Abstract
Background
Falls and their consequences are particularly common in older adults in hospitals and long‐term care (LTC) facilities.
Aim
To avoid falls and their consequences, and provide nurses with an overview of all relevant research literature on fall prevention, and a practice guideline on fall prevention in older adults was developed.
Methods
The development process included a systematic literature review to identify systematic reviews and primary studies on the topic of fall prevention, an assessment of the study quality, the preparation of meta‐analyses to summarize the results, and the application of the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach to grade the scientific literature. The guideline panel and an external multidisciplinary team graded the recommendations using the Delphi method. In addition, the panel and team formulated expert opinions.
Results
A total of 79 randomized controlled trials on fall prevention were identified, which formed the basis of the recommendations. Strongly recommended measures for both settings included multifactorial interventions, professionally supported body exercise interventions, and education and counselling interventions. The panel and team did not recommend the use of a specific assessment tool for fall risk assessment, low‐floor beds in hospitals, or body exercise interventions in frail residents.
Linking Evidence to Action
During the development of this guideline, particular attention was paid to collecting evidence‐based knowledge relevant to practice. By applying the recommendations, the outlined nursing care is justified, enabling healthcare personnel to achieve the overriding goal of providing optimal care to persons at risk of falling. Evidence for several fall prevention interventions was graded as very low. Sound intervention studies are necessary to strengthen the confidence in the evidence for low‐floor beds, alarm sensor systems, medication review, and staff education in hospitals.
Keywords: falls, GRADE approach, guideline, hospital, long‐term care, nursing home
INTRODUCTION
Falls are a global problem. Each year, about 600,000 falls worldwide result in death, which means that falls are one of the leading causes of traumatic deaths (World Health Organization, 2018). Due to biological changes, older adults have a higher risk of falling. About half of nursing home residents suffer a fall at least once a year (Rapp et al., 2012). Nearly 10% of older patients admitted to hospital units experience falls (Castellini et al., 2017), with more than one‐quarter suffering physical injuries (Anderson et al., 2012; Basic & Hartwell, 2015). In addition to physical consequences, falls also have psychological and social consequences. Fear of falling, the most common psychological consequence, leads to a reduction in both physical and social activities (Lavedan et al., 2018).
To prevent these falls and their consequences, we developed a practice guideline for use in hospitals and long‐term care (LTC) institutions. This guideline is intended to support nurses by helping them make shared decisions with patients, residents, and their families when choosing optimal fall prevention interventions.
Currently, there are no updated (i.e., newer than 5 years) international guidelines on fall prevention available for free. Although the guideline from the National Institute for Health and Care Excellence (NICE, 2018) was updated in 2018, the literature was only updated with regard to fall prevention in hospitals. The other seemingly current, available guidelines are merely a synthesis of other guidelines (e.g., Registered Nurses' Association of Ontario, 2017), meaning that the referenced literature is not current. Therefore, an up‐to‐date, freely available guideline based on the best evidence is needed.
Scope
The overriding aim of creating this guideline was to identify effective interventions to prevent falls and provide practical and concrete recommendations for effective fall prevention.
Specific objectives pursued while developing the guideline were to identify risk factors for falls, reduce falls specifically, and avoid the possible consequences of falls. Furthermore, special attention was paid to ensure that the quality of life of the older person would not be adversely affected by the recommended fall prevention interventions.
The target group for this fall prevention guideline was older adults in hospitals or LTC institutions. Older adults are understood to be those over the age of 65. According to the guideline, LTC institutions encompass nursing homes and rehabilitation facilities for older adults. Interventions addressed were those that nurses carry out in hospitals or LTC institutions or that are suggested by nurses on an interdisciplinary basis (e.g., medication review and body exercises). The main outcome, “fall,” is based on the definition developed by the Kellogg International Work Group (1987).
The recommendations in the guideline have primarily been developed for use by nurses who are actively caring for older adults in hospitals and LTC institutions. In addition, the guideline can support the interdisciplinary planning of measures in the respective institutions. Furthermore, the guideline can be used for quality assurance in nursing and healthcare facilities as well as for knowledge transfer in training and continuing education institutions.
METHODS
The guideline panel consisted of nursing scientists from a medical university and clinical practitioners from a university hospital. The guideline members had no conflicts of interests and received no external sponsorship for the guideline development. The development process consisted of preparation and main stages, which are illustrated in Figure 1. The methodological guideline development strategy incorporated the use of the AGREE II tool (Brouwers et al., 2010) to ensure guideline quality.
FIGURE 1.
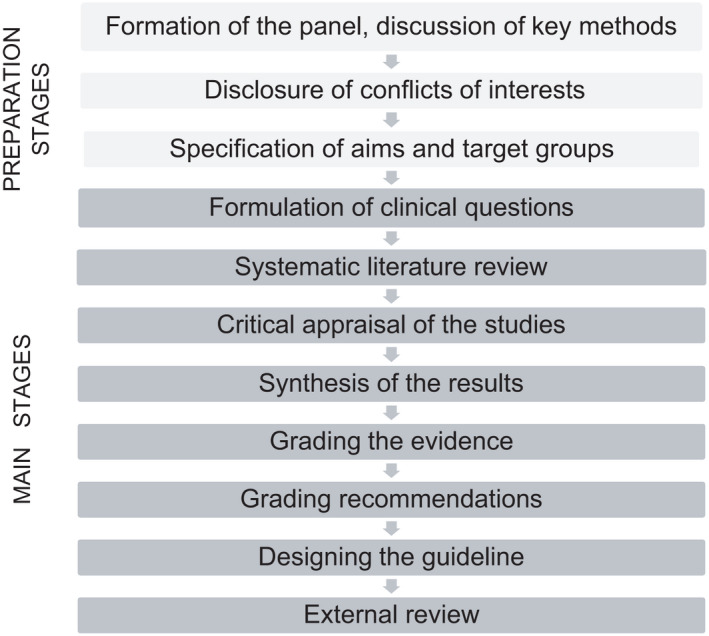
Guideline development process
Based on known fall prevention interventions and the primary endpoint rate of falls and rate of fallers, key questions were formulated by the guideline panel (Appendix S1). Interventions and endpoints were reviewed and completed by external nurses working in hospitals or nursing homes. Secondary endpoints were discussed with older adults who were members from the Cochrane Consumer Network. Four endpoints were identified as relevant: (1) injuries due to falls, (2) fractures, (3) quality of life, and (4) fear of falling. A systematic literature review was conducted for each clinical question, following a two‐step process. First, we searched for systematic reviews (SRs) in the German or English languages published up to March 2018 in PubMed, the CINAHL database, and the Cochrane Database of Systematic Reviews. Second, we searched for more current (i.e., not included in the SRs) randomized controlled trials (RCTs), observational studies, or diagnostic accuracy studies in the PubMed, CINAHL, and Cochrane Central Register of Controlled Trials databases. To identify additional studies, a manual search was performed using the Google Scholar web search engine, and a reference list search was performed in the relevant SRs. Studies were included if they involved patients or residents, at least half of whom were ≥65 years of age; placed a focus on a specific fall prevention intervention defined in the key questions; were carried out in a hospital, nursing homes, care home, or rehabilitation facility for older adults; and had the primary endpoint of a fall or fallers.
Observational studies were only included to answer epidemiological clinical questions. SRs were appraised using the Critical Appraisal Worksheet for Systematic Reviews (Centre for Evidence‐Based Medicine, 2005). SRs were included if they provided a clear description of the search methods, including a comprehensive literature search (of at least two databases); a clear indication of inclusion and exclusion criteria was given; and a quality appraisal of included RCTs with predetermined quality criteria was carried out. We appraised the methodological qualities of the additionally included RCTs using the Critical Appraisal Worksheet for Therapy Studies (Centre for Evidence‐Based Medicine, 2005) and the observational studies using the CASP checklists (Critical Appraisal Skills Program, 2017). A screening of the titles, abstracts, and full text as well as the critical appraisal were carried out by two authors independently.
Data were extracted from the SRs (according to each included and relevant RCT) and the current RCTs. To synthesize the results, similar interventions and outcomes were grouped, and meta‐analyses with a random‐effects model were performed using the software RevMan version 5. Results were calculated in the form of pooled risk ratios or pooled rate ratios, both abbreviated as RR, with 95% confidence intervals (CI). The I² statistic method was used to assess statistical heterogeneity (Deeks et al., 2019).
The GRADE (Grading of Recommendations Assessment Development and Evaluation) method was used to grade the confidence in estimates of the effects (quality of evidence; Balshem et al., 2011) and the recommendations (Andrews et al., 2013). The quality of evidence was graded as high, moderate, low, or very low for each endpoint, depending on the risk of bias identified in the studies of interest, the inconsistency of the study results, the indirectness of the studies, and the imprecision of the estimate of the study effect (Guyatt et al., 2013). To rate the overall confidence in the evidence, the main outcome gradings were used.
The guideline development panel graded the recommendations together with an external panel of clinical experts. The external panel included medical doctors, nurses, physiotherapists, and patient representatives. Both panels issued strong, weak, or no recommendations in three Delphi rounds (McMillan et al., 2016). The recommended criteria for the GRADE method (e.g., benefits, harms, study quality, cost‐effectiveness, presumed values, acceptability, and feasibility) were considered (Andrews et al., 2013). Clinical questions that could not be answered by an assessment of the research (i.e., no randomized controlled studies were available) were discussed by members of the two panels (referred to below as the grading panel) in two workshops using a nominal group technique (Harvey & Holmes, 2012). These consensus statements are labelled as expert opinions in the guideline itself. Moreover, we developed audit criteria that could be used to review the practical application of the guideline and increase its practicability.
The drafted guideline was externally reviewed by nurse managers, care providers, and a methodological expert from Cochrane Austria. The experts’ comments as well as a detailed description of the methods are described in a methods paper that can be requested from the first author.
RESULTS
The literature review yielded 4,315 hits. Of these, 19 SR of RCTs (which included a total of 65 different RCTs), 15 current RCTs (not included in the SR of RCTs), 8 SR of observational studies, 4 current observational studies, 3 SR of diagnostic accuracy studies, and 2 current diagnostic accuracy studies were identified as fulfilling the inclusion and quality criteria (for flow diagrams, see Appendix S2; for included studies, see Appendix S3). Similar interventions and outcomes of the 80 (65+15) RCTs were pooled, and these results provided the basis for the GRADE confidence ratings and recommendations. The quality ratings of the included RCTs are illustrated in Appendix S4 and the characteristics of the included RCTs in Appendix S5. Forest plots with significant findings which led to strong recommendations are shown in Appendix S6. The GRADE profiles with all corresponding meta‐analyses are provided in the methods paper.
Recommentation
The recommendations and expert opinions are presented in Appendix S7, and outlined in more detail below.
Fall risk assessment
Experts recommended that every older adult be assessed for risks of falling (significant risk factors are listed in Table 1). However, the use of an assessment tool for fall risk was not recommended. In one study with 1,125 participants (Meyer et al., 2009), the effectiveness of a fall risk assessment was investigated and had no effect on falls (mean difference [MD] −0.06, 95% CI [−0.64, 0.52]) or fall‐related injuries (MD 0.01, 95% CI [−0.06, 0.08]) ~, and there were increased costs due to the implementation of the tool. Furthermore, the analysis of the diagnostic accuracy studies showed that commonly used tools do not achieve the required values for sensitivity and specificity of at least 80% each (Appendix S8). Due to the lack of benefits, increased effort needed for implementation, and moderate confidence placed in the quality of evidence, the estimation of “no recommendation” was justified.
TABLE 1.
Significant risk factors for falls based on systematic reviews and current observational studies
| Hospital | LTC |
|---|---|
| Fall history (within the last 6 months) | Fall history (within the last 6 months) |
| Old age (>70 years) | High age (>80 years) |
| Male gender | |
| Diseases with an increased risk | |
| Chronic obstructive pulmonary disease | Morbus Parkinson |
| Atrial fibrillation | |
| Dementia | |
| Insult | |
| Multimorbidity (> 3 diseases) | |
| Depression | |
| Arterial hypertension | |
| Urine incontinence | |
| Disease‐related changes | |
| Movement restriction | Dizziness (vertigo) |
| Gait insecurity increased | Cognitive impairment |
| Dizziness (vertigo) | Moderate physical impairment |
| Musculoskeletal restriction | Restricted balance |
| Visual impairment | Restricted gait |
| Sleep disorder | Difficulties with dual tasking |
| Cognitive impairment | |
| Confusion | |
| Need for support during transfer | |
| Difficulties with dual tasking | |
| Additional risk factors in patients with dementia | |
| Mini‐Mental State Examination (MMSE) value <7 | Wandering behaviour |
| Depression | Taking psychoactive medication (the more drugs the higher the risk) |
| Wandering behaviour | |
| Taking more than five drugs | |
| Dependence in daily life activities | |
| Hospital stay over 5 weeks | |
| Additional risk factors in patients with cancer | |
| Pain | |
| Fatigue | |
| Delirium | |
| Malnutrition | |
| Dependence in daily life activities | |
| Taking more than five drugs | |
| Taking antipsychotics | |
| Medication that significantly increases fall risk | |
| Anticonvulsants | Antidepressants |
| Antipsychotics | Antipsychotics |
| Sedatives | Sedatives |
| Vasodilators | |
| Taking more than three drugs | |
| External risk factors | |
| Using walking aides | |
| Wearing slippers | |
For references, see Appendix S2.
Abbreviation: LTC, long‐term care.
Multifactorial interventions
Multifactorial interventions were defined as interventions that consisted of more than two fall prevention measures. A meta‐analysis of studies performed in hospital settings showed a significant reduction in falls (four studies, RR 0.69, 95% CI [0.49, 0.96], I² 59%) with a low confidence in the evidence, but no reduction in fractures due to falls (three studies, RR 0.43, 95% CI [0.10, 1.78], I² 0%) with a very low confidence. The grading panel voted for a strong recommendation because of the significant fall reduction effect.
Studies addressing the LTC setting showed significant effects for the endpoints fallers (eight studies, RR 0.86, 95% CI [0.76, 0.98], I² 52%), recurrent fallers (five studies, RR 0.76, 95% CI [0.60, 0.96], I² 57%), and hip fractures due to falls (three studies, RR 0.48, 95% CI [0.24, 0.98], I² 0%) with a low‐to‐moderate confidence in the evidence for all of these endpoints. No significant effect was detected for the endpoints falls (seven studies, RR 0.78, 95% CI [0.59, 1.04], I² 84%) and injuries due to falls (four studies, RR 0.64, 95% CI [0.28, 1.51], I² 40%), both with a very low confidence in the evidence. The strong recommendation was justified because of the significant reduction in fallers and hip fractures.
Patient or resident education and counselling interventions
Pooling studies performed in hospitals revealed a significant effect of patient education and counselling regarding falls (six studies, RR 0.70, 95% CI [0.62, 0.79], I² 8%) and fallers (five studies, RR 0.71, 95% CI [0.61, 0.82], I² 0%), with moderate confidence in the evidence. The subgroup analysis regarding the intensity of the educational interventions showed that more intensive educational interventions provided higher benefits (four studies, RR 0.67, 95% CI [0.57, 0.78], I² 18%) than interventions with lower intensity (e.g., only one education session; three studies, RR 0.80, 95% CI [0.64, 0.99], I² 0%).
A second subgroup analysis was performed for studies that included patients with or without cognitive impairments. The results showed significance only for studies that had patients without cognitive impairments (three studies, RR 0.91, 95% CI [0.64, 1.29], I² 50% with a low confidence in the evidence; three studies RR 0.54, 95% CI [0.41, 0.70], I² 19% with a high confidence in the evidence). The grading panel decided to assign a strong recommendation for patients without cognitive impairment and a weak recommendation for residents with cognitive impairment based on the observed effect and the level of confidence in the evidence.
Only one study was identified that investigated a group education programme in the LTC setting (Huang et al., 2016). In this study, a significant reduction in falls (p < .001) and a significant reduction in the fear of falling (p < .001) were found. Although the confidence in this evidence was low, the grading panel issued a strong recommendation for resident education and counselling.
Body exercise interventions
Three studies were carried out to investigate body exercise interventions in the hospital setting. These interventions showed a significant reduction in the rate of falls (two studies, RR 0.50, 95% CI [0.27, 0.90], I² 0%) and the rate of fallers (two studies, RR 0.38, 95% CI [0.15, 0.94, I² 0%), with a low and very low confidence in the evidence, respectively. The main exercise measure in these studies was performing additional physiotherapy. Therefore, the measure was placed in the strong recommendation category.
Most of the included studies addressed body exercise interventions in the LTC setting (n = 23). Pooling these studies only revealed an effect when excluding studies with frail residents (15 studies, RR 0.80, 95% CI [0.67, 0.97], I² 64%). No preference was found for combined movement exercises (13 studies, RR 0.82, 95% CI [0.66, 1.03], I² 73%), or movement exercises consisting of individual components (e.g., only balance or strengths training; 8 studies, RR 0.81, 95% CI [0.61, 1.07], I² 80%), with a low or very low confidence in the evidence. Thus, a weak recommendation was assigned. Exercises with technical devices showed a significant effect, with moderate confidence in the evidence when excluding the technical device vibration plate (three studies, RR 0.39, 95% CI [0.26, 0.60], I² 0%). The grading panel decided to issue a strong recommendation due to the large effect observed and the moderate confidence in the evidence. Although, resources are needed to implement a technical devices intervention. Exercises with tai chi had no significant effect on the rate of falls, fallers, or quality of life. However, it showed a significant effect on fear of falling (p < .001). Therefore, exercises with tai chi are only recommended in residents with fear of falling. Subgroup analyses illustrated that exercise interventions in frail residents led to an increased risk of falling (three studies, RR 1.17, 95% CI [1.00, 1.36], I² 0%). Therefore, exercise interventions are not recommended for this subgroup.
Interventions relating to external fall risks
No RCTs could be identified that dealt with the adaption of the environment or external risk factors to prevent falls in hospitals and LTC settings. However, the adaption of the environment was included in several non‐RCT studies in which multifactorial fall prevention interventions were examined. Furthermore, wearing slippers was identified as a significant external risk factor for falls in LTC settings (Table 1). Due to the lack of external evidence, the grading panel formulated several expert opinions.
Medical devices for fall and injury prevention
One study (Haines et al., 2010) surveyed the effect of low‐floor beds in hospitals and showed that they were correlated with an increased fall rate tendency (RR 1.39, 95% CI [0.22, 8.87]). The confidence in this evidence was rated as very low. Therefore, low‐floor beds are not recommended for fall prevention.
Alarm and sensor devices were investigated in two RCTs, but outcomes showed no significant effect on falls (one study, RR 0.42, 95% CI [0.15–1.18]), falls out of the bed (two studies, RR 0.78, CI [0.36, 1.69], I² 20%), or health‐related quality of life (one study, MD 0.01, 95% CI [−0.02, 0.03]) in hospital patients. Similar results were found for the LTC setting in one study (RR 0.65, 95% CI [0.33, 1.27]).
The overall rating of the evidence is very low for both settings. However, due to the practicability of the intervention and possibly more rapid treatment for patients who have fallen, the grading panel decided to issue a weak recommendation for alarm and sensor devices.
The use of hip protectors was investigated in 12 RCTs, all of which addressed the LTC setting. Hip protectors were not shown to decrease the rate of falls (12 studies, RR 1.01, 95% CI [0.91–1.12], I² 85%, a very low confidence in the evidence), but slightly decreased the rate of hip fractures (12 studies, RR 0.74, 95% CI [0.54–1.01], I² 21%, a moderate confidence in the evidence). As hip protectors are developed to reduce hip fractures, this endpoint was prioritized. No significant effect was found for the endpoints of pelvic fractures (four studies, RR 0.76, 95% CI [0.25, 2.34], I² 0%) or other fractures (two studies, RR 1.23, 95% CI [0.62–2.44], I² 0%).
The subgroup analysis results show that there was a preference for soft shell hip protectors (tree studies, RR 0.32, 95% CI [0.12, 0.89], I² 0%) as compared to hard shell hip protectors (seven studies, RR 0.71, 95% CI [0.51, 1.00], I² 14%). The grading panel decided to issue a weak recommendation for the use of hip protectors in LTC settings because of the particularly relevant reduction in hip fractures and considerable resources required.
Medication review
The medication review by a pharmacologist or physician showed that medication did not significantly reduce the rate of falls (four studies, RR 0.75, 95% CI [0.43, 1.30], I² 90%) or rate of fallers (six studies, RR 0.92, CI [0.74, 1.15], I² 64%) in hospital and LTC settings. As the medication review was an important component of several effective multifactorial intervention studies, the grading panel decided to issue a weak recommendation for this intervention.
Complementary interventions
One study investigated the effect of olfactory stimulation with lavender essential oil on fall prevention in LTC residents (Sakamoto et al., 2012). A significant effect on the rate of falls was found (RR 0.57, 95% CI [0.32, 0.99]), with a low confidence in the evidence. The required resources for implementing an olfactory stimulation intervention and the low confidence in the evidence resulted in a weak recommendation.
Measures restricting freedom
As no RCT regarding this topic could be identified, the grading panel formulated an expert opinion in accordance with the Austrian Federal Law on Nursing Profession.
Increased observation
Based on the practical experience of the panel members, the members defined expert opinions for increased observation for patients and residents with recurrent falls.
Staff education
The meta‐analysis of two studies found no significant effect of staff education on fall incidence (two studies, RR 0.90, 95% CI [0.29, 2.80], I² 0%). A very low confidence was placed in this evidence. The grading panel argued that the importance of this intervention permitted the assignment of a weak recommendation for staff education on fall prevention measures.
Six studies were carried out to evaluate the effects of staff education in LTC settings. The pooled results did not reveal a significant benefit regarding staff education on the rate of falls (five studies, RR 0.89, CI [0.72, 1.11], I² 47%), fractures due to falls (2=two studies, 95% CI [0.64, 1.10], I² 0%), and quality of life (p > .05). However, the staff members’ knowledge increased significantly when staff education was provided. The confidence in this evidence was rated as low. The results of subgroup analyses showed a small benefit for more intensive educational interventions (combining multiple strategies such as group education, provision of information material, audits, and feedback) as compared to less intensive educational interventions (e.g., 4‐hour group education) concerning the rate of falls (three studies, RR 0.82, 95% CI [0.61, 1.10], I² 0%; two studies, RR 0.96, 95% CI [0.66, 1.42], I² 83%). The grading panel decided to issue a strong recommendation for active staff education in LTC settings because of the effect on increased knowledge and the marginally insignificant effect on fall reduction.
Post‐fall analysis
No RCT investigated the effect of post‐fall analysis on fall‐related endpoints. Nevertheless, the grading panel formulated an expert opinion for patients and residents who experienced frequent falls using their practical experience.
IMPLEMENTAION AND EVALUATION
A former version of this guideline was implemented in a before and after 2‐year follow‐up study by taking a participatory action research approach in two hospital units (Breimaier et al., 2015; Breimaier et al., 2015). Based on the multifaceted and tailored implementation strategies used, eight recommendations for the guideline implementation can be made: (1) the current situation should be analysed regarding the fall incidence, patients at risk of falls, and fall preventive measures, (2) nursing staff should be familiarized with the guideline, (3) aims and criteria for measuring the achievement of the aims should be defined, (4) all relevant staff should be involved in the implementation process, as well as representatives of other professional groups, (5) various and locally adapted implementation strategies should be used, (6) local conditions like team meetings or the electronic patient record system should be exploited, (7) the implementation process should be reflected upon regularly, and (8) staff should be open to new ideas, and the team should be encouraged to provide ideas and critique. To support the evaluation of the implementation process, quality criteria on the structure, process, and outcome levels based on the main guideline recommendations, and expert opinions have been developed. These indicators should be applied before implementing the guideline recommendations and at regular intervals during the implementation process to evaluate the success of the implementation. To ensure structural quality, medical aids should be available and in functional condition. Process quality indicators include the assessment and documentation of fall risk factors and multidisciplinary case discussions in hospital settings. Outcome quality indicators belong, for example, to a lowered fall rate and reduced injuries caused by falls (Appendix S9).
Limitations of the Guideline
We used the GRADE method and adapted the original four‐stage recommendation grading (Andrews et al., 2013) into a three‐stage grading system. This means that, instead of issuing strong and weak recommendations against an intervention, only the stage “no recommendation” was used. This choice was justified because a similar three‐stage system was used in the former version of the guideline, with which the Austrian nursing staff was already familiar. However, a “no recommendation” may be incorrectly understood as conclusive, neglecting the continuum of desired and undesired effects that are expressed in the original GRADE stages.
Gaps in knowledge
The panel graded the level of confidence in the evidence for several interventions as very low, mainly due to the small number of supporting studies. This means that there is very little confidence in the estimated effect (Balshem et al., 2011). Sounder RCTs are necessary to strengthen this confidence, especially with the interventions of low‐floor beds, alarm sensor systems, medication review, and staff education in hospitals. Although external fall risks and interventions to prevent these were investigated for community settings (Keall et al., 2015), they have rarely been studied in an institutional setting, indicating that additional studies are needed. The patient‐relevant endpoints of quality of life and fear of falling were rarely evaluated in the SRs and RCTs. Therefore, we recommend including these endpoints in further studies.
LINKING EVIDENCE TO ACTION
Patients and residents should be screened for fall risks when they are admitted to the hospital or LTC, but the use of an assessment tool is not recommended
Multifactorial interventions based on individual risk factors significantly reduce falls and are strongly recommended in the hospital and LTC settings.
Patients at risk of falling should be informed about fall risks and receive training and advice regarding fall prevention measures.
In LTC settings, body exercise interventions guided by therapists and supported by technical aids are strongly recommended.
Active educational interventions for caregivers on the subject of falls should be encouraged to increase the employees’ knowledge and prevent residents from falling in LTC settings.
CONCLUSION
Fall prevention is an important nursing task in hospitals and nursing homes. Nurses need to have access to comprehensibly prepared and clearly summarized evidence to provide optimal care. This guideline provides updated, evidence‐based knowledge combined with practical hints on fall prevention and should thus contribute to improvements in the care of patients who are at risk of falling.
Supporting information
Supplementary Material
Schoberer, D. , Breimaier, H.E. , Zuschnegg, J. , Findling, T. , Schaffer, S. & Archan, T , the Guideline Development Group (2022) Fall prevention in hospitals and nursing homes: Clinical practice guideline. Worldviews on Evidence‐Based Nursing, 19, 86–93. 10.1111/wvn.12571
Funding information
This research did not receive any funding from agencies in the public, commercial, or not‐for‐profit sectors.
REFERENCES
- Anderson, O. , Boshier, P.R. & Hanna, G.B. (2012) Interventions designed to prevent healthcare bed‐related injuries in patients. Cochrane Database of Systematic Reviews, 1, CD008931. 10.1002/14651858.CD008931.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews, J. , Guyatt, G. , Oxman, A.D. , Alderson, P. , Dahm, P. , Falck‐Ytter, Y. et al. (2013) GRADE guidelines: 14. Going from evidence to recommendations: The significance and presentation of recommendations. Journal of Clinical Epidemiology, 66(7), 719–725. 10.1016/j.jclinepi.2012.03.013 [DOI] [PubMed] [Google Scholar]
- Balshem, H. , Helfand, M. , Schünemann, H.J. , Oxman, A.D. , Kunz, R. , Brozek, J. et al. (2011) GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology, 64(4), 401–406. 10.1016/j.jclinepi.2010.07.015 [DOI] [PubMed] [Google Scholar]
- Basic, D. & Hartwell, T.J. (2015) Falls in hospital and new placement in a nursing home among older people hospitalized with acute illness. Clinical Interventions in Aging, 10, 1637–1643. 10.2147/cia.S90296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breimaier, H.E. , Halfens, R.J. & Lohrmann, C. (2015) Effectiveness of multifaceted and tailored strategies to implement a fall‐prevention guideline into acute care nursing practice: a before‐and‐after, mixed‐method study using a participatory action research approach. BMC Nursing, 14, 18. 10.1186/s12912-015-0064-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breimaier, H.E. , Heckemann, B. , Halfens, R.J. & Lohrmann, C. (2015) The Consolidated Framework for Implementation Research (CFIR): a useful theoretical framework for guiding and evaluating a guideline implementation process in a hospital‐based nursing practice. BMC Nursing, 14, 43. 10.1186/s12912-015-0088-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwers, M.C. , Kho, M.E. , Browman, G.P. , Burgers, J.S. , Cluzeau, F. , Feder, G. et al. (2010) AGREE II: Advancing guideline development, reporting and evaluation in health care. Canadian Medical Association Journal = Journal De L'association Medicale Canadienne, 182(18), E839–842. 10.1503/cmaj.090449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellini, G. , Demarchi, A. , Lanzoni, M. & Castaldi, S. (2017) Fall prevention: Is the STRATIFY tool the right instrument in Italian Hospital inpatient? A retrospective observational study. BMC Health Services Research, 17(1), 656. 10.1186/s12913-017-2583-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centre for Evidence‐Based Medicine (2005) Critical appraisal worksheets. Retrieved from https://www.cebm.net/2014/06/critical‐appraisal/ [Google Scholar]
- Critical Appraisal Skills Program (2017) CASP checklists. Retrieved from https://casp‐uk.net/casp‐tools‐checklists/ [Google Scholar]
- Deeks, J.J. , Higgins, J.P.T. & Altman, D.G. (2019) Analysing data and undertaking meta‐analyses. In: Higgins, J.P.T. , Thomas, J. , Chandler, J. , Cumpston, M. , Li, T. , Page, M.J. & Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions. Hoboken, NJ: Wiley‐Blackwell, pp. 241–284. [Google Scholar]
- Guyatt, G. , Oxman, A.D. , Sultan, S. , Brozek, J. , Glasziou, P. , Alonso‐Coello, P. et al. (2013) GRADE guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. Journal of Clinical Epidemiology, 66(2), 151–157. 10.1016/j.jclinepi.2012.01.006 [DOI] [PubMed] [Google Scholar]
- Haines, T.P. , Bell, R.A. & Varghese, P.N. (2010) Pragmatic, cluster randomized trial of a policy to introduce low‐low beds to hospital wards for the prevention of falls and fall injuries. Journal of the American Geriatrics Society, 58(3), 435–441. 10.1111/j.1532-5415.2010.02735.x [DOI] [PubMed] [Google Scholar]
- Harvey, N. & Holmes, C.A. (2012) Nominal group technique: an effective method for obtaining group consensus. International Journal of Nursing Practice, 18(2), 188–194. 10.1111/j.1440-172X.2012.02017.x [DOI] [PubMed] [Google Scholar]
- Huang, T.T. , Chung, M.L. , Chen, F.R. , Chin, Y.F. & Wang, B.H. (2016) Evaluation of a combined cognitive‐behavioural and exercise intervention to manage fear of falling among elderly residents in nursing homes. Aging Mental Health, 20(1), 2–12. 10.1080/13607863.2015.1020411 [DOI] [PubMed] [Google Scholar]
- Keall, M.D. , Pierse, N. , Howden‐Chapman, P. , Cunningham, C. , Cunningham, M. , Guria, J. et al. (2015) Home modifications to reduce injuries from falls in the home injury prevention intervention (HIPI) study: a cluster‐randomized controlled trial. Lancet, 385(9964), 231–238. 10.1016/s0140-6736(14)61006-0 [DOI] [PubMed] [Google Scholar]
- Kellogg International Work Group (1987) The prevention of falls in later life. A report of the Kellogg International Work Group on the Prevention of Falls by the Elderly. Danish Medical Bulletin, 34(Suppl. 4), 1–24. [PubMed] [Google Scholar]
- Lavedan, A. , Viladrosa, M. , Jurschik, P. , Botigue, T. , Nuin, C. , Masot, O. et al. (2018) Fear of falling in community‐dwelling older adults: a cause of falls, a consequence, or both? PLoS One, 13(3), e0194967. 10.1371/journal.pone.0194967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillan, S.S. , King, M. & Tully, M.P. (2016) How to use the nominal group and Delphi techniques. International Journal of Clinical Pharmacy, 38(3), 655–662. 10.1007/s11096-016-0257-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer, G. , Köpke, S. , Haastert, B. & Mühlhauser, I. (2009) Comparison of a fall risk assessment tool with nurses’ judgement alone: a cluster‐randomized controlled trial. Age and Ageing, 38(4), 417–423. 10.1093/ageing/afp049 [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (2018) Assessment and prevention of falls in older people. Retrieved from www.nice.org.uk/guidance/cg161 [PubMed] [Google Scholar]
- Rapp, K. , Becker, C. , Cameron, I.D. , Konig, H.H. & Buchele, G. (2012) Epidemiology of falls in residential aged care: Analysis of more than 70,000 falls from residents of Bavarian nursing homes. Journal of the American Medical Directors Association, 13(2), 187.e1–187.e6. 10.1016/j.jamda.2011.06.011 [DOI] [PubMed] [Google Scholar]
- Registered Nurses’ Association of Ontario (2017) Preventing falls and reducing injury from falls, 4th edition. Toronto, ON: Registered Nurses Association of Ontario. Retrieved from https://rnao.ca/bpg/guidelines/prevention‐falls‐and‐fall‐injuries [Google Scholar]
- Sakamoto, Y. , Ebihara, S. , Ebihara, T. , Tomita, N. , Toba, K. , Freeman, S. et al. (2012) Fall prevention using olfactory stimulation with lavender odor in elderly nursing home residents: a randomized controlled trial. Journal of the American Geriatrics Society, 60(6), 1005–1011. 10.1111/j.1532-5415.2012.03977.x [DOI] [PubMed] [Google Scholar]
- World Health Organization (2018) Falls key facts. Retrieved from https://www.who.int/news‐room/fact‐sheets/detail/falls [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


