The clinical significance of this paper is the statistically increased mortality and morbidity on respiratory diseases in outpatients of Swedish foundry workers, particularly COPD, at certain exposure levels. The results can be used as risk assessment for individuals to prevent the development of respiratory diseases and as basis for new occupational exposure limits.
Keywords: COPD, respirable dust, respirable silica, respiratory diseases, silicosis
Objective
The mortality and morbidity pattern for respiratory diseases was determined in a cohort of 1752 Swedish foundry workers, particularly for respirable silica dust exposure.
Methods
The morbidity follow-up in the Swedish National Non-primary Outpatient Register covered 2001 to 2017 (NPR; specialist not in care patients), the mortality from the National Causes of Death Register covered 2001 to 2017. Cumulative exposures to silica and dust were determined.
Results
The morbidity in COPD showed significantly increased risk for all exposure groups, as did silicosis in the high exposure group, these cases corresponded to silica exposure levels below 0.05 mg/m3. The mortality of all causes and respiratory diseases was significantly increased by cumulative silica exposure in the high exposure group.
Conclusions
Significantly increased morbidity for respiratory diseases and COPD was determined at silica exposure levels below the current Swedish OEL.
Exposures in the Swedish iron foundry industry are complex and diverse. Such exposures include different materials, processes, and jobs, resulting in occupational exposures to a wide range of hazardous substances such as dust, chemical agents, gases, and vapors. Most of the investigated morbidity and mortality studies with high resolution have been devoted to exposure-response based on dust and crystalline silica exposure.
Regarding respiratory diseases, the occupational burden of non-malignant respiratory diseases has been evaluated by occupational titles in many reviews and meta-analyses.1–3 Silica exposure has more specifically been linked to emphysema, chronic obstructive lung disease (COPD) and tuberculosis4–7 and evaluated by quantitative silica exposures for certain diseases in only a few studies.8 In particular, silicosis has been evaluated in a number of studies, the most cited evaluating quantitative respirable silica air concentrations and cumulative exposures, suggesting occupational exposure limits (OELs) for preventive purposes.9–11 Decreased lung function and chronic bronchitis have also been related to silica exposure.5,12 Pneumonia caused by invasive pneumococcal disease, is mostly associated with welders exposed to metal fumes. However, other occupations and occupational titles have also been linked to metal exposures and pneumonia, particularly foundry workers and metal grinders exposed to iron dust.13 Idiopatic pulmonary fibrosis (IPF) have been related to metal and stone dust.1 To the best of our knowledge, no published papers on COPD and silica have presented quantitative exposure response data, based on modelled and measured respirable silica exposures data.
In this article, we present quantitative respirable silica and dust exposure-response morbidity data for COPD, silicosis (pneumoconiosis due to dust containing silica), asthma and other interstitial pulmonary diseases (where IPF is the dominating group in our material). Data is based on our historical Swedish cohort on iron foundry workers and quantitative silica exposure data for the whole study period. In addition, we present data on exposures and general mortality for respiratory diseases by cumulative respirable silica and dust exposure.
METHODS
Study Group
Ten Swedish foundries with complete sets of personnel records were selected, diversified among themselves in foundry size, types of sand utilised along the production line, production methods, and the practice of old and new casting techniques. The number of employees ranged from 8 to 388, and the production was between 400 and 120,000 metric tons per year.
Personal record data were processed to identify workers whose employment began before 2005, providing an initial cohort of 4128 employees (Fig. 1). A total of 2376 subjects were excluded due to inadequate employment information (n = 33), identity uncertainties (n = 7), insufficient employment time (n = 806), deceased before 2001 (n = 863), inadequate job titles (n = 434), and female gender (n = 233). The final cohort was 1752 silica/dust-exposed subjects. Employment time ranged from 1 to 52 years. The mean was 11, and the median was 7.
FIGURE 1.
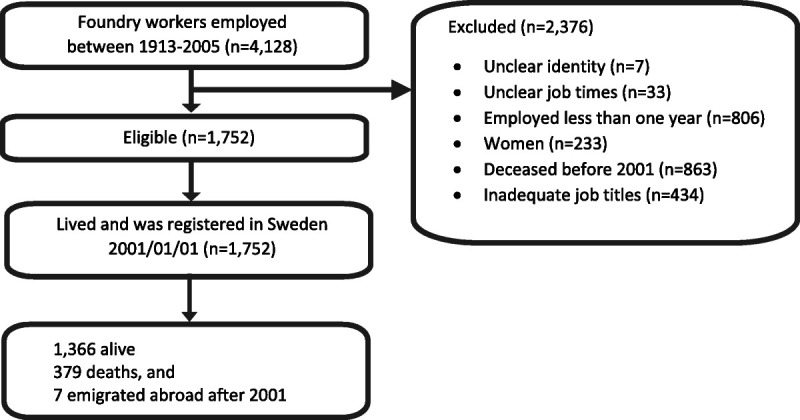
Flowchart description of cohort recruitment process.
Study Design
Recent and Historical Exposure Measurements
Dust measurements were performed between April 2005 and May 2006, taken at numerous sampling sites corresponding to 14 work categories at the foundries. These were pooled together and resulted in 340 samples for analysis. Measurement times ranged from 240 to 600 minutes for recent data and were corrected to an 8- hour time-weighted average (TWA), representing a full workday. Detection limit for respirable dust was 0.10 mg/sample and for respirable silica 0.005 mg/sample resulting in detection concentrations for an 8-hour TWA sample of approximately 0.10 and 0.005 mg/m3, respectively. Measurements taken before 1980 were collected as to total dust samples, and a sedimentation method was used to differentiate the fine fraction.14 Data from 1968 to 1974 were also provided by the Swedish Work Environment Authority (SWEA) and from compulsory measurements conducted by the foundries from 1968 to 2004. In order to properly combine, the historical measurements with the recent ones, the cyclone system used to differentiate the fine fraction of the latter was set with characteristics specified in the Johannesburg Convention from 1979, with a flow rate of 1.9 L/min, thus making historical and recent measurements comparable to each other.
Measurements were made as personal sampling. Each subject was equipped with an SKC aluminium cyclone (SKC 225–01-01, Eighty Four, PA), with a 0.8mmin pore size acetate filter (Millipore), and an air pump (SKC AirCheck 2000 to collect respirable dust. Eighty-Four PA, USA, MSA Escort, Pittsburgh, USA, or GSA SG4000, Gut Vellbröggen, Neuss, Germany) operating at a constant airflow rate of 2.5 L/min.15 The measurements were performed in the workers’ breathing zone. After sampling, the filters were analysed gravimetrically for respirable dust by the Department of Occupational and Environmental Medicine atÖ rebro University Hospital, Sweden. The samples were then analysed for respirable silica by X-ray diffraction with the diffraction angles 2θ = 20°, 26°, and 50°.16
Statistics
Descriptive statistics for the cohort were subdivided according to the year of birth and years of employment. The risk of falling ill from disease was calculated per job title and person-year. A mixed model was designed to assess the respirable dust and silica exposure concentrations for different periods, foundries, and job titles. A natural logarithm was performed since the exposure measurement data were skewed. The calculations projected a yearly cumulative exposure dose (mg/m3) for respirable dust and silica estimated for each cohort member.17
Formula for the mixed model analysis:
Dependent variable* = ß0 + ß1 [time periods] + ß2 [foundries] + ß3 [job titles] + ei ß0 = Intercept, a constant that is the same for all participants ß1 = time periods (1968 to 1979, 1980 to 1989, 1990 to 1999, 2000 to 2005) ß2 = foundries: 10 foundries ß3 = job titles: 12 job titles ei = measurement error (residual) *respirable dust and silica
Exposure among the various work operations was pooled into tertial groups, ≤2.76, 2.77 to 9.82, and 9.83 + for respirable dust and ≤ 0.14, 0.15 to 0.38, and 0.39+ for respirable dust respirable silica, based on mg/m3 lifetime cumulative exposure calculated as an 8-hour TWA.
In Sweden, all registered inhabitants are given a unique personal identification number and are by law granted access to equal healthcare and hospital services. Healthcare providers are legally obliged to record and register diagnoses in the journal system. The cohort was matched against the National Non-primary Outpatient Register (NPR) and the National Causes of Death Register (CDR), maintained and validated by the Swedish National Board of Health and Welfare. Since 2001, the NPR has contained data from public caregivers nationwide, whilst the CDR has had a complete register since 1952. The registered incidence rate of different diseases in the NPR and mortalities in the CDR from the cohort from 2001 to 2017 were collected. From the retrieved data, person-years at risk were calculated and stratified per annum according to the retrieved data to gender and 5-year interval age groups. Standardised Incidence Ratios (SIRs) and Standardised Mortality Ratios (SMRs) with 95% confidence intervals (CI) were calculated using the general Swedish population as a reference while assuming a Poisson distribution for the observed numbers. P < 0.05 were considered statistically significant. Statistical calculations were made with STATAversion 15 (College Station, TX) and SPSS version 25 (Armonk, NY).
RESULTS
For the cohort members, the mean cumulative silica exposure was 0.40 mg/m3 year ranging from 0.02 to 5.7 mg/m3 year, with a corresponding mean respirable dust concentration of 10.1 mg/m3 years, ranging from 0.25 to 92 mg/m3 years. Furnace and ladle repair workers represented the highest cumulative silica exposure. The average duration of employment was 11 years. The cumulative silica exposure in the cohort showed 75% below 0.5 mg/m3 years, 91% below 1 mg/m3 years (Table 1).
TABLE 1.
Number of Workers, Deaths, Year of Birth, Years of Employment, Time at Risk, Cumulative Respirable Dust and Silica mg/m3 Years by Job Title
| Job Categories | Subjects n | Deaths n | Year of Birth AM | Years of Employment AM | Time at Risk Years | Respirable Dust AM, mg/m3year | Respirable Silica AM, mg/m3 year |
|---|---|---|---|---|---|---|---|
| Caster | 64 | 12 | 1954 | 7 | 952 | 10.7 | 0.19 |
| Core maker | 246 | 41 | 1956 | 12 | 3 813 | 9.3 | 0.27 |
| Fettler | 430 | 68 | 1958 | 9 | 6 693 | 10.9 | 0.37 |
| Furnace and ladle repair | 6 | 2 | 1953 | 17 | 88 | 17.4 | 2.7 |
| Maintenance | 171 | 38 | 1949 | 15 | 2 578 | 9.1 | 0.53 |
| Melter | 130 | 24 | 1956 | 11 | 1 958 | 11.1 | 0.34 |
| Moulder | 209 | 45 | 1954 | 10 | 3 118 | 10.6 | 0.40 |
| Sand mixer | 7 | 3 | 1936 | 11 | 86 | 7.0 | 0.76 |
| Shake out | 18 | 4 | 1950 | 8 | 275 | 7.8 | 0.41 |
| Transportation | 26 | 4 | 1951 | 8 | 405 | 7.8 | 0.25 |
| Foundry workers | 196 | 60 | 1946 | 8 | 2 758 | 10.8 | 0.44 |
| Many jobs | 249 | 78 | 1945 | 12 | 3 511 | 8.5 | 0.46 |
| Total | 1 752 | 379 | 1953 | 10 | 26 218 | 10.1 | 0.40 |
AM, arithmetic mean; n, number of subjects/deaths.
Statistically significant increased SMRs was determined for all causes (SMR 1.28) and respiratory disease (SMR 1.66), regardless of exposure. For respiratory diseases and cumulative exposure to silica, a statistically significant increased risk (SMR 1.80) was determined for the high exposure group, 0.39 mg/m3 years, corresponding to an average silica exposure of 0.04 mg/m3 at our duration of exposures (Table 2).
TABLE 2.
Cause of Death in General and Respiratory Diseases in Particular Divided into Tertiles of Cumulative Respirable Dust and Silica Exposure, with Observed and Expected Outcomes of Death Expressed as Standardised Mortality Ratios
| Cause of Death | Exposure Measure | Exposure Groups (mg/m3 year) | Observed | Expected | SMR | 95% CI |
|---|---|---|---|---|---|---|
| All causes | Total | 379 | 295 | 1.28 | 1.16–1.42 | |
| Respirable dust | ≤2.76 | 130 | 107 | 1.21 | 1.01–1.44 | |
| 2.77–9.82 | 133 | 102 | 1.29 | 1.08–1.53 | ||
| 9.83+ | 116 | 85 | 1.36 | 1.12–1.63 | ||
| Respirable silica | ≤0.14 | 86 | 57 | 1.51 | 1.21–1.86 | |
| 0.15–0.38 | 96 | 79 | 1.21 | 0.98–1.48 | ||
| 0.39+ | 197 | 159 | 1.24 | 1.07–1.42 | ||
| Respiratory diseases | Total | 30 | 18.1 | 1.66 | 1.12–2.37 | |
| Respirable dust | ≤2.76 | 13 | 6.7 | 1.93 | 1.03–3.30 | |
| 2.77–9.82 | 12 | 6.4 | 1.87 | 0.96–3.26 | ||
| 9.83+ | 5 | 4.9 | 1.02 | 0.33–2.38 | ||
| Respirable silica | ≤0.14 | 5 | 3.0 | 1.67 | 0.54–3.90 | |
| 0.15–0.38 | 6 | 4.5 | 1.34 | 0.49–2.91 | ||
| 0.39+ | 19 | 10.6 | 1.80 | 1.08–2.81 |
Bold numbers, statistically significant.
CI, confidence interval; SMR, standardized mortality ratio.
The morbidity for all respiratory diseases by dust and silica exposure showed no statistically significant increase, regardless of exposure levels and agent. The morbidity expressed as SIRs for nonprimary outcare patients for COPD showed statistically significant exposure-response for the total group (SIR 1.94), for cumulative respirable dust (SIRs 1.81, 2.04, 1.97) for all types of exposure. These findings corresponded to cumulative respirable dust exposures ranging from 2.8 to 9.8 mg/m3 year, about 0.3 to 1 mg/m3 expressed as a TWA based on 10 years of average exposures. The present Swedish OEL for respirable dust is 5 mg/m3. For cumulative respirable silica, statistically significant morbidity (SIRs 2.35, 2.07,1.64) was determined for all exposure groups. The tertials ranged from 0.14 to 0.39 mg/m3 year, corresponding to 0.01 up to 0.04 mg/m3 expressed as a TWA based on 10 years of average exposures. The present Swedish OEL for respirable silica is 0.1 mg/m3 (Table 3).
TABLE 3.
Respiratory Diseases, COPD, Silicosis, Asthma and Other Interstitial Pulmonary Diseases Expressed as SIR by Tertiles of Cumulative Respirable Dust and Silica Exposure
| ICD10 | Disease | Exposure Measure | Exposure Groups (mg/m3 year) | Observed | Expected | SIR | 95% CI |
|---|---|---|---|---|---|---|---|
| J00-J99 | Respiratory system | Total | 252 | 435.4 | 0.58 | 0.51–0.65 | |
| Respirable dust | ≤2.76 | 100 | 146.2 | 0.68 | 0.56–0.83 | ||
| 2.77–9.82 | 105 | 144.4 | 0.73 | 0.59–0.88 | |||
| 9.83+ | 47 | 144.8 | 0.33 | 0.24–0.43 | |||
| Respirable silica | ≤0.14 | 42 | 139.0 | 0.30 | 0.22–0.41 | ||
| 0.15–0.38 | 48 | 146.1 | 0.33 | 0.24–0.44 | |||
| 0.39+ | 162 | 150.3 | 1.08 | 0.92–1.26 | |||
| J44 | Chronic obstructive pulmonary disease | Total | 101 | 52.2 | 1.94 | 1.58–2.35 | |
| Respirable dust | ≤2.76 | 33 | 18.2 | 1.81 | 1.25–2.54 | ||
| 2.77–9.82 | 35 | 17.2 | 2.04 | 1.42–2.83 | |||
| 9.83+ | 33 | 16.8 | 1.97 | 1.36–2.77 | |||
| Respirable silica | ≤0.14 | 28 | 11.9 | 2.35 | 1.56–3.40 | ||
| 0.15–0.38 | 33 | 15.9 | 2.07 | 1.43–2.91 | |||
| 0.39+ | 40 | 24.3 | 1.64 | 1.17–2.24 | |||
| J62 | Pneumoconiosis due to dust containing silica-silicosis | Total | 6 | 0.3 | 21.99 | 8.07–47.87 | |
| Respirable dust | ≤2.76 | 1 | 0.1 | 10.44 | 0.26–58.17 | ||
| 2.77–9.82 | 0 | 0.1 | – | – | |||
| 9.83+ | 5 | 0.1 | 57.15 | 18.56–133.36 | |||
| Respirable silica | ≤0.14 | 0 | 0.1 | – | – | ||
| 0.15–0.38 | 0 | 0.1 | – | – | |||
| 0.39+ | 6 | 0.1 | 45.87 | 16.83–99.83 | |||
| J45 | Asthma | Total | 24 | 54.9 | 0.44 | 0.28–0.65 | |
| Respirable dust | ≤2.76 | 5 | 18.1 | 0.28 | 0.09–0.64 | ||
| 2.77–9.82 | 9 | 18.2 | 0.49 | 0.23–0.94 | |||
| 9.83+ | 10 | 18.5 | 0.54 | 0.26–0.99 | |||
| Respirable silica | ≤0.14 | 11 | 18.6 | 0.59 | 0.30–1.06 | ||
| 0.15–0.38 | 8 | 18.9 | 0.42 | 0.18–0.83 | |||
| 0.39+ | 5 | 17.3 | 0.29 | 0.09–0.67 | |||
| J84 | Other interstitial pulmonary diseases | Total | 17 | 11.8 | 1.44 | 0.84–2.31 | |
| Respirable dust | ≤2.76 | 2 | 4.1 | 0.49 | 0.06–1.76 | ||
| 2.77–9.82 | 7 | 3.9 | 1.81 | 0.73–3.72 | |||
| 9.83+ | 8 | 3.8 | 2.09 | 0.90–4.12 | |||
| Respirable silica | ≤0.14 | 3 | 2.8 | 1.08 | 0.22–3.14 | ||
| 0.15–0.38 | 4 | 3.7 | 1.09 | 0.30–2.79 | |||
| 0.39+ | 10 | 5.3 | 1.88 | 0.90–3.45 |
Bold numbers, statistically significant.
CI, confidence interval; SIR, standardized incidence ratio.
Regarding silicosis, a statistically significant increased risk (SIR 45.87) of the disease was found for the high exposure group of respirable silica, +0.39 mg/m3 years, corresponding to +0.04 mg/m3 expressed as a TWA based on ten years of average exposures. Asthma or interstitial pulmonary fibrosis did not present any significant exposure-response finding for either respirable dust or respirable silica (Table 3).
DISCUSSION
Main Findings
For foundry workers as non-primary outcare patients, statistically significant morbidity (SIRs 2.35, 2.07, 1.64) was determined for all cumulative respirable silica exposure groups for COPD. The tertials ranged from 0.14 to 0.39 mg/m3 year, silicosis showed a statistically significant increase risk (SIR 45.87) for the high exposure group of respirable silica, +0.39 mg/m3 years, corresponding to +0.04 mg/m3 expressed as a TWA based on our average exposure years.
Statistically significant increased SMR was determined for all causes and respiratory diseases regardless of exposure levels. A statistically significant increased risk of respiratory diseases and cumulative exposure to silica a SMR 1.80 was determined for the high exposure group, 0.39 mg/m3 years, corresponding to an average silica exposure of about 0.04 mg/m3 at our duration of exposures.
To the best of our knowledge, these are the first published data on respiratory diseases for non-primary outcare patients from the iron foundry using quantitative cumulative silica exposure data for exposure-response analysis. A strength of this study is the quality of exposure and morbidity data on a patient in the NPR register. The used NPR and CDR registers are both maintained and validated by the Swedish National Board of Health and Welfare. The Swedish National Patient Register is a reliable tool for epidemiological studies, enabling the possibility of retrieving morbidity data for the entire patient population.18 We have a large database of well-defined silica exposure for each job title and time period for the Swedish iron foundry industry.19
Respiratory Diseases and the Morbidity of COPD
In a study on Taiwanese foundry workers, differences in exposure levels, furnace and fettling areas, 2.76 and 1.86 mg/m3, respectively, on respirable dust were used to establish exposure-response on lung function decreases and respiratory abnormalities with crystalline silica.20 In a U.S. study on foundry workers, trends and exposure-response was analyzed on cumulative silica exposures and respiratory abnormalities. For smokers, an exposure-response trend was determined, however, not for non-smokers. The grouped exposure levels corresponded to TWA 0.006, 0.04, 0.12, and 0.28 mg/m3, respectively.21
A Swedish study on granite crushers referred to in the review by Bröske8 noted significant changes in lung function and airway obstruction status in a follow up after 12 years of respirable silica exposure ranging from 0.16 to 0.21 mg/m3.12 In a Dutch study on concrete workers, mild COPD symptoms was reported at average levels of respirable silica of about 0.06 mg/m3.22 In a Norwegian study on tunnel workers, a non-significant increased risk of obstructive pulmonary disease was determined at respirable silica concentrations of 0.03 mg/m3, cumulative silica exposures ranging from 0.003 to 3.6 mg/m3 years.23,24 Based on conservative use of the duration of exposure for tunnel workers in Bakke,24 10 years, the cumulative exposures would correspond to TWA air concentrations of <0.003 to 0.36 mg/m3. In our data presented here, we determined significantly increased risks for respirable dust and silica and COPD, conservatively at average TWA exposure levels at about 1+ mg/m3 for respirable dust and 0.04+ mg/m3 for respirable silica. Our data is based on exposure data from 1968 to 2006 in Swedish iron foundries and COPD diagnosis 2001 to 2017 from national registers. The COPD diagnosis collected from a specialist not in care patient register allows us to make a statement about exposureresponse on respirable silica and COPD. Most of the published papers mentioned are based on analysing lung function abnormalities rather than COPD diagnosis, and their findings effect are determined at equal or higher silica exposures compared to data presented here.
Silicosis
A number of articles have been published on silicosis and the link between the disease and respirable silica exposure measures, in particular cumulative silica exposure presented as mg/m3 years.9,11,25 In the article by Steenland, 1.9% risk after a lifetime work at the exposure level of 0.1 mg/m3 was estimated, that is, 4 mg/m3 years. In one of the most prominent evaluations11 relative risks (RR) of 1 was presented at 0.99 mg/m3 years, RR 3.39 at 0.99 to 1.97 mg/m3 years. Introducing comparative lifetime risk, silicosis morbidity showed a 47% to 77% excess silica at 0.1 mg/m3, 0.8% at 0.01 mg/m3. OSHA accepts26 an excess risk of 0.1% on serious diseases or deaths in the United States, implying and supporting an OEL at about 0.05 mg/m3 to prevent silicosis morbidity. However, studies on silicosis in the foundry environment were excluded from these meta-analyses. The silicosis risk in foundries have been evaluated in a small study,27 showing 0.4% excess risk at lifetime cumulative exposures below 2 mg/m3 years. Our data, based on nonprimary outpatient care registers, however evaluating small numbers, suggests significantly increased morbidity risk (SIR 45.87) for cumulative silica exposures at +0.39 mg/m3 on an average duration of exposure of 11 years, suggesting an excess risk of silicosis at a TWA of about +0.04 mg/m3, consistent with findings presented in the literature and strongly suggesting a Swedish OEL at about 0.05 mg/m3, at present 0.1 mg/m3.
Asthma
Regarding asthma in our study, we experienced statistically significant under risk for all exposure groups but one on respirable dust and silica. In a review regarding population-based, case–control or asthma cohort studies with the type of exposure revealed, no link could be established between diagnosed asthma and branches and industries related to silica exposures in 21 evaluates papers.1 In an ever more extensive review of agents in the workplaces causing asthma, silica is not in a comprehensive listing of potential asthma inducing agents. However, the foundry environment is listed due to MDI exposure.28 The literature supports our findings.
Could different mechanisms explain our differences in morbidity and mortality patterns? The mechanism of how silica cause COPD is believed to be via cytotoxicity and cause secretion of proinflammatory and fibrogenic factors leading to airflow obstruction and emphysema.5 Small silica particles penetrate the cell walls and give localised fibrotic changes that increase airway resistance and decrease expiratory lung volume.7 Silica may also inactivate α1-AT that could, by passing the endothelium, cause localised fibrosis of small airways and cause chronic bronchitis, bronchiolitis, and emphysema where emphysema are most common.5 Studies show a decline in expiratory lung capacity (FEV1 and FEV1/FVC) with cumulative silica exposure where symptoms appear earlier than for silicotic changes. The mechanism where fibrotic changes and development of emphysema can explain why asthma is not increased from silica exposure.5,8,29
Idiopathic Pulmonary Fibrosis
In a review on nonmalignant respiratory diseases and occupational exposures the occupational burden of IPF was meta-analysed based on six case control studies performed after 1990.1,30 Significant findings related to IPF and jobs were determined for live stock, wood dust textile dust, metal dust, stone dust (silica) and smoking. Four papers were devoted to silica exposure, three of these showed significant findings for silica exposures and stone work.30 No exposure measurement datawas presented in the studies, the exposure data based on occupation and jobs. In this paper we found non-significant exposure-response for both silica and respirable dust at average exposure levels of <0.05 and 1 mg/m3, respectively. The numbers were small, in total 17 workers, but the results are indicative and calls for further studies based on quantitative data. Also the whole ICD chapter J84 where used but IPF is the dominating group. We consider the discrepancies between earlier findings in IPF in traditional and heavier silica exposed workers and our findings as a result of rather low average exposures for our foundry workers, <0.05 mg/m3.
Respiratory Diseases, Mortality
In a review article from 2007, many studies on iron and steel foundry workers were evaluated.7 In a U.S. study on ferrous foundry workers31 a statistically significant excess mortality of non-malignant respiratory disease (SMR 1.77), in particular among the finishers and in the core room, and a British study on steel foundry workers significantly raised SMR of 1.53 was determined for NMPD (non-malignant respiratory disease).32 In a Danish study on foundry workers, statistically significant increased risk was determined for respiratory diseases (SMR 1.39), pneumoconiosis (SMR 73.68), non-significant on chronic bronchitis and emphysema (SMR 1.32) however not on circulatory diseases (SMR 0.95).33 These studies did not present any exposure-response data based on cumulative silica exposures.
In our mortality and morbidity study on iron foundry workers presented here, we determined a statistically significant risk for the mortality on respiratory diseases, SMR 1.66, in line with the earlier findings by Silverstein, Hansen, and Sorahan.31–33 Notably, when an exposure-response analysis was performed and presented here on cumulative silica exposures, statistically significant excess risk of SMR 1.80 was determined at cumulative exposure of 0.39 mg/m3 years, corresponding to 0.04 mg/m3 based on an average duration of exposure of 10 years.
Limitations
A limitation of this study is the lack of data on potential confounding factors that could affect the results, such as specific metal, dusts, gases, or smoking habits. We could not obtain any information on these confounding factors for this cohort, and no complete individual data on smoking habits was available. However, in the papers analysed in the reviews on COPD, other potential dust or gas exposures are most often taken into account when COPD, respirable dust and gases are evaluated.5,8
CONCLUSIONS
This article concludes statistically increased morbidity on respiratory diseases of silica exposed Swedish foundry workers, particularly COPD at exposure levels well below the current Swedish OEL. The morbidity of COPD and silicosis was significantly increased in the high exposure group, corresponding to much the same average silica exposure level < 0.05 mg/m3, about less than half of the Swedish OEL (0.1 mg/m3) at our duration of exposures. The mortality of all causes and respiratory diseases was significantly increased by cumulative silica exposure in the high exposure group, corresponding to an average silica exposure level < 0.05 mg/m3. Furthermore, no increased morbidity on asthma was determined.
Footnotes
This study was supported by the Swedish Research Council for Health, Working Life, and Welfare (FORTE) grant number 2014-0802.
The study was approved by the Regional Ethical Review Board, Uppsala, dnr. 2015/066.
The authors report no conflicts of interest, either commercial or non-commercial.
Clinical significance: The clinical significance of this paper is the statistically increased mortality and morbidity on respiratory diseases in outpatients of Swedish foundry workers, particularly COPD, at certain exposure levels. The results can be used as risk assessment for individuals to prevent the development of respiratory diseases and as basis for new occupational exposure limits.
Contributor Information
Alexander Lenander-Ramirez, Email: lenanderalexander@gmail.com.
Ing-Liss Bryngelsson, Email: ing-liss.bryngelsson@regionorebrolan.se.
Per Vihlborg, Email: per.vihlborg@regionorebrolan.se.
Håkan Westberg, Email: hakan.westberg@regionorebrolan.se.
REFERENCES
- 1.Blanc PD Annesi-Maesano I Balmes JR, et al. The occupational burden of nonmalignant respiratory diseases. An Official American Thoracic Society and European Respiratory Society Statement. Am J Respir Crit Care Med. 2019;199:1312–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bakke PS, Baste V, Hanoa R, Gulsvik A. Prevalence of obstructive lung disease in a general population: relation to occupational title and exposure to some airborne agents. Thorax. 1991;46:863–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rushton L. Occupational causes of chronic obstructive pulmonary disease. Rev Environ Health. 2007;22:195–212. [DOI] [PubMed] [Google Scholar]
- 4.Chen GX Burnett CA Cameron LL, et al. Tuberculosis mortality and silica exposure: a case-control study based on a national mortality database for the years 1983–1992. Int J Occup Environ Health. 1997;3:163–70. [DOI] [PubMed] [Google Scholar]
- 5.Hnizdo E, Vallyathan V. Chronic obstructive pulmonary disease due to occupational exposure to silica dust: a review of epidemiological and pathological evidence. Occup Environ Med. 2003;60:237–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rees D, Murray J. Silica, silicosis and tuberculosis. Int J Tuberc Lung Dis. 2007;11:474–84. [PubMed] [Google Scholar]
- 7.Rushton L. Chronic obstructive pulmonary disease and occupational exposure to silica. Rev Environ Health. 2007;22:255–72. [DOI] [PubMed] [Google Scholar]
- 8.Bröske I, Thiering E, Heinrich J, Huster KM, Nowak D. Respirable quartz dust exposure and airway obstruction: a systematic review and meta-analysis. Occup Environ Med. 2014;71:583–9. [DOI] [PubMed] [Google Scholar]
- 9.Steenland K. One agent, many diseases: exposure-response data and comparative risks of different outcomes following silica exposure. Am J Ind Med. 2005;48:16–23. [DOI] [PubMed] [Google Scholar]
- 10.Rice FL, Stayner LT. Assessment of silicosis risk for occupational exposure to crystalline silica. Scand J Work Environ Health. 1995;21(Suppl 2):87–90. [PubMed] [Google Scholar]
- 11.Mannetje A’t Steenland K Attfield M, et al. Exposure-response analysis and risk assessment for silica and silicosis mortality in a pooled analysis of six cohorts. Occup Environ Med. 2002;59:723–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malmberg P, Hedenström H, Sundblad BS. Changes in lung function of granite crushers exposed to moderately high silica concentrations: a 12 year follow up. Br J Ind Med. 1993;50:726–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Palmer KT, Cosgrove MP. Vaccinating welders against pneumonia. Occup Med. 2012;62:325–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NBOSH . Method Report 1010: Measurements of Respirable Dust and Total Dust (in Swedish). Stockholm, Sweden: National Board of Occupational Safety and Health; 1979. [Google Scholar]
- 15.Health and Safety Executive (HSE 2000). MDHDS: General methods for sampling and gravimetric analysis of inhalable and respirable dust. Report no 14/3, February 2000, Suffolk U.K.
- 16.NIOSH . Manual of analytical methods, 4th edition. Silica, crystalline, by XRD: method 7500. Cincinnati: National Institute of Occupational Safety and Health, US department of health and human services; 1994. [Google Scholar]
- 17.Andersson L, Burdorf A, Bryngelsson IL, Westberg H. Estimating trends in quartz exposure in Swedish iron foundries—predicting past and present exposures. Ann Occup Hyg. 2012;56:362–72. [DOI] [PubMed] [Google Scholar]
- 18.Ludvigsson JF Andersson E Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andersson L, Bryngelsson IL, Ohlson CG, Nayström P, Lilja BG, Westberg H. Quartz and dust exposure in Swedish iron foundries. J Occup Environ Hyg. 2009;6:9–18. [DOI] [PubMed] [Google Scholar]
- 20.Kuo H-W, Chang C-L, Liang W-M, Chung B-C. Respiratory abnormalities among male foundry workers in central Taiwan. Occup Med. 1999;49:499–505. [DOI] [PubMed] [Google Scholar]
- 21.Hertzberg VS, Rosenman KD, Reilly MJ, Rice CH. Effect of occupational silica exposure on pulmonary function. Chest. 2002;122:721–8. [DOI] [PubMed] [Google Scholar]
- 22.Meijer E, Kromhout H, Heederik D. Respiratory effects of exposure to low levels of concrete dust containing crystalline silica. Am J Ind Med. 2001;40:133–40. [DOI] [PubMed] [Google Scholar]
- 23.Ulvestad B, Bakke B, Melbostad E, Fuglerud P, Kongerud J, Lund MB. Increased risk of obstructive pulmonary disease in tunnel workers. Thorax. 2000;55:277–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bakke B, Ulvestad B, Stewart P, Eduard W. Cumulative exposure to dust and gases as determinants of lung function decline in tunnel construction workers. Occup Environ Med. 2004;61:262–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Finkelstein MM. Silica, silicosis, and lung cancer: a risk assessment. Am J Ind Med. 2000;38:8–18. [DOI] [PubMed] [Google Scholar]
- 26.Rodricks JV, Brett SM, Wrenn GC. Significant risk decisions in federal regulatory agencies. Regul Toxicol Pharmacol. 1987;7:307–20. [DOI] [PubMed] [Google Scholar]
- 27.Rosenman KD, Moore-Fuller M, Reilly MJ. Kidney disease and silicosis. Nephron. 2000;85:14–9. [DOI] [PubMed] [Google Scholar]
- 28.Baur X, Bakehe P. Vellguth H Bronchial asthma and COPD due to irritants in the workplace—an evidence-based approach. J Occup Med Tox. 2012;7:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maestrelli P, Boschetto P, Fabbri LM, Mapp CE. Mechanisms of occupational asthma. J Allergy Clin Immunol. 2009;123:531–42. [DOI] [PubMed] [Google Scholar]
- 30.Taskar VS, Coultas DB. Is idiopathic pulmonary fibrosos an environmental disease? Proc Am Thorac Soc. 2006;3:293–8. [DOI] [PubMed] [Google Scholar]
- 31.Silverstein M Maizlich N Park R, et al. Mortality among ferrous foundry workers. Am J Ind Med. 1986;10:27–43. [DOI] [PubMed] [Google Scholar]
- 32.Sorahan T, Faux AM, Cooke MA. Mortality among a cohort of United Kingdom steel foundry workers with special reference to cancers of the stomach and lung, 1946-90. Occup Environ Med. 1994;51:316–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hansen ES. A cohort mortality study of foundry workers. Am J Ind Med. 1997;32:223–33. [DOI] [PubMed] [Google Scholar]


