Abstract
Rationale, Aims and Objectives
The field of implementation science is critical for embedding research evidence into healthcare practice, benefiting individuals, organizations, governments, and the broader community. Implementation science is messy and complex, underpinned by many theories and frameworks. Efficacious interventions for older people with multiple comorbidities exist, yet many lack effectiveness evaluation relevant to pragmatic implementation within aged care practice. This article outlines the conceptualization and development of an Implementation Framework for Aged Care (IFAC), fit‐for‐purpose for an aged care organization, Bolton Clarke, intent on embedding evidence into practice.
Method
A four‐stage process was adopted to (1) explore context and relevant literature to conceptualize the IFAC; (2) identify key elements for a draft IFAC; (3) expand elements and refine the draft in consultation with experts and (4) apply the IFAC to three existing projects, identifying key learnings. A checklist to operationalize the IFAC was then developed.
Results
The IFAC is grounded in codesign principles and encapsulated by the implementation context, from a social, cultural and political perspective. The IFAC addresses the questions of (1) why do we need to change?; (2) what do we know?; (3) who will benefit?; (4) who will make the change?; (5) what strategies will be used?; and (6) what difference are we making? Three pilot projects: early adoption of a Wellness and Reablement approach; a care worker and virtual physiotherapist‐led program to prevent falls; and a therapeutic horticulture program for residential communities, highlight learnings of applying the IFAC in practice.
Conclusion
This fit‐for‐purpose IFAC was developed for a proactive and responsive aged care provider. The simplicity of the six‐question IFAC is underpinned by substantial theoretical perspectives for its elements and their connections. This complexity is then consolidated into an 18‐question checklist to operationalize the IFAC, necessary to advance the translation of evidence into clinical practice.
Keywords: healthcare, health services research
1. INTRODUCTION
Realizing the benefits of effective innovations in healthcare, and likely uptake into practice requires more effort and attention on implementation planning. 1 Research has traditionally concentrated on the efficacy of interventions—what works as a best practice rather than what works in practice 2 ; but there is now far greater focus on accelerating the translation of efficacious interventions through embedded pragmatic trials. 3 The focus has shifted to understanding the adoption (or nonadoption), implementation, and spread of healthcare interventions, 4 , 5 with a growing recognition of the complex adaptive nature of health systems and intricacies of context, 6 the role of healthy collaborations between stakeholders, 7 and more flexible methods to support implementation in these complex adaptive systems. 8 Implementation science is not a neat, linear sequential journey, but rather is chaotic, dynamic, and fluid, 9 making it a challenge to adopt a cohesive plan.
In response to the consistent failure to move research into policy and practice in a timely and cost‐sensitive manner, the field of implementation science in healthcare is burgeoning 10 ; however, the aged care environment remains somewhat neglected and presents its own unique challenges. A growing older population with multiple health conditions and lag in adopting cost‐effective evidence‐based practices is placing increasing demand on healthcare systems. 11 , 12 Complexity science, as an extension of implementation science, is useful for considering both the integrated nature of care required for older people with multimorbidity and that translation of evidence into practice is uncertain, unpredictable, and dependent upon social relations and local context. 13 , 14 Over the last decade in Australia, the aged care system has undergone major reform in response to recurrent calls for improved access, quality, consumer choice and financial sustainability. 15 This has resulted in the Living Longer, Living Better legislation, completion of a Royal Commission into Aged Care Quality and Safety and introduction of the Aged Care Quality Standards. 15 , 16 , 17 These reforms have provided the impetus for change that is necessary within the Australian aged care system. However, changes must be underpinned by implementation science principles, to ensure that effective interventions identified through research actually reach the breadth of their intended audience (i.e., all stakeholders within the aged care system).
To that end, codesign principles must form the foundation of any implementation approach. Codesign methodology entails the active engagement of all stakeholders, drawing on their unique experiences to shape the design of tools, products or programs. 18 , 19 Critical in the process is (a) a systems perspective with recognition of the complex, nonlinear process and local contextual adaptation; (b) centrality of participant experience, through respect, trust and inclusion; and (c) recognition that governance and processes are as important as the outcomes. 20
Implementation and complexity science highlight the multifaceted relational processes inherent in health and aged care systems. Normalization Process Theory is particularly focused on how these social processes influence the integration required to operationalize change in practice. 21 There is an urgent need for a fit‐for‐purpose implementation framework within the Australian aged care environment, drawing on the most appropriate components of work previously undertaken. Although implementation tools and frameworks exist, 22 , 23 there are often insufficient prompts or guidance to effectively operationalize them for aged care practice alongside insufficient focus on implementation outcomes, as distinct from clinical outcomes. The aim of this article is to describe the development of the Bolton Clarke Implementation Framework for Aged Care (IFAC)—a framework that is fit‐for‐purpose in the context of community and residential aged care, drawing on the principles of codesign. While not wanting to add to the plethora of frameworks in circulation, the emphasis of the IFAC is on how it works in practice, guided by a checklist for operationalization. The Double‐Diamond design framework 24 provides a structure for the foundation of the IFAC, adapted in Figure 1 below.
Figure 1.

Adapted codesign framework
This article details the development of the IFAC from its conceptualization, design, expansion of discrete elements through to the final product, highlighting its evolution via three projects undertaken by Bolton Clarke, and is structured according to the four components of the Double‐Diamond Framework.
-
1.
Discover: Conceptualization of the implementation Framework through exploring the literature, gathering insights, and the context of the aged care environment.
-
2.
Define: Identify the key elements of an implementation Framework as relevant for the aged care sector, and draft the IFAC.
-
3.
Develop: Expansion of draft IFAC components, through consultation with implementation science experts.
-
4.
Deliver: Application of the IFAC in three pilot projects in aged care (By Your Side, Wellness and Reablement (W&R) and Let's Dig In!, further described below).
2. METHOD
2.1. Conceptualization of the IFAC
The ‘Discover’ phase for IFAC development comprised two components. First, challenges associated with translating research evidence into practice in the context of aged care were explored, and second, current literature was reviewed to identify existing models, frameworks and theories; to learn from existing research and theory as a basis for this fit for purpose IFAC. Conceptualization of the IFAC occurred through:
-
1.
Initial identification of the need for an implementation framework to guide the work of the aged care provider's Research Institute (C. M., R. O. and J. L.), in alignment with an organization‐specific, proactive and independent Human Research Ethics Committee, an engaged Governing Board and Executive Management team and a strengthening reputation across the organization's home care, retirement living and residential care business streams.
-
2.
Gathering information and insights from multidisciplinary Research Institute team members about the challenges and opportunities of implementing research into practice within the organization.
-
3.
An extensive search of electronic databases for relevant implementation frameworks, models and theories (CINAHL, Medline, PubMed and PsycINFO), using search terms (and derivatives) of ‘implementation’, ‘models’ and ‘frameworks’, (2009–2018), supplementing the work carried out by Ward et al., 23 which identified 28 frameworks, models and theories.
-
4.
Review of identified frameworks, models and theories for relevance according to their appropriateness for embedding evidence into aged care provider practice, while avoiding those which were obscure and overly complex (see Supporting Information Material).
-
5.
Review of the selected frameworks, models and theories, including their strengths and limitations, by Research Institute team members; with input from independent clinical academic experts in Implementation Science (see Supporting Information Material).
2.2. Identify the key elements of an implementation framework as relevant for the aged care sector
The ‘Define’ phase was aimed at synthesizing the ‘Discover’ phase findings, specifically to identify critical IFAC components. 24 For pragmatic reasons, a full systematic review was not undertaken. Including the 28 models identified by Ward et al., 23 we examined a total of 35 frameworks, models and theories for relevance (CM and RO). While most were well‐known and widely utilized, many were deemed inappropriate for the explicit intended purpose of an IFAC. Other frameworks were not directly relevant but provided useful information about underpinning theories. Nine models/frameworks were identified as potentially relevant for an aged care provider, with their corresponding strengths and limitations noted (as pertinent to their function within aged care provider practice (see Supporting Information Material). Most relevant, and thus heavily influencing the components of the IFAC, was the work of Lavis et al., 25 who identified five key questions to support the transfer of knowledge within an organization: what, to whom, by whom, how and with what effect should research knowledge be transferred. After the draft IFAC (Figure 2) was reviewed by staff with the organization, discussed at meetings with different departments, it was considered to be clear and concise, neither ambiguous nor overly prescriptive, and aligned with the organization's values and mission. The socio‐cultural‐political, or broader ‘real world’, context, is crucial to understanding the how or why of research outcome variability and must be accounted for when embedding research into practice. 26 Localized, specific context is also crucial in exploring why research evidence should be embedded into practice at all, given that leaders can only inspire action for change when teams understand why the change is required. 27
Figure 2.
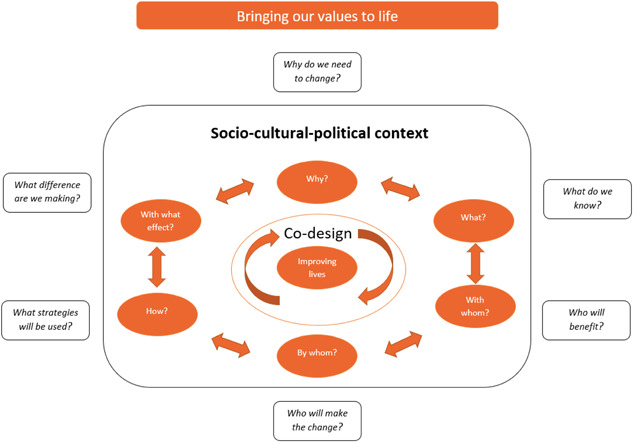
Implementation Framework for Aged Care (IFAC)
At the other end of the spectrum, measuring impact, including short‐ and long‐term outcomes, is critical. As mentioned above, codesign of research, and its implementation into practice, is gaining momentum, identifying and shaping healthcare solutions by the people who are, or may be, directly impacted by the outcomes. 18 , 19 Implementation outcomes, as distinct from dissemination outputs through education and communication, include acceptability (i.e., agreeable or palatable), appropriateness (relevance or compatibility) and feasibility (extent to which it can be successfully used) of interventions. 28 In addition, longer‐term impact is vital, as outlined by the National Health and Medical Research Council, including the influence of research on policy and practice, impact between and within teams, and improvements related to societal participation and the social determinants of health. 29
2.3. Expansion of draft framework components
The third phase of the codesign process was ‘Develop’, whereby the overall IFAC was critically reviewed, each component further scrutinized to ensure its relevance in the IFAC as a whole, and to deepen understanding of its purpose 24 through consultation with implementation science experts.
2.4. Consultation with implementation science experts
Face‐to‐face and online consultative discussions were undertaken with three clinical academic implementation science experts (Professorial level, each with over 25 years' expertise). Their collective feedback informed expansion of the elements of the IFAC through consideration of:
Separation of knowledge generation from implementation, with clear data‐driven questions;
Expansion of the definition of socio‐cultural‐political context;
Articulation of organizational readiness for change;
Prioritization of process evaluation with an emphasis on planning, including theoretical underpinnings with mechanism of action, contextual adaptation and implementation monitoring;
Substantive codesign processes, ensuring representative views of all relevant stakeholders and end knowledge users using various engagement strategies;
Shared goals and shared understanding through relational coordination;
Recognition of, and response to, sustainability at each step, with a reflective process embedded throughout; and
Importance of using other theories, tools and frameworks (from a ‘toolbox’) catering to specific needs, preferences and purposes.
3. RESULTS
3.1. Project/program context
The socio‐cultural‐political context is deliberately depicted in the IFAC as encompassing the iterative, cyclical implementation process. This context is omnipresent, influential to a greater or lesser degree throughout the entire process. Aged care reform has been ongoing for several years, designed to improve quality of care—The Caring for Older Australians report was released by the Productivity Commission in 2011 30 ; the Living Longer Living Better (LLLB) bill passed into legislation in 2013 31 ; the Tune report was an independent review of the LLLB reforms 32 ; and the introduction of mandatory Aged Care Quality Standards in 2019, to name a few. In addition, the 2019–2020 Australian Royal Commission into Aged Care Quality and Safety has prompted further reform across the sector. Aged care providers must respond swiftly to changes at both State/Territory and National levels, with the implementation of research into practice not always the highest priority. Additionally, the context included socially driven campaigns to address ageism, such as EveryAGE Counts 33 and the World Health Organization Global Campaign to Combat Ageism. 34
The Readiness Assessment for Pragmatic Trials (RAPT) model draws attention to alignment with stakeholder priorities as a key factor, 35 which is often related to the broader socio‐cultural‐political context in which implementation will occur. Two recent reviews highlighted the challenge of defining and measuring context, with 12 dimensions crossing micro (individual), meso (organization) and macro (broader aged care landscape) levels. 26 , 36 A standardized approach to context mapping for the IFAC expands on the RAPT model components of alignment (i.e., with external stakeholder priorities), acceptability (i.e., willingness to adopt the intervention), feasibility (i.e., implementing under existing conditions) and cost (i.e., economic viability). 35 These components are included within the final operational checklist for implementation within the provider, Bolton Clarke (see Appendix 1).
3.2. Implementation approach
Codesign is at the heart of implementing evidence into practice and is a way for individuals with different expertise, but similar interests in the outcomes, to work together collaboratively. In a research context, codesign involves all those who may be influenced by the research from design through to dissemination and implementation; and is distinct from conducting research that is to, about or for them. 37 Codesign principles have shifted the paradigm from healthcare experts being the holder of all knowledge, to incorporate valuable knowledge of those receiving and delivering services. 38 Codesign recognizes both explicit (e.g., sourced from literature) and tacit (e.g., insights and experiences) forms of knowledge (e.g., as identified through literature, or clinical guidelines) as complementary, synthesized into new knowledge. 39 , 40 Outputs from a codesign process are likely to be fit‐for‐purpose, acceptable, valuable and enduring. 20 A plethora of frameworks also exist for supporting consumer involvement in research, such that it is suggested organizations choose from a menu of resources rather than relying on a single framework. 41 The Bolton Clarke Research Institute utilizes a combination of the Design Council's Double Diamond Framework 24 and the six‐stage process of ‘engage, plan, explore, develop, decide and change’ as used in New Zealand to plan for improvements to cancer services 18 as per Figure 1. This has also been guided by a Bolton Clarke internal document titled ‘Partnering with Consumers Framework 2018–2025’, which is reflective of the organization's context, purpose and desired outcomes, in accordance with the Partnering with Consumers Standard. 42
3.3. Implementation process
-
1.
Why? One of the most critical questions in gaining the support of the entire team for successful implementation into practice is why do we need to change? There are finite resources within the health and aged care system, and for individual organizations; making it important to understand why we are making a change, if at all. Health and aged care are complex adaptive systems, with complexity science giving insights into ambiguous social practices (i.e., culture), multiple dynamic forces, uncertainty and imprecision that are at the heart of a change process. 13 Competing priorities and pressures must be acknowledged to use limited health and aged care resources most effectively and efficiently. For the purposes of this IFAC, these are categorized into areas affecting: (1) individual older people and their families (e.g., ensuring person‐centred and consumer‐directed care) 43 ; (2) organizational (e.g., ensuring progress toward organizational mission, linked to their espoused values) 44 ; (3) public/community (e.g., upholding societal obligations of a Right to Health) 45 ; (4) regulatory environment (e.g., action planning for inclusive and culturally appropriate services in line with the Aged Care Diversity Framework) 46 and (5) financial considerations (e.g., fiscally adept management of aged care services). Change requires a triggering mechanism, a deep knowing and understanding of why we need to change, so that momentum can be maintained through an often lengthy and intricate process. 13
When unpacking the why in relation to an IFAC, it is also important to consider the distinction between implementation and dissemination. Dissemination involves planned methods (e.g., peer‐review publication and conference presentations) that lead to awareness raising of an evidence‐based intervention, whereas implementation is the process and factors that lead to uptake of the intervention in a particular setting. 47 Not all research needs to be, nor should be, implemented, but if it is to be implemented, then it must be ‘ready to go’, that is, supported by evidence of effectiveness.
-
2.
What? The question of what we need to know focuses attention on whether an intervention/program/tool is ready to be embedded into routine care practice. Evidence is important. Evidence‐based practice that integrates the best available research evidence with clinical expertise and personal preferences and values 48 emphasizes that implicit or tacit knowledge is just as valuable as other more explicit forms of knowledge. Ideally, interventions should be considered efficacious before moving to the next phase of pragmatic testing, with known internal validity under research conditions. 3 Research has historically tended to focus more on the efficacy of interventions (i.e., what works as best practice) with less attention on effectiveness (i.e., what works in practice). 2 In response, there is increasing focus on pragmatic trials, particularly effectiveness‐implementation hybrid designs, 49 with the purpose of moving research into practice in a timely manner (i.e., faster than the estimated 17 years required) to convert 14% of research into patient care. 50 Assessment of each of the nine Readiness for Assessment for Pragmatic Trials (RAPT) domains provide useful guidance, 35 some of which have already been addressed through context mapping above. The remaining domains are assessment of the implementation protocol (i.e., sufficiently detailed to allow replication), evidence (i.e., supportive of efficacy), risk (i.e., understanding intervention safety), measurement (i.e., ensuring capture of outcomes) and impact (i.e., usefulness of results), all of which are included in the operational checklist found in Appendix 1. Additionally, intervention fidelity is a critical consideration, with numerous frameworks available. 51 The core components of an intervention, related to expected outcomes, must be articulated (i.e., components of the intervention that cannot be adapted regardless of the context). 51 , 52
-
3.
With whom?
-
4.
By whom?
Identifying both who will benefit and who will make the change is crucial. Both time and effort are needed to identify all key stakeholders, to understand their roles, motives and required level of engagement/participation for successful implementation. Codesign elements are again prominent in this stage, with implementation informed by a diverse group of stakeholders whom the research evidence impacts. 53 Numerous individuals and organizations benefit from implementation: older people and their carers; frontline health and aged care professionals; organizational management (of various sectors/departments of organizations); local administrators; State/Territory and National policy makers; regulatory bodies; industry bodies; research funders and researchers. Engaging key stakeholders will help to identify the value proposition of the intervention/program/tool; and to develop key messages that will resonate with a variety of audiences. 54 For a aged care organizations, impact of implementation needs to be understood throughout every level of the organization. Support of an executive sponsor is critical, given there are invariably changes to internal policies and procedures necessary for implementation. Importantly, the mere identification of key stakeholders is not sufficient.
To drive implementation, understanding and harnessing stakeholder salience is important to ensure that individuals with the most influence, urgency and legitimacy can best effect change. 55 Implementation research has identified that person/s with established credibility and the necessary skills, experience and attitude, are best placed to implement the targeted change. 10 , 25 This/these person/s will need to be aware of power dynamics and may need to navigate competing or opposing, but equally important, areas. 56 It is crucial for this/these person/s to have an intimate working knowledge of the key areas and have strong relationships with stakeholders so that they are well‐placed to share the evidence for implementation and build capacity as needed to support implementation. 23 , 57 The success of these people as change champions relies not only on what they do but characteristics attributed to who they are, which can aid the selection (e.g., influence, ownership, physical presence, persuasiveness, grit and empathic leadership). 54 , 58 They are not necessarily senior staff, but rather may be representative of a less skilled aged care workforce who are often precluded from initiatives. 59 Mapping stakeholder engagement clarifies the communication and relational requirements necessary to effect change. Questions related to this mapping can be found in the checklist in Appendix 1, with helpful resources from the Victorian Department of Health and Human Services 60 and about Relational Coordination. 61
-
5.
How?
Complexity increases when considering the question of what strategies will be used, essentially how it will be implemented. Likely, multiple methods with multiple personnel will be required. Linkage and exchange efforts, whereby relationships are central, with equal weight placed upon those undertaking implementation and those adopting the implementation, will likely have greater success than purely push strategies (information is pushed to end‐users in various formats) and pull strategies (end‐users seek out and use relevant evidence). 62 , 63
Operationalisation of the IFAC was informed by several theories, including Normalization Process Theory (see Figure 3), to afford a consistent framework that can be used to describe, assess and enhance implementation potential. 64
Normalization Process Theory (NPT): provides the foundational structure for implementation, including the four constructs 21 : (1) coherence (the discovery and sense‐making work, as per the codesign framework outlined above); (2) cognitive participation (the relational work, focused on engaging key stakeholders); (3) collective action (the operational work that people do to enact the intervention) and (4) reflexive monitoring (assessing and understanding how the new intervention affects themselves and others).
-
(1)
Coherence is the sense‐making work that people undertake individually or collectively when faced with operationalising a set of practices.
-
(2)
Cognitive participation is the engagement work required to move evidence into practice. Cognitive participation is heavily influenced by the quality of the relationships between parties and their ability to communicate and function as a team. Relational coordination is an approach, including a mapping exercise, to improving work processes and task integration through communication dimensions (frequent, timely, accurate and problem solving) and relationship dimensions (shared goals, shared knowledge and mutual respect). 61 A change team must be established, including representatives from all stakeholder groups involved in the implementation as outlined above. This change team has the necessary skills and influence to act on the Relational Coordination mapping to improve work processes and task integration through collective action.
-
(3)
Collective action incorporates how people work together, building accountability and confidence in the intervention and each other, and integrating the intervention according to skill levels and context. The Behaviour Change Wheel is key to this component, with its core elements of capability (physical and psychological); opportunity (physical and social) and motivation (automatic and reflective). The principles of the Behaviour Change Wheel have a plethora of ‘active ingredients’ for describing behaviour change techniques that fall under nine categories of: (i) education (e.g., communication/marketing); (ii) persuasion (e.g., guidelines); (iii) incentivisation (e.g., fiscal measures); (iv) coercion (e.g., monitoring and feedback); (v) training (e.g., skill building); (vi) restriction (e.g., legislation); (vii) environmental restructuring (e.g., equipment); (viii) modelling (e.g., demonstration of behaviour) and (ix) enablement (e.g., goal setting and support). 65 Interventions have greater success when underpinned by theory and, in response, the Theoretical Domains Framework (TDF) was developed to guide implementers in theory selection for the most suitable behaviour change techniques. 66 Mapping the barriers and enablers to intervention implementation using the Behaviour Change Wheel, and using these findings to inform the pathway of change using the TDF enables the generation of targeted approaches to pathways of change. 67 Examples of strategies/techniques have been incorporated into the checklist in Appendix 1.
-
(4)
Reflexive monitoring is the final stage, reflecting and evaluating the above components to make a positive difference from implementing evidence into practice as per the next section.
-
(1)
-
6.
With what effect?
Figure 3.

Intersection of several theories to inform the ‘how'
For all stakeholders, formative and summative evaluaiton is critical to answering the question what difference are we making? An implementation outcome taxonomy exists encompassing constructs of: (1) acceptability (i.e., agreeable or palatable); (2) adoption (i.e., uptake of action into practice); (3) appropriateness (i.e., perceived fit and relevance); (4) cost (i.e., accounting for intervention type, implementation strategy and setting); (5) feasibility (i.e., extent to which the intervention can be used in the given setting); (6) fidelity (i.e., degree to which the intervention is implemented as intended); (7) reach/saturation and (8) sustainability (i.e., extent to which the intervention is maintained or embedded into ‘business as usual’). 68 In line with current Australian National Health and Medical Research Council guidelines, ensuring impact, rather than only outputs and short‐term outcomes, is crucial and must be part of an implementation evaluation plan, particularly focusing on health, economic, social and knowledge impact. 29 These constructs have been incorporated into the checklist in Appendix 1.
3.4. Application of the IFAC in three pilot projects in aged care
The ‘Deliver’ phase aimed to apply the IFAC checklist to three Bolton Clarke projects, aligning with the IFAC components and identifying learnings in the implementation process. As mentioned above, the IFAC does not follow a neat linear journey and, as such, the IFAC checklist (Appendix 1) is designed to be flexible for the aged care professionals using it to implement a new evidence‐based intervention into practice. Examples from each of the projects can be seen in Table 1, aligning with the IFAC components and checklist questions, with consideration of the socio‐cultural‐political context and use of codesign principles for each project outlined below.
Table 1.
Application of the IFAC to three project case studies
| IFAC components | IFAC checklist components | Examples from Project 1 by your side | Examples from Project 2 wellness and reablement | Examples from Project 3 Let's Dig In! |
|---|---|---|---|---|
| Why do we need to change? |
Q1: What is the purpose of the implementation? Why is it important? Why should people care? Q6: Is it a priority for the organization? Why? |
The project was initiated in response to an increase in falls rates among home care clientele; a growing focus on reablement for older people; and an organizational imperative to reduce falls in older people receiving home care services. Widespread upscale throughout Bolton Clarke was predicated on having a consistent evidence‐based approach to the management of falls, while enhancing the scope of practice of care workers | This project was instigated in response to the Australian Government directive of a Wellness and Reablement approach throughout all aged care services. Bolton Clarke, as an aged care provider, are mandated to meet the Aged Care Quality Standards. A model of care was developed for Bolton Clarke in response to this directive, to operationalize W&R, with staff required to adopt the principles within their practice | The impetus for change for this project was a care home with an existing garden area that needed revitalization/rehabilitation. Meaningful engagement of residents in care homes is a core tenet of residential care lifestyle programs. The program was created by an enthusiastic lifestyle coordinator who wanted to reestablish a gardening program for her residents, teamed with a highly motivated and physically able resident who had previously worked as a gardener |
| What do we know? | Q2: Which program/tool are you wishing to implement into practice? What evidence is it based upon? | A tried and tested protocol for the Otago Exercise Program was modified for use in this project, underpinned by a strong evidence base, known risks and well‐known outcome measures. Evidence exists for the prevention of falls through exercise, yet older person engagement with exercise is often limited | This project was designed around the evidence‐informed philosophy of Wellness and Reablement (W&R). W&R is a well‐established philosophy, with reablement trials showing some efficacious data. However, there is little guidance for operationalising the approach in practice | This project was designed around the evidence‐informed practice of therapeutic horticulture |
| Who will benefit? |
Q3: In which setting is it to be implemented?Q4 ‐ Who will be involved in the implementation? How will it benefit them? Q5: How will Bolton Clarke, as an organization, benefit? Q7: Who is the Executive sponsor? What are their drivers for supporting the implementation? |
This program was implemented into home care in a region of Melbourne, Australia. An executive sponsor from home care was pivotal, with Bolton Clarke benefiting from a clear framework for the delivery of an exercise‐based intervention for falls prevention. Older people benefit from a program that enhances their functional ability, independence and overall wellbeing, while decreasing their risk of falls. Home care workers benefit by broadening their scope of practice, with greater subjective work satisfaction | This program was implemented into home care across metropolitan and regional areas in Victoria and Queensland, Australia. An Executive sponsor from care innovation was key, with Bolton Clarke benefiting from a model of care that aligned with government mandates. In line with W&R principles, older people benefit from the promotion of independence, being supported to make decisions about what's important to them and how they wish services to be delivered, in alignment with maintaining autonomy and control of their lives. Frontline workers benefit by extending their scope of practice, enhancing independence in the people in their care | This program was implemented into one Bolton Clarke residential aged care home in Queensland, Australia. An Executive sponsor from residential aged care was critical, with Bolton Clarke benefiting through an enhanced lifestyle program attractive to existing and future residents. The residents, staff and volunteers who participate in the gardening program benefit through improved well‐being and satisfaction from meaningful activity/work. Family members of participating residents notice improvements in their loved ones' well‐being and have the garden to look at when they visit. A further benefit is the use of harvested produce to prepare their meals |
| Who will make the change? |
Q4: Who will be involved in the implementation? How will it benefit them? Q12: Which staff roles are likely to be the most appropriate change champions? Q13: Why should others be interested? Q14: Who are the most appropriate individuals for the change team? |
The pilot program was led by a physiotherapist in partnership with care workers and informal carers to support an older person's program participation. For implementation, the change team is led by a program coordinator, responsible for the upskill of all physiotherapists and care workers, while ensuring the logistical support of ancillary staff (e.g., schedulers for home visits). Each region within AHS across Victoria, NSW and Queensland will benefit from a ‘falls champion' | The Principal Advisor for Wellness and Reablement was responsible for the overall management of the project, including development of training materials and resources, conducting training sessions and working closely with the five sites to implement W&R into practice. An important learning from this project was the lack of a ‘change' team, with the enormity of implementing the model of care falling to one key person | The lifestyle coordinator was responsible for the overall coordination of the program, with support from volunteers, the residential manager and a therapeutic horticulturist (e.g., the Soil to Supper program was developed by a certified horticulture therapist with 20 years of experience in garden therapy, including working with people living with dementia). A new Lifestyle Program Manager with a background in research is now leading the delivery of evidence‐based therapeutic interventions in residential aged care. This role involves developing structures and supports to increase uptake of evidence‐based interventions across all of the care homes |
| What strategies will be used? |
Q8: Does the physical environment support the implementation? Q9: Does the workflow environment support the implementation? Q10: Have training needs and processes been established? Q11: Where will information/training resources be located? Q15: What are we asking people to do? Q16: How will we ensure we are respectful of everyone's roles and responsibilities? Q17: How can we help people to change their behaviour? |
Training for care workers was developed using instructional design principles, with learning outcomes clearly articulated. This training is a blend of online and face to face options, designed to enhance the reach of the training, and will eventually be embedded within the onboarding process for new staff. Open and transparent communication between physiotherapists, care workers and management are encouraged. Interviews with older people, care workers and the physiotherapist were used to ascertain feasibility and acceptability of the program | The W&R model of care (developed with subject matter experts) underpinned the development of the training (tailored to various staffing levels and the supporting resources). The training and supporting resources established a consistent and congruent approach, through changing how people work, guiding the use of the ‘My Wellness Plan' template to support person‐centred conversations between staff and older people. In subsequent iterations, this training could be improved by utilizing an instructional designer, skilled in eliciting key learning outcomes for sustainability of the approach and creating an ongoing learning environment. While not yet ideal, reinforcement of the W&R approach was supported by an internal website (holding all necessary resources) and the development of action plans by the five sites for accountability of embedding W&R into practice | Training in horticulture therapy principles was provided to staff and volunteers by the Soil to Supper horticulture therapist. These principles were then supported and monitored by the lifestyle coordinator, who communicated about care/activities with staff during weekly staff meetings. Participants' mobility, strength and balance were assessed. The extent of resident involvement in each session was recorded by the lifestyle coordinator. Residents, staff and volunteers were interviewed to ascertain program feasibility and acceptability |
| With what effect? | Q18: Evaluation methods to consider for measuring impact: AcceptabilityAdoptionAppropriatenessCostFeasibilityFidelityReach/saturationSustainability | Feasibility and acceptability of the pilot program were identified through interviews with key stakeholders (and submitted for publication elsewhere). Program delivery occurred in line with core elements of the Otago Exercise Program to enhance fidelity. Adoption and reach of the program are not yet identified due to the early stage of widespread implementation. A cost analysis is being considered. For sustainability, By Your Side training is to be incorporated into the onboarding process for all new physiotherapists and care workers | Feasibility, appropriateness and acceptability were identified via qualitative methods. For older people, engaging them in the unfamiliar and often frustrating process of goal setting (via the ‘My Wellness Plan' to identify an outcome of importance to them) was difficult. Emphasis is needed on staff knowledge of, skills for and attitudes towards W&R to ensure that goal setting with older people is meaningful and valuable. For sustainability, staff knowledge and understanding of the approach, with ongoing support from a ‘change team', was deemed critical but not fully successful in this project. For longer term sustainability, W&R training is to be incorporated into the onboarding process for all new frontline staff members | Adherence rates were high with, on average, participants attending 10 of 12 (84%) sessions. There were clinically significant improvements in physical function for some participants. Interviews with residents indicated an improvement in subjective well‐being; they felt happier and had a greater sense of purpose and achievement. Interviews with staff and volunteers suggested that the therapeutic horticulture program is feasible and acceptable in care homes. Let's Dig In! was adopted by 19 of the 90 residents of the care home (21%). However, the program reached all residents as the produce harvested from the garden was used to prepare their meals. Fidelity to the program was monitored through following the Soil to Supper principles and aligning with the Spring/Summer program for planting and weekly activities. Let's Dig In! is in its third year of operation at this care home, with a second program started in the dementia care unit. Another six care homes are in the process of establishing a similar program for their residents |
3.5. Project 1: By Your Side: A care worker and virtual physiotherapist led falls prevention program
3.5.1. Project overview
This pilot project recruited 13 older people being supported by home‐based personal care, to participate in a 12‐week falls prevention program based on the Otago Exercise Program. The Otago Exercise Program is effective in reducing the number of falls and fall‐related injuries in high‐risk older people by 35%. 69 , 70 Eight home care workers were trained by a physiotherapist to supervise an individually designed exercise program whilst in the person's home. The physiotherapist was responsible for the initial assessment and development of the exercise program, then provided ongoing support virtually via the home care worker's computer. Physiotherapy assessments, as well as interviews with the exercise participants and the home care workers, were conducted at 8 and 12 weeks.
Socio‐cultural‐political context project execution was episodically impacted by (1) changes to the government funding structures; (2) integration of a new organizational client management system; (3) introduction of the nationwide centralized portal for aged care services (necessitating training as a priority for staff); and (4) care worker case load priorities and scheduling commitments.
3.5.2. Codesign principles
Advisory group consultation flagged client and organizational need in the first instance (‘The Why’). Early in the commencement of the pilot study, a focus group was conducted with four older people to ascertain their views on, and preferences for, various exercise and education content and delivery scenarios (enacted through role play) related to falls prevention.
Key internal stakeholder consultation for implementation of the By Your Side program highlighted the need for a program co‐ordinator, a focus on clients with lower care needs and the upskilling of the entire care worker workforce.
3.6. Project 2: Focus on W&R in‐home support and residential care
3.6.1. Project overview
A W&R approach has been shown to provide numerous benefits for older people, such as improved function, independence, subjective well‐being and quality of life. 71 , 72 , 73 To enable the implementation of a whole of organization evidence‐based W&R approach in home‐based support and residential care, a pilot project was instigated with five specific work groups where staff were to complete and implement a standardized ‘My Wellness Plan’ with older community members. Training was undertaken with 209 staff, including nurses, allied health and personal care workers. Three of the five work groups completed the project, with 18 older people and eight staff interviewed at program completion.
3.6.2. Socio‐cultural‐political context
This project was conducted amidst several external contextual factors that impacted its success: (1) a Royal Commission into Aged Care Quality and Safety; (2) introduction of new mandatory Aged Care Quality Standards and (3) an organizational restructure.
3.6.3. Codesign principles
Implementation of this project was codesigned from the outset via a full‐day planning workshop with key executive and operational management representatives and the ‘change champions’ of the five implementation sites (in metropolitan, regional and rural/remote areas). To ensure the generalizability of the program, the project reference group included staff from clinical, personal care and administrative areas of the business. ‘The Why’ of needing intervention implementation within the organization was understood and confirmed by all, and they determined: (1) appropriate areas of Bolton Clarke for W&R implementation; (2) managerial knowledge and experience of W&R to aid implementation (3) program funding available to deliver the W&R program.
The project materials were also codesigned—W&R principles were developed with key staff members and the ‘My Wellness Plan’ template was developed with a group of community members who form the organization's Community Partnership Group to ensure applicability for users of the materials.
3.7. Project 3: Let's dig in! A therapeutic horticulture pilot program for residential care
3.7.1. Project overview
The growing evidence‐based recognition of the therapeutic value of horticultural and nature‐based activities for individuals in residential aged care 74 prompted the trial of the Let's Dig In! program in an individual care home. The 12‐week program focused on enablement and the promotion of well‐being through a weekly gardening program. Ten residents participated in the program plus assessment of functional capacity pre‐ and postprogram. Seven residents were interviewed at the completion of the program to explore their perceptions of the program.
3.7.2. Socio‐cultural‐political context
Meaningful engagement is a central tenet of residential care home activity programs to promote active participation and optimal wellbeing. For people with cognitive impairment or dementia, this is particularly important to reduce the behavioural and psychological symptoms of dementia. A new activity or program must be integrated into an environment that is often besieged by inadequate staffing levels and skill mix, and unannounced visits for assessment and auditing purposes by the aged care regulator, as outlined in the recent findings of the Royal Commission into Aged Care Quality and Safety. 75
3.7.3. Codesign principles
Codesign of the existing Let's Dig In! program firstly involved all participants recognizing ‘The Why’, followed by focus around the activity delivery for each session. The choice of which herbs and vegetables to plant aligned with, and were modified for, care home resident needs, preferences, and characteristics. The program delivery also accounted for and was adapted to, the local environment, climate and materials.
3.7.4. Learnings from the project case studies
The three project case studies were implemented with varying success, and highlight crucial aspects that were missing during implementation, showcasing important learnings collated in Table 2. NPT, as depicted in Figure 3, provides a structure to contextualize these learnings.
Table 2.
Collated learnings from the three projects
| IFAC component | Collated learnings to inform IFAC |
|---|---|
| Socio‐cultural political context | Comprehensive contextual mapping to be undertaken to understand the internal and external pressures and priorities that may influence implementation. This will ensure that the intervention is acceptable and feasible to all stakeholders, resulting in a strong commitment to the implementation and necessary contingencies in place. With an ongoing iterative codesign methodology, contextual mapping can recur as required throughout the project, given that the aged care landscape can change rapidly. Clear articulation of alignment of the implementation with internal organizational priorities is key, with transparent, timely and actionable decision‐making authority should priorities change |
| Codesign principles | Codesign sessions to be conducted with all key stakeholders, rather than a subset, from the outset of the implementation to identify and pre‐empt potential barriers and challenges. Within an aged care provider, this may include representation from clinical, operational, information technology, learning and development, people and culture and marketing arms of the business. Critically, older people are included as key stakeholders. Codesign is to be an iterative process over time to allow for identification and rectification of errors as distinct from only stakeholder consultation at project commencement. Engagement with executive and operational management to occur early and repeatedly over the course of the implementation. Promotion of an inclusive codesign process will ensure that sessions are accessible to all participants—physically, financially and informational (e.g., access to technology, microphones, large print materials and interpreters) |
| Why do we need to change? | Clear articulation and communication of why a change is to be instigated will ensure that all key stakeholders are engaged with the implementation from the outset. The why is to be transparent and enduring, requiring ongoing commitment from all key stakeholders. A communication strategy in line with the implementation plan can maintain the visibility of the why |
| What do we know? | A program, product or tool should ideally have supportive efficacy data before being embedded into practice. An evidence‐informed program is not sufficient on its own even with efficacy data from explanatory trials. For implementation to be effective, evidence‐informed programs must be ready to be embedded into practice |
| Who will benefit? | Older people will benefit from programs, products or tools that enhance their physical, psychological and social well‐being. Frontline staff and operational management will benefit from enhanced work processes, task integration and team relationships. The organization as a whole will be more effective and efficient, as well as an employer and provider of choice |
| Who will make the change? | A skilled project manager is responsible for overall coordination of the implementation plan, liaising with subject matter experts, consumers and executive/operational teams as required. A ‘change team' is crucial to support the project manager in successful implementation, including people who have the appropriate mix of skills, influence, physical presence and personality traits |
| What strategies will be used? | Coherence (sense making) occurred through codesign to varying degrees and is a crucial upfront component. Relational coordination was not used within the projects in a formalized manner, but clearly, quality relationships and the ability to function as a team is vital. Behaviour change techniques were utilized, focused on capability (e.g., training of staff for all three projects), opportunity (e.g., staff chosen to be the early adopters of Wellness & Reablement) and motivation (e.g., care workers supported by management to extend their scope of practice for By Your Side) |
| What difference are we making? | This section is about impact—health, economic, social and knowledge impact, encompassing constructs of acceptability; adoption; appropriateness; cost; feasibility; fidelity; reach/saturation; and sustainability |
Coherence (sense making) aligns with the IFAC components of the socio‐cultural‐political context and codesign principles. Contextual mapping was undertaken at the commencement of each of the projects, but this did not result in success, as, like any complex system, there was continuing change throughout the programs during implementation. An iterative process throughout would have identified the changing external landscape and organizational priorities earlier, with greater chance of successful adaptation. The relational work, as identified in NPT, was again completed relatively well at the commencement of the projects, but lost momentum throughout. This component is arguably the most important, relying on strong, transparent and enduring relationships with a ‘change’ team comprising people with the necessary skills, influence and personality. The operational work through collective action was consistent throughout the projects but was perhaps overly reliant on key team members. Again, a ‘change’ team would ensure that the burden of operational work does not fall on the shoulders of a few individuals. Evaluation of the implementation was undertaken with varying success, likely to be enhanced in the future by considering all aspects of impact. Reflection on the entire implementation process is critical and yet is often poorly executed due to the pressure of the next competing priority.
4. DISCUSSION
Implementation science aims to move evidence into practice and, as we have learnt over the past years, this is far from a simple linear process. Complexity science provides a more comprehensive lens through which to understand the interconnections in complex, dynamic health and aged care systems. 13 The development of the IFAC was heavily influenced by existing theory, but has been represented visually in a simple, understandable format, easily identifiable by all arms of the Bolton Clarke business. An implementation checklist (Appendix 1) ensures that the complexity is in digestible format to allow the IFAC to be operationalized.
Older people who are clients or residents within aged care services often have high care needs, with multimorbidity and psychosocial issues prevalent. Addressing these challenges through implementing evidence‐informed practice is enhanced using a complexity lens, whereby we acknowledge the messiness, better understand contextual factors and use different mechanisms for change in different circumstances. The learnings from the three project case studies (as seen in Table 2) highlight the importance of contextual mapping using codesign methodology, clear articulation of why change is needed, a ‘change team’ with the necessary skills and influence, and evaluation measures focused on impact.
Even with this approach, there is additional work required to enable successful implementation:
-
1.
In the current aged care context of this organization, there is limited understanding by key decision makers as to the time required to undertake implementation, particularly the preparatory time and ongoing support needed for intervention/activity delivery into practice. More work is needed to increase awareness that new interventions do not ‘just happen’ so that there is recognition and support for the required resources (time and staffing levels) crucial for successful implementation.
-
2.
Codesign, albeit a crucial aspect to effective implementation, is time‐consuming and resource intensive. Mechanisms of backfill for clinical roles is crucial for this component, but the aged care sector does not currently have an adequate workforce to enable this.
-
3.
Development of a learning organization, whereby all stakeholders are engaged in ongoing care delivery improvements, is a challenge within aged care. This is due to both resource constraints, and workplace culture, whereby work undertaken by aged care providers is insufficiently valued, with limited research efforts to support the advancement of care delivery.
5. CONCLUSION
Implementation of evidence into practice is challenging, yet crucial. Numerous theories, models and frameworks exist, but each have their limitations for the purposes of the aged care environment. This article has conceptualized key elements from the implementation science literature into a draft framework, expanded these elements through consultation and application to existing projects. A fit‐for‐purpose framework (the IFAC) has been consolidated, underpinned by several existing theories. Further, the checklist allows for the complexity of the IFAC to be operationalized within community and residential aged care.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
All authors have contributed to the conception or design of the work and/or the acquisition, analysis and interpretation of data for the work. All authors have assisted in drafting the work or revising it critically for important intellectual content.
Supporting information
Supporting information.
Supporting information.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the contribution of Professor Gillian Harvey and Professor Anneke Fitzgerald for their input in ascertaining the relevance of the Implementation Framework for the aged care sector.
Meyer C, Ogrin R, Golenko X, et al. A codesigned fit‐for‐purpose implementation framework for aged care. J Eval Clin Pract. 2022;28:421‐435. 10.1111/jep.13660
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Glasgow R, Vinson C, Chambers D, Khoury M, Kaplan R, Hunter C. National Institutes of Health Approaches to Dissemination and Implementation Science: current and future directions. Am J Public Health. 2012;102(7):1274‐1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Green L. From research to “best practices” in other settings and populations. Am J Health Behav. 2001;2(3):165‐178. [DOI] [PubMed] [Google Scholar]
- 3. Mitchell S, Mor V, Harrison J, McCarthy E. Embedded pragmatic trials in dementia care: realizing the vision of the NIA IMPACT collaboratory. J Am Geriatr Soc. 2020;68(S1‐S7):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Greenhalgh T, Wherton J, Papoutsi C, et al. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale‐up, spread, and sustainability of health and care technologies. J Med Internet Res. 2017;19(11):e367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nordstrum L, LeMahieu P, Berrena E. Implementation science: understanding and finding solutions to variation in program implementation. Quality Assurance in Education. 2017;25(1):58‐73. [Google Scholar]
- 6. Theobald S, Brandes N, Gyapong M, et al. Implementation research: new imperatives and opportunities in global health. Lancet. 2018;392(10160):2214‐2228. [DOI] [PubMed] [Google Scholar]
- 7. Salignac F, Wilcox T, Marjolin A, Adams S. Understanding collective impact in Australia: a new approach to interorganizational collaboration. Aust J Manag. 2018;43(1):371. [Google Scholar]
- 8. Rapport F, Smith J, Hutchinson K, et al. Too much theory and not enough practice? The challenge of implementation science application in healthcare practice. J Eval Clin Pract. 2021;1‐12. [DOI] [PubMed] [Google Scholar]
- 9. Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006;26(1):13‐24. [DOI] [PubMed] [Google Scholar]
- 10. Grimshaw J, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. 2012;7(50):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bayliss E, Edwards A, Steiner J, Main D. Processes of care desired by elderly patients with multimorbidities. Fam Pract. 2008;25(4):287‐293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Berntsen G, Strisland F, Malm‐Nicolaisen K, Smaradottir B, Fensli R, Rohne M. The evidence base for an ideal care pathway for frail multimorbid elderly: combined scoping and systematic intervention review. J Med Internet Res. 2019;21(4):e12517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Braithwaite J, Churruca K, Long J, Ellis L, Herkes J. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med. 2018;16(63):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sturmberg J, Getz L, Stange K, Upshur R, Mercer S. Beyond multimorbidity: what can we learn from complexity science? J Eval Clin Pract. 2021;27:1187‐1193. [DOI] [PubMed] [Google Scholar]
- 15. Productivity Commission. Caring for Older Australians Australian Government; 2011. [Google Scholar]
- 16. Aged Care Quality and Safety Commission . Guidance and resources for providers to support the Aged Care Quality Standards. Aged Care Quality and Safety Commission; 2018. [Google Scholar]
- 17. Australian Government. Royal Commission into Aged Care Quality and Safety. Vol 2020. Australian Government; 2018. [Google Scholar]
- 18. Boyd H, McKernon S, Mullin B, Old A. Achieving successful community engagement: a rapid realist review. N Z Med J. 2012;125(1357):76‐87. [PubMed] [Google Scholar]
- 19. De Weger E, Van Vooren N, Luijkx K, Baan C, Drewes H. Achieving successful community engagement: a rapid realist review. BMC Health Serv Res. 2018;18(1):285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Greenhalgh T, Jacson C, Shaw S, Janamian T. Achieving research impact through co‐creation in community‐based health services: literature review and case study. Milbank Q. 2016;94(2):392‐429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. May CR, Mair F, Finch T, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci. 2009;4(29):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Moullin JC, Dickson KS, Stadnick NA, et al. Ten recommendations for using implementation frameworks in research and practice. Implement Sci Commun. 2020;1(42):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ward V, House A, Hamer S. Knowledge brokering: the missing link in the evidence to action chain? Evid Policy. 2009;5(3):267‐279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Design Council. Design methods for developing services. Design Council; 2015. [Google Scholar]
- 25. Lavis J, Robertson D, Woodside J, McLeod C, Abelson J. How can research organizations more effectively transfer research knowledge to decision makers? Milbank Q. 2003;81(2):221‐248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. 2019;19(189):123‐157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sinek S. Start with why. Penguin Books Ltd; 2011. [Google Scholar]
- 28. Weiner BJ, Lewis CC, Stanick C, et al. Psychometric assessment of three newly developed implementation outcome measures. Implement Sci. 2017;12(108):108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. National Health and Medical Research Council . Research impact; 2020. Accessed May 2021. https://www.nhmrc.gov.au/research-policy/research-translation-and-impact/research-impact
- 30. Productivity Commission . Caring for Older Australians; 2011.
- 31. Aged Care (Living Longer Living Better) Act, 76 (2013).
- 32. Tune D. Legislated Review of Aged Care. Department of Health; 2017. [Google Scholar]
- 33. Benevolent Society . Every AGE Counts campaign. 2019; Accessed September 2020. https://www.everyagecounts.org.au/
- 34. WHO. Global Report on Ageism. World Health Organization; 2021. [Google Scholar]
- 35. Baier R, Jutkowitz E, Mitchell S, McCreedy E, Mor V. Readiness assessment for pragmatic trials (RAPT): a model to assess the readiness of an intervention for testing in a pragmatic trial. BMC Med Res Methodol. 2019;19:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rogers L, De Brun A, McAuliffe E. Defining and assessing context in healthcare implementation studies: a systematic review. BMC Health Serv Res. 2020;20(591):156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. National Institute for Health Research . Co‐Design; 2021. Accessed May 2021. https://www.invo.org.uk/
- 38. Dimopoulos‐Bick T, Dawda P, Maher L, Verma R, Palmer V. Experience‐based co‐design: tackling common challenges. J Health Design. 2018;3(1):86‐93. [Google Scholar]
- 39. Bennett G. The Knowledge Translation Toolkit: Bridging the Know‐do Gap: A Resource for Researchers. SAGE Publications; 2011. [Google Scholar]
- 40. Rynes S, Bartunek J, Daft R. Across the great divide: Knowledge creation and transfer between practitioners and academics. Acad Manag J. 2001;44:340‐355. [Google Scholar]
- 41. Rynes SL, Bartunek JM, Daft RL. Frameworks for supporting patient and public involvement in research: systematic review and co‐design pilot. Health Expect. 2019;22:785‐801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Australian Commission on Safety and Quality in Healthcare . Partnering with Consumers Standard; 2018. Accessed September 2020. https://www.safetyandquality.gov.au/standards/nsqhs-standards/partnering-consumers-standard
- 43. Pascale K. The Goal Directed Care Planning Toolkit: Practical Strategies to Support Effective Goal Setting and Care Planning with HACC Clients. Eastern Metropolitan Region Home and Community Care Alliance, Outer Eastern Health and Community Services Alliance; 2015. [Google Scholar]
- 44. Fox J. How to Lead a Quest: A Guidebook for Pioneering Leaders. John Wiley & Sons Ltd; 2016. [Google Scholar]
- 45. WHO . Social Determinants of Health: The Solid Facts. World Health Organization; 2003. [Google Scholar]
- 46. Department of Health . Shared Actions to Support All Diverse Older People: A Guide for Aged Care Providers. Australian Government; 2019. [Google Scholar]
- 47. Holtrop J, Rabin B, Glasgow R. Dissemination and implementation science in primary care research and practice: contributions and opportunities. J Am Board Fam Med. 2018;31(3):466‐478. [DOI] [PubMed] [Google Scholar]
- 48. Sackett D, Rosenberg W, Gray J, Haynes R, Richardson W. Evidence based medicine: what it is and what it isn't. Br Med J. 2000;312(71):466‐478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Curran G, Bauer M, Mittman B, Pyne J, Stetler C. Effectiveness‐implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217‐226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Weingarten S, Garb C, Blumenthal D, Boren S, Brown G. Improving preventive care by prompting physicians. Arch Intern Med. 2000;160:301‐308. [DOI] [PubMed] [Google Scholar]
- 51. Balas EA, Weingarten S, Garb CT, Blumenthal D, Boren SA, Brown GD. Focusing on fidelity: narrative review and recommendations for improving intervention fidelity within trials of health behaviour change interventions. Health Psychol Behav Med. 2020;8(1):132‐151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ibrahim S, Sidani S. Fidelity of intervention implementation: a review of instruments. Health. 2015;7:1687‐1695. [Google Scholar]
- 53. NIHR. UK Standards for Public Involvement: Better Public Involvement for Better Health and Social Care Research. National Institute for Health Research; 2019. [Google Scholar]
- 54. Miech E, Rattray N, Flanagan M, Damschroder L, Schmid A, Damush T. Inside help: An integrative review of champions in healthcare‐related implementation. SAGE Open Med. 2018;6:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mitchell R, Lee J, Agle B. Stakeholder prioritization work: The role of stakeholder salience in stakeholder research. In: Wasieleski D, Weber J, eds. Stakeholder Management. Emerald Publishing Limited; 2017. [Google Scholar]
- 56. Knight C, Lyall C. Knowledge brokers: the role of intermediaries in producing research impact. Evid Policy J Res Debate Prac. 2013;9(3):309‐316. [Google Scholar]
- 57. Armstrong R, Waters E, Dobbins M, Lavis J, Petticrew M, Christensen R. Knowledge translation strategies for facilitating evidence‐informed public health decision making among managers and policy‐makers. Cochrane Database Syst Rev. 2011;9(6):CD009181. [Google Scholar]
- 58. Bonawitz K, Wetmore M, Heisler M, et al. Champions in context: which attributes matter for change efforts in healthcare? Implement Sci. 2020;15(62):62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Scales K, Bailey S, Middleton J, Schneider J. Power, empowerment, and person‐centred care: using ethnography to examine the everyday practice of unregistered dementia care staff. Sociol Health Illn. 2017;39(2):227‐243. [DOI] [PubMed] [Google Scholar]
- 60. Department of Health and Human Services . Stakeholder Engagement Toolkit. Victorian Government; 2018. [Google Scholar]
- 61. Relational Coordination Analytics . Relational Coordination Theory; 2021; Accessed March 2021. http://rcanalytic.com/rctheory/
- 62. Lavis JN. Research, public policymaking and knowledge translation processes: Canadian efforts to build bridges. J Contin Educ Health Prof. 2006;26(1):37‐45. [DOI] [PubMed] [Google Scholar]
- 63. WHO . Knowledge Translation on Ageing and Health: A Framework for Policy Development. World Health Organization; 2012. [Google Scholar]
- 64. Murray E, Treweek S, Pope C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med. 2010;8(63):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Michie S, van Stralen M, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(42):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Cane J, O'Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7(37):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Cane J, O'connor D, Michie S. Developing theory‐informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci. 2012;7(38):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. French SD, Green SE, O'connor DA, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges and research agenda. Adm Policy Ment Health. 2011;38:65‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Campbell AJ, Robertson MC, Gardner MM, Norton RN,Buchner DM. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age & Ageing. 1999;28(6):513‐518. [DOI] [PubMed] [Google Scholar]
- 70. Robertson MC, Campbell AJ, Gardner MM, Devlin N. Preventing injuries in older people by preventing falls: a meta‐analysis of individual‐level data. J Am Geriatr Soc. 2002;50(5):905‐911. [DOI] [PubMed] [Google Scholar]
- 71. Kus S, Müller M, Strobl R, Grill E. Patient goals in post‐acute geriatric rehabilitation: goal attainment is an indicator for improved functioning. J Rehabil Med. 2011;43(2):156‐161. [DOI] [PubMed] [Google Scholar]
- 72. Levack WMM, Weatherall M, Hay‐Smith EJC, Dean SG, McPherson K, Siegert RJ. Goal setting and strategies to enhance goal pursuit for adults with acquired disability participating in rehabilitation. Cochrane Database Syst Rev. 2015;43(7):156‐161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. World Health Organization . World Report on Ageing and Health. World Health Organization; 2015. [Google Scholar]
- 74. Gagliardi C, Piccinini F. The use of nature–based activities for the well‐being of older people: an integrative literature review. Arch Gerontol Geriat. 2019;83:315‐327. [DOI] [PubMed] [Google Scholar]
- 75. Australian Government . Royal Commission into Aged Care Quality and Safety. 2020; Accessed September 2020. https://agedcare.royalcommission.gov.au/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


