Abstract
Perceived social support has been linked to lower rates of morbidity and mortality. However, more information is needed on the biological mechanisms potentially responsible for such links. The main aim of this paper was to conduct a meta-analytic review of the association between perceived social support and awake ambulatory blood pressure (ABP) which is linked to cardiovascular morbidity and mortality. The review identified 12 studies with a total of 3254 participants. The omnibus meta-analysis showed that higher perceived social support was not significantly related to lower ABP (Zr=−0.052, [−.11, .01]). In addition, there was evidence of significant bias across several indicators. Future research will be needed to explore the boundary conditions linking social support to ABP and its implications for theoretical models and intervention development.
Keywords: Social support, social networks, ambulatory blood pressure, meta-analysis
Perceived social support is often defined as the perception of available support from others and is one of the most robust psychosocial predictors of physical health outcomes (Berkman et al., 2000; Cohen, 2004; House et al., 1988). The meta-analysis by Holt-Lunstad and colleagues (2010) found a significant reduction in mortality rates for individuals who were higher in perceived support and more socially integrated. Importantly, these effect sizes were comparable if not larger than well-established lifestyle factors including obesity and physical activity (Holt-Lunstad et al., 2010).
Given that perceived social support is a reliable and potentially impactful predictor of health, an important question relates to the physiological mechanisms by which social support is related to disease (Uchino, 2006). Such information can provide evidence for the biological plausibility of the link between social support and disease, hence strengthening inferences (Broadhead et al., 1983). There is recent meta-analytic evidence linking social support to lower inflammation and potentially a stronger antibody response to vaccination (Uchino et al., 2018, 2020). Of particular interest might be other direct biological pathways relevant to cardiovascular diseases as they are the leading cause of death in most countries (WHO, 2020) and social support predicts cardiovascular disease outcomes (Lett et al., 2005). The main aim of this meta-analysis was thus to examine the link between perceived social support and ambulatory blood pressure (ABP, Pickering et al., 2006). That is, does perceived support impact ABP which might influence cardiovascular disease outcomes?
Social Support, Ambulatory Blood Pressure, and Health
There are a number of purported biological mechanisms linking social support to health (Holt-Lunstad, 2018). Blood pressure is one of the strongest predictors of stroke and cardiovascular risk (besides age) and hence an important potentially modifiable pathway which varies during everyday life (Banegas et al., 2018; Gaciong et al., 2013; Pickering et al., 2006). However, clinic blood pressure levels may not represent an individual’s daily blood pressure as they are susceptible to white coat/masked hypertension effects and are lower in ecological validity (Turner et al., 2015). As a result ABP levels represent blood pressure assessed in everyday life and appear more strongly linked to future cardiovascular risk compared to clinic blood pressure levels as shown by several reviews (Parati et al., 2014; Pickering et al., 2006).
There are conceptual reasons to expect perceived social support to be associated with lower ABP. Theoretical models highlight the role of social support in reducing stress appraisals and depressive symptoms, as well as increasing feelings of personal control and efficacy (Cohen, 1988; Thoits, 2011; Uchino, 2004). Many of these psychological processes have been linked to health outcomes, including ABP (Grewen et al., 2004; Landsbergis et al., 2013; Steptoe & Willemsen, 2004). Behavioral factors might also be operating as social support is associated with healthier behaviors and greater cooperation with medical regimens in chronic disease populations (DiMatteo, 2004; Yuan et al., 2011).
A number of studies have directly examined the link between social support and ABP. Consistent with the link between social support and cardiovascular risk, several studies have found social support to predict significantly lower ABP (Benotsch et al., 1997; Bowen et al., 2014; Piferi & Lawler, 2006). However, one of the earliest studies in this literature reported no significant association (Landsbergis et al., 1994), a pattern that has appeared in several other studies (Hawkley et al., 2005; Steptoe et al., 2000). Moreover, protective associations are sometimes evident only on one measure of ABP (i.e., either systolic or diastolic blood pressure, Benotsch et al., 1997; Gallo et al., 2004; Piferi & Lawler, 2006). This later point is important as resting SBP appears to have greater prognostic value compared to DBP in predicting cardiovascular risk (Benetos et al., 2003; Tin et al., 2002). The link between ambulatory SBP and cardiovascular risk also appears stronger compared to ambulatory DBP although more work is needed (see meta-analysis by Conen & Bamberg, 2008). Thus, a link between social support and ambulatory SBP might be more health-relevant compared to ambulatory DBP.
There appears to be only one prior systematic review examining the link between social support and measures of ABP. Fortman and Gallo (2013) focused on the link between social support and nocturnal blood pressure dipping which is assessed as the difference between awake and sleep ABP. They reported a protective association between social support (broadly defined) and ABP dipping with effect sizes ranging from medium to large (d’s between 0.41 to 2.01). To date, there does not appear to be a systematic review examining the link between social support and awake ABP that are also linked to cardiovascular risk (Pickering et al., 2006). As a result, this meta-analysis focused on awake ABP and excluded studies examining nocturnal blood pressure dipping unless they also reported relevant data on awake/daytime ABP.
Examining Potential Moderators
There are several important factors that need consideration as moderators (Kiecolt-Glaser et al., 2010). Given heterogeneity in the samples used, one important question relates to whether links are similar in studies utilizing relatively healthy individuals compared to studies focusing on populations with diagnosed cardiovascular disease such as hypertension. Models of social relationships and health highlight possible links to the development and/or course of health conditions. That is, can social support influence the development of disease or is it more influential once such chronic conditions arise and the need for support is high (Uchino, 2009a)? If the association between social support and ABP varies across sample types, then it may suggest stronger associations to particular phases of the disease process. A second important issue is related to whether associations vary by the type of assessment (SBP, DBP). As noted above, SBP appears to have greater prognostic value compared to DBP (Benetos et al., 2003; Conen & Bamberg, 2008). Although there are important conceptual differences in the operationalization of support (e.g., perceived, received, social integration, see Cohen, 1988), only three studies were found that examined measures other than perceived support (Piferi & Lawler, 2006; Rau et al., 2001; Vella et al., 2008) so these studies were excluded to focus on perceived support and ABP.1 The main aim of this review was thus to examine if perceived social support is linked to awake ABP which might explain epidemiological links to cardiovascular disease outcomes. There does not appear to be any meta-analytic review of this literature despite its importance in addressing potential biological mechanisms linking perceived support to cardiovascular disease risk. This meta-analysis thus documented this association and tested several important moderators of such links.
Method
Identification and Inclusion/Exclusion of Studies
The review protocol used in this meta-analysis is detailed below and followed the PRISMA guidelines (Page et al., 2021). A literature search was first conducted using the major databases of PsycInfo, Medline, and the Psychology and Behavioral Sciences Collection by crossing the exact keywords of “social support” with “ambulatory blood pressure.” More focused literature searches using the exact keywords social support and systolic ABP or diastolic ABP did not produce any new articles. The ancestry approach was also used which searched the reference list of eligible articles and review papers on the topic (i.e., Fortmann & Gallo, 2013). This search was run up to February of 2020 and identified 64 records, with 52 remaining after duplicates were removed (see Figure 1). Six records were excluded after abstract review as they were reviews or did not include measures of social support or ABP. Of the remaining 46 records, 34 were excluded for various methodological reasons, the most common being that no direct link between social support and ABP was examined given it was not a primary aim of the study. Of the 34 excluded studies, 12 appeared to have data on social support and ABP but did not report on the association. We contacted the first authors on these 12 papers and 1 author provided the needed information (6 no longer had access to the data and 5 did not respond). Articles were also not included if they did not include a direct measure of general perceived support (e.g., relationship quality, marital status) or focused exclusively on nocturnal dipping. This resulted in a final count of 12 articles for this meta-analysis.
Figure 1.
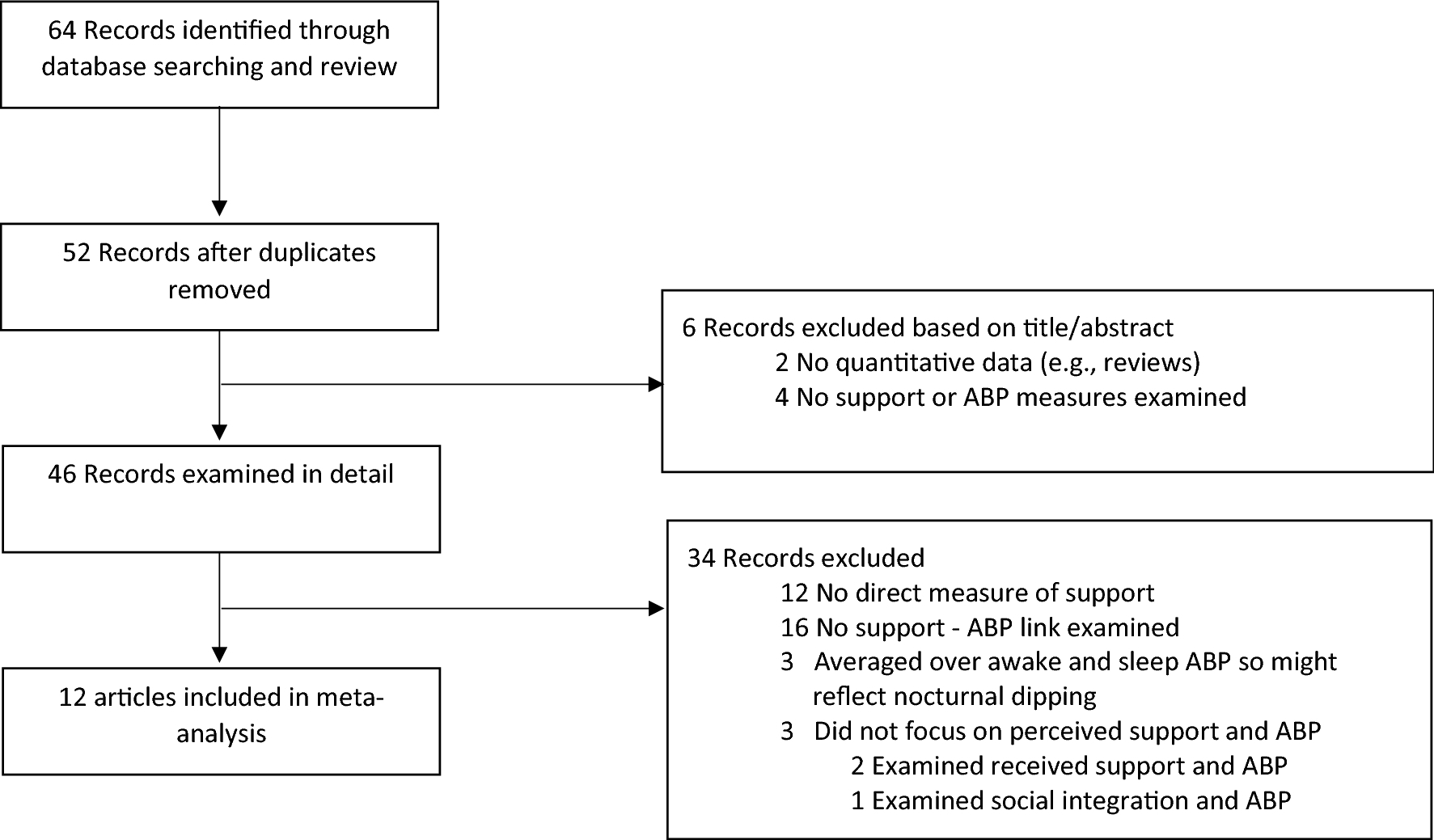
Meta-analytic flow chart describing selection of studies.
Analysis Plan and Data Extraction
Major details regarding studies (e.g., sample, population, outcomes) were first characterized and examined in tabular form. At least two authors verified the accuracy of the details listed in the table that was subsequently also used in the moderator analyses. The subsequent meta-analysis was performed using a commercially available software package (MetaWin V2.1, Rosenberg, Adams, & Gurevitch, 2000) that provided results regarding effect sizes, confidence intervals, tests of variability, moderation analyses, and indicators of bias. These analyses were based on a random effects model that assumes effect sizes vary across studies so that broader inferences can be made (Borenstein et al., 2009). To reduce the problem of nonindependence in omnibus analyses, when multiple assessments were reported (e.g., separate analyses for subgroups) they were first transformed to a common metric (i.e., z-scores), averaged, then entered into the meta-analysis. Correlation coefficients (r) were used as the common metric for data entry. When correlations were not presented, measures of effect size were converted to r values. Standardized regression weights were converted using the formula r=β+.05 λ, (Peterson & Brown, 2005). When p-values were the only source of data, they were transformed using the equation . based on the one-tailed z-score. Results reported as nonsignificant utilized a significance level of .50 (Rosenthal, 1984). Publication bias for the omnibus meta-analysis was examined at the outcome level by calculating a funnel plot, Kendall’s Tau, and the fail-safe n. Meta-regressions were performed to examine the type of population and outcome as moderators. Finally, certainty assessments were based on GRADE (Guyatt et al., 2008) and rated by two authors. As recommended for observational studies, the rating started at “low quality” and was adjusted based on the GRADE criteria.
Results
Overview of Studies
The main characteristics of these studies are shown in Table 1. In total, 3254 participants were included in the meta-analysis. Most of these studies utilized relatively healthy samples (67%), however, a number of studies used samples comprising both normotensive and hypertensive individuals (33%). Only 1 study explicitly mentioned that participants currently on antihypertensive medications were included in their sample (Karlin et al., 2003). Most of the other studies excluded individuals on cardiovascular medication or utilized relatively young samples. Finally, all 12 studies examined SBP while only 10 (83%) reported results for DBP.
Table 1.
Study details used in meta-analytic review.
| Study | N* | Sample | Support Measure | Main ABP Outcome | Effect Size Zr | Var(Zr) |
|---|---|---|---|---|---|---|
|
| ||||||
| (Landsbergis et al., 1994) | 262 men (84% white) | NC | WPS | Awake SBP, DBP | 0.000 | 0.004 |
| (Benotsch et al., 1997) | 24 women, 24 men | NC | GPS | Daytime SBP, DBP | −0.096 | 0.022 |
| (Steptoe et al., 2000) | 102 women, 60 men | NC | GPS | Daytime and evening SBP, DBP | 0.000 | 0.006 |
| (Steffen et al., 2001) | 72 women, 83 men (50% African American, 50% White) | NC | GPS | Awake SBP, DBP | −0.147 | 0.007 |
| (Karlin et al., 2003) | 34 women, 36 men (53% African American, 19% Latino, 10% Asian, 7% White, 1% Native American, 3% mixed races, 7% missing | Both | WPS | Workday SBP, DBP | −0.090 | 0.015 |
| (Hawkley et al., 2003) | 67 women, 68 men (83% white, 7% African American, 7% Asian or Pacific Islander, 3% other or undeclared) | NC | GPS | Daytime and evening SBP, DBP | 0.000 | 0.008 |
| (Gallo et al., 2004) | 108 women (86% White, 10% African American, 2% Latina, 1% Asian, 1% unspecified) | NC | GPS | Workday SBP, DBP | −0.177 | 0.010 |
| (Cooper et al., 2009) | 81 women, 75 men (39% African American, 61% White) | Both | GPS | Awake SBP, DBP | −0.015 | 0.007 |
| (Gallagher & Whiteley, 2012) | 53 women, 12 men (98% white) | NC | GPS | Daytime SBP | −0.412 | 0.016 |
| (Bowen et al., 2013) | 94 women, 94 men (83% white) | NC | GPS | Daytime and evening SBP, DBP | −0.121 | 0.005 |
| (Edmondson et al., 2015) | 507 women, 351 men (28% ethnic/racial minorities) | Both | GPS | Awake SBP, DBP | 0.000 | 0.001 |
| (Sanchez-Martínez et al., 2016) | 515 women, 532 men | Both | GPS | Daytime SBP | 0.007 | 0.001 |
Race/ethnicity is not tabled when not reported.
Note: NC=nonclinical, C=clinical, GPS=General perceived support, WPS=Work perceived support, SBP=systolic blood pressure, DBP=diastolic blood pressure, Zr=Fisher’s transformation of r, var(Zr)=variance of Zr.
Overall Link Between Social Support and ABP
Across all 12 studies, higher social support was not significantly related to lower ABP (Zr=−.052, 95% CI [−.11, .01], p>.05). The confidence interval did indicate that the bulk of plausible values were small, negative associations. Effect sizes ranged from Zr=−.41 to Zr=+.007 and the test of heterogeneity was not significant (Q(11)=12.6, p=.32). The fail-safe n of 16.5 indicated possible publication bias as it was well below the traditional 5k +10 recommendation (above 70 studies for this review). To further examine the possibility of bias, a funnel plot of effect sizes as a function of sample size was plotted. It should show a roughly symmetric funnel plot that varies with increasing samples sizes (Rosenberg et al., 2000). As shown in Figure 2, this pattern was not obtained again suggesting bias in the results. A direct test of the association between effect sizes and sample sizes revealed a significant link (Kendall’s Tau=.61, p=.006) consistent with the other measures of bias. Based on these data, two authors provided a rating of the certainty of evidence based on the GRADE criteria (Guyatt et al., 2008). The meta-analysis was based on observational studies so the rating started on low quality and was adjusted based on the available evidence (e.g., bias, precision, magnitude of effect). Due to the small effect size, inconsistency of the effect sizes across studies, and evidence of bias, both authors agreed that the final rating was very low quality which means that the true effect size is likely to be markedly different from the estimated effect (Guyatt et al., 2008). Thus, the evidence for an association between social support and lower ABP is weak with the possibility that no association exists.
Figure 2.
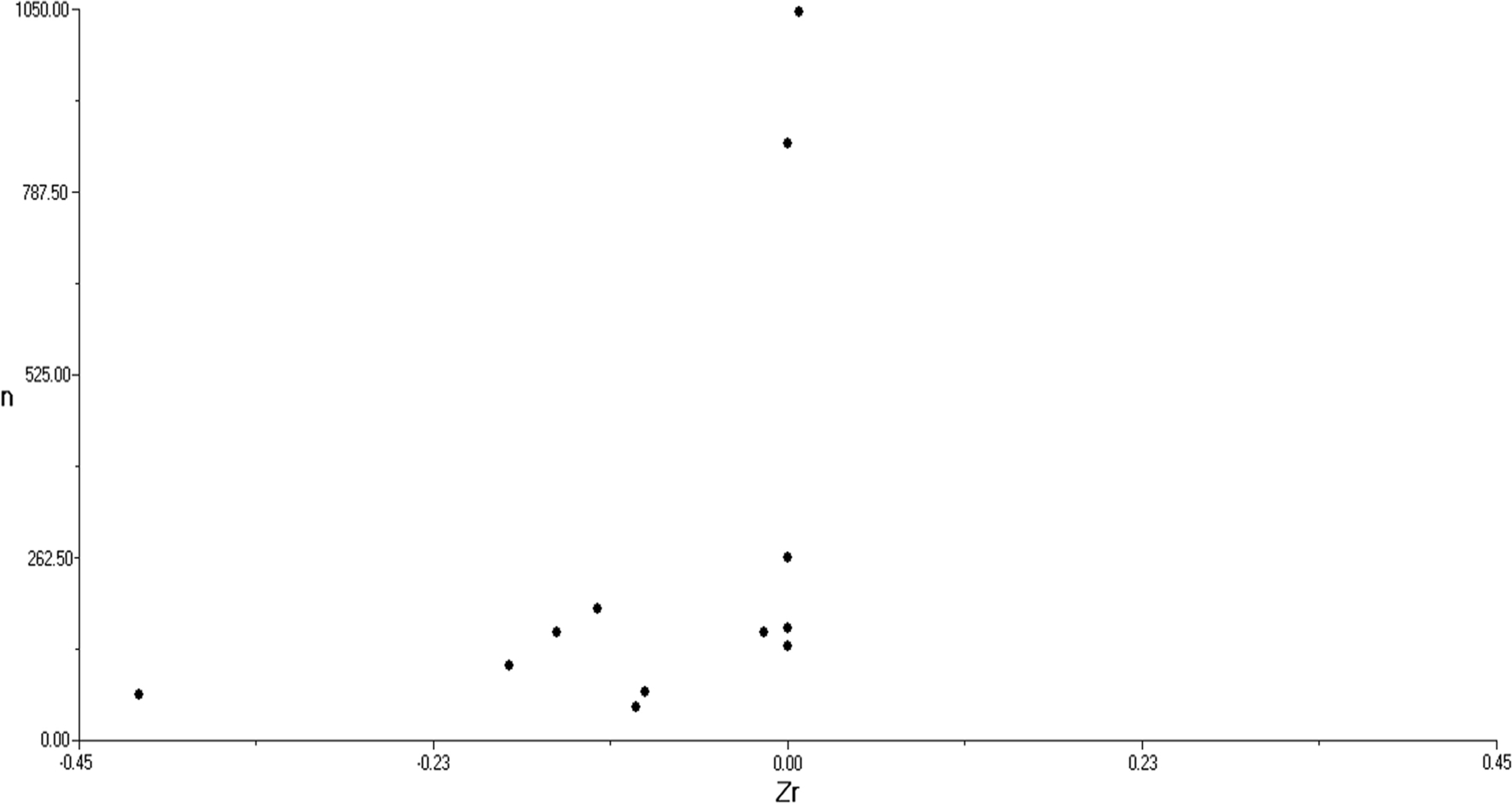
Funnel plot examining effect sizes as a function of sample size.
Exploratory Moderator Analyses
The above analyses suggest uncertainty in the association between social support and ABP. Although the heterogeneity test was not significant, exploratory analyses were conducted given that moderators are especially important when there are inconsistent links and might have implications for future research (Baron & Kenny, 1986). It is possible that effect sizes might differ based on whether the sample has a chronic condition, which is important to understand the potential disease stage possibly linked to social support. Eight studies used a relatively healthy sample and produced the largest significant effect size (Zr=−.09, 95% CI [−.17, −.01]) compared to the 4 studies that had a mix of healthy and clinical populations (Zr=−.004, 95% CI [−.10, .10]). This difference between these effect sizes, however, only approached significance (Q(1)=3.44, p=.06), see Table 2). The type of outcome was also examined given the relatively stronger prognostic risk associated with SBP compared to DBP (Conen & Bamberg, 2008). In these analyses, the effect size for social support appeared comparable for ambulatory SBP (Zr=−.05, 95% CI [−.10, −.003]) and ambulatory DBP (Zr=−.03, 95% CI [−.09, .03]). The difference between these outcomes was not significant (Q(1)=.37, p=.54).
Table 2.
Main results of meta-analysis.
| Moderator | k | Effect Size (Zr) | 95% CI |
|---|---|---|---|
|
| |||
| Sample | |||
| Healthy | 8 | −0.09 | −.17, −.01 |
| Combined healthy and clinical | 4 | −0.004 | −.10, .10 |
| Outcome | |||
| SBP | 12 | −.05 | −.10, −.003 |
| DBP | 10 | −.03 | −.09, .03 |
| Behavioral Controls | |||
| No | 8 | −.04 | −.10, .03 |
| Yes | 4 | −.10 | −.26, .07 |
Finally, although not predicted a priori, another potentially important moderator that emerged during the examination of individual studies was whether studies controlled for within-participant behavioral variables that influence ABP such as posture and activity level (Kamarck et al., 1998). Many studies treat these variables as important sources of error to be statistically controlled and 4 out of 12 studies (33%) did so in the current review. Moderator analyses showed that studies which statistically controlled for such variables had somewhat larger effect sizes (Zr=−0.10, 95% CI [−.26, .07]) compared to studies that did not (Zr=−0.04, 95% CI [−.10, .03]); however, this difference was not statistically significant (Q(1)=1.03, p=.31).
Discussion
The main goal of this review was to examine the meta-analytic link between perceived social support and awake ABP during daily life. Such links would suggest the importance of ABP as a potential mechanism linking social support to cardiovascular risk. Analyses suggested that the effect size was in the predicted direction but there was consistent evidence of bias in published studies. Exploratory moderator analyses did not reveal any significant differences but suggested that effect sizes were larger when examining healthy samples and statistically controlling for within-participant behavioral factors such as posture and activity level. Although the moderator analyses were clearly exploratory, it may be important to guide future research as the current analysis suggests that the evidence for a main effect between social support and overall ABP is of very low quality (certainty of evidence) and includes the possibility that no association exists.
There are several factors that warrant discussion given the present set of findings. It is possible that other indices of ABP might show stronger links to social support. The focus of the current meta-analytic review was on awake ABP which is a predictor of cardiovascular disease risk (Pickering et al., 2006). However, there are other indices of ambulatory blood pressure which are important to examine. One such outcome is nocturnal blood pressure dipping given our meta-analysis excluded such studies (Yano & Kario, 2012). A systematic review based on 11 studies found consistent links between low social support and a non-dipping profile which is related to cardiovascular risk (Fortmann & Gallo, 2013). Future research should also explore ABP variability which is emerging as an additional risk factor (Mena et al., 2017).
If we assume that the effect size is small or zero, moderators become an important consideration as effect sizes might differ depending on other factors. In the current review, we focused a priori on type of population (i.e., healthy, cardiovascular diagnosis) and outcome (i.e., SBP or DBP). The effect sizes in moderation analyses were non-significantly larger for healthy populations and comparable for SBP and DBP as outcomes. Future work will be needed to test if these potential differences emerge as more studies are conducted. In addition, perceived support is only one important operationalization of social relationships that has been linked to health. In this meta-analysis, 10 studies focused on general perceived support, whereas 2 studies focused on work-related perceived support. Given the small number of studies examining work-related support, future work will be needed to examine if more specific sources of support show stronger links to ABP. It is also important to note that complex measures of social integration appear to be more strongly linked to mortality (Holt-Lunstad et al., 2010) and received support is separable from perceived support and appears more contextual (e.g., responsiveness, Selcuk & Ong, 2013). However, there is currently little research examining associations between social integration/received support and ABP. Of the two studies on received support and ABP one found a negative association and the other a positive association (Piferi & Lawler, 2006; Vella et al., 2008).2 The only published study for social integration found it was associated with significantly lower ABP (Rau et al., 2001). Future work that examines other conceptual moderators (e.g., stress-buffering model, Cohen & Wills, 1985; but see Barrera, 1986) might also result in larger effect sizes between social support and ABP.
Another exploratory moderator was whether studies statistically controlled for behavioral states (typically within-participants) that are related to ABP including posture and activity level. Of the studies in this review, 33% statistically controlled for such factors. The assumption of these studies is that such factors add measurement error to ABP assessments given the myriad of factors that might influence blood pressure in the daily environment (Kamarck et al., 1998). Although the contrast was nonsignificant, these studies appeared to be associated with slightly larger effect sizes compared to those that did not. Of course, it is difficult to make strong inferences given that these studies might differ on other characteristics, and it is unknown if study results might have changed if such controls were utilized. Given the correlational nature of existing ABP studies in the natural environment there is justification for use of these controls. However, future research should consider reporting results when such variables are controlled for and when they are not.
Based on the GRADE criteria (Guyatt et al., 2008), certainty judgements suggested that the evidence in this meta-analysis was of very low quality which means that the true effect size is likely to be markedly different from the estimated effect. Future research can improve inferences be including more powerful study designs such as prospective studies that examine changes in both support and ABP over time. It is also possible to conduct randomized control trials (see Lindsay et al., 2019) which seek to modify social support and examine its impact on ABP. In addition, the publication of potential null and positive associations between social support and ABP would reduce bias in this literature and lead to stronger inferences.
There are several limitations of the current review that warrant discussion. First, as noted above the number of studies and associated sample sizes in most cases were not large so future work will be needed to build on these findings. Second, these results are mostly limited to general perceptions of support. Such measures tend to have stronger links to health compared to measures of received support which appears more sensitive to the stressor context (Holt-Lunstad et al., 2010; Uchino, 2009b). However, complex measures of social integration appear to show larger effect sizes on mortality (Holt-Lunstad et al., 2010) so future studies should examine such measures alongside measures of perceived/received support. Relatedly, specific dimensions of perceived support might be more strongly related to ABP so studies that conceptualize perceived support as a multidimensional construct are needed (Bowen et al., 2013). Finally, methodological characteristics of studies besides the inclusion of behavioral covariates (e.g., ABP protocol) might also be important. Overall, this review raised questions about the current strength of a main effect link between social support and overall ABP, a concern that was amplified by the likely presence of bias in published studies. Future work focusing on conceptual (e.g., operationalization of relationships, stress-buffering) and methodological (i.e., within-participant behavioral covariates, type of blood pressure assessment) issues will allow for a more precise understanding of such links and potential boundary conditions that can guide much needed theoretical and intervention work.
Acknowledgments
This research was generously supported by grant number R01HL137606 from the National Heart, Lung, and Blood Institute (PI: Bert N. Uchino).
Footnotes
Inclusion of these 3 studies did not change the conclusions of this meta-analytic review.
We thank Dr. Vella who provided the data for this review (Vella et al., 2008).
The authors have full control of all primary data and agree to allow the journal to review their data if requested.
Contributor Information
Bert N. Uchino, Department of Psychology and Health Psychology Program, University of Utah
Brian R.W. Baucom, Department of Psychology and Health Psychology Program, University of Utah
Joshua Landvatter, Department of Psychology and Health Psychology Program, University of Utah.
Robert G. Kent de Grey, Department of Psychology and Health Psychology Program, University of Utah.
Tracey Tacana, Department of Psychology and Health Psychology Program, University of Utah.
Melissa Flores, Department of Psychology, University of Arizona.
John M. Ruiz, Department of Psychology, University of Arizona
References
- Banegas JR, Ruilope LM, De La Sierra A, Vinyoles E, Gorostidi M, De La Cruz JJ, Ruiz-Hurtado G, Segura J, Rodríguez-Artalejo F, & Williams B (2018). Relationship between clinic and ambulatory blood-pressure measurements and mortality. New England Journal of Medicine, 378(16), 1509–1520. 10.1056/NEJMoa1712231 [DOI] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. [DOI] [PubMed] [Google Scholar]
- Barrera M (1986). Distinctions Between Social Support Concepets, Measures, and Models. American Journal of Community Psychology, 14(4), 413–445. [Google Scholar]
- Benetos A, Thomas F, Bean K, Gautier S, Smulyan H, & Guize L (2003). Prognostic value of systolic and diastolic blood pressure in treated hypertensive men: Clarification [3]. Archives of Internal Medicine, 163(1), 121. 10.1001/archinte.163.1.121 [DOI] [PubMed] [Google Scholar]
- Benotsch EG, Christensen AJ, & McKelvey L (1997). hostility, social support, and ambulatory cardiovascular activity. Journal of Behavioral Medicine, 20(2), 163–176. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, & Seeman TE (2000). From social integration to health: Durkheim in the new millennium. Social Science & Medicine, 51(6), 843–857. 10.1016/S0277-9536(00)00065-4 [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JP ., & Rothstein HR (2009). Introduction to Meta-Analysis. John Wiley & Sons, Ltd. [Google Scholar]
- Bowen KS, Birmingham W, Uchino BN, Carlisle M, Smith TW, & Light KC (2013). Specific dimensions of perceived support and ambulatory blood pressure: Which support functions appear most beneficial and for whom? International Journal of Psychophysiology, 88(3), 317–324. 10.1016/j.ijpsycho.2012.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen KS, Uchino BN, Birmingham W, Carlisle M, Smith TW, & Light KC (2014). The stress-buffering effects of functional social support on ambulatory blood pressure. Health Psychology, 33(11). 10.1037/hea0000005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadhead WE, Kaplan B ., James SA, Wagner EH, Schoenbach VJ, R. G, Heyden S, Tibblin G, & Gehlbach SH (1983). The epidemiologic evidence for a relationship between social support and health. American Journal of Epidemiology, 117(5), 521–537. 10.1093/OXFORDJOURNALS.AJE.A113575 [DOI] [PubMed] [Google Scholar]
- Cohen S (1988). Psychosocial models of the role of social support in the etiology of physical disease. Health Psychology, 7(3), 269–297. 10.1037/0278-6133.7.3.269 [DOI] [PubMed] [Google Scholar]
- Cohen S (2004). Social relationships and health. The American Psychologist, 59(8), 676–684. 10.1037/0003-066X.59.8.676 [DOI] [PubMed] [Google Scholar]
- Cohen S, & Wills TA (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357. 10.1037/0033-2909.98.2.310 [DOI] [PubMed] [Google Scholar]
- Conen D, & Bamberg F (2008). Noninvasive 24-h ambulatory blood pressure and cardiovascular disease: A systematic review and meta-analysis. Journal of Hypertension, 26(7), 1290–1299. 10.1097/HJH.0b013e3282f97854 [DOI] [PubMed] [Google Scholar]
- Cooper DC, Ziegler MG, Nelesen RA, & Dimsdale JE (2009). Racial differences in the impact of social support on nocturnal blood pressure. Psychosomatic Medicine, 71(5), 524–531. 10.1097/PSY.0b013e31819e3a93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMatteo MR (2004). Social support and patient adherence to medical treatment: a meta-analysis. Health Psychology : Official Journal of the Division of Health Psychology, American Psychological Association, 23(2), 207–218. 10.1037/0278-6133.23.2.207 [DOI] [PubMed] [Google Scholar]
- Edmondson D, Arndt J, Alcántara C, Chaplin W, & Schwartz JE (2015). Self-Esteem and the Acute Effect of Anxiety on Ambulatory Blood Pressure. Psychosomatic Medicine, 77(7), 833–841. 10.1097/PSY.0000000000000219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortmann AL, & Gallo LC (2013). Social support and nocturnal blood pressure dipping: A systematic review. American Journal of Hypertension, 26(3), 302–310. 10.1093/ajh/hps041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaciong Z, Siński M, & Lewandowski J (2013). Blood pressure control and primary prevention of stroke: Summary of the recent clinical trial data and meta-analyses. Current Hypertension Reports, 15(6), 559–574. 10.1007/s11906-013-0401-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher S, & Whiteley J (2012). Social support is associated with blood pressure responses in parents caring for children with developmental disabilities. Research in Developmental Disabilities, 33(6), 2099–2105. 10.1016/j.ridd.2012.06.007 [DOI] [PubMed] [Google Scholar]
- Gallo LC, Bogart LM, Vranceanu AM, & Walt LC (2004). Job characteristics, occupational status, and ambulatory cardiovascular activity in women. Annals of Behavioral Medicine, 28(1), 62–73. 10.1207/s15324796abm2801_8 [DOI] [PubMed] [Google Scholar]
- Grewen KM, Girdler SS, Hinderliter A, & Light KC (2004). Depressive symptoms are related to higher ambulatory blood pressure in people with a family history of hypertension. Psychosomatic Medicine, 66(1), 9–16. 10.1097/01.PSY.0000106881.60228.16 [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, & Schünemann HJ (2008). GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. Bmj, 336(7650), 924–926. 10.1136/bmj.39489.470347.ad [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Berntson GG, Engeland CG, Marucha PT, Masi CM, & Cacioppo JT (2005). Stress, Aging, and Resilience: Can Accrued Wear and Tear Be Slowed? Canadian Psychology/Psychologie Canadienne, 46(3), 115–125. 10.1037/h0087015 [DOI] [Google Scholar]
- Hawkley LC, Burleson MH, Berntson GG, & Cacioppo JT (2003). Loneliness in Everyday Life: Cardiovascular Activity, Psychosocial Context, and Health Behaviors. Journal of Personality and Social Psychology, 85(1), 105–120. 10.1037/0022-3514.85.1.105 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J (2018). Why Social Relationships Are Important for Physical Health: A Systems Approach to Understanding and Modifying Risk and Protection. Annual Review of Psychology, 69(1), 437–458. 10.1146/annurev-psych-122216-011902 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, & Layton JB (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Medicine, 7(7). 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS, Landis KR, & Umberson D (1988). Social relationships and health. Science (New York, N.Y.), 241(4865), 540–545. 10.1126/science.3399889 [DOI] [PubMed] [Google Scholar]
- Kamarck TW, Shiffman SM, Smithline L, Goodie JL, Paty J. a, Gnys M, & Jong JY (1998). Effects of task strain, social conflict, and emotional activation on ambulatory cardiovascular activity: daily life consequences of recurring stress in a multiethnic adult sample. Health Psychology : Official Journal of the Division of Health Psychology, American Psychological Association, 17(1), 17–29. 10.1037/0278-6133.17.1.17 [DOI] [PubMed] [Google Scholar]
- Karlin WA, Brondolo E, & Schwartz J (2003). Workplace social support and ambulatory cardiovascular activity in New York City Traffic Agents. Psychosomatic Medicine, 65(2), 167–176. 10.1097/01.PSY.0000033122.09203.A3 [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Gouin JP, & Hantsoo L (2010). Close relationships, inflammation, and health. Neuroscience and Biobehavioral Reviews, 35(1), 33–38. 10.1016/j.neubiorev.2009.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landsbergis PA, Dobson M, Koutsouras G, & Schnall P (2013). Job Strain and Ambulatory Blood Pressure: A Meta-Analysis and Systematic Review. American Journal of Public Health, 103(3), e61. 10.2105/AJPH.2012.301153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landsbergis PA, Schnall PL, Warren K, Pickering TG, & Schwartz JE (1994). Association between ambulatory blood pressure and alternative formulations of job strain. Scandinavian Journal of Work, Environment and Health, 20(5), 349–363. 10.5271/sjweh.1386 [DOI] [PubMed] [Google Scholar]
- Lett HS, Blumenthal JA, Babyak MA, Strauman TJ, Robins C, & Sherwood A (2005). Social support and coronary heart disease: epidemiologic evidence and implications for treatment. Psychosom.Med, 67(1534–7796 (Electronic)), 869–878. 10.1097/01.psy.0000188393.73571.0a [DOI] [PubMed] [Google Scholar]
- Lindsay EK, Young S, Brown KW, Smyth JM, & David Creswell J (2019). Mindfulness training reduces loneliness and increases social contact in a randomized controlled trial. Proceedings of the National Academy of Sciences of the United States of America, 116(9), 3488–3493. 10.1073/pnas.1813588116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mena LJ, Felix VG, Melgarejo JD, & Maestre GE (2017). 24-Hour blood pressure variability assessed by average real variability: A systematic review and meta-analysis. Journal of the American Heart Association, 6(10), 1–10. 10.1161/JAHA.117.006895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, … Moher D (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Medicine, 18(3), 1–15. 10.1371/JOURNAL.PMED.1003583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, Clement D, De La Sierra A, De Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, … Zhang Y (2014). European society of hypertension practice guidelines for ambulatory blood pressure monitoring. Journal of Hypertension, 32(7), 1359–1366. 10.1097/HJH.0000000000000221 [DOI] [PubMed] [Google Scholar]
- Peterson RA, & Brown SP (2005). On the use of beta coefficients in meta-analysis. The Journal of Applied Psychology, 90(1), 175–181. 10.1037/0021-9010.90.1.175 [DOI] [PubMed] [Google Scholar]
- Pickering TG, Shimbo D, & Haas D (2006). Ambulatory Blood-Pressure Monitoring. New England Journal of Medicine, 354(22), 2368–2374. 10.1056/NEJMra060433 [DOI] [PubMed] [Google Scholar]
- Piferi RL, & Lawler KA (2006). Social support and ambulatory blood pressure: An examination of both receiving and giving. International Journal of Psychophysiology, 62(2), 328–336. 10.1016/j.ijpsycho.2006.06.002 [DOI] [PubMed] [Google Scholar]
- Rau R, Georgiades A, Fredrikson M, Lemne C, & de Faire U (2001). Psychosocial work characteristics and perceived control in relation to cardiovascular rewind at night. Journal of Occupational Health Psychology, 6(3), 171–181. 10.1037/1076-8998.6.3.171 [DOI] [PubMed] [Google Scholar]
- Rosenberg MS, Adams DC, & Gurevitch J (2000). MetaWin: Statistial software for meta-analysis. Sinauer Associates. [Google Scholar]
- Rosenthal R (1984). Meta-analytic procedures for social research. Sage. [Google Scholar]
- Sanchez-Martínez M, López-García E, Guallar-Castillón P, Cruz JJ, Orozco E, García-Esquinas E, Rodríguez-Artalejo F, & Banegas JR (2016). Social support and ambulatory blood pressure in older people. Journal of Hypertension, 34(10), 2045–2052. 10.1097/HJH.0000000000001036 [DOI] [PubMed] [Google Scholar]
- Selcuk E, & Ong AD (2013). Perceived partner responsiveness moderates the association between received emotional support and all-cause mortality. Health Psychology, 32(2), 231–235. 10.1037/a0028276 [DOI] [PubMed] [Google Scholar]
- Steffen PR, Hinderliter AL, Blumenthal JA, & Sherwood A (2001). Religious coping, ethnicity, and ambulatory blood pressure. Psychosomatic Medicine, 63(4), 523–530. 10.1097/00006842-200107000-00002 [DOI] [PubMed] [Google Scholar]
- Steptoe A, Lundwall K, & Cropley M (2000). Gender, family structure and cardiovascular activity during the working day and evening. Social Science and Medicine, 50(4), 531–539. 10.1016/S0277-9536(99)00324-X [DOI] [PubMed] [Google Scholar]
- Steptoe A, & Willemsen G (2004). The influence of low job control on ambulatory blood pressure and perceived stress over the working day in men and women from the Whitehall II cohort. Journal of Hypertension, 22(5), 915–920. 10.1097/00004872-200405000-00012 [DOI] [PubMed] [Google Scholar]
- Thoits PA (2011). Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 52(2), 145–161. 10.1177/0022146510395592 [DOI] [PubMed] [Google Scholar]
- Tin LL, Beevers DG, & Lip GYH (2002). Systolic vs diastolic blood pressure and the burden of hypertension. Journal of Human Hypertension, 16(3), 147–150. 10.1038/sj.jhh.1001373 [DOI] [PubMed] [Google Scholar]
- Turner JR, Viera AJ, & Shimbo D (2015). Ambulatory blood pressure monitoring in clinical practice: A review. American Journal of Medicine, 128(1), 14–20. 10.1016/j.amjmed.2014.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino BN (2004). Social support and physical health: Understanding the health consequences of relationships. In Social support and physical health: Understanding the health consequences of relationships. Yale University Press. 10.1093/aje/kwi036 [DOI] [Google Scholar]
- Uchino BN (2006). Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine, 29(4), 377–387. 10.1007/s10865-006-9056-5 [DOI] [PubMed] [Google Scholar]
- Uchino BN (2009a). Understanding the Links Between Social Support and Physical Health: A Life-Span Perspective With Emphasis on the Separability of Perceived and Received Support. Perspectives on Psychological Science, 4(3), 236–255. 10.1111/j.1745-6924.2009.01122.x [DOI] [PubMed] [Google Scholar]
- Uchino BN (2009b). What a lifespan approach might tell us about why distinct measures of social support have differential links to physical health. Journal of Social and Personal Relationships, 26(1), 53–62. 10.1177/0265407509105521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino BN, Landvatter J, Zee K, & Bolger N (2020). Social Support and Antibody Responses to Vaccination: A Meta-Analysis. Annals of Behavioral Medicine, 54(8), 567–574. 10.1093/abm/kaaa029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino BN, Trettevik R, Grey R. G. K. De, Cronan S, Hogan J, & Baucom BRW (2018). Social support, social integration, and inflammatory cytokines: A meta-analysis. Health Psychology, 37(5), 462–471. [DOI] [PubMed] [Google Scholar]
- Vella EJ, Kamarck TW, & Shiffman S (2008). Hostility Moderates the Effects of Social Support and Intimacy on Blood Pressure in Daily Social Interactions. Health Psychology, 27(2 SUPPL. 2), 155–162. 10.1037/0278-6133.27.2(Suppl.).S155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. (2020). The top 10 causes of death. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
- Yano Y, & Kario K (2012). Nocturnal blood pressure and cardiovascular disease: A review of recent advances. Hypertension Research, 35(7), 695–701. 10.1038/hr.2012.26 [DOI] [PubMed] [Google Scholar]
- Yuan SC, Weng SC, Chou MC, Tang YJ, Lee SH, Chen DY, Chuang YW, Yu CH, & Kuo HW (2011). How family support affects physical activity (PA) among middle-aged and elderly people before and after they suffer from chronic diseases. Archives of Gerontology and Geriatrics, 53(3), 274–277. 10.1016/j.archger.2010.11.029 [DOI] [PubMed] [Google Scholar]


