Abstract
Diabetes mellitus is a chronic complication that affects people of all ages. The increased prevalence of diabetes worldwide has led to the development of several synthetic drugs to tackle this health problem. Such drugs, although effective as antihyperglycemic agents, are accompanied by various side effects, costly, and inaccessible to the majority of people living in underdeveloped countries. Medicinal plants have been used traditionally throughout the ages to treat various ailments due to their availability and safe nature. Medicinal plants are a rich source of phytochemicals that possess several health benefits. As diabetes continues to become prevalent, health care practitioners are considering plant-based medicines as a potential source of antidiabetic drugs due to their high potency and fewer side effects. To better understand the mechanism of action of medicinal plants, their active phytoconstituents are being isolated and investigated thoroughly. In this review article, we have focused on pharmacologically active phytomolecules isolated from medicinal plants presenting antidiabetic activity and the role they play in the treatment and management of diabetes. These natural compounds may represent as good candidates for a novel therapeutic approach and/or effective and alternative therapies for diabetes.
Keywords: medicinal plants, traditional medicine, phytoconstituents, diabetes, pharmacology
1. Introduction
Diabetes mellitus is one of the most common endocrine metabolic disorders characterized by chronic hyperglycemia caused by varying degrees of insulin resistance, deficiency in insulin secretion, or both [1]. Nearly 10.5% of the worldwide population is affected by diabetes, with its prevalence increasing at an alarming rate. According to data collected from the International Diabetes Federation (IDF), about 783.2 million people are estimated to be diagnosed with diabetes by 2045 [2]. Diabetes mellitus can be classified into two major categories: Type 1 and Type 2 diabetes, where Type 2 diabetes accounts for about 90% of all cases. Type 1 diabetes, previously known as insulin-dependent diabetes, is an autoimmune disorder that occurs due to the destruction of the pancreatic beta cells leading to significantly reduced secretion of insulin [3]. It is a non-hereditary genetic condition that mainly affects the juvenile under thirty years of age. Type 2 diabetes, also known as non-insulin-dependent diabetes, is the most common form of diabetes, with its prevalence rapidly rising worldwide [4]. It is a hereditary condition caused as a result of insulin resistance, insufficient insulin secretion, or a combination of both, largely affecting an older population than Type 1 diabetes [5]. Both forms of diabetes alter carbohydrate, protein, and fat metabolism. The effect of insulin resistance leads to high blood sugar levels by hindering the uptake and efficient use of glucose by most cells of the body [6]. The progression of the disease is accompanied by tissue or vascular damage resulting in severe complications, including retinopathy, diabetic neuropathy, nephropathy, cardiovascular, pulmonary, cerebral, and peripheral vascular diseases, ulcers, and thyroid gland disorders, leading to serious morbidity and mortality [1,7,8,9]. Available therapies currently in use for the treatment and management of diabetes include insulin and several oral hypoglycemic agents such as metformin, sulfonylureas, α-glucosidase inhibitors, meglitinide analogues, thiazolidinediones, DPP-IV inhibitors, SGLT-2 inhibitors, and GLP-1 mimetics. However, these drugs, intended to boost insulin sensitivity and increase insulin secretion together with the reduction in circulatory plasma glucose levels by increasing glucose excretion or uptake in adipose tissue, are usually associated with many side effects. These include, among others, weight gain, hypoglycemia, gastrointestinal tract disturbances, liver injury, renal failure, hypersensitivity reactions, flatulence, diarrhea, and abdominal bloating [1,10,11]. In addition, these drugs have been known to have other major disadvantages, including drug resistance, and there is also a lack of therapies to prevent the long-term complications of the disease.
The complications associated with insulin and oral antidiabetic agents, together with limited drug tolerability, adverse effects, and cost, have accelerated the search for alternative medicines with better efficacy, potency, and fewer side effects [12]. Interestingly, there has been an increase in popularity surrounding drug discovery research into natural antidiabetic agents, especially those derived from medicinal plants, which could enhance β-cell function and treat diabetes-associated complications with fewer adverse side effects [13].
Herbal medicines contain a diversity of phytochemicals and have been traditionally used for treating a wide variety of diseases. They are considered to be naturally safe and efficacious with fewer side effects [12]. The control and management of diabetes using herbal drugs have proven to be more advantageous over synthetic medicines due to their accessibility, reduced cost, lesser complications, and lower side effects. Herbal medicines act via different mechanisms aiming at reducing insulin resistance, increasing insulin secretion, protecting pancreatic beta cells, and thereby lowering circulating blood glucose levels [14].
Throughout the years, thousands of plant species have been used for their medicinal uses as integrative medicines for various diseases, of which more than 800 plants have been reported to exhibit antidiabetic effects [15]. Such plants have been examined for their use in the treatment of the different types of diabetes and could be potential sources for new natural antidiabetic drug discovery research [16]. A number of medicinal plants used traditionally for their antidiabetic activity are currently under investigation to be formulated commercially as modern drugs. This is particularly the case in developing countries where the cost of allopathic medicine is high, and the traditional use of plants to treat diabetes is common practice [15]. Traditional natural medicines are extensively prescribed in Asian countries (e.g., China, India, Bangladesh, Pakistan, Sri Lanka, Thailand, Nepal, Bhutan, Japan, and others) [17]. Among the medicinal plants possessing hypoglycemic effects, the most common ones used as remedies for diabetes include Acacia arabica, Aegle marmelos, Allium cepa, Allium sativum, Aloe vera, Annona squamosa, Azadirachta indica, Berberis vulgaris, Camellia sinensis, Capsicum frutescens, Cassia alata, Cinnamomum zeylanicum, Eucalyptus globulus, Eugenia jambolana, Helicteres isora, Momordica charantia, Panax ginseng, Punica granatum, Swertia chirayita, Trigonella foenum-graecum, and others [15,16,18,19]. The antidiabetic activity of these plants is thought to be mediated via various mechanisms, including the stimulation of insulin secretion from pancreatic β-cells, increasing insulin binding to receptors, reduction in insulin resistance, and improving glucose tolerance. Other modes of action include enhancing glucose metabolism, improving β-cell mass and function, and increasing plasma insulin, thus decreasing circulating blood glucose levels [20,21,22,23]. In addition to being used to treat diabetes, these plants have also been traditionally employed to treat other conditions such as ulcers, wounds, inflammation, infections, diarrhea, dysentery, malaria, rheumatism, hypertension, obesity, pneumonia, and kidney diseases [12,19,24,25,26]. The main objective of this review is to explore the traditional plant-based therapies and/or their phytoconstituents available for the treatment of diabetes. These could provide the basis for the discovery of new antidiabetic drugs with fewer side effects and stronger efficacy than currently available medicines.
2. Methods
A literature search was carried out via Google Scholar, ScienceDirect, Scopus, and PubMed databases to accumulate data for this review article using the keywords “Diabetes mellitus,” “Medicinal Plants,” “Traditional medicine,” “Antidiabetic phytochemicals,” and “Plant-based antidiabetic therapy.” The data search was not restricted to a specific time period; however, around 98% of the gathered data were published between 2000 and 2022, and only 2% were published before 2000. Our data collection began in early January until late May 2022. More than 700 papers were found relevant to our study, and after performing a primary screening, around 400 papers were selected to be critically examined. An overview of the key findings has been presented in this current review.
3. Ethnomedicines and Their Scope in the Modern World
Ethnomedicine is a traditional health care practice followed by indigenous people concerned with human health. It is the origin of all other traditional medical systems, including Ayurveda, Siddha, Unani, Nature Cure, as well as modern medicine [27]. Knowledge of plants presenting therapeutic properties has been passed on by experimenting through trials and errors from one generation to the next for more than hundreds of years. Ethnomedicines are highly prevalent in the rural and native communities of several developing countries [28]. According to information collected from the World Health Organization, about 80% of the global population relies upon traditional remedies [29]. Medicinal plants have always been recognized as a major source of raw materials for both conventional and traditional medicines [30]. In India, the poor and rural residents are dependent upon natural herbal remedies since they are easily obtainable to them. Indeed, plant-based medicines are the sole source of medical management for people living in remote areas. In countries such as Russia, Africa, and a few European countries, ethnomedicines are being studied by various botanists, anthropologists, folklorists, and medical scientists [27]. The inability for people to access adequate healthcare, alongside financial restrictions, has resulted in the under-provision of modern health care for a majority of the people in underdeveloped countries. [31]. Numerous folk remedies are recorded as being effective in treating various diseases (such as digestive tract disorders, skin diseases, renal and liver diseases, malaria, ulcers, heart diseases, pneumonia, diabetes, and many others), and thus, even developed countries have also considered utilizing these medicines [32].
4. Plant-Based Medicine versus Synthetic Medicine
Many drugs that are currently available have been derived directly or indirectly from natural sources such as medicinal plants and animals [33,34]. Plant-derived natural products have played and continue to play a prominent role in drug discovery and development programs. The increase in the number of herbal drug manufacturing companies, linked to the current increase in interest and demand for herbal medicines, can be largely expanded because of the toxicity and numerous adverse effects of allopathic medicines [35]. The convenience of accessibility, availability, inexpensiveness, and relatively low risks of side effects, have caused plant-based medicines to be an important alternative source of existing therapies, especially in rural and/or developing regions [33]. Plant-based medicines also provide a rich source of biologically active compounds that possess pharmacological activity with minimal undesirable effects [33].
Over the centuries, plant-based medicines have been widely used to treat the ailments of local communities of many developing countries that have easy access to these sources. Densely populated countries, such as China and India, have especially contributed to the advancement of sophisticated traditional medical systems such as acupuncture, ayurvedic medicine, and herbal medicine [36]. Many factors should be considered when selecting the appropriate medications for the management and treatment of diabetes. This includes efficacy, adverse effects, cost, and potential to contribute to weight gain, risks associated with hypoglycemia, comorbidities, and patient compliance. Even though oral antihyperglycemic agents can lower plasma glucose levels by improving insulin secretion or reducing insulin resistance, they are associated with many other adverse effects. Metformin, the mainstay of treatment in type 2 diabetes, has a high safety profile, yet it is still associated with mild side effects such as low risks of hypoglycemia and gastrointestinal tract disturbances (nausea, diarrhea, dyspepsia). Previous studies have shown that continuous use of metformin may result in vitamin B12 and folic acid deficiency in humans [37]. DPP-IV inhibitors such as sitagliptin, saxagliptin, and linagliptin, have been found to cause headaches, nasopharyngitis, and upper respiratory tract infections [38]. The most common adverse effect of sulphonylureas such as glimepiride and gliclazide is hypoglycemia. These drugs are also associated with minor side effects such as weight gain, nausea, headaches, drowsiness, and hypersensitivity reactions. The most serious complication of insulin injections is hypoglycemia. Insulin may also cause weight gain or loss, dizziness, confusion, and sweating [38]. In contrast to synthetic drugs, plant-based medicines do not interrupt the body’s natural healing process; instead, they accelerate the recovery process by strengthening the healing process, ultimately leading to a steady recovery. Alongside their ability to help the body recover to a healthy status, herbal medicines are also known for boosting the immune system. The use of highly effective herbal medicines showing fewer side effects and a strong immune system together with a healthy lifestyle promotes better body metabolism with increased nutritional absorption from the diet [35]. Whether they have insulinotropic, insulin-mimetic, or any other antihyperglycemic effects, medicinal plants are considered safer and more effective alternatives to synthetic antidiabetic drugs [39].
5. Pharmacological Activity of Plant-Based Medicines
Although knowledge of many plant-based therapies has been transmitted through generations, only a few of these have started to come to the fore recently. However, there is still some uncertainty regarding their pharmacological activity as well as their acute/chronic side effects due to such medicines being broadly underreported [40]. Few plants have proven to be efficacious for which they were intended, whilst some were not strongly therapeutically effective and/or sufficient scientific data were lacking to support their expected effects [41]. The increase in the widespread use of plant-based therapies has led to an urgent need for a detailed scientific examination of the chemicals responsible for pharmacological activity. Indeed, such a study of the pharmacological properties and phytoconstituents of plant-based medicines may lead to the discovery of new pharmacological characteristics previously unknown or used in traditional medicine [42]. Herbal medicines have been suggested to exert their mechanism of action by concurrently targeting multiple physiological processes via interactions between different biochemicals and cellular proteins [43].
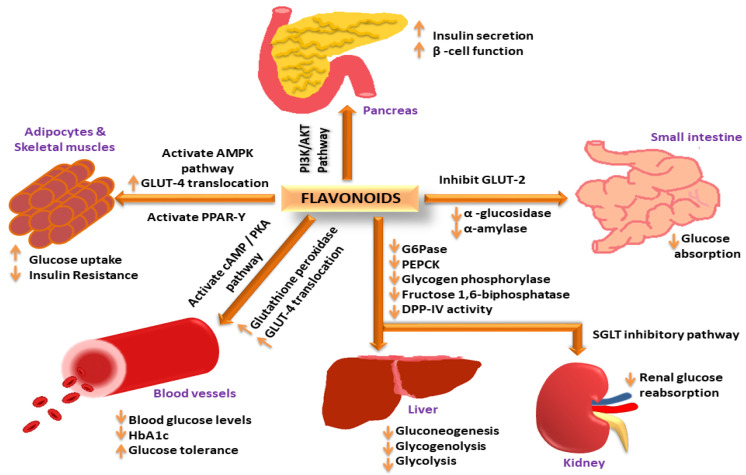
Herbal medications may be able to alter the biological systems from disease to a healthy state by causing the interactions between multi-component and multi-target. Because of the therapeutic properties of the phytomolecules, a lower dosage may be used, resulting in less toxicity and adverse effects. [43]. The antidiabetic activity of medicinal plants is dependent upon the phytochemicals that act through multiple pathways, such as cAMP: which stimulates insulin secretion without affecting the KATP channel [44]; PI3K: which facilitates glucose uptake by the translocation of the glucose transporter in skeletal muscles, adipose tissue, or liver [45]; AMPK: The activation of 5ʹ-adenosine monophosphate-activated protein kinase pathway improves insulin sensitivity by limiting lipolysis and lipogenesis, and AMPK also enhances glucose uptake in skeletal muscles by translocating GLUT4-containing intracellular vesicles across the plasma membrane [46,47]. For example, phlorizin obtained from the bark of apple and pear trees increases glucose excretion in urine by decreasing glucose reabsorption in the kidneys via the inhibition of SGLT and thus, lowers plasma glucose concentration [48]. Some of the phytomolecules have the potential to regenerate and protect pancreatic beta cells from destruction by reducing the glucose load [49], inhibiting α-amylase and α-glucosidase activity, inducing glucose uptake in 3T3L1 cells [50,51], inhibiting aldose reductase enzyme activity, glycogen metabolizing enzymes, exerting hepato-pancreatic protective activity, inhibiting glucose-6-phosphate and DPP-IV, reducing lactic dehydrogenase, γ-glutamyl transpeptidase, glycosylated hemoglobin levels, and inhibiting glycogenolysis and gluconeogenesis in the liver [20,52]. As an example, a summary of the different pathways involved in the antidiabetic activity of flavonoids is illustrated in Figure 1. A summary of antidiabetic medicinal plants and their pharmacological actions has been shown in Table 1.
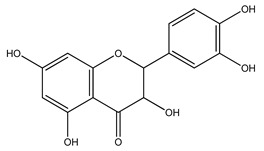
Figure 1.
Flavonoids exerting antidiabetic activity via different mechanistic pathways: Flavonoids increase insulin secretion and improve β-cell function via the PI3K/AKT signaling pathway; increase GLUT-4 translocation through AMPK activation to increase glucose uptake in adipose tissues and skeletal muscles; activate PPAR-γ expression to decrease insulin resistance; activate cAMP/PKA pathway to reduce blood glucose levels and improve glucose tolerance; increase glutathione peroxidase activity to reduce HbA1c levels; decrease G-6-Pase, PEPCK, glycogen phosphorylase, fructose 1,6-biphosphatase and DPP-IV activity in liver to decrease gluconeogenesis, glycogenolysis, and glycoslysis; inhibit SGLT pathway in kidney to decrease renal glucose reabsorption; inhibit GLUT-2, α-amylase and α-glucosidase activity to decrease glucose absorption in the small intestine.
Table 1.
Traditional uses and pharmacological effects of antidiabetic medicinal plants.
| Medicinal Plants | Parts | Traditional Uses | Pharmacological Effects | References |
|---|---|---|---|---|
|
Leaves, seeds | Diabetes, wounds, fever, cough, cold, tetanus | Improves β-cell function, inhibits α-amylase and α-glucosidase activity | [53,54] |
|
Bark, roots | Diabetes, astringent, diarrhea, parasitic worms, diuretic, liver tonic | Lowers blood glucose levels, increases insulin secretion, improves glucose uptake and glucose tolerance | [24,55] |
|
Bark | Diabetes, asthma, bronchitis, diarrhea, obesity, dysentery, skin diseases | Lowers blood glucose levels, increases insulin secretion | [56,57,58] |
|
Leaves | Diabetes, dysentery, inflammation, ulcer, diarrhea, asthma | Lowers blood glucose levels, increases insulin secretion, glucose uptake and metabolism, inhibits aldose reductase and DPP-IV enzyme activity | [56,59,60] |
|
Fruit, leaves | Diabetes, cough, diarrhea, stomach ache, leprosy, hypertension, measles | Lowers plasma glucose levels, inhibits α-amylase and α-glucosidase activity | [61,62] |
|
Leaves | Diabetes, fever, rheumatism, cardiovascular diseases, malaria, wounds, spasms | Lowers blood glucose levels, improves β-cell function, increases insulin secretion | [63,64] |
|
Bark, pods | Diabetes, asthma, diarrhea, infections, dysentery, inflammation | Lowers blood glucose levels, increases insulin secretion, enhances glucose uptake | [56,65,66] |
|
Bark, leaves | Diabetes, eye problems, hemorrhoids, skin diseases, wounds, malaria diarrhea, indigestion | Lowers blood glucose levels, improves glucose tolerance | [16,67] |
|
Bulb | Diabetes, bronchitis, hypertension, skin infections, swelling, lower cholesterol level | Increases insulin secretion and insulin sensitivity, improves glucose uptake | [68,69] |
|
Bulb | Diabetes, fever, hypertension, rheumatism, dysentery, bronchitis, intestinal worms | Increases insulin secretion and insulin sensitivity to cells | [70,71] |
|
Leaves | Diabetes, constipation, infections, ulcer, dysentery, piles, rheumatoid arthritis | Lowers blood glucose levels, increases insulin secretion, reduces insulin resistance, improves glucose tolerance | [72,73] |
|
Leaves, stem bark | Diabetes, fever, hypertension, rheumatism, toothache, piles, dysentery | Lowers blood glucose levels, reduces oxidative stress, decreases total cholesterol and triglyceride levels | [74,75,76] |
|
Rhizome | Diabetes, fever, cough, inflammation, infections, night sweats, dementia | Lowers blood glucose levels, increases insulin sensitivity, improves glucose uptake | [77,78] |
|
Leaves, bark | Diabetes, inflammation, tumors | Lowers blood glucose levels, improves β-cell function, increases insulin secretion | [79,80] |
|
Leaves | Diabetes, wounds, inflammation, hypertension, malaria, insect bites | Lowers blood glucose levels, increases insulin secretion, improves glucose tolerance and β-cell function | [10,81] |
|
Bark | Diabetes, diarrhea, hemorrhoids, dysentery, snake bites, stomach disorders, skin diseases, leprosy | Decreases blood glucose levels, improves β-cell function, increases insulin secretion, inhibits DPP-IV enzyme activity | [56,82,83] |
|
Seeds | Diabetes, inflammation, heart diseases, coagulation, rheumatism, hypertension, Alzheimer’s disease | Increases insulin secretion and insulin sensitivity, improves glucose tolerance | [84,85,86] |
|
Rhizome | Diabetes, wounds, indigestion, gastritis, anemia, hepatitis, cardiovascular diseases, gall bladder disorders | Increases insulin sensitivity, improves glucose uptake, enhances GLUT-4 translocation | [87,88,89] |
|
Leaves, rhizome | Diabetes, diarrhea, malaria, wounds, anemia, inflammation | Lowers blood glucose levels, decreases glycosylated hemoglobin levels | [78,90] |
|
Roots | Diabetes, constipation, ulcers, stomach disorders, cough, inflammation | Increases insulin secretion and action, improves β-cell function, inhibits carbohydrate digestion and absorption | [91,92,93,94] |
|
Rhizome | Diabetes, rheumatism, gastrointestinal diseases, influenza, night blindness, diuretic, stomachic | Lowers blood glucose levels, reduces insulin resistance, improves glucose uptake | [95,96] |
|
Leaves | Diabetes, malaria skin diseases, infections, cardiovascular diseases, intestinal worms | Lowers blood glucose levels, increases insulin secretion, improves pancreatic β-cell function, inhibits α-amylase and α-glucosidase activity, enhances glucose uptake | [56,97,98] |
|
Fruit | Diabetes, wounds, asthma, malaria, diarrhea, hemorrhoids, fever, infections | Increases insulin secretion, improves glucose uptake, inhibits α-glucosidase activity | [99,100] |
|
Root, bark | Diabetes, eye infections, piles, wounds, snake bites, hemorrhoids, dysentery | Reduces blood glucose levels, increases insulin secretion | [101,102] |
|
Root | Diabetes, wounds, hepatitis, diarrhea, urinary tract infections, cold, glandular sclerosis | Increases plasma insulin, improves glucose tolerance, protects or prevents islet degeneration | [103,104] |
|
Flowers, leaves | Diabetes, inflammation, ulcers, sore throat, infections, contraceptive | Regenerates β-cell function, increases plasma insulin levels, reduces intestinal glucosidase activity | [105,106] |
|
Leaves, seeds | Diabetes, arthritis, rheumatism, back pain, coughs, paralysis | Increases insulin secretion and glucose utilization | [16,107] |
|
Leaves, stem bark | Diabetes, headache, arthritis, fever, inflammation | Lowers blood glucose levels, inhibits α-amylase and α-glucosidase activity | [108,109] |
|
Seeds | Diabetes, diarrhea, gastrointestinal disorders, inflammation, obesity, asthma | Lowers blood glucose levels, improves glucose uptake and utilization | [56,110,111] |
|
Leaves | Diabetes, indigestion, flatulence, stomach aches, constipation, fever | Lowers blood glucose levels, protects pancreatic beta cells, decreases oxidative stress | [112,113] |
|
Leaves, bark | Diabetes, fever, infections, wounds, menstrual irregularity, poor eyesight, inflammation, ulcers | Lowers blood glucose levels, increases plasma insulin levels | [114,115] |
|
Leaves | Diabetes, heart diseases, diuretic, astringent, stimulant, flatulence | Increases insulin secretion and action, inhibit insulin glycation, DPP-IV enzyme, and α-amylase activity, improves glucose tolerance | [116,117] |
|
Whole plant | Diabetes, gastrointestinal disorders, toothache, pain, muscle spasms, fever, infections | Increases insulin secretion and insulin sensitivity, improves glucose uptake | [118,119] |
|
Fruit, leaves | Diabetes, gastrointestinal disorders, dengue, malaria, nerve pains, insomnia, constipation | Lowers blood glucose levels, increases insulin secretion, suppresses glucagon secretion | [120,121] |
|
Leaves, seeds | Diabetes, skin diseases, rheumatism, constipation, ringworm, infections, inflammation | Lowers blood glucose levels, inhibits α-glucosidase activity | [122,123] |
|
Stalk | Diabetes, wounds, constipation, piles, skin diseases, asthma, liver diseases, rheumatism, leprosy | Lowers blood glucose levels, increases insulin secretion, improves glucose uptake and utilization | [56,124,125,126,127] |
|
Leaves, roots | Diabetes, hypertension, menstrual irregularity, cancer, wounds, muscle pain | Lowers blood glucose levels, increases insulin sensitivity, improves glucose uptake and utilization | [128,129,130] |
|
Root bark | Diabetes, asthma, bronchitis, heart diseases, inflammation, wounds, hypertension | Lowers blood glucose levels, decreases glycosylated hemoglobin levels | [78,131] |
|
Bark, leaves | Diabetes, constipation, wounds, liver diseases | Increases insulin secretion and insulin sensitivity, improves glucose uptake | [78,132] |
|
Bark | Diabetes, common cold, flu, gastrointestinal disorders, bacterial infections, headache, stomach pain | Increases plasma insulin levels, increases insulin sensitivity, inhibits α-amylase activity | [133,134] |
|
Fruit | Diabetes, hypertension, infections, scurvy, sore throat, rheumatism | Lowers plasma glucose levels, inhibits α-amylase activity | [135,136] |
|
Fruit | Diabetes, insomnia, indigestion, constipation, heartburn, nausea, cardiovascular diseases | Lowers blood glucose levels, increases insulin secretion | [137,138] |
|
Seeds | Diabetes, dysentery, fatigue, CNS stimulant, morning sickness, migraine, indigestion, wounds | Lowers blood glucose levels, increases serum insulin levels | [139,140] |
|
Rhizome | Diabetes, sore throat, whooping cough, dysentery, neurodegenerative diseases | Lowers blood glucose levels, increases insulin sensitivity, improves glucose uptake | [141,142] |
|
Fruit, seeds | Diabetes, pain, inflammation, cardiovascular diseases, liver, and kidney diseases | Lowers blood glucose levels, increases insulin secretion, inhibits α-glucosidase activity, increases GLUT-4 expression | [143,144] |
|
Rhizome | Diabetes, gastric, inflammation, infections, cough, pain, liver diseases | Lowers blood glucose levels, inhibits α-amylase and α-glucosidase activity, increases insulin secretion, improves peripheral glucose uptake, reduces insulin resistance | [78,145,146] |
|
Bark, roots | Diabetes, hepatitis, scabies, bruises, gonorrhea, jaundice, rheumatism | Lowers blood glucose levels, increases insulin secretion, improves glucose uptake and utilization, inhibits DPP-IV enzyme and α-glucosidase activity | [56,147,148] |
|
Fruit | Diabetes, night blindness, arthritis, sprains, constipation, asthma, liver diseases, obesity | Increases insulin secretion, protects pancreatic beta cells, decreases glycosylated hemoglobin levels | [149,150] |
|
Bark | Diabetes, stomach disorders, dysentery, skin diseases, syphilis, nausea, gonorrhea | Lowers blood glucose levels, reduces serum triglyceride and cholesterol levels | [56,151,152] |
|
Leaves, seeds | Diabetes, bronchitis, inflammation, cough | Lowers blood glucose levels, reduces insulin resistance, improves glucose tolerance | [153,154] |
|
Leaves | Diabetes, fever, pain, sinusitis, bronchitis, asthma, chronic rhinitis, | Increases insulin secretion, improves glucose uptake, inhibits insulin glycation and DPP-IV enzyme activity, decreases starch digestion | [155,156] |
|
Leaves | Diabetes, cough, cold, wounds, fungal infections, fever, sore throat, pain | Increases insulin secretion, improves glucose uptake | [157,158] |
|
Root, bark | Diabetes, cough, chest pain, diarrhea, headache, toothache | Lowers blood glucose levels, inhibits α-glucosidase activity | [78,159] |
|
Seeds | Diabetes, skin ulcers, gastritis, constipation, sore throat, liver, and kidney diseases | Lowers blood glucose levels, improves pancreatic β-cell function, increases insulin secretion, inhibits sucrase and maltase activity, improves glucose uptake and metabolism | [56,160,161] |
|
Leaves | Diabetes, respiratory diseases, diarrhea, jaundice, tumors, gonorrhea | Increases insulin release from beta cells, inhibits α-glucosidase activity | [162,163] |
|
Bark, leaves | Diabetes, hypertension, dysentery, diarrhea, pain, ulcers, asthma | Decrease carbohydrate digestion and absorption, lowers blood glucose levels | [164,165] |
|
Seeds | Diabetes, diarrhea, food poisoning, bacterial infections, cough, liver diseases | Inhibits α-amylase activity, decreases glycosylated hemoglobin levels | [166,167] |
|
Seeds | Diabetes, cardiovascular diseases, obesity, cancer | Reduces insulin resistance, improves glucose tolerance | [168,169] |
|
Roots | Diabetes, epilepsy, respiratory diseases, paralysis, jaundice, rheumatism | Lowers blood glucose levels, increases insulin secretion | [56,170] |
|
Leaves | Diabetes, asthma, bronchitis, constipation, jaundice, dyspepsia, hemorrhoids, obesity | Lowers blood glucose levels, regenerates beta cells, increases insulin secretion, improves glucose tolerance | [171,172] |
|
Leaves | Diabetes, cancer, hernia, hypertension, jaundice, malaria, yellow fever | Lowers blood glucose levels, inhibits α-amylase activity | [16,173] |
|
Roots | Diabetes, diarrhea, snake bites, gastrointestinal disorders, spasms | Lowers blood glucose levels, improves glucose uptake | [174,175] |
|
Bark | Diabetes, diarrhea, constipation, dysentery, dermatitis, scabies, goiter | Decreases carbohydrate digestion and glucose absorption, lowers blood glucose levels, increases insulin secretion, improves glucose tolerance, inhibits DPP-IV enzyme activity | [26,51,176] |
|
Roots, seeds | Diabetes, gastric irritations, inflammatory diseases, wounds, and boils | Lowers blood glucose levels, improves β-cell function, increases insulin secretion | [177,178] |
|
Leaves | Diabetes, cough, diarrhea, dysentery, pain, contraceptive | Reduces glucose absorption, lowers blood glucose levels, increases insulin secretion and hepatic glucose utilization, improves glucose tolerance, inhibits DPP-IV activity | [179,180] |
|
Leaves | Diabetes, fever, bacterial and fungal infections, jaundice, muscle pain | Lowers fasting blood glucose levels, improves glucose uptake and utilization | [181,182] |
|
Leaves | Diabetes, asthma, malaria, chicken pox, hypertension, measles | Lowers elevated blood glucose levels, improves glucose tolerance | [183,184] |
|
Seeds | Diabetes, diarrhea, gastrointestinal infections, asthma, bronchitis, atherosclerosis | Lowers blood glucose levels, increases insulin secretion, improves glucose uptake and metabolism | [56,185] |
|
Leaves, seeds | Diabetes, constipation, piles, dysentery, asthma, anemia, hypertension, hemorrhage, | Lowers blood glucose levels, increases insulin secretion, improves glucose uptake, inhibits α-glucosidase and DPP-IV activity | [56,186,187] |
|
Leaves, seeds | Diabetes, malaria, hypertension, scabies, liver diseases, obesity, ulcers, measles | Lowers blood glucose levels, increases insulin secretion and glucose uptake, improves glucose tolerance, decreases gluconeogenesis, inhibits α-glucosidase activity | [56,134,188] |
|
Leaves | Diabetes, asthma, enlarged liver, bacterial infections, eye problems, piles, influenza, diuretic | Reduces glucose absorption, lowers blood glucose levels, improves glucose uptake, inhibits α-amylase activity | [189,190] |
|
Leaves | Diabetes, piles, dysentery, itching, bruises, inflammation | Lowers blood glucose levels, inhibits α-amylase and α-glucosidase activity | [78,191] |
|
Flowers | Diabetes, dysentery, ulcers, hypertension, pain, inflammation, snake bites | Lowers blood glucose levels, increases insulin secretion, decreases glucosylated hemoglobin levels | [192,193] |
|
Seeds | Diabetes, hypertension, gastrointestinal disorders, back pain, paralysis, heart diseases, bacterial infections, malaria | Decreases carbohydrate digestion and absorption, lowers blood glucose levels, increases insulin secretion and sensitivity, improves glucose uptake and utilization | [194,195] |
|
Leaves | Diabetes, headaches, constipation, coughs, kidney diseases, warts | Inhibits α-amylase and α-glucosidase activity, reduces oxidative stress, inhibits glycogenolysis | [196,197,198] |
|
Leaves | Diabetes, ringworm, skin diseases, dysentery, dyspepsia, bronchitis, asthma | Increases insulin secretion, improves glucose uptake and utilization | [149,199] |
|
Leaves | Diabetes, constipation, urinary tract infections, asthma, hypertension, intestinal diseases | Lowers blood glucose levels, increases antioxidant activity | [200,201] |
|
Roots | Diabetes, insomnia, anorexia, confusion, hemorrhage | Improves peripheral insulin action, increases insulin sensitivity, decreases carbohydrate absorption | [202,203] |
|
Stem bark | Diabetes, HIV/AIDS, wounds, rheumatism, intestinal parasites | Lowers blood glucose levels, improves glucose tolerance | [16,204] |
|
Seeds | Diabetes, hypertension, obesity, blood cancer | Reduces insulin resistance, inhibits α-amylase and DPP-IV enzyme activity | [149,205] |
|
Leaves | Diabetes, spleen, liver and kidney diseases, gonorrhea, stomach problems | Lowers blood glucose levels, increases insulin secretion, improves insulin sensitivity | [206,207] |
|
Husk | Diabetes, constipation, diarrhea, hypercholesterolemia, hypertension, hemorrhoids | Improves glucose tolerance, decreases carbohydrate digestion and glucose absorption | [208,209] |
|
Bark | Diabetes, dysentery, cough, diarrhea, skin diseases, wounds, ulcer | Improves pancreatic β-cell function, increases insulin secretion, improves glucose uptake | [149,210,211] |
|
Flowers | Diabetes, urinary tract infections, arthritis, sore throat, skin diseases, anemia | Improves β-cell function, increases insulin secretion | [210,212,213] |
|
Roots | Diabetes, anemia, obesity, kidney diseases, osteoporosis | Improves pancreatic β-cell function, increases insulin secretion, improves glucose uptake, decreases oxidative stress | [214,215] |
|
Bark | Diabetes, jaundice, diarrhea, dysentery, liver tonic, inflammation, hypertension | Lowers blood glucose levels, increases insulin secretion, improves glucose uptake and utilization | [56,216] |
|
Leaves | Diabetes, fever, epilepsy, constipation, colitis, cancer, urinary tract infections | Lowers blood glucose levels, increases insulin secretion, improves glucose uptake and utilization | [56,217] |
|
Seeds | Diabetes, constipation, hypertension, high cholesterol, athlete’s foot | Inhibits α-amylase and α-glucosidase activity, exerts antioxidant activity | [56,218,219] |
|
Leaves | Diabetes, pneumonia, toothache, stomach ache, fever, tumor, tonsilitis | Lowers blood glucose levels, increases insulin secretion, decreases gluconeogenesis, increases glycogenesis | [220,221] |
|
Whole plant | Diabetes, hypercholesterolemia, atherosclerosis, obesity | Lowers blood glucose levels, increases insulin secretion, improves glucose tolerance, inhibits DPP-IV activity | [222,223] |
|
Bark, leaves | Diabetes, malaria, hypertension, epilepsy, liver diseases, weight loss | Lowers blood glucose levels, increases insulin secretion, improves glucose uptake and metabolism, inhibits α-amylase and α-glucosidase | [56,224] |
|
Seeds | Diabetes, diarrhea, dysentery, constipation, abdominal pain, wounds, malaria | Lowers blood glucose levels, increases insulin secretion | [56,225] |
|
Bark | Diabetes, cardiotonic, anemia, viral infections, venereal diseases, ulcers | Lowers blood glucose levels, increases insulin secretion, improves glucose uptake and utilization | [56,226] |
|
Fruit | Diabetes, fever, astringent, constipation, dementia | Improves β-cell function, increases insulin secretion, reduces glycosylated hemoglobin levels | [227,228] |
|
Leaves, roots, stem | Diabetes, dysentery, diarrhea, snake bites, asthma, fever, jaundice | Increases insulin secretion, inhibits gluconeogenesis, increases insulin sensitivity | [149,229] |
|
Seeds | Diabetes, bronchitis, pneumonia, indigestion, dysentery, high cholesterol | Lowers blood glucose levels, increases insulin secretion, improves glucose uptake and utilization | [56,134,230,231] |
|
Leaves | Diabetes, cardiovascular diseases, anemia, rhinitis, arthritis, gout, wounds | Increases insulin sensitivity, improves glucose tolerance | [232,233] |
|
Leaves | Diabetes, gastrointestinal disorders, amoebic dysentery, malaria, helminth infections | Lowers elevated blood glucose levels, inhibits gluconeogenesis and glycogenolysis | [234,235] |
|
Fruit | Diabetes, insomnia, impotence, nervous exhaustion, asthma, liver diseases | Lowers blood glucose levels, improves glucose tolerance | [56,236] |
|
Rhizome | Diabetes, nausea, high cholesterol, heartburn, indigestion, diarrhea, asthma | Lowers fasting blood glucose levels, increases insulin secretion | [119,237] |
6. Phytochemicals and Their Impact on Diabetes
Plants are the primary source of biologically active compounds that may ultimately lead to the discovery and development of potential new drugs [238]. Plants produce both primary and secondary metabolites. Carbohydrates, proteins, and lipids are considered primary metabolites, necessary for the growth and development of plants and involved in essential metabolic pathways, such as photosynthesis and glycolysis. Secondary metabolites are not required for the growth and development of plants; rather, they are responsible for interactions between plant species and the environment and have highly specific functions in plants [239].
Over 13,000 secondary metabolites have been purified and isolated from medicinal plants. These phytochemicals can be categorized into various chemical classes such as alkaloids, flavonoids, terpenoids, phenolics, tannins, saponins, xanthones, and glycosides [78]. Many of these phytochemicals are known to exhibit medicinal properties, including antidiabetic activity [78]. Several phytochemicals isolated from various plant species have been scientifically validated for their contribution to treating and managing diabetes by exerting antihyperglycemic activity and reducing the complications associated with diabetes [171]. For example, the flavonoid rutin, present in the leaves of numerous plants, including Annona squamosa and Azadirachta indica (neem), has been reported to possess many beneficial effects such as anti-inflammatory, anti-cancer, anti-allergic, antiviral, and antioxidative properties [240]. Rutin-containing plants have also been shown to protect against heart disease, hepatotoxicity, and diabetes mellitus [240]. Rutin exerts its antidiabetic effect by lowering plasma glucose, improving the function of pancreatic β-cells, and enhancing glucose tolerance [10]. Two other flavonoids found in the leaves of Annona squamosa, namely quercetin and isoquercetin, have also been reported to possess antihyperglycemic activity by inhibiting α-glucosidase and lowering blood glucose levels [241]. Alongside rutin and quercetin, the tetranortriterpenoid meliacinolin, isolated from the leaves of A. indica, has been found to inhibit α-glucosidase and α-amylase in Type 2 diabetic mice [98]. Nimbidin, extracted from neem seeds, is another phytochemical exhibiting hypoglycemic properties [98]. Quercetin, allicin, allyl-propyl disulfide, cysteine sulfoxide, and S-allyl cysteine sulfoxide from Allium sativum (garlic) have been reported to stimulate insulin secretion from pancreatic β-cells, increase insulin sensitivity to target cells, and prevent insulin activation triggered by the liver [71]. Alliin, from garlic, has been reported to mimic the function of glibenclamide and insulin [71]. Epigallocatechin-3-gallate, epigallocatechin, epicatechin-3-gallate, and epicatechin present in Camellia sinensis (tea) leaves can also lower plasma glucose levels by improving β-cell function, increasing insulin secretion, and enhancing glucose metabolism [117]. These phytomolecules may exert their antidiabetic activity in multiple manners, most commonly by being insulinotropic, insulin-mimetic, and by improving β-cell function, increasing insulin sensitivity, improving glucose tolerance and metabolism, as well as inhibiting various enzyme activities. A summary of antidiabetic medicinal plants and their phytochemicals with potential antidiabetic effects is provided in Table 2. The chemical structures of the antidiabetic phytoconstituents of medicinal plants are given in Table 3.
Table 2.
Phytoconstituents of antidiabetic medicinal plants and their pharmacological effects.
| Medicinal Plants | Parts | Phytoconstituents | Pharmacological Effects | References |
|---|---|---|---|---|
|
Leaves, seeds | Luteolin, lupenone, 24-methylene cycloartenol | Maintains blood glucose levels, promotes insulin secretion, prevents oxidative stress, inhibits inflammation in pancreatic tissues | [16,242,243] |
|
Bark, roots | Quercetin, kaempferol, catechin | Lowers blood glucose levels, increases insulin secretion, reduces insulin resistance, improves glucose tolerance, reduces oxidative stress | [24,244] |
|
Bark | Catechin, epicatechin, catechu tannic acid, gallocatechin, kaempferol | Lowers blood glucose levels, increases plasma insulin levels, reduces insulin resistance, and improves glucose uptake, inhibits α-amylase and α-glucosidase activity | [24,244,245,246,247] |
|
Leaves | Rutin, β-sitosterol, aegelinosides A and B, aegeline, marmelosin | Lowers plasma glucose levels, reduces insulin resistance, decreases glycosylated hemoglobin levels, inhibits α-glucosidase activity, improves β-cell function | [248,249,250,251,252] |
|
Fruit, leaves | 6-paradol, 6-shogaol, 6-gingerol, oleanolic acid | Decreases blood glucose and cholesterol levels, improve glucose tolerance and utilization, inhibits lipid synthesis by adipocytes | [16,253,254,255] |
|
Leaves | Kaempferol, precocene II | Lowers blood glucose levels, increases plasma insulin levels, improves glucose uptake | [16,256] |
|
Bark, pods | Lupeol, oleanolic acid, docosanoic acid, β-sitosterol, catechin, friedelin | Decreases blood glucose and glycosylated hemoglobin levels, reduces nitric oxide, increases insulin levels, activates GLUT2 and GLUT4 | [244,250,255,257,258,259] |
|
Bark, leaves | β-caryophyllene, viridiflorol | Lowers blood glucose levels, increases insulin secretion and sensitivity, reduces glucose absorption, triglyceride, and cholesterol levels | [67,260] |
|
Bulb | Alliin, quercetin, S-methyl cysteine sulfoxide | Reduces fasting glucose levels, increases insulin secretion and sensitivity, decreases triglyceride levels | [16,261,262] |
|
Bulb | Allicin, alliin, diallyl disulfide, quercetin, allyl propyl disulfide | Lowers blood glucose levels, increases insulin secretion and sensitivity, decreases cholesterol and triglyceride levels | [71,261,262,263] |
|
Leaves | Lophenol, aloin, aloetic acid, emodin, glucomannan | Lowers blood glucose levels, increases insulin secretion, improves glucose tolerance, prevents oxidative stress | [16,264,265,266] |
|
Leaves, stem bark | Anacardic acid, lectin | Delays glucose absorption, reduces oxidative stress, inhibits α-glucosidase activity | [16,267] |
|
Rhizome | Mangiferin, neomangiferin, sarsasapogenin | Reduces fasting blood glucose levels, improves glucose tolerance, reduces cholesterol and triglyceride levels, improves diabetic complications | [78,268,269,270] |
|
Leaves, bark | α-copaene, β-caryophyllene, δ-cadinene | Lowers blood glucose levels, increases insulin secretion, improves glucose uptake, reduces glucose absorption, cholesterol, and triglyceride levels | [80,260] |
|
Leaves | Rutin, quercetin, isoquercetin | Lowers blood glucose levels, increases insulin secretion, improves glucose tolerance, reduces glycosylated hemoglobin levels | [10,249,262,271] |
|
Bark | Ellagic acid, β-sitosterol, 3,4,3-tri-O-methylellagic acid | Lowers plasma glucose and glycosylated hemoglobin levels, increases insulin levels, improves β-cell function | [250,272,273] |
|
Seeds | Resveratrol, catechin, rutin, quercetin | Lowers blood glucose levels, increases insulin secretion and glucose uptake, reduces oxidative stress, inhibits α-amylase and α-glucosidase activity | [244,249,262,274] |
|
Rhizome | α and β thujones, thujyl alcohol, azulene, cadinene | Lowers blood glucose levels, activates adenosine monophosphate-activated protein kinase, increases insulin sensitivity | [16,275,276] |
|
Leaves, rhizome | Chrysin, silymarin, isoquercetin | Lowers blood glucose levels, improves β-cell function and glucose tolerance, increases insulin sensitivity, inhibits Pro-inflammatory cytokines | [78,271,277,278] |
|
Roots | Asparagamine, asparagine, kaempferol, quercetin | Lowers blood glucose levels, increases insulin secretion, improves glucose uptake and tolerance | [93,256,262] |
|
Rhizome | Atractans A, B, C, atractylenolide III | Lowers blood glucose levels, decreases insulin resistance | [95,96,279] |
|
Leaves | Azadirachtin, nimbin, rutin, quercetin, campestrol | Lowers blood glucose levels, improves β-cell function, increases insulin secretion, reduces cholesterol and triglyceride levels | [97,98,249,280] |
|
Fruit, seeds | Balantin 1, 2, diosgenin, 3,4,6-tri-O-methyl-D-glucose, triethylphosphine | Increases serum insulin and c-peptide levels, increases glucose metabolism, decreases gluconeogenesis | [16,281] |
|
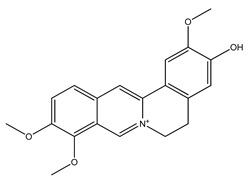
Root bark | Berberine, berbamine | Increases insulin secretion, improves insulin sensitivity, inhibits α-glucosidase and aldose reductase activity | [102,282,283] |
|
Roots | Cytopiloyne, apigenin, luteolin, kaempferol, quercetin | Lowers blood glucose and glycosylated hemoglobin levels, increases insulin expression and secretion from beta cells, stimulates glucose metabolism, increases insulin sensitivity to cells | [16,242,284,285,286] |
|
Flowers, leaves | Pinitol, quercetin, β-sitosterol | Lowers fasting blood glucose and glycosylated hemoglobin levels, increases insulin secretion, improves insulin sensitivity | [16,250,262,287] |
|
Leaves, seeds | Cinnamic acid, kaempferol, aniline | Lowers blood glucose levels, increases insulin secretion and glucose uptake, improves glucose tolerance | [16,256,288] |
|
Leaves, stem bark | Epigallocatechin, epigallocatechin gallate | Lowers blood glucose levels, improves glucose tolerance, enhances insulin secretion, decreases gluconeogenesis | [16,289,290] |
|
Seeds | Linoleic acid, palmitic acid, kaempferol, camphene, linalool | Lowers blood glucose levels, increases insulin levels in blood, improves insulin sensitivity, enhances glucose uptake and tolerance | [256,291,292,293,294] |
|
Leaves | Quercitrin, kaempferol, astragalin, apigenin-7-rhamnoside | Decreases fasting blood glucose levels, increases insulin levels in blood, enhances antioxidant activity, improves glucose uptake, decreases nitric oxide | [16,256,295,296] |
|
Leaves, bark | Caffeic acid, quercetin, esculetin | Lowers blood glucose and glycosylated hemoglobin levels, increases insulin secretion, reduces diabetic oxidative stress, increases GLUT4 expression in adipocytes, improves glucose utilization | [16,262,297,298] |
|
Leaves | Rutin, quercitrin | Lowers blood glucose levels, improves β-cell function, increases insulin secretion, improves glucose tolerance | [117,249,295] |
|
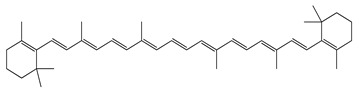
Whole plant | Capsaicin, β-carotene | Lowers blood glucose levels, increases insulin levels, improves glucose tolerance, inhibits pro-inflammatory cytokines | [119,299,300] |
|
Fruit, leaves | Chlorogenic acid, coumarin compounds | Lowers blood glucose levels, stimulates insulin secretion, increases insulin sensitivity, inhibits α-amylase, α-glucosidase, glucose-6-phosphatase, and aldose reductase activity | [16,301,302] |
|
Leaves, seeds | Emodin, kaempferol, β-sitosterol | Lowers blood glucose levels, increases insulin secretion, enhances insulin sensitivity, inhibits phosphoenolpyruvate, carboxykinase, glucose-6-phosphatase activity | [16,250,256,266] |
|
Stalk | Lupeol, kaempferol, catechin, epicatechin | Lowers blood glucose and glycosylated hemoglobin levels, increases insulin levels, reduces nitric oxide, improves glucose tolerance | [244,246,257,303] |
|
Leaves, roots | Gallic acid, chlorogenic acid, vindoline I | Lowers blood glucose levels, stimulates insulin secretion, improves glucose tolerance, decreases pro-inflammatory cytokines | [16,301,304,305] |
|
Root, bark | Isoorientin, stigmast-4-en-3-one, chlorogenic acid, β-sitosterol | Reduces blood glucose levels, improves insulin sensitivity, enhances glucose uptake, decreases cholesterol and triglyceride levels, inhibits glucose-6-phosphatase and hepatic glucose, improves glucose tolerance | [78,306,307] |
|
Bark, leaves | Chlorogenic acid, chicoric acid, gallic acid, kaempferol, quercetin, β-sitosterol | Lowers blood glucose levels, stimulates insulin release, improves insulin sensitivity, inhibits α-amylase, α-glucosidase, glucose-6-phosphatase activity, prevents oxidative stress | [22,78,132,301,308] |
|
Bark | Cinnamaldehyde, eugenol | Decreases blood glucose levels, reduces insulin resistance, inhibits α-glucosidase activity and formation of advanced glycated end products, inhibits sugar binding to albumin | [134,309,310] |
|
Fruit | Diosmin, hesperetin | Lowers blood glucose levels, increases insulin secretion, enhances glucose utilization, stimulates β-endorphine secretion from adrenal glands, inhibits gluconeogenesis | [16,311,312] |
|
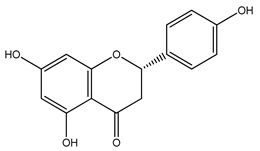
Fruit | Naringin, naringenin, epigallocatechin-3-gallate | Decreases blood glucose levels, increases insulin secretion, improves glucose tolerance, increases GLUT4 translocation in skeletal muscles, decreases gluconeogenesis | [16,289,290,313] |
|
Seeds | D-catechin, L-epicatechin, naringenin, apigenin | Lowers blood glucose levels, increases insulin sensitivity, decreases oxidative stress, inhibits α-amylase and α-glucosidase activity | [16,244,246] |
|
Rhizome | Berberine, jatrorrhizine | Lowers blood glucose levels, enhances aerobic glycolysis, inhibits gluconeogenesis, increases insulin secretion and insulin sensitivity | [33,282,314] |
|
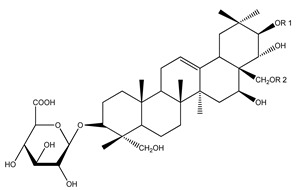
Fruit, seeds | Gymnemagenin, gymnemic acid, ursolic acid | Lowers fasting blood glucose levels, increases insulin secretion, improves glucose uptake and tolerance, inhibits protein glycation | [143,279,315,316] |
|
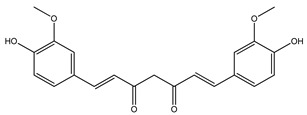
Rhizome | Curcumin, turmerin | Decreases fasting blood glucose, glycosylated hemoglobin, triglyceride, and cholesterol levels, inhibits α-amylase, α-glucosidase activity, and diabetic inflammatory processes | [78,317,318] |
|
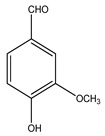
Bark, roots | Kaempferol, vanillin, β-sitosterol | Lowers blood glucose levels, increases insulin levels, decreases serum advanced glycation end products, improves glucose uptake, reduces insulin resistance | [250,256,319,320] |
|
Fruit | Quercetin, kaempferol, gallic acid | Lowers plasma glucose levels, increases insulin secretion, improves glucose tolerance, decreases triglyceride levels | [16,256,262,304] |
|
Bark | Biochanin A, tectorigenin, rhamnoglucoside, dalbergin, dalbergichromene | Lowers blood glucose levels, improves insulin sensitivity and glucose tolerance, reduces insulin resistance | [321,322,323] |
|
Leaves, seeds | Cinchonain-Ib, timosaponin, chlorogenic acid, epicatechin | Lowers blood glucose, total cholesterol, and triglyceride levels, enhances insulin secretion and sensitivity, improves glucose tolerance | [246,279,301,324,325] |
|
Leaves | Betulinic acid, gallic acid, quercitrin, isoquercitrin, rhodomyrtosone E | Lowers blood glucose levels, increases insulin secretion and sensitivity, improves glucose tolerance and antioxidant activity, decreases triglyceride levels, | [155,295,304,326] |
|
Leaves | Eucalyptol, rutin, sesquiterpene | Lowers blood glucose levels, improves β-cell function, increases insulin secretion, reduces oxidative stress | [157,249,327] |
|
Rootbark | Botulin, lupeol, epicatechin | Decreases serum glucose, increases insulin levels, improves insulin sensitivity, decreases glycosylated hemoglobin levels | [78,246,257] |
|
Seeds | Ellagic acid, gallic acid, chlorogenic acid | Lowers blood glucose levels, increases insulin sensitivity, improves β-cell function, improves glucose tolerance, inhibits α-amylase, α-glucosidase, and glucose-6-phosphatase activity | [11,272,301,304] |
|
Leaves | Quercetin, kaempferol, gallic acid | Lowers blood glucose levels, increases insulin secretion, improves glucose tolerance, decreases triglyceride levels, enhances glucose uptake | [162,256,262,304] |
|
Bark, leaves | Rutin, gallic acid, leucopelargonidin-3-O-α-rhamnopyranoside, lupeol, α-amyrin acetate | Decreases blood glucose levels, improve glucose tolerance and β-cell function, increases insulin secretion, | [249,328,329,330] |
|
Seeds | Kolaviron, ascorbic acid | Decreases blood glucose level, stimulates insulin secretion, improves glucose utilization, inhibits glucose-6-phosphatase, exhibits free radical scavenging activity | [16,331,332] |
|
Seeds | Kaempferol, soyasaponin, genistein, β-sitosterol | Lowers blood glucose and glycosylated hemoglobin levels, increases insulin levels in blood, decreases insulin resistance, improves glucose uptake, inhibits glucose absorption | [16,250,256] |
|
Roots | Glycyrrhizin, glycyrrhetinic acid, isoliquiritin | Lowers postprandial rise in blood glucose levels, decreases glycosylated hemoglobin levels | [333,334,335] |
|
Leaves | Gymnemoside A,B,C,D,E,F, quercitol, lupeol, gymnemic acid | Lowers blood glucose and glycosylated hemoglobin levels, increases insulin secretion, inhibits glucose absorption in the small intestine | [149,257,315,336] |
|
Leaves | Harunganin, lupeol, betulinic acid, quercetin, β-sitosterol | Lowers blood glucose and glycosylated hemoglobin levels, increases insulin secretion, decreases insulin resistance, prevents diabetic nephropathy | [16,250,257,262,337,338] |
|
Roots | Gallic acid, vanillin, p-coumaric acid | Lowers blood glucose levels, increases insulin levels in blood, decreases triglyceride levels, reduces serum advanced glycation end products concentration, improves glucose tolerance | [175,304,319,339] |
|
Bark | Stigmasterol, β-sitosterol, epicatechin, procyanidins, proanthocyanidins, quercitrin | Decreases blood glucose and glycosylated hemoglobin levels, increases insulin levels, reduces insulin resistance, improves glucose uptake | [26,176,250,340] |
|
Roots, seeds | Isoquercitrin, quercetin-3-O-gentiobioside | Decreases serum glucose levels, increases insulin secretion, improves glucose tolerance | [16,341] |
|
Leaves | Quercetin, cyanidin, thiamine, ascorbic acid, niacin | Decreases blood glucose concentration, increases insulin synthesis and secretion, reduces oxidative stress, improves endothelial functions, and reduces complications of type 2 diabetes mellitus | [179,262,342,343] |
|
Leaves | Rhoifolin, isoorientin, isoquercitrin | Decreases plasma glucose, cholesterol, and triglyceride levels, stimulates glucose uptake, inhibits DPP-IV activity | [241,306] |
|
Leaves | Lantanoside, ferulic acid, oleanolic acid, caffeic acid | Lowers blood glucose levels, increases insulin secretion, improves glucose utilization, reduces oxidative stress | [255,297,344] |
|
Seeds | Caffeic acid, p-coumaric acid, ferulic acid | Lowers blood glucose and glycosylated hemoglobin levels, increases insulin secretion, reduces diabetic oxidative stress, enhances antioxidant activity | [297,339,344,345] |
|
Leaves, seeds | Mangiferin, gallic acid, kaempferol, curcumin | Lowers fasting blood glucose levels, improves glucose tolerance, increases insulin secretion, reduces triglyceride and cholesterol levels, inhibits oxidative stress and diabetic inflammatory processes | [16,256,269,304,317] |
|
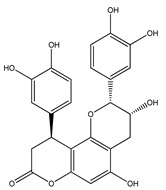
Leaves, seeds | Charantin, vicine, momordicine II, oleanolic acid | Lowers blood glucose levels, stimulates insulin release, inhibits glucose-6-phosphatase and glucose transport in intestines | [22,134,255,336] |
|
Leaves | Quercetin, kaempferol, vanillin, chlorogenic acid | Lowers plasma glucose levels, increases insulin secretion, improves glucose tolerance, decreases the concentration of serum advanced glycation end products | [16,22,189,256,319] |
|
Leaves | Mahanimbine, isomahanine, ascorbic acid, kaempferol, quercetin | Lowers blood glucose levels, reduces triglyceride levels, inhibits α-amylase and α-glucosidase activity, increases insulin secretion, improves glucose tolerance | [78,191,346] |
|
Flowers | Rutin, delphinidin, syringin | Lowers blood glucose levels, increases insulin secretion, reduces reactive oxygen species generation, prevents high glucose-induced cell proliferation | [16,249,347] |
|
Seeds | Thymoquinone, thymol, α-pinene, oleic acid, linoleic acid | Lowers blood glucose, glycosylated hemoglobin, total cholesterol, and triglyceride levels, promotes insulin secretion, reduces insulin resistance, decreases oxidative stress | [291,348,349,350] |
|
Leaves | Linalool, linolen, eugenol, geraniol | Lowers blood glucose levels, improves glucose uptake, inhibits advanced glycation end products generation and α-glucosidase activity | [196,197,310,351] |
|
Leaves | Eugenol, carvacrol, β-sitosterol, linalool | Lowers blood glucose levels, increases insulin secretion, decreases carbohydrate digestion and absorption, inhibits α-glucosidase activity, reduces insulin resistance | [149,248,250,310] |
|
Leaves | Oleuropein, oleanolic acid, luteolin | Maintains blood glucose levels, promotes insulin secretion, improves insulin sensitivity, reduces oxidative stress, inhibits gluconeogenesis | [16,242,255,352] |
|
Roots | Ginsenoside Rb2, Rg2 | Regenerates pancreatic beta cells, increases glucose uptake, reduces insulin resistance, and improves insulin sensitivity | [248,279,353] |
|
Stem bark | Ginsenoside Rb2, protapananadiol/triol | Increases glucose uptake, reduces insulin resistance, and improves insulin sensitivity | [204,353] |
|
Seeds | Hydroxycinnamic acid, rutin, quercetin, orientin, petunidin, catechin | Lowers blood glucose and glycosylated hemoglobin levels, increases insulin secretion, improves glucose tolerance, reduces oxidative stress | [16,149,244,249,262] |
|
Leaves | Oleanolic acid, ursolic acid | Lowers blood glucose levels, increases insulin secretion, improves glucose tolerance, inhibits oxidative stress-induced hepatic insulin resistance, inhibits gluconeogenesis | [16,255,316] |
|
Husk | Kaempferol, catechin, myricetin, pinocembrin | Lowers blood glucose levels, increases insulin secretion, reduces insulin resistance, inhibits α-amylase and α-glucosidase activity | [208,244,256,354] |
|
Bark | Epicatechin, marsupin, carsupin, marsupol | Lowers blood glucose levels, improves insulin sensitivity, enhances insulin release, improves glucose uptake | [149,246] |
|
Flowers | Gallic acid, rutin, nictoflorin | Lowers blood glucose levels, improves β-cell function, increases insulin secretion, improves glucose tolerance, decreases triglyceride levels | [16,249,304] |
|
Roots | Catalpol, rehmannioside | Lowers blood glucose levels, prevents diabetic complications, promotes glucose utilization and glycogen synthesis, reduces oxidative stress | [214,279] |
|
Bark | Spirosantalol, α-santalene, α-santalol, β-santalol, α-bergamotol | Lowers blood glucose and glycosylated hemoglobin levels, decreases total cholesterol and triglyceride levels | [355] |
|
Leaves | Gallic acid, rutin | Decreases plasma glucose and glycosylated hemoglobin levels, improves glucose tolerance, decreases triglyceride levels, inhibits inflammatory cytokines | [249,304,356] |
|
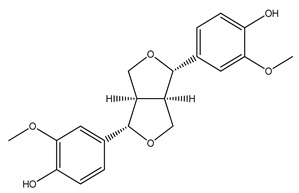
Seeds | Pinoresinol, sesamin, sesaminol | Lowers fasting blood glucose and glycosylated hemoglobin levels, inhibits α-glucosidase activity | [16,357,358] |
|
Leaves | Gallic acid, catechin, epicatechin, rutin, naringenin | Lowers blood glucose levels, improves β-cell function and glucose tolerance, increases insulin secretion, reduces insulin resistance, inhibits α-amylase and α-glucosidase activity | [220,244,246,249,304,313] |
|
Whole plant | p-coumaric acid, catechin, β-carotene | Lowers blood glucose levels, increases insulin levels, reduces insulin resistance, inhibits α-amylase and α-glucosidase activity, reduces oxidative stress and pro-inflammatory biomarkers | [222,244,300,339] |
|
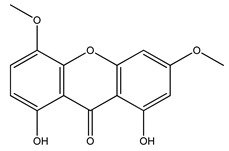
Bark, leaves | Swerchirin, mangiferin, swertiamarin, amarogentin | Lowers blood glucose levels, promotes insulin release, inhibits glucosidase and glucuronidase activity | [30,268,269,336] |
|
Seeds | Apigenin, naringenin, catechin, epictaechin, taxifolin | Lowers blood glucose levels, increases insulin secretion, inhibits α-amylase and α-glucosidase activity, improves glucose tolerance, increases insulin sensitivity | [244,246,313,359] |
|
Bark | Arjungenin, arjunolone, ellagic acid, derivatives of arjunic acid | Lowers blood glucose levels, increases insulin sensitivity, decreases free radical damage | [29,360] |
|
Fruit | Chebulagic acid, gallic acid, ellagic acid, tannic acid | Lowers blood glucose levels, improve glucose tolerance and lipid metabolism, stimulates glucose transport, decreases triglyceride levels | [245,304,360,361,362] |
|
Leaves, roots, stem | Tinosporaside, berberine, syringin | Lowers plasma glucose levels, stimulates insulin synthesis and secretion, decreases triglyceride levels, improves insulin sensitivity, inhibits gluconeogenesis | [149,282,363] |
|
Seeds | Galactomannan, diosgenin, coumarin | Decreases blood glucose levels, stimulates insulin release, inhibits α-glucosidase and aldose reductase activity, increases insulin sensitivity | [16,302,364,365] |
|
Leaves | Quercetin, quercitrin, rutin | Lowers blood glucose and glycosylated hemoglobin levels, increases insulin secretion, reduces insulin resistance, improves antioxidant activity | [16,249,262,295] |
|
Leaves | Sobrerol, vernoamyoside E, luteolin, vitamin E | Lowers blood glucose and glycosylated hemoglobin levels, increases insulin secretion, enhances insulin sensitivity, reduces oxidative stress | [16,235,242,366,367] |
|
Fruit | Withanolides, withacoagulin, withanosides, withaferin A | Lowers blood glucose levels, exhibits free radical scavenging activity, inhibits DPP-IV activity | [368,369] |
|
Rhizome | Gingerol, 6-paradol, 6-shogaol, camphene | Lowers blood glucose levels, increases insulin levels, improves glucose tolerance and utilization, decreases cholesterol levels | [16,253,254,293] |
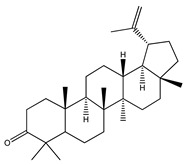
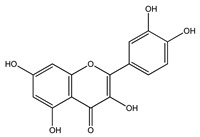
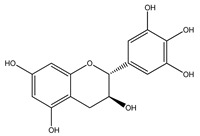
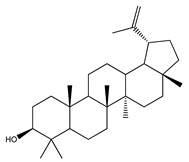
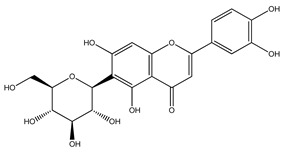
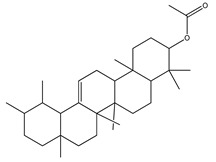
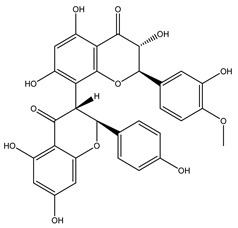
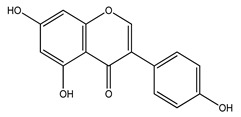
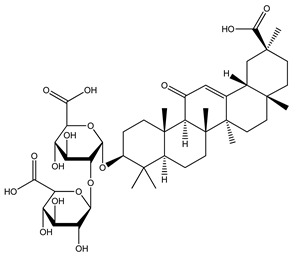
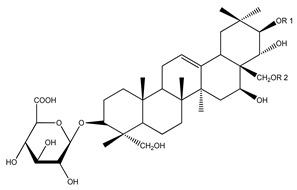
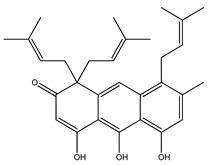
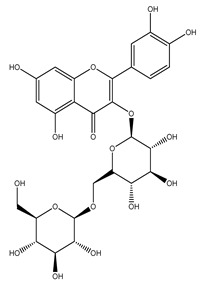
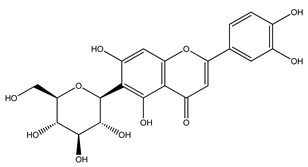
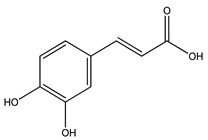
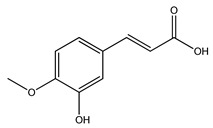
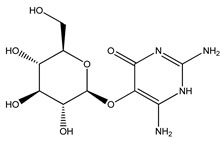
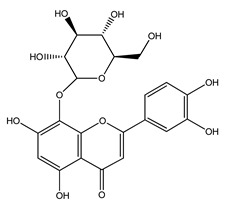
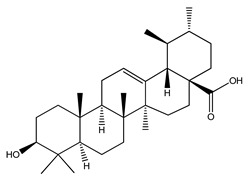
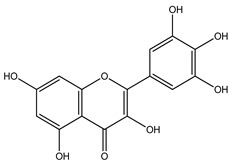
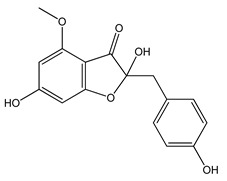
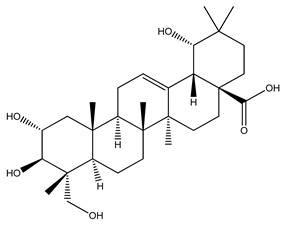
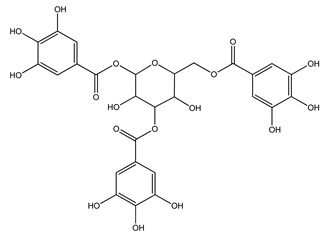
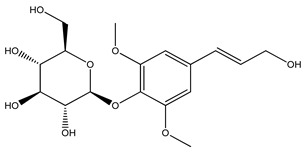
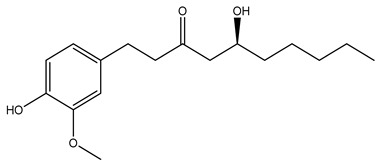
Table 3.
Antidiabetic phytoconstituents of medicinal plants and their chemical structures.
| Medicinal Plants | Phytoconstituents | Chemical Structure |
|---|---|---|
|
Lupenone |
|
|
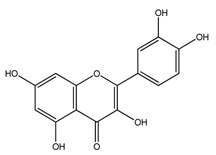
Quercetin |
|
|
Gallocatechin |
|
|
Marmelosin |
|
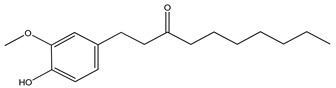
|
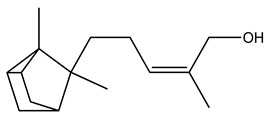
6-paradol |
|
|
Kaempferol |
|
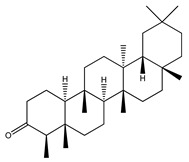
|
Friedelin |
|
|
Viridiflorol |
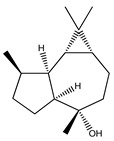
|
|
Alliin |
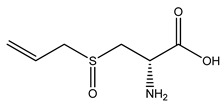
|
|
Allicin |
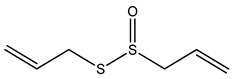
|
|
Aloin |
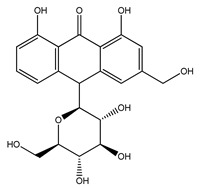
|
|
Anacardic acid |
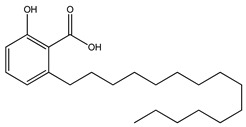
|
|
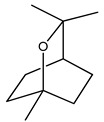
Sarsasapogenin |
|
|
β-caryophyllene |
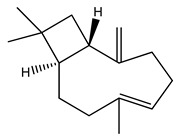
|
|
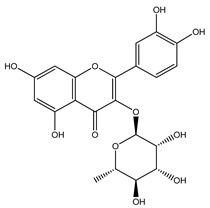
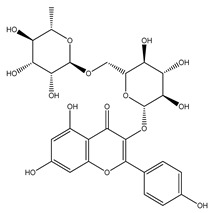
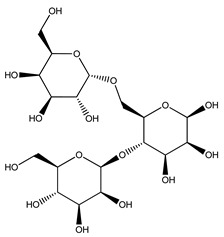
Rutin |
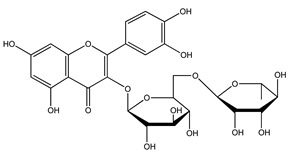
|
|
β-sitosterol |
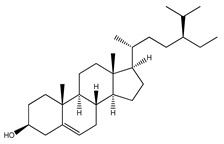
|
|
Resveratrol |
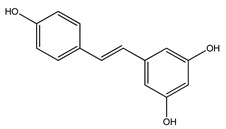
|
|
Azulene |
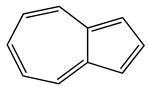
|
|
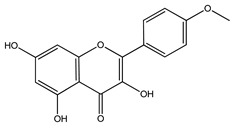
Chrysin |
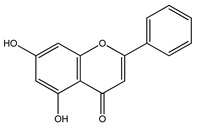
|
|
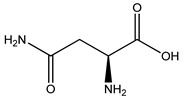
Asparagine |
|
|
Atractylenolide III |
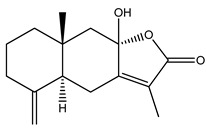
|
|
Nimbin |
|
|
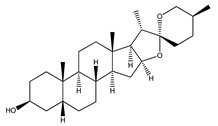
Diosgenin |
|
|
Berberine |
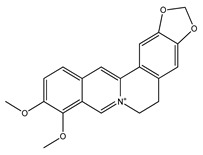
|
|
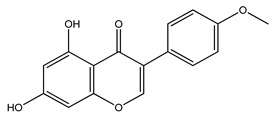
Luteolin |
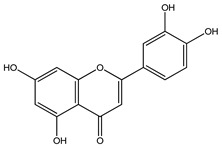
|
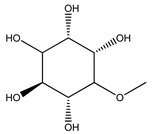
|
Pinitol |
|
|
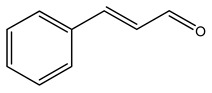
Cinnamic acid |
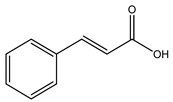
|
|
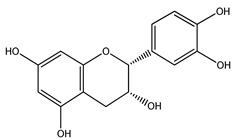
Epigallocatechin gallate |
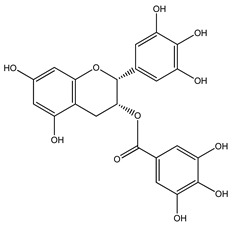
|
|
Palmitic acid |
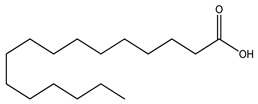
|
|
Astragalin |
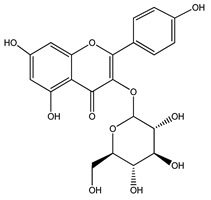
|
|
Esculetin |
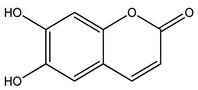
|
|
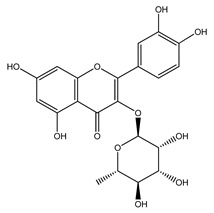
Quercitrin |
|
|
Capsaicin |
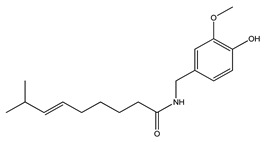
|
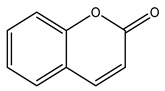
|
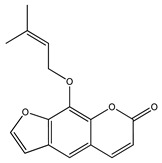
Coumarin |
|
|
Emodin |
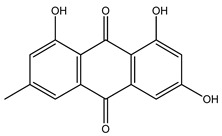
|
|
Lupeol |
|
|
Vindoline |
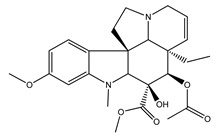
|
|
Isoorientin |
|
|
Chlorogenic acid |
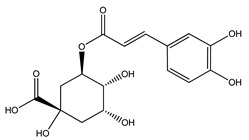
|
|
Cinnamaldehyde |
|
|
Hesperetin |
|
|
Naringin |
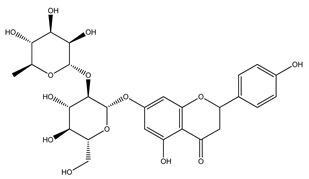
|
|
Apigenin |
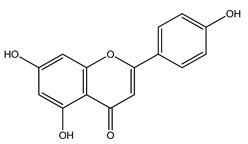
|
|
Jatrorrhizine |
|
|
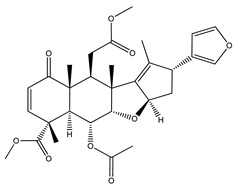
Gymnemic acid |
|
|
Curcumin |
|
|
Vanillin |
|
|
Quercetin |
|
|
Biochanin A |
|
|
Cinchonain ib |
|
|
Rhodomyrtosone E |
|
|
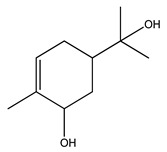
Eucalyptol |
|
|
Epicatechin |
|
|
Ellagic acid |
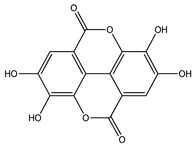
|
|
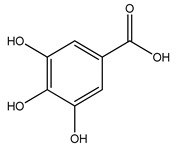
Gallic acid |
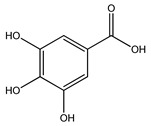
|
|
α-amyrin acetate |
|
|
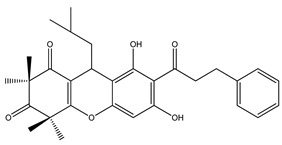
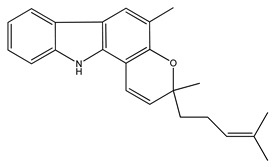
Kolaviron |
|
|
Genistein |
|
|
Glycyrrhizin |
|
|
Gymnemic acid |
|
|
Harunganin |
|
|
p-coumaric acid |
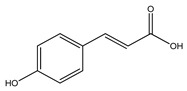
|
|
Stigmasterol |
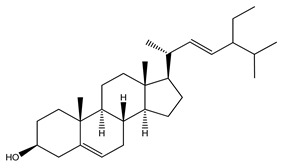
|
|
Quercetin-3-O-gentiobioside |
|
|
Ascorbic acid |
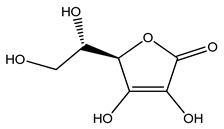
|
|
Isoorientin |
|
|
Caffeic acid |
|
|
Ferulic acid |
|
|
Mangiferin |
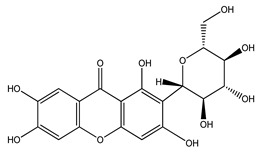
|
|
Vicine |
|
|
Kaempferol |
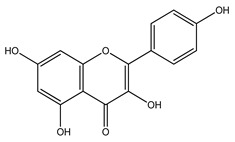
|
|
Mahanimbine |
|
|
Delphinidin |
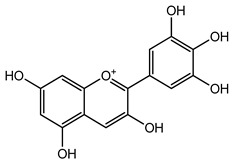
|
|
Thymoquinone |
|
|
Linalool |
|
|
Eugenol |
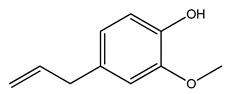
|
|
Oleanolic acid |
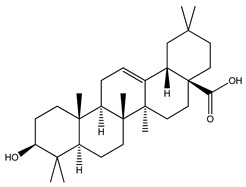
|
|
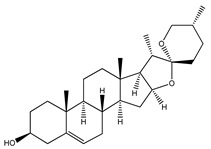
Ginsenoside Rg2 |
|
|
Ginsenoside Rb2 |
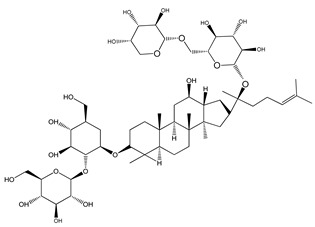
|
|
Orientin |
|
|
Ursolic acid |
|
|
Myricetin |
|
|
Marsupin |
|
|
Nictoflorin |
|
|
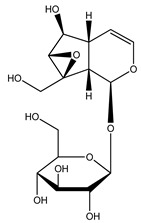
Catalpol |
|
|
β-santalol |
|
|
Gallic acid |
|
|
Pinoresinol |
|
|
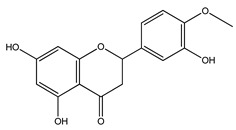
Naringenin |
|
|
β-carotene |
|
|
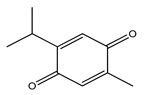
Swerchirin |
|
|
Taxifolin |
|
|
Arjungenin |
|
|
Tannic acid |
|
|
Syringin |
|
|
Galactomannan |
|
|
Quercitrin |
|
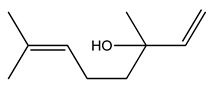
|
Sobrerol |
|
|
Withaferin A |
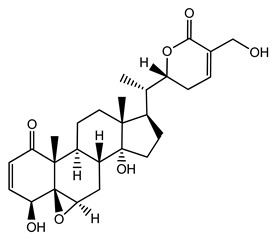
|
|
Gingerol |
|
7. Plant-Based Drug Formulations Available on the Market and Their Role in Diabetes
For the past few decades, there has been an increasingly growing trend in many European countries to develop and sell plant-based medicines [370]. The latter are known as herbal formulations or phytomedicines. These preparations have been standardized and confirmed for their safety profile and effectiveness in the treatment of various diseases. Similar to any other allopathic medicine, herbal formulations can also be prepared as diverse formulations such as tablets, capsules, elixirs, suspensions, solutions, emulsions, and powders [371]. Phytomedicines can either be single herb- or polyherbal formulations [35]. Several phytomedicines have been marketed worldwide for the control and management of diabetes. These include Antibetic, Diabetics, Diabetica, Diabet, Diasol, Diabecon, Diasulin, Dia-Care, Diabecure, Diabeta, Diabeta Plus, Dianex, Diashis, GlucoCare, GlycoNase, Glyoherb, Karmin Plus, SugarMax, and Sugar Loss [35,372]. These products comprise a combination of individual constituents from several antidiabetic plants. Many of these preparations are sold with directions about diet, rest, and physical activities to enhance their effectiveness [35,372].
8. The Future of Plant-Based Antidiabetic Medicines
Nearly 75% of the globally used herbal medicines have been developed based on traditional medicine practitioners [24]. Medicinal plants will continue to be used for their natural safety and potency in many remedies, as well as cosmetics, perfumes, and in the food and beverages industry [373]. Biologically active components derived from traditional medicinal plants have yielded several clinically used drugs and still play a key role in the discovery of new medicines. Thus, it is reasonable to assume that plants used in folk medicine can be used as a potential source for the discovery of new drugs to treat diabetes. The most frequently recommended synthetic drug, metformin, has blood glucose-lowering properties in Type 2 diabetes and the search for many such drugs persists [370]. Moreover, any plant-derived antidiabetic drug with a novel mode of action compared to existing antidiabetic agents has a high potential to be used in clinics [374]. Although the use of plant-based medicines is widespread in developing countries, recently, developed countries have also shown interest in using herbal drugs and therapies. With the rise in the incidence of diabetes mellitus, the demand for plant-based antidiabetic medicines is increasing worldwide. It is expected that countries such as China, India, and Japan, which have an abundance of medicinal plant species and are the greatest exporters of medicinal plants worldwide, will be the most sought [375]. More studies are required regarding the pharmacokinetics/pharmacodynamics of different phytoconstituents in laboratory animals and in clinical use to establish the benefits and mode(s) of action of these compounds in the treatment and management of diabetes. Extensive investigations into the pharmacology, toxicology, metabolism, and tissue distribution of medicinal plants and their phytomolecules are necessary for the development of new potent antidiabetic drugs [376].
9. Conclusions
Diabetes mellitus has risen as a major public health crisis, particularly in underdeveloped countries. Thus, recent research efforts have been centered on the discovery of new natural sources of antidiabetic therapies for the treatment and management of diabetes. As traditional medicinal plants with antidiabetic activity may be considered potential candidates for diabetes management in the long run, they are being extensively researched for novel targets, mechanisms of action, and routes of administration. Plant-based antidiabetic medicines are inexpensive, readily available, and hold low risks of side effects. This makes them promising new antidiabetic agents. With the progression of medicinal plant-based research, scientists and physicians have started to develop newer classes of antidiabetic drugs based on the pharmacology of the phytochemicals isolated from these plants. However, more studies are required for in-depth investigation of these newly discovered antidiabetic drugs at the molecular, therapeutic, and physiological levels in order to control and manage diabetes mellitus worldwide.
Acknowledgments
We would like to extend our appreciation to Peter R Flatt, School of Biomedical Sciences, Ulster University, UK and Independent University, Bangladesh for his aid, guidance, and support in creating the innovative ideas.
Abbreviations
| AMPK | 5′ adenosine monophosphate-activated protein kinase |
| cAMP | cyclic Adenosine monophosphate |
| DPP-IV | Dipeptidyl peptidase-4 |
| G6Pase | Glucose-6-phosphatase |
| GLP-1 | Glucagon-like peptide-1 |
| GLUT-2 | Glucose transporter-2 |
| GLUT-4 | Glucose transporter-4 |
| HbA1c | Hemoglobin A1c |
| IDF | International Diabetes Federation |
| KATP | Adenosine triphosphate-sensitive potassium channel |
| PEPCK | Phosphoenolpyruvate carboxykinase |
| PI3K/AKT | Phosphoinositide 3-kinase/protein kinase B |
| PKA | Protein kinase A |
| PPAR-γ | Peroxisome proliferator-activated receptor-γ |
| SGLT | Sodium–glucose linked transporter |
Author Contributions
Conceptualisation, P.A. and Y.H.A.A.-W.; formal Analysis, P.A. and S.A.; funding acquisition, Y.H.A.A.-W. and J.M.A.H.; investigation, resources, writing, and editing, P.A., S.A., V.S. and N.J.N.; Visualization, P.A. and J.M.A.H.; supervision and reviewing, P.A. and Y.H.A.A.-W. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bastaki S. Diabetes mellitus and its treatment. Int. J. Diabetes Metab. 2005;13:111–134. doi: 10.1159/000497580. [DOI] [Google Scholar]
- 2.Sun H., Saeedi P., Karuranga S., Pinkepank M., Ogurtsova K., Duncan B.B., Stein C., Basit A., Chan J.C., Mbanya J.C. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 2022;183:109119. doi: 10.1016/j.diabres.2021.109119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katsarou A., Gudbjörnsdottir S., Rawshani A., Dabelea D., Bonifacio E., Anderson B.J., Jacobsen L.M., Schatz D.A., Lernmark Å. Type 1 diabetes mellitus. Nat. Rev. Dis. Primers. 2017;3:17016. doi: 10.1038/nrdp.2017.16. [DOI] [PubMed] [Google Scholar]
- 4.Ohlson L.-O., Larsson B., Björntorp P., Eriksson H., Svärdsudd K., Welin L., Tibblin G., Wilhelmsen L. Risk factors for type 2 (non-insulin-dependent) diabetes mellitus. Thirteen and one-half years of follow-up of the participants in a study of Swedish men born in 1913. Diabetologia. 1988;31:798–805. doi: 10.1007/BF00277480. [DOI] [PubMed] [Google Scholar]
- 5.DeFronzo R.A., Ferrannini E., Groop L., Henry R.R., Herman W.H., Holst J.J., Hu F.B., Kahn C.R., Raz I., Shulman G.I. Type 2 diabetes mellitus. Nat. Rev. Dis. Primers. 2015;1:15019. doi: 10.1038/nrdp.2015.19. [DOI] [PubMed] [Google Scholar]
- 6.Hall J.E., Guyton A.C. Guyton and Hall Textbook of Medical Physiology. 13th ed. Elsevier; Philadelphia, PA, USA: 2017. Insulin, Glucagon, and Diabetes Mellitus; pp. 983–999. [Google Scholar]
- 7.Nowakowska M., Zghebi S.S., Ashcroft D.M., Buchan I., Chew-Graham C., Holt T., Mallen C., Van Marwijk H., Peek N., Perera-Salazar R. The comorbidity burden of type 2 diabetes mellitus: Patterns, clusters and predictions from a large English primary care cohort. BMC Med. 2019;17:145. doi: 10.1186/s12916-019-1373-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nathan D.M. Long-term complications of diabetes mellitus. N. Engl. J. Med. 1993;328:1676–1685. doi: 10.1056/NEJM199306103282306. [DOI] [PubMed] [Google Scholar]
- 9.Ansari P., Hannan J.M.A., Azam S., Jakaria M. Challenges in Diabetic Micro-Complication Management: Focus on Diabetic Neuropathy. Int. J. Transl. Med. 2021;1:175–186. doi: 10.3390/ijtm1030013. [DOI] [Google Scholar]
- 10.Ansari P., Flatt P.R., Harriott P., Abdel-Wahab Y.H.A. Evaluation of the antidiabetic and Insulin Releasing Effects of A. squamosa, Including Isolation and Characterization of Active Phytochemicals. Plants. 2020;9:1348. doi: 10.3390/plants9101348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel D., Prasad S.K., Kumar R., Hemalatha S. An overview on antidiabetic medicinal plants having insulin mimetic property. Asian Pac. J. Trop. Biomed. 2012;2:320–330. doi: 10.1016/S2221-1691(12)60032-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaonkar V.P., Hullatti K. Indian Traditional medicinal plants as a source of potent Anti-diabetic agents: A Review. J. Diabetes Metab. Disord. 2020;19:1895–1908. doi: 10.1007/s40200-020-00628-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oh Y.S. Plant-derived compounds targeting pancreatic beta cells for the treatment of diabetes. Evid.-Based Complementary Altern. Med. 2015;2015:629863. doi: 10.1155/2015/629863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jeeva S., Anlin Sheebha Y. A review of antidiabetic potential of ethnomedicinal plants. Med. Aromat. Plants. 2014;3:1–8. [Google Scholar]
- 15.Arumugam G., Manjula P., Paari N. A review: Anti diabetic medicinal plants used for diabetes mellitus. J. Acute Dis. 2013;2:196–200. doi: 10.1016/S2221-6189(13)60126-2. [DOI] [Google Scholar]
- 16.Kasali F.M., Kadima J.N., Peter E.L., Mtewa A.G., Ajayi C.O., Tusiimire J., Tolo C.U., Ogwang P.E., Weisheit A., Agaba A.G. Antidiabetic Medicinal Plants Used in Democratic Republic of Congo: A Critical Review of Ethnopharmacology and Bioactivity Data. Front. Pharmacol. 2021;12:757090. doi: 10.3389/fphar.2021.757090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dar R.A., Shahnawaz M., Qazi P.H. General overview of medicinal plants: A review. J. Phytopharm. 2017;6:349–351. doi: 10.31254/phyto.2017.6608. [DOI] [Google Scholar]
- 18.Moradi B., Abbaszadeh S., Shahsavari S., Alizadeh M., Beyranvand F. The most useful medicinal herbs to treat diabetes. Biomed. Res. Ther. 2018;5:2538–2551. doi: 10.15419/bmrat.v5i8.463. [DOI] [Google Scholar]
- 19.Rizvi S.I., Mishra N. Traditional Indian medicines used for the management of diabetes mellitus. J. Diabetes Res. 2013;2013:712092. doi: 10.1155/2013/712092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oyagbemi A., Salihu M., Oguntibeju O., Esterhuyse A., Farombi E. Antioxidant-Antidiabetic Agents and Human Health. Volume 4. Intech; London, UK: 2014. Some selected medicinal plants with antidiabetic potentials. Antioxidant, Antidiabetic agents and Human Health; pp. 95–113. [Google Scholar]
- 21.Kooti W., Farokhipour M., Asadzadeh Z., Ashtary-Larky D., Asadi-Samani M. The role of medicinal plants in the treatment of diabetes: A systematic review. Electron. Physician. 2016;8:1832–1842. doi: 10.19082/1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alam S., Sarker M.M.R., Sultana T.N., Chowdhury M.N.R., Rashid M.A., Chaity N.I., Zhao C., Xiao J., Hafez E.E., Khan S.A. Antidiabetic Phytochemicals from Medicinal Plants: Prospective Candidates for New Drug Discovery and Development. Front. Endocrinol. 2022;13:800714. doi: 10.3389/fendo.2022.800714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rafe M.R. A review of five traditionally used anti-diabetic plants of Bangladesh and their pharmacological activities. Asian Pac. J. Trop. Med. 2017;10:933–939. doi: 10.1016/j.apjtm.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 24.Ansari P., Flatt P.R., Harriott P., Hannan J.M.A., Abdel-Wahab Y.H.A. Identification of Multiple Pancreatic and Extra-Pancreatic Pathways Underlying the Glucose-Lowering Actions of Acacia arabica Bark in Type-2 Diabetes and Isolation of Active Phytoconstituents. Plants. 2021;10:1190. doi: 10.3390/plants10061190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wanjohi B.K., Sudoi V., Njenga E.W., Kipkore W.K. An ethnobotanical study of traditional knowledge and uses of medicinal wild plants among the Marakwet Community in Kenya. Evid.-Based Complementary Altern. Med. 2020;2020:3208634. doi: 10.1155/2020/3208634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ansari P., Azam S., Seidel V., Abdel-Wahab Y.H.A. In vitro and in vivo antihyperglycemic activity of the ethanol extract of Heritiera fomes bark and characterization of pharmacologically active phytomolecules. J. Pharm. Pharmacol. 2022;74:415–425. doi: 10.1093/jpp/rgac010. [DOI] [PubMed] [Google Scholar]
- 27.Vedavathy S. Scope and importance of traditional medicine. Indian J. Tradit. Knowl. 2003;2:236–239. [Google Scholar]
- 28.Ghosh A. Herbal folk remedies of Bankura and Medinipur districts, West Bengal. Indian J. Tradit. Knowl. 2003;2:393–396. [Google Scholar]
- 29.Morshed M.A., Haque A., Rokeya B., Ali L. Anti-hyperglycemic and lipid lowering effect of Terminalia arjuna Bark extract on Streptozotocin induced Type-2 Diabetic Model Rats. Int. J. Pharm. Pharm. Sci. 2011;3:450–454. [Google Scholar]
- 30.Dey P., Singh J., Suluvoy J.K., Dilip K.J., Nayak J. Utilization of Swertia chirayita Plant Extracts for Management of Diabetes and Associated Disorders: Present Status, Future Prospects and Limitations. Nat. Prod. Bioprospecting. 2020;10:431–443. doi: 10.1007/s13659-020-00277-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vaidya A., Vaidya R.A. Ancient Insights and Modern Discoveries in the Process of Aging-An Overview. Indian J. Med. Sci. 1997;51:349–363. [PubMed] [Google Scholar]
- 32.Soren A.D., Soren P., Jamir W. Traditional Herbal Medicines—How safe are they? In: Sonowal A., editor. PARISAR (The Scope) Purbayon Publication; Assam, India: 2020. pp. 132–138. [Google Scholar]
- 33.Salehi B., Ata A., V Anil Kumar N., Sharopov F., Ramírez-Alarcón K., Ruiz-Ortega A., Abdulmajid Ayatollahi S., Valere Tsouh Fokou P., Kobarfard F., Amiruddin Zakaria Z. Antidiabetic potential of medicinal plants and their active components. Biomolecules. 2019;9:551. doi: 10.3390/biom9100551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coulter-Parkhill A., McClean S., Gault V.A., Irwin N. Therapeutic Potential of Peptides Derived from Animal Venoms: Current Views and Emerging Drugs for Diabetes. Clin. Med. Insights: Endocrinol. Diabetes. 2021;14:117955142110060. doi: 10.1177/11795514211006071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaur M., Valecha V. Diabetes and antidiabetic herbal formulations: An alternative to Allopathy. Eur. J. Med. 2014;6:226–240. doi: 10.13187/ejm.2014.6.226. [DOI] [Google Scholar]
- 36.Vlachogianni T., Loridas S., Fiotakis K., Valavanidis A. From the Traditional Medicine to the Modern Era of Synthetic Pharmaceuticals. Pharmakeftiki. 2014;26:16–30. [Google Scholar]
- 37.Fogelman Y., Kitai E., Blumberg G., Golan-Cohen A., Rapoport M., Carmeli E. Vitamin B12 screening in metformin-treated diabetics in primary care: Were elderly patients less likely to be tested? Aging Clin. Exp. Res. 2017;29:135–139. doi: 10.1007/s40520-016-0546-1. [DOI] [PubMed] [Google Scholar]
- 38.Chaudhury A., Duvoor C., Reddy Dendi V.S., Kraleti S., Chada A., Ravilla R., Marco A., Shekhawat N.S., Montales M.T., Kuriakose K. Clinical review of antidiabetic drugs: Implications for type 2 diabetes mellitus management. Front. Endocrinol. 2017;8:6. doi: 10.3389/fendo.2017.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Balekari U., Veeresham C. Insulinotropic agents from medicinal plants. J. Pharm. Sci. Emerg. Drugs. 2013;1:2. doi: 10.4172/2380-9477.1000101. [DOI] [Google Scholar]
- 40.Walji R., Boon H., Barnes J., Austin Z., Baker G.R., Welsh S. Adverse event reporting for herbal medicines: A result of market forces. Healthc. Policy. 2009;4:77. doi: 10.12927/hcpol.2009.20820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bachtel N., Israni-Winger K. Focus: Plant-based Medicine and Pharmacology: Introduction. Yale J. Biol. Med. 2020;93:227. [Google Scholar]
- 42.Subramoniam A. Present scenario, challenges and future perspectives in plant based medicine development. Ann. Phytomed. 2014;3:31–36. [Google Scholar]
- 43.Gu J., Chen L., Yuan G., Xu X. A drug-target network-based approach to evaluate the efficacy of medicinal plants for type II diabetes mellitus. Evid.-Based Complementary Altern. Med. 2013;2013:203614. doi: 10.1155/2013/203614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Seino S. Cell signalling in insulin secretion: The molecular targets of ATP, cAMP and sulfonylurea. Diabetologia. 2012;55:2096–2108. doi: 10.1007/s00125-012-2562-9. [DOI] [PubMed] [Google Scholar]
- 45.Świderska E., Strycharz J., Wróblewski A., Szemraj J., Drzewoski J., Śliwińska A. Role of PI3K/AKT pathway in insulin-mediated glucose uptake. In: Szablewski L., editor. Blood Glucose Levels. Volume 1. IntechOpen; London, UK: 2018. pp. 1–18. [Google Scholar]
- 46.Dutta D., Kalra S., Sharma M. Adenosine monophosphate-activated protein kinase-based classification of diabetes pharmacotherapy. J. Postgrad. Med. 2017;63:114–121. doi: 10.4103/0022-3859.191007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Habegger K.M., Hoffman N.J., Ridenour C.M., Brozinick J.T., Elmendorf J.S. AMPK enhances insulin-stimulated GLUT4 regulation via lowering membrane cholesterol. Endocrinology. 2012;153:2130–2141. doi: 10.1210/en.2011-2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cai Q., Li B., Yu F., Lu W., Zhang Z., Yin M., Gao H. Investigation of the protective effects of phlorizin on diabetic cardiomyopathy in db/db mice by quantitative proteomics. J. Diabetes Res. 2013;2013:263845. doi: 10.1155/2013/263845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hosseini A., Shafiee-Nick R., Ghorbani A. Pancreatic beta cell protection/regeneration with phytotherapy. Braz. J. Pharm. Sci. 2015;51:1–16. doi: 10.1590/S1984-82502015000100001. [DOI] [Google Scholar]
- 50.Oyedemi S.O., Oyedemi B.O., Ijeh I.I., Ohanyerem P.E., Coopoosamy R.M., Aiyegoro O.A. Alpha-amylase inhibition and antioxidative capacity of some antidiabetic plants used by the traditional healers in Southeastern Nigeria. Sci. World J. 2017;2017:3592491. doi: 10.1155/2017/3592491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ansari P., Flatt P.R., Harriott P., Abdel-Wahab Y.H.A. Insulin secretory and antidiabetic actions of Heritiera fomes bark together with isolation of active phytomolecules. PLoS ONE. 2022;17:e0264632. doi: 10.1371/journal.pone.0264632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kaushal S., Dev D., Prasad D., Sharma R., Hira S. Antidiabetic Potential of Herbal Plants. J. Drug Deliv. Ther. 2019;9:1085–1093. doi: 10.22270/jddt.v9i3-s.2958. [DOI] [Google Scholar]
- 53.Garaniya N., Bapodra A. Ethno botanical and Phytophrmacological potential of Abrus precatorius L.: A review. Asian Pac. J. Trop. Biomed. 2014;4:S27–S34. doi: 10.12980/APJTB.4.2014C1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Boye A., Barku V.Y.A., Acheampong D.O., Ofori E.G. Abrus precatorius Leaf Extract Reverses Alloxan/Nicotinamide-Induced Diabetes Mellitus in Rats through Hormonal (Insulin, GLP-1, and Glucagon) and Enzymatic (α-Amylase/α-Glucosidase) Modulation. BioMed Res. Int. 2021;2021:9920826. doi: 10.1155/2021/9920826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rajvaidhya S., Nagori B., Singh G., Dubey B., Desai P., Jain S. A review on Acacia arabica-an Indian medicinal plant. Int. J. Pharm. Sci. Res. 2012;3:1995–2005. [Google Scholar]
- 56.Ansari P., Hannon-Fletcher M.P., Flatt P.R., Abdel-Wahab Y.H.A. Effects of 22 traditional anti-diabetic medicinal plants on DPP-IV enzyme activity and glucose homeostasis in high-fat fed obese diabetic rats. Biosci. Rep. 2021;41:BSR20203824. doi: 10.1042/BSR20203824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sunil M., Sunitha V., Radhakrishnan E., Jyothis M. Immunomodulatory activities of Acacia catechu, a traditional thirst quencher of South India. J. Ayurveda Integr. Med. 2019;10:185–191. doi: 10.1016/j.jaim.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ikarashi N., Toda T., Okaniwa T., Ito K., Ochiai W., Sugiyama K. Anti-obesity and anti-diabetic effects of acacia polyphenol in obese diabetic KKAy mice fed high-fat diet. Evid.-Based Complementary Altern. Med. 2011;2011:952031. doi: 10.1093/ecam/nep241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ansari P., Afroz N., Jalil S., Azad S.B., Mustakim M.G., Anwar S., Haque S.N., Hossain S.M., Tony R.R., Hannan J.M.A. Anti-hyperglycemic activity of Aegle marmelos (L.) corr. is partly mediated by increased insulin secretion, α-amylase inhibition, and retardation of glucose absorption. J. Pediatric Endocrinol. Metab. 2017;30:37–47. doi: 10.1515/jpem-2016-0160. [DOI] [PubMed] [Google Scholar]
- 60.Sankeshi V., Kumar P.A., Naik R.R., Sridhar G., Kumar M.P., Gopal V.H., Raju T.N. Inhibition of aldose reductase by Aegle marmelos and its protective role in diabetic cataract. J. Ethnopharmacol. 2013;149:215–221. doi: 10.1016/j.jep.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 61.Dzoyem J., McGaw L., Kuete V., Bakowsky U. Anti-inflammatory and anti-nociceptive activities of African medicinal spices and vegetables. In: Kuete V., editor. Medicinal Spices and Vegetables from Africa. 1st ed. Academic Press; Cambridge, MA, USA: 2017. pp. 239–270. [Google Scholar]
- 62.Mohammed A., Gbonjubola V.A., Koorbanally N.A., Islam M.S. Inhibition of key enzymes linked to type 2 diabetes by compounds isolated from Aframomum melegueta fruit. Pharm. Biol. 2017;55:1010–1016. doi: 10.1080/13880209.2017.1286358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ming L.C. Ageratum conyzoides: A tropical source of medicinal and agricultural products. In: Janick J., editor. Perspectives on New Crops and New Uses. ASHS Press; Alexandria, VA, USA: 1999. pp. 469–473. [Google Scholar]
- 64.Agbafor K., Onuohah S., Ominyi M., Orinya O., Ezeani N., Alum E. Antidiabetic, Hypolipidemic and Antiathrogenic Properties of Leaf Extracts of Ageratum conyzoides in Streptozotocin-Induced diabetic rats. Int. J. Curr. Microbiol. Appl. Sci. 2015;4:816–824. [Google Scholar]
- 65.Patel P.A., Parikh M.P., Johari S., Gandhi T.R. Antihyperglycemic activity of Albizzia lebbeck bark extract in streptozotocin-nicotinamide induced type II diabetes mellitus rats. Ayu. 2015;36:335. doi: 10.4103/0974-8520.182752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Verma S., Vashishth E., Singh R., Kumari A., Meena A., Pant P., Bhuyan G., Padhi M. A review on parts of Albizia lebbeck (L.) Benth. used as ayurvedic drugs. Res. J. Pharm. Technol. 2013;6:1307–1313. [Google Scholar]
- 67.Maroyi A. Albizia Adianthifolia: Botany, Medicinal Uses, Phytochemistry, and Pharmacological Properties. Sci. World J. 2018;2018:7463584. doi: 10.1155/2018/7463584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kumar K.S., Debjit B., Pankaj T. Allium cepa: A traditional medicinal herb and its health benefits. J. Chem. Pharm. Res. 2010;2:283–291. [Google Scholar]
- 69.Kianian F., Marefati N., Boskabady M., Ghasemi S.Z., Boskabady M.H. Pharmacological Properties of Allium cepa, Preclinical and Clinical Evidences; A Review. Iran. J. Pharm. Res. 2021;20:107. doi: 10.22037/ijpr.2020.112781.13946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mbaveng A.T. Allium sativum. In: Kuete V., editor. Medicinal Spices and Vegetables from Africa. 1st ed. Academic Press; Cambridge, MA, USA: 2017. pp. 363–377. [Google Scholar]
- 71.El-Saber Batiha G., Magdy Beshbishy A., Wasef L.G., Elewa Y.H., Al-Sagan A.A., El-Hack A., Mohamed E., Taha A.E., Abd-Elhakim Y.M., Prasad Devkota H. Chemical constituents and pharmacological activities of garlic (Allium sativum L.): A review. Nutrients. 2020;12:872. doi: 10.3390/nu12030872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Adams K., Eliot T., Gerald A. Extent of Use of Aloe vera Locally Extracted Products for Management of Ailments in Communities of Kitagata Sub-county in Sheema District, Western Uganda. Int. J. Sci. Basic Appl. Res. 2014;15:1–15. [PMC free article] [PubMed] [Google Scholar]
- 73.Kim K., Kim H., Kwon J., Lee S., Kong H., Im S.-A., Lee Y.-H., Lee Y.-R., Oh S.-T., Jo T.H. Hypoglycemic and hypolipidemic effects of processed Aloe vera gel in a mouse model of non-insulin-dependent diabetes mellitus. Phytomedicine. 2009;16:856–863. doi: 10.1016/j.phymed.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 74.Chan E., Baba S., Chan H.T., Kainuma M., Inoue T., Wong S.K. Ulam herbs: A review on the medicinal properties of Anacardium occidentale and Barringtonia racemosa. J. Appl. Pharm. Sci. 2017;7:241–247. doi: 10.7324/JAPS.2017.70235. [DOI] [Google Scholar]
- 75.Iyare G., Omorodion N., Erameh T., Achukwu P., Ogochukwu A. The effects of Anacardium occidentale leaves extract on histology of selected organs of Wistar rats. MOJ Biol. Med. 2017;2:216–221. [Google Scholar]
- 76.Olatunji L.A., Okwusidi J.I., Soladoye A.O. Antidiabetic effect of Anacardium occidentale. Stem-bark in fructose-diabetic rats. Pharm. Biol. 2005;43:589–593. doi: 10.1080/13880200500301712. [DOI] [Google Scholar]
- 77.Piwowar A., Rembiałkowska N., Rorbach-Dolata A., Garbiec A., Ślusarczyk S., Dobosz A., Długosz A., Marchewka Z., Matkowski A., Saczko J. Anemarrhenae asphodeloides rhizoma Extract Enriched in Mangiferin Protects PC12 Cells against a Neurotoxic Agent-3-Nitropropionic Acid. Int. J. Mol. Sci. 2020;21:2510. doi: 10.3390/ijms21072510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Singh R., Arif T., Khan I., Sharma P. Phytochemicals in antidiabetic drug discovery. J. Biomed. Ther. Sci. 2014;1:1–33. [Google Scholar]
- 79.Costa E.V., Dutra L.M., de Jesus H.C.R., de Lima Nogueira P.C., de Souza Moraes V.R., Salvador M.J., de Holanda Cavalcanti S.C., dos Santos R.L.C., do Nacimento Prata A.P. Chemical composition and antioxidant, antimicrobial, and larvicidal activities of the essential oils of Annona salzmannii and A. pickelii (Annonaceae) Nat. Prod. Commun. 2011;6:908–912. doi: 10.1177/1934578X1100600636. [DOI] [PubMed] [Google Scholar]
- 80.Cascaes M.M., Carneiro O.d.S., Nascimento L.D.d., de Moraes Â.A.B., de Oliveira M.S., Cruz J.N., Guilhon G.M.S.P., Andrade E.H.d.A. Essential Oils from Annonaceae Species from Brazil: A Systematic Review of Their Phytochemistry, and Biological Activities. Int. J. Mol. Sci. 2021;22:12140. doi: 10.3390/ijms222212140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ma C., Chen Y., Chen J., Li X., Chen Y. A review on Annona squamosa L.: Phytochemicals and biological activities. Am. J. Chin. Med. 2017;45:933–964. doi: 10.1142/S0192415X17500501. [DOI] [PubMed] [Google Scholar]
- 82.Patil U., Gaikwad D. Ethno-pharmacological review of a herbal drug: Anogeissus latifolia. Int. J. Pharma Sci. Res. 2011;2:41–43. [Google Scholar]
- 83.Ramachandran S., Naveen K.R., Rajinikanth B., Akbar M., Rajasekaran A. Antidiabetic, antihyperlipidemic and in vivo antioxidant potential of aqueous extract of Anogeissus latifolia bark in type 2 diabetic rats. Asian Pac. J. Trop. Dis. 2012;2:S596–S602. doi: 10.1016/S2222-1808(12)60229-1. [DOI] [Google Scholar]
- 84.Patel J.K., Sharma M.K. Origin, Bioactivities and Therapeutic uses of Arachis hypogaea (Peanut/Fabaceae) Plant Cell Biotechnol. Mol. Biol. 2019;20:1172–1179. [Google Scholar]
- 85.Akter F., Jahan N., Sultana N. Effect of Peanut (Arachis hypogaea L.) on Fasting Blood Glucose and HbA1c in Alloxan Induced Diabetic Male Rats. J. Bangladesh Soc. Physiol. 2014;9:48–53. doi: 10.3329/jbsp.v9i2.22796. [DOI] [Google Scholar]
- 86.Karra G., Nadenla R., Kiran R.S., Srilatha K., Mamatha P., Rao V.U. An overview on Arachis hypogaea plant. Int. J. Pharm. Sci. Res. 2013;4:4508–4518. [Google Scholar]
- 87.Batiha G.E.-S., Olatunde A., El-Mleeh A., Hetta H.F., Al-Rejaie S., Alghamdi S., Zahoor M., Magdy Beshbishy A., Murata T., Zaragoza-Bastida A. Bioactive Compounds, Pharmacological Actions, and Pharmacokinetics of Wormwood (Artemisia absinthium) Antibiotics. 2020;9:353. doi: 10.3390/antibiotics9060353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Daradka H.M., Abas M.M., Mohammad M.A., Jaffar M.M. Antidiabetic effect of Artemisia absinthium extracts on alloxan-induced diabetic rats. Comp. Clin. Pathol. 2014;23:1733–1742. doi: 10.1007/s00580-014-1963-1. [DOI] [Google Scholar]
- 89.Hausner E.A., Poppenga R.H. Small Animal Toxicology. 3rd ed. Elsevier Inc.; Amsterdam, The Netherlands: 2012. Hazards Associated with the Use of Herbal and Other Natural Products; pp. 335–356. [DOI] [Google Scholar]
- 90.Jagtap U., Bapat V. Artocarpus: A review of its traditional uses, phytochemistry and pharmacology. J. Ethnopharmacol. 2010;129:142–166. doi: 10.1016/j.jep.2010.03.031. [DOI] [PubMed] [Google Scholar]
- 91.Hannan J.M.A., Ali L., Khaleque J., Akhter M., Flatt P.R., Abdel-Wahab Y.H.A. Antihyperglycaemic activity of Asparagus racemosus roots is partly mediated by inhibition of carbohydrate digestion and absorption, and enhancement of cellular insulin action. Br. J. Nutr. 2012;107:1316–1323. doi: 10.1017/S0007114511004284. [DOI] [PubMed] [Google Scholar]
- 92.Goyal R., Singh J., Lal H. Asparagus racemosus—An update. Indian J. Med. Sci. 2003;57:408–414. [PubMed] [Google Scholar]
- 93.Marikani K. Antidiabetic and antihyperlipidemic activities of Asparagus racemosus in alloxan induced diabetic rats. J. Pharm. Res. 2012;5:2469–2472. [Google Scholar]
- 94.Hannan J.M.A., Marenah L., Ali L., Rokeya B., Flatt P.R., Abdel-Wahab Y.H.A. Insulin secretory actions of extracts of Asparagus racemosus root in perfused pancreas, isolated islets and clonal pancreatic β-cells. J. Endocrinol. 2007;192:159–168. doi: 10.1677/joe.1.07084. [DOI] [PubMed] [Google Scholar]
- 95.Lee D.H., Han J.M., Yang W.M. The effects of Atractylodes japonica Koidz. on type 2 diabetic rats. J. Korean Med. 2015;36:75–85. doi: 10.13048/jkm.15007. [DOI] [Google Scholar]
- 96.Zhang W.-J., Zhao Z.-Y., Chang L.-K., Cao Y., Wang S., Kang C.-Z., Wang H.-Y., Zhou L., Huang L.-Q., Guo L.-P. Atractylodis Rhizoma: A review of its traditional uses, phytochemistry, pharmacology, toxicology and quality control. J. Ethnopharmacol. 2021;266:113415. doi: 10.1016/j.jep.2020.113415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Alzohairy M.A. Therapeutics role of Azadirachta indica (Neem) and Their Active Constituents in Diseases Prevention and Treatment. Evid.-Based Complementary Altern. Med. 2016;2016:7382506. doi: 10.1155/2016/7382506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yarmohammadi F., Mehri S., Najafi N., Amoli S.S., Hosseinzadeh H. The protective effect of Azadirachta indica (neem) against metabolic syndrome: A review. Iran. J. Basic Med. Sci. 2021;24:280–292. doi: 10.22038/ijbms.2021.48965.11218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chothani D.L., Vaghasiya H. A review on Balanites aegyptiaca Del (desert date): Phytochemical constituents, traditional uses, and pharmacological activity. Pharmacogn. Rev. 2011;5:55. doi: 10.4103/0973-7847.79100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ezzat S.M., Abdel Motaal A., El Awdan S.A.W. In vitro and in vivo antidiabetic potential of extracts and a furostanol saponin from Balanites aegyptiaca. Pharm. Biol. 2017;55:1931–1936. doi: 10.1080/13880209.2017.1343358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rahimi-Madiseh M., Lorigoini Z., Zamani-Gharaghoshi H., Rafieian-Kopaei M. Berberis vulgaris: Specifications and traditional uses. Iran. J. Basic Med. Sci. 2017;20:569. doi: 10.22038/IJBMS.2017.8690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Meliani N., Dib M.E.A., Allali H., Tabti B. Hypoglycaemic effect of Berberis vulgaris L. in normal and streptozotocin-induced diabetic rats. Asian Pac. J. Trop. Biomed. 2011;1:468–471. doi: 10.1016/S2221-1691(11)60102-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Xuan T.D., Khanh T.D. Chemistry and pharmacology of Bidens pilosa: An overview. J. Pharm. Investig. 2016;46:91–132. doi: 10.1007/s40005-016-0231-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yang W.C. Botanical, pharmacological, phytochemical, and toxicological aspects of the antidiabetic plant Bidens pilosa L. Evid.-Based Complementary Altern. Med. 2014;2014:698617. doi: 10.1155/2014/698617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ghogar A., Jiraungkoorskul K., Jiraungkoorskul W. Paper Flower, Bougainvillea spectabilis: Update properties of traditional medicinal plant. J. Nat. Remedies. 2016;16:82–87. doi: 10.18311/jnr/2016/5703. [DOI] [Google Scholar]
- 106.Ghogar A., Jiraungkoorskul W. Antifertility effect of Bougainvillea spectabilis or paper flower. Pharmacogn. Rev. 2017;11:19. doi: 10.4103/phrev.phrev_44_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kumar V., Thakur A.K., Barothia N.D., Chatterjee S.S. Therapeutic potentials of Brassica juncea: An overview. CellMed. 2011;1:2.1–2.16. doi: 10.5667/tang.2011.0005. [DOI] [Google Scholar]
- 108.Mahomoodally M.F., Jugreet S., Sinan K.I., Zengin G., Ak G., Ceylan R., Jekő J., Cziáky Z., Angelini P., Angeles Flores G. Pharmacological Potential and Chemical Characterization of Bridelia ferruginea Benth.—A Native Tropical African Medicinal Plant. Antibiotics. 2021;10:223. doi: 10.3390/antibiotics10020223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Olajide O.A., Aderogba M.A., Okorji U.P., Fiebich B.L. Bridelia ferruginea produces antineuroinflammatory activity through inhibition of nuclear factor-kappa B and p38 MAPK signalling. Evid.-Based Complementary Altern. Med. 2012;2012:546873. doi: 10.1155/2012/546873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Giancarlo S., Rosa L.M., Nadjafi F., Francesco M. Hypoglycaemic activity of two spices extracts: Rhus coriaria L. and Bunium persicum Boiss. Nat. Prod. Res. 2006;20:882–886. doi: 10.1080/14786410500520186. [DOI] [PubMed] [Google Scholar]
- 111.Seri A., Khorsand M., Rezaei Z., Hamedi A., Takhshid M.A. Inhibitory effect of Bunium persicum hydroalcoholic extract on glucose-induced albumin glycation, oxidation, and aggregation in vitro. Iran. J. Med. Sci. 2017;42:369. [PMC free article] [PubMed] [Google Scholar]
- 112.Hussain L., Qadir M.I., ur Rehman S. Antihyperglycemic and hypolipidemic potential of Caesalpinia decapetala in alloxan-induced diabetic rabbits. Bangladesh J. Pharmacol. 2014;9:529–532. doi: 10.3329/bjp.v9i4.19961. [DOI] [Google Scholar]
- 113.Parveen A., Akash M.S.H., Rehman K., Mahmood Q., Qadir M.I. Analgesic, anti-inflammatory and anti-pyretic activities of Caesalpinia decapetala. Bioimpacts. 2014;4:43. doi: 10.5681/bi.2014.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Arora D., Rani A., Sharma A. A review on phytochemistry and ethnopharmacological aspects of genus Calendula. Pharmacogn. Rev. 2013;7:179. doi: 10.4103/0973-7847.120520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Athaiban M.A. Effect of Calendula officinalis Extract against Streptozotocin Induced Diabetes in Male Rats. Int. J. Pharm. Phytopharm. Res. 2018;8:22–28. [Google Scholar]
- 116.Chopade V., Phatak A., Upaganlawar A., Tankar A. Green tea (Camellia sinensis): Chemistry, Traditional, Medicinal uses and its Pharmacological activities-a review. Pharmacogn. Rev. 2008;2:157–162. [Google Scholar]
- 117.Ansari P., Flatt P.R., Harriott P., Abdel-Wahab Y.H.A. Anti-hyperglycaemic and insulin-releasing effects of Camellia sinensis leaves and isolation and characterisation of active compounds. Br. J. Nutr. 2021;126:1149–1163. doi: 10.1017/S0007114520005085. [DOI] [PubMed] [Google Scholar]
- 118.Batiha G.E.-S., Alqahtani A., Ojo O.A., Shaheen H.M., Wasef L., Elzeiny M., Ismail M., Shalaby M., Murata T., Zaragoza-Bastida A. Biological Properties, Bioactive Constituents, and Pharmacokinetics of Some Capsicum spp. and Capsaicinoids. Int. J. Mol. Sci. 2020;21:5179. doi: 10.3390/ijms21155179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Manukumar H., Shiva Kumar J., Chandrasekhar B., Raghava S., Umesha S. Evidences for diabetes and insulin mimetic activity of medicinal plants: Present status and future prospects. Crit. Rev. Food Sci. Nutr. 2017;57:2712–2729. doi: 10.1080/10408398.2016.1143446. [DOI] [PubMed] [Google Scholar]
- 120.Aravind G., Bhowmik D., Duraivel S., Harish G. Traditional and medicinal uses of Carica papaya. J. Med. Plants Stud. 2013;1:7–15. [Google Scholar]
- 121.Solikhah T.I., Setiawan B., Ismukada D.R. Antidiabetic activity of papaya leaf extract (Carica Papaya L.) isolated with maceration method in alloxan-induces diabetic mice. Syst. Rev. Pharm. 2020;11:774–778. doi: 10.31838/srp.2020.9.109. [DOI] [Google Scholar]
- 122.Varghese G.K., Bose L.V., Habtemariam S. Antidiabetic components of Cassia alata leaves: Identification through α-glucosidase inhibition studies. Pharm. Biol. 2013;51:345–349. doi: 10.3109/13880209.2012.729066. [DOI] [PubMed] [Google Scholar]
- 123.Fatmawati S., Purnomo A.S., Bakar M.F.A. Chemical constituents, usage and pharmacological activity of Cassia alata. Heliyon. 2020;6:e04396. doi: 10.1016/j.heliyon.2020.e04396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Mwangi R.W., Macharia J.M., Wagara I.N., Bence R.L. The medicinal properties of Cassia fistula L.: A review. Biomed. Pharmacother. 2021;144:112240. doi: 10.1016/j.biopha.2021.112240. [DOI] [PubMed] [Google Scholar]
- 125.Danish M., Singh P., Mishra G., Srivastava S., Jha K., Khosa R. Cassia fistula Linn. (Amulthus)—An important medicinal plant: A review of its traditional uses, phytochemistry and pharmacological properties. J. Nat. Prod. Plant Resourse. 2011;1:101–118. [Google Scholar]
- 126.Einstein J.W., Mohd Rais M., Mohd M.A. Comparative evaluation of the antidiabetic effects of different parts of Cassia fistula Linn, a Southeast Asian Plant. J. Chem. 2013;2013:714063. doi: 10.1155/2013/714063. [DOI] [Google Scholar]
- 127.Jarald E., Joshi S., Jain D., Edwin S. Biochemical evaluation of the hypoglycemic effects of extract and fraction of Cassia fistula Linn. in alloxan-induced diabetic rats. Indian J. Pharm. Sci. 2013;75:427. doi: 10.4103/0250-474X.119823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kumar S., Singh B., Singh R. Catharanthus roseus (L.) G. Don: A review of its ethnobotany, phytochemistry, ethnopharmacology and toxicities. J. Ethnopharmacol. 2022;284:114647. doi: 10.1016/j.jep.2021.114647. [DOI] [PubMed] [Google Scholar]
- 129.Tiong S.H., Looi C.Y., Hazni H., Arya A., Paydar M., Wong W.F., Cheah S.C., Mustafa M.R., Awang K. Antidiabetic and Antioxidant Properties of Alkaloids from Catharanthus roseus (L.) G. Don. Molecules. 2013;18:9770–9784. doi: 10.3390/molecules18089770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ahmed M.F., Kazim S.M., Ghori S.S., Mehjabeen S.S., Ahmed S.R., Ali S.M., Ibrahim M. Antidiabetic activity of Vinca rosea extracts in alloxan-induced diabetic rats. Int. J. Endocrinol. 2010;2010:841090. doi: 10.1155/2010/841090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Rivera-Mondragón A., Ortíz O.O., Bijttebier S., Vlietinck A., Apers S., Pieters L., Caballero-George C. Selection of chemical markers for the quality control of medicinal plants of the genus Cecropia. Pharm. Biol. 2017;55:1500–1512. doi: 10.1080/13880209.2017.1307421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Street R.A., Sidana J., Prinsloo G. Cichorium intybus: Traditional Uses, Phytochemistry, Pharmacology, and Toxicology. Evid.-Based Complementary Altern. Med. 2013;2013:579319. doi: 10.1155/2013/579319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wang J., Su B., Jiang H., Cui N., Yu Z., Yang Y., Sun Y. Traditional uses, phytochemistry and pharmacological activities of the genus Cinnamomum (Lauraceae): A review. Fitoterapia. 2020;146:104675. doi: 10.1016/j.fitote.2020.104675. [DOI] [PubMed] [Google Scholar]
- 134.Ota A., Ulrih N.P. An overview of herbal products and secondary metabolites used for management of type two diabetes. Front. Pharmacol. 2017;8:436. doi: 10.3389/fphar.2017.00436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Basli A., Younici S., Benkerrou Z., Khettal B., Madani K. Evaluation of in-vitro antidiabetic and hypolipidaemic activities of extracts citrus lemon fruit. J. Environ. Sci. Eng. A. 2016;5:612–618. doi: 10.17265/2162-5298/2016.12.003. [DOI] [Google Scholar]
- 136.Klimek-Szczykutowicz M., Szopa A., Ekiert H. Citrus limon (Lemon) Phenomenon—A Review of the Chemistry, Pharmacological Properties, Applications in the Modern Pharmaceutical, Food, and Cosmetics Industries, and Biotechnological Studies. Plants. 2020;9:119. doi: 10.3390/plants9010119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Sharma M., Fernandes J., Ahirwar D., Jain R. Hypoglycemic and hypolipidimic activity of alcoholic extract of citrus aurantium in normal and alloxan-induced diabetic rats. Pharmacologyonline. 2008;3:161–171. [Google Scholar]
- 138.Suryawanshi J.A.S. An overview of Citrus aurantium used in treatment of various diseases. Afr. J. Plant Sci. 2011;5:390–395. doi: 10.5897/AJPS.9000015. [DOI] [Google Scholar]
- 139.Erukainure O.L., Sanni O., Ijomone O.M., Ibeji C.U., Chukwuma C.I., Islam M.S. The antidiabetic properties of the hot water extract of kola nut (Cola nitida (Vent.) Schott & Endl.) in type 2 diabetic rats. J. Ethnopharmacol. 2019;242:112033. doi: 10.1016/j.jep.2019.112033. [DOI] [PubMed] [Google Scholar]
- 140.Adeosun O.I., Olaniyi K.S., Amusa O.A., Jimoh G.Z., Oniyide A.A. Methanolic extract of Cola nitida elicits dose-dependent diuretic, natriuretic and kaliuretic activities without causing electrolyte impairment, hepatotoxicity and nephrotoxicity in rats. Int. J. Physiol. Pathophysiol. Pharmacol. 2017;9:231. [PMC free article] [PubMed] [Google Scholar]
- 141.Zhen Z., Chang B., Li M., Lian F.-M., Chen L., Dong L., Wang J., Yu B., Liu W.K., Li X.Y. Anti-Diabetic Effects of a Coptis chinensis Containing New Traditional Chinese Medicine Formula in Type 2 Diabetic Rats. Am. J. Chin. Med. 2011;39:53–63. doi: 10.1142/S0192415X11008646. [DOI] [PubMed] [Google Scholar]
- 142.Friedemann T., Ying Y., Wang W., Kramer E.R., Schumacher U., Fei J., Schröder S. Neuroprotective Effect of Coptis chinensis in MPP+ and MPTP-Induced Parkinson’s Disease Models. Am. J. Chin. Med. 2016;44:907–925. doi: 10.1142/S0192415X16500506. [DOI] [PubMed] [Google Scholar]
- 143.He K., Song S., Zou Z., Feng M., Wang D., Wang Y., Li X., Ye X. The Hypoglycemic and Synergistic Effect of Loganin, Morroniside, and Ursolic Acid Isolated from the Fruits of Cornus officinalis. Phytother. Res. 2016;30:283–291. doi: 10.1002/ptr.5529. [DOI] [PubMed] [Google Scholar]
- 144.Kim J.S. Seeds of Cornus officinalis and Diabetic Cataracts. In: Preedy V.R., editor. Handbook of Nutrition, Diet and the Eye. 1st ed. Academic Press; Cambridge, MA, USA: 2014. pp. 451–458. [DOI] [Google Scholar]
- 145.Tung B.T., Nham D.T., Hai N.T., Thu D.K. Curcuma longa, the Polyphenolic Curcumin Compound and Pharmacological Effects on Liver. In: Watson R.R., Preedy V.R., editors. Dietary Interventions in Liver Disease. Academic Press; Cambridge, MA, USA: 2019. pp. 125–134. [DOI] [Google Scholar]
- 146.Olatunde A., Joel E., Tijjani H., Obidola S., Luka C. Anti-diabetic activity of aqueous extract of Curcuma longa (Linn) rhizome in normal and alloxan-induced diabetic rats. Researcher. 2014;6:58–65. [Google Scholar]
- 147.Fukai T., Oku Y., Hou A.J., Yonekawa M., Terada S. Antimicrobial activity of Hydrophobic Xanthones from Cudrania cochinchinensis against Bacillus subtilis and Methicillin-Resistant Staphylococcus aureus. Chem. Biodivers. 2004;1:1385–1390. doi: 10.1002/cbdv.200490101. [DOI] [PubMed] [Google Scholar]
- 148.Antu K.A., Riya M.P., Mishra A., Anilkumar K.S., Chandrakanth C.K., Tamrakar A.K., Srivastava A.K., Raghu K.G. Antidiabetic property of Symplocos cochinchinensis is mediated by inhibition of alpha glucosidase and enhanced insulin sensitivity. PLoS ONE. 2014;9:e105829. doi: 10.1371/journal.pone.0105829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Tran N., Pham B., Le L. Bioactive Compounds in Anti-Diabetic Plants: From Herbal Medicine to Modern Drug Discovery. Biology. 2020;9:252. doi: 10.3390/biology9090252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Singh S., Bhagwati D. Cyamopsis tetragonoloba (L). Taub.: A Phyto-Pharmacological Review. Int. J. Pharm. Pharm. Res. 2016;7:166–174. [Google Scholar]
- 151.Shah M.H., Mukhtar I., Khan S.N. Medicinal importance and association of pathological constraints with Dalbergia sissoo. Pak. J. Phytopathol. 2010;22:135–138. [Google Scholar]
- 152.Sehra S., Sharma J. Pharmacological Effects and Medicinal Importance of Dalbergia sissoo—A Review. Int. J. Pharm. Chem. Biol. Sci. 2018;8:234–243. [Google Scholar]
- 153.Tanaka K., Nishizono S., Makino N., Tamaru S., Terai O., Ikeda I. Hypoglycemic Activity of Eriobotrya japonica Seeds in Type 2 Diabetic Rats and Mice. Biosci. Biotechnol. Biochem. 2008;72:686–693. doi: 10.1271/bbb.70411. [DOI] [PubMed] [Google Scholar]
- 154.Baljinder S., Seena G., Dharmendra K., Vikas G., Bansal P. Pharmacological potential of Eriobotrya japonica—An overview. Int. Res. J. Pharm. 2010;1:95–99. [Google Scholar]
- 155.Ansari P., Flatt P.R., Harriott P., Abdel-Wahab Y.H.A. Insulinotropic and antidiabetic properties of Eucalyptus citriodora leaves and isolation of bioactive phytomolecules. J. Pharm. Pharmacol. 2021;23:1049–1061. doi: 10.1093/jpp/rgab030. [DOI] [PubMed] [Google Scholar]
- 156.Saba I., Iqbal M., Iqbal M. Bioactivity of Eucalyptus citriodora leaves essential oil. J. Agrochim. 2013;57:128. [Google Scholar]
- 157.Gray A.M., Flatt P.R. Antihyperglycemic actions of Eucalyptus globulus (Eucalyptus) are associated with pancreatic and extra-pancreatic effects in mice. J. Nutr. 1998;128:2319–2323. doi: 10.1093/jn/128.12.2319. [DOI] [PubMed] [Google Scholar]
- 158.Hayat U., Jilani M.I., Rehman R., Nadeem F. A Review on Eucalyptus globulus: A new perspective in therapeutics. Int. J. Chem. Biochem. Sci. 2015;8:85–91. [Google Scholar]
- 159.Maroyi A. Euclea undulata Thunb.: Review of its botany, ethnomedicinal uses, phytochemistry and biological activities. Asian Pac. J. Trop. Med. 2017;10:1030–1036. doi: 10.1016/j.apjtm.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 160.Jana K., Bera T.K., Ghosh D. Antidiabetic effects of Eugenia jambolana in the streptozotocin-induced diabetic male albino rat. Biomark. Genom. Med. 2015;7:116–124. doi: 10.1016/j.bgm.2015.08.001. [DOI] [Google Scholar]
- 161.Khalique A., Rauf A. An overview of Jamun (Eugenia Jambolana Linn): A traditional multipotential drug. Indian J. Unani Med. 2016;9:71–75. [Google Scholar]
- 162.Ghosh P., Ghosh C., Das S., Das C., Mandal S., Chatterjee S. Botanical Description, Phytochemical Constituents and Pharmacological Properties of Euphorbia hirta Linn.: A review. Int. J. Health Sci. Res. 2019;9:273–286. [Google Scholar]
- 163.Kumar S., Malhotra R., Kumar D. Euphorbia hirta: Its Chemistry, Traditional and Medicinal Uses, and Pharmacological Activities. Pharmacogn. Rev. 2010;4:58. doi: 10.4103/0973-7847.65327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Rizvi S.I., Matteucci E., Atukeren P. Traditional Medicine in Management of Type 2 Diabetes Mellitus. J. Diabetes Res. 2013;2013:580823. doi: 10.1155/2013/580823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Patel R., Gautam P. Medicinal Potency of Ficus Bengalensis: A Review. Int. J. Med. Chem. Anal. 2014;4:53–58. [Google Scholar]
- 166.Adaramoye O. Antidiabetic effect of kolaviron, a biflavonoid complex isolated from Garcinia kola seeds, in Wistar rats. Afr. Health Sci. 2012;12:498–506. doi: 10.4314/ahs.v12i4.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Emmanuel O., Uche M.E., Dike E.D., Etumnu L.R., Ugbogu O.C., Ugbogu E.A. A review on Garcinia kola Heckel: Traditional uses, phytochemistry, pharmacological activities, and toxicology. Biomarkers. 2021;27:101–117. doi: 10.1080/1354750X.2021.2016974. [DOI] [PubMed] [Google Scholar]
- 168.Mahmoud M.H., Taha M.M., Shahy E.M. Germination of Glycine max seeds potentiates its antidiabetic effect in streptozotocin induced diabetic rats. Int. J. Pharm. Clin. Res. 2016;8:1429–1437. [Google Scholar]
- 169.Lee K.J., Baek D.-Y., Lee G.-A., Cho G.-T., So Y.-S., Lee J.-R., Ma K.-H., Chung J.-W., Hyun D.Y. Phytochemicals and Antioxidant Activity of Korean Black Soybean (Glycine max L.) Landraces. Antioxidants. 2020;9:213. doi: 10.3390/antiox9030213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Batiha G.E.S., Beshbishy A.M., El-Mleeh A., Abdel-Daim M.M., Devkota H.P. Traditional Uses, Bioactive Chemical Constituents, and Pharmacological and Toxicological Activities of Glycyrrhiza glabra L. (Fabaceae) Biomolecules. 2020;10:352. doi: 10.3390/biom10030352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Khan F., Sarker M., Rahman M., Ming L.C., Mohamed I.N., Zhao C., Sheikh B.Y., Tsong H.F., Rashid M.A. Comprehensive review on phytochemicals, pharmacological and clinical potentials of Gymnema sylvestre. Front. Pharmacol. 2019;10:1223. doi: 10.3389/fphar.2019.01223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Kanetkar P., Singhal R., Kamat M. Gymnema sylvestre: A Memoir. J. Clin. Biochem. Nutr. 2007;41:77–81. doi: 10.3164/jcbn.2007010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kadima J., Kasali F., Bavhure B., Mahano A., Bwironde F. Comparative Antidiabetic Potential and Survival Function of Harungana madagascariensis, Physalis peruviana, Solanum americanum and Tithonia diversifolia Extracts on Alloxan-Induced Diabetes in Guinea-Pigs. Int. J. Pharm. Pharm. Res. 2016;5:196–206. [Google Scholar]
- 174.Suthar M., Rathore G., Pareek A. Antioxidant and Antidiabetic Activity of Helicteres isora (L.) Fruits. Indian J. Pharm. Sci. 2009;71:695. doi: 10.4103/0250-474X.59557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kumar N., Singh A.K. Plant profile, phytochemistry and pharmacology of Avartani (Helicteres isora Linn.): A review. Asian Pac. J. Trop. Biomed. 2014;4:S22–S26. doi: 10.12980/APJTB.4.2014C872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Mahmud I., Islam M.K., Saha S., Barman A.K., Rahman M.M., Anisuzzman M., Rahman T., Al-Nahain A., Jahan R., Rahmatullah M. Pharmacological and Ethnomedicinal Overview of Heritiera fomes: Future Prospects. Int. Sch. Res. Not. 2014;2014:938543. doi: 10.1155/2014/938543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Sabitha V., Ramachandran S., Naveen K., Panneerselvam K. Antidiabetic and antihyperlipidemic potential of Abelmoschus esculentus (L.) Moench. in streptozotocin-induced diabetic rats. J. Pharm. Bioallied Sci. 2011;3:397. doi: 10.4103/0975-7406.84447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Chanchal D.K., Alok S., Kumar M., Bijauliya R.K., Rashi S., Gupta S. A Brief Review on Abelmoschus esculentus Linn. Okra. Int. J. Pharm. Sci. Res. 2018;9:58–66. doi: 10.13040/IJPSR.0975-8232.9(1).58-66. [DOI] [Google Scholar]
- 179.Ansari P., Azam S., Hannan J.M.A., Flatt P.R., Wahab Y.H.A. Anti-hyperglycaemic activity of H. rosa-sinensis leaves is partly mediated by inhibition of carbohydrate digestion and absorption, and enhancement of insulin secretion. J. Ethnopharmacol. 2020;253:112647. doi: 10.1016/j.jep.2020.112647. [DOI] [PubMed] [Google Scholar]
- 180.Jadhav V., Thorat R., Kadam V., Sathe N. Traditional medicinal uses of Hibiscus rosa-sinensis. J. Pharm. Res. 2009;2:1220–1222. [Google Scholar]
- 181.Kumar J., Singh S.P., Choudhary G.K. Pharmacological evaluation of leaves of Jatropha curcas L. for anti-diabetic activity in alloxan induced diabetic rats. Indian J. Anim. Sci. 2016;86:387–391. [Google Scholar]
- 182.Pabón L.C., Hernández-Rodríguez P. Chemical importance of Jatropha curcas and its biological, pharmacological and industrial applications. Rev. Cuba. De Plantas Med. 2012;17:194–209. [Google Scholar]
- 183.Sen S., Chakraborty R. Pharmacognostic and anti-hyperglycemic evaluation of Lantana camara (L.) var. aculeate leaves in alloxan-induced hyperglycemic rats. Int. J. Res. Pharm. Sci. 2010;1:247–252. [Google Scholar]
- 184.Kirimuhuzya C., Waako P., Joloba M., Odyek O. The anti-mycobacterial activity of Lantana camara a plant traditionally used to treat symptoms of tuberculosis in South-western Uganda. Afr. Health Sci. 2009;9:40–45. [PMC free article] [PubMed] [Google Scholar]
- 185.Palla A.H., Khan N.A., Bashir S., Iqbal J., Gilani A.H. Pharmacological basis for the medicinal use of Linum usitatissimum (Flaxseed) in infectious and non-infectious diarrhea. J. Ethnopharmacol. 2015;160:61–68. doi: 10.1016/j.jep.2014.11.030. [DOI] [PubMed] [Google Scholar]
- 186.Saleem M., Tanvir M., Akhtar M.F., Iqbal M., Saleem A. Antidiabetic Potential of Mangifera indica L. cv. Anwar Ratol Leaves: Medicinal Application of Food Wastes. Medicina. 2019;55:353. doi: 10.3390/medicina55070353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Shah K., Patel M., Patel R., Parmar P. Mangifera indica (mango) Pharmacogn. Rev. 2010;4:42. doi: 10.4103/0973-7847.65325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Bortolotti M., Mercatelli D., Polito L. Momordica charantia, a nutraceutical approach for inflammatory related diseases. Front. Pharmacol. 2019;10:486. doi: 10.3389/fphar.2019.00486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Azad S.B., Ansari P., Azam S., Hossain S.M., Shahid M.I.-B., Hasan M., Hannan J.M.A. Anti-hyperglycaemic activity of Moringa oleifera is partly mediated by carbohydrase inhibition and glucose-fibre binding. Biosci. Rep. 2017;3:BSR20170059. doi: 10.1042/BSR20170059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Mishra G., Singh P., Verma R., Kumar S., Srivastav S., Jha K., Khosa R. Traditional uses, phytochemistry and pharmacological properties of Moringa oleifera plant: An overview. Der Pharm. Lett. 2011;3:141–164. [Google Scholar]
- 191.Balakrishnan R., Vijayraja D., Jo S.-H., Ganesan P., Su-Kim I., Choi D.-K. Medicinal Profile, Phytochemistry, and Pharmacological Activities of Murraya koenigii and its Primary Bioactive Compounds. Antioxidants. 2020;9:101. doi: 10.3390/antiox9020101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Murthy S.S.N., Felicia C. Antidiabetic activity of Musa sapientum fruit peel extract on streptozotocin induced diabetic rats. Int. J. Pharma Bio Sci. 2015;6:537–543. [Google Scholar]
- 193.Imam M.Z., Akter S. Musa paradisiaca L. and Musa sapientum L.: A Phytochemical and Pharmacological Review. J. Appl. Pharm. Sci. 2011;1:14–20. [Google Scholar]
- 194.Hannan J.M.A., Ansari P., Haque A., Sanju A., Huzaifa A., Rahman A., Ghosh A., Azam S. Nigella sativa stimulates insulin secretion from isolated rat islets and inhibits the digestion and absorption of (CH2O) n in the gut. Biosci. Rep. 2019;39:BSR20190723. doi: 10.1042/BSR20190723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Salehi B., Quispe C., Imran M., Ul-Haq I., Živković J., Abu-Reidah I.M., Sen S., Taheri Y., Acharya K., Azadi H. Nigella Plants–Traditional Uses, Bioactive Phytoconstituents, Preclinical and Clinical Studies. Front. Pharmacol. 2021;12:417. doi: 10.3389/fphar.2021.625386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Ezeani C., Ezenyi I., Okoye T., Okoli C. Ocimum basilicum extract exhibits antidiabetic effects via inhibition of hepatic glucose mobilization and carbohydrate metabolizing enzymes. J. Intercult. Ethnopharmacol. 2017;6:22–28. doi: 10.5455/jice.20161229054825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.El-Beshbishy H., Bahashwan S. Hypoglycemic effect of basil (Ocimum basilicum) aqueous extract is mediated through inhibition of α-glucosidase and α-amylase activities: An in vitro study. Toxicol. Ind. Health. 2012;28:42–50. doi: 10.1177/0748233711403193. [DOI] [PubMed] [Google Scholar]
- 198.Joshi R.K. Chemical composition and antimicrobial activity of the essential oil of Ocimum basilicum L. (sweet basil) from Western Ghats of North West Karnataka, India. Anc. Sci. Life. 2014;33:151. doi: 10.4103/0257-7941.144618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Hannan J.M.A., Marenah L., Ali L., Rokeya B., Flatt P.R., Abdel-Wahab Y.H.A. Ocimum sanctum leaf extracts stimulate insulin secretion from perfused pancreas, isolated islets and clonal pancreatic β-cells. J. Endocrinol. 2006;189:127–136. doi: 10.1677/joe.1.06615. [DOI] [PubMed] [Google Scholar]
- 200.Qadir N.M., Ali K.A., Qader S.W. Antidiabetic effect of Oleuropein from Olea europaea Leaf against Alloxan Induced Type 1 Diabetic in Rats. Braz. Arch. Biol. Technol. 2016;59:347–350. doi: 10.1590/1678-4324-2016150116. [DOI] [Google Scholar]
- 201.Khan Y., Panchal S., Vyas N., Butani A., Kumar V. Olea europaea: A phyto-pharmacological review. Pharmacogn. Rev. 2007;1:114–118. [Google Scholar]
- 202.Attele A.S., Zhou Y.-P., Xie J.-T., Wu J.A., Zhang L., Dey L., Pugh W., Rue P.A., Polonsky K.S., Yuan C.S. Antidiabetic Effects of Panax ginseng Berry Extract and the Identification of an Effective Component. Diabetes. 2002;51:1851–1858. doi: 10.2337/diabetes.51.6.1851. [DOI] [PubMed] [Google Scholar]
- 203.Xiang Y.Z., Shang H.C., Gao X.M., Zhang B.L. A comparison of the ancient use of ginseng in traditional Chinese medicine with modern pharmacological experiments and clinical trials. Phytother. Res. 2008;22:851–858. doi: 10.1002/ptr.2384. [DOI] [PubMed] [Google Scholar]
- 204.Muhoya F.K., Kadima J.N., Ranarivelo N., Frédérich M., Hubert P., Marini R.D. Preliminary Phytochemical Content and Antidiabetic Potential Investigations of Panda oleosa (Pierre) Used in Kisangani Areas. Am. J. Anal. Chem. 2017;8:564–581. doi: 10.4236/ajac.2017.89041. [DOI] [Google Scholar]
- 205.Saleem Z.M., Ahmed S., Hasan M.M. Phaseoulus vulgaris Linn.: Botany, Medicinal Uses, Phytochemistry and Pharmacology. World J. Pharm. Res. 2016;5:1611–1616. doi: 10.20959/wjpr201611-7371. [DOI] [Google Scholar]
- 206.Lawson-Evi P., Eklu-Gadegbeku K., Agbonon A., Aklikokou K., Creppy E., Gbeassor M. Antidiabetic activity of Phyllanthus amarus Schum and Thonn (Euphorbiaceae) on Alloxan Induced Diabetes in Male Wistar Rats. J. Appl. Sci. 2011;11:2968–2973. doi: 10.3923/jas.2011.2968.2973. [DOI] [Google Scholar]
- 207.Patel J.R., Tripathi P., Sharma V., Chauhan N.S., Dixit V.K. Phyllanthus amarus: Ethnomedicinal uses, phytochemistry and pharmacology: A review. J. Ethnopharmacol. 2011;138:286–313. doi: 10.1016/j.jep.2011.09.040. [DOI] [PubMed] [Google Scholar]
- 208.Hannan J.M.A., Ali L., Khaleque J., Akhter M., Flatt P.R., Abdel-Wahab Y.H.A. Aqueous extracts of husks of Plantago ovata reduce hyperglycaemia in type 1 and type 2 diabetes by inhibition of intestinal glucose absorption. Br. J. Nutr. 2006;96:131–137. doi: 10.1079/BJN20061819. [DOI] [PubMed] [Google Scholar]
- 209.Madgulkar A.R., Rao M.R., Warrier D. Characterization of Psyllium (Plantago ovata) Polysaccharide and Its Uses. In: Ramawat K., Mérillon J.M., editors. Polysaccharides. Springer; New York, NY, USA: 2015. pp. 871–890. [DOI] [Google Scholar]
- 210.Reyad-ul-Ferdous M., Ahmmed A., Kamal M.A.H.M., Ansari P., Shahjahan D.S., Akter F., Sakib M.H. Herbal remedies as Alternative to Antidiabetic and Plants are Available in Bangladesh: A comprehensive. World J. Pharm. Res. 2015;4:2382–2389. [Google Scholar]
- 211.Rahman M.S., Mujahid M., Siddiqui M.A., Rahman M.A., Arif M., Eram S., Khan A., Azeemuddin M. Ethnobotanical Uses, Phytochemistry and Pharmacological Activities of Pterocarpus marsupium: A Review. Pharmacogn. J. 2018;10:s1–s8. doi: 10.5530/pj.2018.6s.1. [DOI] [Google Scholar]
- 212.Tang D., Liu L., Ajiakber D., Ye J., Xu J., Xin X., Aisa H.A. Anti-diabetic Effect of Punica granatum Flower Polyphenols Extract in Type 2 Diabetic Rats: Activation of Akt/GSK-3β and Inhibition of IRE1α-XBP1 Pathways. Front. Endocrinol. 2018;9:586. doi: 10.3389/fendo.2018.00586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Bhowmik D., Gopinath H., Kumar B.P., Kumar K. Medicinal Uses of Punica granatum and Its Health Benefits. J. Pharmacogn. Phytochem. 2013;1:28–35. [Google Scholar]
- 214.Zhu H., Wang Y., Liu Z., Wang J., Wan D., Feng S., Yang X., Wang T. Antidiabetic and antioxidant effects of catalpol extracted from Rehmannia glutinosa (Di Huang) on rat diabetes induced by streptozotocin and high-fat, high-sugar feed. Chin. Med. 2016;11:25. doi: 10.1186/s13020-016-0096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Zhang R.-X., Li M.-X., Jia Z.-P. Rehmannia glutinosa: Review of botany, chemistry and pharmacology. J. Ethnopharmacol. 2008;117:199–214. doi: 10.1016/j.jep.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 216.Kumar R., Anjum N., Tripathi Y. Phytochemistry and Pharmacology of Santalum album L.: A Review. World J. Pharm. Res. 2015;4:1842–1876. [Google Scholar]
- 217.Paswan S.K., Gautam A., Verma P., Rao C.V., Sidhu O.P., Singh A.P., Srivastava S. The Indian Magical Herb ‘Sanjeevni’(Selaginella bryopteris L.)—A Promising Anti-inflammatory Phytomedicine for the Treatment of Patients with Inflammatory Skin Diseases. J. Pharmacopunct. 2017;20:93–99. doi: 10.3831/KPI.2017.20.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Amutha K., Godavari A. In-vitro-antidiabetic activity of N-butanol extract of Sesamum indicum. Asian J. Pharm. Clin. Res. 2016;9:60–62. [Google Scholar]
- 219.Anilakumar K.R., Pal A., Khanum F., Bawa A.S. Nutritional, medicinal and industrial uses of sesame (Sesamum indicum L.) seeds-an overview. Agric. Conspec. Sci. 2010;75:159–168. [Google Scholar]
- 220.Nyaga S.N., Mathiu P.M., Onyango C.M., Areba G.O. Antidiabetic Properties of Solanum Villosum and Solanum Nigrum Var. sarrachoides in a Streptozotocin-induced Diabetic Mice Model. Int. J. Basic Clin. Pharmacol. 2019;8:2396–2402. doi: 10.18203/2319-2003.ijbcp20194774. [DOI] [Google Scholar]
- 221.Kuete V. Toxicological Survey of African Medicinal Plants. Elsevier Inc.; Amsterdam, The Netherlands: 2014. Physical, hematological, and histopathological signs of toxicity induced by African medicinal plants; pp. 635–657. [DOI] [Google Scholar]
- 222.Hannan J.M.A., Ansari P., Azam S., Flatt P.R., Wahab Y.H.A. Effects of Spirulina platensis on insulin secretion, dipeptidyl peptidase IV activity and both carbohydrate digestion and absorption indicate potential as an adjunctive therapy for diabetes. Br. J. Nutr. 2020;124:1021–1034. doi: 10.1017/S0007114520002111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Kumari D.J., Babitha B., Jaffar S., Prasad M.G., Ibrahim M., Khan M.S. Potential health benefits of Spirulina platensis. Int. J. Adv. Pharm. Sci. 2011;2:417–422. [Google Scholar]
- 224.Kumar V., Van Staden J. A review of Swertia chirayita (Gentianaceae) as a traditional medicinal plant. Front. Pharmacol. 2016;6:308. doi: 10.3389/fphar.2015.00308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Kuru P. Tamarindus indica and its health related effects. Asian Pac. J. Trop. Biomed. 2014;4:676–681. doi: 10.12980/APJTB.4.2014APJTB-2014-0173. [DOI] [Google Scholar]
- 226.Amalraj A., Gopi S. Medicinal Properties of Terminalia arjuna (Roxb.) Wight & Arn.: A review. J. Tradit. Complementary Med. 2017;7:65–78. doi: 10.1016/j.jtcme.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Kumar G.P.S., Arulselvan P., Kumar D.S., Subramanian S.P. Anti-diabetic Activity of Fruits of Terminalia chebula on Streptozotocin Induced Diabetic Rats. J. Health Sci. 2006;52:283–291. doi: 10.1248/jhs.52.283. [DOI] [Google Scholar]
- 228.Jokar A., Masoomi F., Sadeghpour O., Nassiri-Toosi M., Hamedi S. Potential therapeutic applications for Terminalia chebula in Iranian traditional medicine. J. Tradit. Chin. Med. 2016;36:250–254. doi: 10.1016/S0254-6272(16)30035-8. [DOI] [PubMed] [Google Scholar]
- 229.Saha S., Ghosh S. Tinospora cordifolia: One plant, many roles. Anc. Sci. Life. 2012;31:151–159. doi: 10.4103/0257-7941.107344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Hannan J.M.A., Ali L., Rokeya B., Khaleque J., Akhter M., Flatt P.R., Abdel-Wahab Y.H.A. Soluble dietary fibre fraction of Trigonella foenum-graecum (fenugreek) seed improves glucose homeostasis in animal models of type 1 and type 2 diabetes by delaying carbohydrate digestion and absorption and enhancing insulin action. Br. J. Nutr. 2007;97:514–521. doi: 10.1017/S0007114507657869. [DOI] [PubMed] [Google Scholar]
- 231.Mandal S., DebMandal M. Fenugreek (Trigonella foenum-graecum L.) Oils. In: Preedy V.R., editor. Essential Oils in Food Preservation, Flavor and Safety. Academic Press; Cambridge, MA, USA: 2016. pp. 421–429. [DOI] [Google Scholar]
- 232.Ahangarpour A., Mohammadian M., Dianat M. Antidiabetic effect of hydroalcholic Urtica dioica leaf extract in male rats with fructose-induced insulin resistance. Iran. J. Med. Sci. 2012;37:181–186. [PMC free article] [PubMed] [Google Scholar]
- 233.Hall J., Bravo-Clouzet R. Anti-Inflammatory Herbs for Arthritis. In: Watson R.R., Preedy V.R., editors. Bioactive Food as Dietary Interventions for Arthritis and Related Inflammatory Diseases. 2nd ed. Academic Press; Cambridge, MA, USA: 2013. pp. 619–631. [Google Scholar]
- 234.Asante D.-B., Effah-Yeboah E., Barnes P., Abban H.A., Ameyaw E.O., Boampong J.N., Ofori E.G., Dadzie J.B. Antidiabetic effect of young and old ethanolic leaf extracts of Vernonia amygdalina: A comparative study. J. Diabetes Res. 2016;2016:8252741. doi: 10.1155/2016/8252741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Oyeyemi I.T., Akinlabi A.A., Adewumi A., Aleshinloye A.O., Oyeyemi O.T. Vernonia amygdalina: A folkloric herb with anthelminthic properties. Beni-Suef Univ. J. Basic Appl. Sci. 2018;7:43–49. doi: 10.1016/j.bjbas.2017.07.007. [DOI] [Google Scholar]
- 236.Gupta P.C. Withania coagulans Dunal-an overview. Int. J. Pharm. Sci. Rev. Res. 2012;12:68–71. [Google Scholar]
- 237.Akram M., Shah M.I., Usmanghan K., Mohiuddin E., Sami A., Asif M., Shah S.A., Ahmed K., Shaheen G. Zingiber officinale roscoe (A medicinal plant) Pak. J. Nutr. 2011;10:399–400. doi: 10.3923/pjn.2011.399.400. [DOI] [Google Scholar]
- 238.Firdous S. Phytochemicals for treatment of diabetes. EXCLI J. 2014;13:451–453. [PMC free article] [PubMed] [Google Scholar]
- 239.Prabhakar P., Banerjee M. Antidiabetic phytochemicals: A comprehensive review on opportunities and challenges in targeted therapy for herbal drug development. Int. J. Pharm. Res. 2020;12:1673–1696. [Google Scholar]
- 240.Soni H., Malik J., Yadav A.P., Yadav B. Characterization of rutin isolated by leaves Annona squamosa by modern analytical techniques. Eur. J. Biomed. Pharm. Sci. 2018;5:484–489. [Google Scholar]
- 241.Zhang R., Yao Y., Wang Y., Ren G. Antidiabetic activity of isoquercetin in diabetic KK-A y mice. Nutr. Metab. 2011;8:85. doi: 10.1186/1743-7075-8-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Sangeetha R. Luteolin in the Management of Type 2 Diabetes Mellitus. Curr. Res. Nutr. Food Sci. J. 2019;7:393–398. doi: 10.12944/CRNFSJ.7.2.09. [DOI] [Google Scholar]
- 243.Xu F., Wu H., Wang Y., Yang Y., Wang X. Study on the Mechanism of Lupenone for Treating type 2 Diabetes by Integrating Pharmacological Evaluation and Network Pharmacology. Pharm. Biol. 2021;60:997–1010. doi: 10.1080/13880209.2022.2067568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Pawar M.R.V., Karthikeyan E. Role of Catechins in Diabetes Mellitus. Eur. J. Mol. Clin. Med. 2020;7:7604–7609. [Google Scholar]
- 245.Celine S., Tomy S., Ujwala T., Johnson S., Chander U. A detailed overview of medicinal plants having hypoglycemic activity. Int. J. Phytomedicine. 2016;8:139–175. doi: 10.5138/09750185.1817. [DOI] [Google Scholar]
- 246.Abdulkhaleq L.A., Assi M.A., Noor M.H.M., Abdullah R., Saad M.Z., Taufiq-Yap Y.H. Therapeutic uses of epicatechin in diabetes and cancer. Vet. World. 2017;10:869–872. doi: 10.14202/vetworld.2017.869-872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Lakshmi T., Ramasamy R., Thirumalaikumaran R. Preliminary phytochemical analysis and in vitro antioxidant, FTIR spectroscopy, anti-diabetic activity of Acacia catechu ethanolic seed extract. Pharmacogn. J. 2015;7:356–362. doi: 10.5530/pj.2015.6.7. [DOI] [Google Scholar]
- 248.Bharti S.K., Krishnan S., Kumar A., Kumar A. Antidiabetic phytoconstituents and their mode of action on metabolic pathways. Ther. Adv. Endocrinol. Metab. 2018;9:81–100. doi: 10.1177/2042018818755019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Niture N.T., Ansari A.A., Naik S.R. Anti-hyperglycemic activity of rutin in streptozotocin-induced diabetic rats: An effect mediated through cytokines, antioxidants and lipid biomarkers. Indian J. Exp. Biol. 2014;52:720–727. [PubMed] [Google Scholar]
- 250.Ramalingam S., Packirisamy M., Karuppiah M., Vasu G., Gopalakrishnan R., Gothandam K., Thiruppathi M. Effect of β-sitosterol on glucose homeostasis by sensitization of insulin resistance via enhanced protein expression of PPRγ and glucose transporter 4 in high fat diet and streptozotocin-induced diabetic rats. Cytotechnology. 2020;72:357–366. doi: 10.1007/s10616-020-00382-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Nigam V., Nambiar V. Therapeutic potential of Aegle marmelos (L.) Correa leaves as an antioxidant and anti-diabetic agent: A review. Int. J. Pharma Sci. Res. 2015;6:611–621. [Google Scholar]
- 252.Baliga M.S., Thilakchand K.R., Rai M.P., Rao S., Venkatesh P. Aegle marmelos (L.) Correa (Bael) and its phytochemicals in the treatment and prevention of cancer. Integr. Cancer Ther. 2013;12:187–196. doi: 10.1177/1534735412451320. [DOI] [PubMed] [Google Scholar]
- 253.Wei C.-K., Tsai Y.-H., Korinek M., Hung P.-H., El-Shazly M., Cheng Y.-B., Wu Y.-C., Hsieh T.-J., Chang F.-R. 6-Paradol and 6-Shogaol, the Pungent Compounds of Ginger, Promote Glucose Utilization in Adipocytes and Myotubes, and 6-Paradol Reduces Blood Glucose in High-Fat Diet-Fed Mice. Int. J. Mol. Sci. 2017;18:168. doi: 10.3390/ijms18010168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Son M.J., Miura Y., Yagasaki K. Mechanisms for antidiabetic effect of gingerol in cultured cells and obese diabetic model mice. Cytotechnology. 2015;67:641–652. doi: 10.1007/s10616-014-9730-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Wang X., Li Y.L., Wu H., Liu J.Z., Hu J.X., Liao N., Peng J., Cao P.P., Liang X., Hai C.X. Antidiabetic effect of oleanolic acid: A promising use of a traditional pharmacological agent. Phytother. Res. 2011;25:1031–1040. doi: 10.1002/ptr.3385. [DOI] [PubMed] [Google Scholar]
- 256.Chandramohan G., Al-Numair K.S., Alsaif M.A., Veeramani C. Antidiabetic effect of kaempferol a flavonoid compound, on streptozotocin-induced diabetic rats with special reference to glycoprotein components. Prog. Nutr. 2015;17:50–57. [Google Scholar]
- 257.Gupta R., Sharma A.K., Sharma M., Dobhal M., Gupta R. Evaluation of antidiabetic and antioxidant potential of lupeol in experimental hyperglycaemia. Nat. Prod. Res. 2012;26:1125–1129. doi: 10.1080/14786419.2011.560845. [DOI] [PubMed] [Google Scholar]
- 258.Sunil C., Irudayaraj S.S., Duraipandiyan V., Alrashood S.T., Alharbi S.A., Ignacimuthu S. Friedelin exhibits antidiabetic effect in diabetic rats via modulation of glucose metabolism in liver and muscle. J. Ethnopharmacol. 2021;268:113659. doi: 10.1016/j.jep.2020.113659. [DOI] [PubMed] [Google Scholar]
- 259.Kumar D., Dash G., Tripathy N. Hypoglycaemic activity of bark extracts of Albizia lebbeck Benth. in streptozotocin induced diabetic rats. Int. J. Pharm. Sci. Rev. Res. 2013;18:28–32. [Google Scholar]
- 260.Hashiesh H.M., Meeran M.F.N., Sharma C., Sadek B., Kaabi J.A., Ojha S.K. Therapeutic Potential of β-Caryophyllene: A Dietary Cannabinoid in Diabetes and Associated Complications. Nutrients. 2020;12:2963. doi: 10.3390/nu12102963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Zhai B., Zhang C., Sheng Y., Zhao C., He X., Xu W., Huang K., Luo Y. Hypoglycemic and hypolipidemic effect of S-allyl-cysteine sulfoxide (alliin) in DIO mice. Sci. Rep. 2018;8:3527. doi: 10.1038/s41598-018-21421-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Chan C.-H., Ngoh G.-C., Yusoff R. A brief review on anti diabetic plants: Global distribution, active ingredients, extraction techniques and acting mechanisms. Pharmacogn. Rev. 2012;6:22–28. doi: 10.4103/0973-7847.95854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Abdulghafoor H.A., Ramadhan S.J., Nawfal A.J. Therapeutic Effects of Allicin against the Diabetes Mellitus Induced by Streptozotocin in Male Rats. Nat. Volatiles Essent. Oils J. 2021;8:8934–8945. [Google Scholar]
- 264.Zhong R., Chen L., Liu Y., Xie S., Li S., Liu B., Zhao C. Anti-diabetic effect of aloin via JNK-IRS1/PI3K pathways and regulation of gut microbiota. Food Sci. Hum. Wellness. 2022;11:189–198. doi: 10.1016/j.fshw.2021.07.019. [DOI] [Google Scholar]
- 265.Alinejad-Mofrad S., Foadoddini M., Saadatjoo S.A., Shayesteh M. Improvement of glucose and lipid profile status with Aloe vera in pre-diabetic subjects: A randomized controlled-trial. J. Diabetes Metab. Disord. 2015;14:22. doi: 10.1186/s40200-015-0137-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Martorell M., Castro N., Victoriano M., Capó X., Tejada S., Vitalini S., Pezzani R., Sureda A. An update of anthraquinone derivatives emodin, diacerein, and catenarin in diabetes. Evid.-Based Complementary Altern. Med. 2021;2021:3313419. doi: 10.1155/2021/3313419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Palheta I., Ferreira L. Hypoglycemic potential of Anacardium occidentale L. J. Anal. Pharm. Res. 2018;7:152–153. [Google Scholar]
- 268.Prabhakar P.K., Doble M. A target based therapeutic approach towards diabetes mellitus using medicinal plants. Curr. Diabetes Rev. 2008;4:291–308. doi: 10.2174/157339908786241124. [DOI] [PubMed] [Google Scholar]
- 269.Muruganandan S., Srinivasan K., Gupta S., Gupta P., Lal J. Effect of mangiferin on hyperglycemia and atherogenicity in streptozotocin diabetic rats. J. Ethnopharmacol. 2005;97:497–501. doi: 10.1016/j.jep.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 270.Liu Y.W., Hao Y.C., Chen Y.J., Yin S.Y., Zhang M.Y., Kong L., Wang T.Y. Protective effects of sarsasapogenin against early stage of diabetic nephropathy in rats. Phytother. Res. 2018;32:1574–1582. doi: 10.1002/ptr.6088. [DOI] [PubMed] [Google Scholar]
- 271.Jayachandran M., Zhang T., Ganesan K., Xu B., Chung S.S.M. Isoquercetin ameliorates hyperglycemia and regulates key enzymes of glucose metabolism via insulin signaling pathway in streptozotocin-induced diabetic rats. Eur. J. Pharmacol. 2018;829:112–120. doi: 10.1016/j.ejphar.2018.04.015. [DOI] [PubMed] [Google Scholar]
- 272.Amor A.J., Gómez-Guerrero C., Ortega E., Sala-Vila A., Lázaro I. Ellagic Acid as a Tool to Limit the Diabetes Burden: Updated Evidence. Antioxidants. 2020;9:1226. doi: 10.3390/antiox9121226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Sharma V.C., Kaushik A., Dey Y.N., Srivastava B., Wanjari M., Pawar S., Chougule S. Nephroprotective potential of Anogeissus latifolia Roxb. (Dhava) against gentamicin-induced nephrotoxicity in rats. J. Ethnopharmacol. 2021;273:114001. doi: 10.1016/j.jep.2021.114001. [DOI] [PubMed] [Google Scholar]
- 274.Szkudelski T., Szkudelska K. Anti-diabetic effects of resveratrol. Ann. N. Y. Acad. Sci. 2011;1215:34–39. doi: 10.1111/j.1749-6632.2010.05844.x. [DOI] [PubMed] [Google Scholar]
- 275.Dabe N.E., Kefale A.T. Antidiabetic Effects of Artemisia Species: A Systematic Review. Anc. Sci. Life. 2017;36:175–181. doi: 10.4103/asl.ASL_87_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Bakun P., Czarczynska-Goslinska B., Goslinski T., Lijewski S. In vitro and in vivo biological activities of azulene derivatives with potential applications in medicine. Med. Chem. Res. 2021;30:834–846. doi: 10.1007/s00044-021-02701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Ramírez-Espinosa J.J., Saldaña-Ríos J., García-Jiménez S., Villalobos-Molina R., Ávila-Villarreal G., Rodríguez-Ocampo A.N., Bernal-Fernández G., Estrada-Soto S. Chrysin Induces Antidiabetic, Antidyslipidemic and Anti-Inflammatory Effects in Athymic Nude Diabetic Mice. Molecules. 2018;23:67. doi: 10.3390/molecules23010067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Voroneanu L., Nistor I., Dumea R., Apetrii M., Covic A. Silymarin in Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Diabetes Res. 2016;2016:5147468. doi: 10.1155/2016/5147468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Mousavi L., Salleh M., Vikneswaran M., Asmawi M. Anti-diabetic chemical constituents isolated from traditional medicinal plants. J. Glob. Trends Pharm. Sci. 2016;7:3074–3083. [Google Scholar]
- 280.Maji S. Role of Phytochemicals in Human Physiological Disorders: Diabetes and Obesity. Scholars’ Press; Atlanta, GA, USA: 2020. Role of Neem leaves in Diabetes and Obesity; pp. 85–102. [Google Scholar]
- 281.Zaky A.S., Kandeil M., Abdel-Gabbar M., Fahmy E.M., Almehmadi M.M., Ali T.M., Ahmed O.M. The Antidiabetic Effects and Modes of Action of the Balanites aegyptiaca Fruit and Seed Aqueous Extracts in NA/STZ-Induced Diabetic Rats. Pharmaceutics. 2022;14:263. doi: 10.3390/pharmaceutics14020263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Yin J., Ye J., Jia W. Effects and mechanisms of berberine in diabetes treatment. Acta Pharm. Sin. B. 2012;2:327–334. doi: 10.1016/j.apsb.2012.06.003. [DOI] [Google Scholar]
- 283.Sankaranarayanan C., Nishanthi R., Pugalendi P. Ameliorating effect of berbamine on hepatic key enzymes of carbohydrate metabolism in high-fat diet and streptozotocin induced type 2 diabetic rats. Biomed. Pharmacother. 2018;103:539–545. doi: 10.1016/j.biopha.2018.04.066. [DOI] [PubMed] [Google Scholar]
- 284.Chang C.L.-T., Liu H.-Y., Kuo T.-F., Hsu Y.-J., Shen M.-Y., Pan C.-Y., Yang W.-C. Antidiabetic effect and mode of action of cytopiloyne. Evid.-Based Complementary Altern. Med. 2013;2013:685642. doi: 10.1155/2013/685642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Barky A., Ezz A., Mohammed T. The Potential role of apigenin in diabetes mellitus. Int. J. Clin. Case Rep. Rev. 2020;3:32. doi: 10.31579/2690-4861/032. [DOI] [Google Scholar]
- 286.Parveen G., Ali M. Extraction Isolation and Phytochemical Screening of Leaves and Stems of Bidens Pilosa and Evaluation of Antifungal Potential of Extracts. J. Pharm. Biol. Sci. 2019;14:73–85. doi: 10.9790/3008-1404027385. [DOI] [Google Scholar]
- 287.Kim H.J., Park K.S., Lee S.K., Min K.W., Han K.A., Kim Y.K., Ku B.J. Effects of pinitol on glycemic control, insulin resistance and adipocytokine levels in patients with type 2 diabetes mellitus. Ann. Nutr. Metab. 2012;60:1–5. doi: 10.1159/000334834. [DOI] [PubMed] [Google Scholar]
- 288.Hafizur R.M., Hameed A., Shukrana M., Raza S.A., Chishti S., Kabir N., Siddiqui R.A. Cinnamic acid exerts anti-diabetic activity by improving glucose tolerance in vivo and by stimulating insulin secretion in vitro. Phytomedicine. 2015;22:297–300. doi: 10.1016/j.phymed.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 289.Ortsäter H., Grankvist N., Wolfram S., Kuehn N., Sjöholm Å. Diet supplementation with green tea extract epigallocatechin gallate prevents progression to glucose intolerance in db/db mice. Nutr. Metab. 2012;9:11. doi: 10.1186/1743-7075-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Wolfram S., Raederstorff D., Preller M., Wang Y., Teixeira S.R., Riegger C., Weber P. Epigallocatechin gallate supplementation alleviates diabetes in rodents. J. Nutr. 2006;136:2512–2518. doi: 10.1093/jn/136.10.2512. [DOI] [PubMed] [Google Scholar]
- 291.Belury M.A., Cole R.M., Snoke D.B., Banh T., Angelotti A. Linoleic acid, glycemic control and Type 2 diabetes. Prostaglandins Leukot. Essent. Fat. Acids. 2018;132:30–33. doi: 10.1016/j.plefa.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Pu J., Peng G., Li L., Na H., Liu Y., Liu P. Palmitic acid acutely stimulates glucose uptake via activation of Akt and ERK1/2 in skeletal muscle cells [S] J. Lipid Res. 2011;52:1319–1327. doi: 10.1194/jlr.M011254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Mishra C., Code Q. Comparative anti-diabetic study of three phytochemicals on high-fat diet and streptozotocin-induced diabetic dyslipidemic rats. Int. J. Biomed. Adv. Res. 2018;9:286–293. doi: 10.7439/ijbar. [DOI] [Google Scholar]
- 294.Majidi Z., Bina F., Kahkeshani N., Rahimi R. Bunium persicum: A review of ethnopharmacology, phytochemistry, and biological activities. Tradit. Integr. Med. 2020;5:150–176. doi: 10.18502/tim.v5i3.4322. [DOI] [Google Scholar]
- 295.Babujanarthanam R., Kavitha P., Pandian M.R. Quercitrin, a bioflavonoid improves glucose homeostasis in streptozotocin-induced diabetic tissues by altering glycolytic and gluconeogenic enzymes. Fundam. Clin. Pharmacol. 2010;24:357–364. doi: 10.1111/j.1472-8206.2009.00771.x. [DOI] [PubMed] [Google Scholar]
- 296.Han X.-X., Jiang Y.-P., Liu N., Wu J., Yang J.-M., Li Y.-X., Sun M., Sun T., Zheng P., Yu J.-Q. Protective effects of astragalin on spermatogenesis in streptozotocin-induced diabetes in male mice by improving antioxidant activity and inhibiting inflammation. Biomed. Pharmacother. 2019;110:561–570. doi: 10.1016/j.biopha.2018.12.012. [DOI] [PubMed] [Google Scholar]
- 297.Yusuf M., Nasiruddin M., Sultana N., Akhtar J., Khan M.I., Ahmad M. Regulatory Mechanism of Caffeic acid on glucose Metabolism in Diabetes. Res. J. Pharm. Technol. 2019;12:4735–4740. doi: 10.5958/0974-360X.2019.00816.3. [DOI] [Google Scholar]
- 298.Kadakol A., Malek V., Goru S.K., Pandey A., Sharma N., Gaikwad A.B. Esculetin ameliorates insulin resistance and type 2 diabetic nephropathy through reversal of histone H3 acetylation and H2A lysine 119 monoubiquitination. J. Funct. Foods. 2017;35:256–266. doi: 10.1016/j.jff.2017.05.051. [DOI] [Google Scholar]
- 299.Song J.-X., Ren H., Gao Y.-F., Lee C.-Y., Li S.-F., Zhang F., Li L., Chen H. Dietary capsaicin improves glucose homeostasis and alters the gut microbiota in obese diabetic ob/ob mice. Front. Physiol. 2017;8:602. doi: 10.3389/fphys.2017.00602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Marcelino G., Machate D.J., de Cássia Freitas K., Hiane P.A., Maldonade I.R., Pott A., Asato M.A., Candido C.J., de Cássia Avellaneda Guimarães R. β-Carotene: Preventive Role for Type 2 Diabetes Mellitus and Obesity: A Review. Molecules. 2020;25:5803. doi: 10.3390/molecules25245803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Meng S., Cao J., Feng Q., Peng J., Hu Y. Roles of chlorogenic acid on regulating glucose and lipids metabolism: A review. Evid.-Based Complementary Altern. Med. 2013;2013:801457. doi: 10.1155/2013/801457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Ranđelović S., Bipat R. A Review of Coumarins and Coumarin-Related Compounds for Their Potential Antidiabetic Effect. Clin. Med. Insights: Endocrinol. Diabetes. 2021;14:11795514211042023. doi: 10.1177/11795514211042023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Malik A., Jamil U., Butt T.T., Waquar S., Gan S.H., Shafique H., Jafar T.H. In silico and in vitro studies of lupeol and iso-orientin as potential antidiabetic agents in a rat model. Drug Des. Dev. Ther. 2019;13:1501–1513. doi: 10.2147/DDDT.S176698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Bak E.-J., Kim J., Jang S., Woo G.-H., Yoon H.-G., Yoo Y.-J., Cha J.-H. Gallic acid improves glucose tolerance and triglyceride concentration in diet-induced obesity mice. Scand. J. Clin. Lab. Investig. 2013;73:607–614. doi: 10.3109/00365513.2013.831470. [DOI] [PubMed] [Google Scholar]
- 305.Goboza M., Aboua Y.G., Chegou N., Oguntibeju O.O. Vindoline effectively ameliorated diabetes-induced hepatotoxicity by docking oxidative stress, inflammation and hypertriglyceridemia in type 2 diabetes-induced male Wistar rats. Biomed. Pharmacother. 2019;112:108638. doi: 10.1016/j.biopha.2019.108638. [DOI] [PubMed] [Google Scholar]
- 306.Alonso-Castro A.J., Zapata-Bustos R., Gómez-Espinoza G., Salazar-Olivo L.A. Isoorientin reverts TNF-α-induced insulin resistance in adipocytes activating the insulin signaling pathway. Endocrinology. 2012;153:5222–5230. doi: 10.1210/en.2012-1290. [DOI] [PubMed] [Google Scholar]
- 307.Cadena-Zamudio J.D., Nicasio-Torres M.d.P., Guerrero-Analco J.A., Ibarra-Laclette E. Ethnopharmacological studies of Cecropia obtusifolia (Urticaceae) and its importance in the treatment of type 2 diabetes mellitus: A mini-review. Acta Bot. Mex. 2019;126 doi: 10.21829/abm126.2019.1361. [DOI] [Google Scholar]
- 308.Abbas Z.K., Saggu S., Sakeran M.I., Zidan N., Rehman H., Ansari A.A. Phytochemical, antioxidant and mineral composition of hydroalcoholic extract of chicory (Cichorium intybus L.) leaves. Saudi J. Biol. Sci. 2015;22:322–326. doi: 10.1016/j.sjbs.2014.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Guo X., Sun W., Huang L., Wu L., Hou Y., Qin L., Liu T. Effect of cinnamaldehyde on glucose metabolism and vessel function. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2017;23:3844–3853. doi: 10.12659/MSM.906027. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 310.Singh P., Jayaramaiah R.H., Agawane S.B., Vannuruswamy G., Korwar A.M., Anand A., Dhaygude V.S., Shaikh M.L., Joshi R.S., Boppana R. Potential dual role of eugenol in inhibiting advanced glycation end products in diabetes: Proteomic and mechanistic insights. Sci. Rep. 2016;6:18798. doi: 10.1038/srep18798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Hsu C.-C., Lin M.H., Cheng J.-T., Wu M.C. Diosmin, a Citrus Nutrient, Activates Imidazoline Receptors to Alleviate Blood Glucose and Lipids in Type 1-Like Diabetic Rats. Nutrients. 2017;9:684. doi: 10.3390/nu9070684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Revathy J., Sheik Abdullah S. The role of hesperetin in the management of diabetes mellitus and its complications. J. Cancer Treat. Res. 2017;5:1–6. doi: 10.11648/j.jctr.20170501.11. [DOI] [Google Scholar]
- 313.Den Hartogh D.J., Tsiani E. Antidiabetic Properties of Naringenin: A Citrus Fruit Polyphenol. Biomolecules. 2019;9:99. doi: 10.3390/biom9030099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Yan F., Benrong H., Qiang T., Qin F., Jizhou X. Hypoglycemic activity of jatrorrhizine. J. Huazhong Univ. Sci. Technol. [Med. Sci.] 2005;25:491–493. doi: 10.1007/BF02895996. [DOI] [PubMed] [Google Scholar]
- 315.Li Y., Sun M., Liu Y., Liang J., Wang T., Zhang Z. Gymnemic acid alleviates type 2 diabetes mellitus and suppresses endoplasmic reticulum stress in vivo and in vitro. J. Agric. Food Chem. 2019;67:3662–3669. doi: 10.1021/acs.jafc.9b00431. [DOI] [PubMed] [Google Scholar]
- 316.Castro A.J.G., Frederico M.J.S., Cazarolli L.H., Mendes C.P., Bretanha L.C., Schmidt E.C., Bouzon Z.L., de Medeiros Pinto V.A., da Fonte Ramos C., Pizzolatti M.G. The mechanism of action of ursolic acid as insulin secretagogue and insulinomimetic is mediated by cross-talk between calcium and kinases to regulate glucose balance. Biochim. Et Biophys. Acta (BBA)-Gen. Subj. 2015;1850:51–61. doi: 10.1016/j.bbagen.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 317.Marton L.T., Pescinini-e-Salzedas L.M., Camargo M.E.C., Barbalho S.M., Haber J.F., Sinatora R.V., Detregiachi C.R.P., Girio R.J., Buchaim D.V., Cincotto dos Santos Bueno P. The effects of curcumin on diabetes mellitus: A systematic review. Front. Endocrinol. 2021;12:443. doi: 10.3389/fendo.2021.669448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Lekshmi P., Arimboor R., Raghu K., Menon A.N. Turmerin, the antioxidant protein from turmeric (Curcuma longa) exhibits antihyperglycaemic effects. Nat. Prod. Res. 2012;26:1654–1658. doi: 10.1080/14786419.2011.589386. [DOI] [PubMed] [Google Scholar]
- 319.Zabad I.E.M., Amin M.N., El-Shishtawy M.M. Protective effect of vanillin on diabetic nephropathy by decreasing advanced glycation end products in rats. Life Sci. 2019;239:117088. doi: 10.1016/j.lfs.2019.117088. [DOI] [PubMed] [Google Scholar]
- 320.Zhou Q., Chen L., Chen Q.-W., Chen H.-W., Dong J.-X. Chemical constituents of Cudrania cochinchinensis. J. Chin. Med. Mater. 2013;36:1444–1447. [PubMed] [Google Scholar]
- 321.Oza M.J., Kulkarni Y.A. Biochanin A improves insulin sensitivity and controls hyperglycemia in type 2 diabetes. Biomed. Pharmacother. 2018;107:1119–1127. doi: 10.1016/j.biopha.2018.08.073. [DOI] [PubMed] [Google Scholar]
- 322.Yao X., Li K., Liang C., Zhou Z., Wang J., Wang S., Liu L., Yu C.-L., Song Z.-B., Bao Y.-L. Tectorigenin enhances PDX1 expression and protects pancreatic β-cells by activating ERK and reducing ER stress. J. Biol. Chem. 2020;295:12975–12992. doi: 10.1074/jbc.RA120.012849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Sultana S., Asif H.M., Naveed Akhtar N., Akhtar N. Dalbergia sissoo Roxb: Monograph. Int. J. Pharmacogn. 2015;2:440–443. [Google Scholar]
- 324.Yuan Y.-L., Guo C.-R., Cui L.-L., Ruan S.-X., Zhang C.-F., Ji D., Yang Z.-L., Li F. Timosaponin B-II ameliorates diabetic nephropathy via TXNIP, mTOR, and NF-κB signaling pathways in alloxan-induced mice. Drug Des. Dev. Ther. 2015;9:6247–6258. doi: 10.2147/DDDT.S96435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Qa’dan F., Verspohl E.J., Nahrstedt A., Petereit F., Matalka K.Z. Cinchonain Ib isolated from Eriobotrya japonica induces insulin secretion in vitro and in vivo. J. Ethnopharmacol. 2009;124:224–227. doi: 10.1016/j.jep.2009.04.023. [DOI] [PubMed] [Google Scholar]
- 326.Song T.-J., Park C.-H., In K.-R., Kim J.-B., Kim J.H., Kim M., Chang H.J. Antidiabetic effects of betulinic acid mediated by the activation of the AMP-activated protein kinase pathway. PLoS ONE. 2021;16:e0249109. doi: 10.1371/journal.pone.0249109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Kim D.Y., Kang M.-K., Lee E.-J., Kim Y.-H., Oh H., Kim S.-I., Oh S.Y., Na W., Kang Y.-H. Eucalyptol Inhibits Amyloid-β-Induced Barrier Dysfunction in Glucose-Exposed Retinal Pigment Epithelial Cells and Diabetic Eyes. Antioxidants. 2020;9:1000. doi: 10.3390/antiox9101000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Kolhe S.S., Rachh P.R. Review on potent anti-diabetic plants or herbs from traditional medicine. J. Drug Deliv. Ther. 2018;8:92–98. doi: 10.22270/jddt.v8i5.1856. [DOI] [Google Scholar]
- 329.Cherian S., Kumar R.V., Augusti K., Kidwai J. Antidiabetic effect of a glycoside of pelargonidin isolated from the bark of Ficus bengalensis Linn. Indian J. Biochem. Biophys. 1992;29:380–382. [PubMed] [Google Scholar]
- 330.Murugesu S., Selamat J., Perumal V. Phytochemistry, Pharmacological Properties, and Recent Applications of Ficus benghalensis and Ficus religiosa. Plants. 2021;10:2749. doi: 10.3390/plants10122749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Ayepola O.R., Chegou N.N., Brooks N.L., Oguntibeju O.O. Kolaviron, a Garcinia biflavonoid complex ameliorates hyperglycemia-mediated hepatic injury in rats via suppression of inflammatory responses. BMC Complementary Altern. Med. 2013;13:363. doi: 10.1186/1472-6882-13-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Ogunmoyole T., Olalekan O., Fatai O., Makun J., Kade I. Antioxidant and phytochemical profile of aqueous and ethanolic extract of Garcinia kola. J. Pharmacogn. Phytother. 2012;4:66–74. doi: 10.5897/JPP12.020. [DOI] [Google Scholar]
- 333.Sharma V., Katiyar A., Agarwal R.C. Glycyrrhiza glabra: Chemistry and Pharmacological Activity. In: Ramawat K., Mérillon J.M., editors. Sweeteners. Springer; New York, NY, USA: 2018. pp. 87–100. [DOI] [Google Scholar]
- 334.Takii H., Kometani T., Nishimura T., Nakae T., Okada S., Fushiki T. Antidiabetic effect of glycyrrhizin in genetically diabetic KK-Ay mice. Biol. Pharm. Bull. 2001;24:484–487. doi: 10.1248/bpb.24.484. [DOI] [PubMed] [Google Scholar]
- 335.Kalaiarasi P., Pugalendi K.V. Antihyperglycemic effect of 18β-glycyrrhetinic acid, aglycone of glycyrrhizin, on streptozotocin-diabetic rats. Eur. J. Pharmacol. 2009;606:269–273. doi: 10.1016/j.ejphar.2008.12.057. [DOI] [PubMed] [Google Scholar]
- 336.Gupta R., Bajpai K.G., Johri S., Saxena A. An overview of Indian novel traditional medicinal plants with anti-diabetic potentials. Afr. J. Tradit. Complementary Altern. Med. 2008;5:1–17. [PMC free article] [PubMed] [Google Scholar]
- 337.Ahangarpour A., Oroojan A.A., Khorsandi L., Shabani R., Mojaddami S. Preventive effects of betulinic acid on streptozotocinnicotinamide induced diabetic nephropathy in male mouse. J. Nephropathol. 2016;5:128–133. doi: 10.15171/jnp.2016.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Iwalewa E.O., Adewale I.O., Taiwo B.J., Arogundade T., Osinowo A., Daniyan O.M., Adetogun G.E. Effects of Harungana madagascariensis stem bark extract on the antioxidant markers in alloxan induced diabetic and carrageenan induced inflammatory disorders in rats. J. Complementary Integr. Med. 2008;5 doi: 10.2202/1553-3840.1088. [DOI] [Google Scholar]
- 339.Amalan V., Vijayakumar N., Indumathi D., Ramakrishnan A. Antidiabetic and antihyperlipidemic activity of p-coumaric acid in diabetic rats, role of pancreatic GLUT 2: In vivo approach. Biomed. Pharmacother. 2016;84:230–236. doi: 10.1016/j.biopha.2016.09.039. [DOI] [PubMed] [Google Scholar]
- 340.Wang J., Huang M., Yang J., Ma X., Zheng S., Deng S., Huang Y., Yang X., Zhao P. Anti-diabetic activity of stigmasterol from soybean oil by targeting the GLUT4 glucose transporter. Food Nutr. Res. 2017;61:1364117. doi: 10.1080/16546628.2017.1364117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Sindhu R.K., Puri V. Phytochemical, nutritional and pharmacological evidences for Abelmoschus esculentus (L.) J. Phytopharm. 2016;5:238–241. doi: 10.31254/phyto.2016.5606. [DOI] [Google Scholar]
- 342.Anwar A., Azmi M.A., Siddiqui J.A., Panhwar G., Shaikh F., Ariff M. Thiamine level in type I and type II diabetes mellitus patients: A comparative study focusing on hematological and biochemical evaluations. Cureus. 2020;12:e8027. doi: 10.7759/cureus.8027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Shi L., Du X., Guo P., Huang L., Qi P., Gong Q. Ascorbic acid supplementation in type 2 diabetes mellitus: A protocol for systematic review and meta-analysis. Medicine. 2020;99:e23125. doi: 10.1097/MD.0000000000023125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Chowdhury S., Ghosh S., Das A.K., Sil P.C. Ferulic acid protects hyperglycemia-induced kidney damage by regulating oxidative insult, inflammation and autophagy. Front. Pharmacol. 2019;10:27. doi: 10.3389/fphar.2019.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Wang H., Wang J., Qiu C., Ye Y., Guo X., Chen G., Li T., Wang Y., Fu X., Liu R.H. Comparison of phytochemical profiles and health benefits in fiber and oil flaxseeds (Linum usitatissimum L.) Food Chem. 2017;214:227–233. doi: 10.1016/j.foodchem.2016.07.075. [DOI] [PubMed] [Google Scholar]
- 346.Mitra A., Mahadevappa M. Antidiabetic and hypolipidemic effects of mahanimbine (carbazole alkaloid) from Murraya koenigii (rutaceae) leaves. Int. J. Phytomedicine. 2010;2:22–30. doi: 10.5138/ijpm.2010.0975.0185.02004. [DOI] [Google Scholar]
- 347.Song S.E., Jo H.J., Kim Y.-W., Cho Y.-J., Kim J.-R., Park S.-Y. Delphinidin prevents high glucose-induced cell proliferation and collagen synthesis by inhibition of NOX-1 and mitochondrial superoxide in mesangial cells. J. Pharmacol. Sci. 2016;130:235–243. doi: 10.1016/j.jphs.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 348.Desai S., Saheb S.H., Das K.K., Haseena S. Phytochemical Analysis of Nigella sativa and its Antidiabetic Effect. J. Pharm. Sci. Res. 2015;7:527–532. [Google Scholar]
- 349.Abdelrazek H., Kilany O.E., Muhammad M.A., Tag H.M., Abdelazim A.M. Black seed thymoquinone improved insulin secretion, hepatic glycogen storage, and oxidative stress in streptozotocin-induced diabetic male Wistar rats. Oxidative Med. Cell. Longev. 2018;2018:8104165. doi: 10.1155/2018/8104165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Saravanan S., Pari L. Role of thymol on hyperglycemia and hyperlipidemia in high fat diet-induced type 2 diabetic C57BL/6J mice. Eur. J. Pharmacol. 2015;761:279–287. doi: 10.1016/j.ejphar.2015.05.034. [DOI] [PubMed] [Google Scholar]
- 351.More T.A., Kulkarni B.R., Nalawade M.L., Arvindekar A.U. Antidiabetic activity of linalool and limonene in streptozotocin-induced diabetic rat: A combinatorial therapy approach. Int. J. Pharm. Pharm. Sci. 2014;6:159–163. [Google Scholar]
- 352.Al-Azzawie H.F., Alhamdani M.S.S. Hypoglycemic and antioxidant effect of oleuropein in alloxan-diabetic rabbits. Life Sci. 2006;78:1371–1377. doi: 10.1016/j.lfs.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 353.Dai S., Hong Y., Xu J., Lin Y., Si Q., Gu X. Ginsenoside Rb2 promotes glucose metabolism and attenuates fat accumulation via AKT-dependent mechanisms. Biomed. Pharmacother. 2018;100:93–100. doi: 10.1016/j.biopha.2018.01.111. [DOI] [PubMed] [Google Scholar]
- 354.Li Y., Zheng X., Yi X., Liu C., Kong D., Zhang J., Gong M. Myricetin: A potent approach for the treatment of type 2 diabetes as a natural class B GPCR agonist. FASEB J. 2017;31:2603–2611. doi: 10.1096/fj.201601339R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Kulkarni C.R., Joglekar M.M., Patil S.B., Arvindekar A.U. Antihyperglycemic and antihyperlipidemic effect of Santalum album in streptozotocin induced diabetic rats. Pharm. Biol. 2012;50:360–365. doi: 10.3109/13880209.2011.604677. [DOI] [PubMed] [Google Scholar]
- 356.Paswan S.K., Verma P., Azmi L., Srivastava S., Venkateswara Rao C. Phytochemical Investigation and HPTLC Fingerprinting Analysis of Selaginella bryopteris Ethanolic Plant Extract for Analgesic and Anti-inflammatory Activities in Animals. J. Biol. Act. Prod. Nat. 2021;11:395–405. doi: 10.1080/22311866.2021.1918023. [DOI] [Google Scholar]
- 357.Neeta M., Mukta N., Bilwa K. Comparative qualitative phytochemical analysis of Sesamum indicum L. Int. J. Curr. Microbiol. Appl. Sci. 2015;2:172–181. [Google Scholar]
- 358.Mohammad Shahi M., Zakerzadeh M., Zakerkish M., Zarei M., Saki A. Effect of sesamin supplementation on glycemic status, inflammatory markers, and adiponectin levels in patients with type 2 diabetes mellitus. J. Diet. Suppl. 2017;14:65–75. doi: 10.1080/19390211.2016.1204404. [DOI] [PubMed] [Google Scholar]
- 359.Bhadoriya S.S., Ganeshpurkar A., Bhadoriya R.P.S., Sahu S.K., Patel J.R. Antidiabetic potential of polyphenolic-rich fraction of Tamarindus indica seed coat in alloxan-induced diabetic rats. J. Basic Clin. Physiol. Pharmacol. 2018;29:37–45. doi: 10.1515/jbcpp-2016-0193. [DOI] [PubMed] [Google Scholar]
- 360.Harakeh S., Almuhayawi M., Al Jaouni S., Almasaudi S., Hassan S., Al Amri T., Azhar N., Abd-Allah E., Ali S., El-Shitany N. Antidiabetic effects of novel ellagic acid nanoformulation: Insulin-secreting and anti-apoptosis effects. Saudi J. Biol. Sci. 2020;27:3474–3480. doi: 10.1016/j.sjbs.2020.09.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Chang C.L., Lin C.S. Phytochemical composition, antioxidant activity, and neuroprotective effect of Terminalia chebula Retzius extracts. Evid.-Based Complementary Altern. Med. 2012;2012:125247. doi: 10.1155/2012/125247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Liu X., Kim J.-k., Li Y., Li J., Liu F., Chen X. Tannic acid stimulates glucose transport and inhibits adipocyte differentiation in 3T3-L1 cells. J. Nutr. 2005;135:165–171. doi: 10.1093/jn/135.2.165. [DOI] [PubMed] [Google Scholar]
- 363.Rajalakshmi M., Anita R. β-cell regenerative efficacy of a polysaccharide isolated from methanolic extract of Tinospora cordifolia stem on streptozotocin-induced diabetic Wistar rats. Chem.-Biol. Interact. 2016;243:45–53. doi: 10.1016/j.cbi.2015.11.021. [DOI] [PubMed] [Google Scholar]
- 364.Kalailingam P., Kannaian B., Tamilmani E., Kaliaperumal R. Efficacy of natural diosgenin on cardiovascular risk, insulin secretion, and beta cells in streptozotocin (STZ)-induced diabetic rats. Phytomedicine. 2014;21:1154–1161. doi: 10.1016/j.phymed.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 365.Leng J., Li X., Tian H., Liu C., Guo Y., Zhang S., Chu Y., Li J., Wang Y., Zhang L. Neuroprotective effect of diosgenin in a mouse model of diabetic peripheral neuropathy involves the Nrf2/HO-1 pathway. BMC Complementary Med. Ther. 2020;20:126. doi: 10.1186/s12906-020-02930-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Alara O.R., Abdurahman N.H., Ukaegbu C.I., Kabbashi N.A. Extraction and characterization of bioactive compounds in Vernonia amygdalina leaf ethanolic extract comparing Soxhlet and microwave-assisted extraction techniques. J. Taibah Univ. Sci. 2019;13:414–422. doi: 10.1080/16583655.2019.1582460. [DOI] [Google Scholar]
- 367.Balbi M.E., Tonin F.S., Mendes A.M., Borba H.H., Wiens A., Fernandez-Llimos F., Pontarolo R. Antioxidant effects of vitamins in type 2 diabetes: A meta-analysis of randomized controlled trials. Diabetol. Metab. Syndr. 2018;10:18. doi: 10.1186/s13098-018-0318-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Ram H., Kumar P., Purohit A., Kashyap P., Kumar S., Kumar S., Singh G., Alqarawi A.A., Hashem A., Abd-Allah E.F. Improvements in HOMA indices and pancreatic endocrinal tissues in type 2-diabetic rats by DPP-4 inhibition and antioxidant potential of an ethanol fruit extract of Withania coagulans. Nutr. Metab. 2021;18:43. doi: 10.1186/s12986-021-00547-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Peerzade N., Sayed N., Das N. Antimicrobial and phytochemical screening of methanolic fruit extract of Withania coagulans L. Dunal for evaluating the antidiabetic activity. Pharma Innov. J. 2018;7:197–204. [Google Scholar]
- 370.Osadebe P.O., Odoh E.U., Uzor P.F. Natural products as potential sources of antidiabetic drugs. J. Pharm. Res. Int. 2014;4:2075–2095. doi: 10.9734/BJPR/2014/8382. [DOI] [Google Scholar]
- 371.Dev S. Prime Ayurvedic Plant Drugs: A Modern Scientific Appraisal. 1st ed. Ane Books Pvt. Limited; New Delhi, India: 2012. p. 464. [Google Scholar]
- 372.Adedapo A., Ogunmiluyi I. The use of natural products in the management of diabetes: The current trends. J. Drug Deliv. Ther. 2020;10:153–162. doi: 10.22270/jddt.v10i1.3839. [DOI] [Google Scholar]
- 373.Kalita P., Deka S., Saharia B.J., Chakraborty A., Basak M., Deka M. An overview and future scope on traditionally used herbal plants of Assam having Antidiabetic activity. Int. J. Adv. Pharm. Biol. Chem. 2014;3:299–304. [Google Scholar]
- 374.Rout S.P., Chowdary K., Kar D., Das L. Plants as source of novel anti-diabetic drug: Present scenario and future perspectives. Curr. Trends Biotechnol. Pharmacol. 2008;3:614–632. [Google Scholar]
- 375.Verma S., Singh S. Current and future status of herbal medicines. Vet. World. 2008;1:347. doi: 10.5455/vetworld.2008.347-350. [DOI] [Google Scholar]
- 376.Kifle Z.D., Abdelwuhab M., Melak A.D., Meseret T., Adugna M. Pharmacological evaluation of medicinal plants with antidiabetic activities in Ethiopia: A review. Metab. Open. 2022;13:100174. doi: 10.1016/j.metop.2022.100174. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.