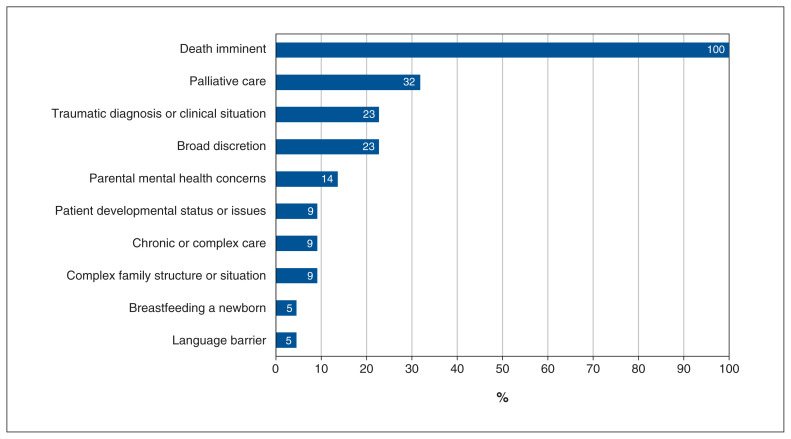
Although most respondents (n = 20, 83%) were unaware of a list of acceptable reasons for exceptions, all (n = 24, 100%) indicated that exceptions were needed in extenuating circumstances and would be granted at end of life. Approaches to decision-making about policy exceptions are outlined in Table 5. Figure 1 depicts reasons respondents gave for granting exceptions.
Table 5:
Approach to policy exceptions and decision-making authority — survey responses (n = 24)
| Factor | No. (%) of respondents |
|---|---|
| Approach to policy exceptions* | |
| Exceptions enabled by policy | 10 (42) |
| Processes understood but not formalized | 4 (17) |
| No initial policy or process, but developed over study period | 7 (29) |
| No policy | 3 (13) |
| Agreement, no. of pairs (% agreement)† | 5 (100) |
| Decision-making authority | |
| PICU (physician, manager or charge nurse) | 9 (38) |
| Hospital director | 8 (33) |
| Infection prevention and control or emergency operations | 6 (25) |
| Hospital executive | 1 (4) |
| Agreement, no. of pairs (% agreement)† | 5 (40) |
Note: PICU = pediatric intensive care unit.
Exceptions referred to enabling deviation from policy in certain circumstances. Examples of exceptions were: allowing more people at the bedside; allowing siblings; allowing more frequent switches of parents or other family members.
Physician chief and operations manager pairs from the same unit for which both provided an answer to the given variable.
Figure 1:
Stated reasons for granting exceptions to restrictions, where an exception was an increase in the number of family members present at a single time, or increased frequency of switches (n = 24 respondents).
The process for granting exceptions varied among units. Final decision-making was perceived to be held outside the PICU (n = 15, 62%) more often than within it (n = 9, 38%; 100% chief–manager agreement). However, 10 (42%) respondents described the ability of PICU personnel to grant urgently needed exceptions (80% chief–manager agreement).
Screening and personal protective equipment
Perceived approaches to screening for contagious diseases and family member use of personal protective equipment are outlined in Table 6.
Table 6:
PICU in-room masking requirements and screening for parents and support people — survey responses (n = 24)
| Factor | No. (%) of respondents | |||
|---|---|---|---|---|
|
| ||||
| March 2020 | August–December 2020 | |||
|
|
|
|||
| Patients without SARS-CoV-2 infection | Patients with confirmed or suspected SARS-CoV-2 infection | Patients without SARS-CoV-2 infection | Patients with confirmed or suspected SARS-CoV-2 infection | |
| Masking in patient room | ||||
|
| ||||
| Always | 4 (17) | 11 (46) | 10 (42) | 15 (62) |
|
| ||||
| Never | 17 (71) | 11 (46) | 8 (33) | 3 (12) |
|
| ||||
| When a health care provider is present | 2 (8) | 2 (8) | 6 (25) | 6 (25) |
|
| ||||
| If child is infectious | 1 (4) | NA | 0 (0) | NA |
|
| ||||
| Agreement, no. of pairs (% agreement)* | 5 (80) | 5 (100) | 5 (80) | 5 (80) |
|
| ||||
| SARS-CoV-2 screening for parents and support people† | ||||
|
| ||||
| Preadmission questionnaire | 20 (83) | – | – | – |
|
| ||||
| Hospital or PICU entry screening questionnaire | 20 (83) | – | – | – |
|
| ||||
| Daily PICU symptom screening | 8 (33) | – | – | – |
|
| ||||
| Temperature check | 3 (13) | – | – | – |
|
| ||||
| Admission swab | 1 (4) | – | – | – |
|
| ||||
| Agreement, no. of pairs (% agreement)* | 5 (60) | – | – | – |
Note: NA = not applicable, PICU = pediatric intensive care unit.
Physician chief and operations manager pairs from the same unit for which both provided an answer to the given variable.
Respondents could choose more than 1 screening method.
Interpretation
We present a descriptive summary of family presence policy and practice in PICUs during the COVID-19 pandemic, identified through a review of public-facing documents and from a survey of PICU leadership. We identified a paucity of publicly accessible information that would enable families travelling to a PICU or children’s hospital to plan their stay adequately, requiring direct inquiries to PICU leadership to clarify the policy and practice environment. Canadian PICU patients were spared the extreme restrictions faced by adults22,31 and by some pediatric patients in other countries.24 However, the restriction of family presence to 1 or 2 parents and the exclusion of siblings and other members of a child’s support circle was a deviation from the family-centred approach of Canadian children’s hospitals before the COVID-19 pandemic.32 This deviation had the potential for negative impacts on mental health, decision-making, family functioning and sibling adjustment.6,20,33–35 We also identified relaxation of restrictions and the development of more formalized policy exceptions as the pandemic progressed.
Although the number of family members allowed at the bedside in Canadian PICUs was similar to that reported in children’s hospitals in the US,23 our report also describes practice elements associated with COVID-19 restrictions that may affect patients and families. In the family-centred care models embraced by Canadian PICUs, families are seen as core members of the health care team, as well as vulnerable individuals experiencing trauma who are in need of care themselves.36 Mobility restrictions were a substantial deviation from usual practices, and they introduced novel issues around caring for families. Several PICU leaders spoke of family members being restricted to their child’s room, unable to leave even during traumatic events. The PICU literature suggests that the rates of acute and post-traumatic stress in family members is already high;37,38 such practice changes may have worsened this morbidity. Removal of family presence from rounds during COVID-19 has also been reported in other PICUs24 and NICUs25 and may have affected the ability of families to participate in decision-making and care;39 although a family member was allowed at bedside, they were no longer part of the team.
We identified a concerning lack of participation in policy design and implementation on the part of families, bedside health care providers and PICU leadership. This finding denotes a centralized approach that does not acknowledge the local and specialized needs of critically ill children and their families. Such circumstances can create a situation of moral hazard, in which those who are empowered to parse risk and fashion responses (decision-makers) are not those who live with the burdens (decision-bearers).40 Examination of the impacts of these practices on family members is needed.
Because previous descriptions of visitation policy have relied on reports from single institutional representatives,24,31,41 we sought to examine the consistency of chief–manager dyad responses and noted multiple discrepancies across stages of the COVID-19 pandemic. This finding may have arisen from differences between leaders who did and did not work at the bedside, may have come from differences in bedside practice and experiences, or may reflect communication breakdown and underscore a need in organizations to ensure alignment between policy and practice.42,43 As well, an examination of publicly accessible policy information demonstrated substantial interhospital variation. Inconsistency between leaders and among Canadian PICUs meant that families across the country had unequal access to their critically ill child, both at a baseline and during periods of restriction. Consensus on the essential elements of family presence policies, which can be used to guide policy in any context, should be a priority for the PICU community.
Building on our previous work44,45 optimizing parental presence at the bedside in PICUs before the pandemic, we are implementing a program of research to examine the experience of restricted family presence in the PICU for front-line clinicians, pediatric patients and their family members.
Study strengths included the use of multiple sources for policy information, survey administration during the pandemic to minimize recall bias, representation from both managers (hospital administrators who are familiar with policy) and chiefs (front-line staff who experience actual practice), and representation from all Canadian PICUs, creating a geographically diverse and complete sample.
Limitations
This environmental scan did not consider changes to policy and practice that have occurred since December 2020, limiting current applicability. Publicly accessible document searches were limited to Web searches and may have missed site-based posters and pamphlets, and online documents that were removed before archiving. Because the survey collected information about the perceptions of the PICU leadership and we demonstrated multiple disagreements within units, policy-based information must be interpreted cautiously. Lack of participation from all chiefs and managers limited interpretations of disparity, and higher representation from physician chiefs may have biased survey results to the perceptions of bedside staff. Finally, the intention of the present study was to report on policies and practices in PICUs; we did not examine the views and experiences of patients and their families, which should be explored in future study.
Conclusion
Pandemic-related family presence policies in Canadian PICUs varied among centres. Initial COVID-19 restrictions universally limited family presence and often restricted mobility and participation in decision-making activities without consistent provision for extenuating circumstances. Policies and practices in PICUs adapted as the pandemic progressed.
Supplementary Material
Acknowledgements
The authors thank Dr. Sonny Dhanani and Dr. Paul Hébert for their critical review of the manuscript. The authors also thank the Canadian Critical Care Trials Group and their patient–parent partners for longitudinal input on study design and interpretation of results.
Footnotes
Competing interests: Jennifer Foster, Laurie Lee and Jamie Seabrook are co–principal applicants and Laura Betts, Stacy Burgess, Corey Slumkoski, Martha Walls and Daniel Garros are coinvestigators on a grant from the Canadian Institutes of Health Research to examine the impact of restricted family presence policies in pediatric intensive care units and strategies for optimizing policies and practices in the future. No other competing interests were declared.
This article has been peer reviewed.
Contributors: Jennifer Foster, Laurie Lee and Daniel Garros conceived of the project. All authors were involved in study and survey design; Jennifer Foster and Laurie Lee performed data collection and, with Molly Ryan, analysis; Jennifer Foster drafted the initial manuscript; and all authors reviewed the manuscript carefully for important content. All authors approve the final manuscript and agree to be accountable for all aspects of the work.
Funding: This study was funded by a project grant from IWK Health, Halifax, Nova Scotia, which had no role in the study’s design, implementation or analysis.
Data sharing: The data that support the findings of this study are available on request from the corresponding author.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/10/3/E622/suppl/DC1.
References
- 1.Kaye EC. COVID-19 caregiver restrictions in pediatrics. Hosp Pediatr. 2021;11:e12–4. doi: 10.1542/hpeds.2020-004291. [DOI] [PubMed] [Google Scholar]
- 2.Andrist E, Clarke RG, Harding M. Paved with good intentions: hospital visitation restrictions in the age of coronavirus disease 2019. Pediatr Crit Care Med. 2020;21:e924–6. doi: 10.1097/PCC.0000000000002506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Virani AK, Puls HT, Mitsos R, et al. Benefits and risks of visitor restrictions for hospitalized children during the COVID pandemic. Pediatrics. 2020;146:e2020000786. doi: 10.1542/peds.2020-000786. [DOI] [PubMed] [Google Scholar]
- 4.Bannerman K, Aitken L, Donnelly P, et al. Parental perceptions of the impact of COVID-19 restrictions on family-centred care at a paediatric intensive care unit. Br J Child Health. 2021;2:195–200. [Google Scholar]
- 5.Rennick JE, Johnston CC, Dougherty G, et al. Children’s psychological responses after critical illness and exposure to invasive technology. J Dev Behav Pediatr. 2002;23:133–44. doi: 10.1097/00004703-200206000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Shudy M, Lihinie de Almeida M, Ly S, et al. Impact of pediatric critical illness and injury on families: a systematic literature review. Pediatrics. 2006;118(Suppl 3):S203–18. doi: 10.1542/peds.2006-0951B. [DOI] [PubMed] [Google Scholar]
- 7.Roth A, Rapoport A, Widger K, et al. General paediatric inpatient deaths over a 15-year period. Paediatr Child Health. 2017;22:80–3. doi: 10.1093/pch/pxx005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson BH, Seale Jeppson E, Redburn L. Caring for children and families: guidelines for hospitals. 1st ed. Bethesda (MD): Association for the Care of Children’s Health; 1992. [Google Scholar]
- 9.About Children’s Healthcare Canada. Ottawa: Children’s Healthcare Canada; 2020. [accessed 2020 May 12]. Available: www.childrenshealthcarecanada.ca/about. [Google Scholar]
- 10.Patient & family centered care. Edmonton: Stollery Children’s Hospital, Alberta Health Services; 2020. [accessed 2020 May 21]. Available: www.albertahealthservices.ca/stollery/Page14041.aspx. [Google Scholar]
- 11.Family centred care: Alberta Children’s Hospital. Edmonton: Alberta Health Services; 2020. [accessed 2020 May 21]. Available: www.albertahealthservices.ca/ach/Page16893.aspx. [Google Scholar]
- 12.Vision and values. Montréal: Montreal Children’s Hospital; 2020. [accessed 2020 May 21]. Available: www.thechildren.com/careers-and-volunteering/why-work-childrens/vision-and-values. [Google Scholar]
- 13.Vision, mission, values. Vancouver: BC Children’s Hospital; 2020. [accessed 2020 May 21]. Available: www.bcchildrens.ca/about/vision-mission-values. [Google Scholar]
- 14.Our core values and mission. Halifax: IWK Health Centre; 2022. [accessed 2022 May 10]. Available: www.iwk.nshealth.ca/about-us/our-core-values-mission-and-vision. [Google Scholar]
- 15.Baird J, Davies B, Hinds PS, et al. What impact do hospital and unit-based rules have upon patient and family-centered care in the pediatric intensive care unit? J Pediatr Nurs. 2015;30:133–42. doi: 10.1016/j.pedn.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jolley J, Shields L. The evolution of family-centered care. J Pediatr Nurs. 2009;24:164–70. doi: 10.1016/j.pedn.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 17.Virani A, Singh G, Bewick D, et al. Guiding cardiac care during the COVID-19 pandemic: how ethics shapes our health system response. Can J Cardiol. 2020;36:1313–6. doi: 10.1016/j.cjca.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kinlaw K, Barrett DH, Levine RJ. Special focus ethical guidelines in pandemic influenza: recommendations of the Ethics Subcommittee of the Advisory Committee of the Director, Centers for Disease Control and Prevention. Disaster Med Public Health Prep. 2009;3(Suppl 2):S185–92. doi: 10.1097/DMP.0b013e3181ac194f. [DOI] [PubMed] [Google Scholar]
- 19.Jee RA, Shepherd JR, Boyles CE, et al. Evaluation and comparison of parental needs, stressors, and coping strategies in a pediatric intensive care unit. Pediatr Crit Care Med. 2012;13:e166–72. doi: 10.1097/PCC.0b013e31823893ad. [DOI] [PubMed] [Google Scholar]
- 20.Colville G, Darkins J, Hesketh J, et al. The impact on parents of a child’s admission to intensive care: integration of qualitative findings from a cross-sectional study. Intensive Crit Care Nurs. 2009;25:72–9. doi: 10.1016/j.iccn.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Nelson LP, Gold JI. Posttraumatic stress disorder in children and their parents following admission to the pediatric intensive care unit: a review. Pediatr Crit Care Med. 2012;13:338–47. doi: 10.1097/PCC.0b013e3182196a8f. [DOI] [PubMed] [Google Scholar]
- 22.Fiest KM, Krewulak KD, Hiploylee C, et al. Canadian Critical Care Trials Group. An environmental scan of visitation policies in Canadian intensive care units during the first wave of the COVID-19 pandemic. Can J Anaesth. 2021;68:1474–84. doi: 10.1007/s12630-021-02049-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vance AJ, Duy J, Laventhal N, et al. Visitor guidelines in US Children’s Hospitals during COVID-19. Hosp Pediatr. 2021;11:e83–9. doi: 10.1542/hpeds.2020-005772. [DOI] [PubMed] [Google Scholar]
- 24.Camporesi A, Zanin A, Kanaris C, et al. Impact of COVID-19 pandemic on pediatric intensive care units (PICUs) visiting policies: a worldwide survey. J Pediatr Intensive Care. 2021 Nov 16; doi: 10.1055/s-0041-1739263.. [Epub ahead of print] [DOI] [Google Scholar]
- 25.Darcy Mahoney A, White RD, Velasquez A, et al. Impact of restrictions on parental presence in neonatal intensive care units related to coronavirus disease 2019. J Perinatol. 2020;40(Suppl 1):36–46. doi: 10.1038/s41372-020-0753-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Environmental scan process. Canadian Agency for Drugs and Technologies in Health; 2015. [accessed 2021 Dec. 28]. Available: www.cadth.ca/sites/default/files/pdf/ESExternalAudienceProcessDoc.pdf. [Google Scholar]
- 27.Frankel LR, Hsu BS, Yeh TS, et al. Voting Panel. Criteria for critical care infants and children: PICU admission, discharge, and triage practice statement and levels of care guidance. Pediatr Crit Care Med. 2019;20:847–87. doi: 10.1097/PCC.0000000000001963. [DOI] [PubMed] [Google Scholar]
- 28.Stang AS, Joshi A. The evolution of freestanding children’s hospitals in Canada. Paediatr Child Health. 2006;11:501–6. doi: 10.1093/pch/11.8.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burns KEA, Duffett M, Kho ME, et al. ACCADEMY Group. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008;179:245–52. doi: 10.1503/cmaj.080372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. 2006;27:237–46. [Google Scholar]
- 31.Valley TS, Schutz A, Nagle MT, et al. Changes to visitation policies and communication practices in Michigan ICUs during the COVID-19 pandemic. Am J Respir Crit Care Med. 2020;202:883–5. doi: 10.1164/rccm.202005-1706LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Farmanova E, Judd M, Maika C, et al. Much more than just a visit: a review of visiting policies in select Canadian acute care hospitals. Ottawa: Canadian Foundation for Healthcare Improvement; 2015. [accessed 2020 Nov. 15]. Available: www.cfhi-fcass.ca/sf-docs/default-source/patient-engagement/better-together-baseline-report.pdf?sfvrsn=bb65d044_10. [Google Scholar]
- 33.Lindemann H. Why families matter. Pediatrics. 2014;134(Suppl 2):S97–103. doi: 10.1542/peds.2014-1394E. [DOI] [PubMed] [Google Scholar]
- 34.Rozdilsky JR. Enhancing sibling presence in pediatric ICU. Crit Care Nurs Clin North Am. 2005;17:451–61. xii. doi: 10.1016/j.ccell.2005.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meert KL, Clark J, Eggly S. Family-centered care in the pediatric intensive care unit. Pediatr Clin North Am. 2013;60:761–72. doi: 10.1016/j.pcl.2013.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Richards CA, Starks H, O’Connor MR, et al. Elements of family-centered care in the pediatric intensive care unit. J Hosp Palliat Nurs. 2017;19:238–46. doi: 10.1097/NJH.0000000000000335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mortensen J, Simonsen BO, Eriksen SB, et al. Family-centred care and traumatic symptoms in parents of children admitted to PICU. Scand J Caring Sci. 2015;29:495–500. doi: 10.1111/scs.12179. [DOI] [PubMed] [Google Scholar]
- 38.Rees G, Gledhill J, Garralda ME, et al. Psychiatric outcome following paediatric intensive care unit (PICU) admission: a cohort study. Intensive Care Med. 2004;30:1607–14. doi: 10.1007/s00134-004-2310-9. [DOI] [PubMed] [Google Scholar]
- 39.McPherson G, Jefferson R, Kissoon N, et al. Toward the inclusion of parents on pediatric critical care unit rounds. Pediatr Crit Care Med. 2011;12:e255–61. doi: 10.1097/PCC.0b013e3181fe4266. [DOI] [PubMed] [Google Scholar]
- 40.Marshall MF, Epstein EG. Moral hazard and moral distress: a marriage made in purgatory. Am J Bioeth. 2016;16:46–8. doi: 10.1080/15265161.2016.1181895. [DOI] [PubMed] [Google Scholar]
- 41.Giannini A, Miccinesi G, Prandi E ODIN Study Group 2. Parental presence in Italian pediatric intensive care units: a reappraisal of current visiting policies. Intensive Care Med. 2017;43:458–9. doi: 10.1007/s00134-016-4628-5. [DOI] [PubMed] [Google Scholar]
- 42.Hawryluck L, Lapinsky SE, Stewart TE. Clinical review: SARS — lessons in disaster management. Crit Care. 2005;9:384–9. doi: 10.1186/cc3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Booth CM, Stewart TE. Communication in the Toronto critical care community: important lessons learned during SARS. Crit Care. 2003;7:405–6. doi: 10.1186/cc2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Foster JR, Al Othmani FI, Seabrook JA, et al. Parental presence at the bedside of critically ill children in a unit with unrestricted visitation. Pediatr Crit Care Med. 2018;19:e387–93. doi: 10.1097/PCC.0000000000001597. [DOI] [PubMed] [Google Scholar]
- 45.Miller L, Richard M, Krmpotic K, et al. Parental presence at the bedside of critically ill children in the pediatric intensive care unit: a scoping review. Eur J Pediatr. 2022;181:823–31. doi: 10.1007/s00431-021-04279-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.