Intensive care unit (ICU) sedation practices have dramatically changed over the last 20 years [1–4]. Historically, patients were often deeply sedated to “let them rest” [4]. Strong evidence indicates these practices are dangerous and associated with poor outcomes [5, 6]. Current practice is to use minimum sedation and wake patients up daily while assuring patient comfort [2] (Supplementary Fig. 1).
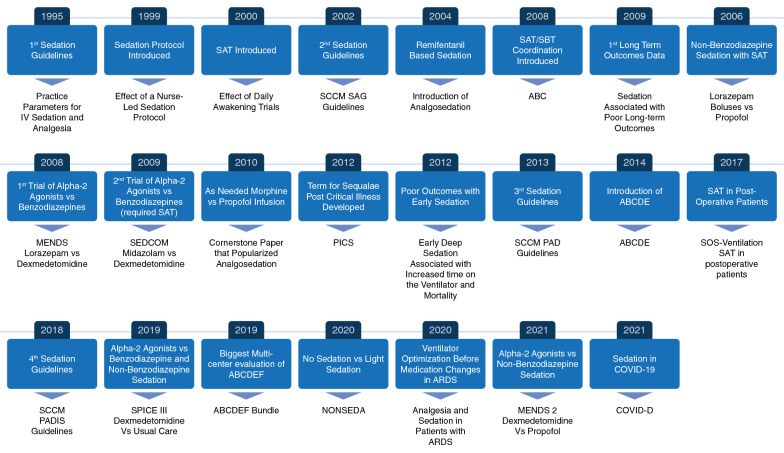
ICU sedation management has changed over the years (Fig. 1). The first set of guidelines on sedation management were published in 1995. These guidelines recommended using midazolam or propofol for short-term sedation and lorazepam for long-term sedation [4]. The Clinical Practice Guidelines for the Sustained Use of Sedatives and Analgesics in the Critically Ill Adult (SAG) [3] were published in 2002. Sedation guidelines were recommended based off data by Brook et al. in 1999 showing protocol-driven sedation resulted in decreased time on ventilation [3]. SAG also suggested to set a daily sedation goal or provide daily interruption of sedation. This recommendation was based off data from Kress et al. showing that a spontaneous awakening trial (SAT) resulted in decreased time on ventilation [3]. In terms of medications, SAG recommended propofol if patients needed rapid neurologic assessments and midazolam for short-term sedation. Lorazepam was recommended as sedation for most patients; no mention of titrating lorazepam to light levels of sedation occurred. Statements indicating paradoxical agitation and post-traumatic stress disorder (PTSD) with light sedation were included.
Fig. 1.
This is timeline of selected landmark trials involved in the evolution of sedation in the ICU. References for this figure are listed from left to right starting at the top in the Electronic Supplementary Material 2. IV, intravenous; SAT, spontaneous awakening trial; SCCM, Society of Critical Care Medicine; SAG, The Clinical Practice Guidelines for the Sustained Use of Sedatives and Analgesics in the Critically Ill Adult; SBT, spontaneous breathing trial; MENDS, Maximizing the Efficacy of Sedation and Reducing Neurological Dysfunction; SEDCOM, Safety and Efficacy of Dexmedetomidine versus Midazolam; PICS, Post Intensive Care Syndrome; PAD, The Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in Adult ICU Patients; ABCDE, Awakening and Breathing Coordination, Delirium monitoring/management, and Early exercise/mobility; SOS, Immediate interruption of sedation compared with usual sedation care in critically ill postoperative patients; PADIS, The Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU; ABCDEF, “A” for Assessment, Prevention, and Manage pain; “B” for Both Spontaneous Awakening Trials and Spontaneous Breathing Trials; “C” for Choice of Analgesia and Sedation; “D” for Delirium Assess, Prevent, and Manage; "E" for Early Mobility and Exercise; and “F” for Family Engagement and Empowerment; SPICE 3, Sedation Practice in Intensive Care Evaluation; NONSEDA, No Sedation or Light Sedation in Critically Ill, Mechanically Ventilated Patients; ARDS, Acute Respiratory Distress Syndrome; MENDS 2, Maximizing the Efficacy of Sedation and Reducing Neurological Dysfunction and Mortality in Sepsis
The Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in Adult ICU Patients (PAD) were published in 2013 [1]. PAD recommended sedatives be titrated to a light level of sedation unless contraindicated. This recommendation was based on studies like Girard et al. which showed that daily SAT coordinated with daily spontaneous breathing trial (SBT) resulted in better clinical outcomes [1] and Treggiari et al. which showed that patients receiving deep sedation were more likely to have PTSD [1]. The concept of “analgosedation” was introduced in the early 2000s by Muellejans et al. [1] using remifentanil based sedation, while Strom et al. implemented a “no sedation” strategy using intermittent morphine [1]. The Richmond Agitation Sedation Scale (RASS) and Sedation Agitation Scale (SAS) were determined to be the most accurate level of arousal assessment tools.
PAD suggested non-benzodiazepines may be preferred to improve clinical outcomes. Carson et al. found that patients randomized to propofol had shorter time on ventilation versus patients that received intermittent lorazepam [1]. Maximizing the Efficacy of Sedation and Reducing Neurological Dysfunction (MENDS) showed that patients that received dexmedetomidine had less delirium and coma and were more likely to be within 1 point of target RASS versus lorazepam [1]. The Safety and Efficacy of Dexmedetomidine versus Midazolam (SEDCOM) study showed that patients that received dexmedetomidine spent less time on ventilation and had less delirium [1].
The ICU Liberation Bundle (ABCDEF: “A” Assessment, Prevention, and Manage pain; “B” Both SAT SBT; “C” Choice of Analgesia and Sedation; “D” Delirium Assess, Prevent, and Manage; "E" Early Mobility and Exercise; and “F” Family Engagement and Empowerment) was developed to implement PAD [7]. ABCDEF has now been studied in over 25,000 patients showing improvement in clinical outcomes. In 2012, Post Intensive Care Syndrome (PICS) was defined as patients that have physical, cognitive, and/or psychological impairment post critical illness [6] which is often secondary to delirium and increased time in the ICU. In 2012, Shehabi et al. found that early deep sedation resulted in increased time on ventilation and mortality [5]. In postoperative patients without severe acute respiratory distress syndrome (ARDS), Chanques et al. reported that the immediate interruption of sedation compared to moderate sedation was associated better clinical outcomes [8].
The Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU (PADIS) were published in 2018 [2]. PADIS suggested light sedation. PADIS suggested using propofol in cardiac patients and either propofol or dexmedetomidine in medical or non-cardiac surgical patients.
Since publication of PADIS, Sedation Practice in Intensive Care Evaluation (SPICE 3) [9] and Maximizing the Efficacy of Sedation and Reducing Neurological Dysfunction and Mortality in Sepsis (MENDS 2) [10] have been published showing no difference in dexmedetomidine versus usual care (SPICE III) or propofol (MENDS 2) in clinical outcomes. No Sedation or Light Sedation in Critically Ill, Mechanically Ventilated Patients (NONSEDA) randomized patients to no sedation versus light sedation finding no difference in 90 day mortality or ventilator/ICU free days [11].
Greater than 503 million cases of coronavirus disease 2019 (COVID-19) have been reported as of April 2022. Patients with severe COVID-19 can develop ARDS sometimes require deep sedation placing patients at risk for delirium and coma. The COVID-D study found that 64% and 71% of patients received benzodiazepines and propofol for a median of 7 days respectively [12]. In patients with ARDS, choosing the best ventilator setting should be prioritized over increasing analgosedation [13]. However, it is clear that light sedation is not possible in most with severe ARDS or during neuromuscular blockade. This highlights the importance of daily interprofessional discussion of the ABCDEF Bundle to ensure that an individualized approach is taken toward sedation management and utilization of light sedation occurs again when possible.
High quality evidence is lacking in sedation research secondary to heterogeneity of data and resistance to practice change. Future directions include using a standardized approach allowing for meaningful comparisons between studies [14]. Additionally, use of inhaled anesthetics for sedation of critically ill patients is promising [15].
This paper provided an overview of how ICU sedation practices have evolved over the last 20 years. Contemporary ICU sedation practices include light levels of sedation, SAT, and use of non-benzodiazepines. The current COVID-19 pandemic has placed unprecedented demands on ICU workforce and challenged sedation practices [13]. It is urgent that clinicians reengage bundled based strategies such as the ABCDEF Bundle to promote liberation from the ventilator and promote recovery and survivorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 Approach to Sedation Management in the Intensive Care Unit. This shows an approach to using sedation in patients in the Intensive Care Unit. RASS=Richmond Agitation Sedation Scale, SAS=Sedation Agitation Scale, SAT=Spontaneous Awakening Trial, SBT=Spontaneous Breathing Trial (PDF 57 kb)
Conflict of interests
JLS is the Vice Co-Chair of the Society of Critical Care Medicine’s most recent Pain, Agitation, Delirium, Immobility and Sleep Clinical Practice Guideline Committee. MCB is the Co-Chair of the Society of Critical Care Medicine’s most recent Pain, Agitation, Delirium, Immobility and Sleep Clinical Practice Guideline Committee. GC is the Analgesia Lead of the Society of Critical Care Medicine’s most recent Pain, Agitation, Delirium, Immobility and Sleep Clinical Practice Guideline Committee
Funding
MCB currently receives research support from the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number R01HL14678-01. She has received past honoraria from the Society of Critical Care Medicine for her work related to the ICU Liberation Collaborative. GC received fees for speaker (Orion Pharma, Aspen Medical) and for expert board (Orion Pharma).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Barr J, Fraser GL, Puntillo K, Ely EW, Gelinas C, Dasta JF, Davidson JE, Devlin JW, Kress JP, Joffe AM, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263–306. doi: 10.1097/CCM.0b013e3182783b72. [DOI] [PubMed] [Google Scholar]
- 2.Devlin JW, Skrobik Y, Gelinas C, Needham DM, Slooter AJC, Pandharipande PP, Watson PL, Weinhouse GL, Nunnally ME, Rochwerg B, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46(9):e825–e873. doi: 10.1097/CCM.0000000000003299. [DOI] [PubMed] [Google Scholar]
- 3.Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002;30(1):119–141. doi: 10.1097/00003246-200201000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Shapiro BA, Warren J, Egol AB, Greenbaum DM, Jacobi J, Nasraway SA, Schein RM, Spevetz A, Stone JR. Practice parameters for intravenous analgesia and sedation for adult patients in the intensive care unit: an executive summary. Society of Critical Care Medicine. Crit Care Med. 1995;23(9):1596–1600. doi: 10.1097/00003246-199509000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Shehabi Y, Bellomo R, Reade MC, Bailey M, Bass F, Howe B, McArthur C, Seppelt IM, Webb S, Weisbrodt L, et al. Early intensive care sedation predicts long-term mortality in ventilated critically ill patients. Am J Respir Crit Care Med. 2012;186(8):724–731. doi: 10.1164/rccm.201203-0522OC. [DOI] [PubMed] [Google Scholar]
- 6.Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, Zawistowski C, Bemis-Dougherty A, Berney SC, Bienvenu OJ, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012;40(2):502–509. doi: 10.1097/CCM.0b013e318232da75. [DOI] [PubMed] [Google Scholar]
- 7.Pun BT, Balas MC, Barnes-Daly MA, Thompson JL, Aldrich JM, Barr J, Byrum D, Carson SS, Devlin JW, Engel HJ, et al. Caring for critically ill patients with the ABCDEF bundle: results of the ICU liberation collaborative in over 15,000 adults. Crit Care Med. 2019;47(1):3–14. doi: 10.1097/CCM.0000000000003482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chanques G, Conseil M, Roger C, Constantin JM, Prades A, Carr J, Muller L, Jung B, Belafia F, Cisse M, et al. Immediate interruption of sedation compared with usual sedation care in critically ill postoperative patients (SOS-Ventilation): a randomised, parallel-group clinical trial. Lancet Respir Med. 2017;5(10):795–805. doi: 10.1016/S2213-2600(17)30304-1. [DOI] [PubMed] [Google Scholar]
- 9.Shehabi Y, Howe BD, Bellomo R, Arabi YM, Bailey M, Bass FE, Bin Kadiman S, McArthur CJ, Murray L, Reade MC, et al. Early sedation with dexmedetomidine in critically ill patients. N Engl J Med. 2019;380(26):2506–2517. doi: 10.1056/NEJMoa1904710. [DOI] [PubMed] [Google Scholar]
- 10.Hughes CG, Mailloux PT, Devlin JW, Swan JT, Sanders RD, Anzueto A, Jackson JC, Hoskins AS, Pun BT, Orun OM, et al. Dexmedetomidine or propofol for sedation in mechanically ventilated adults with sepsis. N Engl J Med. 2021;384(15):1424–1436. doi: 10.1056/NEJMoa2024922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olsen HT, Nedergaard HK, Strom T, Oxlund J, Wian KA, Ytrebo LM, Kroken BA, Chew M, Korkmaz S, Lauridsen JT, et al. Nonsedation or light sedation in critically ill, mechanically ventilated patients. N Engl J Med. 2020;382(12):1103–1111. doi: 10.1056/NEJMoa1906759. [DOI] [PubMed] [Google Scholar]
- 12.Pun BT, Badenes R, Heras La Calle G, Orun OM, Chen W, Raman R, Simpson BK, Wilson Linville S, Hinojal Olmedillo B, Vallejo de la Cueva A, et al. Prevalence and risk factors for delirium in critically ill patients with COVID-19 (COVID-D): a multicentre cohort study. Lancet Respir Med. 2021;9(3):239–250. doi: 10.1016/S2213-2600(20)30552-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chanques G, Constantin JM, Devlin JW, Ely EW, Fraser GL, Gelinas C, Girard TD, Guerin C, Jabaudon M, Jaber S, et al. Analgesia and sedation in patients with ARDS. Intensive Care Med. 2020;46(12):2342–2356. doi: 10.1007/s00134-020-06307-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ward DS, Absalom AR, Aitken LM, Balas MC, Brown DL, Burry L, Colantuoni E, Coursin D, Devlin JW, Dexter F, et al. Design of clinical trials evaluating sedation in critically ill adults undergoing mechanical ventilation: recommendations from Sedation Consortium on Endpoints and Procedures for Treatment, Education, and Research (SCEPTER) Recommendation III. Crit Care Med. 2021;49(10):1684–1693. doi: 10.1097/CCM.0000000000005049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meiser A, Volk T, Wallenborn J, Guenther U, Becher T, Bracht H, Schwarzkopf K, Knafelj R, Faltlhauser A, Thal SC, et al. Inhaled isoflurane via the anaesthetic conserving device versus propofol for sedation of invasively ventilated patients in intensive care units in Germany and Slovenia: an open-label, phase 3, randomised controlled, non-inferiority trial. Lancet Respir Med. 2021;9(11):1231–1240. doi: 10.1016/S2213-2600(21)00323-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary file1 Approach to Sedation Management in the Intensive Care Unit. This shows an approach to using sedation in patients in the Intensive Care Unit. RASS=Richmond Agitation Sedation Scale, SAS=Sedation Agitation Scale, SAT=Spontaneous Awakening Trial, SBT=Spontaneous Breathing Trial (PDF 57 kb)