Abstract
Objective
To report the global, regional, and national burden of chronic obstructive pulmonary disease (COPD) and its attributable risk factors between 1990 and 2019, by age, sex, and sociodemographic index.
Design
Systematic analysis.
Data source
Global Burden of Disease Study 2019.
Main outcome measures
Data on the prevalence, deaths, and disability adjusted life years (DALYs) of COPD, and its attributable risk factors, were retrieved from the Global Burden of Disease 2019 project for 204 countries and territories, between 1990 and 2019. The counts and rates per 100 000 population, along with 95% uncertainty intervals, were presented for each estimate.
Results
In 2019, 212.3 million prevalent cases of COPD were reported globally, with COPD accounting for 3.3 million deaths and 74.4 million DALYs. The global age standardised point prevalence, death, and DALY rates for COPD were 2638.2 (95% uncertainty intervals 2492.2 to 2796.1), 42.5 (37.6 to 46.3), and 926.1 (848.8 to 997.7) per 100 000 population, which were 8.7%, 41.7%, and 39.8% lower than in 1990, respectively. In 2019, Denmark (4299.5), Myanmar (3963.7), and Belgium (3927.7) had the highest age standardised point prevalence of COPD. Egypt (62.0%), Georgia (54.9%), and Nicaragua (51.6%) showed the largest increases in age standardised point prevalence across the study period. In 2019, Nepal (182.5) and Japan (7.4) had the highest and lowest age standardised death rates per 100 000, respectively, and Nepal (3318.4) and Barbados (177.7) had the highest and lowest age standardised DALY rates per 100 000, respectively. In men, the global DALY rate of COPD increased up to age 85-89 years and then decreased with advancing age, whereas for women the rate increased up to the oldest age group (≥95 years). Regionally, an overall reversed V shaped association was found between sociodemographic index and the age standardised DALY rate of COPD. Factors contributing most to the DALYs rates for COPD were smoking (46.0%), pollution from ambient particulate matter (20.7%), and occupational exposure to particulate matter, gases, and fumes (15.6%).
Conclusions
Despite the decreasing burden of COPD, this disease remains a major public health problem, especially in countries with a low sociodemographic index. Preventive programmes should focus on smoking cessation, improving air quality, and reducing occupational exposures to further reduce the burden of COPD.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common chronic respiratory condition resulting in gradual deterioration and worsening of symptoms. Although preventable, once established it cannot be cured, but effective self-management strategies can lessen the burden of disease and improve quality of life.1 In 1990, COPD was the second most common cause of death (in terms of age standardised death rate) across the world and in 2019 COPD was the third most common cause of death.2 From 2007 to 2017, an increase of 15.6% in the prevalence of COPD was reported, although the age standardised prevalence decreased by 10.1% in men.3 COPD is considered a systemic disease and is more common in individuals with a history of tobacco smoking.4 5 A wide range of comorbidities and risk factors are associated with the disease, including genetics, smoking, infections, malnutrition, ageing, occupational exposures, indoor and outdoor air pollutants, asthma, and low socioeconomic status.4 6 Together, these factors could lead to vascular abnormalities, such as loss of alveolar capillary endothelial cells, destruction of alveolar cells, and alveolar space enlargement, which are important contributors in the progression of COPD.6 Clinical manifestations of COPD, such as dyspnoea, cough, wheezing, and phlegm, are more severe in the early morning and evening, negatively affecting the patient’s quality of life.7 The prognosis of COPD is determined by measuring forced expiratory volume in one second, a measure of airflow.8 Moreover, COPD can affect the prognosis of other diseases, such as covid-19,9 cancer, mental health conditions, cardiovascular diseases, gastrointestinal disorders, and musculoskeletal disorders.10
Several major international collaborations have provided data on COPD. For example, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) programme was established in 1998 and provides regular updates and evidence based recommendations for the management of COPD.11 The European Community Respiratory Health Survey was established in 1990 in response to the increased prevalence of asthma in the 1980s, with the aim of determining the distribution of asthma and its healthcare burden in the European community.12 In the last iteration of the European Community Respiratory Health Survey (European Community Respiratory Health Survey III), the effects of atopic status and asthma on the development of COPD were evaluated.13 Based on the GOLD criteria, a diagnosis of COPD is suspected if the patient presents with related symptoms (eg, chronic cough, sputum, and shortness of breath) and risk factors (eg, tobacco smoking and occupational exposures) but is confirmed by the presence of a post-bronchodilator forced expiratory volume in one second/forced vital capacity value of <0.7.11 Commonly used drug treatments for COPD are β agonists, anticholinergic agents, and corticosteroids, and other options include α-1 antitrypsin augmentation therapy, antitussive agents, and vasodilators.11
Previous systematic reviews on the epidemiology of COPD have reported a global prevalence ranging from 7.6% in 2004 to 11.4% in 2014.14 15 The prevalence of COPD has been reported to be higher in men, in urban areas, and in high income countries.14 Also, COPD imposes a substantial economic burden, ranging from €1963 (£1685; $2068) in Belgium to €10 701 in Norway annually, and the cost is positively correlated with a late diagnosis, severe COPD, a greater number of exacerbations, and hospital admissions.16
Current evidence on the epidemiology of COPD has not used a modelling approach to estimate the burden of COPD, but instead used systematic reviews to provide a pooled estimation of the prevalence of COPD.14 15 Several analytical epidemiological studies have reported prevalence and incidence data for many sites worldwide, including whole countries, with standardised diagnostic criteria, and these provide real prevalence data.17 18 19 20 The most recent study based on the Global Burden of Disease 2017 data reported the prevalence and burden of chronic respiratory diseases, such as COPD and asthma combined, and did not report the disease specific burden; these estimates need updating.5 Moreover, based on the Global Burden of Disease 2017 data, the trends and risk factors for mortality and disability adjusted life years (DALYs) due to COPD have been published, but the prevalent numbers and rates have not been reported.21 Updated information on the burden of important chronic respiratory diseases is needed for public health and advocacy purposes.
Recently, data from the Global Burden of Disease 2019 study were used to report the burden of COPD attributable to one specific risk factor (that is, ambient PM2.5), but the overall burden of COPD and the burden attributable to other risk factors were not estimated.22 Here, we report the prevalence, deaths, and DALYs associated with COPD, and the attributable risk factors by age, sex, and sociodemographic index in 204 countries and territories from 1990 to 2019.
Methods
The Global Burden of Disease 2019 study estimated the burden of 369 diseases and injuries and 87 risk factors from 1990 to 2019 in 204 countries and territories and 21 regions.2 Detailed descriptions of the methodologies have been reported,2 23 24 and fatal and non-fatal estimates have been published (https://vizhub.healthdata.org/gbd-compare/ and https://ghdx.healthdata.org/gbd-results-tool).
Case definition and data sources
The GOLD definition of COPD was used in this study: a value of <0.7 for forced expiratory volume in one second/forced vital capacity (one second of forceful exhalation/total forced expiration) with spirometry, after bronchodilation. The definitions that we used for the severity of COPD also followed the GOLD criteria: class I=mild, ≥80% of normal; class II=moderate, 50-79% of normal; classes III and IV=severe, <50% of normal.2 Alternative definitions for evaluating whether an individual has COPD include the GOLD criteria before bronchodilation, lower limit of normal after bronchodilation, lower limit of normal before bronchodilation, and European Respiratory Society guidelines.2
A systematic literature review was not undertaken on the data from the Global Burden of Disease 2019 study; the last systematic review was carried out for the Global Burden of Disease 2016 study by the Institute for Health Metrics and Evaluation. Table S1 provides details on the search terms used in the previous systematic literature review. The Global Burden of Disease 2019 study used several data sources for extracting data on COPD (that is, prevalence, incidence, and remission data) from the literature: hospital claims data, proportion data for each of the GOLD definitions for the severity of COPD, and data from the Burden of Obstructive Lung Disease study.
Data on the prevalence, incidence, and remissions for COPD were extracted from the literature provided by collaborators at the Institute for Health Metrics and Evaluation, and all included studies used measures based on spirometry. Hospital claims data were used for non-fatal estimates and vital registrations for cause of death. Proportion data for each of the GOLD definitions for the severity of COPD were extracted from the literature, when information about severity was available. The models estimated the three classes of severity of COPD (I, II, III-IV) separately, and this information was used in the modelling process to categorise COPD according to the level of severity. The English Longitudinal Study of Ageing and claims data from the USA were added to the data for the Global Burden of Disease 2019 study. In total, data were obtained for 57 of the 204 countries and territories, which were collapsed and aggregated to produce estimates for each age group, sex, location, and year.2 The studies included in the modelling process can be found here https://ghdx.healthdata.org/gbd-2019/data-input-sources.
Mortality from COPD was estimated from vital registration and surveillance data from the Global Burden of Disease cause of death database, but verbal autopsy data were only mapped to an overall chronic respiratory disease model. Individual data were excluded when the data points were implausibly high or low, conflicted substantially with established age or temporal patterns, or conflicted substantially with other data sourced from the same locations or similar locations (that is, similar sociodemographic index).2
Disease model
Mortality from COPD was estimated with Cause of Death Ensemble modelling (CODEm) for an age range of 1 to ≥95 years, with specific models for men and women. Table S2 shows the covariates used in the CODEm.
The burden of COPD was estimated in two stages: the DisMod-MR 2.1 model was used to estimate the prevalence and incidence of COPD and the proportion of patients in each of the GOLD severity classes for COPD was estimated with DisMod-MR 2.1. Then, the prevalence and incidence of COPD were categorised by age, sex, and location for each level of severity.2 In stage 1, remission was set at 0, because individuals do not recover when they have COPD because symptoms can only be managed. The incidence ceiling was set at 0.0002 before age 15 years and at 0.0005 before age 30 years, to prevent any spurious overestimation in the age ranges with little or no primary data.2 The models also included country level covariates that described spatiotemporal patterns to improve estimations, particularly in locations with inadequate data. Also, covariates included in the models were the COPD standardised exposure covariates (SEV, a scalar that combines exposure to all Global Burden of Disease risks that influence COPD), healthcare access and quality index, and the proportion of countries with an elevation above 1500 m.2 In stage II, data from the surveys that reported the prevalence of COPD for each of the GOLD severity classes were used to estimate the overall percentage of all patients with COPD in each of the severity classes.2
Severity and years lived with disability
Codes from the ICD-10 (international classification of diseases, 10th revision; J41, J42, J43, J44, and J47) and ICD-9 (international classification of diseases, ninth revision; 491-492, and 496) were use for mapping COPD. In the Global Burden of Disease 2017 study, J40 and 490 (bronchitis, not specified as acute or chronic) and J47 and 494 (bronchiectasis) were not included, however.2 The three GOLD classes are not a direct measure of disease severity, but rather reflect a grading system based on a physiological measurement. Data from the Medical Expenditure Panel Survey (US, 2001-2011) were used to map the epidemiological findings into the three COPD health states, for which disability weights had been previously identified. More specifically, the GOLD class designations estimated for the US in 2005 (midpoint of the years included in the Medical Expenditure Panel Survey) were converted into the Global Burden of Disease classifications of asymptomatic, mild, moderate, and severe COPD. Table S3 shows the three health states for COPD (mild, moderate, and severe), lay descriptions, and disability weights.2 Finally, the severity levels were multiplied by the severity specific disability weights to produce the years lived with disability.
Compilation of results
The number of deaths in each age group was multiplied by the remaining life expectancy in that age group, according to the Global Burden of Disease standard life table, to estimate the years of life lost. Years of life lost and years lived with disability were then summed to produce DALYs. The level of uncertainty was calculated by sampling 1000 draws at each computational step and combining uncertainty from several different sources (that is, input data, corrections of measurement error, and estimates of residual non-sampling error). The uncertainty intervals were defined as the 25th and 975th values of the ordered draws. The relation between the burden of COPD (DALYs) and sociodemographic index for the 21 regions and 204 countries and territories were examined with Smoothing Splines models.25 Sociodemographic index, which ranges from 0 (least developed) to 1 (most developed), is a composite indicator of lag dependent income per capita and consists of the gross domestic product per capita (smoothed over the previous decade), average number of years of education for the population (>15 years old), and total fertility rate in those aged <25 years. The age standardised point prevalence, death, and DALY rates were mapped with R software (version 3.5.2).
Risk factors
Strong evidence indicates that the risk factors that cause COPD are24: smoking status, pollution from ambient particulate matter, occupational exposure to particulate matter, gases, and fumes, household air pollution from solid fuels, exposure to secondhand smoke, ambient ozone pollution, low temperatures, and high temperatures. The proportion of DALYs that were attributable to each COPD risk factor was also reported. Definitions of these risk factors and their relative risks for COPD have been previously reported.24
Patient and public involvement
Because the study used publicly available aggregate data, no patients were involved in setting the research question or the outcome measures, nor were they involved in the design or implementation of the study.
Results
Global level
In 2019, 212.3 million (table 1) prevalent cases of COPD were reported globally, with an age standardised point prevalence of 2638.2 per 100 000, a decrease of 8.7% since 1990. COPD accounted for 3.3 million deaths in 2019, with an age standardised rate of 42.5, a decrease of 41.7% since 1990. In 2019, the number of DALYs for COPD globally was 74.4 million, with an age standardised rate of 926.1 DALYs per 100 000, a 39.8% decrease since 1990 (table 1).
Table 1.
Prevalent cases, deaths, and disability adjusted life years (DALYs) for chronic obstructive pulmonary disease in 2019, and percentage change in age standardised rates (ASRs) per 100 000, by Global Burden of Disease region, from 1990 to 2019 (generated from data available at https://ghdx.healthdata.org/gbd-results-tool)
| Prevalence (95% UI) | Deaths (95% UI) | DALYs (95% UI) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No, in millions (95% UI) | ASRs per 100 000 (95% UI) | Percentage change in ASRs from 1990 to 2019 |
No, in thousands (95% UI) | ASRs per 100 000 (95% UI) | Percentage change in ASRs from 1990 to 2019 |
No, in thousands (95% UI) | ASRs per 100 000 (95% UI) | Percentage change in ASRs from 1990 to 2019 |
|||
| Global | 212.3 (200.4 to 225.1) | 2638.2 (2492.2 to 2796.1) | −8.7 (−10.2 to −7.3) | 3280.6 (2902.9 to 3572.4) | 42.5 (37.6 to 46.3) | −41.7 (−48 to −31.1) | 74432.4 (68204.1 to 80193.3) | 926.1 (848.8 to 997.7) | −39.8 (−44.9 to −30.2) | ||
| High income Asia Pacific | 6.6 (6.1 to 7.1) | 1500.7 (1384.2 to 1621.3) | −20.5 (−23 to −17.5) | 49.3 (37.7 to 63.1) | 8.2 (6.4 to 10.4) | −41.8 (−51.4 to −25.6) | 1071.2 (912.7 to 1249.7) | 224.5 (193.6 to 258.4) | −34.4 (−39.5 to −25.6) | ||
| High income North America | 22.0 (21.0 to 22.8) | 3558.4 (3412.9 to 3694.4) | 1.1 (−1.9 to 4.9) | 211.4 (174.0 to 229.9) | 31.2 (25.9 to 33.8) | 17.7 (−4.6 to 28.6) | 5346.3 (4812.3 to 5695.2) | 848.4 (765.9 to 903) | 4.1 (−5.7 to 9.3) | ||
| Western Europe | 26.3 (25.1 to 27.6) | 3017.5 (2874.7 to 3165.8) | 0.5 (−0.7 to 1.7) | 212.5 (186.0 to 233.3) | 19.2 (17 to 21.1) | −23.6 (−29.5 to −17.8) | 4306.9 (3887.6 to 4666.2) | 460.8 (418.3 to 499.6) | −19.1 (−22.8 to −15.2) | ||
| Australasia | 1.5 (1.5 to 1.6) | 3192.8 (3027.7 to 3372.1) | −10.1 (−13.2 to −6.6) | 11.4 (9.6 to 13.0) | 20.6 (17.4 to 23.3) | −32.2 (−39.8 to −23.6) | 257.8 (228.5 to 285.0) | 512.1 (455.1 to 564.8) | −30 (−34.9 to −24.6) | ||
| Andean Latin America | 0.8 (0.8 to 0.9) | 1382.6 (1297.9 to 1464.5) | 17.8 (14.2 to 21.3) | 8.1 (6.4 to 9.9) | 15.4 (12.2 to 18.9) | −24.9 (−40 to −7) | 155.8 (130.5 to 184.3) | 281.9 (236.1 to 335.1) | −31 (−41.7 to −18.3) | ||
| Tropical Latin America | 6.3 (5.8 to 6.9) | 2634.5 (2436.3 to 2860.8) | −15.5 (−18.8 to −12.5) | 69.7 (62.0 to 78.8) | 30.6 (27.2 to 34.7) | −38.4 (−43 to −31.4) | 1454.6 (1339.1 to 1596.9) | 613.2 (563.9 to 674) | −36.2 (−39.9 to −30.6) | ||
| Central Latin America | 5.2 (4.8 to 5.5) | 2186.5 (2052.6 to 2332.4) | 10.3 (8.3 to 12.3) | 64.3 (54.8 to 74.2) | 29.2 (24.9 to 33.7) | −12.6 (−22.9 to −0.6) | 1214.7 (1059.5 to 1391.0) | 530 (461.5 to 605.6) | −13.8 (−22.9 to −3.1) | ||
| Southern Latin America | 2.2 (2.1 to 2.3) | 2741.7 (2619.3 to 2875) | 19.8 (16.6 to 22.9) | 22.7 (19.7 to 25.3) | 26.4 (23 to 29.5) | 2.1 (−10.5 to 15.1) | 453.5 (409.5 to 500.7) | 544.8 (493 to 601.2) | −3.1 (−11.2 to 6.1) | ||
| Caribbean | 1.1 (1.0 to 1.1) | 2044.2 (1944.5 to 2141) | 29.2 (26.5 to 32) | 10.7 (8.9 to 12.4) | 20.6 (17.2 to 23.9) | 9.7 (−8.4 to 26.6) | 237.9 (205.5 to 270.4) | 463.2 (400.1 to 527.7) | 12.6 (−2.3 to 27.5) | ||
| Central Europe | 4.8 (4.5 to 5.0) | 2427.4 (2316.9 to 2552.3) | −0.4 (−2.2 to 1.4) | 38.8 (33.7 to 44.8) | 17.3 (15 to 19.9) | −43.2 (−50.4 to −34.5) | 941.5 (839.4 to 1047.0) | 452.8 (402.7 to 504.1) | −34.6 (−40.7 to −28.5) | ||
| Eastern Europe | 5.7 (5.3 to 6.1) | 1821.5 (1705.9 to 1949.5) | −29.5 (−31.5 to −27.5) | 52.4 (45.9 to 66.1) | 15.0 (13.1 to 18.9) | −55.8 (−61.9 to −35.7) | 1270.3 (1122.4 to 1498.7) | 381.5 (336.8 to 448.4) | −50.8 (−56.3 to −36.6) | ||
| Central Asia | 1.7 (1.6 to 1.7) | 2257.2 (2169.4 to 2349.1) | −12.5 (−14.2 to −10.9) | 17.2 (15.4 to 20.0) | 31.5 (27.9 to 36.8) | −16.4 (−26.6 to 6.4) | 450.9 (408.7 to 509.4) | 662.8 (602.4 to 747.8) | −24.1 (−32 to −6.9) | ||
| North Africa and Middle East | 10.7 (10.3 to 11.2) | 2333.9 (2230.1 to 2443.6) | 30.6 (28.2 to 33) | 89.9 (76.8 to 101.8) | 26.1 (22.2 to 29.5) | −18 (−30.9 to −2.8) | 2761.8 (2436.8 to 3062.6) | 649.1 (574.6 to 717.7) | −11.8 (−21.1 to −0.9) | ||
| South Asia | 45.7 (43.1 to 48.4) | 3298.8 (3104.7 to 3490.8) | −5 (−6.9 to −3.2) | 1048.7 (838.4 to 1216.1) | 93.2 (74.5 to 107.8) | −30.3 (−43.4 to −17.3) | 25068.3 (21179.0 to 28364.4) | 1915.9 (1617 to 2171.7) | −29.5 (−39.9 to −18.8) | ||
| South East Asia | 15.0 (14.2 to 15.8) | 2480.1 (2353 to 2624.5) | 3.9 (2.5 to 5.4) | 189.0 (160.2 to 210.4) | 38.8 (33.2 to 43) | −33.3 (−42.1 to −20.5) | 5135.3 (4483.3 to 5641.3) | 895.6 (785 to 981.4) | −28.5 (−36.6 to −17.7) | ||
| East Asia | 46.7 (42.6 to 51.2) | 2396.1 (2191.3 to 2620.1) | −27.1 (−31 to −22.8) | 1075.5 (924.7 to 1301.4) | 64.6 (55.3 to 78.9) | −69.6 (−74.8 to −53.4) | 20687.0 (18186.6 to 24532.6) | 1100.0 (964.1 to 1299.4) | −68.9 (−73.8 to −54.3) | ||
| Oceania | 0.2 (0.2 to 0.2) | 2514.7 (2435.2 to 2581.7) | −0.6 (−2.5 to 1.1) | 5.8 (4.5 to 7.4) | 112.1 (86.8 to 139.9) | −11.8 (−29 to 7.2) | 158.3 (125.7 to 199.3) | 2309.9 (1847.5 to 2874.6) | −12.8 (−28.9 to 6.5) | ||
| Western sub-Saharan Africa | 4.0 (3.8 to 4.2) | 1618.4 (1521.6 to 1721.3) | −4.5 (−6.5 to −2) | 35.5 (29.7 to 41.0) | 24.3 (20.5 to 27.8) | −17.5 (−32.3 to −3.8) | 1256.9 (1102.0 to 1409.7) | 619 (542.8 to 692.7) | −16 (−29 to −5.6) | ||
| Eastern sub-Saharan Africa | 3.3 (3.1 to 3.5) | 1503.5 (1408 to 1608.7) | −4.7 (−6.2 to −2.9) | 37.1 (31.6 to 43.5) | 29.3 (25.1 to 33.7) | −27.2 (−36.3 to −17.6) | 1233.6 (1081.8 to 1417.1) | 707.5 (622.5 to 801.7) | −25.9 (−33.2 to −18.4) | ||
| Central sub-Saharan Africa | 1.3 (1.2 to 1.4) | 1943.2 (1816.7 to 2076.2) | 12.3 (9.1 to 15.7) | 15.8 (11.1 to 23.4) | 42.6 (29.6 to 66.7) | −18.6 (−36 to 3) | 505.2 (396.0 to 653.0) | 964.5 (743.7 to 1321.3) | −15.6 (−30.2 to 1.4) | ||
| Southern sub-Saharan Africa | 1.3 (1.3 to 1.4) | 2243.9 (2090 to 2411.7) | −9.7 (−12.2 to −7.1) | 14.9 (13.5 to 16.3) | 32.4 (29 to 35.4) | −17.1 (−32.7 to −1.8) | 464.5 (427.7 to 502.7) | 838.6 (772.6 to 907.8) | −16.3 (−27.4 to −6.6) | ||
95% UI=95% uncertainty intervals.
Regional level
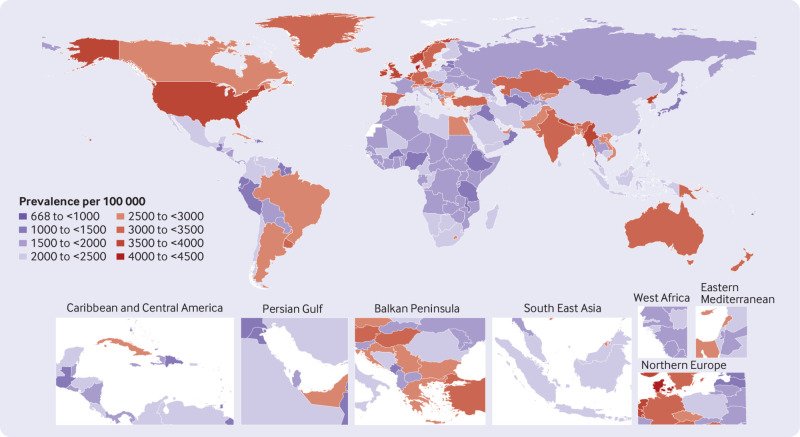
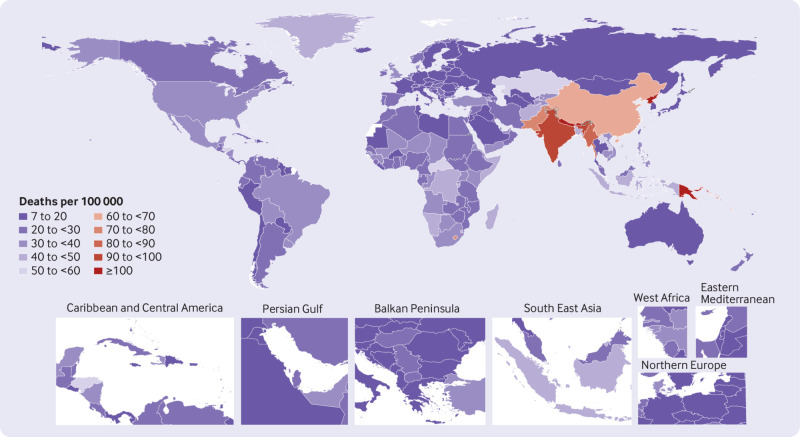
In 2019, high income North America (3558.4), South Asia (3298.8), and Australasia (3192.8) had the highest age standardised point prevalences for COPD (per 100 000), whereas Andean Latin America (1382.6), high income Asia Pacific (1500.7), and eastern sub-Saharan Africa (1503.5) had the lowest (table 1). Oceania (112.1), South Asia (93.2), and East Asia (64.6) had the highest age standardised death rates from COPD in 2019, with the lowest rates in high income Asia Pacific (8.2), eastern Europe (15.0), and Andean Latin America (15.4) (table 1). In 2019, Oceania (2309.9), South Asia (1915.9), and East Asia (1100.0) had the highest age standardised DALY rates (per 100 000), whereas high income Asia Pacific (224.5), Andean Latin America (281.9), and eastern Europe (381.5) had the lowest (table 1). Figures S1-S3 show the age standardised point prevalence, death, and DALY rates of COPD, respectively, by sex in 2019 for all regions in the Global Burden of Disease study.
The largest increases in the age standardised point prevalence of COPD, from 1990 to 2019, were found in North Africa and the Middle East (30.6%), Caribbean (29.2%), and southern Latin America (19.8%), with the greatest decreases in eastern Europe (−29.5%), East Asia (−27.1%), and high income Asia Pacific (−20.5%) (table 1). In the same period, all regions showed a decrease in the age standardised death rates from COPD, with the largest decreases in East Asia (−69.6%), eastern Europe (−55.8%), and central Europe (−43.2%) (table 1). The age standardised DALY rates decreased in all regions from 1990 to 2019, with the largest decreases in East Asia (−68.9%), Eastern Europe (−50.8%), tropical Latin America (−36.2%), and central Europe (−34.6%) (table 1). Figures S4-S6 show the percentage change, from 1990 to 2019, in age standardised point prevalence, death, and DALY rates for COPD by sex, respectively.
The number of prevalent cases of COPD increased from 114.9 million in 1990 to 212.3 million in 2019. East Asia, South Asia, and western Europe had the highest numbers of prevalent cases in 1990, and the same regions had the largest numbers in 2019 (table S4). The number of deaths caused by COPD increased from 2.5 million in 1990 to 3.3 million in 2019, with East Asia, South Asia, and western Europe having the highest numbers of deaths in 2019 (table S5). The number of DALYs due to COPD increased from 59.2 million in 1990 to 74.4 million in 2019, with South Asia, East Asia, and high income North America having the highest numbers of DALYs in 2019 (table S6).
National level
In 2019, the national age standardised point prevalence of COPD ranged from 668.5 to 4299.5 cases per 100 000. Denmark (4299.5), Myanmar (3963.7), and Belgium (3927.7) had the highest age standardised point prevalences of COPD, with Fiji (668.5), Guam (1010.0), and Kiribati (1019.4) having the lowest estimates (fig 1 and table S4). The national age standardised death rates for COPD in 2019 varied from 7.4 to 182.5 deaths per 100 000. The highest rates were seen in Nepal (182.5), Papua New Guinea (145.0), and the Democratic People’s Republic of Korea (105.2), whereas the lowest rates were found in Japan (7.4), Barbados (8.3), and Kuwait (8.3) (fig 2 and table S5). In 2019, the national age standardised DALY rate of COPD ranged from 177.7 to 3318.4 patients per 100 000. The highest rates were seen in Nepal (3318.4), Papua New Guinea (2902.7), and the Solomon Islands (2178.6) whereas the lowest rates were in Barbados (177.7), Antigua and Barbuda (178.2), and Peru (189.6) (fig S7 and table S6).
Fig 1.
Age standardised point prevalence of chronic obstructive pulmonary disease per 100 000 population in 2019, by country (generated from data available at https://ghdx.healthdata.org/gbd-results-tool)
Fig 2.
Age standardised death rate of chronic obstructive pulmonary disease per 100 000 population in 2019, by country (generated from data available at https://ghdx.healthdata.org/gbd-results-tool)
The percentage change in the age standardised point prevalence, from 1990 to 2019, differed noticeably between countries, with Egypt (62.0%), Georgia (54.9%), and Nicaragua (51.6%) having the largest increases. In contrast, Turkmenistan (−47.9%), Singapore (−47.3%), and Ukraine (−45.6%) had the largest decreases (table S4). Over the same period, Nicaragua (68.5%), Norway (63.5%), and Sweden (36.9%) had the largest increases in the age standardised death rate, whereas the largest decreases were found in Singapore (−81.0%), China (−70.1%), and Turkmenistan (−69.9%) (table S5). Nicaragua (44.3%), Cuba (38.6%), and Norway (38.5%) had the largest increases in age standardised DALY rate of COPD from 1990 to 2019. In contrast, the greatest decreases during the study period were found in Singapore (−73.8%), China (−69.5%), and Turkmenistan (−65.1%) (table S6).
Age and sex patterns
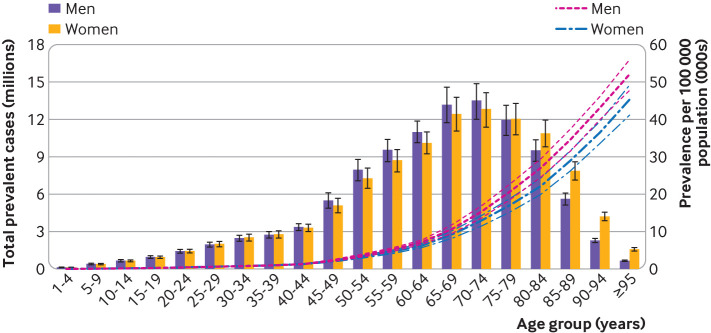
In 2019, the global point prevalence of COPD started to increase in the 20-24 age group and peaked in the oldest age group (≥95 years). Similarly, the number of prevalent cases was highest in the 70-74 age group, but then decreased with increasing age. The number of prevalent cases of COPD was higher in men up to age 70-74 years, but COPD was more common in women older than 74 years (fig 3). In 2019, the global COPD death rate reached its highest level in the oldest age group (≥95 years) and was higher in men across all age groups. The number of deaths was highest in the 80-84 age groups, for both sexes, after which the numbers decreased with increasing age. The number of deaths caused by COPD was higher in men aged up to 85-89 years (fig S8). In men, the global DALY rate of COPD increased up to age 85-89 years and then decreased with advancing age, whereas for women, the DALY rate increased up to the oldest age group (≥95 years). This rate was higher in men across all age groups. Also, the number of DALYs peaked in the 70-74 age groups and was higher in men up to age 85-89 years (fig S9).
Fig 3.
Number of prevalent cases globally and prevalence of chronic obstructive pulmonary disease per 100 000 population, by age and sex in 2019. Lines indicate prevalent case with 95% uncertainty intervals for men and women (generated from data available at https://ghdx.healthdata.org/gbd-results-tool)
Association with the sociodemographic index
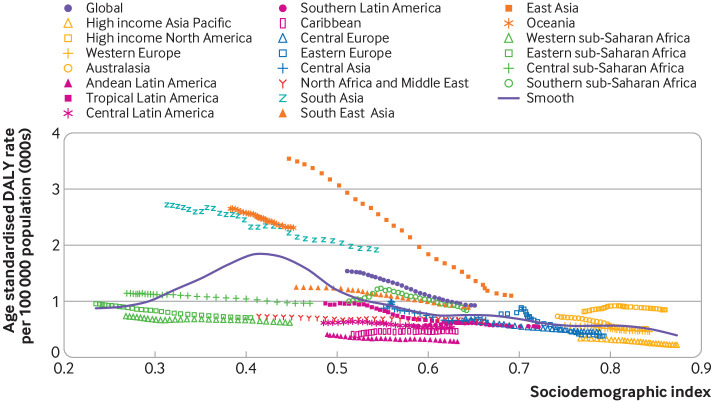
At the regional level, we found a reversed V shaped association between the sociodemographic index and the age standardised DALY rate of COPD, from 1990 to 2019. The age standardised DALY rate increased exponentially with increases in sociodemographic index, up to a sociodemographic index of about 0.4, before decreasing again. South Asia, Oceania, East Asia, and high income North America had higher than expected DALY rates, based on their sociodemographic index, from 1990 to 2019. In contrast, western sub-Saharan Africa, north Africa and the Middle East, tropical Latin America, central Latin America, Andean Latin America, southern Latin America, Caribbean, central Europe, and high income Asia Pacific had lower than expected burdens from 1990 to 2019 (fig 4).
Fig 4.
Age standardised disability adjusted life year (DALY) rates of chronic obstructive pulmonary disease for the 21 Global Burden of Disease regions by sociodemographic index, 1990–2019. Thirty points are plotted for each region and show the observed age standardised DALY rates from 1990 to 2019 for that region. Expected values, based on sociodemographic index and disease rates in all locations, are shown as a solid line. Regions above the solid line represent a higher than expected burden (eg, South Asia) and regions below the line show a lower than expected burden (eg, western sub-Saharan Africa) (generated from data available at https://ghdx.healthdata.org/gbd-results-tool)
At the country level, in 2019, the burden of COPD increased with increasing socioeconomic development up to a sociodemographic index of about 0.42, but then decreased up to a sociodemographic index of about 0.81 (fig S10). Countries and territories such as Nepal, Papua New Guinea, the Solomon Islands, the Democratic People’s Republic of Korea, India, and Bhutan had much higher than expected burdens, whereas Singapore, Peru, Guatemala, Ethiopia, and South Sudan had much lower than expected burdens (fig S10).
Risk factors
The proportion of DALYs due to COPD that were attributable to individual risk factors differed across the Global Burden of Disease regions. Globally, smoking (46.0%), pollution from ambient particulate matter (20.7%), and occupational exposure to particulate matter, gases, and fumes (15.6%) had the highest contributions to DALYs due to COPD (fig 5). The proportion of DALYs due to COPD that were attributable to these three risk factors were higher in men (figs S11 and S12).
Fig 5.
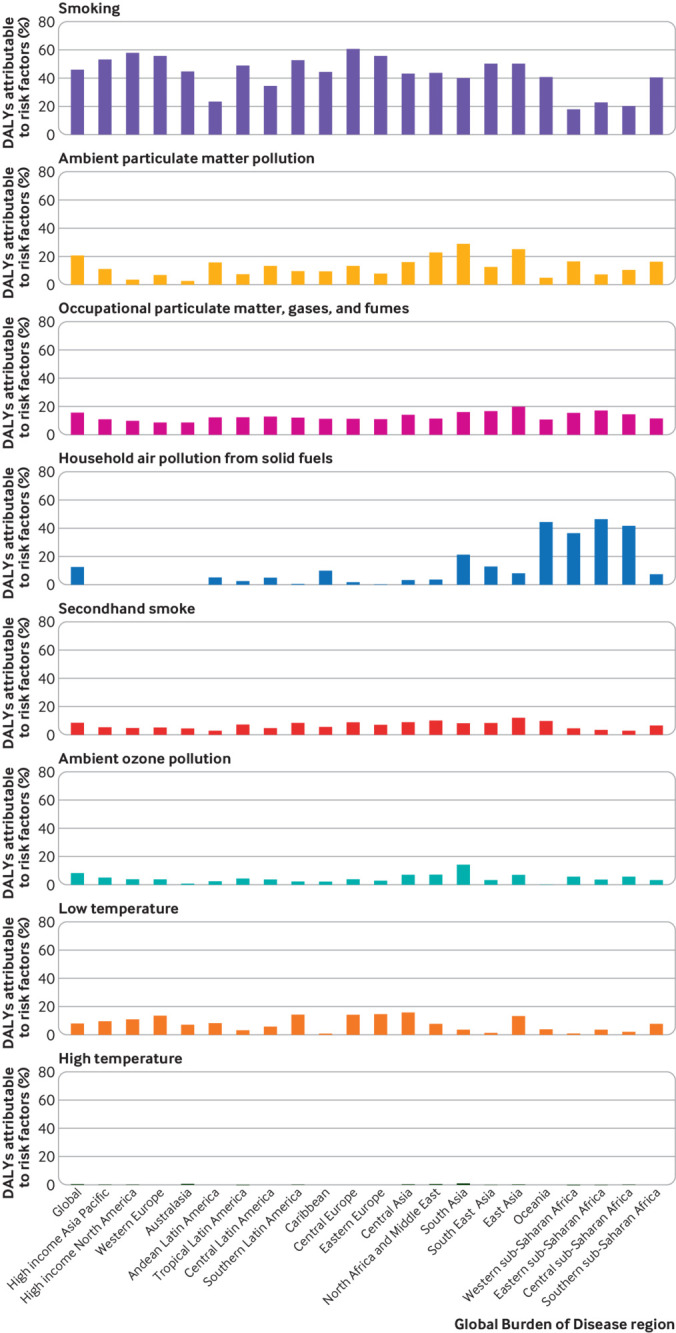
Percentage of disability adjusted life years (DALYs) due to chronic obstructive pulmonary disease attributable to each risk factor for the 21 Global Burden of Disease regions in 2019 (generated from data available at https://ghdx.healthdata.org/gbd-results-tool)
The proportion of DALYs due to COPD attributable to individual risk factors also differed by age group. The proportion of attributable DALYs for smoking increased with age up to 70-74 years and then decreased. Although the highest attributable DALYs for ambient particulate matter pollution was in the 65-69 age group, values did not differ significantly from other age groups. Moreover, the DALYs due to COPD attributable to occupational exposure to particulate matter, gases, and fumes increased with age, and the highest proportion was found in the 70-74 age group (17.9%) (fig S13). Figures S14 and S15 show the proportion of DALYs due to COPD attributable to the individual risk factors for men and women, respectively.
Discussion
Principal findings
In this study, based on data from the Global Burden of Disease 2019 study, we have provided up-to-date information on the prevalence, death, and DALY counts of COPD from 1990 to 2019, together with the age standardised rates across 204 countries and territories. Globally, COPD accounted for 212.3 million prevalent cases, 3.3 million deaths, and 74.4 million DALYs in 2019. Although the age standardised point prevalence, deaths, and DALYs rates due to COPD have decreased over the past three decades, the absolute counts are on the rise, which could be as a result of population growth, as well as population ageing and an increase in life expectancy.
Comparison with other studies
A study in 2018 reported a decrease in the rates of COPD of 2.8% (95% uncertainty interval −6.9% to 0.9%) in years lived with disability at the global level between 2007 and 2017.3 We found a decrease of 39.8% in the age standardised DALY rate of COPD between 1990 and 2019 globally. The differences could be because of variations in time intervals and methodology used in the studies. Also, a direct comparison with the Global Burden of Disease 2017 study is difficult because of several methodological changes between the two datasets.2 A recent study reported the burden of COPD attributable to one risk factor (ambient PM2.5).22 Although the prevalence estimates were not reported, the overall results for the increased death and DALY counts, despite the reduced corresponding rates, were consistent with our findings.22
Epidemiological surveys have shown a prevalence of 11.8% based on the GOLD criteria, 6.0% based on the lower limit of normal criteria in Spain,18 17.8% in the Abeshge District of Ethiopia,19 4.9% in Iran,20 17.5% in Tanzania,26 and 5.9% in China.27 This study found a global age standardised prevalence rate of 2.6%, however, which is considerably lower than in these studies. Several factors could be responsible for this difference: the year the study was conducted, the diagnostic criteria used, the number of participants included in each study, several of the studies were conducted at the subnational rather than the country level, and different methodologies were used to report the prevalence of COPD. Therefore, the observations of individual studies on the burden of COPD cannot be compared with our results because different criteria were used for the definition of COPD and the interpretation of the spirometry results, either before or after inhalation of bronchodilators.28 In the Global Burden of Disease 2017 study, the reference definition used was based on the GOLD criteria after bronchodilation and alternative definitions were adjusted in relation to the reference definition.2
The decrease in the burden of COPD that we found might be explained by the multiple strategies that have been implemented in recent years, such as the universal and comprehensive efforts to restrict tobacco use, improvements in occupational and environmental safety, reducing ambient and household pollution, better access to treatments for reducing the progression of the disease and relieving comorbidities, raising public awareness about preventive strategies, and the increased availability of diagnostic tests for differentiating between COPD and other chronic respiratory diseases.4 28 The Global Burden of Disease project uses an estimation or modelling process, however, rather than reporting real data on the burden of COPD. This process might underestimate the actual COPD burden, which could lead to erroneous policy decisions.
The highest age standardised death rate in 2019 was found in Nepal, with 182.5 deaths per 100 000 population. A recent study used data from the Global Burden of Disease 2019 study to evaluate the burden of respiratory diseases attributable to pollution from ambient particular matter.29 The authors found that Nepal had the highest death rate from COPD caused by air pollution in 2019; 25.9% of the deaths from COPD were caused by exposure to this risk factor.29 With rapid urbanisation in Nepal, the use of motorised vehicles has increased from nearly 224 000 in 1990 to 1.3 million in 2012.30 The high rate of deaths in Nepal might be because of failure to effectively regulate air pollutants and ineffective implementation of air quality control measures.30
We found poor concordance between the point prevalence and death rates attributable to COPD when the regions were ranked. For example, although high income North America had the highest point prevalence for COPD for death rates, it was ranked eighth. This discrepancy is likely because of improvements in diagnostic measures, and better management of COPD and related comorbidities. Conversely, despite having the highest death rate, Oceania was ranked ninth for point prevalence rates, which could be because of premature mortality. Limited access to diagnostic tests and the subsequent late start of treatment, along with poor availability of medications, might shorten the overall survival rate of patients with COPD. This finding was more evident in low income countries where healthcare services are designed to treat acute conditions, such as infectious disorders, and are not appropriately developed to manage chronic diseases.31 The World Health Organization reported that in 2019, bronchodilators and steroid inhalers were covered by only 55% and 19% of primary public healthcare facilities, respectively, in low income countries.32 Also, COPD is often difficult to diagnose,33 and ensuring that sufficient diagnostic equipment is available for each primary healthcare setting in regions where resource are restricted is needed to improve early detection and increase the chances of successful treatment.
The burden of COPD reaches its peak in older adults. Physiologically, diminished lung function in advanced ages, and impaired lung tissue repair and baseline inflammations, could contribute to the increased risk of death.34 35 Moreover, COPD is associated with compromised health status 36 37 and multiple comorbidities,38 which together with the natural comorbidity of old age increases the mortality rate of COPD in elderly people. This study found that people aged 80-84 years accounted for the highest numbers of deaths related to COPD. Previous research has reported that the most significant effect of total air pollution, among non-communicable diseases, is on deaths related to COPD.39 Furthermore, research has estimated that the highest number of deaths from total air pollution were seen in those aged 80-84 years.39 This age pattern is the same as the burden of COPD, suggesting that older individuals are more vulnerable to the adverse effects of air pollution.40
Similar to previous studies,22 39 we found that men had slightly higher age standardised point prevalence, death, and DALY rates, primarily reflecting differential smoking behaviours and exposure to occupational pollution. Studies have postulated that women are more susceptible to developing COPD from smoking than men, however.41 42 A systematic review found that, even after smoking fewer cigarettes, women who smoked had a faster annual reduction in forced expiratory volume in one second than men.43 Also, being a woman was associated with a higher risk of death and admission to hospital from respiratory failure and comorbidities caused by severe COPD.44
This study found that risk factors, such as smoking, pollution from ambient particulate matter, and occupational exposure to particulate matter, gases, and fumes, were the largest contributors to the burden of COPD. Because these risk factors are mainly preventable and the disease can be effectively treated, controlling the burden of COPD requires more attention and a focused effort. Multiple initiatives have been developed to reduce exposure to these risk factors.45 For example, in 2007, WHO endorsed a practical and cost effective plan for controlling the tobacco epidemic, MPOWER: Monitor tobacco use and prevention policies; Protect people from tobacco smoke; Offer help to quit tobacco use; Warn about the dangers of tobacco; Enforce bans on tobacco advertising, promotion, and sponsorship; and Raise taxes on tobacco.46 This programme has six measures, focusing mainly on educating the public about the dangers of tobacco use and banning trade and advertising of tobacco products.46 The latest report on the global tobacco epidemic indicates that 75% of countries, comprising a population of 5.3 billion people, are currently subject to at least one MPOWER measure at the highest level of achievement.28
Global tobacco smoking has decreased by 27.5% over the past three decades.47 Smoking is the most common risk factor for all chronic respiratory conditions5 and, apart from being the leading risk factor for COPD, nearly half of smokers eventually develop the disease.48 49 Therefore, preventing exposure to tobacco smoke would be the most effective long term strategy for reducing the burden of COPD.47 The US has had success in controlling air pollution, mainly driven by interventions such as the 1990 Clean Air Act Amendments and the 2002 Nitrogen Oxides (NOx) State Implementation Plan Call regulation,50 along with provisions for reducing anthropogenic emissions from different types of vehicles.51 Accordingly, the US death burden caused by non-communicable diseases, particularly COPD, substantially decreased (by 54%) from 1990 to 2010.52
In some low income regions, such as Oceania, and western, eastern, and central sub-Saharan Africa, household air pollution from solid fuels was the leading risk factor for COPD, rather than smoking, and this finding was more evident in women. In agreement with our results, a recent study in 13 low and middle income countries reported that participants with a history of exposure to household air pollution were 41% more likely to develop COPD, with a stronger association in women.53 Furthermore, although household air pollution accounted for 13.5% of the prevalence of COPD, smoking explained 12.4% of the prevalence.53 Research in China showed that women who did not smoke had a two to three times higher risk of COPD in rural areas, where exposure to biomass fuels was higher, than women in urban areas.54 Measures such as the use of alternative clean fuels, improving kitchen ventilation, and providing better stoves could reduce the risk of COPD and improve the lung dysfunction in patients with the disease.55 56 57 Consequently, formulating strict health measures towards preventing tobacco smoking and improving air pollution could be crucial approaches for healthcare policy makers in alleviating the burden of COPD. The new Air Quality Guidelines issued by WHO on 21 September 2021 recommend lower concentrations for gaseous and particulate pollutants based on recent evidence of the harmful effects from concentrations below those recommended in 2005.58 Moreover, in November 2021, the European Environment Agency estimated that 58% (178 000) of premature deaths could have been avoided in 2019 if the new WHO’s Air Quality Guidelines had been implemented.59
The relation between DALYs due to COPD and sociodemographic index was not monotonic at the national level, such that a positive association was found between the burden of COPD and the development level of countries, up to middle scores on the sociodemographic index, and then a decreasing trend was observed. Similarly, WHO reported that about 80% of deaths due to COPD occurred in low and middle income countries.60 Moreover, based on the results of the Global Burden of Disease 2019 study, a reverse V shaped correlation was found between the burden of COPD caused by exposure to ambient PM2.5 and the sociodemographic index level.22 Ambient PM2.5 is the leading cause of disease from air pollution globally and the most populated countries, like China and India with middle sociodemographic index scores, are estimated to have had the highest increase in deaths attributable to PM2.5 over the past decade.39 Exposure to ambient particular matter is growing for countries with a lower sociodemographic index and decreasing for countries with a higher sociodemographic index.24 The level of exposure to smoking has decreased for countries with high and middle sociodemographic index scores but the largest reduction were found in countries with a high sociodemographic index.24 Apart from the effect of these individual level risk factors on the relation between sociodemographic index and the burden of COPD, the sociodemographic index is a broad surrogate indicator of poverty. Therefore, countries with a lower sociodemographic index would generally have poor access to healthcare services, including limited availability and affordability of diagnostic and therapeutic measures. These systemic deficiencies contribute to a high disease burden and premature death in patients with COPD.
Ultimately, equitable resource allocation and massive investments in regions with the most DALYs must be made to reduce the burden of COPD more effectively, with recognition that much less attention is paid to chronic respiratory diseases compared with other non-communicable diseases.61 Also, the data reported here showed the substantial variations in the burden of COPD between countries, which should prompt the authorities of the most affected countries to fund new epidemiological surveys to enable a thorough understanding of the natural history of COPD. Because different chronic respiratory diseases have overlapping diagnostic criteria,62 the COPD estimations might benefit from the provision of the least essential diagnostic modalities for every resource limited setting.
Strengths and limitations of this study
A strength of the study is that we have provided up-to-date and comprehensive estimates of levels and trends associated with COPD and its risk factors at the global, regional, and national levels, between 1990 and 2019. The study had several limitations. Firstly, only a small number of high quality epidemiological databases were available to estimate the burden of COPD. Secondly, some risk factors, such as genetic predisposition, although rare, could not be taken into account in our estimations. Thirdly, incorporating claims data into the input record might make the evidence unreliable because the validity is highly dependent on the bias correction process. Underdiagnosis of COPD is likely because of relief of respiratory symptoms by limiting activities that reduce the patient’s likelihood of seeking medical attention. Also, poor access to spirometry and lack of expertise in performing and interpreting spirometry data are important contributors to underdiagnosing COPD.33 Fourthly, many countries do not have efficient systems for registering deaths, and therefore only verbal autopsy studies could be relied on for estimates of deaths. However, as previous studies did not differentiate between the distinct types of chronic respiratory diseases, this information could not be included for reporting the death estimates related to COPD,2 suggesting possible underestimation of the evidence. Improving vital registration systems might improve the accuracy of these data and allow better management of the disease burden. These limitations highlight the importance of improving the accuracy of data collection and the use of more integrated case definitions, which would make comparisons between countries more valid.
Conclusions and policy implications
COPD is a major public health problem with extensive healthcare and economic costs. Although the point prevalence, death, and DALY rates declined during the study period, the corresponding counts are increasing. With an ageing population, COPD will continue to become an even greater problem in the future. The reported global, regional, and national burden of COPD, and its risk factors, could help to provide a more accurate projection of the future disease burden. This knowledge could guide policy makers in planning control measures and supply services to meet the rising healthcare demands that COPD and its comorbidities will create.
What is already known on this topic
A considerable proportion of the burden of chronic respiratory diseases is caused by chronic obstructive pulmonary disease (COPD)
The most recent study to use data from the Global Burden of Disease 2017 study reported decreases in the age standardised mortality and disability adjusted life year (DALY) rates from 1990 to 2017
Smoking was the largest risk factor for deaths due to COPD, and a negative association was found between the burden of COPD and the sociodemographic index
What this study adds
The global age standardised point prevalence, death, and DALY rates for COPD in 2019 were 8.7%, 41.7%, and 39.8% lower than in 1990, respectively
In men, the global DALY rate of COPD increased up to age 85-89 years and then decreased with advancing age, whereas the rate increased up to age ≥95 years in women
Regionally, a reversed V shaped association was found between sociodemographic index and the age standardised DALY rate of COPD, with smoking, ambient particulate matter pollution, and occupational exposure to particulate matter, gases and fumes contributing most to DALYs due to COPD
Acknowledgments
We would like to thank the staff of the Institute for Health Metrics and Evaluation and its collaborators who prepared these publicly available data. The study is based on publicly available data and solely reflects the opinion of its authors and not that of the Institute for Health Metrics and Evaluation. We would also like to acknowledge the support of the Social Determinants of Health Research Centre at the Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Web extra.
Extra material supplied by authors
Web appendix: Supplementary materials
Contributors: SS and A-AK contributed equally as corresponding authors and designed the study. SS and MAM analysed the data and performed the statistical analyses. SS, KC-C, MN, SAN, MJMS, JAH, KA, GSC, A-AK, JSK drafted the initial manuscript. SS and A-AK are the guarantors. All authors reviewed the drafted manuscript for critical content. All authors approved the final version of the manuscript. The corresponding authors (SS and A-AK) attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: The Bill and Melinda Gates Foundation, who were not involved in any way in the preparation of this manuscript, funded the Global Burden of Disease study. This report was funded by Shahid Beheshti University of Medical Sciences, Tehran, Iran (grant No 30336). The funder had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: support from Shahid Beheshti University of Medical Sciences for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Dissemination to participants and related patient and public communities: The results will be disseminated through media outlets and presentations at scientific conferences and academic events. Given that no patients were recruited for the study, there are no plans to disseminate the results to study participants.
The manuscript’s guarantors (SS and A-AK) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Provenance and peer review: Not commissioned; externally peer reviewed.
Publisher’s note: Published maps are provided without any warranty of any kind, either express or implied. BMJ remains neutral with regard to jurisdictional claims in published maps.
Ethics statements
Ethical approval
The study was reviewed and approved by the ethics committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (IR.SBMU.RETECH.REC.1400.862).
Data availability statement
The data used for the analyses in the study are publicly available at https://ghdx.healthdata.org/gbd-results-tool.
References
- 1. Cannon D, Buys N, Sriram KB, Sharma S, Morris N, Sun J. The effects of chronic obstructive pulmonary disease self-management interventions on improvement of quality of life in COPD patients: A meta-analysis. Respir Med 2016;121:81-90. 10.1016/j.rmed.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 2. Vos T, Lim SS, Abbafati C, et al. GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1204-22. 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. James SL, Abate D, Abate KH, et al. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1789-858. 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet 2007;370:765-73. 10.1016/S0140-6736(07)61380-4. [DOI] [PubMed] [Google Scholar]
- 5. Soriano JB, Kendrick PJ, Paulson KR, et al. GBD Chronic Respiratory Disease Collaborators . Prevalence and attributable health burden of chronic respiratory diseases, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir Med 2020;8:585-96. 10.1016/S2213-2600(20)30105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Huertas A, Palange P. COPD: a multifactorial systemic disease. Ther Adv Respir Dis 2011;5:217-24. 10.1177/1753465811400490. [DOI] [PubMed] [Google Scholar]
- 7. Lopez-Campos JL, Calero C, Quintana-Gallego E. Symptom variability in COPD: a narrative review. Int J Chron Obstruct Pulmon Dis 2013;8:231-8. 10.2147/COPD.S42866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Petty TL. Definition, epidemiology, course, and prognosis of COPD. Clin Cornerstone 2003;5:1-10. 10.1016/S1098-3597(03)90003-2. [DOI] [PubMed] [Google Scholar]
- 9. Gerayeli FV, Milne S, Cheung C, et al. COPD and the risk of poor outcomes in COVID-19: A systematic review and meta-analysis. EClinicalMedicine 2021;33:100789. 10.1016/j.eclinm.2021.100789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. May SM, Li JTC. Burden of chronic obstructive pulmonary disease: healthcare costs and beyond. Allergy Asthma Proc 2015;36:4-10. 10.2500/aap.2015.36.3812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.criteria GIfCOLDG. GLOBAL STRATEGY FOR PREVENTION, DIAGNOSIS AND MANAGEMENT OF COPD: 2022 Report 2022 [Available from: https://goldcopd.org/2022-gold-reports-2/ accessed April 2, 2022 2022.
- 12. Burney PG, Luczynska C, Chinn S, Jarvis D. The European Community Respiratory Health Survey. Eur Respir J 1994;7:954-60. 10.1183/09031936.94.07050954 [DOI] [PubMed] [Google Scholar]
- 13.(ECRHS) ECRHS. About the ECRHS 2022 [cited 2022]. Available from: https://www.ecrhs.org/ accessed April 2, 2022 2022.
- 14. Adeloye D, Chua S, Lee C, et al. Global Health Epidemiology Reference Group (GHERG) . Global and regional estimates of COPD prevalence: Systematic review and meta-analysis. J Glob Health 2015;5:020415-15. 10.7189/jogh.05.020415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J 2006;28:523-32. 10.1183/09031936.06.00124605. [DOI] [PubMed] [Google Scholar]
- 16. Rehman AU, Hassali MAA, Muhammad SA, Harun SN, Shah S, Abbas S. The economic burden of chronic obstructive pulmonary disease (COPD) in Europe: results from a systematic review of the literature. Eur J Health Econ 2020;21:181-94. 10.1007/s10198-019-01119-1. [DOI] [PubMed] [Google Scholar]
- 17. Bhatta L, Leivseth L, Mai X-M, et al. Prevalence and trend of COPD from 1995-1997 to 2006-2008: The HUNT study, Norway. Respir Med 2018;138:50-6. 10.1016/j.rmed.2018.03.020. [DOI] [PubMed] [Google Scholar]
- 18. Soriano JB, Alfageme I, Miravitlles M, et al. Prevalence and determinants of COPD in Spain: EPISCAN II. Arch Bronconeumol (Engl Ed) 2021;57:61-9. 10.1016/j.arbr.2020.07.017. [DOI] [PubMed] [Google Scholar]
- 19. Woldeamanuel GG, Mingude AB, Geta TG. Prevalence of chronic obstructive pulmonary disease (COPD) and its associated factors among adults in Abeshge District, Ethiopia: a cross sectional study. BMC Pulm Med 2019;19:181. 10.1186/s12890-019-0946-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sharifi H, Ghanei M, Jamaati H, et al. Burden of obstructive lung disease study in Iran: First report of the prevalence and risk factors of copd in five provinces. Lung India 2019;36:14-9. 10.4103/lungindia.lungindia_129_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Li X, Cao X, Guo M, Xie M, Liu X. Trends and risk factors of mortality and disability adjusted life years for chronic respiratory diseases from 1990 to 2017: systematic analysis for the Global Burden of Disease Study 2017. BMJ 2020;368:m234. 10.1136/bmj.m234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yang X, Zhang T, Zhang Y, Chen H, Sang S. Global burden of COPD attributable to ambient PM2.5 in 204 countries and territories, 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. Sci Total Environ 2021;796:148819. 10.1016/j.scitotenv.2021.148819. [DOI] [PubMed] [Google Scholar]
- 23. Wang H, Abbas KM, Abbasifard M, et al. GBD 2019 Demographics Collaborators . Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1160-203. 10.1016/S0140-6736(20)30977-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Murray CJL, Aravkin AY, Zheng P, et al. GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1223-49. 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang Y. Smoothing splines: methods and applications. Chapman and Hall/CRC, 2011. 10.1201/b10954. [DOI] [Google Scholar]
- 26. Magitta NF, Walker RW, Apte KK, et al. Prevalence, risk factors and clinical correlates of COPD in a rural setting in Tanzania. Eur Respir J 2018;51:1700182. 10.1183/13993003.00182-2017. [DOI] [PubMed] [Google Scholar]
- 27. Zhu B, Wang Y, Ming J, Chen W, Zhang L. Disease burden of COPD in China: a systematic review. Int J Chron Obstruct Pulmon Dis 2018;13:1353-64. 10.2147/COPD.S161555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. López-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology 2016;21:14-23. 10.1111/resp.12660. [DOI] [PubMed] [Google Scholar]
- 29. Wu Y, Song P, Lin S, et al. Global burden of respiratory diseases attributable to ambient particulate matter pollution: findings from the Global Burden of Disease Study 2019. Front Public Health 2021;9:740800. 10.3389/fpubh.2021.740800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kurmi O, Regmi PR, Pant PR. Implication of air pollution on health effects in Nepal: lessons from global research. Nepal J Epidemiol 2016;6:525-7. 10.3126/nje.v6i1.14733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Beran D, Zar HJ, Perrin C, Menezes AM, Burney P, Forum of International Respiratory Societies working group collaboration . Burden of asthma and chronic obstructive pulmonary disease and access to essential medicines in low-income and middle-income countries. Lancet Respir Med 2015;3:159-70. 10.1016/S2213-2600(15)00004-1. [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization. Assessing national capacity for the prevention and control of noncommunicable diseases: report of the 2019 global survey 2020. https://apps.who.int/iris/rest/bitstreams/1272195/retrieve.
- 33. Diab N, Gershon AS, Sin DD, et al. Underdiagnosis and overdiagnosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2018;198:1130-9. 10.1164/rccm.201804-0621CI. [DOI] [PubMed] [Google Scholar]
- 34. Mannino DM, Davis KJ. Lung function decline and outcomes in an elderly population. Thorax 2006;61:472-7. 10.1136/thx.2005.052449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ito K, Barnes PJ. COPD as a disease of accelerated lung aging. Chest 2009;135:173-80. 10.1378/chest.08-1419. [DOI] [PubMed] [Google Scholar]
- 36. Mannino DM, Doherty DE, Sonia Buist A. Global Initiative on Obstructive Lung Disease (GOLD) classification of lung disease and mortality: findings from the Atherosclerosis Risk in Communities (ARIC) study. Respir Med 2006;100:115-22. 10.1016/j.rmed.2005.03.035. [DOI] [PubMed] [Google Scholar]
- 37. Janson C, Marks G, Buist S, et al. The impact of COPD on health status: findings from the BOLD study. Eur Respir J 2013;42:1472-83. 10.1183/09031936.00153712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: Role of comorbidities. Eur Respir J 2006;28:1245-57. 10.1183/09031936.00133805 [DOI] [PubMed] [Google Scholar]
- 39. State of Global Air . 2020 2020. https://www.stateofglobalair.org/sites/default/files/documents/2020-10/soga-2020-report-10-26_0.pdf.
- 40. Bateson TF, Schwartz J. Who is sensitive to the effects of particulate air pollution on mortality? A case-crossover analysis of effect modifiers. Epidemiology 2004;15:143-9. 10.1097/01.ede.0000112210.68754.fa. [DOI] [PubMed] [Google Scholar]
- 41. Sørheim IC, Johannessen A, Gulsvik A, Bakke PS, Silverman EK, DeMeo DL. Gender differences in COPD: are women more susceptible to smoking effects than men?. Thorax 2010;65:480-5. 10.1136/thx.2009.122002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Barnes PJ. Sex differences in chronic obstructive pulmonary disease mechanisms. Am J Respir Crit Care Med 2016;193:813-4. 10.1164/rccm.201512-2379ED. [DOI] [PubMed] [Google Scholar]
- 43. Gan WQ, Man SF, Postma DS, Camp P, Sin DD. Female smokers beyond the perimenopausal period are at increased risk of chronic obstructive pulmonary disease: a systematic review and meta-analysis. Respir Res 2006;7:52. 10.1186/1465-9921-7-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Prescott E, Bjerg AM, Andersen PK, Lange P, Vestbo J. Gender difference in smoking effects on lung function and risk of hospitalization for COPD: results from a Danish longitudinal population study. Eur Respir J 1997;10:822-7. [PubMed] [Google Scholar]
- 45. Duan R-R, Hao K, Yang T. Air pollution and chronic obstructive pulmonary disease. Chronic Dis Transl Med 2020;6:260-9. 10.1016/j.cdtm.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. MPOWER . 2021. https://www.who.int/initiatives/mpower2021.
- 47. Reitsma MB, Flor LS, Mullany EC, Gupta V, Hay SI, Gakidou E. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and initiation among young people in 204 countries and territories, 1990-2019. Lancet Public Health 2021;6:e472-81. 10.1016/S2468-2667(21)00102-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Rennard SI, Vestbo J. COPD: the dangerous underestimate of 15%. Lancet 2006;367:1216-9. 10.1016/S0140-6736(06)68516-4. [DOI] [PubMed] [Google Scholar]
- 49. Lundbäck B, Lindberg A, Lindström M, et al. Obstructive Lung Disease in Northern Sweden Studies . Not 15 but 50% of smokers develop COPD?--Report from the Obstructive Lung Disease in Northern Sweden Studies [published Online First: 2003/02/18]. Respir Med 2003;97:115-22. 10.1053/rmed.2003.1446. [DOI] [PubMed] [Google Scholar]
- 50. Chestnut LG, Mills DM. A fresh look at the benefits and costs of the US acid rain program. J Environ Manage 2005;77:252-66. 10.1016/j.jenvman.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 51. Fann N, Baker KR, Fulcher CM. Characterizing the PM2.5-related health benefits of emission reductions for 17 industrial, area and mobile emission sectors across the U.S. Environ Int 2012;49:141-51. 10.1016/j.envint.2012.08.017. [DOI] [PubMed] [Google Scholar]
- 52. Zhang Y, West JJ, Mathur R, et al. Long-term trends in the ambient PM2.5- and O3-related mortality burdens in the United States under emission reductions from 1990 to 2010. Atmos Chem Phys 2018;18:15003-16. 10.5194/acp-18-15003-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Siddharthan T, Grigsby MR, Goodman D, et al. Association between household air pollution exposure and chronic obstructive pulmonary disease outcomes in 13 low- and middle-income country settings. Am J Respir Crit Care Med 2018;197:611-20. 10.1164/rccm.201709-1861OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ran PX, Wang C, Yao WZ, et al. [The risk factors for chronic obstructive pulmonary disease in females in Chinese rural areas]. Zhonghua Nei Ke Za Zhi 2006;45:974-9. [PubMed] [Google Scholar]
- 55. Zhou Y, Zou Y, Li X, et al. Lung function and incidence of chronic obstructive pulmonary disease after improved cooking fuels and kitchen ventilation: a 9-year prospective cohort study. PLoS Med 2014;11:e1001621. 10.1371/journal.pmed.1001621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Romieu I, Riojas-Rodríguez H, Marrón-Mares AT, Schilmann A, Perez-Padilla R, Masera O. Improved biomass stove intervention in rural Mexico: impact on the respiratory health of women. Am J Respir Crit Care Med 2009;180:649-56. 10.1164/rccm.200810-1556OC [DOI] [PubMed] [Google Scholar]
- 57. Chapman RS, He X, Blair AE, Lan Q. Improvement in household stoves and risk of chronic obstructive pulmonary disease in Xuanwei, China: retrospective cohort study. BMJ 2005;331:1050. 10.1136/bmj.38628.676088.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Organization WH. Environment WECf. WHO global air quality guidelines: particulate matter (PM2. 5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. World Health Organization, 2021. [PubMed] [Google Scholar]
- 59.European Environment Agency (EEA). Cleaner air could have saved at least 178 000 lives across the EU in 2019. 2021.
- 60.Chronic obstructive pulmonary disease (COPD) 2021 [Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)2021.
- 61. Gross CP, Anderson GF, Powe NR. The relation between funding by the National Institutes of Health and the burden of disease. N Engl J Med 1999;340:1881-7. 10.1056/NEJM199906173402406. [DOI] [PubMed] [Google Scholar]
- 62. Perez-Padilla R. Hidden respiratory disease-associated deaths. Int J Tuberc Lung Dis 2008;12:458-64. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary materials
Data Availability Statement
The data used for the analyses in the study are publicly available at https://ghdx.healthdata.org/gbd-results-tool.