Abstract
The individual inclination to lead an autonomous life until death is associated with requirements that may be of physiological, psychosocial and environmental nature. We aim to describe a conceptual oro‐facial health model with an emphasis on oro‐facial function, taking the domains of quality of life and patient‐centred values into account. In the context of oro‐facial function, the requirements of life are met when the oro‐facial system is in a fit state. ‘Fitness of the oro‐facial system, that is oro‐facial health, is a state that is characterised by an absence of, or positive coping with physical disease, mental disease, pain and negative environmental and social factors. It will allow natural oro‐facial functions such as sensing, tasting, touching, biting, chewing, swallowing, speaking, yawning, kissing and facial expression’. In the presented conceptual model of oro‐facial health, it is postulated that each individual has present and future potentials related to biological prerequisites and resources that are developed by an individual through the course of life. These potentials form the oro‐facial functional capacity. When the individual potentials together do not meet the requirements of life anymore, dysfunction and disease result. The oro‐facial system is subject to physiological ageing processes, which will inevitably lead to a decrease in the oro‐facial functional capacity. Furthermore, comorbid medical conditions might hamper oro‐facial function and, alongside with the ageing process, may lead to a state of oral hypofunction. Currently, there is a lack of widespread, validated, easy‐to‐use instruments that help to distinguish between states of oro‐facial fitness as opposed to oral hypofunction. Clearly, research is needed to establish adequate, validated instruments alongside with functional rehabilitation procedures.
Keywords: conceptual model, individual capacity, oral health, oro‐facial fitness, oro‐facial function
Fitness of the orofacial system, i.e. orofacial health, is a state that is characterized by an absence of, or positive coping with, physical disease, mental disease, pain, and negative environmental‐ and social factors. It will allow natural orofacial functions such as sensing, tasting, touching, biting, chewing, swallowing, speaking, yawning, kissing, and facial expression.

1. INTRODUCTION
Since the very onset of academic dentistry, the dental profession has focused on diagnosis and treatment of dental diseases. Furthermore, a significant part of dentistry comprised mechanistic aspects such as the fabrication of dentures, and lately, there is a strong focus in the dental profession on digital planning and computer‐assisted manufacturing of endosseous oral implants and dental prostheses. For many decades, these trends have led to an artificial separation in dental education, research, patient care and public health policy from general medicine and its disciplines. 8
However, with the general improvement in prevention, management and prognosis our models for oral health may need to better reflect a more comprehensive view on oro‐facial function as it becomes more and more conspicuous that the oro‐facial system can only be regarded in a broader context of health and function. 9 This position paper will critically discuss oral health models with new proposals for laying emphasis on oro‐facial function and taking the domains of quality of life and patient‐centred values into account.
2. ORAL HEALTH MODELS
The oro‐facial system is an integral part of the body and exhibits key functions related to the biological, social and psychosocial well‐being of any individual. Structural integrity and function of the oro‐facial system are closely interrelated. They must be considered in an oral health model that aims to integrate not only states of structural integrity and correct function, that is oro‐facial fitness, but also states of disease and dysfunction. Today, there are at least 13 different oral health models with varying scopes and characteristics. 10
The World Health Organisation's (WHO) definition of oral health acknowledges the wide implications of the integrity of the oro‐facial system, and lays emphasis on disease and disorders: ‘Oral health means more than good teeth; it is integral to general health and essential for well‐being. It implies being free of chronic oro‐facial pain, oral and pharyngeal (throat) cancer, oral tissue lesions, birth defects such as cleft lip and palate, and other diseases and disorders that affect the oral, dental and craniofacial tissues, collectively known as the craniofacial complex’. 11 The Fédération Dentaire Internationale's (FDI) definition of oral health mentions selected functions: ‘Oral health is multi‐faceted and includes the ability to speak, smile, smell, taste, touch, chew, swallow and convey a range of emotions through facial expressions with confidence and without pain, discomfort and disease of the craniofacial complex’. 12
There is a recent shift in general health models towards a more integrated understanding of health, like the One Health approach of the WHO. 13 Lately, the Meikirch Model for a definition of health was introduced, which recognises the broad interactions of the human existence (Figure 1). It states that: ‘Health is a state of wellbeing emergent from conducive interactions between individuals’ potentials, life's demands, and social and environmental determinants’. 1 , 14
FIGURE 1.
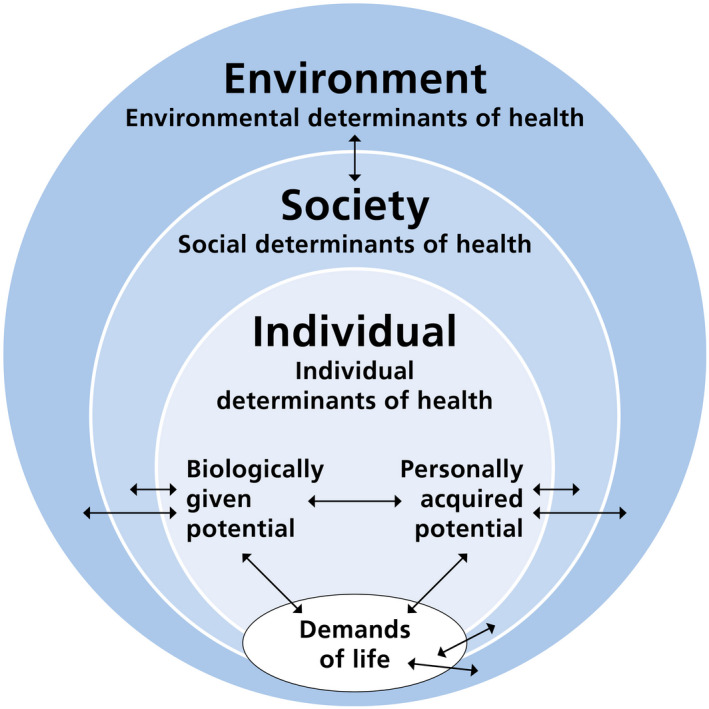
Graphic representation of the Meikirch model of health with its five components: (1) the demands of life such as adequate mastication; (2) the biologically given potential such as normal intra‐uterine development of the craniofacial complex; (3) the personally acquired potential such as training of complex motor skills with new dentures; (4) The social determinants such as aesthetics or speech; and 5. the environmental determinants of health such as the socio‐economic background as an important determinant of oro‐facial health. The double arrows express ten complex interactions between these components. Figure redrawn from Ref. 7 under Creative Commons Licence (CC BY 4.0)
3. ORAL HEALTH CARE
Oral health models reflect in part how health care is organised and how their services are being used by the general population. 15 As a consequence, health care and medical and dental sciences often fail to deal with chronic conditions 16 , 17 and focus on short‐ to mid‐term outcomes of administered treatment approaches (eg root canal treatments, placing dental implants, dental restorations). Pathological conditions of the oral cavity, such as caries, cancer or trauma, may be acute and need immediate attention. Further, tooth‐related factors may be related to mineralisation disorders, such as amelogenesis imperfecta, dentinogenesis imperfecta or molar‐incisor hypomineralisation. Some oro‐facial conditions, however, may develop from an acute condition to a chronic state, such as oro‐facial pain, or may not fall in one of these categories, such as bruxism or obstructive sleep apnoea syndrome. Additionally, most oro‐facial conditions, such as periodontitis, tooth loss, impaired oral food processing or hyposalivation, are chronic and hence require attention for prolonged periods of time. Following rehabilitation, there are also long‐term technical and biological risks related to dental devices and biomaterials that might be considered as chronic conditions. Individuals may or may not adapt to or cope to various degrees with these chronic conditions of the oro‐facial system.
Furthermore, there is an increasing body of evidence that oro‐facial health and general health are interrelated. Conditions of the oro‐facial system might be the origin or modify general diseases such as aspiration pneumonia, or general conditions such as cancer or treatment thereof might manifest themselves in the oral cavity and hamper oro‐facial function. 18 , 19
The medical and dental literature only recently started including patients’ wishes, views and perspectives on a disease, on its treatment or, more generally, on the provision of health care itself. 20 , 21 Health care is often viewed upon nowadays that it should provide cure, whereas providing long‐term care and maintaining quality of life (QoL) to an, from a person's point of view, acceptable standard have gained little attention so far.
Quality of life, or more specifically in the current context, oral health‐related quality of life, is a multidimensional construct that encompasses biological, social and psychological aspects. It was proposed that oral health–related quality of life may be assessed in four domains: oral function, oro‐facial pain, oro‐facial appearance and psychosocial impact. Any outcome of a disease, intervention or long‐term effects of a health‐related issues should be evaluated to this regard, as it is directly related to perceived patient‐related benefits. 22 Pain‐related problems and prevention needs are the most common patient's health concern. Specifically, in orthodontics, oro‐facial appearance, that is aesthetics, is the most common reason to visit a dentist. 9
In the context of the overall burden of oral disease, only few conditions in oral health care and dentistry involve multidisciplinary approaches. Oro‐facial diagnosis and treatment often seems to be driven more by technical progress and less by patient demand and views. 8 In this context, patient adherence to long‐term management for chronic conditions is often poor, as patient´s views, habits, and psychological and social context are often neglected.
4. AIM
We aim to describe a conceptual oro‐facial health model with emphasis on oro‐facial function, taking the domains of quality of life and patient‐centred values into account. We thereby put emphasis on:
Description of a conceptual model of Orofacial Health based on the Meikirch model of health. The new model focuses on oro‐facial fitness and also serves to conceptualise oro‐facial hypofunction.
In the context of ageing, applying the conceptual model to states of oro‐facial fitness and oro‐facial hypofunction.
In the context of comorbid medical conditions, applying the conceptual model to expand the view beyond the dental context.
Description of current assessment and management strategies of oro‐facial function with proposals for their further development.
These points will be discussed in the following four sections. In order to facilitate the reading, a glossary of relevant terms has also been included.
GLOSSARY
| Biologically given potential | Present and future resources as defined by the biological basis of life of an individual. It results directly from genetics and intra‐uterine development and diminishes during the course of life. Modifying factors might be disease, trauma or physiological ageing processes. 1 |
| Complex adaptive system | A human being may be described as a complex adaptive system that comprises a multitude of cooperative parts that interact not only with each other but also with the environment. 2 , 3 |
| First, second, third and fourth age | According to Laslett's theory of the third age, 4 one's life consists of four ages: first age—an era for dependence, socialisation, immaturity and learning; second age—an era for independence, maturity, responsibility and working; third age—an era for personal achievement and fulfilment after retirement; and fourth age—an era for the final dependence, decrepitude and death. |
| Meikirch model of health | The Meikirch model is the definition of health that describes health on a meta‐level by its structure and functions. The model uses a framework of health, consisting of five components that are related to each other by 10 complex interactions. 1 |
| Non‐communicable diseases | Diseases that are not transmitted by one living being to another (eg cardiovascular disease) and might include oro‐facial conditions such as caries, cancer, chronic pain, obstructive sleep apnoea syndrome. |
| Oral frailty, oral hypofunction, oral dysfunction | A set of terms coined by the Japanese Society of Gerodontology to describe the hypothesis that reversible states of oral frailty and oral hypofunction develop during the process of functional pathophysiological changes towards irreversible oral dysfunction. It was proposed that decreased articulation, slight choking or spillage while eating, and an increase in the number of non‐chewable foods in older people might serve for diagnosis. 5 |
| Oro‐facial fitness | A state of the oro‐facial system that is characterised by an absence of, or positive coping with, physical disease, mental disease, pain, and negative environmental and social factors. It will allow natural oro‐facial functions such as sensing, tasting, touching, biting, chewing, swallowing, speaking, yawning, kissing and facial expression and meets the demands of life. The term ‘oro‐facial’ reflects the fact that function and dysfunction of the discussed structures have strong interactions with biological, psychological and social components beyond the oral cavity. |
| Oral health‐related quality of life (OHRQoL) | Concept that intends to capture how oral conditions impact patients’ everyday life. It is multidimensional and comprises the domains oral function, oro‐facial pain, oro‐facial appearance and psychosocial impact. 6 |
| Oro‐facial function | Oro‐facial function is the dental discipline that deals with the normal and disordered functioning of the oro‐facial system, that is the teeth, periodontium, bone, intra‐ and perioral soft tissues, masticatory muscles and temporomandibular joints, and the peripheral and central nervous system that integrates, coordinates and controls associated movements. |
| Oro‐facial functional capacity | Current and future functional capacity of the oro‐facial system. |
| Oro‐facial system | A complex adaptive system that comprises teeth, periodontium, bone, intra‐ and perioral soft tissues, masticatory and accessory muscles, temporomandibular joints and the peripheral and central nervous system that integrates, coordinates and controls associated oro‐facial movements. |
| Personally acquired potential | Present and future resources as developed by an individual through the course of life. It comprises factors, such as maturation of the immune system, functional training or individual coping strategies related to functional deficiencies and impairment. 1 |
| Requirements of life | Physiological, psychosocial and environmental demand of an individual to lead an independent life. 7 |
4.1. Oral health and disease, oro‐facial function and dysfunction in the context of the Meikirch model
According to the Meikirch model of health, 7 it is stated that every biological system needs to satisfy the demands of life. If these demands are not met, it may be defined as the absence of health, that is dysfunction or disease. The demands may be of physiological, psychosocial and environmental nature. The requirements for a healthy life may comprise the following: (1) for the body, they may be nutrition, water intake, hygiene, housing, medical care, etc.; (2) for social and psychological aspects, these may entail successful integration and participation in society; and (3) for the environment, factors comprise availability of food, access to clean water, absence of pollution, control of microbiological threats, etc.
According to the Meikirch model, ‘Health is a dynamic state of well‐being emergent from conducive interactions between individuals’ potentials, life's demands, and social and environmental determinants. Health results throughout the life course when individuals’ potentials – and social and environmental determinants – suffice to respond satisfactorily to the demands of life. Life's demands can be physiological, psychosocial, or environmental, and vary across individual and context, but in every case unsatisfactory responses lead to disease’. 7
To fulfil the requirement of life in a time of steadily growing life expectancy with still very high prevalence of dental diseases and the desire of most individuals to lead a self‐determined life until death, resources are needed. In order to meet the demands of life, any person is given a ‘biologically given potential’ and ‘personally acquired potential’. The term ‘potential’ refers to present and future resources of each individual. 7 In the scope of the current position paper, we suggest to define the oro‐facial functional capacity as the current and future functional capacity of the oro‐facial system. The term oro‐facial reflects the fact that function and dysfunction of the discussed structures have strong interactions with biological, psychological, and social components beyond the oral cavity.
The biologically given potential is mostly determined by genetics or, in an early stage of life, by the intra‐uterine development. With increasing age, the biologically given potential decreases because of the inherent ageing process of the human body, disease or trauma. 23 , 24 With respect to the oro‐facial system, the biologically given potential may comprise the development of the craniofacial complex, which may lead to normal growth or, in case of genetic syndromes, may be reduced, such as in persons with cheilognathopalatoschisis. The personally acquired potential may be developed unconsciously, such as the maturation of the immune system, or consciously, such as muscle mass through training, acquiring skills, attitude to life, acquired deficiencies such as trauma, and quite importantly the coping with pain and reduced function, as often experienced after tooth loss (Figure 2). With increasing age, the personally acquired potential or individual coping strategies are key to overcome age‐related functional deficiencies and impairment, such as training of new motor skills with dentures. 25
FIGURE 2.
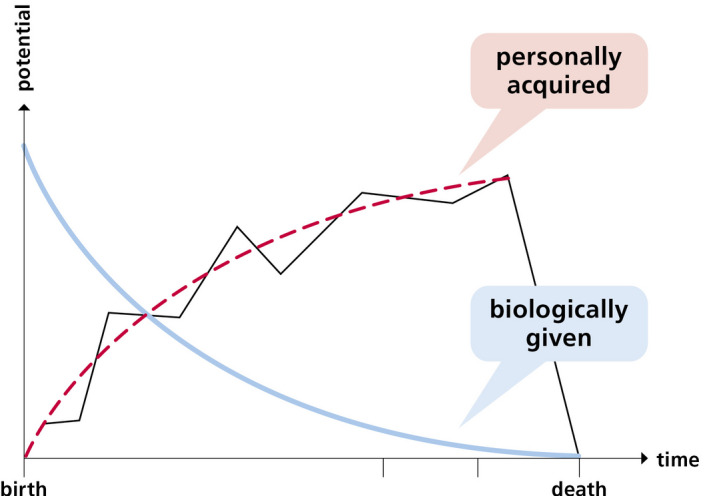
Graphic representation of the personally acquired potential and the biologically given potential during the course of life. These potentials represent the present and future resources of the individual. The personally acquired potential is developed by an individual through the course of life. It comprises factors such as maturation of the immune system, functional training, or individual coping strategies related to functional deficiencies and impairment, such as tooth loss or chronic pain. The red line depicts the trend in this function; however, at certain points in life the personally acquired potential might be reduced and might also be regained (black line), for example if lost teeth are replaced with dental prostheses. The biologically given potential is defined by the biological basis of life of an individual. It results directly from genetics and intra‐uterine development such as normal development of the craniofacial complex and diminishes during the course of life (blue line). Modifying factors might be disease such as eating disorders (bulimia) or caries, facial trauma, or physiological ageing processes such as sarcopenia of the masticatory muscles. Figure redrawn from Ref. 1 under Creative Commons Licence (CC BY 3.0)
A human being may be described as a complex adaptive system that comprises a multitude of cooperative parts that interact not only with each other, but also with the environment. 2 , 3 For each life phase, viz. first, second, third and fourth age, there are specific requirements of life that may be of physiological, psychosocial and environmental nature. 4 , 26 , 27 If these requirements are not met by the individual person anymore due to evolving demands, adaptive changes on the structural and functional level will occur. These may be successful and then constitute a new equilibrium in the complex adaptive system that would then still constitute a state of health, or the changes may occur too slowly, inappropriately or not at all, which would constitute a state of disease. 2
4.1.1. A definition of Oro‐facial Health based on oro‐facial fitness
The definition of fitness according to Oxford dictionary is ‘the condition of being physically fit and healthy, the quality of being suitable to fulfil a particular role or task’. The concept of ‘oro‐facial fitness’ is not yet widely introduced in the scientific literature, but is frequently encountered in the more laymen description of oral health, and in particular related to oral care, viz. the prevention of caries and periodontal diseases. It is proposed that efforts will be directed to expand the scientific and public awareness of oro‐facial fitness and to relate this construct not only to oral care but especially to oro‐facial function. Oro‐facial fitness in this manner may be conceptualised as ‘the individual and sufficient amount of activity that will maintain and/or restore oro‐facial health’, or increase in the personally acquired potential.
Specifying the core elements of the Meikirch model of health in regard to oro‐facial function, the authors of this position paper have defined oro‐facial health as follows: ‘Fitness of the orofacial system, i.e. orofacial health, is a state that is characterized by an absence of, or positive coping with, physical disease, mental disease, pain, and negative environmental‐ and social factors. It will allow natural orofacial functions such as sensing, tasting, touching, biting, chewing, swallowing, speaking, yawning, kissing, and facial expression’. In this state, the oro‐facial functional capacity suffices to meet the requirements of life. Table 1 gives a further overview on important functions of the oro‐facial system. This definition comprises the four domains of oral health–related quality of life and may serve for the development of validated, easy‐to‐use instruments to assess oro‐facial fitness.
TABLE 1.
Physiological requirements in relation to oro‐facial function
| Physical/body requirements |
| Sensing |
| Tasting |
| Touching |
| Breathing and yawning |
| Biting |
| Chewing |
| Salivation |
| Forming a bolus that is safe to swallow |
| Swallowing |
| Psychosocial aspects |
| Facial expression |
| Oro‐facial appearance |
| Kissing |
| Speaking |
| Enjoying meals in the company of others |
| Environment |
| Adequate food, adapted to the oro‐facial functional capacity |
| Diet low in sugar |
| Adequate hydration |
In their position paper of the Japanese Society of Gerodontology, Minakuchi et al. 5 use the term ‘oral frailty’ to describe an unfavourable oral condition in older people that is characterised by decreased articulation, slight choking or spillage while eating, and an increase in the number of non‐chewable foods. These characteristics are derived from numerous epidemiological studies, mainly from Japan (for an overview, see, eg, Ref. 28). Oral frailty may be the first step towards manifest painful and functional problems, which can be qualified as oral hypofunction, or even as oral dysfunction. 5 From other studies, it is well known that pain is a significant risk factor for frailty among older adults (eg Ref. 29). Hypofunction is a less fit state and may be followed by dysfunction, leading to signs and symptoms in the oro‐facial system. Training may increase the personally acquired potential and is one option to stay fit or to regain fitness. Furthermore, the rehabilitation of lost oral hard and soft tissues plays an important role in regaining fitness. The frail patient may be susceptible or vulnerable to change in function, as his or her biological resources decline, that is decline in biologically given potential. 5
In the context of oro‐facial function, the oro‐facial functional capacity is reduced in many individuals. The most important modifier on an epidemiological level is caries as it is the most common non‐communicable disease worldwide. It leads to destruction of tooth substance, alterations of tooth morphology, pain, infections and abscesses, and, ultimately, tooth loss. 15 Caries has important cofactors that modify the disease, such as hyposalivation 30 and alterations of the oral microbiome due to high sugar intake. 31 On a functional level, the progress of the disease significantly alters oro‐facial functions such as biting, chewing and swallowing and subsequently induces changes in the somatosensory and motor cortex. 24 , 32 , 33 , 34 , 35 The disease‐induced decrease in oro‐facial functions negatively affects the physiological and psychosocial demands of life with severe impact on nutritional state and oral health–related quality of life, and is a burden for the healthcare systems. 36 , 37 , 38 However, caries and the related decrease in oro‐facial fitness is a very good example that the decline in the oro‐facial functional capacity in this context can largely be prevented. 39 If teeth and related alveolar bone are lost as the final outcome of the caries process, the oro‐facial functional capacity may even be increased with the placement of dental prostheses, additional training of oro‐facial function (eg mastication, biting) and nutritional counselling. 40
In the overall context of oral health–related quality of life, oro‐facial frailty or oro‐facial hypofunction should also take into account factors that relate to the domains oral function, oro‐facial pain, oro‐facial appearance and psychosocial impact, as they relate to the reasons as to why patients seek help from dental and medical professionals. 41 , 42
4.2. Oro‐facial function in the context of ageing
The world's population continues to grow and to live longer. Ageing is, indeed, another important example of an inevitable decrease in the oro‐facial functional capacity. It is a physiological phenomenon that is, however, often accompanied by multimorbidity, polypharmacy, and decline in cognitive and oro‐facial function.
The oro‐facial system is subject to physiological ageing processes such as any biological system. The process of ageing is irreversible; it progresses and affects every aspect of the oro‐facial complex. Hence, ageing inevitably leads to changes of structure, function and psychological aspects that occur in the course of life. 43 Cell damage and tissue damage accumulate. In other words, the biologically given potential decreases. If the spare capacity of the oro‐facial system is exceeded and thus the personally acquired potential cannot fully compensate the changes, the system is then more susceptible to develop a disease.
This physiological process of ageing does not imply that the individual may experience a loss of oro‐facial functional capacity that would not meet the requirements of life or compromise oral health–related quality of life, or nutritional state. There is a large physiological spare capacity to compensate these changes. For example, the oro‐facial system usually finds a new equilibrium after the loss of molar teeth. If there is sufficient occlusal contact, typically 10 occluding pairs of teeth, associated with otherwise intact oro‐facial functions (eg salivary gland function, sufficient muscle force), oral health–related quality of life and nutritional state, may be maintained. 44 An example in which an additional pathological cofactor would lead to insufficient function would be the additional loss of masticatory force due to age‐related atrophy of the involved muscles in very old individuals. 24
Factors for successful ageing of the mouth may be genetic, but are mainly related to lifestyle choices and hence often depend on socio‐economic status. 15 The consumption of a high sugary diet, smoking or inadequate oral hygiene is observed more frequently in persons from low socio‐economic background, and very often in old individuals. 45 , 46 As a consequence, the number of remaining teeth is higher in persons of high socio‐economic status compared with poorer social classes. Consequently, in the Western world, edentulism decreases since many decades and now has its highest prevalence in very old persons with multiple diseases and low socio‐economic status. 47 In turn, this often leads to severely reduced oro‐facial functional capacity and low oral health–related quality of life.
Neurocognitive and neurodegenerative disorders are predominantly observed in elderly individuals and may imply an impairment of muscle coordination, so in the initial stages of the disease, additional retention from dental implants may be welcomed to replace impaired muscle skills for denture retention. In Parkinson's patients, both the stabilisation of removable dentures and the insertion of fixed restorations may be indicated, because jaw motor control is severely impaired in this condition. People rehabilitated with dental implants may start improving biting or chewing immediately after the insertion of the implant‐based crowns or dentures, but several studies have clearly identified impairment in masticatory parameters, suggesting that implant‐rehabilitated patients may need to be trained to relearn optimal function. 33 , 48 , 49 , 50 Learning and training of new functions is also an age‐dependent process that may take a longer time for the elderly to master. Furthermore, pain, bruxism, motivation and other sensory inputs may significantly interfere with the ability to learn new motor tasks. 51 , 52 , 53 , 54 , 55 , 56 The key point is that rehabilitation of oro‐facial function as defined above is not only related to the anatomical restoration of teeth or the dental arches or to preservation of the dentition, but it also deals with regaining oro‐facial fitness. This may require specific training or re‐learning of lost or compromised parts of oro‐facial function. 57
4.3. Oro‐facial function in the context of comorbid diseases
As part of the global ageing process, it is also clear that individuals may not only have a single health issue, but most likely more and complex disorders at the same time. Besides ageing, there are numerous comorbid conditions that may have negative effects on the oro‐facial fitness. While many medical conditions occur in the absence of disorders of the oro‐facial system, some can be considered as comorbid medical conditions, that is if they co‐occur with a primary condition in the oro‐facial system.
Examples of comorbid medical conditions in which a dental practitioner could play a role in the early diagnosis and possibly in their prevention and management include, but are not limited to: systemic disorders such as rheumatoid arthritis, Sjögren´s syndrome, diabetes and gastroesophageal reflux; movement disorders such as dyskinesia, dystonia and Parkinson's disease; and sleep disorders such as snoring and obstructive sleep apnoea. Most of these comorbid medical conditions are associated with oro‐facial conditions that may also affect oro‐facial function in either one of the following categories:
4.3.1. Category 1
The medical condition manifests itself in the oral cavity. For example, the damage caused to dental hard tissues, such as in the case of reflux of stomach content causing chemical tooth wear, can lead to pain, loss of aesthetics and—in extreme cases—loss of masticatory function (for a review, see Ref. 58). Sleep bruxism is an example of a condition that can manifest itself in the oral cavity (eg mechanical tooth wear). There are psychiatric diseases with possible deleterious effects, such as eating disorders. 59 Also, a potentially life‐threatening condition such as cancer will go with several and diverse oral manifestations, for example pain and soft and hard tissue lesions that may hamper normal function. Other examples of a medical conditions with oral manifestations are Sjögren´s syndrome, which leads to severe hyposalivation or congenital oro‐facial anomalies such as progenia, micrognathia and cheilognathopalatoschisis. Symptoms of genetic syndromes such as Down syndrome, or haematological and autoimmune diseases are often evident in the oro‐facial system as well. Further, a direct effect on the oral cavity was demonstrated for stroke and amyotrophic lateral sclerosis patients who lose much of their sensory and motor abilities and hence show impaired bolus control and swallowing disorders, leading to frequent feeding problems, low oral health–related quality of life and aspiration pneumonia. 60 , 61
4.3.2. Category 2
The medical condition is caused or influenced by an oro‐facial condition. For example, mouth breathing may be associated with obstructive sleep apnoea and complaints of a dry mouth/xerostomia (for a review, see Ref. 62). Further examples are under‐ and malnutrition in the elderly, as well as aspiration pneumonia related to poor oral health. 18 , 36 , 63 , 64
4.3.3. Category 3
The medical condition is prevented, managed, or treated via the oro‐facial system. For example, the insertion of a mandibular advancement appliance in the case of obstructive sleep apnoea with the purpose to increase the oro‐pharyngeal space during breathing might, in turn, lead to orthodontic changes and thus to loss of aesthetics and a deterioration of masticatory function, as well as to (transient) complaints of hypersalivation and pain in the masticatory muscles and/or the temporomandibular joints (for a review, see Ref. 65).
4.3.4. Category 4
The treatment of the medical condition affects the oral cavity. For example, pharmacological treatment may yield a hyposalivation and thus a dry mouth/xerostomia, especially in cases of polypharmacy (for a review, see Ref. 66). In turn, this impairs food processing and makes the oral cavity vulnerable for all kinds of dental conditions such as caries, periodontitis and tooth wear—the latter again possibly leading to pain, loss of aesthetics and—in extreme cases—loss of masticatory function. In addition, hyposalivation may lead to taste disturbances, that is hypogeusia (impaired taste sensitivity) or dysgeusia (distorted taste), which in turn may lead to decreased food intake and changes in food choices, with possible under‐ and/or malnutrition as a consequence. Another important example in this category is the treatment of cancer, especially in the oro‐facial region. Radio‐ and/or chemotherapy leads to severe damage of tissues with a high cell turnover, such as in the salivary glands and the oral mucosa. In the acute phase of the treatment, normal oro‐facial function is almost impossible to execute, and the treatment frequently leads to scarring of the oro‐facial mucosa and irreversible damage of salivary glands. 67 Furthermore, if tumour mass in the head and neck area is removed or reduced surgically, severe impairment of oral and facial functions results, with extensive consequences on most biological, psychological and social functions.
4.4. Assessment and rehabilitation strategies for oro‐facial function
A central point in the discussion of oro‐facial health in this position paper is related to a better understanding of oro‐facial function and its assessment and strategies for management.
Although from a global perspective inequalities exist in the accessibility of oral health care 68 , socially advantaged members of society usually visit their dentist on a regular basis for a periodical check‐up, as opposed to their general medical practitioner, whom they often consult only in case of a possible medical condition. Thus, dental professionals are in a unique position for the early screening or diagnosis of comorbid medical conditions. Recently, there has been a shift in the profession towards the development of novel strategies to assess comorbid diseases and maintain or rehabilitate ‘oro‐facial fitness’. This will be discussed in the following.
Exemplarily, the Japanese Society for Gerodontology has proposed a set of quantitative instruments for the diagnosis of oral hypofunction. It comprises a standardised assessment of oral hygiene, oral dryness, maximum voluntary bite force, tongue‐lip and motor functions through the assessment of oral diadochokinesis, maximum voluntary tongue pressure, masticatory performance and the EAT‐10 questionnaire for swallowing function. Based on reference values and cut‐off values, a diagnosis of oral hypofunction was proposed. 5 However, no further patient‐reported outcomes such as chewing ability or oral health‐related quality of life were included.
There are currently limited possibilities for the instrumental assessment of oro‐facial function, in particular when measures of ‘learning’ or ‘training’ are being considered. Generally speaking, there can be subject‐based assessment, using standardised questions and questionnaires, for example related to the perceived effort or difficulty to perform a given oral task. 54 Also, assessment of motivation to engage in a rehabilitation programme may be useful to monitor by self‐reports. 69 The next level will be assessment of the physical task, for example the accuracy and precision by which the individual can repeat the given task. 70 , 71 , 72 Other measures could be ‘throughput’, which is the number of successful trials or performances within a defined period of time. This means one may be able to learn to perform a particular task, but it may take a very long time in order to do so. Preliminary results from implant‐rehabilitated patients have indeed indicated that they can learn to perform a sunflower‐seed splitting task with the front teeth to the same level as individuals with natural dentition, but the implant‐rehabilitated patients take a longer period of time.
Neurophysiological measures of training and learning can be obtained using transcranial magnetic stimulation (TMS) of the motor cortex in humans and recordings of the associated motor‐evoked potentials (MEPs) from the trained muscles. This provides a direct insight into the corticobulbar tract function, that is how efficiently the brain controls the voluntary muscles. Several recent studies have used the TMS‐MEP technique to test the effects of specific tongue‐training paradigms, 56 , 73 , 74 , 75 biting tasks 76 , 77 , 78 and manipulation of food items (oro‐facial dexterity). 78 Also, more elaborate techniques, such as brain imaging using fMRI or PET scans, can be used for a further research‐centred insight into the importance of the brain for learning. 79
The current understanding of training and re‐learning of oro‐facial function is that the brain needs to be actively involved and capable of storing the neuronal signatures in order to restore or improve compromised function, that is hypofunction. This process is termed ‘cortical plasticity’ and will be the neurophysiological underpinning of maintenance and rehabilitation of oro‐facial fitness. 57
There are complex biological, psychological and social interactions related to oro‐facial function. Exemplary, masticatory efficiency is defined as ‘the effort required to achieve a standard degree of comminution of food’, 80 but this definition falls short of the implications a deficient mastication has on biological, social and psychological requirements of a human being. From a physiological point of view, mastication aims to increase the surface of the nutrient, to form a bolus that is safe to swallow, and is coupled with the swallowing reflex. 81 Psychosocial components of mastication are related to self‐confidence while chewing, eating‐related quality of life and social interaction (Figure 3). Hence, the evaluation of mastication should be multidimensional since it depends on a multitude of factors and has complex implications if impaired due to reduced oro‐facial functional capacity.
FIGURE 3.
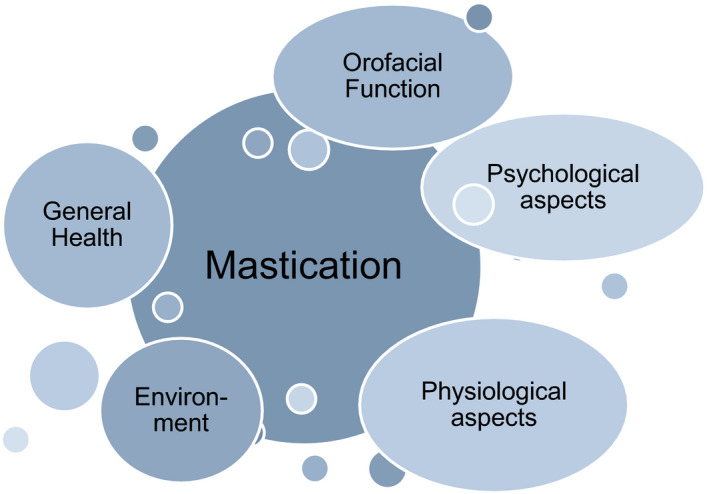
There are multidimensional interactions of oro‐facial function, for example for the masticatory function. Mastication and the involved structures are an obvious example for a complex adaptive system. Rheological characteristics of food and the oro‐facial functional capacity to comminute it are most often the main aspect of assessment. 87 However, mastication also largely depends on physiological properties such as appetite, taste, vision and/or smell; on psychological aspects such as conditioning, expectations and/or preferences; and on environmental constraints such as availability of food, inadequate cooking facilities and/or an absence of an incentive to cook. 88 , 89 , 90 There are broad implications for general health (nutrition) and psychosocial well‐being of an individual
Prevention and rehabilitation of decreased masticatory function through tooth loss, sarcopenia (ie, the degenerative loss of skeletal muscle mass, quality, and strength) of the masticatory muscles, hyposalivation or deficient dental prostheses may maintain or increase the personally acquired potential as a dimension of the oro‐facial functional capacity.
Currently, there are few specific clinical management strategies for maintenance or rehabilitation of oro‐facial function, such as for jaw exercises (for, eg, reduced jaw opening capacity or temporomandibular disorders, lip training (for, eg, improving swallowing function in stroke patients). 82 , 83 , 84 However, there is no holistic management strategy to improve overall oro‐facial fitness as conceptualised in the current model for oro‐facial health. There is a need for the dental profession to catch up with empirically based rehabilitation strategies for, eg, swallowing disorders, and for rehabilitation of lost function following traumatic brain injuries, stroke or other neurodegenerative diseases. Rehabilitation of dysphagia is often based on therapeutic tongue exercises, which, however, lack scientific evidence and sufficient understanding of the neurobiological mechanisms. 69 Currently, there is a lack of distinction between rehabilitation of acquired, learned functions, such as mastication, and inherent functions, such as swallowing.
5. DISCUSSION
The requirements of life, such as biting, chewing, smiling and breathing, can be assured if an individual maintains an oro‐facial functional capacity by using its individual potentials.
In the presented model of oro‐facial health that puts emphasis on oro‐facial function, it is postulated that during the course of life, the biologically given potential decreases as a result of the general, irreversible process of ageing. Parallel to this decline, and compensating the possible negative implications on the oro‐facial functional capacity, the personally acquired potential increases, insuring the state of health. When the individual potentials together do not meet the requirements of life anymore, dysfunction and disease result. Selected components of the oro‐facial functional capacity may be already quantifiable with the current available evidence, but cut‐off values are often only available for selected geographical regions, cultural and linguistic backgrounds. Currently, epidemiological studies are being conducted to meet this current lack of knowledge (eg Study of Health in Pomerania). However, in line with the authors of the Meikirch model, the individual potentials might be difficult to quantify. 85
As the decrease in the biologically given potential is inevitable due to the ageing process, oro‐facial fitness may be maintained by prevention of oro‐facial disease or adequate treatment and training. Hereby, the replacement of lost oro‐facial tissues such as teeth, alveolar bone, soft tissues, mechanoreceptors or even entire oro‐facial components through trauma or cancer may partly be compensated with surgical and dental interventions, but may often require additional functional training. Decrease in the oro‐facial functional capacity due to reduced neuro‐plastic capacity may partly be compensated with training of oro‐facial structures, such as tongue movement.
The oro‐facial system is an integral part of the body, and hence, its functions are key to maintaining general health, quality of life and vice versa. Hence, novel strategies to assess, maintain and rehabilitate oro‐facial fitness should be developed and tested in the view of the general ageing of the world population.
Apart from the resulting necessary medical training of dentists, it is important to provide dentists with reliable, valid, easy‐to‐use and cost‐effective tools that they can use for the chair‐side assessment of not only oro‐facial pain and dysfunction but also possible comorbid medical conditions. For some of these medical conditions, the dentist could even play a role in the prevention and/or management and thus be a partner for medical doctors as an ‘oro‐facial physician’. Importantly, it could be expected that by improving comorbid medical conditions, oro‐facial function will also improve, and vice versa, since in some cases both aspects are mutually linked to each other. Thus, the dentist should be part of an integrated care team. Diagnosis and treatment of these comorbid medical conditions would help to bring dentistry and the medical specialties closer together and foster the mutual understanding of comorbid medical and dental conditions. 86
In regard to assessment and rehabilitation strategies for oro‐facial fitness, there are numerous approaches to assess single functional components of the oro‐facial function. They find widespread use in the assessment of conditions such as obstructive sleep apnoea, oral food processing and swallowing, oro‐facial pain or bruxism. A first proposal to integrate several oro‐facial functional aspects into the joint diagnosis of oral hypofunction was provided by the Japanese Society of Gerodontology. 5 However, this diagnosis emphasises dysfunction and the reference studies that provide cut‐off values included exclusively Japanese cohorts. 28 The diagnostic tools are also mostly available only in Japan. There is a justified need to develop objective tests in regard to a broader understanding of oro‐facial fitness as opposed to oro‐facial dysfunction, to make these tests available for all researchers and medical/ dental professionals, and to define population‐based reference values for individuals with various geographical, cultural and environmental backgrounds.
There are a several limitations of the proposed conceptual model for oro‐facial health, which adapts several lines of thought of the Meikirch model for health. Firstly, the proposed definitions, the model and its possible implications need to stand the proof of scientific verification. Although the proposed definitions are based on extensive research and clinical practice, it remains to be proven that the potentials can be assessed in qualitative and quantitative ways. 14 The complex adaptive system of the human body, its environment and social interaction might be too complex to be fully understood or quantified.
One of the major challenges in the future will be to develop easy‐to‐use tests to assess oro‐facial fitness and to validate those in larger cohorts of healthy and sick populations. We need to find quantifiable measures and thresholds to better understand the oro‐facial functional capacity based on individual parameters in the sense of personalised (dental) medicine. As in general medicine, we need to find predictive values if patients may benefit from dental/ oro‐facial interventions, in regard to all domains of oral health–related quality of life. This will also help to estimate the biologically given potential, that is physiological spare capacity, in the elderly, who often undergo extensive dental interventions, such as serial extractions and the provision of removable dentures, to whom they often cannot adapt—functionally, socially and psychologically.
6. CONCLUSIONS
Most definitions of oral health and their respective conceptual models fall short in distinguishing between the inherent biologically given potential and the acquired personally acquired potential of the oro‐facial system. We propose that oro‐facial fitness is a state in which the physiological, psychosocial and environmental requirements of life of an individual are met.
We propose, in line with the Meikirch model for health, that there is an age‐related decline of the biologically given potential of the oro‐facial system during the course of life.
Comorbid medical diseases may negatively affect the oro‐facial functional capacity, and may result in dysfunction and disease. The loss of oro‐facial function may or may not be restored through dental intervention, or training.
There are well‐known prosthetic strategies to improve the oro‐facial functional capacity for food processing; however, their effect on oro‐facial fitness is often poorly understood. Reduced neuro‐plastic capacity in old individuals might preclude a positive outcome of these strategies that might need to be accompanied by functional training and nutritional counselling.
There is a lack of widespread, validated, easy‐to‐use instruments that help to distinguish between states of oro‐facial fitness as opposed to oro‐facial hypofunction.
CONFLICT OF INTEREST
The current paper is based on a series of meetings of the authors that were financed by SUNSTAR SUISSE SA (Etoy, Switzerland).
AUTHOR CONTRIBUTIONS
All authors contributed equally to the development of the conceptual model and wrote drafted and finalised parts of the manuscript related to their specific expertise.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/joor.13250.
ACKNOWLEDGMENT
Open Access Funding provided by Universitat Bern.
Schimmel M, Aarab G, Baad‐Hansen L, Lobbezoo F, Svensson P. A conceptual model of oro‐facial health with an emphasis on function. J Oral Rehabil. 2021;48:1283–1294. 10.1111/joor.13250
DATA AVAILABILITY STATEMENT
There are no original data for this article available.
REFERENCES
- 1. Bircher J, Hahn E. Will the Meikirch Model, a New Framework for Health, Induce a Paradigm Shift in Healthcare? Cureus. 2017;9:e1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bircher J, Hahn EG. Applying a complex adaptive system's understanding of health to primary care. F1000Res. 2016;5:1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sturmberg JP, Martin CM, Katerndahl DA. Systems and complexity thinking in the general practice literature: an integrative, historical narrative review. Ann Fam Med. 2014;12:66‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Laslett P. The emergence of the third age. Ageing Soc. 2008;7:133‐160. [Google Scholar]
- 5. Minakuchi S, Tsuga K, Ikebe K, et al. Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016. Gerodontology. 2018;35(4):317‐324. [DOI] [PubMed] [Google Scholar]
- 6. John MT, Rener‐Sitar K, Baba K, et al. Patterns of impaired oral health‐related quality of life dimensions. J Oral Rehabil. 2016;43:519‐527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bircher J, Hahn E. Understanding the nature of health: New perspectives for medicine and public health. Improved wellbeing at lower costs. F1000Research. 2016;5:167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ship J. Oral health in the elderly—What’s missing? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:625‐626. [DOI] [PubMed] [Google Scholar]
- 9. John MT, Sekulić S, Bekes K, et al. Why Patients Visit Dentists – A Study in all World Health Organization Regions. J Evid Based Dent Pract. 2020;20(3):101459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sekulic S, Theis‐Mahon N, Rener‐Sitar K. A systematic scoping review of oral health models. Qual Life Res. 2019;28:2651‐2668. [DOI] [PubMed] [Google Scholar]
- 11. Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century–the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2003;31(Suppl 1):3‐23. [DOI] [PubMed] [Google Scholar]
- 12. Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. J Am Dent Assoc. 2016;147:915‐917. [DOI] [PubMed] [Google Scholar]
- 13. WHO . One Health, 2020. https://www.who.int/news‐room/q‐a‐detail/one‐health. Accessed on 23.11.2020.
- 14. Bircher J, Kuruvilla S. Defining health by addressing individual, social, and environmental determinants: new opportunities for health care and public health. J Public Health Policy. 2014;35:363‐386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Peres MA, Macpherson LMD, Weyant RJ, et al. Oral diseases: a global public health challenge. Lancet. 2019;394:249‐260. [DOI] [PubMed] [Google Scholar]
- 16. Miles A, Asbridge E. The chronic illness problem. The person‐centered solution. Eur J Pers Cent Healthc. 2016;4:1‐5. [Google Scholar]
- 17. Watt RG, Daly B, Allison P, et al. Ending the neglect of global oral health: time for radical action. Lancet. 2019;394:261‐272. [DOI] [PubMed] [Google Scholar]
- 18. Müller F. Oral hygiene reduces the mortality from aspiration pneumonia in frail elders. J Dent Res. 2015;94:14S‐S16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Szczesniak MM, Maclean J, Zhang T, Graham PH, Cook IJ. Persistent dysphagia after head and neck radiotherapy: a common and under‐reported complication with significant effect on non‐cancer‐related mortality. Clinic Oncol. 2014;26:697‐703. [DOI] [PubMed] [Google Scholar]
- 20. Brocklehurst PR, McKenna G, Schimmel M, et al. How do we incorporate patient views into the design of healthcare services for older people: a discussion paper. BMC Oral Health. 2018;18:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chebib N, Abou‐Ayash S, Maniewicz S, et al. Exploring Preferred Dental Services of Swiss Older People for When They Become Dependent. Swiss Dent J. 2020;130:876‐884. [DOI] [PubMed] [Google Scholar]
- 22. John MT. Foundations of oral health‐related quality of life. J Oral Rehabil. 2021;48(3):355‐359. [DOI] [PubMed] [Google Scholar]
- 23. Lopez‐Otin C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153:1194‐1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sato N, Ono T, Kon H, et al. Ten‐year longitudinal study on the state of dentition and subjective masticatory ability in community‐dwelling elderly people. J Prosthodont Res. 2016;60:177‐184. [DOI] [PubMed] [Google Scholar]
- 25. Müller F, Hasse‐Sander I. Experimental studies of adaptation to complete dentures related to ageing. Gerodontology. 1993;10:23‐27. [DOI] [PubMed] [Google Scholar]
- 26. Kydd A, Fleming A, Gardner S, Hafford‐Letchfield T. Ageism in the Third Age. In: Ayalon L, Tesch‐Römer C, eds. Contemporary Perspectives on Ageism. Springer International Publishing; 2018:115‐130. [Google Scholar]
- 27. WHO . World Report on Ageing and Health. WHO Press; 2015. [Google Scholar]
- 28. Tanaka T, Takahashi K, Hirano H, et al. Oral frailty as a risk factor for physical frailty and mortality in community‐dwelling elderly. J Gerontol A Biol Sci Med Sci. 2018;73:1661‐1667. [DOI] [PubMed] [Google Scholar]
- 29. Megale RZ, Ferreira ML, Ferreira PH, et al. Association between pain and the frailty phenotype in older men: longitudinal results from the Concord Health and Ageing in Men Project (CHAMP). Age Ageing. 2018;47:381‐387. [DOI] [PubMed] [Google Scholar]
- 30. Dodds M, Roland S, Edgar M, Thornhill M. Saliva A review of its role in maintaining oral health and preventing dental disease. BDJ Team. 2015;2:15123. [Google Scholar]
- 31. Meyer‐Lueckel H, Paris S. When and How to Intervene in the Caries Process. Oper Dent. 2016;41:S35‐S47. [DOI] [PubMed] [Google Scholar]
- 32. Lobbezoo F, Trulsson M, Jacobs R, Svensson P, Cadden SW, van Steenberghe D. Topical review: Modulation of trigeminal sensory input in humans: Mechanisms and clinical implications. J Orofac Pain. 2002;16:9‐21. [PubMed] [Google Scholar]
- 33. Trulsson M, van der Bilt A, Carlsson GE, et al. From brain to bridge: masticatory function and dental implants. J Oral Rehabil. 2012;39:858‐877. [DOI] [PubMed] [Google Scholar]
- 34. Ono T, Hori K, Nokubi T. Pattern of tongue pressure on hard palate during swallowing. Dysphagia. 2004;19:259‐264. [DOI] [PubMed] [Google Scholar]
- 35. Kosaka T, Ono T, Yoshimuta Y, et al. The effect of periodontal status and occlusal support on masticatory performance: the Suita study. J Clin Periodontol. 2014;41:497‐503. [DOI] [PubMed] [Google Scholar]
- 36. Sheiham A, Steele JG, Marcenes W, Finch S, Walls AW. The relationship between oral health status and Body Mass Index among older people: a national survey of older people in Great Britain. Br Dent J. 2002;192:703‐706. [DOI] [PubMed] [Google Scholar]
- 37. McKenna G, Allen F, Schimmel M, Müller F. Editorial: Who's picking up the bill? Gerodontology. 2015;32:161‐162. [DOI] [PubMed] [Google Scholar]
- 38. Stenman U, Ahlqwist M, Bjorkelund C, Hakeberg M. Oral health‐related quality of life ‐ associations with oral health and conditions in Swedish 70‐year‐old individuals. Gerodontology. 2012;29:e440‐e446. [DOI] [PubMed] [Google Scholar]
- 39. Paris S, Banerjee A, Bottenberg P, et al. How to Intervene in the Caries Process in Older Adults: A Joint ORCA and EFCD Expert Delphi Consensus Statement. Caries Res. 2020;54:1‐7. [DOI] [PubMed] [Google Scholar]
- 40. Kito N, Matsuo K, Ogawa K, et al. Positive Effects of "Textured Lunches" Gatherings and Oral Exercises Combined with Physical Exercises on Oral and Physical Function in Older Individuals: A Cluster Randomized Controlled Trial. J Nutr Health Aging. 2019;23:669‐676. [DOI] [PubMed] [Google Scholar]
- 41. Bekes K, John MT, Rener‐Sitar K, et al. Pediatric patients’ reasons for visiting dentists in all WHO regions. Health Qual Life Outcomes. 2021;19:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. John MT, Sekulić S, Bekes K, et al. Why Patients Visit Dentists – A Study in all World Health Organization Regions. Journal of Evidence Based Dental Practice. 2020;20:101459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Schimmel M, Abou‐Ayash S. The Ageing Mouth. In: Kossioni A, ed. Gerodontology Essentials for Health Care Professionals. Springer International Publishing; 2020:17‐48. [Google Scholar]
- 44. Wallace M, Samietz S, McKenna G, Woodside JV, Schimmel M. Impact of prosthodontic rehabilitation on the masticatory performance of partially dentate older patients: Can it predict nutritional state? Results from a RCT. J Dentist. 2018;68:66‐71. [DOI] [PubMed] [Google Scholar]
- 45. Gilbert GH, Duncan RP, Shelton BJ. Social determinants of tooth loss. Health Serv Res. 2003;38:1843‐1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Petersen PE, Kandelman D, Arpin S, Ogawa H. Global oral health of older people–call for public health action. Community Dent Health. 2010;27:257‐267. [PubMed] [Google Scholar]
- 47. Slade GD, Akinkugbe AA, Sanders AE. Projections of U.S. Edentulism prevalence following 5 decades of decline. J Dent Res. 2014;93:959‐965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Grigoriadis J, Trulsson M, Svensson KG. Motor behavior during the first chewing cycle in subjects with fixed tooth‐ or implant‐supported prostheses. Clin Oral Implants Res. 2016;27:473‐480. [DOI] [PubMed] [Google Scholar]
- 49. Svensson KG, Grigoriadis J, Trulsson M. Alterations in intraoral manipulation and splitting of food by subjects with tooth‐ or implant‐supported fixed prostheses. Clin Oral Implants Res. 2013;24:549‐555. [DOI] [PubMed] [Google Scholar]
- 50. Svensson KG, Trulsson M. Impaired force control during food holding and biting in subjects with tooth‐ or implant‐supported fixed prostheses. J Clin Periodontol. 2011;38:1137‐1146. [DOI] [PubMed] [Google Scholar]
- 51. Boudreau S, Romaniello A, Wang K, Svensson P, Sessle BJ, Arendt‐Nielsen L. The effects of intra‐oral pain on motor cortex neuroplasticity associated with short‐term novel tongue‐protrusion training in humans. Pain. 2007;132:169‐178. [DOI] [PubMed] [Google Scholar]
- 52. Boudreau SA, Hennings K, Svensson P, Sessle BJ, Arendt‐Nielsen L. The effects of training time, sensory loss and pain on human motor learning. J Oral Rehabil. 2010;37:704‐718. [DOI] [PubMed] [Google Scholar]
- 53. Ikuta M, Iida T, Kothari M, Shimada A, Komiyama O, Svensson P. Impact of sleep bruxism on training‐induced cortical plasticity. J Prosthodont Res. 2019;63:277‐282. [DOI] [PubMed] [Google Scholar]
- 54. Kothari M, Svensson P, Jensen J, et al. Training‐induced cortical plasticity compared between three tongue‐training paradigms. Neuroscience. 2013;246:1‐12. [DOI] [PubMed] [Google Scholar]
- 55. Kothari M, Svensson P, Jensen J, et al. Tongue‐controlled computer game: a new approach for rehabilitation of tongue motor function. Arch Phys Med Rehabil. 2014;95:524‐530. [DOI] [PubMed] [Google Scholar]
- 56. Kothari M, Liu X, Baad‐Hansen L, Kumar A, Bin G, Svensson P. Influence of visual observational conditions on tongue motor learning. Eur J Oral Sci. 2016;124:534‐539. [DOI] [PubMed] [Google Scholar]
- 57. Kumar A, Kothari M, Grigoriadis A, Trulsson M, Svensson P. Bite or brain: Implication of sensorimotor regulation and neuroplasticity in oral rehabilitation procedures. J Oral Rehabil. 2018;45:323‐333. [DOI] [PubMed] [Google Scholar]
- 58. Wetselaar P, Lobbezoo F. The tooth wear evaluation system: a modular clinical guideline for the diagnosis and management planning of worn dentitions. J Oral Rehabil. 2016;43:69‐80. [DOI] [PubMed] [Google Scholar]
- 59. Kisely S, Baghaie H, Lalloo R, Johnson NW. Association between poor oral health and eating disorders: systematic review and meta‐analysis. Br J Psychiatry. 2015;207:299‐305. [DOI] [PubMed] [Google Scholar]
- 60. Schimmel M, Ono T, Lam OL, Müller F. Oro‐facial impairment in stroke patients. J Oral Rehabil. 2017;44:313‐326. [DOI] [PubMed] [Google Scholar]
- 61. Schimmel M, Leuchter I, Heritier Barras A, et al. Oral function in Amyotrophic Lateral Sclerosis patients: a matched case‐control study. Clin Nutr. 2021;40:4904‐4911. [DOI] [PubMed] [Google Scholar]
- 62. Stupak HD, Park SY. Gravitational forces, negative pressure and facial structure in the genesis of airway dysfunction during sleep: a review of the paradigm. Sleep Med. 2018;51:125‐132. [DOI] [PubMed] [Google Scholar]
- 63. Sheiham A, Steele JG, Marcenes W, Finch S, Walls AW. The impact of oral health on stated ability to eat certain foods; findings from the National Diet and Nutrition Survey of Older People in Great Britain. Gerodontology. 1999;16:11‐20. [DOI] [PubMed] [Google Scholar]
- 64. O'Donnell LE, Smith K, Williams C, et al. Dentures are a Reservoir for Respiratory Pathogens. J Prosthodont. 2016;25:99‐104. [DOI] [PubMed] [Google Scholar]
- 65. Araie T, Okuno K, Ono Minagi H, Sakai T. Dental and skeletal changes associated with long‐term oral appliance use for obstructive sleep apnea: A systematic review and meta‐analysis. Sleep Med Rev. 2018;41:161‐172. [DOI] [PubMed] [Google Scholar]
- 66. Barbe AG, Schmidt‐Park Y, Hamacher S, Derman SHM, Noack MJ. Efficacy of GUM(R) Hydral versus Biotene(R) Oralbalance mouthwashes plus gels on symptoms of medication‐induced xerostomia: a randomized, double‐blind, crossover study. Clin Oral Investig. 2018;22:169‐180. [DOI] [PubMed] [Google Scholar]
- 67. van den Boorn HG, Stroes CI, Zwinderman AH, et al. Health‐related quality of life in curatively‐treated patients with esophageal or gastric cancer: A systematic review and meta‐analysis. Crit Rev Oncol Hematol. 2020;154:103069. [DOI] [PubMed] [Google Scholar]
- 68. WHO . Oral Health. WHO; 2012. [Google Scholar]
- 69. Kothari M, Svensson P, Huo X, Ghovanloo M, Baad‐Hansen L. Motivational conditions influence tongue motor performance. Eur J Oral Sci. 2013;121:111‐116. [DOI] [PubMed] [Google Scholar]
- 70. Kumar A, Grigoriadis J, Trulsson M, Svensson P, Svensson KG. Effects of short‐term training on behavioral learning and skill acquisition during intraoral fine motor task. Neuroscience. 2015;306:10‐17. [DOI] [PubMed] [Google Scholar]
- 71. Kumar A, Tanaka Y, Grigoriadis A, Grigoriadis J, Trulsson M, Svensson P. Training‐induced dynamics of accuracy and precision in human motor control. Sci Rep. 2017;7:6784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Zhang H, Kumar A, Luo X, Svensson K, Trulsson M, Svensson P. Effect of short‐term training on fine motor control in trigeminally innervated versus spinally innervated muscles. Hum Mov Sci. 2018;58:132‐139. [DOI] [PubMed] [Google Scholar]
- 73. Svensson P, Romaniello A, Wang K, Arendt‐Nielsen L, Sessle BJ. One hour of tongue‐task training is associated with plasticity in corticomotor control of the human tongue musculature. Exp Brain Res. 2006;173:165‐173. [DOI] [PubMed] [Google Scholar]
- 74. Svensson P, Romaniello A, Arendt‐Nielsen L, Sessle BJ. Plasticity in corticomotor control of the human tongue musculature induced by tongue‐task training. Exp Brain Res. 2003;152:42‐51. [DOI] [PubMed] [Google Scholar]
- 75. Komoda Y, Iida T, Kothari M, et al. Repeated tongue lift movement induces neuroplasticity in corticomotor control of tongue and jaw muscles in humans. Brain Res. 2015;1627:70‐79. [DOI] [PubMed] [Google Scholar]
- 76. Iida T, Komiyama O, Obara R, Baad‐Hansen L, Kawara M, Svensson P. Repeated clenching causes plasticity in corticomotor control of jaw muscles. Eur J Oral Sci. 2014;122:42‐48. [DOI] [PubMed] [Google Scholar]
- 77. Deng H, Gao S, Lu S, Kumar A, Zhang Z, Svensson P. Alteration of occlusal vertical dimension induces signs of neuroplastic changes in corticomotor control of masseter muscles: Preliminary findings. J Oral Rehabil. 2018;45:710‐719. [DOI] [PubMed] [Google Scholar]
- 78. Zhang H, Kumar A, Kothari M, et al. Can short‐term oral fine motor training affect precision of task performance and induce cortical plasticity of the jaw muscles? Exp Brain Res. 2016;234:1935‐1943. [DOI] [PubMed] [Google Scholar]
- 79. Arima T, Yanagi Y, Niddam DM, et al. Corticomotor plasticity induced by tongue‐task training in humans: a longitudinal fMRI study. Exp Brain Res. 2011;212:199‐212. [DOI] [PubMed] [Google Scholar]
- 80. The Academy of Prosthodontics . The Glossary of Prosthodontic Terms: Ninth Edition. J Prosthet Dent. 2017;117:e1‐e105. [DOI] [PubMed] [Google Scholar]
- 81. Woda A, Hennequin M, Peyron MA. Mastication in humans: finding a rationale. J Oral Rehabil. 2011;38:781‐784. [DOI] [PubMed] [Google Scholar]
- 82. Lindfors E, Arima T, Baad‐Hansen L, et al. Jaw Exercises in the Treatment of Temporomandibular Disorders‐An International Modified Delphi Study. J Oral Facial Pain Headache. 2019;33:389‐398. [DOI] [PubMed] [Google Scholar]
- 83. Hägg M, Tibbling L. Longstanding effect and outcome differences of palatal plate and oral screen training on stroke‐related dysphagia. Open Rehabil J. 2013;6:35‐42. [Google Scholar]
- 84. McKenna VS, Zhang B, Haines MB, Kelchner LN. A Systematic Review of Isometric Lingual Strength‐Training Programs in Adults With and Without Dysphagia. Am J Speech Lang Pathol. 2017;26:524‐539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Bircher J. Towards a dynamic definition of health and disease. Med Health Care Philos. 2005;8:335‐341. [DOI] [PubMed] [Google Scholar]
- 86. Hendricson WD, Cohen PA. Oral Health Care in the 21st Century: Implications for Dental and Medical Education. Acad Med. 2001;76:1181‐1206. [DOI] [PubMed] [Google Scholar]
- 87. Goncalves T, Schimmel M, van der Bilt A, et al. Consensus on the terminologies and methodologies for masticatory assessment. J Oral Rehabil. 2021;48:745‐761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Peyron MA, Lassauzay C, Woda A. Effects of increased hardness on jaw movement and muscle activity during chewing of visco‐elastic model foods. Exp Brain Res. 2002;142:41‐51. [DOI] [PubMed] [Google Scholar]
- 89. Peyron MA, Woda A, Bourdiol P, Hennequin M. Age‐related changes in mastication. J Oral Rehabil. 2017;44:299‐312. [DOI] [PubMed] [Google Scholar]
- 90. Ettinger RL. Changing dietary patterns with changing dentition: how do people cope? Spec Care Dentist. 1998;18:33‐39. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
There are no original data for this article available.


