Abstract
Background:
Anxiety disorders are highly prevalent and cause significant distress, disability, and cost. Medication adverse effects and interactions increase in mid-life and late-life, highlighting the need for effective non-pharmacological interventions.
Objectives:
We aimed to evaluate the extent of evidence supporting exercise interventions for anxiety and subthreshold anxiety disorders in mid-life and late-life.
Design:
Systematic review.
Data Sources and Methods:
We searched MEDLINE, PsycINFO, Embase, Emcare, Ovid Nursing, CINAHL Plus, Cochrane Library, Health Collection, Humanities & Social Sciences Collection, and https://clinicaltrials.gov databases for trials published January 1994–May 2019. Randomised controlled trials of exercise interventions involving aerobic exercise or resistance training for adults aged 40 years and above with anxiety or subthreshold anxiety disorders in residential or health settings were identified. The primary outcome was change in anxiety. We excluded trials including participants aged below 40 years, participants with diagnosis of separation anxiety, selective mutism, obsessive-compulsive disorder, acute stress disorder and post-traumatic stress disorder, and head-to-head comparisons of interventions. Trial quality was assessed using the Cochrane Risk of Bias Tool and evidence synthesised in narrative form.
Results:
Four trials totalling 132 participants met inclusion criteria, although some had methodological limitations. Interventions included a home-based resistance training intervention, supervised group-based aerobic intervention, Tai Chi intervention, and supervised group-based aerobic and strength intervention. Three trials included late-life participants and the fourth mid-life. Three trials demonstrated greater reductions in anxiety in the intervention group compared with control. The fourth trial showed pre–post reductions in anxiety in both groups, with between-group difference not reaching statistical significance.
Conclusion:
There is limited supportive evidence suggesting that exercise interventions have potential to be effective, feasible and safe non-pharmacological interventions for anxiety and subthreshold anxiety disorders in mid-life and late-life. The heterogeneity, limited number and high risk of bias of some trials meant that we were not able to conduct a meta-analysis. Tailoring of interventions may improve uptake and reduce dropout. The paucity of research in this area with only four included trials demonstrates the urgent need for future and larger trials to provide proof of concept, data about effective types and doses of exercise interventions, and guidance to community, clinical, and public health services.
Keywords: anxiety, exercise, physical activity, mid and late life, randomised clinical trials
Introduction
Anxiety disorders are the most prevalent type of mental health condition, with a lifetime prevalence of 28.8% in the United States. 1 The point prevalence of anxiety disorders globally is 10.4% with geographical variation: Euro/Anglo 10.4%, Indo/Asia 5.3%, African 5.3%, Central/Eastern Europe 7.2%, North Africa/Middle East 8.0% and Ibero/Latin 7.3%. 2 They are also highly prevalent in older adults. There have been less prevalence studies in late-life anxiety with a review suggesting a reduction in prevalence in older age. 2 However, studies which adapted diagnostic tools to the older adult population, such as the large MentDis ICF65+ study, found a 12-month prevalence of 17.2% for anxiety disorders in community dwelling adults aged 65–84 years in Europe and Israel. 3 Point prevalence of anxiety disorders in older adults varied geographically, for example, in China 0.1–0.2%, India 0.8–3.0% and Peru 2.2–9.6% (rural–urban figures, respectively, for each country). 4
Subthreshold anxiety disorders are those that do not reach the threshold of diagnostic criteria, may have comparable burden of disease to the threshold disorder, have increased risk of developing threshold disorder, and are even more prevalent than anxiety disorders.5,6 There is no consensus definition for subthreshold anxiety disorders, although usually the definition involves relaxing one or more of the diagnostic criteria. 6 Despite the lack of a consensus definition, the significant impact of these conditions means that they warrant research attention. The COVID-19 pandemic has been associated with a detrimental impact on mental health, including high rates of anxiety. 7 Late-life anxiety disorders have adverse effects on quality of life, similar to depression, and more than type II diabetes or recent myocardial infarction. 8 They are also associated with functional impairment, physical disability, excess mortality and increased healthcare costs.9 –11 A systematic review and meta-analysis found that direct costs of anxiety disorders accounted for 2.08% of healthcare costs and 0.22% of GDP, while indirect costs accounted for 0.23% of GDP; and generalised anxiety disorder was the most costly type of anxiety disorder. 12 Furthermore, there is increasing evidence to suggest that anxiety and subthreshold anxiety disorders may be a risk factor for developing dementia, but further evidence is required to confirm this link.13 –17
Despite the high prevalence of late-life anxiety disorders and their significant consequences, these conditions have received much less research attention when compared with other conditions such as late-life depression. 13 Clinical practice guidelines for anxiety disorders, such as those of the Royal Australian and New Zealand College of Psychiatrists, discuss the higher likelihood of medication interactions and adverse events of pharmacological therapy in older adults compared with younger adults. 18 Given the safety issues associated with pharmacological therapies, there should also be a focus on non-pharmacological therapies for anxiety disorders, particularly in older age groups. 19 In addition, psychological therapies may become more challenging and less effective with cognitive impairment, which increases in prevalence with age.
Exercise interventions are non-pharmacological therapies that have myriad benefits for physical and cognitive health, as well as longevity. 20 There is also emerging evidence for the benefits of exercise for anxiety across the adult lifespan, but less so in mid-life and late-life. A systematic review and meta-analysis of exercise interventions for people across the adult lifespan with anxiety and stress-related disorders identified only six randomised controlled trials with 262 participants who met criteria for inclusion. 21 The review found that the included aerobic exercise interventions reduced anxiety symptoms relative to control conditions with a moderate effect size with standardised mean difference of −0.582. 21 Two of the included trials involved participants with Post-Traumatic Stress Disorder which is no longer classified as an anxiety disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). 22 The mean age of participants in the included trials ranged from 21 to 47 years. Another systematic review and meta-analysis that included anxiety disorders as well as those with clinically elevated anxiety levels identified 15 randomised controlled trials with 675 participants. 23 This review found that aerobic exercise was effective in reducing anxiety compared with control conditions with a similar effect size with standardised mean difference of −0.41. 23
There is very limited research into exercise interventions for anxiety in older adults specifically. Two reviews addressed this question in relation to anxiety symptoms but specifically excluded those who had anxiety disorders.24,25 One systematic review of exercise interventions for anxiety symptoms in older adults identified five randomised controlled trials, two cross-sectional studies and one cohort study, but the authors were unable to conduct a meta-analysis due to the methodological heterogeneity between studies. 25 Another systematic review included a broader age range of mid-life and late-life (defined as 40 years and older) female participants, and identified 10 randomised controlled trials with 1463 participants for inclusion in meta-analysis. 24 The authors found that exercise interventions of 12–16 weeks’ duration were effective in reducing anxiety compared with control conditions with a similar effect size of −0.42; however, they found that interventions of 6–14 months’ duration were not effective. 24
While reviews have included trials conducted in younger adults as well as those conducted with older adults with anxiety symptoms, but not disorders, there is a clear gap in the evidence base relating to exercise interventions for anxiety and subthreshold anxiety disorders in mid-life and late-life adults. Given the importance of non-pharmacological therapies for anxiety and subthreshold anxiety disorders in mid-life and late-life adults, and the emerging evidence for exercise interventions for anxiety, a review of this area is needed to guide clinicians and researchers. Furthermore, mid-life is increasingly recognised as an important time for preventive health interventions such as dementia risk reduction, 26 and hence a critical life stage during which to target interventions. The aim of this systematic review was to evaluate the extent and quality of the available randomised controlled trial evidence relating to exercise interventions for anxiety in mid-life and late-life adults with anxiety disorders and subthreshold anxiety disorders.
Methods
Search strategy and selection criteria
This systematic review was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 27 A protocol was registered in the International Prospective Register of Systematic Reviews, PROSPERO (CRD42019135403).
Publications were identified through a systematic search of nine databases: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Daily and Versions(R) 1946 to 15 May 2019; PsycINFO 1806 to May week 2 2019 (Ovid); Embase 1974 to 15 May 2019 (Ovid); Ovid Emcare 1995 to 2019 week 19; Ovid Nursing Database 1946 to May week 2 2019; CINAHL Plus with Full Text (EBSCOhost); Cochrane Library; Health Collection, Humanities & Social Sciences Collection (Informit); and https://clinicaltrials.gov.
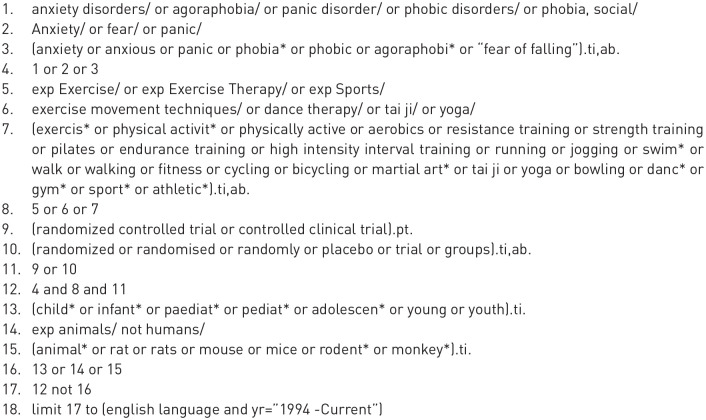
Search strategies were developed by a medical research librarian (HW) in consultation with the review team. Strategies combined the general concepts of anxiety AND exercise AND randomised controlled trials, using a combination of text words and subject headings appropriate to each database. Animal and paediatric studies were removed. Results were limited to English language and publications from 1994 onwards, given that DSM-IV 28 was published in 1994, and the review aimed to focus on relatively contemporary diagnostic criteria. An initial strategy was developed for Medline (Figure 1) and adapted for other databases (see supplementary material). All searches were carried out between 16 and 23 May 2019. We consulted topic experts within our team and did not conduct a manual search.
Figure 1.
Search strategy for Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Daily and Versions(R) 1946 to 15 May 2019.
Search results were exported to Endnote bibliographic management software and the duplicates removed. Records were screened by publication type, and dissertations, conference abstracts, conference papers, letters, notes, comments, and book reviews were excluded. All remaining records were loaded into Covidence systematic review software 29 for screening on title and abstract, and then full text.
The inclusion and exclusion criteria for the title and abstract screen and full-text screen were the same. The criteria for inclusion in this review were:
Adults aged 40 years and above (mid-life and late-life).
Diagnosis of anxiety disorder as defined by DSM-5 or DSM-IV or diagnosis of subthreshold anxiety disorder. In the absence of a consensus definition of subthreshold anxiety disorder, this was defined as the presence of anxiety symptoms not fulfilling diagnostic criteria for an anxiety disorder or not scoring above the relevant cut-point on a validated anxiety symptom scale.
Exercise interventions involving aerobic exercise or resistance training with definitions below. Exercise is defined as ‘a subset of physical activity that is planned, structured, and repetitive and has as a final or an intermediate objective the improvement or maintenance of physical fitness’. 30 Aerobic exercise ‘refers to exercises in which the body’s large muscles move in a rhythmic manner for sustained periods’. 31 ‘This form of activity uses large muscle groups such as arms and legs, and increases heart rate and breathing. Examples of aerobic activity include walking, running, swimming, cycling and dancing and many sports’. 32 Progressive resistance training is defined as ‘applying a load to a movement to increase strength and/or power, and regularly adjusting this load as muscle adaptation occurs’. 33
Randomised Controlled Trial with inactive control conditions such as a wait-list or treatment as usual. Treatment as usual could consist of active treatments such as cognitive-behavioural therapy or pharmacotherapy as long as this was consistent across the intervention and control groups. This was the case in one included trial. 34
The randomised controlled trial includes the measurement of change in anxiety score using a validated scale.
Exclusion criteria included:
Samples with participants aged below 40 years.
DSM-5 anxiety diagnoses of Separation Anxiety and Selective Mutism as these are mainly disorders affecting children.
DSM-IV anxiety diagnoses of Obsessive-Compulsive Disorder, Acute Stress Disorder, and Post-Traumatic Stress Disorder as these conditions are no longer classified as anxiety disorders in DSM-5.
Head-to-head comparison trials with interventions that have evidence of efficacy, such as cognitive-behavioural therapy or pharmacotherapy, were excluded. These trials were excluded as the aim of the review was to investigate the efficacy of exercise interventions compared with placebo or treatment as usual, as opposed to a comparison with established effective interventions. Trials with ‘control’ interventions, such as stretching or health education, were not excluded.
Each record was independently screened on title and abstract by two reviewers (TWHC plus HW or SK or SB) in accordance with the inclusion and exclusion criteria. Where consensus was not reached, an additional reviewer (EC) resolved the conflict. The full-text screening was undertaken independently by two reviewers (TWHC and SK) with an additional reviewer (EC) to resolve any conflicts where consensus could not be reached. Data extraction and risk of bias assessment were then performed independently by two reviewers (TWHC and SK) who reached consensus.
Data analysis
Data extraction included:
Study design details.
Sample – number of participants, demographic and baseline characteristics, anxiety medication use.
Exercise intervention – length of trial, type, duration, intensity, and frequency of exercise.
Control conditions – ‘control’ interventions such as stretching or health education, waiting list or treatment as usual.
Methodological factors – including the diagnostic criteria and the scales used to measure anxiety symptoms, information to assess risk of bias.
Outcomes – primary (extraction of the mean and standard deviation from pre- and post-test anxiety symptom rating scales for both control and exercise groups) and secondary measures (such as physical activity/fitness, quality of life, cognition, depression, and adverse events if available).
Study adherence and discontinuation rates in both conditions.
The risk of bias (quality) assessment was undertaken using the Cochrane Risk of Bias Tool for Randomised Controlled Trials Version 1. 35 This tool collects information on the following domains to facilitate the assessment of bias: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other sources of bias. The characteristics of the identified studies are described below.
It was decided that a meta-analysis would be conducted if there are sufficient trials without excessive heterogeneity in participant characteristics and intervention used, and significant risk of bias. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
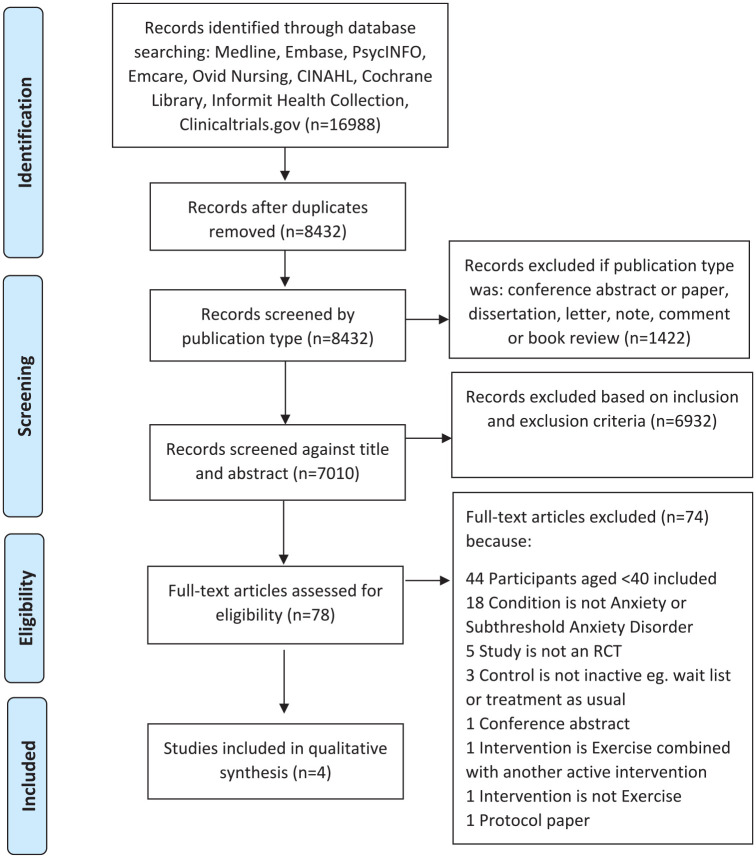
The initial search yielded 16,988 records which was reduced to 8,432 after removal of duplicates. This was further reduced to 7010 after removal of conference abstracts or papers, dissertations, letters, notes, comments, and book reviews. Of the 7,010 title and abstracts that were screened, 78 did not meet exclusion criteria and proceeded to full-text review. After full-text review, four trials met inclusion criteria. A PRISMA flow diagram is included as Figure 2. 27
Figure 2.
PRISMA flow diagram.
The four included trials have been discussed qualitatively and their main characteristics are described in Table 1 followed by a summary of their results in Table 2.
Table 1.
Main characteristics of included trials.
| Study (country) | Sample size | Mean (SD) age (years) | Gender (% female) | Diagnosis | |||
|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | ||
| Aguinaga et al. (USA) 36 | 15 | 12 | 69.6 (4.3) | 71.3 (4.6) | 86.7 | 91.7 | Anxiety defined as HADS-A score ⩾ 8 |
| Carmeli et al. (Israel) 37 | 8 | 8 | 47.8 (8) | 51.8 (4) | 66.7 | 50 | Anxiety and mild Intellectual Disability |
| Song et al. (China) 34 | 16 | 16 | 65.3 (7.1) | 66.1 (8.3) | NS | NS | Anxiety Disorder in CCMD-3 with HAM-A score ⩾ 14 |
| Villaverde Gutiérrez et al. (Spain) 38 | 27 | 30 | 64.2 (2.8) | 63.5 (3.3) | 100 | 100 | Anxiety defined as HAM-A ⩾ 6 and depression defined by GDS ⩾ 11 |
CCMD-3, Chinese Classification and Diagnostic Criteria of Mental Disorders; GDS, Geriatric Depression Scale; HADS-A, Hospital Anxiety and Depression Scale – Anxiety Subscale; HAM-A, Hamilton Anxiety Scale; NS, not stated; SD, standard deviation.
Table 2.
Summary of results of included trials.
| Study (country) | Intervention | Outcome time point | Group | p | Retention | ||
|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | ||||
| Aguinaga et al. (USA) 36 | Flexibility, Toning and Balance DVD versus Healthy Aging DVD | HADS-A | 0.30 | 50% | 91% | ||
| Baseline | 9.3 | 11.4 | |||||
| 6 months | 5.3 | 8.9 | |||||
| Change | –4 | –2.5 | |||||
| Carmeli et al. (Israel) 37 | Aerobic Training versus Non-physical Activities | HAM-A a | ⩽0.05 | 75% | 75% | ||
| Baseline | 8 | 8 | |||||
| 6 months | 4 | 8 | |||||
| Change | –4 | 0 | |||||
| Song et al. (China) 34 | Tai Chi with Paroxetine versus Paroxetine Only | HAM-A | <0.05 | NS | NS | ||
| Baseline | 19.4 | 19.7 | |||||
| 45 days | 10.7 | 14.5 | |||||
| Change | –8.7 | –5.2 | |||||
| Villaverde Gutiérrez et al. (Spain) 38 | Aerobic and Strength Training versus Inactive Control | HAM-A | 90% | 100% | |||
| Minor (6–14) | |||||||
| Baseline | 7.33 | 7.2 | |||||
| 6 months | 5.27 | 7.1 | |||||
| Change | –2.06 | –0.08 | <0.01 | ||||
| HAM-A | |||||||
| Major (>14) | |||||||
| Baseline | 16.8 | 16.4 | |||||
| 6 months | 15.0 | 17.0 | |||||
| Change | –1.74 | 0.64 | <0.05 | ||||
| GDS | |||||||
| Moderate (11–14) | |||||||
| Baseline | 12.0 | 11.9 | |||||
| 6 months | 9.76 | 11.9 | |||||
| Change | –2.26 | 0.06 | <0.05 | ||||
| GDS | |||||||
| Severe (15–30) | |||||||
| Baseline | 17.3 | 17.2 | |||||
| 6 months | 13.5 | 16.9 | |||||
| Change | –3.85 | –0.38 | <0.01 | ||||
GDS, Geriatric Depression Scale; HADS-A, Hospital Anxiety and Depression Scale – Anxiety Subscale; HAM-A, Hamilton Anxiety Scale; NS, not stated.
HAM-A scale adapted for participants with Intellectual Disability.
Home-based DVD-delivered physical activity programme for older adults with elevated anxiety
Aguinaga et al. 36 conducted a randomised controlled trial of a home-based DVD-delivered Physical Activity Intervention for older adults. The intervention involved flexibility, toning and balance exercises for 6 months with telephone support while the control group received a DVD about healthy ageing and the same amount of telephone contact.
Inclusion criteria for the trial included being age 65 years and above, being ‘inactive’ defined as less than 2 days per week of at least 30 minutes of physical activity over the past 6 months, English speaking, able to safely participate in a physical activity programme as determined by a physician and a score of 21 or higher on the 13-item modified Telephone Interview of Cognitive Status measure. This study recruited 307 participants and then a subgroup analysis was performed using results from participants with elevated anxiety defined as a Hospital Anxiety and Depression Scale (HADS) anxiety score of 8 or above. There were no significant differences between the groups at baseline with regard to age, sex, race, education and income. 36
Repeated measures analysis of variance was used to compare the effects of the intervention and control conditions on HADS anxiety score over time, with Cohen’s d calculated to estimate the effect size. Both the intervention and control groups demonstrated a reduction in HADS anxiety score at 6 months, and there was no statistically significant difference between the two groups. The difference of effect size was larger in the intervention group (d = 2.90) compared with the control group (d = 0.73), but did not reach statistical significance (p = 0.30). Of note, the intervention group (50%) had a higher dropout rate than the control group (9%). The reasons for dropping out were not reported by group. Overall, three participants dropped out due to no longer being interested, two due to personal issues and one due to injury unrelated to the programme. 36 The authors did not postulate any reasons for this difference in retention and dropout.
Aerobic training for adults with anxiety and mild intellectual disability
Carmeli et al. 37 conducted a randomised controlled trial of an aerobic exercise intervention for adults with anxiety and mild intellectual disability. The intervention group received aerobic training involving three supervised group treadmill or ergometric bicycle sessions aiming for 20 minutes of low to moderate training intensity (50–70% of heart rate reserve) each week for 6 months. Another group received a leisure intervention which included 20- to 40-minute sessions involving exercises and games that focused on flexibility, stability and balance, while the control group received vocational activities, such as packing candles. 37
Inclusion criteria for the trial included having dual diagnosis of mild intellectual disability and anxiety with their ages ranging from 45 to 55 years. Exclusion criteria included use of antidepressant medication, use of medication that would contra-indicate exercise training and medical contraindication to exercise. 37 The primary outcome measure was the Hamilton Anxiety Scale (HAM-A) which was adjusted to be more appropriate for the participant’s intellectual disability diagnosis through the removal of four items – intellectual, autonomic, visceral and insomnia symptoms. The authors describe the use of Student’s t test to compare participants’ health and lifestyle factors in the intervention and control groups at baseline; however, the results of this analysis are not reported. 37
One-way analysis of variance was used to compare the effects of the interventions and control conditions on HAM-A scores over time. The exercise intervention and leisure intervention groups both demonstrated a statistically significant reduction in HAM-A score while the control group did not. The overall dropout rate was 20%, and the reasons for dropping out were not reported by group. Overall, two participants dropped out due to a medical condition and three due to being unwilling to continue or no indicated reason. Further to this, three participants did not agree to complete the HAM-A scale at 6 months, leaving the results of 16 participants. 37
Tai Chi exercise for older adults with anxiety disorder
Song et al. 34 conducted a randomised controlled trial of Tai Chi exercise for older adults with anxiety disorder. The intervention group received Paroxetine 10 mg twice a day and Tai Chi for 35 minutes morning and evening for 45 days, including stretching and postures. The control group only received Paroxetine 10 mg twice a day for 45 days. 34
Inclusion criteria for the trial included participants aged between 60 and 75 years who met diagnostic criteria for anxiety disorder in the Chinese Classification and Diagnostic Criteria of Mental Disorders (CCMD-3) with HAM-A score of 14 or higher. Exclusion criteria included other mental disorders, severe organic or somatic diseases that were not defined in any further detail. Comparison of ‘basic data’ between the intervention and control groups at baseline was reported to not demonstrate any differences; however, the factors that were compared and the statistical technique used were not reported. 34
T tests were used to compare pre and post intervention HAM-A scores within the intervention and control groups as well as comparing between the intervention and control groups. Both groups had significant improvement in HAM-A scores at 45 days, and this improvement was significantly greater in the intervention group. The study results demonstrated a similar improvement in quality of life scale scores at 45 days in both groups with the intervention significantly greater than the control group. Participants who were deemed to be ‘cured’ at 45 days ceased Paroxetine, but continued Tai Chi if they were in the intervention group for a further 2 months. At this 2-month follow-up, 43% of the ‘cured’ participants in the control group had relapsed, compared with 9% of the intervention group. 34 The authors did not define ‘cure’ or ‘relapse’.
Aerobic and strength training for postmenopausal women with symptoms of anxiety and depression
Villaverde Gutiérrez et al. 38 conducted a randomised controlled trial of an aerobic and strength training intervention for postmenopausal women with anxiety and depression symptoms. The intervention group received a 6-month supervised aerobic intervention aiming initially for 50–70% of maximum heart rate reserve, then increasing to 60–85% for the second half of the programme. This was combined with 4 weeks of muscle training exercises. The control group did not receive any intervention.30,38
The participants were selected consecutively from primary healthcare clinics with inclusion criteria including aged 60–70 years, postmenopausal status, HAM-A score of 6 or above and Geriatric Depression Scale score of 11 or above. Exclusion criteria included previous history of fractures, orthostatic hypotension, dizziness, vertigo, balance problems or other medical contraindication to physical exercise. 38
T tests were used to compare between groups. The intervention groups had significant improvement in anxiety and depression compared with the control groups. This was the case for the minor and major anxiety groups as well as the moderate and severe depression groups. Adherence was high with only three participants not meeting 80% adherence to the intervention. 38
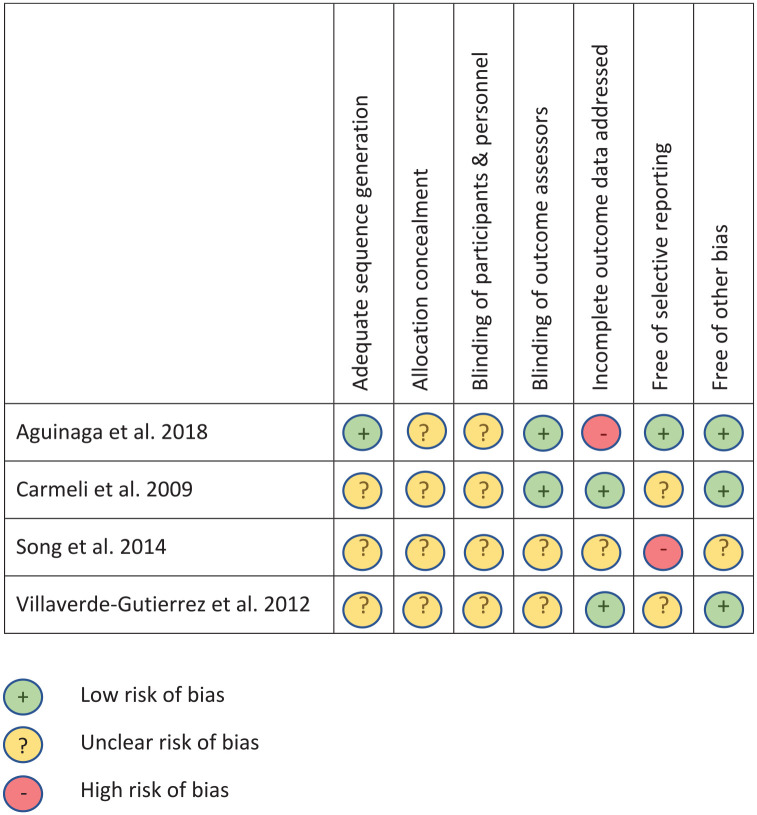
Methodological quality
All four trials had small sample sizes and none reported a power analysis. Overall, aside from one trial, the other trials appeared to have many domains with unclear or high risk of bias. The Cochrane risk of bias quality assessment results are summarised in Figure 3.
Figure 3.
Quality assessment of included trials (Cochrane Risk of Bias Tool).
The home-based DVD physical activity trial reported by Aguinaga et al. 36 was rated as low risk of bias in all domains except three. The trial was registered with clincialtrials.gov and the trial protocol was published, but did not report an intention to undertake the subgroup analysis for participants with elevated anxiety. 39 This trial was rated as high risk of bias for incomplete outcome data due to the high dropout rate of 50% in the intervention group. The high dropout rate may increase the risk of over-stating benefits of the intervention as those who dropped out may have been participants who were likely to receive less benefit from the intervention. The allocation concealment and blinding of participants and personnel domains were rated as unclear as there was insufficient information provided for us to accurately assess the risk of bias. In addition, the published report of the main trial described the study as ‘single-blind’ in design. 40 Lack of blinding of study participants may influence retention rate as well as self-rating of benefit and adverse effects.
The aerobic physical activity trial reported by Carmeli et al. 37 was rated as low risk of bias in three domains. Four domains were rated as unclear risk of bias as there was insufficient information provided for us to accurately assess the risk of bias. These four domains were adequate sequence generation, allocation concealment, blinding of participants and personnel and selective outcome reporting. Trial registration and publication of a trial protocol would have been helpful with our assessment of risk of bias.
The Tai Chi trial reported by Song et al. 34 was assessed as unclear risk of bias in all domains except for selective outcome reporting. The domains were rated as unclear due to insufficient information being provided for us to accurately assess the risk of bias. The selective outcome domain was reported as high risk of bias due to the lack of reporting of the dropout rate and adverse event rate, as well as the trial not being registered or having a published trial protocol. 34 Overall, this study was assessed as having a high risk of bias given the limited information reported.
The aerobic and strength trial reported by Villaverde Gutiérrez et al. 38 was assessed as unclear risk of bias in all domains except for incomplete outcome data addressed and other bias. The domains were reported as unclear due to insufficient information being provided for us to accurately assess the risk of bias. The level of bias could have been reduced by more detailed reporting of trial methodology and registration of the trial or publication of a trial protocol. It was also noted that the observations of three participants in the intervention group were not included in the analysis due to their lack of adherence to at least 80% of the intervention. This exclusion may lead to risk of bias in the outcome analysis.
A meta-analysis was not performed due to the small number of included studies, the heterogeneity in participant characteristics and intervention types, and level of risk of bias in some included studies.
Discussion
This systematic review identified only four randomised controlled trials meeting inclusion criteria, all with relatively small sample sizes, which highlights the paucity of research in this area. Three of the trials reported that exercise interventions were more effective at reducing anxiety than control interventions.34,37,38 The fourth trial showed a pre–post reduction in anxiety in both the intervention and control groups, but the difference between groups did not reach statistical significance. 36
Of note, this fourth trial had the highest rate of dropout which was predominantly in the intervention group. 36 The evaluation of the effect of exercise for participants with anxiety was a subgroup analysis of a larger trial. 40 This may suggest that an exercise intervention for participants with anxiety may need to be more tailored to their specific needs given that anxiety is often a barrier towards engaging in exercise. 41 The overall dropout rates and reported adverse events seem to suggest that exercise interventions in this group may be feasible and safe; however, the level of reporting of these parameters varied between trials. Importantly, intervention adherence also impacts effectiveness and was not reported in three out of four trials. One trial reported 90% of participants adhered to the intervention, defined as attending at least 80% of exercise sessions. 38
The review suggests that the extent of available evidence for exercise interventions is quite limited for anxiety disorders in mid-life and late-life, and even more so for subthreshold anxiety disorder which is more prevalent. In the review, trials which examined the effects of exercise on anxiety levels in participants with conditions other than anxiety disorders, such as cancer, respiratory illness and chronic pain were identified, but did not meet inclusion criteria as the samples were heterogeneous and included participants without anxiety disorders. These trials could provide some indirect evidence for the effect of exercise on anxiety, but do not provide direct evidence in the clinical context of anxiety disorders and subthreshold anxiety disorder.
Similarly, two trials of medical yoga interventions for ‘stress’ were identified during the review but did not meet inclusion criteria as they included participants without anxiety disorders.42,43 The concept of ‘stress’ has some overlap with anxiety. Daukantaitė et al. 42 conducted a trial involving 105 participants with a mean age of 54 years and demonstrated that a 5-week medical yoga intervention resulted in a statistically significant reduction in HADS anxiety score (10.3–6.9) compared with an inactive control (8.9–7.8) with p = 0.002. 42 At baseline, 81% of the cohort scored 7 or above on the HADS anxiety scale which demonstrates clinically significant anxiety (personal communication from authors). Köhn et al. 43 conducted a trial involving 37 participants with mean age 53 years and demonstrated that a 12-week medical yoga intervention resulted in a statistically significant reduction in HADS anxiety score (11.8–6.4) compared with inactive control (12.7–10.5) with p = 0.019. 43 At baseline, 89% of the cohort scored 7 or above on the HADS anxiety scale (personal communication from authors). These two trials thus provide some further supportive evidence of the effectiveness of exercise interventions for reducing anxiety in two cohorts where the majority of participants experience clinically significant anxiety.
To our knowledge, this is the first review that has examined exercise interventions for anxiety disorders in these age groups. A key strength of this review is its broad search strategy to minimise the possibility of missing trials. Limitations of this review include the inclusion of only trials published in English and that the heterogeneity, limited number, and high risk of bias of some included trials meant that we were not able to conduct a meta-analysis.
While the identified studies are small in number and size, they provide an encouraging signal that exercise interventions may be an effective, feasible and safe treatment option for anxiety and subthreshold anxiety disorders in mid-life and late-life. While acknowledging that the evidence is still limited and some trials had methodological limitations, these findings can provide clinicians with some encouragement to prescribe exercise interventions for mid-life and late-life adults with anxiety and subthreshold anxiety disorders, as they may provide benefit in reducing anxiety. This encouragement is supported by the existing evidence base that exercise interventions are beneficial to many other aspects of health and are likely to be feasible and safe. As there is not yet a sizable evidence base relating to the types and doses of exercise are effective in reducing anxiety, a practical approach for clinicians in the meantime would be to recommend their relevant national or international physical activity guidelines, as these have been prepared with consideration given to general health benefits and safety for the population.
Future research could include larger trials with a view to providing proof of concept and guidance to clinicians, as well as studies to inform the types and doses of exercise interventions that are effective. The concept of stress has some overlap with anxiety, and trials in this area may provide another productive avenue for future research. Given that exercise anxiety is a potential barrier to undertaking exercise interventions, there is a need for qualitative research into how best to bridge this gap and tailor interventions for individuals who have significant anxiety.
Conclusion
The results of this review suggest that exercise interventions have the potential to be an effective non-pharmacological intervention for anxiety and subthreshold anxiety disorders in mid-life and late-life, despite the limited extent of the evidence base. The paucity of research in this area is another example of the relative neglect of anxiety and subthreshold anxiety disorders in mid-life and late-life despite their high prevalence and resultant significant distress, disability and cost. There is a clear need to have effective evidence-based non-pharmacological interventions given that susceptibility to medication adverse effects and interactions generally increase with age. Furthermore, psychological therapies may have some limitations in the context of cognitive impairment which increases in prevalence with age.
Exercise interventions that are tailored to an individual’s function and health have been found to be beneficial in many health conditions and longevity. 20 Examining which types and doses of exercise are effective for treating anxiety and subthreshold anxiety disorders is a significant opportunity to expand treatment options. This could include head-to-head studies. The increasing use of technology such as wearable activity monitors and smart phones provides a unique opportunity to research and facilitate exercise interventions, while the effects of the COVID-19 pandemic on mental health, in particular anxiety, make this research all the more urgent.
Supplemental Material
Supplemental material, sj-docx-1-tpp-10.1177_20451253221104958 for Exercise interventions to reduce anxiety in mid-life and late-life anxiety disorders and subthreshold anxiety disorder: a systematic review by Terence W.H. Chong, Scherazad Kootar, Helen Wilding, Sarah Berriman, Eleanor Curran, Kay L. Cox, Alex Bahar-Fuchs, Ruth Peters, Kaarin J. Anstey, Christina Bryant and Nicola T. Lautenschlager in Therapeutic Advances in Psychopharmacology
Acknowledgments
We are grateful to A/Prof. Daiva Daukantaitė and colleagues and A/Prof. Elisabeth Westerdahl and colleagues for providing raw data from their trials.
Footnotes
Ethics approval and consent to participate: Not applicable
Consent for publication: Not applicable
Author contributions: Terence W.H. Chong: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Validation; Visualization; Writing – original draft; Writing – review & editing.
Scherazad Kootar: Data curation; Formal analysis; Investigation; Validation; Visualization; Writing – original draft; Writing – review & editing.
Helen Wilding: Conceptualization; Data curation; Investigation; Methodology; Visualization; Writing – original draft; Writing – review & editing.
Sarah Berriman: Formal analysis; Investigation; Writing – review & editing
Eleanor Curran: Formal analysis; Investigation; Writing – review & editing.
Kay L. Cox: Conceptualization; Methodology; Supervision; Writing – review & editing.
Alex Bahar-Fuchs: Conceptualization; Methodology; Supervision; Writing – review & editing.
Ruth Peters: Methodology; Supervision; Writing – review & editing.
Kaarin J. Anstey: Conceptualization; Funding acquisition; Methodology; Supervision; Writing – review & editing.
Christina Bryant: Conceptualization; Methodology; Supervision; Writing – review & editing.
Nicola T. Lautenschlager: Conceptualization; Funding acquisition; Methodology; Supervision; Writing – review & editing.
ORCID iD: Terence W.H. Chong  https://orcid.org/0000-0003-2432-8193
https://orcid.org/0000-0003-2432-8193
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: TWHC is funded by the NHMRC Centre for Research Excellence in Cognitive Health 110579, SK by NHMRC GNT1171279, RP by NHMRC Dementia Centre for Research Collaboration Grant and KA by ARC FL190100011.
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: Not applicable
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Terence W.H. Chong, Academic Unit for Psychiatry of Old Age, Department of Psychiatry, The University of Melbourne and St Vincent’s Hospital Melbourne, St George’s Campus, 283 Cotham Road, Kew, VIC 3101, Australia.
Scherazad Kootar, School of Psychology, University of New South Wales, Sydney, NSW, Australia; Lifecourse Ageing Research Centre, Neuroscience Research Australia, Sydney, NSW, Australia.
Helen Wilding, St Vincent’s Hospital Melbourne, Fitzroy, VIC, Australia.
Sarah Berriman, Academic Unit for Psychiatry of Old Age, Department of Psychiatry, The University of Melbourne, Parkville, VIC, Australia; St Vincent’s Hospital Melbourne, Fitzroy, VIC, Australia.
Eleanor Curran, Academic Unit for Psychiatry of Old Age, Department of Psychiatry, The University of Melbourne, Parkville, VIC, Australia; St Vincent’s Hospital Melbourne, Fitzroy, VIC, Australia; NorthWestern Mental Health, The Royal Melbourne Hospital, Parkville, VIC, Australia.
Kay L. Cox, Medical School, Royal Perth Hospital Unit, The University of Western Australia, Perth, WA, Australia
Alex Bahar-Fuchs, Academic Unit for Psychiatry of Old Age, Department of Psychiatry, The University of Melbourne, Parkville, VIC, Australia.
Ruth Peters, School of Psychology, University of New South Wales, Sydney, NSW, Australia; Lifecourse Ageing Research Centre, Neuroscience Research Australia, Sydney, NSW, Australia.
Kaarin J. Anstey, School of Psychology, University of New South Wales, Sydney, NSW, Australia Lifecourse Ageing Research Centre, Neuroscience Research Australia, Sydney, NSW, Australia.
Christina Bryant, Melbourne School of Psychological Sciences, The University of Melbourne, Parkville, VIC, Australia.
Nicola T. Lautenschlager, Academic Unit for Psychiatry of Old Age, Department of Psychiatry, The University of Melbourne, Parkville, VIC, Australia St Vincent’s Hospital Melbourne, Fitzroy, VIC, Australia; NorthWestern Mental Health, The Royal Melbourne Hospital, Parkville, VIC, Australia.
References
- 1. Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 2005; 62: 593–602. [DOI] [PubMed] [Google Scholar]
- 2. Baxter AJ, Scott KM, Vos T, et al. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med 2013; 43: 897–910. [DOI] [PubMed] [Google Scholar]
- 3. Canuto A, Weber K, Baertschi M, et al. Anxiety disorders in old age: psychiatric comorbidities, quality of life, and prevalence according to age, gender, and country. Am J Geriatr Psychiatry 2018; 26: 174–185. [DOI] [PubMed] [Google Scholar]
- 4. Prina AM, Ferri CP, Guerra M, et al. Prevalence of anxiety and its correlates among older adults in Latin America, India and China: cross-cultural study. Br J Psychiatry 2011; 199: 485–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Grenier S, Preville M, Boyer R, et al. The impact of DSM-IV symptom and clinical significance criteria on the prevalence estimates of subthreshold and threshold anxiety in the older adult population. Am J Geriatr Psychiatry 2011; 19: 316–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Volz HP, Saliger J, Kasper S, et al. Subsyndromal generalised anxiety disorder: operationalisation and epidemiology – a systematic literature survey. Int J Psychiatry Clin Pract 2021: 1–10. [DOI] [PubMed] [Google Scholar]
- 7. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord 2020; 277: 55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wetherell JL, Thorp SR, Patterson TL, et al. Quality of life in geriatric generalized anxiety disorder: a preliminary investigation. J Psychiatr Res 2004; 38: 305–312. [DOI] [PubMed] [Google Scholar]
- 9. Bryant C, Mohlman J, Gum A, et al. Anxiety disorders in older adults: looking to DSM5 and beyond. Am J Geriatr Psychiatry 2013; 21: 872–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hohls JK, Konig HH, Raynik YI, et al. A systematic review of the association of anxiety with health care utilization and costs in people aged 65 years and older. J Affect Disord 2018; 232: 163–176. [DOI] [PubMed] [Google Scholar]
- 11. Meier SM, Mattheisen M, Mors O, et al. Increased mortality among people with anxiety disorders: total population study. Br J Psychiatry 2016; 209: 216–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Konnopka A, Konig H. Economic burden of anxiety disorders: a systematic review and meta-analysis. Pharmacoeconomics 2020; 38: 25–37. [DOI] [PubMed] [Google Scholar]
- 13. Chong TWH, Lautenschlager NT, Anstey KJ, et al. Anxiety disorders in late life – why are we not more worried? Int J Geriatr Psychiatry 2020; 35: 955–961. [DOI] [PubMed] [Google Scholar]
- 14. Santabarbara J, Lipnicki DM, Bueno-Notivol J, et al. Updating the evidence for an association between anxiety and risk of Alzheimer’s disease: a meta-analysis of prospective cohort studies. J Affect Disord 2020; 262: 397–404. [DOI] [PubMed] [Google Scholar]
- 15. Pietrzak RH, Lim YY, Neumeister A, et al. Amyloid-beta, anxiety, and cognitive decline in preclinical Alzheimer disease: a multicenter, prospective cohort study. JAMA Psychiatry 2015; 72: 284–291. [DOI] [PubMed] [Google Scholar]
- 16. Mah L, Binns MA, Steffens DC, et al. Anxiety symptoms in amnestic mild cognitive impairment are associated with medial temporal atrophy and predict conversion to Alzheimer disease. Am J Geriatr Psychiatry 2015; 23: 466–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pink A, Krell-Roesch J, Syrjanen JA, et al. A longitudinal investigation of Abeta, anxiety, depression, and mild cognitive impairment. Alzheimers Dement. Epub ahead of print 8 December 2021. DOI: 10.1002/alz.12504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Andrews G, Bell C, Boyce P, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of panic disorder, social anxiety disorder and generalised anxiety disorder. Aust NZ J Psychiatry 2018; 52: 1109–1172. [Google Scholar]
- 19. Sikkes SAM, Tang Y, Jutten RJ, et al. Toward a theory-based specification of non-pharmacological treatments in aging and dementia: focused reviews and methodological recommendations. Alzheimers Dement 2021; 17: 255–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Vina J, Sanchis-Gomar F, Martinez-Bello V, et al. Exercise acts as a drug; the pharmacological benefits of exercise. Br J Pharmacol 2012; 167: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stubbs B, Vancampfort D, Rosenbaum S, et al. An examination of the anxiolytic effects of exercise for people with anxiety and stress-related disorders: a meta-analysis. Psychiatry Res 2017; 249: 102–108. [DOI] [PubMed] [Google Scholar]
- 22.Diagnostic and statistical manual of mental disorders: DSM-5. Arlington, VA: American Psychiatric Association, 2013. [Google Scholar]
- 23. Aylett E, Small N, Bower P. Exercise in the treatment of clinical anxiety in general practice – a systematic review and meta-analysis. BMC Health Serv Res 2018; 18: 559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Martinez-Dominguez SJ, Lajusticia H, Chedraui P, et al. The effect of programmed exercise over anxiety symptoms in midlife and older women: a meta-analysis of randomized controlled trials. Climacteric 2018; 21: 123–131. [DOI] [PubMed] [Google Scholar]
- 25. Mochcovitch MD, Deslandes AC, Freire RC, et al. The effects of regular physical activity on anxiety symptoms in healthy older adults: a systematic review. Braz J Psychiatry 2016; 38: 255–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chong TW, Macpherson H, Schaumberg MA, et al. Dementia prevention: the time to act is now. Med J Aust 2021; 214: 302–304. [DOI] [PubMed] [Google Scholar]
- 27. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009; 339: b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Diagnostic and statistical manual of mental disorders: DSM-IV. Washington, DC: American Psychiatric Association, 1994. [Google Scholar]
- 29.Covidence systematic review software. Melbourne, VIC, Australia: Veritas Health Innovation, 2021. [Google Scholar]
- 30. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep 1985; 100: 126–131. [PMC free article] [PubMed] [Google Scholar]
- 31. Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc 2009; 41: 1510–1530. [DOI] [PubMed] [Google Scholar]
- 32. Lautenschlager N, Cox K, Hill KD, et al. Physical activity guidelines for older Australians with mild cognitive impairment or subjective cognitive decline. Melbourne, VIC, Australia: Dementia Collaborative Research Centres, 2018. [Google Scholar]
- 33. Earles DR, Judge JO, Gunnarsson OT. Velocity training induces power-specific adaptations in highly functioning older adults. Arch Phys Med Rehabil 2001; 82: 872–878. [DOI] [PubMed] [Google Scholar]
- 34. Song QH, Shen GQ, Xu RM, et al. Effect of Tai Chi exercise on the physical and mental health of the elder patients suffered from anxiety disorder. Int J Physiol Pathophysiol Pharmacol 2014; 6: 55–60. [PMC free article] [PubMed] [Google Scholar]
- 35. Higgins JPT, Altman DG. Assessing risk of bias in included studies. In: Higgins JPT, Green S. (eds) Cochrane handbook for systematic reviews of interventions. Chichester: John Wiley & Sons Incorporated, ProQuest Ebook Central, 2008, pp. 205–228. [Google Scholar]
- 36. Aguinaga S, Ehlers DK, Salerno EA, et al. Home-based physical activity program improves depression and anxiety in older adults. J Phys Act Health 2018; 15: 692–696. [DOI] [PubMed] [Google Scholar]
- 37. Carmeli E, Barak S, Morad M, et al. Physical exercises can reduce anxiety and improve quality of life among adults with intellectual disability. Int SportMed J 2009; 10, https://hdl.handle.net/10520/EJC48373 [Google Scholar]
- 38. Villaverde Gutiérrez C, Torres Luque G, Abalos Medina GM, et al. Influence of exercise on mood in postmenopausal women. J Clin Nurs 2012; 21: 923–928. [DOI] [PubMed] [Google Scholar]
- 39. McAuley E, Wojcicki TR, White SM, et al. Physical activity, function, and quality of life: design and methods of the FlexToBa trial. Contemp Clin Trials 2012; 33: 228–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. McAuley E, Wojcicki TR, Gothe NP, et al. Effects of a DVD-delivered exercise intervention on physical function in older adults. J Gerontol A Biol Sci Med Sci 2013; 68: 1076–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mason JE, Faller YN, LeBouthillier DM, et al. Exercise anxiety: a qualitative analysis of the barriers, facilitators, and psychological processes underlying exercise participation for people with anxiety-related disorders. Ment Health Phys Act 2019; 16: 128–139. [Google Scholar]
- 42. Daukantaitė D, Tellhed U, Maddux RE, et al. Five-week yin yoga-based interventions decreased plasma adrenomedullin and increased psychological health in stressed adults: a randomized controlled trial. PLoS ONE 2018; 13: e0200518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Köhn M, Persson Lundholm U, Bryngelsson IL, et al. Medical yoga for patients with stress-related symptoms and diagnoses in primary health care: a randomized controlled trial. Evid Based Complement Alternat Med 2013; 2013: 215348. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-tpp-10.1177_20451253221104958 for Exercise interventions to reduce anxiety in mid-life and late-life anxiety disorders and subthreshold anxiety disorder: a systematic review by Terence W.H. Chong, Scherazad Kootar, Helen Wilding, Sarah Berriman, Eleanor Curran, Kay L. Cox, Alex Bahar-Fuchs, Ruth Peters, Kaarin J. Anstey, Christina Bryant and Nicola T. Lautenschlager in Therapeutic Advances in Psychopharmacology