Abstract
Purpose
The World Health Organization is developing a Package of Eye Care Interventions (PECI) to support the integration of eye health care into national health programmes. Interventions included in the PECI should be based on robust evidence where available. Refractive error is a leading cause of blindness and vision impairment and is a PECI priority condition. The aim of this study was to provide high‐quality evidence to support the development of the PECI by identifying and critically appraising clinical practice guidelines (CPGs), and extracting recommendations for refractive error interventions.
Methods
We searched for CPGs on refractive error published in the last 10 years. We conducted the searches initially in February and March 2019 and repeated them in March 2020. We evaluated the quality of potentially relevant guidelines using the Appraisal of Guidelines for Research and Evaluation (AGREE) II tool.
Results
We identified 12 high‐quality CPGs relevant to refractive error, written by six organisations from three high‐income countries. Organisations used a variety of frameworks to assess the strength of recommendations based on available evidence, with the Grading of Recommendations Assessment, Development and Evaluation (GRADE) being most common. Vision screening for children aged 3 to 5 years was recommended consistently. Evidence for screening and eye evaluations at other ages was weaker, although ophthalmic professional organisations consistently recommended regular evaluations. Recommendations on optical and laser correction of refractive error were limited and did not consider implications for low resource settings. Interventions for slowing myopia progression in children were recommended, but these will need regular updating as new evidence emerges.
Conclusions
Current high‐quality guidelines on refractive error have been formulated in high‐income countries. Recommendations focused on prevention and treatment of refractive error in low‐and middle‐income countries are lacking. Regular updating of systematic reviews and CPGs is essential to ensure that robust evidence is promptly appraised and incorporated into recommendations for eye health care practitioners.
Keywords: clinical practice guidelines, refractive error
Key points.
The World Health Organization is developing a Package of Eye Care Interventions to support the integration of eye health care into national health programmes.
Recommendations from 12 high‐quality clinical practice guidelines on refractive error provide evidence to support the development of the Package of Eye Care Interventions.
Clinical practice guidelines applicable to a broader range of settings are required, and these guidelines need to be regularly updated to support effective and equitable delivery of eye health care.
INTRODUCTION
In 2015, the United Nations General Assembly adopted the 2030 Agenda for Sustainable Development with the overarching aim to end poverty, protect the planet and ensure prosperity for all. 1 Goal 3 of the 17 Sustainable Development Goals aims to “ensure healthy lives and promote well‐being for all ages” and identifies Universal Health Coverage (UHC) as a key requirement to achieve this.
The World Health Organization (WHO) World Report on Vision draws attention to the increasing need for eye care and identifies that eye care must become an integral part of UHC in order to address the inequities in access to, and provision of, eye care services across populations. 2 To facilitate this integration, WHO is developing a package of eye care interventions (PECI) to be used by countries to plan, budget and integrate eye‐care interventions into national health services, packages and policies. 3 An important principle of the PECI is that the choice of interventions should be based on robust evidence where available.
Uncorrected refractive error is one of the leading causes of blindness and vision impairment in the world. In 2020 an estimated 3–4 million people were blind due to uncorrected refractive error and between 140 and 175 million people were vision impaired. 4 These figures are expected to increase substantially in the coming decades due to population aging (presbyopia) and lifestyle factors (myopia). 5 , 6 Uncorrected refractive error poses a substantial economic burden; annual global productivity losses associated with vision impairment from uncorrected myopia and presbyopia alone have been estimated to be US$ 244 billion and US$ 25.4 billion, respectively. 7 , 8
We aimed to identify the best available evidence on eye care interventions for refractive error from a systematic review of high‐quality clinical practice guidelines (CPGs) to help inform the development of the PECI with respect to refractive error interventions.
METHODS
This report follows the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) reporting guidelines (Appendix S1). 9 A protocol was prepared prior to starting the project (Appendix S2). The experience gained from this work was used to develop the protocol for the development of the PECI. 3
We searched bibliographic databases, guideline databases and professional society websites for clinical practice guidelines (CPGs), using pre‐defined selection criteria (Table 1) and search strategies as set out in Table S1. We limited searches to the last 10 years and English language reports. We followed a two‐step process with screening of titles and abstracts followed by scrutiny of the full text of potentially relevant guidelines. All screening was completed by two authors independently and conflicts resolved by discussion. The searches were conducted initially in March 2019 and repeated in March 2020. 3 A top‐up search of the guideline databases in October 2021 did not identify any further updated guidelines relevant to this topic.
TABLE 1.
Selection criteria
| Item | Criteria for inclusion |
|---|---|
| Clinical practice guideline | Institute of Medicine definition: “statements that include recommendations, intended to optimise patient care, that are informed by a systematic review of evidence and an assessment of the benefits and harms of alternative care options” 12 |
| Type of participants | People with refractive error including myopia, hyperopia, astigmatism, presbyopia and anisometropia. There were no restrictions on the population considered: all ages and all locations. |
| Type of intervention | All interventions for refractive error, including interventions related to the identification of refractive error, for example, vision screening. |
| Date of publication | From 2010 onwards |
| Conflict of interest | No commercial funding and no unmanaged conflicts of interest; affiliations of all authors available. |
| Recommendations | Information available on the strength of the recommendations |
| Quality | AGREE II: average score of 3 for items 4, 7, 12, 22 and the overall average score for each of nine items of 4, 7, 8, 10, 12, 13, 15, 22, 23 was 45 or more |
AGREE II: Appraisal of Guidelines for Research and Evaluation II.
Two authors independently evaluated the quality of potentially relevant guidelines using the Appraisal of Guidelines for Research and Evaluation II (AGREE II) tool. 10 Conflicts were resolved by discussion. Criteria developed by the WHO Package of Rehabilitation Interventions were used to assess whether the CPG was of sufficient quality. 11 Specifically, we included CPGs where the average score was 3 or more for four key items: the guideline development group included individuals from all relevant professional groups (item 4); systematic methods were used to search for evidence (item 7); there was an explicit link between the recommendations and supporting evidence (item 12) and the views of the funding body had not influenced the content of the guidelines (item 22). In addition, we required an average sum score for nine selected items (set out in Table S2) to be 45 or more. For each included guideline, we calculated an overall mean domain score following the methods set out in the AGREE II manual. 10
We used a pre‐piloted standardised form for data extraction and collected standardised information on the guideline, adapted from the Reporting Items for practice Guidelines in HealThcare (RIGHT) checklist (Appendix S3) 13 : information on the recommendations (type of recommendation, dosage, target group, etc.), strength of the recommendations, and quality of the evidence supporting the recommendation. We used the same terminology to describe the recommendations as used in the guideline reports. The terms ‘screening’, ‘evaluation’ and ‘examination’ were used in the guidelines but were not defined explicitly in any of the reports. We have used eye evaluations as a general term encompassing both examinations and screening.
RESULTS
The results of the searches are summarised in Figure 1. We screened 1563 records identified from the electronic searches. On screening of titles and abstracts, 1515 of these reports did not meet the inclusion criteria or were duplicates, leaving 48 reports that we considered potentially relevant. We excluded 36 reports on full‐text screening for the following reasons: not a guideline or not relevant to refractive error (23 reports); no information on the strength of recommendation (7); significant conflict of interest (2); insufficient quality (2) and full text not available (2).
FIGURE 1.
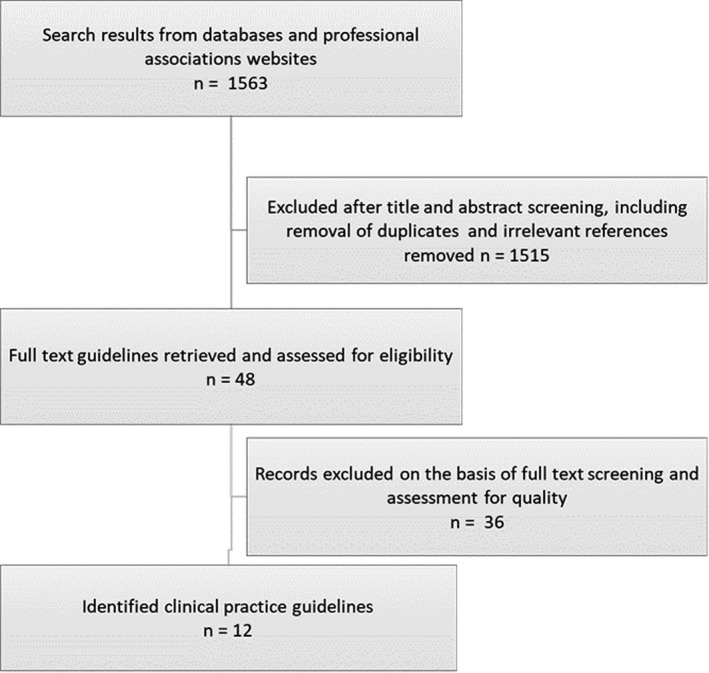
Results of the screening process.
We included 12 guidelines that met the inclusion criteria (Table 2). These guidelines broadly fell into two groups covering assessment (eight guidelines) and treatment (four guidelines). For assessment, five guidelines considered vision screening, 14 , 15 , 16 , 17 , 18 three in children 14 , 15 , 16 and two in adults. 17 , 18 Three guidelines considered some form of comprehensive medical eye evaluation, two in adults 19 , 20 and one in children. 21 The comprehensive medical eye evaluations guidelines were directed at optometrists 19 , 21 and ophthalmologists. 22 The intervention guidelines covered optical, pharmacological, laser and surgical treatments for refractive error. 23 , 24 , 25 , 26
TABLE 2.
Clinical practice guidelines for refractive error
| Guideline title | Organisation, Country | Publication date | |
|---|---|---|---|
| Children | |||
| 1 | Child vision screening | National Screening Committee, UK | 2013 |
| 2 | Vision screening in children aged 6 months to 5 years | US Preventive Services Taskforce, USA | 2017 |
| 3 | Comprehensive pediatric eye and vision examination | American Optometric Association, USA | 2017 |
| 4 | Pediatric eye evaluations: preferred practice pattern | American Academy of Ophthalmology, USA | 2017 |
| Adults | |||
| 5 | Comprehensive adult eye and vision examination | American Optometric Association, USA | 2015 |
| 6 | Comprehensive adult medical eye evaluation: preferred practice pattern | American Academy of Ophthalmology, USA | 2015 |
| Older adults | |||
| 7 | Corneal inlay implantation for correction of presbyopia (IPG455) | National Institute for Health and Care Excellence (NICE), UK | 2013 |
| 8 | Impaired visual acuity in older adults: screening | US Preventive Services Task Force, USA | 2016 |
| 9 | Screening for impaired visual acuity and vision‐ related functional limitations in adults 65 years and older in primary health care | Canadian Task Force on Preventive Health Care, Canada | 2018 |
| Age not specified | |||
| 10 | Intraocular lens insertion for the correction of refractive error with preservation of the natural lens (IPG289) | NICE, UK | 2009 |
| 11 | Laser correction of refractive error following non‐refractive ophthalmic surgery (IPG385) | NICE, UK | 2011 |
| 12 | Refractive errors & refractive surgery: preferred practice pattern | American Academy of Ophthalmology, USA | 2017 |
The selected guidelines were developed by six different organizations in three countries: the Canadian Task Force on Preventive Health Care in Canada; the National Institute for Health and Care Excellence (NICE) and National Screening Committee (NSC) in the UK and the American Academy of Ophthalmology (AAOphth), American Optometric Association (AOA) and US Preventive Services Taskforce (USPSTF) in the USA. The AGREE II domain scores are in Table S3.
The guidelines used a variety of different frameworks to develop recommendations. The most commonly used framework was the GRADE (Grading of Recommendations, Assessment, Development and Evaluations) approach, 27 which was used by the American Academy of Ophthalmology and the Canadian Task Force on Preventive Health Care. 18 , 20 , 22 , 26 GRADE offers two strengths of recommendation, strong and weak, based on judgements of the balance between desirable and undesirable outcomes, certainty in the size of the effect estimate, values and preferences. USPSTF used a similar approach to grade the certainty of the evidence regarding net benefit 16 , 17 as high, moderate or low, and provides potential recommendations (offer or provide this service, offer or provide this service for selected patients depending on individual circumstances, discourage use of this service) depending on the evidence of net benefit. They also have a category for “insufficient evidence”. Similar to USPSTF, NICE make four types of recommendations for interventional procedures guidance: standard arrangements, special arrangements, only in research or do not use. 23 , 24 , 25 The strength of the recommendation is based on the certainty of the available evidence and safety and effectiveness of the procedure. The AOA had three recommendation levels based on the quality of the evidence: strong recommendation, recommendation and consensus recommendation. 19 , 21
The recommendations are shown in full in Table S4.
Vision screening
We identified four different recommendations on vision screening from three guidelines. 16 , 17 , 18 The USPSTF recommended vision screening at least once in all children aged 3–5 years inclusive to detect amblyopia or its risk factors (including anisometropia). The recommendation was considered high certainty of net benefit i.e., the available evidence was judged sufficient. Although a number of different screening tests were mentioned in the report, the results were not disaggregated by type of test. In contrast, at younger ages (before the age of 3 years), the USPSTF concluded the evidence was insufficient to recommend vision screening. The USPSTF was used as a basis for recommendations on vision screening for other guidelines, for example, the AAOphth, which recommended instrument‐based screening every 1–2 years 22
Two guidelines made recommendations on vision screening in people aged 65 years and above. 17 , 18 The USPTSF concluded that the current evidence was insufficient to assess the balance of benefits and harms of screening for impaired visual acuity in older adults and the Canadian Task Force of Preventive Health Care gave a weak recommendation against screening based on low‐quality evidence.
Eye examinations
There were 12 recommendations on eye examinations from four US‐based guidelines, two orientated for ophthalmologists 20 , 22 and two for optometrists. 19 , 21 These guidelines each recommended some form of eye examination for infants, pre‐school children, school‐age children and adults. There were differences, however, in the specified type, targeted population and frequency of that examination. For example, the AAOphth recommended a comprehensive examination only for children who either fail vision screening, have subjective visual symptoms and/or have personal or familial risk factors for eye disease. In contrast, the AOA recommended comprehensive eye examinations for all children before school entry and annually thereafter. Both the AAOphth and AOA recommended eye examinations for adults, albeit with differing frequencies (AAOphth: 5–10 yearly for age <40 years, 2–4 yearly for 40–54 years old, 1–3 yearly for 55–64 years old, and 1–2 yearly for ≥65 years; AOA: at least every 2 years for age <65 years, annually for age ≥65 years). Although many of these recommendations were “strong”, it was notable that they were largely based on consensus statements rather than evidence as such.
Interventions
Optical correction for refractive error
Specific recommendations on use of spectacles and contact lenses were rare but were implicit in all the guidelines. One guideline gave specific guidelines for refractive correction in infants and young children, 22 and one guideline highlighted the increased risk of corneal infections with overnight contact lens wear. 26
Laser and surgical interventions for refractive error
Six recommendations from four guidelines 23 , 24 , 25 , 26 addressed laser and surgical interventions for refractive error. LASEK, PRK and LASIK were judged to be equally effective in correcting myopia and it was recommended that individual patient and surgeon preferences apply, although the importance of careful discussion of adverse effects was highlighted. 26 Evidence for laser correction of surgically‐induced refractive error following non‐refractive ophthalmic surgery (for example, cataract surgery) was judged adequate, 25 but evidence for short‐term safety was only available for refractive error induced after insertion of an intraocular lens. 24 Corneal inlay for correction of presbyopia was not recommended. 23
Interventions to slow the progression of myopia
There were three recommendations for interventions to slow the progression of myopia from one guideline. 26 The guideline recommended the use of antimuscarinic agents (atropine) as well as orthokeratology to prevent progression of myopia and spending more time outdoors to prevent onset of myopia, but the strength of the recommendation applied mainly to atropine and time spent outdoors. The lack of evidence for acupuncture was noted.
DISCUSSION
We have performed a systematic review of CPGs for refractive error. A wide‐ranging search of bibliographic and guideline databases and professional society websites identified a relatively limited (n = 12) set of high‐quality guidelines. All identified guidelines were developed in high‐income countries.
The terms ‘screening’, ‘evaluation’ and ‘examination’ were used in these guidelines, but were not defined explicitly in any of the reports. In general, the term screening was restricted to recommendations where the intention was to identify individuals at higher risk rather than provide a definitive diagnosis; however, recommendations for eye examinations in otherwise healthy individuals could also be considered a type of screening i.e., “the presumptive identification of unrecognised disease by the application of tests, examinations or other procedures.” 28 The American Academy of Ophthalmology set out recommendations for “eye evaluations” 20 , 22 and the American Optometric Association for “eye examinations”. 19 , 21 However, neither organisation restricted discussion to these terms, and the reports largely used the terms examination and evaluation interchangeably. We have not attempted to reclassify the terms as used in the recommendations, but in this report, we have used eye evaluations as a general term encompassing both examinations and screening. There is consensus from high‐quality clinical practice guidelines that children between the ages of 3 and 5 years inclusive should have an eye evaluation (either comprehensive examination or vision screening) to detect strabismus, significant refractive errors and amblyopia. There was less consistency as to recommendations for eye evaluations at other ages. CPGs developed by ophthalmic specialty organisations – the American Academy of Ophthalmology and American Optometric Association ‐ both recommended regular eye evaluations, and specified in some detail what should be included in the examination, but this was largely based on expert consensus. Public health organizations were more likely to acknowledge the weakness of the evidence supporting screening recommendations – both the USPSTF and the Canadian Task Force for Prevention advised against population vision screening in older people (65 years and above) based on lack of evidence or weak evidence of no effect, and the USPSTF concluded there was insufficient evidence to support vision screening of children younger than 3 years of age. However, the evidence on which these recommendations was based was largely drawn from high‐income countries, often where a large proportion of the population have access to good quality eye care services. The extent to which these recommendations apply to settings where high‐quality eye health care is less accessible, and the prevalence of correctable vision impairment is higher, is unclear.
Although recommendations on eye evaluations for school‐aged children were made in these guidelines, and comment was made on the educational impact of spectacles, 21 , 22 vision screening in the school setting was not specifically addressed. Evidence from systematic reviews suggests that school vision screening programmes with provision of free spectacles leads to improvement in the number of children wearing the spectacles they need and this may be associated with better educational outcomes. 29
There were relatively few specific guideline recommendations on the use of spectacles and contact lenses. This may reflect the fact that these interventions are embedded in eye health care and so recommendations on their use would be judged superfluous. Only one CPG included recommendations on thresholds for refractive correction based on ‘professional experience and clinical impressions’ since there are ‘no scientifically rigorous published data for guidance’. 22 Contact lens recommendations related to harms of overnight wear. It is notable that all the available guidelines had a high‐income country focus. The implications of limited resources were not addressed ‐ for example, the feasibility of contact lens use in lower resource settings, both in terms of cost and health care staffing requirements, but also increased risk of infection with potentially lower access to clean water. Interventions aimed to reduce the cost of provision of spectacles, for example, ready‐made spectacles or guidance on acceptable spherical equivalent were also not addressed. 29
Research on interventions to slow the progression of myopia is a rapidly moving field reflecting dramatic changes in the prevalence and incidence of this condition and concern about projected trends. 5 Evidence for use of antimuscarinic agents in schoolchildren is good/adequate, but there is currently insufficient evidence regarding the long‐term safety and optimal dosing. Other promising developments in this area include orthokeratology contact lenses and soft multifocal contact lenses. A recently published Cochrane Review was potentially out of date when it was published in January 2020 with 25 studies awaiting assessment and a further 74 studies identified as ongoing. 30 As evidence accumulates as to the best approaches for delaying the onset and preventing the progression of myopia, regularly updated high‐quality guidelines will be important to communicate and appraise the evidence generated by systematic reviews. Cochrane Eyes and Vision is planning a “living systematic review” and network meta‐analysis on interventions for myopia control in children. 31 The results of such living reviews will inform guideline producers, but the availability of up‐to‐date guidelines will also require a mechanism for rapid incorporation of evidence and guideline updates to assess the evidence to make recommendations for health‐care decision makers. Although not specifically recommended in our included guidelines, awareness raising for myopia prevention will be important.
There were relatively few recommendations on laser interventions for refractive error. Given the widespread use of these procedures in high‐ and some middle‐income settings, it would be good to see more detailed and up‐to‐date recommendations. The American Academy of Ophthalmology suggested that all currently available procedures were roughly equivalent, and this was based on results of Cochrane Reviews. 32 , 33 , 34
In conclusion, there is consensus from high‐quality clinical practice guidelines that children between the ages of 3 and 5 years inclusive should have some form of eye evaluation. However there were differences as to whether this should be vision screenings to detect children at risk or a comprehensive eye examination including cycloplegic refraction and dilation. Recommendations for vision screening and eye evaluations at other ages varied from recommending against screening to recommending annual comprehensive eye examinations and were less evidence‐based. There is a significant lack of guidelines focused on low‐ and middle‐income countries that are required, particularly given the pressing need for good quality refraction and provision of spectacles, to address refractive error in many parts of the world. Regular updating of systematic reviews and clinical practice guidelines is essential to ensure that robust evidence on preventing the progression of myopia is appraised and incorporated promptly into recommendations for eye health care practitioners. The evidence outlined in this systematic review will assist in informing the selection of interventions for inclusion in the PECI. 3 As part of the expert review process within PECI, consideration will also be given to whether it is practical and realistic that the interventions can be implemented within low and intermediate resource settings.
CONFLICTS OF INTEREST
The views expressed in this paper are those of the authors and do not necessarily reflect the views of WHO.
AUTHOR CONTRIBUTION
Jennifer Evans: Conceptualization (equal); Data curation (equal); Formal analysis (lead); Investigation (equal); Methodology (equal); Project administration (equal); Writing – original draft (lead). John Gerard Lawrenson: Data curation (equal); Formal analysis (equal); Investigation (equal); Writing – review & editing (equal). Jacqueline Ramke: Data curation (equal); Formal analysis (equal); Investigation (equal); Writing – review & editing (equal). Gianni Virgili: Data curation (equal); Formal analysis (equal); Investigation (equal); Writing – review & editing (supporting). Iris Gordon: Data curation (equal); Methodology (equal). Gareth Lingham: Data curation (equal); Writing – review & editing (equal). Sumrana Yasmin: Conceptualization (equal); Methodology (equal); Writing – review & editing (supporting). Stuart Keel: Conceptualization (equal); Investigation (equal); Methodology (equal); Validation (equal); Writing – review & editing (equal).
Supporting information
Appendix S1‐S3
Table S1‐S4
ACKNOWLEDGEMENTS
This research received no specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors. Cochrane Eyes and Vision is supported by grants from the National Institute for Health Research (NIHR) Cochrane Infrastructure Grant and Northern Ireland Health and Social Care Agency. JR’s position at the University of Auckland is supported by The Buchanan Charitable Foundation, New Zealand.
Biography
John G Lawrenson studied optometry at Aston University, graduating with a first class honours degree. After a pre‐registration year at Moorfields Eye Hospital London, he completed a College of Optometrists‐funded postgraduate scholarship at City, University of London, leading to a PhD in Visual Science. Following a post‐doctoral research fellowship in neuroscience at University College London, he returned to join the academic staff at City, where he currently holds a chair in Clinical Visual Science. Professor Lawrenson's interests lie in basic and clinical medical sciences. He has edited the eye and orbit sections in the last three editions of Grays Anatomy, probably the best‐known anatomy textbook in the world. He is an advocate for evidence‐based clinical practice, holds a Master's degree in Evidence‐based Healthcare from the University of Oxford, and is a Co‐ordinating Editor for the Cochrane Eyes and Vision review group. Professor Lawrenson's main research interests lie in the diagnosis and management of age‐related eye disease; particularly glaucoma, diabetic eye disease and age‐related macular degeneration (AMD). He has published over 100 peer‐reviewed papers and authored 8 book chapters.

Evans JR, Lawrenson JG, Ramke J, et al. Identification and critical appraisal of evidence for interventions for refractive error to support the development of the WHO package of eye care interventions: a systematic review of clinical practice guidelines. Ophthalmic Physiol Opt 2022;42:526–533. doi: 10.1111/opo.12963
REFERENCES
- 1. United Nations . Sustainable development goals. 2015; www.un.org/sustainabledevelopment/development‐agenda Accessed 3 Nov 2020.
- 2. WHO . World report on vision. Geneva: WHO; 2019. [Google Scholar]
- 3. Keel S, Evans JR, Block S, et al. Strengthening the integration of eye care into the health system: methodology for the development of the WHO package of eye care interventions. BMJ Open Ophthalmol 2020;5:e000533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Burton MJ, Ramke J, Marques AP, et al. The lancet global health commission on global eye health: vision beyond 2020. Lancet Global Health. 2021;9:e489–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016;123:1036–42. [DOI] [PubMed] [Google Scholar]
- 6. Fricke TR, Tahhan N, Resnikoff S, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: systematic review, meta‐analysis, and modelling. Ophthalmology 2018;125:1492–9. [DOI] [PubMed] [Google Scholar]
- 7. Naidoo KS, Fricke TR, Frick KD, et al. Potential lost productivity resulting from the global burden of myopia: systematic review, meta‐analysis, and modeling. Ophthalmology 2019;126:338–46. [DOI] [PubMed] [Google Scholar]
- 8. Frick KD, Joy SM, Wilson DA, Naidoo KS, Holden BA. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmology 2015;122:1706–10. [DOI] [PubMed] [Google Scholar]
- 9. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. BMJ 2009;339:b2535. 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. AGREE Next Steps Consortium . The AGREE II Instrument [Electronic version]. 2017. Available from: https://www.agreetrust.org/wp‐content/uploads/2017/12/AGREE‐II‐Users‐Manual‐and‐23‐item‐Instrument‐2009‐Update‐2017.pdf. Accessed 15 February, 2022.
- 11. Rauch A, Negrini S, Cieza A. Toward strengthening rehabilitation in health systems: methods used to develop a WHO package of rehabilitation interventions. Arch Phys Med Rehabil 2019;100:2205–11. [DOI] [PubMed] [Google Scholar]
- 12.Institute of Medicine (US) Committee on standards for developing trustworthy clinical practice guidelines. Clinical Practice Guidelines We Can Trust. 2011; Available from: https://www.ncbi.nlm.nih.gov/books/NBK209539/ doi: 10.17226/13058. Accessed 3 November 2020. [DOI]
- 13. Chen Y, Yang K, Marusic A, et al. A reporting tool for practice guidelines in health care: the RIGHT statement. Ann Intern Med 2017;166:128–32. [DOI] [PubMed] [Google Scholar]
- 14. UK National Screening Committee . Screening in the UK: making effective recommendations. London, UK: Public Health England; 2013. [Google Scholar]
- 15. Donahue SP, Ruben JB; American Academy of Ophthalmology , et al. US preventive services task force vision screening recommendations. Pediatrics. 2011;127:569–70. [DOI] [PubMed] [Google Scholar]
- 16. US Preventive Services Task Force , Grossman DC, Curry SJ, et al. Vision screening in children aged 6 months to 5 years: US preventive services task force recommendation statement. JAMA 2017;318:836–44. [DOI] [PubMed] [Google Scholar]
- 17. US Preventive Services Task Force , Siu AL, Bibbins‐Domingo K, et al. Screening for impaired visual acuity in older adults: US preventive services task force recommendation statement. JAMA 2016;315:908–14. [DOI] [PubMed] [Google Scholar]
- 18. Wilson BJ, Courage S, Bacchus M, et al. Screening for impaired vision in community‐dwelling adults aged 65 years and older in primary care settings. CMAJ 2018;190:E588–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. American Optometric Association . Comprehensive adult eye and vision examination. St Louis, Missouri, USA: American Optometric Association; 2015. Available from: https://www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/EBO%20Guidelines/Comprehensive%20Adult%20Eye%20and%20Vision%20Exam.pdf. Accessed 15 February, 2022. [Google Scholar]
- 20. American Academy of Ophthalmology . Comprehensive adult medical eye evaluation preferred practice pattern. 2015. 10.1016/j.ophtha.2015.10.047 [DOI] [PubMed]
- 21. American Optometric Association . Comprehensive pediatric eye and vision examination. St Louis, Missouri, USA: American Optometric Association; 2017. Available from: https://www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/EBO%20Guidelines/Comprehensive%20Pediatric%20Eye%20and%20Vision%20Exam.pdf. Accessed 15 February, 2022. [Google Scholar]
- 22. American Academy of Ophthalmology . Pediatric eye evaluations preferred practice pattern. 2017. Available from: https://www.aao.org/preferred‐practice‐pattern/pediatric‐eye‐evaluations‐ppp‐2017. Accessed 15 February, 2022.
- 23. NICE . Corneal inlay implantation for correction of presbyopia. 2013. Available from: https://www.nice.org.uk/guidance/ipg455/resources/corneal‐inlay‐implantation‐for‐correction‐of‐presbyopia‐pdf‐1899869812156357. Accessed 15 February, 2022.
- 24. NICE . Intraocular lens insertion for correction of refractive error, with preservation of the natural lens. 2009. Available from: https://www.nice.org.uk/guidance/ipg289. Accessed 15 February, 2022.
- 25. NICE . Laser correction of refractive error following non‐refractive ophthalmic surgery. 2011. Available from: https://www.nice.org.uk/guidance/ipg385/documents/laser‐correction‐of‐refractive‐error‐following‐nonrefractive‐ophthalmic‐surgery‐consultation‐document. Accessed 15 February, 2022.
- 26. American Academy of Ophthalmology . Refractive errors & refractive surgery preferred practice pattern. 2017. Available from: https://www.aao.org/preferred‐practice‐pattern/refractive‐errors‐refractive‐surgery‐ppp‐2017. Accessed 15 February, 2022.
- 27. Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wilson JMG, Jungner G; World Health Organization . Principles and practice of screening for disease. Geneva: World Health Organisation; 1968. [Google Scholar]
- 29. Evans JR, Morjaria P, Powell C. Vision screening for correctable visual acuity deficits in school‐age children and adolescents. Cochrane Database Syst Rev. 2018;2:CD005023. 10.1002/14651858.CD005023.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Walline JJ, Lindsley KB, Vedula SS, et al. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev 2020;1:CD004916. https://doi.org/10.1002/14651858.CD004916.pub4. Accessed 13 January, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lawrenson JG, Dhakal R, Verkicharla PK, et al. Interventions for myopia control in children: protocol for a living systematic review and network meta‐analysis. Cochrane Database Syst Rev 2021. 10.1002/14651858.CD014758. Accessed 9 August, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kuryan J, Cheema A, Chuck RS. Laser‐assisted subepithelial keratectomy (LASEK) versus laser‐assisted in‐situ keratomileusis (LASIK) for correcting myopia. Cochrane Database Syst Rev 2017. 10.1002/14651858.CD011080.pub2. Accessed 9 August, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Li S‐M, Zhan S, Li S‐Y, et al. Laser‐assisted subepithelial keratectomy (LASEK) versus photorefractive keratectomy (PRK) for correction of myopia. Cochrane Database Syst Rev 2016. 10.1002/14651858.CD009799.pub2. Accessed 9 August, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shortt AJ, Allan BDS, Evans JR. Laser‐assisted in‐situ keratomileusis (LASIK) versus photorefractive keratectomy (PRK) for myopia. Cochrane Database Syst Rev 2013. 10.1002/14651858.CD005135.pub3. Accessed 9 August, 2021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1‐S3
Table S1‐S4


