Abstract
Objective:
Behavioral obesity treatment implemented in primary care is efficacious but typically involves face-to-face or phone contact. We evaluated enrollment, engagement, and 12-week weight losses in a fully-automated online behavioral weight loss intervention implemented pragmatically in a primary care network.
Methods
As part of routine primary care, providers and nurse care managers offered a no-cost online obesity treatment program to 1721 patients. Of these, 721 consented and were eligible (aged 18–75 years with a BMI≥25kg/m2 and Internet access) and 464 started the program. The program included 12 weekly online lessons, a self-monitoring platform, and automated feedback.
Results:
More than one quarter of patients offered the program (26%) initiated treatment. In intent-to-treat analyses using all data available, mean 12-week weight change was −5.10% (SE = 0.21). Patients who submitted their weights on all 12 weeks (37% of 464) lost an estimated 7.2% body weight vs 3.4% in those submitting less frequently.
Conclusions:
This fully-automated online program, implemented into the routine workflow of a primary care setting without any human counseling or researcher involvement, produced clinically meaningful short-term weight losses. Greater program engagement was associated with greater weight loss; efforts are needed to understand barriers to engagement.
Keywords: Obesity, behavioral weight loss, primary care, pragmatic trial
INTRODUCTION
Obesity affects over 40% of U.S. adults and heightens risk for cardiometabolic disease, cognitive decline, other forms of morbidity, and mortality [1,2], making obesity treatment a vital public health priority. Gold-standard behavioral obesity treatments (i.e., diet, exercise, behavior therapy) elicit 5–10% weight loss and confer long-term health benefits [2,3]. Despite their known efficacy, the reach of behavioral weight loss programs is limited by low availability caused by a lack of trained providers, and high treatment costs for providers/patients [2,4], thus diminishing their potential public health impact.
One method for improving the reach and impact of behavioral weight loss programs is to implement them in the most widely utilized healthcare setting in the U.S.: primary care [5]. Primary care medical teams (e.g., physicians, nurses, care coordinators) serve nearly 25% of the U.S. population every month [6]. This patient population is racially and socio-economically diverse, and the majority (60%) meet criteria for overweight/obesity [6]. Current guidelines for primary care providers [2,7] recommend obesity screening, diagnosis, and referral to intensive lifestyle interventions as standard practice. However, rates of obesity treatment in primary care are low. Between 2008–2012, rates of providing and referring patients to obesity treatment declined from 33% in 2008–2009 to 21% in 2012–2013 [8]. Common barriers for medical teams include lack of time, training, resources, and reimbursement [9].
Automated online delivery of empirically-based behavioral weight loss treatment has the potential to reduce costs, improve access, and facilitate integration into the existing workflow of primary care delivery. Our team developed a fully-automated, 12-week online lifestyle intervention, Rx Weight Loss (RxWL), that has produced mean weight losses of 5.8±4.4% in 154 primary care patients [10], 5.8±5.2% in 75 adults in a work setting [11], and 4.2±5.3% in 230 community adults [4] across 3 clinical trials. RxWL demonstrates good patient acceptability and engagement, and it is more cost-effective than in-person treatment [4,10]. Further, whereas many available treatments require regular clinician contact and coaching [12,13], the full automation of RxWL substantially reduces burden on the medical team and thus maximizes scalability in routine care settings.
Having demonstrated the efficacy of the program, we are currently conducting a clinical trial to determine the effectiveness of the RxWL program offered by medical teams to a broad range of patients and implemented without researcher or clinician-involvement. The aims of the clinical trial are a) to determine whether providing enhanced (vs. basic) training to nurse care managers improves implementation outcomes in the primary care setting and b) to compare two different schedules for a 9-month maintenance program against an education control condition on 1-year weight loss outcomes. Although the trial is ongoing, we believe it is important to present results related to recruitment, initial weight losses, and engagement in the 12-week program. The primary outcomes analysis will be conducted using data from the electronic health record (EHR) and most patients will not have had a clinic visit within 12 weeks of the clinical encounter that led to them enrolling in the RxWL program. Thus, the test of primary outcomes, which focuses on weight loss at 1-year, will not yield a precise estimate of weight loss at the end of the initial 12-week program, which we present here. Also, to our knowledge, this is the first fully-automated online behavioral weight loss program to be integrated into the routine workflow of a state-wide primary care organization [5], and thus this paper’s 12-week outcome data will provide an important benchmark for evaluating future pragmatic implementations of weight loss programs in primary care.
METHODS
Design Overview
We conducted a type II hybrid effectiveness-implementation trial [14] that tested an online obesity treatment and its implementation in primary care. The rationale and design of this trial have been previously described [15]. The trial met PRECIS criteria for a pragmatic trial [16] and was conducted in partnership with a state-wide primary care organization. The study protocol was approved by the Rhode Island Hospital Institutional Review Board.
In brief, the study was conducted at Rhode Island Primary Care Physician’s Corporation (RIPCPC), a primary care practice organization which includes approximately 60 practices with 100 physicians. The 16 nurse care managers (NCMs) employed by RIPCPC were randomly assigned to an enhanced or a standard implementation arm (results presented here are for all NCMs combined) and offered the RxWL program to patients during routine care. NCMs briefly described the weight loss program to patients whom they believed to be eligible and appropriate for this intervention (based on age, weight status, and overall health). Patients who expressed interest were given a “prescription for weight loss” with a unique referral code to access the online study platform. The number of “prescriptions” distributed by the nurses was used to determine the potential reach of the program. Patients who visited the study website were provided with study information, invited to complete an electronic informed consent, and screened for eligibility. All eligible participants received access to the free 12-week RxWL program. Participants were randomly assigned to one of three maintenance programs upon joining RxWL (two different schedules of 9-month maintenance program or education control group) but were not informed about this assignment until after completing the 12-week program. Data collection and analysis for the maintenance phase is ongoing. The present manuscript focuses on the recruitment, engagement, and weight losses during the initial 12-week treatment.
Participants
RIPCPC patients who had a body mass index (BMI) ≥ 25kg/m2, were age 18–75 years old, had Internet access, and were English fluent and literate were eligible. Broad inclusion criteria such as these are appropriate for pragmatic trials in which a medical team selects individuals for treatment and also to maximize potential reach and uptake in a usual care setting. Exclusion criteria included current use of a weight loss medication or liquid diet; current, planned, or recent (<6 months) pregnancy; a medical condition that restricts unsupervised physical activity; and inability to walk two blocks without stopping. Participants who were not eligible were referred back to their primary care team for alternative treatment options.
Intervention
RxWL is a behavioral weight loss program with an initial 12-week weight loss phase that is informed by the intervention strategy used in the Diabetes Prevention Program [17] and Look AHEAD Intensive Lifestyle Intervention [18]. The program, which targets healthy eating, physical activity, and behavioral skills to promote weight change, has been described in detail in a prior publication [13]. RxWL includes 3 core components: weekly online lessons, submission of self-monitored weight, energy intake, and activity data, and personalized, automated feedback [15]. Participants are given goals for weight loss (i.e., 10% of initial body weight), daily energy intake (i.e., 1200–1500kcal/day for patients weighing ≤250lbs, and 1500–1800kcal/day for patients weighing >250lbs), and activity (i.e., gradual increase to 200 mins/week of moderate-to-vigorous intensity physical activity). Participants self-monitor their progress toward these goals daily and submit self-monitored data within the RxWL portal each week. The program provides options for reducing energy intake by reducing fat intake or following a Mediterranean-style eating plan and for self-monitoring using a commercially-available smartphone application that was linked to the RxWL platform, or paper diaries. Participants are strongly encouraged to have a scale at home to allow for regular weighing or use a scale available in the community (e.g., at a local gym); scales are not provided. Automated feedback that is tailored for the participant based on their self-monitored data is provided weekly. The feedback included encouragement, praise for meeting goals, and/or constructive feedback. The program was made available at no cost to all patients who consented.
Measures
Demographics.
After consenting, participants self-reported their age, biological sex, racial background (i.e., American Indian/Alaskan Native, Asian or Pacific Islander, Black or African American, White, Other) and ethnic background (i.e., Hispanic/Latinx, Non-Hispanic) via an electronic survey at baseline. This information was collected to characterize the sample; the participants chose from categories selected by the researchers.
Body weight.
Participants were asked to weigh themselves at least once weekly, preferably daily, and submitted their self-reported body weight data using the online portal each week. These self-reported data were used to calculate percent weight loss from Week 1 to Week 12 (post-treatment). The final weight reported each week was used to calculate weight change for that week. Prior work demonstrates that self-reported and measured weights are highly correlated [19].
Engagement.
We used 2 different measures of engagement with RxWL: the proportion of RxWL lessons accessed and proportion of weeks that at least one body weight was reported. Both measures were automatically extracted from the online intervention platform.
Statistical Analyses
Analyses were conducted using IBM SPSS Statistics v.25.0 [20] and R v.3.6.0 [21]. Descriptive statistics were computed for baseline characteristics and demographics. Independent samples t-tests and Pearson’s chi-square analyses examined potential differences between individuals who achieved a minimum level of engagement with the intervention necessary for inclusion in this analysis and those who did not.
The analysis examining 12-week weight change was conducted via linear mixed effects models using maximum likelihood estimation, following the intent-to-treat (ITT) principle. All available weights entered by patients were included in analysis. The model included fixed linear and quadratic effects of time on the primary outcome—weight change—operationalized as percent change from baseline. Covariates of patient age, BMI, sex (male/female), and identification with a racial/ethnic minority group (yes/no) were included as fixed effects. Random intercepts and linear time slopes accounted for nesting of observations within individuals. Least-squares mean estimates of weight loss at 12 weeks were also calculated.
Given the novelty of testing a fully-automated online obesity treatment with no routine adjunctive intervention from clinicians/researchers (which typically increase engagement [22] and weight loss[23]), it was also important to examine engagement metrics in this trial. To summarize patient engagement with the RxWL platform (i.e., adherence), descriptive statistics were computed for accessing the video lessons and frequency of self-reporting weight. For both measures, we calculated the total number of weeks (maximum 12) in which a patient viewed a video lesson, as well as the number of weeks in which a patient reported at least one weight. We then examined the association between program engagement and weight change by adding dichotomous predictor variables representing lessons accessed (all 12 lessons versus fewer) and number of weeks that weight was reported (all 12 versus fewer) to the linear mixed effects model. Finally, we used multivariate linear regression to test whether demographic characteristics or baseline BMI were associated with engagement.
RESULTS
Patient Enrollment
As outlined in the CONSORT Diagram (Figure 1), 1,765 patients were referred to the program, of whom 721 (41%) consented and were eligible to participate. Of these, 654 patients enrolled in the program and created RxWL accounts; 464 of the 654 enrolled patients (71%) entered at least one weight after baseline, allowing them to be included in analysis (i.e., 26% of those originally offered the program). Since patients who were offered the program but did not enroll in the program did not provide informed consent, it was not possible to compare their characteristics to those who did enroll. However, no significant differences were detected on age, BMI, sex, race, or ethnicity when comparing engaged participants (N=464) versus those who enrolled in the study but did not engage with the intervention by entering at least one weight after baseline (N=190; ps≥.22).
Figure 1. Flow of Participants Through the Trial.
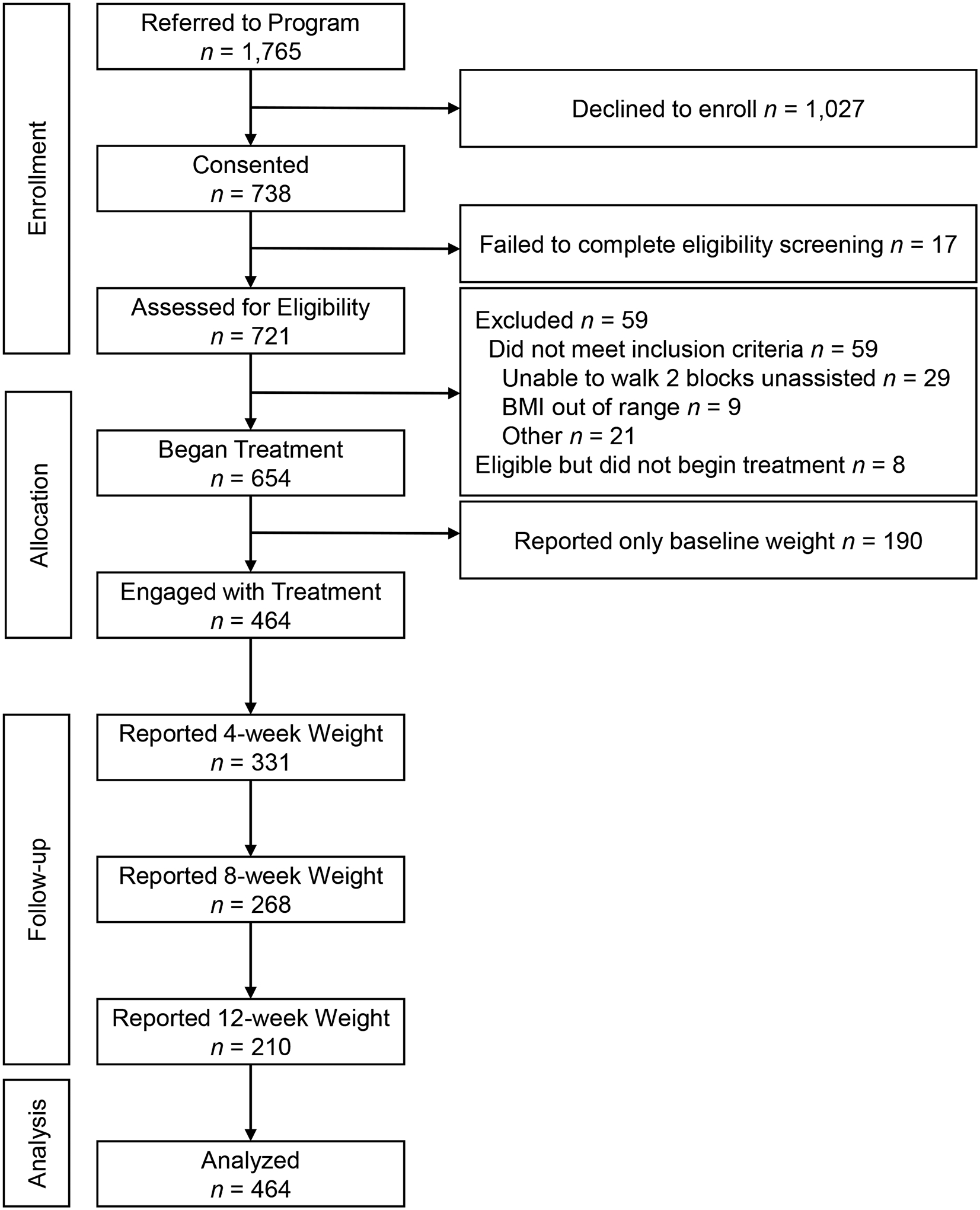
Primary care patients were recruited to participate in a pragmatic trial of a fully-automated online obesity treatment in the state of Rhode Island between 2018–2021.
Patient Characteristics
The 464 participants who engaged with the treatment program were 52.6 (SD=13.2) years of age, and the average BMI was 36.2 (SD=6.9). The majority of patients in the sample were female (70%) and White (94%). A small portion of the sample (n=11; 2%) self-identified as Hispanic or Latinx ethnicity. Patient characteristics are reported in Table 1.
Table 1.
Baseline characteristics of participants analyzed in this study (N=454).
| Characteristic | N (%) or M (SD) |
|---|---|
| Gender | |
| Female | 326 (70.3%) |
| Male | 138 (29.7%) |
| Race | |
| American Indian/Alaska Native | 1 (0.2%) |
| Asian or Pacific Islander | 5 (1.1%) |
| Black or African American | 12 (2.6%) |
| White | 437 (94.2%) |
| Other | 9 (1.9%) |
| Ethnicity | |
| Hispanic/Latinx | 11 (2.4%) |
| Non-Hispanic | 453 (97.6%) |
| Age | 52.6 (13.2) |
| BMI (kg/m2) | 36.2 (6.9) |
Notes: M = Mean; BMI = Body Mass Index; SD = Standard Deviation.
12-Week Weight Change Outcomes
Figure 2 shows weight loss estimates; the estimated marginal mean weight change at week 12 was −5.1% (SE=0.2), which corresponded to a change of −5.1 kg (SE=.02). Significant fixed linear (b=−0.52, SEb=0.02, t(737.01) = −26.27, p<.0001) and quadratic (b=0.02, SEb=0.001, t(2957.86) =14.02, p<.0001) effects of time on percent weight loss were detected, indicating that patient weight declined on average from baseline to 12 weeks, and that the rate of weight loss slowed over time (Figure 2). There were no significant fixed intercept effects of age, BMI, sex, or identification with a racial/ethnic minority group on weight loss (ps≥.18).
Figure 2. Proportion (%) of Patients Reporting Weight and Weight Loss by Week of Treatment in an Online Obesity Treatment Program.
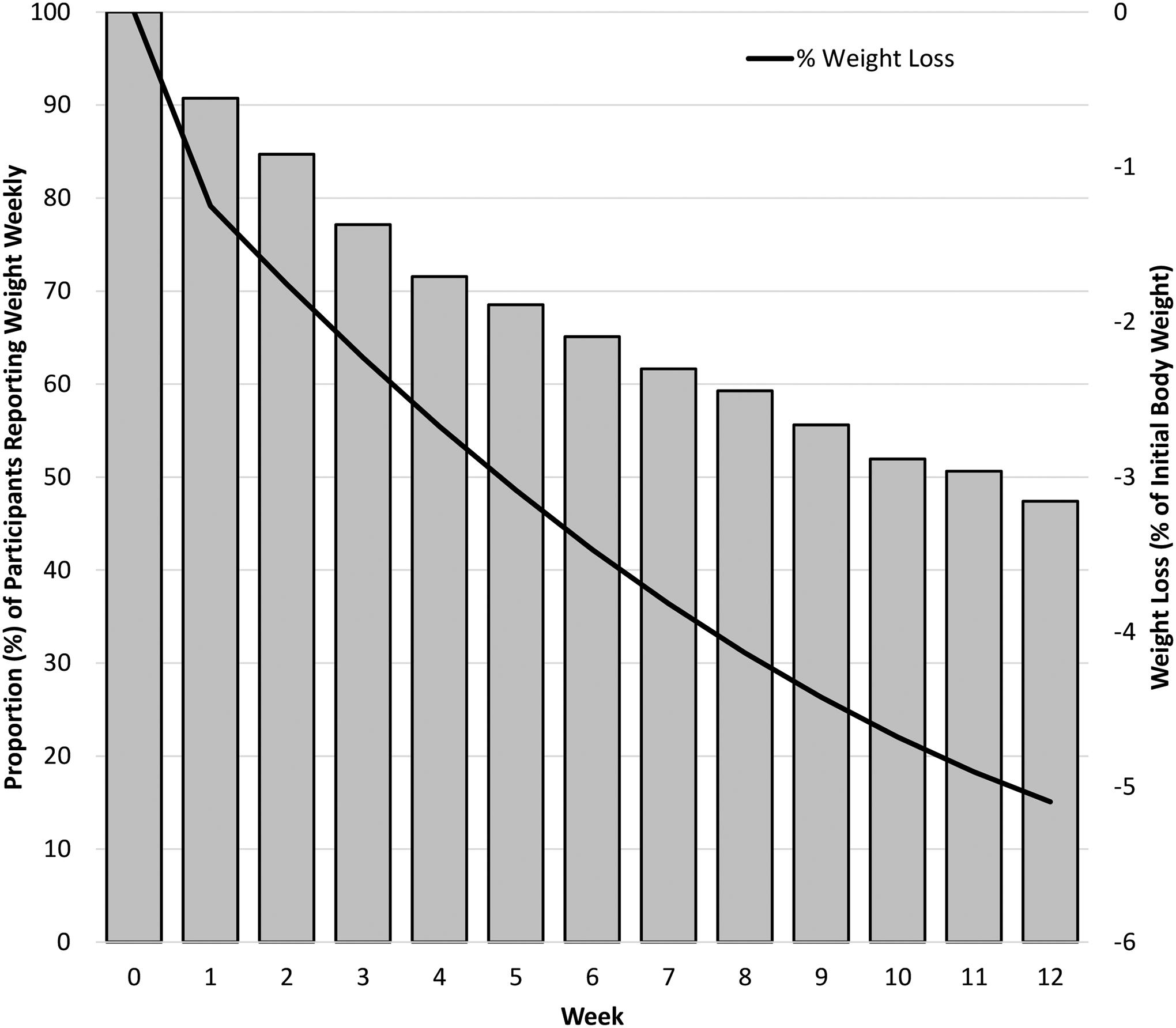
Figure depicts the percent of all primary care patients who reported their weight (a metric of engagement), and weight loss (percent of initial body weight) by the number of weeks since enrollment in the program. Patients participated in a pragmatic trial of a fully-automated online obesity treatment in the state of Rhode Island from 2018 to 2021.
Program Engagement and Weight loss Outcomes
As expected, the proportion of patients entering a weight decreased gradually over the 12-week period (see bars in Figure 2). Patients entered a weight on an average of 7.8 of the 12 weeks post-baseline (SD=4.3), with 172 (37%) reporting weight on all 12 weeks. The mean number of lessons viewed was 6.5 (SD=4.1). Although a number of patients only accessed 1 video lesson (n=53; 12%) or 2 lessons (n=47; 10%) throughout the program, 91 patients (20%) accessed all 12 video lessons. Most (86%) of patients who watched all 12 lessons also provided weight data on all weeks. On average, patients reached the 7th week before discontinuing their engagement with the video lessons (M=7.2, SD=4.2).
Patients who reported their weight on all 12 weeks achieved an estimated weight loss of 7.2% (SE=0.3) compared to 3.4% (SE=0.3) for patients who submitted their weight on fewer than 12 weeks (p<.0001). Similarly, patients who accessed all 12 lessons achieved an estimated weight loss of 8.0% (SE=0.4) compared to 4.2% (SE = 0.2) for patients who accessed fewer lessons (p<.0001). Neither BMI, sex, nor identification with a racial/ethnic minority group were associated with these measures of engagement (ps≥.19), but age was associated with a greater number of lessons viewed (b=0.09, SEb=0.01, t(456)=6.73, p<.0001.)
DISCUSSION
In our earlier efficacy studies [4,10,11], the initial 12-week weight loss phase of an automated online behavioral obesity treatment program—RxWL—produced weight losses of approximately 5.6 kg or 5% of initial body weight. In a previous randomized controlled trial conducting in the primary care setting, this weight loss was significantly greater than the 1.4% observed in an online newsletter control condition [10]. We now provide effectiveness data for the 12-week RxWL program when it was implemented in a state-wide primary care practice network in 464 patients with overweight/obesity. To our knowledge, this is one of the first studies to examine the effectiveness of a fully automated, comprehensive weight loss intervention delivered as part of the routine clinical workflow of primary care. Thus, the results reported here are novel, and provide some of the first data on the effectiveness of a fully automated program on 12-week weight loss. ITT analysis showed that RxWL produced an estimated mean weight loss of 5.1% of initial body weight (M =5.1kg, SE= 0.2) at 12-weeks. In primary care settings, most e-health obesity treatments report mean weight losses of about 2.5% initial body weight at 12- or 24-weeks in ITT analyses [13,24,25], and fully-remote e-health programs typically produce mean weight losses of 2.2 kg [12].
These weight loss findings are particularly notable because RxWL is a fully-automated program that was pragmatically implemented in primary care, and the weight losses observed here are largely the result of patients’ independent efforts. Clinical providers identified and enrolled patients and supported their participation but did not provide regular, ongoing support during participation. Furthermore, the research team had no participant contact except to resolve basic technical problems with the online platform (e.g., password reset) and did not provide incentives for reporting weights at any point. Even among digital lifestyle interventions that have been offered in primary care, most require significant researcher involvement, trained provider time [24], or in-person or phone contact [26,27], minimizing scalability. The few fully-remote weight loss programs that have been integrated into primary care settings are low-intensity and produce weight losses of only 0.8%−2.4% [13,25,28]. Given that weight losses of 3–5% are recommended to improve cardiovascular risk factors among individuals with obesity [2], the weight losses produced by RxWL as implemented here are clinically significant. If used widely, the public health impact of such an effective, low-cost, easily scalable program could be considerable.
Engagement with RxWL was variable, as expected, given the pragmatic implementation of the RxWL program in the RIPCPC practice network. Patients who engaged for at least one week (71%) tended to self-report their weight on about two-thirds of the weeks and on average accessed just over half the skills training lessons. These findings are on par with those from a lower-intensity digital weight loss program [25], which found that although 38% of participants either never logged in or only watched 1–2 lessons, those who engaged watched a mean 8.6 of 12 lessons. In ITT analysis using all available data from RxWL, individuals who accessed all 12 lessons (20% of the sample) were estimated to achieve nearly double the weight loss of those who accessed fewer than 12 lessons (about 8% versus 4%). A similar pattern was observed for adherence to self-monitoring of weight; weight losses of those who entered their weight on all 12 weeks (37% of the sample) were twice as large as those who entered fewer weights (7.4% vs 3.2%). Thus, although there are challenges to engaging patients in online obesity treatment [29], those who do engage tend to achieve very favorable outcomes. Moreover, in this study 20–37% of the patients studied met these high criteria for engagement.
Our analyses also suggested that the weight loss outcomes did not differ significantly across sex, age, BMI, or race/ethnicity. While older individuals had better engagement with the online lessons, as is typical [30], we found no effect of age on weight loss outcomes. This differs from prior studies suggesting that older individuals have better initial weight loss outcomes [31,32], even in studies using online programs [33]. Our ability to examine race/ethnicity was hampered by the fact that 94% of participants self-identified as White. Nevertheless, it is encouraging that the online program appeared to have consistent effects across demographic groups.
We found that 26% of those who accepted a “prescription” to the program ultimately engaged with it (i.e., entered at least one week of weight loss data). Previous studies of online weight loss programs in primary care report uptake rates of 7% [26], 15% [25], 26% [24], and 27% [13], suggesting that rates of uptake in RxWL were better than or on par with prior work. There were two major points of disengagement: a) about half of patients who accepted a “prescription” never engaged with the online platform at all, and b) an additional 29% disengaged after beginning the program but before completing the first week. The failure to even visit the program may reflect the fact that it was easier for a patient to accept a referral than it would be to decline it. The second point of disengagement, which is consistent with the rate at which commercial apps are downloaded but used only once [20], may reflect ambivalence on the part of the patient or a decision that the program does not fit their needs. There are very few data from other weight loss programs for comparison, because it is hard to define the number of individuals who are invited to join any given program. Further elucidation of the potential reasons why patients did not pursue the full program after receiving a “prescription” are beyond the scope of this paper, however, in a qualitative formative evaluation with RIPCPC clinicians, several factors were perceived as barriers to patient uptake and engagement, including challenges with technology literacy, motivation, fear of change, and other conditions that complicate treatment (i.e., depression and anxiety [34]). Additional research is needed to better understand barriers to engagement with online obesity treatment in primary care, and how to address them using innovative intervention approaches.
Key strengths of this study include use of a fully-automated online obesity treatment program with established efficacy [4,10,11] and a pragmatic implementation that relied entirely on primary care treatment teams to engage and support patients. This approach allowed us to study real-world rates of uptake and engagement. In addition, the analytic approach followed the ITT principle and is thus superior to a completers-only approach.
This report also has important limitations. The initial 12-week weight loss program was offered to all eligible participants, and thus there was no control group for comparison. However, in our original efficacy study [10], we found that RxWL produced significantly greater weight losses than a 12-week internet-delivered education-only intervention. The data presented are based on self-reported weight which have been shown to be accurate but are not without some bias [19]. Future reports will capitalize on data from the EHR to evaluate longer-term weight loss outcomes. However, because most patients are unlikely to have a clinic visit within 3 months of enrolling in the program, it was necessary to use self-reported weight data in this report. Another important limitation is the homogeneous sample of largely White women (the demographic who present most often for behavioral obesity treatment) who are likely to have been highly motivated to engage with treatment. Engaging men, individuals of racial and ethnic minority backgrounds, and individuals with treatment ambivalence remains a significant challenge [35–37], which we had hoped would be mitigated by delivery in the primary care setting. Further analyses will help determine whether the disproportionately small number of men and racial/ethnic minorities enrolled in this program results from the characteristics of the patients seen in these practices, a bias on the part of the clinicians in referring patients to the program, or lack of interest in weight loss expressed by these patients. Efforts to increase initial engagement with the program will help determine the effectiveness of the program in patients who may be less motivated to lose weight.
CONCLUSION
Pragmatic implementation of an established, fully-automated online behavioral obesity treatment in a large primary care practice network produced a mean weight loss of 5% of initial body weight at the end of the initial 12-week treatment period. This is consistent with national guidelines [2] for minimum clinically significant weight loss for first-line treatment. Individuals with high treatment engagement lost an estimated 7–8%, a very favorable outcome. This report provides preliminary evidence for the potential of fully-automated online treatment to serve as a pragmatic resource in the primary care setting for addressing the epidemic of obesity.
Study Importance Questions.
- What is already known about this subject?
- Primary care is often where obesity is first addressed, but primary care clinicians often have few resources to offer patients for weight loss.
- Previous trials of behavioral obesity treatment delivered in the primary care setting have typically involved intensive researcher involvement to deliver treatment and/or maintain participants’ engagement with the research study.
- What are the new findings in your manuscript?
- This is one of the first times that a fully automated online obesity treatment program has been tested pragmatically in a large primary care practice network with clinicians taking responsibility for identifying patients, offering the program, and supporting its use.
- Primary care clinicians were able to implement the program pragmatically and weight loss outcomes were encouraging, and similar to those observed in efficacy trials.
- How might your results change the direction of research or the focus of clinical practice?
- This manuscript demonstrates that clinicians can successfully implement an online obesity treatment program pragmatically in a large primary care practice network.
- The results have implications for implementing and disseminating behavioral obesity treatment in the primary care setting and for pragmatic research studying implementation and effectiveness outcomes.
Acknowledgements
Contributors.
We wish to thank study participants for devoting their time and energy to participate in this research, Rhode Island Primary Care Physicians Corporation (RIPCPC) leadership and nurse care managers for implementing the study and treatment program within their practice network, and members of our research team for assisting with data collection.
Funders.
This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (R18 DK114715) and training grants from the National Heart, Lung, and Blood Institute (T32 HL076134; K23 HL136845) and the National Institute on Minority Health and Health Disparities (K23 MD015092).
Declaration of Interest:
The authors report grants from NIH/NIDDK during the conduct of the study. Dr. Thomas also reports personal fees from Lumme Health Inc., and Dr. Wing reports personal fees from Noom Inc., outside the submitted work. The other authors have no conflicts of interest to declare.
Footnotes
Clinical Trial Registration Number: ClinicalTrials.Gov identifier NCT03488212: https://clinicaltrials.gov/ct2/show/NCT03488212
Prior presentations. None
Data sharing statement.
Deidentified study data representing reported findings may be available on reasonable request from the corresponding author, JGT.
References
- 1.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief, no 360. Hyattsville, MD: National Center for Health Statistics. 2020. [PubMed] [Google Scholar]
- 2.Jensen MD, Ryan DH, Donato KA, et al. Executive summary: guidelines (2013) for the management of overweight and obesity in adults. Obesity. 2014;22:S5–S39. [DOI] [PubMed] [Google Scholar]
- 3.Look AHEAD Research Group. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170:1566–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leahey TM, Thomas G, Fava JL, et al. Adding evidence-based behavioral weight loss strategies to a statewide wellness campaign: a randomized clinical trial. Am J Public Health. 2014;104:1300–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tronieri JS, Wadden TA, Chao AM, Tsai AG. Primary care interventions for obesity: review of the evidence. Curr Obes Rep. 2019;8:128–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Ambulatory care use and physician office visits. http://www.cdc.gov/nchs/fastats/physician-visits.htm. Updated April 14, 2021. Accessed October 30, 2020.
- 7.Curry SJ, Krist AH, Owens DK, et al. Behavioral weight loss interventions to prevent obesity-related morbidity and mortality in adults: US Preventive Services Task Force recommendation statement. JAMA. 2018;320:1163–1171. [DOI] [PubMed] [Google Scholar]
- 8.Fitzpatrick SL, Stevens VJ. Adult obesity management in primary care, 2008–2013. Prev Med. 2017;99:128–133. [DOI] [PubMed] [Google Scholar]
- 9.Kraschnewski JL, Sciamanna CN, Stuckey HL, et al. A silent response to the obesity epidemic: decline in US physician weight counseling. Med Care. 2013:186–192. [DOI] [PubMed] [Google Scholar]
- 10.Thomas JG, Leahey TM, Wing RR. An automated internet behavioral weight-loss program by physician referral: a randomized controlled trial. Diabetes Care. 2015;38:9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ross KM, Wing RR. Implementation of an internet weight loss program in a worksite setting. J Obes. 2016;2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hutchesson MJ, Rollo ME, Krukowski R, et al. eHealth interventions for the prevention and treatment of overweight and obesity in adults: a systematic review with meta-analysis. Obes Rev. 2015;16:376–392. [DOI] [PubMed] [Google Scholar]
- 13.Little P, Stuart B, Hobbs FR, et al. An internet-based intervention with brief nurse support to manage obesity in primary care (POWeR+): a pragmatic, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4:821–828. [DOI] [PubMed] [Google Scholar]
- 14.Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50:217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Espel-Huynh HM, Wing RR, Goldstein CM, Thomas JG. Rationale and design for a pragmatic effectiveness-implementation trial of online behavioral obesity treatment in primary care. Contemp Clin Trials. 2019;82:9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thorpe KE, Zwarenstein M, Oxman AD, et al. A pragmatic–explanatory continuum indicator summary (PRECIS): a tool to help trial designers. J Clin Epidemiol. 2009;62:464–475. [DOI] [PubMed] [Google Scholar]
- 17.Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25:2165–2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Look AHEAD Research Group. The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity. 2006;14:737–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luo J, Thomson CA, Hendryx M, et al. Accuracy of self-reported weight in the Women’s Health Initiative. Public Health Nutr. 2019;22:1019–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.IBM Corp. IBM SPSS Statistics for Windows. Version 25.0. Armonk, NY: IBM Corp; 2017. [Google Scholar]
- 21.R Core Team. R: A language and environment for statistical computing. Version 3.4.1. Vienna, Austria: R Foundation for Statistical Computing; 2019. [Google Scholar]
- 22.Beleigoli A, Andrade AQ, Diniz MDF, Ribeiro AL. Personalized web-based weight loss behavior change program with and without dietitian online coaching for adults with overweight and obesity: randomized controlled trial. J Med Internet Res. 2020;22:e17494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McVay M, Steinberg D, Askew S, Bennett GG. Provider Counseling and Weight Loss Outcomes in a Primary Care-Based Digital Obesity Treatment. J Gen Intern Med. 2019;34:992–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bennett GG, Herring SJ, Puleo E, Stein EK, Emmons KM, Gillman MW. Web-based weight loss in primary care: a randomized controlled trial. Obesity. 2010;18:308–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yardley L, Ware LJ, Smith ER, et al. Randomised controlled feasibility trial of a web-based weight management intervention with nurse support for obese patients in primary care. Int J Behav Nutr Phys Act. 2014;11:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ma J, Yank V, Xiao L, et al. Translating the Diabetes Prevention Program lifestyle intervention for weight loss into primary care: a randomized trial. JAMA Intern Med. 2013;173:113–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McDoniel SO, Wolskee P, Shen J. Treating obesity with a novel hand-held device, computer software program, and Internet technology in primary care: the SMART motivational trial. Patient Educ Couns. 2010;79:185–191. [DOI] [PubMed] [Google Scholar]
- 28.Rothert K, Strecher VJ, Doyle LA, et al. Web-based weight management programs in an integrated health care setting: a randomized, controlled trial. Obesity. 2006;14:266–272. [DOI] [PubMed] [Google Scholar]
- 29.Bennett GG, Glasgow RE. The delivery of public health interventions via the Internet: actualizing their potential. Annu Rev Public Health. 2009;30:273–292. [DOI] [PubMed] [Google Scholar]
- 30.Burgess E, Hassmén P, Pumpa KL. Determinants of adherence to lifestyle intervention in adults with obesity: a systematic review. Clin Obes. 2017;7:123–135. [DOI] [PubMed] [Google Scholar]
- 31.Diabetes Prevention Program Research Group. The influence of age on the effects of lifestyle modification and metformin in prevention of diabetes. J Gerontol A Biol Sci Med Sci. 2006;61:1075–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Espeland MA, Rejeski WJ, West DS, et al. Intensive weight loss intervention in individuals ages 65 years or older: results from the Look AHEAD type 2 diabetes trial. J Am Geriatr Soc. 2013;61:912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Svetkey LP, Clark JM, Funk K, et al. Greater weight loss with increasing age in the weight loss maintenance trial. Obesity. 2014;22:39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Espel-Huynh HM, Goldstein CM, Finnegan OL, Elwy AR, Wing RR, Thomas JG. Primary care clinicians’ perspectives on clinical decision support to enhance outcomes of online obesity treatment in primary care: a qualitative formative evaluation. J Technol Behav Sci. 2021:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Byrd AS, Toth AT, Stanford FC. Racial disparities in obesity treatment. Curr Obes Rep. 2018;7:130–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity. 2012;20:1234–1239. [DOI] [PubMed] [Google Scholar]
- 37.Goldberg JH, Kiernan M. Innovative techniques to address retention in a behavioral weight-loss trial. Health Educ Res. 2005;20:439–447. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Deidentified study data representing reported findings may be available on reasonable request from the corresponding author, JGT.


