Abstract
Background
The Age‐Friendly Health Systems (AFHS) aims to improve the experience of care for adults aged 65 years and older through the 4Ms framework, an evidence‐based approach to care planning that emphasizes what matters most to the older person, mentation, mobility, and medication. The aim of this study was to examine clinicians' attitudes, knowledge, and practices concerning AFHS and the 4Ms.
Methods
We surveyed U.S.‐based health care providers randomly identified from the Medscape database. The sample was weighted based on sex, U.S. Census region, and ethnic diversity of health occupations. We examined the differences between cohorts using proportions tests and logistic regression models.
Results
More than 90% of clinicians (n = 1684) agreed that “older patients require a different approach to care than younger patients.” Fifty percent of clinicians “always” take the age of their patient into consideration when determining care. A majority of clinicians said they discuss each of the 4Ms with older patients and/or their family caregivers. Screening for depression and review of high‐risk medication use are among the leading types of age‐friendly care that clinicians provide to older patients. A minority of clinicians are asking older adults about and aligning the care plan with What Matters.
Conclusions
A majority of clinicians acknowledged the benefits of providing care via AFHS but reported limited knowledge of the specificities of the 4Ms framework and are not necessarily taking the age of their patients into consideration when determining the best form of care. Health care settings that have implemented the 4Ms framework appear to be doing so in an incomplete way. Our study reinforces the case for training primary care providers on how to adopt the evidence‐based 4Ms framework in clinical practice effectively and consistently.
Keywords: 4Ms framework, Age‐Friendly Health Systems, health care
Key points
The evidence‐based 4Ms framework emphasizes what matters, mentation, mobility, and medication.
Clinicians are not consistently applying 4Ms framework when determining care for older adults.
Why does this paper matter?
Personalized, age‐friendly care based on the 4Ms framework can improve clinical outcomes.
INTRODUCTION
Older adults are major consumers of health care and experience high levels of contact with health systems. Adults aged 65 and older (described throughout as older patients) represent approximately 45% of the top 10% of health care users in terms of expenditures. 1 In 2019, 95.8% of older adults had a least one physician visit for any reason compared with an average of 82% for younger age groups. 2 Older adults also average three visits per year to primary care offices. 3 Many older people remain productive, creative, and engaged in their later years, challenging the prevailing view of aging as a period of decline and disease. Nonetheless, approximately 80% of adults over the age of 65 have at least one chronic condition such as hypertension (58%), ischemic heart disease (29%), and diabetes (28%). Approximately 75% have two or more chronic conditions. 4 , 5 , 6 Older adults also experience higher prevalence of Alzheimer's disease and related dementias. Such conditions can limit the ability of older adults to perform daily activities, reduce their independence, increase financial and care requirements, and increase the prevalence of hospitalizations. 7 However, older adults, especially older Black adults, are vulnerable to variability in health care delivery and often experience negative attitudes and age‐related discrimination from health care providers and health systems. 8 , 9 The fragmented system of health care in the United States contributes to unreliable care for older adults, including overutilization (e.g., diagnostic tests) and underutilization (e.g., preventive health) of services, which have the potential to cause personal and financial harm. 1
The John A. Hartford Foundation, Institute for Healthcare Improvement (IHI), American Hospital Association (AHA), and the Catholic Health Association have created a fresh approach to providing safe and effective care for older adults. The Age‐Friendly Health Systems (AFHS) movement builds on existing models of geriatric care and articulates with a wider ecosystem of age‐friendly public health, policies, cities, and states. 10 , 11 The goal of the AFHS initiative is to improve the experience of care for older adults, reduce health care‐related harm, improve satisfaction with care, reduce costs, and optimize value for patients, families, caregivers, health care providers, and health systems. 12 , 13 The AFHS initiative engendered the 4Ms framework to achieve these goals. This framework for implementing age‐friendly care focuses on knowing and acting on What Matters most to the older person as well as addressing key care concepts related to Mentation, Medication, and Mobility. 13
Evidence for the 4Ms framework
What Matters
Asking about What Matters through a values assessment and incorporating those values into individualized care plans is an anchoring practice for the 4Ms framework. 14 , 15 This vital step ensures shared decision‐making and collaborative goal setting, which improves physical and psychological health outcomes and health status indicators (e.g., hypertension and diabetes management, better medication adherence). 16 , 17 , 18
Mentation
Mentation is an important element of the 4Ms framework to ensure screening and management of depression, dementia, delirium, and cognitive impairment. Depression causes considerable distress among older adults but is often unrecognized or undertreated. Screening rates for depression in primary care remain low for older adults. 19 Delirium is associated with increased length of in‐patient hospital stay, higher likelihood of nursing home placement, incidence of falls, pressure injuries and incontinence, and decreasing cognitive and physical functioning. 20 Dementia is also a significant community health problem. More than 10% of older adults have dementia and almost one third of adults over 85 years have dementia. Several validated tools can be used as part of a 4Ms approach to screening for the mental health issues to support early implementation of care strategies that preserve function and reduce the need for pharmacology and restraints. 21 , 22
Medication
Medication practices in the 4Ms framework ensure safe dosing, deprescribing or avoidance of high‐risk medications, which have a direct bearing on What Matters, Mentation, and Mobility. At least 90% of older adults who are Medicare beneficiaries take at least one prescription medication and 40% take at least five prescription medications. 23 , 24 Polypharmacy and overprescribing are highly prevalent practices in the care of older adults that increase the risk for drug–drug interactions, reduce physical functioning and the ability to perform daily activities, and impact clinical outcomes. 23 The 4Ms framework provides a strategy to review and document high‐risk medication use, deprescribe high‐risk medication, ensure appropriate prescribing when such medication is necessary, and limit polypharmacy. The American Geriatric Society Beers Criteria for Potentially Inappropriate Medication Use in Older Adults and the STOPP/START (Screening Tool of Older Persons' Prescriptions/Screening Tool to Alert to Right Treatment) criteria provide evidence‐based protocols for screening and evaluating medication prescribing that are consistent with the 4Ms framework. 25 , 26
Mobility
Mobility encourages approaches that assist older adults in moving safely and regularly to maintain functional ability. The 4Ms framework can help to identify mobility limitations and support early, frequent, and safe activities that improve mobility. 14 Screening tools for mobility that are age‐friendly can be used to assess impairments that reduce mobility; evaluate environments to ensure mobility safety; and set individualized goals for daily mobility. A 4Ms approach to mobility can preserve function and reduce falls, pressure injury risk, functional decline, and risk for respiratory complications. 27 , 28
Study aims
These four essential elements are buttressed by a robust evidence base and designed to be implemented as a set of integrated, interprofessional practices that guide health care interactions with older adults and drive quality and safety in care planning. 29 Although the AFHS initiative is being disseminated across multiple hospitals, ambulatory practices, convenience care clinics, long‐term care/nursing home settings, specialist care settings, and cancer care, 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 there is little research on clinician and patient interactions regarding the 4Ms framework in primary care. The aim of this study was to describe how clinicians approach patient populations older than 65 years; explore primary care clinician perceptions of older patients; and assess clinician attitudes, knowledge, and practices concerning AFHS and the 4Ms.
METHODS
Survey methodology
We surveyed primary care clinicians practicing in the United States from early October to late December in 2020. Clinicians were randomly identified via Medscape, an active database with over 1.5 million clinician members that includes 61% of primary care American Medical Association physicians and provided a strong sampling frame for this study. We invited primary care clinicians via email to participate in a 7–8 min online survey. Respondents were required to be family medicine or internal medicine specialists, see 25 or more patients ages 65 or older in an average month, and self‐identify as Hispanic origin, White, Asian, or Black. The response rate was 0.9%. 35 Qualified survey completers received an Amazon gift card. Standard quality control measures included checking for clear question wording, proper question ordering, and the use of appropriate scales and response categories. During the field period, the surveys were checked to ensure that respondents were answering all questions logically and that skip pattern programming functioned as expected. Respondents who completed the surveys in less than 25% of the median survey completion time were removed from the final data analysis. The sample was weighted to match the sex, U.S. Census region, and race and ethnicity proportions of corresponding health occupations (2011–2015). 36 Respondents of Hispanic origin were counted once to address overlap between Hispanic origin with other race/ethnicity categories.
We applied statistical modeling techniques to examine the differences between cohorts (e.g., specialty) whereas adjusting for the effects of the following covariates: race/ethnicity, age, sex, region, practice location setting, work situation, practice setting, and level of operational management responsibility. The multivariate logistic regression models were fitted to the binary responses, and General Linear Models were fitted to quantitative responses. The statistical differences at the 95% confidence level were noted with uppercase letters in the tables.
RESULTS
Demographics
Participants included 1684 primary care clinicians, specifically physicians (n = 575), nurse practitioners (NPs) (n = 613), and physician assistants (PAs) (n = 496). On average, clinicians reported treating at least 236 patients per month in person or virtually. The majority of older patients seen per month was aged 65 to 74 years. Just over half of the total patients for physicians and NPs were 65 years or older, and slightly less than half for PAs. NPs (40%) and PAs (37%) reported more total patients on Medicaid than physicians (27%) and NPs (38%) reported more older patients on Medicaid than physicians (29%). The majority of patients aged 65 or older were White and approximately 20% were Black. NPs saw a higher proportion of Black patients (24%) than physicians (20%) and PAs saw more patients of Hispanic, Latino/a, or Spanish origin (22%) than physicians and NPs (both 18%). Clinicians in urban settings reported a higher number of Black (31%) and Hispanic (29%) patients than clinicians in rural/frontier settings. Clinicians in suburban and rural settings reported a higher number of White patients than clinicians in urban settings. Tables S1 and S2 summarize the demographic characteristics of the patients by clinicians' specialty and primary practice location.
Perceptions of patients
The majority of clinicians “strongly” or “somewhat agree” that “older patients require a different approach to care than younger patients”; “there is not enough attention given to the health care needs of older patients today”; and “patients are not always treated fairly because of their socioeconomic background or racial/ethnic identity.” NPs and PAs were more likely to “strongly” or “somewhat agree” that “there is not enough attention given to the health care needs of older patients today” than are physicians. Forty‐three percent of physicians tended to “strongly” or “somewhat agree” that “it is up to the patient to tell me what their needs are,” whereas a similar proportion of NPs and PAs “somewhat” or “strongly disagree.” About 40% of clinicians “strongly” or “somewhat agree” that “older patients are more proactive than younger patients in managing their own health care” (Table 1). Non‐Hispanic Black physicians (58%) were more likely to “strongly agree” that “patients are not always treated fairly because of their socioeconomic background or racial/ethnic identity” compared to Non‐Hispanic White physicians (26%).
TABLE 1.
Clinician perceptions and characteristics of overall patient and age‐friendly care
| Physicians (A) | NPs (B) | PAs (C) | |
|---|---|---|---|
| Perceptions of patients by clinicians | |||
| Base: total respondents | 575 | 613 | 496 |
| Older patients require a different approach to care than younger patients | |||
| Strongly/somewhat agree (NET) | 93% | 96% | 97% |
| Neither agree nor disagree | 5% B,C | 2% A | 2% A |
| Somewhat/strongly disagree (NET) | 2% | 1% | 1% |
| There is not enough attention given to the health care needs of older patients today | |||
| Strongly/somewhat agree (NET) | 61% B,C | 78% A | 72% A |
| Neither agree nor disagree | 20% B,C | 10% A,C | 15% A,B |
| Somewhat/strongly disagree (NET) | 19% B,C | 12% A | 13% A |
| It is up to the patient to tell me what their needs are | |||
| Strongly/somewhat agree (NET) | 43% | 37% | 38% |
| Neither agree nor disagree | 22% | 19% | 23% |
| Somewhat/strongly disagree (NET) | 35% B | 44% A | 40% |
| Patients are not always treated fairly because of their socioeconomic background or racial/ethnic identity | |||
| Strongly/somewhat agree (NET) | 68% | 63% | 71% |
| Neither agree nor disagree | 12% | 16% | 12% |
| Somewhat/strongly disagree (NET) | 19% | 21% | 16% |
| Older patients are more proactive than younger patients in managing their own health care | |||
| Strongly/somewhat agree (NET) | 42% | 37% | 41% |
| Neither agree nor disagree | 34% | 31% | 28% |
| Somewhat/strongly disagree (NET) | 23% B,C | 32% A | 31% A |
| Types of age‐friendly care provided by clinicians | |||
| Base: total respondents | 575 | 613 | 496 |
| Review for high‐risk medication use | 84% | 91% | 85% |
| Screen for depression | 84% | 90% | 86% |
| Screen for cognitive impairment | 79% | 85% | 81% |
| Deprescribe and dose‐adjust high‐risk medications and avoid their use whenever possible | 78% | 80% | 83% |
| Screen for mobility limitations | 73% | 82% | 76% |
| If depression screen is positive, identify and manage factors contributing to depression and initiate, or refer out for treatment | 70% | 77% | 74% |
| If cognitive impairment screen is positive, refer for further evaluation and manage manifestations of cognitive impairment | 60% B | 70% A | 67% |
| Ensure early, frequent, and safe mobility | 56% | 61% | 56% |
| Ask the older adult What Matters | 36% | 42% | 40% |
| Align the care plan with What Matters | 29% | 32% | 31% |
| Other | 2% | 2% | 2% |
| None of the above | 2% B,C | 1% A | 1% A |
Note: An uppercase letter next to a data point indicates a significant difference at the 95% confidence level between the subsegments that are being compared (e.g., A next to the number indicates that it is different from Physicians, B that is different from NPs, and C that it is different from PAs).
Familiarity with the AFHS concept and 4Ms framework
Fifty percent of clinicians “always” take the age of their patient into consideration when determining care. More NPs (69%) “always” consider age compared with physicians and PAs (50% and 55%, respectively, with a significantly larger effect size for NPs, Figure 1A). Physicians and PAs reported less familiarity with the concept of AFHS than NPs. About 40% of physicians and PAs are “slightly” or “not at all familiar” with the concept of AFHS compared to NPs (32%). At least three‐quarters of clinicians are “slightly” or “not at all familiar” with the 4Ms framework (Figure 1B).
FIGURE 1.
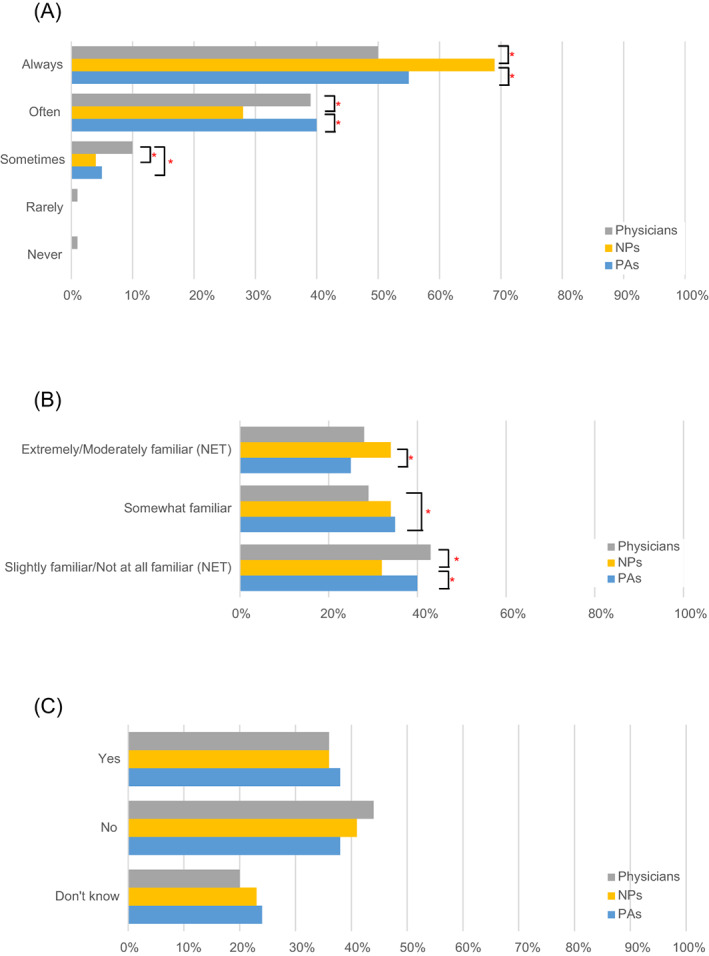
Attitudes and behaviors around the 4Ms and Age‐Friendly Health Systems. Prevalence of taking patient's age into consideration when determining care (A); familiarity with the Age‐Friendly Health System 4Ms framework (B); and clinician current use of the Age‐Friendly Health Systems approach (C). The differences between the specialties were analyzed using logistic regression models adjusting for demographics and other covariates as described in Methods. The brackets and asterisk (*) indicate statistically significant differences at the 95% confidence level
Clinicians with “a lot” of operational management responsibility are more likely to be “extremely” or “moderately familiar” with the 4Ms framework than are clinicians who have no such responsibility (Table 2). Approximately 60% of clinicians are either not currently using the AFHS approach in their health care setting (40%) or are unaware whether their health care setting is currently using this approach (Figure 1C).
TABLE 2.
Familiarity with the AFHS 4Ms framework by clinician level of operational management responsibility
| A lot (A) | Some (B) | Not that much (C) | None at all (D) | |
|---|---|---|---|---|
| Base: total physician respondents | 144 | 203 | 160 | 68 |
| Extremely/moderately familiar (NET) | 14% D | 12% | 9% | 4% A |
| Somewhat familiar | 17% C | 18% C,D | 8% A,B | 7% B |
| Slightly familiar/not at all familiar (NET) | 69% | 70% | 83% | 88% |
| Base: total NP respondents | 106 | 191 | 189 | 127 |
| Extremely/moderately familiar (NET) | 26% B,C,D | 14% A,D | 10% A | 6% A,B |
| Somewhat familiar | 17% C,D | 15% | 8% A | 8% A |
| Slightly familiar/not at all familiar (NET) | 57% C,D | 71% | 82% A | 87% A |
| Base: total PA respondents | 58 | 163 | 172 | 103 |
| Extremely/moderately familiar (NET) | 31% B,C,D | 12% A,C,D | 3% A,B | 3% A,B |
| Somewhat familiar | 16% D | 13% D | 7% | 3% A,B |
| Slightly familiar/not at all familiar (NET) | 53% C,D | 75% | 90% A | 94% A |
Note: An uppercase letter next to a data point indicates a significant difference at the 95% confidence level between the subsegments that are being compared (e.g., A next to the number indicates that it is different from “A lot,” B that is different from ”Some,” etc.).
Types of age‐friendly care provided by clinicians
Screening for depression and review of high‐risk medication use are among the leading types of age‐friendly care that clinicians provide to older patients. A minority of clinicians are asking older adults about and aligning the care plan with What Matters. More NPs than physicians (70% vs. 60%) are referring patients for further evaluation and managing signs of cognitive impairment if the cognitive impairment screen is positive (Table 1).
Clinicians with “a lot” of operational management responsibility say their health care settings are more often asking the older adult What Matters than peers who have no operational responsibility (Physicians = 48% vs. 15%; NPs = 59% vs. 30%). Clinicians with “a lot” of operational management responsibility are more often aligning the care plan with What Matters compared to their counterparts with no operational responsibility (Physicians = 38% vs. 15%; NPs = 55% vs. 23%; PAs = 50 vs. 24%) (Table 2).
4Ms most challenging in practice
Mentation was the most challenging 4M element to address with older patients for physicians and PAs. NPs found Medication the most challenging. Physicians in hospitals found Medication the most challenging 4M compared with physicians in office settings (38% vs. 25%). All clinicians identified Mobility as the least challenging of the 4Ms to address (Figure 2A).
FIGURE 2.
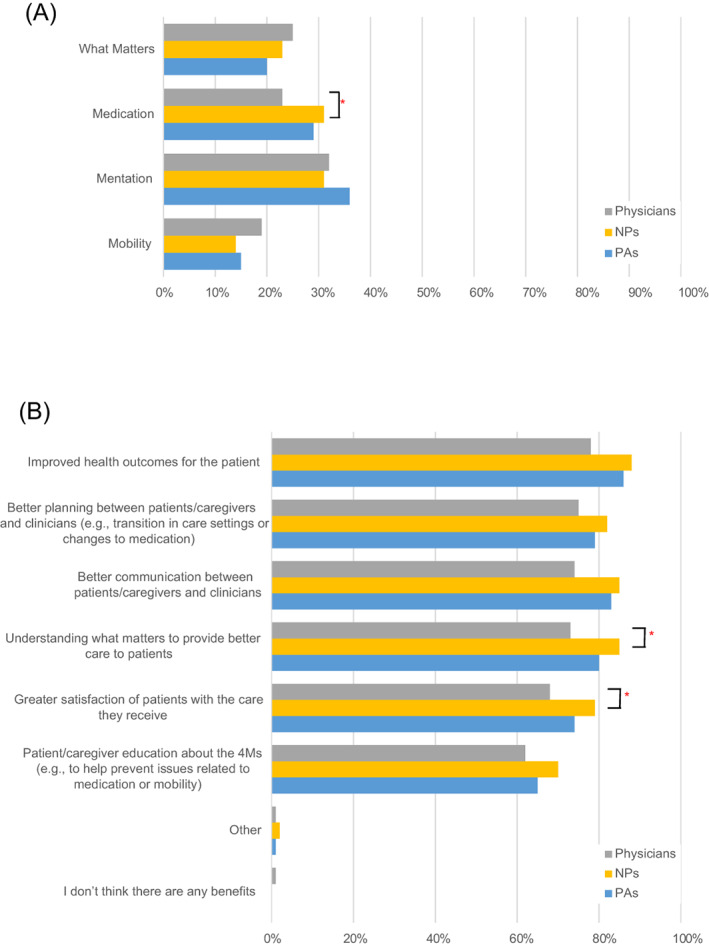
Perceptions and benefits of the 4Ms approach 4Ms most challenging in practice by clinicians (A), benefits of discussing the 4Ms (B). The differences between the specialties were analyzed using logistic regression models adjusting for demographics and other covariates as described in Methods. The brackets and asterisk (*) indicate statistically significant differences at the 95% confidence level
Discussing the 4Ms with patients and caregivers
A majority of clinicians said they discuss each of the 4Ms with older patients and/or their family caregivers. Clinicians tend to discuss What Matters, Medication, and Mobility more often with patients than with caregivers. NPs were more likely to discuss What Matters with caregivers of older patients than were PAs. Improved health outcomes, better planning between patients/caregivers and clinicians, and better communication between patients/caregivers and clinicians were the top reported benefits of having discussions about the 4Ms with older patients and their caregivers. NPs were more likely to cite “understanding what matters to provide better care” and “greater satisfaction of patients with the care they receive” as benefits to having these discussions compared to physicians (Figure 2B).
Barriers and facilitators to adopt the AFHS approach and ensure successful 4Ms care
More NPs than PAs reported their team's unfamiliarity with the 4Ms as a barrier to care. More physicians reported lack of time as a barrier for them and their team to address the 4Ms compared to NPs (Figure 3A). Clinicians identified training on effective implementation of the 4Ms in their health care setting, resources to educate nonclinical staff about the 4Ms as it relates to their role, and an outlined care approach model tailored to their specific health care setting as the leading tools or resources they need to adopt an age‐friendly health system approach (Figure 3B).
FIGURE 3.
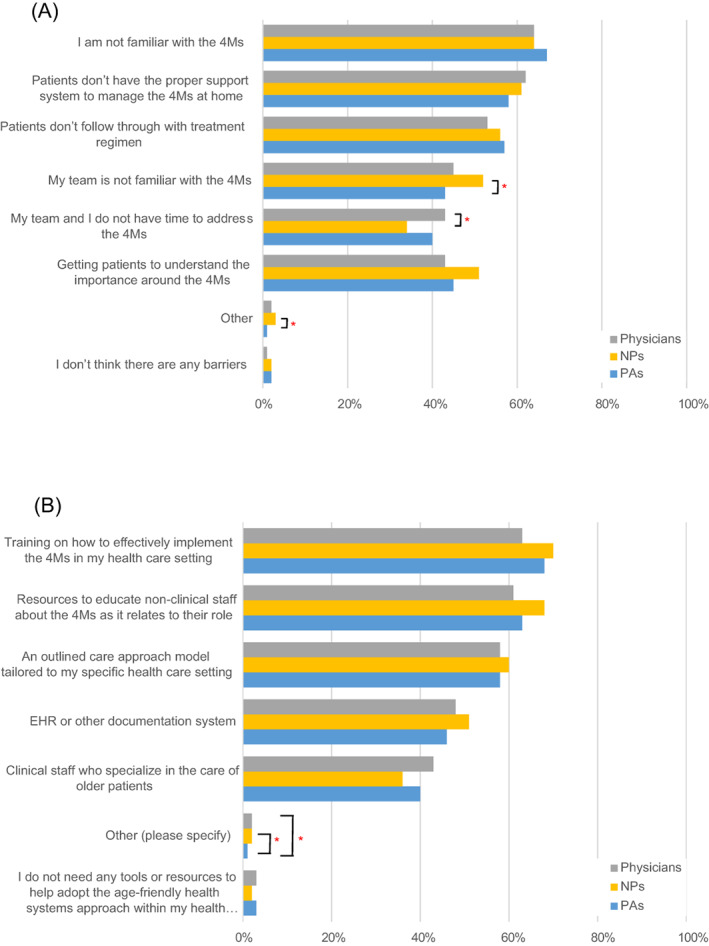
Barriers of the 4Ms and tools needed to adopt the AFHS approach. Barriers to ensuring successful 4Ms care by clinicians (A), and tools or resources needed to adopt the Age‐Friendly Health Systems approach (B). The differences between the specialties were analyzed using logistic regression models adjusting for demographics and other covariates as described in Methods. The brackets and asterisk (*) indicate statistically significant differences at the 95% confidence level
DISCUSSION
Familiarity with and appreciation for an age‐friendly approach to care is increasing
Clinicians in this study care for a high volume of older patients with at least half of their patients aged 65 years or older. Physician office visit and services have become increasingly concentrated among older adults, who comprise 45% of physician visits in primary care and 55% in medical or surgical specialties. 37 Given this volume, it is heartening to see that a majority (>90%) of clinicians in the study recognize that older patients require a different approach to care than younger patients. Most clinicians (60% of physicians and PAs; approximately 70% of NPs) were familiar with the general concept of AFHS, especially clinicians with greater operational management responsibility. Most clinicians acknowledged the benefits of providing care via the 4Ms framework, such as improved health outcomes, better planning between patients/caregivers and clinicians, and better communication between patients/caregivers and clinicians. These findings are important because negative attitudes toward older adults in health care have long been persistent across professional disciplines and care settings. 38 Indeed, a recent longitudinal analysis of data from the Health and Retirement Study reported that one in five adults over the age of 50 experience age‐related discrimination in health care. 39
Gaps remain in familiarity with and implementation of the 4Ms framework
Recognition of the importance of an age‐friendly approach to care and familiarity with AFHS as a broad concept are tempered by lack of clinician awareness about whether their health care setting is using an age‐friendly approach to care, limited knowledge of the specificities of the 4Ms framework, and gaps in practice. To our knowledge, no other study has examined differences in clinicians' behavior related to 4Ms, although nurses have been at the forefront of developing geriatric care models. 22 Clinicians are not taking the age of their patients into consideration when determining the best form of care. NPs fared somewhat better in this respect. Approximately half of physicians and PAs consider age as part of their routine practice versus 69% of NPs. Although most clinicians were unfamiliar with the 4Ms framework, clinicians are initiating conversations about age‐friendly care, engaging caregivers in these discussions, and providing specific types of age‐friendly care that align with a focus on Mentation, Medication, and Mobility, such as screening for depression and reviewing for high‐risk medication use. NPs were statistically more likely than physicians to emphasize the importance of understanding what matters to patients as a foundation for providing better care and increasing patient satisfaction with the care they receive (odds ratio = 1.42, p‐value = 0.0465). This significant difference in awareness of the 4Ms framework might reflect ongoing efforts to empower nurses to deliver geriatric care using the 4Ms framework. For instance, programs such as the Nurses Improving Care for Healthsystem Elders (NICHE) initiative have been designed to educate the nursing workforce about how to assess older patients and implement personalized plans of care using the 4Ms framework. 27 Nonetheless, only a minority say their health care setting is asking the older adult What Matters and aligning the care plan accordingly.
Barriers to implementing the 4Ms framework
Although the majority of clinicians (75%–80%) did not rate What Matters as the most challenging 4M to implement, 30%–40% of clinicians are not asking older patients What Matters nor are they aligning care plans with What Matters in their current practice. Other barriers to implementing the 4Ms as a framework for providing reliable, evidence‐based, age‐friendly care include lack of familiarity with this approach, lack of a support system for patients to manage the 4Ms at home, and lack of patient follow‐through with treatment. Initiatives within specific health systems have shown that integrating the 4M framework is both feasible and improves clinical outcomes. For instance, a quality improvement initiative in MedStar's Center for Successful Aging ambulatory clinical pathway resulted in an upward trend in patients receiving 4Ms care during their new patient visits. 40 Providers were enthusiastic about the incorporation of the 4Ms framework in the high‐risk rounds discussion and clinical outcomes improved for high‐risk medications and deprescribing. 40 The Geriatrics Workforce Enhancement Program funded by the Health Resources and Services Administration now requires a 4Ms approach at all of its training sites, which will help increase implementation. A special theme issue of the journal HSR is soliciting health services research articles on the impact of age‐friendly care. 41 , 42
Limitations
The Medscape sample might not be demographically representative of actual clinician populations. To balance the survey population for each subgroup (MD, NP, PA), we developed weights to match each subgroup on sex, U.S. Census region, and race proportions to data from the U.S. Department of Health and Human Services. 36 We oversampled and weighted underrepresented groups to minimize potential variability of results due to sampling errors. The survey had a low response rate and may have other limitations typical to the online studies, such as honesty in responses and lack of depth. The quality control measures were taken as described in the Methods to ensure reliability of the results.
CONCLUSION
The American population is experiencing an age‐related demographic shift. By 2034, adults over the age of 65 years will outnumber children for the first time in U.S. history. 43 The number of people aged over 65 years in the United States is expected to double by 2060 to 95 million, comprising 25% of the population. 6 , 43 At the same time, the United States is becoming more racially and ethnically heterogeneous. By 2030, the non‐Hispanic white population will be the numerical minority population whereas racial and ethnic minority populations are projected to increase from 23% to 34%. 6 , 43 Health care delivery will have to change to meet the needs of this demographic shift. For instance, digital health technologies such as voice‐ and sensor‐based applications that detect changes in neurological status or falls, as well as socially assistive robots that help with physical tasks, will likely augment health care delivery for aging adults with multimorbidity and complex health needs. 44 These demographic and technology changes underscore the need for health care providers to be skilled in assessing older adults about their needs, values, and preferences as a foundation for an age‐friendly approach to managing chronic conditions, care coordination, and medication adherence. However, at present, the education of health care providers across the continuum from undergraduate to continuing professional development lacks a uniform focus on reliable content related to What Matters, Medication, Mentation, and Mobility. 27 Our approach is to provide the 4Ms framework as an elegant model that will support health care providers in developing a consistent approach to assessment in these areas utilizing the comprehensive list of available resources and the opportunity to join action communities led by the IHI and the AHA. 29 , 45
Our study highlights persistent knowledge and skill gaps among primary care providers and reinforces the case for training clinicians on how to adopt this core set of evidence‐based care practices effectively and consistently in their health care settings. Clinician awareness and implementation of 4Ms is vital to the expansion of equitable, person‐centered, high‐quality health care for older adults. When personalized, age‐friendly care based on the 4Ms framework is integrated into older adult care, clinical outcomes improve. The time is ripe to move the needle from incorporating some of the 4Ms, some of the time, to all the 4Ms all of the time.
CONFLICT OF INTEREST
The authors have no conflicts. Two of the co‐authors (MRE and TF) work for The John A. Harford Foundation. Four of the co‐authors (SL, SZ, CL, and JW) work for WebMD.
AUTHOR CONTRIBUTIONS
Terry Fulmer, Marcus R. Escobedo, and John Whyte conceived the study concept and design. Christina Louie and Sarah Lesser oversaw the subject recruitment and data collection. Sarah Lesser and Stanislav Zakharkin performed the data analysis. Sarah Lesser prepared the draft. All authors contributed to interpretation of the data, participated in revising the manuscript for important intellectual content, and gave final approval of the submitted version.
SPONSOR'S ROLE
Two of the co‐authors (MRE and TF) work for The John A. Harford Foundation.
FINANCIAL DISCLOSURE
Funding was provided by The John A. Hartford Foundation.
Supporting information
Table S1. Demographic characteristics of patients by the clinicians' specialty.
Table S2. Race and ethnicity of patients by the clinicians' primary practice location.
ACKNOWLEDGMENTS
We thank Alexandra Howson, PhD, of Thistle, for assistance in writing and editing the manuscript.
Lesser S, Zakharkin S, Louie C, Escobedo MR, Whyte J, Fulmer T. Clinician knowledge and behaviors related to the 4Ms framework of Age‐Friendly Health Systems. J Am Geriatr Soc. 2022;70(3):789‐800. doi: 10.1111/jgs.17571
Funding information The study was sponsored by The John A. Hartford Foundation.
REFERENCES
- 1. Zayas CE, He Z, Yuan J, et al. Examining healthcare utilization patterns of elderly middle‐aged adults in the United States. Proc Int Fla AI Res Soc Conf. 2016;2016:361‐366. [PMC free article] [PubMed] [Google Scholar]
- 2. National Center for Health Statistics . Percentage of Having a Doctor Visit for any Reason in the Past 12 Months for Adults Aged 18 and over, United States, 2019. National Health Interview Survey. Centers for Disease Control and Prevention; 2021. [Google Scholar]
- 3. Petterson SMR, Klink K, Meyers D, Bazemore A. The State of Primary Care in the United States. A Chartbook of Facts and Statistics. Robert Graham Center; 2018. [Google Scholar]
- 4. National Center for Chronic Disease Prevention and Health Promotion (U.S.). Division of Adult and Community Health . Healthy Aging at a Glance, 2015: Helping People to Live Long and Productive Lives and Enjoy a Good Quality of Life. Centers for Disease Control and Prevention; 2011:5. [Google Scholar]
- 5. National Institute on Deafness and Other Communication Disorders . Quick statistics about hearing. 2021. Accessed August 20, 2021. https://www.nidcd.nih.gov/health/statistics/quick-statistics-hearing
- 6. The Administration for Community Living . 2020 Profile of Older Americans; 2021.
- 7. Gilchrist C, Eagen T, Herrera‐Venson A. Data Trends, Publications, and Implications from National CDSME and Falls Prevention Database. National Council on Aging; 2019. [Google Scholar]
- 8. Wyman MF, Shiovitz‐Ezra S, Bengel J. Ageism in the health care system: providers, patients, and systems. In: Ayalon L, Tesch‐Römer C, eds. Contemporary Perspectives on Ageism. Springer International Publishing; 2018:193‐212. [Google Scholar]
- 9. Population Reference Bureau . Key Factors Underlying Racial Disparities in Health between Black and White Older Americans. Population Reference Bureau; 2021. [Google Scholar]
- 10. Mate KS, Berman A, Laderman M, Kabcenell A, Fulmer T. Creating Age‐Friendly Health Systems ‐ a vision for better care of older adults. Healthc (Amst). 2018;6(1):4‐6. [DOI] [PubMed] [Google Scholar]
- 11. Fulmer T, Patel P, Levy N, et al. Moving toward a global age‐friendly ecosystem. J Am Geriatr Soc. 2020;68(9):1936‐1940. [DOI] [PubMed] [Google Scholar]
- 12. Tabbush V, Pelton L, Make K, Duong T. The Business Case for Becoming an Age‐Friendly Health System. Institute for Healthcare Improvement. 2019. Accessed August 20, 2021. http://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Documents/IHI_Business_Case_for_Becoming_Age_Friendly_Health_System.pdf
- 13. Fulmer T, Mate KS, Berman A. The age‐friendly health system imperative. J Am Geriatr Soc. 2018;66(1):22‐24. [DOI] [PubMed] [Google Scholar]
- 14. Carmody J, Black K, Bonner A, Wolfe M, Fulmer T. Advancing gerontological nursing at the intersection of age‐friendly communities, health systems, and public health. J Gerontol Nurs. 2021;47(3):13‐17. [DOI] [PubMed] [Google Scholar]
- 15. Cacchione PZ. Age‐Friendly Health Systems: the 4Ms framework. Clin Nurs Res. 2020;29(3):139‐140. [DOI] [PubMed] [Google Scholar]
- 16. Whitehead L. The effects of personalized care planning for adults living with chronic conditions. Int J Nurs Pract. 2016;22(2):138‐140. [DOI] [PubMed] [Google Scholar]
- 17. Berlowitz DR, Foy CG, Kazis LE, et al. Effect of intensive blood‐pressure treatment on patient‐reported outcomes. N Engl J Med. 2017;377(8):733‐744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Naik AD, Palmer N, Petersen NJ, et al. Comparative effectiveness of goal setting in diabetes mellitus group clinics: randomized clinical trial. Arch Intern Med. 2011;171(5):453‐459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Akincigil A, Matthews EB. National rates and patterns of depression screening in primary care: results from 2012 and 2013. Psychiatr Serv. 2017;68(7):660‐666. [DOI] [PubMed] [Google Scholar]
- 20. Krogseth M, Wyller TB, Engedal K, Juliebø V. Delirium is a risk factor for institutionalization and functional decline in older hip fracture patients. J Psychosom Res. 2014;76(1):68‐74. [DOI] [PubMed] [Google Scholar]
- 21. Pierre JS, Twibell R. Developing nurses' geriatric expertise through the geriatric resource nurse model. Geriatr Nurs. 2012;33(2):140‐149. [Google Scholar]
- 22. Pettis J. Nurses leading the way to age‐friendly care using the 4Ms model. Geriatr Nurs. 2020;41(2):195‐197. [DOI] [PubMed] [Google Scholar]
- 23. Charlesworth CJ, Smit E, Lee DS, Alramadhan F, Odden MC. Polypharmacy among adults aged 65 years and older in the United States: 1988‐2010. J Gerontol A Biol Sci Med Sci. 2015;70(8):989‐995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kirzinger A, Neuman T, Cubanski J, Brodie M. Data Note: Prescription Drugs and Older Adults. 2019. Accessed June 8, 2021.
- 25. By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel . American Geriatrics Society 2019 updated AGS beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674‐694. [DOI] [PubMed] [Google Scholar]
- 26. O'Mahony D, O'Sullivan D, Byrne S, O'Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213‐218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Squires A, Murali KP, Greenberg SA, Herrmann LL, D'Amico CO. A scoping review of the evidence about the nurses improving care for healthsystem elders (NICHE) program. Gerontologist. 2019;61(3):e75‐e84. [DOI] [PubMed] [Google Scholar]
- 28. Klein LM, Young D, Feng D, et al. Increasing patient mobility through an individualized goal‐centered hospital mobility program: a quasi‐experimental quality improvement project. Nurs Outlook. 2018;66(3):254‐262. [DOI] [PubMed] [Google Scholar]
- 29. Mate K, Fulmer T, Pelton L, et al. Evidence for the 4Ms: interactions and outcomes across the care continuum. J Aging Health. 2021;33:469‐481. doi: 10.1177/0898264321991658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shah RC, Supiano MA, Greenland P. Aligning the 4Ms of Age‐Friendly Health Systems with statin use for primary prevention. J Am Geriatr Soc. 2020;68(3):463‐464. [DOI] [PubMed] [Google Scholar]
- 31. Dolansky MA, Pohnert A, Ball S, McCormack M, Hughes R, Pino L. Pre‐implementation of the Age‐Friendly Health Systems evidence‐based 4Ms framework in a multi‐state convenient care practice. Worldviews Evid Based Nurs. 2021;18(2):118‐128. [DOI] [PubMed] [Google Scholar]
- 32. Greenberg S, Pino L, McCormack M, et al. Embedding age‐friendly care using the 4Ms framework in the convenient care setting. Innov Aging. 2020;4(Suppl 1):902. [Google Scholar]
- 33. Edelman LS, Drost J, Moone RP, et al. Editorial: applying the age‐friendly health system framework to long term care settings. J Nutr Health Aging. 2021;25(2):141‐145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Vonnes C, Mason TM. Crafting age friendly cancer care: a model for improvement utilizing the 4Ms framework across the continuum of an NCI‐designated Cancer Center. J Geriatr Oncol. 2021;12(1):152‐156. [DOI] [PubMed] [Google Scholar]
- 35. American Association of Public Opinion Research . Response Rates – An Overview. 2016. Accessed August 20, 2021. https://www.aapor.org/Education-Resources/For-Researchers/Poll-Survey-FAQ/Response-Rates-An-Overview.aspx
- 36. United States Department of Health and Services. Health Resources and Services Administration, National Center for Health Workforce Analysis . Sex, Race, and Ethnic Diversity of U.S, Health Occupations (2011‐2015). United States Department of Health and Services; 2017. [Google Scholar]
- 37. Cherry DLC, Decker SL. Population aging and the use of office‐based physician services. NCHS Data Brief. 2010;41:1‐8. [PubMed] [Google Scholar]
- 38. Institute of Medicine . Retooling for an Aging America: Building the Health Care Workforce. National Academies Press; 2008. [PubMed] [Google Scholar]
- 39. Rogers SE, Thrasher AD, Miao Y, Boscardin WJ, Smith AK. Discrimination in healthcare settings is associated with disability in older adults: Health and Retirement Study, 2008‐2012. J Gen Intern Med. 2015;30(10):1413‐1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Guth A, Chou J, Courtin SO, Ford C, Hennawi G, Brandt N. An interdisciplinary approach to implementing the age‐friendly health system 4Ms in an ambulatory clinical pathway with a focus on medication safety. J Gerontol Nurs. 2020;46(10):7‐11. [DOI] [PubMed] [Google Scholar]
- 41. Edelman LS, Drost J, Moone RP, et al. Applying the age‐friendly health system framework to long term care settings. J Nutr Health Aging. 2021;25:c141‐c145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Health Services Research . Special Issue Call for Abstracts: Age‐Friendly Health Systems. Accessed October 19, 2021. https://www.hsr.org/special-issue-call-abstracts-age-friendly-health-system
- 43. Vespa JML, Armstrong DA. Demographic Turning Points for the United States: Population Projections for 2020 to 2060. United States Census Bureau. Population Estimates and Projections; 2020. [Google Scholar]
- 44. Evangelista L, Steinhubl SR, Topol EJ. Digital health care for older adults. Lancet. 2019;393(10180):1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. The Institute for Healthcare Improvement . Resources to Practice Age‐Friendly Care. Accessed October 10, 2021. http://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Pages/Resources.aspx
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Demographic characteristics of patients by the clinicians' specialty.
Table S2. Race and ethnicity of patients by the clinicians' primary practice location.


