Abstract
Background
Prior US studies have shown increasing rotator cuff repair rates through 2009. We hypothesize that rotator cuff repair rates are continuing to increase and the comorbidity profiles of patients are becoming more complex over time.
Methods
We identified rotator cuff repairs in a large US cohort of people 18-64 years of age with ≥1 year of commercial insurance coverage. Repair rate trends across time were standardized by age, sex, and geographic region. Procedures were categorized as inpatient vs. outpatient and as arthroscopic vs. open. Prevalent comorbidities were defined as 1 inpatient diagnosis claim or 2 outpatient diagnosis claims during the year before rotator cuff repair. General population comorbidity prevalence was determined based on a random 5% sample of the commercially insured population and compared with patients with rotator cuff repair using standardized morbidity ratios.
Results
From 2007 to 2016, 314,239 rotator cuff repairs were identified (165 repairs per 100,000 person-years). Rotator cuff repairs were performed more frequently in men, older people, and in the Midwest. Across time, cuff repair rates increased by 1.6% per year (95% confidence interval [CI] = +1.4%-1.7%) adjusting for demographics. The highest increases in repair rates were observed among patients aged 50-64 years (+2.0%, 95% CI = +1.8%-2.2%). Rotator cuff repairs were more frequently performed using an arthroscopic approach and in an outpatient setting in later calendar years. In 2016, 83% of rotator cuff repairs were arthroscopic procedures and 99% were performed as outpatient procedures. Comorbidity prevalence in rotator cuff repair patients increased across calendar time by 4.5% per year for hypertension (95% CI = +4.2%-4.7%), 2.3% per year for diabetes (+1.9%-2.7%), 0.9% per year for hypercholesterolemia (+0.3%-1.5%), 2.9% for congestive heart failure (+0.8%-4.9%), 4.2% for peripheral vascular disease (+2.4%-6.0%), and 4.2% for chronic pulmonary disease (+3.6%-4.8%). Comorbidity prevalence in repair patients was higher than prevalence in the general population, and prevalence relative to the general population was most heightened during later calendar years. For example, hypertension prevalence was 1.58 times higher in repair patients than the general population in 2007 (95% CI = 1.53-1.62), and 2.06 times higher in 2016 (95% CI = 2.02-2.11).
Conclusion
Rotator cuff repair is becoming more frequent in the US commercially insured population, particularly in those 50-64 years of age. More rotator cuff repairs are being performed using an arthroscopic approach and in an outpatient setting. Over time, the comorbidity profile of patients undergoing rotator cuff repair is becoming more complex with greater prevalence of numerous conditions, including hypertension, peripheral vascular disease, and chronic pulmonary disease.
Keywords: Rotator cuff repair, Arthroscopy, Hypertension, Diabetes, Hypercholesterolemia, Peripheral vascular disease, Chronic pulmonary disease
Rotator cuff disease is the most common cause of shoulder pain and disability in middle-aged and elderly populations with advancing age representing the most important risk factor for the development of rotator cuff tears.33,34 Rotator cuff repair rates in the United States have been increasing steadily, with the most recent studies tracking trends through 2009 in private insurance35 and 2014 in Medicare.3 For degenerative rotator cuff tears, randomized trials have not demonstrated conclusive evidence favoring operative treatment over nonoperative treatment in all settings.18,25 However, certain patients may be more likely to benefit from operative treatment, such as patients with traumatic tears, acute on chronic tears, or degenerative tears in patients younger than 65 years of age that have failed nonoperative management.19 The degree to which increasing repair rates in the United States are driven by increases in disease rates vs. expanding indications for surgery is unclear. A clearer understanding of the trends in healthcare utilization for rotator cuff disease is an important step toward defining policy and allocating resources related to care.
The prevalence of a number of comorbidities that could increase the risk of surgical complications is increasing in the US general population, including diabetes, hypertension, and hypercholesterolemia.7,26 These in turn can influence cardiovascular comorbidities such as peripheral vascular disease and congestive heart failure. As diabetes, hypertension, and hypercholesterolemia have been hypothesized to increase the risk of developing a symptomatic rotator cuff tear,1,10,15 one would expect that these conditions are becoming more common in the rotator cuff repair patient population as well. We hypothesize that rotator cuff repair is continuing to become more frequent over time and that the comorbidity profile of the patient population is becoming more complex over time. To investigate these trends in a nationally representative sample of the adult population, we used a large administrative claims database of commercially insured individuals.
Materials and methods
Study population and measurements
A large cohort of commercially insured US adults 18-64 years of age was identified using the IBM MarketScan Commercial Database (MarketScan).2 The MarketScan database contains administrative claims data from approximately 100 employer-sponsored health insurance plans which cover all 50 states and has been used previously in studies of orthopedic procedures.12,23,32 It includes claims from both inpatient and outpatient settings and allows tracking of patients over time with encrypted patient identifiers. We obtained access to the MarketScan data covering the years 2006 through 2016.
Our study population included people 18-64 year of age, as the MarketScan database does not include data on people 65 years of age and older. Furthermore, we limited our cohort to people with at least 1 year of commercial insurance coverage to allow time for the capture of prevalent comorbidities before rotator cuff repair. As a result, rotator cuff repairs were captured from 2007 to 2016.
Rotator cuff repairs were defined based on the presence of Current Procedural Terminology (CPT)-4 or International Classification of Disease (ICD) procedure codes indicating a rotator cuff repair (CPT-4 = 29827, 23410, 23412, or 23420, ICD-9-CM = 83.63, ICD-10-PCS = 0LQ14ZZ, 0LQ24ZZ, 0LQ10ZZ, 0LQ20ZZ). Repairs were categorized as an arthroscopic approach if a CPT-4 code of 29827, ICD-9-CM code of 80.21, or ICD-10-PCS codes of 0LQ14ZZ or 0LQ24ZZ were present and an open approach otherwise. The MarketScan database also provides patient demographic data, such as age, sex, and geographic region at the beginning of the enrollment period. Geographic region provides information on the census region in which each enrollee resides.5 Prevalent comorbidities at the time of rotator cuff repair were defined based on a standard algorithm in which a comorbidity was defined as the presence of two outpatient diagnostic claims more than 30 days apart or 1 inpatient diagnostic claim in the year before the date of rotator cuff repair.13,21,27 We examined prevalence of hypertension, diabetes, hypercholesterolemia, peripheral vascular disease, congestive heart failure, and chronic pulmonary disease. An Elixhauser readmission score was also calculated for each rotator cuff repair patient using the index developed by the Agency for Healthcare Research and Quality.24 To compare the observed prevalence of comorbidities in the rotator cuff repair patients to the expected prevalence in the general commercially insured population, we took a 5% sample of enrollees in each calendar year and assessed the presence of comorbidities in the 1 year before July 1 using the same claims definition.
This study was determined to be exempt from ethical review by the Washington University Institutional Review Board as only deidentified data were used.
Analysis
Repair rates were calculated by dividing the total number of rotator cuff repairs by the total number of enrollees in the MarketScan database in a given calendar year. As trends over calendar time may be influenced by changing demographics of the underlying population included in the Marketscan data, standardized rates were calculated to account for differences in age, sex, and geographic region across time. For standardized estimates, stratum-specific rates (stratified by sex, geographic region, and 1-year age groups) for each calendar year were weighted to reflect the distributions of these groups in the year 2010, thus reflecting the estimated rotator cuff repair rates if the MarketScan database population had maintained the same population age, sex, and geographic region characteristics across time. Calendar trends were described overall and within three age groups (18-34, 35-49, and 50-64 years of age). Poisson regression models were used to calculate incidence rate ratios to estimate the associations between age, sex, geographic region, and calendar year with rotator cuff repair rates. Multivariable Poisson models included age, sex, geographic region, and calendar year in the same model. When trends over calendar time did not appear linear, spline terms were used in models to estimate separate incidence rate ratios for different time periods.
Among rotator cuff repair cases, the proportion with different comorbidities was calculated for each calendar year.24 Changes in the prevalence of comorbidities across calendar time were calculated using log-binomial regression to estimate prevalence ratios. Multivariable log-binomial regression models were used to adjust for age, sex, and geographic region. Mean Elixhauser comorbidity scores were also estimated for rotator cuff repair cases in each calendar year and the average change in score with increasing calendar year was estimated with linear regression models adjusted for age, sex, and geographic region.
To compare comorbidity prevalence in rotator cuff repair cases to that of the general commercially-insured population, expected prevalence estimates were calculated based on age-, sex-, geographic region–, and calendar year-specific prevalence in a 5% random sample of the full MarketScan database population (this 5% sample includes more than 600,000 people in each calendar year). Specifically, stratum-specific prevalence estimates calculated from the 5% sample were applied to the relevant subgroups of rotator cuff repair cases in each calendar year to produce the number of affected rotator cuff repair cases we would expect if comorbidity prevalence was the same as the general population. The observed number of affected cases was then divided by the expected numbers of cases in each calendar year to calculate standardized morbidity ratios to compare comorbidity prevalence in rotator cuff repair cases with the general population prevalence.
Results
From 2007 to 2016, a total of 119,547,573 people with at least 1 full year of commercial insurance were included in the MarketScan database. People were covered for a median of 1.9 years beyond their first year of coverage (interquartile range = 0.9-3.7 years). In total, 314,239 rotator cuff repairs were identified for a rate of 165 repairs per 100,000 person-years in this population.
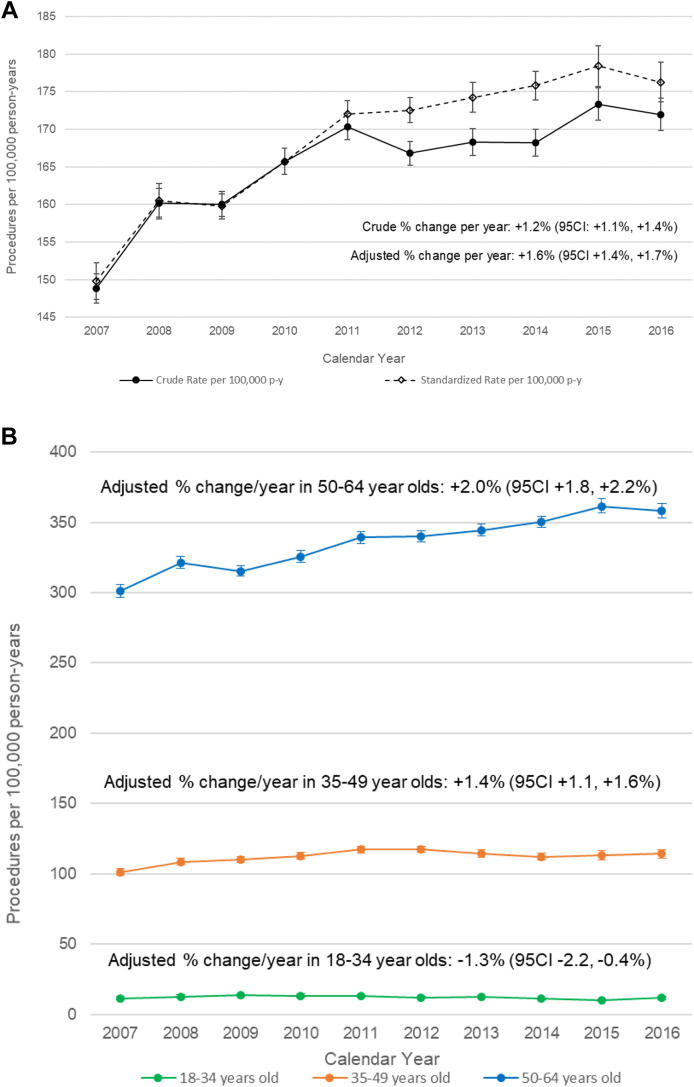
Across time, rotator cuff repair rates increased by 1.2% per year (95% confidence interval [CI]: +1.1, +1.4%) (Fig. 1, A). Rotator cuff repairs were performed more frequently in men than women, with a rate of 203 repairs per 100,000 person-years in men (95% CI: 202, 204). When examined by geographic region, rates were highest in the Midwest (183 repairs per 100,000 person-years; 95% CI: 181, 184) and lowest in the West (147 repairs per 100,000 person-years; 95% CI: 146, 148). Rotator cuff repair rates also increased consistently with age, though notably our population did not include people older than 64 years of age (Table I). These rates ranged from 8 repairs per 100,000 person-years among those 18-34 to 423 repairs per 100,000 person-years among those 50-64.
Figure 1.
Rotator cuff repair rates by calendar year (A) overall and (B) stratified by age. Standardized rates and adjusted % change estimates account for changes in the distribution of age, sex, and geographic region of population over time. 95 CI, 95% confidence interval.
Table I.
Rotator cuff repair rates stratified by population characteristics.
| Rotator cuff repairs |
Incidence rate ratio (95% CI) |
|||
|---|---|---|---|---|
| N | Incidence rate per 100,00 person-years (95% CI) | Unadjusted | Adjusted∗ | |
| Sex | ||||
| Male | 182854 | 202.8 (201.9, 203.7) | Referent | Referent |
| Female | 131385 | 131.6 (130.9, 132.3) | 0.65 (0.64, 0.65) | 0.64 (0.63, 0.64) |
| Region† | ||||
| Northeast | 43031 | 142.3 (141.0, 143.7) | 0.82 (0.81, 0.83) | 0.78 (0.77, 0.79) |
| Midwest | 80032 | 182.5 (181.3, 183.8) | 1.05 (1.04, 1.06) | 1.01 (1.01, 1.02) |
| South | 130975 | 173.5 (172.5, 174.4) | Referent | Referent |
| West | 52544 | 146.8 (145.6, 148.1) | 0.85 (0.84, 0.86) | 0.84 (0.83, 0.85) |
| Unknown | 7657 | 165.0 (161.3, 168.7) | 0.95 (0.93, 0.97) | 0.91 (0.89, 0.94) |
| Age | ||||
| 18-24 | 2027 | 8.1 (7.8, 8.5) | ||
| 25-29 | 1337 | 9.9 (9.4, 10.5) | ||
| 30-34 | 3398 | 20.3 (19.6, 21) | ||
| 35-39 | 9209 | 48.0 (47.0, 49.0) | ||
| 40-44 | 21683 | 100.2 (98.9, 101.5) | ||
| 45-49 | 41950 | 175.2 (173.5, 176.8) | ||
| 50-54 | 66614 | 261.5 (259.5, 263.4) | ||
| 55-59 | 83268 | 340.0 (337.7, 342.3) | Per decade estimate | Per decade estimate |
| 60-64 | 84753 | 422.8 (419.9, 425.6) | 2.35 (2.34, 2.36) | 2.35 (2.34, 2.36) |
CI, confidence interval.
Estimates from multivariable Poisson regression model including age, sex, geographic region, and calendar year.
Northeast, Midwest, South, and West correspond to the United States Census Bureau regions (https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf).
After accounting for these predictors of repair rates simultaneously in a Poisson regression model, the same associations were observed with higher rates in men, older people, and those living in the Midwest (Table I). After accounting for demographic differences across time, repair rates increased by 1.6% per year (95% CI: +1.4, +1.7%). The highest increases in repair rates across time were observed among patients aged 50-64 years (+2.0%, 95% CI: +1.8, +2.2%; Fig. 1, B). By contrast, repair rates decreased slightly in those 18-34 years of age (-1.3%, 95% CI: -2.2, -0.4%). As trends did not appear linear across time, we assessed changes in rates before and after 2010. From 2007 to 2010, overall rates increased by 3.4% per year (95% CI: +3.0, +3.9), while from 2011 to 2016, significantly smaller increases of 0.9% per year were observed (95%CI: +0.7, +1.1). Similar patterns were observed in specific age groups. In those 18-34 and 35-49 years of age, increase in repair rates was observed from 2007 to 2010 but not during 2011 to 2016 (18-34 years = -3.2%, 95% CI: -4.6%, -1.8%; 35-49 years = -0.1%, 95% CI: -0.5%, +0.4%). In those 50- to 64-years-old individuals, significant increases in repair rates were still observed during the later 2011-2016 period (+1.5%, 95% CI: +1.3%, +1.8%), but these increases were smaller than those observed in the previous 2007-2010 period (+3.3%, 95% CI: +2.8%, +3.8%).
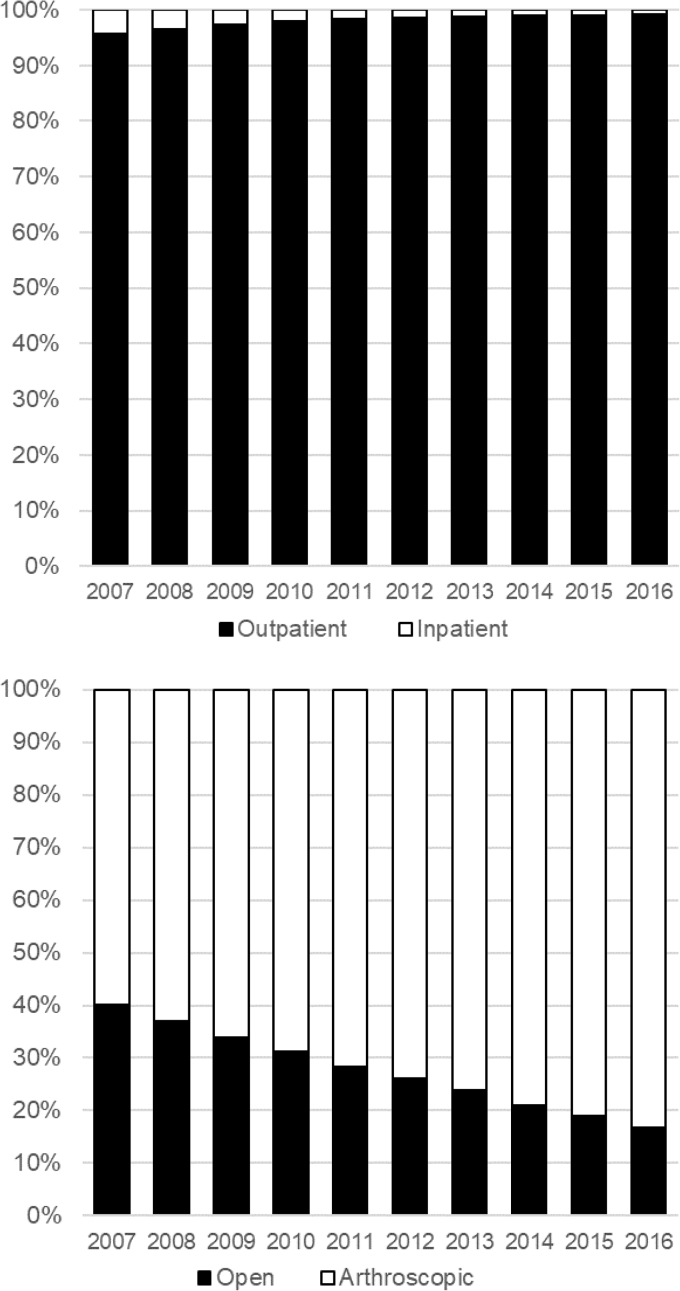
Rotator cuff repairs were more frequently performed using an arthroscopic approach and in an outpatient setting in later calendar years (Fig. 2). In 2007, 60% of rotator cuff repairs were arthroscopic procedures and 96% were performed as outpatient procedures. By contrast, in 2016, 83% of rotator cuff repairs were arthroscopic procedures and 99% were performed as outpatient procedures.
Figure 2.
Rotator cuff repair cases by approach and hospital admission. Arthroscopic approach defined as procedures coded with CPT code 29827. Open approach defined as procedures coded with CPT codes 23410, 23412, and 23420. CPT, Current Procedural Terminology.
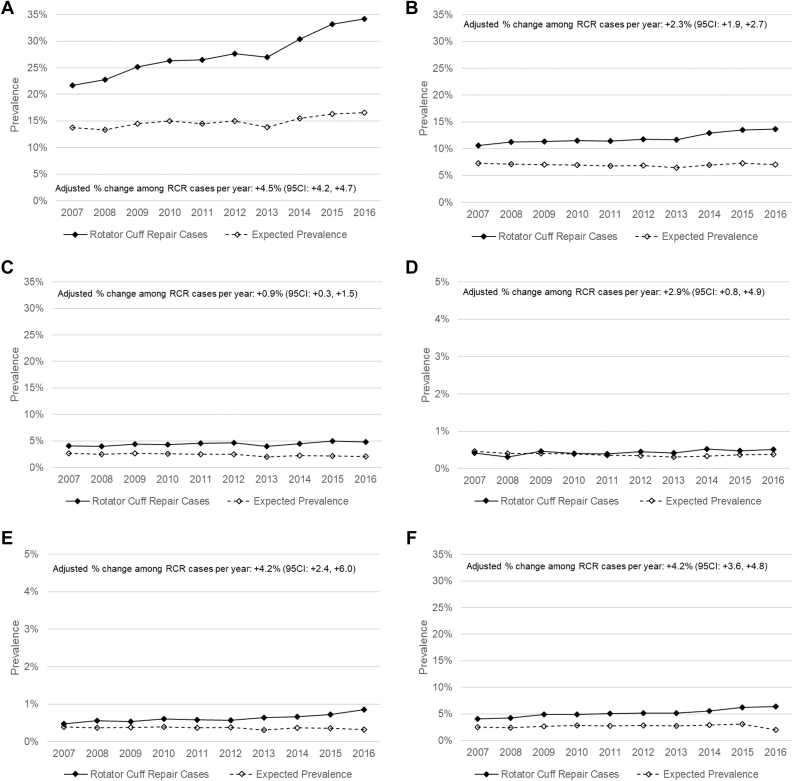
Prevalence of examined comorbidities in rotator cuff repair patients increased significantly across calendar time by 4.5% per year for hypertension (95% CI: +4.2, +4.7%), 2.3% per year for diabetes (+1.9, +2.7%), 0.9% per year for hypercholesterolemia (+0.3, +1.5%), 2.9% for congestive heart failure (+0.8, +4.9%), 4.2% for peripheral vascular disease (+2.4, +6.0%), and 4.2% for chronic pulmonary disease (+3.6, +4.8%) (Fig. 3, A–F). Elixhauser readmission comorbidity scores also increased across time from a mean score of 2.08 in 2007 to a mean score of 2.82 in 2016 with an average increase of 0.07 per year (95% CI: 0.07, 0.08; Table II).
Figure 3.
Observed prevalence among rotator cuff repair cases and expected prevalence based on the general commercially insured population for (A) hypertension, (B) diabetes, (C) hypercholesterolemia, (D) congestive heart failure, (E) peripheral vascular disease, and (F) chronic obstructive pulmonary disease. Comorbidities were defined as presence of 1 inpatient claim or 2 outpatient claims within the past year. Expected prevalence is calculated by applying age-specific prevalence estimates from a 5% sample of the MarketScan database’s commercially insured population to age strata in the rotator cuff repair population during each calendar year.
Table II.
Trend in Elixhauser comorbidity scores among rotator cuff repair cases across time.
| Calendar year | N | Mean Elixhauser score (SD) | Unadjusted mean score change per year (95% CI) | P value |
|---|---|---|---|---|
| 2007 | 23,131 | 2.08 (5.17) | 0.08 (0.07, 0.09) | <.0001 |
| 2008 | 26,809 | 2.13 (5.19) | ||
| 2009 | 37,053 | 2.30 (5.47) | ||
| 2010 | 33,833 | 2.38 (5.66) | ||
| 2011 | 35,534 | 2.42 (5.67) | ||
| 2012 | 42,243 | 2.50 (5.91) | ||
| 2013 | 32,251 | 2.45 (5.71) | Adjusted mean score change per year (95% CI)∗ | Adjusted P value |
| 2014 | 34,475 | 2.63 (6.00) | ||
| 2015 | 24,692 | 2.84 (6.35) | 0.07 (0.07, 0.08) | <.0001 |
| 2016 | 24,218 | 2.82 (6.48) |
CI, confidence interval; SD, standard deviation.
Elixhauser Comorbidity Readmission score based on index developed by AHRQ: https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp.
Estimates from multivariable linear regression model including age, sex, and geographic region.
Prevalence of these comorbidities in the rotator cuff repair population was consistently higher than prevalence observed in the general commercially insured population. In 2007, the prevalence of all comorbidities examined, except congestive heart failure, was higher in rotator cuff repair patients than in the general commercially insured population even after accounting for age, sex, and geographic region (Table III). Furthermore, the heightened prevalence increased across calendar time. The elevations in prevalence observed in 2016 were significantly higher than those observed in 2007 for all comorbidities. For example, hypertension prevalence was 1.58 times higher in patients with rotator cuff repair than the general population in 2007 (95% CI = 1.53-1.62) and 2.06 times higher in patients with cuff repair than the general population in 2016 (95% CI = 2.02-2.11).
Table III.
Standardized morbidity ratios comparing observed prevalence of comorbidities in patients with rotator cuff repair with expected comorbidities based on a 5% sample of the commercially insured population.
| Comorbidity | 2007 |
2016 |
||
|---|---|---|---|---|
| SMR | 95% CI | SMR | 95% CI | |
| Hypertension | 1.58 | 1.53, 1.62 | 2.06 | 2.02, 2.11 |
| Diabetes | 1.46 | 1.40, 1.52 | 1.94 | 1.88, 2.01 |
| Hypercholesterolemia | 1.55 | 1.45, 1.65 | 2.31 | 2.18, 2.45 |
| Congestive heart failure | 0.91 | 0.73, 1.10 | 1.35 | 1.12, 1.61 |
| Peripheral vascular disease | 1.22 | 1.00, 1.47 | 2.64 | 2.29, 3.03 |
| Chronic pulmonary disease | 1.65 | 1.55, 1.76 | 3.25 | 3.09, 3.41 |
CI, confidence interval; SMR, standardized morbidity ratio.
Discussion
This study represents one of the most comprehensive assessments of rotator cuff repair trends in the US population younger than 65 years of age. We demonstrated that rotator cuff repair rates have continued to increase over time, largely driven by older patients. In addition, we saw increasing trends in the prevalence of numerous comorbidities among cuff repair patients, which could in turn influence complication rates and functional outcomes.
Prior articles have shown increasing US rotator cuff repair rates in the early 2000s.3,35 We observed these same trends and also showed continued increases in repair rates through 2016. However, the rate of increase slowed after 2010. Increasing repair rates also coincided with continued increases in the proportion of procedures that were performed arthroscopically and in the outpatient setting as has been observed in previous years.9,17,35 It may appear paradoxical that procedures are more frequently being performed in the outpatient setting over the same time period when comorbidities are becoming more common in patients. However, trends toward less-invasive surgical approaches and better regional pain control have likely made these procedures more amenable to the outpatient setting even in patients with comorbidities. After looking at trends for different age groups, we found that most of the increase in repair rates was attributable to trends in older patients, specifically those 50 to 64 years of age. In fact, this was the only age group in which increases in repair rates were observed after 2010. This could be owing to greater increases in symptomatic cuff tears in this age group and/or larger changes in preferences for surgical cuff repair over other treatment options.
Geographically, the highest rotator cuff repair rates were seen in the South and the Midwest. Studies have shown that geographic variation can directly relate to surgeon availability and geographic differences in surgical indications.3,11 Variation could also be driven by occupational differences, as more individuals hold jobs requiring physical labor in the Midwest and South. For instance, a significantly higher proportion of the working population in the Midwest and South was used in the manufacturing industry compared with the Northeast and West during 2014-2018.31 This may be particularly relevant to the cuff repair rates in our study population which consisted of people who are still below traditional retirement age.
Among patients undergoing rotator cuff repair we observed an increasing prevalence of all the comorbidities, we examined over time. In later calendar years compared to earlier years, the average patient generally appeared to be in poorer health as captured by the Elixhauser comorbidity readmission score. Higher prevalence of comorbidities was observed in cuff repair patients than the general population, which may be attributable to these comorbidities serving as risk factors for rotator cuff degeneration or being closely linked to risk factors for rotator cuff degeneration such as smoking and obesity.1,4,6,10,16 However, not only was prevalence in patients with cuff repair higher than in the general population but prevalence increased more rapidly over time in patients with cuff repair than in the general population. This likely represents an expansion in the population being indicated for rotator cuff repair surgery. Whether because of increasing prevalence in the US population or changes in surgical indications, as comorbidities become more prevalent in patients with cuff repair, this may have important implications for surgical outcomes. Beyond the higher Elixhauser readmission scores we calculated, presence of many of these comorbidities will lead to higher scores for several indices such as the Modified Frailty Index, Charlson comorbidity index, and American Society of Anesthesiologists classification, which have been shown to predict risk of complications in orthopedic surgery generally and rotator cuff repair specifically.20,28, 29, 30 Meanwhile, inferior functional and radiographic outcomes are reported among patients with diabetes and hypercholesterolemia.8,14,22
This study has several strengths. It provides a very large, geographically representative sample of the adult US population younger than the age of 65 years. Using this sample, we are able to produce some of the most up-to-date assessments of trends in cuff repairs. In addition, we identified numerous chronic comorbidities in patients with cuff repair, enabling a more detailed characterization of the condition of these patients going into surgery than most prior studies.
This study also has important limitations. First, while we had a large sample population, the MarketScan database does not cover all patients obtaining cuff repairs in United States and disproportionately captures people working for large corporations. As a result, our population likely under-samples people with lower socioeconomic status who may have more comorbidities, worse overall health, and worse surgical outcomes. As most people in the United States of age 65 years and older use Medicare rather than commercial insurance, our study did not include this older age group, even though these individuals would be most at risk for developing new symptomatic rotator cuff tears. Furthermore, while administrative data provide reliable capture of rotator cuff repairs, it is a less reliable source for rotator cuff disease as capture is dependent on presentation to clinical care and appropriate diagnosis. As such, we cannot determine the extent to which differences in surgery rates are due to differences in underlying disease rates.
Conclusions
From 2007 to 2016 rotator cuff repairs became more frequent in the US commercially insured population, particularly in those 50-64 years of age. In later calendar years, more rotator cuff repairs were being performed using an arthroscopic approach and in an outpatient setting. Over the same time period, the comorbidity profile of patients undergoing rotator cuff repair became more complex with greater prevalence of numerous conditions, including hypertension, peripheral vascular disease, and chronic pulmonary disease. These increases in comorbidities were not explained by proportionate increases in the general population and could lead to worsening surgical outcomes.
Disclaimers
Funding: ELY received funding from the National Institutes of Health K01AR073318. This study was supported by the Washington University Center for Administrative Data Research. The Center for Administrative Data Research is supported in part by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR002345 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) and Grant Number R24 HS19455 through the Agency for Healthcare Research and Quality (AHRQ).
Conflicts of interest: ELY reports grants from the National Institutes of Health and the Orthopaedic Research and Education Foundation. AMC reports personal fees from DePuy/Mitek, Arthrex, grants from Zimmer Biomet, and grants from National Institutes of Health outside the submitted work. JDK reports consulting fees and royalties from Shoulder Innovations and Wright Medical, and a grant from the National Institutes of Health.
Acknowledgments
The authors would like to specifically acknowledge analytic work performed by Andrew Tipping at the Center for Administrative Data Research to support this research.
Footnotes
This research was determined exempt from institutional review board approval because it involved use of a limited data set and execution of a Data Use Agreement.
References
- 1.Abboud J.A., Kim J.S. The effect of hypercholesterolemia on rotator cuff disease. Clin Orthop Relat Res. 2010;468:1493–1497. doi: 10.1007/s11999-009-1151-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adamson D.M., Chang S., Hansen L.G. In: Analytics T.H., editor. Thomson Medstat; Ann Arbor, MI: 2005. Health research data for the real world: The MarketScan Databases. [Google Scholar]
- 3.Austin D.C., Torchia M.T., Lurie J.D., Jevsevar D.S., Bell J.E. Identifying regional characteristics influencing variation in the utilization of rotator cuff repair in the United States. J Shoulder Elbow Surg. 2019;28:1568–1577. doi: 10.1016/j.jse.2018.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baumgarten K.M., Gerlach D., Galatz L.M., Teefey S.A., Middleton W.D., Ditsios K., et al. Cigarette smoking increases the risk for rotator cuff tears. Clin Orthop Relat Res. 2010;468:1534–1541. doi: 10.1007/s11999-009-0781-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bureau of the Census . Commerce UDo. 1994. Geographic Areas Reference Manual.https://www.census.gov/programs-surveys/geography/guidance/geographic-areas-reference-manual.html Available at: Bureau of the Census. [Google Scholar]
- 6.Carbone S., Gumina S., Arceri V., Campagna V., Fagnani C., Postacchini F. The impact of preoperative smoking habit on rotator cuff tear: cigarette smoking influences rotator cuff tear sizes. J Shoulder Elbow Surg. 2012;21:56–60. doi: 10.1016/j.jse.2011.01.039. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention . Data and Statistics. 2019. The Diabetes Atlas.https://www.cdc.gov/diabetes/data/ Available at: Centers for Disease Control and Prevention. [Google Scholar]
- 8.Chung S.W., Oh J.H., Gong H.S., Kim J.Y., Kim S.H. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med. 2011;39:2099–2107. doi: 10.1177/0363546511415659. [DOI] [PubMed] [Google Scholar]
- 9.Colvin A.C., Egorova N., Harrison A.K., Moskowitz A., Flatow E.L. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94:227–233. doi: 10.2106/JBJS.J.00739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Djerbi I., Chammas M., Mirous M.P., Lazerges C., Coulet B., French Society For S., et al. Impact of cardiovascular risk factor on the prevalence and severity of symptomatic full-thickness rotator cuff tears. Orthop Traumatol Surg Res. 2015;101:S269–S273. doi: 10.1016/j.otsr.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Dunn W.R., Schackman B.R., Walsh C., Lyman S., Jones E.C., Warren R.F., et al. Variation in orthopaedic surgeons' perceptions about the indications for rotator cuff surgery. J Bone Joint Surg Am. 2005;87A:1978–1984. doi: 10.2106/JBJS.D.02944. [DOI] [PubMed] [Google Scholar]
- 12.Farley K.X., Wilson J.M., Spencer C.C., Karas S., Xerogeanes J., Gottschalk M.B., et al. Preoperative opioid use is a risk factor for revision surgery, complications, and increased resource utilization after arthroscopic rotator cuff repair. Am J Sports Med. 2020;48:3339–3346. doi: 10.1177/0363546520960122. [DOI] [PubMed] [Google Scholar]
- 13.Fowles J.B., Lawthers A.G., Weiner J.P., Garnick D.W., Petrie D.S., Palmer R.H. Agreement between physicians' office records and medicare part B claims data. Health Care Financ Rev. 1995;16:189–199. [PMC free article] [PubMed] [Google Scholar]
- 14.Garcia G.H., Liu J.N., Wong A., Cordasco F., Dines D.M., Dines J.S., et al. Hyperlipidemia increases the risk of retear after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2017;26:2086–2090. doi: 10.1016/j.jse.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 15.Gumina S., Arceri V., Carbone S., Albino P., Passaretti D., Campagna V., et al. The association between arterial hypertension and rotator cuff tear: the influence on rotator cuff tear sizes. J Shoulder Elbow Surg. 2013;22:229–232. doi: 10.1016/j.jse.2012.05.023. [DOI] [PubMed] [Google Scholar]
- 16.Gumina S., Candela V., Passaretti D., Latino G., Venditto T., Mariani L., et al. The association between body fat and rotator cuff tear: the influence on rotator cuff tear sizes. J Shoulder Elbow Surg. 2014;23:1669–1674. doi: 10.1016/j.jse.2014.03.016. [DOI] [PubMed] [Google Scholar]
- 17.Iyengar J.J., Samagh S.P., Schairer W., Singh G., Valone F.H., 3rd, Feeley B.T. Current trends in rotator cuff repair: surgical technique, setting, and cost. Arthroscopy. 2014;30:284–288. doi: 10.1016/j.arthro.2013.11.018. [DOI] [PubMed] [Google Scholar]
- 18.Karjalainen T.V., Jain N.B., Heikkinen J., Johnston R.V., Page C.M., Buchbinder R. Surgery for rotator cuff tears. Cochrane Database Syst Rev. 2019;12:CD013502. doi: 10.1002/14651858.CD013502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keener J.D., Patterson B.M., Orvets N., Chamberlain A.M. Degenerative rotator cuff tears: refining surgical indications based on natural history data. J Am Acad Orthop Surg. 2019;27:156–165. doi: 10.5435/JAAOS-D-17-00480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khazi Z.M., Lu Y., Cregar W., Shamrock A.G., Gulbrandsen T.R., Mascarenhas R., et al. Inpatient arthroscopic rotator cuff repair is associated with higher postoperative complications compared with same-day discharge: a matched cohort analysis. Arthroscopy. 2021;37:42–49. doi: 10.1016/j.arthro.2020.07.021. [DOI] [PubMed] [Google Scholar]
- 21.Klabunde C.N., Potosky A.L., Legler J.M., Warren J.L. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–1267. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 22.Lee S., Park I., Lee H.A., Shin S.J. Factors related to symptomatic failed rotator cuff repair leading to revision surgeries after primary arthroscopic surgery. Arthroscopy. 2020;36:2080–2088. doi: 10.1016/j.arthro.2020.04.016. [DOI] [PubMed] [Google Scholar]
- 23.Lunati M.P., Wilson J.M., Farley K.X., Gottschalk M.B., Wagner E.R. Preoperative depression is a risk factor for complication and increased health care utilization following total shoulder arthroplasty. J Shoulder Elbow Surg. 2021;30:89–96. doi: 10.1016/j.jse.2020.04.015. [DOI] [PubMed] [Google Scholar]
- 24.Moore B.J., White S., Washington R., Coenen N., Elixhauser A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: The AHRQ Elixhauser Comorbidity index. Med Care. 2017;55:698–705. doi: 10.1097/MLR.0000000000000735. [DOI] [PubMed] [Google Scholar]
- 25.Pedowitz R.A., Yamaguchi K., Ahmad C.S., Burks R.T., Flatow E.L., Green A., et al. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on: optimizing the management of rotator cuff problems. J Bone Joint Surg Am. 2012;94:163–167. [PubMed] [Google Scholar]
- 26.Pilkerton C.S., Singh S.S., Bias T.K., Frisbee S.J. Changes in cardiovascular health in the United States, 2003-2011. J Am Heart Assoc. 2015;4:e001650. doi: 10.1161/JAHA.114.001650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quam L., Ellis L.B.M., Venus P., Clouse J., Taylor C.G., Leatherman S. Using claims data for epidemiologic research. the concordance of claims-based criteria with the medical record and patient survey for identifying a hypertensive population. Med Care. 1995;31:498–507. [PubMed] [Google Scholar]
- 28.Runner R.P., Bellamy J.L., Vu C.C.L., Erens G.A., Schenker M.L., Guild G.N., 3rd Modified frailty index is an effective risk assessment tool in primary total knee arthroplasty. J Arthroplasty. 2017;32:S177–S182. doi: 10.1016/j.arth.2017.03.046. [DOI] [PubMed] [Google Scholar]
- 29.Sager B., Ahn J., Tran J., Khazzam M. Timing and risk factors for venous thromboembolism after rotator cuff repair in the 30-day perioperative period. Arthroscopy. 2019;35:3011–3018. doi: 10.1016/j.arthro.2019.05.045. [DOI] [PubMed] [Google Scholar]
- 30.Traven S.A., McGurk K.M., Reeves R.A., Walton Z.J., Woolf S.K., Slone H.S. Modified frailty index predicts medical complications, length of stay, readmission, and mortality following total shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28:1854–1860. doi: 10.1016/j.jse.2019.03.009. [DOI] [PubMed] [Google Scholar]
- 31.U.S. Census Bureau . 2014-2018 American Community Survey 5-Year Estimates. 2018. Selected Economic Characteristics.https://www.census.gov/acs/www/data/data-tables-and-tools/american-factfinder/ Available at: U.S. Census Bureau. [Google Scholar]
- 32.Wilson J.M., Farley K.X., Broida S.E., Bradbury T.L., Guild G.N. Metformin use is associated with fewer complications in patients with type-2 diabetes undergoing total knee arthroplasty: a propensity score-matched analysis. J Bone Joint Surg Am. 2021;103:601–608. doi: 10.2106/JBJS.20.01535. [DOI] [PubMed] [Google Scholar]
- 33.Yamaguchi K., Ditsios K., Middleton W.D., Hildebolt C.F., Galatz L.M., Teefey S.A. The demographic and morphological features of rotator cuff disease. J Bone Joint Surg Am. 2006;88A:1699–1704. doi: 10.2106/JBJS.E.00835. [DOI] [PubMed] [Google Scholar]
- 34.Yamamoto A., Takagishi K., Osawa T., Yanagawa T., Nakajima D., Shitara H., et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19:116–120. doi: 10.1016/j.jse.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 35.Zhang A.L., Montgomery S.R., Ngo S.S., Hame S.L., Wang J.C., Gamradt S.C. Analysis of rotator cuff repair trends in a large private insurance population. Arthroscopy. 2013;29:623–629. doi: 10.1016/j.arthro.2012.11.004. [DOI] [PubMed] [Google Scholar]