Abstract
Introduction
Understanding educational patterns in excess mortality during the coronavirus disease 2019 (COVID-19) pandemic may help to identify strategies to reduce disparities. It is unclear whether educational inequalities in COVID-19 mortality have persisted throughout the pandemic, spanned the full range of educational attainment, or varied by other demographic indicators of COVID-19 risks, such as age or occupation.
Methods
This study analyzed individual-level California Department of Public Health data on deaths occurring between January 2016 and February 2021 among individuals aged ≥25 years (1,502,202 deaths). Authors applied ARIMA (autoregressive integrated moving average) models to subgroups defined by the highest level of education and other demographics (age, sex, race/ethnicity, U.S. nativity, occupational sector, and urbanicity). Authors estimated excess deaths (the number of observed deaths minus the number of deaths expected to occur under the counterfactual of no pandemic) and excess deaths per 100,000 individuals.
Results
Educational inequalities in excess mortality emerged early in the pandemic and persisted throughout the first year. The greatest per-capita excess occurred among people without high-school diplomas (533 excess deaths/100,000), followed by those with a high-school diploma but no college (466/100,000), some college (156/100,000), and bachelor's degrees (120/100,000), and smallest among people with graduate/professional degrees (101/100,000). Educational inequalities occurred within every subgroup examined. For example, per-capita excess mortality among Latinos with no college experience was 3.7 times higher than among Latinos with at least some college experience.
Conclusions
Pervasive educational inequalities in excess mortality during the pandemic suggest multiple potential intervention points to reduce disparities.
INTRODUCTION
Educational inequalities prevail in numerous measures of morbidity and mortality,1, 2, 3, 4 including during the coronavirus disease 2019 (COVID-19) pandemic. Evidence from California documented educational inequalities in excess mortality during the pandemic (i.e., the discrepancy between the observed number of deaths and the expected number of deaths under the counterfactual of no pandemic).5 ‒ 7 National data also showed large disparities in all-cause mortality during the pandemic between those with and without college degrees.5 , 6 This previous work documented education as a driver of pandemic-related health inequities but left critical unanswered questions. Unanswered questions include whether educational differences in COVID-19 mortality persisted throughout the pandemic, spanned the full range of educational attainment, or varied by other demographic indicators of risk.
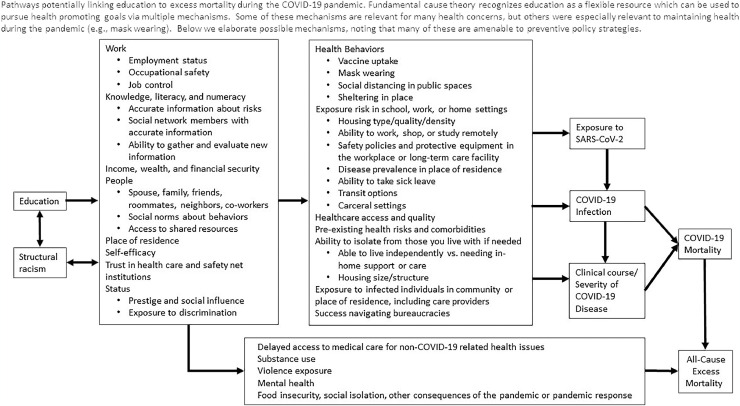
Consistent with Fundamental Cause Theory,8 education may influence pandemic-related mortality through multiple mechanisms (Figure 1 ). Education influences work, health literacy, financial security, social networks, place of residence, and access to institutional resources. These factors may have consequences for risk of exposure, infection, or severe illness from severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2). Learning about those mechanisms is an essential step in reducing inequalities.
Figure 1.
A conceptual model for the relationship between educational attainment and COVID-19 mortality, based on Link and Phelan's Theory of Fundamental Causes.
This study addresses 3 questions about educational inequalities in excess mortality, with the goal of understanding how and why education influences mortality. First, it assesses whether educational inequalities in excess mortality persisted throughout the pandemic, even as more was learned about effective preventive measures. Second, it evaluates whether disparities across levels of educational attainment are apparent across finer educational gradients. Finally, it quantifies disparities in excess mortality across subgroups for whom different mechanisms are most relevant, such as those defined by race/ethnicity, occupation, or age.
METHODS
Study Sample
The study uses data obtained on all deaths occurring on or after January 1, 2016 through February 28, 2021. The study was approved by the State of California Committee for the Protection of Human Subjects. The analysis was restricted to decedents aged ≥25 years to remove individuals who were too young to receive a college degree under traditional timelines. Analyses of occupational sector were restricted to decedents aged 25‒65 years. The pandemic period of interest was defined as March 1, 2020 through February 28, 2021.
Measures
The study defined 5 levels of educational attainment as reported on the death certificates. In some analyses, education was collapsed into 2 groups: at least some college experience or not. This decision was based on evidence that educational differences in per-capita excess mortality were most pronounced between those with and those without college experience.9
Race/ethnicity was conceptualized as a marker of exposure to structural racism and categorized into 4 groups: Asian, Black, Latino, and White. Occupational sector was defined by first converting free-text values to standardized occupational codes using an automated system. These occupation codes were then manually assigned to sectors by a team of 3 researchers.10 , 11 This manuscript uses the term sector rather than industry to maintain consistency with California's definition and to avoid confusion because the groups are not based on National Institute for Occupational Safety and Health industry codes. Urbanicity was defined using a ZIP code‒level measure updated to 202012 and dichotomized as metropolitan areas versus not metropolitan.
Missing values occurred among <3% of decedents for variables of interest, including in doubly stratified analyses; for education, this percentage was 2.7%. Records with missing values were excluded using a complete-case approach.
Statistical Analysis
For each group of interest, the following procedure was repeated. The data were aggregated by weeks. As in previous work,9 , 11 time-series models were fit for the number of weekly all-cause deaths.13 These models were used to forecast the number of expected deaths; the number of excess deaths was estimated by subtracting the number of expected deaths from the number of observed deaths. Because this study estimates excess mortality separately for each group of interest, it is possible for sums across groups to be slightly discrepant with the total (e.g., it is possible for the number of excess deaths in each age group to not sum exactly to the estimated number of excess deaths among all individuals). To address this issue and to facilitate comparisons, the authors standardized the estimated number of group-specific excess deaths to relevant totals.
The study additionally reports per-capita excess deaths: the observed number of deaths minus the expected number of deaths divided by the population size (obtained from the 2019 American Community Survey). Both relative (through division) and absolute (through subtraction) measures of inequalities were calculated. Most reference groups were defined as the group with the lowest risk, but for education, bachelor's degree was selected as the reference instead of graduate degree to improve comparability with other research. In further analyses, the study compared per-capita excess mortality between individuals with and those without at least some college experience, among various subgroups.
All analyses were conducted in R, Version 4.04. Statistical analysis was conducted between May and October 2021.
The study estimates excess mortality using all-cause mortality because COVID-19 deaths are widely recognized to be underreported,14 and this underreporting might differ across levels of education.
RESULTS
Per 100,000 individuals, there were 967, 978, 957, 973, and 1,254 all-cause deaths in 2016 through 2020, with years redefined to begin on March 1 and end on the last day of February. Among individuals aged ≥25 years, an estimated 76,897 (95% prediction interval [PI]=69,798, 84,039) excess deaths occurred over the first full year of the COVID-19 pandemic (Table 1 ), with an estimated 45,356 (95% PI=42,784, 47,979) excess deaths during the fourth quarter of the year (coinciding with the 2020–2021 winter pandemic surge). Among groups defined by education, excess deaths were highest among individuals with no high-school degree (24,634, 95% PI=23,183, 26,098) and among individuals with a high-school diploma but no college experience (27,830, 95% PI=26,239, 29,437). Per-capita excess mortality was 575 (95% PI=541, 609) per 100,000 among individuals with no high-school degree and 502 (95% PI=473, 531) per 100,000 among individuals with a high-school diploma but no college experience. The elevation in mortality appeared to decrease with increasing levels of education: individuals with a bachelor's degree experienced per-capita excess mortality of 130 (95% PI=112, 148) per 100,000 individuals and 109 (95% PI=73, 146) among those with a graduate or professional degree. The per-capita excess mortality in the lowest education group was 5.3 times the per-capita excess mortality in the highest education group, equating to an absolute difference of 466 deaths per 100,000 people.
Table 1.
Excess Mortality Among Californians Aged ≥25 Years, March 2020 Through February 2021
| Variables | Excess mortality (95% PI) |
Pairwise comparison (95% PI) |
|||
|---|---|---|---|---|---|
| Observed deaths | Excess deaths | Per-capita excessa | Differenceb | Ratioc | |
| Aged ≥25 years | 337,808 | 76,897 (69,798, 84,039) | 285 (259, 312) | ||
| Education | |||||
| No high-school diploma | 70,328 | 24,634 (23,183, 26,098) | 575 (541, 609) | 445 (429, 461) | 4.4 (4.1, 4.9) |
| High-school diploma | 114,835 | 27,830 (26,239, 29,437) | 502 (473, 531) | 372 (359, 385) | 3.9 (3.6, 4.3) |
| Some college | 71,444 | 12,914 (11,471, 14,366) | 168 (149, 187) | 38 (37, 40) | 1.3 (1.3, 1.3) |
| Bachelor's degree | 43,781 | 7,672 (6,597, 8,749) | 130 (112, 148) | ref | ref |
| Graduate/professional degree | 26,692 | 3,847 (2,566, 5,132) | 109 (73, 146) | −20 (−39 to −2) | 0.8 (0.7, 1.0) |
| Age, years | |||||
| 25–54 | 39,318 | 11,688 (11,149, 12,238) | 72 (68, 75) | ref | ref |
| 55–64 | 45,245 | 11,821 (11,334, 12,313) | 247 (236, 257) | 175 (168, 182) | 3.4 (3.4, 3.5) |
| 65–79 | 104,369 | 25,017 (23,463, 26,578) | 565 (530, 601) | 494 (462, 526) | 7.9 (7.7, 8.0) |
| ≥80 | 148,876 | 28,370 (25,703, 31,052) | 2,011 (1,822, 2,201) | 1,939 (1,753, 2,126) | 28.1 (26.7, 29.4) |
| Sex | |||||
| Male | 182,400 | 45,725 (41,280, 50,185) | 346 (313, 380) | 119 (98, 140) | 1.5 (1.5, 1.6) |
| Female | 155,406 | 31,171 (29,252, 33,112) | 227 (213, 241) | ref | ref |
| Race/ethnicity | |||||
| Asian | 36,692 | 9,410 (8,566, 10,254) | 218 (198, 237) | 1 (−22 to 25) | 1.0 (0.9, 1.1) |
| Black | 26,210 | 5,908 (5,284, 6,534) | 389 (348, 430) | 173 (171, 175) | 1.8 (1.7, 2.0) |
| Latino | 87,598 | 35,422 (32,683, 38,152) | 387 (357, 417) | 171 (157, 184) | 1.8 (1.6, 2.1) |
| White | 178,378 | 23,961 (19,275, 28,676) | 216 (174, 259) | ref | ref |
| Country of birth | |||||
| U.S. | 222,141 | 37,818 (34,986, 40,675) | 218 (202, 235) | ref | ref |
| Other | 115,667 | 39,078 (37,360, 40,799) | 406 (388, 424) | 187 (183, 192) | 1.9 (1.8, 1.9) |
| Sectord | |||||
| Facilities | 15,246 | 4,463 (4,252, 4,677) | 191 (182, 200) | 150 (145, 155) | 4.7 (4.5, 4.9) |
| Food/agriculture | 6,840 | 2,502 (2,293, 2,711) | 183 (168, 198) | 142 (131, 154) | 4.5 (4.4, 4.6) |
| Manufacturing | 5,140 | 1,639 (1,592, 1,688) | 156 (151, 160) | 115 (113, 116) | 3.8 (3.6, 4.1) |
| Transportation/logistic | 9,726 | 3,222 (2,998, 3,448) | 209 (195, 224) | 168 (157, 179) | 5.1 (5.0, 5.2) |
| Other essential | 15,717 | 3,816 (3,601, 4,034) | 76 (72, 80) | 35 (34, 35) | 1.9 (1.8, 1.9) |
| Not essential | 16,640 | 2,889 (2,624, 3,158) | 41 (37, 45) | ref | ref |
| Unemployed/missing | 15,254 | 4,233 (3,968, 4,503) | 134 (125, 142) | 93 (88, 98) | 3.3 (3.2, 3.4) |
| Urbanicity | |||||
| Metropolitan | 313,459 | 73,181 (66,626, 79,757) | 288 (262, 314) | 47 (35, 59) | 1.2 (1.1, 1.3) |
| Not metropolitan | 23,144 | 3,715 (3,222, 4,214) | 241 (209, 273) | ref | ref |
Defined as the observed number of deaths minus the expected number of deaths divided by the population size multiplied by 100,000.
Defined as the per-capita excess mortality in the group minus the per-capita excess mortality in the reference group.
Defined as the per-capita excess mortality in the group divided by the per-capita excess mortality in the reference group.
Analysis restricted to individuals aged 25–65 years.
PI, prediction interval.
Across other groups (besides those defined by education), per-capita excess mortality was relatively high among individuals aged 65–79 years (565, 95% PI=530, 601) or aged ≥80 years (2,011, 95% PI=1,822, 2,201) as well as Black (389, 95% PI=348, 430), Latino (387, 95% PI=357, 417), and foreign-born (406, 95% PI=388, 424) individuals. In analysis restricted to working-age individuals, per-capita excess mortality was relatively high among transportation/logistic workers (209, 95% PI=195, 224), facilities workers (191, 95% PI=182, 200), and food/agriculture workers (183, 95% PI=168, 198). Aside from the oldest age groups, no group had per-capita excess mortality exceeding that observed among individuals with no high-school diploma.
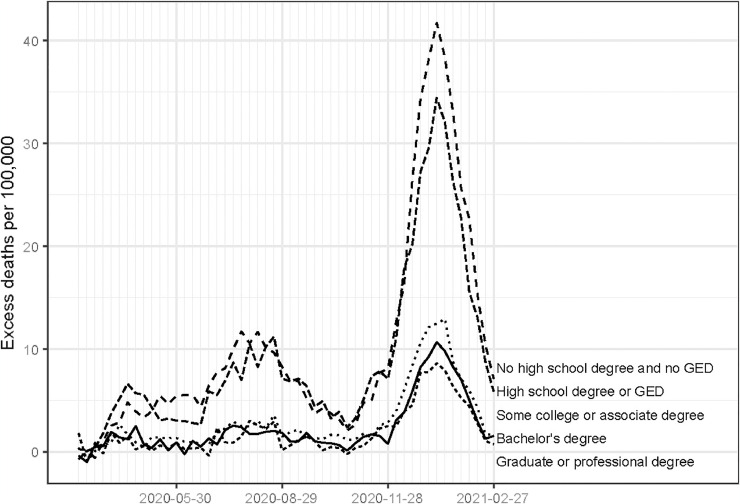
The educational gradient in per-capita excess mortality was established within the first month of the pandemic and persisted throughout the first year of the pandemic (Figure 2 ). Every education group experienced similar temporal trends, with peaks corresponding to California's first, second, and third waves of mortality (roughly March through May 2020, July through September 2020, and November 2020 through February 2021, respectively), but these surges were markedly attenuated for the groups with at least some college experience. Similarly, in analyses stratified by race/ethnicity (Appendix Figure 1, available online), per-capita excess mortality was consistently elevated among individuals with no college experience compared with that among individuals with at least some college experience.
Figure 2.
Per-capita excess mortality by levels of educational attainment, California, March 2020 through February 2021.
Table 2 shows—overall and within subgroups defined by age, sex, race/ethnicity, country of birth, and occupational sector—excess deaths, per-capita excess mortality, and absolute and relative measures of gaps in per-capita excess mortality comparing individuals with no college experience with individuals with at least some college experience. Among all Californians aged ≥25 years, per-capita excess mortality was higher among individuals without college experience by 388 (95% PI=377, 400) per 100,000 on an absolute scale or a factor of 3.7 (95% PI=3.5, 3.9) on a relative scale.
Table 2.
Excess Mortality Among Californians Aged ≥25 Years, March 2020 Through February 2021
| Variables | Per-capita excessa (95% PI) |
Pairwise comparison (95% PI) |
||
|---|---|---|---|---|
| No college | At least some college | Differenceb | Ratioc | |
| Aged ≥25 years | 532 (508, 556) | 144 (131, 157) | 388 (377, 400) | 3.7 (3.5, 3.9) |
| Age, years | ||||
| 25–54 | 148 (142, 154) | 30 (28, 32) | 118 (113, 121) | 5.0 (4.7, 5.0) |
| 55–64 | 470 (421, 520) | 97 (80, 114) | 373 (338, 402) | 4.8 (4.4, 5.1) |
| 65–79 | 1,040 (955, 1,125) | 288 (254, 322) | 752 (692, 792) | 3.6 (3.4, 3.6) |
| ≥80 | 2,677 (2,153, 3,203) | 1,461 (1,130, 1,792) | 1,216 (981, 1,347) | 1.8 (1.7, 1.8) |
| Sex | ||||
| Female | 443 (373, 514) | 112 (82, 141) | 331 (286, 366) | 4.0 (3.4, 4.3) |
| Male | 619 (578, 659) | 179 (152, 205) | 440 (417, 443) | 3.5 (3.0, 3.6) |
| Race/ethnicity | ||||
| Asian | 435 (385, 486) | 138 (121, 155) | 297 (257, 322) | 3.2 (3.0, 3.0) |
| Black | 722 (670, 774) | 236 (188, 284) | 486 (464, 480) | 3.1 (2.6, 3.4) |
| Latino | 538 (510, 566) | 146 (125, 168) | 392 (378, 388) | 3.7 (3.2, 3.9) |
| White | 531 (354, 708) | 135 (102, 167) | 396 (246, 531) | 3.9 (3.3, 4.0) |
| Country of birth | ||||
| U.S. | 462 (383, 541) | 123 (108, 139) | 338 (275, 403) | 3.7 (3.6, 3.9) |
| Other | 602 (572, 632) | 198 (186, 211) | 404 (387, 422) | 3.0 (3.0, 3.1) |
| Sectord | ||||
| Facilities | 284 (270, 297) | 80 (69, 92) | 203 (201, 205) | 3.5 (3.2, 3.9) |
| Food/agriculture | 270 (248, 293) | 81 (68, 94) | 189 (179, 200) | 3.3 (3.1, 3.7) |
| Manufacturing | 256 (241, 272) | 68 (54, 82) | 189 (187, 190) | 3.8 (3.3, 4.5) |
| Transportation/logistic | 319 (295, 344) | 98 (85, 111) | 221 (210, 233) | 3.3 (3.1, 3.5) |
| Other essential | 209 (201, 216) | 47 (43, 52) | 161 (158, 164) | 4.4 (4.1, 4.7) |
| Not essential | 148 (136, 160) | 26 (21, 31) | 122 (115, 129) | 5.7 (5.2, 6.5) |
| Unemployed/missing | 185 (175, 195) | 49 (42, 57) | 136 (133, 139) | 3.8 (3.4, 4.2) |
| Urbanicity | ||||
| Metropolitan | 537 (518, 557) | 144 (129, 159) | 393 (389, 403) | 3.7 (3.6, 4.1) |
| Not metropolitan | 454 (353, 554) | 143 (116, 170) | 310 (238, 389) | 3.2 (3.0, 3.4) |
Defined as the observed number of deaths minus the expected number of deaths divided by the population size multiplied by 100,000.
Defined as the per-capita excess mortality among individuals with college experience minus the per-capita excess mortality among individuals without college experience.
Defined as the per-capita excess mortality among individuals with college experience divided by the per-capita excess mortality among individuals without college experience.
Analysis restricted to individuals aged 25–65 years.
PI, prediction interval.
In every demographic subgroup evaluated, per-capita excess mortality was higher for individuals with no college than for those with at least some college. The largest absolute excesses occurred in high-risk subgroups (e.g., older individuals), and the largest relative excesses were observed in low-risk subgroups (e.g., younger individuals). For example, by age, the absolute measure of the educational gap was highest among individuals aged ≥80 years (1,216 per 100,000; 95% PI=981, 1,347), whereas the relative measure was highest among individuals aged 25–54 years (5.0; 95% PI=4.7, 5.0). By sex, the absolute educational gap was highest among males (440; 95% PI=417, 443), whereas the largest relative gap was among females (4.0; 95% PI=3.4, 4.3). Across racial/ethnic groups, the absolute measure of the educational gap was highest among Black Californians (486; 95% PI=464, 480), whereas the relative measure was highest among White Californians (3.9; 95% PI=3.3, 4.0). In analyses restricted to working-age individuals, the absolute comparison of per-capita excess mortality between individuals with and without at least some college experience was highest among transportation/logistic workers (221; 95% PI=210, 233), whereas the relative measure was highest among individuals not working in essential sectors (5.7; 95% PI=5.2, 6.5). By urbanicity, the largest absolute (393; 95% PI=389, 403) and relative (3.7; 95% PI=3.6, 4.1) gap was among those living in nonmetropolitan areas.
DISCUSSION
Using comprehensive mortality data from the state of California, the study finds persistent disparities in excess mortality across levels of education throughout the first year of the COVID-19 pandemic. Per-capita excess mortality showed an inverse gradient, with smaller excess mortality associated with each increment in education. The largest gap was between those with a high-school diploma or less and those who had at least some college. Educational inequalities were observed for every subgroup examined, including groups defined by age, sex, race/ethnic identity, U.S. nativity, occupational sector, and urbanicity. On a relative scale, low educational attainment was one of the strongest risk factors for excess mortality across the characteristics considered, superseded only by excess risk in the oldest age groups and some occupational sectors.
The findings extend an earlier California study showing inequalities in excess mortality by education during the first 6 months of the pandemic9; work using preliminary, aggregate national data to show educational gradients in COVID-19 mortality5 , 6; and a large body of research documenting inequalities in other health outcomes across educational groups.1 ‒ 4 This study fills several gaps in the literature, including extending data through the winter 2021 surge, finer gradations of education than previously reported, and evaluation of disparities across other demographic factors known to influence COVID-19 risk.
The magnitude of risk associated with low educational attainment is comparable with the heightened COVID-19 mortality risk associated with medical conditions such as diabetes,15, 16, 17, 18 immunosuppression,15 , 19 kidney disease,15 , 16 , 20 , 21 and lung disease.15 , 16 , 22 Educational inequalities were also comparable with or larger than other social inequalities. For example, the ratio of per-capita excess mortality among individuals working in the transportation/logistic sector compared with that among workers in nonessential sectors was 5.1, whereas the ratio of per-capita excess mortality among Californians with a high-school diploma only compared with that among those with a bachelor's degree was 3.9.
Large educational inequalities in pandemic-related mortality are consistent with the Theory of Fundamental Causes,7 which suggests that education influences resources, including knowledge, work, income, social networks, self-efficacy, trust, and status. These flexible resources shape health behaviors, exposure risk, healthcare access, comorbidities, the ability to isolate, exposure to infected individuals, and success in navigating bureaucracies, all of which determine the risk of SARS-CoV-2 infection and severity of illness among the infected (Figure 1). Because different subgroups would likely be differentially affected by specific pathways, observing inequalities in every subgroup suggests that multiple pathways are relevant, consistent with Fundamental Cause Theory. More detailed notes about the implications of each subgroup analysis and the trend tests are available in Appendix Table 1 (available online), and the most compelling implications are discussed below.
Fundamental Cause Theory recognizes that SES increases both access to accurate information about risk reduction and the capacity of individuals to take advantage of such information.23 Access to accurate information may be a crucial mechanism of educational inequalities during the pandemic.24 Public health messaging may not be adequately reaching individuals with lower educational attainment. Such groups have used fewer news resources during the COVID-19 pandemic and may be improperly informed about risk-minimization strategies.25, 26, 27, 28 Public health messaging regarding COVID-19 may have been difficult to follow.29, 30, 31 Low literacy may make individuals vulnerable to conflicting or inconsistent messages. Strong associations between education and adherence to individual protective behaviors may reflect inaccurate information or distrust of information sources.32 , 33
People with more education may have the status to command safe working conditions. Access to personal protective equipment has been low in many workplaces.34, 35, 36, 37 The relatively low excess mortality observed in healthcare settings may reflect access to personal protective equipment in those settings.5 , 6 Ventilation may be inadequate in settings where individuals with low educational attainment work, such as garment factories or meat-processing plants. An outbreak investigation in a meat-processing plant in Germany identified poor ventilation as a likely contributor.38
Prepandemic Bureau of Labor Statistics data indicated that only 4% of individuals without a high-school diploma could work from home, compared with 52% of individuals with a college degree.39 For any given set of work demands, more highly educated employees have greater decision latitude about how to meet those demands.40 , 41 Even within the same occupation or industry, education may enhance the likelihood that an employee has the power to modify their working conditions to enhance safety, for example, by increasing physical distance from coworkers or using personal protective equipment. Occupational safety enforcement that relies on worker complaints may exacerbate inequalities if low-education workers are least empowered to complain. In California, sectors with the highest excess pandemic-related mortality did not have the highest number of complaints to safety authorities.42
Household density may be an important mechanism of risk.29 Isolation or quarantine may be impossible in cramped housing.43 Resources to help people isolate are a possible solution. For example, through private donations, San Francisco has offered resources to individuals unable to safely isolate or quarantine.44 Similarly, the County of Santa Clara (California) offers motel rooms to those who need assistance.45
Infectious disease risk can quickly multiply through social networks because individuals often socialize with those of similar education.46 Low-wage essential workers, for example, may be more likely to socialize with, live with, and receive personal care from other essential workers and face more challenges in isolating after infection.44 , 47 Such stratification of social networks translates not just to sharing of risks but also, potentially, to sharing of knowledge and norms surrounding COVID-19 protections.25
Finally, the findings suggest that overlapping fundamental causes (Figure 1) result in particularly heightened risk. For example, Black people without college experience had 5.1 times the excess mortality of White people with college experience. Differential access to education is an important mechanism by which structural racism creates health inequities, and some mechanisms of educational inequalities are also relevant for racial/ethnic disparities in COVID-19.48, 49, 50
Prevention policies might effectively address multiple resources outlined in the theoretical framework. For example, sick leave can help to protect the financial resources of low-wage workers and reduce exposure in workplace settings.51 Although California mandated paid sick leave for reasons relating to COVID-19, this policy was not implemented until a year after the beginning of the pandemic and has not covered employees at small businesses.52
Limitations
Study limitations include the potential generalizability of findings to other areas. However, many of the processes leading to educational inequalities in California are likely commonplace. The study analyzed all-cause deaths rather than deaths with COVID-19 as a listed cause because COVID-19 deaths are widely understood to be underreported (COVID-19 deaths accounted for only 78% of excess deaths in this study, similar to previous reports).53, 54, 55 Some excess deaths however may have been indirectly caused by the pandemic or pandemic response; deaths due to some causes may also have declined during the pandemic. Further exploration of inequalities in specific non‒COVID-19 causes of death is warranted. The death certificate data may have inaccuracies—although previous research suggests that these inaccuracies may slightly underestimate educational inequalities.56 Death certificates do not include information on literacy or medical access.
Exclusion of records with missing values could in theory have biased the results, but only 4.0% of death certificates for Black individuals were missing information on education, compared with 1.9% among certificates for Asian decedents. These differences are quite small compared with the magnitude of excess deaths.
CONCLUSIONS
The COVID-19 pandemic had a devastating effect on California, hitting populations with low educational attainment particularly hard. The effects of the pandemic thus far likely extend beyond mortality, to bereavement,57, 58, 59 loss of caregivers, financial hardship,60 , 61 housing instability,62, 63, 64 and declining mental health.65, 66, 67 Recovery must include cross-sectoral partnerships to target mechanisms most relevant for populations with low educational attainment.
CREDIT AUTHOR STATEMENT
Yea-Hung Chen: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Visualization, Writing – original draft, Writing – review & editing. Ellicott C. Matthay: Conceptualization, Investigation, Methodology, Writing – review & editing. Ruijia Chen: Investigation, Methodology, Writing – review & editing. Michelle A. DeVost: Investigation, Visualization, Writing – review & editing. Kate A. Duchowny: Investigation, Writing – review & editing. Alicia R. Riley: Investigation, Writing – review & editing. Kirsten Bibbins-Domingo: Conceptualization, Funding acquisition, Investigation, Methodology, Writing – review & editing. M. Maria Glymour: Conceptualization, Investigation, Methodology, Writing – review & editing.
CRediT authorship contribution statement
Yea-Hung Chen: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Visualization, Writing – original draft, Writing – review & editing. Ellicott C. Matthay: Conceptualization, Investigation, Methodology, Writing – review & editing. Ruijia Chen: Investigation, Methodology, Writing – review & editing. Michelle A. DeVost: Investigation, Visualization, Writing – review & editing. Kate A. Duchowny: Investigation, Writing – review & editing. Alicia R. Riley: Investigation, Writing – review & editing. Kirsten Bibbins-Domingo: Conceptualization, Funding acquisition, Investigation, Methodology, Writing – review & editing. M. Maria Glymour: Conceptualization, Investigation, Methodology, Writing – review & editing.
Acknowledgments
ACKNOWLEDGMENTS
ARR, KD, and MAD were supported by a National Institute on Aging training Grant: T32AG049663.
No financial disclosures were reported by the authors of this paper.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2022.06.020.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.Ross CE, Cl Wu. The links between education and health. Am Sociol Rev. 1995;60(5):719–745. doi: 10.2307/2096319. [DOI] [Google Scholar]
- 2.Kawachi I, Adler NE, Dow WH. Money, schooling, and health: mechanisms and causal evidence. Ann N Y Acad Sci. 2010;1186:56–68. doi: 10.1111/j.1749-6632.2009.05340.x. [DOI] [PubMed] [Google Scholar]
- 3.Hummer RA, Hamilton ER. University of California Press; Berkeley, CA: 2019. Population Health in America. [Google Scholar]
- 4.Glymour MM, Avendano M, Kawachi I. Social Epidemiology. 2nd ed., Oxford University Press; United Kingdom: 2014. Socioeconomic status and health; pp. 17–62. [Google Scholar]
- 5.Case A, Deaton A. National Bureau of Economic Research; Cambridge, MA: 2021. The great divide: education, despair and death. Published September 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Case A, Deaton A. No increase in relative mortality rates for those without a college degree during COVID-19: an anomaly. medRxiv. Preprint. Posted July 23, 2021. 10.1101/2021.07.20.21260875. [DOI]
- 7.Feldman JM, Bassett MT. Variation in COVID-19 mortality in the US by race and ethnicity and educational attainment. JAMA Netw Open. 2021;4(11) doi: 10.1001/jamanetworkopen.2021.35967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51(suppl):S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- 9.Chen YH, Glymour MM, Catalano R, et al. Excess mortality in California during the coronavirus disease 2019 pandemic, March to August 2020. JAMA Intern Med. 2021;181(5):705–707. doi: 10.1001/jamainternmed.2020.7578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Essential workforce. California ALL - COVID19.CA.GOV. https://covid19.ca.gov/essential-workforce/. Updated February 14, 2022. Accessed February 1, 2022.
- 11.Chen YH, Glymour M, Riley A, et al. Excess mortality associated with the COVID-19 pandemic among Californians 18-65 years of age, by occupational sector and occupation: march through November 2020. PLoS One. 2021;16(6) doi: 10.1371/journal.pone.0252454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.U.S. Department of Agriculture, Economic Research Service; 2020. Rural-urban commuting area codes. [Google Scholar]; https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/. Updated August 17, 2020. Accessed February 12, 2022.
- 13.Hyndman RJ, Athanasopoulos G. Forecasting: Principles and Practice. 2nd ed., Melbourne, Australia: OTexts; 2018. https://otexts.com/fpp2/. Accessed February 12, 2022
- 14.Stokes AC, Lundberg DJ, Bor J, Bibbins-Domingo K. Excess deaths during the COVID-19 pandemic: implications for US death investigation systems. Am J Public Health. 2021;111(suppl 2):S53–S54. doi: 10.2105/AJPH.2021.306331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim L, Garg S, O'Halloran A, et al. Risk factors for Intensive Care Unit admission and in-hospital mortality among hospitalized adults identified through the U.S. coronavirus disease 2019 (COVID-19)-associated hospitalization surveillance network (COVID-NET) Clin Infect Dis. 2021;72(9):e206–e214. doi: 10.1093/cid/ciaa1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh AK, Gillies CL, Singh R, et al. Prevalence of co-morbidities and their association with mortality in patients with COVID-19: a systematic review and meta-analysis. Diabetes Obes Metab. 2020;22(10):1915–1924. doi: 10.1111/dom.14124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar A, Arora A, Sharma P, et al. Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes Metab Syndr. 2020;14(4):535–545. doi: 10.1016/j.dsx.2020.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang I, Lim MA, Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia – a systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. 2020;14(4):395–403. doi: 10.1016/j.dsx.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bello-Chavolla OY, Bahena-López JP, Antonio-Villa NE, et al. Predicting mortality due to SARS-CoV-2: a mechanistic score relating obesity and diabetes to COVID-19 outcomes in Mexico. J Clin Endocrinol Metab. 2020;105(8):dgaa346. doi: 10.1210/clinem/dgaa346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gansevoort RT, Hilbrands LB. CKD is a key risk factor for COVID-19 mortality. Nat Rev Nephrol. 2020;16(12):705–706. doi: 10.1038/s41581-020-00349-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kant S, Menez SP, Hanouneh M, et al. The COVID-19 nephrology compendium: AKI, CKD, ESKD and transplantation. BMC Nephrol. 2020;21(1):449. doi: 10.1186/s12882-020-02112-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Drake TM, Docherty AB, Harrison EM, et al. Outcome of hospitalization for COVID-19 in patients with interstitial lung disease. An international multicenter study. Am J Respir Crit Care Med. 2020;202(12):1656–1665. doi: 10.1164/rccm.202007-2794OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995 doi: 10.2307/2626958. Spec No: 80–94. [DOI] [PubMed] [Google Scholar]
- 24.Smith MY, Bahri P, Gaudino JA, Moreira RS, Danyluk GM, Palevsky SL. The role of epidemiologists in communicating SARS-CoV-2 evidence: a call for adopting standards. Int J Epidemiol. 2021;50(5):1410–1415. doi: 10.1093/ije/dyab128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ali SH, Foreman J, Tozan Y, Capasso A, Jones AM, DiClemente RJ. Trends and predictors of COVID-19 information sources and their relationship with knowledge and beliefs related to the pandemic: nationwide cross-sectional study. JMIR Public Health Surveill. 2020;6(4):e21071. doi: 10.2196/21071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Georgiou N, Delfabbro P, Balzan R. COVID-19-related conspiracy beliefs and their relationship with perceived stress and pre-existing conspiracy beliefs. Pers Individ Dif. 2020;166 doi: 10.1016/j.paid.2020.110201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clements JM. Knowledge and behaviors toward COVID-19 among U.S. residents during the early days of the pandemic: cross-sectional online questionnaire. JMIR Public Health Surveill. 2020;6(2):e19161. doi: 10.2196/19161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bhuiya T, Klares Iii R, Conte MA, Cervia JS. Predictors of misperceptions, risk perceptions, and personal risk perceptions about COVID-19 by country, education and income. J Investig Med. 2021;69(8):1473–1478. doi: 10.1136/jim-2021-001835. [DOI] [PubMed] [Google Scholar]
- 29.Heath S. Clinician, public health messaging tips for COVID-19 vaccine boosters. Danvers, MA: Xtelligent Healthcare Media.https://patientengagementhit.com/news/clinician-public-health-messaging-tips-for-covid-19-vaccine-boosters. Published September 22, 2021. Accessed October 5, 2021.
- 30.Chang A. New phase of pandemic met with confusion and exhaustion. npr. August 2, 2021. https://www.npr.org/transcripts/1023907905. Accessed October 5, 2021.
- 31.Fischhoff B. The COVID communication breakdown how to fix public health messaging. Foreign Affairs. October 4, 2021 https://www.foreignaffairs.com/articles/united-states/2021-10-04/covid-communication-breakdown Accessed February 12, 2022. [Google Scholar]
- 32.Islam JY, Vidot DC, Camacho-Rivera M. Determinants of COVID-19 preventive behaviours among adults with chronic diseases in the USA: an analysis of the nationally representative COVID-19 impact survey. BMJ Open. 2021;11(2) doi: 10.1136/bmjopen-2020-044600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Latkin CA, Dayton L, Strickland JC, Colon B, Rimal R, Boodram B. An assessment of the rapid decline of trust in US sources of public information about COVID-19. J Health Commun. 2020;25(10):764–773. doi: 10.1080/10810730.2020.1865487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Michaels D, Wagner GR. Occupational Safety and Health Administration (OSHA) and worker safety during the COVID-19 pandemic. JAMA. 2020;324(14):1389–1390. doi: 10.1001/jama.2020.16343. [DOI] [PubMed] [Google Scholar]
- 35.Garces A. Oakland McDonald’s workers sue management over COVID-19 outbreak. KQED. June 16, 2020 https://www.kqed.org/news/11824634/oakland-mcdonalds-workers-sue-management-over-covid-19-outbreak Accessed February 12, 2022. [Google Scholar]
- 36.Cimini K. No face masks so California’s farm workers are left unprotected. CAL Matters. March 26, 2020 https://calmatters.org/california-divide/2020/03/farmworkers-unprotected-face-masks-coronavirus/ Accessed February 12, 2022. [Google Scholar]
- 37.Paul K. Lyft sparks uproar after opening store to sell masks to its drivers. The Guardian. July 17, 2020 https://www.theguardian.com/technology/2020/jul/17/lyft-drivers-masks-ppe-store-covid-19 Accessed February 12, 2022. [Google Scholar]
- 38.Günther T, Czech-Sioli M, Indenbirken D, et al. SARS-CoV-2 outbreak investigation in a German meat processing plant. EMBO Mol Med. 2020;12(12):e13296. doi: 10.15252/emmm.202013296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Davenport C, Gregg A, Timberg C. Working from home reveals another fault line in America's racial and educational divide. The Washington Post. March 22, 2020 https://www.washingtonpost.com/business/2020/03/22/working-home-reveals-another-fault-line-americas-racial-educational-divide/ Accessed October 16, 2021. [Google Scholar]
- 40.Karasek RA. Job demands, job decision latitude, and mental strain: implications for job redesign. Admin Sci Q. 1979;24(2):285. doi: 10.2307/2392498. [DOI] [Google Scholar]
- 41.Tausig M, Fenwick R, Sauter SL, Murphy LR, Graif C. In: Exploring Interpersonal Dynamics (Research in Occupational Stress and Well Being) Perrewe PL, Ganster DC, editors. Vol. 4. Emerald Group Publishing Limited; Bingley, United Kingdom: 2004. The changing nature of job stress: risk and resources; pp. 93–126. [Google Scholar]
- 42.Thomas MD, Matthay EC, Duchowny KA, et al. A descriptive analysis of 2020 California Occupational Safety and Health Administration Covid-19-related complaints. SSM Popul Health. 2022;17 doi: 10.1016/j.ssmph.2021.101016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bilmes L. Harvard Kennedy School; Cambridge, MA: 2021. Estimating the costs and benefits of supported quarantine and isolation in Massachusetts: the missing link in Covid-19 response. [Google Scholar]; https://live.hks.harvard.edu/publications/estimating-costs-and-benefits-supported-quarantine-and-isolation-massachusetts-missing. Published February 2021. Accessed February 12, 2022.
- 44.COVID-19. Department of Homelessness and Supportive Housing. https://hsh.sfgov.org/covid-19/. Updated March 14, 2022. Accessed October 5, 2021.
- 45.Santa Clara County: Emergency Operations Center, Isolation & Quarantine Support Program. County of Santa Clara Public Health.https://covid19.sccgov.org/isolation-and-quarantine-support. Updated July 7, 2022. Accessed February 12, 2022.
- 46.Berkman LF, Krishna A. Social Epidemiology. 2nd. Oxford University Press; Oxford, United Kingdom: 2014. Social network epidemiology. [Google Scholar]
- 47.Cepić D, Tonković Ž. How social ties transcend class boundaries? Network variability as tool for exploring occupational homophily. Soc Netw. 2020;62:33–42. doi: 10.1016/j.socnet.2020.02.003. [DOI] [Google Scholar]
- 48.Faust JS, Chen AJ, Nguemeni Tiako MJ, et al. Leading causes of death among adults aged 25 to 44 years by race and ethnicity in Texas during the COVID-19 pandemic, March to December 2020. JAMA Intern Med. 2022;182(1):87–90. doi: 10.1001/jamainternmed.2021.6734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rossen LM, Branum AM, Ahmad FB, Sutton P, Anderson RN. Excess deaths associated with COVID-19, by age and race and ethnicity - United States, January 26–October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(42):1522–1527. doi: 10.15585/mmwr.mm6942e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lopez L, 3rd, Hart LH, 3rd, Katz MH. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;325(8):719–720. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- 51.Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59(1):137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kamal S. California’s extra sick leave for COVID-19 ended, but is it time to restore it? LAist. January 10, 2022 https://laist.com/news/health/californias-extra-sick-leave-for-covid-19-ended-but-is-it-time-to-restore-it Accessed February 12, 2022. [Google Scholar]
- 53.Woolf SH, Chapman DA, Sabo RT, Zimmerman EB. Excess deaths from COVID-19 and other causes in the US, March 1, 2020, to January 2, 2021. JAMA. 2021;325(17):1786–1789. doi: 10.1001/jama.2021.5199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stokes AC, Lundberg DJ, Elo IT, Hempstead K, Bor J, Preston SH. COVID-19 and excess mortality in the United States: a county-level analysis. PLoS Med. 2021;18(5) doi: 10.1371/journal.pmed.1003571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rossen LM, Ahmad FB, Anderson RN, et al. Disparities in excess mortality associated with COVID-19 - United States, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(33):1114–1119. doi: 10.15585/mmwr.mm7033a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rostron BL, Boies JL, Arias E. Education reporting and classification on death certificates in the United States. Vital Health Stat 2. 2010(151):1–21. https://www.cdc.gov/nchs/data/series/sr_02/sr02_151.pdf. Accessed February 12, 2022. [PubMed]
- 57.Stroebe M, Schut H. Bereavement in times of COVID-19: a review and theoretical framework. Omega. 2021;82(3):500–522. doi: 10.1177/0030222820966928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Katz NT, McInerney M, Ravindran G, Gold M. Silent suffering of the dying and their families: impact of COVID-19. Intern Med J. 2021;51(3):433–435. doi: 10.1111/imj.15101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Spurio MG. Mourning from Covid-19 and post traumatic stress disorder. New therapeutic tools in the treatment of pathological bereavement. Psychiatr Danub. 2021;33(suppl 9):102–107. [PubMed] [Google Scholar]
- 60.Sampson L, Ettman CK, Abdalla SM, et al. Financial hardship and health risk behavior during COVID-19 in a large U.S. national sample of women. SSM Popul Health. 2021;13 doi: 10.1016/j.ssmph.2021.100734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mann FD, Krueger RF, Vohs KD. Personal economic anxiety in response to COVID-19. Pers Individ Dif. 2020;167 doi: 10.1016/j.paid.2020.110233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sills SJ, Rich BA. Housing instability and public health: implications of the eviction moratoria during the COVID-19 pandemic. N C Med J. 2021;82(4):271–275. doi: 10.18043/ncm.82.4.271. [DOI] [PubMed] [Google Scholar]
- 63.Benfer EA, Vlahov D, Long MY, et al. Eviction, health inequity, and the spread of COVID-19: housing policy as a primary pandemic mitigation strategy. J Urban Health. 2021;98(1):1–12. doi: 10.1007/s11524-020-00502-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bushman G, Mehdipanah R. Housing and health inequities during COVID-19: findings from the national Household Pulse Survey. J Epidemiol Community Health. 2022;76(2):121–127. doi: 10.1136/jech-2021-216764. [DOI] [PubMed] [Google Scholar]
- 65.Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hossain MM, Tasnim S, Sultana A, et al. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020;9:636. doi: 10.12688/f1000research.24457.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Torales J, O'Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.