Abstract
Objectives
This systematic review aims to summarize the mycological and clinical features of COVID-19-associated fungal infections (CAFIs) in Iran.
Methods
PubMed, Web of Science, Scopus, Cochrane Library, SID, Magiran, IranDoc, and Google Scholar were searched for Persian and English articles published from January 1, 2020, to November 5, 2021, using a systematic search strategy. Studies on Iranian patients suffering from CAFIs were included in the review.
Results
Twenty-two studies comprising 169 patients were retrieved. Reported CAFIs included candidiasis (85, 50.30%), mucormycosis (35, 20.71%), aspergillosis (29, 17.16%), fusariosis (6, 3.55%), three cases caused by rare pathogens (Rhodotorula mucilaginosa, Diaporthe foeniculina, and Sarocladium kiliense) and 11 (6.51%) uncharacterized mold infections. The most common underlying diseases were diabetes (67/168, 39.88%), cardiovascular diseases (55/168, 32.74%), and hypertension (43/168, 25.59%). The use of antibiotics (111/124, 89.52%), corticosteroids (93/132, 70.44%), and mechanical ventilation (66, 51.16%) were the most common predisposing factors. Totally, 72 (50.35%) of 143 patients with CAFIs died (data were not available for 26 patients).
Conclusion
Fungal infections are evident to be a complication of COVID-19 in Iran; thus, clinicians should consider them as a differential diagnosis, especially in patients with comorbidities and previous antibiotic or corticosteroid use.
Introduction
The coronavirus disease 2019 (COVID-19), which started as a pneumonia epidemic in Wuhan, China, in December 2019, has become a global issue due to its high prevalence and rapid transmission [1]. It has been diagnosed in hundreds of million cases and killed millions of people around the world [2]. In addition to the harmful effects of the virus, such as dysregulation of immune response and direct damage to pulmonary and extra-pulmonary tissues, COVID-19 can be accompanied by infections caused by other microorganisms [3, 4].
Fungal, bacterial, and viral co-infections and super-infections have been detected in patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), leading to more difficult management and increased morbidity and mortality [5]. Fungal infections have been reported in 3.7% of COVID-19 patients, with a higher occurrence (9.6%) in ICU-admitted cases [6]. They have been shown to increase fatality in COVID-19 patients, which can be reduced with the prescription of antifungal medications [7]. Aspergillosis, candidiasis, and mucormycosis are the most commonly reported CAFIs while other infections such as cryptococcosis, Pneumocystis jirovecii pneumonia, coccidioidomycosis, Paracoccidioidomycosis, and histoplasmosis have also been disclosed [8, 9].
COVID-19 weakens the cellular immunity due to decreasing T lymphocytes and alters the respiratory and gastrointestinal microbiota, which can make patients more susceptible to fungal infections [10, 11]. Long stays at hospitals, especially ICU, mechanical ventilation, the use of broad-spectrum antibiotics and corticosteroids in COVID-19 patients may also contribute to an increased risk of mycoses [12, 13].
Following the COVID-19 spread in Iran, cases of CAFIs have been reported from different parts of the country [14–16]. To date, there is no comprehensive study of fungal infections in patients with COVID-19 in Iran. In this systematic review, we aim to summarize the studies that have reported CAFIs in Iran.
Methods
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (S1 File) [17], and the protocol of this review was registered in the International Prospective Register of Systematic Reviews (PROSPERO registration code: CRD42021287258). We performed a comprehensive search for studies concerning fungal infections diagnosed in COVID-19 patients reported from Iran during 2020 and 2021.
Electronic databases, including PubMed, Web of Science, Scopus, Cochrane Library, SID, Magiran, and IranDoc, as well as Google Scholar search engine, were searched on November 5, 2021. The systematic search was conducted with a combination of keywords such as ‘COVID-19’, ‘SARS-CoV-2’, ‘fungal infections’, ‘candidiasis’, ‘mucormycosis’, ‘aspergillosis’, and ‘Iran’. An exhaustive list of keywords and MeSH terms used for PubMed search is provided in S2 File. The search results were filtered for Persian and English languages and publication date from January 1, 2020. There was no limitation on the study design. Moreover, references of selected articles were investigated for additional relevant articles.
The inclusion criteria were: (1) the studies concerned patients diagnosed with COVID-19, (2) the subjects became infected with a type of fungi simultaneously or after contracting COVID-19, (3) the studies took place in Iran, (4) the articles were written in English or Persian. Reviews, letters, animal studies, and studies that did not contain clinical data of infected patients were excluded.
Titles and abstracts of the retrieved articles were screened independently by two reviewers. Next, the full-text articles were reviewed by two independent authors to determine the eligibility of reports based on the inclusion criteria. The risk of bias of the studies was assessed by two independent reviewers using the Joanna Briggs Institute critical appraisal tools (https://jbi.global/critical-appraisal-tools). In case of any disagreement between the two authors in each stage, a third author was consulted. Two researchers independently extracted data, including bibliographic, demographic, and clinical details. Disagreement between data collectors was resolved through discussing a third reviewer.
The bibliographic data included the first author, year of publication, and study design. Demographic features consisted of the province, sample size, incidence, mortality rate, age, gender, past medical history, and drug history. Clinical details included signs and symptoms, laboratory and radiological findings, diagnostic methods, and treatment separately for COVID-19 and fungal infections; as well as duration between COVID-19 and fungal infection diagnosis, genera and species of fungi, site of fungal infection, antifungal susceptibility tests, and outcome of treatment. The extracted data were reviewed, and variables with an acceptable proportion of available values were summarized as mean ± SD or frequency (percentage).
Results
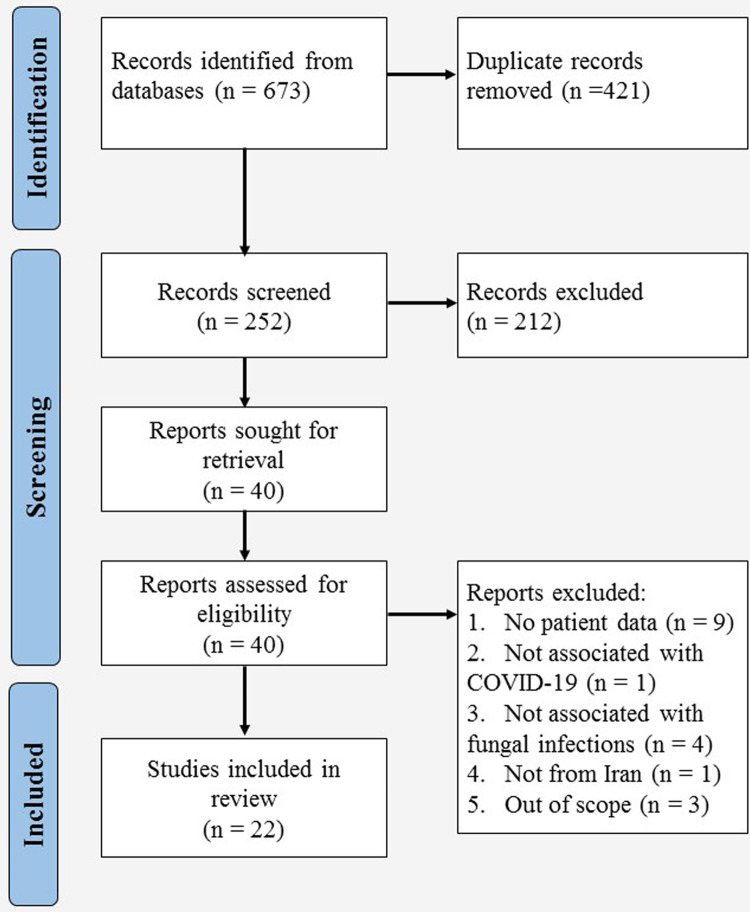
Database searching resulted in 673 articles, of which 22, including 16 case reports and six cross-sectional studies, were included in the present study (Fig 1) [15, 16, 18–37]. Details of the articles and results of the quality assessment are presented in Table 1 and S3 File, respectively. The reviewed studies comprised 169 cases of fungal infections among Iranian COVID-19 patients with the dominance of candidiasis (85, 50.30%), followed by mucormycosis (35, 20.71%), aspergillosis (29, 17.16%), and fusariosis (6, 3.55%). Three cases of rare infections and 11 (6.51%) cases of uncharacterized mold infections were also found. Details of comorbidities, risk factors, diagnosis, treatment, and outcome are summarized in Tables 2 and 3, separately for the three common fungal infections.
Fig 1. The PRISMA flow diagram for selection of studies reporting data on COVID-19-associated fungal infections in Iran up to November 5, 2021.
Table 1. Details of 22 studies with data of COVID-19-associated fungal infections among Iranian patients published up to November 5, 2021.
| First author | Year of publication | Type of study | Type of fungal infection (N of patients) | Province | Ref. |
|---|---|---|---|---|---|
| Abolghasemi | 2021 | Case report | Aspergillosis (1) | Tehran | [18] |
| Arastehfar | 2021 | Cross-sectional | Candidemia (6), Rhodotorula mucilaginosa fungemia (1) | Khorasan Razavi | [19] |
| Davoodi | 2021 | Case report | Candidemia and endocarditis (1) | Mazandaran | [20] |
| Fazeli | 2021 | Cross-sectional | Mucormycosis (12) | Kermanshah | [21] |
| Ghazanfari | 2021 | Cross-sectional | Aspergillosis (22), fusariosis (6), unidentified mold infections (11), Diaporthe foeniculina infection (1) | Mazandaran | [16] |
| Hakimifard | 2021 | Case report | Aspergillosis (1) | Isfahan | [22] |
| Heydarifard | 2021 | Case report | Mucormycosis (1) | Tehran | [23] |
| Hosseinikargar | 2021 | Case report | Aspergillosis (1) | Khorasan Razavi | [24] |
| Karimi-Galougahi | 2021 | Case report | Mucormycosis (1) | Tehran | [25] |
| Khodavaisy | 2021 | Case report | Aspergillosis (1) | Tehran | [26] |
| Mehrabi | 2021 | Case report | Mucormycosis (1) | Bushehr/Fars | [27] |
| Mohammadi | 2021 | Case report | Mucormycosis (1) | Qazvin | [28] |
| Nasri | 2020 | Case report | Aspergillosis (1) | Isfahan | [29] |
| Ostovan | 2021 | Case report | Mucormycosis (1) | Fars | [30] |
| Pakdel | 2021 | Cross-sectional | Mucormycosis (15) | Tehran | [15] |
| Ranjbar-Mobarake | 2021 | Case report | Sarocladium kiliense infection (1) | Isfahan | [31] |
| Salehi | 2020 | Cross-sectional | Oropharyngeal candidiasis (53) | Tehran | [32] |
| Salehi | 2021 | Case report | Aspergillosis (1) | Tehran | [33] |
| Sharifpour | 2021 | Case report | Aspergillosis (1) | Mazandaran | [34] |
| Shirvani | 2021 | Cross-sectional | Pulmonary candidiasis (25) | Tehran | [35] |
| Tabarsi | 2021 | Case report | Mucormycosis (1) | Tehran | [36] |
| Veisi | 2021 | Case series | Mucormycosis (2) | Tehran | [37] |
Table 2. Frequency of comorbidities and risk factors in COVID-19-associated fungal infection cases reported from Iran up to November 5, 2021.
| Variables | Frequencies based on the type of fungal infection | ||
|---|---|---|---|
| Candidiasis | Mucormycosis | Aspergillosis | |
| Past medical history | Diabetes mellitus (21, 24.70%) | Diabetes mellitus (27, 77.14%) | Diabetes mellitus (10, 35.71%) |
| Immunosuppressive diseases (25, 29.41%) | Hypertension (17, 48.57%) | Hypertension (13, 46.43%) | |
| Cardiovascular diseases (29, 34.11%) | Cardiovascular disease (7, 20%) | Cardiovascular disease (11, 39.28%) | |
| Pulmonary diseases (5, 5.88%) | Pulmonary diseases (4, 11.43%) | Pulmonary diseases (5, 17.24%) | |
| Malignancy (8, 9.41%) | Malignancy (2, 5.71%) | Malignancy (4, 14.28%) | |
| Chronic kidney disease (11, 12.94%) | Chronic kidney disease (2, 5.71%) | Chronic kidney disease (2, 7.14%) | |
| Others (23, 27.05%) | Others (9, %) | Others (4, 13.79%) | |
| Healthy (5, 5.88%) | Healthy (4, 11.43%) | Healthy (3, 10.71%) | |
| Unknown (1) | |||
| Mechanical ventilation | 22/60, 36.7% | 3/22, 13.64% | 23/27, 85.19% |
| Unknown (25) | Unknown (13) | Unknown (2) | |
| Central venous catheter | 11/60, 18.3% | ||
| Unknown (25) | Unknown (35) | Unknown (29) | |
| Intensive care unit hospitalization | 33/60, 55% | 9/26, 34.62% | 26/27, 96.3% |
| Unknown (25) | Unknown (9) | Unknown (2) | |
| Corticosteroid therapy | 25/54, 46.3% | 23/32, 71.87% | 26/27, 96.3% |
| Unknown (31) | Unknown (3) | Unknown (2) | |
| Antibiotic consumption | 56/60, 93.33% | 10/16, 62.5% | 25/28, 89.29% |
| Unknown (25) | Unknown (19) | Unknown (1) | |
Table 3. Description of diagnosis, treatment and outcome of COVID-19-associated fungal infection cases reported from Iran up to November 5, 2021.
| Variables | Frequencies based on the type of fungal infection | ||
|---|---|---|---|
| Candidiasis | Mucormycosis | Aspergillosis | |
| COVID-19 diagnostic method (n, %) | PCR (29, 48.33%) | PCR (18, 51.43%) | PCR + CT (28, 96.55%) |
| PCR + CT (1, 1.66%) | PCR + CT (14, 40%) | CT (1, 3.45%) | |
| Clinical (30, 50%) | CT (2, 5.71%) | ||
| Unknown (25) | Clinical (1, 2.86%) | ||
| Days between COVID-19 and fungal infection diagnosis (mean ± SD) | 8.97 ± 8.89 | 17.18 ± 12.44 | 29 ± 19.3 |
| Unknown (25) | Unknown (1) | Unknown (23) | |
| Fungal infection diagnostic method (n, %) | Microscopic + molecular + culture (53, 62.35%) | Microscopic + imaging (18, 51.43%) | Culture + biomarkera (17, 58.62%) |
| Molecular (25, 29.41%) | Microscopic (15, 42.86%) | Culture (5, 17.24%) | |
| Molecular + culture (6, 7.06%) | Microscopic + culture + molecular + imaging (2, 5.71%) | Biomarker + imaging (2, 6.89%) | |
| Molecular + culture + imaging (1, 1.17%) | Microscopic + culture + Molecular + biomarker + imaging (2, 6.89%) | ||
| Microscopic + culture + Molecular + imaging (2, 6.89%) | |||
| Microscopic + culture + imaging (1, 3.45%) | |||
| Fungal infection treatment (n, %) | FCZ (22, 36.66%) | AMB (1, 2.86%) | VCZ (2, 6.9%) |
| FCZ + NYS (20, 33.33%) | AMB + SI (25, 71.43%) | VCZ + CSP (1, 3.45%) | |
| NYS (10, 16.66%) | AMB + PSZ+ SI (5, 14.28%) | VCZ + AMB (2, 6.9%) | |
| FCZ + CSP (5, 8.33%) | AMB + PSZ + CSP + SI (1, 2.86%) | FCZ + AMB + surgical intervention (1, 3.45%) | |
| CSP (1, 1.66%) | AMB + CSP + SI (2, 5.71%) | AMB (1, 3.45%) | |
| AMB (1, 1.66%) | Systemic antifungal + SI (1, 2.86%) | No treatment (22, 75.86%) | |
| No treatment (1, 1.66%) | |||
| Case fatality rate (%) | 16.66% | 55.88% | 86.2% |
| Unknown (25) | Unknown (1) | ||
PCR: Polymerase chain reaction; CT: computerized tomography scan; FCZ: fluconazole; AMB: Amphotericin B; VCZ: voriconazole; NYS: nystatin; CSP: caspofungin; PSZ: posaconazole; SI: surgical intervention.
aEither galactomannan or β-D-glucan in serum or bronchoalveolar lavage sample.
Candidiasis among Iranian COVID-19 patients
Four studies comprising 85 cases of candidiasis were found among Iranian COVID-19 patients. The mean ± SD of age was 61.98 ± 17.10 years, and 44 (51.76%) patients were female. The cases included oropharyngeal candidiasis (53, 62.35%), pulmonary candidiasis (25, 29.41%), candidemia (6, 7.06%), and endocarditis (1, 1.18%). In total, 97 Candida isolates were recovered from the patients (9 cases of mixed infection), and C. albicans (74, 76.29%) was the most common species, followed by C. glabrata (4, 4.71%), C. dubliniensis (3, 3.53%), C. tropicalis (2, 2.35%), C. parapsilosis (1, 1.18%), and C. krusei (1, 1.18%).
Mixed infection cases included C. albicans + C. glabrata (2, 2.35%), C. albicans + C. parapsilosis (2, 2.35%), C. albicans + C. tropicalis (1, 1.18%), C. albicans + C. dubliniensis (1, 1.18%), C. albicans + C. glabrata + C. dubliniensis (2, 2.35%), and C. albicans + C. glabrata + C. parapsilosis (1, 1.18%).
Mucormycosis among Iranian COVID-19 patients
Nine studies composed of 35 cases of mucormycosis, 19 (54.29%) males and 16 (45.71%) females, were retrieved. The mean ± SD of age was 55.97 ± 12.93 years. All patients had rhino-orbital-cerebral manifestations, with orbital involvement in 32 (91.43%) and rhino-sinusitis in three (8.57%) cases. The orbital infections comprised of rhino-sino-orbital (17, 48.57%), rhino-orbital (7, 20%), sino-orbital (5, 14.29%), orbital (2, 5.71%), and rhino-sino-orbito-cerebral (1, 2.86%) involvements. Definitive identification of the causative agents was made for only two cases of Rhizopus arrhizus (R. oryzae).
Aspergillosis among Iranian COVID-19 patients
Eight studies comprising 29 cases of aspergillosis were reported among patients with COVID-19 from Iran. The patients were 62.97 ± 12.68 years old, and 15 (51.72%) were male. Pulmonary infection (27, 93.1%) was the most common clinical form of the disease; in addition, one patient (3.45%) with disseminated (pulmonary + cerebral) and one patient (3.45%) with rhinosinusitis were reported. In total, 26 out of 29 isolates were identified to the species level. Aspergillus flavus (15/26, 57.69%) was the most common etiological agent, and the remaining isolates included A. fumigatus (3, 11.54%), A. japonicus (3, 11.54%), A. niger (2, 7.69%), A. ochraceus (1, 3.85%), A. terreus (1, 3.85%), and A. tubingensis (1, 3.85%).
Fusariosis among Iranian COVID-19 patients
Six cases of pulmonary fusariosis, two males (33.33%) and four females (66.67%), were found in PCR-confirmed COVID-19 cases with a mean ± SD age of 67 ± 12.66 years. The causative agents, including Fusarium incranatum (3, 50%), F. fujikuroi (1, 16.67%), F. equiseti (1, 16.67%), and F. solani (1, 16.67%) were detected through bronchoalveolar lavage (BAL) culture; and five patients had positive BAL galactomannan (GM) test.
Hypertension (4, 66.67%), cardiovascular diseases (3, 50%), diabetes mellitus (2, 33.33%), and chronic kidney diseases (1, 16.67%) were the reported underlying diseases. All six patients were admitted to ICU, mechanically ventilated, and received antibiotics and corticosteroids. None of the patients received antifungal medications, and all of them regrettably died.
Rare or uncharacterized fungal infections among Iranian COVID-19 patients
Three cases of CAFI caused by rare fungi were reported:
Fungemia due to Rhodotorula mucilaginosa in an ICU-admitted, mechanically ventilated, 68-year-old female without underlying diseases, who was effectively treated with fluconazole.
Disseminated infection due to Sarocladium kiliense in a 74-year-old diabetic female receiving corticosteroid and antibiotics. She did not survive despite receiving liposomal amphotericin B.
Pulmonary infection due to Diaporthe foeniculina in a 67-year-old female with diabetes, hypertension, chronic kidney disease and ischemic heart disease, with a history of ICU admission, mechanical ventilation, corticosteroid and antibiotic therapy. The patient received no antifungal treatment and died.
Eleven cases of uncharacterized pulmonary mold infections were also found in ICU-admitted patients who underwent mechanical ventilation, corticosteroid and antibiotic therapy. They were detected by high levels of GM (serum GM index > 0.5 or BAL GM index ≥ 1). None of the patients were prescribed antifungals, and all except one passed away.
Discussion
This systematic review showed that the most common fungal infections reported in Iranian COVID-19 patients are candidiasis, mucormycosis, and aspergillosis. Previous global reviews also found members of Candida, Aspergillus, and Mucorales among the most frequent fungi causing secondary infections in people with COVID-19 [6, 8, 9, 38].
Results of the present review are based on a limited number of studies, mainly case reports, which are prone to variation by future reports. Meanwhile, the thorough systematic search and exhaustive data collection provide a comprehensive description of CAFIs to the date of database searching across the country, which could be considered a strength of this report.
COVID-19-associated candidiasis (CAC)
Candida is the most prevalent fungal pathogen causing superinfections and the second most common source of coinfections in COVID-19 patients [39]. A cross-sectional study of the patients’ registry in an American hospital showed that 12% of patients diagnosed with COVID-19 had candidiasis, and patients with candidiasis were 3.73 times more likely to be diagnosed with COVID-19 [40]. In this review, around half of the reported CAFI cases were caused by Candida spp., the most common fungal pathogens in Iranian COVID-19 patients.
The exact pathogenesis of CAC is not clarified, but several factors have been suggested to explain the predisposition of patients with COVID-19 to Candida infections. The SARS-CoV-2 infection can cause lymphopenia and consequent impairment of immune defense against fungal agents including Candida spp. [41, 42]. Severe COVID-19 is associated with elevation of blood lactate and acidosis [43, 44], which enables Candida to restructure its cell wall to mask β-glucans and escape the recognition by the host immune system [45]. Moreover, an important virulence factor of Candida that helps it evade phagocytosis is the ability to form biofilms, which can be triggered by COVID-19 through increasing oxidative stress and pH imbalance [41].
On the other hand, COVID-19 patients are at an increased risk of contracting candidiasis because of the treatments they receive. Consumption of corticosteroids, antibiotics, and TNF-α inhibitors, as well as undergoing mechanical ventilation, central venous catheterization, and extracorporeal membrane oxygenation (ECMO) are risk factors for developing candidiasis [41, 46–48]. Concordant to previous studies, a significant proportion of the patients in our review were exposed to antibiotic consumption, corticosteroid use, mechanical ventilation, and central venous catheterization. However, we did not find any report of patients with CAC who had received a TNF-α inhibitor or went through ECMO, as these are less commonly indicated for COVID-19 treatment.
Another predictor of developing CAC is admission to ICU, which is often accompanied by interventions such as mechanical ventilation and central venous catheterization and can raise the risk of nosocomial Candida infections [41]. In our study, 55% of the CAC cases (100% of patients with candidemia) stayed in ICU, emphasizing the need for more attention to ICU patients in terms of prompt diagnosis of candidiasis.
A global review showed that CAC is more likely to involve male patients with more than 40 years of age [38]. This is probably because of the fact that higher age and male gender are associated with more severe COVID-19 and the need for ICU admission [49, 50]. Expectedly, the Iranian CAC cases were about 62 years old on average. However, with female patients being reported slightly more than males, no significant gender difference was found in our review.
The most common species causing CAC throughout the world is C. albicans, which has also been the most frequent causative agent of candidiasis before the pandemic [38, 51]. Similarly, the majority of Candida isolates obtained from Iranian patients were identified as C. albicans. The following frequent pathogens in Iran were C. glabrata, C. dubliniensis, C. parapsilosis, and C. tropicalis; which were also among the most common species in other countries [52–56]. Furthermore, Salehi et al. reported one case of CAC caused by C. krusei [32]. A less prevalent species, this pathogen was detected in two other CAC cases from India and Spain [54, 55].
While cases of C. auris, C. lusitaniae, C. orthopsilosis, and C. inconspicua were reported globally, they were not found in Iranian patients [55, 57–62]. This is not surprising as we know there are regional differences in the global distribution of Candida species [63]. For example, while C. auris outbreaks have been reported from India, Pakistan, USA, Venezuela, South Africa, Spain and the United Kingdom [64]; only limited sporadic cases of this species were reported from Iran [65–67]. In addition, C. auris and other rare pathogens might have been missed due to the lack of proper diagnostic tools in Iran; thus, the differences might result from the use of culture and PCR for identifying the causative agents [65, 68, 69].
Oropharyngeal candidiasis (OPC) is a common form of Candida infection, which has been reported in people with COVID-19 as well [48, 70]. In the majority of CAC patients described in this review, the infection was localized in the oropharyngeal area. Pulmonary candidiasis rarely happens in critically ill patients with multiple risk factors [71, 72]. Although Shirvani et al. reported 25 cases of COVID-19 patients with Candida spp. detected in their BAL fluid [35], no other pulmonary CAC was reported from other countries. There is no consensus on whether Candida can actually cause pulmonary infection or whether its presence in BAL samples is due to colonization [73, 74].
Candidemia, which is 3–8 times more frequent in COVID-19 patients compared to the non-COVID-19 population [75, 76], was confirmed in six Iranian COVID-19 patients [19]. Moreover, a case of endocarditis caused by C. tropicalis was reported in an Iranian patient with prosthetic heart valves, who died despite receiving liposomal amphotericin B [20]. Another case of endocarditis caused by C. albicans was diagnosed in an Italian COVID-19 patient with a central venous catheter [77]. Fungal endocarditis is a rare and hard-to-treat condition leading to a 50% mortality, with C. albicans being the causative agent in 24–46% of cases [78]. In a study conducted in 2009–2011 on Iranian patients with infective endocarditis who did not respond to antibacterial treatment, C. albicans has been documented in two out of eleven cases. These two patients were intravenous drug abusers and responded to treatment with surgical removal and amphotericin B [79]. What this study brings to mind is that surgical removal of the vegetations might have improved the outcome as the C. tropicalis isolate was proved to be sensitive to amphotericin. Based on a review of global studies, CAC has a mortality rate ranging from 11 to 100% based on the infection site and clinical conditions [38]. In this study, all cases with candidemia and endocarditis died; nonetheless, the overall mortality rate was 16.66% because of the low fatality of OPC. Studies with large sample sizes and adjustments of underlying factors are warranted to estimate the attributable mortality of different categories of CAC.
COVID-19-associated mucormycosis (CAM)
Over the last decade, mucormycosis has been more frequently diagnosed, especially in India [80]. A pre-pandemic study showed an increased incidence (about 2.5 times) of mucormycosis during the years 2008–2014 in Iran [81]. Besides, this infection has become 50 times more prevalent in the COVID-19 era globally [82]. CAM has been primarily seen in India, while cases from other countries, including Iran, have also been reported [83].
Two major risk factors of CAM are diabetes mellitus (present in 79–85% of patients) and use of corticosteroids (prescribed in 76.3–85% of cases) [8, 38, 84–86]. Similarly, the most frequent risk factor in Iranian CAM patients was diabetes mellitus, present in the majority (77.14%) of patients, and corticosteroid treatment with a 71.87% frequency. It should be noted that corticosteroids are not always prescribed correctly, as it is demonstrated that only 28.8% of cases in India and 52.6% in other countries received corticosteroids based on indication and with accurate dosage [83]. Male gender might also be related to a higher incidence of CAM, as several studies have shown more than 70% of patients were men [38, 85–88]. However, with men accounting for 54% of Iranian patients, the male preponderance was not as significant as in previous studies. Since limited cases have been studied, more extensive research is needed to understand the gender distribution of CAM both in Iran and the world. The average age of CAM patients was 56 years in Iran, roughly similar to a 55 years median in worldwide studies [89].
Making up 57% of culture results, Rhizopus spp. are the most commonly identified fungi in CAM cases worldwide [84]. Mucor spp. and Lichteimia spp. were also diagnosed in a small number of cases [38]. In the studies of this review, the species were not identified except for two cases of R. arrhizus. The rationale for the lack of data about species is that identifying mucormycosis agents to the level of genera and species for clinical management is not strongly supported by evidence, although recommended for epidemiological purposes [90]. Besides, culture has a low sensitivity (50%) to identify the species, and molecular techniques are not yet standardized and yield heterogeneous results [91].
The most common form of the disease, with or without COVID-19, is rhino-orbital-cerebral mucormycosis (ROCM) [80, 92]. All 35 CAM cases from Iran fell into this category, with a 91.43% orbital and 2.86% cerebral involvement. While not found in our review, several cases of lung, bone, gastrointestinal, and skin involvement were reported from other countries [93–101]. The absence of reported CAM cases of organs other than the nose, sinus, and orbits from Iran might be because of the rarity of these infections, the non-specificity of their presentations, and the lack of awareness among clinicians about the uncommon presentations of mucormycosis. The mortality rate of CAM has been estimated at 30–52% in various review studies [38, 84, 86, 102]. In the present review, 55.88% of patients died despite treatment, comparable to the 61.9% mortality rate in countries other than India [83]. The mortality rate of CAM in India is lower (14–36.5%), probably because of the higher prevalence of ROCM in Indian patients [83, 87], as it is known that disseminated and pulmonary mucormycosis are associated with higher mortality rates than ROCM and cutaneous infection [90]. Nevertheless, since none of the Iranian cases had disseminated or pulmonary infection, this cannot be the reason for the higher fatality rate. However, the higher prevalence of orbital involvement in the Iranian (91.43%) compared to the Indian (72%) CAM cases might be a sign of neglect and delayed diagnosis, as well as the possible source of the poorer prognosis, as orbital involvement with vision loss is associated with a higher mortality rate [87].
The treatment of choice for mucormycosis is amphotericin B, which is more effective when combined with surgical interventions [103]. Isavuconazole and posaconazole, alone or in combination with amphotericin B, are recommended as first-line or salvage therapy [104, 105]. Almost all patients in our review received amphotericin B and surgical interventions (Table 3). Although we did not analyze the data statistically, it was noticed that all eight cases that received one or two drugs (caspofungin, posaconazole or both) in addition to Amphotericin B survived while monotherapy with Amphotericin B led to ~73% mortality. This highlights the need for further clinical trials as the efficiency of combination therapy is proposed by limited studies yet not supported by enough evidence [104, 106].
COVID-19-associated aspergillosis (CAA)
Observed in 7.7–27.7% of patients with severe COVID-19, aspergillosis is another fungal infection frequently seen along with this viral infection [107]. COVID-19-associated pulmonary aspergillosis (CAPA) affects up to 35% of ICU patients with COVID-19, leading to a 54.9% mortality rate [108, 109]. CAA of the nose and sinuses was also reported from India and Egypt [110–113]. Twenty-nine CAA cases were reported from Iran, of which 27 were diagnosed with CAPA, in addition to two patients with rhinosinusitis and disseminated infection.
CAPA is almost exclusive to ICU-admitted patients, while Aspergillus rhinosinusitis was reported in several outpatient COVID-19 cases [108, 111, 114, 115]. All except one of the Iranian cases with available data were admitted to ICUs. Corticosteroids (96.3%), antibiotics (89.29%), and mechanical ventilation (85.19%) were used in a large proportion of the patients in our review. A global study revealed a high frequency of mechanical ventilation (94.1%), but corticosteroid use was less frequent (52.7%) [115]. The exact antibiotic use frequency has not been reported in CAPA patients, but a 75% proportion could be presumed based on data from ICU-admitted COVID-19 patients [116]. The differences can be explained by the prescription of dexamethasone, ceftriaxone and azithromycin per institutional protocol in all patients of the Ghazanfari et al. study, which is the reference for the majority of our patients [16].
Hypertension was the most common comorbidity both in our study (46.43%) and a worldwide review (24%) [108]. Another study reported cardiovascular diseases (50.5%) as the most prevalent underlying condition in CAPA patients [115], and we found it in 39.28% of patients in our review. Diabetes mellitus, malignancies and pulmonary diseases are also common among CAPA patients both in Iran and other countries [108, 115, 117]. However, none of these comorbidities are significantly different in CAPA and other ICU-admitted COVID-19 patients [117].
The most prevalent causative agent of CAPA is A. fumigatus, observed in more than 80% of cases globally [108, 114, 116]. However, in Iran, A. fumigatus was the second most common pathogen after A. flavus, identified in more than half of Iranian CAPA cases. This is not unexpected as previous studies on species distribution of Aspergillus in Iran before the COVID-19 outbreak showed that A. flavus had the highest prevalence, followed by A. fumigatus, A. niger, and A. terreus [118, 119]. The disseminated aspergillosis case was caused by A. ochraceus, which has not been reported, to our knowledge, in other COVID-19 patients. A. ochraceus is a rare pathogen, previously described in two case reports of chronic pulmonary aspergillosis and allergic bronchopulmonary aspergillosis [120, 121].
The fatality rate of CAA in Iran was estimated at 86.2%, which is remarkably higher than CAPA all-cause mortality rates in global studies (42.6–54.1%) [108, 115, 122]. The global rate is even lower when the cause of death is limited to CAPA (17.2%) [115]. Apostolopoulou et al. found an association between age, male sex and pulmonary diseases with mortality of CAPA in a global review [108]. None of these factors can be the reason for the higher mortality in the Iranian patients, who were on average 62.97 years old (vs 67% worldwide), 51.72% male (vs 75.4% worldwide), and 17.85% with pulmonary comorbidities (vs 20% worldwide) [108]. The difference in the mortality rate of Iranian and global cases can be explained by the fact that 22 out of 29 patients, for an unknown reason, did not receive antifungal treatment [16]. Only two out of seven patients who received antifungal treatment survived; both received voriconazole, which is considered the first-line therapy of invasive pulmonary aspergillosis and is the most frequently prescribed drug for CAPA worldwide [108, 114, 116].
COVID-19-associated fusariosis and other CAFIs
Scattered cases of fusariosis have been reported in COVID-19 patients across the globe. For instance, two patients with severe COVID-19 infected with F. verticillioides and F. proliferatum were reported from Argentina and France, respectively [123, 124]. In addition, two cases of fusariosis were detected in mechanically-ventilated COVID-19 patients among subjects of observational studies from France and Spain [125, 126]. In one of the studies we reviewed, six COVID-19 patients with acute respiratory distress syndrome (ARDS) had pulmonary fusariosis [16].
It is noteworthy that none of these patients had the classic risk factors of invasive fusariosis, i.e., hematologic malignancy and history of transplant [127]. However, all of them were mechanically ventilated and received corticosteroids and antibiotics, emphasizing the role of COVID-19 and its treatment in triggering Fusarium invasion. Treatment of fusariosis is difficult due to the resistance to most antifungal drugs, its optimal treatment is yet to be discovered, and its mortality rate remains high [128–130]. Thus, it is not unexpected that all Iranian patients died, with this in mind that all were high-risk COVID-19 ICU patients and did not receive any antifungal drugs.
COVID-19 patients are prone to infections by uncommon fungal pathogens. Three instances of very rare fungal infections were reported in Iranian COVID-19 patients, namely R. mucilaginosa and S. kiliense, and D. foeniculina [16, 19, 31]. This highlights the importance of considering emerging and rare fungi as a differential diagnosis of COVID-19 complications. To the best of our knowledge, these fungi have not been reported in other patients with COVID-19 at the time of writing this article.
Eleven cases described as probable pulmonary mold infections were detected by serum or BAL GM [16]. GM testing in serum and BAL samples is used as a screening and diagnostic tool; however, its positive predictive value ranges between 0 and 100% [131]. Therefore, the diagnosis of mold infection in these cases is undetermined, as the respiratory features and radiological findings can be attributed to SARS-CoV-2 or other organisms.
Conclusion
Fungal infections are evident to be a complication of COVID-19 in Iran, especially in patients with diabetes mellitus, cardiovascular diseases, and those receiving antibiotics, corticosteroids, and mechanical ventilation. Candidiasis, mucormycosis and aspergillosis are the most common CAFIs in Iran. However, less common infections like fusariosis and cases of rare infections have also been reported. Accordingly, clinicians should avoid neglecting fungal infections by acknowledging them as differential diagnoses and ordering confirmative laboratory tests in high-risk patients or those not responding to routine treatments.
Supporting information
(DOCX)
(DOCX)
(XLSX)
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
SM received a grant (grant number: 1400-3-99-22062) from Iran University of Medical Sciences, Tehran, Iran. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Naserghandi A, Allameh S, Saffarpour RJNM, Infections N. All about COVID-19 in brief. 2020;35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Worldometers.Info. Dover, Delaware, U.S.A.2022 [Available from: https://www.worldometers.info/coronavirus/.
- 3.Lansbury L, Lim B, Baskaran V, Lim WSJJOI. Co-infections in people with COVID-19: a systematic review and meta-analysis. 2020;81(2):266–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar A, Narayan RK, Prasoon P, Kumari C, Kaur G, Kumar S, et al. COVID-19 Mechanisms in the Human Body—What We Know So Far. Frontiers in Immunology. 2021;12. doi: 10.3389/fimmu.2021.693938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia-Vidal C, Sanjuan G, Moreno-García E, Puerta-Alcalde P, Garcia-Pouton N, Chumbita M, et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. 2021;27(1):83–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alhumaid S, Al Mutair A, Al Alawi Z, Alshawi AM, Alomran SA, Almuhanna MS, et al. Coinfections with Bacteria, Fungi, and Respiratory Viruses in Patients with SARS-CoV-2: A Systematic Review and Meta-Analysis. Pathogens. 2021;10(7). 10.3390/pathogens10070809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.White PL, Dhillon R, Cordey A, Hughes H, Faggian F, Soni S, et al. A National Strategy to Diagnose Coronavirus Disease 2019-Associated Invasive Fungal Disease in the Intensive Care Unit. Clin Infect Dis. 2021;73(7):e1634–e44. doi: 10.1093/cid/ciaa1298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abdoli A, Falahi S, Kenarkoohi A. COVID-19-associated opportunistic infections: a snapshot on the current reports. Clin Exp Med. 2021:1–20. doi: 10.1007/s10238-021-00751-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amin A, Vartanian A, Poladian N, Voloshko A, Yegiazaryan A, Al-Kassir AL, et al. Root Causes of Fungal Coinfections in COVID-19 Infected Patients. Infect Dis Rep. 2021;13(4):1018–35. doi: 10.3390/idr13040093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. The Lancet Respiratory medicine. 2020;8(4):420–2. doi: 10.1016/S2213-2600(20)30076-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang B, Zhang L, Wang Y, Dai T, Qin Z, Zhou F, et al. Alterations in microbiota of patients with COVID-19: potential mechanisms and therapeutic interventions. Signal Transduct Target Ther. 2022;7(1):143. doi: 10.1038/s41392-022-00986-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song G, Liang G, Liu WJM. Fungal co-infections associated with global COVID-19 pandemic: a clinical and diagnostic perspective from China. 2020:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gangneux JP, Bougnoux ME, Dannaoui E, Cornet M, Zahar JR. Invasive fungal diseases during COVID-19: We should be prepared. Journal de Mycologie Médicale. 2020;30(2):100971. doi: 10.1016/j.mycmed.2020.100971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salehi M, Ahmadikia K, Badali H, Khodavaisy SJM. Opportunistic fungal infections in the epidemic area of COVID-19: a clinical and diagnostic perspective from Iran. 2020;185(4):607–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pakdel F, Ahmadikia K, Salehi M, Tabari A, Jafari R, Mehrparvar G, et al. Mucormycosis in patients with COVID-19: A cross-sectional descriptive multicentre study from Iran. Mycoses. 2021;64(10):1238–52. doi: 10.1111/myc.13334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghazanfari M, Arastehfar A, Davoodi L, Charati JY, Moazeni M, Abastabar M, et al. Pervasive but Neglected: A Perspective on COVID-19-Associated Pulmonary Mold Infections Among Mechanically Ventilated COVID-19 Patients. Front Med (Lausanne). 2021;8:13. doi: 10.3389/fmed.2021.649675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Page MJ, Mckenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abolghasemi S, Hakamifard A, Sharifynia S, Toutkaboni MP, Tehrani HA. Fatal invasive pulmonary aspergillosis in an immunocompetent patient with COVID-19 due to Aspergillus terreus: A case study. Clin Case Rep. 2021;9(4):2414–8. doi: 10.1002/ccr3.4051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arastehfar A, Shaban T, Zarrinfar H, Roudbary M, Ghazanfari M, Hedayati MT, et al. Candidemia among Iranian Patients with Severe COVID-19 Admitted to ICUs. J Fungi (Basel). 2021;7(4). doi: 10.3390/jof7040280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davoodi L, Faeli L, Mirzakhani R, Jalalian R, Shokohi T, Kermani FJCMM. Catastrophic Candida prosthetic valve endocarditis and COVID-19 comorbidity: A rare case. Curr Med Mycol. 2021;7(2):43–7. doi: 10.18502/cmm.7.2.7157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fazeli MA, Rezaei L, Javadirad E, Iranfar K, Khosravi A, Saman JA, et al. Increased incidence of rhino-orbital mucormycosis in an educational therapeutic hospital during the COVID-19 pandemic in western Iran: An observational study. Mycoses. 2021;64(11):1366–77. doi: 10.1111/myc.13351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hakamifard A, Hashemi M, Fakhim H, Aboutalebian S, Hajiahmadi S, Mohammadi R. Fatal disseminated aspergillosis in an immunocompetent patient with COVID-19 due to Aspergillus ochraceus. J Mycol Med. 2021;31(2):101124. doi: 10.1016/j.mycmed.2021.101124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heydarifard Z, Safaei M, Zadheidar S, Ehsan S, Shafiei‐Jandaghi NZ. Mucormycosis infection in severe COVID‐19 patient with multiple underlying health conditions. Clin Case Rep. 2021;9(10). doi: 10.1002/ccr3.5009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hosseinikargar N, Basiri R, Asadzadeh M, Najafzadeh MJ, Zarrinfar H. First report of invasive Aspergillus rhinosinusitis in a critically ill COVID-19 patient affected by acute myeloid leukemia, northeastern Iran. Clin Case Rep. 2021;9(10):e04889. doi: 10.1002/ccr3.4889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karimi-Galougahi M, Arastou S, Haseli S. Fulminant mucormycosis complicating coronavirus disease 2019 (COVID-19). Int Forum Allergy Rhinol. 2021;11(6):1029–30. doi: 10.1002/alr.22785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khodavaisy S, Khajavirad N, Izadi A, Dehghan Manshadi SA, Abdollahi A, Aliramezani A, et al. Proven pulmonary aspergillosis in a COVID-19 patient: A case report. Curr Med Mycol. 2021;7(2):39–42. doi: 10.18502/cmm.7.2.7031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mehrabi Z, Salimi M, Niknam K, Mohammadi F, Mamaghani HJ, Sasani MR, et al. Sinoorbital Mucormycosis Associated with Corticosteroid Therapy in COVID-19 Infection. Case Reports in Ophthalmological Medicine. 2021;2021:9745701. doi: 10.1155/2021/9745701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mohammadi F, Badri M, Safari S, Hemmat N. A case report of rhino-facial mucormycosis in a non-diabetic patient with COVID-19: a systematic review of literature and current update. BMC Infect Dis. 2021;21(1):906. doi: 10.1186/s12879-021-06625-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nasri E, Shoaei P, Vakili B, Mirhendi H, Sadeghi S, Hajiahmadi S, et al. Fatal Invasive Pulmonary Aspergillosis in COVID-19 Patient with Acute Myeloid Leukemia in Iran. Mycopathologia. 2020;185(6):1077–84. doi: 10.1007/s11046-020-00493-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ostovan VR, Rezapanah S, Behzadi Z, Hosseini L, Jahangiri R, Anbardar MH, et al. Coronavirus disease (COVID-19) complicated by rhino-orbital-cerebral mucormycosis presenting with neurovascular thrombosis: a case report and review of literature. J Neurovirol. 2021;27(4):644–9. doi: 10.1007/s13365-021-00996-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ranjbar-Mobarake M, Nowroozi J, Badiee P, Mostafavi SN, Mohammadi R. Fatal disseminated infection due to Sarocladium kiliense in a diabetic patient with COVID-19. Clin Case Rep. 2021;9(9):6. 10.1002/ccr3.4596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salehi M, Ahmadikia K, Mahmoudi S, Kalantari S, Jamalimoghadamsiahkali S, Izadi A, et al. Oropharyngeal candidiasis in hospitalised COVID-19 patients from Iran: Species identification and antifungal susceptibility pattern. Mycoses. 2020;63(8):771–8. doi: 10.1111/myc.13137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salehi M, Khajavirad N, Seifi A, Salahshour F, Jahanbin B, Kazemizadeh H, et al. Proven Aspergillus flavus pulmonary aspergillosis in a COVID-19 patient: A case report and review of the literature. Mycoses. 2021;64(8):809–16. doi: 10.1111/myc.13255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sharifpour A, Zakariaei Z, Fakhar M, Banimostafavi ES, Nakhaei M, Soleymani M. Post-COVID-19 co-morbidity of emerged Lophomonas infection and invasive pulmonary aspergillosis: First case report. Clin Case Rep. 2021;9(9):e04822. doi: 10.1002/ccr3.4822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shirvani F, Fattahi A. Pulmonary Candidiasis Associated with COVID-19: Evaluation of Causative Agents and their Antifungal Susceptibility Patterns. Tanaffos. 2021;20(1):29–35. [PMC free article] [PubMed] [Google Scholar]
- 36.Tabarsi P, Khalili N, Pourabdollah M, Sharifynia S, Naeini AS, Ghorbani J, et al. Case Report: Coronavirus Disease 2019-associated Rhinosinusitis Mucormycosis Caused by Rhizopus arrhizus: A Rare but Potentially Fatal Infection Occurring After Treatment with Corticosteroids. Am J Trop Med Hyg. 2021;105(2):449–53. doi: 10.4269/ajtmh.21-0359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Veisi A, Bagheri A, Eshaghi M, Rikhtehgar MH, Rezaei Kanavi M, Farjad R. Rhino-orbital mucormycosis during steroid therapy in COVID-19 patients: A case report. Eur J Ophthalmol. 2021:11206721211009450. doi: 10.1177/11206721211009450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Frías-De-León MG, Pinto-Almazán R, Hernández-Castro R, García-Salazar E, Meza-Meneses P, Rodríguez-Cerdeira C, et al. Epidemiology of Systemic Mycoses in the COVID-19 Pandemic. J Fungi (Basel). 2021;7(7). doi: 10.3390/jof7070556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Musuuza JS, Watson L, Parmasad V, Putman-Buehler N, Christensen L, Safdar N. Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: A systematic review and meta-analysis. PLoS One. 2021;16(5):e0251170. doi: 10.1371/journal.pone.0251170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Katz J. Prevalence of candidiasis and oral candidiasis in COVID-19 patients: a cross-sectional pilot study from the patients’ registry in a large health center. Quintessence Int. 2021;52(8):714–8. doi: 10.3290/j.qi.b1491959 [DOI] [PubMed] [Google Scholar]
- 41.Ahmed N, Mahmood MS, Ullah MA, Araf Y, Rahaman TI, Moin AT, et al. COVID-19-Associated Candidiasis: Possible Patho-Mechanism, Predisposing Factors, and Prevention Strategies. Curr Microbiol. 2022;79(5):127. doi: 10.1007/s00284-022-02824-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anka AU, Tahir MI, Abubakar SD, Alsabbagh M, Zian Z, Hamedifar H, et al. Coronavirus disease 2019 (COVID-19): An overview of the immunopathology, serological diagnosis and management. Scand J Immunol. 2021;93(4):e12998. doi: 10.1111/sji.12998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nechipurenko YD, Semyonov DA, Lavrinenko IA, Lagutkin DA, Generalov EA, Zaitceva AY, et al. The Role of Acidosis in the Pathogenesis of Severe Forms of COVID-19. Biology (Basel). 2021;10(9). doi: 10.3390/biology10090852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carpenè G, Onorato D, Nocini R, Fortunato G, Rizk JG, Henry BM, et al. Blood lactate concentration in COVID-19: a systematic literature review. Clinical Chemistry and Laboratory Medicine (CCLM). 2022;60(3):332–7. doi: 10.1515/cclm-2021-1115 [DOI] [PubMed] [Google Scholar]
- 45.Ballou ER, Avelar GM, Childers DS, Mackie J, Bain JM, Wagener J, et al. Lactate signalling regulates fungal β-glucan masking and immune evasion. Nat Microbiol. 2016;2:16238. doi: 10.1038/nmicrobiol.2016.238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Concia E, Azzini AM, Conti M. Epidemiology, incidence and risk factors for invasive candidiasis in high-risk patients. Drugs. 2009;69 Suppl 1:5–14. doi: 10.2165/11315500-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 47.Arastehfar A, Carvalho A, Nguyen MH, Hedayati MT, Netea MG, Perlin DS, et al. COVID-19-Associated Candidiasis (CAC): An Underestimated Complication in the Absence of Immunological Predispositions? J Fungi (Basel). 2020;6(4). doi: 10.3390/jof6040211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pankhurst CL. Candidiasis (oropharyngeal). BMJ Clin Evid. 2013;2013:1304. [PMC free article] [PubMed] [Google Scholar]
- 49.Peckham H, De Gruijter NM, Raine C, Radziszewska A, Ciurtin C, Wedderburn LR, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11(1):6317. doi: 10.1038/s41467-020-19741-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Romero Starke K, Reissig D, Petereit-Haack G, Schmauder S, Nienhaus A, Seidler A. The isolated effect of age on the risk of COVID-19 severe outcomes: a systematic review with meta-analysis. BMJ Global Health. 2021;6(12):e006434. doi: 10.1136/bmjgh-2021-006434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Turner SA, Butler G. The Candida pathogenic species complex. Cold Spring Harbor perspectives in medicine. 2014;4(9):a019778–a. doi: 10.1101/cshperspect.a019778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Riche CVW, Cassol R, Pasqualotto AC. Is the Frequency of Candidemia Increasing in COVID-19 Patients Receiving Corticosteroids? J Fungi (Basel). 2020;6(4). doi: 10.3390/jof6040286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nucci M, Barreiros G, Guimarães LF, Deriquehem VaS, Castiñeiras AC, Nouér SA. Increased incidence of candidemia in a tertiary care hospital with the COVID-19 pandemic. Mycoses. 2021;64(2):152–6. doi: 10.1111/myc.13225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Segrelles-Calvo G, De SaGR, Llopis-Pastor E, Carrillo J, Hernández-Hernández M, Rey L, et al. Candida spp. co-infection in COVID-19 patients with severe pneumonia: Prevalence study and associated risk factors. Respir Med. 2021;188:106619. doi: 10.1016/j.rmed.2021.106619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chowdhary A, Tarai B, Singh A, Sharma A. Multidrug-Resistant Candida auris Infections in Critically Ill Coronavirus Disease Patients, India, April-July 2020. Emerg Infect Dis. 2020;26(11):2694–6. doi: 10.3201/eid2611.203504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bishburg E, Okoh A, Nagarakanti SR, Lindner M, Migliore C, Patel P. Fungemia in COVID-19 ICU patients, a single medical center experience. J Med Virol. 2021;93(5):2810–4. doi: 10.1002/jmv.26633 [DOI] [PubMed] [Google Scholar]
- 57.Villanueva-Lozano H, Treviño-Rangel RJ, González GM, Ramírez-Elizondo MT, Lara-Medrano R, Aleman-Bocanegra MC, et al. Outbreak of Candida auris infection in a COVID-19 hospital in Mexico. Clin Microbiol Infect. 2021;27(5):813–6. 10.1016/j.cmi.2020.12.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Magnasco L, Mikulska M, Giacobbe DR, Taramasso L, Vena A, Dentone C, et al. Spread of Carbapenem-Resistant Gram-Negatives and Candida auris during the COVID-19 Pandemic in Critically Ill Patients: One Step Back in Antimicrobial Stewardship? Microorganisms. 2021;9(1). 10.3390/microorganisms9010095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cataldo MA, Tetaj N, Selleri M, Marchioni L, Capone A, Caraffa E, et al. Incidence of bacterial and fungal bloodstream infections in COVID-19 patients in intensive care: An alarming "collateral effect". J Glob Antimicrob Resist. 2020;23:290–1. doi: 10.1016/j.jgar.2020.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Calderaro A, Buttrini M, Montecchini S, Piccolo G, Martinelli M, Dell, et al. Detection of SARS-CoV-2 and Other Infectious Agents in Lower Respiratory Tract Samples Belonging to Patients Admitted to Intensive Care Units of a Tertiary-Care Hospital, Located in an Epidemic Area, during the Italian Lockdown. Microorganisms. 2021;9(1):185. doi: 10.3390/microorganisms9010185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lv Z, Cheng S, Le J, Huang J, Feng L, Zhang B, et al. Clinical characteristics and co-infections of 354 hospitalized patients with COVID-19 in Wuhan, China: a retrospective cohort study. Microbes Infect. 2020;22(4–5):195–9. doi: 10.1016/j.micinf.2020.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rodriguez JY, Le Pape P, Lopez O, Esquea K, Labiosa AL, Alvarez-Moreno C. Candida auris: A Latent Threat to Critically Ill Patients With Coronavirus Disease 2019. Clinical Infectious Diseases. 2020;73(9):e2836–e7. 10.1093/cid/ciaa1595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Colombo AL, Perfect J, Dinubile M, Bartizal K, Motyl M, Hicks P, et al. Global Distribution and Outcomes for Candida Species Causing Invasive Candidiasis: Results from an International Randomized Double-Blind Study of Caspofungin Versus Amphotericin B for the Treatment of Invasive Candidiasis. European Journal of Clinical Microbiology and Infectious Diseases. 2003;22(8):470–4. doi: 10.1007/s10096-003-0973-8 [DOI] [PubMed] [Google Scholar]
- 64.Lone SA, Ahmad A. Candida auris-the growing menace to global health. Mycoses. 2019;62(8):620–37. doi: 10.1111/myc.12904 [DOI] [PubMed] [Google Scholar]
- 65.Abastabar M, Haghani I, Ahangarkani F, Rezai MS, Taghizadeh Armaki M, Roodgari S, et al. Candida auris otomycosis in Iran and review of recent literature. Mycoses. 2019;62(2):101–5. doi: 10.1111/myc.12886 [DOI] [PubMed] [Google Scholar]
- 66.Taghizadeh Armaki M, Mahdavi Omran S, Kiakojuri K, Khojasteh S, Jafarzadeh J, Tavakoli M, et al. First fluconazole-resistant Candida auris isolated from fungal otitis in Iran. Curr Med Mycol. 2021;7(1):51–4. doi: 10.18502/cmm.7.1.6243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mirhendi H, Charsizadeh A, Aboutalebian S, Mohammadpour M, Nikmanesh B, De Groot T, et al. South Asian (Clade I) Candida auris meningitis in a paediatric patient in Iran with a review of the literature. Mycoses. 2022;65(2):134–9. doi: 10.1111/myc.13396 [DOI] [PubMed] [Google Scholar]
- 68.Mahmoudi S, Agha Kuchak Afshari S, Aghaei Gharehbolagh S, Mirhendi H, Makimura K. Methods for identification of Candida auris, the yeast of global public health concern: A review. Journal de Mycologie Médicale. 2019;29(2):174–9. doi: 10.1016/j.mycmed.2019.04.004 [DOI] [PubMed] [Google Scholar]
- 69.Karimi L, Mirhendi H, Khodadadi H, Mohammadi R. Molecular identification of uncommon clinical yeast species in Iran. Current medical mycology. 2015;1(2):1–6. doi: 10.18869/acadpub.cmm.1.2.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Riad A, Gomaa E, Hockova B, Klugar M. Oral candidiasis of COVID-19 patients: Case report and review of evidence. J Cosmet Dermatol. 2021;20(6):1580–4. doi: 10.1111/jocd.14066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Masur H, Rosen PP, Armstrong D. Pulmonary disease caused by Candida species. Am J Med. 1977;63(6):914–25. doi: 10.1016/0002-9343(77)90546-0 [DOI] [PubMed] [Google Scholar]
- 72.Schnabel RM, Linssen CF, Guion N, Van Mook WN, Bergmans DC. Candida pneumonia in intensive care unit? Open Forum Infect Dis. 2014;1(1):ofu026. doi: 10.1093/ofid/ofu026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pemán J, Ruiz-Gaitán A, García-Vidal C, Salavert M, Ramírez P, Puchades F, et al. Fungal co-infection in COVID-19 patients: Should we be concerned? Rev Iberoam Micol. 2020;37(2):41–6. doi: 10.1016/j.riam.2020.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Meena DS, Kumar D. Candida Pneumonia: An Innocent Bystander or a Silent Killer? Med Princ Pract. 2021. doi: 10.1159/000520111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Casalini G, Giacomelli A, Ridolfo A, Gervasoni C, Antinori S. Invasive Fungal Infections Complicating COVID-19: A Narrative Review. J Fungi (Basel). 2021;7(11). doi: 10.3390/jof7110921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Baddley JW, Thompson GR, Chen SC 3rd, White PL, Johnson MD, Nguyen MH, et al. Coronavirus Disease 2019-Associated Invasive Fungal Infection. Open Forum Infect Dis. 2021;8(12):ofab510. doi: 10.1093/ofid/ofab510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Antinori S, Bonazzetti C, Gubertini G, Capetti A, Pagani C, Morena V, et al. Tocilizumab for cytokine storm syndrome in COVID-19 pneumonia: an increased risk for candidemia? Autoimmun Rev. 2020;19(7):102564. doi: 10.1016/j.autrev.2020.102564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yuan SM. Fungal Endocarditis. Braz J Cardiovasc Surg. 2016;31(3):252–5. doi: 10.5935/1678-9741.20160026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Badiee P, Amirghofran AA, Ghazi Nour M, Shafa M, Nemati MH. Incidence and outcome of documented fungal endocarditis. Int Cardiovasc Res J. 2014;8(4):152–5. [PMC free article] [PubMed] [Google Scholar]
- 80.Prakash H, Chakrabarti A. Global Epidemiology of Mucormycosis. J Fungi (Basel). 2019;5(1):26. doi: 10.3390/jof5010026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dolatabadi S, Ahmadi B, Rezaei-Matehkolaei A, Zarrinfar H, Skiada A, Mirhendi H, et al. Mucormycosis in Iran: A six-year retrospective experience. J Mycol Med. 2018;28(2):269–73. doi: 10.1016/j.mycmed.2018.02.014 [DOI] [PubMed] [Google Scholar]
- 82.Hussain S, Riad A, Singh A, Klugarová J, Antony B, Banna H, et al. Global Prevalence of COVID-19-Associated Mucormycosis (CAM): Living Systematic Review and Meta-Analysis. J Fungi (Basel). 2021;7(11). doi: 10.3390/jof7110985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Muthu V, Rudramurthy SM, Chakrabarti A, Agarwal R. Epidemiology and Pathophysiology of COVID-19-Associated Mucormycosis: India Versus the Rest of the World. Mycopathologia. 2021;186(6):739–54. doi: 10.1007/s11046-021-00584-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bhattacharyya A, Sarma P, Kaur H, Kumar S, Bhattacharyya J, Prajapat M, et al. COVID-19-associated rhino-orbital-cerebral mucormycosis: A systematic review, meta-analysis, and meta-regression analysis. Indian J Pharmacol. 2021;53(6):499–510. doi: 10.4103/ijp.ijp_839_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pal R, Singh B, Bhadada SK, Banerjee M, Bhogal RS, Hage N, et al. COVID-19-associated mucormycosis: An updated systematic review of literature. Mycoses. 2021;64(12):1452–9. doi: 10.1111/myc.13338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Singh AK, Singh R, Joshi SR, Misra A. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes Metab Syndr. 2021;15(4):102146. doi: 10.1016/j.dsx.2021.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sen M, Honavar SG, Bansal R, Sengupta S, Rao R, Kim U, et al. Epidemiology, clinical profile, management, and outcome of COVID-19-associated rhino-orbital-cerebral mucormycosis in 2826 patients in India—Collaborative OPAI-IJO Study on Mucormycosis in COVID-19 (COSMIC), Report 1. Indian J Ophthalmol. 2021;69(7):1670–92. doi: 10.4103/ijo.IJO_1565_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Arora R, Goel R, Khanam S, Kumar S, Shah S, Singh S, et al. Rhino-Orbito-Cerebral-Mucormycosis During the COVID-19 Second Wave in 2021—A Preliminary Report from a Single Hospital. Clin Ophthalmol. 2021;15:3505–14. doi: 10.2147/OPTH.S324977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hoenigl M, Seidel D, Carvalho A, Rudramurthy SM, Arastehfar A, Gangneux J-P, et al. The emergence of COVID-19 associated mucormycosis: a review of cases from 18 countries. The Lancet Microbe. 2022. doi: 10.1016/S2666-5247(21)00237-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA, Dannaoui E, Hochhegger B, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019;19(12):e405–e21. doi: 10.1016/S1473-3099(19)30312-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dannaoui E. Recent Developments in the Diagnosis of Mucormycosis. J Fungi (Basel). 2022;8(5). 10.3390/jof8050457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ahmadikia K, Hashemi SJ, Khodavaisy S, Getso MI, Alijani N, Badali H, et al. The double-edged sword of systemic corticosteroid therapy in viral pneumonia: A case report and comparative review of influenza-associated mucormycosis versus COVID-19 associated mucormycosis. Mycoses. 2021;64(8):798–808. doi: 10.1111/myc.13256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Garg D, Muthu V, Sehgal IS, Ramachandran R, Kaur H, Bhalla A, et al. Coronavirus Disease (Covid-19) Associated Mucormycosis (CAM): Case Report and Systematic Review of Literature. Mycopathologia. 2021;186(2):289–98. doi: 10.1007/s11046-021-00528-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Placik DA, Taylor WL, Wnuk NM. Bronchopleural fistula development in the setting of novel therapies for acute respiratory distress syndrome in SARS-CoV-2 pneumonia. Radiology Case Reports. 2020;15(11):2378–81. doi: 10.1016/j.radcr.2020.09.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Johnson AK, Ghazarian Z, Cendrowski KD, Persichino JG. Pulmonary aspergillosis and mucormycosis in a patient with COVID-19. Medical Mycology Case Reports. 2021;32:64–7. doi: 10.1016/j.mmcr.2021.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kanwar A, Jordan A, Olewiler S, Wehberg K, Cortes M, Jackson BR. A Fatal Case of Rhizopus azygosporus Pneumonia Following COVID-19. Journal of Fungi. 2021;7(3):174. doi: 10.3390/jof7030174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zurl C, Hoenigl M, Schulz E, Hatzl S, Gorkiewicz G, Krause R, et al. Autopsy Proven Pulmonary Mucormycosis Due to Rhizopus microsporus in a Critically Ill COVID-19 Patient with Underlying Hematological Malignancy. Journal of Fungi. 2021;7(2):88. doi: 10.3390/jof7020088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mishra N, Mutya VSS, Thomas A, Rai G, Reddy B, Mohanan AA, et al. A case series of invasive mucormycosis in patients with COVID-19 infection. Int J Otorhinolaryngol Head Neck Surg. 2021;7(5):867–70. [Google Scholar]
- 99.Moorthy A, Gaikwad R, Krishna S, Hegde R, Tripathi KK, Kale PG, et al. SARS-CoV-2, Uncontrolled Diabetes and Corticosteroids—An Unholy Trinity in Invasive Fungal Infections of the Maxillofacial Region? A Retrospective, Multi-centric Analysis. Journal of Maxillofacial and Oral Surgery. 2021;20(3):418–25. doi: 10.1007/s12663-021-01532-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Monte Junior ESD, Santos MELD, Ribeiro IB, Luz GDO, Baba ER, Hirsch BS, et al. Rare and Fatal Gastrointestinal Mucormycosis (Zygomycosis) in a COVID-19 Patient: A Case Report. Clin Endosc. 2020;53(6):746–9. doi: 10.5946/ce.2020.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Khatri A, Chang K-M, Berlinrut I, Wallach F. Mucormycosis after Coronavirus disease 2019 infection in a heart transplant recipient – Case report and review of literature. Journal of Medical Mycology. 2021;31(2):101125. doi: 10.1016/j.mycmed.2021.101125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Afzal S, Nasir M. Aspergillosis and Mucormycosis in COVID-19 Patients; a Systematic Review and Meta-analysis. medRxiv. 2021. [DOI] [PubMed] [Google Scholar]
- 103.Yasmin F, Najeeb H, Naeem A, Dapke K, Phadke R, Asghar MS, et al. COVID-19 Associated Mucormycosis: A Systematic Review from Diagnostic Challenges to Management. Diseases. 2021;9(4). 10.3390/diseases9040065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Azhar A, Khan WH, Khan PA, Alhosaini K, Owais M, Ahmad A. Mucormycosis and COVID-19 pandemic: Clinical and diagnostic approach. J Infect Public Health. 2022;15(4):466–79. doi: 10.1016/j.jiph.2022.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ghosh A, Sarkar A, Paul P, Patel P. The rise in cases of mucormycosis, candidiasis and aspergillosis amidst COVID19. Fungal Biol Rev. 2021;38:67–91. doi: 10.1016/j.fbr.2021.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sipsas NV, Gamaletsou MN, Anastasopoulou A, Kontoyiannis DP. Therapy of Mucormycosis. Journal of Fungi. 2018;4(3):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rabagliati R, Rodríguez N, Núñez C, Huete A, Bravo S, Garcia P. COVID-19–Associated Mold Infection in Critically Ill Patients, Chile. Emerging infectious diseases. 2021;27(5):1454. doi: 10.3201/eid2705.204412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Apostolopoulou A, Esquer Garrigos Z, Vijayvargiya P, Lerner AH, Farmakiotis D. Invasive pulmonary aspergillosis in patients with SARS-CoV-2 infection: a systematic review of the literature. Diagnostics. 2020;10(10):807. doi: 10.3390/diagnostics10100807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mitaka H, Kuno T, Takagi H, Patrawalla P. Incidence and mortality of COVID‐19‐associated pulmonary aspergillosis: A systematic review and meta‐analysis. Mycoses. 2021;64(9):993–1001. doi: 10.1111/myc.13292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sebastian SK, Kumar VB, Gupta M, Sharma Y. Covid Assossiated Invasive Fungal Sinusitis. Indian J Otolaryngol Head Neck Surg. 2021:1–4. doi: 10.1007/s12070-021-02471-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Shetty S, Shilpa C, Kavya S, Sundararaman A, Hegde K, Madhan S. Invasive Aspergillosis of Nose and Paranasal Sinus in COVID-19 Convalescents: Mold Goes Viral? Indian J Otolaryngol Head Neck Surg. 2022:1–6. 10.1007/s12070-022-03073-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Dokania V, Gaikwad NS, Gite V, Mhashal S, Shetty N, Shinde P, et al. Emergence of Invasive Fungal Rhinosinusitis in Recently Recovered COVID-19 Patients. Ann Otol Rhinol Laryngol. 2021:34894211060923. doi: 10.1177/00034894211060923 [DOI] [PubMed] [Google Scholar]
- 113.El-Kholy NA, El-Fattah AMA, Khafagy YW. Invasive Fungal Sinusitis in Post COVID-19 Patients: A New Clinical Entity. Laryngoscope. 2021;131(12):2652–8. doi: 10.1002/lary.29632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chong WH, Neu KP. Incidence, diagnosis and outcomes of COVID-19-associated pulmonary aspergillosis (CAPA): a systematic review. Journal of Hospital Infection. 2021;113:115–29. doi: 10.1016/j.jhin.2021.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Salmanton-García J, Sprute R, Stemler J, Bartoletti M, Dupont D, Valerio M, et al. COVID-19-Associated Pulmonary Aspergillosis, March-August 2020. Emerg Infect Dis. 2021;27(4):1077–86. doi: 10.3201/eid2704.204895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Arastehfar A, Carvalho A, Van De Veerdonk FL, Jenks JD, Koehler P, Krause R, et al. COVID-19 associated pulmonary aspergillosis (CAPA)—from immunology to treatment. Journal of Fungi. 2020;6(2):91. doi: 10.3390/jof6020091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Prattes J, Wauters J, Giacobbe DR, Salmanton-García J, Maertens J, Bourgeois M, et al. Risk factors and outcome of pulmonary aspergillosis in critically ill coronavirus disease 2019 patients-a multinational observational study by the European Confederation of Medical Mycology. Clin Microbiol Infect. 2022;28(4):580–7. doi: 10.1016/j.cmi.2021.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chadeganipour M, Mohammadi R. A 9-Year Experience of Aspergillus Infections from Isfahan, Iran. Infection and Drug Resistance. 2020;13:2301. doi: 10.2147/IDR.S259162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Tavakoli M, Yazdani Charati J, Hedayati MT, Moosazadeh M, Badiee P, Seyedmousavi S, et al. National trends in incidence, prevalence and disability-adjusted life years of invasive aspergillosis in Iran: a systematic review and meta-analysis. Expert review of respiratory medicine. 2019;13(11):1121–34. doi: 10.1080/17476348.2019.1657835 [DOI] [PubMed] [Google Scholar]
- 120.Moazam S, Denning DW. Aspergillus nodules in chronic granulomatous disease attributable to Aspergillus ochraceus. Medical mycology case reports. 2017;17:31–3. doi: 10.1016/j.mmcr.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Novey HS, Wells ID. Allergic bronchopulmonary aspergillosis caused by Aspergillus ochraceus. Am J Clin Pathol. 1978;70(5):840–3. doi: 10.1093/ajcp/70.5.840 [DOI] [PubMed] [Google Scholar]
- 122.Chong WH, Saha BK, Neu KP. Comparing the clinical characteristics and outcomes of COVID-19-associate pulmonary aspergillosis (CAPA): a systematic review and meta-analysis. Infection. 2022;50(1):43–56. doi: 10.1007/s15010-021-01701-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Barberis F, Benedetti MF, De Abreu MS, Pola SJ, Posse G, Capece P, et al. Invasive fusariosis in a critically ill patient with severe COVID-19 pneumonia: A case report. Medical Mycology Case Reports. 2022;35:5–8. doi: 10.1016/j.mmcr.2021.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Poignon C, Blaize M, Vezinet C, Lampros A, Monsel A, Fekkar A. Invasive pulmonary fusariosis in an immunocompetent critically ill patient with severe COVID-19. Clinical Microbiology and Infection. 2020;26(11):1582–4. doi: 10.1016/j.cmi.2020.06.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gangneux J-P, Dannaoui E, Fekkar A, Luyt C-E, Botterel F, De Prost N, et al. Fungal infections in mechanically ventilated patients with COVID-19 during the first wave: The French multicentre MYCOVID study. The Lancet Respiratory Medicine. 2021. doi: 10.1016/S2213-2600(21)00442-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Meira F, Moreno-García E, Linares L, Macaya I, Tomé A, Hernández-Meneses M, et al. Impact of inflammatory response modifiers on the incidence of hospital-acquired infections in patients with COVID-19. Infectious Diseases and Therapy. 2021;10(3):1407–18. doi: 10.1007/s40121-021-00477-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Nucci F, Nouér SA, Capone D, Anaissie E, Nucci M. Fusariosis. Semin Respir Crit Care Med. 2015;36(5):706–14. doi: 10.1055/s-0035-1562897 [DOI] [PubMed] [Google Scholar]
- 128.Muhammed M, Coleman JJ, Carneiro HA, Mylonakis E. The challenge of managing fusariosis. Virulence. 2011;2(2):91–6. doi: 10.4161/viru.2.2.15015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kim J-Y, Kang C-I, Lee JH, Lee WJ, Huh K, Cho SY, et al. Clinical Features and Outcomes of Invasive Fusariosis: A Case Series in a Single Center with Literature Review. Infect Chemother. 2021;53(2):e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Horn DL, Freifeld AG, Schuster MG, Azie NE, Franks B, Kauffman CA. Treatment and outcomes of invasive fusariosis: review of 65 cases from the PATH Alliance(®) registry. Mycoses. 2014;57(11):652–8. doi: 10.1111/myc.12212 [DOI] [PubMed] [Google Scholar]
- 131.Avcu G, Karapinar DY. A review of a diagnostic tool: galactomannan. Journal of Immunological Sciences. 2018;2(4). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(XLSX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.