Abstract
Background:
Nighttime noise carries a significant disease burden. The World Health Organization (WHO) recently published guidelines for the regulation of environmental noise based on a review of evidence published up to the year 2015 on the effects of environmental noise on sleep.
Objectives:
This systematic review and meta-analysis will update the WHO evidence review on the effects of environmental noise on sleep disturbance to include more recent studies.
Methods:
Investigations of self-reported sleep among residents exposed to environmental traffic noise at home were identified using Scopus, PubMed, Embase, and PsycINFO. Awakenings, falling asleep, and sleep disturbance were the three outcomes included. Extracted data were used to derive exposure–response relationships for the probability of being highly sleep disturbed by nighttime noise [average outdoor A-weighted noise level () 2300–0700 hours] for aircraft, road, and rail traffic noise, individually. The overall quality of evidence was assessed using Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) criteria.
Results:
Eleven studies ( responses) were included in addition to 25 studies ( responses) from the original WHO analysis. When sleep disturbance questions specifically mentioned noise as the source of disturbance, there was moderate quality of evidence for the probability of being highly sleep disturbed per 10-dB increase in for aircraft [; 95% confidence interval (CI): 2.01, 2.36], road (; 95% CI: 2.28, 2.79), and railway (; 95% CI: 2.57, 3.43) noise. When noise was not mentioned, there was low to very low quality of evidence for being sleep disturbed per 10-dB increase in for aircraft (; 95% CI: 1.20, 1.93), road (; 95% CI: 1.08, 1.21), and railway (; 95% CI: 0.91, 1.49) noise. Compared with the original WHO review, the exposure–response relationships closely agreed at low (40 dB ) levels for all traffic types but indicated greater disturbance by aircraft traffic at high noise levels. Sleep disturbance was not significantly different between European and non-European studies.
Discussion:
Available evidence suggests that transportation noise is negatively associated with self-reported sleep. Sleep disturbance in this updated meta-analysis was comparable to the original WHO review at low nighttime noise levels. These low levels correspond to the recent WHO noise limit recommendations for nighttime noise, and so these findings do not suggest these WHO recommendations need revisiting. Deviations from the WHO review in this updated analysis suggest that populations exposed to high levels of aircraft noise may be at greater risk of sleep disturbance than determined previously. https://doi.org/10.1289/EHP10197
Introduction
Sleep is a vital component of human life that serves many critical roles in physical and mental health and well-being.1 Sufficient quantity and quality of sleep are requirements for optimal daytime alertness and performance, and high quality of life.2 Experimental studies suggest that restricted sleep duration causes blood vessel dysfunction,3 induces changes in glucose metabolism4,5 and appetite regulation,6 and impairs memory consolidation.7 Accordingly, epidemiological studies have consistently found that chronic short or interrupted sleep is associated with negative health outcomes, including obesity,8 diabetes,9 hypertension,10 cardiovascular disease,11 all-cause mortality,12 and poorer cognitive function.13 Chronic insufficient or disrupted sleep is therefore of public health relevance, and sleep disturbance is considered a major adverse consequence of exposure to environmental noise.14
In Europe, there is a substantial burden of disease from environmental noise, primarily from aircraft, road, and rail traffic.15,16 In 2011, the World Health Organization (WHO) attributed the majority of this disease burden to noise-induced sleep disturbance, with 903,000 disability-adjusted life years lost annually in Western Europe alone.14 Environmental noise is also a problem outside of Europe, for example, recent data from the U.S. Bureau of Transportation Statistics estimates that 41.7 million people in the United States are exposed to air and road traffic noise at 24-h average levels () dB.17 This noise level, per conversion data from Brink et al.18 is equivalent to a nighttime (2300–0700 hours) level of 45.3 dB (), which is around or above the level associated with adverse effects on sleep.15 Nighttime noise can fragment sleep structure by inducing awakenings and shifts to lighter, less restorative sleep.19 Importantly, these effects do not seem to habituate fully, and arousals and awakenings induced by aircraft noise can occur even among chronically exposed individuals.20–22 Although noise-induced sleep fragmentation and reductions in total sleep time are less severe than in sleep restriction studies, sleep disturbance by chronic noise exposure may lead to the development of disease in the long term. Experimental studies have found adverse effects of nocturnal aircraft noise on parameters of endothelial function, oxidative stress, and inflammation.23,24 This points to the importance of noise-induced sleep disturbance for cardiovascular disease risk, and, indeed, this is supported with epidemiological data where nighttime noise is more strongly associated with indicators of vascular stiffness and hypertension compared with daytime noise.25 The ubiquity of exposure to environmental noise in industrialized nations, and the chronic nature of that exposure, therefore poses a significant threat to health.26
In 2018, the WHO published recommendations for protecting human health from exposure to environmental noise.15 These guidelines included strong recommendations for target nighttime noise levels to mitigate adverse effects of traffic noise on sleep, which were 45 dB for road traffic, 44 dB for rail traffic, and 40 dB for air traffic. These recommendations were based primarily on a systematic review and meta-analysis on the effects of noise on sleep, which included studies published up to the year 2015 only.19 There has been continued and substantial interest and research in the domain of noise and sleep during the intervening years. We therefore updated the earlier systematic review and meta-analysis to include studies published up to the year 2021. This updated analysis is restricted to field studies on the effects of nocturnal traffic noise on self-reported sleep in adults, and it has the overarching aim of synthesizing updated exposure–response relationships for the probability of being highly sleep disturbed.
Methods
This review and analysis was prepared following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement guidelines.27 The completed PRISMA checklist is given in Table S1. The review and analysis protocol was defined a priori and registered in PROSPERO (record CRD42021229587) before conducting any preliminary searches, screening of articles, or data extraction. The University of Pennsylvania institutional review board (IRB) determined that the study did not meet the definition of human subjects research given that no identifiable information was being obtained, and therefore review or approval of the study by the IRB was not required.
The analytic approach is described in detail below and was consistent with the previous WHO review,19 with the following exceptions: a) Exposures were limited to traffic noise from aircraft, road, and rail traffic, and b) effects on sleep were limited to self-reported questionnaire outcomes. These form the basis of the highly sleep disturbed exposure–response relationships and calculations of the burden of disease by noise and are, therefore, are critical outcomes from a noise policy perspective. Studies on acute noise-induced awakenings using objective measures, such as actigraphy or polysomnography, were not included.
Eligibility Criteria
Studies were restricted to primary investigations in humans exposed to environmental noise from aircraft, road, and rail traffic at home. Studies investigating other sources, such as wind turbine noise or hospital noise, were excluded. Studies were eligible only if sound pressure levels were measured or predicted at the participant’s home. Studies with subjective evaluation of the noise levels, distance to the noise source as a surrogate measure of noise level, or noise levels not specific to a participant’s home address were excluded. A minimum of two different noise level categories were required so that exposure–response relationships for sleep disturbance could be constructed.
Studies were eligible if they employed prospective, retrospective, cohort, longitudinal, cross-sectional, or case–control study designs. Laboratory studies, intervention studies, or studies in which noise was introduced artificially were excluded due to low generalizability in real-world settings. Studies were restricted to original research published or accepted for publication in the year 2000 or later. Article language was restricted to English, Dutch, French, and German.
This review and analysis focuses on self-reported sleep disturbance by traffic noise. Eligible studies included at least one of the three most common outcomes of self-reported disturbance that were identified in the original WHO review19:
Awakenings from sleep
The process of falling asleep
Sleep disturbance
Studies were eligible if they either explicitly mentioned noise as the source of disturbance, for example, “How often is your sleep disturbed by noise from aircraft?”, or included more general sleep questions that did not explicitly mention noise, for example, “How often do you have difficulties sleeping?”. So that the probability of being highly sleep disturbed could be determined, eligible studies were required to include outcome scales that indicated either the severity or the frequency of symptoms or disturbance on a nonbinary scale. A binary response scale was, however, permitted if the phrasing of the question was such that a binary response would indicate being highly sleep disturbed, for example, “Is your sleep highly disturbed by noise from road noise?”. Studies reporting other measures of self-reported sleep not described above (e.g., perceived sleep quality, estimated total sleep time, morning sleepiness), and studies on objective sleep (e.g., polysomnography, actigraphy) or sleep medication use, were excluded.
Study Selection
All studies identified in the WHO evidence review19 for which data were already available for meta-analysis were included in the updated synthesis. We also identified studies published later than the WHO review from a scoping synthesis by van Kamp et al.28 Because van Kamp et al.28 included studies published up to June 2019 only, we further searched four electronic databases (Scopus, PubMed, Embase, PsycINFO), to identify more recent relevant studies published up to 31 December 2021. This search was done with the same search terms and strategy from van Kamp et al.28 that were relevant for traffic noise and self-reported sleep. The full electronic search strategy is given in Table S2. Any studies of which we were aware but that were not identified during the literature search were also screened for eligibility.
Two reviewers (M.G.S. and M.C.) independently and manually screened the title and abstract of each identified study against the study eligibility criteria. If eligibility could not be determined from the title and abstract alone, the full text was reviewed. Any differences in eligibility judgments were resolved by discussion and consensus, with input from a third reviewer (M.B.) if needed.
Data Extraction and Synthesis
The following variables were extracted by a single investigator from the original records for review by the authorship team: article title, authors, publication year, traffic mode, noise level, noise metric and time base, noise exposure methodology, sleep disturbance question(s) and response scale(s), study design, country, city, effective sample size, number of data points per respondent, and sleep disturbance point estimates. If data could not be extracted directly from the published articles and supplemental materials, we directly contacted all study authors for whom contact details were available to request data. We requested a list of relevant questions on sleep and the response scales used, the total number of respondents in 5-dB bins, and the percentage of respondents reporting being highly sleep disturbed in each 5-dB bin. We requested only these summary data, and no identifiable information on any study respondents was requested or obtained. If the study authors did not reply after they were sent two reminders, the contact was considered a nonresponse and the study was excluded.
The exposure variable of interest for the meta-analysis was average nighttime outdoor A-weighted noise level from a single traffic mode (air, road, and rail) during the night, hereafter termed , measured in decibels. A-weighting is a filter network that is used to simulate the nonlinear frequency response of human hearing. The night period was defined as 2300–0700 hours, in line with EU Environmental Noise Directive 2002/49/EC.29 In studies where noise levels were reported as a different metric, we converted to using the conversion formulae from Brink et al.18 given below. was not treated as a continuous variable but, rather, was categorized into 5-dB bins, following the approach used in the WHO review.19 For open-ended noise level categories, we assigned a noise level that was 2.5 dB above or below the cutoff, for instance, and would be coded as 47.5 dB and 52.5 dB, respectively. The midpoints of each 5-dB bin were used as the noise exposure levels in the statistical analyses.
The primary outcome of interest was the probability of self-reporting high sleep disturbance for a given noise level. We a priori defined three separate domains of questions that were used to determine sleep disturbance. First, “awakenings from sleep,” referring to the period between sleep onset and final awakening. These awakenings are defined as events where a participant wakes from sleep, regains consciousness, and recalls the awakening the following morning. Second, the “process of falling asleep,” defined as the transition from wakefulness to sleep. Third, “sleep disturbance,” defined as the internal or external interference with sleep onset or sleep continuity. Included studies had to address at least one of these domains in the form of at least one self-reported question. For each of these three question types, the coding of whether a respondent was highly sleep disturbed depended on the response scale used. For responses using 5- or 11-point scales referring to the severity of the disturbance, the top two and top three categories were, respectively, defined as highly sleep disturbed, following previous conventions for the International Commission on the Biological Effects of Noise (ICBEN) annoyance scale.30 For responses that referred to the frequency of symptoms, a frequency of “often” or at least three times per week was considered as highly sleep disturbed because this frequency of difficulty sleeping is a diagnostic criterion of insomnia.31 One study used a dichotomous filter question, “Do you have any trouble with your sleep?”, to determine if a respondent would answer a question on the frequency of difficulty falling asleep.32 Any responses of “no” to this filter question were coded as not highly sleep disturbed.
Study-Specific Exposure and Response Characterization
One study reported noise exposure as 24-h average levels ().33 These noise levels were converted to using the following conversion equations18:
One study reported road noise as the day-evening-night level (),34 which was converted to as follows18:
One study reported noise level as Livello di Valutazione del Aeroportuale (LVA),35 which is similar to the day-night level (), except that the night period is 7 h (2300–0600 hours) rather than 8 h.36 Formulae to convert directly from LVA to are unavailable; therefore, we made the following assumptions in converting to : The 1-h shorter night when using LVA means that the same exposure assessed as will be lower because applies a 10-dB penalty to the night period. We assume given that that is the difference in metrics with a 1-h difference in the night period (8 vs. 9 h) for aircraft noise.18 We then incorporated this difference into an appropriate conversion equation to convert from LVA to 18:
One study used a noise category that was 10-dB-wide (65–75 dB LVA).35 We subdivided these data into 5-dB-wide bins, assuming ()/2 respondents in each bin (35 respondents per bin) and the same prevalence of high sleep disturbance in each bin as in the 10-dB-wide category.
Two studies assessed noise exposure as both calculated long-term outdoor noise levels and measured indoor noise levels over 3–6 nights.20,21 We used the calculated outdoor noise levels as the exposure metric to be consistent with other studies in the meta-analysis.
In one study,21 sleep in the previous night was assessed repeatedly over several mornings. Because of these repeated measures, we first calculated the probability of being highly disturbed using all five to six responses per respondent. We then used these probabilities to determine the number of individuals that would have reported being highly sleep disturbed if only one response was obtained per person. In this way, each respondent contributed only a single data point to the analysis.
One study calculated exposure to railway traffic as including noise from trains, trams, and subways.37 The questions regarding “sleep disturbance by tram/subway noise” and “sleep disturbance by train noise” in this study were therefore averaged into a single sleep disturbance variable.
Risk of Bias and Quality of Evidence
The risk of bias at the outcome level within individual studies was assessed using the methodology developed within the WHO review,19 with the following two amendments to the assessment criteria (Table 1). First, in line with recommendations for cross-sectional studies by the National Institutes of Health,38 a study was considered at high risk of selection bias if the response rate was , down from the 60% criterion in the WHO review. Second, bias due to the sleep measurement outcome was not assessed because our updated analysis focused on only a single sleep measurement outcome (sleep questionnaires), whereas the WHO review included also heart rate or blood pressure, actigraphy, polysomnography, and other objective physiologic measurements. The risk of bias in each domain was assessed independently by two investigators (M.G.S. and M.C.). All studies were included in the meta-analysis regardless of the bias assessment.
Table 1.
Criteria for assessing risk of bias of individual studies (adapted from the WHO review19).
| Bias domain | Criteria | Risk of bias |
|---|---|---|
| A. Selection bias | Random sampling, areas selected based on noise exposure, response rate,a inclusion criteria not contingent on sleep and health conditions | Low |
| a. response rate,a or b. Non-random sampling, or c. Sampling not based on noise exposure, or d. Individuals were excluded based on sleep and health criteria |
High | |
| Insufficient information to make a judgment | Unclear | |
| B. Information bias (exposure assessment) | a. Based on measurements for at least 1 wk, or b. Based on a noise map that was verified by noise measurements, or c. Based on a noise map that was based on actual traffic data |
Low |
| a. Based on measurements of , or measurements were not continuous, or b. Based on a noise map that was not verified by noise measurements, or the predictions were not based on actual traffic data |
High | |
| Insufficient information to make a judgment | Unclear | |
| C. Bias due to confounding | All most-important confounders accounted for in analysis | Low |
| No accounting for important confounders | High | |
| Insufficient information to make a judgment | Unclear | |
| D. Reporting bias | Complete reporting of all outcomes analyzed including nonsignificant results | Low |
| Not all outcomes reported, underreporting methods or statistical analysis, not reporting conflicts of interest | High | |
| Insufficient information to make a judgment | Unclear |
Note: WHO, World Health Organization.
aThe 50% response rate criterion was based on recommendations for cross-sectional studies by the National Institutes of Health.38
To evaluate heterogeneity between studies, we calculated odds ratios (ORs) for each outcome within each study using binary logistic regression in SPSS (version 26; IBM Corp.). For consistency with the WHO review,19 the range of was not restricted in this analysis. Forest plots for all outcomes across studies were generated using RevMan (version 5.4.1; Cochrane Collaboration) using an inverse-variance (IV) random effects method. Heterogeneity between studies for each outcome was assessed using the statistic. We interpreted values using thresholds defined by the Cochrane Collaboration.39 Publication bias across studies was investigated using funnel plots of the individual study estimates.
The quality of evidence across studies for the effects of exposure to aircraft, road, and rail traffic noise on self-reported sleep outcomes where noise was specified, and self-reported sleep outcomes where noise was not specified, was assessed independently by two investigators using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) criteria.40 Any differences in the risk of bias assessments for individual studies, or in the quality of evidence across studies for each outcome (GRADE), were resolved by consensus with input from a third investigator if needed.
Meta-Analytic Approach
The primary goal of the meta-analysis was to generate updated exposure–response relationships for the probability of high sleep disturbance for each of the three disturbance types (awakenings, falling asleep, and sleep disturbance) for each traffic mode (air, road, and rail). In line with the WHO review,19 we also generated a combined estimate for high sleep disturbance across the three different types of disturbance questions, using the following approach: If a study included two or three relevant sleep disturbance questions, the combined estimate was calculated by averaging the responses to those questions for each respondent within a study. This approach was adopted so that each respondent would contribute only a single data point to the analysis of each separate outcome. If a study included only one sleep outcome, the combined estimate and the single study outcome assessed would be the same.
Data for individual studies were provided directly by the authors of each study, binned in 5-dB-wide noise categories. One line of data was created for each sleep disturbance question from each study respondent. For instance, if a study had 500 respondents in the noise category with a 47.5 dB midpoint, and 10% were classified as highly sleep disturbed, we generated 450 data lines with non-highly sleep disturbed respondents () and 50 data lines with highly sleep disturbed respondents (). Each data line also carried the midpoint of the 5-dB -exposure category, a three-level categorical variable for traffic mode (air, road, and rail), a dichotomous variable indicating whether questionnaire data originated from questions that did or did not explicitly mention noise as a source of disturbance in the question for each traffic mode, dichotomous study location indicated a European or non-European study, and a study identification number.
Statistical Analysis
Exposure–response relationships were generated with the following approach: Random study effect logistic regression models with (midpoint of the noise exposure category) as the only explanatory variable were performed with the NLMIXED procedure in SAS (version 9.4; SAS Institute, Inc.). This approach accounts for the fact that respondents were clustered within studies, and the weight of a study increases with its sample size. Analyses were restricted to levels between 40 and 65 dB because of inaccuracy in predicting noise levels and that the highest exposure limit common to all three traffic modes was 65 dB . Separate regression models were run stratified by the three traffic modes (air, road, or rail), four sleep disturbance outcome (awakenings, falling asleep, sleep disturbance, or combined estimate of all questions within a study), and the dichotomous noise-specificity of the disturbance question (noise mentioned or noise not mentioned), yielding a total separate regression analyses. Estimate statements were used to generate point estimates and 95% confidence intervals (CIs). Data are reported as dose–response curves and as ORs per 10-dB increase in .
To investigate whether a response differed depending between European and non-European studies location, we added study location as a covariate to the logistic regression model and repeated the analysis for the combined estimates of sleep disturbance. These analyses were restricted to the four outcomes where both European and non-European data were available.
We performed a sensitivity analysis to investigate the risks of exposure bias on sleep disturbance. We repeated the logistic regression for the combined estimates of sleep disturbance, restricted between 40–65 dB , and stratified analysis by studies that were judged to have a low or high risk of bias in the exposure assessment.
Results
Study Selection
Study identification, screening and selection are summarized in Figure 1. All 25 studies in the WHO review were included.19 Twenty-one studies published between January 2014 and June 2019 were identified by van Kamp et al.28 Our electronic search additionally identified 82 studies published later than June 2019, after excluding duplicates. After assessing the abstracts and, if needed, the full texts, 11 new studies eligible for the meta-analysis were identified. We also manually identified a further 2 studies that were not identified by the electronic literature searches [the UK Survey of Noise Attitudes (Civil Aviation Authority)41 and German Noise-Related Annoyance, Cognition and Health (NORAH)42 projects]. We manually extracted the study documents from project webpages41,42 and judged both studies to be eligible for inclusion after undergoing the standard screening protocol.
Figure 1.
![Figure 1 depicts a flowchart with three steps: identification, screening, and inclusion. Step 1: Identification: The previous version of the review included 25 studies. 21 records were published in June 2019 and earlier identified from scoping reviews (van Kamp and others [reference 28]). Records from databases ranging from July 2019 to December 2021 were identified, including 46 from SCOPUS, 40 from PubMed, 12 from PsycINFO, and 60 from Embase. 76 duplicate records were removed from the screening. There are two manual identifications of relevant scientific projects which are not identified by the electronic literature search. Step 2: Screening: 103 records were screened, from which 69 records were excluded. 34 reports were sought for retrieval and assessed for eligibility, excluding 8 reports related to noise which were not specific to home address, 1 report related to daytime noise only, 5 reports related to not self-reported sleep, 8 reports related to ineligible sleep outcome or response scale, and 1 report which was included in the previous meta-analysis. For new studies identified via other methods, 2 reports were sought for retrieval and 2 studies were assessed for eligibility. Step 3: Included: 13 new studies were included in the review. 38 studies were included in the review, excluding 1 study from the meta-analysis and 1 report of noise exposure specific to a home address that is unavailable from the meta-analysis. A total of 36 studies were included in the meta-analysis.](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/60bd/9272916/5dba896bd2df/ehp10197_f1.jpg)
Flow diagram of study identification, screening, and selection. “Study” refers to a data collection campaign including a defined group of participants and one or more outcomes. In one instance, a study was reported in multiple articles41,42 and is counted as study. “Report” is a journal article, preprint, conference abstract, study register entry, clinical study report, dissertation, unpublished manuscript, government report, or other document supplying relevant information about a particular study or studies.
Two studies initially deemed eligible could not be included in the meta-analysis43,44 because data could not be obtained or noise exposure specific to the home address was unavailable (Table S3). We therefore identified 11 studies in total published since the WHO review to include in the meta-analysis,20,21,32,34,35,37,41,42,45–47 in addition to the 25 studies included in the original review19 (Tables 2–4).
Table 2.
Studies on exposure to aircraft noise and self-reported sleep outcomes (adapted from the WHO review19).
| Outcome | Study | Location | Disturbance question and responses | Noise metric, (level range) | |
|---|---|---|---|---|---|
| Awakenings: noise mentioned (total ) | Nguyen et al.32,a | 559 | Hanoi, Vietnam | In daily life, how much do you feel disturbed when an aircraft passes by in the following cases: When you are awakened in your sleep? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (32.5–62.5 dB) |
| Nguyen et al.48 | 1,093 | Hanoi, Vietnam | In daily life, when an aeroplane passes by, to what degree are you disturbed in the following cases: When you are awakened in your sleep? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (37.5–57.5 dB) | |
| Yano et al.49 | 776 | Hanoi, Vietnam | Same as above | , 2200–0600 hours (37.5–57.5 dB) | |
| Nguyen et al.50 | 511 | Da Nang City, Vietnam | Same as above | , 2200–0600 hours (37.5–57.5 dB) | |
| Nguyen et al.51,52 | 804 | Hanoi, Vietnam | Same as above | , 2200–0600 hours (37.5–52.5 dB) | |
| Nguyen et al.53 | 870 | Ho Chi Minh City, Vietnam | Same as above | , 2200–0600 hours (42.5–62.5 dB) | |
| Falling asleep: noise mentioned (total ) | Nguyen et al.32,a | 545 | Hanoi, Vietnam | In daily life, how much do you feel disturbed when an aircraft passes by in the following cases: When it makes it difficult for you to fall asleep? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (32.5–62.5 dB) |
| NORAH42,a | 3,505 | Frankfurt, Germany 2011 | In the last 12 months aircraft noise has disturbed you when falling asleep? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (32.5–57.5 dB) | |
| NORAH42,a | 3,502 | Frankfurt, Germany 2012 | Same as above | , 2200–0600 hours (32.5–67.5 dB) | |
| NORAH42,a | 3,505 | Frankfurt, Germany 2013 | Same as above | , 2200–0600 hours (32.5–62.5 dB) | |
| NORAH42,a | 5,527 | Berlin, Germany 2012 | Same as above | , 2200–0600 hours (32.5–52.5 dB) | |
| NORAH42,a | 2,947 | Cologne-Bonn, Germany 2013 | Same as above | , 2200–0600 hours (32.5–67.5 dB) | |
| NORAH42,a | 1,970 | Stuttgart, Germany 2013 | Same as above | , 2200–0600 hours (32.5–52.5 dB) | |
| Nguyen et al.48 | 1,095 | Hanoi, Vietnam | In daily life, when an aeroplane passes by, at what degree are you disturbed in the following cases: When it makes it difficult for you to fall asleep? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (37.5–57.5 dB) | |
| Yano et al.49 | 780 | Hanoi, Vietnam | Same as above | , 2200–0600 hours (37.5–57.5 dB) | |
| Nguyen et al.50 | 512 | Da Nang City, Vietnam | Same as above | , 2200–0600 hours (37.5–52.5 dB) | |
| Nguyen et al.51,52 | 805 | Hanoi, Vietnam | Same as above | , 2200–0600 hours (37.5–52.5 dB) | |
| Nguyen et al.53 | 868 | Ho Chi Minh City, Vietnam | Same as above | , 2200–0600 hours (42.5–62.5 dB) | |
| Schreckenberg et al.54 | 2,308 | Germany | How much has aircraft noise in the last 12 months disturbed falling asleep? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (37.5–57.5 dB) | |
| Sleep disturbance: noise mentioned (total ) | Rocha et al.45,a | 396 | Atlanta, Georgia, USA | Thinking about the last 12 months or so, when you were at home, how much was your sleep disturbed by noise from aircraft? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2300–0700 hours (37.5–52.5 dB) |
| Brink et al.46,a | 2,925 | Switzerland | Thinking about the last twelve months at your home, during nighttime when you want to sleep, how much did aircraft noise bother, disturb, or annoy you? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2300–0700 hours (22.5–62.5 dB) | |
| Civil Aviation Authority41,a | 1,200 | United Kingdom | Thinking about the summer, when you were here at home, what number from 0 to 10 best shows the degree to which your sleep was disturbed by noise from aeroplanes? Not at all disturbed (0) to Extremely disturbed (10) (HSD 8,b 9,b 10b) | 2300–0700 hours, summer (37.5–62.5 dB) | |
| NORAH42,a | 3,505 | Frankfurt, Germany 2011 | In the last 12 months aircraft noise has disturbed you when sleeping in the night? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (32.5–57.5 dB) | |
| NORAH42,a | 3,502 | Frankfurt, Germany 2012 | Same as above | , 2200–0600 hours (32.5–67.5 dB) | |
| NORAH42,a | 3,505 | Frankfurt, Germany 2013 | Same as above | , 2200–0600 hours (32.5–62.5 dB) | |
| NORAH42,a | 5,519 | Berlin, Germany 2012 | Same as above | , 2200–0600 hours (32.5–52.5 dB) | |
| NORAH42,a | 2,939 | Cologne–Bonn, Germany 2013 | Same as above | , 2200–0600 hours (32.5–67.5 dB) | |
| NORAH42,a | 1,973 | Stuttgart, Germany 2013 | Same as above | , 2200–0600 hours (32.5–52.5 dB) | |
| Schreckenberg et al.54 | 2,309 | Germany | How much has aircraft noise in the last 12 months disturbed sleeping during the night? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (37.5–57.5 dB) | |
| Awakenings: noise not mentioned (total ) | Rocha et al.45,a | 309 | Atlanta, Georgia, USA | How often did the following occur during the past month: You had trouble sleeping because you wake up in the middle of the night or early morning? Not during the past month, Less than once a week, Once or twice a week, Three or more times a weekb | , 2300–0700 hours (37.5–52.5 dB) |
| Basner et al.20,a | 39 | Philadelphia, Pennsylvania, USA | During the past month, how often have you had trouble sleeping because you wake up in the middle of the night or early morning? Not during the past month, Less than once a week, Once or twice a week, Three or more times a weekb | , 2300–0700 hours (47.5–57.5 dB) | |
| Carugno et al.35,a | 400 | Bergamo, Italy | Frequent nocturnal awakening (last month)? No, Yesb | LVA, 2300–0600 hours (57.5–72.5 dB) | |
| Brink et al. (2003 study)55 | 1,450 | Switzerland | How often do you have the following symptoms: Problems with sleeping through? Never, Rarely, Sometimes, Often, Very Often,b Alwaysb | , 2200–0600 hours (27.5–62.5 dB) | |
| Brink et al. (2001 study)55 | 1,528 | Switzerland | Same as above | , 2200–0600 hours (27.5–62.5 dB) | |
| Falling asleep: noise not mentioned (total ) | Smith et al.21,a | 33 | Atlanta, Georgia, USA | Please evaluate last night’s sleep: falling asleep was Very easy (0) to Very difficult (10) (HSD 8,b 9,b 10b) | , 2300–0700 hours (37.5–57.5 dB) |
| Nguyen et al.32,a | 620 | Hanoi, Vietnam | Do you have any trouble with your sleep? Difficult to fall asleep? Rarely/not at all, Once or twice a week, Three or more times per weekb | , 2200–0600 hours (32.5–62.5 dB) | |
| Rocha et al.45,a | 309 | Atlanta, Georgia, USA | How often did the following occur during the past month: You had trouble sleeping because you cannot get to sleep within 30 minutes? Not during the past month, Less than once a week, Once or twice a week, Three or more times a weekb | , 2300–0700 hours (37.5–52.5 dB) | |
| Basner et al.20,a | 39 | Philadelphia, Pennsylvania, USA | During the past month, how often have you had trouble sleeping because you cannot get to sleep within 30 minutes? Not during the past month, Less than once a week, Once or twice a week, Three or more times a weekb | , 2300–0700 hours (47.5–57.5 dB) | |
| Carugno et al.35,a | 400 | Bergamo, Italy | Long time to fall asleep (last month)? No, Yesb | LVA, 2300–0600 hours (57.5–72.5 dB) | |
| Brink et al. (2003 study)55 | 1,450 | Switzerland | How often do you have the following symptoms: Problems falling asleep? Never, Rarely, Sometimes, Often, Very Often,b Alwaysb | , 2200–0600 hours (27.5–62.5 dB) | |
| Brink et al. (2001 study)55 | 1,528 | Switzerland | Same as above | , 2200–0600 hours (27.5–62.5 dB) | |
| Sleep disturbance: noise not mentioned (total ) | Brink56 | 195 | Switzerland | During the last 4 weeks, have you suffered from any of the following disorders or health problems? Difficulty in sleeping or insomnia? Not at all, Somewhat, Very Muchb | , 2200–0600 hours (32.5–52.5 dB) |
Note: HSD, highly sleep disturbed; , nighttime noise; LVA, Livello di Valutazione del Aeroportuale; NORAH, Noise-Related Annoyance, Cognition and Health; WHO, World Health Organization.
aStudies not included in the WHO review.19
bResponse alternatives designated as highly sleep disturbed.
Table 4.
Studies on exposure to railway noise and self-reported sleep outcomes (adapted from the WHO review19).
| Outcome | Study | Location | Disturbance question and responses | Noise metric (level range) | |
|---|---|---|---|---|---|
| Awakenings: noise mentioned (total ) | Bodin et al.33 | 2,344 | Sweden | Do you experience any of the following because of railway noise? You wake up? Never, Sometimes, Oftenb | (37.5–62.5 dB) |
| Sato et al.65 | 1,418 | Hokkaido, Japan | How much are you disturbed by awakening during nighttime by train passing? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0700 hours (27.5–62.5 dB) | |
| 1,549 | Kyushu, Japan | , 2200–0700 hours (27.5–72.5) | |||
| Falling asleep: noise mentioned (total ) | NORAH42,a | 3,266 | Frankfurt, Germany 2012 | In the last 12 months railway noise has disturbed you when falling asleep? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (27.5–82.5 dB) |
| Bodin et al.33 | 2,342 | Sweden | Do you experience any of the following because of railway noise? Difficulties falling asleep? Never, Sometimes, Oftenb | (37.5–62.5 dB) | |
| Schreckenberg66 | 1,198 | Germany | To what extent have the following outcomes of railway noise occurred in the past 12 months? Railway noise disturbs when falling asleep. Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (42.5–82.5 dB) | |
| Sato et al.65 | 1,418 | Hokkaido, Japan | How much are you disturbed in falling asleep by train passing? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0700 hours (27.5–62.5 dB) | |
| 1,562 | Kyushu, Japan | , 2200–0700 hours (27.5–72.5 dB) | |||
| Sleep disturbance: noise mentioned (total ) | NORAH42,a | 3,266 | Frankfurt, Germany 2012 | In the last 12 months railway noise has disturbed you when sleeping in the night? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (27.5–82.5 dB) |
| Brink et al.46,a | 3,543 | Switzerland | Thinking about the last twelve months at your home, during nighttime when you want to sleep, how much did railway noise bother, disturb, or annoy you? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2300–0700 hours (22.5–77.5 dB) | |
| Evandt et al.37,a | 12,476 | Norway | How disturbed have you been by noise during the night (falling asleep and waking up) from rail noise in the last 12 months? Not at all, Slightly, Rather, Very,b Extremelyb | , 2300–0700 hours, (37.5–67.5 dB) | |
| Schreckenberg66 | 1,199 | Germany | To what extent have the following outcomes of railway noise occurred in the past 12 months? Railway disturbs when sleeping during the night. Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (42.5–82.5 dB) | |
| Hong et al.61 | 610 | Korea | How much have you been disturbed in your sleep by railway noise at night when you are sleeping in your house over the last 12 months? 11 point scale used from 0 (not disturbed at all) to 10 (extremely disturbed) (HSD 8,b 9,b 10b) | , 2200–0700 hours (47.1–70 dB) | |
| Awakenings: noise not mentioned (total ) | Evandt et al.37,a | 12,577 | Norway | Have you noticed any of the following in the last 12 months? Repeatedly waking with difficulty falling back to sleep? No/rarely, Less than once a week, 1–2 times per week, 3–5 times per week,b Almost every nightb | , 2300–0700 hours, (37.5–67.5 dB) |
| Bodin et al.33 | 2,575 | Sweden | Do you wake up at night? Rarely/never, A few times per month, A few times a week, Almost every dayb | (37.5–62.5 dB) | |
| Frei et al.63 | 1,231 | Switzerland | How often does it happen, that you wake up at night multiple times? Never, Rarely, Sometimes, Oftenb | , 2200–0600 hours (27.5–57.5 dB) | |
| Falling asleep: noise not mentioned (total ) | Evandt et al.37,a | 12,745 | Norway | Have you noticed any of the following in the last 12 months? Difficulty falling asleep? No/rarely, Less than once a week, 1–2 times per week, 3–5 times per week,b Almost every nightb | , 2300–0700 hours, (37.5–67.5 dB) |
| Bodin et al.33 | 2,576 | Sweden | Do you have problems falling asleep? Rarely/never, A few times per month, A few times a week, Almost every dayb | (37.5–62.5 dB) | |
| Frei et al.63 | 1,232 | Switzerland | How often does it happen, that you cannot fall asleep well? Never, Rarely, Sometimes, Oftenb | , 2200–0600 hours (27.5–57.5 dB) | |
| Sleep disturbance: noise not mentioned (total ) | Frei et al.63 | 1,229 | Switzerland | How often does it happen that your sleep is restless? Never, Rarely, Sometimes, Oftenb | , 2200–0600 hours (27.5–57.5 dB) |
| Brink et al.56 | 4,685 | Switzerland | During the last 4 weeks, have you suffered from any of the following disorders or health problems? Difficulty in sleeping, or insomnia? Not at all, Somewhat, Very Muchb | , 2200–0600 hours (32.5–77.5 dB) |
Table 3.
Studies on exposure to road traffic noise and self-reported sleep outcomes (adapted from the WHO review19).
| Outcome | Study | Location | Disturbance question and responses | Noise metric (level range) | |
|---|---|---|---|---|---|
| Awakenings: noise mentioned (total ) | Bodin et al.33 | 2,438 | Sweden | Do you experience any of the following because of road traffic noise? You wake up? Never, Sometimes, Oftenb | (37.5–62.5 dB) |
| Phan et al.57 Shimoyama et al.58 | 1,454 | Hanoi, Vietnam | How much are you disturbed by awakening during nighttime by road traffic? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (62.5–77.5 dB) | |
| Phan et al.57 Shimoyama et al.58 | 1,460 | Ho Chi Minh City, Vietnam | Same as above | , 2200–0600 hours (67.5–77.5 dB) | |
| Phan et al.57 Shimoyama et al.58 | 479 | Da Nang, Vietnam | Same as above | , 2200–0600 hours (57.5–67.5 dB) | |
| Phan et al.57 Shimoyama et al.58 | 680 | Hue, Vietnam | Same as above | , 2200–0600 hours (52.5–72.5 dB) | |
| Phan et al.57 Shimoyama et al.58 | 777 | Thai Nguyen, Vietnam | Same as above | , 2200–0600 hours (52.5–67.5 dB) | |
| Sato et al.59 | 1,291 | Gothenburg, Sweden | Does the road traffic noise cause the following conditions? Awakening? No, Little Disturbed, Rather Disturbed, Very Disturbedb | , 2200–0700 hours (42.5–72.5 dB) | |
| Sato et al.59 | 819 | Kumamoto, Japan | Same as above | , 2200–0700 hours (47.5–77.5 dB) | |
| Sato et al.59 | 779 | Sapporo, Japan | Same as above | , 2200–0700 hours (52.5–67.5 dB) | |
| Falling asleep: noise mentioned (total ) | NORAH42,a | 3,162 | Frankfurt, Germany 2012 | In the last 12 months road traffic noise has disturbed you when falling asleep? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (32.5–72.5 dB) |
| Bodin et al.33 | 2,444 | Sweden | Do you experience any of the following because of road traffic noise? Difficulties falling asleep. Never, Sometimes, Oftenb | (37.5–62.5 dB) | |
| Phan et al.57 Shimoyama et al.58 | 1,471 | Hanoi, Vietnam | How much are you disturbed in falling asleep by road traffic? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (62.5–77.5 dB) | |
| Phan et al.57 Shimoyama et al.58 | 1,458 | Ho Chi Minh City, Vietnam | Same as above | , 2200–0600 hours (67.5–77.5 dB) | |
| Phan et al.57 Shimoyama et al.58 | 481 | Da Nang, Vietnam | Same as above | , 2200–0600 hours (57.5–67.5 dB) | |
| Phan et al.57 Shimoyama et al.58 | 682 | Hue, Vietnam | Same as above | , 2200–0600 hours (52.5–72.5 dB) | |
| Phan et al.57 Shimoyama et al.58 | 781 | Thai Nguyen, Vietnam | Same as above | , 2200–0600 hours (52.5–67.5 dB) | |
| Sato et al.59 | 1,302 | Gothenburg, Sweden | Does the road traffic noise cause the following conditions? Difficulty to fall asleep? No, Little Disturbed, Rather Disturbed, Very Disturbedb | , 2200–0700 hours (42.5–72.5 dB) | |
| Sato et al.59 | 814 | Kumamoto, Japan | Same as above | , 2200–0700 hours (47.5–77.5 dB) | |
| Sato et al.59 | 779 | Sapporo, Japan | Same as above | , 2200–0700 hours (52.5–67.5 dB) | |
| Sleep disturbance: noise mentioned (total ) | NORAH42,a | 3,162 | Frankfurt, Germany 2012 | In the last 12 months road traffic noise has disturbed you when sleeping in the night? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2200–0600 hours (32.5–72.5 dB) |
| Brink et al.46,a | 5,222 | Switzerland | Thinking about the last twelve months at your home, during nighttime when you want to sleep, how much did road noise bother, disturb, or annoy you? Not at all, Slightly, Moderately, Very,b Extremelyb | , 2300–0700 hours (22.5–72.5 dB) | |
| Evandt et al.37,a | 12,305 | Norway | How disturbed have you been by noise during the night (falling asleep and waking up) from road noise in the last 12 months? Not at all, Slightly, Rather, Very,b Extremelyb | , 2300–0700 hours (37.5–67.5 dB) | |
| Brown et al.60 | 8,841 | Hong Kong | How much is your sleep disturbed by road traffic noise? 11 point scale used from 0 (not disturbed at all) to 10 (extremely disturbed) (HSD 8,b 9,b 10b) | (42.5–67.5 dB) | |
| Hong et al.61 | 550 | Korea | How much have you been disturbed in your sleep by road traffic noise at night when you are sleeping in your house over the last 12 months? 11 point scale used from 0 (not disturbed at all) to 10 (extremely disturbed) (HSD 8,b 9,b 10b) | , 2200–0700 hours (50.0–73.0 dB) | |
| Ristovska et al.62 | 510 | Macedonia | Do you think that your sleep was disturbed due to night-time noise or noise events during the night in the last twelve months and more? Not at all, Very little, Moderate, Highb, Very Highb | , 2300–0700 hours (42.5–62.5 dB) | |
| Awakenings: noise not mentioned (total ) | Martens et al.34,a | 14,622 | The Netherlands | How often during the past 4 weeks did you awaken during your sleep time and have trouble falling asleep again? Never, Seldom, Sometimes, Often,b Most of the time,b Alwaysb | (32.5–72.5 dB) |
| Evandt et al.37,a | 12,113 | Norway | Have you noticed any of the following in the last 12 months? Repeatedly waking with difficulty falling back to sleep? No/rarely, Less than once a week, 1–2 times per week, 3–5 times per week,b Almost every nightb | , 2300–0700 hours, (37.5–67.5 dB) | |
| Bodin et al.33 | 2,519 | Sweden | Do you wake up at night? Rarely/never, A few times per month, A few times a week, Almost every dayb | (37.5–62.5 dB) | |
| Frei et al.63 | 1,231 | Switzerland | How often does it happen, that you wake up at night multiple times? Never, Rarely, Sometimes, Oftenb | , 2200–0600 hours (27.5–62.5 dB) | |
| Halonen et al.64 | 6,853 | Finland | How many times during the past 4 weeks have you had the following symptoms? Frequently waking up during the night. Never, 1 per month, 1 per week, 2–4 per week,b 5–6 per week,b nearly every nightb | , 2200–0700 hours (42.5–57.5 dB) | |
| Falling asleep: noise not mentioned (total ) | Bartels et al.47 | 2,188 | Sweden | During the past 12 months, how often have you had problems falling asleep in the evening? Never/seldom, A few times per month, Once per week, Several times per week,b Every dayb | , 2200–0600 hours (22.5–72.5 dB) |
| Martens et al.34,a | 14,616 | The Netherlands | How often during the past 4 weeks did you have trouble falling asleep? Never, Seldom, Sometimes, Often,b Most of the time,b Alwaysb | (32.5–72.5 dB) | |
| Evandt et al.37,a | 12,276 | Norway | Have you noticed any of the following in the last 12 months? Difficulty falling asleep? No/rarely, Less than once a week, 1–2 times per week, 3–5 times per week,b Almost every nightb | , 2300–0700 hours, (37.5–67.5 dB) | |
| Bodin et al.33 | 2,520 | Sweden | Do you have problems falling asleep? Rarely/never, A few times per month, A few times a week, Almost every dayb | (37.5–62.5 dB) | |
| Frei et al.63 | 1,232 | Switzerland | How often does it happen, that you cannot fall asleep well? Never, Rarely, Sometimes, Oftenb | , 2200–0600 hours (27.5–62.5 dB) | |
| Halonen et al.64 | 6,793 | Finland | How many times during the past 4 weeks have you had the following symptoms? Difficulty falling asleep? Never, 1 per month, 1 per week, 2–4 per week,b 5–6 per week,b Nearly every nightb | , 2200–0700 hours (42.5–57.5 dB) | |
| Sleep disturbance: noise not mentioned (total ) | Martens et al.34,a | 14,619 | The Netherlands | How often during the past 4 weeks did you feel that your sleep was not quiet (moving restlessly, feeling tense, speaking, etc.) while sleeping? Never, Seldom, Sometimes, Often,b Most of the time,b Alwaysb | (32.5–72.5 dB) |
| Frei et al.63 | 1,229 | Switzerland | How often does it happen that your sleep is restless? Never, Rarely, Sometimes, Oftenb | , 2200–0600 hours (27.5–62.5 dB) | |
| Brink et al.56 | 8,245 | Switzerland | During the last 4 weeks, have you suffered from any of the following disorders or health problems? Difficulty in sleeping, or insomnia? Not at all, Somewhat, Very Muchb | , 2200–0600 hours (32.5–77.5 dB) |
Note: HSD, highly sleep disturbed; , air and road traffic noise at 24-h average levels; , day-evening-night level; , nighttime noise; NORAH, Noise-Related Annoyance, Cognition and Health; WHO, World Health Organization.
aStudies not included in the WHO review.19
bResponse alternatives designated as highly sleep disturbed.
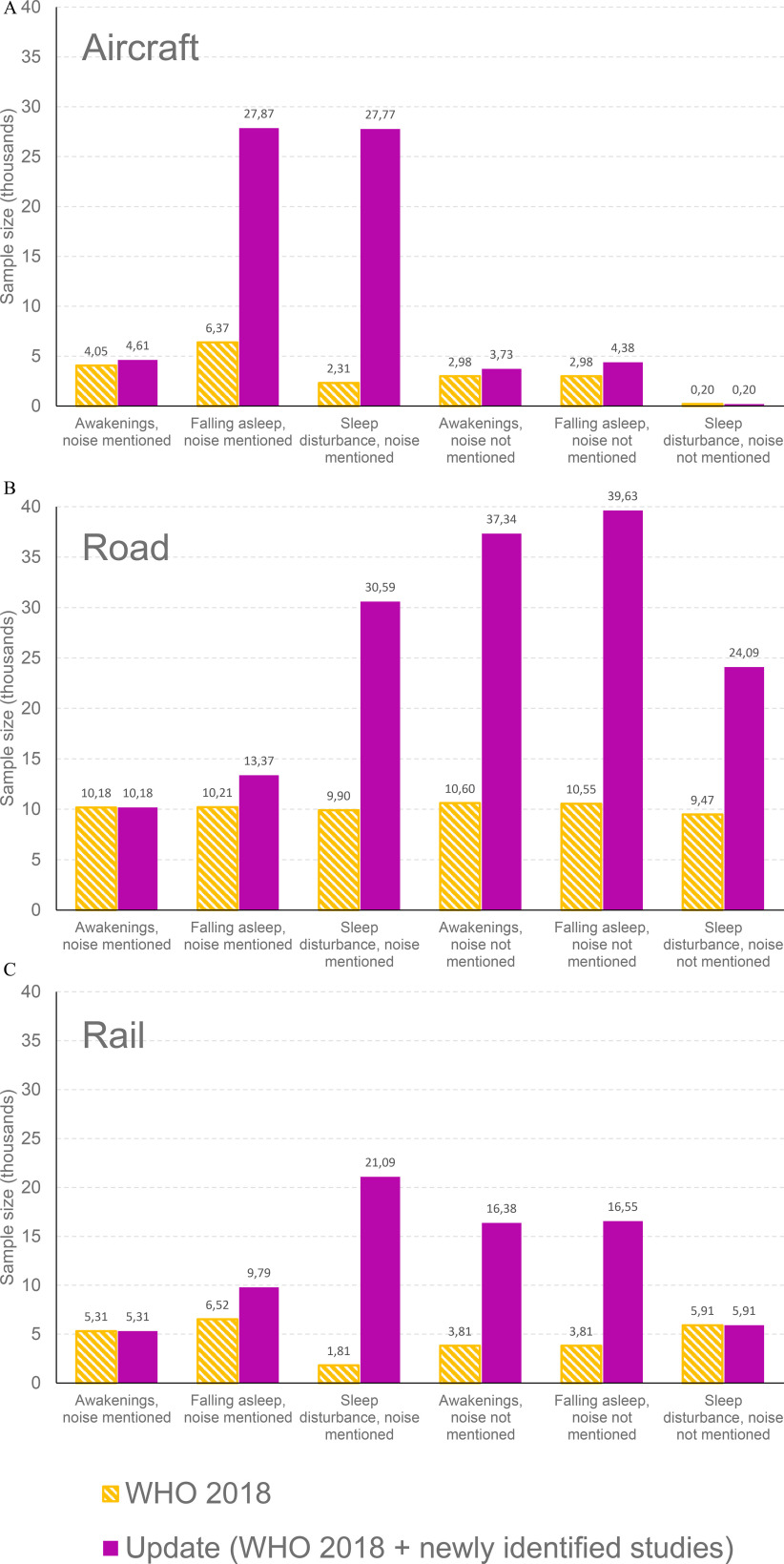
Comparison with Previous WHO Review
The effective sample size for each sleep outcome and for each traffic mode, determined using all data in the updated analysis (responses from the WHO analysis plus the 11 newly identified studies) is compared against the sample sizes from the WHO analyses in Figure 2. Sample sizes for the combined estimates where responses to multiple questions were averaged within studies are given in Figure S1. For all three traffic modes, our updated analysis includes a substantially higher number of respondents for all self-reported disturbance questions.
Figure 2.
Effective sample sizes for (A) aircraft, (B) road, and (C) rail for each sleep disturbance question in the present updated analysis, determined from the original WHO analysis plus the 11 newly included studies, compared with sample sizes from the WHO 2018 review only.19 Note: WHO, World Health Organization.
Sleep Disturbance by Noise: Individual Studies
ORs for the probability of being highly sleep disturbed by noise for each study are shown in Figure 3 (aircraft), Figure 4 (road traffic), and Figure 5 (railway). Also shown is the risk of bias assessment for each study (Table S4 for the rationale for each judgment). With a 10-dB increase in , there was a statistically significant probability of being sleep disturbed by noise for all three traffic modes. This increased probability was independent of whether noise was specifically mentioned in the sleep question. There were significant differences between the subgroups for each traffic mode, and the ORs were lower in studies that did not specifically mention noise. There was considerable heterogeneity () for all three traffic modes when the sleep question mentioned noise. There was substantial heterogeneity () between studies of aircraft and road traffic when the sleep question did not specifically mention noise. The heterogeneity between studies of railway noise was deemed unimportant () when the sleep question did not specifically mention noise.
Figure 3.
![Figure 3 is a forest plot, plotting study of subgroup and odds ratio inverse variance, random, 95 percent confidence intervals year, including (bottom to top) Aircraft: Non noise specific: Total (95 percent confidence intervals), 2.30 (1.87, 2.82); Test for subgroup differences: Chi squared equals 10.85, degrees of freedom equals 1 (uppercase p equals 0.0010); I squared equals 90.8 precent. Test for overall effect: uppercase z equals 7.91 (uppercase p equals 0.00001); Heterogeneity: Tau squared equals 0.15; Chi squared equals 190.63, degrees of freedom equals 17 (uppercase p equals 0.00001); I squared equals 91 precent. Test for overall effect: uppercase z equals 2.29 (uppercase p equals 0.02); Heterogeneity: Tau squared equals 0.12; Chi squared equals 23.78, degrees of freedom equals 6 (uppercase p equals 0.0006); I squared equals 75 precent; Subtotal (95 percent confidence intervals), 1.48 [1.06, 2.06]; Nguyen and others [32], 2.74 [1.99, 3.77] 2020; Rocha and others [45], 1.49 [1.08, 2.07] 2019; Basner and others [20], 24.43 [0.38, 1582.99] 2019; Carugno and others [35], 1.40 [0.79, 2.50] 2018; Brink [55], 0.33 [0.06, 1.73] 2011; Brink and others (2001 data) [55], 1.22 [0.94, 1.58] 2005; Brink and others (2003 data) [55], 1.20 [0.92, 1.57] 2005; Aircraft: Noise specific: Test for overall effect: uppercase z equals 10.16 (uppercase p less than 0.00001); Heterogeneity: Tau squared equals 0.09; Chi squared equals 87.86, degrees of freedom equals 10 (uppercase p equals 0.0001); I squared equals 89 precent; Subtotal (95% CI), 2.84 [2.32, 3.47]; Nguyen and others [32], 6.90 [4.78, 9.96] 2020; Rocha and others [45], 3.72 [2.61, 5.31] 2019; Brink and others [46], 4.48 [3.76, 5.32] 2019; Civil Air Authority [41], 2.04 [1.47, 2.83] 2017; Yano and others [49] 2.34 [1.69, 3.24] 2015; Nguyen and others [48], 2.70 [2.13, 3.42] 2015; NORAH [42], 2.83 [2.68, 2.98] 2015; Nguyen et al. [50], 1.14 [0.69, 1.88] 2013; Nguyen and others [51, 52], 1.46 [0.99, 2.16] 2011; Schreckenberg and others [54], 2.44 [2.05, 2.91] 2009; and Nguyen and others [53], 4.65 [2.96, 7.31] 2009 (y-axis) across less disturbed, ranging from 0.05 to 0.2 in increments of 0.15 and 0.2 to 1 in increments of 0.8, and more disturbed, ranging from 1 to 5 in increments of 4 and 5 to 20 in increments of 15 (x-axis) for Risk of bias, including selection bias, exposure assessment bias, bias due to confounding, and reporting bias.](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/60bd/9272916/74214aaacab5/ehp10197_f3.jpg)
Forest plot for the odds of being highly sleep disturbed by aircraft noise per 10-dB increase in (combined estimate derived from all relevant outcomes within studies). Subgroups are presented for questions that mentioned noise as the source of the disturbance, and questions that did not specify noise as the source of the disturbance. Risk of bias: A: selection bias; B: exposure assessment; C: confounding; D: reporting bias. Green () denotes low risk of bias, red (–) denotes high risk of bias, yellow (?) denotes unclear risk of bias. Plots were generated using an inverse-variance (IV) random effects method across the full noise range for each individual study (not restricted to 40–65 dB ). Note: CI, confidence interval; df, degrees of freedom; , nighttime noise; NORAH, Noise-Related Annoyance, Cognition and Health.
Figure 4.
![Figure 4 is a forest plot, plotting Study or subgroup and odds ratio inverse variance, random, 95 percent confidence intervals year, including (bottom to top) Road: Non noise specific: Total (95 percent confidence intervals), 1.80 [1.50, 2.17]; Test for subgroup differences: Chi squared equals 43.62, degrees of freedom equals 1 (uppercase p equals 0.00001); I squared equals 97.7 precent. Test for overall effect: uppercase z equals 6.26 (uppercase p equals 0.00001); Heterogeneity: Tau squared equals 0.16; Chi squared equals 466.45, degrees of freedom equals 21 (uppercase p equals 0.00001); I squared equals 95 precent. Test for overall effect: uppercase z equals 3.14 (uppercase p equals 0.002); Heterogeneity: Tau squared equals 0.01; Chi squared equals 17.44, degrees of freedom equals 6 (uppercase p equals 0.0008); I squared equals 66 precent; Subtotal (95 percent confidence intervals), 1.13 [1.05, 1.22]; Bartels and others [47], 1.01 [0.88, 1.15] 2021; Martens and others [34], 1.10 [1.02, 1.18] 2018; Evandt and others [37], 1.20 [1.11, 1.30] 2017; Bodin and others [33], 1.12 [0.96, 1.31] 2015; Frei and others [63], 1.22 [1.03, 1.44] 2014; Halonen and others [64], 0.99 [0.88, 1.12] 2012; Brink [56], 1.43 [1.18, 1.72] 2011; Road: Noise specific: Test for overall effect: uppercase z equals 8.28 (uppercase p equals 0.00001); Heterogeneity: Tau squared equals 0.11; Chi squared equals 95.40, degrees of freedom equals 14 (uppercase p less than 0.00001); I squared equals 85 precent; Subtotal (95 percent confidence intervals), 2.32 [1.90, 2.84]; Brink and others [46], 2.56 [2.27, 2.90] 2019; Evandt and others [37], 3.19 [2.68, 3.78] 2017; NORAH [42], 1.92 [1.63, 2.26] 2015; Brown and others [60], 2.55 [2.15, 3.02] 2015; Bodin and others [33], 2.44 [1.84, 3.24] 2015; Phan and others Thai Nguyen [57], 19.93 [8.27, 48.02] 2010; Phan and others Hue [57], 1.49 [0.98, 2.26] 2010; Phan and others Ho Chi Minh City [57] 1.13 [0.76, 1.70] 2010; Phan and others Hanoi [57], 1.28 [0.86, 1.90] 2010; Phan and others Da Nang [57], 12.49 [4.64, 33.60] 2010; Hong and others [61], 1.26 [0.74, 2.14] 2010; Ristovska and others [62], 2.45 [1.71, 3.50] 2009; Sato and others Kumamoto [59], 1.41 [0.94, 2.12] 2002; Sato and others Gothenburg [57], 3.50 [2.34, 5.22] 2002; and Sato and others Sapporo [59], 2.66 [1.20, 5.89] 2002 (y-axis) across Less disturbed, ranging from 0.02 to 0.1 in increments of 0.1 and 0.1 to 1 in increments of 0.9, and 1 to 10 in increments of 9 and 10 to 50 in increments of 40 (x-axis) for risk of bias, including selection bias, exposure assessment bias, bias due to confounding, and reporting bias.](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/60bd/9272916/7e51b25c35f1/ehp10197_f4.jpg)
Forest plot for the odds of being highly sleep disturbed by road noise per 10-dB increase in (combined estimate derived from all relevant outcomes within studies). Subgroups are presented for questions that mentioned noise as the source of the disturbance, and questions that did not specify noise as the source of the disturbance. Risk of bias: A: selection bias; B: exposure assessment; C: confounding; D: reporting bias. Green () denotes low risk of bias, red (–) denotes high risk of bias, yellow (?) denotes unclear risk of bias. Plots were generated using an inverse-variance (IV) random effects method across the full noise range for each individual study (not restricted to 40–65 dB ). Note: CI, confidence interval; df, degrees of freedom; , nighttime noise; NORAH, Noise-Related Annoyance, Cognition and Health.
Figure 5.
![Figure 5 is a forest plot, plotting Study or subgroup and odds ratio inverse variance, random, 95 percent confidence intervals year, including (bottom to top) Total (95 percent confidence intervals), 2.14 [1.54, 2.97]; Test for subgroup differences: Chi squared equals 62.31, degrees of freedom equals 1 (uppercase p equals 0.00001); I squared equals 98.4 precent. Test for overall effect: uppercase z equals 4.55 (uppercase p equals 0. 00001); Heterogeneity: Tau squared equals 0.32; Chi squared equals 490.79, degrees of freedom equals 11 (uppercase p equals 0.00001); I squared equals 98 precent. Test for overall effect: uppercase z equals 2.44 (uppercase p equals 0.01); Heterogeneity: Tau squared equals 0.00; Chi squared equals 0.39, degrees of freedom equals 3 (uppercase p equals 0.94); I squared equals 0 precent; Subtotal (95 percent confidence intervals), 1.09 [1.02, 1.18]; Evandt and others [37], 1.12 [1.00, 1.25] 2017; Bodin and others [33], 1.09 [0.95, 1.24] 2015; Frei and others [63], 1.06 [0.73, 1.53] 2014; Brink [56], 1.06 [0.92, 1.23] 2011; Railway: Noise specific: Test for overall effect: uppercase z equals 8.97 (uppercase p equals 0.00001); Heterogeneity: Tau squared equals 0.10; Chi squared equals 88.70, degrees of freedom equals 7 (uppercase p less than 0.00001); I squared equals 92 precent; Subtotal (95 percent confidence intervals), 3.01 [2.37, 3.83]; Brink and others [46], 3.43 [3.03, 3.88] 2019; Evandt and others [37], 4.77 [4.02, 5.66] 2017; Bodin and others [33], 5.18 [3.44, 7.79] 2015; NORAH [42], 2.11 [1.85, 2.40] 2015; Schreckenberg and others [66], 3.00 [2.56, 3.50] 2013; Hong and others [61], 2.98 [2.14, 4.17] 2010; Sato and others Hokkaido [65], 2.36 [1.62, 3.44] 2004; and Sato and others Kyushu [65], 1.94 [1.61, 2.34] 2004 (y-axis) across less disturbed, ranging from 0.1 to 0.2 in increments of 0.1, 0.2 to 0.5 in increments of 0.3, and 0.5 to 1 in increments 0.5, and more disturbed, ranging from 1 to 2 in unit increments, 2 to 5 in increments of 3, and 5 to 10 in increments of 5 (x-axis) for risk of bias, including selection bias, exposure assessment bias, bias due to confounding, and reporting bias.](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/60bd/9272916/a799850e670f/ehp10197_f5.jpg)
Forest plot for the odds of being highly sleep disturbed by railway noise per 10-dB increase in (combined estimate derived from all relevant outcomes within studies). Subgroups are presented for questions that mentioned noise as the source of the disturbance, and questions that did not specify noise as the source of the disturbance. Risk of bias: A: selection bias; B: exposure assessment; C: confounding; D: reporting bias. Green () denotes low risk of bias, red (–) denotes high risk of bias, yellow (?) denotes unclear risk of bias. Plots were generated using an inverse-variance (IV) random effects method across the full noise range for each individual study (not restricted to 40–65 dB ). Note: CI, confidence interval; , nighttime noise; NORAH, Noise-Related Annoyance, Cognition and Health.
Sleep Disturbance by Noise: Overall Analysis
The ORs for the probability of being highly sleep disturbed by nighttime noise, calculated using data from all studies and restricted to 40–65 dB , are presented in Table 5. When the question mentioned noise as the source of disturbance, there was a higher probability of being significantly disturbed by noise for all three outcomes, as well as for the combined estimate. When the question did not mention noise, significant relationships were observed only for aircraft and road noise, and for only some of the sleep disturbance outcomes. A substantial proportion of studies into road and railway noise were judged as having a high risk of exposure assessment bias when the question mentioned noise. We decided post hoc to perform a sensitivity analysis for these traffic types, to elucidate the influence of these risks of bias on sleep disturbance. There was a greater probability of being highly sleep disturbed by noise in studies with a low risk of exposure assessment bias compared with studies with a high risk of exposure assessment bias (Table S5).
Table 5.
Odds ratios per 10-dB increase in for the percent highly sleep disturbed by aircraft, road, and railway traffic noise.
| Noise source | Outcome | Noise mentioned as source of disturbance | Noise not mentioned as source of disturbance | ||||
|---|---|---|---|---|---|---|---|
| Studies ()a | Sample size ()a | OR per 10 dB (95% CI) | Studies ()a | Sample size ()a | OR per 10 dB (95% CI) | ||
| Aircraft noise | Awakenings | 6 | 4,137 | 2.34 (1.87, 2.93) | 5 | 2,571 | 1.11 (0.81, 1.53) |
| Falling asleep | 8 | 17,107 | 2.09 (1.91, 2.28) | 7 | 3,120 | 1.67 (1.27, 2.19) | |
| Sleep disturbance | 5 | 15,345 | 2.28 (2.03, 2.56) | 1 | 153 | 1.22 (0.08, 18.20) | |
| Combined estimate | 11 | 19,488 | 2.18 (2.01, 2.36) | 8 | 3,275 | 1.52 (1.20, 1.93) | |
| Road noise | Awakenings | 8 | 5,355 | 1.75 (1.24, 2.47) | 5 | 29,358 | 1.10 (1.01, 1.20) |
| Falling asleep | 9 | 7,754 | 2.31 (1.85, 2.89) | 6 | 31,136 | 1.15 (1.08, 1.23) | |
| Sleep disturbance | 6 | 26,372 | 2.57 (2.26, 2.93) | 3 | 18,052 | 1.15 (0.93, 1.43) | |
| Combined estimate | 14 | 31,738 | 2.52 (2.28, 2.79) | 7 | 38,380 | 1.14 (1.08, 1.21) | |
| Railway noise | Awakenings | 3 | 3,576 | 2.54 (1.49, 4.33) | 3 | 3,197 | 1.09 (0.78, 1.53) |
| Falling asleep | 5 | 6,730 | 2.70 (2.14, 3.42) | 3 | 3,219 | 1.27 (0.84, 1.90) | |
| Sleep disturbance | 5 | 7,262 | 3.35 (2.75, 4.09) | 2 | 1,168 | 1.27 (0.11, 15.15) | |
| Combined estimate | 8 | 10,846 | 2.97 (2.57, 3.43) | 4 | 4,326 | 1.17 (0.91, 1.49) | |
Note: ORs were calculated in logistic regression models with included as the only fixed effect and study included as a random effect, restricted to the noise exposure range 40–65 dB . Models were run separately for each traffic mode and for sleep questionnaire outcomes that did or did not mention noise. The combined estimate was calculated using average responses of the awakening, falling asleep, and sleep disturbance questions within studies. CI, confidence interval; , nighttime noise; OR, odds ratio.
aIn the range 40–65 dB for which ORs were calculated.
The ORs for the probability of being highly sleep disturbed, stratified by studies performed in Europe and outside of Europe, are given in Table S6. Analyses were restricted to aircraft, road, and railway traffic when the question mentioned noise, plus aircraft traffic when noise was not specifically mentioned, because these were the outcomes where sleep disturbance data were available for both locations. Non-European study respondents were more highly sleep disturbed by railway traffic when noise was mentioned in the question and by aircraft traffic when noise was not specifically mentioned. Non-Europeans were also less disturbed by road traffic when noise was mentioned. However, none of these effects were significant.
Exposure–Response Curves: Questions Specifically Mentioning Noise
The exposure–response curves for the probability of being highly sleep disturbed, derived using data from questions that specifically mentioned noise, are given in Figure 6. Second-order polynomial equations for each curve are given in Table S7. Disturbance was substantially higher for aircraft noise for all three disturbance questions than for road or railway noise of the same level. Disturbance was similar for road and rail noise at low noise levels, and it was slightly higher for railway noise than road noise at higher noise levels.
Figure 6.
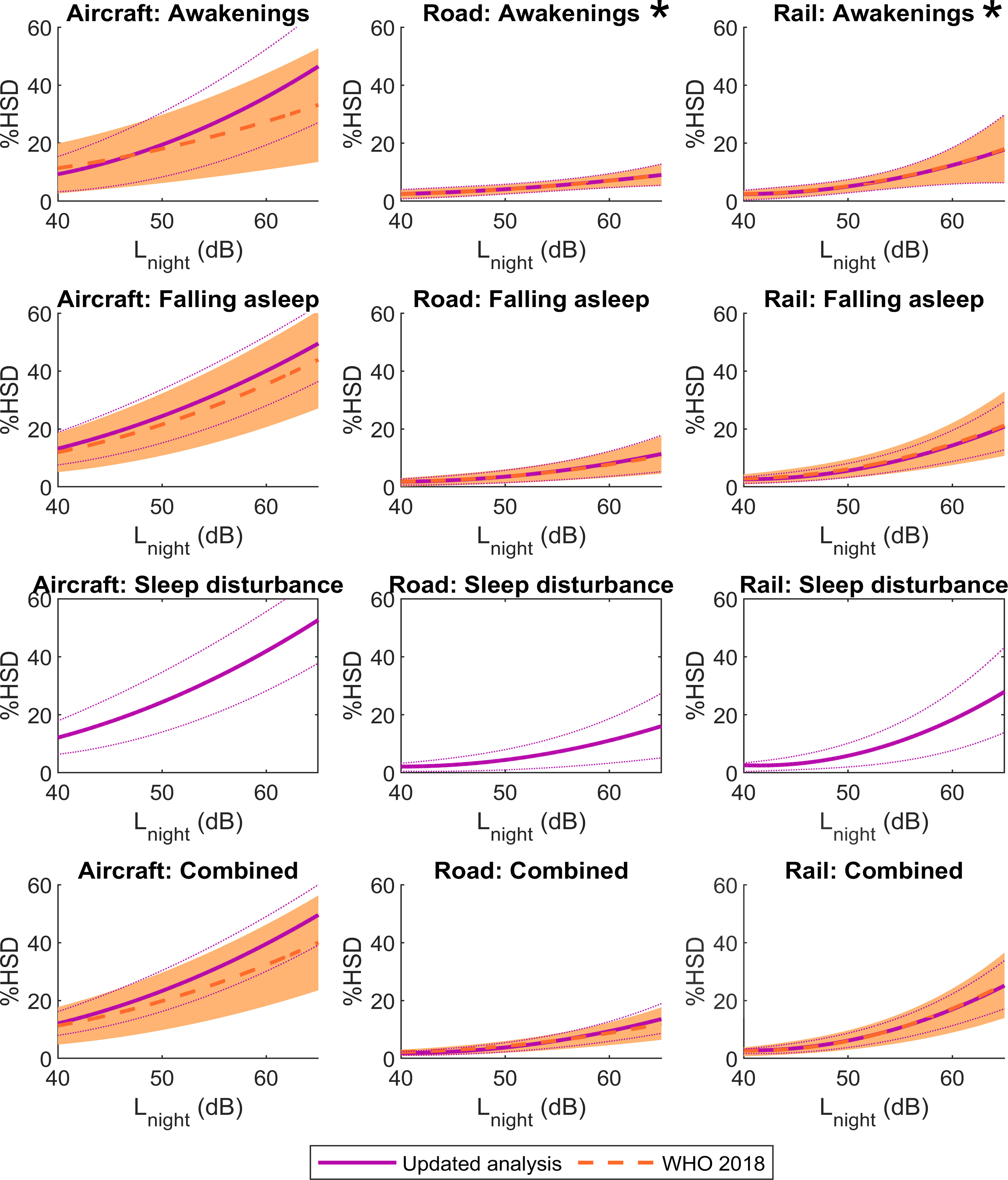
Probability of being highly sleep disturbed (%HSD) by nighttime noise, determined via questions that mention noise as the source of disturbance, stratified by disturbance question and traffic mode. Exposure–response relationships were derived using all available data, from the original WHO review19 and the 11 newly identified studies. Results of the present updated analysis (solid purple lines with dotted 95% CIs) are compared against results of the 2018 WHO review19 (dashed orange lines with shaded 95% CIs). Relationships for the sleep disturbance questions were not calculated previously. Asterisks (*) indicate sleep outcomes for which no new studies have been published since the WHO review. Parameter estimates were calculated in logistic regression models with included as the only fixed effect and study included as a random effect, restricted to the noise exposure range 40–65 dB . Models were run separately for each traffic mode and disturbance question. The combined estimate was calculated using average responses of the awakening, falling asleep, and sleep disturbance questions within studies. Note: CI, confidence interval; , nighttime noise; WHO, World Health Organization.
We compared the updated exposure–response curves to curves derived using only the 11 new studies published since the WHO review19 (Figure 7). This was done for the combined estimate only, given that there was a limited sample size for certain sleep questions in these recent studies. For aircraft noise, the recent studies indicated a higher probability of being highly sleep disturbed compared with the analysis incorporating all available data. For road traffic noise, the point estimates were slightly higher at the highest noise levels in the recent studies compared with the overall analysis (2.6% higher at 65 dB ). For railway noise, the recent studies were essentially identical to the overall analysis.
Figure 7.
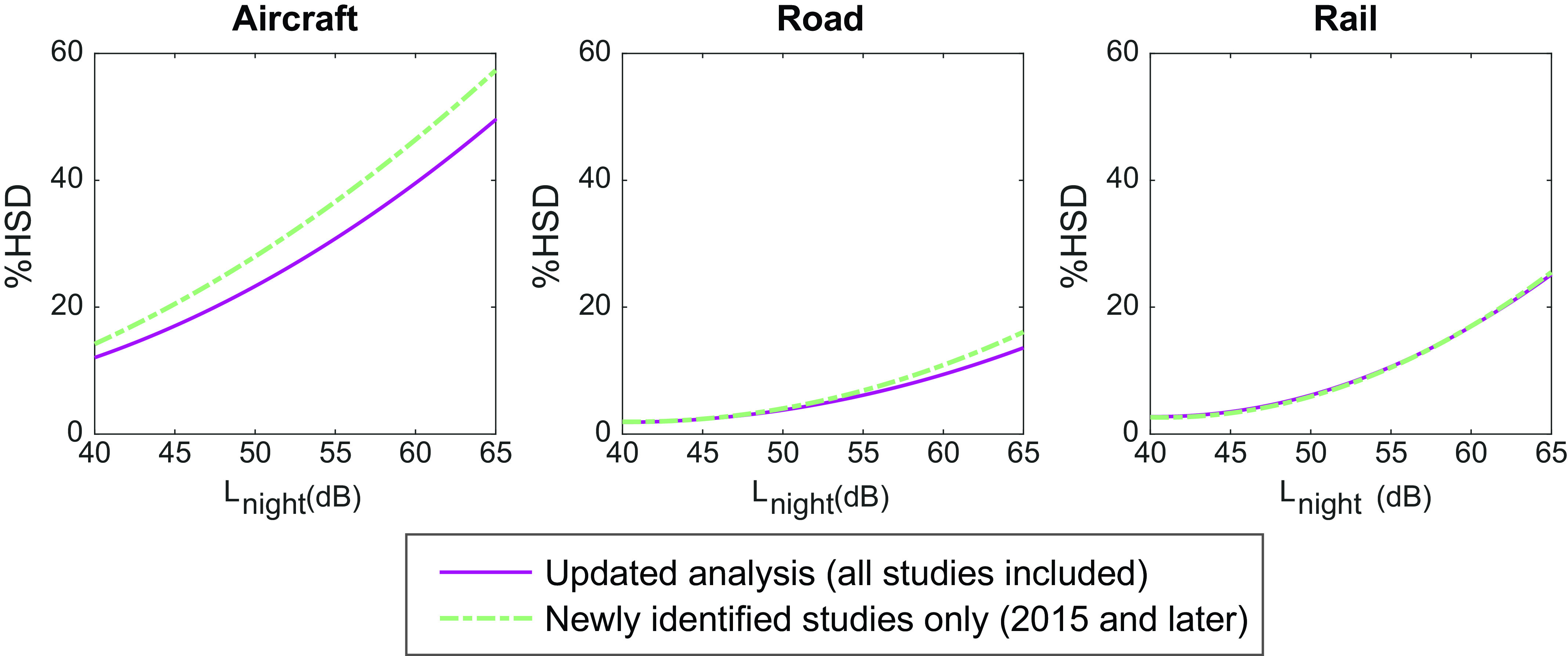
Exposure–response relationships for the probability of being highly sleep disturbed (%HSD) by nighttime noise for questions that mention noise. Curves are shown for the updated analysis that includes all available data (solid purple lines), and for analysis including only newly identified studies published after the WHO review19 (dashed green lines). Data are calculated as the combined response using average responses of the awakening, falling asleep, and sleep disturbance questions within studies, determined as the within-study average of disturbance questions that explicitly mentioned noise as the source of sleep disturbance. Parameter estimates were calculated in logistic regression models with included as the only fixed effect and study included as a random effect, restricted to the noise exposure range 40–65 dB . Models were run separately for each traffic mode. Note: , nighttime noise; WHO, World Health Organization.
The exposure–response curves calculated in the original WHO review19 are given in Figure 6. Relationships for the sleep disturbance question were not calculated in the WHO review due to an insufficient number of studies at the time. Point estimates for aircraft noise are generally slightly higher in the present analyses compared with the previous relationships, particularly at higher noise levels, although they still lie within the 95% CIs of the WHO review. Point estimates for the falling asleep and combined estimate outcomes are almost identical for road and rail traffic in the present analysis compared with the WHO review. For each disturbance question and traffic mode, all of the previous curves lie within the 95% CIs of the updated analyses. As expected, given that no additional studies were included for awakenings by aircraft or road traffic, exposure–response curves for these outcomes were identical to curves in the WHO review.
Exposure–Response Curves: Questions Not Specifically Mentioning Noise
The exposure–response curves for the probability of being highly sleep disturbed, derived using data from general sleep questions that did not specifically mention noise, are given in Figure 8. Second-order polynomial equations for each curve are given in Table S7. With increasing , there was a small increase in disturbance for all questions, although the gradient of the exposure–response curves was generally smaller compared with questions that mentioned noise (Figure 6). The differences between the three traffic modes were also less clear compared with questions mentioning noise (Figure 6).
Figure 8.
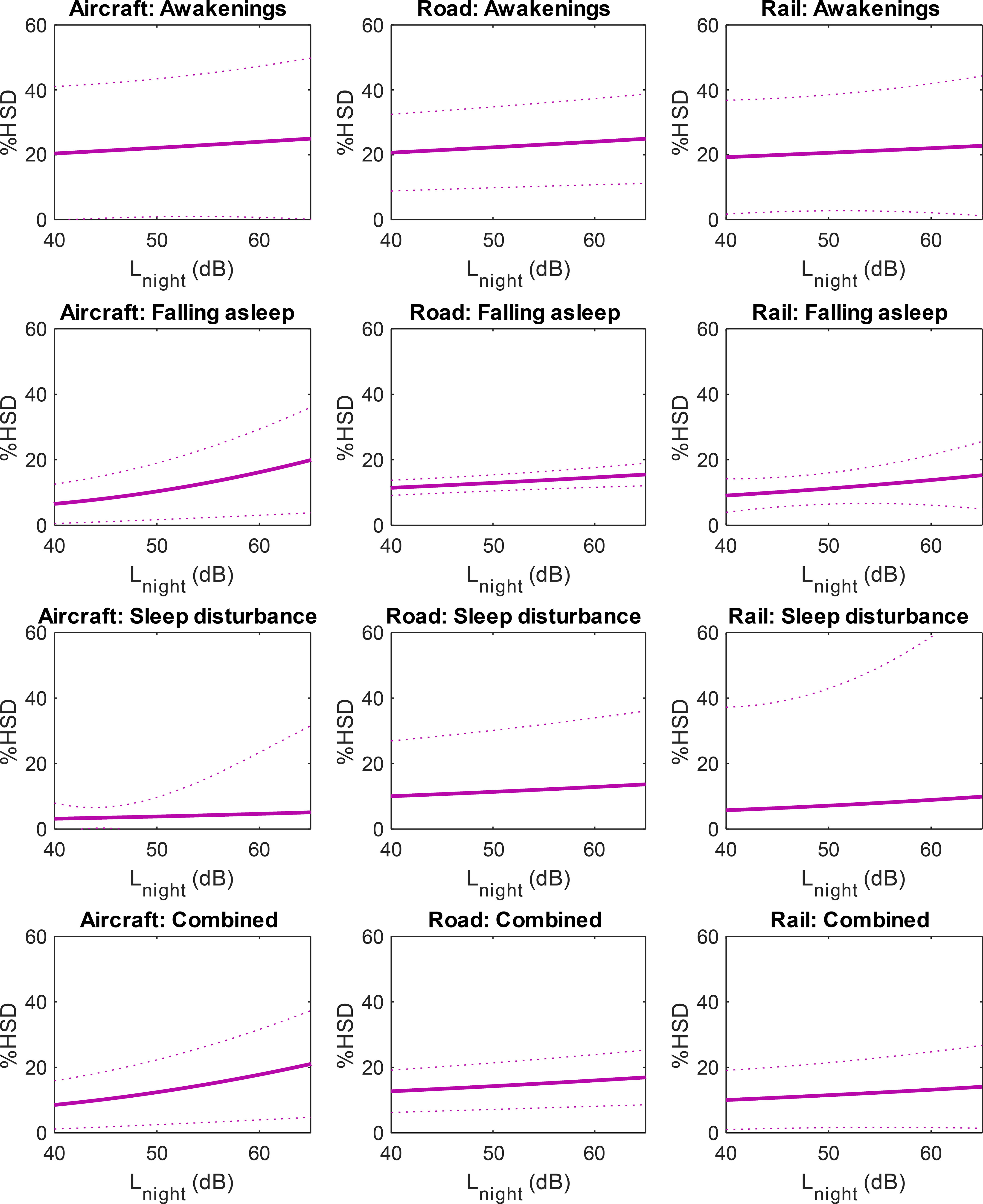
Probability of being highly sleep disturbed (%HSD) by nighttime noise, determined via questions that did not specifically mention noise as the source of disturbance, stratified by disturbance question and traffic mode. Exposure–response relationships were derived using all available data, from the original WHO review19 and the 11 newly identified studies. Dotted lines indicate 95% CIs. Parameter estimates were calculated in logistic regression models with included as the only fixed effect and study included as a random effect, restricted to the noise exposure range 40–65 dB . Models were run separately for each traffic mode and disturbance question. The combined estimate was calculated using average responses of the awakening, falling asleep, and sleep disturbance questions within studies. Note: CI, confidence interval; , nighttime noise; WHO, World Health Organization.
Quality of Evidence for Being Highly Sleep Disturbed by Noise
Funnel plots of the combined estimate for each traffic mode are given in Figure S2. The plots were approximately symmetrical, indicating a low likelihood of publication bias.
The GRADE profile for the assessment of the quality of evidence across studies is given in Table 6. In the assessment, we deemed that for the majority of studies to be considered high quality (study limitations domain), there should be a low risk of selection bias and also a low risk of exposure assessment bias. If there was a high risk for one or both of these biases in the majority of studies, then overall study quality was deemed low. The overall quality of evidence for nighttime noise from aircraft, road, and railway traffic was rated as moderate when the question mentioned noise. When the question did not mention noise, the quality of evidence was low for aircraft and road traffic noise and very low for railway noise.
Table 6.
GRADE Evidence profile (adapted from the WHO review19).
| Domain | Criterion | Assessment | Grade change |
|---|---|---|---|
| Sleep disturbance questions: noise mentioned | |||
| Start level | ; | All cross-sectional studies | Low quality |
| Study limitations | Majority of studies low quality | Aircraft and railway: majority of studies have low risk of selection bias (10/19) and exposure assessment bias (14/19) | Aircraft and railway: no downgrade |
| Road: majority of studies have low risk of selection bias (11/15) and high risk of exposure assessment bias (10/15) | Road: downgrade one level | ||
| Inconsistency | Conflicting results; high | High heterogeneity between studies () | Downgrade one level |
| Indirectness | Direct comparison; same PECO | Same PECO | No downgrade |
| Precision | CIs contain 25% harm or benefit | CIs narrower than 25% except for few outcomes at high noise levels | No downgrade |
| Publication bias | Indicated by funnel plot | Symmetrical plots | No downgrade |
| Judgment after downgrades | — | — | Aircraft, road, and railway: very low quality |
| Dose–response | Significant trend | Statistically significant trend for all outcomes | Upgrade one level |
| Magnitude of effect | for 11 of 12 outcomes | Upgrade one level | |
| Confounding adjusted | Effect in spite of confounding working toward the null | Not observed | No upgrade |
| Overall judgment | — | — | Aircraft, road, and railway: moderate quality |
| Sleep disturbance questions: noise not mentioned | |||
| Start level | ; | All cross-sectional studies | Low quality |
| Study limitations | Majority of studies low quality | Majority of studies have high risk of selection bias (10/18) and low risk of exposure assessment bias (15/18) | Downgrade one level |
| Inconsistency | Conflicting results; high | Railway: unimportant heterogeneity between studies () | Railway: no downgrade |
| Aircraft and road: substantial to considerable heterogeneity between studies () | Aircraft and road: downgrade one level | ||
| Indirectness | Direct comparison; same PECO | Same PECO | No downgrade |
| Precision | CIs contain 25% harm or benefit | Wide CIs | Downgrade one level |
| Publication bias | Indicated by funnel plot | Symmetrical plots | No downgrade |
| Judgment after downgrades | — | — | Aircraft, road, and railway: very low quality |
| Dose–response | Significant trend | Aircraft: statistically significant trend for falling asleep and combined estimate | Railway: no upgrade |
| Railway: not significant | Aircraft and road: upgrade one level | ||
| Road: statistically significant trend for awakenings, falling asleep and combined estimate | |||
| Magnitude of effect | for all outcomes | No upgrade | |
| Confounding adjusted | Effect in spite of confounding working toward the null | Not observed | No upgrade |
| Overall judgment | — | — | Railway: very low quality |
| Aircraft and road: low quality | |||
Note: —, not applicable; CI, confidence interval; GRADE, Grading of Recommendations, Assessment, Development, and Evaluations (criteria); OR, odds ratio; PECO, Patient/Problem, Exposure, Comparison and Outcome (framework); RR, risk ratio; WHO, World Health Organization.
Discussion
Noise-Specific Sleep Disturbance
In an update to the latest WHO evidence review and meta-analysis for the effects of traffic noise on self-reported sleep disturbance,19 we found significant exposure–response relationships for being highly sleep disturbed by nighttime aircraft, road, and railway traffic when the sleep questions explicitly mentioned noise. With increasing nighttime noise levels, and for all three traffic modes, there were increased probabilities of reporting awakenings, having difficulties falling asleep, or having disrupted or disturbed sleep. When the sleep disturbance outcomes were combined for each traffic mode separately, the resulting exposure–response curves for road and railway noise were very similar to those calculated in the WHO review (Figure 6). The similarity in the exposure–response curves improves confidence in the earlier estimates, which informed recent WHO recommendations for nighttime noise from road (45 dB ) and rail (44 dB ).15 For aircraft noise, our updated estimates show a higher probability of being highly sleep disturbed at high levels. At 40 dB , however, which is the WHO recommendation for nighttime aircraft noise,15 our updated estimates closely match the point estimates from the previous evidence review.19
The ORs for aircraft noise were lower than for both road and railway noise. This is a consequence of the properties of ORs as a relative measure, given that a much higher proportion of people were sleep disturbed by aircraft noise at low reference noise levels. The exposure–response curves show that aircraft noise was in fact more disturbing than road or rail noise of the same level. This finding, although also seen in the original WHO review,19 is superficially surprising in light of experimental studies showing that aircraft noise is less disruptive to physiological sleep than road or rail traffic.67 The reasons for higher self-reported disturbance by aircraft are unclear but could result from the timing of aircraft noise events. Nighttime noise levels from aircraft are typically dominated by passenger plane takeoffs and landings that occur at the very start and the very end of the night period (2300–0700 hours). The early night is a period when many people are trying to fall asleep, and the end of the night is a period when people may be awakened by noise more easily, or have greater difficulty falling back asleep after awakenings, because sleep pressure has been dissipated over the preceding night. Noise around these times could therefore have a greater impact on self-reported disturbance than at other times of night. Such an explanation is supported by the higher disturbance for specific questions on awakenings and difficulties falling asleep owing to aircraft noise.
It is also possible that the higher disturbance by aircraft is a result of exposure misclassification. In most studies, noise was assessed at the most exposed façade, and the exposure levels specifically in the bedroom are not known. Noise levels in the bedroom for road and railway traffic are most likely lower, on average, than at the most exposed façade, because bedrooms may be located on quieter sides of the building. There is probably less exposure misclassification for aircraft noise, especially for homes that lie under flight paths, given that the positions of aircraft as noise sources are more dynamic relative to the home. Finally, it is possible that particular characteristics of air traffic are somehow more disturbing than road or rail noise of the same level. Aircraft noise events have a much longer duration than the other traffic modes, and so there are longer windows to become cognizant of the noise and attribute it as a source of sleep disturbance. However, each of these explanations cannot be thoroughly explored without additional temporal, spatial, and acoustical data for the noise sources.
Non-Noise-Specific Sleep Disturbance
The probability of being highly sleep disturbed was less clear when studies used general sleep questions that did not mention noise. For those sleep outcomes, all ORs were in the same direction and , suggesting potentially increasing disturbance with noise level. However, the effect sizes were smaller compared with noise-specific questions, and they were significant for only a minority of outcomes (5 of 12) assessed across all traffic modes.
Differences in sleep disturbance between studies employing general sleep questions and studies that specifically mention noise could result from heterogeneity between studies generally, which is discussed in detail later. When a question mentions a particular traffic source, a respondent may be better able to correctly attribute noise-induced sleep disturbance to that source, which could also explain the higher effect sizes in studies mentioning noise. Misattributing noise as the reason for an endogenous sleep is also possible, for instance, if respondents awaken spontaneously in the absence of noise, and a noise event that is later recalled coincidentally occurs during the awakening bout. A further important effect modifier could be noise sensitivity. Because noise-sensitive individuals may be more likely to report sleep disturbance than their less-sensitive counterparts,68–70 they might rate themselves as more sleep disturbed to questions explicitly mentioning noise.
Risk of Bias, Quality of Evidence, and Study Heterogeneity
Most newly included studies were rated as having a high risk of selection bias. In most cases, this was due to response rates being . Low survey response rates in public health research are becoming increasingly common,71 something that can increase the risk of nonresponse bias.72 However, nonresponse bias can occur in studies with both low and high response rates.73 More important than response rates is that the survey responses are representative of the target population sampled,74 and surveys can still be representative even with lower response rates. Lacking nonresponse analyses, we cannot be certain of the representativeness of the exposure–response relationships, although the high risk of selection bias in the included studies does not necessarily mean that the sleep outcomes are unrepresentative of the overall population exposed to noise. Further studies with increased response rates would decrease the likelihood of nonresponse bias.
Sensitivity analysis revealed that sleep disturbance was lower in studies with a high risk of exposure assessment bias. One possible explanation is that road and railway noise exposure in the bedroom was overestimated in studies judged to have a high risk of bias. This would, in effect, shift the exposure–response relationships to the right in these studies. Alternatively, differences in sleep disturbance could be confounded by the fact that all studies with high risk of exposure assessment bias were published between 2002 and 2010, whereas the low risk of bias studies were from published more recently, between 2013 and 2021. It is plausible that the higher probability of high sleep disturbance in newer studies is attributable to nonacoustical factors, such as changes in attitudes to noise. Temporal changes in self-reported response would align with observed trends for increasing annoyance by a given level of traffic noise, although these trends have been observed predominantly for aircraft rather than road or rail traffic.75 There have also been changes in the acoustical character of noise, with newer vehicles being typically quieter but with noise occurring more often as traffic flows increase, which may negatively influence perceived sleep disturbance.
The overall quality of evidence differed between studies where sleep disturbance questions did or did not mention noise. The assessment of a moderate quality of evidence for sleep disturbance when the question mentioned noise agrees with the assessment in the WHO review.19 When the question did not specifically mention noise, we graded the quality of evidence for exposure to railway noise as very low, again agreeing with the WHO review, and the quality of evidence as low for aircraft and road traffic noise, which is one level higher than the very low quality assessment in the WHO review. The reason for the upgrade for aircraft and road noise was due to the statistically significant trends for awakenings (road only), falling asleep, and the combined estimates, that were not found previously. Since the previous review, three major cross-sectional studies involving road traffic noise exposure, with a combined sample size of respondents, were published.34,37,47 The exposure–response relationships for non-noise-dependent disturbance are thus more representative, and with substantially greater power, than previously found.
There was substantial heterogeneity between studies for all outcomes except studies of railway noise that employed general sleep questionnaires. The heterogeneity could result from variations in the specific phrasing of the sleep disturbance question across studies, even when ostensibly measuring the same outcome. There was also a diverse range of response scales, with 11-point numerical and 3-, 4-, or 5-point verbal scales used to assess sleep disturbance, further diversified by assessing either the severity or the frequency of disturbance. These questions were administered in 14 nations, hence, there may be linguistic differences in the interpretation of certain phrases, as well as cultural differences in attitudes to sleep or noise, as well as contextual differences generally across specific studies. Questions also differed in the reference time frame for sleep disturbance, varying from the last 12 months to the last 4 wk to referencing specific noise events or no time frame at all. Finally, self-reported response to noise can be modified by contextual factors separate from noise level alone, including lifestyle, access to green space, access to quiet areas, social interaction, recreational activities, and local economy of the neighbourhood.76 One or several of these factors could have contributed to study heterogeneity within specific sleep outcomes, across studies of different traffic modes, or across studies that used either general sleep questions or noise-specific disturbance questions.
Study Location
The majority of new studies originated from Europe. All newly included studies of road34,37,42,46,47 and railway37,42,46 noise were European, as were the majority of respondents across the studies of aircraft noise.35,41,42,46 Although there was one study of aircraft noise from Asia,32 and three from the United States,20,21,45 these studies were small, with sample sizes ranging from to . European studies continue to be overrepresented (Figure S3). However, we found no statistically significant differences in sleep disturbance between European and non-European studies. On one hand, this suggests that there are, in fact, no differences in response between the two locations, that the degree of sleep disturbance by noise is rather global in nature, and that results of the present analyses are relevant outside of Europe. Conversely, the point estimates were rather different between study location for several sleep disturbance outcomes. This could indicate underlying cultural differences in attitudes to noise and perceived sleep disturbance that have not been captured in studies to date. Future investigations outside of Europe may uncover relevant international differences, as well as increasing confidence that existing studies are representative of noise-induced sleep disturbance among these underinvestigated regions.
Considerations on Self-Reported Sleep Disturbance
Our overall findings of self-reported disturbance by noise should be treated with some caution when considering noise-induced effects on sleep. Sleep is, by its nature, an unconscious process, meaning that its subjective evaluation is difficult. Accordingly, there can be substantial differences between self-reported and physiologically derived measures of sleep and noise-induced sleep disturbance.77–79 Self-report may also suffer from recall bias, particularly when questions relate to the preceding 12 months, as was typical for questions on sleep disturbance in most studies included in our meta-analysis. It is likely that responses to questions on these timescales are driven by noise exposure in the more recent past. However, self-reported sleep outcomes are methodologically convenient and inexpensive to implement in field studies, meaning that we could perform the meta-analysis with a number of studies and sample size that would not have been possible if focusing on physiologic outcomes. As such, we have higher confidence in the accuracy and representativeness of the analysis. A further advantage is that self-reported disturbance is a valuable end point per se, considered by the WHO as a primary health outcome. By focusing our analysis on these outcomes, the results may be useful in future estimates of the disease burden of environmental noise80 and recommendations for nighttime noise limits,15 both of which derive from self-reported sleep disturbance. Finally, self-reported outcomes capture habitual sleep quality and disturbance, unlike physiologic measurements that capture only acute effects within single nights. It does, however, remain unclear how long-term self-reported sleep disturbance by noise relates to overall health.
Future large-scale field studies with objective measurements of noise and sleep can offer mechanistic insights linking nocturnal noise, sleep disruption, and epidemiological observations of the development of cardiovascular and metabolic disease associated with exposure to environmental noise in addition to the derivation of exposure–response relationships.81 A better understanding of the underlying pathophysiological pathways is especially valuable when considering vulnerable populations who may be at increased risk of disturbance. These vulnerable groups include the elderly, who can suffer from age-related declines in sleep quantity and quality82; populations who may have already poor sleep quality, such as people with mental health or sleep disorders83; and populations with obesity, who are at increased risk of suffering from obstructive sleep apnea, as well as having increased risk for cardiometabolic diseases generally.84,85 Infants, children, and adolescents can also be considered as vulnerable groups because of the importance of sleep of sufficient quality and duration for development.80,86,87
Limitations
Data could not be obtained for two studies that were initially deemed to be eligible for inclusion. It is unlikely that including the study of road traffic noise44 would have substantially altered the updated relationships because the sample size was low () compared with the overall sample size for all road traffic studies (). Including the study of aircraft noise,43 however, may have altered the sleep outcomes where noise was not mentioned for falling asleep, sleep disturbance, and the combined estimate. Compared with sample sizes of for questions on falling asleep and just for sleep disturbance questions that were included in our analysis, the omitted study had a sample size of , which would have reflected a substantial proportion of the total data set. The change in effect size that would have resulted from including this study is unclear because the relevant sleep-disturbance questions were single items that formed only part of the insomnia severity index (ISI). Because only overall results from the ISI were published, we do not know whether the relevant items were related to noise exposure, or to what extent.
A limitation of the meta-analysis was that many studies modeled noise exposure at the most exposed façade of the residence, and thus noise levels specifically at the bedroom façade are unknown. This means there is probably some exposure misclassification, with lower noise levels if the bedroom faces away from the noise source. This is more likely for road and railway noise than aircraft noise, with the latter source being less fixed in position relative to the bedroom. This would, in effect, shift the exposure–response curves to the left, leading to an increased probability of disturbance at lower noise levels, given that noise levels at the bedrooms are, on average, probably lower than assuming they are all positioned at the most exposed façade. This was supported by two studies in the meta-analysis that found that a lower proportion of respondents were highly sleep disturbed by road traffic noise46 or reported insomnia symptoms37 when the bedroom faced away from the street. Furthermore, disturbance was lower when the difference in noise level between the bedroom and the most exposed façade was greater.46 A second limitation of the meta-analysis is that we did not adjust for potentially relevant effect modifiers. We adopted this approach so that results would be directly comparable to those in the WHO review, which also did not include such adjustments.19 Sleep, and its disturbance by noise, may differ depending on age, sex, socioeconomic status, and preexisting sleep disorders. Further, sleep disturbance is not unique to noise exposure and may arise from other environmental stressors, including air pollution,88–90 vibration (from, for instance, freight trains on railway lines),91 light,92 and temperature and humidity.93,94 Future studies should consider the consequences of exposure to multiple stressors, and their interactions on sleep.
Summary of Evidence
Our main objective was to update the WHO meta-analysis on sleep disturbance by traffic noise with evidence published after 2015.19 The main findings and quality of evidence are summarized in Table 7. There was a significant probability of being highly sleep disturbed by nocturnal noise from aircraft, road, and railway noise when the disturbance question mentioned noise, and the quality of evidence for these outcomes was moderate. Exposure–response curves were similar to the WHO review for road and railway noise in our updated analysis, and we found an increased probability of being highly sleep disturbed by aircraft noise at high noise levels. Because of the number of studies published since 2015, for the first time, we were able to generate exposure–response relationships for sleep outcomes that did not explicitly mention noise. Point estimates for these outcomes were smaller than questions mentioning noise, and were often not statistically significant, and the quality of evidence was graded lower, from low to very low. Our findings do not suggest that the recent WHO recommendations for nighttime noise need to be revisited,15 although quantitative assessments of sleep disturbance by aircraft noise at high exposure levels should consider the implications of our analysis. We did not find significant indications of international differences in sleep disturbance by noise, but future large-scale studies in non-European nations may necessitate a reevaluation of the evidence.
Table 7.
Summary of meta-analytic and evidence quality findings.
| Sleep outcome | Noise source | Studies ()a | Respondents ()a | Quality of evidence | Noise metric | OR per 10-dB increase (95% CI) |
|---|---|---|---|---|---|---|
| Self-reported sleep disturbance in adults Noise specified as source of disturbance |
Aircraft | 11 | 19,488 | Moderate | 2.18 (2.01, 2.36) | |
| Road | 14 | 31,738 | Moderate | 2.52 (2.28, 2.79) | ||
| Railway | 8 | 10,846 | Moderate | 2.97 (2.57, 3.43) | ||
| Self-reported sleep disturbance in adults Noise not specified as source of disturbance |
Aircraft | 8 | 2,571 | Low | 1.52 (1.20, 1.93) | |
| Road | 7 | 38,380 | Low | 1.14 (1.08, 1.21) | ||
| Railway | 4 | 4,326 | Very low | 1.17 (0.91, 1.49) |
Note: ORs were calculated in logistic regression models with included as the only fixed effect and study included as a random effect, restricted to the noise exposure range 40–65 dB . Models were run separately for each traffic mode and for sleep questionnaire outcomes that did or did not mention noise. Data shown are for the combined estimates calculated using average responses of the awakening, falling asleep, and sleep disturbance questions within studies. , nighttime noise; OR, odds ratio.
aIn the range 40–65 dB for which ORs were calculated.
Supplementary Material
Acknowledgments
Contributions of the authors are as follows—M.G.S.: investigation, formal analysis, data curation, writing (original draft), and visualization; M.C.: investigation and writing (review and editing); and M.B.: conceptualization, methodology, formal analysis, writing (review and editing), supervision, and funding acquisition.
We are grateful to G.M. Aasvang, J. Evandt, T.L. Nguyen, M. Reedijk, D. Schreckenberg, R. Vermeulen, K. Persson Waye, S. Bartels, and S. Fredriksson for sharing additional deidentified self-reported sleep data from their studies to facilitate the updated meta-analysis. We also thank T. Bodin, M. Brink, L. Brown, J. Halonen, J. Hong, T.L. Nguyen, G. Ristovska, M. Röösli, D. Schreckenberg, and T. Yano, who graciously shared sleep data for the original WHO meta-analysis, which was included in this updated analysis.
This work was funded by the Department for Environmental, Food and Rural Affairs (DEFRA) on behalf of the Interdepartmental Group on Costs and Benefits Noise Subject Group, project no. 30116. DEFRA had no role in designing the study or collection, analysis, and interpretation of data. DEFRA had the opportunity to comment on a draft of this manuscript, but made no substantive edits. M.C. was supported by the National Institutes of Health/National Institute of Nursing Research (K99NR019862).
The information and views set out in this report are those of the authors and do not necessarily reflect the official opinion of DEFRA. DEFRA does not guarantee the accuracy of the data included in this review. Neither DEFRA nor any person acting on behalf of DEFRA may be held responsible for the use which might be made of the information contained therein.
References
- 1.Consensus Conference Panel; Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, et al. 2015. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. Sleep 38(8):1161–1183, PMID: , 10.5665/sleep.4886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banks S, Dinges DF. 2007. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med 3(5):519–528, PMID: , 10.5664/jcsm.26918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dettoni JL, Consolim-Colombo FM, Drager LF, Rubira MC, Cavasin de Souza SBP, Irigoyen MC, et al. 2012. Cardiovascular effects of partial sleep deprivation in healthy volunteers. J Appl Physiol (1985) 113(2):232–236, PMID: , 10.1152/japplphysiol.01604.2011. [DOI] [PubMed] [Google Scholar]
- 4.Buxton OM, Cain SW, O’Connor SP, Porter JH, Duffy JF, Wang W, et al. 2012. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med 4(129):129ra43, PMID: , 10.1126/scitranslmed.3003200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buxton OM, Pavlova M, Reid EW, Wang W, Simonson DC, Adler GK. 2010. Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes 59(9):2126–2133, PMID: , 10.2337/db09-0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taheri S, Lin L, Austin D, Young T, Mignot E. 2004. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 1(3):e62, PMID: , 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diekelmann S, Born J. 2010. The memory function of sleep. Nat Rev Neurosci 11(2):114–126, PMID: , 10.1038/nrn2762. [DOI] [PubMed] [Google Scholar]
- 8.Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, et al. 2008. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 31(5):619–626, PMID: , 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knutson KL, Spiegel K, Penev P, Van Cauter E. 2007. The metabolic consequences of sleep deprivation. Sleep Med Rev 11(3):163–178, PMID: , 10.1016/j.smrv.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE, et al. 2006. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep 29(8):1009–1014, PMID: , 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 11.Badran M, Yassin BA, Fox N, Laher I, Ayas N. 2015. Epidemiology of sleep disturbances and cardiovascular consequences. Can J Cardiol 31(7):873–879, PMID: , 10.1016/j.cjca.2015.03.011. [DOI] [PubMed] [Google Scholar]
- 12.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. 2010. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 33(5):585–592, PMID: , 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferrie JE, Shipley MJ, Akbaraly TN, Marmot MG, Kivimäki M, Singh-Manoux A. 2011. Change in sleep duration and cognitive function: findings from the Whitehall II Study. Sleep 34(5):565–573, PMID: , 10.1093/sleep/34.5.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO (World Health Organization) Regional Office for Europe. 2011. Burden of Disease from Environmental Noise. Quantification of Healthy Life Years Lost in Europe. Copenhagen, Denmark: World Health Organization Regional Office for Europe. [Google Scholar]
- 15.WHO Regional Office for Europe. 2018. Environmental Noise Guidelines for the European Region. Copenhagen, Denmark: World Health Organization Regional Office for Europe. [Google Scholar]
- 16.Hänninen O, Knol AB, Jantunen M, Lim TA, Conrad A, Rappolder M, et al. 2014. Environmental burden of disease in Europe: assessing nine risk factors in six countries. Environ Health Perspect 122(5):439–446, PMID: , 10.1289/ehp.1206154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.U.S. Department of Transportation Bureau of Transport Statistics. 2020. Under a quarter of population exposed to office-type transportation noise. https://www.bts.gov/newsroom/under-quarter-population-exposed-office-type-transportation-noise [accessed 19 March 2021].
- 18.Brink M, Schäffer B, Pieren R, Wunderli JM. 2018. Conversion between noise exposure indicators Leq24h, LDay, LEvening, LNight, Ldn and Lden: principles and practical guidance. Int J Hyg Environ Health 221(1):54–63, PMID: , 10.1016/j.ijheh.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Basner M, McGuire S. 2018. WHO Environmental Noise Guidelines for the European Region: a systematic review on environmental noise and effects on sleep. Int J Environ Res Public Health 15(3):519, PMID: , 10.3390/ijerph15030519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Basner M, Witte M, McGuire S. 2019. Aircraft noise effects on sleep—results of a pilot study near Philadelphia International Airport. Int J Environ Res Public Health 16(17):3178, PMID: , 10.3390/ijerph16173178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith MG, Rocha S, Witte M, Basner M. 2020. On the feasibility of measuring physiologic and self-reported sleep disturbance by aircraft noise on a national scale: a pilot study around Atlanta airport. Sci Total Environ 718:137368, PMID: , 10.1016/j.scitotenv.2020.137368. [DOI] [PubMed] [Google Scholar]
- 22.Basner M, Samel A, Isermann U. 2006. Aircraft noise effects on sleep: application of the results of a large polysomnographic field study. J Acoust Soc Am 119(5 pt 1):2772–2784, PMID: , 10.1121/1.2184247. [DOI] [PubMed] [Google Scholar]
- 23.Münzel T, Gori T, Babisch W, Basner M. 2014. Cardiovascular effects of environmental noise exposure. Eur Heart J 35(13):829–836, PMID: , 10.1093/eurheartj/ehu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kröller-Schön S, Daiber A, Steven S, Oelze M, Frenis K, Kalinovic S, et al. 2018. Crucial role for Nox2 and sleep deprivation in aircraft noise-induced vascular and cerebral oxidative stress, inflammation, and gene regulation. Eur Heart J 39(38):3528–3539, PMID: , 10.1093/eurheartj/ehy333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Münzel T, Kröller-Schön S, Oelze M, Gori T, Schmidt FP, Steven S, et al. 2020. Adverse cardiovascular effects of traffic noise with a focus on nighttime noise and the new WHO noise guidelines. Annu Rev Public Health 41(1):309–328, PMID: , 10.1146/annurev-publhealth-081519-062400. [DOI] [PubMed] [Google Scholar]
- 26.Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. 2014. Auditory and non-auditory effects of noise on health. Lancet 383(9925):1325–1332, PMID: , 10.1016/S0140-6736(13)61613-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. 2021. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71, PMID: , 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Kamp I, Simon S, Notley H, Baliatsas C, van Kempen E. 2020. Evidence relating to environmental noise exposure and annoyance, sleep disturbance, cardio-vascular and metabolic health outcomes in the context of IGCB (N): a scoping review of new evidence. Int J Environ Res Public Health 17(9):3016, PMID: , 10.3390/ijerph17093016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.European Council. 2002. Directive 2002/49/EC of the European Parliament and of the Council of 25 June 2002 relating to the assessment and management of environmental noise. Off J Eur Communities L 189:12–24. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:32002L0049 [accessed 22 June 2022]. [Google Scholar]
- 30.Fields JM, De Jong RG, Gjestland T, Flindell IH, Job RFS, Kurra S, et al. 2001. Standardized general-purpose noise reaction questions for community noise surveys: research and a recommendation. J Sound Vib 242(4):641–679, 10.1006/jsvi.2000.3384. [DOI] [Google Scholar]
- 31.Roth T. 2007. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med 3(suppl 5):S7–S10, PMID: , 10.5664/jcsm.26929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nguyen TL, Trieu BL, Hiraguri Y, Morinaga M, Morihara T, Yano T. 2020. Effects of changes in acoustic and non-acoustic factors on public health and reactions: follow-up surveys in the vicinity of the Hanoi Noi Bai International Airport. Int J Environ Res Public Health 17(7):2597, PMID: , 10.3390/ijerph17072597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bodin T, Björk J, Ardö J, Albin M. 2015. Annoyance, sleep and concentration problems due to combined traffic noise and the benefit of quiet side. Int J Environ Res Public Health 12(2):1612–1628, PMID: , 10.3390/ijerph120201612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martens AL, Reedijk M, Smid T, Huss A, Timmermans D, Strak M, et al. 2018. Modeled and perceived RF-EMF, noise and air pollution and symptoms in a population cohort. Is perception key in predicting symptoms? Sci Total Environ 639:75–83, PMID: , 10.1016/j.scitotenv.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 35.Carugno M, Imbrogno P, Zucchi A, Ciampichini R, Tereanu C, Sampietro G, et al. 2018. Effects of aircraft noise on annoyance, sleep disorders, and blood pressure among adult residents near the Orio al Serio International Airport (BGY), Italy. Med Lav 109(4):253–263, PMID: , 10.23749/mdl.v109i4.7271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Filomena V, De Vivo L, Notarnicola L, Aversano R, Tusciano M. 2014. Noise assessment in the neighbourhood of Italian military airports. In: Proceedings of the 43rd International Congress on Noise Control Engineering: INTER.NOISE 2014. Davy J, Don C, McMinn T, Dowsett L, Broner N, Burgess M, eds. 16–19 November 2014. Australian Capital Territory, Australia: Australian Acoustical Society, 260. [Google Scholar]
- 37.Evandt J, Oftedal B, Hjertager Krog N, Nafstad P, Schwarze PE, Aasvang GM. 2017. A population-based study on nighttime road traffic noise and insomnia. Sleep 40(2):zsw055, PMID: , 10.1093/sleep/zsw055. [DOI] [PubMed] [Google Scholar]
- 38.National Heart, Lung, and Blood Institute. 2021. Study quality assessment tools: quality assessment tool for observational cohort and cross-sectional studies. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools [accessed 4 May 2021].
- 39.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. (eds.). 2021. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.2 (updated February 2021). London, UK: Cochrane Collaboration. [Google Scholar]
- 40.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. 2008. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336(7650):924–926, PMID: , 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Civil Aviation Authority. 2017. Survey of Noise Attitudes 2014: Aircraft Noise and Annoyance. 2nd ed. CAP 1506. http://publicapps.caa.co.uk/modalapplication.aspx?appid=11&mode=detail&id=7744.
- 42.NORAH (Noise-Related Annoyance, Cognition, and Health). 2021. Overview of results from the NORAH sleep study. http://www.laermstudie.de/ergebnisse/ergebnisse-schlafstudie/ueberblick/ [accessed 22 June 2022].
- 43.Kwak KM, Ju YS, Kwon YJ, Chung YK, Kim BK, Kim H, et al. 2016. The effect of aircraft noise on sleep disturbance among the residents near a civilian airport: a cross-sectional study. Ann Occup Environ Med 28(1):38, PMID: , 10.1186/s40557-016-0123-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Paiva KM, Cardoso MRA, Zannin PHT. 2019. Exposure to road traffic noise: annoyance, perception and associated factors among Brazil’s adult population. Sci Total Environ 650(pt 1):978–986, PMID: , 10.1016/j.scitotenv.2018.09.041. [DOI] [PubMed] [Google Scholar]
- 45.Rocha S, Smith MG, Witte M, Basner M. 2019. Survey results of a pilot sleep study near Atlanta International Airport. Int J Environ Res Public Health 16(22):4321, PMID: , 10.3390/ijerph16224321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brink M, Schäffer B, Vienneau D, Pieren R, Foraster M, Eze IC, et al. 2019. Self-reported sleep disturbance from road, rail and aircraft noise: exposure-response relationships and effect modifiers in the SiRENE study. Int J Environ Res Public Health 16(21):4186, PMID: , 10.3390/ijerph16214186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bartels S, Ögren M, Kim JL, Fredriksson S, Persson Waye K. 2021. The impact of nocturnal road traffic noise, bedroom window orientation, and work-related stress on subjective sleep quality: results of a cross-sectional study among women. Int Arch Occup Environ Health 94(7):1523–1536, PMID: , 10.1007/s00420-021-01696-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nguyen LT, Nguyen TL, Yano T, Morinaga M, Yamada I, Tetsumi S, et al. 2015. Social surveys around Noi Bai Airport before and after the opening of a new terminal building. In: Proceedings of the 44th International Congress on Noise Control Engineering (Internoise 2015). Burroughs C, ed. 9–12 August 2015. Reston, VA: Institute of Noise Control Engineering, 4270. [Google Scholar]
- 49.Yano T, Nguyen TL, Nguyen TL, Takada M, Yamada I, Morinaga M, et al. 2015. Community response to a step change in aircraft noise exposure: The first socio-acoustic survey around Noi Bai Airport in Hanoi. In: Proceedings of the International Congress on Sound and Vibration (22ICSV), Florence, Italy, 12–16 July 2015. [Google Scholar]
- 50.Nguyen TL, Yano T, Nguyen HQ, Nguyen KTT, Fukushima H, Kawai K, et al. 2012. Aircraft and road traffic noise annoyance in Da Nang City, Vietnam. In: Proceedings of the 41st International Congress and Exposition on Noise Control Engineering 2012 (INTER-NOISE 2012). Burroughs C, Conlon S, eds. 19–22 August 2012. Indianapolis, IN: Institute of Noise Control Engineering, 1661. [Google Scholar]
- 51.Nguyen TL, Yano T, Nguyen HQ, Hoang TL, Nishimura T, Morihara T, et al. 2010. Community response to aircraft and combined noises in Hanoi. In: Proceedings of the 39th International Congress on Noise Control Engineering 2010 (INTER-NOISE 2010). 13–16 June 2010. Lisbon, Portugal: Sociedade Portuguesa de Acustica, 4038. [Google Scholar]
- 52.Nguyen TL, Yano T, Nguyen HQ, Nishimura T, Fukushima H, Sato T, et al. 2011. Community response to aircraft noise in Ho Chi Minh City and Hanoi. Appl Acoust 72(11):814–822, 10.1016/j.apacoust.2011.05.002. [DOI] [Google Scholar]
- 53.Yano T, Nguyen TL, Nishimura T, Sato T. 2019. Social survey on community response to aircraft noise in Ho Chi Minh City. In: Proceedings of the 38th International Congress and Exposition on Noise Control Engineering 2009 (INTER-NOISE 2009). Bolton JS, Burroughs C, Gover B, eds. 23–26 August 2009. Ashland, OH: Noise Control Foundation, 482. [Google Scholar]
- 54.Schreckenberg D, Heudorf U, Eikmann T, Herr C, Nieden A, Meis M. 2009. Aircraft noise and health of residents living in the vicinity of Frankfurt airport . In: Proceedings of the 8th European Conference on Noise Control 2009 (EURONOISE 2009). 26–28 October 2009. St. Albans Hertfordshire, UK: Institute of Acoustics, 511. [Google Scholar]
- 55.Brink M, Wirth K, Rometsch R, Schierz C. 2005. Lärmstudie 2000: Zusammenfassung [In German]. Zurich, Switzerland: Institute for Organizational and Occupational Sciences (ZOA). [Google Scholar]
- 56.Brink M. 2011. Parameters of well-being and subjective health and their relationship with residential traffic noise exposure—a representative evaluation in Switzerland. Environ Int 37(4):723–733, PMID: , 10.1016/j.envint.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 57.Phan HYT, Yano T, Phan HAT, Nishimura T, Sato T, Hashimoto Y. 2010. Community responses to road traffic noise in Hanoi and Ho Chi Minh City. Appl Acoust 71(2):107–114, 10.1016/j.apacoust.2009.08.004. [DOI] [Google Scholar]
- 58.Shimoyama K, Nguyen TL, Yano T, Morihara T. 2014. Social surveys on community response to road traffic in five cities in Vietnam . In: Proceedings of the 43rd International Congress on Noise Control Engineering: INTER.NOISE 2014. Davy J, Don C, McMinn T, Dowsett L, Broner N, Burgess M, eds. 16–19 November 2014. Australian Capital Territory, Australia: Australian Acoustical Society, 109. [Google Scholar]
- 59.Sato T, Yano T, Björkman M, Rylander R. 2002. Comparison of community response to road traffic noise in Japan and Sweden—part I: outline of surveys and dose–response relationships. J Sound Vib 250(1):161–167, 10.1006/jsvi.2001.3892. [DOI] [Google Scholar]
- 60.Brown AL, Lam KC, van Kamp I. 2015. Quantification of the exposure and effects of road traffic noise in a dense Asian city: a comparison with Western cities. Environ Health 14(1):22, PMID: , 10.1186/s12940-015-0009-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hong J, Kim J, Lim C, Kim K, Lee S. 2010. The effects of long-term exposure to railway and road traffic noise on subjective sleep disturbance. J Acoust Soc Am 128(5):2829–2835, PMID: , 10.1121/1.3493437. [DOI] [PubMed] [Google Scholar]
- 62.Ristovska G, Gjorgjev D, Stikova E, Petrova V, Cakar MD. 2009. Noise induced sleep disturbance in adult population: cross sectional study in Skopje urban centre. Maced J Med Sci 2(3):255–260. http://www.mjms.mk/Online/MJMS_2009_2_3/MJMS.1857-5773.2009-0060.pdf [accessed 22 June 2022]. [Google Scholar]
- 63.Frei P, Mohler E, Röösli M. 2014. Effect of nocturnal road traffic noise exposure and annoyance on objective and subjective sleep quality. Int J Hyg Environ Health 217(2–3):188–195, PMID: , 10.1016/j.ijheh.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 64.Halonen JI, Vahtera J, Stansfeld S, Yli-Tuomi T, Salo P, Pentti J, et al. 2012. Associations between nighttime traffic noise and sleep: the Finnish public sector study. Environ Health Perspect 120(10):1391–1396, PMID: , 10.1289/ehp.1205026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sato T, Yano T, Morihara T, Masden K. 2004. Relationships between rating scales, question stem wording, and community responses to railway noise. J Sound Vib 277(3):609–616, 10.1016/j.jsv.2004.03.023. [DOI] [Google Scholar]
- 66.Schreckenberg D. 2013. Exposure–response relationship for railway noise annoyance in the Middle Rhine Valley. In: Proceedings of the 42nd International Congress and Exposition on Noise Control Engineering 2013 (INTER-NOISE 2013). 15–18 September 2013. Vienna, Austria: Austrian Noise Abatement Association, 4716. [Google Scholar]
- 67.Smith MG, Younes M, Aeschbach D, Elmenhorst EM, Müller U, Basner M. 2022. Traffic noise-induced changes in wake-propensity measured with the Odds-Ratio Product (ORP). Sci Total Environ 805:150191, PMID: , 10.1016/j.scitotenv.2021.150191. [DOI] [PubMed] [Google Scholar]
- 68.Marks A, Griefahn B. 2007. Associations between noise sensitivity and sleep, subjectively evaluated sleep quality, annoyance, and performance after exposure to nocturnal traffic noise. Noise Health 9(34):1–7, PMID: , 10.4103/1463-1741.34698. [DOI] [PubMed] [Google Scholar]
- 69.Li S, Fong DYT, Wong JYH, McPherson B, Lau EYY, Huang L, et al. 2021. Noise sensitivity associated with nonrestorative sleep in Chinese adults: a cross-sectional study. BMC Public Health 21(1):643, PMID: , 10.1186/s12889-021-10667-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Park J, Chung S, Lee J, Sung JH, Cho SW, Sim CS. 2017. Noise sensitivity, rather than noise level, predicts the non-auditory effects of noise in community samples: a population-based survey. BMC Public Health 17(1):315, PMID: , 10.1186/s12889-017-4244-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Czajka JL, Beyler A. 2016. Background Paper: Declining Response Rates in Federal Surveys: Trends and Implications. Reference No. 40146.D4C. 15 June 2016. Washington, DC: Mathematica Policy Research. https://aspe.hhs.gov/sites/default/files/private/pdf/255531/Decliningresponserates.pdf [accessed 22 June 2022]. [Google Scholar]
- 72.Dillman DA, Smyth JD, Christian LM. 2014. Internet, Phone, Mail, and Mixed-Mode Surveys: The Tailored Design Method. 4th ed. Indianapolis, IN: John Wiley & Sons. [Google Scholar]
- 73.Groves RM, Peytcheva E. 2008. The impact of nonresponse rates on nonresponse bias: a meta-analysis. Public Opin Q 72(2):167–189, 10.1093/poq/nfn011. [DOI] [Google Scholar]
- 74.Cook C, Heath F, Thompson RL. 2000. A meta-analysis of response rates in web- or internet-based surveys. Educ Psychol Meas 60(6):821–836, 10.1177/00131640021970934. [DOI] [Google Scholar]
- 75.Guski R, Schreckenberg D, Schuemer R. 2017. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and annoyance. Int J Environ Res Public Health 14(12):1539, PMID: , 10.3390/ijerph14121539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Peris E, Fenech B. 2020. Associations and effect modification between transportation noise, self-reported response to noise and the wider determinants of health: a narrative synthesis of the literature. Sci Total Environ 748:141040, PMID: , 10.1016/j.scitotenv.2020.141040. [DOI] [PubMed] [Google Scholar]
- 77.Silva GE, Goodwin JL, Sherrill DL, Arnold JL, Bootzin RR, Smith T, et al. 2007. Relationship between reported and measured sleep times: the Sleep Heart Health Study (SHHS). J Clin Sleep Med 3(6):622–630, PMID: , 10.5664/jcsm.26974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Basner M, Müller U, Elmenhorst EM. 2011. Single and combined effects of air, road, and rail traffic noise on sleep and recuperation. Sleep 34(1):11–23, PMID: , 10.1093/sleep/34.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Smith MG, Ögren M, Thorsson P, Hussain-Alkhateeb L, Pedersen E, Forssén J, et al. 2020. A laboratory study on the effects of wind turbine noise on sleep: results of the polysomnographic WiTNES study. Sleep 43(9):zsaa046, PMID: , 10.1093/sleep/zsaa046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fritschi L, Brown AL, Kim R, Schwela DH, Kephalopoulos S. 2011. Burden of Disease from Environmental Noise: Quantification of Healthy Life Years Lost in Eupope. Copenhagen, Denmark: World Health Organization. [Google Scholar]
- 81.van Kempen E, Casas M, Pershagen G, Foraster M. 2018. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int J Environ Res Public Health 15(2):379, PMID: , 10.3390/ijerph15020379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. 2004. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep 27(7):1255–1273. 73, PMID: , 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 83.Sygna K, Aasvang GM, Aamodt G, Oftedal B, Krog NH. 2014. Road traffic noise, sleep and mental health. Environ Res 131:17–24, PMID: , 10.1016/j.envres.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 84.Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G. 2013. Obstructive sleep apnea: a cardiometabolic risk in obesity; and the metabolic syndrome. J Am Coll Cardiol 62(7):569–576, PMID: , 10.1016/j.jacc.2013.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Klein S, Allison DB, Heymsfield SB, Kelley DE, Leibel RL, Nonas C, et al. 2007. Waist circumference and cardiometabolic risk: a consensus statement from Shaping America’s Health: Association for Weight Management and Obesity Prevention; NAASO, the Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Am J Clin Nutr 85(5):1197–1202, PMID: , 10.1093/ajcn/85.5.1197. [DOI] [PubMed] [Google Scholar]
- 86.Scher A. 2005. Infant sleep at 10 months of age as a window to cognitive development. Early Hum Dev 81(3):289–292, PMID: , 10.1016/j.earlhumdev.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 87.Tarokh L, Saletin JM, Carskadon MA. 2016. Sleep in adolescence: physiology, cognition and mental health. Neurosci Biobehav Rev 70:182–188, PMID: , 10.1016/j.neubiorev.2016.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wei F, Nie G, Zhou B, Wang L, Ma Y, Peng S, et al. 2017. Association between Chinese cooking oil fumes and sleep quality among a middle-aged Chinese population. Environ Pollut 227:543–551, PMID: , 10.1016/j.envpol.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 89.Shen YL, Liu WT, Lee KY, Chuang HC, Chen HW, Chuang KJ. 2018. Association of PM2.5 with sleep-disordered breathing from a population-based study in Northern Taiwan urban areas. Environ Pollut 233:109–113, PMID: , 10.1016/j.envpol.2017.10.052. [DOI] [PubMed] [Google Scholar]
- 90.Strøm-Tejsen P, Zukowska D, Wargocki P, Wyon DP. 2016. The effects of bedroom air quality on sleep and next-day performance. Indoor Air 26(5):679–686, PMID: , 10.1111/ina.12254. [DOI] [PubMed] [Google Scholar]
- 91.Persson Waye K, Smith MG, Hussain-Alkhateeb L, Koopman A, Ögren M, Peris E, et al. 2019. Assessing the exposure-response relationship of sleep disturbance and vibration in field and laboratory settings. Environ Pollut 245:558–567, PMID: , 10.1016/j.envpol.2018.09.082. [DOI] [PubMed] [Google Scholar]
- 92.Cho JR, Joo EY, Koo DL, Hong SB. 2013. Let there be no light: the effect of bedside light on sleep quality and background electroencephalographic rhythms. Sleep Med 14(12):1422–1425, PMID: , 10.1016/j.sleep.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 93.Haskell EH, Palca JW, Walker JM, Berger RJ, Heller HC. 1981. The effects of high and low ambient temperatures on human sleep stages. Electroencephalogr Clin Neurophysiol 51(5):494–501, PMID: , 10.1016/0013-4694(81)90226-1. [DOI] [PubMed] [Google Scholar]
- 94.Okamoto-Mizuno K, Mizuno K, Michie S, Maeda A, Iizuka S. 1999. Effects of humid heat exposure on human sleep stages and body temperature. Sleep 22(6):767–773, PMID: , 10.1093/sleep/22.6.767. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.