Abstract
Extensive drug treatment for coronavirus disease 2019 (COVID-19) includes low molecular weight heparin (LMWH). At therapeutic doses of LMWH, there is an increased risk of bleeding complications. Spontaneous, non-traumatic bleeding into the retroperitoneum is a life-threatening condition that can progress very rapidly. We describe a complication of COVID-19 bronchopneumonia treatment in which a patient developed a shock condition caused by non-traumatic bleeding into the retroperitoneum and abdominal wall due to LMWH overdose. The patient was operated on under difficult conditions - in biosafety level 3 (BSL-3). This case is exceptionally fascinating and informative. Nowadays, it is essential to point out possible complications associated with the treatment of COVID-19. Based on this report, we emphasize the need for careful LMWH dosing and quick and accurate diagnosis. Surgeons should maintain a higher index of suspicion for spontaneous bleeding in non-specific abdominal pain patients with COVID-19 or patients receiving therapeutic doses of LMWH.
Keywords: retroperitoneal hemorrhage, spontaneous bleeding, lmwh overdose, anticoagulant therapy, covid-19
Introduction
The coronavirus disease 2019 (COVID-19) has been associated with thrombosis as one of the disease's complications [1]. Once patients are hospitalized with COVID-19, they usually receive treatment accompanied by anticoagulants to prevent thrombosis [2]. The drug name, dosage, or duration is not yet strictly defined, as there is still a lack of guidelines in this matter. The thromboembolic pathologies and mortality have increased in individuals infected with COVID-19 [3]. Clinical studies [4-6] already in the first pandemic period have reported that COVID-19 patients are predisposed to thromboembolism.
On the other hand, Tanal et al.’s [2] findings of non-traumatic focused hemorrhages are unexpected. Several clinical reports [7-12] describing cases of severe spontaneous abdominal or retroperitoneal bleeding were published during the most fulminant phase of the pandemic. Retroperitoneal hematoma is a rare radiologically diagnosed complication, defined as bleeding in the retroperitoneal space, usually without associated trauma or iatrogenic manipulation. It is generally seen in patients receiving systemic anticoagulation including warfarin [13]. Other than anticoagulant therapies and clotting disorders, it has been associated with hematologic diseases, malignancies, trauma, and Evans syndrome [14]. Compared to other areas of bleeding, as Tanal et al. [2] show, retroperitoneal hematoma diagnosis can be challenging due to asymptomatic or non-specifically symptomatic conditions. Its treatment can be even more challenging because other comorbidities usually should be taken care of [2].
Case presentation
A 43-year-old patient was admitted to the intensive care unit (ICU) of the Pneumology Department on December 28, 2020, because of bilateral COVID-19 bronchopneumonia. According to the chest X-ray, bilateral inflammatory infiltrates were present. The blood test showed dehydration, severe hypoxemia, hypocapnia, and elevated inflammation.
We initiated high-flow nasal oxygen (HFNO - 40/40) therapy treatment, intravenous antibiotic therapy (ceftriaxone, moxifloxacin, fluconazole), systematic corticoids (dexamethasone), and low molecular weight heparin (LMWH) in the full anticoagulation dose (Clexane, 2 x 0.8 mL subcutaneously). We also started regular antiviral therapy during the treatment (acidum ascorbicum, vigantol, cetirizine, famotidine).
From his personal history from 2013, we knew that he underwent bilateral transplantation of lungs because of idiopathic pulmonary arterial hypertension. The patient's therapy was also consulted with the transplant center. Standard post-transplant treatment with tacrolimus for immunosuppression at 2.5 mg/24 hours was continued. The patient's clinical state and respiratory parameters gradually improved.
From January 5, 2021, the patient complained about experiencing stomach pain within the hypogastrium, bilaterally, and more on his left side. The symptoms and pain worsened with time. During the ultrasound examination of the abdomen, the fluid formations were found. One fluid formation of the size 120 x 100 x 80 mm was located in left mesohypogastrium, and other two fluid formations were located in the left retroperitoneum and the right musculus rectus abdominis. Final evaluation of the ultrasound examination suspected hematomas.
The patient was hemodynamically unstable. Blood test displayed a decreased hemoglobin level of 90 g/L, Leu of 28 x 109/L, INR of 1.15, APTT of 1.02 seconds, fibrinogen of 2.33 g/L, hypotension (87/55 mm Hg), heart rate of 112 beats per minute. Computed tomography (CT) of the abdomen and small pelvis revealed active bleeding in the abdominal cavity, left retroperitoneum, and right musculus rectus abdominis. The left retroperitoneum hematoma was 170 x 125 x 120 mm, attached to the left musculus psoas major, and presented with active bleeding. (Figures 1-3).
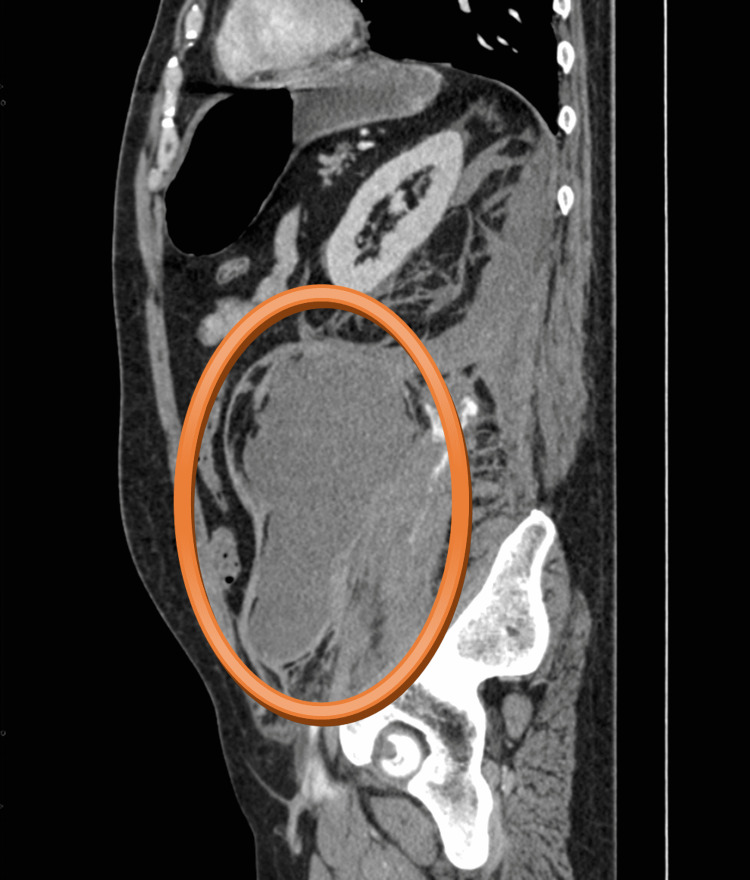
Figure 1. CT scan - sagittal plane.
The hematoma in the left retroperitoneum was of size 170 x 125 x 120 mm, attached to the left musculus psoas major, with present active bleeding
Figure 2. CT scan - coronal plane.
The hematoma in the left retroperitoneum was of size 170 x 125 x 120 mm, attached to the left musculus psoas major, with present active bleeding
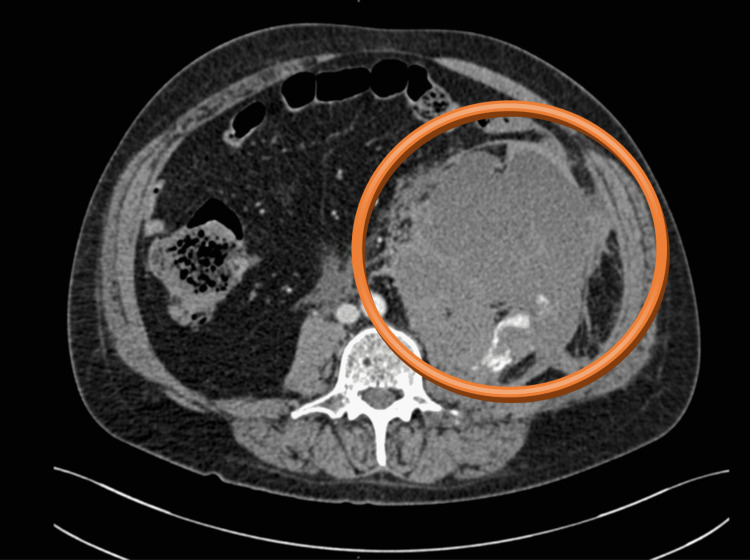
Figure 3. CT scan - axial plane.
The hematoma in the left retroperitoneum was of size 170 x 125 x 120 mm, attached to the left musculus psoas major, with present active bleeding
Similar fluid formation of size 130 x 80 x 50 mm was also present in the right musculus rectus abdominis, with active bleeding also present (Figures 4, 5). We decided on an immediate surgical revision. The surgery was performed in biosafety level 3 (BSL-3). We started the surgery 150 minutes after the CT examination.
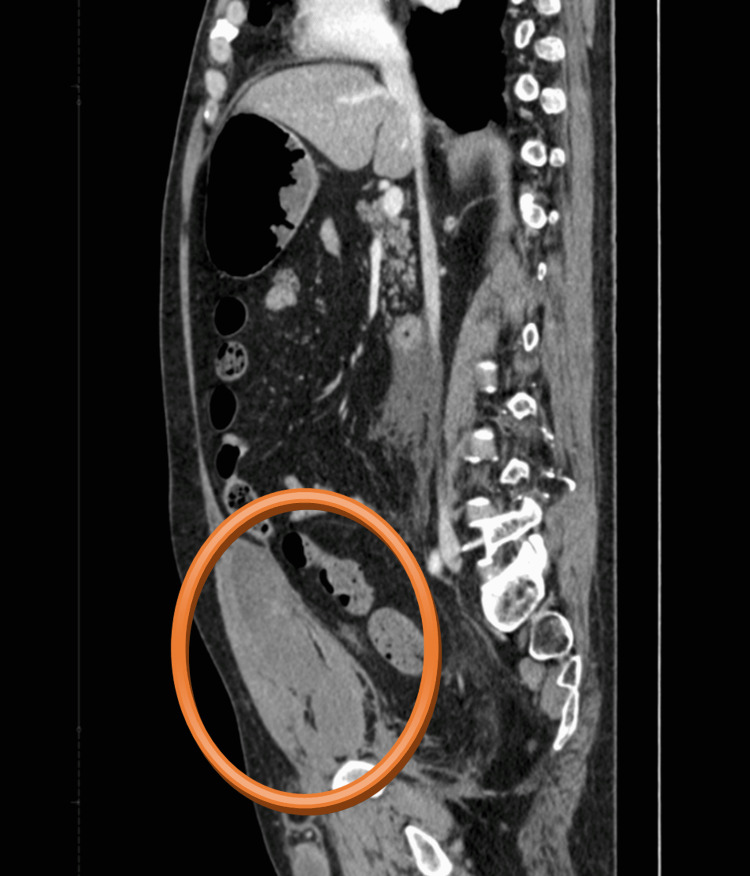
Figure 4. CT scan - sagittal plane.
Hematoma of size 130 x 80 x 50 mm in the right musculus rectus abdominis can be seen
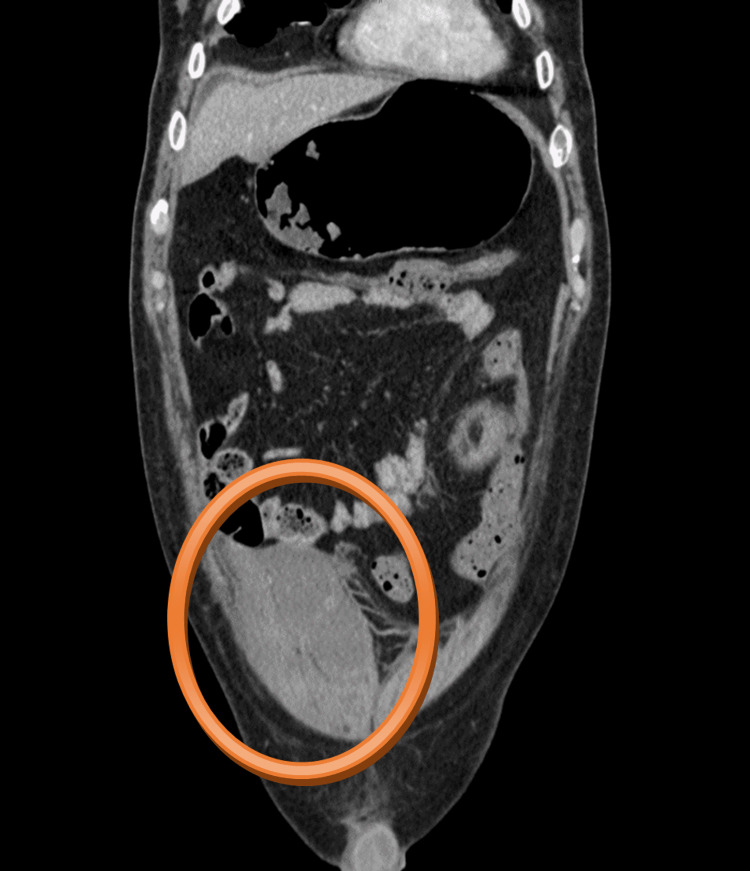
Figure 5. CT scan - coronal plane.
Hematoma of size 130 x 80 x 50 mm in the right musculus rectus abdominis can be seen
We opened the abdomen by midline laparotomy prolonged to both sides. When entering the abdomen cavity, a massive hematoma outpoured from the right musculus rectus abdominis (400 mL). Immediate asystole occurred, followed by cardiopulmonary resuscitation with a 15-minute external heart massage. A definite source of bleeding was not identified. The diffuse bleeding was present in the retroperitoneal area. We proceeded with hemostasis accompanied by hot surgical cloths, and then we performed the Mikulicz tamponade of the left retroperitoneal space with five surgical cloths. We inserted a silicone drain into the pouch of Douglas and sutured the abdominal cavity by anatomical levels.
The duration of the surgery was 1 hour, and overall perioperative blood loss was measured to be approximately 2,500 mL. After the surgery, the patient was transferred to the ICU of the anesthesiology department, where the therapy continued. The patient still needed vasopressor support with noradrenaline, supplementing the circulating volume with crystalloids and blood derivatives.
Overall, the patient received 6x blood transfusions, 7x fresh frozen plasma, and 6g of fibrinogen. Protamine and tranexamic acid were given for antagonization of LMWH. Bicarbonates were applied due to severe metabolic acidosis.
Despite using all the support of circulation, the patient faced multiple organ failure, his respiratory parameters worsened, and aggressive ventilation support was incorporated. Persisting anuria and mixed acidosis continued and worsened as well.
The patient passed away 10 hours after the surgery.
Discussion
The pandemic of more than two years has created challenges in every part of the society and medical profession is no exception to that. COVID-19 may appear in a severe, complicated form, and as shown by Al-Ani et al., Huang et al., and Chen et al. [4-6], it creates a thromboembolic situation in patients, independent of their age and comorbidities [15]. Thus, anticoagulant therapies are usually added to these patients, which is also recommended in international guidelines [16]. In our hospital, the therapeutic strategy is to reach the therapeutic dose of LWMH therapy, which seems beneficial to the majority of the patients. However, as presented in this case, a life-threatening condition may develop.
Yeoh et al. [17] showed that diagnosis of retroperitoneal hematoma requires a high degree of clinical suspicion as patients do not exhibit any clinically apparent signs and symptoms until a substantial amount of blood loss has occurred. Due to high doses of anticoagulants, frequently together with low platelets levels, these patients are at a high risk of bleeding. Yeoh et al. [17] recommend suspecting it in patients with significant groin, flank, abdominal, back pain, or hemodynamic instability after an interventional procedure or in anticoagulated patients. As shown by Kalayci [11,12], the ideal and straightforward diagnostic method is to check the hemoglobin level regularly. A contrast-enhanced CT scan of the abdomen remains the imaging modality of choice for early detection and prompt intervention [17]. As showed in our case report, COVID-19 patients treated with anticoagulants are at a risk of developing a spontaneous retroperitoneal hematoma. Although rare, it should remain a probable cause of bleeding, especially when patients present with flank pain, anemia, and signs of hypovolemia. Close monitoring and early intervention only can improve the outcome in this group of patients.
Conclusions
The challenging era of the COVID-19 pandemic has brought many challenges to all healthcare professionals, including our surgical department, which was reprofiled to the COVID-19 department. We usually treated patients with COVID-19 bronchopneumonia in this ward; in minor cases, surgical patients with COVID-19 as an accompanying diagnosis were hospitalized in this ward. Rarely, we cured COVID-19 patients with a surgical complication such as severe bleeding into the retroperitoneal space. In our patient, there was no history of the previous injury, and clinical signs were non-specific. The patient complained of abdominal pain; and objective signs were hypotension, tachycardia, and anemia. The only possible life-saving method is a quick diagnosis and follow-up surgery. Prevention could be optimalization of anticoagulant therapy. Although treatment of LMWH in patients with severe COVID-19 bronchopneumonia is necessary, a high risk of spontaneous bleeding should be considered at therapeutic doses. Clinicians need to be aware of the high bleeding risk, which can be challenging to treat or manage, even surgically. They need to consider this as a likely cause or differential in case of unexpected anemia and non-specific abdominal symptoms. Indication for an immediate imaging examination is the only way to get us to the correct diagnosis.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: a systematic review and meta-analysis. Malas MB, Naazie IN, Elsayed N, Mathlouthi A, Marmor R, Clary B. EClinicalMedicine. 2020;29:100639. doi: 10.1016/j.eclinm.2020.100639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Unexpected tendency to bleeding in COVID-19 patients: a case of spontaneous retroperitoneal hematoma. Tanal M, Celayir MF, Kale ZS. SAGE Open Med Case Rep. 2021;9:2050313. doi: 10.1177/2050313X211067907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Life-threatening retroperitoneal hematoma in a patient with COVID-19. Shah M, Colombo JP, Chandna S, Rana H. Case Rep Hematol. 2021;2021:8774010. doi: 10.1155/2021/8774010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thrombosis risk associated with COVID-19 infection. A scoping review. Al-Ani F, Chehade S, Lazo-Langner A. Thromb Res. 2020;192:152–160. doi: 10.1016/j.thromres.2020.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Huang C, Wang Y, Li X, et al. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Chen N, Zhou M, Dong X, et al. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Therapeutic anti-coagulation in COVID-19 and the potential enhanced risk of retroperitoneal hematoma. Ottewill C, Mulpeter R, Lee J, et al. QJM. 2021;114:508–510. doi: 10.1093/qjmed/hcab059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Life-threatening psoas hematoma due to retroperitoneal hemorrhage in a COVID-19 patient on enoxaparin treated with arterial embolization: a case report. Patel I, Akoluk A, Douedi S, Upadhyaya V, Mazahir U, Costanzo E, Flynn D. J Clin Med Res. 2020;12:458–461. doi: 10.14740/jocmr4256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Case report: iliopsoas hematoma during the clinical course of severe COVID-19 in two male patients. Nakamura H, Ouchi G, Miyagi K, et al. Am J Trop Med Hyg. 2021;104:1018–1021. doi: 10.4269/ajtmh.20-1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Catastrophic retroperitoneal hemorrhage in COVID-19 patients under anticoagulant prophylaxis. Javid A, Kazemi R, Dehghani M, Bahrami Samani H. Urol Case Rep. 2021;36:101568. doi: 10.1016/j.eucr.2021.101568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rectus sheath hematoma due to low molecular weight heparin in a COVID-19 patient in Turkey. Kalayci T. Cureus. 2021;13:0. doi: 10.7759/cureus.14870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abdominal lateral wall hematoma developed due to enoxaparin in a Covid-19 patient. Kalaycı T. J Emerg Med Case Rep. 2021;12:100–102. [Google Scholar]
- 13.Spontaneous abdominal hematoma in a patient treated with clopidogrel therapy: a case report. Guven A, Sokmen G, Bulbuloglu E, Tuncer C. https://pubmed.ncbi.nlm.nih.gov/15626275/ Ital Heart J. 2004;5:774–776. [PubMed] [Google Scholar]
- 14.Spontaneous retroperitoneal bleeding in a patient with Evans syndrome. Tsai CL, Lu TC, Chen WJ. Ann Hematol. 2004;83:789–790. doi: 10.1007/s00277-004-0916-1. [DOI] [PubMed] [Google Scholar]
- 15.Practical diagnosis and treatment of suspected venous thromboembolism during COVID-19 pandemic. Obi AT, Barnes GD, Wakefield TW, Brown S, Eliason JL, Arndt E, Henke PK. J Vasc Surg Venous Lymphat Disord. 2020;8:526–534. doi: 10.1016/j.jvsv.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.COVID-19 Treatment Guidelines. Antithrombotic Therapy in Patients With COVID-19. [ Feb; 2022 ];https://www.covid19treatmentguidelines.nih.gov/therapies/antithrombotic-therapy/ 2022
- 17.Spontaneous retroperitoneal hematoma: a rare bleeding occurrence in COVID-19. Yeoh WC, Lee KT, Zainul NH, Syed Alwi SB, Low LL. Oxf Med Case Reports. 2021;2021:0. doi: 10.1093/omcr/omab081. [DOI] [PMC free article] [PubMed] [Google Scholar]