Hannah Stamberger
Hannah Stamberger, MD, PhD
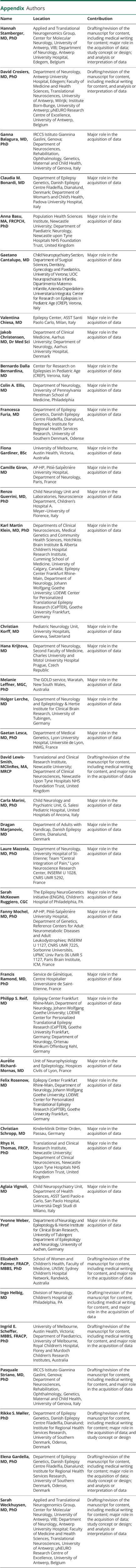
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,✉,
David Crosiers
David Crosiers, MD, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Ganna Balagura
Ganna Balagura, MD, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Claudia M Bonardi
Claudia M Bonardi, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Anna Basu
Anna Basu, MA, FRCPCH, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Gaetano Cantalupo
Gaetano Cantalupo, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Valentina Chiesa
Valentina Chiesa, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Jakob Christensen
Jakob Christensen, MD, Dr Med Sci
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Bernardo Dalla Bernardina
Bernardo Dalla Bernardina, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Colin A Ellis
Colin A Ellis, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Francesca Furia
Francesca Furia, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Fiona Gardiner
Fiona Gardiner, BSc
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Camille Giron
Camille Giron, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Renzo Guerrini
Renzo Guerrini, MD, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Karl Martin Klein
Karl Martin Klein, MD, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Christian Korff
Christian Korff, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Hana Krijtova
Hana Krijtova, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Melanie Leffner
Melanie Leffner, MGC, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Holger Lerche
Holger Lerche, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Gaetan Lesca
Gaetan Lesca, MD, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
David Lewis-Smith
David Lewis-Smith, MClinRes, MA, MRCP
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Carla Marini
Carla Marini, MD, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Dragan Marjanovic
Dragan Marjanovic, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Laure Mazzola
Laure Mazzola, MD, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Sarah McKeown Ruggiero
Sarah McKeown Ruggiero, CGC
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Fanny Mochel
Fanny Mochel, MD, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Francis Ramond
Francis Ramond, MD, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Philipp S Reif
Philipp S Reif, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Aurélie Richard-Mornas
Aurélie Richard-Mornas, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Felix Rosenow
Felix Rosenow, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Christian Schropp
Christian Schropp, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Rhys H Thomas
Rhys H Thomas, FRCP, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Aglaia Vignoli
Aglaia Vignoli, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Yvonne Weber
Yvonne Weber, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Elizabeth Palmer
Elizabeth Palmer, FRACP, MBBS, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Ingo Helbig
Ingo Helbig, MD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Ingrid E Scheffer
Ingrid E Scheffer, MBBS, FRACP, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Pasquale Striano
Pasquale Striano, MD, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Rikke S Møller
Rikke S Møller, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,
Elena Gardella
Elena Gardella, MD, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,*,
Sarah Weckhuysen
Sarah Weckhuysen, MD, PhD
1From the Applied and Translational Neurogenomics Group (H.S., S.W.), VIB Center for Molecular Neurology, University of Antwerp; Department of Neurology (H.S., D.C., S.W.), Antwerp University Hospital; Faculty of Medicine and Health Sciences (D.C., S.W.), Translational Neurosciences, Institute Born-Bunge (D.C.), and µNEURO Research Centre of Excellence (D.C., S.W.), University of Antwerp, Belgium; IRCCS Istituto Giannina Gaslini (G.B., P.S.), Genova; Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (G.B., P.S.), University of Genova, Italy; Department of Epilepsy Genetics (C.M.B., F.F., R.S.M., E.G.), Danish Epilepsy Centre Filadelfia, Dianalund, Denmark; Department of Woman's and Child's Health (C.M.B.), Padova University Hospital, Italy; Population Health Sciences Institute (A.B.), Newcastle University; Department of Paediatric Neurology (A.B.), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neuropsychiatry Section (G.C.), Department of Surgical Sciences, Dentistry, Gynecology and Paediatrics, University of Verona; UOC Neuropsichiatria Infantile (G.C.), Dipartimento Materno-Infantile, Azienda Ospedaliero-Universitaria Integrata, Verona; Center for Research on Epilepsies in Pediatric Age (CREP) (G.C., B.D.B.), Verona; Epilepsy Center (V.C.), ASST Santi Paolo Carlo, Milan, Italy; Department of Clinical Medicine (J.C.), Aarhus University; Department of Neurology (J.C.), Aarhus University Hospital, Denmark; Department of Neurology (C.A.E.), University of Pennsylvania Perelman School of Medicine, Philadelphia; Institute for Regional Health Services Research (F.F., R.S.M., E.G.), University of Southern Denmark, Odense; University of Melbourne, Austin Health (F.G., I.E.S.), Victoria, Australia; AP-HP (C.G.), Pitié-Salpêtrière University Hospital, Department of Neurology, Paris, France; Child Neurology Unit and Laboratories (R.G.), Neuroscience Department, Children's Hospital A. Meyer–University of Florence, Italy; Departments of Clinical Neurosciences (K.M.K.), Medical Genetics and Community Health Sciences, Hotchkiss Brain Institute & Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Canada; Epilepsy Center Frankfurt Rhine-Main (K.M.K., P.S.R., F. Rosenow), Department of Neurology, Johann Wolfgang Goethe University; LOEWE Center for Personalized Translational Epilepsy Research (CePTER) (K.M.K., P.S.R., F. Rosenow), Goethe University Frankfurt, Frankfurt am Main, Germany; Pediatric Neurology Unit (C.K.), University Hospitals, Geneva, Switzerland; Department of Neurology (H.K.), Second Faculty of Medicine, Charles University and Motol University Hospital Prague, Czech Republic; The GOLD Service (M.L.), Waratah, New South Wales, Australia; Department of Neurology and Epileptology & Hertie Institute for Clinical Brain Research (H.L., Y.W.), University of Tubingen, Germany; Department of Medical Genetics (G.L.), Lyon University Hospital, Université de Lyon, INMG, France; Translational and Clinical Research Institute (D.L.-S., R.H.T.), Newcastle University; Department of Clinical Neurosciences (D.L.-S., R.H.T.), Newcastle Upon Tyne Hospitals NHS Foundation Trust, United Kingdom; Child Neurology and Psychiatric Unit (C.M.), G. Salesi Pediatric Hospital, United Hospitals of Ancona, Italy; Department of Adults with Handicap (D.M.), Danish Epilepsy Centre, Dianalund, Denmark; Department of Neurology (L.M.), University Hospital of St-Etienne; Team “Central Integration of Pain” (L.M.), Lyon Neuroscience Research Center, INSERM U 1028, CNRS UMR 5292, France; The Epilepsy NeuroGenetics Initiative (ENGIN) (S.M.R.), Children's Hospital of Philadelphia, PA; AP-HP (F.M.), Pitié-Salpêtrière University Hospital, Department of Genetics, Reference Centers for Adult Neurometabolic Diseases and Adult Leukodystrophies; INSERM U 1127 (F.M.), CNRS UMR 7225, Sorbonne Universités, UPMC Univ Paris 06 UMR S 1127, Paris Brain Institute, ICM; Service de Génétique (F. Ramond), Centre Hospitalier Universitaire de Saint-Etienne, France; Department of Neurology (P.S.R.), Ortenau Klinikum Offenburg Kehl, Germany; Unit of Neurophysiology and Epileptology (A.R.-M.), Hospices Civils of Lyon, France; Kinderklinik Dritter Orden (C.S.), Passau, Germany; Child Neuropsychiatry Unit (A.V.), Department of Health Sciences, ASST Santi Paolo e Carlo, San Paolo Hospital, Università Degli Studi di Milano, Italy; Department of Epileptology and Neurology (Y.W.), University of Aachen, Germany; School of Women and Children's Health (E.P.), Faculty of Medicine, UNSW; Sydney Children's Hospital Network (E.P.), Randwick, Australia; Division of Neurology (I.H.), Children's Hospital of Philadelphia, PA; and Department of Paediatrics (I.E.S.), University of Melbourne, Royal Children's Hospital, Florey and Murdoch Children's Research Institutes, Melbourne, Australia.
1,*