Abstract
Background
The global public health burden of obesity has increased with socio-economic development. The Korean Society for the Study of Obesity released the 2021 Obesity Fact Sheet to address trends in obesity prevalence and comorbid conditions by different age groups.
Methods
Individuals ≥20 years old who underwent a health checkup provided by the Korean National Health Insurance Service between 2009 and 2019 were included. The prevalence of obesity and abdominal obesity was standardized by age and sex based on the 2010 population and housing census. The incidence of obesity-related comorbidities was tracked from 2009 to 2019, and the incidence per 1,000 person-years was calculated using Poisson regression adjusted for age and sex.
Results
Obesity and abdominal obesity prevalence has increased for the entire population over the past 11 years. Obesity prevalence has risen rapidly in individuals in their 20s and 80s compared with other age groups. Additionally, class III obesity prevalence in both men and women has significantly increased by nearly threefold. The relative risk of developing type 2 diabetes, myocardial infarction, ischemic stroke, and cancers in people with obesity or abdominal obesity is greater than in people without obesity or abdominal obesity. The relative risk was higher in young and middle-aged individuals than in the older population.
Conclusion
The findings based on the 2021 Obesity Fact Sheet suggest the need to better understand obesity characteristics according to age and sex and to establish individualized treatment strategies.
Keywords: Obesity, Obesity class, Prevalence, Fact sheet, National Health Insurance Service
INTRODUCTION
Obesity prevalence has increased substantially worldwide and is being labeled a pandemic. In most countries, obesity-associated disease burden continues to increase in public health and socio-economic terms.1 The recent obesity epidemic is being called a “global syndemic,” along with malnutrition and climate change, encompassing the most important health problems that humans and environment face.2 Increases in obesity are major metabolic risk factors that contribute to increasing risk of non-communicable diseases (NCDs), including cardiovascular disease, cancer, chronic respiratory disease, and diabetes.3-5 Furthermore, in recent years, obesity has been recognized as a predictor of poor prognosis in patients with coronavirus disease 2019 (COVID-19).6 In response to these public health challenges, tackling overweight and obesity with appropriate strategies is a key challenge in reducing disease burden and premature mortality caused by NCDs in every country. Therefore, better surveillance data on obesity and risk of obesity-related disease are essential for research and healthcare policy.
Since 2015, the Korean Society for the Study of Obesity (KSSO) has annually updated the Obesity Fact Sheets, based on representative data from the National Health Insurance Service (NHIS), to report the national obesity status and its impacts. In Korea, up to 40% of the population is obese, defining obesity as a body mass index (BMI) of ≥25 kg/m2, and obesity and abdominal obesity prevalence has increased dramatically over decades.7 Additionally, compared with Western populations, Koreans are considerably leaner, but more likely to develop obesity-related diseases for a given BMI level.8
The 2021 Obesity Fact Sheet presents trends in obesity and abdominal obesity prevalence among Korean adults from 2009 to 2019 according to age and sex, and risk of major comorbidities, such as type 2 diabetes mellitus (T2DM), cardiovascular diseases, and cancers. This study sought to analyze differences in obesity prevalence and comorbidity risk by different age groups to understand age-specific differences and to develop targeted interventions for those subgroups. Additionally, this fact sheet is intended to improve obesity care and provide a valuable resource for establishing national health policies in Korea.
METHODS
Data resource and study participants
This retrospective study used the National Health Checkup Database provided by the Korean NHIS. The Korean NHIS is an insurer that manages the National Health Insurance program, which contains medical information covering approximately 97% of Koreans. The National Health Insurance Corporation (NHIC) provides a biannual health checkup program that includes anthropometric measurements, blood tests, and health surveys, including general health behaviors and disease diagnosis according to the International Classification of Disease, 10th revision (ICD-10). Detailed information from the NHIS database has been described elsewhere.9,10 Information on individuals aged ≥20 years who had undergone at least one health checkup provided by the Korean NHIC between January 1, 2009, and December 31, 2019, were assessed. The study protocol was approved by the Institutional Review Board of the Kangbuk Samsung Hospital (No. KBSMC 2020-05-002).
Definitions of obesity and abdominal obesity
Participant body weight (kg), height (cm), and waist circumference (WC; cm) were measured by trained examiners. BMI (kg/m2) was calculated by dividing weight (kg) by height squared (m2). We defined obesity as BMI ≥25 kg/m2 according to the Asia-Pacific criteria of the World Health Organization guidelines. Obesity classes were defined using the 2020 KSSO Obesity Treatment Guideline as follows, class I obesity, BMI 25.0–29.9 kg/m2; class II obesity, 30.0–34.9 kg/m2; class III obesity, ≥35.0 kg/m2. Abdominal obesity was defined as a WC ≥90 cm in men and ≥85 cm in women according to the KSSO definition.11
Definition of comorbidities
T2DM was defined as a fasting plasma glucose ≥126 mg/dL or at least one claim per year for an antidiabetic medication prescription under ICD-10 codes E11–E14. Myocardial infarction was defined according to ICD-10 code I20–I21 and admission history due to myocardial infarction. Ischemic stroke was defined as an event-related hospitalization under ICD-10 code I63 or I64 and claims for brain magnetic resonance imaging or brain computed tomography. Cancer was defined as ICD-10 codes C16 for stomach cancer, C18–C20 for colorectal cancer, C22 for liver cancer, C73 for thyroid cancer, C34 for lung cancer, C61 for prostate cancer, and C50 for breast cancer.
Statistical analysis
Prevalence was presented using NHIS data with values standardized for age and sex based on the 2010 population and housing census from Statistics Korea. The incidence of obesity-related comorbidities was tracked from 2009 to 2019, and the incidence per 1,000 person-years was calculated using a Poisson regression model adjusted for age and sex. Statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Prevalence of obesity and abdominal obesity from 2009 to 2019
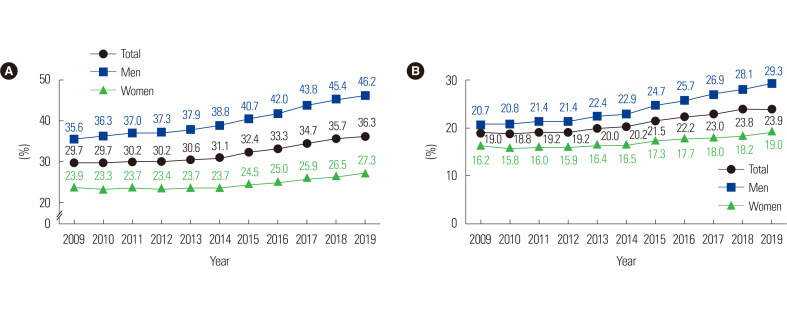
Obesity prevalence has steadily increased over the past 11 years between 2009 and 2019 for the total population; from 29.7% in 2009 to 36.3% in 2019 (Fig. 1A). Obesity prevalence has increased significantly in men from 35.6% in 2009 to 46.2% in 2019, and 23.9% in 2009 to 27.3% in 2019 in women. The prevalence of abdominal obesity increased between 2009 and 2019 in both sexes, but most prominently in men; 19.0% vs. 23.9% in the total population, 20.7% vs. 29.3% in men, and 16.2% vs. 19.0% in women (Fig. 1B).
Figure 1.
Prevalence of obesity (A) and abdominal obesity (B) over the last 11 years between 2009 and 2019. The grey, blue, and green lines represent the prevalence of total population, men, and women, respectively.
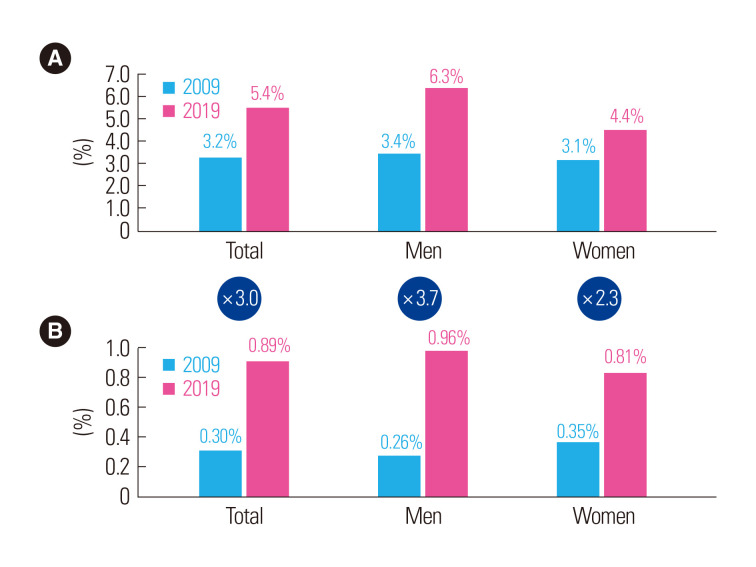
The prevalence of obesity in all classes has increased for the total population over the past 11 years. The prevalence of class II obesity in the total population, men, and women was 3.2%, 3.4%, and 3.1% in 2009 and 5.4%, 6.3%, and 4.4% in 2019, respectively (Fig. 2A). The prevalence of class III obesity has increased by nearly threefold over the past 11 years from 0.30% in 2009 to 0.89% in 2019 in the total population: 3.7 times in men (0.26% in 2009 to 0.96% in 2019) and 2.3 times in women (0.35% in 2009 to 0.81% in 2019) (Fig. 2B).
Figure 2.
Prevalence of class II obesity (A) and class III obesity (B) in 2009 and in 2019. The circles represents the fold increase in obesity prevalence in 2019 compared to in 2009.
Age-specific prevalence of obesity and abdominal obesity from 2009 to 2019
Over the past 11 years, obesity prevalence showed an increasing trend in all age groups (Supplementary Fig. 1). In 2019, the obesity prevalence was the highest in people in their 70s among the total population (40.5%). The obesity prevalence in people in their 20s and over 80 years old was low when compared to other age groups, but it has been rising relatively steeply between 2009 and 2019; from 18.5% to 28.9% in people in their 20s, and from 22.9% to 32.5% in people in their 80s or older.
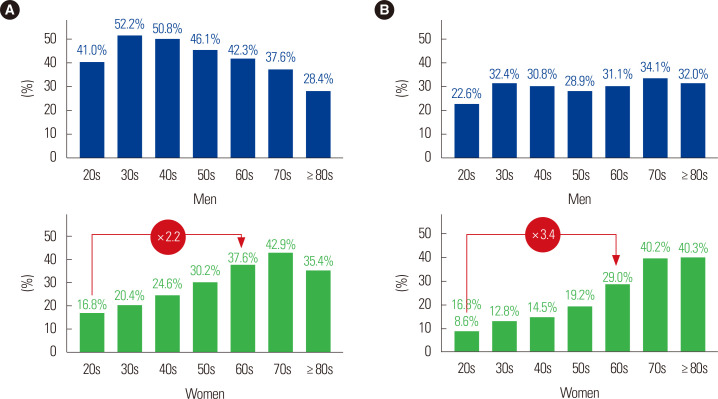
Obesity prevalence in men increased in all age groups, particularly in men ≥80 years: 18.5% in 2009 and 28.4% in 2019 (Supplementary Fig. 2A). However, compared with other age groups, the obesity prevalence among men ≥70 years was relatively low in 2019 (Fig. 3A). In 2019, 52.2% of men in their 30s and 50.8% of men in their 40s were obese. The change in the obesity prevalence in women was generally more gradual than in men: however, it increased among women in their 20s and 30s (Supplementary Fig. 2B). The obesity prevalence among women in their 20s increased from 8.6% in 2009 to 16.8% in 2019, whereas among women in their 50s and 60s it changed from 32.7% to 30.2% and from 41.4% to 37.6%, respectively. Unlike men, obesity among elderly women in their 60s and 70s was significantly higher than in women in their 20s and 30s—2.2 times higher in women in their 60s than in women in their 20s (37.6% vs. 16.8%) in 2019 (Fig. 3A).
Figure 3.
Age-specific prevalence of obesity (A) and abdominal obesity (B) stratified by sex between 2009 and 2019.
Over the past 11 years, the abdominal obesity prevalence steadily increased in all age groups except among people in their 60s (Supplementary Fig. 3). However, it increased significantly in people in their 20s and 30s, from 9.0% to 15.6% and from 15.8% to 24.6%, respectively. Unlike obesity prevalence, abdominal obesity showed an increasing trend with age that was high even among people ≥80 years.
Abdominal obesity prevalence in men increased regardless of age over 11 years, and the increasing trend was most evident in men in their 20s and 30s (Supplementary Fig. 4A). Abdominal obesity mostly increased during the transition period from the 20s to the 30s; for example, in 2019, it was 22.6% in men in their 20s and 32.4% in men in their 30s (Fig. 3B). The increase in abdominal obesity prevalence in women was more moderate than in men and it also increased with age (Supplementary Fig. 4B). Among women in their 20s, abdominal obesity prevalence nearly doubled from 4.4% in 2009 to 8.6% in 2019, although it decreased in women in their 60s. Abdominal obesity among elderly women in their 60s and 70s increased significantly compared with women in their 20s and 30s, which was 3.4 times higher among women in their 60s than in women their 20s (29.0% vs. 8.6%) in 2019 (Fig. 3B).
Risk of major comorbidities related to obesity
The relative risk of T2DM, myocardial infarction, and ischemic stroke was 2.6, 1.2, and 1.1 times higher, respectively, in people with obesity than in people without obesity (Supplementary Fig. 5). Compared to adults without abdominal obesity, the relative risk of T2DM, myocardial infarction, and ischemic stroke was 2.6, 1.3, and 1.2 times higher, respectively, in adults with abdominal obesity than people without abdominal obesity (Supplementary Fig. 5).
The relative risk of thyroid cancer in men with obesity was 1.5 times higher than in men without obesity (Supplementary Fig. 6A). In men with abdominal obesity, the relative risk of thyroid cancer was 1.5 times higher than in men without abdominal obesity. The relative risk of liver and colorectal cancer was also 1.2 times higher (Supplementary Fig. 6B). In obese women, the relative risk of liver and thyroid cancer was 1.2 times higher than in women without obesity (Supplementary Fig. 7A). In women with abdominal obesity, the relative risk of liver, colorectal, and thyroid cancer was 1.2–1.3 times higher than in women without abdominal obesity (Supplementary Fig. 7B).
Age-specific risk of obesity-related major comorbidities
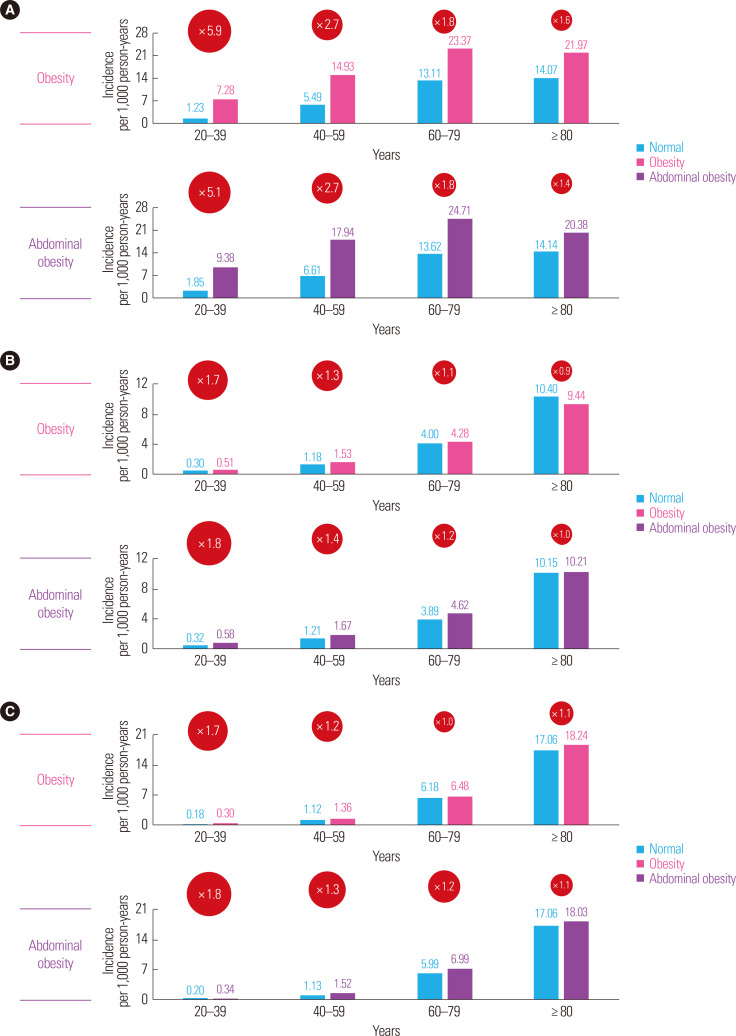
A more pronounced increase in the relative risk of T2DM was found in younger people with obesity and abdominal obesity compared to those without obesity and abdominal obesity (Fig. 4A). The relative risk of T2DM of adults with obesity was higher than in adults without obesity (5.9 times higher [20s and 30s], 2.7 times [40s and 50s], 1.8 times [60s and 70s], and 1.6 times [≥80 years old]). The relative risk of T2DM in adults with abdominal obesity was higher than in adults without abdominal obesity (5.1 times higher [20s and 30s], 2.7 times [40s and 50s], 1.8 times [60s and 70s], and 1.4 times [≥80 years old]). Similar patterns were observed for myocardial infarction (Fig. 4B) and ischemic stroke (Fig. 4C). The incidence of both myocardial infarction and ischemic stroke was 1.7 times higher in people in their 20s and 30s with obesity, and 1.8 times higher in people in the same age group with abdominal obesity than in people without either obesity or abdominal obesity, respectively. The relative risk of obesity-related comorbidities at two life transition points, defined by Korean NHIS as ages 40 and 66 years,12 also showed similar trends (Supplementary Fig. 8).
Figure 4.
Age-specific incidence per 1,000 person-years of comorbidities; type 2 diabetes (A), myocardial infarction (B), and ischemic stroke (C) in people with obesity and abdominal obesity, and people without obesity and abdominal obesity. The circle represents the relative risk of comorbidities in people with obesity and abdominal obesity compared with people without obesity and abdominal obesity, respectively.
DISCUSSION
The prevalence of obesity and abdominal obesity has steadily increased over the past 11 years among the total population. In particular, class III obesity prevalence has increased nearly threefold over the past 11 years (from 0.30% to 0.89%). Globally morbid obesity increased consistently. A recent study predicted that nearly 1 in 2 adults in the United States of America would have obesity (BMI ≥30 kg/m2), and nearly 1 in 4 adults will have severe obesity (BMI ≥35 kg/m2) by 2030.13 Severe obesity is predicted to become the most common BMI category among the population in this study. Increases in class II and III obesity is not only observed in Western countries.14 In a study in Taiwan using the Nutrition and Health Survey, which is a nationally representative sample, the prevalence of overweight and mild obesity (BMI of 27.0–29.9 kg/m2) was stabilized from 1993–1996, 2005–2008, and 2013–2014, but the prevalence of moderate obesity (BMI of 30.0–34.9 kg/m2) and morbid obesity (BMI ≥30.0 kg/m2) increased sharply, from 11.8%, 17.9%, to 22.0% and 0.4%, 0.6%, to 1.4%, respectively.15 Although the association of class I obesity and mortality was controversial with issues of the obesity paradox, class II or III obesity is known to be related to higher mortality.16 In this respect, policies for obesity should be addressed to avoid a global epidemic of severe obesity in the future.
Obesity prevalence by age shows an upward trend in all age groups, especially among people in their 20s and 80s. Although obesity prevalence is lower in those groups than in other age groups, there has been a clear upward trend since 2009. In particular, obesity increased the most during the transition period from the 20s to the 30s. The prevalence of abdominal obesity is also increasing, and significantly increased in people in their 20s and 30s. In the 20s group, both abdominal obesity and obesity prevalence were lower than in other age groups, and the prevalence of abdominal obesity was high among people in their 80s or older, while the prevalence of obesity was low. It can be inferred that obesity prevalence decreases after age 80, but abdominal obesity prevalence increases, accompanied by weight loss due to muscle loss.
We found that age-stratified obesity prevalence differed by sex. For example, the prevalence of obesity and abdominal obesity in women consistently increased with age. The obesity and abdominal obesity prevalence among elderly women was significantly higher than in young women: 2.2 times and 3.4 times higher among women in their 60s than in women in their 20s, respectively. However, abdominal obesity prevalence in men significantly increased during the transition period from the 20s to the 30s, and it stabilized beyond that. Moreover, the increasing trend was most evident in men in their 20s and 30s; therefore, abdominal obesity prevalence among men in their 30s became higher than in men in their 40s starting in 2018. Regarding obesity, a steep prevalence increase during the transition period from the 20s to the 30s was also observed, and more than half of men in their 30s and 40s were obese, resulting in the highest prevalence of obesity among adult men. This phenomenon may be more strongly associated with environmental, social, and lifestyle changes in the transition period than other biological and genetic factors.
Several studies have focused on the effect of events in the transition period, such as leaving the parental home, entering college or employment, and marriage.17-19 A study showed that the transition into employment increased obesity prevalence, especially in younger men in Korea.20 The 2019 Obesity Fact Sheet revealed that obesity prevalence was higher among people working in longer hours,21 and it may be related to work behavior in the transition period. According to a report using Korea National Health and Nutrition Examination Survey (KNHANES) data in 2019, the subjective obesity awareness rate of young adults (19–39 years) with obesity was high at 91.8%, but the weight loss attempt rate was 60.2%. With respect to dietary behaviors related to obesity, the rate of skipping breakfast (44.7%, 27.5%, and 5.1%), the rate of eating out more than once a day (38.1%, 30.4%, and 4.3%), and the rate of excessive energy intake (20.3%, 13.9%, and 9.6%) were significantly higher in young adults than in middle-aged (40–64 years) and elderly (≥65 years) adults.22 More comprehensive studies are needed to identify the environmental and social factors related to differences or changes in health behaviors in the young adult population, and these should be accompanied by supportive efforts from society and the government.
This study focused on the burden of obesity-related comorbidities stratified by age groups. The incidence of obesity-related comorbidities among young people was lower than among middleaged and elderly people, however, the increase in relative risk in obese people compared with people without obesity and abdominal obesity was more prominent in young adults. For example, the relative risk of T2DM in people with obesity was 5.9 times higher in young adults versus 2.7 times higher in middle-aged adults compared with the same age group without obesity. Because the increases in the prevalence of all obesity classes were greater in young adults than middle-aged and elderly adults,7 the impact of obesity on comorbidities in young adults will be increasingly strong. Once comorbidities develop, young adults tend to show improper management and low adherence to medical therapy in T2DM management23 and secondary prevention for coronary heart disease.24 Therefore, a global public health priority should be preventing and treating obesity in young adults to decrease the risk of related comorbidities and mortality.
This study has some limitations. First, when we assessed the prevalence of obesity and abdominal obesity, many related factors could not be considered. Second, the subjects of NHIS were different according to age. Before 2019, the subjects for health checkups provided by NHIS among the 20s–30s were limited to only beneficiaries of company medical insurance. This might result in weakening the representation of the young age group. Third, we assessed the incidence rate of comorbidities standardizing by age and sex, however, we could not adjust for several confounding factors for each comorbidity. However, the overall population of Korea who underwent national health checkups are representative of the entire Korean population; hence, we provide valuable data on national health statistics on obesity and abdominal obesity trends and their impact on comorbidities by stratifying age and sex.
In conclusion, based on the 2021 Obesity Fact Sheet findings, obesity and abdominal obesity prevalence in the entire population has increased over the past 11 years. Particularly, class III obesity has increased by nearly threefold. Age-stratified obesity prevalence differed by sex, and obesity and abdominal obesity prevalence increased steeply among men during the transition period from the 20s to the 30s. The relative risk of obesity-related comorbidities in obese people compared to people without obesity and abdominal obesity was higher in young and middle-aged people than in the elderly. These findings suggest a need to better understand obesity characteristics according to age and sex and to establish individualized treatment strategies.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found online at https://doi.org/10.7570/jomes22024.
ACKNOWLEDGMENTS
This work was partially supported by the Korean Society for the Study of Obesity. We cordially thank the National Health Insurance Service and the Korean Society for the Study of Obesity for their support.
Footnotes
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Study concept and design: YSY, BDH, KH, JHJ, and JWS; acquisition of data: all authors; statistical analysis: KH and JHJ; interpretation of data: all authors; drafting of the manuscript: YSY, BDH, and JWS; critical revision of the manuscript: all authors; and study supervision: JWS.
REFERENCES
- 1.Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et al. GBD 2015 Obesity Collaborators, author. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27. doi: 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Swinburn BA, Kraak VI, Allender S, Atkins VJ, Baker PI, Bogard JR, et al. The global syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. Lancet. 2019;393:791–846. doi: 10.1016/S0140-6736(18)32822-8. [DOI] [PubMed] [Google Scholar]
- 3.Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 4.Nyberg ST, Batty GD, Pentti J, Virtanen M, Alfredsson L, Fransson EI, et al. Obesity and loss of disease-free years owing to major non-communicable diseases: a multicohort study. Lancet Public Health. 2018;3:e490–7. doi: 10.1016/S2468-2667(18)30139-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim DS, Scherer PE. Obesity, diabetes, and increased cancer progression. Diabetes Metab J. 2021;45:799–812. doi: 10.4093/dmj.2021.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grosso G. Obesity during COVID-19: an underrated pandemic? EClinicalMedicine. 2021;39:101062. doi: 10.1016/j.eclinm.2021.101062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nam GE, Kim YH, Han K, Jung JH, Rhee EJ, Lee WY, et al. Obesity fact sheet in Korea, 2020: prevalence of obesity by obesity class from 2009 to 2018. J Obes Metab Syndr. 2021;30:141–8. doi: 10.7570/jomes21056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–8. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 9.Song SO, Jung CH, Song YD, Park CY, Kwon HS, Cha BS, et al. Background and data configuration process of a nationwide population-based study using the Korean national health insurance system. Diabetes Metab J. 2014;38:395–403. doi: 10.4093/dmj.2014.38.5.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim YH, Han K, Son JW, Lee SS, Oh SW, Kwon HS, et al. Data analytic process of a nationwide population-based study on obesity using the National Health Information Database presented by the National Health Insurance Service 2006-2015. J Obes Metab Syndr. 2017;26:23–7. doi: 10.7570/jomes.2017.26.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim BY, Kang SM, Kang JH, Kang SY, Kim KK, Kim KB, et al. 2020 Korean Society for the Study of Obesity Guidelines for the management of obesity in Korea. J Obes Metab Syndr. 2021;30:81–92. doi: 10.7570/jomes21022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim HS, Shin DW, Lee WC, Kim YT, Cho B. National screening program for transitional ages in Korea: a new screening for strengthening primary prevention and follow-up care. J Korean Med Sci. 2012;27 Suppl(Suppl):S70–5. doi: 10.3346/jkms.2012.27.S.S70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ward ZJ, Bleich SN, Cradock AL, Barrett JL, Giles CM, Flax C, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381:2440–50. doi: 10.1056/NEJMsa1909301. [DOI] [PubMed] [Google Scholar]
- 14.NCD Risk Factor Collaboration (NCD-RisC), author Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016;387:1377–96. doi: 10.1016/S0140-6736(16)30054-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang HC, Yang HC, Chang HY, Yeh CJ, Chen HH, Huang KC, et al. Morbid obesity in Taiwan: prevalence, trends, associated social demographics, and lifestyle factors. PLoS One. 2017;12:e0169577. doi: 10.1371/journal.pone.0169577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA. Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obesity (Silver Spring) 2008;16:2205–11. doi: 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- 18.Mooyaart JE, Liefbroer AC, Billari FC. Becoming obese in young adulthood: the role of career-family pathways in the transition to adulthood for men and women. BMC Public Health. 2019;19:1511. doi: 10.1186/s12889-019-7797-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Winpenny EM, van Sluijs EM, White M, Klepp KI, Wold B, Lien N. Changes in diet through adolescence and early adulthood: longitudinal trajectories and association with key life transitions. Int J Behav Nutr Phys Act. 2018;15:86. doi: 10.1186/s12966-018-0719-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kang YJ, Lee DW, Park MY, Kang MY. Employment status transition predicts adult obesity trajectory: evidence from a cohort study in South Korea. J Occup Environ Med. 2021;63:e861–7. doi: 10.1097/JOM.0000000000002388. [DOI] [PubMed] [Google Scholar]
- 21.Nam GE, Kim YH, Han K, Jung JH, Rhee EJ, Lee SS, et al. Obesity fact sheet in Korea, 2019: prevalence of obesity and abdominal obesity from 2009 to 2018 and Social Factors. J Obes Metab Syndr. 2020;29:124–32. doi: 10.7570/jomes20058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim DY, Park SY, Kim YJ, Oh KW. National health statistics plus: current status of obesity prevalence in Korean adults and related factors [Internet] Korea Disease Control and Prevention Agency; Cheongju: 2021. [cited 2022 Jun 23]. Available from: https://knhanes.kdca.go.kr/knhanes/sub04/sub04_04_02.do . [Google Scholar]
- 23.Nanayakkara N, Pease AJ, Ranasinha S, Wischer N, Andrikopoulos S, de Courten B, et al. Younger people with type 2 diabetes have poorer self-care practices compared with older people: results from the Australian National Diabetes Audit. Diabet Med. 2018;35:1087–95. doi: 10.1111/dme.13660. [DOI] [PubMed] [Google Scholar]
- 24.Koopman C, Vaartjes I, Heintjes EM, Spiering W, van Dis I, Herings RM, et al. Persisting gender differences and attenuating age differences in cardiovascular drug use for prevention and treatment of coronary heart disease, 1998-2010. Eur Heart J. 2013;34:3198–205. doi: 10.1093/eurheartj/eht368. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.