Abstract
Background
Cardiac rehabilitation (CR) is associated with improved cardiovascular outcomes. Racial and ethnic differences in CR have been identified, but whether income may attenuate these disparities remains unknown. We evaluated (1) racial/ethnic differences in CR participation in a contemporary sample of insured US adults, and (2) assessed how household income modifies associations between race or ethnicity and CR participation.
Methods and Results
We identified 107 199 individuals with a CR‐qualifying diagnosis between January 1, 2016 and December 31, 2018 in Optum’s de‐identified Clinformatics database. We evaluated associations between race or ethnicity and participation in CR, and assessed interaction between race or ethnicity and annual household income. The mean±SD age of all participants was 70.4±11.6 years; 37.4% were female and 76.0% were White race. Overall, 28 443 (26.5%) attended ≥1 CR sessions. After adjustment, compared with White individuals, the probability of attending CR was 31% lower for Asian individuals (95% CI, 27%–36%), 19% lower for Black individuals (95% CI, 16%–22%), and 43% lower for Hispanic individuals (95% CI, 40%–45%), all P<0.0001. The time to CR attendance was also significantly longer for Asian, Black, and Hispanic individuals. Associations between race or ethnicity and attendance at CR differed significantly across household income categories (P interaction=0.0005); however, Asian, Black, and Hispanic individuals were less likely to attend CR at all incomes.
Conclusions
In a geographically and racially diverse cohort, participation in CR was low overall, and was lowest among Asian, Black, and Hispanic candidates. Household income may impact the link between race or ethnicity and attendance at CR, but substantial racial and ethnic disparities exist across incomes.
Keywords: cardiac rehabilitation, racial disparities, social determinants of health, socioeconomic status
Subject Categories: Cardiovascular Disease, Disparities, Health Services, Social Determinants of Health
Nonstandard Abbreviations and Acronyms
- CR
cardiac rehabilitation
Clinical Perspective.
What Is New?
In a diverse cohort of insured individuals, participation in cardiac rehabilitation (CR) remains low; Asian, Black, and Hispanic individuals were less likely than White individuals to attend CR and had a longer time to CR initiation.
Among Hispanic individuals only, higher income partially attenuated the lower CR participation; however, among all racial and ethnic groups, persistent disparities remained across all incomes.
What Are the Clinical Implications?
New initiatives—such as automatic referral, virtual delivery options, development of CR facilities in underserved or rural areas, community‐based CR, evening delivery options, and home‐based CR—are urgently needed to optimize the secondary prevention benefits of CR and promote equitable cardiovascular outcomes.
Cardiac rehabilitation (CR) combines structured exercise with counseling to optimize secondary prevention of cardiovascular disease. 1 Participation in CR has been associated with reductions in rehospitalization, recurrent cardiovascular events, depression and anxiety, and mortality 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 ; available evidence has suggested that many of these benefits also occur in low‐and middle‐income countries. 13 Professional society guidelines recommend CR for individuals with recent acute myocardial infarction (AMI) or other acute coronary syndrome, chronic stable angina, coronary artery bypass grafting, percutaneous coronary intervention, heart transplant, valve surgery, peripheral arterial disease, or heart failure. 14 Evidence also suggests that both the dose of CR sessions 15 and the time to initiation of CR 16 , 17 , 18 may impact outcomes.
Nevertheless, CR participation remains low. Referral rates range from 10% to 60%, with higher rates among individuals with procedural‐qualifying diagnoses. 19 , 20 , 21 , 22 , 23 Among those referred to CR, few attend, from 14% in those with AMI to 47% among those with coronary artery bypass grafting. 24 , 25 , 26 , 27 Individual factors associated with low CR participation have been identified and include female sex, Black race, Hispanic ethnicity, high comorbidity, low socioeconomic status, longer distance from a CR facility, older age, and nonprocedural‐qualifying diagnosis. 19 , 20 , 21 , 22 , 23 , 25 , 26 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 The National Institute of Minority Health and Health Disparities Research Framework outlines several domains that influence health outcomes among minority individuals, including the health care system, sociocultural environment, the physical or built environment, and behavioral factors. For example, in addition to structural barriers, bias in clinical referral practices may contribute to differences in CR participation and outcomes. 23 However, although disparities in CR participation have been well documented, the extent to which multiple social factors—such as race or ethnicity and income—intersect to influence CR participation is less clear. Our aims in this study were 2‐fold: first, we evaluated contemporary racial and ethnic differences in CR participation in a large contemporary cohort of insured US adults. Second, we examined how household income modifies participation in CR across races and ethnicities to delineate how social disadvantage may provide barriers to CR participation. We hypothesized that Asian, Black, and Hispanic individuals may have lower participation than those of White race, but that the difference would be attenuated by higher household income.
Methods
Study Population
We conducted a retrospective analysis of health claims data, which are available directly from Optum Clinformatics Data Mart (Eden Prairie, MN, optum.com). Because of commercial licensing, the authors do not have permission or authority to share these data or provide direct access to them. Optum is an administrative database including de‐identified inpatient, outpatient, emergency department, pharmacy, and laboratory health claims from individuals with a commercial health insurance plan and Medicare Advantage (C and D). The database is updated annually and provides a geographically and socially diverse sample. Medical claims include diagnostic and procedural coding from the International Classification of Diseases, Ninth and Tenth Revisions (ICD‐9 and ICD‐10) and Current Procedural Terminology. The University of Pittsburgh Institutional Review Board approved this study and classified this investigation as not constituting human subjects research. Because data are entirely de‐identified, informed consent was waived.
We identified individuals aged ≥18 years with an incident CR‐qualifying diagnosis using ICD or Current Procedural Terminology codes between January 1, 2016 and December 31, 2018. CR‐eligible events included those covered by Medicare that required procedural intervention: (1) AMI listed as the first or second diagnosis, (2) coronary artery bypass grafting surgery, (3) valve repair or replacement, and (4) percutaneous coronary intervention. The ICD‐9, ICD‐10, and Current Procedural Terminology codes used to identify qualifying events are listed in Table S1.
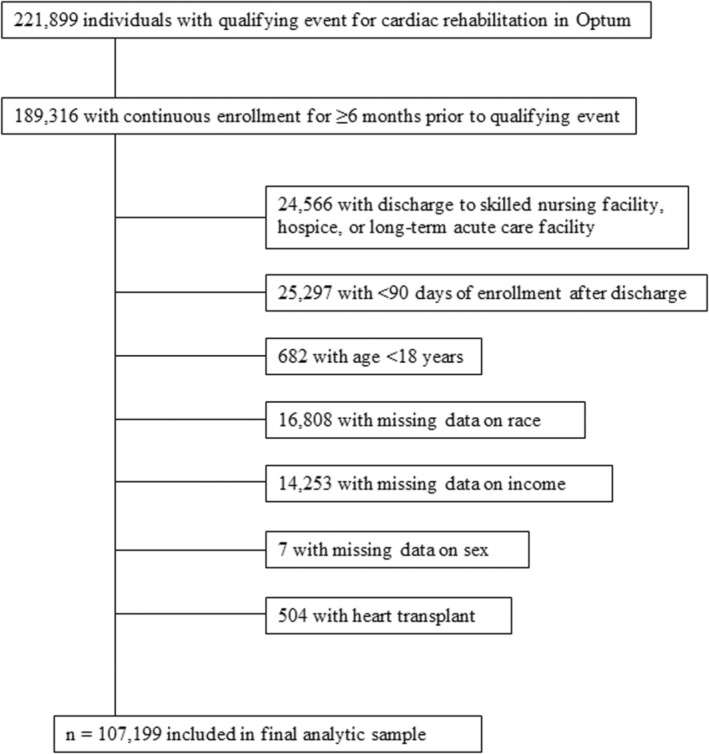
Qualifying events were defined as the first CR‐qualifying event in individuals with continuous enrollment in the database for ≥6 months before the event. The date of study entry was defined as the discharge date for the qualifying diagnosis. Individuals were excluded for disenrollment within 90 days of the hospital discharge. We also excluded individuals discharged to a nursing facility or hospice or missing data on sex, race, ethnicity, or income. We excluded individuals who had cardiac transplant as a qualifying diagnosis because the number of individuals was small and they are likely to have robust social support. Figure 1 summarizes the derivation of the analytic sample.
Figure 1. Flow diagram for participants included in analysis.
Sociodemographic Variables
Collection of sociodemographic variables in Optum has been discussed previously. 37 Age, sex, race, and ethnicity are included in the Optum Clinformatics claims data. Specifically, race and ethnicity are ascertained by public records and imputed from commercial software that utilizes validated algorithms incorporating racial and ethnic neighborhood composition from the US Census, residential zip code, and first and last name. 38 Race and ethnicity were subsequently categorized by Optum as Asian, Black, Hispanic, or non‐Hispanic White.
Derivation of household income in Optum has been described. 37 Briefly, annual household income was estimated and validated from surveys of US households using a comprehensive set of variables that encompass ZIP+4 (a highly specific geographic locator), Internal Revenue Service data, address‐level home value, aggregated credit, and short‐term loans. For this analysis, we analyzed income according to 5 categories: <$40 000; $40 000–$59 999; $60 000–$74 999; $75 000–$99 999; and ≥$100 000.
Covariates
Education level was derived from Census data at the ZIP+4 level and categorized as <12th grade, high school, less than bachelor’s degree, bachelor’s degree or higher, or unknown. To improve model stability, we collapsed these categories into 3 groups: high school or less, less than bachelor's degree, and bachelor’s degree or higher. Clinical covariates included hypertension, diabetes, depression, and ischemic stroke. The Elixhauser Comorbidity Index, a validated index that predicts hospital use and mortality, 39 was calculated using a previously described algorithm 40 and used to adjust for overall comorbid conditions. ICD codes and comorbidity weights are summarized in Table S2. All covariates were defined by ICD‐9 or ICD‐10 codes in claims before or at the time of the incident qualifying diagnosis.
Outcomes
We identified CR participation using appropriate Current Procedural Terminology codes. Our primary outcome was defined as participation (≥1 session) in CR in the 1‐year period following the CR‐qualifying event, stratified by race or ethnicity. Secondary outcomes included (1) number of CR sessions attended by participants who had ≥1 session, and (2) time to initiation of CR, defined as the number of days from discharge to initial CR session.
Statistical Analysis
We characterized sociodemographic and clinical characteristics of CR‐eligible individuals by their means and SDs for continuous variables and by their distributions for categorical variables. We compared these characteristics across race and ethnicity using Kruskal–Wallis tests for continuous variables and χ2 tests for categorical variables.
We evaluated associations between race or ethnicity and initiation of CR by calculating risk ratios and 95% CIs using multivariable‐adjusted Poisson regression. Mean differences and 95% CI for both the number of CR sessions attended and time to initiation of CR were compared with multivariable‐adjusted linear regression. These models were sequentially adjusted using a stepwise process to assess the relative impact of different covariates on the parameter estimates. Model 1 adjusted for age and sex; model 2 additionally adjusted for Elixhauser score, hypertension, diabetes, depression, and ischemic stroke; and model 3 further adjusted for income and education. Model 4 was a fully adjusted model that included the model 3 variables and qualifying event type. To evaluate effect modification of racial and ethnic differences by household income, we included a term for interaction between race or ethnicity and income in models evaluating each outcome; we further visualized the interaction through stratification by household income. Because CR is often underutilized in older adults, 41 we also evaluated interaction between race or ethnicity and age, comparing individuals aged <65 years to those aged ≥65 years to reflect Medicare eligibility. P values for the interaction terms were calculated using generalized score tests for binary outcomes and F tests for continuous outcomes. In all models, we specified empirical SEs. Because of skewness in the continuous outcomes, we replicated these analyses using log‐transformed values and obtained similar results.
All analyses were conducted using SAS version 9.4 (Cary, NC). An a priori 2‐sided α of <0.05 was considered statistically significant.
Results
After application of inclusion and exclusion criteria, the final sample size was 107 199. Eligible individuals were age 70.4±11.6 years; 37.4% were female and 76.0% were White race (Table 1). Overall, 34.2% had a high school degree or lower, and 31.5% had an annual household income of <$40 000. Black individuals were most likely to have a history of hypertension and ischemic stroke, and had the highest Elixhauser comorbidity score. Percutaneous coronary intervention was the most common qualifying diagnosis for CR.
Table 1.
Sociodemographic and Clinical Characteristics of Patients Eligible for Cardiac Rehabilitation, by Race or Ethnicity
| Variable | Total* (N=107 199) | Race or Ethnicity | P value† | |||
|---|---|---|---|---|---|---|
|
Asian n=2651 (2.5%) |
Black n=12 613 (11.8%) |
Hispanic n=10 462 (9.8%) |
White n=81 473 (76.0%) |
|||
| Demographics | ||||||
| Age (y), mean±SD | 70.4±11.6 | 68.7±12.7 | 69.4±11.5 | 70.2±12.1 | 70.6±11.6 | <0.0001 |
| Female sex, n (%) | 40 172 (37.4) | 793 (29.9) | 6211 (49.2) | 3901 (37.3) | 29 267 (35.9) | <0.0001 |
| Household income ($), n (%) | ||||||
| <40k | 33 820 (31.5) | 449 (16.9) | 7083 (56.2) | 3831 (36.6) | 22 457 (27.6) | <0.0001 |
| 40k–<60k | 19 489 (18.2) | 345 (13.0) | 2530 (20.1) | 2389 (22.8) | 14 225 (17.5) | |
| 60k–<75k | 13 153 (12.3) | 324 (12.2) | 1189 (9.4) | 1323 (12.6) | 10 317 (12.7) | |
| 75k–<100k | 17 126 (16.0) | 507 (19.1) | 1027 (8.1) | 1388 (13.3) | 14 204 (17.4) | |
| ≥100k | 23 611 (22.0) | 1026 (38.7) | 784 (6.2) | 1531 (14.6) | 20 270 (24.9) | |
| Education, n (%) | ||||||
| ≤High school | 36 633 (34.2) | 517 (19.5) | 7047 (55.9) | 5306 (50.7) | 23 763 (29.2) | <0.0001 |
| <Bachelor’s degree | 57 647 (53.8) | 1377 (51.9) | 5074 (40.2) | 4443 (42.5) | 46 753 (57.4) | |
| Bachelor’s degree | 12 822 (12.0) | 754 (28.4) | 482 (3.8) | 708 (6.8) | 10 878 (13.4) | |
| Clinical characteristics | ||||||
| Hypertension, n (%) | 99 384 (92.7) | 2387 (90.0) | 12 134 (96.2) | 9913 (94.8) | 74 950 (92.0) | <0.0001 |
| Diabetes, n (%) | 53 822 (50.2) | 1529 (57.7) | 7746 (61.4) | 6826 (65.2) | 37 721 (46.3) | <0.0001 |
| Depression, n (%) | 27 789 (25.9) | 378 (14.3) | 3140 (24.9) | 2729 (26.1) | 21 542 (26.4) | <0.0001 |
| Ischemic stroke/TIA, n (%) | 41 528 (38.7) | 919 (34.7) | 5101 (40.4) | 3927 (37.5) | 31 581 (38.8) | <0.0001 |
| Elixhauser, mean±SD | 16.7±12.5 | 16.1±12.5 | 18.4±12.8 | 16.9±12.6 | 16.4±12.4 | <0.0001 |
| CR qualifying diagnosis, n (%) | ||||||
| Myocardial infarction | 24 040 (24.1) | 581 (23.5) | 3719 (32.0) | 2630 (27.2) | 17 110 (22.5) | <0.0001 |
| CABG | 17 782 (17.8) | 514 (20.8) | 1750 (15.1) | 1630 (16.8) | 13 888 (18.3) | |
| Valve repair/replacement | 16 812 (16.8) | 333 (13.5) | 1582 (13.6) | 1415 (14.6) | 13 482 (17.7) | |
| PCI/stent | 41 170 (41.3) | 1040 (42.1) | 4557 (39.3) | 4005 (41.4) | 31 568 (41.5) | |
CABG indicates coronary artery bypass graft; CR, cardiac rehabilitation; PCI, percutaneous coronary intervention; and TIA, transient ischemic attack.
Percentages for some variables reflect missing values.
From χ2 tests for categorical variables and Kruskal–Wallis tests for continuous variables.
Overall, 28 443 (26.5%) of eligible individuals attended ≥1 CR sessions, ranging from 14.4% in Hispanic individuals to 29.6% in White individuals (Table 2). White individuals were significantly more likely than Asian, Black, or Hispanic individuals to attend CR; after full adjustment, the probability of attending CR was 31% lower for Asian individuals (95% CI, 27%–36%), 19% lower for Black individuals (95% CI, 16%–22%), and 43% lower for Hispanic individuals (95% CI, 40%–45%) relative to White individuals, all P<0.0001. Furthermore, these racial and ethnic differences in CR participation were more pronounced among those aged ≥65 years compared with those aged <65 years, particularly for Asian and Hispanic individuals (Table S3). Among those who participated in CR, the number of sessions attended was 15.3±13.7, which differed significantly by race and ethnicity (P<0.0001). Following adjustment for demographic, clinical, and social factors (model 4), we observed that Black individuals attended a mean 1.4 (95% CI, 0.8– 2.0, P<0.0001) more sessions than White individuals, whereas Hispanic individuals attended 0.8 (95% CI, −1.5 to −0.1, P=0.02) fewer sessions. The time to initiation of CR was 45.8±46.5 days. Compared with White individuals, the time to initiation of CR was an adjusted 9.4 (95% CI, 5.2–13.7), 10.4 (95% CI, 8.1–12.8), and 8.5 (95% CI, 5.8–11.2) days longer for Asian, Black, and Hispanic individuals, respectively.
Table 2.
Association Between Race or Ethnicity and Participation in Cardiac Rehabilitation
| Outcome | Race or Ethnicity | P value* | |||
|---|---|---|---|---|---|
|
Asian n=2651 (2.5%) |
Black n=12 613 (11.8%) |
Hispanic n=10 462 (9.8%) |
White n=81 473 (76.0%) |
||
| Attendance at ≥1 CR sessions | |||||
| n, (%) | 597 (22.5) | 2217 (17.6) | 1510 (14.4) | 24 119 (29.6) | |
| Model 1,† RR (95% CI) | 0.72 (0.67 to 0.77) | 0.61 (0.58 to 0.63) | 0.49 (0.46 to 0.51) | Ref | <0.0001 |
| Model 2‡ | 0.73 (0.68 to 0.78) | 0.64 (0.61 to 0.66) | 0.51 (0.48 to 0.53) | Ref | <0.0001 |
| Model 3§ | 0.67 (0.63 to 0.72) | 0.76 (0.73 to 0.79) | 0.55 (0.53 to 0.58) | Ref | <0.0001 |
| Model 4|| | 0.69 (0.64 to 0.73) | 0.81 (0.78 to 0.84) | 0.57 (0.55 to 0.60) | Ref | <0.0001 |
| Number of sessions attended | |||||
| Mean±SD | 13.6±13.5 | 15.9±14.2 | 13.3±13.4 | 15.4±13.7 | |
| Model 1,† mean diff (95% CI) | 0.7 (−0.2 to 1.7) | 1.4 (0.8 to 2.0) | −0.6 (−1.2 to 0.1) | Ref | <0.0001 |
| Model 2‡ | 0.7 (−0.3 to 1.6) | 1.3 (0.7 to 1.9) | −0.6 (−1.3 to 0.0) | Ref | <0.0001 |
| Model 3§ | 0.7 (−0.3 to 1.6) | 1.4 (0.8 to 2.0) | −0.6 (−1.3 to 0.0) | Ref | <0.0001 |
| Model 4|| | 0.6 (−0.4 to 1.6) | 1.4 (0.8 to 2.0) | −0.8 (−1.5 to −0.1) | Ref | <0.0001 |
| Time to initiation of CR, d | |||||
| Mean±SD | 52.3±51.2 | 57.0±52.4 | 52.7±51.0 | 44.1±45.3 | |
| Model 1,† mean diff (95% CI) | 10.0 (5.9 to 14.1) | 12.8 (10.5 to 15.0) | 9.5 (6.9 to 12.1) | Ref | <0.0001 |
| Model 2‡ | 9.5 (5.4 to 13.5) | 10.9 (8.7 to 13.1) | 8.1 (5.5 to 10.7) | Ref | <0.0001 |
| Model 3§ | 9.2 (5.1 to 13.2) | 10.6 (8.4 to 12.9) | 8.0 (5.4 to 10.6) | Ref | <0.0001 |
| Model 4|| | 9.4 (5.2 to 13.7) | 10.4 (8.1 to 12.8) | 8.5 (5.8 to 11.2) | Ref | <0.0001 |
CR indicates cardiac rehabilitation; and RR, risk ratio.
Score statistic from Poisson or linear regression models. Robust variances were specified in all models.
Adjusted for age and sex.
Adjusted for variables in model 1+Elixhauser score, hypertension, diabetes, depression, and ischemic stroke.
Adjusted for variables in model 2+income and education.
Adjusted for variables in model 3+qualifying diagnosis.
Table 3 summarizes that White individuals were significantly more likely than Asian, Black, or Hispanic individuals to attend ≥1 CR sessions at all income levels. However, the association between race or ethnicity and CR attendance differed across income (adjusted P interaction <0.0001). Notably, an income in the highest 2 categories (≥$75 000 or ≥$100 000) was associated with an attenuation of the lower probability of CR attendance for Hispanic individuals only, although even at the highest income level, the probability of attendance remained substantially lower than for White individuals (risk ratio=0.71, 95% CI, 0.65–0.77, P<0.0001). After adjustment, Black individuals attended significantly more CR sessions than White individuals with the same income for incomes <$100 000, but not for incomes ≥$100 000; this association was not observed for Asian or Hispanic individuals (P interaction=0.04), nor in unadjusted analyses (Table S4). The association between race or ethnicity and time to initiation of CR did not vary significantly by income (P interaction=0.28) (Table 3).
Table 3.
Association Between Race or Ethnicity and Participation in Cardiac Rehabilitation, by Income
| Outcome* by income category, RR (95% CI) | Race or Ethnicity | P interaction† | |||
|---|---|---|---|---|---|
|
Asian n=2651 (2.5%) |
Black n=12 613 (11.8%) |
Hispanic n=10 462 (9.8%) |
White n=81 473 (76.0%) |
||
| Attendance at ≥1 CR sessions‡ | |||||
| <40k | 0.67 (0.53 to 0.84) | 0.83 (0.77 to 0.88) | 0.52 (0.47 to 0.58) | Ref | <0.0001 |
| 40k–<60k | 0.58 (0.46 to 0.74) | 0.78 (0.72 to 0.85) | 0.49 (0.43 to 0.55) | Ref | |
| 60k–<75k | 0.68 (0.56 to 0.84) | 0.77 (0.69 to 0.86) | 0.47 (0.41 to 0.55) | Ref | |
| 75k–<100k | 0.67 (0.57 to 0.79) | 0.83 (0.75 to 0.92) | 0.67 (0.60 to 0.74) | Ref | |
| ≥100k | 0.72 (0.65 to 0.79) | 0.87 (0.79 to 0.96) | 0.71 (0.65 to 0.77) | Ref | |
| Number of CR sessions attended§ | |||||
| <40k | 2.9 (−0.2 to 6.0) | 1.7 (0.7 to 2.7) | −0.5 (−2.0 to 1.0) | Ref | 0.04 |
| 40k–<60k | 1.7 (−1.8 to 5.2) | 1.6 (0.2 to 2.9) | −0.3 (−1.9 to 1.4) | Ref | |
| 60k–<75k | −0.8 (−3.7 to 2.1) | 1.7 (−0.1 to 3.5) | −2.1 (−4.1 to −0.2) | Ref | |
| 75k–<100k | 1.8 (−0.6 to 4.3) | 1.8 (0.3 to 3.4) | −0.9 (−2.3 to 0.6) | Ref | |
| ≥100k | 0.1 (−1.2 to 1.4) | −1.0 (−2.5 to 0.5) | −1.0 (−2.1 to 0.2) | Ref | |
| Time to initiation of CR, d§ | |||||
| <40k | 14.7 (−0.1 to 29.4) | 9.3 (5.4 to 13.3) | 5.8 (−0.2 to 11.8) | Ref | 0.28 |
| 40k–<60k | 9.5 (−4.9 to 24.0) | 12.6 (7.4 to 17.9) | 8.0 (2.2 to 13.7) | Ref | |
| 60k–<75k | −0.4 (−10.2 to 9.4) | 12.7 (5.9 to 19.5) | 5.0 (−1.4 to 11.4) | Ref | |
| 75k–<100k | 13.1 (2.9 to 23.2) | 10.7 (4.8 to 16.6) | 13.1 (6.6 to 19.6) | Ref | |
| ≥100k | 10.1 (4.1 to 16.1) | 4.6 (−1.1 to 10.2) | 9.2 (3.8 to 14.6) | Ref | |
CR indicates cardiac rehabilitation; and RR, risk ratio.
Adjusted for age, sex, Elixhauser score, hypertension, diabetes, depression, ischemic stroke, education, and qualifying diagnosis. Robust variances were specified in all models.
From Poisson or linear regression models with a term for interaction between race or ethnicity and income. P values were calculated with the use of generalized score tests for binary outcomes and F tests for continuous outcomes.
Risk ratios (95% CI) from Poisson regression models.
Mean differences (95% CI) from linear regression models.
Figure 2 highlights the differences in attendance at ≥1 CR sessions, with adjustment for sociodemographic and clinical covariates and stratified by both race or ethnicity and income, where White individuals with an income >$100 000 serve as the referent. Among those with the highest income, individuals of Asian race had a 28% lower probability of attending ≥1 CR sessions compared with the referent (95% CI, 20%–34%, P<0.0001). Similarly, individuals of Black race had an 11% lower probability of attendance (95% CI, 2%–20%, P=0.02) and individuals of Hispanic ethnicity had a 28% lower probability (95% CI, 21%–33%, P<0.0001). Within each racial and ethnic group, income was positively associated with CR attendance in a dose–response manner. Differences in CR attendance relative to the referent were most striking among Asian, Black, or Hispanic individuals with the lowest incomes. For example, compared with White individuals with a household income of ≥$100 000, Hispanic individuals earning <$40 000 annually had a 64% lower probability of attending ≥1 CR sessions (95% CI, 60%–67%, P<0.0001).
Figure 2. Associations between income and participation in ≥1 cardiac rehabilitation sessions, by race or ethnicity.
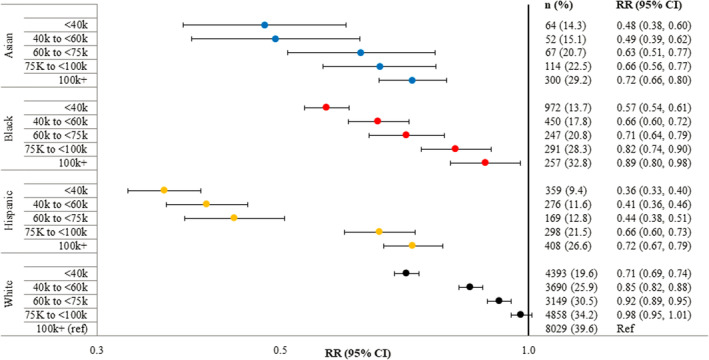
Relative to individuals of White race in the highest income category, those of other race or ethnicity and lower income were less likely to attend ≥1 cardiac rehabilitation sessions. The associations with income differed significantly across race and ethnicity (P interaction <0.0001), but these disparities persisted across all racial/ethnic groups. All results are from Poisson regression models with adjustment for age, sex, Elixhauser score, hypertension, diabetes, depression, ischemic stroke, education, and qualifying diagnosis. RR indicates risk ratio.
Discussion
In this study of a large diverse sample of individuals with qualifying events for CR, most did not participate in CR. Compared with White individuals, Asian, Black, and Hispanic individuals were significantly less likely to attend CR. Asian, Black, and Hispanic individuals also had significantly longer time from their qualifying event to initiation of CR. The association between race or ethnicity and participation in CR varied across income levels; however, racial and ethnic differences persisted at all incomes, even among those in the highest income category. Differences in attendance were most extreme among Asian, Black, and Hispanic individuals in the lowest income categories.
CR Participation by Race or Ethnicity
Our finding that 26.5% of individuals with a CR‐eligible diagnosis participated in CR is consistent with previous work, including a large study of Medicare beneficiaries, in which 24.4% participated. 34 That study also found lower participation among Black and Hispanic individuals. In another analysis of individuals receiving Medicare, Asian, Black, and Hispanic individuals were significantly less likely than White individuals to receive a referral to CR 23 ; a related study found similar results for enrollment in CR among those undergoing cardiac valve surgery. 25 Absence of equitable referral to CR across all races and ethnicities may explain our findings. It has further been noted that individuals of White race are more likely to initiate CR than those of other races and ethnicities, 33 potentially because of structural barriers to participation. Consistent with evidence that older individuals may be less likely to attend CR, 42 we also found larger racial and ethnic differences in CR participation among those aged ≥65 years. Overall, our study further demonstrates significant differences in CR participation across races and ethnicities, possibly exacerbated by age.
Interaction Between Race or Ethnicity and Household Income
Our finding of a positive association between income and attendance at CR is consistent with evidence that socioeconomic factors affect CR participation. 43 , 44 , 45 However, studies of the interaction between race and income in CR are scarce. Several studies have suggested that racial differences in health may vary depending on social factors such as income, although prior research has not focused on CR participation. 46 , 47 , 48 The observation that an income ≥$75 000 was associated with a sharp increase in CR attendance only among Hispanic individuals warrants additional investigation. Nevertheless, differences by race and ethnicity remained at all incomes, with Asian, Black, and Hispanic individuals in the lowest income categories least likely to attend CR. Although few studies have examined racial or ethnic differences in the timing of CR, our observation that Asian, Black, and Hispanic individuals had a significantly longer time to initiation represents an additional challenge even for those who attend CR. In light of the benefit associated with a shorter time to starting CR, 16 , 17 , 18 interventions to promote earlier initiation may augment secondary prevention of cardiovascular outcomes.
Clinical and Public Health Significance
Because CR is a standard of secondary prevention for cardiovascular disease, our observation that Asian, Black, and Hispanic individuals and those of lower income are not fully benefitting from CR, even in a cohort of insured individuals, represents a major clinical concern. The causes of racial and income‐related disparities in CR participation are complex. Neighborhood deprivation has been associated with the use of CR 43 ; cost, transportation, and distance to CR present specific potential barriers. 49 , 50 Even among insured individuals, cost sharing has been associated with lower CR participation in a dose–response manner 51 ; future research should investigate whether variable coverage of CR might mediate racial or ethnic differences in CR participation. In addition, a recent meta‐analysis demonstrated a positive association between health literacy and adherence to treatment, particularly among patients with cardiovascular disease 52 ; however, the role of health literacy in CR participation remains less clear. 53 Structural racism, social capital, or other systemic factors may mediate health outcomes in socially disadvantaged individuals. For example, in a recent study, a social vulnerability index that included a variety of social risk factors was inversely associated with CR participation. 54 To eliminate disparities in individuals eligible for CR, it is crucial to address how social factors influence the utilization of CR services.
Our findings have important implications for developing interventions that may promote CR participation. Initiatives such as automatic referral, virtual delivery options, establishment of CR facilities in underserved or rural areas, community‐based CR, or evening delivery options all have potential to increase participation. Interest has grown recently in home‐based CR, 55 which may provide an alternative to center‐based programs and improve access. However, additional funding is necessary to promote widespread incorporation of home‐based programs into health systems, which will likely require changes in policy. 56 Because home‐based CR may require exercise equipment or mobile supervision, the socioeconomic impediments to these programs also merit consideration. CR practitioners should also better reflect the multicultural diversity of the communities they serve, because the perceived benefit of and rationale for CR may vary across socioeconomic groups. Finally, interventions to improve CR participation must be accessible to all vulnerable groups, such as older adults. Given the benefit of CR for morbidity and mortality, efforts to increase participation rates have the potential to improve clinical outcomes. In addition, alternative secondary prevention programs may be necessary to reach patients who are unable to attend CR. 57
Our study has important strengths. The large sample was racially, ethnically, and socially diverse, facilitating our assessment of interaction. Also, we were able to adjust for clinical and sociodemographic characteristics that are likely related to CR participation.
Study Limitations
Several limitations should be noted. First, we are not able to verify race or ethnicity as provided by Optum. Second, income and education are not individually derived. However, the ZIP+4 is a highly specific geographic indicator and determined without regard to CR participation. Hence, we expect misclassification by income to be nondifferential. Third, because claims data exist primarily for billing and reimbursement, they may incompletely capture qualifying diagnosis or covariates. Fourth, we cannot rule out the possibility of residual confounding, in particular by unmeasured social variables such as health literacy, distance to CR, rurality, family composition, tobacco use, or other factors that may influence the outcomes studied here. For example, we were unable to adjust for geographic location, which has been associated with CR participation. 20 , 34 Fifth, because we excluded those with <90 days of enrollment after discharge or with missing data for some variables, the possibility of selection bias cannot be discounted. However, the resulting sample size provides adequate statistical power for our observations. Finally, our study included only insured individuals; therefore, our results likely underestimate the association between low income and CR participation.
Conclusions
In summary, in a large sample of individuals eligible for CR, participation was low; Asian, Black, and Hispanic individuals were less likely to attend CR and had a longer time to CR initiation. These disparities in CR participation may be modified by household income; nevertheless, they were evident in all income groups. Future studies that evaluate the impact of other social variables—such as health literacy, household composition, or employment status—may further elucidate how social factors interact with race and ethnicity to contribute to disparities in CR participation. This work highlights critical disparities by race and ethnicity, exacerbated by income, and missed opportunities in disadvantaged individuals to achieve the secondary prevention and health benefits of CR.
Sources of Funding
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health (Bethesda, MD) under Award Number T32GM008208. Dr Magnani is supported by National Institutes of Health awards R01HL14301 and R33HL144669; Dr Forman by NIH awards R01AG060499, R01AG058883, and P30AG02482; and Dr Guhl by award T32HL083825 from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosures
None.
Supporting information
Tables S1–S4
For Sources of Funding and Disclosures, see page 9.
References
- 1. Thomas RJ, Balady G, Banka G, Beckie TM, Chiu J, Gokak S, Ho PM, Keteyian SJ, King M, Lui K, et al. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J Am Coll Cardiol. 2018;71:1814–1837. doi: 10.1016/j.jacc.2018.01.004 [DOI] [PubMed] [Google Scholar]
- 2. Choo CC, Chew PKH, Lai SM, Soo SC, Ho CS, Ho RC, Wong RC. Effect of cardiac rehabilitation on quality of life, depression and anxiety in Asian patients. Int J Environ Res Public Health. 2018;15:1095. doi: 10.3390/ijerph15061095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dunlay SM, Pack QR, Thomas RJ, Killian JM, Roger VL. Participation in cardiac rehabilitation, readmissions, and death after acute myocardial infarction. Am J Med. 2014;127:538–546. doi: 10.1016/j.amjmed.2014.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Eijsvogels TMH, Maessen MFH, Bakker EA, Meindersma EP, van Gorp N, Pijnenburg N, Thompson PD, Hopman MTE. Association of cardiac rehabilitation with all‐cause mortality among patients with cardiovascular disease in The Netherlands. JAMA Netw Open. 2020;3:e2011686. doi: 10.1001/jamanetworkopen.2020.11686 [DOI] [PubMed] [Google Scholar]
- 5. Goel K, Pack QR, Lahr B, Greason KL, Lopez‐Jimenez F, Squires RW, Zhang Z, Thomas RJ. Cardiac rehabilitation is associated with reduced long‐term mortality in patients undergoing combined heart valve and CABG surgery. Eur J Prev Cardiol. 2015;22:159–168. doi: 10.1177/2047487313512219 [DOI] [PubMed] [Google Scholar]
- 6. Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship between cardiac rehabilitation and long‐term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation. 2010;121:63–70. doi: 10.1161/circulationaha.109.876383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kasperowicz A, Cymerys M, Kasperowicz T. Effectiveness of cardiac rehabilitation in exercise capacity increase in patients with ST‐segment elevation myocardial infarction. Int J Environ Res Public Health. 2019;16:4085. doi: 10.3390/ijerph16214085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lawler PR, Filion KB, Eisenberg MJ. Efficacy of exercise‐based cardiac rehabilitation post‐myocardial infarction: a systematic review and meta‐analysis of randomized controlled trials. Am Heart J. 2011;162:571–584.e572. doi: 10.1016/j.ahj.2011.07.017 [DOI] [PubMed] [Google Scholar]
- 9. Martin BJ, Hauer T, Arena R, Austford LD, Galbraith PD, Lewin AM, Knudtson ML, Ghali WA, Stone JA, Aggarwal SG. Cardiac rehabilitation attendance and outcomes in coronary artery disease patients. Circulation. 2012;126:677–687. doi: 10.1161/circulationaha.111.066738 [DOI] [PubMed] [Google Scholar]
- 10. Milani RV, Lavie CJ. Impact of cardiac rehabilitation on depression and its associated mortality. Am J Med. 2007;120:799–806. doi: 10.1016/j.amjmed.2007.03.026 [DOI] [PubMed] [Google Scholar]
- 11. Suaya JA, Stason WB, Ades PA, Normand SL, Shepard DS. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54:25–33. doi: 10.1016/j.jacc.2009.01.078 [DOI] [PubMed] [Google Scholar]
- 12. Taylor RS, Walker S, Smart NA, Piepoli MF, Warren FC, Ciani O, Whellan D, O'Connor C, Keteyian SJ, Coats A, et al. Impact of exercise rehabilitation on exercise capacity and quality‐of‐life in heart failure: individual participant meta‐analysis. J Am Coll Cardiol. 2019;73:1430–1443. doi: 10.1016/j.jacc.2018.12.072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mamataz T, Uddin J, Ibn Alam S, Taylor RS, Pakosh M, Grace SL. Effects of cardiac rehabilitation in low‐and middle‐income countries: a systematic review and meta‐analysis of randomised controlled trials. Prog Cardiovasc Dis. 2022;70:119–174. doi: 10.1016/j.pcad.2021.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, Gibbons RJ, Grundy SM, Hiratzka LF, Jones DW, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124:2458–2473. doi: 10.1161/CIR.0b013e318235eb4d [DOI] [PubMed] [Google Scholar]
- 15. Santiago de Araújo Pio C, Marzolini S, Pakosh M, Grace SL. Effect of cardiac rehabilitation dose on mortality and morbidity: a systematic review and meta‐regression analysis. Mayo Clin Proc. 2017;92:1644–1659. doi: 10.1016/j.mayocp.2017.07.019 [DOI] [PubMed] [Google Scholar]
- 16. Candelaria D, Zecchin R, Ferry C, Ladak L, Randall S, Gallagher R. Shorter wait times to cardiac rehabilitation associated with greater exercise capacity improvements: a MULTISITE STUDY. J Cardiopulm Rehabil Prev. 2021;41:243–248. doi: 10.1097/hcr.0000000000000548 [DOI] [PubMed] [Google Scholar]
- 17. Fell J, Dale V, Doherty P. Does the timing of cardiac rehabilitation impact fitness outcomes? An observational analysis. Open Heart. 2016;3:e000369. doi: 10.1136/openhrt-2015-000369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Johnson DA, Sacrinty MT, Gomadam PS, Mehta HJ, Brady MM, Douglas CJ, Paladenech CC, Robinson KC. Effect of early enrollment on outcomes in cardiac rehabilitation. Am J Cardiol. 2014;114:1908–1911. doi: 10.1016/j.amjcard.2014.09.036 [DOI] [PubMed] [Google Scholar]
- 19. Aragam KG, Dai D, Neely ML, Bhatt DL, Roe MT, Rumsfeld JS, Gurm HS. Gaps in referral to cardiac rehabilitation of patients undergoing percutaneous coronary intervention in the United States. J Am Coll Cardiol. 2015;65:2079–2088. doi: 10.1016/j.jacc.2015.02.063 [DOI] [PubMed] [Google Scholar]
- 20. Beatty AL, Truong M, Schopfer DW, Shen H, Bachmann JM, Whooley MA. Geographic variation in cardiac rehabilitation participation in Medicare and Veterans Affairs populations: opportunity for improvement. Circulation. 2018;137:1899–1908. doi: 10.1161/circulationaha.117.029471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brown TM, Hernandez AF, Bittner V, Cannon CP, Ellrodt G, Liang L, Peterson ED, Piña IL, Safford MM, Fonarow GC. Predictors of cardiac rehabilitation referral in coronary artery disease patients: findings from the American Heart Association's Get With the Guidelines Program. J Am Coll Cardiol. 2009;54:515–521. doi: 10.1016/j.jacc.2009.02.080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Golwala H, Pandey A, Ju C, Butler J, Yancy C, Bhatt DL, Hernandez AF, Fonarow GC. Temporal trends and factors associated with cardiac rehabilitation referral among patients hospitalized with heart failure: findings from Get With the Guidelines‐Heart Failure Registry. J Am Coll Cardiol. 2015;66:917–926. doi: 10.1016/j.jacc.2015.06.1089 [DOI] [PubMed] [Google Scholar]
- 23. Li S, Fonarow GC, Mukamal K, Xu H, Matsouaka RA, Devore AD, Bhatt DL. Sex and racial disparities in cardiac rehabilitation referral at hospital discharge and gaps in long‐term mortality. J Am Heart Assoc. 2018;7:e008088. doi: 10.1161/jaha.117.008088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Goel K, Lennon RJ, Tilbury RT, Squires RW, Thomas RJ. Impact of cardiac rehabilitation on mortality and cardiovascular events after percutaneous coronary intervention in the community. Circulation. 2011;123:2344–2352. doi: 10.1161/circulationaha.110.983536 [DOI] [PubMed] [Google Scholar]
- 25. Patel DK, Duncan MS, Shah AS, Lindman BR, Greevy RA Jr, Savage PD, Whooley MA, Matheny ME, Freiberg MS, Bachmann JM. Association of cardiac rehabilitation with decreased hospitalization and mortality risk after cardiac valve surgery. JAMA Cardiol. 2019;4:1250–1259. doi: 10.1001/jamacardio.2019.4032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–1662. doi: 10.1161/circulationaha.107.701466 [DOI] [PubMed] [Google Scholar]
- 27. Zullo MD, Gathright EC, Dolansky MA, Josephson RA, Cheruvu VK, Hughes JW. Influence of depression on utilization of cardiac rehabilitation Postmyocardial infarction: a study of 158 991 MEDICARE BENEFICIARIES. J Cardiopulm Rehabil Prev. 2017;37:22–29. doi: 10.1097/hcr.0000000000000222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Allen JK, Scott LB, Stewart KJ, Young DR. Disparities in women's referral to and enrollment in outpatient cardiac rehabilitation. J Gen Intern Med. 2004;19:747–753. doi: 10.1111/j.1525-1497.2004.30300.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Armstrong MJ, Sigal RJ, Arena R, Hauer TL, Austford LD, Aggarwal S, Stone JA, Martin BJ. Cardiac rehabilitation completion is associated with reduced mortality in patients with diabetes and coronary artery disease. Diabetologia. 2015;58:691–698. doi: 10.1007/s00125-015-3491-1 [DOI] [PubMed] [Google Scholar]
- 30. Balady GJ, Ades PA, Bittner VA, Franklin BA, Gordon NF, Thomas RJ, Tomaselli GF, Yancy CW. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124:2951–2960. doi: 10.1161/CIR.0b013e31823b21e2 [DOI] [PubMed] [Google Scholar]
- 31. Colella TJ, Gravely S, Marzolini S, Grace SL, Francis JA, Oh P, Scott LB. Sex bias in referral of women to outpatient cardiac rehabilitation? A meta‐analysis. Eur J Prev Cardiol. 2015;22:423–441. doi: 10.1177/2047487314520783 [DOI] [PubMed] [Google Scholar]
- 32. Dunlay SM, Witt BJ, Allison TG, Hayes SN, Weston SA, Koepsell E, Roger VL. Barriers to participation in cardiac rehabilitation. Am Heart J. 2009;158:852–859. doi: 10.1016/j.ahj.2009.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Prince DZ, Sobolev M, Gao J, Taub CC. Racial disparities in cardiac rehabilitation initiation and the effect on survival. PM R. 2014;6:486–492. doi: 10.1016/j.pmrj.2013.11.016 [DOI] [PubMed] [Google Scholar]
- 34. Ritchey MD, Maresh S, McNeely J, Shaffer T, Jackson SL, Keteyian SJ, Brawner CA, Whooley MA, Chang T, Stolp H, et al. Tracking cardiac rehabilitation participation and completion among Medicare beneficiaries to inform the efforts of a national initiative. Circ Cardiovasc Qual Outcomes. 2020;13:e005902. doi: 10.1161/circoutcomes.119.005902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Samayoa L, Grace SL, Gravely S, Scott LB, Marzolini S, Colella TJ. Sex differences in cardiac rehabilitation enrollment: a meta‐analysis. Can J Cardiol. 2014;30:793–800. doi: 10.1016/j.cjca.2013.11.007 [DOI] [PubMed] [Google Scholar]
- 36. Shanmugasegaram S, Oh P, Reid RD, McCumber T, Grace SL. Cardiac rehabilitation barriers by rurality and socioeconomic status: a cross‐sectional study. Int J Equity Health. 2013;12:72. doi: 10.1186/1475-9276-12-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. LaRosa AR, Claxton J, O'Neal WT, Lutsey PL, Chen LY, Bengtson L, Chamberlain AM, Alonso A, Magnani JW. Association of household income and adverse outcomes in patients with atrial fibrillation. Heart. 2020;106:1679–1685. doi: 10.1136/heartjnl-2019-316065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. DeFrank JT, Bowling JM, Rimer BK, Gierisch JM, Skinner CS. Triangulating differential nonresponse by race in a telephone survey. Prev Chronic Dis. 2007;4:A60 [PMC free article] [PubMed] [Google Scholar]
- 39. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD‐9‐CM and ICD‐10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83 [DOI] [PubMed] [Google Scholar]
- 40. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004 [DOI] [PubMed] [Google Scholar]
- 41. Lutz AH, Forman DE. Cardiac rehabilitation in older adults: Apropos yet significantly underutilized. Prog Cardiovasc Dis. 2022;70:94–101. doi: 10.1016/j.pcad.2022.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sun EY, Jadotte YT, Halperin W. Disparities in cardiac rehabilitation participation in the United States: a systematic review and meta‐analysis. J Cardiopulm Rehabil Prev. 2017;37:2–10. doi: 10.1097/hcr.0000000000000203 [DOI] [PubMed] [Google Scholar]
- 43. Bachmann JM, Huang S, Gupta DK, Lipworth L, Mumma MT, Blot WJ, Akwo EA, Kripalani S, Whooley MA, Wang TJ, et al. Association of neighborhood socioeconomic context with participation in cardiac rehabilitation. J Am Heart Assoc. 2017;6:e006260. doi: 10.1161/jaha.117.006260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Graversen CB, Johansen MB, Eichhorst R, Johnsen SP, Riahi S, Holmberg T, Larsen ML. Influence of socioeconomic status on the referral process to cardiac rehabilitation following acute coronary syndrome: a cross‐sectional study. BMJ Open. 2020;10:e036088. doi: 10.1136/bmjopen-2019-036088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lemstra ME, Alsabbagh W, Rajakumar RJ, Rogers MR, Blackburn D. Neighbourhood income and cardiac rehabilitation access as determinants of nonattendance and noncompletion. Can J Cardiol. 2013;29:1599–1603. doi: 10.1016/j.cjca.2013.08.011 [DOI] [PubMed] [Google Scholar]
- 46. Bell CN, Thorpe RJ Jr, Bowie JV, LaVeist TA. Race disparities in cardiovascular disease risk factors within socioeconomic status strata. Ann Epidemiol. 2018;28:147–152. doi: 10.1016/j.annepidem.2017.12.007 [DOI] [PubMed] [Google Scholar]
- 47. Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60:191–204. doi: 10.1016/j.socscimed.2004.04.026 [DOI] [PubMed] [Google Scholar]
- 48. Karlamangla AS, Merkin SS, Crimmins EM, Seeman TE. Socioeconomic and ethnic disparities in cardiovascular risk in the United States, 2001–2006. Ann Epidemiol. 2010;20:617–628. doi: 10.1016/j.annepidem.2010.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Leung YW, Brual J, Macpherson A, Grace SL. Geographic issues in cardiac rehabilitation utilization: a narrative review. Health Place. 2010;16:1196–1205. doi: 10.1016/j.healthplace.2010.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sérvio TC, Britto RR, de Melo Ghisi GL, da Silva LP, Silva LDN, Lima MMO, Pereira DAG, Grace SL. Barriers to cardiac rehabilitation delivery in a low‐resource setting from the perspective of healthcare administrators, rehabilitation providers, and cardiac patients. BMC Health Serv Res. 2019;19:615. doi: 10.1186/s12913-019-4463-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Farah M, Abdallah M, Szalai H, Berry R, Lagu T, Lindenauer PK, Pack QR. Association between patient cost sharing and cardiac rehabilitation adherence. Mayo Clin Proc. 2019;94:2390–2398. doi: 10.1016/j.mayocp.2019.07.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Miller TA. Health literacy and adherence to medical treatment in chronic and acute illness: a meta‐analysis. Patient Educ Couns. 2016;99:1079–1086. doi: 10.1016/j.pec.2016.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Aaby A, Friis K, Christensen B, Maindal HT. Health literacy among people in cardiac rehabilitation: associations with participation and health‐related quality of life in the heart skills study in Denmark. Int J Environ Res Public Health. 2020;17:443. doi: 10.3390/ijerph17020443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kianoush S, Al Rifai M, Patel J, George J, Gulati M, Taub P, Moran T, Shapiro MD, Agarwala A, Ullah W, et al. Association of participation in Cardiac Rehabilitation with Social Vulnerability Index: the behavioral risk factor surveillance system. Prog Cardiovasc Dis. 2022. doi: 10.1016/j.pcad.2022.02.003 [DOI] [PubMed] [Google Scholar]
- 55. Thomas RJ, Beatty AL, Beckie TM, Brewer LC, Brown TM, Forman DE, Franklin BA, Keteyian SJ, Kitzman DW, Regensteiner JG, et al. Home‐based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation. 2019;140:e69–e89. doi: 10.1161/cir.0000000000000663 [DOI] [PubMed] [Google Scholar]
- 56. Chindhy S, Taub PR, Lavie CJ, Shen J. Current challenges in cardiac rehabilitation: strategies to overcome social factors and attendance barriers. Expert Rev Cardiovasc Ther. 2020;18:777–789. doi: 10.1080/14779072.2020.1816464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ades PA, Khadanga S, Savage PD, Gaalema DE. Enhancing participation in cardiac rehabilitation: focus on underserved populations. Prog Cardiovasc Dis. 2022;70:102–110. doi: 10.1016/j.pcad.2022.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S4


