Abstract
Introduction
The burden of chronic breathlessness on individuals, family, society and health systems is significant and set to increase exponentially with an ageing population with complex multimorbidity, yet there is a lack of services. This has been further amplified by the coronavirus disease 2019 pandemic. Online breathlessness interventions have been proposed to fill this gap, but need development and evaluation based on patient preferences and choices. This study aimed to explore the preferences and choices of patients regarding the content of an online self-guided chronic breathlessness supportive intervention (SELF-BREATHE).
Methods
Semi-structured telephone interviews were conducted with adults living with advanced malignant and nonmalignant disease and chronic breathlessness (July to November 2020). Interviews were analysed using conventional and summative content analysis.
Results
25 patients with advanced disease and chronic breathlessness (COPD n=13, lung cancer n=8, interstitial lung disease n=3, bronchiectasis n=1; 17 male; median (range) age 70 (47–86) years; median (range) Medical Research Council dyspnoea score 3 (2−5)) were interviewed. Individuals highlighted strong preferences for focused education, methods to increase self-motivation and engagement, interventions targeting breathing and physical function, software capability to personalise the content of SELF-BREATHE to make it more meaningful to the user, and aesthetically designed content using various communication methods including written, video and audio content. Furthermore, they identified the need to address motivation as a key potential determinant of the success of SELF-BREATHE.
Conclusion
Our findings provide an essential foundation for future digital intervention development (SELF-BREATHE) and scaled research.
Short abstract
Patient preferences and choices will directly inform the content development of an online, self-guided chronic breathlessness supportive intervention (SELF-BREATHE) to optimise acceptability and potential for benefit https://bit.ly/3OX9PML
Introduction
Chronic breathlessness, i.e. persistent breathlessness despite optimal pharmacological treatment of the underlying disease is a major clinical and public health problem worldwide [1–3]. Prior to the coronavirus disease 2019 (COVID-19) global pandemic, the burden of chronic breathlessness on individuals, family, society and health systems was already substantial, and set to increase with an ageing population and complex multimorbidity. This has been further amplified by the COVID-19 pandemic, with emerging data suggesting that >40% of COVID-19 survivors have persistent (chronic) breathlessness [4, 5].
Chronic breathlessness is associated with increased healthcare expenditure. Treatment costs are strongly driven by emergency department attendance, re-attendance and hospitalisation, increasing with disease progression [1–3]. In a UK prospective observational study by Hutchinson et al. [2], the prevalence of acute-on-chronic breathlessness as a reason to present to the major emergencies area of emergency department was 20.2% (245 out of 1212; 95% CI 17.9–22.5%). A proportion of these attendances and re-attendances are potentially avoidable if patients have self-management strategies/management plans in place. Considering the ongoing healthcare crisis resulting from the COVID-19 pandemic, a proactive approach is required to build capacity and resilience within health systems to tackle chronic breathlessness.
Pulmonary rehabilitation is effective at slowing the rate of functional decline due to disease progression and breathlessness in patient with chronic respiratory disease [6]. However, uptake of pulmonary rehabilitation is varied, especially in advanced disease where patients find it difficult to leave home [7]. There is a growing interest in mind–body–movement therapies and arts-in-health programmes to support those living with chronic respiratory disease; however, the evidence to date demonstrates inconsistent benefits [8–10].
There is good evidence for face-to-face delivered transdiagnostic breathlessness-specific interventions, referred to as breathlessness support services for patients living with chronic breathlessness. A systematic review and meta-analyses demonstrated reductions in numeric rating scale distress due to breathlessness (n=324; mean difference (MD) −2.30, 95% CI −4.43 to −0.16; p=0.03) and Hospital Anxiety and Depression Scale depression scores (n=408; MD −1.67, 95% CI −2.52 to −0.81; p<0.001) favouring the face-to-face delivered breathlessness supportive intervention [11].
Core interventional components of these breathlessness support services include educational materials, a hand-held fan, breathing techniques, exercises and energy-conservation techniques to improve physical functioning, and breathlessness crisis self-management planning. Qualitative data consistently demonstrate the value of these nonpharmacological self-management approaches which increase patients’ control over their breathlessness (mastery), confidence, dignity and self-worth [12–14].
Digitisation and delivery of these clinically effective breathlessness support services online would increase the reach and impact of targeted nonpharmacological interventions for chronic breathlessness, as internet connectivity is available to ⩾55% of the global population [15]. There are >5 billion mobile phone users and the availability of thousands of mobile health applications has provided unprecedented access to online health and wellbeing supportive tools [15]. In the UK, in 2021, 95% of the adult population were internet users, which is expected to increase to 97.5% by 2025 [16]. Global data suggest that internet use, and in particular the use of video communication applications have increased exponentially during the COVID-19 pandemic [15, 17].
Development of an online breathlessness intervention would address an unmet clinical need, as patients with advanced disease living with chronic breathlessness who have access to the internet are motivated and willing to use online interventions if given the opportunity, skills and confidence to do so [18]. When attempting to develop an online self-guided breathlessness intervention, inclusion of patients in all aspects of this iterative process is key, as patient choice and preferences influence whether they engage with interventions [19, 20]. Understanding patient perspectives as to what they believe to be important regarding the content of online self-guided breathlessness interventions is important in co-design, to ensure that digital health interventions meet the needs of the target user group [19, 20].
The aim of this study was to explore preferences and choices with regards to the content of an in development online self-management intervention (SELF-BREATHE) for individuals living with chronic breathlessness due to advanced disease.
Methods
Study design
The methodology builds on the new Medical Research Council (MRC) framework for developing and evaluating complex interventions [20] and the Integrate, Design, Assess and Share (IDEAS) framework for the development of digital behavioural change interventions [21].
This research is grounded in a pragmatist research paradigm. Pragmatism is oriented towards solving practical problems in real-world settings. It recognises that knowledge is understood through human experience and becomes meaningful when coupled with action. Pragmatism encourages experimentation and reflection, and therefore is appropriate for use in the development of interventions such as SELF-BREATHE [22]. Semi-structured qualitative interviews were conducted with patients with advanced malignant and nonmalignant disease and chronic breathlessness. Findings are reported in line with Consolidated Framework for Reporting Qualitative Research guidance [23].
Ethical approval
Ethical and local research and development approval was obtained prior to commencing this research (research ethics committee reference number 20/LO/0160). The study was registered at www.clinicaltrials.gov (identifier NCT04466020).
Setting
Standard practice within our department is to offer patients their preferred method and location with regard to how and where research interviews are conducted, i.e. face-to-face or remote, at home or within the hospital. However, in line with the Department of Health and Social Care and Public Health England COVID-19 guidance, we were unable to do any in-person research activities and these semi-structured qualitative interviews were conducted over the telephone with patients at their place of residence between 1 July and 1 November 2020.
Participants
Inclusion criteria were adult patients aged >18 years; chronic breathlessness on exertion and or rest (MRC dyspnoea score >2) [24, 25]; and advanced disease such as cancer, COPD, chronic heart failure or interstitial lung disease (ILD), where the underlying disease was deemed to be optimally medically managed by the referring clinician.
Exclusion criteria were breathlessness of unknown cause; a primary clinical diagnosis of chronic hyperventilation syndrome; patients unable to speak English; and patients not capable of providing informed consent.
Sampling strategy
Patients with chronic breathlessness were purposively sampled to give maximum variation in diagnosis (malignant n=10–12, nonmalignant n=10–12), breathlessness severity (MRC 2–3 n=10–12, MRC 3–5 n=10–12), age (≤70 years n=10−12, ≥71 years n=10–12) and sex (male n=10–12, female n=10–12).
Recruitment
Patients were recruited from King's College Hospital NHS Foundation Trust (Denmark Hill and Princess Royal sites, London, UK) through respiratory medicine, oncology, physiotherapy and pulmonary rehabilitation services, which included virtual clinics offered in response to the COVID-19 pandemic.
Clinicians checked the eligibility of patients during routine consultations. If eligible, clinical staff asked the patient for permission to pass their contact details to the study principal investigator (C.C. Reilly), who provided them with a copy (paper via the post or electronic via email) of the patient information sheet. Thereafter, the principal investigator or researcher (A. Roach) contacted the patient after 72 h (minimum) to discuss the projects with them and answer any questions regarding the study. If the patient was happy to participate, an interview was scheduled at a mutually convenient time. Prior to the interview, the researcher asked the participant to verbally consent and sign and date the consent form. The consent process was audio-recorded. Participants returned the signed consent form to the research team using a pre-paid return envelope.
Sample size
Recruitment continued until data saturation was indicated (i.e. no new codes or themes relevant to the study aim emerged). This was determined by preliminary analysis of detailed reflective notes taken immediately after interviews, and constant comparison of new data with existing findings [26]. We anticipated that this would occur after recruitment of ∼20–25 participants.
Interview content
Interviews followed a semi-structured interview schedule guided by relevant literature [23] the views of relevant professionals, and study patient and public involvement (PPI) representatives. The topic guide explored whether individuals had internet access, positive and negative experiences of using the internet and enablers and barriers to internet use with specific reference to the development and content of an in-development online breathlessness supportive intervention called SELF-BREATHE.
Participants were introduced to the concept of SELF-BREATHE. The interviewer described the potential for developing SELF-BREATHE, an online platform where patients log on and learn about breathlessness and how to access tools such as breathing exercises, relaxation, distraction techniques and strengthening exercises that can be done at home which may help self-management of breathlessness. Following this brief overview of SELF-BREATHE, individuals were asked to reflect upon their own personal experiences and needs, to share their views, positive and negative, around the concept of SELF-BREATHE, what they identify as potential challenges that we may incur when developing SELF-BREATHE, and how we may overcome potential obstacles. Patients were asked to reflect upon their lived experiences and suggest content that they felt was important to include in SELF-BREATHE. Patients were asked about the need for human interaction within SELF-BREATHE, and what would influence their decision to use SELF-BREATHE, if given the opportunity.
Interviews were scheduled to last ∼60 min and conducted by a researcher (A. Roach, C.C. Reilly) with experience in qualitative palliative care research. Participants were not known to the interviewer prior to interview. Patient characteristics such as age, ethnicity, MRC dyspnoea score and living situation, summarised in table 1, were obtained via direct questioning prior to conducting the semi-structured interviews. Interviews were digitally audio-recorded. A reflexive diary was completed after each interview.
TABLE 1.
Patient characteristics of the individuals living with chronic breathlessness due to advanced disease who took part in the semi-structured interviews
| All | Internet users | Non-internet users | |
| Patients n | 25 | 21 | 4 |
| Age, years | 70 (47–86) | 67 (47–84) | 84 (70–86) |
| Age category | |||
| 41–50 | 1 (4%) | 1 (5%) | |
| 51–60 | 6 (24%) | 6 (29%) | |
| 61–70 | 7 (28%) | 6 (29%) | 1 (25%) |
| 71–80 | 6 (24%) | 6 (29%) | |
| 81–90 | 5 (20%) | 2 (10%) | 3 (75%) |
| MRC dyspnoea score | 3 (2–5) | 3 (2–4) | 4 (4–5) |
| MRC dyspnoea category | |||
| MRC 2 | 6 (24%) | 6 (29%) | |
| MRC 3 | 11 (44%) | 11 (52%) | |
| MRC 4 | 7 (28%) | 4 (19%) | 3 (75%) |
| MRC 5 | 1 (4%) | 1 (25%) | |
| Sex (male:female) n:n | 15:10 | 13:8 | 2:2 |
| Ethnicity | |||
| White | 21 (84%) | 17 (81%) | 4 (100%) |
| Asian or Asian British | 2 (8%) | 2 (9.5%) | 0 (0%) |
| Black, African, Caribbean or Black British | 2 (8%) | 2 (9.5%) | 0 (0%) |
| Primary diagnosis | |||
| COPD | 13 (52%) | 10 (48%) | 3 (75%) |
| Lung cancer | 8 (32%) | 7 (33%) | 1 (25%) |
| ILD | 3 (12%) | 3 (14%) | 0 (0%) |
| Bronchiectasis | 1 (4%) | 1 (5%) | 0 (0%) |
| Smoking status | |||
| Nonsmoker | 3 (12%) | 3 (14%) | 0 (0%) |
| Ex-smoker | 19 (76%) | 17 (81%) | 2 (50%) |
| Current smoker | 3 (12%) | 1 (5%) | 2 (50%) |
| Living situation | |||
| Living alone | 14 (56%) | 13 (62%) | 1 (25%) |
| Living with significant other/family | 11 (44%) | 8 (38%) | 3 (75%) |
| Support provided by a carer | |||
| Yes | 5 (20%) | 2 (9.5%) | 3 (75%) |
| No | 20 (80%) | 19 (90.5%) | 1 (25%) |
Data are presented as n (%) or median (range), unless otherwise stated. MRC: Medical Research Council; ILD: interstitial lung disease.
Analysis
The interview audio-recordings were transcribed verbatim, with care taken to use pseudonyms and anonymise patient-or staff-identifiable references. A reflexive diary was completed to reflect upon the flow of the interview, contextual factors, participant responses and personal reflections. A combination of conventional and summative content analysis was conducted supported by Microsoft Word and Excel software [27]. Initial conventional content analysis was inductive and commenced with immersion in the data. Reading each transcript word-by-word, codes were derived to capture key thoughts and concepts. Codes were refined and sorted into categories or meaningful clusters. Initial coding was conducted by the primary researcher (C.C. Reilly), who has experience of conducting and analysing qualitative research. Coding was supported by the qualitative lead for the project (K. Bristowe), who conducted line-by-line coding on extracts of a sample of interviews, and any discrepancies were discussed and resolved with discussion with the wider research team as required. Findings were discussed with the broader research team on development of the initial coding frame, following refinement, and on completion of the analysis. A secondary summative approach was employed to describe patterns in views. An iterative and concurrent process of recruitment and analysis was used in the development and refinement of categories and their properties. Analysis was guided by the underpinning pragmatist epistemology with a focus on understanding experiences to identify and overcome potential problems and inform development of the intervention [27].
Results
Participants
25 patients with chronic breathlessness due to advanced disease (COPD n=13, lung cancer n=8, ILD n=3, bronchiectasis n=1; 17 males; median (range) age 70 (47–86) years; and MRC dyspnoea score of 3 (2–5); table 1) were interviewed. Of these, 21 (84%) patients had access to the internet, of whom 20 (95%) reported that they would use an intervention like SELF-BREATHE, if given the opportunity.
Findings
Patients described their preferences for content and design of an online breathlessness support service (SELF-BREATHE) to optimise engagement. These were 1) education on chronic breathlessness; 2) ways to increase self-motivation and engagement; 3) ways to improve breathing and physical functioning; 4) software capability to personalise the content to make it more meaningful to the user; and 5) aesthetically designed content using a variety of communication tools.
Education on chronic breathlessness
Many participants described not fully understanding their breathlessness. They wanted to be more informed; however, information provision from health professionals was often lacking and the content available online overwhelming and often conflicting. SELF-BREATHE was viewed positively as a reliable resource to address this unmet need.
Information about breathlessness would be useful because the doctors never tell me anything. Basically, they just say, “you have got shortness of breath, we will give you a new inhaler”. COPD, male, 61–70 years, MRC dyspnoea score 2
As well as providing knowledge, education played a fundamental role in helping individuals to understand the relationship between their breathlessness and activity. It empowered them to understand what activities they could do, but also what they could do to improve their symptoms.
It's really important that people have an understanding or, at least, a little bit of education around what's going on [breathlessness]. Knowledge is power, okay. Part of me not doing anything [physical activity] was because I didn't know how it [my breathing] was going to react and my body. I was frightened to do anything in case I made things worse. I learned [from pulmonary rehabilitation] that, actually, by doing some exercise it will increase my lung capacity, which would help me. I didn't know that. If there was some information to let people know that by doing certain exercises it's going to work your airways and we all need oxygen all over the body in the muscles, everything. Information like that would be useful. COPD, female, 51–60 years, MRC dyspnoea score 4
Providing a reliable source of education and knowledge not only helps individuals to understand their illness, but can help to challenge negative health beliefs, misconceptions and fears about exercising and breathlessness.
I think that the website [SELF-BREATHE] should include, is that you're not going to keel over from just exerting yourself a little bit. I was really frightened to do any exercise in case I made things worse. ILD, male, 51–60 years, MRC dyspnoea score 3
The potential benefits of the SELF-BREATHE intervention were described beyond the individual patient level. Provision of reliable educational content could also support relationships between patients and those close to them, by helping them also to understand the nature and limitations of their often “invisible” condition.
I know this is a silly request, my grandson is nine, and we are as close as close as you can be. He does worry and he does not understand a lot of it. Lung disease, how do you explain it? You know? I wonder if maybe there was something that a child could look at where I can explain to him, “this is what is happening to nanny?” I mean I am diabetic, so I inject and that, and he understands that I test my blood to see how much sugars I have got or do not, I take the insulin and do not eat too many sweet things. He understands that bit. But the lung bit is a bit harder because I do not want to frighten him with scary words. COPD, female, 51–60 years, MRC dyspnoea score 3
Ways to increase self-motivation and engagement
Participants talked about the importance of incorporating strategies to increase motivation and engagement within the SELF-BREATHE intervention. One such suggestion was activity trackers and targets, which could serve as a potentially useful motivator to maintain engagement with this self-management intervention.
Maybe, a monitor thing so that you and see how you're doing. Chop it up, minutes, days and weeks. Do you know what I mean? I have to try and have little targets in my head of things I'm going to do, because otherwise everything seems too far away, if that makes sense. Like a progress tracker, it doesn't have to be a major thing like “you have visited this number of times” without it looking too judgemental, if that's possible. COPD, male, 51–60 years, MRC dyspnoea 3
Participants also described the importance of pairing trackers with appropriate education and guidance to help them build up gradually and set and achieve realistic goals. These were also described as vital to support individuals when commencing a training programme where targets can seem unattainable, thus building confidence to maximise chances of success.
Something to keep you going, like a little chart that you fill in. Something that you can map your progress would be good. Also, there should be some guidelines, you know “Don't overexert yourself, little baby steps”. Things like that, it's always good to have. Sometimes when you look at something and it looks like a mountain, you think, “There's no way I am climbing that mountain”. So, you don't even start, you don't even try. COPD, female, 51–60 years, MRC dyspnoea score 4
Another perceived benefit of the addition of self-monitoring was in the development and maintenance of positive behaviour change. Incorporating ways to log and monitor increases in activities would serve to build confidence and motivation to continue.
To develop the habit [self-monitoring], that really important with exercise. It's only after an amount of time that you think, “Actually, I'm doing these exercises and finding them easier”. But the first half a dozen times or so, you're thinking, “Well, this is such hard work”. When you turn that corner, you think, “Right, I am obviously making some headway here”. Do you know what I mean? It becomes self-perpetuating, and then you go, “Now, I can do 15 and I don't need to sit down to rest”. And then, you're able to do two lots of 15 without sitting down. It's that sort of thing, I am trying to say. It feels like you are achieving, you feel like things are getting better. If you feel that you're making headway, it encourages you. Cancer, male, 61–70 years, MRC dyspnoea score 3
Ways to improve breathing and physical functioning
As well as education about breathlessness itself, participants also described a preference for inclusion of specific exercises and interventions to improve their breathing and physical function within the SELF-BREATHE intervention. Frequently, participants talked about wanting breathing exercises to improve their chronic breathlessness self-management.
Breathing exercises and things like that, that are advantageous to you for your breathing. The dos and do nots. Cancer, male, 81–90 years, MRC dyspnoea score 3
Participants highlighted the value of instructional pre-recorded videos with a physiotherapist demonstrating breathing exercises. These not only helped to show exactly how to carry out the exercise, but acted as an ongoing source of support to refer to.
For example, if you go to physio, they tell you how to do things [exercises] and then by the time you get home you've forgotten it. Whereas, if you've got a video, you can always fall back on it and make sure you are doing it correctly. ILD, male, 71–80 years, MRC dyspnoea score 3
There were limitations described in relation to pre-recorded content, when compared to a face-to-face interaction with a professional, including not being able to ask questions, and limitations of internet connectivity. However, it was recognised that this would vary from individual to individual, and depend on how and why the resource was being accessed, which may change over time or due to specific needs.
I've watched pre-recorded things and it works. I think it's just different. If I have a preference, it is face to face. Then, sometimes with that [video call], suddenly, the connection goes a bit funny, they turn into robots, it becomes incredibly frustrating, and you lose half of it. So, it's “swings and roundabouts”. I think it's all “horses for courses” with that, personally. There are things where I want to be able to ask questions and make it a two-way thing and there are other times when you just want to watch stuff. COPD, male, 51–60 years, MRC dyspnoea 3
Critically, individuals shared the importance of consideration of context and environment in the choice of content for the SELF-BREATHE intervention. Specifically, any exercise interventions should be focused on what might be available to individuals within their own home.
A lot of people think you've got to go to the gym. You don't have to, you can do it [exercise] at home. You could do exercises by using household things, like bottles of water. Doing squats holding the back of a chair, two tins of beans in each arm. You know? COPD, female, 51–60 years, MRC dyspnoea score 4
In addition to exercises to improve physical function, breathing control exercises, such as pursed-lipped breathing, to be used during an acute on chronic breathlessness crisis, were considered a vital source of support to include within the intervention.
A good video, teaching how to control your breathing, because I pant like a dog [when breathless]. I was always told, if I get out of breath, to just lean on a trolley, if you were shopping, and blow through your mouth. I breathe in and then I sort of purse my lips and blow out [helpful]. COPD, female, 81–90 years, MRC dyspnoea 3
As well as breathing exercises, practical tips and suggestions of how to manage exacerbations were also welcomed by individuals. They shared the lived experience of breathlessness and the fear and anxiety associated with it. They described how simple approaches to breathlessness management, such as fan therapy or facial cooling, helped to improve their symptoms. This was highlighted as an important modality to include within the information and guidance of SELF-BREATHE.
My mother died of lung disease, she had fibrosis, so she had scarring all over her lungs and eventually it covered her lung and I mean, there's no way you can breathe after a while, and I know this is mind over matter, but do you know those little propeller handheld fans? I mean, this is just mind over matter for sure, but that feeling of air just on her face calmed her down, and when we had that hot weather, I felt [breathlessness] “Oh my God, I am going to suffocate in a minute”. It felt like someone was sat on my chest. I put the cold air blower [fan] on in my room that calmed me down. It's [the fan] not giving me any more oxygen, but I need that air flowing around me. It's calming, it's so calming, isn't it. COPD, male, 51–60 years, MRC dyspnoea score 2
Participants talked about the interaction between their physical symptoms and their psychological and social wellbeing. They talked specifically about how stress can cause breathlessness, but also the anxiety caused by breathlessness itself. Therefore, a holistic approach to breathlessness self-management and breathlessness triggers should be incorporated within the SELF-BREATHE intervention to help individuals recognise these relationships and ameliorate the sequelae.
The stress makes you breathless as well, so you need to learn to relax. I think we all need to be reminded sometimes how to breathe properly because it's easy to panic and just get into bad habits. What I think is also important, a lot of people, need to be taught how to cough properly because when you have COPD you do have stuff in your lungs which you need to get rid of. COPD, female, 61–70 years, MRC dyspnoea score 2
The relationship between and careful pairing of educational and exercise information was described. Participants talked about the need for clear, basic and factual information paired with motivation and encouragement to optimise the potential benefits of the SELF-BREATHE intervention.
People get turned off if there's too much information. They want the basics. So, the basic information of why you need to do these exercises, how it's going to help you, and encouragement to keep on doing it. COPD, female, 51–60 years, MRC dyspnoea score 4
Software cabability to personalise the content to make it meaningful to the user
Participants described the challenges of developing the content for the SELF-BREATHE intervention due to the variation of needs and preferences for the target population. Finding ways to individualise the intervention experience was recognised as an important factor in the design of the platform.
The whole of humanity has lungs, doesn't it (laughter) we are not all the same sort of people. COPD, male, 51–60 years, MRC dyspnoea 3
One potential approach to personalising the SELF-BREATHE experience described by participants was goal-setting. This was viewed as a way of enabling individuals to achieve meaningful improvements in their lives.
You need to have your own personal aim [personal goal], like I have said, it gives you the incentive to do something. If you have got nothing to aim for, you have got no incentive, then you don't do it. To be honest with you, with this disease, if you don't do anything, you just die, you have to fight it. Bronchiectasis, male, 51–60 years, MRC dyspnoea score 3
Moreover, some patients felt the option to have some element of human interaction would be beneficial to the SELF-BREATHE intervention. For example, the functionality to ask questions about the content of SELF-BREATHE, or get some feedback on goal attainment or progress with specific exercises, may help to personalise the intervention and increase motivation.
Just because it's online, it doesn't mean there can't be any face-to-face thing [human interaction]. I think maybe, every now and again, have almost like a mentor. Rather than a doctor, have a mentor sort of scheme, just so you can talk to someone about how it is going. It doesn't need to be every week, but every now and again, just to check in. Maybe? COPD, male, 51–60 years, MRC dyspnoea 3
Aesthetically designed content using a variety of communication methods
Participants talked about the importance of careful consideration of the design of the intervention, content, and modes of delivery to maximise uptake and motivation to continue using the intervention. It was highlighted that the educational content of the SELF-BREATHE intervention needs to use a positive framing approach and be accessible, entertaining and motivating, in line with other modern training applications.
The education should be “entertaining”, educational, not someone going, “And if you do this”…they should make it enjoyable. I mean, we live in an age of entertain me now…you don't see joggers without earphones, do you know what I mean…education me in an entertaining way…educate me in a way that doesn't sound like I'm being lectured at. COPD, male, 51–60 years, MRC dyspnoea score 3
This included the using varied modes of delivery to meet the preferences of different individuals, but also to improve the experience of SELF-BREATHE. Use of different modes of delivery would help it to be varied, enjoyable and informative to ensure optimal engagement and retention within the service.
Websites should make you feel good. When you look at a website, if it's difficult to read or it's difficult to understand or if's nasty looking, you know, it's boring, people won't take interest in it that deteriorates the information that they are trying to put over. COPD, female, 61–70 years, MRC dyspnoea score 3
The importance of video-based content was also highlighted to support those for whom written content may be less accessible.
I am dyslexic, so it is really hard. I do not really understand a lot of it [written information]. All the big, long words, I just do not get it. It has got to be layman's terms, where you can go, “Ah yes, I get that”. COPD, female, 51–60 years, MRC dyspnoea score 3
Lastly, participants talked about the importance of honesty and transparency throughout the SELF-BREATHE intervention, in the education and knowledge provided, but also in relation to the potential benefits of the intervention itself on illness and function. This was vital to give the intervention credibility, improve engagement and enable motivation to achieve meaningful and achievable improvements.
I like things to be honest. Do you understand? Sometimes, its like, “miracle cure”, blah-blah-blah, and I never believe any of it. I like, “This will make a 5% difference to your life, but a 5% difference to your life might do this”, rather than, “This will change your world”. Do you know what I mean? I am a grown up, and I think too often, people try and tell lies and I switch off. I have been a hustler myself and I can smell it, even on a video, I can smell it coming out of the computer screen. You know? COPD, male, 51–60 years, MRC dyspnoea 3
Discussion
Key findings
This is the first article to describe the content preferences of individuals living with chronic breathlessness due to advanced disease, with regards to an in-development online self-guided breathlessness supportive intervention (SELF-BREATHE). Individuals highlighted strong preferences for focused education, methods to increase self-motivation and engagement, interventions targeting breathing and physical function, software capability to personalise the content of SELF-BREATHE to make it more meaningful to the user and aesthetically designed content using various communication methods including written, video and audio content. Furthermore, they identified the need to address motivation as a key potential determinant of the success of SELF-BREATHE. These findings will be fundamental to the content development of SELF-BREATHE, and other online interventions for chronic breathlessness, to optimise acceptability and potential for benefit.
Relevance of findings
The content, structure and mode of delivery of digital health interventions are wide-ranging, and their potential effects are well documented. A systematic review and meta-analysis of internet-based interventions targeting health behaviour in noncommunicable disease (n=43 236) showed significant improvements in risk-related behaviour, such as physical activity (effect size 0.24, 95% CI 0.09–0.38), dietary behaviour (effect size 0.20, 95% CI 0.02–0.37) and alcohol consumption (effect size 0.14, 95% CI 0.00–0.27) [28]. Evidence-based digital interventions have the potential to improve patient self-management [29] at low cost [30].
Disease-specific digital supportive online interventions such as myCOPD are feasible and acceptable to patients, with preliminary results indicating that myCOPD is associated with improved inhaler technique and hospital admission rates [31, 32]. However, other disease-specific online interventions have reported challenges with recruiting, retaining and engaging patients [33]. It must be acknowledged that during the COVID-19 pandemic, online delivery of both the educational and exercise components of pulmonary rehabilitation have demonstrated positive outcomes [34]. In contrast to disease specific interventions, SELF-BREATHE is a transdiagnostic online supportive self-management intervention for individuals living with chronic breathlessness due to advanced disease, supporting individuals during daily life and at the point of breathlessness crisis.
There is a growing literature on digital rehabilitation and self-management interventions, yet most studies are limited to quantitative data. A perceived advantage of using qualitative interviews to identify content of SELF-BREATHE by individuals living with chronic breathlessness is that it draws on lived experience. According to Bandura [35], to achieve successful and sustainable self-management, “people have to learn to monitor their health behaviour and the circumstances under which it occurs”. Self- regulatory and self-efficacy theories for promoting self-management suggest that the greatest improvements in self-care of chronic conditions typically occur following some initial success in changing behaviour, i.e. mastery. A modest change, for example in breathlessness mastery, may generate a cascade of behaviour change leading to better health outcomes and health service utilisation. For instance, a patient may learn about acute on chronic breathlessness, and use new skills such as breathing control exercises and/or the handheld fan to manage their symptoms daily, leading to increased sense of mastery and confidence to self-manage breathlessness crisis, and fewer crises that result in emergency contacts with health services. In addition, the importance of methods to increase self-motivation, such as self-monitoring of symptoms and goal setting were highlighted as key to the success of SELF-BREATHE; therefore, evidence-based principles of behaviour change will be used to strengthen the design of SELF-BREATHE [28].
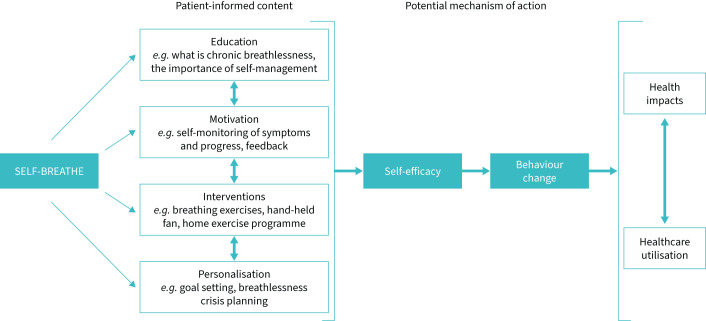
In the context of chronic lung disease, the lung disease itself is often irreversible. However, there are other extrinsic modifiable factors that can influence chronic breathlessness, such as fear avoidance, anxiety and exercise intolerance that increase breathlessness intensity [36]. Understanding and addressing patients’ health beliefs and behavioural responses to chronic breathlessness will be central to the development of SELF-BREATHE, which aligns with the MRC framework for developing and evaluating complex interventions [20] and the IDEAS framework for the development of digital behavioural change interventions [21]. In light of our findings, Leventhal's common-sense model of self-regulation provides a potential theoretical model to underpin the development of SELF-BREATHE (figure 1) [37]. Leventhal's common-sense model of self-regulation states that patient health beliefs (positive and negative) determine behavioural response and coping strategies in response to illness, consequently resulting in positive or negative outcomes [37]. Our findings highlight that people with chronic breathlessness often believe that getting breathless on exertion is harmful to them: “Part of me not doing anything [physical activity] was because I didn't know how it [my breathing] was going to react and my body. I was frightened to do anything in case I made things worse”, resulting in reduced physical activity and task avoidance.
FIGURE 1.
SELF-BREATHE is underpinned by Leventhal's common-sense model of self-regulation, where patient health beliefs (positive and negative) determine behavioural response and coping strategies in response to illness, consequently resulting in positive or negative outcomes. Interventional components of SELF-BREATHE target modifiable factors, i.e. patient health beliefs and behaviours to improve patient outcomes. Bi-directional arrows suggest the beneficial health impacts and reductions in healthcare utilisation.
This produces a “spiral of disability”, whereby physical inactivity creates deconditioning, reduced aerobic capacity and raised resting neural respiratory drive (NRD) [36, 38]. Increased NRD at rest further perpetuates dysfunctional breathing patterns, increases breathlessness awareness and results in a negative behavioural and emotional responses [36, 38]. SELF-BREATHE aims to improve a patient's self and response efficacy to chronic breathlessness (mastery), using self-guided interventions to address misconceptions and behavioural responses to chronic breathlessness.
It is important to recognise that the development and evaluation of any online health intervention is an iterative and inclusive process. With patients, clinicians and digital health experts working together to ensure that the intervention reflects patient healthcare needs and incorporates evolving digital technologies. Behavioural research indicates that actively engaging participants (decision-making) in their care can improve health outcomes [39] through factors such as improved autonomy [40], empowerment and mastery [41]. Patients described how persuasive design patterns, e.g. reminders and monitoring can be used in this digital intervention development to address the challenge of obtaining sustained user engagement and behaviour change among patients with chronic breathlessness [42].
Multimedia approaches, e.g. videos, written text and audio files were highlighted by patients to be important components of SELF-BREATHE, to facilitate participation and inclusion; a successful approach used within the charity sector to provide disease-specific information. However, information provision is only one facet of SELF-BREATHE. Patients highlighted the importance of symptom monitoring, active interventions such as breathing exercises and strengthening exercises that could be learnt at home in conjunction with the ability to personalise SELF-BREATHE through goal-setting (figure 1).
As per the IDEAS framework (phase 1: empathise with target users; phase 2: specify target behaviour) [21] and the new MRC framework for developing and evaluation complex interventions (phase 1: intervention identification/development) [20], these qualitative interviews provide a deep understanding of the specific needs, preferences and choices of patients regarding the content of SELF-BREATHE. These finding will inform innovative and creative solutions within SELF-BREATHE to meet the identified needs of potential users, e.g. interactive symptom monitoring and personalised breathlessness crisis planning. Motivation was identified by patients as a key modifiable behaviour with the potential to influence uptake and success of SELF-BREATHE. Entertainment, fun and enjoyment within the educational content of SELF-BREATHE were also specifically identified as key motivators to engagement [21]. This highlights the importance of including behavioural theory such as Capability–Opportunity–Motivation Behaviour based theory of change model (COM-B) [43] within the development of SELF-BREATHE to optimise motivation and engagement.
There is now a growing consensus that we need to optimise interventions to ensure acceptability to those delivering and receiving them [44]. Evidence shows that the acceptability of interventions impacts on their implementation, uptake, adherence and effectiveness [45]. The evaluation of a digital platforms such as SELF-BREATHE need to extend further than simply adhering to the digital intervention. It is vital that such an evaluation should explore patient acceptability, how they are used and actively incorporated into everyday life, e.g. though personal goal attainment or physical active monitoring through the use of wearable technology [29, 41].
Technologies can use different approaches to support engagement and motivation toward rehabilitation and self-management, including personalisation, tracking, monitoring, reminders and feedback. However, they should take into account the potential for demotivation due to overburdening caused by different devices and apps, privacy concerns, lack of trust, lack of interest and system usability [42]. If not properly accounted for, these issues can impact the acceptability of systems and become major hindrances to effective rehabilitation and self-management [42]. Our data highlight the importance of personal choice as to whether such functionality, i.e. text prompts/reminders are enabled by the individual.
Effective self-management requires patients to change (or sustain) behaviours. An individual's inclination to change behaviour depends on the extent to which they are motivated to change [46]. Our findings reflect the work of Tadas et al. [42], who highlight that motivation for action is driven by both individual factors, such as personal responsibility, emotions and goals, and external influences, such as friends, family, caregivers and health professionals. Although patients are in charge of their health-related behaviours, it is important that they are able to reflect on the stages of their illness, requirements for care and which decisions may need clinician support [47]. Self-management interventions such as SELF-BREATHE should aim to build upon and foster greater engagement with healthcare professionals/services rather than replace or be viewed as an alternative.
These data demonstrate the potential positive impact of SELF-BREATHE on individuals living with chronic breathlessness and advanced disease. For those who have internet access and are keen to engage in a self-management intervention, SELF-BREATHE is potentially an effective way of providing access to nonpharmacological interventions in the absence of face-to-face breathlessness-specific services, or for those for whom travel to the hospital is extremely challenging.
Strengths and limitations
We acknowledge that this is a small sample of the population, and regional, cultural and socioeconomic factors are also important to consider when developing, testing and implementing digital health interventions such as SELF-BREATHE. Following national COVID-19 guidance, semi-structured qualitative interviews were conducted over the telephone with patients. An advantage of this approach is that, potentially, a wider group of individuals can be reached than by face-to-face meetings alone. However, building rapport can be more challenging, especially in the absence of visual cues including body language and facial expressions. Nevertheless, this paper includes evocative, open, honest and rich quotes, not all positive findings, demonstrating that participants were comfortable and confident to speak openly, suggestive of a good rapport between interviewer and interviewee.
We did not use respondent validation of our findings due to COVID-19 challenges of face-to-face to contact with these clinically vulnerable patients during the COVID-19 pandemic. Moreover, some of the participants had died due to the severity of their illness by the time data analysis took place. However, our findings were reviewed by PPI members to add further depth to our interpretation.
Strengths of this study include an inclusive sample of patients with mixed diagnoses, ethnicity, degrees of breathlessness and online access. The study methodology combines the new MRC framework for developing and evaluating complex interventions and the IDEAS framework development [17]. Our findings provide an essential foundation for future digital intervention development and scaled research.
Conclusion
Individuals living with chronic breathlessness highlighted strong preferences for focused education, interventions targeting breathing and physical function, methods to increase self-motivation and software capability to personalise the content of SELF-BREATHE. Furthermore, they identified the need to address motivation as a key potential determinant of the success of SELF-BREATHE. These findings provide an essential foundation on which to develop the content of SELF-BREATHE, and potentially other patient facing interventions for chronic breathlessness, to optimise acceptability and effectiveness.
Footnotes
Provenance: Submitted article, peer reviewed.
The study is registered at www.clinicaltrials.gov with identifier number NCT04466020.
Author contributions: C.C. Reilly was the grant award holder (ICA-CL-2018-04-ST2-001) and chief investigator. Conception and design: C.C. Reilly, K. Bristowe, T. Chalder, I.J. Higginson and M. Maddocks. Data acquisition: C.C. Reilly and A. Roach. Data analysis and interpretation was led by C.C. Reilly, K. Bristowe and T. Chalder. All authors contributed to the integration of the interpretation of the data and provided critical revision of the manuscript for important intellectual content. All authors read and approved the final manuscript.
Conflict of interest: C.C. Reilly reports receiving support for the present manuscript from NIHR Clinical Lectureship ICA-CL-2018-04-ST2-001, which funds all aspects of this research; grants or contracts from King's Together: Multi and Interdisciplinary research scheme and Royal Brompton Hospital – King's Health Partnership Transformation funding, outside the submitted work.
Conflict of interest: K. Bristowe reports receiving grants or contracts from National Institute for Health Research, Medical Research Council, Health Education England, European Commission and Marie Curie, outside the submitted work.
Conflict of interest: A. Roach has nothing to disclose.
Conflict of interest: T. Chalder reports receiving support for the present manuscript via salary support from the National Institute for Health Research (NIHR) Mental Health Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London (KCL). The views expressed in this article are those of the authors and not necessarily those of the NIHR or the NHS.
Conflict of interest: M. Maddocks reports receiving grants or contracts from National Institute for Health Research (NIHR) Career Development Fellowship (CDF-2017–10-009), and NIHR Applied Research Collaboration South London (NIHR ARC South London) at King's College Hospital NHS Foundation Trust, outside the submitted work.
Conflict of interest: I.J. Higginson reports receiving grants or contracts from NIHR, UKRI, Cicely Saunders International and Marie Curie, outside the submitted work.
Support statement: A National Institute for Health and Care Research (NIHR) Clinical Lectureship (ICA-CL-2018-04-ST2-001) supports C.C. Reilly. M. Maddocks is supported by an NIHR Career Development Fellowship (CDF-2017-10-009). M. Maddocks and I.J. Higginson are supported by the NIHR Applied Research Collaboration South London (NIHR ARC South London) at King's College Hospital NHS Foundation Trust. I.J. Higginson is an NIHR Senior Investigator Emeritus. This publication presents independent research funded by the NIHR. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, NIHR or the Dept of Health and Social Care. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Kelly AM, Keijzers G, Klim S, et al. An observational study of dyspnea in emergency departments: the Asia, Australia, and New Zealand Dyspnea in Emergency Departments Study (AANZDEM). Acad Emerg Med 2017; 24: 328–336. doi: 10.1111/acem.13118 [DOI] [PubMed] [Google Scholar]
- 2.Hutchinson A, Pickering A, Williams P, et al. Breathlessness and presentation to the emergency department: a survey and clinical record review. BMC Pulm Med 2017; 17: 53. doi: 10.1186/s12890-017-0396-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Currow DC, Chang S, Ekström M, et al. Health service utilisation associated with chronic breathlessness: random population sample. ERJ Open Res 2021; 7: 00415-2021. doi: 10.1183/23120541.00415-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.D'Cruz RF, Waller MD, Perrin F, et al. Chest radiography is a poor predictor of respiratory symptoms and functional impairment in survivors of severe COVID-19 pneumonia. ERJ Open Res 2021; 7: 00655-2020. doi: 10.1183/23120541.00655-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cares-Marambio K, Montenegro-Jiménez Y, Torres-Castro R, et al. Prevalence of potential respiratory symptoms in survivors of hospital admission after coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Chron Respir Dis 2021; 18: 14799731211002240. doi: 10.1177/14799731211002240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2015; 2: CD003793. doi: 10.1002/14651858.CD003793.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stone PW, Hickman K, Steiner MC, et al. Predictors of pulmonary rehabilitation completion in the UK. ERJ Open Res 2021; 7: 00509-2020. doi: 10.1183/23120541.00509-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gendron LM, Nyberg A, Saey D, et al. Active mind-body movement therapies as an adjunct to or in comparison with pulmonary rehabilitation for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2018; 10: CD012290. doi: 10.1002/14651858.CD012290.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mularski RA, Munjas BA, Lorenz KA, et al. Randomized controlled trial of mindfulness-based therapy for dyspnea in chronic obstructive lung disease. J Altern Complement Med 2009; 15: 1083–1090. doi: 10.1089/acm.2009.0037 [DOI] [PubMed] [Google Scholar]
- 10.Yeh GY, Litrownik D, Wayne PM, et al. BEAM study (Breathing, Education, Awareness, Movement): a randomised controlled feasibility trial of tai chi exercise in patients with COPD. BMJ Open Respir Res 2020; 7: e000697. doi: 10.1136/bmjresp-2020-000697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brighton LJ, Miller S, Farquhar M, et al. Holistic services for people with advanced disease and chronic breathlessness: a systematic review and meta-analysis. Thorax 2019; 74: 270–281. doi: 10.1136/thoraxjnl-2018-211589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gysels M, Reilly CC, Jolley CJ, et al. Dignity through integrated symptom management: lessons from the breathlessness support service. J Pain Symptom Manage 2016; 52: 515–524. doi: 10.1016/j.jpainsymman.2016.04.010 [DOI] [PubMed] [Google Scholar]
- 13.Gysels M, Reilly CC, Jolley CJ, et al. How does a new breathlessness support service affect patients? Eur Respir J 2015; 46: 1515–1518. doi: 10.1183/13993003.00751-2015 [DOI] [PubMed] [Google Scholar]
- 14.Smallwood N, Moran T, Thompson M, et al. Integrated respiratory and palliative care leads to high levels of satisfaction: a survey of patients and carers. BMC Palliat Care 2019; 18: 7. doi: 10.1186/s12904-019-0390-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Global Digital Population as of January 2021. 2021.. www.statista.com/statistics/617136/digital-population-worldwide
- 16.Internet Usage in the United Kingdom (UK) – Statistics and Facts. 2021. www.statista.com/topics/3246/internet-usage-in-the-uk/
- 17.Polgar O, Patel S, Walsh JA, et al. Digital habits of pulmonary rehabilitation service-users following the COVID-19 pandemic. Chron Respir Dis 2022; 19: 14799731221075647. doi: 10.1177/14799731221075647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reilly CC, Bristowe K, Roach A, et al. “You can do it yourself and you can do it at your convenience”: internet accessibility and willingness of people with chronic breathlessness to use an internet-based breathlessness self-management intervention (SELF-BREATHE): during the COVID-19 pandemic. ERJ Open Res 2022; 8: 00557-2021. doi: 10.1183/23120541.00557-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bate P, Robert G. Experience-based design: from redesigning the system around the patient to co-designing services with the patient. Qual Saf Health Care 2006; 15: 307–310. doi: 10.1136/qshc.2005.016527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Skivington K, Matthews L, Simpson SA, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 2021; 374: n2061. doi: 10.1136/bmj.n2061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mummah SA, Robinson TN, King AC, et al. IDEAS (Integrate, Design, Assess, and Share): a framework and toolkit of strategies for the development of more effective digital interventions to change health behavior. J Med Internet Res 2016; 18: e317. doi: 10.2196/jmir.5927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Long KM, McDermott F, Meadows GN. Being pragmatic about healthcare complexity: our experiences applying complexity theory and pragmatism to health services research. BMC Med 2018; 16: 94. doi: 10.1186/s12916-018-1087-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19: 349–357. doi: 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 24.Johnson MJ, Yorke J, Hansen-Flaschen J, et al. Chronic breathlessness: re-thinking the symptom. Eur Respir J 2018; 51: 1800340. doi: 10.1183/13993003.02326-2017 [DOI] [PubMed] [Google Scholar]
- 25.Higginson IJ, Bausewein C, Reilly CC, et al. An integrated palliative and respiratory care service for patients with advanced disease and refractory breathlessness: a randomised controlled trial. Lancet Respir Med 2014; 2: 979–987. doi: 10.1016/S2213-2600(14)70226-7 [DOI] [PubMed] [Google Scholar]
- 26.Given LM. The Sage Encyclopedia of Qualitative Research Methods. Thousand Oaks, Sage Publications, 2008. [Google Scholar]
- 27.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005; 15: 1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 28.Webb TL, Joseph J, Yardley L, et al. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res 2010; 12: e4. doi: 10.2196/jmir.1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tighe SA, Ball K, Kensing F, et al. Toward a digital platform for the self-management of noncommunicable disease: systematic review of platform-like interventions. J Med Internet Res 2020; 22: e16774. doi: 10.2196/16774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Athilingam P, Jenkins B. Mobile phone apps to support heart failure self-care management: integrative review. JMIR Cardio 2018; 2: e10057. doi: 10.2196/10057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.North M, Bourne S, Green B, et al. A randomised controlled feasibility trial of E-health application supported care vs usual care after exacerbation of COPD: the RESCUE trial. NPJ Digit Med 2020; 3: 145. doi: 10.1038/s41746-020-00347-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Crooks MG, Elkes J, Storrar W, et al. Evidence generation for the clinical impact of myCOPD in patients with mild, moderate and newly diagnosed COPD: a randomised controlled trial. ERJ Open Res 2020; 6: 00460-2020. doi: 10.1183/23120541.00460-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Houchen-Wolloff L, Orme M, Barradell A, et al. Web-based self-management program (SPACE for COPD) for individuals hospitalized with an acute exacerbation of chronic obstructive pulmonary disease: nonrandomized feasibility trial of acceptability. JMIR Mhealth Uhealth 2021; 9: e21728. doi: 10.2196/21728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Michaelchuk W, Oliveira A, Marzolini S, et al. Design and delivery of home-based telehealth pulmonary rehabilitation programs in COPD: a systematic review and meta-analysis. Int J Med Inform 2022; 162: 104754. doi: 10.1016/j.ijmedinf.2022.104754 [DOI] [PubMed] [Google Scholar]
- 35.Bandura A. Health promotion by social cognitive means. Health Educ Behav 2004; 31: 143–164. doi: 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- 36.Jolley CJ, Moxham J. A physiological model of patient-reported breathlessness during daily activities in COPD. Eur Respir Rev 2009; 18: 66–79. doi: 10.1183/09059180.00000809 [DOI] [PubMed] [Google Scholar]
- 37.Leventhal H, Phillips LA, Burns E. The common-sense model of self-regulation (CSM): a dynamic framework for understanding illness self-management. J Behav Med 2016; 39: 935–946. doi: 10.1007/s10865-016-9782-2 [DOI] [PubMed] [Google Scholar]
- 38.Reilly CC, Ward K, Jolley CJ, et al. Neural respiratory drive, pulmonary mechanics and breathlessness in patients with cystic fibrosis. Thorax 2011; 66: 240–246. doi: 10.1136/thx.2010.142646 [DOI] [PubMed] [Google Scholar]
- 39.Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med 2012; 27: 520–526. doi: 10.1007/s11606-011-1931-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Clark RA, Conway A, Poulsen V, et al. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol 2015; 22: 35–74. doi: 10.1177/2047487313501093 [DOI] [PubMed] [Google Scholar]
- 41.Lupton D. The digitally engaged patient: self-monitoring and self-care in the digital health era. Social Theory Health 2013; 11: 256–270. doi: 10.1057/sth.2013.10 [DOI] [Google Scholar]
- 42.Tadas S, Coyle D. Barriers to and facilitators of technology in cardiac rehabilitation and self-management: systematic qualitative grounded theory review. J Med Internet Res 2020; 22: e18025. doi: 10.2196/18025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011; 6: 42. doi: 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O'Cathain A, Croot L, Duncan E, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open 2019; 9: e029954. doi: 10.1136/bmjopen-2019-029954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Haynes B. Can it work? Does it work? Is it worth it? The testing of healthcare interventions is evolving. BMJ 1999; 319: 652–653. doi: 10.1136/bmj.319.7211.652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000; 55: 68–78. doi: 10.1037/0003-066X.55.1.68 [DOI] [PubMed] [Google Scholar]
- 47.Nunes F, Verdezoto N, Fitzpatrick G, et al. Self-care technologies in HCI: trends, tensions, and opportunities. ACM Trans Comput-Hum Interact 2015; 22: 33. doi: 10.1145/2803173 [DOI] [Google Scholar]