Abstract
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic has lasted for two years and caused millions of infections and deaths in humans. Although the origin of SARS-CoV-2 infection in humans remains unknown, infection in animals has been frequently reported in varieties of animals all over the world. Both experimental and natural infections of SARS-CoV-2 in different animal species provide useful information on viral host range and pathogenicity. As the pandemic continues to evolve, SARS-CoV-2 infection in animals will be expanding. In this review, we summarized SARS-CoV-2 testing and infection in animals as well as SARS-CoV-2 strains and transmission in animals. Current data showed that at least 18 different animal species tested positive for SARS-CoV-2. These 18 animal species belong to pet, captive, farmed, and wild animals. Fifteen of the eighteen animal species were known to be positive for the Delta variant and ten animal species were infected with two different types of variants. Human-to-animal, animal-to-animal, and animal-to-human transmission events were suggested in different outbreaks involved in animal infection with SARS-CoV-2. Continued testing, immunization, and surveillance are warranted.
Keywords: SARS-CoV-2, testing, animal species, infection, strain, transmission route
1. Introduction
Coronavirus disease 2019 (COVID-19) was first reported in humans in Wuhan, China in December 2019, and is caused by severe acute respiratory syndrome (SARS) coronavirus 2 (SARS-CoV-2). COVID-19 causes different types of presentations ranging from asymptomatic/mild symptoms to severe illness and mortality. Common COVID-19 symptoms include fever, cough, shortness of breath, malaise, and respiratory distress. As of 5 March 2022, the SARS-CoV-2 global pandemic has caused the infection of over 443 million people and over 6 million deaths. The origin of SARS-CoV-2 remains unclear. The current evidence shows that SARS-CoV-2 could be a bat-origin coronavirus since it has the highest shared identity (96%) with a bat coronavirus RaTG13 strain [1]. Whether SARS-CoV-2 jumps directly from bats to humans or through an intermediate host remains to be determined. The animal species that are susceptible to SARS-CoV-2 also remains unclear.
Coronaviridae is a large family consisting of four genera, with seven human coronaviruses and varieties of animal coronavirus species. The first coronavirus discovered was the infectious bronchitis virus in chickens in the 1930s [2]. Research on coronaviruses has been increasing, with three coronavirus pandemics in humans (SARS-CoV in 2003, Middle East respiratory syndrome coronavirus (MERS-CoV) in 2012, and SARS-CoV-2 in 2020) in the past two decades. Over the past two years of the SARS-CoV-2 pandemic, several animals have tested SARS-CoV-2 positive. In this review, SARS-CoV-2, SARS-CoV-2 testing in animals, SARS-CoV-2 infection in animals, SARS-CoV-2 strains in animals, and SARS-CoV-2 transmission routes will be reviewed.
2. SARS-CoV-2
SARS-CoV-2 is a single-stranded, positive-sense, enveloped RNA virus. It belongs to lineage B betacoronavirus in the family of Coronaviridae. SARS-CoV-2 was originally identified and characterized through next-generation sequencing [3]. Different from influenza, SARS-CoV, and MERS CoV, SARS-CoV-2 has a relatively higher basic reproductive rate (R0) and transmits more efficiently in hosts [4]. Coronaviruses utilize different receptors for binding to host cells, and SARS-CoV-2 uses the same Angiotensin-converting enzyme-2 (ACE2) receptor as SARS-CoV [5]. SARS-CoV-2 is continuously mutating in hosts, and different variants such as the Alpha, Delta, and Omicron variants have emerged in the field, which raises concerns about the effectiveness of the SARS-CoV-2 vaccine [6].
3. SARS-CoV-2 Testing in Animals
SARS-CoV-2 testing in animals includes the detection of active infection and of previous exposure. To detect active infection, a molecular polymerase chain reaction (PCR) assay, virus isolation, and antigen tests are used [7,8]. Real-time reverse transcription PCR is commonly used in the detection of SARS-CoV-2 in animals such as cats [9,10], dogs [11], and large cats [7,8,12,13]. In addition, antigen tests and virus isolation were also used for case investigation of SARS-CoV-2 in animals [7,8]. Different from PCR with a higher sensitivity, it was shown that the antigen test has a higher specificity and produces fewer false positives [14]. Other than these routine test methods, sequencing, including next-generation sequencing, is usually utilized to characterize strains involved in the outbreaks [7,8,12].
In terms of testing previous exposure to SARS-CoV-2, the virus neutralization test (VNT), surrogate virus neutralization test (sVNT), and enzyme-linked immunosorbent assay (ELISA) have been used for the evaluation of antibody immune responses. VNT requires a biosafety level 3 (BSL3) laboratory. Different from conventional VNT, sVNT utilizes the interaction of SARS-CoV-2 receptor binding domain and ACE2, which will be blocked by specific viral antibodies in serum samples [15]. The sVNT assay skips the requirement of BSL3 and can be applied to different animal species. ELISA has been reported to determine antibody responses in animals [16,17]. A commercial double antigen multi-species ELISA was used for the detection of antibodies against the N protein for any type of susceptible animal species [16]. An in-house developed species-specific ELISA was also applied for the detection of SARS-CoV-2 antibodies [17].
4. SARS-CoV-2 Infection in Animals
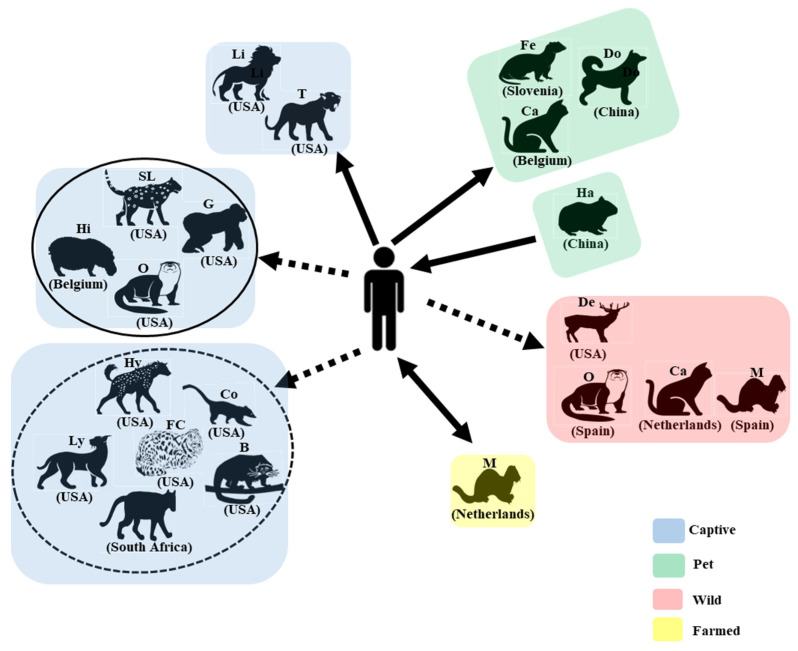
SARS-CoV-2 infection in animals is either asymptomatic or causes symptoms ranging from mild respiratory and gastroenteric signs to pneumonia and death. Two months after COVID-19 was reported, SARS-CoV-2 was first detected in dogs from households with positive owners in Hong Kong [11]. In March 2020, it was first reported that a domestic cat caught the SARS-CoV-2 infection, possibly through its owner who first tested SARS-CoV-2 positive in Belgium [9]. SARS-CoV-2 was detected in the nasopharyngeal swab, vomitus, and feces of the cat, and the cat developed clinical signs including vomiting, lethargy, poor appetite to anorexia, diarrhea, sneezing, coughing, and labored breathing. Following that, tigers and lions were found to be SARS-CoV-2 positive in the Bronx Zoo in New York, USA. Four tigers and three lions developed clinical signs of dry coughing and sneezing [7]. Sequence analysis suggested a potential human-to-tiger transmission. Other captive animals first found to be SARS-CoV-2 positive included a puma in South Africa in July 2020 [13]; a snow leopard (December 2020), a gorilla (January 2021), an otter (April 2021), a hyena, a fishing cat, a binturong, a coatimundi (October 2021), and a lynx (December 2021) in the USA; and hippo in Belgium in December 2021 (Figure 1). Farmed minks were first found to be SARS-CoV-2 positive in the Netherlands in April and May 2020 [18]. Since then, SARS-CoV-2 has been detected in minks in hundreds of mink farms in 14 countries (Figure 2). Other pet animals, including domestic ferrets and hamsters, also tested positive in Slovenia in November 2020 and in China in January 2022, respectively [19,20]. Other than domestic, captive, and farmed animals, SARS-CoV-2 in wild animals including deer, feral minks, feral cats, and wild otters were reported in the USA, Spain, the Netherlands, and Spain, respectively [21,22,23,24] (Figure 1). Since the first detection in these animals in different countries, SARS-CoV-2 has been detected in gorillas in the Netherlands, tigers and lions in European countries, cougars in the USA and Argentina, a domestic ferret in the USA, dogs and cats in many countries, and deer in Canada (Figure 2).
Figure 1.
SARS-CoV-2-positive animal species are divided into four different categories: captive, pet, wild, and farmed animals. Countries in which these animals first tested SARS-CoV-2 positive are provided. Solid arrows indicate that evidence supports transmission between humans and animals, and dashed arrows suggest potential transmission. Animal species in the captive group with a dashed circle are from zoos with other animals positive for SARS-CoV-2, while those in the captive group with a solid circle are from zoos with only a single species testing positive. B: binturong; Ca: cat; Co: coatimundi; De: deer; Do: dog; Fe: ferret; FC: fishing cat; G: gorilla; Ha: hamster; Hi: Hippo; Hy: hyena; Li: lion; Ly: lynx; M: mink; O: otter, P: puma; SL: snow leopard; T: tiger.
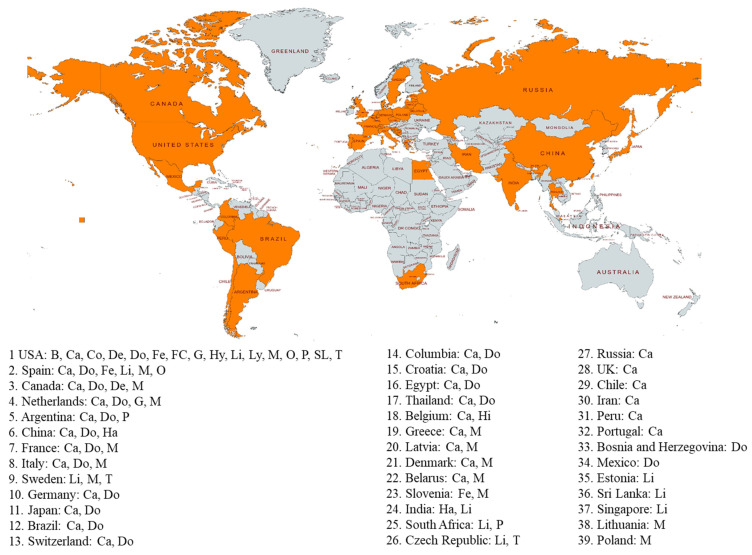
Figure 2.
Countries with positive SARS-CoV-2 animals are marked with orange color. Animal species positive for SARS-CoV-2 in each country are provided. Until 12 May 2022, a total of 39 countries had animals that tested positive for SARS-CoV-2. B: binturong; Ca: cat; Co: coatimundi; De: deer; Do: dog; Fe: ferret; FC: fishing cat; G: gorilla; Ha: hamster; Hi: Hippo; Hy: hyena; Li: lion; Ly: lynx; M: mink; O: otter; P: puma; SL: snow leopard; T: tiger.
In summary, SARS-CoV-2 has been detected in 18 different animal species from ten families (Felida, Viverridae, Hyaenidae, Canidae, Mustelidae, Procyonidae, Cervidae, Hippopotamidae, Hominidae, and Cricetidae) of four animal orders (Carnivora, Artiodactyla, Primates, and Rodentia). These 18 animal species consist of pet (dog, cat, ferret, and hamster), captive (tiger, lion, snow leopard, cougar, lynx, fishing cat, binturong, hyena, otter, coatimundi, hippo, and gorilla), farmed (mink), and wild (deer, wild otter, feral mink, and cat) animals (Figure 1). The USA has 16 animal species that have tested positive for SARS-CoV-2, followed by Spain with six positive species, two countries (Canada and Netherlands) with four animal species, five countries (Argentina, China, France, Italy, and Sweden) with three positive species, 17 countries with two positive animal species (no. 10 to no. 26), and 13 countries with one positive animal species (no. 27 to no. 39) (Figure 2).
5. SARS-CoV-2 Strains in Animals
Similarly to other RNA viruses, SARS-CoV-2 continuously mutates in its hosts, resulting in new variants including Alpha, Beta, Gamma, Omicron, Lambda, and Mu GH. Some (Alpha, Beta, Gamma, and Omicron) are Variants of Concern (VOCs), while others are Variants of Interest (VOIs: Lambda, Mu GH) or Variants Under Monitoring (VUM: GU/490R). Based on the GISAID database [25] accessed on 12 May 2022, there are sequences available for 15 of the 18 animal species (no sequence for coatimundi, lynx, and cougar) (Table 1). Since most of animal SARS-CoV-2 cases were due to human-to-animal transmission events, strains in animals were non-variant in the earlier period, and then, variants in the latter stage of the pandemic. The Delta variant was predominantly detected in all 15 of the animal species (Table 1). Six animal species (ferret, hippo, hyena, fishing cat, and binturong) were only infected by the Delta variant, whereas ten animal species (cat, dog, mink, deer, tiger, lion, snow leopard, gorilla, hamster, and Otter) were infected by more than one type of variant, and eight animal species (dog, cat, mink, deer, tiger, lion, snow leopard, and gorilla) were also infected by non-variant strains. Cats were infected by five variants: Alpha, Delta, Gamma, Lambda, and Omicron; deer were infected by four variants: Alpha, Delta, Gamma, and Omicron; dogs and minks were infected by Alpha, Delta, and Omicron; tigers, lions, gorillas, and otters were infected by the Alpha and Delta variants; hamsters were infected by the Delta and Omicron variants; and snow leopards were infected by the Delta and Mu GH variants (Table 1).
Table 1.
Number of sequences of variant and nonvariant strains of SARS-CoV-2 in 18 animal species. GISAID SARS-CoV-2 sequence database was accessed on 12 May 2022. NA: not available; Non-Var: non-variant.
| Species | Total | Alpha | Delta | Gamma | Omicron | Lambda | MU GH | Non-Var |
|---|---|---|---|---|---|---|---|---|
| Cat | 140 | 11 | 27 | 1 | 5 | 3 | 93 | |
| Deer | 159 | 3 | 38 | 1 | 4 | 113 | ||
| Mink | 1366 | 6 | 60 | 2 | 1298 | |||
| Dog | 84 | 5 | 24 | 7 | 48 | |||
| Lion | 74 | 3 | 42 | 29 | ||||
| Tiger | 43 | 3 | 27 | 13 | ||||
| Gorilla | 15 | 2 | 12 | 1 | ||||
| Otter | 8 | 5 | 3 | |||||
| Hamster | 24 | 12 | 12 | |||||
| Snow Leopard | 9 | 4 | 4 | 1 | ||||
| Binturong | 1 | 1 | ||||||
| Hyena | 1 | 1 | ||||||
| Ferret | 1 | 1 | ||||||
| Hippo | 1 | 1 | ||||||
| Fishing Cat | 1 | 1 | ||||||
| Lynx | NA | |||||||
| Cougar | NA | |||||||
| Coatimundi | NA |
6. SARS-CoV-2 Transmission Routes
Since the first case of animal infection with SARS-CoV-2 in 2020, much effort has been put into tracking the infection sources in animals, which is the key to controlling infection in them. Several lines of evidence suggest that infection in dogs [11,16,26,27], cats [9], large cats [7,8,12,13], and domestic ferrets [19] were due to human-to-animal transmissions (Figure 1). In the case of the farmed minks, it was reported that minks were infected through a human-to-mink transmission route [18]; then, infected minks transmitted the virus back to humans [28] (Figure 1). Infected hamster-to-human transmission has also been suggested in Hong Kong [29] (Figure 1). Although the exact mechanism by which deer caught the SARS-CoV-2 remains unclear, the findings from one previous study indicated that human-to-deer and deer-to-deer transmission events could occur [21]. Animal-to-animal transmission events in other animal species are highly possible as long as two or more animals are involved in the outbreaks. Feral cats testing positive for SARS-CoV-2 could contract it through mink-to-cat or cat-to-cat transmission events [23]. Unlike infections in pet, captive, and farmed animals, it is more difficult to trace and control infections in wild animals, and how these wild animals caught the virus remains unclear. These wild animals (deer, mink, and otter) could catch the virus through a contaminated environment (such as water) and close contact with domestic animals and humans.
7. Conclusions
SARS-CoV-2 infection in animals has become complicated since different types of animals have tested positive for SARS-CoV-2. There are different strategies used to control infections in animals and humans, including culling farmed animals, the isolation of infected pet and captive animals, and the vaccination of captive animals. In 2021, lots of zoo animals were immunized with a recombinant vaccine donated by the Zoetis company. There is also a commercial SARS-CoV-2 animal vaccine, Carnivac-Cov, available in Russia. This vaccine is designed for carnivores [30]. Surveillance of SARS-CoV-2 in wild animals has been conducted in Europe and America [21,22,23,24,31], and the control of SARS-CoV-2 infection in wild animals is quite challenging. A possible approach for controlling SARS-CoV-2 in wildlife is the application of an oral vaccine to them, which is similar to the strategy used to control rabies in wildlife.
Acknowledgments
The authors sincerely appreciate the researchers worldwide who sequenced and shared the complete genome data of SARS-CoV-2 in animal strains from GISAID (https://www.gisaid.org/ (accessed on 12 May 2022)).
Author Contributions
Writing—original draft preparation, S.C. and P.Y.; writing—review and editing, S.C., Y.L., J.Z., X.P., G.L., W.S., Y.P., D.Z., P.Y. and Q.W.; supervision, P.Y.; project administration, S.C.; All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this manuscript are available in Figure 2 and Table 1.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by the Special Research Project of Capital Health Development from Beijing Municipal Health Commission [2022-1G-3014], by the Collaboration Project (2020-jk-cd-019) from Beijing CDC, and by the Beijing Science and Technology Planning Project from Beijing Municipal Science and Technology Commission (Z211100002521019, Z211100002521015).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., Si H.R., Zhu Y., Li B., Huang C.L., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schalk A.F., Hawn M.C. An apparently new respiratory disease of baby chicks. J. Am. Vet. Med. Assoc. 1931;78:413–423. [Google Scholar]
- 3.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petersen E., Koopmans M., Go U., Hamer D.H., Petrosillo N., Castelli F., Storgaard M., Al Khalili S., Simonsen L. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect. Dis. 2020;20:e238–e244. doi: 10.1016/S1473-3099(20)30484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medina-Enriquez M.M., Lopez-Leon S., Carlos-Escalante J.A., Aponte-Torres Z., Cuapio A., Wegman-Ostrosky T. ACE2: The molecular doorway to SARS-CoV-2. Cell Biosci. 2020;10:148. doi: 10.1186/s13578-020-00519-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petersen E., Ntoumi F., Hui D.S., Abubakar A., Kramer L.D., Obiero C., Tambyah P.A., Blumberg L., Yapi R., Al-Abri S., et al. Emergence of new SARS-CoV-2 Variant of Concern Omicron (B.1.1.529)—highlights Africa’s research capabilities, but exposes major knowledge gaps, inequities of vaccine distribution, inadequacies in global COVID-19 response and control efforts. Int. J. Infect. Dis. 2022;114:268–272. doi: 10.1016/j.ijid.2021.11.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McAloose D., Laverack M., Wang L., Killian M.L., Caserta L.C., Yuan F., Mitchell P.K., Queen K., Mauldin M.R., Cronk B.D., et al. From People to Panthera: Natural SARS-CoV-2 Infection in Tigers and Lions at the Bronx Zoo. mBio. 2020;11:e02220-20. doi: 10.1128/mBio.02220-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernandez-Bellon H., Rodon J., Fernandez-Bastit L., Almagro V., Padilla-Sole P., Lorca-Oro C., Valle R., Roca N., Grazioli S., Trogu T., et al. Monitoring Natural SARS-CoV-2 Infection in Lions (Panthera leo) at the Barcelona Zoo: Viral Dynamics and Host Responses. Viruses. 2021;13:1683. doi: 10.3390/v13091683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garigliany M., Van Laere A.S., Clercx C., Giet D., Escriou N., Huon C., van der Werf S., Eloit M., Desmecht D. SARS-CoV-2 Natural Transmission from Human to Cat, Belgium, March 2020. Emerg. Infect. Dis. 2020;26:3069–3071. doi: 10.3201/eid2612.202223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lenz O.C., Marques A.D., Kelly B.J., Rodino K.G., Cole S.D., Perera R., Weiss S.R., Bushman F.D., Lennon E.M. SARS-CoV-2 Delta Variant (AY.3) in the Feces of a Domestic Cat. Viruses. 2022;14:421. doi: 10.3390/v14020421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sit T.H.C., Brackman C.J., Ip S.M., Tam K.W.S., Law P.Y.T., To E.M.W., Yu V.Y.T., Sims L.D., Tsang D.N.C., Chu D.K.W., et al. Infection of dogs with SARS-CoV-2. Nature. 2020;586:776–778. doi: 10.1038/s41586-020-2334-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grome H.N., Meyer B., Read E., Buchanan M., Cushing A., Sawatzki K., Levinson K.J., Thomas L.S., Perry Z., Uehara A., et al. SARS-CoV-2 Outbreak among Malayan Tigers and Humans, Tennessee, USA, 2020. Emerg. Infect. Dis. 2022;28:833–836. doi: 10.3201/eid2804.212219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koeppel K.N., Mendes A., Strydom A., Rotherham L., Mulumba M., Venter M. SARS-CoV-2 Reverse Zoonoses to Pumas and Lions, South Africa. Viruses. 2022;14:120. doi: 10.3390/v14010120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Currie D.W., Shah M.M., Salvatore P.P., Ford L., Whaley M.J., Meece J., Ivacic L., Thornburg N.J., Tamin A., Harcourt J.L., et al. Relationship of SARS-CoV-2 Antigen and Reverse Transcription PCR Positivity for Viral Cultures. Emerg. Infect. Dis. 2022;28:717–720. doi: 10.3201/eid2803.211747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tan C.W., Chia W.N., Qin X., Liu P., Chen M.I., Tiu C., Hu Z., Chen V.C., Young B.E., Sia W.R., et al. A SARS-CoV-2 surrogate virus neutralization test based on antibody-mediated blockage of ACE2-spike protein-protein interaction. Nat. Biotechnol. 2020;38:1073–1078. doi: 10.1038/s41587-020-0631-z. [DOI] [PubMed] [Google Scholar]
- 16.Goletic S., Goletic T., Softic A., Zahirovic A., Rukavina D., Kavazovic A., Omeragic J., Umihanic S., Hukic M. The Evidence of SARS-CoV-2 Human-to-Pets Transmission in Household Settings in Bosnia and Herzegovina. Front. Genet. 2022;13:839205. doi: 10.3389/fgene.2022.839205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhao S., Schuurman N., Li W., Wang C., Smit L.A.M., Broens E.M., Wagenaar J.A., van Kuppeveld F.J.M., Bosch B.J., Egberink H. Serologic Screening of Severe Acute Respiratory Syndrome Coronavirus 2 Infection in Cats and Dogs during First Coronavirus Disease Wave, the Netherlands. Emerg. Infect. Dis. 2021;27:1362–1370. doi: 10.3201/eid2705.204055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oreshkova N., Molenaar R.J., Vreman S., Harders F., Oude Munnink B.B., Hakze-van der Honing R.W., Gerhards N., Tolsma P., Bouwstra R., Sikkema R.S., et al. SARS-CoV-2 infection in farmed minks, the Netherlands, April and May 2020. Eurosurveillance. 2020;25:2001005. doi: 10.2807/1560-7917.ES.2020.25.23.2001005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Racnik J., Kocevar A., Slavec B., Korva M., Rus K.R., Zakotnik S., Zorec T.M., Poljak M., Matko M., Rojs O.Z., et al. Transmission of SARS-CoV-2 from Human to Domestic Ferret. Emerg. Infect. Dis. 2021;27:2450–2453. doi: 10.3201/eid2709.210774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kok K.H., Wong S.C., Chan W.M., Wen L., Chu A.W., Ip J.D., Lee L.K., Wong I.T., Lo H.W., Cheng V.C., et al. Co-circulation of two SARS-CoV-2 variant strains within imported pet hamsters in Hong Kong. Emerg. Microbes Infect. 2022;11:689–698. doi: 10.1080/22221751.2022.2040922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hale V.L., Dennis P.M., McBride D.S., Nolting J.M., Madden C., Huey D., Ehrlich M., Grieser J., Winston J., Lombardi D., et al. SARS-CoV-2 infection in free-ranging white-tailed deer. Nature. 2022;602:481–486. doi: 10.1038/s41586-021-04353-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aguilo-Gisbert J., Padilla-Blanco M., Lizana V., Maiques E., Munoz-Baquero M., Chillida-Martinez E., Cardells J., Rubio-Guerri C. First Description of SARS-CoV-2 Infection in Two Feral American Mink (Neovison vison) Caught in the Wild. Animals. 2021;11:1422. doi: 10.3390/ani11051422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Aart A.E., Velkers F.C., Fischer E.A.J., Broens E.M., Egberink H., Zhao S., Engelsma M., Hakze-van der Honing R.W., Harders F., de Rooij M.M.T., et al. SARS-CoV-2 infection in cats and dogs in infected mink farms. Transbound. Emerg. Dis. 2021 doi: 10.1111/tbed.14173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Padilla-Blanco M., Aguilo-Gisbert J., Rubio V., Lizana V., Chillida-Martinez E., Cardells J., Maiques E., Rubio-Guerri C. The Finding of the Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV-2) in a Wild Eurasian River Otter (Lutra lutra) Highlights the Need for Viral Surveillance in Wild Mustelids. Front. Vet. Sci. 2022;9:826991. doi: 10.3389/fvets.2022.826991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elbe S., Buckland-Merrett G. Data, disease and diplomacy: GISAID’s innovative contribution to global health. Glob. Chall. 2017;1:33–46. doi: 10.1002/gch2.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patterson E.I., Elia G., Grassi A., Giordano A., Desario C., Medardo M., Smith S.L., Anderson E.R., Prince T., Patterson G.T., et al. Evidence of exposure to SARS-CoV-2 in cats and dogs from households in Italy. Nat. Commun. 2020;11:6231. doi: 10.1038/s41467-020-20097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rivero R., Garay E., Botero Y., Serrano-Coll H., Gastelbondo B., Munoz M., Ballesteros N., Castaneda S., Patino L.H., Ramirez J.D., et al. Human-to-dog transmission of SARS-CoV-2, Colombia. Sci. Rep. 2022;12:7880. doi: 10.1038/s41598-022-11847-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oude Munnink B.B., Sikkema R.S., Nieuwenhuijse D.F., Molenaar R.J., Munger E., Molenkamp R., van der Spek A., Tolsma P., Rietveld A., Brouwer M., et al. Transmission of SARS-CoV-2 on mink farms between humans and mink and back to humans. Science. 2021;371:172–177. doi: 10.1126/science.abe5901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yen H.L., Sit T.H.C., Brackman C.J., Chuk S.S.Y., Gu H., Tam K.W.S., Law P.Y.T., Leung G.M., Peiris M., Poon L.L.M., et al. Transmission of SARS-CoV-2 delta variant (AY.127) from pet hamsters to humans, leading to onward human-to-human transmission: A case study. Lancet. 2022;399:1070–1078. doi: 10.1016/S0140-6736(22)00326-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chavda V.P., Feehan J., Apostolopoulos V. A Veterinary Vaccine for SARS-CoV-2: The First COVID-19 Vaccine for Animals. Vaccines. 2021;9:631. doi: 10.3390/vaccines9060631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moreira-Soto A., Walzer C., Czirjak G.A., Richter M.H., Marino S.F., Posautz A., De Yebra Rodo P., McEwen G.K., Drexler J.F., Greenwood A.D. Serological Evidence That SARS-CoV-2 Has Not Emerged in Deer in Germany or Austria during the COVID-19 Pandemic. Microorganisms. 2022;10:748. doi: 10.3390/microorganisms10040748. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this manuscript are available in Figure 2 and Table 1.