Abstract
Background
We performed a meta-analysis to compare the efficacy and safety of the femoral neck system (FNS) with cannulated cancellous screws (CCSs) in treating femoral neck fractures (FNFs) in controlled clinical trials.
Methods
Eligible scientific articles published prior to September 2021 were retrieved from the PubMed, Web of Science, Springer, ScienceDirect and Cochrane Library databases. The statistical analysis was performed with RevMan 5.1.
Results
Seven retrospective studies met the inclusion criteria. Meta-analysis showed that there were significant differences in perioperative blood loss, the postoperative Harris score, healing time, fluoroscopy frequency, total complications, femoral head necrosis, femoral neck shortening and screw cutout. No significant differences were found regarding operation time, length of hospital stay or nonunion between the two groups.
Conclusion
Compared with CCSs, the FNS showed better clinical efficacy and fewer complications in treating FNFs. Due to the limited quality and data of the currently available evidence, more high-quality randomized controlled trials are needed.
Keywords: femoral neck fracture, internal fixation, femoral neck system, cannulated screw, meta-analysis
Introduction
Hip fracture, a common fracture in the geriatric population, is estimated to affect 2.6 million individuals worldwide in 2025. 1 The age-standardized incidence in Austria was 408/100 000 in 2018. 2 A Swedish register-based study reported that approximately 20% of patients with hip fractures died within 1 year of the fracture event. 3 The total costs for hospitalization showed a steep rise from US $60 million in 2012 to US $380 million in 2016. 4
Femoral neck fractures (FNFs) account for approximately half of hip fractures. 5 Several implants have been used to fix FNFs, such as cannulated cancellous screws (CCSs), 6 dynamic hip screws (DHSs), DHSs with anti-rotation screws, 7 DHSs with blades, 8 and proximal femoral locking plates or similar implants. The ideal implant is controversial; it should be minimally invasive and stable with few complications. CCSs are relatively minimally invasive and have been a common surgical intervention for FNFs in patients younger than 60 years old. 9 However, implant-related complications, such as screw cutout, femoral neck shortening and femoral head necrosis, have been noted. 10 DHSs provide more angular stability than fixation by multiple screws, with fewer clinical complications, especially for unstable FNFs. 11
Recently, combining the advantages of angular stability and minimally invasive surgery, a new implant femoral neck system (FNS, DePuy Synthes Products, USA) was developed for FNFs. The FNS has a shorter locking plate than DHSs. It also has a blunt-headed anti-rotation screw that can be locked to the screw bolt. 12 Several studies have compared the FNS with CCSs in treating FNFs. However, whether the FNS is superior to CCSs remains controversial. Therefore, we performed a meta-analysis with a large sample to compare the efficacy and safety of the FNS with CCSs in treating FNFs.
Materials and Methods
Search Strategy
This meta-analysis was conducted in accordance with the relevant preferred reported items for systematic reviews and meta-analyses (PRISMA) guidelines. Potentially relevant published academic articles, published from the inception of the electronic databases and searched to September 2021, were retrieved from the PubMed, Web of Science, Springer, ScienceDirect and Cochrane Library databases. The references of the identified articles were also searched for relevant articles. None of the studies were excluded due to language restrictions. The keywords used for the search were “femoral neck system,” “cannulated screws” and “femoral neck fracture.”
Inclusion Criteria
Studies were considered eligible for inclusion if they met the following criteria: (1) the sample included FNF patients treated with internal fixation; (2) the test group was treated with the FNS and the control group was treated with CCSs; (3) the clinical outcomes included operative time, perioperative blood loss, fluoroscopy frequency, healing time, the length of hospital stay, the postoperative functional score, the visual analog scale (VAS) score and/or complications; and (4) the study was a published comparative trial, including randomized controlled trials (RCTs) and non-RCTs. Two independent reviewers determined the suitability of the articles. A third reviewer resolved any disagreements.
Exclusion Criteria
We excluded articles that (1) were repeat published articles or articles with the same patients, contents, and results; (2) were case reports, theoretical studies, conference reports, systematic reviews, meta-analyses, expert comments, and economic analyses; and (3) evaluated outcomes that were not relevant.
Data Extraction
The data were extracted from the included articles by two independent reviewers. When necessary, the corresponding author of the study was contacted for details. The following information was extracted: The first author’s name, publication year, intervening measures, comparable baselines, and outcome measures. Other relevant parameters were also extracted from the individual studies.
Quality Assessment
The methodological quality of the RCTs was evaluated using a modification of the generic evaluation tool described in the Cochrane handbook for systematic reviews of interventions. 13 The methodological quality of the non-RCTs was assessed by the methodological index for nonrandomized studies (MINORS). 14
Data Analysis and Statistical Methods
RevMan 5.1 (The Cochrane Collaboration, Oxford, United Kingdom) was used to analyze the pooled data. The P values and I2 values from the standard chi-square test were used to estimate the level of heterogeneity. When I2 > 50%, a P < .1 was considered to indicate significant heterogeneity, and a random-effects model was used for the data analysis. When I2 < 50%, a P > .1 was considered to indicate nonsignificant heterogeneity. A fixed-effects model was used for the data analysis when nonsignificant heterogeneity was found. Subgroup analysis was performed when significant heterogeneity was found to investigate the sources of heterogeneity. The mean differences (MDs) and 95% confidence intervals (CIs) were determined for the continuous variables. The dichotomous data are expressed as the risk differences (RDs) and 95% CIs.
Results
Search Results
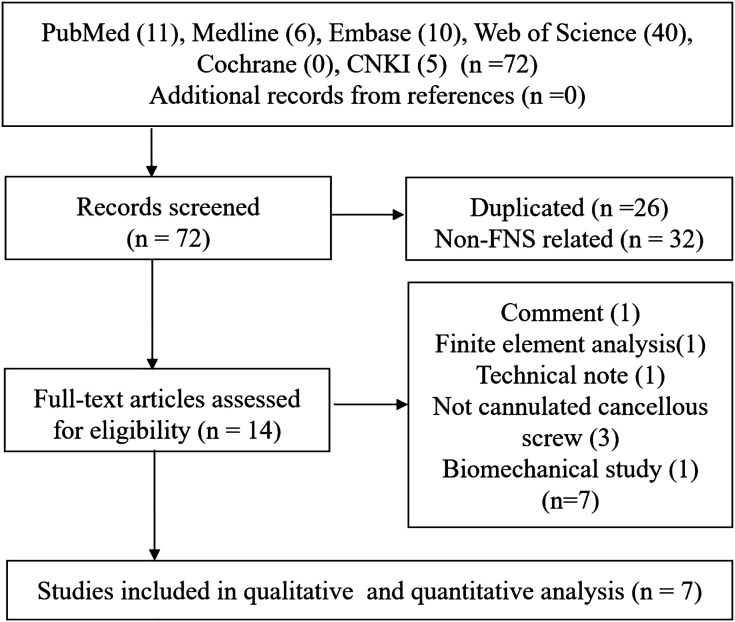
A total of 72 studies were identified as potentially relevant literature reports. There were no additional studies identified through other sources. Fifty-eight studies were excluded, including 26 with duplicate titles and 32 with non-FNS-related titles. After carefully scanning the titles, abstracts and full texts, several records were further excluded: One comment, one finite element analysis, one technical note, three studies that did not use CCSs, and one biomechanical study. Eventually, seven retrospective case–control studies15-21 were eligible for data extraction and meta-analysis. The search process is shown in Figure 1.
Figure 1.
Flowchart of the study selection process.
Characteristics of the Included Studies
The demographic characteristics and other details of the included studies are presented in Table 1. In each study, the baseline characteristics of the two groups were similar.
Table 1.
Characteristics of included studies.
| Author | Group | Cases (n) | Mean age (year) | Female (n, %) | Garden type (I, II, III, IV) | Pauwels type (I, II, III) | Follow-up (months) |
|---|---|---|---|---|---|---|---|
| Hu HJ | FNS | 20 | 50.45 ± 8.45 | 8 (40%) | 0,6,8,6 | 1,14,5 | 12 |
| CCS | 24 | 50.46 ± 9.26 | 10 (41.7%) | 4,6,7,7 | 4,13,7 | ||
| Tang YF | FNS | 47 | 57.4 ± 15.0 | 13 (22.7%) | 0,6,29,12 | 5,12,30 | 14-24 |
| CCS | 45 | 54.8 ± 11.7 | 8 (17.8%) | 0,5,31,9 | 6,10,29 | ||
| Vazquez O | FNS | 15 | 86.1 ± 4.6 | 13 (86.7%) | I, II | NR | 6 |
| CCS | 32 | 85 ± 6.6 | 28 (87.5%) | I, II | NR | ||
| Yan CP | FNS | 24 | 52 (47, 63) | 14 (58.3%) | 0,4,12,8 | 0,6,18 | 3-12 |
| CCS | 58 | 49 (47, 56) | 20 (34.5%) | 2,10,32,14 | 0,22,36 | 6-18 | |
| Yang JZ | FNS | 28 | 51 (45, 56) | 11 (39.3%) | 0,5,12,11 | 0,0,28 | 3-14 |
| CCS | 31 | 49 (39, 51) | 14 (45.2%) | 0,4,16,11 | 0,0,31 | ||
| Yang YJ | FNS | 15 | 42 | 6 (40%) | 2,4,11,2 | NR | 6 |
| CCS | 19 | 41.2 | 7 (36.8%) | 1,3,10,1 | NR | ||
| Zhou XQ | FNS | 30 | 54.53 ± 6.71 | 18 (60%) | NR | 0,0,30 | 10-22 |
| CCS | 30 | 53.14 ± 7.19 | 18 (60%) | NR | 0,0,51 |
FNS: Femoral neck system, CCS: Cannulated cancellous screw, NR: Not reported.
Risk of Bias Assessment
All included retrospective case–control studies were evaluated by the MINORS, and their scores ranged from 18 to 20 (Table 2). Due to the major limitations of retrospective studies, no prospective calculation of sample size or data collection was reported. Three studies followed patients for more than 12 months, while other studies followed some patients for less than 12 months. A short follow-up time may not be sufficient to identify femoral head necrosis or final union.
Table 2.
Quality assessment for non-randomized trials.
| Quality assessment for non-randomized trials | Hu HJ | Tang YF | Vazquez O | Yan CP | Yang JZ | Yang YJ | Zhou XQ |
|---|---|---|---|---|---|---|---|
| A clearly stated aim | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Inclusion of consecutive patients | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Prospective data collection | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Endpoints appropriate to the aim of the study | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Unbiased assessment of the study endpoint | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| A follow-up period appropriate to the aims of study | 2 | 2 | 0 | 0 | 0 | 0 | 2 |
| Less than 5% loss to follow-up | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Prospective calculation of the sample size | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| An adequate control group | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Contemporary groups | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Baseline equivalence of groups | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Adequate statistical analyses | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Total score | 20 | 20 | 18 | 18 | 18 | 18 | 20 |
Outcomes of the Meta-Analysis
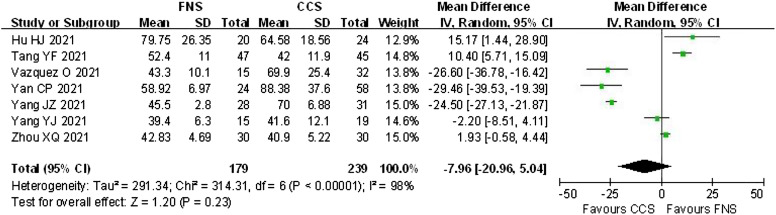
Operative Time
Operative time was recorded in 7 studies. The pooled results demonstrated that the operative time in the FNS group was similar to that in the CCS group (MD = −7.96, 95% CI: −20.96 to 5.04; P = .23; Figure 2).
Figure 2.
Forest plot showing operative time.
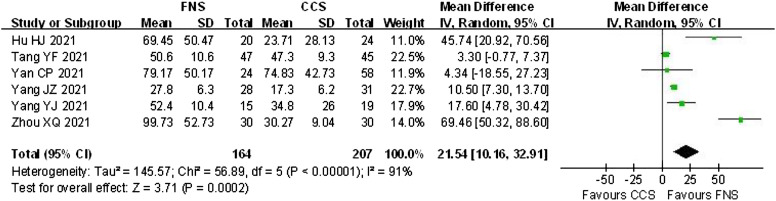
Perioperative Blood Loss
Perioperative blood loss was reported in 6 studies. The pooled results demonstrated that perioperative blood loss in the FNS group was higher than that in the CCS group (MD = 21.54, 95% CI: 10.16 to 32.91; P = .0002; Figure 3).
Figure 3.
Forest plot showing perioperative blood loss.
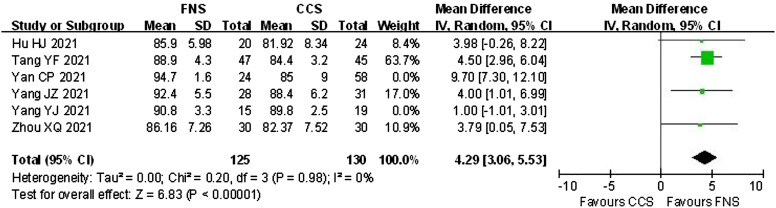
Postoperative Harris Score
The postoperative Harris score was recorded in 6 studies. The pooled results demonstrated that the postoperative Harris score in the FNS group was higher than that in the CCS group (MD = −4.52, 95% CI: 1.98 to 7.06; P = .0005; Figure 4).
Figure 4.
Forest plot showing the postoperative Harris score.
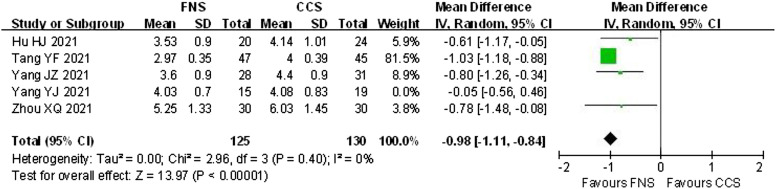
Healing Time
Healing time was documented in 5 studies. Among these studies, only the study by Hu et al. clearly reported the definition of healing time as “There was no obvious percussion pain in the hip joint or lower limbs on the operative side. X-ray or CT showed that the fracture line was blurred, and the original fracture end had continuous cancellous bone trabeculae passing through.” 15 The pooled results demonstrated that the healing time in the FNS group was shorter than that in the CCS group (MD = −.69, 95% CI: −1.06 to −.32; P = .0003; Figure 5).
Figure 5.
Forest plot showing healing time.
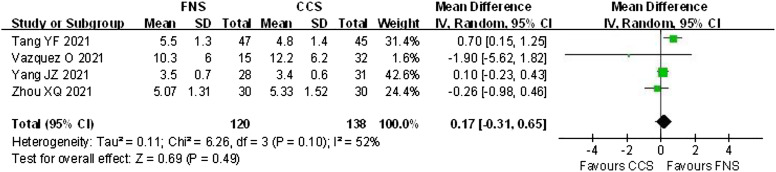
Length of Hospital Stay
The length of hospital stay was assessed in 5 studies. The pooled results demonstrated that the length of hospital stay in the FNS group was similar to that in the CCS group (MD = .17; 95% CI: −.31 to .65; P = .49; Figure 6).
Figure 6.
Forest plot showing the length of hospital stay.
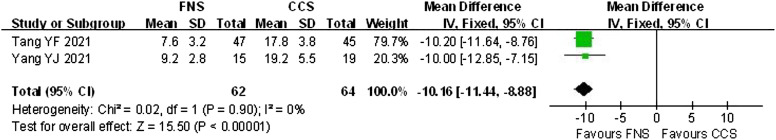
Fluoroscopy Frequency
Fluoroscopy frequency data were available in 2 studies. The pooled results demonstrated that the fluoroscopy frequency in the FNS group was higher than that in the CCS group (MD = 3.93, 95% CI: 3.02 to 4.87; P = .00001; Figure 7).
Figure 7.
Forest plot showing fluoroscopy frequency.
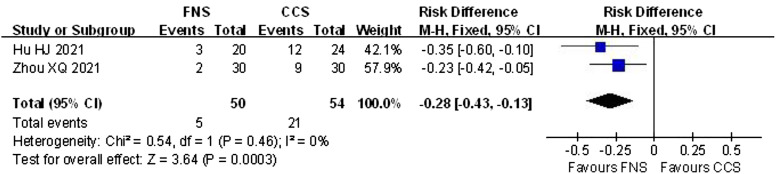
Total Complications
Total complications were reported in 2 studies. The pooled results demonstrated that the incidence of total complications in the FNS group was lower than that in the CCS group (RD = −.28; 95% CI: −.43 to .13; P = .0003; Figure 8).
Figure 8.
Forest plot showing total complications.
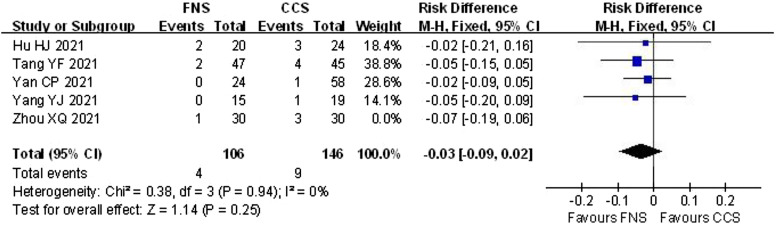
Nonunion
Nonunion was documented in 5 studies. Among these studies, only 2 clearly reported the definition of nonunion as occurring more than 9 months from fixation.18,20 The pooled results demonstrated that the incidence of nonunion in the FNS group was similar to that in the CCS group (RD = −.04; 95% CI: −.10 to .01; P = .13; Figure 9).
Figure 9.
Forest plot showing nonunion.
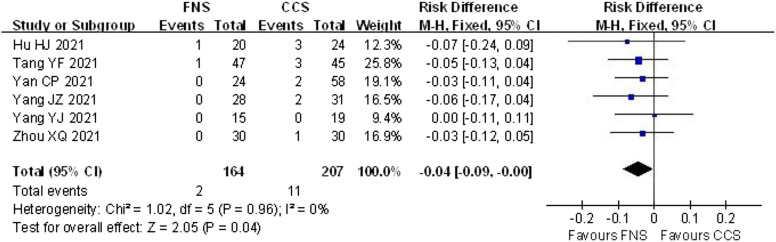
Femoral Head Necrosis
The incidence of femoral head necrosis was available in 6 studies. The pooled results demonstrated that the incidence of femoral head necrosis in the FNS group was lower than that in the CCS group (RD = −.04; 95% CI: −.09 to .00; P = .04; Figure 10).
Figure 10.
Forest plot showing femoral head necrosis.
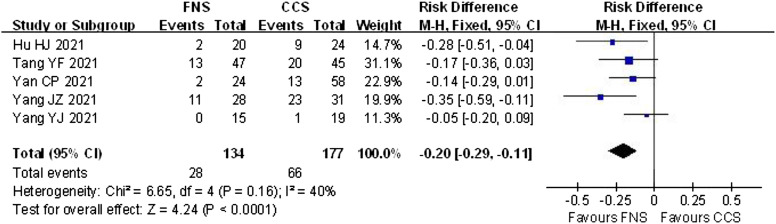
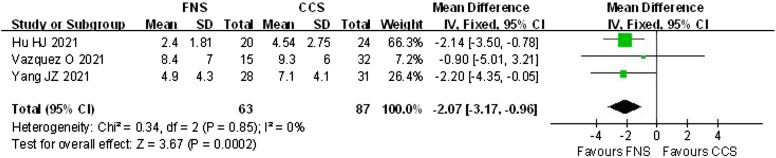
Femoral Neck Shortening
The incidence of femoral neck shortening was provided in 6 studies. The pooled results demonstrated that the incidence of femoral neck shortening in the FNS group was lower than that in the CCS group (RD = −.20; 95% CI: −.29 to −.11; P = .0001; Figure 11). The degree of femoral neck shortening was provided in three studies. The pooled results demonstrated that the degree of femoral neck shortening in the FNS group was lower than that in the CCS group (MD = −2.07; 95% CI: −3.17 to −.96; P = .0002; Figure 12).
Figure 11.
Forest plot showing the incidence of femoral neck shortening.
Figure 12.
Forest plot showing the degree of femoral neck shortening.
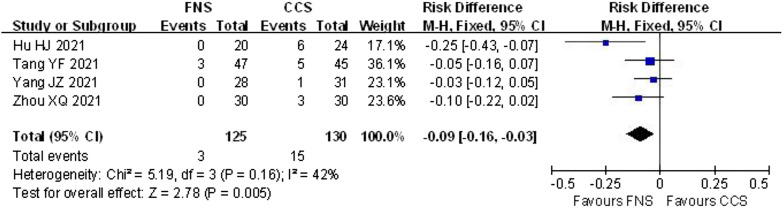
Screw Cutout
The incidence of screw cutout was reported in 4 studies. The pooled results demonstrated that the incidence of screw cutout in the FNS group was lower than that in the CCS group (RD = −.09; 95% CI: −.16 to −.03; P = .005; Figure 13).
Figure 13.
Forest plot showing screw cutout.
Discussion
Our meta-analysis included 7 studies. All included studies were retrospective, small and had short follow-ups. The purpose of our meta-analysis was to compare the efficacy and safety of the FNS and CCSs in treating FNFs. In the current study, we found that compared with CCSs, the FNS was associated with improved Harris Hip scores, an earlier time to union and fewer complications. To our knowledge, the present study is the first quantitative meta-analysis to evaluate the efficacy and safety of the FNS in treating FNFs.
The Harris score is the most commonly used tool for the evaluation of hip function. Four of the included studies showed better results in patients treated with the FNS. The current meta-analysis also confirmed better Harris scores for patients in the FNS group. In one previous meta-analysis comparing CCSs and DHSs, a similar Harris score was achieved. 22 Several factors that can influence function after FNF fixation include the condition of the patients, fracture displacement, the adequacy of internal fixation, and the quality of reduction. 22 The stronger stability of fixation with the FNS may allow early rehabilitation for patients to gain better function.12,23
Implant-related complications also have a negative effect on postoperative function. A previous study found that one-third of patients had shortening of more than 5 mm, which was negatively associated with hip function. 24 An association between femoral neck shortening and worse function has been reported in other studies.25-27 Femoral neck shortening was previously reported to be the primary reason for the difference in the Harris score between the FNS and CCS groups. 16 In a study including patients younger than 55 years, fixation with multiple cancellous screws led to moderate and severe shortening in 22.8% and 12.9% of the patients, respectively. 27 In the current study, moderate and severe shortening were reported in 28/134 (20.9%) patients in the FNS group and 66/177 (37.3%) patients in the CCS group. The lower incidence of femoral neck shortening in patients treated with the FNS may be due to its locking structure. Due to the disadvantageous effect of osteoporosis on bone structure and healing,28-31 the locking FNS may be suitable for patients with osteoporosis.32,33
Fracture healing is an important problem for FNF patients, and it was reported in 6 included studies. The healing time ranged from 2.97 to 6.03 months. Less healing time (.98 months) was required for patients treated by FNS fixation. The locking mechanism and anti-rotation effect of the FNS may provide a more stable construct. The dynamic compression between fracture fragments using the FNS also has a positive contribution to fracture healing. 20 In the current study, patients with fracture nonunion were not significantly different between the two groups. Sufficient follow-up (longer than 12 months) is necessary to observe the final healing progress for some patients with delayed union. 20
Necrosis of the femoral head is another serious complication of FNFs, which may lead to reoperation for some patients due to serious pain. In the FAITH trial, which included 557 patients treated with sliding hip screws and 551 patients treated with cancellous screws, the avascular necrosis rates were 9% and 5% in the sliding hip screw and CCS groups, respectively. Significantly more total hip arthroplasties were observed for patients treated with sliding hip screws than for those treated with CCSs (12% vs 7%, respectively). 34 In a systematic review of 1971 patients over 60 years old with stable FNFs, the incidence of osteonecrosis was 5.3%. 35 Another meta-analysis reported that the necrosis rates in the DHS and CCS groups were 10.3% and 7.9%, respectively. 22 Similarly, in the current study, the necrosis rate was 5.3% for patients treated with CCSs. In contrast, only two patients treated with the FNS were reported to develop necrosis in two studies, with a pooled necrosis rate of 1.2% (2 out of 164). The possible reasons for the significantly lower necrosis rate in the FNS group include the stability of the fracture fragments after FNS treatment, 36 a greater ability to maintain good reduction, 37 and a small implant volume that does not interfere with revascularization. 20 In a recent study, the mean time to necrosis was 1.4 ± .7 years after surgery. 37 This length of time may be not long enough to make a confirming conclusion for the necrosis rate for different groups. Future investigation should be performed to confirm the advantages of reduced necrosis rates in patients treated by the FNS.
Less blood loss, a shorter operative time and early postoperative rehabilitation could be favorable to decrease complications and increase hip function for FNF patients. Vazquez O et al. reported outcomes after FNF fixation, and the FNS group showed a shorter operative time than the CCS and DHS groups. 17 In the present analysis, the pooled result showed a similar operative time between FNS and CCS fixation. The specific design of the FNS requires minimally invasive exposure for it to be placed. Although more blood loss was noticed for the FNS group in the integrated analysis, the difference in the amount (21.5 mL) is acceptable in the clinic. The simple design of the FNS may contribute to the lower fluoroscopy frequency during the operation. Generally, on behalf of possible early postoperative rehabilitation after fixation by the FNS, it should be a good choice for unstable FNF patients.
Several potential limitations of this review should be noted: (1) No RCTs and only 7 non-RCTs were included, and the sample size of all the studies was relatively small; (2) the suboptimal methodological quality of the included studies and their insufficient outcomes may weaken our analysis; and (3) the FNS is a newly designed implant for FNFs, with the first biomechanical study published in 2017, and all included studies were published in 2021 and had a short follow-up period, which may lead to the underestimation of complications.
Conclusion
This meta-analysis of the current literature indicates that the FNS shows better clinical efficacy and fewer complications than CCSs in treating FNFs. Due to the limited quality and data of the currently available evidence, more high-quality randomized controlled trials are needed.
Supplemental Material
Supplemental Material for Comparison Between Femoral Neck Systems and Cannulated Cancellous Screws in Treating Femoral Neck Fractures: A Meta-Analysis by Peng Tian, Lan Kuang, Zhi-jun Li, Gui-jun Xu, and Xin Fu in Geriatric Orthopaedic Surgery & Rehabilitation
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Tianjin Health Science and Technology Project (RC20120 and ZC20096).
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
References
- 1.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7(5):407-413. [DOI] [PubMed] [Google Scholar]
- 2.Dimai HP, Reichardt B, Zitt E, et al. Thirty years of hip fracture incidence in Austria: is the worst over? Osteoporos Int. 2021;33:97-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meyer AC, Ek S, Drefahl S, Ahlbom A, Hedstrom M, Modig K. Trends in hip fracture incidence, recurrence, and survival by education and comorbidity: A Swedish register-based study. Epidemiology. 2021;32(3):425-433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang C, Feng J, Wang S, et al. Incidence of and trends in hip fracture among adults in urban China: A nationwide retrospective cohort study. PLoS Med. 2020;17(8):e1003180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Florschutz AV, Langford JR, Haidukewych GJ, Koval KJ. Femoral neck fractures: Current management. J Orthop Trauma. 2015;29(3):121-129. [DOI] [PubMed] [Google Scholar]
- 6.Nousiainen MT, Omoto DM, Zingg PO, Weil YA, Mardam-Bey SW, Eward WC. Training femoral neck screw insertion skills to surgical trainees: computer-assisted surgery versus conventional fluoroscopic technique. J Orthop Trauma. 2013;27(2):87-92. [DOI] [PubMed] [Google Scholar]
- 7.Makki D, Mohamed AM, Gadiyar R, Patterson M. Addition of an anti-rotation screw to the dynamic hip screw for femoral neck fractures. Orthopedics. 2013;36(7):e865-e868. [DOI] [PubMed] [Google Scholar]
- 8.Zhao W, Liu L. Effect of dynamic hip system blade on the treatment of femoral neck fractures in elderly patients with osteoporosis. Chin J Traumatol. 2014;17(5):275-278. [PubMed] [Google Scholar]
- 9.Huang TW, Hsu WH, Peng KT, Lee CY. Effect of integrity of the posterior cortex in displaced femoral neck fractures on outcome after surgical fixation in young adults. Injury. 2011;42(2):217-222. [DOI] [PubMed] [Google Scholar]
- 10.Ju FX, Hou RX, Xiong J, Shi H, Chen Y, Wang J. Outcomes of femoral neck fractures treated with cannulated internal fixation in elderly patients: A long-term follow-up study. Orthop Surg. 2020;12(3):809-818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siavashi B, Aalirezaei A, Moosavi M, Golbakhsh MR, Savadkoohi D, Zehtab MJ. A comparative study between multiple cannulated screws and dynamic hip screw for fixation of femoral neck fracture in adults. Int Orthop. 2015;39(10):2069-2071. [DOI] [PubMed] [Google Scholar]
- 12.Stoffel K, Zderic I, Gras F, et al. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: A comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma. 2017;31(3):131-137. [DOI] [PubMed] [Google Scholar]
- 13.Handoll HH, Gillespie WJ, Gillespie LD, Madhok R. The cochrane collaboration: A leading role in producing reliable evidence to inform healthcare decisions in musculoskeletal trauma and disorders. Indian J Orthop. 2008;42(3):247-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-716. [DOI] [PubMed] [Google Scholar]
- 15.Hu H, Cheng J, Feng M, Gao Z, Wu J, Lu S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res. 2021;16(1):370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tang Y, Zhang Z, Wang L, Xiong W, Fang Q, Wang G. Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res. 2021;16(1):504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vazquez O, Gamulin A, Hannouche D, Belaieff W. Osteosynthesis of non-displaced femoral neck fractures in the elderly population using the femoral neck system (FNS): Short-term clinical and radiological outcomes. J Orthop Surg Res. 2021;16(1):477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yan C, Wang X, Xiang C, et al. Comparison of effectiveness of femoral neck system and cannulate compression screw in treatment of femoral neck fracture in young and middle-aged patients. Chin J Reparative Reconstr Surg. 2021;35(10):1286-1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang Y, Ma T, Zhang X, Luo X, Fan T, Wang Y. Short-term effectiveness of femoral neck system in the treatment of femoral neck fracture. Chin J Reparative Reconstr Surg. 2021;35(5):539-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou XQ, Li ZQ, Xu RJ, et al. Comparison of early clinical results for femoral neck system and cannulated screws in the treatment of unstable femoral neck fractures. Orthop Surg. 2021. 13, 1802-1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang J, Zhou X, Li L, et al. Comparison of femoral neck system and inverted triangle cannulated screws fixations in treatment of Pauwels typle Ⅲ femoral neck fractures. Chin J Reparative Reconstr Surg. 2021;35(09):1111-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li L, Zhao X, Yang X, Tang X, Liu M. Dynamic hip screws versus cannulated screws for femoral neck fractures: A systematic review and meta-analysis. J Orthop Surg Res. 2020;15(1):352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schopper C, Zderic I, Menze J, et al. Higher stability and more predictive fixation with the femoral neck system versus Hansson Pins in femoral neck fractures Pauwels II. J Orthop Translat. 2020;24:88-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Felton J, Slobogean GP, Jackson SS, et al. Femoral neck shortening after hip fracture fixation is associated with inferior hip function: Results from the FAITH trial. J Orthop Trauma. 2019;33(10):487-496. [DOI] [PubMed] [Google Scholar]
- 25.Zielinski SM, Keijsers NL, Praet SF, et al. Femoral neck shortening after internal fixation of a femoral neck fracture. Orthopedics. 2013;36(7):e849-e858. [DOI] [PubMed] [Google Scholar]
- 26.Weil YA, Khoury A, Zuaiter I, Safran O, Liebergall M, Mosheiff R. Femoral neck shortening and varus collapse after navigated fixation of intracapsular femoral neck fractures. J Orthop Trauma. 2012;26(1):19-23. [DOI] [PubMed] [Google Scholar]
- 27.Slobogean GP, Stockton DJ, Zeng BF, Wang D, Ma B, Pollak AN. Femoral neck shortening in adult patients under the age of 55 years is associated with worse functional outcomes: Analysis of the prospective multi-center study of hip fracture outcomes in China (SHOC). Injury. 2017;48(8):1837-1842. [DOI] [PubMed] [Google Scholar]
- 28.Goldhahn J, Suhm N, Goldhahn S, Blauth M, Hanson B. Influence of osteoporosis on fracture fixation--A systematic literature review. Osteoporos Int. 2008;19(6):761-772. [DOI] [PubMed] [Google Scholar]
- 29.Nikolaou VS, Efstathopoulos N, Kontakis G, Kanakaris NK, Giannoudis PV. The influence of osteoporosis in femoral fracture healing time. Injury. 2009;40(6):663-668. [DOI] [PubMed] [Google Scholar]
- 30.Goldhahn S, Kralinger F, Rikli D, Marent M, Goldhahn J. Does osteoporosis increase complication risk in surgical fracture treatment? A protocol combining new endpoints for two prospective multicentre open cohort studies. BMC Muscoskel Disord. 2010;11:256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Konstantinidis L, Papaioannou C, Blanke P, Hirschmuller A, Sudkamp NP, Helwig P. Failure after osteosynthesis of trochanteric fractures. Where is the limit of osteoporosis? Osteoporos Int. 2013;24(10):2701-2706. [DOI] [PubMed] [Google Scholar]
- 32.Min BW, Lee KJ, Bae KC, Lee SW, Lee SJ, Choi JH. Result of internal fixation for stable femoral neck fractures in elderly patients. Hip Pelvis. 2016;28(1):43-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sung YB, Jung EY, Kim KI, Kim SY. Risk factors for neck shortening in patients with valgus impacted femoral neck fractures treated with three parallel screws: Is bone density an affecting factor? Hip Pelvis. 2017;29(4):277-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hanusch BC, Zomar M, Lee J. Fracture fixation in the operative management of hip fractures (FAITH): An international, multicentre, randomised controlled trial. Lancet. 2017;389(10078):1519-1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim SJ, Park HS, Lee DW. Complications after internal screw fixation of nondisplaced femoral neck fractures in elderly patients: A systematic review. Acta Orthop Traumatol Turcica. 2020;54(3):337-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dargan DP, Callachand F, Diamond OJ, Connolly CK. Three-year outcomes of intracapsular femoral neck fractures fixed with sliding hip screws in adults aged under sixty-five years. Injury. 2016;47(11):2495-2500. [DOI] [PubMed] [Google Scholar]
- 37.Wang Y, Ma JX, Yin T, et al. Correlation between reduction quality of femoral neck fracture and femoral head necrosis based on biomechanics. Orthop Surg. 2019;11(2):318-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Comparison Between Femoral Neck Systems and Cannulated Cancellous Screws in Treating Femoral Neck Fractures: A Meta-Analysis by Peng Tian, Lan Kuang, Zhi-jun Li, Gui-jun Xu, and Xin Fu in Geriatric Orthopaedic Surgery & Rehabilitation