Abstract
Objective
To compare the dental and skeletal effects of intermaxillary elastics on the correction of mild Angle's Class II division 1 malocclusion with clear aligner treatment (CA) versus fixed multibracket (FMB) in growing patients.
Settings and sample population
The study sample consisted of 49 consecutively patients (mean age ± SD 12.9 ± 1.7 years), 32 females and 17 males referred from the School of Orthodontics of the University of Bratislava Comenius (Slovakia). All patients were treated with a non‐extraction orthodontic treatment, 25 with FMB and 24 with CA.
Methods
The cephalometric analysis was performed at the beginning (T0) and the end of the treatment (T1). The t test for unpaired data was carried out to compare cephalometric values at T0 and changes at T1‐T0 between the two groups. The level of significance was set as P < .0035.
Results
The two groups showed no statistically significant differences (ANPg = −0.1°; P = .762) in the correction of the sagittal intermaxillary relation. The analysis of vertical skeletal changes showed no statistically significant effects on mandibular inclination (SN/MP = 0.1°; P = .840). The two treatments had a statistically significant and clinically relevant difference in controlling the inclination of the lower incisors (L1/GoGn = 4.8°, CAG = −0.5°± 3.9°; FMB = 4.3°± 5.8°; P < .001).
Conclusions
Class II elastics combined with CA and FMB produce a similar correction on sagittal discrepancies in growing patients. CA presented a better control in the proclination of the lower incisors. CA and elastics might be a good alternative in the correction of mild Class II malocclusion in cases where a proclination of lower incisors is unwanted.
Keywords: adolescents, Class II elastics, Class II malocclusion, clear aligners
1. INTRODUCTION
In the last decades, there has been a significant increase in the use of clear aligners (CA) for the treatment of malocclusions in adults and children. 1 , 2 , 3 , 4 The concept of clear aligner treatment (CAT) comprises an aesthetic orthodontic treatment that may allow for better oral hygiene, periodontal health and safety of the roots. 5 , 6 , 7 , 8 Patients seem to show a greater degree of acceptance and collaboration towards CAT and a very high satisfaction level with the final result. 9 Thanks to the progress in the biomechanics of the CAT and to the improvement in physical and chemical properties of the material, 10 , 11 new scenarios have opened for the clinical use of aligners, which increased the number of cases being treated with this therapy. 12 The biomechanics of these instruments allows the clinician to plan and to obtain a wide range of dental movements, such as molar distalization, molar derotation and incisor torque. 13 , 14
Several approaches have been developed for the treatment of Class II malocclusions, which include a variety of options due to the high prevalence of the malocclusion 15 : extraoral tractions, dental and skeletal expansion, functional jaw orthopaedic appliances, fixed therapy and intermaxillary elastics, and much more. 16 The conventional fixed multibracket therapy (FMB) approach associated with intermaxillary elastics is one of the most common approaches to treat dental Class II malocclusion. 17 Class II elastics are effective in correcting Class II malocclusions, and their effects are mainly dentoalveolar, including lingual tipping, retrusion and extrusion of the maxillary incisors; labial tipping and intrusion of the mandibular incisors; mesialization and extrusion of the mandibular molars; and an increase in the occlusal plane angle during treatment. 18 On the other hand, the treatment with aligners and intermaxillary elastics in Class II patients is still unexplored in several aspects. One study evaluated the effect of molar distalization on the vertical dentoskeletal dimension finding an excellent control of both the vertical dimension and the incisal anchorage loss 19 ; however, the literature analysing the Class II treatment is prevalently made of case reports and case series. 17 , 20 Hence, the purpose of this study was to compare the effects of intermaxillary elastics on the correction of mild Angle's Class II division 1 malocclusion between two groups of growing patients undergoing orthodontic treatment respectively with FMB and CAT. The primary outcome of this retrospective study was to evaluate the effects of these two treatments on the sagittal skeletal discrepancy (ANPg).
2. MATERIALS AND METHODS
This retrospective study followed the STROBE Statement checklist for reports of observational studies. 21 The study protocol complied fully with the principles of the Helsinki Declaration and was approved by the Ethical Committee at the University of Naples Federico II (67/17).
2.1. Sample
The a priori sample size calculation, performed based on the main outcome (ANPg), showed that at least 22 patients per group were required.
Inclusion criteria for the selection in the study were as follows: patients treated by means of clear aligners or fixed multibracket appliances and elastics; patients with ages between 9 and 16 at the beginning of treatment, Class II division 1 malocclusion, late mixed (eruption of lower second premolars and/or eruption of upper canines) or permanent dentition, ANPg ≥3°, and overjet ≥4 mm and at least End‐to‐End Class II molar and canine relationship, molar and canine Class I at the end of treatment.
Subjects were excluded from the study if they had one of the following exclusion criteria: craniofacial abnormalities, congenital syndromes of the craniofacial area, periodontal disease, or temporomandibular disorders, treated with functional appliances, treated with elastics on miniscrews, extractions in the treatment plan.
2.2. Clinical protocol
All patients were treated with a non‐extraction orthodontic treatment, and the selected subjects were divided into two groups:
2.2.1. Fixed multibracket therapy group (FMB)
The treatment was performed with a multibracket fixed appliance with slot size 0.022 × 0.028 and MBT prescription (Mini Sprint® II, Forestadent). The following arch sequence was used: 0.014 nickel titanium (NiTi), 0.014 × 0.025‐inch NiTi straight arch, 0.019 × 0.025‐inch NiTi straight arch, 0.019 × 0.025‐inch stainless steel with 1/4" 6 oz intermaxillary elastics. Patients were invited to wear the elastics bilaterally from the hooks of the upper cuspid to the hooks of lower first molar for 22 hours, except during the meals. Elastics were applied when the 0.019 × 0.025‐inch stainless steel archwires were placed.
2.2.2. Clear aligners group (CAG)
Treatment was performed with aligners (Invisalign®, Align Technology). Starting from the third aligner, 1/4” 6 oz intermaxillary elastics were accommodated by using precision cuts on the upper canines and metal buttons placed at the level of the first lower molars and were worn throughout the day.
Each patient was assigned 4 sets of aligners at a time and checked, on average, every 28 days. Each aligner was worn for 7 days.
2.3. Measurements and timing
The skeletal and dental changes, due to the treatment, were evaluated on the lateral cephalograms in centric occlusion through cephalometric analysis (Figure 1, Table 1). All the cephalograms were performed with the same cephalometric X‐ray, ART Plus C (Ajat). Lateral cephalograms were performed in centric occlusion, with relaxed lips and with the heads oriented according to the Frankfurt plane. On each lateral cephalogram, the cephalometric tracing was performed by a single operator. For both groups, two lateral cephalograms were included, one at the beginning of treatment (T0) and one at the end of treatment (T1), when a good alignment and a Class I molar, and canine relationship were achieved.
FIGURE 1.
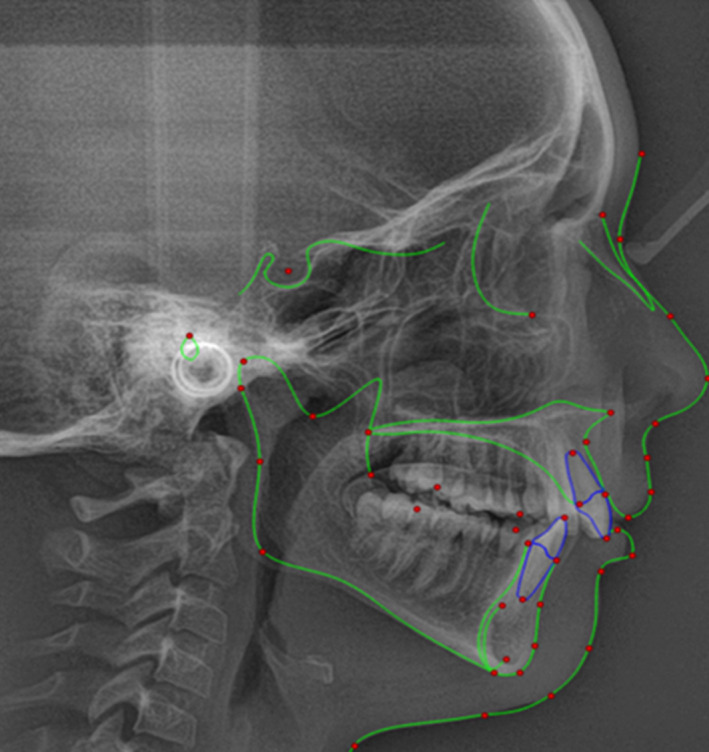
Cephalometric analysis and tracing: Sagittal skeletal: SNA (°), SNPg (°), ANPg (°), WITS (mm), Co‐Gn (mm), Vertical skeletal: SN to palatal plane (°), SN to mandibular plane (°), Palatal plane to mandibular plane (°), CoGoMe (°), Co‐Go (mm). Interdental: Overjet (mm), Overbite (mm). Maxillary dentoalveolar: U1 to palatal plane (°). Mandibular dentoalveolar: L1 to mandibular plane (°)
TABLE 1.
Descriptive statistics and statistical comparisons of baseline characteristics
| Cephalometric measures | FMB | CAG | P | |||||
|---|---|---|---|---|---|---|---|---|
| n = 25 | n = 24 | |||||||
| Mean | SD | 95% CI | Mean | SD | 95% CI | |||
| Sagittal Skeletal | ||||||||
| SNA (°) | 81.4 | 3.2 | 80.0;82.7 | 80.6 | 2.9 | 79.3;81.8 | .366 | |
| SNPg (°) | 77.1 | 3.5 | 75.7;78.7 | 77.6 | 2.9 | 75.9;78.4 | .960 | |
| ANPg (°) | 4.8 | 1.6 | 4.1;5.4 | 4.3 | 1.4 | 3.7;4.9 | .276 | |
| Wits (mm) | 4.0 | 2.3 | 3.1;5.0 | 3.3 | 1.9 | 2.5;4.1 | .271 | |
| Co‐Gn (mm) | 103.3 | 6.5 | 100.6;105.9 | 104.8 | 7.5 | 101.7;108.0 | .430 | |
| Vertical Skeletal | ||||||||
| SN/PP (°) | 8.2 | 3.7 | 6.7;9.7 | 8.6 | 3.3 | 7.2;10.0 | .673 | |
| SN/MP (°) | 31.8 | 5.5 | 29.5;34.1 | 32.7 | 6.4 | 30.0;35.4 | .591 | |
| PP/MP (°) | 20.4 | 5.1 | 18.3;22.6 | 21.4 | 6.4 | 18.7;24.1 | .555 | |
| CoGoMe (°) | 127.0 | 6.5 | 124.3;129.7 | 128.3 | 8.7 | 124.6;132.0 | .569 | |
| Co‐Go (mm) | 51.2 | 4.8 | 49.2;53.2 | 52.0 | 5.5 | 49.7;54.3 | .590 | |
| Interdental | ||||||||
| Overjet (mm) | 5.3 | 1.5 | 4.7;5.9 | 5.0 | 1.3 | 4.4;5.5 | .461 | |
| Overbite (mm) | 2.6 | 1.8 | 1.8;3.3 | 2.6 | 1.9 | 1.8;3.4 | .952 | |
| Maxillary dentoalveolar | ||||||||
| U1/PP (°) | 111.0 | 7.2 | 108.1;114.0 | 109.7 | 7.5 | 106.5;112.8 | .517 | |
| Mandibular dentoalveolar | ||||||||
| L1/GoGn (°) | 101.9 | 6.0 | 99.4;104.3 | 99.7 | 7.2 | 96.6;102.7 | .257 | |
Significance level was set at P < .0035. Data are reported as mean ± standard deviation (SD) and 95% confidence interval (95%CI).
Abbreviations: CAG, clear aligners group; FMB, fixed multibracket group.
All X‐rays were scanned using a scanner (Expression 1680 Pro; Epson Italy) with a resolution of 300 dpi and 256 levels of grey, then saved in the jpeg format and then subjected to cephalometric analysis using Dolphin Imaging 11.0 software (Dolphin Imaging). The examiner was extensively trained in electronic cephalometric analysis and was blinded to the patients’ names and allocations. The dates of the radiographs were also concealed from the examiner during the measurements. T0 and T1 radiographs were randomly submitted to the examiner.
Digital dental casts were used to assess amount of crowding at the lower arch, amount of interproximal reduction (IPR) at the lower front teeth (canine to canine) and molar relationship. Digital dental casts at the beginning and at the end of treatment were collected. The digital dental casts were analysed by means of Autodesk MeshMixer (Autodesk INC.). Crowding was defined as the difference between the sum of mesiodistal segment of teeth from second bicuspids to second bicuspids at the lower jaw and the arch length. The arch length was measured in four segments: right and left posterior arch lengths (mesial to the first molar up to distal to the canine) and right and left anterior arch lengths (distal to the canine up to the midpoint between the central incisors). The mesiodistal tooth width was measured from the second bicuspids to the incisors. 22 For measuring the amount of the IPR, the mesiodistal tooth width was evaluated also in the digital casts at the end of treatment, only for the lower jaw from cuspid to cuspid. For each tooth, the difference in mm between the mesiodistal width at T0 minus the mesiodistal width at T1 was calculated. Finally, the molar class relation was evaluated analysing the digital cast in occlusion. The molar relation was divided according to the American Board of Orthodontics definition in End‐to‐End Class II molar relationship and full‐step Class II molar relationship.
2.4. Method error
The technical errors of measurement were calculated from 40 randomly selected cephalograms. A set of measurements was reassessed by the same examiner after a memory washout period of at least 4 weeks. The method error for all measurements was calculated using Dahlberg's formula. 23
Systematic differences between duplicated measurements were tested using a paired Student's t test with the type I error set at 0.05.
2.5. Statistical analysis
For each parameter (demographic and cephalometric) collected, the main descriptive statistics (mean and standard deviation for continuous data) were described.
The G*Power software version 3.1.9 (Universität Kiel) was used for sample size calculation. Considering an alpha = 0.05, a beta = 0.20, the t test for unpaired data and an effect size of 0.9 (difference of ANPg means of −1.45° with a grouped standard deviation of 1.3°), 24 at least 22 patients per group were required.
Statistical tests were carried out to compare each cephalometric variable analysed within the two groups, data distribution was assessed by means of Shapiro‐Wilk test and Q‐Q plot analysis, and due to the normal distribution of the data, the comparisons of cephalometric variables at T0 and of the differences T1‐T0 between groups were performed by means of t test for unpaired data. The significance level was adjusted according to Bonferroni's correction (P < .0035; α/multiple comparisons; 0.05/14). All statistical analyses were performed using the standard statistical software package (SPSS version 22.0, IBM SPSS).
3. RESULTS
The study sample consisted of 49 consecutively treated patients (mean age ± SD 12.9 ± 1.7 years), 32 females and 17 males referred from the School of Orthodontics of the University of Bratislava Comenius (Slovakia) and analysed at the School of Orthodontics of the Department of Neuroscience, Reproductive Sciences and Oral Sciences of the University of Naples Federico II (Italy).
The fixed multibracket therapy group (FMB) included 25 patients (mean age ± SD 13.1 ± 1.8 years), 16 females and 9 males.
The clear aligners group (CAG) included 24 patients (mean age ± SD 12.7 ± 1.7 years), 16 females and 8 males.
Before treatment for the CAG group, 16 patients were in End‐to‐End Class II molar relationship and 8 patients in full‐step Class II molar relationship; for the FMB, 16 patients were in End‐to‐End Class II molar relationship and 9 patients in full‐step Class II molar relationship. At the end of the treatment, all the patients achieved a Class I molar and canine relationship.
The method error ranged between 0.20° (ANPg) and 1.18° (U1/PP) for cephalometric angular measurements and between 0.49 mm (OVJ) and 0.94 mm (Co‐Gn) for linear measurements. There was no systematic error for any measurements (Student's t test: P > .01).
In the analysis of the starting forms, the two groups presented the same characteristics for all the analysed variables (P > .05). The amount of crowding at the beginning of the treatment was similar between the two groups (CAG = −0.4 ± 1.5, range −2.3‐2.7; FMB = −1.0 ± 1.6, range −3 ‐ 2; P = .135). The treatment duration presented a statistically significant difference between CAG (1.16 ± 0.5 years) and FMB (1.9 ± 0.4 years; P < .001).
The FMB group had an average ANPg of 4.8°±1.6° while the CAG had an average ANPg of 4.3°±1.4° (Table 1). At the end of the treatment, the two groups showed no statistically significant differences (−0.1°, P = .762) in the correction of the sagittal intermaxillary relationship (ANPg, Table 2).
TABLE 2.
Descriptive statistics and statistical comparisons of the T1‐T0 changes
| Cephalometric measures | FMB | CAG | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n = 25 | n = 24 | |||||||||
| Mean | SD | 95% CI | Mean | SD | 95% CI | Mean difference | P | 95% CI Lower limit | 95% CI Upper limit | |
| Sagittal Skeletal | ||||||||||
| SNA (°) | −0.7 | 1.4 | −1.2;−0.1 | −0.6 | 1.1 | −1.1;−0.1 | −0.1 | .836 | −0.8 | 0.7 |
| SNPg (°) | 0.5 | 1.1 | 0.1;1.0 | 0.3 | 1.5 | −0.4;0.9 | 0.2 | .505 | −0.5 | 1.0 |
| ANPg (°) | −0.8 | 1.0 | −1.2;−0.4 | −0.7 | 1.1 | −1.2;−0.3 | −0.1 | .762 | −0.7 | 0.5 |
| Wits (mm) | −2.1 | 2.1 | −2.9:−1.2 | −1.8 | 2.4 | −2.8;−0.8 | −0.3 | .676 | −1.6 | 1.0 |
| Co‐Gn (mm) | 5.7 | 4.0 | 4.0;7.4 | 5.2 | 3.9 | 3.5;6.8 | 0.5 | .650 | −1.7 | 2.8 |
| Vertical Skeletal | ||||||||||
| SN/PP (°) | 0.3 | 1.9 | −0.5;1.1 | 0.7 | 1.3 | 0.2;1.3 | −0.5 | .323 | −1.4 | 0.5 |
| SN/MP (°) | −0.2 | 1.5 | −0.8;0.5 | −0.3 | 2.2 | −1.2;0.7 | 0.1 | .840 | −1.0 | 1.2 |
| PP/MP (°) | −0.3 | 2.7 | −1.4;0.8 | −1.0 | 2.0 | −1.8;−0.1 | 0.7 | .294 | −0.6 | 2.1 |
| CoGoMe (°) | 1.8 | 5.4 | −0.4;4.1 | −2.5 | 8.6 | −6.1;1.1 | 4.3 | .038 | 0.3 | 8.4 |
| Co‐Go (mm) | 4.1 | 3.3 | 2.7;5.4 | 3.8 | 3.9 | 2.2;5.4 | 0.3 | .789 | −1.8 | 2.3 |
| Interdental | ||||||||||
| Overjet (mm) | −1.9 | 1.8 | −2.7;−1.2 | −1.7 | 1.5 | −2.3;−1.0 | −0.2 | .609 | −1.2 | 0.7 |
| Overbite (mm) | −1.7 | 1.9 | −2.4;−0.9 | −1.2 | 1.4 | −1.8;−0.6 | −0.4 | .345 | −1.4 | 0.5 |
| Maxillary dentoalveolar | ||||||||||
| U1/PP (°) | 3.4 | 8.5 | −0.1;6.9 | 0.5 | 9.2 | −3.3;4.4 | 2.8 | .268 | −2.2 | 7.9 |
| Mandibular dentoalveolar | ||||||||||
| L1/GoGn (°) | 4.3 | 5.8 | 1.9;6.7 | −0.5 | 3.9 | −2.1;1.2 | 4.8 | <.001 | 1.9 | 7.6 |
Significance level was set at P < .035. Data are reported as mean ± standard deviation (SD) and 95% confidence interval (95%CI). Bold type: statistically significant.
Abbreviations: CAG, clear aligners group; FMB, fixed multibracket group.
The analysis of vertical skeletal changes showed similar effects on the mandibular inclination (SN/MP 0.1°). An average slight mandibular posterior rotation in the FMB group (−0.2°± 1.5°) compared to an average slight anterior rotation in the CAG (−0.3°± 2.2°) was recorded, but this difference was not statistically significant (P = .840).
The different effects of the two treatments are particularly evident in the dentoalveolar component. Both groups showed a similar OVJ (FMB: −1.9°± 1.7°; CAG: −1.7°± 1.5°) and OVB correction (FMB: −1.7°± 1.9°; CAG: −1.2°± 1.4°), but the two treatments had a statistically significant and clinically relevant difference in controlling the inclination of the lower incisors (L1/GoGn). Patients treated with FMB recorded an average proclination of 4.3°± 5.8°, while patients treated with aligners recorded a slight reclination (−0.5°± 3.9°). The difference between the two treatments (4.8°) was statistically significant (P < .001). Finally, both groups included a similar amount of IPR in the frontal lower teeth in their treatment plan (CAG = 0.64 ± 0.69 [max 2.9 mm]; FMB = 0.63 ± 0.89 [max 2.6 mm]; P = .967).
4. DISCUSSION
This study investigated the effects of two orthodontic treatments, CAT and fixed multibracket therapy with intermaxillary elastics, on the Class II malocclusion in growing patients.
Considering the results of this study, the two treatments achieved similar results, but it is important to underline that CAT presented a better control in the proclination of the lower incisors.
One of the limits in the therapy of Class II elastics with fixed therapy is the proclination achieved, as reported in several studies. 18 In some cases, this proclination is considered a desired movement, for example, to correct Class II malocclusion with a deep bite and retroclined lower incisors; however, in some cases, this proclination is unwanted. For example, in high angle patients a Class II malocclusion, due to the clockwise rotation of the mandible, is often present, which is associated with crowding and proclined lower incisors. In this case, the proclination of the lower incisors can be considered an undesired movement that could damage the patient and create a recession in the lower incisors. 25 The results suggest that, in our sample of growing patients, there are no statistically significant improvements for both treatments in the sagittal skeletal relationship, and this is consistent with previous studies on fixed appliances and Class II elastics. 18 In growing patients, often the aetiology of Class II malocclusion is related to a retruded mandible that may require a treatment with functional orthopaedic appliances. 26 , 27 Class II functional appliances are indicated in the correction of mandibular deficiencies since they allow mandibular postural changes by holding the mandible forward and/or downward, although their effectiveness is debated. 16 In general, there is still no sufficient evidence to either suggest or discourage the functional treatment in Class II patients. The lack of definite evidence is mainly due to the small number of well‐conducted randomised studies. 26 Considering the dentoalveolar effects, there are other auxiliaries that can be used for Class II malocclusion correction, such as the Forsus™ Fatigue Resistance Device (Forsus FRD®; 3 M Unitek), which is a fixed functional appliance that has received increased interest as an effective and noncompliant option for Class II Division 1 treatment. Although the Forsus FRD® is a valuable option for the correction of Class II malocclusion, providing a shorter treatment period and requiring minimal patient compliance, 28 it proclines the lower incisors similarly to the intermaxillary elastics with fixed appliances. 29 , 30 The Herbst appliance represents a further option in Class II correction: it promotes a postural alteration in the mandible, positioning it anteriorly. It consists of a reciprocal intermaxillary anchored intraoral device. The device action of advancing the mandible causes an equal and opposite reaction in the upper arch. Thus, the appliance produces a forward force on the lower teeth and a backward force on the upper teeth. 31 , 32 Gerszewski et al 33 evaluated lower incisor changes after treatment with Herbst appliance, and there was a statistically significant increase in the IMPA in the treated group (3.2°±12.8°).
This study showed that the CAT with intermaxillary elastics represents an important therapeutic option for some types of patients when we need to maintain the position of the lower incisors. Probably, the greater control is associated with the rigidity of the aligner in maintaining all the arch locked, or with a better distribution of forces produced by the elastics on the aligner compared to what happens with the brackets. Hence, it could be supposed that, thanks to its structure, the CAT avoids the proclination of the lower incisors due to the Class II elastics.
Another possible advantage of the CAT therapy is the bite‐block effect, which should allow a greater control of verticality, as confirmed in previous studies. 19 , 34 Indeed, Class II elastics with fixed therapy usually create molar extrusion and a clockwise rotation of the occlusal plane. 18 However, in this study the difference in the changes of the mandibular plane (SN/MP) was not statistically significant.
The CAG showed a shorter treatment duration respect to the FMB. This was a great advantage of the CAT; indeed, also Zheng et al showed a significant short treatment duration of CAT in mild‐to‐moderate cases. 35 This aspect has been confirmed by another study. 36 This difference may be ascribed to the possibility of CAT to use elastics from the first stages of treatment. For example, in the protocol used in this study each patient in CAG began wearing intermaxillary elastics with the third aligner (after 14 days of treatment), while patients in FMB started wearing intermaxillary elastics only with the fourth steel arch (after approximately 180 days of treatment). Moreover, the aligners were changed every 7 days, reducing the treatment time.
Although this protocol is widely used in clinical practice, there is a lack of evidence in the relevant literature to support it. This study could be source of inspiration for further investigations, because despite the limitation of being a retrospective and short‐term study, the homogeneity and the sample size give the results a certain reliability. All the included patients achieved a Class I molar and canine relationship, and this was necessary to simulate the optimum result of both treatments and to evaluate the effects until the achievement of a good occlusion.
In this retrospective study, some source of bias might be present. In both group, it was not possible to monitor patients’ compliance, and this could influence treatment duration.
The inclination of lower incisors might be influenced by the amount of crowding and the IPR. However, in this study these data were calculated and did not differ in the two groups. Another, possible source of bias was the correction of the Curve of Spee that was not recorded in the study. The levelling of the Curve of Spee is often associated to a proclination of the lower incisors, with the reduction of OVJ and OVB. However, between the two groups the OVJ and OVB did not show statistically significant differences at both the time points.
5. CONCLUSIONS
Class II elastics combined with CA and FMB produced a similar correction of sagittal discrepancies (ANPg) in growing patients.
There were no statistically significant differences between the two treatments on vertical skeletal changes.
Clear aligners presented a better control in the proclination of the lower incisors. CA and elastics might be a good alternative in the correction of mild Class II malocclusion in cases where a proclination of lower incisors is unwanted.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
VD, RR and SD involved in conceptualization; SD, VD, RR and LF involved in methodology; RR and RB involved in formal analysis; SD, RB, VD and RR involved in investigation; SD, AM and VD involved in resources; RR involved in data curation; SD, RR and RB wrote the original draft preparation; VD, LF and AM involved in writing, reviewing and editing; AM and VD involved in supervision; SD and RR involved in project administration.
ACKNOWLEDGEMENTS
The study was supported with a grant from Align Technology with a 2017 International Align Research Award Grant. Open Access Funding provided by Universita degli Studi di Napoli Federico II within the CRUI‐CARE Agreement. [Correction added on 21 May 2022, after first online publication: CRUI funding statement has been added.]
Dianiskova S, Rongo R, Buono R, Franchi L, Michelotti A, D’Antò V. Treatment of mild Class II malocclusion in growing patients with clear aligners versus fixed multibracket therapy: A retrospective study. Orthod Craniofac Res.2022;25:96–102. 10.1111/ocr.12500
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author (VD) upon reasonable request.
REFERENCES
- 1. Shalish M, Cooper‐Kazaz R, Ivgi I, et al. Adult patients’ adjustability to orthodontic appliances. Part I: a comparison between Labial, Lingual, and InvisalignTM . Eur J Orthod. 2012;34:724‐730. [DOI] [PubMed] [Google Scholar]
- 2. Rosvall MD, Fields HW, Ziuchkovski J, Rosenstiel SF, Johnston WM. Attractiveness, acceptability, and value of orthodontic appliances. Am J Orthod Dentofacial Orthop. 2009;135(3):276.e1‐276.e12. [DOI] [PubMed] [Google Scholar]
- 3. Walton DK, Fields HW, Johnston WM, Rosenstiel SF, Firestone AR, Christensen JC. Orthodontic appliance preferences of children and adolescents. Am J Orthod Dentofacial Orthop. 2010;138(6):698.e1‐698.e12. [DOI] [PubMed] [Google Scholar]
- 4. Zhang B, Huang X, Huo S, et al. Effect of clear aligners on oral health‐related quality of life: a systematic review. Orthod Craniofac Res. 2020;23(4):363‐370. [DOI] [PubMed] [Google Scholar]
- 5. Azaripour A, Weusmann J, Mahmoodi B, et al. Braces versus Invisalign®: gingival parameters and patients’ satisfaction during treatment: a cross‐sectional study. BMC Oral Health. 2015;15:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pango Madariaga AC, Bucci R, Rongo R, Simeon V, D’Antò V, Valletta R. Impact of fixed orthodontic appliance and clear aligners on the periodontal health: a prospective clinical study. Dent J. 2020;8:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fang X, Qi R, Liu C. Root resorption in orthodontic treatment with clear aligners: a systematic review and meta‐analysis. Orthod Craniofac Res. 2019;22:259‐269. [DOI] [PubMed] [Google Scholar]
- 8. Iliadi A, Koletsi D, Eliades T. Forces and moments generated by aligner‐type appliances for orthodontic tooth movement: a systematic review and meta‐analysis. Orthod Craniofac Res. 2019;22:248‐258. [DOI] [PubMed] [Google Scholar]
- 9. Melkos AB. Advances in digital technology and orthodontics: a reference to the Invisalign method. Med Sci Monit Int Med J Exp. Clin Res. 2005;11(5):PI39‐PI42. [PubMed] [Google Scholar]
- 10. Bucci R, Rongo R, Levatè C, et al. Thickness of orthodontic clear aligners after thermoforming and after 10 days of intraoral exposure: a prospective clinical study. Prog Orthod. 2019;20:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Martina S, Rongo R, Bucci R, Razionale AV, Valletta R, D’Antò V. In vitro cytotoxicity of different thermoplastic materials for clear aligners. Angle Orthod. 2019;89:942‐945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Robertson L, Kaur H, Fagundes NCF, Romanyk D, Major P, Flores MC. Effectiveness of clear aligner therapy for orthodontic treatment: a systematic review. Orthod Craniofac Res. 2020;23:133‐142. [DOI] [PubMed] [Google Scholar]
- 13. Ravera S, Castroflorio T, Garino F, Daher S, Cugliari G, Deregibus A. Maxillary molar distalization with aligners in adult patients: a multicenter retrospective study. Prog Orthod. 2016;17:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Simon M, Keilig L, Schwarze J, Jung BA, Bourauel C. Forces and moments generated by removable thermoplastic aligners: incisor torque, premolar derotation, and molar distalization. Am J Orthod Dentofacial Orthop. 2014;145:728‐736. [DOI] [PubMed] [Google Scholar]
- 15. Paduano S, Rongo R, Bucci R, et al. Is there an association between various aspects of oral health in Southern Italy children? An epidemiological study assessing dental decays, periodontal status, malocclusions and temporomandibular joint function. Eur J Paediatr Dent. 2018;19:176‐180. [DOI] [PubMed] [Google Scholar]
- 16. Pacha MM, Fleming PS, Johal A. Complications, impacts, and success rates of different approaches to treatment of Class II malocclusion in adolescents: a systematic review and meta‐analysis. Am J Orthod Dentofac Orthop. 2020;158:477‐494. [DOI] [PubMed] [Google Scholar]
- 17. Papageorgiou SN, Koletsi D, Iliadi A, Peltomaki T, Eliades T. Treatment outcome with orthodontic aligners and fixed appliances: a systematic review with meta‐analyses. Eur J Orthod. 2020;42:331‐343. [DOI] [PubMed] [Google Scholar]
- 18. Janson G, Sathler R, Fernandes TMF, Branco NCC, de Freitas MR. Correction of class II malocclusion with class II elastics: a systematic review. Am J Orthod Dentofac Orthop. 2013;143:383‐392. [DOI] [PubMed] [Google Scholar]
- 19. Caruso S, Nota A, Ehsani S, Maddalone E, Ojima K, Tecco S. Impact of molar teeth distalization with clear aligners on occlusal vertical dimension: a retrospective study. BMC Oral Health. 2019;19:182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sabouni W, Eichelberger A, Des GO. Treatment of class II for growing patients by clear aligners: which protocol? Orthod Fr. 2019;90:13‐27. [DOI] [PubMed] [Google Scholar]
- 21. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;147:573‐577. [DOI] [PubMed] [Google Scholar]
- 22. Yoon JH, Yu H‐S, Choi Y, Choi T‐H, Choi S‐H, Cha J‐Y. Model analysis of digital models in moderate to severe crowding: In Vivo Validation and Clinical Application. Biomed Res Int. 2018;2018:8414605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dahlberg G. Statistical methods for medical and biological students. Br Med J. 1940;2(4158):358‐359. [Google Scholar]
- 24. Mossaz CF, Byloff FK, Kiliaridis S. Cervical headgear vs pendulum appliance for the treatment of moderate skeletal class II malocclusion. Am J Orthod Dentofacial Orthop. 2007;132:616‐623. [DOI] [PubMed] [Google Scholar]
- 25. Antoun JS, Mei L, Gibbs K, Farella M. Effect of orthodontic treatment on the periodontal tissues. Periodontol. 2000;2017(74):140‐157. [DOI] [PubMed] [Google Scholar]
- 26. D’Antò V, Bucci R, Franchi L, Rongo R, Michelotti A, Martina R. Class II functional orthopaedic treatment: a systematic review of systematic reviews. J Oral Rehabil. 2015;42:624‐642. [DOI] [PubMed] [Google Scholar]
- 27. Rongo R, Bucci R, Adaimo R, et al. Two‐dimensional versus three‐dimensional Frӓnkel Manoeuvre: a reproducibility study. Eur J Orthod. 2020;42:157‐162. [DOI] [PubMed] [Google Scholar]
- 28. Ehsani S, Nebbe B, Normando D, Lagravere MO, Flores‐Mir C. Short‐term treatment effects produced by the Twin‐block appliance: a systematic review and meta‐analysis. Eur J Orthod. 2015;37:170‐176. [DOI] [PubMed] [Google Scholar]
- 29. Aras I, Pasaoglu A. Class II subdivision treatment with the forsus fatigue resistant device vs intermaxillary elastics. Angle Orthod. 2017;87:371‐376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Linjawi AI, Abbassy MA. Dentoskeletal effects of the forsusTM fatigue resistance device in the treatment of class II malocclusion: a systematic review and meta‐analysis. J Orthod Sci. 2018;7:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Martina S, Di Stefano ML, Paduano FP, Aiello D, Valletta R, Paduano S. Evaluation of profile changes in class II individuals treated by means of herbst miniscope appliance. Dent J. 2020;8:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ruf S, Bock NC. Long‐term (≥15 years) effects of Class II treatment: a longitudinal and cross‐sectional study on signs and symptoms of temporomandibular disorders. Eur J Orthod. 2019;41:172‐179. [DOI] [PubMed] [Google Scholar]
- 33. Gerszewski C, Topolski F, Correr GM, Gomes RAP, Morais ND, Moro A. Dentoalveolar evaluation of lower incisors by Cbct after treatment with herbst appliance. Braz Dent J. 2018;29:562‐568. [DOI] [PubMed] [Google Scholar]
- 34. Harris K, Ojima K, Dan C, et al. Evaluation of open bite closure using clear aligners: a retrospective study. Prog Orthod. 2020;21:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zheng M, Liu R, Ni Z, Yu Z. Efficiency, effectiveness and treatment stability of clear aligners: a systematic review and meta‐analysis. Orthod Craniofac Res. 2017;20:127‐133. [DOI] [PubMed] [Google Scholar]
- 36. Ke Y, Zhu Y, Zhu M. A comparison of treatment effectiveness between clear aligner and fixed appliance therapies. BMC Oral Health. 2019;19:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author (VD) upon reasonable request.


