Abstract
Background
Varicose veins are one of the earliest clinical features of superficial venous insufficiency (SVI) of the lower limbs that affects around 20–40% of the population with a lot of burden on patients’ quality of life (QoL) and health systems if left untreated. They are defined as subcutaneous veins in the lower extremities which are dilated to ≥3 mm in diameter in the upright position and retrograde flow of >0.5 s in duration. (VVs) could occur in the great saphenous vein (GSV) or small saphenous vein (SSV) and/or in any of their tributaries.
Methods
A prospective non-randomized comparative study for three methods of treatment of varicose veins was conducted. All symptomatic varicose veins with Clinical, Etiological, Anatomical, Pathophysiological (CEAP) Clinical classes of 2 or greater and demonstrated venous reflux with a duration of 0.5 s or greater on duplex ultrasound imaging GSV larger than 10 mm in diameter by duplex ultrasound were included.
Results
A total of 150 patients with 183 legs in all three groups are treated. The mean age of the patients in all groups was comparable (37.32) years, and a total of 87% were women. Demographic and preoperative clinical features, presentations, and anatomic characteristics were comparable in all groups. Disfigurement was the main presenting complaint in all. All postoperative complications were significantly higher in the group of surgery over 48 months of follow up the degree of satisfaction measured by VCSS score was highest among the RFA group followed by the EVLA group.
Conclusion
The results of our study suggest that the long-term results of endovenous thermal ablation methods (EVLA, RFA) are superior to open surgery for the management of varicose veins, with the RFA group showing better results in terms of improvement in QoL based on VCSS compared to the EVLA group.
Keywords: Varicose veins, EVLA, RFA, Surgery, Quality of life (QoL), Venous clinical severity score (VCSS)
Highlights
-
•
Varicose veins are a very common disorder in all communities.
-
•
A very wide variety of treatment options are available.
-
•
The ideal method of treatment is still debatable.
-
•
Our research paper tries to answer the question of what is the most suitable method of treatment for varicose veins.
1. Introduction
Varicose veins (VVs) are one of the earliest clinical features of superficial venous insufficiency (SVI) of the lower limbs that affects around 20–40% of the population with a lot burden on patients’ quality of life (QoL) and health systems if left untreated [1,2]. The great saphenous vein (GSV) is much more commonly affected and this can commence in any part of the vein and tends over time to propagate distally and proximally as well as between superficial and deep systems [3,4].
Varicose veins are defined as subcutaneous veins in the lower extremities which are dilated to ≥3 mm in diameter in the upright position and retrograde flow of >0.5 s in duration [5,6]. VVs could occur in the great saphenous vein GSV or small saphenous vein (SSV) and/or in any of their tributaries [7].
Most current theories that explain the pathophysiology of the VVs are that they represent primary venous disease and occur as a result of the structural weakening of the wall of the vein, which can be focal in nature or diffuse [8]. Since VVs are considered a disease of the developed countries, hence a lot of advancement has been made in the modalities of their management [9].
While open surgery used to be the only definitive management of patients diagnosed with VVs, albeit with recurrence rates of around 40%, in the past two decades it has been broadly abandoned in most parts of the world and replaced with endovenous thermal, mechanical, or chemical ablations [10,11].
Recently, the percutaneous thermal ablation modalities attained worldwide acceptance. It includes endovenous laser ablation (EVLA) and radiofrequency ablation (RFA) [12]. Each of these methods that causing thermal-induced energy causing transmural injury to the endothelium of the vein with eventual thrombosis and closure [13]. Both methods of ablation have undergone a lot of advancement to achieve optimal results and decrease recurrence rates with 2–5% recurrence rates reported [14,15].
The introduction of the endovenous thermal ablation modalities is relatively new in our country, with open surgery still being practiced in a lot of vascular centers. To the best of our knowledge, there hasn't been any published data comparing open surgery for VVs with short and long-term outcomes of both EVLA and RFA in Iraq.
2. Patients and methods
We conducted a prospective non-randomized comparative study for three methods of treatment of VVs. A total of one hundred and fifty patients were included between June 2016 and December 2019. Verbal and written consent was obtained from all participants for publication. All symptomatic VVs with Clinical, Etiological, Anatomical, Pathophysiological (CEAP) Clinical classes of 2 or greater and demonstrated venous reflux with a duration of 0.5 s or greater on duplex ultrasound imaging, all GSV larger than 10 mm in diameter by duplex ultrasound were consecutively included.
All patients who presented with secondary varicose veins were excluded from the study. The protocol and conduct of this study were reviewed and approved by our institutional review board. The same vascular surgeon performed all the clinical evaluations and endovenous thermal ablation procedures, The same sonographer interpreted the duplex findings. Reflux was considered significant if reversal of flow was present for 0.5 s or more after compression and decompression of the distal vein segment in the standing position. The diameters of the GSV were measured at several points, including the saphenofemoral junction (SFJ); the high, mid, and low thigh; and the high, mid, and low calf. Disease severity was assessed using the “C” of the CEAP clinical classification. Treatment modality chose according to the decision of the surgeon and the patient's preference.
All procedures were carried out under spinal anesthesia no tumescent anesthesia was used to minimize the bias of the outcomes. The group of surgery all has standard high ligation of the saphenofemoral junction with the stripping of the GSV down to 2 cm below knee joint added to that multiple mini-phlebectomies for all visible and palpable abnormal dilated veins. For the group EVLA, we used Surgical laser ENDOTHERME™ 1470 ring light radial fibers by lsomedical, France. While for the group of RFA we used ThermoBLOCK Thermal Coagulation RF device Turkey.
All the cases were day cases and the protocol of follow-up and treatment was used for all three groups. They were followed up for 48 months by clinical and Doppler evaluation. Our post-procedure follow-up protocol includes duplex ultrasound scanning within 1 week; then at 1, 6, and 12 months after ablation; and annually thereafter. The Venous Clinical Severity Score (VCSS) [16] was used to evaluate the outcome postoperatively for all the 3 groups.
Patient demographics collected included age, gender, and occupation comorbidities. Other covariates captured included the pretreatment baseline characteristics such as disease severity by CEAP classification scores and GSV diameter.
Treatment details recorded included the anatomic location of vein ablated and adjunctive procedures such as phlebectomy. Posttreatment complications recorded included pulmonary embolism, DVT, endothermal heat-induced thrombosis, and neuropathy.
Recurrence data recorded included the date, anatomic site, and pattern of recurrence. The lower extremities of patients who underwent bilateral saphenous ablation were considered separately. The primary endpoints for the study were clinical recurrence and duplex-detected recurrence.
All statistical computation is enhanced by using the (IBM® SPSS®) Statistics 21. The data had been coded, tabulated, and presented in a descriptive form. The statistical procedure that was applied to determine the results of the present study included: Descriptive statistical data analysis (Frequency, Percentage, Mean, and Stander deviation). For the Inferential data analysis: The chi-Square test used. To calculate the differences between the survival curves, the log-rank test was used. A p-value of less than 0.05 was considered statistically significant. Kaplan-Meier survival analysis was used to assess time to clinical recurrence and the VCSS post-operative score was used to assess the degree of satisfaction from the procedure.
Ethical approval obtained from our Institutional Review Board by act no. 1178/September 8th,2021. Our work has been reported in line with the STROCSS2021 criteria [17]. This study was registered on ResearchRegistry.com (registration number: researchregistry7854).
3. Results
A total of 150 patients with 183 legs in all three groups were treated. The mean age of the patients in all groups was comparable (37.32) years, and a total of 87% were women. Demographic and preoperative clinical features, presentations, and anatomic characteristics were comparable in all groups. Strangely pain was not an important presentation for all groups, while disfigurement was the main presenting complaint in all. In this series of patients, the frequency of the right and left sides were statistically not significant. The occupation of the patients was again comparable in all groups, as the more frequent were housewives (73% of all the cases). The majority were not smokers. The body mass index (BMI) calculation showed that most of the patients were overweight (mean BMI = 24.47), the significant point is that the rate of overweight and obesity was significantly higher in the group of surgery (Table 1).
Table (1).
Distribution of the preoperative demographics.
| Demographics | Items | EVLA cases |
RFA Case |
Surgery case |
All |
||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Age | <25 | 3 | 6.0 | 6 | 12 | 5 | 10 | 14 | 9.33 |
| 25–34 | 19 | 38.0 | 15 | 30 | 16 | 32 | 50 | 33.33 | |
| 35–44 | 17 | 34.0 | 17 | 34 | 21 | 42 | 55 | 36.67 | |
| 45–54 | 9 | 18.0 | 10 | 20 | 6 | 12 | 25 | 16.67 | |
| >54 | 2 | 4.0 | 2 | 4 | 2 | 4 | 6 | 4.00 | |
| Mean ± S.D | 37.16 ± 8.51 | 38.24 ± 9.99 | 36.56 ± 8.74 | 37.32 ± 9.07 | |||||
| Sex | Male | 21 | 42.0 | 23 | 46 | 19 | 38 | 63 | 42.00 |
| Female | 29 | 58.0 | 27 | 54 | 31 | 62 | 87 | 58.00 | |
| Site | Right | 15 | 30.0 | 21 | 42 | 24 | 48 | 60 | 40.00 |
| Left | 19 | 38.0 | 16 | 32 | 22 | 44 | 57 | 38.00 | |
| Bilateral | 16 | 32.0 | 13 | 26 | 4 | 8 | 33 | 22.00 | |
| Pain | No | 50 | 100.0 | 48 | 96 | 50 | 100 | 148 | 98.67 |
| Yes | 0 | 0.0 | 2 | 4 | 0 | 0 | 2 | 1.33 | |
| Disfigurement | No | 0 | 0.0 | 2 | 4 | 0 | 0 | 2 | 1.33 |
| Yes | 50 | 100.0 | 48 | 96 | 50 | 100 | 148 | 98.67 | |
| Job | Employ | 7 | 14.0 | 8 | 16 | 12 | 24 | 27 | 18.00 |
| Free lance | 1 | 2.0 | 8 | 16 | 3 | 6 | 12 | 8.00 | |
| Housewife | 27 | 54.0 | 21 | 42 | 25 | 50 | 73 | 48.67 | |
| Barber | 8 | 16.0 | 7 | 14 | 3 | 6 | 18 | 12.00 | |
| Restaurant | 7 | 14.0 | 6 | 12 | 7 | 14 | 20 | 13.33 | |
| Smoking | No | 41 | 82.0 | 43 | 86 | 39 | 78 | 123 | 82.00 |
| Yes | 9 | 18.0 | 7 | 14 | 11 | 22 | 27 | 18.00 | |
| Comorbidities | No | 44 | 88.0 | 49 | 98 | 42 | 84 | 135 | 90.00 |
| Yes | 6 | 12.0 | 1 | 2 | 8 | 16 | 15 | 10.00 | |
| Obese | 3 | 50.0 | 0 | 0 | 5 | 62.5 | 8 | 53.33 | |
| If Yes | HTN | 3 | 50.0 | 1 | 100 | 1 | 12.5 | 5 | 33.33 |
| type 2DM | 0 | 0.0 | 0 | 0 | 2 | 25 | 2 | 13.34 | |
| Total | 6 | 100.0 | 1 | 100 | 8 | 100 | 15 | 10.00 | |
| BMI | Underweight | 0 | 0.0 | 0 | 0 | 2 | 4 | 2 | 1.33 |
| Normal weight | 21 | 42.0 | 23 | 46 | 26 | 52 | 70 | 46.67 | |
| Over Weight | 27 | 54.0 | 26 | 52 | 18 | 36 | 71 | 47.33 | |
| Obese | 2 | 4.0 | 1 | 2 | 4 | 8 | 7 | 4.67 | |
| Mean ± S.D | 24.86 ± 3.07 | 24.14 ± 2.99 | 24.42 ± 3.86 | 24.47 ± 3.32 | |||||
| General exam | 1 | 38 | 76.0 | 46 | 92 | 49 | 98 | 133 | 88.67 |
| 2 | 12 | 24.0 | 4 | 8 | 1 | 2 | 17 | 11.33 | |
| Total | 50 | 50 | 100.0 | 50 | 100 | 50 | 100 | 150 | |
The preoperative CEAP class 4 was the most frequent of the three groups, while CEAP class 5 was the second most frequent. The preoperative VCSS score for all groups was nearly similar 20.9–21.3 (mean 21.55).
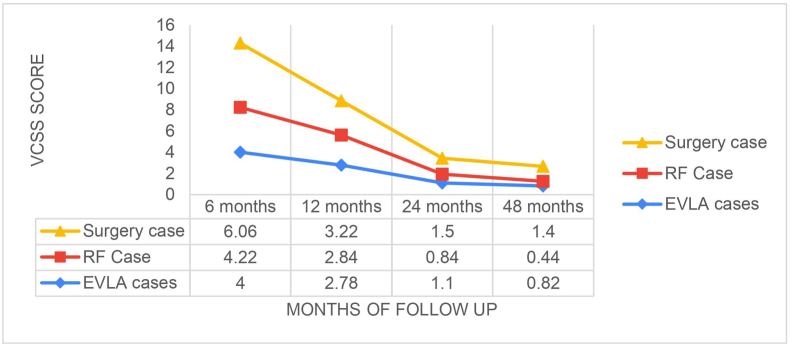
The preoperative Doppler measured reflux was grade three in the majority for all groups (EVLA grade 3 = 84%, RFA grade 3 = 80%, Surgery grade 3 = 68%). In all groups, mini-phlebotomy was performed for all and in only a minority accessory saphenous was ablated (Table 2). All postoperative complications (pain, hematoma, swelling, nerve damage, infection, Deep vein thrombosis (DVT), pulmonary embolism (PE), and Endovenous heat-induced thrombosis (EHIT) were significantly higher in the group of surgery as shown in Table 3. Over 48 months of follow up the degree of satisfaction measured by the VCSS score was highest among the RFA group followed by the EVLA group as demonstrated by the Kaplan-Meier graph in Fig. 1.
Table (2).
Distribution of the preoperative workup and operative details.
| Parameters | Items | EVLA cases |
RFA Case |
Surgery case |
All |
||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| CEAP | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 1 | 0.67 |
| 3 | 3 | 6 | 4 | 8 | 2 | 4 | 9 | 6.00 | |
| 4 | 29 | 58 | 32 | 64 | 23 | 46 | 84 | 56.00 | |
| 5 | 17 | 34 | 14 | 28 | 22 | 44 | 53 | 35.33 | |
| 6 | 0 | 0 | 0 | 0 | 3 | 6 | 3 | 2.00 | |
| Mean ± S.D | 4.22 ± 0.74 | 4.2 ± 0.57 | 4.53 ± 0.68 | 4.31 ± 0.68 | |||||
| VCSS | <15 | 4 | 8 | 1 | 2 | 6 | 12 | 11 | 7.33 |
| 15–20 | 16 | 32 | 13 | 26 | 15 | 30 | 44 | 29.33 | |
| >20 | 30 | 60 | 36 | 72 | 29 | 58 | 95 | 63.33 | |
| Mean ± S.D | 21.32 ± 5.3 | 22.44 ± 3.68 | 20.9 ± 4.86 | 21.55 ± 4.68 | |||||
| Doppler reflux grade | 1 | 0 | 0 | 0 | 0 | 3 | 6 | 3 | 2.00 |
| 2 | 8 | 16 | 10 | 20 | 13 | 26 | 31 | 20.67 | |
| 3 | 42 | 84 | 40 | 80 | 34 | 68 | 116 | 77.33 | |
| Phlebectomy | 2 | 49 | 98 | 50 | 100 | 50 | 100 | 149 | 99.33 |
| 4 | 1 | 2 | 0 | 0 | 0 | 0 | 1 | 0.67 | |
| Accessory saphenous vein ablation | No | 18 | 36 | 22 | 44 | 50 | 100 | 90 | 60.00 |
| Yes | 32 | 64 | 28 | 56 | 0 | 0 | 60 | 40.00 | |
| Hospital stay | 1 | 50 | 100 | 50 | 100 | 50 | 100 | 150 | 100.00 |
| Total | 50 | 100 | 50 | 100 | 50 | 100 | 150 | 100 | |
Table (3).
Distribution of the postoperative complications.
| Parameters | Items | EVLA cases |
RF Cases |
Surgery cases |
All |
||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| pain VAS | 1 | 0 | 0 | 0 | 0 | 1 | 2 | 1 | 0.67 |
| 2 | 1 | 2 | 1 | 2 | 0 | 0 | 2 | 1.33 | |
| 3 | 7 | 14 | 2 | 4 | 3 | 6 | 12 | 8.00 | |
| 4 | 15 | 30 | 9 | 18 | 4 | 8 | 28 | 18.67 | |
| 5 | 11 | 22 | 13 | 26 | 3 | 6 | 27 | 18.00 | |
| 6 | 9 | 18 | 13 | 26 | 10 | 20 | 32 | 21.33 | |
| 7 | 4 | 8 | 5 | 10 | 11 | 22 | 20 | 13.33 | |
| 8 | 1 | 2 | 7 | 14 | 12 | 24 | 20 | 13.33 | |
| 9 | 2 | 4 | 0 | 0 | 4 | 8 | 6 | 4.00 | |
| 10 | 0 | 0 | 0 | 0 | 2 | 4 | 2 | 1.33 | |
| Mean ± S.D | 4.92 ± 1.54 | 5.56 ± 1.47 | 6.6 ± 1.91 | 5.69 ± 1.79 | |||||
| Hematoma | No | 47 | 94 | 48 | 96 | 38 | 76 | 133 | 88.67 |
| Yes | 3 | 6 | 2 | 4 | 12 | 24 | 17 | 11.33 | |
| Swelling | No | 48 | 96 | 47 | 94 | 46 | 92 | 141 | 94.00 |
| Yes | 2 | 4 | 3 | 6 | 4 | 8 | 9 | 6.00 | |
| Nerve damage | No | 49 | 98 | 49 | 98 | 47 | 94 | 145 | 96.67 |
| Yes | 1 | 2 | 1 | 2 | 3 | 6 | 5 | 3.33 | |
| Infection | No | 49 | 98 | 48 | 96 | 45 | 90 | 142 | 94.67 |
| Yes | 1 | 2 | 2 | 4 | 5 | 10 | 8 | 5.33 | |
| DVT | No | 49 | 98 | 49 | 98 | 49 | 98 | 147 | 98.00 |
| Yes | 1 | 2 | 1 | 2 | 1 | 2 | 3 | 2.00 | |
| PE | No | 50 | 100 | 50 | 100 | 50 | 100 | 150 | 100.00 |
| EHIT | Yes | 50 | 100 | 49 | 98 | 50 | 100 | 149 | 99.33 |
| Yes | 0 | 0 | 1 | 2 | 0 | 0 | 1 | 0.67 | |
| Vein removed completely | No | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.00 |
| Yes | 50 | 100 | 50 | 100 | 50 | 100 | 150 | 100.00 | |
| Neo arch formation | No | 50 | 100 | 50 | 100 | 50 | 100 | 150 | 100.00 |
| Yes | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.00 | |
| Total | 50 | 100 | 100 | 50 | 100 | 50 | 100 | 150 | |
Fig. 1.
48 months of follow-up the degree of satisfaction measured by the VCSS score among the RFA group followed by the EVLA group is demonstrated by the Kaplan-Meier graph.
According to the study of the association between (EVLA, RF, and Surgery) cases concerning the sociodemographic characteristics, there were statistically significant associations (or differences) between EVLA, RF, and Surgery) cases in the site of the VV (p-value = 0.038) and General exam (p-value = 0.002) because the result of the p-value was less than the common alpha of 0.05. While, there were no statistically significant associations (or differences) between EVLA, RF, and Surgery) cases in other sociodemographic characteristics as the (p-value >0.05) (Table 4).
Table (4).
Association between (EVLA, RF and surgery) and Demographics.
| Demographics | Items | EVLA cases |
RF Case |
surgery case |
Significant Test |
||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | p-value | |||
| Age | <25 | 3 | 6.0 | 6 | 12 | 5 | 10 | 3.142 | 0.925 |
| 25–34 | 19 | 38.0 | 15 | 30 | 16 | 32 | |||
| 35–44 | 17 | 34.0 | 17 | 34 | 21 | 42 | |||
| 45–54 | 9 | 18.0 | 10 | 20 | 6 | 12 | |||
| >54 | 2 | 4.0 | 2 | 4 | 2 | 4 | |||
| Mean ± S.D | 37.16 ± 8.51 | 38.24 ± 9.99 | 36.56 ± 8.74 | F = 0.437(0.647) | |||||
| Sex | Male | 21 | 42.0 | 23 | 46 | 19 | 38 | 0.657 | 0.72 |
| Female | 29 | 58.0 | 27 | 54 | 31 | 62 | |||
| Site | Right | 15 | 30.0 | 21 | 42 | 24 | 48 | 10.138 | 0.038 |
| Left | 19 | 38.0 | 16 | 32 | 22 | 44 | |||
| Bilateral | 16 | 32.0 | 13 | 26 | 4 | 8 | |||
| Pain | No | 50 | 100.0 | 48 | 96 | 50 | 100 | 4.053 | 0.132 |
| Yes | 0 | 0.0 | 2 | 4 | 0 | 0 | |||
| Disfigurement | No | 0 | 0.0 | 2 | 4 | 0 | 0 | 4.054 | 0.132 |
| Yes | 50 | 100.0 | 48 | 96 | 50 | 100 | |||
| Job | Employ | 7 | 14.0 | 8 | 16 | 12 | 24 | 11.256 | 0.188 |
| Free lance | 1 | 2.0 | 8 | 16 | 3 | 6 | |||
| Housewife | 27 | 54.0 | 21 | 42 | 25 | 50 | |||
| Barber | 8 | 16.0 | 7 | 14 | 3 | 6 | |||
| Restaurant | 7 | 14.0 | 6 | 12 | 7 | 14 | |||
| Smoking | No | 41 | 82.0 | 43 | 86 | 39 | 78 | 1.084 | 0.582 |
| Yes | 9 | 18.0 | 7 | 14 | 11 | 22 | |||
| Comorbidities | No | 44 | 88.0 | 49 | 98 | 42 | 84 | 5.778 | 0.056 |
| Yes | 6 | 12.0 | 1 | 2 | 8 | 16 | |||
| Obese | 3 | 50.0 | 0 | 0 | 5 | 62.5 | 5.297 | 0.258 | |
| If Yes | HTN | 3 | 50.0 | 1 | 100 | 1 | 12.5 | ||
| type 2DM | 0 | 0.0 | 0 | 0 | 2 | 25 | |||
| Total | 6 | 100.0 | 1 | 100 | 8 | 100 | |||
| BMI | Underweight | 0 | 0.0 | 0 | 0 | 2 | 4 | 8.599 | 0.197 |
| Normal weight | 21 | 42.0 | 23 | 46 | 26 | 52 | |||
| Over Weight | 27 | 54.0 | 26 | 52 | 18 | 36 | |||
| Obese | 2 | 4.0 | 1 | 2 | 4 | 8 | |||
| Mean ± S.D | 24.86 ± 3.07 | 24.14 ± 2.99 | 24.42 ± 3.86 | F = 0.594(0.553) | |||||
| General exam | 1 | 38 | 76.0 | 46 | 92 | 49 | 98 | 12.87 | 0.002 |
| 2 | 12 | 24.0 | 4 | 8 | 1 | 2 | |||
There was a statistically significant difference between EVLA, RF, and Surgery cases in Accessory saphenous vein ablation (p-value = 0.000) because the result of the p-value was less than 0.05. (Table 5).
Table (5).
Comparison of the (EVLA, RFA and Surgery) parameters.
| Parameters | Items | EVLA cases |
RF Case |
surgery case |
Significant Test |
||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | p-value | |||
| CEAP | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 12.016 | 0.151 |
| 3 | 3 | 6 | 4 | 8 | 2 | 4 | |||
| 4 | 29 | 58 | 32 | 64 | 23 | 46 | |||
| 5 | 17 | 34 | 14 | 28 | 22 | 44 | |||
| 6 | 0 | 0 | 0 | 0 | 3 | 6 | |||
| Mean ± S.D | 4.22 ± 0.74 | 4.2 ± 0.57 | 4.53 ± 0.68 | F = 3.63(0.029) | |||||
| VCSS | <15 | 4 | 8 | 1 | 2 | 6 | 12 | 4.678 | 0.322 |
| 15–20 | 16 | 32 | 13 | 26 | 15 | 30 | |||
| >20 | 30 | 60 | 36 | 72 | 29 | 58 | |||
| Mean ± S.D | 21.32 ± 5.3 | 22.44 ± 3.68 | 20.9 ± 4.86 | F = 1.456(0.237) | |||||
| Doppler reflux grade | 1 | 0 | 0 | 0 | 0 | 3 | 6 | 8.122 | 0.087 |
| 2 | 8 | 16 | 10 | 20 | 13 | 26 | |||
| 3 | 42 | 84 | 40 | 80 | 34 | 68 | |||
| Phlebectomy | 2 | 49 | 98 | 50 | 100 | 50 | 100 | 2.013 | 0.365 |
| 4 | 1 | 2 | 0 | 0 | 0 | 0 | |||
| Accessory saphenous vein ablation | No | 18 | 36 | 22 | 44 | 50 | 100 | 50.667 | 0.000 |
| Yes | 32 | 64 | 28 | 56 | 0 | 0 | |||
Over the entire duration of the study, the sonographic rate of recurrence was higher in the group of surgery and lowest in the group of RFA. While cosmetic complaints were again higher in surgery cases and lowest in RFA cases (Table 6).
Table (6).
Comparison of the rate of recurrence of the VVs and cosmetic outcome for the 3 groups.
| parameters | Items | EVLA cases |
RF Case |
Surgery case |
Significant Test |
||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | p-value | |||
| Varicose Vein recurrence by annual Doppler | No | 47 | 94 | 48 | 96 | 47 | 94 | 0.264 | 0.876 |
| Yes | 3 | 6 | 2 | 4 | 3 | 6 | |||
| Cosmetic complain | Yes | 48 | 96 | 47 | 94 | 34 | 68 | 20.266 | 0.000 |
| No | 2 | 4 | 3 | 6 | 16 | 32 | |||
4. Discussion
This non-randomized comparative study between endovenous thermal ablation methods (EVLA and RFA) and open surgery for managing varicose veins demonstrates the endovenous methods to be more superior to open surgery over the course of 48 months of follow-up in terms of improvement in QoL based on VCSS.
While other studies have shown both modalities of RFA and EVLA to be as equally effective over the short term and more than one-year follow-up [[18], [19], [20], [21]], we believe that the decline of the VCSS in our study is due to the fact that we performed the endovenous procedures in the theatre under spinal anesthesia making with the patients very comfortable with the whole experience.
As the pain has not been the major complaint of the patients, therefore, they have been highly contempt with the immediate cosmetic results provided by the intraoperative phlebectomies done in the same session. While other studies have shown the superiority of EVLA over RFA after 6 months of follow-up [22,23].
Although most of these studies don't have the same follow-up period of 48 months as ours and have reported a shorter duration of follow-up, the number of the study population is close to ours with minor changes as economic problems in our locality make performing minimally invasive procedures by our teams more challenging.
Our results have shown statistically significant improvement in QoL in the RFA group over the EVLA group and both of them over surgery after 48 months of follow-up, even though the majority of the patients in all groups have undergone micro-phlebectomy in the same session due to patient preference of removing the dilated, tortoise veins surgically over other methods yet patient satisfaction regarding cosmetic results have been equally superior to the open surgery group.
Strengths: The results of this study that superiority in short term and long-term for RFA is different from most all other studies, which in general in favor EVLA [3,4,12]. As well the duration of clinical and sonographic follow-up is relatively longer than most of the researchers about VVs.
Limitations: The sample size of our groups of patients is relatively small.
5. Conclusion
The results of our study suggest that the long-term results of endovenous thermal ablation methods (EVLA, RFA) are superior to open surgery for the management of varicose veins, with the RFA group showing better results in terms of improvement in QoL based on VCSS compared to the EVLA group. We recommend further groups take this fining into consideration and start further investigations.
Ethical approval
Ethical approval obtained from our Institutional Review Board by act no. 1178/September 8th, 2021.
Sources of funding for your research
No any private or public fund received for this paper.
Author contributions
AB; data collection, performing surgeries, study design, statistical analysis, draft revising, corresponding author and grantor.
DFS: data collection, performing surgeries, study design, statistical analysis, draft revising.
BHS: study design, statistical analysis, draft revising.
Declaration of competing interest
No conflicts of interest to declare.
Registration of research studies
-
1.
Name of the registry: ResearchRegistry.com
-
2.
Unique Identifying number or registration ID: researchregistry7854
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/browse-the-registry#home/registrationdetails/626beafb21bfba001e109c34/
Guarantor
The Guarantor is the one or more people who accept full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request”.
Acknowledgments
We would like to acknowledge all our personnel who assisted in serving our patients.
Contributor Information
Aram Baram, Email: aram.baramm@gmail.com, aram.baram@univsul.edu.iq.
Dezhin Faeq Rashid, Email: dezhynsolae@gmail.com.
Bashar Hana Saqat, Email: basharsaqat68@gmail.com.
Abbreviations
Not applicable.
References
- 1.Branisteanu D.-E., Feodor T., Baila S., Mitea I.-A., Vittos O. Impact of chronic venous disease on quality of life: results of vein alarm study. Exp. Ther. Med. 2019 Feb;17(2):1091–1096. doi: 10.3892/etm.2018.7054.Epub.2018.Dec.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campbell B. Physician turned patient with varicose veins. Phlebology. 2021 Oct;36(9):676–677. doi: 10.1177/02683555211011794.Epub.2021.Apr.26. [DOI] [PubMed] [Google Scholar]
- 3.Tuan T.A., Duc N.M., Minh L.N., Ha H.D., Luu V.D., Thong P.M. Comparing the efficacy of radiofrequency ablation versus laser ablation for chronic venous insufficiency in the lower extremities: a Vietnamese report. Med. Arch. 2020 Apr;74(2):100–104. doi: 10.5455/medarh.2020.74.100-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paravastu S.C.V., Dodd P.D. Endovenous ablation therapy (LASER or radiofrequency) or foam sclerotherapy versus conventional surgical repair for short saphenous varicose veins. Cochrane Database Syst. Rev. 2016 Nov 29;11(11):CD010878. doi: 10.1002/14651858.CD010878.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nandhra S., Wallace T., El-Sheikha J., Leung C., Carradice D., Chetter I. A randomized clinical trial of buffered tumescent local anaesthesia during endothermal ablation for superficial venous incompetence. Eur. J. Vasc. Endovasc. Surg. 2018 Nov;56(5):699–708. doi: 10.1016/j.ejvs.2018.05.017. Epub 2018 Jun 29. [DOI] [PubMed] [Google Scholar]
- 6.Gloviczki P., Comerota A.J., Dalsing M.C., Eklof B.G., Gillespie D.L., Gloviczki M.L., et al. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J. Vasc. Surg. 2011 May;53(5 Suppl):2S–48S. doi: 10.1016/j.jvs.2011.01.079. [DOI] [PubMed] [Google Scholar]
- 7.Healy D.A., Kimura S., Power D., Elhaj A., Abdeldaim Y., Cross K.S., et al. A systematic review and meta-analysis of thrombotic events following endovenous thermal ablation of the great saphenous vein. Eur. J. Vasc. Endovasc. Surg. 2018 Sep;56(3):410–424. doi: 10.1016/j.ejvs.2018.05.008. Epub 2018 Jun 9. [DOI] [PubMed] [Google Scholar]
- 8.Vuylsteke M.E., Klitfod L., Mansilha A. Endovenous ablation. Endovenous ablation. Int. Angiol. 2019 Feb;38(1):22–38. doi: 10.23736/S0392-9590.18.04047-6. Epub 2018 Nov 20. [DOI] [PubMed] [Google Scholar]
- 9.Bozoglan O., Mese B., Eroglu E., Ekerbiçer H.C., Yasim A. Comparison of endovenous laser and radiofrequency ablation in treating varices in the same patient. J Lasers Med Sci . Winter. 2017;8(1):13–16. doi: 10.15171/jlms.2017.03.Epub.2017.Jan.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hamann S.A.S., Timmer-de Mik L., Fritschy W.M., Kuiters G.R.R., Nijsten T.E.C., van den Bos R.R. Randomized clinical trial of endovenous laser ablation versus direct and indirect radiofrequency ablation for the treatment of great saphenous varicose veins. Br. J. Surg. 2019 Jul;106(8):998–1004. doi: 10.1002/bjs.11187.Epub.2019.May.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kheirelseid E.A.H., Crowe G., Sehgal R., Liakopoulos D., Bela H., Mulkern E., et al. Systematic review and meta-analysis of randomized controlled trials evaluating long-term outcomes of endovenous management of lower extremity varicose veins. J Vasc Surg Venous Lymphat Disord. 2018 Mar;6(2):256–270. doi: 10.1016/j.jvsv.2017.10.012. Epub 2017 Dec 29. [DOI] [PubMed] [Google Scholar]
- 12.Staniszewska A., Tambyraja A., Afolabi E., Bachoo P., Brittenden J. The Aberdeen Varicose Vein Questionnaire, patient factors and referral for treatment. Eur. J. Vasc. Endovasc. Surg. 2013 Dec;46(6):715–718. doi: 10.1016/j.ejvs.2013.08.019. Epub 2013 Sep 7. [DOI] [PubMed] [Google Scholar]
- 13.Mansilha A., Sousa J. Pathophysiological mechanisms of chronic venous disease and implications for venoactive drug therapy. Int. J. Mol. Sci. 2018 Jun 5;19(6):1669. doi: 10.3390/ijms19061669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eifell R.K., Bhattacharya V., Stansby G.P. Endovenous ablation (radiofrequency and laser) and foam sclerotherapy versus conventional surgery for long saphenous vein varices. Cochrane Database Syst. Rev. 2014 Jul 30;(7):CD005624. doi: 10.1002/14651858.CD005624.pub3. [DOI] [PubMed] [Google Scholar]
- 15.Gohel M.S., Heatley F., Liu X., Bradbury A., Bulbulia R., Cullum N., et al. Early versus deferred endovenous ablation of superficial venous reflux in patients with venous ulceration: the EVRA RCT. Health Technol. Assess. 2019 May;23(24):1–96. doi: 10.3310/hta23240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rutherford R.B., Padberg F.T., Jr., Comerota A.J., Kistner R.L., Meissner M.H., Moneta G.L. Venous severity scoring: an adjunct to venous outcome assessment. J. Vasc. Surg. 2000 Jun;31(6):1307–1312. doi: 10.1067/mva.2000.107094. [DOI] [PubMed] [Google Scholar]
- 17.Mathew G., Riaz Agha R., STROCSS Group Strocss 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int. J. Surg. 2021 Dec;96 doi: 10.1016/j.ijsu.2021.106165. Epub 2021 Nov 11. [DOI] [PubMed] [Google Scholar]
- 18.Sydnor M., Mavropoulos J., Slobodnik N., Wolfe L., Strife B., Komorowski D. A randomized prospective long-term (>1 year) clinical trial comparing the efficacy and safety of radiofrequency ablation to 980 nm laser ablation of the great saphenous vein. Phlebology. 2017 Jul;32(6):415–424. doi: 10.1177/0268355516658592.Epub.2016.Jul.15. [DOI] [PubMed] [Google Scholar]
- 19.Balint R., Farics A., Parti K., Vizsy L., Batorfi J., Menyhei G., et al. Which endovenous ablation method does offer a better long-term technical success in the treatment of the incompetent great saphenous vein? Review. Vascular. 2016 Dec;24(6):649–657. doi: 10.1177/1708538116648035.Epub.2016.Apr.28. [DOI] [PubMed] [Google Scholar]
- 20.Lawson J.A., Gauw S.A., van Vlijmen C.J., Pronk P., Gaastra M.T.W., Tangelder M.J., et al. Prospective comparative cohort study evaluating incompetent great saphenous vein closure using radiofrequency-powered segmental ablation or 1470-nm endovenous laser ablation with radial-tip fibers (Varico 2 study) J Vasc Surg Venous Lymphat Disord. 2018 Jan;6(1):31–40. doi: 10.1016/j.jvsv.2017.06.016. Epub 2017 Aug 24. [DOI] [PubMed] [Google Scholar]
- 21.Park I., Park S.C. Comparison of short-term outcomes between endovenous 1,940-nm laser ablation and radiofrequency ablation for incompetent saphenous veins. Front Surg. 2020 Dec 11;7 doi: 10.3389/fsurg.2020.620034.eCollection.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mese B., Bozoglan O., Eroglu E., Erdem K., Acipayam M., Ekerbicer H.C., et al. A Comparison of 1,470-nm endovenous laser ablation and radiofrequency ablation in the treatment of great saphenous veins 10 mm or more in size. Ann. Vasc. Surg. 2015 Oct;29(7):1368–1372. doi: 10.1016/j.avsg.2015.03.063. Epub 2015 Jun 27. [DOI] [PubMed] [Google Scholar]
- 23.Yoon W.J., Dresher M., Crisostomo P.R., Halandras P.M., Bechara C.F., Aulivola B. Delineating the durability outcome differences after saphenous ablation with laser versus radiofrequency. J Vasc Surg Venous Lymphat Disord. 2019 Jul;7(4):486–492. doi: 10.1016/j.jvsv.2018.11.013. [DOI] [PubMed] [Google Scholar]