Abstract
Purpose
To investigate the attitudes and understanding of optometrists in the UK and Ireland towards Digital Eye Strain (DES), and to examine related practice patterns.
Methods
An anonymous online questionnaire was developed, covering attitude and understanding of DES, examination of patients who may be experiencing DES and approaches to management options. The questionnaire was promoted to UK and Ireland optometrists via professional bodies and local and area optometric committees.
Results
406 responses were included in the analysis. Most respondents agreed that DES was an important concern for optometrists (88.9%). 91.4% reported they felt confident in discussing possible symptoms of DES and management options; this was weakly and negatively associated with number of years qualified (r s = −0.198, p ≤ 0.001). Estimations of the proportion of patients affected by DES were lower than reports in the literature (median 25%, IQR 10%–50%). Most respondents always (60.6%) or frequently (21.9%) inquired about device usage in routine case history taking, and also asked follow‐up questions, although 29.3% only asked about the presence of symptoms half the time or less. Advising on regular breaks (84.0%), lubricants (55.7%) and environment/set up (69.2%) were felt to be extremely or very important by most respondents. Advising on specialist spectacle lenses, specifically blue filtering designs, was considered extremely or very important by 34.2% and 15.2%, respectively.
Conclusion
Given the agreement that DES is a significant issue causing frequent and persistent symptoms, and practitioners reported high levels of confidence in discussing DES, patients can expect to receive advice on symptoms and management from their optometrist. Simple management strategies were felt to be most important to advise on, with more uncertainty linked to specialist spectacle lenses.
Keywords: computer vision syndrome, digital eye strain, optometrists
Key Points.
Most respondents agreed that Digital Eye Strain is an important concern and reported confidence in discussing the syndrome, indicating that patients can expect to receive pertinent advice from optometrists.
Most optometrists reported incorporating questions about Digital Eye Strain in their routine case history, and many reported modification of the eye examination for patients who may be affected.
Respondents felt that simple management strategies for Digital Eye Strain were important; some uncertainty was associated with the use of specialist spectacle lenses for the syndrome.
INTRODUCTION
The substantial growth in use and ownership of digital devices over recent years has been well documented. It is accepted that most adults (and increasingly, children) 1 , 2 spend significant amounts of time on a daily basis using digital devices for professional, educational and/or lifestyle purposes. At the beginning of 2020, Ofcom research 3 highlighted that adults in the UK were spending over 25 h per week online, with internet access increasingly through portable devices (particularly smartphones) rather than conventional computers. With the ongoing COVID‐19 pandemic, screen time has increased further and the average daily time spent online for UK adults reached record levels at over 4 h per day in April 2020. 4 Notably, ‘time online’ does not encompass all screen time, and estimates suggest that typical adults spend around 40% of their waking hours viewing device screens. 5
‘Digital Eye Strain’ (DES), also referred to as ‘Computer Vision Syndrome,’ describes a range of eye and vision‐related symptoms which may occur with digital device usage, particularly for prolonged periods. 6 , 7 Symptoms of DES may be frequent and persistent, and negatively impact upon work productivity and accuracy in affected individuals. 8 , 9 The symptoms most commonly experienced are eyestrain, headaches, blurred vision or focussing problems, dry or irritable eyes and pain in the neck and shoulders. 7 , 10 , 11 Prevalence of the syndrome is high, with published reports over the last decade consistently estimating that 50% or more of regular device users experience DES symptoms, 11 , 12 , 13 including children. 14 Given the widespread changes to working practices, education and social activities due to COVID‐19, it is feasible that DES is now affecting more individuals than ever before.
A range of remedial options is available for the management of DES. The simple approach of taking frequent breaks away from screen viewing to look into the distance is commonly recommended, and is often referred to as the 20–20–20 rule (every 20 min, look at something 20 feet (6 m) away for 20 s). 7 , 15 , 16 Optimising workstation set up and device positioning 17 along with considering environmental factors such as room humidity 18 can also reduce symptoms. More specialised ophthalmic approaches include the management of refractive errors 19 and binocular vision anomalies 20 at the viewing distance of specific devices. A variety of specialist spectacle lenses have become commercially available for computer users in recent years, including options for ‘accommodative support’ for pre‐presbyopes and blue light filtering designs, although the evidence basis for clinical application of the latter in reducing DES has been questioned. 21 , 22 Considering the ocular surface, evaluation and treatment of dry eye 23 may minimise DES symptoms, and blinking exercises to optimise the efficacy of blinks during device usage have also been proposed. 24
Given the high prevalence of the syndrome, many optometrists will be examining multiple patients with DES each day. Furthermore, affected patients may reasonably expect specialist advice on management from their optometrist given the ocular and visual nature of most DES symptoms. However, little is known about how optometrists perceive the growing problem of DES and their approaches to identifying and managing patients who may be affected. 25 To date, no previous studies have assessed practitioners' knowledge and attitudes to DES, or whether current practice patterns are consistent with both the available research evidence in this field and guidance, such as from the College of Optometrists (UK) on examining display screen equipment (DSE) and/or computer users 26 and the use of blue filtering spectacle lenses. 22 Hence, the present study sought to survey UK and Irish optometrists' knowledge, attitudes and clinical practices regarding DES.
METHODS
The study received a favourable opinion from the Aston University Research Ethics Committee and was conducted according to the tenets of the Declaration of Helsinki. A web‐based survey of registered optometrists in the UK and Ireland was conducted, following a pilot version to optimise the coverage and comprehension. Participation was voluntary, and before beginning the survey, respondents were required to indicate their consent after reading the participant information and transparency statement. The participant information section highlighted that the survey was open only to UK and Ireland registered optometrists and respondents consented to participate in line with the information provided. The questionnaire was anonymous, although respondents had the option of providing their email address if they wished to be informed of the results of the study. No financial incentive was provided to respondents.
Sample and materials
Qualified optometrists registered in the UK and Ireland were eligible to participate in the study. The number of optometrists in the UK and Ireland combined is approximately 17,800 based on circa 17,000 optometrists in the UK 27 and circa 800 in Ireland. 28 For 95% confidence and a ± 5% margin of error in responses, a sample size of 376 responses was required for the survey. 29
The questionnaire was designed to examine the attitude towards, and understanding of, DES by optometrists; how optometrists approach the examination of patients who may be affected by DES and the opinions of optometrists towards various management options. Following initial development of the questionnaire by academic optometrists with research interests in Digital Eye Strain and the ocular surface/dry eye, a pilot online survey of eligible respondents was undertaken to obtain feedback on the relevance and ease of understanding of the items. Minor changes to the survey items were made following feedback from the pilot; none of the 19 pilot responses were included in the final analysis.
The questionnaire was hosted by Online Surveys (onlinesurveys.ac.uk), a General Data Protection Regulation (GDPR) compliant platform designed for academic research. The survey consisted of 22 items in four key areas: respondent details (three items); attitude and understanding of DES (six items); examination of possible DES sufferers (seven items) and management of DES (seven items). A summary of the final questionnaire is shown in Table 1 . Following the section collecting data on participant demographics, 14 of the remaining 19 items gathered ordinal responses using 5‐point scales allowing neutral responses. A Likert‐type scale was used to measure agreement with attitude statements (e.g., Digital Eye Strain is an important concern for optometrists), a reported frequencies scale was used for behaviours (e.g., How often do you ask patients about their computer or digital device use during routine case history?) and a stated importance scale for the various management options (e.g., How important do you think it is to advise on taking regular breaks and looking into the distance for Digital Eye Strain?). 30 Three items in the attitude and understanding of DES section required free‐text responses (What do you understand by the term Digital Eye Strain? What percentage of patients attending your clinic do you believe are affected by Digital Eye Strain? What do you consider to be the typical symptoms of Digital Eye Strain?). Respondents also had the opportunity to provide free‐text responses to those items linked to: modification of the eye examination routine for patients who may be affected by DES; advice given regarding office environment and workstation set up; names of preferred (if any) topical lubricants, specialist spectacle lenses and blue‐blocking lenses. Additionally, the final item of the survey asked for any other comments respondents wished to provide linked to DES and optometric management. Within the survey, if respondents reported that they ‘never’ asked patients about their use of digital devices, the subsequent four questions linked to case history were skipped. Similarly, if respondents stated that they ‘never’ modified their routine eye examination for patients who may be affected by DES, the associated question about clinical tests performed was skipped. The approximate time required for respondents to complete the full survey was 10 min.
TABLE 1.
Summary of 22‐item Digital Eye Strain questionnaire for optometrists in the UK and Ireland, hosted on Online Surveys
| Section | Question numbers | Summarised questions |
|---|---|---|
| About you | 1–3 |
Main practice setting. Country of practice. Number of years since qualification. |
| Attitude towards and understanding of DES | 4–9 |
Importance of DES to optometrists. Understanding of the term ‘DES.’ Proportion of patients believed to be affected by DES. Typical symptoms of DES. Level of agreement that DES can cause frequent and persistent symptoms. Confidence discussing DES symptoms. |
| Examination of those possibly affected by DES | 10–16 |
Frequency of asking re: digital device usage in routine case history. Frequency of asking re: type of device(s) used. Frequency of asking re: time spent on device(s). Frequency of asking re: working distance of device(s). Frequency of asking re: symptoms of DES. Frequency of modifying eye examination for those possibly affected by DES. Clinical tests performed if examination modified. |
| Management of DES | 17–22 |
Importance of regular breaks. Importance of topical lubricants. Importance of advising on environment and workstation set up. Importance of specialist spectacle lenses. Importance of ‘blue‐blocking’ spectacle lenses. Any other comments re: optometric management of DES. |
The survey was open between October 2020 and February 2021. All local or area optometric committees in the UK and the Association of Optometrists (Ireland) were contacted by email by the research team to request circulation of an invitation to their membership to participate in the research or promotion via their social media. Following a request to the College of Optometrists (UK) research team, a Tweet also promoted the survey to College followers.
Following closure of the survey, data were exported into Excel (Microsoft, microsoft.com) for initial analysis and cleaned by 2 members of the research team (PAM and ALS) to remove any inappropriate responses (e.g., incomplete answers). For items evaluating agreement with a statement, responses were grouped into three categories: Agree (Strongly Agree + Agree); Neither Agree or Disagree (No Opinion) and Disagree (Strongly Disagree + Disagree). This grouping was used to enable expression of whether respondents felt generally favourable, neutral or unfavourable to the statements. Item 6 asked respondents to indicate numerically the percentage of patients attending their clinic who they believed were affected by DES; if respondents indicated a range of values, then the midpoint value was included in the analysis, whilst non‐numeric responses were removed. The median and interquartile range were calculated. Spearman's r was used to examine the relationship between number of years since qualification and (1) level of agreement with DES being an important concern for optometrists and (2) level of confidence in discussing symptoms and advising on management options. A p value of <0.05 was considered significant. For items involving free text responses, answers were manually coded and assigned to categories by a single investigator (PAM) before being reviewed by the other investigators (ALS and JSW); this process was conducted using Excel where responses with the same theme were grouped together (e.g., eye strain, asthenopia, ocular fatigue, were grouped together in the ‘symptoms’ question).
RESULTS
Profile of respondents
Four hundred and 10 responses were received in total; four responses in which the country of registration (Ireland or UK) had not been stated were removed from the analysis. Approximately 2.3% of registered optometrists in Ireland and the UK completed the survey and with 406 responses in the final analysis, the required sample size of 376 was surpassed. Of the respondents, 327 (80.5%) were based in the UK and 79 (19.5%) in Ireland. Table 2 illustrates the number of years registered and main practice setting of respondents; the most common main practice types were independent (46.6%) and large multiple (33.7%).
TABLE 2.
Number of years registered as an optometrist and main practice setting of respondents, n = 406
| Years registered | Main practice setting | ||
|---|---|---|---|
| Percentage (n) | Percentage (n) | ||
| 0–5 years | 16.7 (68) | Independent | 46.6 (189) |
| 6–10 years | 13.5 (55) | Large multiple | 33.7 (137) |
| 11–15 years | 12.6 (51) | Small multiple | 6.7 (27) |
| 16–20 years | 15.3 (62) | Education/academic | 5.9 (24) |
| 21–25 years | 13.1 (53) | Public hospital | 3.7 (15) |
| ≥26 years | 28.8 (117) | Private hospital | 1.7 (7) |
| Other | 1.7 (7) | ||
Attitude towards and understanding of Digital Eye Strain
Most respondents agreed that DES was an important concern for optometrists (88.9%) and that it may cause frequent and persistent symptoms for sufferers (91.9%). Most respondents reported they felt confident in discussing possible symptoms of DES and management options with patients (91.4%, Table 3 ). There was no significant relationship between number of years qualified and agreement that DES was an important concern for optometrists (p = 0.40), and although respondents who had been qualified for longer periods were less likely to agree that they felt confident in discussing DES with patients, the relationship between the variables was weak (r s = −0.198, p < 0.001).
TABLE 3.
Attitude towards DES, n = 406
| Percentage (n) | |||
|---|---|---|---|
| Agree | Disagree | Neither agree or disagree | |
| DES is an important concern for optometrists | 88.9 (361) | 6.2 (25) | 4.9 (20) |
| DES may cause frequent and persistent symptoms for sufferers | 91.9 (373) | 3.0 (12) | 5.2 (21) |
| I feel confident discussing ocular symptoms associated with computer usage and advising on management options | 91.4 (371) | 3.2 (13) | 5.4 (22) |
Figure 1 illustrates respondents' estimates of the proportion of patients attending their clinic whom they believe are affected by DES; 392 valid numerical responses were received for this item. Overall, the median response was 25% (IQR = 10%–50%), with 59.7% of respondents estimating that 30% or fewer of their patients are affected.
FIGURE 1.
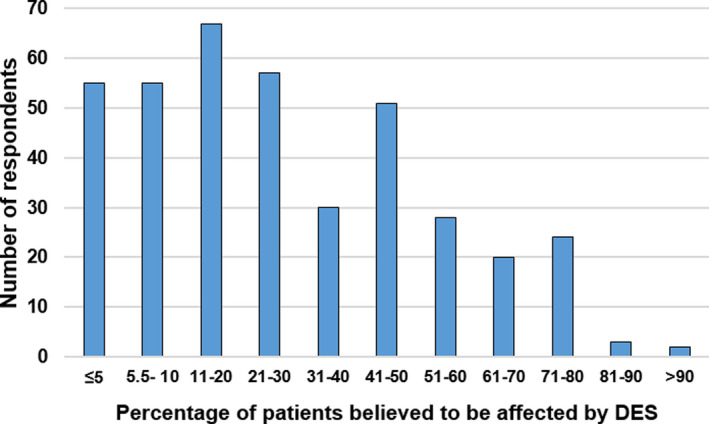
Practitioner perceptions of the proportion of patients attending their clinic who they believe are affected by DES, n = 392
Regarding practitioner understanding of DES, out of 388 valid written responses, 4 respondents (1.0%) indicated they were unsure of the meaning of DES, whilst 3 (0.8%) expressed scepticism/disbelief regarding the existence of DES. Of the remaining 381 responses, most (90.3%) included reference to use of some form of screen‐based technology leading to symptoms, and 65.6% alluded to a variety of digital devices (rather than just conventional personal computers) being implicated. Of the symptoms that respondents associated with DES, 93.9% referred to more than one key symptom, with the most frequently cited key symptoms being asthenopia or eye strain/fatigue (72.6%), headache (64.7%), dry or irritated eyes (56.0%) and focussing difficulties or blurred vision (48.8%). Table 4 details the symptoms respondents associated with DES.
TABLE 4.
Key symptoms of DES cited by n = 391 optometrist respondents
| Symptom | Percentage of respondents citing (n) |
|---|---|
| Asthenopia or eye strain/ fatigue | 72.6 (284) |
| Headache | 64.7 (253) |
| Dry or irritated eyes | 56.0 (219) |
| Focussing issues or blurred vision | 48.8 (191) |
| Ocular soreness or redness | 35.8 (140) |
| Non‐specific discomfort | 6.6 (26) |
| Photophobia or glare | 6.1 (24) |
| Binocular vision disturbance e.g. diplopia | 3.6 (14) |
| Musculoskeletal issues | 3.1 (12) |
| Insomnia | 1.5 (6) |
| Lid twitching | 1.0 (4) |
| Don't know | 0.5 (2) |
Digital Eye Strain and the eye examination
Figure 2 illustrates the frequency of respondents asking various questions regarding digital device usage during routine case history taking. Most respondents (82.5%) reported that they always (60.6%) or frequently (21.9%) asked patients regarding their use of digital devices, with only 5.1% reporting they infrequently asked. Zero respondents reported that they never asked about device usage. Amongst respondents that asked about their patients' device usage, 78.8% always or frequently asked about the type of device, whilst 75.1% always/frequently asked about usage time per day and 9.1% reported that they infrequently or never asked regarding these details. Information about working distance was ascertained by a similar proportion of respondents, with 74.1% always or frequently asking and 9.3% asking infrequently or never. Asking about the presence of symptoms with device usage received the fewest ‘always’ responses (32.0%) of the case history questions, although 38.7% also reported they frequently asked; 13.8% infrequently or never asked regarding the presence of symptoms.
FIGURE 2.
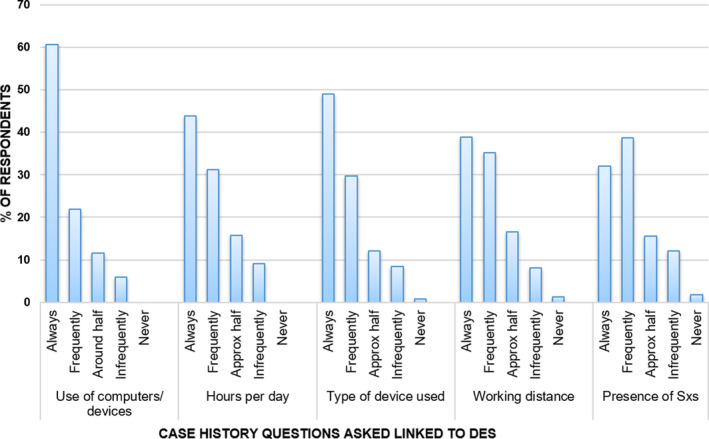
Frequency of asking questions regarding digital device usage during routine case history, n = 406. Sxs, symptoms
Regarding the clinical elements of the eye examination, 63.5% of respondents reported that they always or frequently modified the eye examination for patients who may be affected by DES; 19.7% did so infrequently or never. The modifications cited were: assessment of acuity at the specific distance of the device (81.5%); slit lamp biomicroscope examination of the ocular surface (79.1%); other dry eye assessment techniques (67.7%); near point of convergence (50.7%); cover test at working distance of device (43.1%); amplitude of accommodation (36.5%); fixation disparity at working distance of device (25.1%) and use of a dry eye questionnaire (7.9%). Other modifications including dynamic retinoscopy, accommodative facility, macular pigment optical density, contrast sensitivity, AC/A ratio, range of clear vision and effect of a small amount of extra positive sphere power were each cited by less than 1% of respondents.
Attitude towards management options
Figure 3 illustrates respondents' attitudes towards the importance of advising on the various management options for DES. Advising on regular breaks was considered to be extremely or very important by most respondents (84.0%), with only 2.0% reporting that this was not so/ not at all important. Advising on ocular lubricants and workstation set up was felt to be extremely or very important by 55.7% and 69.2% of respondents respectively, with just 6.4% and 3.9% of respondents, respectively, stating they felt advising on these was not so/not at all important. Details of advice given regarding environment/workstation set up was provided by 252 respondents (62.1%). Of these responses, discussion of screen/desk/chair height was the most common recommendation, cited by 65.1%, followed by consideration of working distance (49.6%), environmental factors such as humidity and air conditioning (44.0%), optimising lighting (40.1%) and avoiding glare (25.4%).
FIGURE 3.
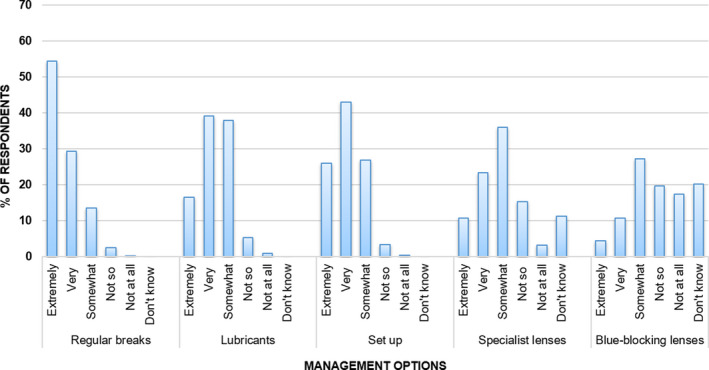
Respondents' perceptions of the importance of advising patients on various management options for DES, n = 406
More mixed responses were received regarding the use of spectacle lenses for DES. For specialist spectacle lenses in general, 34.2% felt these were extremely or very important, whilst a substantial minority (11.3%) reported that they did not know how important it was to advise on these. Information on the lens type(s) they recommended for patients with DES was provided by 203 respondents; amongst these responses ‘office’ type lenses were most commonly cited (54.7%), followed by anti‐reflective coated (26.1%) and blue‐filtering lenses (25.1%). Accommodative support lenses and prescribing a refractive correction specific for the working distance were each mentioned by 17.7%.
Few respondents felt that specific ‘blue‐blocking’ lenses were extremely (4.4%) or very important (10.8%) in the management of DES; 27.3% indicated they were somewhat important, while 37.2% felt they were not so/not at all important and 20.2% reported that they did not know. One hundred and forty one respondents (34.7%) indicated that they advised on the use of these, with Essilor (29.1% of 141 respondents to this sub‐question), own‐brand (27.0%), Hoya (14.9%) and Zeiss (12.8%) variants being most commonly cited.
DISCUSSION
This cross‐sectional study of the attitudes, knowledge and practice patterns of optometrists in the UK and Ireland included a diverse range of respondents, with a broad range of clinical experience and practice settings. The results of the survey highlight that optometrists in the UK and Ireland consider DES to be a significant issue for professionals, and a complaint that can cause frequent and persistent symptoms in those affected. A high level of confidence in discussing DES with patients and advising on available management options was identified. Together, these findings indicate that patients presenting to their optometrist with DES can expect to receive advice on symptoms and how to manage them.
Respondents' estimates of the proportion of patients in clinic affected by DES (median 25%; IQR 10%–50%) were generally lower than the prevalences of the syndrome reported in relatively recent studies. Amongst office workers, DES prevalence has been reported as 53% in Spanish civil servants using a validated questionnaire, 31 and in New York City‐based workers, approximately 40% experienced tired eyes ‘at least half of the time’. 11 A large‐scale US‐based survey of the general population (rather than computer workers specifically), found an overall self‐reported prevalence of 65%, 13 and a recent study based in Saudi Arabia reported a 78% prevalence of DES during COVID‐19 restrictions. 32 Gauging DES prevalence remains a challenge, with a range of diagnostic criteria used in previous studies, 25 although the estimates provided by respondents in the present study do appear to be low. The low estimates could be reflective of the practice types of many respondents and an assumption that older individuals, who often comprise a large part of the patient base for community optical practices, are less likely to experience DES. There is a paucity of published evidence regarding the prevalence and impact of DES amongst older individuals, although it is known that amongst older age groups, engagement with digital devices and internet use has increased substantially in recent years, 33 , 34 and the positive correlation between DES and dry eye symptoms 11 suggests that a significant proportion are indeed likely to be affected.
The role of a range of digital devices was highlighted in approximately two thirds (65.6%) of responses to the question ‘What do you understand by the term Digital Eye Strain?’ Many studies have reported on ocular and visual symptoms arising from the extended use of tablets, smartphones and mobile reading devices. 35 , 36 , 37 , 38 Whilst the aetiology of associated symptoms may be different compared to conventional computers (due to size, positioning and viewing angle), 39 it is accepted that use of these types of device can lead to DES. Consequently, the term ‘Digital Eye Strain’ has been advocated rather than ‘Computer Vision Syndrome.’ 25 , 40 The potential for multiple symptoms to be experienced due to DES was recognised by most respondents (93.9%), and the symptoms most frequently stated (eye fatigue and asthenopia, headache, dry eyes and focusing issues) were in alignment with commonly reported symptoms from previous studies. 11 , 31 , 32 Only a small proportion of respondents (3.1%) cited musculo‐skeletal symptoms such as neck and shoulder pain. Musculo‐skeletal impacts have been included as part of the syndrome by numerous authors and organisations such as the American Optometric Association, 7 and may be largely attributable to improper posture and/or device positioning, 20 although there are ophthalmic prescribing implications, particularly for presbyopic patients, in ensuring that prescriptions are appropriate for the required task distance and gaze angle. 40
Regarding routine case history taking, most respondents (82.5%) reported that they always or frequently asked about digital device usage. Importantly, information about type of device (78.8%), usage time (75.1%) and working distance (74.1%) was usually gathered by respondents. Each of these factors can influence the likelihood of symptoms and approaches to management. Gaze angle (and therefore palpebral aperture size and tear film distribution) will vary with different types of device, which in turn can impact upon symptoms. However, understanding of the interrelationship between device position/gaze angle and symptoms is limited by some ambiguity in previous studies as to whether angles represent eye rotation only or include neck flexion. 39 , 41 Text size on some devices may be a problem, particularly with smartphones, where the visual acuity demand can be approximately 6/6. 42 Given that a two‐times acuity reserve (i.e., threshold acuity of 6/3 for a 6/6 demand level) is needed for comfortable prolonged reading from a digital device in younger age groups, and a higher reserve is needed for older patients or those with visual deficits, 43 small text size can be a significant contributor to DES symptoms. Information about both the type of device and working distance/position are useful in understanding the ergonomics of use and in the provision of appropriate advice for the patient, 44 as highlighted in the College of Optometrists' guidance on examining patients who work with display screen equipment. 26 Linked to usage time, it has been reported in many previous studies that the severity of DES symptoms increases with longer durations of use, and contact lens wearers may be particularly susceptible to symptoms following extended periods of use. 12 Notably, the presence of symptoms with device usage was asked least frequently by respondents, with 29.3% reporting that they asked around half the time (15.5%) or less (13.8%), suggesting that many affected patients may not be receiving appropriate advice on management/avoidance of symptoms.
The most commonly cited modifications of the eye examination for patients who may be experiencing DES were assessment of acuity at the working distance of the device(s) and slit lamp biomicroscope examination of the ocular surface. Appropriate correction of refractive error is important for digital device users, with uncorrected (simulated) astigmatism of as little as 0.50–1.00 DC having been shown to have a detrimental effect on subjective comfort with computer use 19 ; an effect which may be a particular problem amongst contact lens wearers with residual astigmatism 45 or presbyopic users of ‘ready‐made readers.’ 25 Furthermore, any near add must be appropriate for the individual's habitual activities, recognising that multitasking with digital (and non‐digital) tasks will likely involve a range of viewing distances and gaze angles. 13 , 32 Recent research indicates that the typical viewing distance for presbyopic smartphone users is 39.0 cm, whereas minimum distances of 50.0–63.5 mm have been recommended for desktop screens. 46 , 47 Most respondents indicated they would assess the ocular surface or evaluate other indicators of dry eye, and many reported use of accommodation and binocular vision tests in DES, highlighting that factors leading to both internal and external symptoms are being investigated by those who modify their routine in patients experiencing DES. However, with 36.5% of respondents adapting the eye examination around half the time or even less frequently, factors contributing to the development of DES may not be explored in a significant proportion of patients.
In line with research demonstrating the beneficial effects of regular breaks on subjective comfort and working efficiency, 48 , 49 and recommendations from organisations such as the College of Optometrists, 50 most respondents felt advising on breaks was important in the management of DES. Environmental factors and workstation set up were also perceived as important areas for advice. Ergonomic and environmental considerations for comfortable computer use include lighting and glare, screen and hardware positions, workstation furniture and temperature/air quality, and are covered by the Health and Safety Executive (HSE) guidance. 51
The use of specialist spectacle lenses in DES management was an area of less confidence amongst respondents, with 11.3% reporting they did not know how important it was to advise on these and just 34.2% feeling that they were extremely or very important. Apprehension regarding the value of blue‐filtering lenses in DES was apparent, with just 15.2% of respondents indicating that advising on these was extremely/very important, and 57% reporting that these were not of value, or they did not know, although 34.7% reported that they did advise on particular blue‐filtering lens types. Similar scepticism from the profession regarding blue‐filtering spectacle lenses was reported by Singh et al. 52 following a survey of Australian optometrists, where most respondents (89.2%) felt that the quality of evidence to support the use of the lenses in DES was low or moderate, and only 3.8% felt that there was high quality evidence in this area. Despite concerns regarding available evidence, three quarters of Australian optometrists reported that they recommended these in practice, with the most common reasons being device usage and suspected DES. In both studies, an appreciation of the lack of good quality evidence in this field is apparent (in line with the College of Optometrists’ position statement on blue‐blocking spectacle lenses), 22 although they were still recommended by many respondents which may be reflective of commercial pressures within optometry, or the belief of an associated placebo effect. 52 Presently, there is also limited evidence for the efficacy of accommodative support lenses, which offer progressive low addition powers, to reduce symptoms of digital eye strain in pre‐presbyopes. A recent double‐blinded randomised control trial of low add powers 53 did report that a +0.75 add was preferred compared with a control lens or +0.50 or +1.25 add powers by pre‐presbyopic DES sufferers, although only the immediate effect was examined. Additional research on the potential longer‐term benefits of accommodative support lenses in alleviating DES symptoms would be valuable. With a range of specialist lens types now available for both pre‐presbyopic and presbyopic heavy users of digital devices and office workers, this could represent an area where more professional education, based on the latest available scientific evidence, would be of value. Resources such as continuing professional development articles and events, guidance from professional bodies and editorial pieces may all be of value in supporting practitioners to engage with the latest relevant research findings and apply these to practice.
Similar to previous surveys of the profession, a limitation of the present study is that optometrists motivated by personal interest in the topic may be more likely to respond than others (i.e., it is a self‐selected sample), 54 leading to a possible overestimation of confidence/skills in this area of practice compared to the profession as a whole. Random sampling of the profession could have been employed, e.g., through direct email to randomised members of the College of Optometrists, as employed by Dabasia et al., 54 although not all optometrists are members of the College and this would not overcome the issue of those with a particular interest in the topic being most likely to respond. The 406 respondents represent around 2.3% of optometrists registered in the UK and Ireland, with the response profile of UK respondents aligning reasonably closely to that of optometrists in the 2015 Optical Workforce Survey, 55 where most respondents worked primarily in independent/small group practice (52.7%) or for a national company (32.7%). In the present study, UK respondents were mainly from independent/small group practice (52.7%) or large multiples (36.4%). Amongst responses from Ireland (19.5%), a smaller proportion of respondents worked mainly in large multiples (24.1%) compared to the UK, but more were from the private hospital sector (7.6% vs 0.3%).
It has been reported previously that practice patterns determined from survey‐based research may not be reflective of true practice, with respondents tending to report higher standards of practice than may actually apply. 56 It is feasible, therefore, that the results linked to case history questioning and modification of the eye examination may overestimate the frequency of enquiring regarding DES and undertaking investigations linked to the syndrome in patients who may be affected. Analysis of case records or use of clinical vignettes 57 could be used in future research to better understand practice in this area. Such approaches could also facilitate the investigation of additional aspects such as the clinical signs identified in patients with DES, recommended management options and follow‐up of affected individuals.
CONCLUSION
The present study provides a valuable insight into the attitudes and practice patterns of optometrists in the UK and Ireland regarding the growing issue of DES. Given that optometrists consider DES to be both a significant problem for affected individuals and an important concern for optometrists, and most respondents reported they felt confident discussing DES with patients, the findings indicate that patients experiencing the syndrome can expect to receive useful clinical input from their optometrist. Overall, estimates of the proportion of patients affected by DES were significantly lower than reported prevalences in the scientific literature, and whilst most respondents indicated they asked patients about their device usage in routine case history taking, more routine questioning specifically linked to symptoms could help to identify a greater number of affected individuals. Respondents felt advising on frequent breaks, ocular lubricants and workstation/device set up were the most important management considerations, with more mixed views on specialist spectacle lenses for DES, particularly ‘blue‐filtering’ designs, although a significant proportion of respondents did indicate that they recommended these options. Spectacle lens prescribing in DES may represent an area where further professional education would be of value.
CONFLICT OF INTEREST
PAM reports no conflicts of interest and no authors have proprietary interest in any of the materials mentioned in this article. ALS receives an honorarium for consultancy from Bausch and Lomb. JSW receives honoraria for consultancy from from AtiaVision, Bausch and Lomb, Alcon, CooperVision, Johnson and Johnson Vision, Nevakar, Novartis and Thea Pharmaceutical. No commercial organisation was involved with any aspect of the study.
AUTHOR CONTRIBUTIONS
Patrick A Moore: Data curation (equal); Investigation (lead); Methodology (supporting); Project administration (lead); Writing‐original draft (supporting); Writing‐review & editing (supporting). James Wolffsohn: Conceptualization (equal); Methodology (equal); Supervision (supporting); Writing‐review & editing (supporting). Amy L Sheppard: Conceptualization (equal); Data curation (equal); Formal analysis (equal); Methodology (equal); Writing‐original draft (lead).
Moore PA, Wolffsohn JS, Sheppard AL. Attitudes of optometrists in the UK and Ireland to Digital Eye Strain and approaches to assessment and management. Ophthalmic Physiol Opt. 2021;41:1165–1175. 10.1111/opo.12887
REFERENCES
- 1. Madigan S, Browne D, Racine N, Mori C, Tough C. Association between screen time and children’s performance on a developmental screening test. JAMA Pediatr 2019;173:244–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chen W, Adler JL. Assessment of screen exposure in young children, 1997 to 2014. JAMA Pediatr 2019;173:391–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ofcom ofcom.org.uk/__data/assets/pdf_file/0031/196375/adults‐media‐use‐and‐attitudes‐2020‐report.pdf
- 4. Ofcom UK’s internet use surges to record levels. 2020. Available at: Ofcom.org.uk/about‐Ofcom.latest/features‐and‐news/uk‐internet‐use‐surges Accessed April 19, 2021.
- 5. Ofcom . Media Nations 2020. 2020. Available at: ofcom.org.uk/research‐and‐data/tv‐radio‐and‐on‐demand/media‐nations‐reports/media‐nations‐2020#:~:text=This%20is%20Ofcom's%20third%20annual,radio%20and%20other%20audio%20sectors Accessed April 21, 2021.
- 6. Rosenfield M. Computer vision syndrome: a review of ocular causes and potential treatments. Ophthalmic Physiol Opt 2011;31:502–515. [DOI] [PubMed] [Google Scholar]
- 7. American Optometric Association . Computer vision syndrome. 2021. Available at: aoa.org/healthy‐eyes/eye‐and‐vision‐conditions/computer‐vision‐syndrome?sso=y Accessed May 20, 2021.
- 8. Daum KM, Clore KA, Simms SS, et al. Productivity associated with visual status of computer users. Optometry 2004;75:33–47. [DOI] [PubMed] [Google Scholar]
- 9. Wilkinson RT, Robinshaw HM. Proof‐reading: VDU and paper text compared for speed, accuracy and fatigue. Behav Inform Technol 1987;6:125–133. [Google Scholar]
- 10. Blehm C, Vishnu S, Khattak A, Mitra S, Yee RW. Computer vision syndrome: a review. Surv Ophthalmol 2005;50:253–262. [DOI] [PubMed] [Google Scholar]
- 11. Portello JK, Rosenfield M, Bababekova Y, Estrada JM, Leon A. Computer‐related visual symptoms in office workers. Ophthalmic Physiol Opt 2012;32:375–382. [DOI] [PubMed] [Google Scholar]
- 12. Tauste A, Ronda E, Molina MJ, Segui M. Effect of contact lens use on computer vision syndrome. Ophthalmic Physiol Opt 2016;36:112–119. [DOI] [PubMed] [Google Scholar]
- 13. The Vision Council . Eyes overexposed: the digital device dilemma. 2016 Digital Eye Strain Report. 2016. Available at: thevisioncouncil.org/ Accessed May 25, 2021.
- 14. Mohan A, Sen P, Shah C, Jain E, Jain S. Prevalence and risk factor assessment of digital eye strain among children using online e‐learning during the COVID‐19 pandemic: digital eye strain among kids (DESK study‐1). Indian J Ophthalmol 2021;69:140–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. American Academy of Ophthalmology . Computers, digital devices and eye strain. 2021. Available at: aao.org/eye‐health/tips‐prevention/computer‐usage Accessed May 25, 2021.
- 16. Alghamdi WM, Alrasheed SH. Impact of an educational intervention using the 20/20/20 rule on computer vision syndrome. African Vis Eye Health 2020;79:a554. 10.4102/aveh.v79i1.554 [DOI] [Google Scholar]
- 17. Anshel J. Computer vision syndrome. In: Anshel J, editor. Visual ergonomics handbook. Boca Raton, FL: CRC Press; 2005. [Google Scholar]
- 18. Wang MTM, Chan E, Ea L, et al. Randomized trial of desktop humidifier for dry eye relief in computer users. Optom Vis Sci 2017;94:1052–1057. [DOI] [PubMed] [Google Scholar]
- 19. Wiggins NP, Daum KM. Visual discomfort and astigmatic refractive errors in VDT use. J Am Optom Assoc 1991;62:680–684. [PubMed] [Google Scholar]
- 20. Sheedy JE, Parsons SD. The Video Display Terminal Eye Clinic: clinical report. Optom Vis Sci 1990;67:622–626. [DOI] [PubMed] [Google Scholar]
- 21. Lawrenson JG, Hull CC, Downie LE. The effect of blue‐light blocking spectacle lenses on visual performance, macular health and the sleep‐wake cycle: a systematic review of the literature. Ophthalmic Physiol Opt 2017;37:644–654. [DOI] [PubMed] [Google Scholar]
- 22. College of Optometrists . Blue blocking spectacle lenses: position statement. 2018. Available at: college‐optometrists.org/the‐college/policy/position‐statements/blue‐blocking‐spectacle‐lenses.html Accessed May 25, 2021.
- 23. Acosta MC, Gallar J, Belmonte C. The influence of eye solutions on blinking and ocular comfort at rest and during work at video display terminals. Exp Eye Res 1999;68:663–669. [DOI] [PubMed] [Google Scholar]
- 24. Portello JK, Rosenfield M, Chu CA. Blink rate, incomplete blinks and computer vision syndrome. Optom Vis Sci 2013;90:482–487. [DOI] [PubMed] [Google Scholar]
- 25. Sheppard AL, Wolffsohn JS. Digital eye strain: prevalence, measurement and amelioration. BMJ Open Ophthalmol 2018;3:e000146. 10.1136/bmjophth-2018-000146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. College of Optometrists . Examining patients who work with display screen equipment or computers. 2021. Available at: guidance.college‐optometrists.org/home/ Accessed May 10, 2021.
- 27. General Optical Council . General optical council annual report 2019‐20. 2020. Available at: optical.org/en/news_publications/Publications/annual_reports_archive.cfm Accessed May 16, 2021.
- 28. FODO Ireland . Optical sector survey. 2018. Available at: fodoireland.ie/Publications/2018/FODO%20Ireland%20Optical%20Sector%20Survey%20Report.pdf Accessed April 15, 2021.
- 29. Bartlett JE, Kotrlik JW, Higgins CC. Organisational research: determining appropriate sample size in survey research. Inf Technol Learn Perform J 2001;19:43–50. [Google Scholar]
- 30. Rabe‐Hesketh S, Skrondal A. Generalized linear mixed models. In: Peterson P, Baker E, McGaw B, editors. International encyclopedia of education. 3rd ed. Oxford, UK: Elsevier; 2010. p. 171–177. [Google Scholar]
- 31. Segui Mdel M, Cabrero‐Garcia J, Crespo A, Verdu J, Ronda E. A reliable and valid questionnaire was developed to measure computer vision syndrome at the workplace. J Clin Epidemiol 2015;68:662–673. [DOI] [PubMed] [Google Scholar]
- 32. Alabdulkader B. Effect of digital device use during COVID‐19 on digital eye strain. Clin Exp Optom 2021;22:1–7. [DOI] [PubMed] [Google Scholar]
- 33. Hunsaker A, Hargittai E. A review of Internet use among older adults. New Media Soc 2018;20:3937–3954. [Google Scholar]
- 34. Chang J, McAllister C, McCaslin R. Correlates of, and barriers to, internet use among older adults. J Gerontol Soc Work 2015;581:66–85. [DOI] [PubMed] [Google Scholar]
- 35. Moon JH, Kim KW, Moon NJ. Smartphone use is a risk factor for pediatric dry eye disease according to region and age: a case control study. BMC Ophthalmol 2016;16:188. 10.1186/s12886-016-0364-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dj K, Lim CY, Gu N, Park CY. Visual fatigue induced by viewing a tablet computer with a high‐resolution display. Korean J Ophthalmol 2017;31:388–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Maducdoc MM, Haider A, Nalbandian A, et al. Visual consequences of electronic reader use: a pilot study. Int Ophthalmol 2017;37:433–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Long J, Cheung R, Duong S, Paynter R, Asper L. Viewing distance and eyestrain symptoms with prolonged viewing of smartphones. Clin Exp Optom 2017;100:133–137. [DOI] [PubMed] [Google Scholar]
- 39. Jaiswal S, Asper L, Long J, et al. Ocular and visual discomfort associated with smartphones, tablets and computers: what we do and do not know. Clin Exp Optom 2019;102:463–477. [DOI] [PubMed] [Google Scholar]
- 40. Rosenfield M. Computer vision syndrome (A.K.A. digital eye strain). Optom Pract 2016;17:1–10. [Google Scholar]
- 41. Köpper M, Mayr S, Buchner A. Reading from computer screen versus reading from paper: does it still make a difference? Ergonomics 2016;59:615–632. [DOI] [PubMed] [Google Scholar]
- 42. Bababekova Y, Rosenfield M, Hue JE, Huang RR. Font size and viewing distance of handheld smart phones. Optom Vis Sci 2011;88:795–797. [DOI] [PubMed] [Google Scholar]
- 43. Kochurova O, Portello JK, Rosenfield M. Is the 3x reading rule appropriate for computer users? Displays 2015;38:38–43. [Google Scholar]
- 44. Coles‐Brennan C, Sulley A, Young G. Management of digital eye strain. Clin Exp Optom 2019;102:18–29. [DOI] [PubMed] [Google Scholar]
- 45. Wiggins NP, Daum KM, Snyder CA. Effects of residual astigmatism in contact lens wear on visual discomfort in VDT use. J Am Optom Assoc 1992;63:177–181. [PubMed] [Google Scholar]
- 46. German DIN 66234 . Characteristic values for the adaptation of workstations with fluorescent screens to humans. Parts 1‐9. Berlin, Germany: German DIN Association; 1981. [Google Scholar]
- 47. Ankum DR. Viewing distance at computer workstations. Workplace Ergon 1996;2:10–13. [Google Scholar]
- 48. Galinsky T, Swanson N, Sauter S, et al. Supplementary breaks and stretching exercises for data entry operators: a follow‐up field study. Am J Ind Med 2007;50:519–527. [DOI] [PubMed] [Google Scholar]
- 49. McLean L, Tingley M, Scott RN, Rickards J. Computer terminal work and the benefit of microbreaks. Appl Ergon 2001;32:225–237. [DOI] [PubMed] [Google Scholar]
- 50. College of Optometrists . Winter eye health. 2020. Available at: college‐optometrists.org/the‐college/media‐hub/media‐campaigns/winter‐eye‐health.html Accessed May 5, 2021.
- 51. Health and Safety Executive . Display screen equipment (DSE) workstation checklist. 2021. Available at: hse.gov.uk/pubns/ck1.htm Accessed May 15, 2021.
- 52. Singh S, Anderson AJ, Downie LE. Insights into Australian optometrists’ knowledge and attitude towards prescribing blue light‐blocking ophthalmic devices. Ophthalmic Physiol Opt 2019;39:194–204. [DOI] [PubMed] [Google Scholar]
- 53. Yammouni R, Evans BJW. An investigation of low power convex lenses (adds) for eyestrain in the digital age (CLEDA). J Optom 2020;13:198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Dabasia PL, Edgar DF, Garway‐Heath DF, Lawrenson JG. A survey of current and anticipated use of standard and specialist equipment by UK optometrists. Ophthalmic Physiol Opt 2014;34:592–613. [DOI] [PubMed] [Google Scholar]
- 55. College of Optometrists . The optical workforce survey: full report. 2015. Available at: college‐optometrists.org/the‐college/research/research‐projects/optical‐workforce‐survey2.html Accessed May 25, 2021.
- 56. Theodossiades J, Myint J, Murdoch IE, Edgar DF, Lawrenson JG. Does optometrists’ self‐reported practice in glaucoma detection predict actual practice as determined by standardised patients? Ophthalmic Physiol Opt 2012;32:234–241. [DOI] [PubMed] [Google Scholar]
- 57. Shah R, Edgar DF, Evans BJ. A comparison of standardised patients, record abstraction and clinical vignettes for the purpose of measuring clinical practice. Ophthalmic Physiol Opt 2010;30:209–224. [DOI] [PubMed] [Google Scholar]


