Abstract
Objective:
Despite the efficacy of pre-exposure prophylaxis (PrEP) in reducing risk of HIV infection, uptake remains low among many who are most vulnerable to HIV, such as Black and Latinx women. Interventions that target social networks to encourage at-risk women to initiate PrEP are underutilized.
Design:
This study employed an egocentric network design and sampled Black/African-American (BAA) and Latinx women at risk of HIV as well as people from their social networks (N=211) in a small, western city.
Methods:
Multivariable Generalized Linear Mixed Effects Models (GLMM) regression models investigated individual-level and network-level characteristics associated with likely future PrEP use.
Results:
PrEP awareness was low, but once informed, 36% considered themselves likely to take it in the future. Perceived risk of HIV, perceived barriers to HIV testing, and participation in a 12-step program increased odds of anticipated PrEP use. A higher proportion of friends in one’s network decreased odds of future PrEP use, while a higher proportion of network members who tested regularly for HIV increased odds of future PrEP use. A marginally significant interaction was detected between proportion of friends in one’s network and proportion of the network perceived to test for HIV regularly (i.e. testing norms). When HIV testing norms were low, a higher proportion of friends in the network decreased odds of likely PrEP use. However, this effect was reversed in contexts with strong testing norms.
Conclusion:
Women who are interested in PrEP may be embedded within social and normative contexts that can foster or inhibit PrEP uptake.
Keywords: pre-exposure prophylaxis, social networks, social norms, Black women, Latinx women
Introduction
Despite recent declines, racial/ethnic minority women in the United States (US) are disproportionately affected by HIV. The incidence rate among Black/African American (BAA) women is 15 times the rate of white women (24.2 vs. 1.6 per 100,000 in 2017)1 and the rate for Latinx women is three times the rate of their White counterparts (4.9 vs. 1.6 per 100,000). While these rates are dwarfed when compared to rates of infection among men who have sex with men (MSM),2 HIV among women of color is worthy of attention given the demographic landscape of the US—the disease burden remains large despite declining rates. To that end, the Ending the HIV Epidemic (EHE) campaign is a 2019 federal initiative to reduce HIV transmission 90 percent by 2030 with data-driven interventions.3,4 Pre-exposure prophylaxis (PrEP) is a biomedical prevention strategy that lowers risk of HIV infection,5 recommended for use among people who are considered high risk, and has the potential to reduce racial disparities in HIV incidence. PrEP uptake is rising among men who have sex with men (MSM).6–8 Fewer studies focus on women at risk for HIV, such as women who inject drugs9,10 and women of color. When they do, they find that awareness and uptake of PrEP is low.11,12 Given progress in raising PrEP awareness, uptake, and adherence among MSM it is time for research to investigate other at-risk groups in order to offer meaningful and tailored PrEP interventions.
Despite low awareness, women are interested in PrEP once they learn about it,13,14 especially those who perceive themselves at-risk.15 Beyond awareness, however, decisions about PrEP are influenced by numerous factors: advantages and disadvantages,16 cost,17 and providers’ willingness to prescribe.18,19 Racial disparities in PrEP access highlight intersectional challenges associated with poverty, racism, and stigma.20 Black women are more likely to express medical mistrust,21,22 which is a barrier to PrEP. However, they were also more likely to take PrEP if their friends did, highlighting the importance of peers over relationships with healthcare providers.17 Because social, structural, and cultural factors influence interest in and willingness to use PrEP for HIV prevention,22,23 research on PrEP intentions should account for the social context. In this study, we use a social network approach to explore the association between characteristics of the social context and intentions to initiate PrEP.
Social networks structure information flows and establish norms that can impact sexual health interventions.24,25 For example, network size was associated with PrEP use in a study among MSM26 and women who engaged in conversations with peers or providers were more PrEP-aware,27 suggesting that informal and formal connections could be leveraged to encourage PrEP. Peer and familial relationships may also provide a unique context for increasing the perceived acceptability of PrEP.28 A qualitative study among Black mothers and their daughters found they expressed favorable attitudes and a willingness to engage in conversations about PrEP.29 Networks may also inhibit PrEP uptake. Racial/ethnic minorities are embedded within social worlds where vicarious experiences of discrimination can generate mistrust of medical providers30 and diffuse across social networks.31 A qualitative study found that women who have previously taken antiretroviral medications express concerns that could dissuade others from taking PrEP.32 Further, network-level stigma may influence perceptions of acceptability and willingness to use PrEP.33 Norms framing PrEP as a license to engage in behavior deemed ‘socially unacceptable’(e.g., promiscuity) can inhibit uptake.34 The impact of networks, however, is contingent upon other factors. For example, having a more PrEP-aware network was associated with women’s intentions to take PrEP but this association was modified by a history of intimate partner violence.12 Collectively, these results highlight mechanisms through which social networks may influence PrEP intentions.
The motivations for this study are threefold. First, PrEP care continuum research often focuses on MSM.26,35,36 While this is driven by elevated infection rates, it leaves other at-risk groups understudied. Second, research often focuses on individual-level characteristics (e.g., perceived risk). Despite the acknowledgement that relationships matter,27,37 studies do not often explicitly model the social network (see Willie et. al12 for an exception). Interventions with a relational dimension often focus on healthcare settings27,38 ignoring other relationships. Third, most HIV and PrEP-related research was conducted in dense, urban coastal communities with larger BAA and/or Latinx populations. Little is known about interest in PrEP in communities that are more rural and less diverse. This study addresses these gaps by examining social network factors associated with intention to use PrEP in a sample of racially/ethnically diverse women (including transwomen) and members of their networks in the western US.
Methods
Setting & Sample
Data were drawn from a study examining social and cultural influences on HIV risk and uptake of HIV testing among BAA and Latinx women and members of their social networks in a small western city where less than 3% of the population is BAA and 25% is Latinx. Participants were recruited 2016–2018 through convenience sampling and incentivized 1-step referral. These methods are effective when populations are difficult to locate or part of a stigmatized group.39 Index participants had to be women (cisgender or transgender), aged ≥ 18 years, self-identified as BAA or Latinx, willing to refer others, had an unknown or negative HIV status, and at risk for HIV as determined by screening questions. The screener asked about past six-month HIV risk behaviors, defined as: multiple sex partners, injecting drugs, transactional sex, and sex with a high-risk partner (partner injects drugs, partner engages in transactional sex, partner has concurrent partners, partner is an MSM). Eligible participants completed a two-hour, interviewer-administered survey measuring attitudes, self-reported behaviors, and the social network. Index participants were provided coupons to refer network members to participate. Referred participants had to be linked to an index participant but they could be any race/ethnicity, sex, or gender. Referred participants did not recruit further. Participants were compensated $45 and indexes could receive $5 for recruited referrals (up to five). Participants provided written informed consent and protocols were approved by the [University] Institutional Review Board.
Measures
The dependent variable is self-reported likelihood of future PrEP use, asked as: “How likely is it that you will take PrEP in the future?” (1=Not at all likely to 5=Very likely). Prior to the question, participants were provided a brief explanation that PrEP “is a medication prescribed by a doctor to prevent HIV transmission.”
Independent variables included individual-level and network-level measures. First, socio-demographics included sex/gender (Female, Male / Transfemale, Transmale, Gender queer/nonbinary, Other), age, race/ethnicity (select all that apply: Black/African American, Hispanic/Latinx, Asian, American Indian/Alaskan Native, Native Hawaiian/Pacific Islander, White), homelessness (past six months), and education (years). Other measures included having ever been arrested, having ever experienced childhood physical/sexual abuse, and having ever been forced to have sex, all collected as binary measures (i.e., yes/no). Drug use and sexual behavior were assessed as binary indicators of past six month alcohol use, non-injection drug use, injection drug use, receptive syringe and paraphernalia sharing, unprotected sex with casual and regular partners, transactional sex, and high-risk partners [defined as HIV positive, MSM, injects drugs, or incarcerated in past 6 months]. Two questions measured previous participation in a drug detox/treatment program or a 12-step program such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) (binary measures; yes/no). Discrimination was captured with a 10-item scale where participants reported past year experiences with things such as being ignored/excluded, treated with hostility, or denied a job due to one’s race [Multiple Discrimination Scale – Race (MDSR); range: 0 to 10; current study Cronbach’s alpha=.79 ].40
Current/past PrEP use was measured with a single item, “Are you now or have you ever taken PrEP?” with the responses: ‘Yes, currently,’ ‘Yes, in the past,’ ‘No, never,’ and ‘Never heard of PrEP.’ Perceived risk of HIV was measured with a single ordinal item (range: 0=Not at all at risk to 4=Extremely at risk) and perceived HIV testing barriers were measured with a 10-item scale (possible average score range 1–5; current study Cronbach’s alpha=.80).41 Past HIV testing was measured with one question (range: 1=Never tested to 5=More than 2 times/year). Anticipated HIV testing in the next six months was measured with a single question (range: 1=Not at all likely to 5=Very likely).
Social context was measured with network-level indicators collected through an egocentric elicitation42 where respondents (i.e., egos) were asked to list “20 people with whom you have communicated in the past 6 months. This might be communication by phone, email, social media, text, or in person.” Then, participants were asked questions about each alter.43 For example, ego was asked to report alter’s gender, perceptions about alter’s attitudes and behaviors (e.g., Does [the alter] get tested regularly for HIV?). Structural aspects of the network were captured with measures of network size (number of alters, maximum 20) and density. Density is defined as the number of reported ties among alters relative to total possible ties and expressed as a proportion between zero and one with higher values indicating more densely connected networks.44 Data were collected through an open-source software package designed for network data collection (EgoWeb 2.0, computer software).
Analytic Strategy
For the purposes of this study, we grouped cisgender and transgender women together. There were only three transgender women in our sample, so it was not feasible to analyze them separately. While we recognize that gender identity can impact risk and health outcomes, identity is not central to our research question. Therefore, we included all eligible respondents while controlling for characteristics that might differ between cisgender and transgender women (e.g., perceived risk). Prior to analysis, several measures were recoded. The variables of ‘likely future PrEP use’ and ‘future HIV testing’ were dichotomized based on the distribution of responses as ‘Likely’ (including ‘Somewhat’ and ‘Very’ likely) and ‘Not likely’ (all others). Past HIV testing was dichotomized into ever/never tested. Using standard social network techniques,43 individual alter-level attributes (e.g., gender) were aggregated to describe ego’s network as a proportion with a given characteristic (e.g., network is 20% women). Network-level variables were considered as linear and curvilinear, continuous and dichotomous but without a strong statistical or substantive justification guiding these decisions,45 we left them as continuous and linear in the analysis.
Analysis occurred in three stages. First, the sample descriptives and bivariate analyses compared ‘Likely’ and ‘Not likely’ PrEP users using chi-square, Fisher’s exact test, and t-tests. Second, marginally significant variables (p<.10) in the bivariate analyses were considered in a Generalized Linear Mixed Effects Model (GLMM),46,47 which accounts for the clustering of respondents in referral networks. The ‘full model’ includes all variables and the ‘reduced model’ used manual backward selection with a p-value cutoff of 0.05. Adjusted odds ratios for the network proportion variables are applied to a 0.1 unit (10%) increase in the proportion of the network with a given trait. Finally, considering the EHE’s data-driven approach, it is useful to understand specific contexts associated with willingness to take PrEP. Previous research on PrEP interest among women found a significant interaction between having experienced intimate partner violence and having a PrEP aware social network.12 Therefore, the current study conducted an exploratory post hoc analysis for possible interactions.
Results
The analytic sample consisted 211 participants; 113 were index participants (100% women; 73% BAA, 34% Latinx, 21% White, and 19% other, which sums to greater than 100% since respondents could select multiple racial/ethnic categories, and Latinx ethnicity was assessed independent of race as per NIH guidelines) and 98 were referred from index participants’ social networks (47% women and 53% men; 45% BAA, 14% Latinx, 45% White, and 23% other). Index and referred participants are collapsed in all subsequent results.
Table 1 describes demographics, PrEP and HIV testing behavior, HIV risk behaviors, and social networks. Most respondents were women (75%), BAA (60%), and did not identify as Latinx (76%). Half (51%) were recently homeless and 74% had ever been arrested. No one was currently taking PrEP, though one person had previously. Most (61%) had never heard of PrEP. Around one-in-three (36%) participants were ‘likely future PrEP users.’ Alcohol and non-injection drug use were prevalent (84% and 69%, respectively), while injection drug use was less common (18%). Participation in a drug detoxification program (37%) or 12-step recovery program (47%) was common. Nearly half (48%) had a past-six-month casual sex partner and 79% had a regular partner. Three-fourths (73%) had unprotected sex and many (38%) had sex with a high-risk partner. The average size of an ego’s network was 14 people. Overall, respondents’ networks were 50% women, 34% family members, and 70% friends (not mutually exclusive). Perceived PrEP use among alters was extremely rare (only one participant reported any PrEP use in their network), while perceived HIV testing was higher (15% of alters).
Table 1.
Descriptive Statistics of the Sample, Overall and by Anticipated Future PrEP Use (N=211)
| Future PrEP | ||||
|---|---|---|---|---|
| Overall Sample | Not Likely (n=135; 64%) |
Likely (n=76; 36%) |
||
|
|
||||
| N (%) or Mean (SD) |
N (%) or Mean (SD) |
N (%) or Mean (SD) |
p-value◊ | |
|
|
||||
| Outcome: Anticipated PrEP Use | ||||
| Not at all likely | 105 (49.8%) | 135 (100.0%) | - | |
| Somewhat unlikely | 12 (5.7%) | |||
| Not likely or unlikely | 18 (8.5%) | |||
| Somewhat likely | 46 (21.8%) | 76 (100.0%) | ||
| Very Likely | 30 (14.2%) | |||
| Demographics | ||||
| Women (including four transwomen) | 159 (75.4%) | 99 (73.3%) | 60 (79.0%) | .36 |
| Age (mean (SD)) | 37.2 (13.2) | 37.0 (13.6) | 37.5 (12.4) | .77 |
| Black/African American (BAA) | 126 (59.7%) | 79 (58.5%) | 47 (61.8%) | .64 |
| Hispanic/Latinx | 51 (24.2%) | 35 (25.9%) | 16 (21.1%) | .43 |
| Homeless (past 6m) | 107 (50.7%) | 61 (45.2%) | 46 (60.5%) | <.05* |
| Arrested (ever) | 157 (74.4%) | 93 (68.9%) | 64 (84.2%) | <.05* |
| Discrimination (MDSR; mean (SD); range 0–10) □ | 2.6 (2.4) | 2.4 (2.2) | 3.0 (2.6) | <.05* |
| Childhood physical abuse (missing=9) | 94 (46.5%) | 60 (46.9%) | 34 (46.0%) | .90 |
| Childhood sexual abuse (missing=10) | 98 (48.8%) | 63 (48.5%) | 35 (49.3%) | .91 |
| Ever been forced to have sex (missing=7) | 92 (45.1%) | 51 (38.6%) | 41 (56.9%) | <.05* |
| PrEP & HIV Testing | ||||
| Are you now or have you ever taken PrEP? | ||||
| Yes, I am currently taking it | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | .47 |
| Yes, I have taken it in the past | 1 (0.5%) | 0 (0.0%) | 1 (0.5%) | |
| No, never taken it | 81 (38.4%) | 53 (39.3%) | 28 (36.8%) | |
| I’ve never heard of it | 129 (61.1%) | 82 (60.7%) | 47 (61.8%) | |
| Perceived risk of HIV (mean (SD); missing=1; range 0–4) | 1.0 (1.0) | 0.8 (0.9) | 1.4 (1.2) | <.0001*** |
| Barriers to HIV testing (mean (SD); range 1–4.9) □ | 2.8 (0.7) | 2.6 (0.7) | 3.0 (0.8) | <.001** |
| Ever previously tested for HIV (missing=1) | 172 (81.9%) | 108 (80.0%) | 64 (85.3%) | .34 |
| Likely to test for HIV in the future (missing=2) | 119 (56.9%) | 65 (48.5%) | 54 (72.0%) | <.001** |
| Risk Behaviors | ||||
| Consumed alcohol (past 6m; missing=5) | 172 (83.5%) | 106 (79.7%) | 66 (90.4%) | <.05* |
| Non-injection drug use (past 6m) | 146 (69.2%) | 92 (68.2%) | 54 (71.1%) | .66 |
| Injection drug use (past 6m) | 39 (18.5%) | 22 (16.3%) | 17 (22.4%) | .28 |
| Receptive syringe/paraph. sharing (past 6m; missing=5) | 22 (10.7%) | 12 (9.1%) | 10 (13.5%) | .32 |
| Drug detoxification or treatment (ever; missing=1) | 78 (37.1%) | 45 (33.6%) | 33 (43.4%) | .16 |
| 12-step participation such as AA or NA (ever) | 99 (46.9%) | 54 (40.0%) | 45 (59.2%) | <.05* |
| Casual sex partner (past 6m; missing=11) | 95 (47.5%) | 52 (40.9%) | 43 (58.9%) | <.05* |
| Regular sex partner (past 6m; missing=11) | 157 (78.5%) | 101 (79.5%) | 56 (76.7%) | .64 |
| High risk sex partner (past 6m; missing=22) | 71 (37.6%) | 41 (33.3%) | 30 (45.5%) | .10 |
| Unprotected sex (past 6m) | 155 (73.5%) | 92 (68.2%) | 63 (82.9%) | <.05* |
| Social Network Characteristics | ||||
| Size (mean (SD)) | 14.3 (6.1) | 14.8 (6.1) | 13.5 (6.1) | .13 |
| Density (mean (SD)) | 0.4 (0.3) | 0.4 (0.3) | 0.4 (0.3) | .98 |
| Prop. family (mean (SD)) | 0.3 (0.3) | 0.3 (0.3) | 0.4 (0.3) | <.05* |
| Prop. friend (mean (SD); missing=2) | 0.7 (0.3) | 0.7 (0.3) | 0.6 (0.4) | <.05* |
| Prop. female (mean (SD); missing=2) | 0.5 (0.2) | 0.5 (0.2) | 0.5 (0.2) | .09 |
| Prop. taking PrEP (mean (SD); missing=1) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.01) | .32 |
| Prop. regularly tests for HIV (mean (SD); missing=2) | 0.2 (0.3) | 0.1 (0.3) | 0.2 (0.4) | .08 |
| Prop. supportive of ego HIV testing (mean (SD); missing=2) | 0.8 (0.4) | 0.8 (0.4) | 0.9 (0.3) | .71 |
p-values derived from chi-square test and Fisher’s exact test for categorical variables and t-tests for ordinal and continuous variables
Cronbach’s alpha for scales in the current study are as follows: MDSR α=.79; Barriers to HIV testing α=.80
Respondents who said they are likely to take PrEP in the future more frequently reported being recently homeless (61% vs. 45%, p<0.05), having been arrested (84% vs. 69%, p<0.05), and having experienced forced sex (57% vs. 39%, p<0.05). They reported higher scores on the discrimination scale (range 0–10; 3.0 vs. 2.4, p<0.05), higher perceived HIV risk (range 0–5; 1.4 vs. 0.8, p<0.001), and more HIV testing barriers (range 1–5; 3.0 vs. 2.6, p<0.001). ‘Likely PrEP Users’ more frequently reported recent alcohol use (90% vs. 80%, p<0.05) and having ever participated in a 12-step recovery program (59% vs. 41%, p<.05). For sexual behavior, ‘Likely PrEP Users’ were more likely to report a recent casual sex partner (59% vs. 41%, p<0.05) and unprotected sex (83% vs. 68%, p<0.05). Likely PrEP users were also more likely to have networks with a greater proportion of family (0.39 vs. 0.31, p<.05) and a lower proportion of friends (0.63 vs. 0.74, p<.05).
Table 2 presents results from the GLMM regression models. The reduced model includes five significant variables: perceived risk of HIV (aOR=1.82, 95% CI=1.14, 2.92), barriers to HIV testing (aOR=4.76, 95% CI=1.66, 13.63), having participated in a 12-step program (aOR=4.39, 95% CI=1.39, 13.85), having a network where a higher proportion of members test regularly for HIV (aOR=1.27, 95% CI=1.06, 1.53), and having a network with a lower proportion of friends (aOR=.82, 95% CI=.67, .99). Models were replicated without transgender women (n=3) and excluding a cisgender woman with prior PrEP history (n=1). The significance of findings did not change, so we retained these individuals in our final model.
Table 2.
Multivariable Generalized Linear Mixed Effects Models (GLMM) Regression Models of Individual and Network Characteristics on Likely Future PrEP Use
| Full Model (n=184) |
Reduced Model (n=206) | |
|---|---|---|
| aOR, (95% CI) | aOR, (95% CI) | |
|
| ||
| Perceived risk of HIV □ | 1.40 (0.83, 2.37) | 1.82 (1.14, 2.92) |
| Barriers to HIV testing □ | 4.35 (1.72, 10.99) | 4.76 (1.66, 13.63) |
| Likely to HIV test in the future | 1.23 (0.92, 1.64) | |
| Homeless (past 6m) | 1.37 (0.47, 3.94) | |
| Arrested (ever) | 0.84 (0.20, 3.48) | |
| Discrimination (MDSR) □ | 0.91 (0.73, 1.14) | |
| Ever been forced to have sex | 1.36 (0.50, 3.74) | |
| Consumed alcohol (past 6m) | 2.58 (0.67, 9.96) | |
| 12-step participation (AA or NA; ever) | 3.71 (1.18, 11.71) | 4.39 (1.39, 13.85) |
| Casual sex partner (past 6m) | 1.07 (0.36, 3.12) | |
| Unprotected sex (past 6m) | 1.13 (0.29, 4.37) | |
| Network proportion family ◊ | 1.06 (0.89, 1.26) | |
| Network proportion friend ◊ | 0.87 (0.74, 1.02) | 0.82 (0.67, 0.99) |
| Network proportion female ◊ | 0.95 (0.75, 1.19) | |
| Network proportion regularly HIV testing ◊ | 1.22 (1.03, 1.44) | 1.27 (1.06, 1.53) |
aOR in terms of a one-unit increase on the scale: Perceived risk range 0–4; Barriers to HIV testing scale range 0–4.9; Discrimination scale range 0–10)
The unit for network proportion variables is .10, so aORs are applied to a 10% increase in the network proportion with a particular trait.
Finally, a post hoc analysis revealed a marginally significant interaction between proportion of friends in network and proportion in network who tests regularly for HIV (p=.06, Table 3). Figure 1 depicts the interaction by providing predicted probabilities of likely future PrEP use in a hypothetical network of ten alters, assuming median perceived risk and HIV testing barriers, and with previous 12-step involvement. When one’s network has weak HIV testing norms (i.e., no one in the network tests regularly), the probability of likely future PrEP use decreases as the proportion of friends in the network decreases. However, when one’s network has strong HIV testing norms (i.e., everyone tests regularly), additional friends increase the predicted probability of likely PrEP use: 55% where two of ten network members are friends, 78% with six of ten are friends, and 88% when nine of ten are friends.
Table 3.
Reduced Generalized Linear Mixed Effects Models (GLMM) Model with Interaction Term
| Coefficient | Standard Error | p-value | aOR, (95% CI) | ||
|---|---|---|---|---|---|
| Intercept | −5.13 | 1.74 | <.01 | - | - |
| Perceived risk of HIV | 0.62 | 0.25 | <.05 | 1.87 | (1.14, 3.05) |
| Barriers to HIV testing | 1.59 | 0.57 | <.01 | 4.91 | (1.58, 15.26) |
| 12-step participation (AA or NA ever) | 1.53 | 0.61 | <.05 | 4.61 | (1.39, 15.35) |
| Network proportion friend ◊ | −2.76 | 1.18 | <.05 | 0.82 | (0.02, 1.02) |
| Network proportion regularly HIV testing ◊ | −1.70 | 2.15 | 0.43 | 1.23 | (1.02, 1.49) |
| Proportion friend * Proportion tests regularly | 5.32 | 2.79 | 0.06 | aOR not generated for interaction term | |
aOR in terms of a one-unit increase on the scale: Perceived risk range 0–4; Barriers to HIV testing scale range 0–4.9; Discrimination scale range 0–10)
The unit for network proportion variables is .10, so aORs are applied to a 10% increase in the network proportion with a particular trait.
Figure 1.
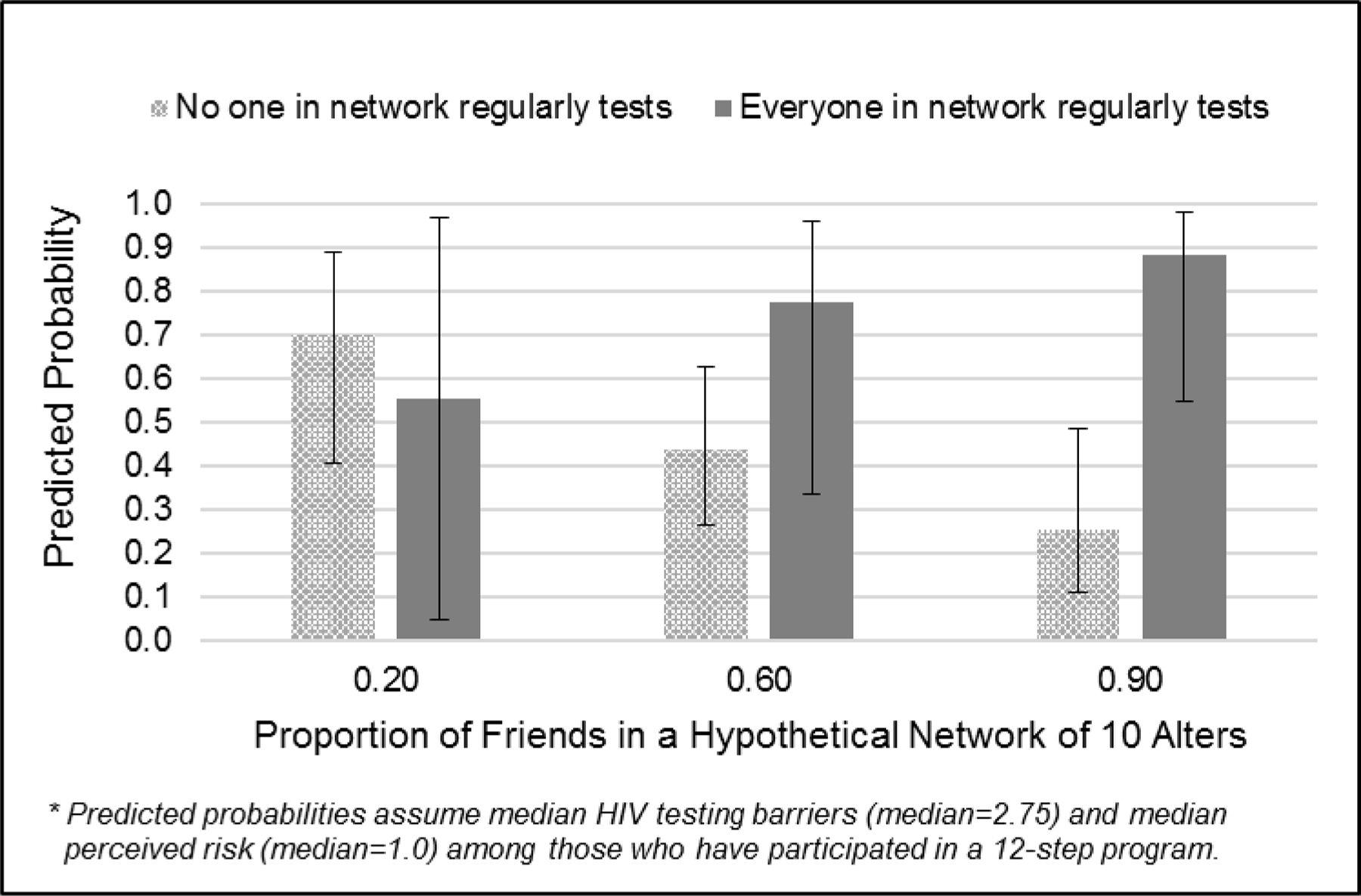
Predicted Probabilities of Likely Future PrEP Use: Interaction Effect of Network Proportion Friends and Network Proportion who Tests Regularly for HIV
Discussion
Our findings highlight the importance of social networks. We found low levels of PrEP awareness, which underscores a need for education about PrEP. Perceived risk, barriers to HIV testing, participation in a 12-step group, and having a social network that tests more regularly for HIV increased odds of likely PrEP use, whereas having a network with a higher proportion of friends decreased the odds. Notably, several risk and testing behaviors were not retained in the final model. It is possible that in our sample perceived risk fully mediated the associations between reported risk, testing, and future PrEP. However, such an inquiry was beyond the scope of what could be accomplished in this sample. Further, strong HIV testing norms moderated the association between the proportion friends in the network and likely future PrEP intentions. As such, resources for communities at-risk should consider how an individual’s broader network of relationships may facilitate or impede PrEP uptake. Someone’s anticipated PrEP use might be jointly conditioned by the presence of important relationships (e.g., friends) and broader norms. This suggests that when networks hold favorable, pro-health norms, they can be a source of encouragement for the uptake of health interventions such as PrEP. Fostering norms that encourage women to bring in others that they believe may be at high risk and capitalizing on networks of friends may be appropriate network-level strategies. Additionally, while 12-step and other recovery programs do not explicitly address sexual health, one practical application of our results would be to co-locate PrEP education services with addiction treatment, 12-step recovery, or other mutual-aid-based recovery programs. The association between PrEP intentions and 12-step participation may reflect the strong social bonds and pro-health norms within these groups. Conversely, it may be that people with elevated HIV risk are more likely to use drugs/alcohol and join 12-step groups. Until this relationship can be investigated more thoroughly, co-locating PrEP resources in the context of an existing peer support environment could help with uptake and adherence of PrEP.48
Though they did not persist in the final model, our bivariate findings also support previous research that many people who stand to benefit from PrEP may be located at multiple, intersecting positions of disadvantage. This is especially true in BAA communities where historical abuses from providers have rightfully caused mistrust.49 It is also true of people who are homeless, since procuring and storing PrEP will be especially challenging.50 Interventions should accommodate the needs of individuals who may benefit from taking PrEP and think creatively about solutions, such as connecting women to free PrEP options or helping those who are unhoused storing/accessing their PrEP. For example, one study heard from a woman who was unstably housed and asked to store her PrEP in a friend’s garage for safekeeping.51 Our bivariate results suggest that many individuals who are interested in PrEP have experienced interpersonal and structural violence. ‘Likely future PrEP users’ more frequently experienced discrimination, a history of forced sex, and prior arrest. Therefore, solutions may integrate HIV prevention services within other services, such as domestic violence or criminal justice agencies. Having trauma-informed PrEP education and counseling interventions may be especially important to mitigate the harms caused by interpersonal and structural violence.37
These results should be considered in light of the study’s limitations. First, this took place in a small city where less than 3% is BAA. Additionally, recruitment allowed for the inclusion of network members who were not themselves BAA/Latinx or women. Therefore, the findings from this study are not necessarily representative of BAA women in other locations, though they speak to a more diverse sample. Second, alter characteristics were perception-based. Findings should be interpreted as cognitive representations of network members rather than direct reports and may be inaccurate. However, research suggests that individuals are able to accurately assess the attitudes and behaviors of their network members,52 and in this case perceived behavior may be more important than actual behavior. To understand the influence of network composition, we stratified our interaction analysis based on everyone tests vs. no one tests to allow for interpretation. However, actual networks are unlikely to reflect these extremes, and future analyses should thoroughly investigate the nuanced relationship between networks and health. Third, respondents in the study were provided a brief description about PrEP and were not provided in-depth counseling on eligibility, efficacy, or side effects. Based on this initial impression, our outcome measured intentions around PrEP use, which may not predict future behavior. Nevertheless, intentions around PrEP are important behavioral precursors across the PrEP care continuum.12 Finally, we are not able to make claims about the pathways through which these variables are associated with future PrEP intentions. Future analyses using structural equation or path modeling could help disentangle the relationships between norms of HIV testing, risk profiles, and PrEP intentions. Despite these limitations, this study contributes to the growing literature on at-risk women and members of their social networks outside large cities.
Conclusion
Despite PrEP promise in reducing racial/ethnic disparities in HIV infection rates, research often focuses on individual factors among samples of MSM and within urban communities. Using a diverse sample composed of BAA and Latinx women and people in their networks in a small western city, our study highlights several individual and network characteristics that may be important for interventionists and practitioners to consider when promoting PrEP. At the individual-level, perceived HIV risk, barriers to HIV testing, and participation in a 12-step recovery program increased odds of anticipated future PrEP use. For social networks, the analysis depicted a moderated relationship between network characteristics, such that having more friends in one’s network was positively associated with PrEP intentions when HIV testing norms in the network were strong. This study contributes to the CDC’s EHE initiative and suggests tailoring interventions to the needs of individuals who are socially disadvantaged, underscores the need for trauma-informed care, proposes the co-location of PrEP resources in environments where people can find peer support such as drug and alcohol treatment programs, and emphasizes that individuals are embedded in broader social networks.
Source of Funding
This research was part of a larger project, “Capitalizing On Networks to Decrease Obstacles to Testing” (CONnect the DOTs), supported by the National Institute On Drug Abuse (NIDA) of the National Institutes of Health under Award Number R01DA038185 (K.D.W.). Additional funding sources include K01DA031031 and the San Diego Center for AIDS Research P30AI036214 (J.K.S.) and NIDA R21DA043417–02 (A.M.R. and M.F.).
Footnotes
Conflicts of Interest
The authors have no conflicts of interest to disclose.
Contributor Information
Laura M. JOHNSON, University of Nevada, Reno
Harold D. GREEN, Jr., Indiana University.
Brandon KOCH, University of Nevada, Reno.
Jamila K. STOCKMAN, University of California, San Diego.
Marisa FELSHER, Johns Hopkins University.
Alexis M. ROTH, Drexel University.
Karla D. WAGNER, University of Nevada Reno.
References
- 1.Centers for Disease Control and Prevention. Estimated HIV Incidence and Prevalence in the United States 2010–2016. HIV Surveill Suppl Rep 2019;(24 (No. 1)). Accessed June 19, 2020. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html [Google Scholar]
- 2.HIV and Gay and Bisexual Men | HIV by Group | HIV/AIDS | CDC Published June 4, 2020. Accessed September 10, 2020. https://www.cdc.gov/hiv/group/msm/index.html
- 3.HIV.gov. What is ‘Ending the HIV Epidemic: A Plan for America’? HIV.gov Published February 26, 2020. Accessed April 22, 2020. https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview
- 4.Office of National AIDS Policy. National HIV/AIDS Strategy for the United States: Updated to 2020 White House Office of National AIDS Policy; Washington, DC; 2015. [Google Scholar]
- 5.Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med 2012;367(5):399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peng P, Su S, Fairley CK, et al. A global estimate of the acceptability of pre-exposure prophylaxis for HIV among men who have sex with men: a systematic review and meta-analysis. AIDS Behav 2018;22(4):1063–1074. [DOI] [PubMed] [Google Scholar]
- 7.Cohen SE, Vittinghoff E, Bacon O, et al. High Interest in Pre-exposure Prophylaxis Among Men Who Have Sex with Men at Risk for HIV-Infection: Baseline Data from the US PrEP Demonstration Project. J Acquir Immune Defic Syndr 1999 2015;68(4):439–448. doi: 10.1097/QAI.0000000000000479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riddell J, Amico KR, Mayer KH. HIV preexposure prophylaxis: a review. Jama 2018;319(12):1261–1268. [DOI] [PubMed] [Google Scholar]
- 9.Felsher M, Ziegler E, Smith LR, et al. An Exploration of Pre-exposure Prophylaxis (PrEP) Initiation Among Women Who Inject Drugs. Arch Sex Behav Published online 2020. [DOI] [PMC free article] [PubMed]
- 10.Sherman SG, Schneider KE, Park JN, et al. PrEP awareness, eligibility, and interest among people who inject drugs in Baltimore, Maryland. Drug Alcohol Depend 2019;195:148–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roth AM, Tran NK, Piecara BL, Shinefeld J, Brady KA. Pre-Exposure Prophylaxis (PrEP) Awareness Is Low Among Heterosexual People of Color Who Might Benefit From PrEP in Philadelphia. J Prim Care Community Health 2019;10:2150132719847383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Willie TC, Stockman JK, Keene DE, Calabrese SK, Alexander KA, Kershaw TS. Social Networks and Its Impact on Women’s Awareness, Interest, and Uptake of HIV Pre-exposure Prophylaxis (PrEP): Implications for Women Experiencing Intimate Partner Violence. JAIDS J Acquir Immune Defic Syndr 2019;80(4):386. doi: 10.1097/QAI.0000000000001935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Auerbach JD, Kinsky S, Brown G, Charles V. Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDs 2015;29(2):102–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel AS, Goparaju L, Sales JM, et al. PrEP Eligibility Among At-Risk Women in the Southern United States: Associated Factors, Awareness, and Acceptability. J Acquir Immune Defic Syndr 1999 2019;80(5):527–532. doi: 10.1097/QAI.0000000000001950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sales JM, Steiner RJ, Brown JL, Swartzendruber A, Patel AS, Sheth AN. PrEP eligibility and interest among clinic-and community-recruited young black women in Atlanta, Georgia, USA. Curr HIV Res 2018;16(3):250–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bond KT, Gunn AJ. Perceived advantages and disadvantages of using Pre-Exposure Prophylaxis (PrEP) among sexually active black women: an exploratory study. J Black Sex Relatsh 2016;3(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wingood GM, Dunkle K, Camp C, et al. Racial Differences and Correlates of Potential Adoption of Pre-exposure Prophylaxis (PrEP): Results of a National Survey. J Acquir Immune Defic Syndr 1999 2013;63(0 1):S95–S101. doi: 10.1097/QAI.0b013e3182920126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Edelman EJ, Moore BA, Calabrese SK, et al. Primary care physicians’ willingness to prescribe HIV pre-exposure prophylaxis for people who inject drugs. AIDS Behav 2017;21(4):1025–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krakower DS, Mayer KH. The role of healthcare providers in the roll-out of PrEP. Curr Opin HIV AIDS 2016;11(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elopre L, Kudroff K, Westfall AO, Overton ET, Mugavero MJ. The right people, right places, and right practices: disparities in PrEP access among African American men, women and MSM in the Deep South. J Acquir Immune Defic Syndr 1999 2017;74(1):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hill BS, Patel VV, Haughton LJ, Blackstock OJ. Leveraging social media to explore Black women’s perspectives on HIV pre-exposure prophylaxis. J Assoc Nurses AIDS Care JANAC 2018;29(1):107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tekeste M, Hull S, Dovidio JF, et al. Differences in Medical Mistrust Between Black and White Women: Implications for Patient–Provider Communication About PrEP. AIDS Behav 2019;23(7):1737–1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Flash CA, Stone VE, Mitty JA, et al. Perspectives on HIV prevention among urban Black women: A potential role for HIV pre-exposure prophylaxis. AIDS Patient Care STDs 2014;28(12):635–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kadushin C Understanding Social Networks: Theories, Concepts, and Findings OUP USA; 2012. [Google Scholar]
- 25.Valente TW, Fosados R. Diffusion of Innovations and Network Segmentation: The Part Played by People in Promoting Health: Sex Transm Dis 2006;33(Supplement):S23–S31. doi: 10.1097/01.olq.0000221018.32533.6d [DOI] [PubMed] [Google Scholar]
- 26.Kuhns LM, Hotton AL, Schneider J, Garofalo R, Fujimoto K. Use of Pre-exposure Prophylaxis (PrEP) in Young Men Who Have Sex with Men is Associated with Race, Sexual Risk Behavior and Peer Network Size. AIDS Behav 2017;21(5):1376–1382. doi: 10.1007/s10461-017-1739-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walters SM, Reilly KH, Neaigus A, Braunstein S. Awareness of pre-exposure prophylaxis (PrEP) among women who inject drugs in NYC: the importance of networks and syringe exchange programs for HIV prevention. Harm Reduct J 2017;14(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Felsher M, Koku E, Lankenau S, Brady K, Bellamy S, Roth AM. Motivations for PrEP-Related Interpersonal Communication Among Women Who Inject Drugs: A Qualitative Egocentric Network Study: Qual Health Res Published online September 1, 2020. doi: 10.1177/1049732320952740 [DOI] [PMC free article] [PubMed]
- 29.Fletcher FE, Fisher C, Buchberg MK, et al. “Where Did This [PrEP] Come From?” African American Mother/Daughter Perceptions Related to Adolescent Preexposure Prophylaxis (PrEP) Utilization and Clinical Trial Participation. J Empir Res Hum Res Ethics 2018;13(2):173–184. [DOI] [PubMed] [Google Scholar]
- 30.Jaiswal J, Halkitis PN. Towards a more inclusive and dynamic understanding of medical mistrust informed by science. Behav Med 2019;45(2):79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bogart LM, Ransome Y, Allen W, Higgins-Biddle M, Ojikutu BO. HIV-related medical mistrust, HIV testing, and HIV risk in the national survey on HIV in the Black community. Behav Med 2019;45(2):134–142. doi: 10.1080/08964289.2019.1585324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goparaju L, Experton LS, Praschan NC, Warren-Jeanpiere L, Young MA, Kassaye S. Women want Pre-Exposure Prophylaxis but are Advised Against it by Their HIV-positive Counterparts. J AIDS Clin Res 2015;6(11):1–10. doi: 10.4172/2155-6113.1000522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Calabrese SK, Underhill K. How stigma surrounding the use of HIV preexposure prophylaxis undermines prevention and pleasure: a call to destigmatize “Truvada Whores.” Am J Public Health 2015;105(10):1960–1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Knight R, Small W, Carson A, Shoveller J. Complex and Conflicting Social Norms: Implications for Implementation of Future HIV Pre-Exposure Prophylaxis (PrEP) Interventions in Vancouver, Canada. Prestage G, ed. PLOS ONE 2016;11(1):e0146513. doi: 10.1371/journal.pone.0146513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cahill SE. Emotional Capital and Professional Socialization: The Case of Mortuary Science Students (and Me). Soc Psychol Q 1999;62(2):101–116. doi: 10.2307/2695852 [DOI] [Google Scholar]
- 36.Phillips G, Neray B, Birkett M, Felt D, Janulis P, Mustanski B. Role of Social and Sexual Network Factors in PrEP Utilization Among YMSM and Transgender Women in Chicago. Prev Sci 2019;20(7):1089–1097. doi: 10.1007/s11121-019-00995-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Garfinkel DB, Alexander KA, McDonald-Mosley R, Willie TC, Decker MR. Predictors of HIV-related risk perception and PrEP acceptability among young adult female family planning patients. AIDS Care 2017;29(6):751–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garretson M, Scanlin K, Myers J, Blackstock O, Edelstein Z. Knowledge, Attitudes and Behaviors surrounding PrEP among Black and Latina Cisgender Women: Findings from the 2017 New York City Sexual Health Survey. In: APHA’s 2019 Annual Meeting and Expo (Nov. 2-Nov. 6) American Public Health Association; 2019. [Google Scholar]
- 39.Kimbrough LW, Fisher HE, Jones KT, Johnson W, Thadiparthi S, Dooley S. Accessing social networks with high rates of undiagnosed HIV infection: the social networks demonstration project. Am J Public Health 2009;99(6):1093–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bogart LM, Landrine H, Galvan FH, Wagner GJ, Klein DJ. Perceived discrimination and physical health among HIV-positive Black and Latino men who have sex with men. AIDS Behav 2013;17(4):1431–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Earnshaw VA, Smith LR, Chaudoir SR, Lee I-C, Copenhaver MM. Stereotypes about people living with HIV: implications for perceptions of HIV risk and testing frequency among at-risk populations. AIDS Educ Prev 2012;24(6):574–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Perry BL, Pescosolido BA. Functional specificity in discussion networks: The influence of general and problem-specific networks on health outcomes. Soc Netw 2010;32(4):345–357. doi: 10.1016/j.socnet.2010.06.005 [DOI] [Google Scholar]
- 43.Perry BL, Pescosolido BA, Borgatti SP. Egocentric Network Analysis: Foundations, Methods, and Models Cambridge University Press; 2018. [Google Scholar]
- 44.Wasserman S, Faust K. Social Network Analysis: Methods and Applications Vol 8. Cambridge university press; 1994. [Google Scholar]
- 45.Ranganathan P, Pramesh CS, Aggarwal R. Common pitfalls in statistical analysis: Logistic regression. Perspect Clin Res 2017;8(3):148–151. doi: 10.4103/picr.PICR_87_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kennedy WJ, Bancroft TA. Model building for prediction in regression based upon repeated significance tests. Ann Math Stat 1971;42(4):1273–1284. [Google Scholar]
- 47.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis Vol 998. John Wiley & Sons; 2012. [Google Scholar]
- 48.Simoni JM, Huh D, Frick PA, et al. Peer Support and Pager Messaging to Promote Antiretroviral Modifying Therapy in Seattle: A Randomized Controlled Trial. JAIDS J Acquir Immune Defic Syndr 2009;52(4):465–473. doi: 10.1097/QAI.0b013e3181b9300c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Benkert R, Cuevas A, Thompson HS, Dove-Meadows E, Knuckles D. Ubiquitous yet unclear: A systematic review of medical mistrust. Behav Med 2019;45(2):86–101. doi: 10.1080/08964289.2019.1588220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wenzel SL, Rhoades H, Harris T, Winetrobe H, Rice E, Henwood B. Risk behavior and access to HIV/AIDS prevention services in a community sample of homeless persons entering permanent supportive housing. AIDS Care 2017;29(5):570–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Felsher M, Koku E, Lankenau SE, Wagner K, Roth AM. Motivations for PrEP-Related Interpersonal Communication within Personal Networks of Women who Inject Drugs Oral Presentation presented at the: The International Sunbelt Social Network Conference; June 2019; Montreal, Canada. [Google Scholar]
- 52.Green HD, Hoover MA, Wagner GJ, Ryan GW, Ssegujja E. Measuring agreement between egos and alters: Understanding informant accuracy in personal network studies. Field Methods 2014;26(2):126–140. doi: 10.1177/1525822X13492676 [DOI] [Google Scholar]


