Abstract
Background
Diabetes is a chronic metabolic disease characterized by hyperglycemia that often occurs in adults. Many studies have indicated that exercise is beneficial to the medical management of diabetes. Bibliometric analysis can help investigators to identify the current research concerns to guide future research directions. Nevertheless, the overview bibliometric analysis of this global research topic related to exercise and diabetes is lacking. The present bibliometric study aimed to investigate development trends and research hotspots of exercise and diabetes research and provide researchers with new perspectives in further studies.
Materials and Methods
The articles and reviews regarding exercise and diabetes between 2000 and 2020 were retrieved from the Web of Science Core Collection. The scientometrics analytical tool CiteSpace software was used to analyze the cooperation among countries/institutions/journals/authors, analysis of co-occurrence keywords, keywords bursts, and references.
Results
In all, 3,029 peer-reviewed papers were found with a persistently increased tendency over time. The most prolific country and institution were the USA (965) and Univ Alberta (76), respectively. Diabetes Care published most papers (178) and was the most co-cited journal (2,630). Riddell MC had the most publications (53), and Sigal RJ was the most influential author (503 cited times). Colberg et al.'s paper (co-citation counts: 183) showed the strongest citation bursts by the end of 2020, which was the most representative reference. The four research focuses were mellitus, exercise, physical activity, and glycemic control. The two frontiers trends were sedentary behavior and stress. The combination of aerobic and resistance training can effectively improve glycemic control, decrease HbA1c levels, enhance cardiorespiratory fitness, improve lipid levels, and decrease the demand for non-insulin antihyperglycemic agents.
Conclusions
This study offers a scientific perspective on exercise and diabetes research and provides investigators with valuable information to detect the current research condition, hotspots, and emerging trends for further study.
Keywords: bibliometric analysis, exercise, diabetes, CiteSpace, research hotspots
Introduction
Diabetes mellitus is a metabolic disease characterized by hyperglycemia for a prolonged period (1). As a chronic medical disease that causes many clinical symptoms and complications, diabetes is related to long-term damage, deterioration, and dysfunction of different organs and systems, especially the kidneys, eyes, nervous system, and cardiovascular system (2). A recent study indicated that about 537 million people worldwide have diabetes, equivalent to 9.8% of the world's adult (20–79 years) population. In 2021, approximately 6.7 million adults aged 20–79 worldwide will die from diabetes, and its complications, with 80% of cases occurring in low- and middle-income countries (3). Given the sizable scope and passive influence of diabetes in the public health area, the effective therapeutic intervention of diabetes has continuously been a research hotspot in medicine.
The previous studies have shown that the problematic situation regarding diabetes could be relieved through advisable medical management and health education (4). With the spread of the idea of “exercise is medicine,” appropriate physical activity and exercise according to the individual characteristics and health status of diabetic patients are crucial for their blood glucose management and overall health (5, 6). Various therapeutic exercise therapies are applied to intervene in diabetes. Many studies have revealed that aerobic exercise, resistance exercise, flexibility, and balance exercises can improve the quality of life of diabetic patients in many aspects, such as enhancing the function of the cardiovascular system, reducing the insulin resistance, improving the blood glucose control, and reducing the risk of falling (7–9). However, there is a lack of relevant quantitative bibliometric analysis summarizing the research progress of exercise therapy intervention in diabetes in recent decades.
Bibliometric analysis, a series of mathematics and statistical analysis for assessing and quantifying publication data, has been utilized to detect the vital researchers, institutions, and countries and their cooperation. Analysis of keywords, references, and co-citation analysis can reveal the global trends and research hotspots (10). In recent years, bibliometrics have been applied in various research fields, such as pain, dyslexia, depression, and cancer rehabilitation (11–13). Outcomes from the bibliometric study can help investigators to identify the current research concerns to guide future research directions. Given the considerable superiority of this method, applying bibliometrics has great significance in the domain of exercise and diabetes research.
This study conducts bibliometrics of exercise and diabetes research based on relevant papers published from 2000 to 2020 to identify the emerging global trends and obtain new insights to guide future research directions.
Materials and Methods
Data Acquisition
We performed a comprehensive search of original articles and reviews from 1 January 2000 to 31 December 2020, using the SCIE of the Web of Science Core Collection (WoSCC) on 6 November 2021. Despite the many literature databases available for the study of global trends and research hotspots, we selected the WoSCC database because it included much documents information, especially in the fields of diabetes and public health. The data search strategy was “TI = (exercise* OR kinesitherapy OR training OR “physical activit*” OR sport* OR fitness OR walk* OR run* OR swim* OR jog* OR cycling OR pilates* OR yoga OR qigong OR “tai chi”) AND TI = (diabetes OR “diabetes mellitus”) AND Language = English.” In this study, the publication types were restricted to “article” or “review,” time span = 2000–2020.
Analysis Tools
The CiteSpace 5.8.R 2 Version (Drexel University, Philadelphia, USA), a Java-based application, was utilized to perform the bibliometric analysis on the papers, involving the analysis of publications, journals, authors, references, countries, institutions, and keywords. The CiteSpace V software, an exemplary scientometric analysis method, was utilized to conduct literature analysis (14). The arguments of CiteSpace software were set as follows: time span = 2000–2020, years per slice = 1, term source = all selection, node type = select the corresponding analysis target at a time, selection criteria = top 50, and pruning = none.
In the network map, the different nodes represent a journal, institution, or country, while the magnitude of the node circle represents productivity (15). The links between different nodes reflected the network of collaboration, co-citation, or co-occurrence relationships, and a wider line represents a stronger association (12). The CiteSpace 5.8.R 2 version could identify the citation bursts of references and keywords. A citation burst shows growing attention to the potential research over a specific duration, which is a pivotal indicator for exploring emerging tendencies (16). Furthermore, the Microsoft Excel 2019 software was used to describe the global output and development trend of related papers, and IBM SPSS Statistical 26.0 (SPSS, Inc., Chicago, IL, USA) was applied to execute linear regression analysis to assess the changes in the recent two decades. The p < 0.05 was regarded as statistical significance. Finally, according to the Journal Citation Reports (2020), the impact factor (IF) indicates the impact of journals.
Results
General Information of Exercise and Diabetes Research
Analysis of Publications Outputs
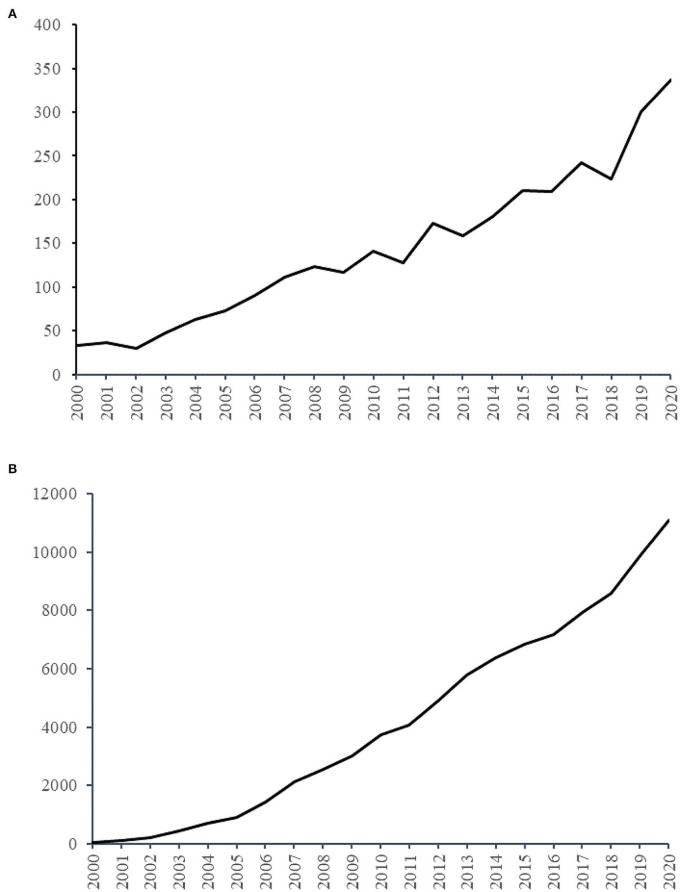
A total of 3,029 publications from 2000 to 2020 related to exercise and diabetes research, including 2,673 articles and 356 reviews, with an average annual output of 144. As presented in Figure 1A, the annual number of publications rised from 33 in 2000 to 337 in 2020. Although the number of published papers fluctuated in certain periods, the total annual output showed an upward tendency. In addition, the outcomes of linear regression analysis revealed a significant papers growth in the past two decades (t = 17. 848, p < 0. 001). The 3,029 publications have been cited 96,317 times from 2000 to 2020. As presented in Figure 1B, the amount of citations increased from 26 in 2000 to 11,105 in 2020, and the growth was statistically significant (t = 23.958, p < 0.001).
Figure 1.
The number of publications and citations. (A) The number of annual publications on exercise and diabetes mellitus research from 2000 to 2020. (B) The number of annual citations on exercise and diabetes mellitus research from 2000 to 2020.
Analysis of Countries and Institutions
Eighty-one countries and 3,783 institutions published 3,029 publications on exercise and diabetes research. The list of the top 10 countries and institutions is presented in Table 1.
Table 1.
Top 10 countries and institutions on exercise and diabetes mellitus research from 2000 to 2020.
| Rank | Country | Publications | Centrality | Institution | Publications | Centrality |
|---|---|---|---|---|---|---|
| 1 | USA | 965 | 0.57 | Univ Alberta (Canada) | 76 | 0.05 |
| 2 | Canada | 347 | 0.07 | Univ Copenhagen (Denmark) | 67 | 0.10 |
| 3 | England | 305 | 0.33 | York Univ (Canada) | 60 | 0.09 |
| 4 | Australia | 287 | 0.15 | Univ Calgary (Canada) | 52 | 0.04 |
| 5 | Peoples R China | 148 | 0.01 | Univ Queensland (Australia) | 51 | 0.07 |
| 6 | Brazil | 146 | 0.07 | Univ Colorado (USA) | 48 | 0.08 |
| 7 | Italy | 128 | 0.07 | Harvard Univ (USA) | 42 | 0.10 |
| 8 | Japan | 107 | 0.04 | Univ Sydney (Australia) | 42 | 0.06 |
| 9 | Germany | 105 | 0.04 | Maastricht Univ (Netherlands) | 39 | 0.05 |
| 10 | Denmark | 104 | 0.04 | Univ Pittsburgh (USA) | 37 | 0.04 |
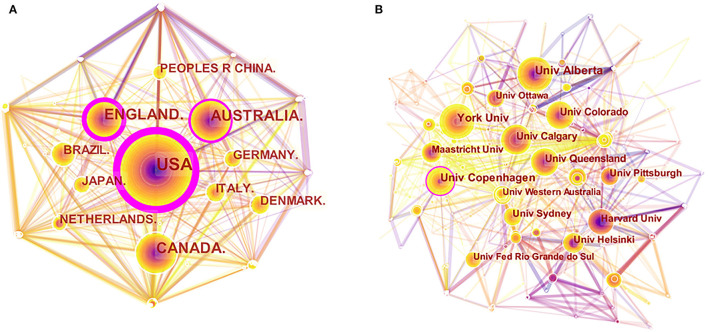
As presented in Figure 2A, the cooperation network map of countries was produced by the CiteSpace software. The purple ring reflects centrality, and the country with high centrality was known as a vital point in the publications. The USA had the most publications (965 publications), followed by Canada (347 publications), England (305 publications), Australia (287 publications), and China (148 publications). The USA also had the highest centrality (0.57), followed by England (0.33), Australia (0.15), Canada (0.07), and Brazil (0.07).
Figure 2.
The cooperation of countries and institutions. (A) Map of countries with publications in exercise and diabetes mellitus research from 2000 to 2020. (B) Map of institutions with publications in exercise and diabetes mellitus research from 2000 to 2020.
The collaboration network map of institutions is shown in Figure 2B. Alberta University had the most studies (76 publications), followed by the University of Copenhagen (67 publications), York University (60 publications), University of Calgary (52 publications), and University of Queensland (51 publications). Copenhagen and Harvard University showed the highest centrality (0.10).
Analysis of Journals and Co-Cited Journals
In all, 688 journals published papers on exercise and diabetes research. The top 10 journals generated 775 documents, making up 25.34% of the 3,029 publications. In terms of the number of published papers on exercise and diabetes research, as presented in Table 2, Diabetes Care (IF 2020 = 19.112) was the most productive journal (178 publications, 5.88%), followed by the Diabetologia (96 publications), Diabetes Research and Clinical Practice (87 publications), and Diabetic Medicine (81 publications). Among the top 10 journals, the IF was ranked between 2.140 and 19.112, the average IF was 6.516.
Table 2.
Top 10 journals related to exercise and diabetes mellitus research from 2000 to 2020.
| Rank | Journal | Publications | Percentage (%) | IF*(2020) |
|---|---|---|---|---|
| 1 | Diabetes Care | 178 | 5.88% | 19.112 |
| 2 | Diabetologia | 96 | 3.17% | 10.122 |
| 3 | Diabetes Research and Clinical Practice | 87 | 2.87% | 5.602 |
| 4 | Diabetic Medicine | 81 | 2.67% | 4.359 |
| 5 | Plos One | 76 | 2.51% | 3.240 |
| 6 | Medicine and Science in Sports and Exercise | 62 | 2.05% | 5.411 |
| 7 | Canadian Journal of Diabetes | 56 | 1.85% | 4.190 |
| 8 | Diabetes Educator | 49 | 1.62% | 2.140 |
| 9 | Pediatric Diabetes | 47 | 1.55% | 4.866 |
| 10 | Diabetes Technology & Therapeutics | 43 | 1.42% | 6.118 |
IF according to Journal Citation Reports (2020). IF, impact factor.
In addition, Figure 3 presented the scholarly journals co-cited map associated with publications on exercise and diabetes research. Figure 3 and Table 3 showed co-citation combined with centrality. The top 5 co-cited journals were Diabetes Care, Diabetologia, Medicine and Science in Sports and Exercise, Diabetes, and JAMA-Journal of the American Medical Association.
Figure 3.
Journal co-citation map associated with publications on exercise and diabetes mellitus research from 2000 to 2020.
Table 3.
Top 10 co-cited journals on exercise and diabetes mellitus research from 2000 to 2020.
| Rank | Co-citation counts | Cited journal | Centrality | Cited journal |
|---|---|---|---|---|
| 1 | 2,630 | Diabetes Care | 0.04 | British Journal of Nutrition |
| 2 | 1,599 | Diabetologia | 0.04 | Journal of the American Dietetic Association |
| 3 | 1,576 | Medicine and Science in Sports and Exercise | 0.04 | Journal of Hypertension |
| 4 | 1,369 | Diabetes | 0.03 | Annals of Medicine |
| 5 | 1,294 | JAMA-Journal of the American Medical Association | 0.03 | Biochemical and Biophysical Research Communications |
| 6 | 1,155 | New England Journal of Medicine | 0.03 | Endocrinology |
| 7 | 1,081 | Journal of Applied Physiology | 0.03 | Patient Education and Counseling |
| 8 | 983 | Diabetes Research and Clinical Practice | 0.03 | Journals of Gerontology Series A- Biological Sciences and Medical Sciences |
| 9 | 975 | Diabetic Medicine | 0.03 | American Journal of Public Health |
| 10 | 901 | Circulation | 0.03 | American Journal of Physiology-Heart and Circulatory Physiology |
Analysis of Authors
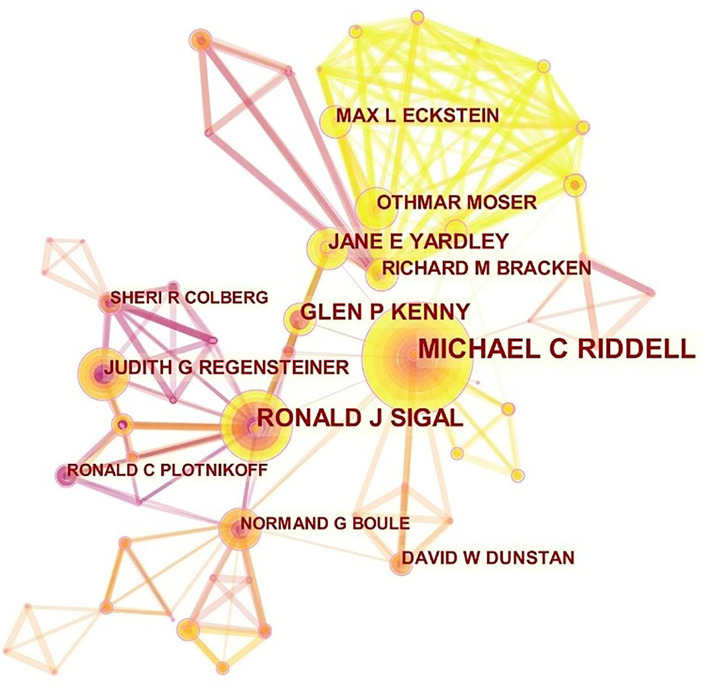
As many as 13,000 authors published 3,029 papers contributing to research on exercise and diabetes. To summarize the cooperation among authors, a network map was generated using CiteSpace (Figure 4). Judging from the situations of cooperation map, the scale of collaboration among authors was relatively light and needed to strengthen the overall connection. The top 10 authors, co-cited authors of exercise and diabetes research, are presented in Table 4. Among the top 10 authors, Riddell MC ranked first with 53 articles, followed by Sigal RJ with 39 articles, Kenny GP with 24 articles, and Yardley JE with 22 articles. Riddell MC came from York University, Canada, Sigal RJ, Kenny GP, and Yardley JE were from the University of Ottawa, Canada, Bracken RM, and Moser O came from Swansea University, United Kingdom, Regensteiner JG came from University of Colorado, USA, Eckstein ML came from the Division of Endocrinology and Diabetology, Medical Austria, Blair SN came from the University of South Carolina, USA, and Plotnikoff RC came from the University of Alberta, Canada.
Figure 4.
Network map of authors who contributed to exercise and diabetes mellitus research from 2000 to 2020.
Table 4.
Top 10 authors and co-cited authors on exercise and diabetes mellitus research from 2000 to 2020.
| Rank | Author | Published articles | Co-cited author | Cited times | Centrality |
|---|---|---|---|---|---|
| 1 | Riddell MC | 53 | Sigal RJ | 503 | 0.02 |
| 2 | Sigal RJ | 39 | Colberg SR | 464 | 0.03 |
| 3 | Kenny GP | 24 | Boule NG | 405 | 0.08 |
| 4 | Yardley JE | 22 | Amer Diabet Assoc | 332 | 0.02 |
| 5 | Bracken RM | 18 | Knowler WC | 304 | 0.01 |
| 6 | Regensteiner JG | 17 | Church TS | 253 | 0.04 |
| 7 | Moser O | 16 | Balducci S | 226 | 0.03 |
| 8 | Eckstein ML | 15 | Dunstan DW | 224 | 0.04 |
| 9 | Blair SN | 14 | Hu FB | 217 | 0.03 |
| 10 | Plotnikoff RC | 14 | Umpierre D | 204 | 0.01 |
Research Hotspots
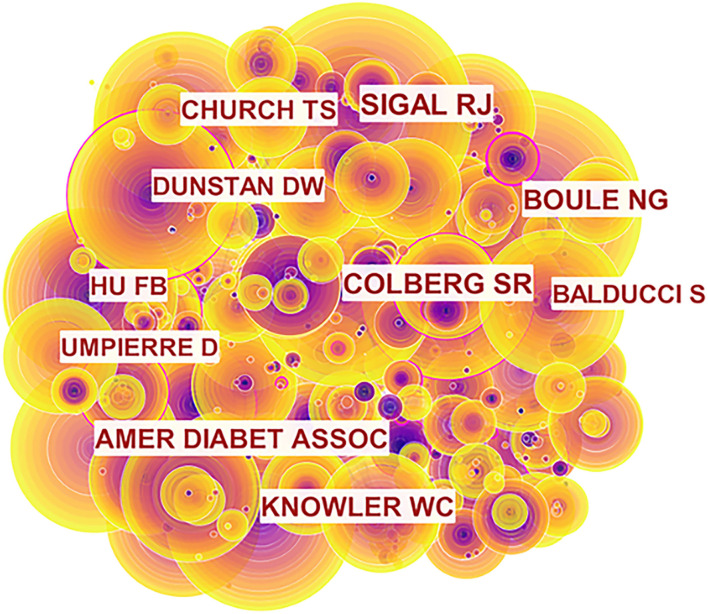
Analysis of Co-Cited Authors
The network map of co-cited authors is shown in Figure 5. Sigal RJ ranked first with 503 cited times, followed by Colberg SR, Boule NG, and Amer Diabet Assoc with 464, 405, and 332 cited times, respectively (Table 4). Among them, Boule NG had the highest centrality (0.08). The top 10 co-cited authors' citation amounts exceeded 200, which indicated that they were yauld and influential researchers in the domain of exercise and diabetes research. Sigal RJ came from the muscle health research center at York University, Canada. Colberg SR came from the department of human movement sciences at Old Dominion University, USA. Boule NG was from the institute of human kinetics at the University of Ottawa, Canada. Knowler WC was from the diabetes prevention program coordinating center at George Washington University, USA.
Figure 5.
Map of co-cited authors related to exercise and diabetes mellitus research from 2000 to 2020.
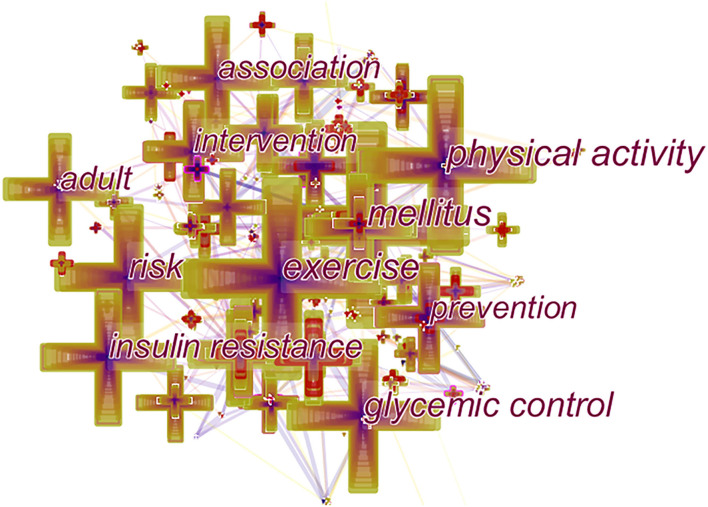
Analysis of Co-Occurrence Keywords
Figure 6 shows the co-occurrence network of keywords from 2000 to 2020, indicating the scope of research topics on exercise and diabetes. As shown in Table 5, The most common keyword was “mellitus,” with 637 co-occurrences, followed by “exercise” (591 times), “physical activity” (556 times), “glycemic control” (406 times), “risk” (382 times), “insulin resistance,” “association,” “adult,” “prevention,” and “intervention.” Among them, “intervention” had the highest centrality (0.28).”
Figure 6.
Map of the co-occurrence keywords in publications on exercise and diabetes mellitus research from 2000 to 2020.
Table 5.
Top 10 keywords related to exercise and diabetes mellitus research from 2000 to 2020.
| Rank | Frequency | Keyword | Centrality | Rank | Frequency | Keyword | Centrality |
|---|---|---|---|---|---|---|---|
| 1 | 637 | Mellitus | 0.08 | 6 | 302 | Insulin resistance | 0.15 |
| 2 | 591 | Exercise | 0.02 | 7 | 272 | Association | 0.02 |
| 3 | 556 | Physical activity | 0.14 | 8 | 262 | Adult | 0.08 |
| 4 | 406 | Glycemic control | 0.00 | 9 | 218 | Prevention | 0.23 |
| 5 | 382 | Risk | 0.02 | 10 | 216 | Intervention | 0.28 |
Analysis of Co-Cited References
In all, 67,063 references were performed from 3,029 papers to analyze co-cited references. Table 6 lists the top 5 co-cited references related to exercise and diabetes research between 2000 and 2020. The first article was the study of Colberg et al. (5) had the maximum co-citation counts (183), which proposed that physical activity/exercise should be a part of glycemic control and overall health management for all patients with diabetes. And the specific type and intensity of exercise will vary depending on the type of diabetic patient, age, and presence of diabetes-related health complications.
Table 6.
Top 5 co-cited references related to exercise and diabetes mellitus research from 2000 to 2020.
| Rank | Co-citation counts | Co-cited reference | References |
|---|---|---|---|
| 1 | 183 | Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association | (5) |
| 2 | 158 | Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis | (17) |
| 3 | 150 | Physical Activity/Exercise and Type 2 Diabetes A consensus statement from the American Diabetes Association | (18) |
| 4 | 125 | Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin | (19) |
| 5 | 124 | Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial | (20) |
The second article was the study of Umpierre et al. (17) with the co-citation counts of 158, which reviewed that structured exercise training was related to improved glycemic control in persons with type 2 diabetes. Still, physical activity was only related to improved glycemic control when combined with dietary recommendations.
The third article was the study of Sigal et al. (18) with the co-citation counts of 150, a consensus statement from the American Diabetes Association. They summarized the exercise/physical activity associated with diabetes and made the different levels of the recommendations based on the levels of evidence.
The fourth and fifth articles were published in 2002 and 2007 by Knowler et al. (19) and Sigal et al. (20), respectively. Knowler et al. (19) found that lifestyle intervention and metformin treatment delayed and prevented type 2 diabetes, particularly in the former. Sigal et al. (20) discovered that aerobic and resistance training improved glycemic control and combining the two methods was more effective than either one alone.
Global Trends of Exercise and Diabetes Research
Analysis of Keywords with the Strongest Citation Bursts
The top 45 keywords with the strongest citation bursts on exercise and diabetes study between 2000 and 2020 are presented in Table 7. The latest burst keywords were “system,” “type 1,” “sedentary behavior,” “stress”.
Table 7.
Top 45 keywords with the strongest citation bursts.
| Keywords | Year | Strength | Begin | End | 2000–2020 |
|---|---|---|---|---|---|
| NIDDM | 2000 | 17.35 | 2000 | 2007 |

|
| Impaired glucose tolerance | 2000 | 13.57 | 2000 | 2010 |

|
| Insulin | 2000 | 13.32 | 2000 | 2007 |

|
| Women | 2000 | 6.96 | 2000 | 2007 |

|
| Human | 2000 | 3.9 | 2000 | 2008 |

|
| IDDM | 2000 | 3.6 | 2000 | 2007 |

|
| Metabolism | 2000 | 3.4 | 2000 | 2003 |

|
| Men | 2000 | 10.54 | 2001 | 2007 |

|
| Glucose tolerance | 2000 | 8.18 | 2001 | 2006 |

|
| Glucose transport | 2000 | 5.39 | 2001 | 2009 |

|
| Blood pressure | 2000 | 4.53 | 2001 | 2005 |

|
| Life style | 2000 | 13.49 | 2002 | 2007 |

|
| Coronary heart disease | 2000 | 6.65 | 2002 | 2007 |

|
| Prevention | 2000 | 6.11 | 2002 | 2007 |

|
| 3rd national health | 2000 | 3.66 | 2002 | 2005 |

|
| Rat | 2000 | 3.58 | 2002 | 2008 |

|
| Gene expression | 2000 | 5.26 | 2003 | 2011 |

|
| Response | 2000 | 3.63 | 2003 | 2008 |

|
| Tolerance | 2000 | 5.96 | 2004 | 2013 |

|
| Homeostasis model assessment | 2000 | 5.47 | 2004 | 2008 |

|
| Coronary artery disease | 2000 | 4.19 | 2004 | 2013 |

|
| Determinant | 2000 | 6.82 | 2005 | 2010 |

|
| Necrosis factor alpha | 2000 | 5.09 | 2005 | 2008 |

|
| Cardiomyopathy | 2000 | 3.46 | 2005 | 2009 |

|
| Counterregulatory response | 2000 | 5.09 | 2006 | 2010 |

|
| Improves glycemic control | 2000 | 6.9 | 2007 | 2010 |

|
| Plasma glucose | 2000 | 3.82 | 2007 | 2010 |

|
| Predictor | 2000 | 3.65 | 2007 | 2010 |

|
| Self management | 2000 | 4.8 | 2008 | 2012 |

|
| Atherosclerosis | 2000 | 3.3 | 2008 | 2013 |

|
| Reduction | 2000 | 6.08 | 2009 | 2016 |

|
| Energy expenditure | 2000 | 3.19 | 2009 | 2013 |

|
| Hypertension | 2000 | 3.6 | 2010 | 2013 |

|
| Randomized controlled trial | 2000 | 7.95 | 2011 | 2018 |

|
| US adult | 2000 | 4.47 | 2011 | 2017 |

|
| Validity | 2000 | 3.9 | 2011 | 2016 |

|
| American college | 2000 | 3.32 | 2011 | 2016 |

|
| Cardiovascular risk factor | 2000 | 7.23 | 2012 | 2015 |

|
| Endothelial function | 2000 | 4.72 | 2012 | 2015 |

|
| MA | 2000 | 3.14 | 2014 | 2017 |

|
| Gait | 2000 | 3.77 | 2015 | 2018 |

|
| System | 2000 | 4.41 | 2016 | 2020 |

|
| Type 1 | 2000 | 3.99 | 2016 | 2020 |

|
| Sedentary behavior | 2000 | 3.63 | 2016 | 2020 |

|
| Stress | 2000 | 3.54 | 2016 | 2020 |

|
Analysis of References with the Strongest Citation Bursts
The top 20 references from 2000 to 2020 are presented in Table 8. The red rectangles indicate references cited continually, and the other color rectangles were cited infrequently. Analysis of the citation bursts of references, the papers between 2014 and 2017 initiated the research upsurge of exercise therapy for diabetes. The authors of the top five strongest citation bursts references were Colberg SR, Riddell MC, Mitranun W, Bohn B, and Jelleyman C. The highest strength burst reference started in 2016 from Colberg et al. (5).
Table 8.
Top 20 references co-citation with the strongest citation bursts.
| References | Year | Strength | Begin | End | 2000–2020 |
|---|---|---|---|---|---|
| Colberg SR, 2016, DIABETES CARE, V39, P2065, DOI 10.2337/dc16-1728 | 2016 | 66.65 | 2018 | 2020 |

|
| Riddell MC, 2017, LANCET DIABETES ENDO, V5, P377, DOI 10.1016/S2213-8587(17)30014-1 | 2017 | 39 | 2018 | 2020 |

|
| Mitranun W, 2014, SCAND J MED SCI SPOR, V24, P0, DOI 10.1111/sms.12112 | 2014 | 18.91 | 2016 | 2020 |

|
| Bohn B, 2015, DIABETES CARE, V38, P1536, DOI 10.2337/dc15-0030 | 2015 | 17.09 | 2017 | 2020 |

|
| Jelleyman C, 2015, OBES REV, V16, P942, DOI 10.1111/obr.12317 | 2015 | 12.8 | 2017 | 2020 |

|
| Moser O, 2015, PLOS ONE, V10, P0, DOI 10.1371/journal.pone.0136489 | 2015 | 11.37 | 2017 | 2020 |

|
| WHO, 2016, GLOBAL REPORT DIABET, V0, P0 | 2016 | 11.01 | 2017 | 2020 |

|
| Hollekim-Strand SM, 2014, J AM COLL CARDIOL, V64, P1758, DOI 10.1016/j.jacc.2014.07.971 | 2014 | 10.61 | 2016 | 2020 |

|
| Aune D, 2015, EUR J EPIDEMIOL, V30, P529, DOI 10.1007/s10654-015-0056-z | 2015 | 10.56 | 2016 | 2020 |

|
| Weston KS, 2014, BRIT J SPORT MED, V48, P1227, DOI 10.1136/bjsports-2013-092576 | 2014 | 10.22 | 2016 | 2020 |

|
| Quirk H, 2014, DIABETIC MED, V31, P1163, DOI 10.1111/dme.12531 | 2014 | 10.1 | 2015 | 2020 |

|
| McAuley SA, 2016, DIABETOLOGIA, V59, P1636, DOI 10.1007/s00125-016-3981-9 | 2016 | 9.94 | 2017 | 2020 |

|
| Schwingshackl L, 2014, DIABETOLOGIA, V57, P1789, DOI 10.1007/s00125-014-3303-z | 2014 | 9.82 | 2016 | 2020 |

|
| Grace A, 2017, CARDIOVASC DIABETOL, V16, P0, DOI 10.1186/s12933-017-0518-6 | 2017 | 9.12 | 2018 | 2020 |

|
| Robertson K, 2014, PEDIATR DIABETES, V15, P203, DOI 10.1111/pedi.12176 | 2014 | 8.64 | 2016 | 2020 |

|
| Lascar N, 2014, PLOS ONE, V9, P0, DOI 10.1371/journal.pone.0108019 | 2014 | 8.53 | 2018 | 2020 |

|
| AmericanDiabetesAssociation, 2015, Diabetes Care, V38 Suppl, P0, DOI 10.2337/dc15-S005 | 2015 | 8.35 | 2017 | 2020 |

|
| Franc S, 2015, DIABETES OBES METAB, V17, P1150, DOI 10.1111/dom.12552 | 2015 | 8.16 | 2017 | 2020 |

|
| Campbell MD, 2015, BMJ OPEN DIAB RES CA, V3, P0 | 2015 | 7.93 | 2016 | 2020 |

|
| Moser O, 2016, NUTRIENTS, V8, P0, DOI 10.3390/nu8080489 | 2016 | 7.81 | 2018 | 2020 |

|
Discussion
General Information for Exercise and Diabetes Research
The research on exercise and diabetes has received tremendous attention in the past two decades. This phenomenon may be related to the increase in the morbidity of diabetes and the increased economic burden it brings, and the popularization of the concept of “exercise is medicine.” Moreover, eight are developed countries among the top 10 countries, and only two are developing countries. There was still a considerable gap between developing and developed countries in this research domain. Moreover, the USA has the most published papers (965) and the highest centrality (0.57), which shows that the USA is the leading in this research area. The output institutions are mainly from Univ Alberta and Univ Calgary of Canada, Univ Copenhagen of Denmark, York Univ of USA, and Univ Queensland of Australia. The top 10 institutions make up 16.969% of total publication yields, which implied that they had obtained considerable academic achievements. Nevertheless, compared with the collaboration between countries, the collaboration between those institutions was not apparent. Cooperation helps researchers who investigate exercise and diabetes research exchange thoughts and resources, critical for further research development. Thus, stronger cooperation relationships should be built among researchers, countries, and institutions.
The articles about exercise and diabetes research were published in 688 diverse academic periodicals, and the top 10 journals came out 25.34% of publications. Among the top 10 journals with IF > 10 (Diabetes Care, IF, 2020 = 19.112 and Diabetologia IF, 2020 = 10.122), and three had 5 < IF < 10. About 23.969% (IF, 2020 > 5.000, 15.385%; 3.000 ≤ IF, 2020 ≤ 5.000, 8.584%) of the 3,029 publications were came out in the top 10 periodicals with high IF (>3.000). Thus, it was challenging to publish relevant publications in high impact factor journals.
The data on crucial authors can help investigators to find the underlying cooperators. Authors Riddell MC, Sigal RJ, Colberg SR, and Boule NG were the most productive and influential authors in the exercise and diabetes area, as identified by an omnibus analysis of amounts of published papers and co-citations. Riddell MC offered the latest consensus on exercise management for type 1 diabetic patients who exercise regularly, including blood glucose goals when performing different exercise programs (21). Sigal et al. summarized the up-to-date clinical research progress related to exercise and type 2 diabetes and recommendations (18). Colberg et al. provided a review and evidence-based recommendations concerning exercise in individuals with diabetes and prediabetes (5). Boule et al. showed that regular exercise has a significant clinical effect on maximal oxygen uptake in individuals with type 2 diabetes and higher intensity exercise has additional benefits on cardiorespiratory fitness (22).
Research Hotspots for Exercise and Diabetes Research
The research focuses of the current study were explored from the three sides of co-occurrence keywords, co-cited authors, and co-cited references, which refer to numerous interrelated topics discussed within a particular scholastic discipline (10).
According to the co-cited authors, Sigal et al., Colberg et al., and Boule et al. had a long-term collaboration (5, 20, 22, 23). Sigal RJ and Colberg SR often cooperated to give recommendations and precautions for different types of exercises to persons with type 2 diabetes, such as the types and quantities of exercise that can be performed by individuals with type 2 diabetes, along with the announcements required to maximize the safety of physical activities in those using multifarious medications and accompany with diabetes-related complications. Boule NG mainly focused on applying aerobic exercise, resistance exercise, and mixed exercise mode in patients with type 2 diabetes, which can effectively improve glycemic control, enhance cardiorespiratory fitness, and decrease the demand for non-insulin antihyperglycemic agents.
Our analysis of co-occurrence keywords indicated that the four most commonly used keywords are mellitus, exercise, physical activity, and glycemic control. Exercise is a crucial component of diabetes management because it can decrease blood glucose levels, lose weight, and improve lipid levels (23). However, a systematic review and meta-analysis about the influences of structured exercise programs (aerobic, resistance, or both) on HbA1c (A1C) and body weight in individuals with type 2 diabetes revealed that A1C decreased remarkably after exercise intervention. On the contrary, there was no significant change in body mass after intervention (24). Hence, structured exercise regimens had a significant beneficial impact on A1C and glycemic control, and this influence was not primarily regulated by bodyweight reduction. Exercise more than 2.5 h per week is related to greater A1C decline than those who do not have enough structured exercise time (17). Moreover, the combination of aerobic and resistance training can improve the level of A1C in patients with type 2 diabetes, but this beneficial effect cannot be achieved by aerobic or resistance training alone (20). Although exercise has long been considered the sustentaculum of diabetes management, many physicians have not prescribed it. According to the five references cited most, physicians should be reminded that managements used to intervene in type 2 diabetes should aggrandize lifestyle improvements, such as increased physical activity level in daily life, rather than replace them (23).
Global Trends of Exercise and Diabetes Research
Keywords with citation bursts are known as indicators of frontier topics. Two emerging trends in exercise and diabetes research were identified in line with the comprehensive analysis of the latest keyword bursts; details are listed as follows:
Sedentary behavior: Sedentary behaviors refer to activities that have a low energy expenditure (≤1.5 metabolic equivalents) while in a sitting or lying down position (25). Greater sedentary behavior time was positively related to an increased risk for premature mortality and type 2 diabetes incidence (26). Conducted a cohort study among adults over 45 years old in Australia, the results showed that subjects who reported <8 h of sedentary time per day could decrease 14% the risk of latently preventable hospitalization. Moreover, the deleterious effects of sedentary behavior time usually decreased in magnitude among persons who performed higher physical activity/exercise levels than lower levels (27). Recent studies found that breaking up the sedentary behavior may be related to beneficial changes in the cardiometabolic and inflammatory risk in the type 2 diabetes population, interrupting sedentary behavior time by adding low-intensity physical activity breaks (28, 29). Greater evidence indicated that interrupting prolonged sedentary status by light-intensity walking is an effective method for improving postprandial glucose level (30), and performing light ambulation breaks reduced the 7 h glucose of type 2 diabetes patients compared with the prolonged sitting position (31). However, physical activity/exercise strategies to reduce the adverse effects of sedentary behavior on healthy populations and diabetic patients should be further investigated.
Stress: The COVID-19 pandemic is a severe medical crisis that has had a powerful negative impact on daily life worldwide. In order to control the epidemic, many countries implemented lockdown strategies that led to considerable changes in social behavior (32). A previous study revealed a lockdown related to increased levels of emotional distress (33). These alterations in daily life, behavior patterns, physical activities, and increased emotion of stress and anxiety are all known to affect the healthcare and glycemic control of diabetes patients (34, 35). Moreover, chronic psychological stress has been associated with high level of A1C (36). The previous studies of diabetes found that acute psychological stress caused a delayed reduction in the postprandial glucose concentrations (35, 37). However, the potential pathomechanism for the different glucose concentrations in response to psychological stress remains unclear. Thus, diabetes healthcare professionals should consider the aspects of psychological stress alteration when discussing diabetes management and exercise promotes health.
Instead of exploring all the burst references, the subsequent discussions will concern the top 5 references by the end of 2020.
As presented in Table 8, a study by Colberg et al. (5) represented the strongest burst by the end of 2020. This research offered a review and evidence-based recommendations about exercise/physical activity in individuals with prediabetes, type 1, type 2, and gestational diabetes. Exercise should be prescribed to all persons with diabetes to manage glycemic control and healthcare. Adults should be encouraged to reduce the sedentary time and interrupt the sedentary behavior with frequent activity.
The study by Riddell et al. (21) represented the second strongest burst by the end of 2020. This review offered the latest consensus on exercise management for persons with type 1 diabetes mellitus who exercise regularly, involving glucose goals for safe and effective physical activities and nutritional and insulin dose regulations to defend against exercise-related glucose fluctuations.
The following paper investigated the effects of continuous and interval aerobic exercise training on macro- and microvascular reactivity and glycemic control in individuals with type 2 diabetes (38). This study indicated that continuous and interval exercise training effectively improved glycemic control and maximal aerobic fitness. The high-intensity interval exercise training could produce greater improvements in vascular complications that individuals with type 2 diabetes often suffer.
The fourth paper investigated the effects of exercise on glycemic control and cardiovascular risk factors in subjects with type 1 diabetes (39). This research found a negative correlation between physical activity and A1C, dyslipidemia, diabetic ketoacidosis, body mass index, hypertension, retinopathy, and microalbuminuria. Therefore, the authors recommended regular physical activity for patients with type 1 diabetes.
The fifth research explored the impact of high-intensity interval training (HIIT) on insulin resistance and glucose regulation compared to continuous training and control conditions (40). The results showed a significant reduction in insulin resistance after HIIT in comparison to other groups. Compared with control conditions, A1C and body weight decreased significantly following HIIT. HIIT appears to improve metabolic health in those at risk of or with type 2 diabetes.
This study is the first to investigate the global trends and research hotspots of exercise and diabetes research based on papers published between 2000 and 2020 by a bibliometrics method. Our study offers new historical perspectives for scientific growth and analyzes different sides of academic literature. However, this study still has several limitations. First, the relevant papers retrieved were only performed in SCIE of WoS and lacked other databases, such as Scopus. Second, we excluded the non-English publications, and this limitation may cause publication bias.
Conclusion
This bibliometric study could help researchers to find the publication patterns, research hotspots, and emerging exercise, and diabetes research trends from 2000 to 2020. The current research status indicated that exercise and diabetes research still has promising development potential. The most influential country, institution, journal, and author were the USA, Univ Alberta, Diabetes Care, and Sigal RJ. “Sedentary behavior” and “stress” may be the up-to-date research frontiers. In general, this study offers a scientific perspective on exercise and diabetes study, providing helpful information for relevant investigators, funding agencies, and policymakers.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author Contributions
YuZ, ZZ, and XC conceptualized, designed, and performed the study. YuZ, QW, and TC contributed to collecting data. YuZ, ZZ, TC, and CL interpreted data and wrote the manuscript. YuZ, CL, YiZ, XW, XC, and ZZ revised the manuscript. All authors approved the final version of the manuscript.
Funding
This research was supported by the Construction Project of Administration of Traditional Chinese Medicine of Henan Province (2021-30) and the Project of Science Research of Traditional Chinese Medicine of Henan Province of China (2019ZY1028).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank Professor C. M. Chen for developing the free-to-use CiteSpace software.
References
- 1.Shi Y, Hu FB. The global implications of diabetes and cancer. Lancet. (2014) 383:1947–8. 10.1016/S0140-6736(14)60886-2 [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association . Diagnosis and classification of diabetes mellitus. Diabetes Care. (2013) 36:S67–74. 10.2337/dc13-S067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Diabetes Federation (2021). Available online at: https://diabetesatlas.org/data/en/world/ (accessed January 15, 2022).
- 4.Vijan S, Stevens DL, Herman WH, Funnell MM, Standiford CJ. Screening, prevention, counseling, and treatment for the complications of type ii diabetes mellitus. Putting evidence into practice. J Gen Intern Med. (1997) 12:567–80. 10.1046/j.1525-1497.1997.07111.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, et al. Physical activity/exercise and diabetes: a position statement of the American diabetes association. Diabetes Care. (2016) 39:2065–79. 10.2337/dc16-1728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sallis RE. Exercise is medicine and physicians need to prescribe it! Br J Sports Med. (2009) 43:3–4. 10.1136/bjsm.2008.054825 [DOI] [PubMed] [Google Scholar]
- 7.Tonoli C, Heyman E, Roelands B, Buyse L, Cheung SS, Berthoin S, et al. Effects of different types of acute and chronic (training) exercise on glycaemic control in type 1 diabetes mellitus: a meta-analysis. Sports Med. (2012) 42:1059–80. 10.1007/BF03262312 [DOI] [PubMed] [Google Scholar]
- 8.Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. (2012) 2012:CD007146. 10.1002/14651858.CD007146.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Snowling NJ, Hopkins WG. Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis. Diabetes Care. (2006) 29:2518–27. 10.2337/dc06-1317 [DOI] [PubMed] [Google Scholar]
- 10.Zhang J, Zhang Y, Hu L, Huang X, Liu Y, Li J, et al. Global trends and performances of magnetic resonance imaging studies on acupuncture: a bibliometric analysis. Front Neurosci. (2020) 14:620555. 10.3389/fnins.2020.620555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang S, Fan H, Zhang Y. The 100 top-cited studies on dyslexia research: a bibliometric analysis. Front Psychiatry. (2021) 12:714627. 10.3389/fpsyt.2021.714627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang XQ, Peng MS, Weng LM, Zheng YL, Zhang ZJ, Chen PJ. Bibliometric study of the comorbidity of pain and depression research. Neural Plast. (2019) 2019:1657498. 10.1155/2019/1657498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stout NL, Alfano CM, Belter CW, Nitkin R, Cernich A, Lohmann Siegel K, et al. A bibliometric analysis of the landscape of cancer rehabilitation research (1992–2016). J Natl Cancer Inst. (2018) 110:815–24. 10.1093/jnci/djy108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.You Y, Wang D, Wang Y, Li Z, Ma X. A bird's-eye view of exercise intervention in treating depression among teenagers in the last 20 years: a bibliometric study and visualization analysis. Front Psychiatry. (2021) 12:661108. 10.3389/fpsyt.2021.661108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng KY, Dai GY, Lan Y, Wang XQ. Trends of repetitive transcranial magnetic stimulation from 2009 to 2018: a bibliometric analysis. Front Neurosci. (2020) 14:106. 10.3389/fnins.2020.00106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miao Y, Xu SY, Chen LS, Liang GY, Pu YP, Yin LH. Trends of long non-coding rna research from 2007 to 2016: a bibliometric analysis. Oncotarget. (2017) 8:83114–27. 10.18632/oncotarget.20851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Umpierre D, Ribeiro PA, Kramer CK, Leitão CB, Zucatti AT, Azevedo MJ, et al. Physical activity advice only or structured exercise training and association with hba1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA. (2011) 305:1790–9. 10.1001/jama.2011.576 [DOI] [PubMed] [Google Scholar]
- 18.Sigal RJ, Kenny GP, Wasserman DH, Castaneda-Sceppa C, White RD. Physical activity/exercise and type 2 diabetes: a consensus statement from the American diabetes association. Diabetes Care. (2006) 29:1433–8. 10.2337/dc06-9910 [DOI] [PubMed] [Google Scholar]
- 19.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New Engl J Med. (2002) 346:393–403. 10.1056/NEJMoa012512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sigal RJ, Kenny GP, Boulé NG, Wells GA, Prud'homme D, Fortier M, et al. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Ann Intern Med. (2007) 147:357–69. 10.7326/0003-4819-147-6-200709180-00005 [DOI] [PubMed] [Google Scholar]
- 21.Riddell MC, Gallen IW, Smart CE, Taplin CE, Adolfsson P, Lumb AN, et al. Exercise management in type 1 diabetes: a consensus statement. Lancet Diabetes Endocrinol. (2017) 5:377–90. 10.1016/S2213-8587(17)30014-1 [DOI] [PubMed] [Google Scholar]
- 22.Boulé NG, Kenny GP, Haddad E, Wells GA, Sigal RJ. Meta-analysis of the effect of structured exercise training on cardiorespiratory fitness in type 2 diabetes mellitus. Diabetologia. (2003) 46:1071–81. 10.1007/s00125-003-1160-2 [DOI] [PubMed] [Google Scholar]
- 23.Colberg SR, Sigal RJ. Prescribing exercise for individuals with type 2 diabetes: recommendations and precautions. Physician Sportsmed. (2011) 39:13–26. 10.3810/psm.2011.05.1909 [DOI] [PubMed] [Google Scholar]
- 24.Boulé NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA. (2001) 286:1218–27. 10.1001/jama.286.10.1218 [DOI] [PubMed] [Google Scholar]
- 25.Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary Behavior Research Network (Sbrn)—terminology consensus project process and outcome. Int J Behav Nutr Phys Act. (2017) 14:75. 10.1186/s12966-017-0525-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA. (2011) 305:2448–55. 10.1001/jama.2011.812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. (2015) 162:123–32. 10.7326/M14-1651 [DOI] [PubMed] [Google Scholar]
- 28.Chastin SF, Egerton T, Leask C, Stamatakis E. Meta-analysis of the relationship between breaks in sedentary behavior and cardiometabolic health. Obesity. (2015) 23:1800–10. 10.1002/oby.21180 [DOI] [PubMed] [Google Scholar]
- 29.Duvivier BM, Schaper NC, Hesselink MK, van Kan L, Stienen N, Winkens B, et al. Breaking sitting with light activities vs structured exercise: a randomised crossover study demonstrating benefits for glycaemic control and insulin sensitivity in type 2 diabetes. Diabetologia. (2017) 60:490–8. 10.1007/s00125-016-4161-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bailey DP, Locke CD. Breaking up prolonged sitting with light-intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. J Sci Med Sport. (2015) 18:294–8. 10.1016/j.jsams.2014.03.008 [DOI] [PubMed] [Google Scholar]
- 31.Dempsey PC, Larsen RN, Sethi P, Sacre JW, Straznicky NE, Cohen ND, et al. Benefits for type 2 diabetes of interrupting prolonged sitting with brief bouts of light walking or simple resistance activities. Diabetes Care. (2016) 39:964–72. 10.2337/dc15-2336 [DOI] [PubMed] [Google Scholar]
- 32.Mayr V, Nußbaumer-Streit B, Gartlehner G. [Quarantine alone or in combination with other public health measures to control covid-19: a rapid review (review)]. Gesundheitswesen. (2020) 82:501–6. 10.1055/a-1164-6611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sardinha LB, Magalhães JP, Santos DA, Júdice PB. Sedentary patterns, physical activity, and cardiorespiratory fitness in association to glycemic control in type 2 diabetes patients. Front Physiol. (2017) 8:262. 10.3389/fphys.2017.00262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Faulenbach M, Uthoff H, Schwegler K, Spinas GA, Schmid C, Wiesli P. Effect of psychological stress on glucose control in patients with type 2 diabetes. Diabet Med. (2012) 29:128–31. 10.1111/j.1464-5491.2011.03431.x [DOI] [PubMed] [Google Scholar]
- 36.Lloyd CE, Dyer PH, Lancashire RJ, Harris T, Daniels JE, Barnett AH. Association between stress and glycemic control in adults with type 1 (insulin-dependent) diabetes. Diabetes Care. (1999) 22:1278–83. 10.2337/diacare.22.8.1278 [DOI] [PubMed] [Google Scholar]
- 37.Wiesli P, Schmid C, Kerwer O, Nigg-Koch C, Klaghofer R, Seifert B, et al. Acute psychological stress affects glucose concentrations in patients with type 1 diabetes following food intake but not in the fasting state. Diabetes Care. (2005) 28:1910–5. 10.2337/diacare.28.8.1910 [DOI] [PubMed] [Google Scholar]
- 38.Mitranun W, Deerochanawong C, Tanaka H, Suksom D. Continuous vs. interval training on glycemic control and macro- and microvascular reactivity in type 2 diabetic patients. Scand J Med Sci Sports. (2014) 24:e69–76. 10.1111/sms.12112 [DOI] [PubMed] [Google Scholar]
- 39.Bohn B, Herbst A, Pfeifer M, Krakow D, Zimny S, Kopp F, et al. Impact of physical activity on glycemic control and prevalence of cardiovascular risk factors in adults with type 1 diabetes: a cross-sectional multicenter study of 18,028 patients. Diabetes Care. (2015) 38:1536–43. 10.2337/dc15-0030 [DOI] [PubMed] [Google Scholar]
- 40.Jelleyman C, Yates T, O'Donovan G, Gray LJ, King JA, Khunti K, et al. The effects of high-intensity interval training on glucose regulation and insulin resistance: a meta-analysis. Obes Rev. (2015) 16:942–61. 10.1111/obr.12317 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.