Abstract
The interaction between the metabolic activities of the intestinal microbiome and its host forms an important part of health. The basis of this interaction is in part mediated by the release of microbially-derived metabolites that enter the circulation. These products of microbial metabolism thereby interface with the immune, metabolic, or nervous systems of the host to influence physiology. Here, we review the interactions between the metabolic activities of the microbiome and the systemic metabolism of the host. The concept that the endocrine system includes more than just the eukaryotic host component enables the rational design of exogenous interventions that shape human metabolism. An improved mechanistic understanding of the metabolic microbiome-host interaction may therefore pioneer actionable microbiota-based diagnostics or therapeutics that allow the control of host systemic metabolism via the microbiome.
Keywords: Microbiome, Metabolism, Metabolites, Nutrients
Background
In recent years, the rates of obesity have reached pandemic proportions. More than half of the US population is overweight or obese [1], and the prevalence worldwide is following a similar trend [2]. Obesity is strongly associated with several comorbidities indicative of systemic metabolic dysregulation, including fatty liver disease, type 2 diabetes (T2D), and cardiovascular disease. This pandemic of obesity and metabolic dysregulation is increasing mortality, morbidity, and health care costs of individuals and societies across the globe. An improved understanding of the factors that regulate metabolic homeostasis in health and disease is urgently required [3].
Emerging evidence suggests that the intestinal microbiome is an important factor regulating systemic metabolic homeostasis [4–6]. The intestinal microbiome refers to the collective genetic material of the microbes populating the intestine, which allows for a substantial diversification of the metabolic activities available to the colonized host. Thus, the genetic and biochemical composition of the microbiome will determine the metabolic activities occurring in the intestine, which can then impact the development and function of the metabolic, immune, and nervous systems [7, 8]. These interactions provide a potential mechanistic basis whereby the microbiome can regulate systemic metabolic homeostasis.
Early evidence suggesting the intestinal microbiome plays a role in systemic metabolism came from observational reports. For instance, long-term exposure to antibiotics, performed in humans more than 60 years ago, and routinely performed in livestock to this day, has consistently led to an increase in body fat mass [9, 10]. However, it was not until the 2000s that important studies in mice robustly described an altered microbiota upon obesity [11]. It was found that feeding the exact same diet to genetically obese ob/ob mice and their lean siblings resulted in large differences in their microbiome composition [11]. The ob/ob mice had a 50% reduction in Bacteroidetes and a corresponding increase in Firmicutes. Further, this altered gut microbiota has been reproduced independently in both obese mice and humans. Additional studies showed that the microbiome generally has an enhanced property of energy harvesting in obesity [4, 6, 12].
Building on these observations, several groups have since aimed to study the causal role of the microbiome in systemic metabolism. One early report suggesting causality found that germ-free mice, which are mice entirely lacking a microbiome from birth, have reduced body fat compared to mice with a conventional microbiome [4]. Moreover, upon colonization of adult germ-free mice with the microbiome of conventionally raised mice, there was a 60% increase in body fat, despite reduced food intake [4, 5]. Further transplantation experiments have since been performed using the microbiota from mouse or human donors into germ-free mice, with the result that the microbiota transplant from obese donors resulted in increased obesity compared with transplants from lean donors [12, 13]. Taken together, these results suggest that the microbiome has properties that modulate the energy balance of the host, which has important implications in human dietary regulation and metabolic disease.
Thus, there is growing attention for the intestinal microbiome as a mediator of environmental factors that influences systemic metabolic homeostasis and may contribute to the global trends of obesity and metabolic dysregulation pervasive in our post-industrialized civilization. As the microbiome field progresses, it will be critical to achieve a more detailed mechanistic understanding whereby the microbiome regulates organismal metabolism.
Systemic metabolism and the microbiome
Systemic metabolism is a complex structure of individual metabolic processes across cells, tissues, and organ systems that intersect to orchestrate organism-wide metabolite flux. The future of understanding host-microbiome metabolic interactions lies in obtaining a finely resolved picture regarding which of these processes are influenced by the microbiome. Although this remains a relatively young field of research, significant progress has been made over the last 15 years since the initial observations of metabolic regulation by the microbiome. Here, we review several recent examples whereby the microbiome can mechanistically influence systemic metabolism. To structure this discussion, we will consider energy balance and metabolite balance in turn.
Energy balance
Organisms require energy to perform the functions of life. Energy balance refers to the equilibrium between the amount of energy absorbed from food and the amount expended through the metabolic activities of the organism, the thermic effect of food, and the energy excreted in the feces or urine. The healthy human organism has a remarkable ability to adjust food intake to the need generated by the current state of energy expenditure within a very narrow window—a process which is disturbed in obesity. The role of the microbiome in these processes is still a developing field, but several recent animal studies have provided first insights into the role for the microbiome in energy balance (Fig. 1).
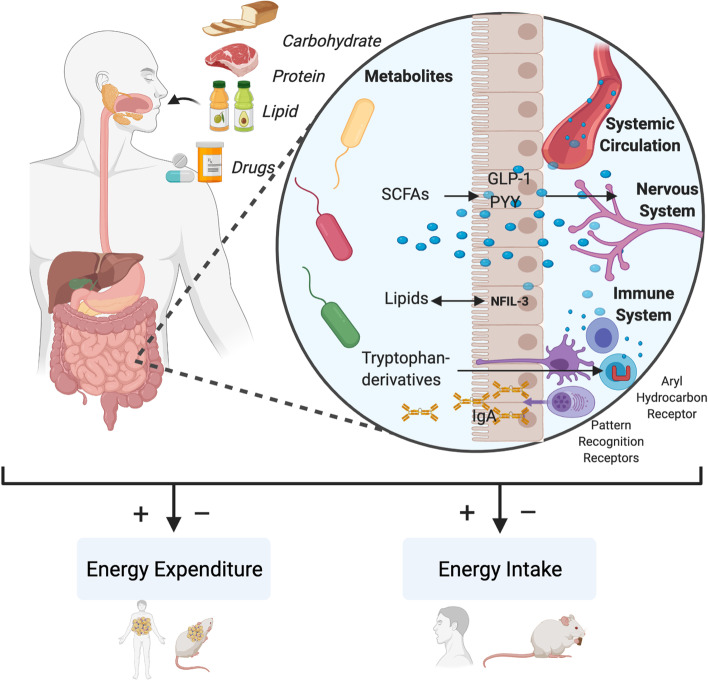
Fig. 1.
Mechanisms of metabolic host-microbiome crosstalk. Host-microbiome interaction contributes to the organismic balance between energy intake and energy expenditure. For instance, the metabolic activities of the microbiome can produce diverse metabolites such as derivatives of tryptophan metabolism, short chain fatty acids (SCFAs), and other lipid metabolites that can interact with the immune or nervous systems of the colonized host to regulate energy intake and expenditure. SCFAs induce GLP-1 and PYY release from enteroendocrine cells. Epithelial Nfil3 regulates a lipid absorption program in a microbiome-regulated manner. Tryptophan metabolites influence immune cell activities
Energy intake
The microbiome can modulate energy intake directly via modulation of the digestion of complex macronutrients or indirectly via influences on hunger and satiety. Early studies in the field that connected the microbiome to energy homeostasis demonstrated that the microbiome modulates how much of the ingested energy is excreted [13, 14]. These investigations of the impact of the microbiome on obesity suggested that the microbiome of obese and lean hosts are different in composition and metabolic activity, thereby playing a role in the ability of the host to extract energy from food [13]. The mechanisms by which microbiomes differ in their overall ability to extract caloric content from food remain largely unknown, but a recent study indicated an involvement of the metabolite dimethylglycine in enhanced energy extraction and resultant weight gain [15].
In addition to the direct modulation of caloric extraction from food, the microbiome can modulate hunger and satiety signaling through interactions with the neuro-endocrine axis [16]. For example, microbiome-derived circulating short-chain fatty acids (SCFAs), products of carbohydrate fermentation by commensal bacteria, can trigger endogenous secretion of hunger-regulating peptides such as glucagon-like peptide 1 (GLP-1) and peptide YY (PYY) (Fig. 1). In particular, enteroendocrine cells of the gastrointestinal tract both express the SCFA receptors GPR (G-protein coupled receptor)-41 and GPR-43 [17–19] and secrete satiety-inducing PYY and GLP-1 once activated [20, 21]. The appetite-suppressive effects of SCFAs constitute a form of a negative feedback mechanism in response to food consumption, highlighting the role of the microbiome as a key mediator in regulating physiological adaptation to environmental factors in order to promote energy balance. Apart from SCFAs, other mechanisms might exist by which the microbiome regulates hunger and satiety. For instance, Escherichia coli can produce a mimic of a melanocyte-stimulating hormone (α-MSH), ClpB, stimulating PYY release and inducing proopiomelanocortin (POMC) neuron activity [22].
The relationship between the microbiome and energy intake represents an important component of metabolic homeostasis, and the microbiome has been implicated in the regulation of energy absorption and food intake, as detailed above. However, energy balance is not only a matter of energy intake, but also energy expenditure. Next, we consider the role of the microbiome from this side of the energy equation.
Energy expenditure
Expenditure of energy can occur by growth (anabolic) or combustion (catabolic). The role of the microbiome in growth is still a developing field and has been reviewed elsewhere [23]. Here we focus on the role of the microbiome in regulating catabolic processes that influence energy expenditure. In particular, we will focus on the process of non-shivering thermogenesis which has garnered significant interest due to its association with improved cardiometabolic health in humans [24–28].
Non-shivering thermogenesis refers to a specialized form of heat production that is facilitated by brown and beige adipocytes to maintain body temperature during cold exposure [29]. Beige adipocytes, also referred to as “brite” adipocytes, combined features of white and brown adipocytes and are induced by prolonged cold exposure in classical white adipose depots, although more efficiently in subcutaneous than visceral depots. Non-shivering thermogenesis in both brown and beige adipocytes is dependent on the protein uncoupling protein 1 (UCP-1), which dissipates the proton gradient across the inner mitochondrial membrane thereby uncoupling respiration from ATP synthesis [30]. Given the emerging interest for the role of the gut microbiome in systemic metabolism and energy expenditure, several groups have therefore studied the potential modulation of non-shivering thermogenesis by the microbiome. An early study on this topic found that germ-free mice as well as mice treated with antibiotics have improved insulin sensitivity and increased expression of Ucp1 in subcutaneous and visceral white adipose tissue [31]. On the other hand, a study published more recently found the opposite, namely that gut microbiota depletion impairs thermoregulation, reduces energy metabolism, and that recolonization of depleted microbiota partially rescues this impaired thermogenesis effect in part through the SCFA butyrate [32]. Yet another report found no effect of microbiome depletion on recruitment of thermogenic tissues or energy expenditure but did find a role for the microbiome in contributing amino acid metabolites to optimize hepatic TCA cycle fluxes in support of gluconeogenesis [33]. Thus, there is debate in the field regarding the role for the microbiome in regulating energy expenditure through non-shivering thermogenesis. Importantly, understanding the nuances of this relationship between the microbiome and non-shivering thermogenesis might provide alternative paths toward metabolic regulation for individuals in a hypercaloric or hypometabolic state [34, 35]. Whether the microbiome plays a role in regulating non-shivering thermogenesis in humans remains unchartered.
Metabolite balance
Similar to the previously discussed mechanisms of whole-organism energy homeostasis, metabolite influx and efflux must be balanced in order to maintain health. Metabolites can function as both fuel and signals, and the same is true for microbially-derived metabolites. In the following section, we review specific metabolites and mechanisms that are regulated by the metabolic activities of the microbiome, playing a role in the metabolism of all three macronutrients: carbohydrates, proteins, and fats.
Carbohydrate metabolism
One of the most striking metabolic phenotypes of germ-free mice is their profoundly blunted serum glucose response to carbohydrate intake [36]. While the exact mechanisms underlying this phenomenon are not completely understood, several recent studies have contributed to our understanding. For instance, imidazole propionate was identified as a microbial metabolite produced from histidine by bacteria whose abundance is associated with T2D; imidazole propionate inhibits insulin signaling through the mTOR and AMPK pathways [37, 38], thus offering a potential explanation for the microbiome impact on systemic glucose homeostasis and providing a target for intervention.
In addition, the microbiome has been found to regulate adipose tissue biology and glucose homeostasis through the regulation of the non-coding RNA mir-181. By regulating the systemic levels of indole metabolites, which in turn suppress mir-181 expression in adipose tissue, the microbiome is involved in the transcriptional control of genes involved in insulin signaling and glucose metabolism [39].
Another area of focus is the interaction between the microbiome and enteroendocrine cells, the major glucoregulatory epithelial cells of the intestine. GLP-1 is strongly elevated in germ-free and antibiotics-treated mice, indicating an enhanced incretin effect in response to carbohydrate intake in the absence of the microbiome [40]. On the other hand, microbiome-derived metabolites, such as SCFAs and indoles, have been shown to induce GLP-1 release from enteroendocrine cells [20]. These studies complement the evidence previously described in the section on energy intake, where the microbiome can regulate hormone secretion to exert systemic influences on the host.
Recently, the microbiome has been implicated in the neuronal control of glucose homeostasis. For example, microbially-produced acetate has been found to activate the parasympathetic nervous system, thereby promoting glucose-stimulated insulin release from the pancreas in rats [41]. Propionate induces sympathetic activation, glucagon release, and insulin resistance in mice; this effect was also seen in a double-blind, placebo-controlled human study, and plasma propionate decreased with weight loss [42]. These two studies demonstrate how the microbiome can influence both nervous and endocrine elements together to tune blood sugar levels with opposing mechanism. Additionally, a microbiome-induced CART-expressing subset of neurons in the enteric nervous system can regulate blood glucose and connect polysynaptically to the liver and pancreas [43], representing interconnected neuro-endocrine control of systemic metabolism with input from the microbiome. Taken together, these studies support the notion that the microbiome has evolved mechanisms to control blood glucose via diverse autonomic and somatic neuroendocrine mechanisms. Therapeutically, each of these avenues represents a potential point of intervention that could be exogenously modulated.
Amino acids
Essential amino acids must be provided by the diet, and the microbiome has a major impact on the metabolism of dietary amino acids, with important effects on host physiology. For instance, the microbiome metabolizes dietary tryptophan and its metabolites, such indoles and tryptamine, which can then be sensed by the aryl hydrocarbon receptor (AHR) [44–46]. This receptor and transcriptional regulator can subsequently influence downstream physiological transcriptional programs [47]. Interestingly, some SCFAs also interact with AHR [48], suggesting a potential mechanism of cross-talk between microbiome processing of different macronutrients. Indole can also reduce intestinal permeability and stimulate the release of GLP-1 [49, 50], relating back to other GLP-1 control mechanisms discussed in the previous section.
Tryptamine and kynurenine, two potentially microbially-produced tryptophan metabolites, also modulate metabolic functions. Tryptamine can induce the release of serotonin to stimulate gastrointestinal motility [51, 52], while kynurenine has been shown to have various inflammatory, metabolic, and neurological effects [53]. Phenylalanine and tyrosine, the two other aromatic amino acids, can also be metabolized to biologically active products that modulate intestinal permeability and systemic immunity [54, 55]. Beyond the role of amino acids in metabolism and immunity, there have been reports of amino acids regulating feeding behavior in a microbiome-dependent manner. For example, in flies, the lack of any one essential amino acid from the diet produces a strong and specific appetite for proteinaceous or amino acid–rich food [56]. Remarkably, however, it was found that flies with a specific microbiome composition do not develop this protein appetite, since Acetobacter pomorum and Lactobacilli were found to be able to suppress this protein appetite. This raises the question whether in addition to local gastrointestinal metabolism, the microbiome contributes to the stability of organismal metabolites levels via a feedback loop that regulates food choice. Taken together, these studies suggest that amino acid metabolism by the microbiome has far-reaching effects, altering metabolic homeostasis, inflammation, and neurological functions.
Lipids
Together with carbohydrates and protein, lipids are the third major macronutrient, and their metabolism is also partially under control of the microbiome [57, 58]. As briefly described above, germ-free mice are largely resistant to high fat diet-induced obesity, excrete more lipids in feces, and have altered cholesterol metabolism [36]. The microbiome helps respond to dietary lipid changes by modulating intestinal epithelial digestive and absorptive processes in mice and zebrafish [59, 60]. Similarly, antibiotics reduce lipid absorption in rats [61]. More recent studies have focused on specific cellular actors, showing that metabolites from different bacterial species can regulate enterocyte lipid metabolism [62]. Lactate produced by L. paracasei promotes lipid storage in enterocytes by generating malonyl-CoA, and that acetate produced by E. coli promotes lipid oxidation in enterocytes by upregulating the AMPK/PGC-1α/PPARα pathway. Another study found that a previously uncultured bacterium in humans is able to convert cholesterol to a poorly absorbed sterol and is correlated with lower cholesterol levels [63]. These studies highlight the potential for developing specific bacteria- and metabolite-based therapeutic interventions to improve outcomes in for example obesity and atherosclerosis. Furthermore, dietary fat consisting of saturated fats, but not fats like fish oil, increases inflammation in WAT in a microbiome-dependent manner [64], demonstrating a link between diet, the microbiome, and systemic processes. In terms of fat metabolism, bile acids, necessary for the absorption of dietary fat, are modified by the microbiome, which transform them from primary to secondary bile acids. Bile acids themselves act as signaling molecules to control their own production and other metabolic functions [65, 66]. Widely conserved microbial bile salt hydrolases (BSH) add additional complexity to the bile acid pool [67]. BSH expression decreases weight gain, cholesterol, and triglycerides while inhibition increases weight gain [68, 69]. The interaction between bile and the microbiome represents a distinct mechanism of lipid regulation by the microbiome to impact energy intake in terms of a specific macronutrient.
A number of recent studies have added interesting facets to this general model of lipid metabolism, whereby the intestinal microbiome can interface with the immune system to influence lipid absorption in the gut. In the absence of regulation by CD4+ T cells, microbiome-controlled type 3 innate lymphoid cells (ILC3s) shape lipid metabolism by the secretion of IL-22, which modulates the expression of epithelial lipid transporters [70]. The same IL-22-dependent pathway of intestinal ILC3s responding to the microbiota involves the circadian clock protein nuclear factor, interleukin-3-regulated (NFIL3), which in turn regulates lipid absorption in intestinal epithelial cells [71, 72]. IL-22 production in intestinal ILC3s is also partly dependent on free fatty acid receptor 2 (FFAR2), which is agonized by microbially-produced SCFAs [73]. These studies together suggest that there exists substantial crosstalk between the host and the microbiome partially mediated by cells of the immune system, particularly on lipid metabolism.
Ultimately, the involvement of the microbiome in macronutrient absorption demonstrates a triad between nutrition, the microbiome, and systemic health. Understanding the role of microbiota-derived metabolites in human health may provide a more precise modulation of human metabolism via microbiome-directed therapies.
Pharmacological microbiome metabolism
In addition to the previously discussed body of evidence regarding the role of the microbiome in systemic metabolism, we will finally highlight another aspect by which the microbiome strongly impacts host physiology: the metabolism of drugs.
Most drugs are taken orally, and thus will be exposed to the microbiome prior to reaching the blood stream to mediate a therapeutic effect. The microbiome can play a major role in drug metabolism, availability, efficacy, and safety. The microbiome has been shown to alter drugs in myriad mechanisms, including demethylation, deamination, dehydroxylation, deacylation, decarboxylation, oxidation, hydrolysis, deconjugation, and acetylation [74, 75]. The microbiome can also influence drug metabolism indirectly, by impacting the levels of drug-metabolizing enzymes, such as glutathione transferases in the liver and colon [76], or microbial metabolites themselves can compete for the same human enzyme that a drug may be targeting [77]. Since the microbiome has a significant impact on metabolic disease and systemic metabolic homeostasis, this has spurred important studies to elucidate the interaction between the microbiome and the drugs used to treat metabolic disease [78, 79].
Statins
One group of drugs with major applications in metabolic disease are those that target lipid metabolism in the treatment of elevated triglycerides or cholesterol. Statins (also known as HMG-CoA reductase inhibitors) are a class of cholesterol-lowering agents that reduce mortality in patients at high risk of cardiovascular disease and are the most prescribed drug in the world. Statin therapy is associated with myopathy and T2D in humans, and an initial study in mice found that statin therapy reduced microbiome butyrate production, altered bile acids, and impaired fasting glucose [80]. However, in a large human study, statin therapy negatively correlated with inflammation-associated microbiota Bacteroides2 (Bact2) enterotype [81]; Bact2 dysbiosis is characterized by an increased Bacteroides:Faecalbacterium ratio, is associated with inflammatory bowel disease and obesity, and was reduced in obese patients on statin therapy [81]. More work is required to elucidate the interactions and mechanisms by which statin therapy modulates the microbiome.
Metformin
In T2D, various classes of drugs interact with the microbiome [82]. Metformin is the first-line medication for the treatment of T2D with pleiotropic mechanisms of action. Indeed, more recently it has been suggested that metformin may in part exert a therapeutic benefit by impacting the metabolic activity of the microbiome in patients with type II diabetes [83, 84]. In these studies, it was found that metformin treatment alters the gut microbiome of individuals with treatment-naïve T2D, and the therapeutically beneficial effects of metformin on glucose tolerance could be transferred via fecal transplant from the metformin-treated patients. In mice, metformin was found to decrease B. fragilis and increase the bile acid glycoursodeoxycholic acid (GUDCA), and it was suggested that the benefits of metformin were in part mediated by the inhibition of intestinal farnesoid X receptor (FXR) by GUDCA, which was counteracted by B. fragilis, and transferable upon fecal transplant from metformin-treated patients [83]. Metformin use also is associated with increased abundance of Akkermansia muciniphila, which contributes to better glycemic control [85, 86].
Other drugs
Given the microbiome’s prime location to interact with orally administered drugs and vast array of metabolic and enzymatic activity, it is notable that interactions have been shown with many medications [79]. In humans, the microbial metabolite p-cresol competes with acetaminophen for sulfonation, a common reaction that many other drugs undergo [77]. High-throughput methodologies show significant promise in uncovering specific interactions between the microbiome and host. Only a small number of microbiome-drug interactions have been elucidated in detail, and recent studies have shown that the range of interactions between the microbiome and xenobiotic compounds may be much larger than previously anticipated [78, 87]. A screen of 1000 marketed non-antibiotic drugs found that 24% of the drugs inhibited the growth of at least one bacterial species of the 40 tested in vitro at physiologically relevant concentrations; all classes of drugs were represented, and antipsychotics were particularly prominent [79]. One path forward is personalized screening for microbiome drug metabolism. Using human fecal cultures combined with HPLC-MS to detect drug metabolism and metabolites, many previous microbially metabolized drugs were confirmed and several new ones identified, including spironolactone, tolcapone, misoprostol, mycophenolate mofetil, capecitabine, hydrocortisone, and vorinostat [88]. In addition to modifying drugs, the microbiome can also modulate the effect of medications by bioaccumulation and sequestration; for example, the antidepressant duloxetine accumulates in several species while also altering metabolite secretion, which in turn affects community composition [89]. The identification and quantification of microbially metabolized drugs offers increased precision and safety moving forward that should be taken into consideration when designing and optimizing therapeutic interventions [90].
These studies offer reason to believe that it is important to evaluate drug exposure in terms of microbiome interactions when developing novel orally active pharmaceuticals in the future. High throughput methodologies represent a paradigm that could be used to scrutinize bioavailability in the context of diverse microbial compositions [91]. These studies could explain some of the less well understood mechanisms of substantially differing responses to commonly administered agents. Perhaps, probiotics could be administered in conjunction with different oral drugs to optimize clinical efficacy.
Clinical applications, therapeutics, and diagnostics
An important aspect of the identification of microbiome-derived pathways controlling systemic metabolism is that these pathways might be amenable to therapeutic intervention. Microbiome-based therapies are attractive due to their non-invasiveness, low potential for toxicity, and ease of administration. There are a number of promising leads moving forward, whereby discoveries related to the microbiome can be leveraged to hopefully improve human metabolic health in the future.
Currently, the only clinically approved microbiome-based intervention is microbiota transplantation (FMT) in the context of C. difficile infection. Community replacement by FMT or antibiotic treatment as therapeutic strategies for obesity and metabolic disease has not proven effective across different studies [92, 93], indicating that more refined approaches are required to modulate systemic metabolism via the gut [94].
Several such refined approaches are actively being investigated, most of them based on live bacteria (probiotics) or their metabolites (postbiotics). A prototypical example for a microbial species-based intervention is the discovery that Akkermansia is negatively correlated with obesity [95], which has spurred an effort to test the potential therapeutic benefit of A. muciniphila administration. A recent double-blind randomized controlled trial with 32 overweight and insulin-resistant human volunteers provided preliminary evidence to suggest that pasteurized A. muciniphila administration may improve insulinemia and plasma cholesterol in overweight humans [96]. A. muciniphila can also secrete a protein that induces thermogenesis and GLP-1 secretion in mice fed a high-fat-diet to improve weight and metabolic measures [97]. Similar to preclinical mouse studies, there have also been attempts to transfer a “lean” microbiome into obese individuals; these interventions did not significantly reduce body weight but did improve insulin sensitivity and several other secondary markers [98, 99]. Building off of preclinical observations of microbiota energy harvesting, a recent randomized cross-over dietary intervention and randomized, double-blind, placebo-controlled study found more stool calorie loss in underfeeding vs. overfeeding and with vancomycin treatment vs. placebo [100]. Finally, the effects of bariatric surgery, the most effective treatment for weight loss, were recently found to be partially mediated by the microbial production of a secondary bile acid [101, 102].
These instances of positive evidence notwithstanding, there are a number of challenges that must be overcome related to prebiotic and probiotic interventions, including unresolved mechanisms, conflicting clinical results, and the use of surrogate or subjective study endpoints in clinical trials to date [103]. Regarding mechanism, several explanations have been put forward, including increased SCFAs, hormone signaling, mucus thickness, and barrier integrity along with decreased inflammation, but readouts across different studies have not been consistent. Furthermore, while treatment with single probiotic species is preferable to establish causality [104], some studies using the same mixtures have found conflicting results. For example, the probiotic mixture VSL#3, which contains Streptococcus thermophilus, Lactobacillus, and Bifidobacterium species, has shown metabolic benefits in overweight adults [105] and improved BMI in obese children with non-alcoholic fatty liver disease (NAFLD) [106], while also paradoxically increasing adiposity and weight in obese adolescents [107]. Finally, subjective secondary measures, such as waist circumference, should be avoided. In addition, while some preclinical studies and early-stage clinical trials have been promising, most large-scale human trials of probiotics in weight loss have seen no or marginal benefits [108]. While it is difficult to directly compare probiotic studies due to different probiotics, doses, and duration, several meta-analyses have seen no weight benefits in adults [109, 110] or children [111]. Other meta-analyses have seen statistically significant benefits for overweight adults, but none of the effect sizes observed were larger than 1 kg of weight loss [112–114].
Given the relatively strong preclinical evidence, there are several reasons why probiotic therapies may have had difficulty translating to humans. Mice used in preclinical models are typically young, live in highly controlled environments, equilibrate microbiomes within cages [115], and eat homogenous diets. In contrast, the human microbiome varies dramatically by geography, age, sex, and diet [116, 117]. Variation in the human microbiome determines effective colonization by probiotic species, as some people are highly resistant to engraftment [118].
Given heterogeneous responses to probiotic and other microbiome-targeted therapies, recent studies have suggested that there may be potential in harnessing the microbiome as a diagnostic tool to develop precision medicine treatments for metabolic disorders and obesity. For example, post-prandial glycemic response to diets can by predicted by microbiome composition, opening the possibility of personalized nutrition programs to optimize host metabolism based on microbiota composition [119]. Importantly, recent clinical trials using such personalized interventions demonstrated improved glycemic control and reduced HbA1c in both prediabetic and newly diagnosed T2D when compared to a Mediterranean diet intervention [120, 121]. Understanding how microbial species, gene pathways, and dietary components interact is of upmost importance to harness the power of microbiome data. Two studies that screened the human microbiome for the ability to break down various fiber species identified upregulated gene pathways and species able to outcompete with given nutrients [122, 123]. Individual responses to highly controlled diets containing these fibers in human subjects led to differential changes in the plasma proteome [122]. Similarly, another human trial saw an increase in microbial glycan-degrading genes after a high-fiber diet, while a diet rich in fermented foods increased alpha diversity and decreased markers of inflammation [124]. Two recent studies utilized data from the PREDICT 1 trial with over a thousand patients from the UK, including twin pairs, and a validation cohort in the USA [125, 126]. They found that microbiome composition was a good predictor of postprandial lipid, and to a lesser extent, glycemic response as well as fasting cardiovascular metabolic markers. Varied, plant-based, unprocessed diets were associated with healthier microbiome species, some of the strongest of which were only identified through metagenomic assemblies, emphasizing the need for further characterization. Taken together, these studies suggest that harnessing both taxonomic and metagenomic data to predict individual responses to microbiome-targeting interventions may elucidate and address why intervention responses are so heterogenous and sometimes irreproducible.
In addition to the direct impacts of microbiome composition on host health, we have reviewed numerous examples whereby microbial metabolites influence human health in diverse ways. Modulating these metabolites represents a second therapeutic path to translate microbiome findings. An example for metabolite-based interventions is provided by trimethylamine-N-oxide (TMAO). TMAO is formed from trimethylamine (TMA) produced from microbial metabolism of choline and other TMA-containing molecules. Increased TMAO levels are linked to heart disease, atherosclerosis, T2D, thrombosis, Alzheimer’s disease, and stroke [127–135]. Preclinical targeting of bacterial TMA production was therapeutic in mouse models of atherosclerosis and platelet aggregation [136, 137]. TMAO has been used as a biomarker in several clinical trials [138, 139], and treatments targeting TMAO are now being investigated in chronic kidney disease [140] and cardiovascular disease [141]. TMAO is one of the best-described microbial metabolites, but there are many more that hold therapeutic potential moving forward [142].
Outside of therapeutics, a deeper detailing of the microbiome in patients with various diseases outside of metabolic syndrome could offer valuable information about diagnosis and potential response to standard of care treatments. For instance, the staging and diagnosis of non-alcoholic fatty liver disease has represented a significant challenge in modern medicine. There has been a growing body of evidence which suggests that microbial analysis may lead to minimally invasive approaches to address this challenge. There have been impressive results that have linked dysbiosis to the clinical phenotype of patients with NAFLD-related fibrosis. More specifically, fibrosis has been linked to a decrease in overall microbial diversity and an increase in gram-negative bacteria, which has been postulated to be a source of inflammatory endotoxin [143].
Conclusions and outlook
The identification of the microbiome impact on systemic metabolism marks the birth of the modern era of microbiome research. In the past 15 years since the discovery that germ-free mice show an abnormal metabolism—including lower blood glucose levels, reduced body fat content, and slower weight gain on high-fat diet compared to conventionally colonized counterparts [4]—the underlying mechanisms have been extensively explored [144]. Possible explanations include the regulation of epithelial lipid uptake by the microbiome [60, 145], the regulation of transcription in metabolic tissues via HDAC3 and mir-181 [39, 146], the regulation of hepatic gluconeogenesis [33], regulation of circadian host biology [147–154], the impact on glucoregulatory viscerofugal enteric neurons [43], and the regulation of insulin signaling [37]. It is likely that all of these mechanisms act in concert and that several other elements of the metabolic microbiota-host crosstalk remain to be discovered.
Systemic metabolism can be understood as the diverse processes that influence physiological energy accounting. The microbiome plays a crucial role as a moderator of these activities. In terms of energy balance, the microbiome not only influences energy harvesting, but also influences neuroendocrine functions, which control hunger and satiety. Of note, the microbiome influence on thermogenesis and energy expenditure has yet to be fully elucidated but represents an important direction for future research. The microbiome has also evolved to interact with each of the three major macronutrient classes in various ways, emphasizing that host metabolite flux cannot be fully interpreted without metagenomic considerations.
Both the promise and the challenge of the field lie in the ability to translate these findings into meaningful clinical interventions, which may take the form of microbiome transplants, pre-, pro-, or post-biotics, metabolite targeting, diagnostics, or precision medicine [155]. In addition to the vast inter-individual and inter-geographical differences in microbiome composition and function in the human population, the lack of a precise understanding of microbiome temporal dynamics and metabolite fluxes between the gastrointestinal lumen and the host systemic circulation presents a formidable challenge. Currently, precision engineering approaches targeting the microbiome largely assume a stable model of host-microbiome interactions, whereby exogenous interventions aimed at modifying microbial community composition will have a durable effect on host metabolites. This is likely not the case. On the basic research side, a detailed understanding of metabolite fluxes between the microbial cells inhabiting the gastrointestinal tract and the eukaryotic cells that compose metabolic tissues would be an important step forward. This can be achieved by the systematic application of metabolite tracing using quantitative flux analysis of labeled molecules. On the clinical side, large-scale multi-center studies, ideally spanning several geographical areas, will be needed to assess the robustness of microbiome-based interventions for metabolic health across different environments, ethnicities, and dietary habits. If the progress of the last 15 years since the initial metabolic characterization of germ-free mice is any indication, the field of metabolic host-microbiome interactions is poised for a decade and a half of deep insights ahead.
Acknowledgements
We thank the members of the Thaiss lab for valuable input.
Authors’ contributions
TOC, PL, KN, and CAT performed research and wrote the manuscript. All authors read and approved the final manuscript.
Funding
C.A.T. is a Pew Biomedical Scholar and Kathryn W. Davis scholar supported by the NIH Director’s New Innovator Award (DP2AG067492), the Edward Mallinckrodt, Jr. Foundation, an Agilent Early Career Professor Award, the Thyssen Foundation, the Human Frontier Science Program, the MMPC Mouse Microbiome Metabolic Research Program, the Penn Diabetes Research Center (P30-DK-019525), and the Penn Institute on Aging. T.O.C. is supported by an NIH/NIA training grant (T32AG000255-23). P.L. is supported by an NIH/NIAID training grant (T32AI141393). K.N. received a Pincus-Magaziner Family Undergraduate Research Award.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Timothy O. Cox, Patrick Lundgren, and Kirti Nath share equal contributions.
References
- 1.Stevens J, Oakkar EE, Cui Z, Cai J, Truesdale KP. US adults recommended for weight reduction by 1998 and 2013 obesity guidelines, NHANES 2007-2012. Obesity (Silver Spring) 2015;23:527–531. doi: 10.1002/oby.20985. [DOI] [PubMed] [Google Scholar]
- 2.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27. [DOI] [PMC free article] [PubMed]
- 4.Backhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, Semenkovich CF, Gordon JI. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci U S A. 2004;101:15718–15723. doi: 10.1073/pnas.0407076101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Backhed F, Manchester JK, Semenkovich CF, Gordon JI. Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc Natl Acad Sci U S A. 2007;104:979–984. doi: 10.1073/pnas.0605374104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan MT, Nieuwdorp M, Backhed F. Microbial modulation of insulin sensitivity. Cell Metab. 2014;20:753–760. doi: 10.1016/j.cmet.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 7.Cho I, Blaser MJ. The human microbiome: at the interface of health and disease. Nat Rev Genet. 2012;13:260–270. doi: 10.1038/nrg3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lundgren P, Thaiss CA. The microbiome-adipose tissue axis in systemic metabolism. Am J Physiol Gastrointest Liver Physiol. 2020;318:G717–G724. doi: 10.1152/ajpgi.00304.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thaiss CA, Elinav E. The remedy within: will the microbiome fulfill its therapeutic promise? J Mol Med (Berl) 2017;95:1021–1027. doi: 10.1007/s00109-017-1563-z. [DOI] [PubMed] [Google Scholar]
- 10.Haight TH, Pierce WE. Effect of prolonged antibiotic administration of the weight of healthy young males. J Nutr. 1955;56:151–161. doi: 10.1093/jn/56.1.151. [DOI] [PubMed] [Google Scholar]
- 11.Ley RE, Backhed F, Turnbaugh P, Lozupone CA, Knight RD, Gordon JI. Obesity alters gut microbial ecology. Proc Natl Acad Sci U S A. 2005;102:11070–11075. doi: 10.1073/pnas.0504978102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ridaura VK, Faith JJ, Rey FE, Cheng J, Duncan AE, Kau AL, Griffin NW, Lombard V, Henrissat B, Bain JR, et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science. 2013;341:1241214. doi: 10.1126/science.1241214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 14.Lund J, Gerhart-Hines Z, Clemmensen C. Role of energy excretion in human body weight regulation. Trends Endocrinol Metab. 2020;31:705–708. doi: 10.1016/j.tem.2020.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Fluhr L, Mor U, Kolodziejczyk AA, Dori-Bachash M, Leshem A, Itav S, et al. Gut microbiota modulates weight gain in mice after discontinued smoke exposure. Nature. 2021;600:713–19. [DOI] [PubMed]
- 16.Fetissov SO. Role of the gut microbiota in host appetite control: bacterial growth to animal feeding behaviour. Nat Rev Endocrinol. 2017;13:11–25. doi: 10.1038/nrendo.2016.150. [DOI] [PubMed] [Google Scholar]
- 17.Karaki S, Tazoe H, Hayashi H, Kashiwabara H, Tooyama K, Suzuki Y, Kuwahara A. Expression of the short-chain fatty acid receptor, GPR43, in the human colon. J Mol Histol. 2008;39:135–142. doi: 10.1007/s10735-007-9145-y. [DOI] [PubMed] [Google Scholar]
- 18.Karaki S, Mitsui R, Hayashi H, Kato I, Sugiya H, Iwanaga T, Furness JB, Kuwahara A. Short-chain fatty acid receptor, GPR43, is expressed by enteroendocrine cells and mucosal mast cells in rat intestine. Cell Tissue Res. 2006;324:353–360. doi: 10.1007/s00441-005-0140-x. [DOI] [PubMed] [Google Scholar]
- 19.Tazoe H, Otomo Y, Karaki S, Kato I, Fukami Y, Terasaki M, Kuwahara A. Expression of short-chain fatty acid receptor GPR41 in the human colon. Biomed Res. 2009;30:149–156. doi: 10.2220/biomedres.30.149. [DOI] [PubMed] [Google Scholar]
- 20.Tolhurst G, Heffron H, Lam YS, Parker HE, Habib AM, Diakogiannaki E, Cameron J, Grosse J, Reimann F, Gribble FM. Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein-coupled receptor FFAR2. Diabetes. 2012;61:364–371. doi: 10.2337/db11-1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Psichas A, Sleeth ML, Murphy KG, Brooks L, Bewick GA, Hanyaloglu AC, Ghatei MA, Bloom SR, Frost G. The short chain fatty acid propionate stimulates GLP-1 and PYY secretion via free fatty acid receptor 2 in rodents. Int J Obes. 2015;39:424–429. doi: 10.1038/ijo.2014.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Breton J, Tennoune N, Lucas N, Francois M, Legrand R, Jacquemot J, Goichon A, Guerin C, Peltier J, Pestel-Caron M, et al. Gut Commensal E. coli proteins activate host satiety pathways following nutrient-induced bacterial growth. Cell Metab. 2016;23:324–334. doi: 10.1016/j.cmet.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 23.Robertson RC, Manges AR, Finlay BB, Prendergast AJ. The human microbiome and child growth - first 1000 days and beyond. Trends Microbiol. 2019;27:131–147. doi: 10.1016/j.tim.2018.09.008. [DOI] [PubMed] [Google Scholar]
- 24.Becher T, Palanisamy S, Kramer DJ, Eljalby M, Marx SJ, Wibmer AG, Butler SD, Jiang CS, Vaughan R, Schöder H, et al. Brown adipose tissue is associated with cardiometabolic health. Nat Med. 2021;27:58–65. doi: 10.1038/s41591-020-1126-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cypess AM, Lehman S, Williams G, Tal I, Rodman D, Goldfine AB, Kuo FC, Palmer EL, Tseng Y-H, Doria A, et al. Identification and importance of brown adipose tissue in adult humans. N Engl J Med. 2009;360:1509–1517. doi: 10.1056/NEJMoa0810780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Orava J, Nuutila P, Lidell ME, Oikonen V, Noponen T, Viljanen T, Scheinin M, Taittonen M, Niemi T, Enerback S, Virtanen KA. Different metabolic responses of human brown adipose tissue to activation by cold and insulin. Cell Metab. 2011;14:272–279. doi: 10.1016/j.cmet.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 27.Van Marken Lichtenbelt WD, Vanhommerig JW, Smulders NM, Drossaerts JMAFL, Kemerink GJ, Bouvy ND, Schrauwen P, Teule GJJ. Cold-activated brown adipose tissue in healthy men. N Engl J Med. 2009;360:1500–1508. doi: 10.1056/NEJMoa0808718. [DOI] [PubMed] [Google Scholar]
- 28.Virtanen KA, Lidell ME, Orava J, Heglind M, Westergren R, Niemi T, Taittonen M, Laine J, Savisto N-J, Enerbäck S, Nuutila P. Functional brown adipose tissue in healthy adults. N Engl J Med. 2009;360:1518–1525. doi: 10.1056/NEJMoa0808949. [DOI] [PubMed] [Google Scholar]
- 29.Chouchani ET, Kazak L, Spiegelman BM. New Advances in Adaptive Thermogenesis: UCP1 and Beyond. Cell Metab. 2019;29:27–37. doi: 10.1016/j.cmet.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 30.Cannon B, Nedergaard J. Brown adipose tissue: function and physiological significance. Physiol Rev. 2004;84:277–359. doi: 10.1152/physrev.00015.2003. [DOI] [PubMed] [Google Scholar]
- 31.Suarez-Zamorano N, Fabbiano S, Chevalier C, Stojanovic O, Colin DJ, Stevanovic A, Veyrat-Durebex C, Tarallo V, Rigo D, Germain S, et al. Microbiota depletion promotes browning of white adipose tissue and reduces obesity. Nat Med. 2015;21:1497–1501. doi: 10.1038/nm.3994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li B, Li L, Li M, Lam SM, Wang G, Wu Y, Zhang H, Niu C, Zhang X, Liu X, et al. Microbiota depletion impairs thermogenesis of brown adipose tissue and browning of white adipose tissue. Cell Rep. 2019;26(2720-2737):e2725. doi: 10.1016/j.celrep.2019.02.015. [DOI] [PubMed] [Google Scholar]
- 33.Krisko TI, Nicholls HT, Bare CJ, Holman CD, Putzel GG, Jansen RS, Sun N, Rhee KY, Banks AS, Cohen DE. Dissociation of adaptive thermogenesis from glucose homeostasis in microbiome-deficient mice. Cell Metab. 2020;31(592-604):e599. doi: 10.1016/j.cmet.2020.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thaiss CA, Itav S, Rothschild D, Meijer MT, Levy M, Moresi C, Dohnalova L, Braverman S, Rozin S, Malitsky S, et al. Persistent microbiome alterations modulate the rate of post-dieting weight regain. Nature. 2016;540:544–551. doi: 10.1038/nature20796. [DOI] [PubMed] [Google Scholar]
- 35.Thaiss CA, Shapiro H, Elinav E. Post-dieting weight gain: the role of persistent microbiome changes. Future Microbiol. 2017;12:555–559. doi: 10.2217/fmb-2017-0045. [DOI] [PubMed] [Google Scholar]
- 36.Rabot S, Membrez M, Bruneau A, Gerard P, Harach T, Moser M, Raymond F, Mansourian R, Chou CJ. Germ-free C57BL/6J mice are resistant to high-fat-diet-induced insulin resistance and have altered cholesterol metabolism. FASEB J. 2010;24:4948–4959. doi: 10.1096/fj.10-164921. [DOI] [PubMed] [Google Scholar]
- 37.Koh A, Molinaro A, Stahlman M, Khan MT, Schmidt C, Manneras-Holm L, Wu H, Carreras A, Jeong H, Olofsson LE, et al. Microbially produced imidazole propionate impairs insulin signaling through mTORC1. Cell. 2018;175(947-961):e917. doi: 10.1016/j.cell.2018.09.055. [DOI] [PubMed] [Google Scholar]
- 38.Koh A, Manneras-Holm L, Yunn NO, Nilsson PM, Ryu SH, Molinaro A, Perkins R, Smith JG, Backhed F. Microbial imidazole propionate affects responses to metformin through p38gamma-dependent inhibitory AMPK phosphorylation. Cell Metab. 2020;32(643-653):e644. doi: 10.1016/j.cmet.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Virtue AT, McCright SJ, Wright JM, Jimenez MT, Mowel WK, Kotzin JJ, et al. The gut microbiota regulates white adipose tissue inflammation and obesity via a family of microRNAs. Sci Transl Med. 2019;11:eaav1892. [DOI] [PMC free article] [PubMed]
- 40.Wichmann A, Allahyar A, Greiner TU, Plovier H, Lunden GO, Larsson T, Drucker DJ, Delzenne NM, Cani PD, Backhed F. Microbial modulation of energy availability in the colon regulates intestinal transit. Cell Host Microbe. 2013;14:582–590. doi: 10.1016/j.chom.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 41.Perry RJ, Peng L, Barry NA, Cline GW, Zhang D, Cardone RL, Petersen KF, Kibbey RG, Goodman AL, Shulman GI. Acetate mediates a microbiome-brain-beta-cell axis to promote metabolic syndrome. Nature. 2016;534:213–217. doi: 10.1038/nature18309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tirosh A, Calay ES, Tuncman G, Claiborn KC, Inouye KE, Eguchi K, et al. The short-chain fatty acid propionate increases glucagon and FABP4 production, impairing insulin action in mice and humans. Sci Transl Med. 2019;11:eaav0120. [DOI] [PubMed]
- 43.Muller PA, Matheis F, Schneeberger M, Kerner Z, Jove V, Mucida D. Microbiota-modulated CART(+) enteric neurons autonomously regulate blood glucose. Science. 2020;370:314–321. doi: 10.1126/science.abd6176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Roager HM, Licht TR. Microbial tryptophan catabolites in health and disease. Nat Commun. 2018;9:3294. doi: 10.1038/s41467-018-05470-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zelante T, Iannitti RG, Cunha C, De Luca A, Giovannini G, Pieraccini G, Zecchi R, D'Angelo C, Massi-Benedetti C, Fallarino F, et al. Tryptophan catabolites from microbiota engage aryl hydrocarbon receptor and balance mucosal reactivity via interleukin-22. Immunity. 2013;39:372–385. doi: 10.1016/j.immuni.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 46.Agus A, Planchais J, Sokol H. Gut microbiota regulation of tryptophan metabolism in health and disease. Cell Host Microbe. 2018;23:716–724. doi: 10.1016/j.chom.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 47.Rothhammer V, Quintana FJ. The aryl hydrocarbon receptor: an environmental sensor integrating immune responses in health and disease. Nat Rev Immunol. 2019;19:184–197. doi: 10.1038/s41577-019-0125-8. [DOI] [PubMed] [Google Scholar]
- 48.Jin UH, Cheng Y, Park H, Davidson LA, Callaway ES, Chapkin RS, Jayaraman A, Asante A, Allred C, Weaver EA, Safe S. Short chain fatty acids enhance Aryl Hydrocarbon (Ah) responsiveness in mouse colonocytes and Caco-2 human colon cancer cells. Sci Rep. 2017;7:10163. doi: 10.1038/s41598-017-10824-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bansal T, Alaniz RC, Wood TK, Jayaraman A. The bacterial signal indole increases epithelial-cell tight-junction resistance and attenuates indicators of inflammation. Proc Natl Acad Sci U S A. 2010;107:228–233. doi: 10.1073/pnas.0906112107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chimerel C, Emery E, Summers DK, Keyser U, Gribble FM, Reimann F. Bacterial metabolite indole modulates incretin secretion from intestinal enteroendocrine L cells. Cell Rep. 2014;9:1202–1208. doi: 10.1016/j.celrep.2014.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Takaki M, Mawe GM, Barasch JM, Gershon MD, Gershon MD. Physiological responses of guinea-pig myenteric neurons secondary to the release of endogenous serotonin by tryptamine. Neuroscience. 1985;16:223–240. doi: 10.1016/0306-4522(85)90059-4. [DOI] [PubMed] [Google Scholar]
- 52.Bhattarai Y, Williams BB, Battaglioli EJ, Whitaker WR, Till L, Grover M, Linden DR, Akiba Y, Kandimalla KK, Zachos NC, et al. Gut Microbiota-produced tryptamine activates an epithelial G-protein-coupled receptor to increase colonic secretion. Cell Host Microbe. 2018;23(775-785):e775. doi: 10.1016/j.chom.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cervenka I, Agudelo LZ, Ruas JL. Kynurenines: Tryptophan's metabolites in exercise, inflammation, and mental health. Science. 2017;357:eaaf9794. [DOI] [PubMed]
- 54.Dodd D, Spitzer MH, Van Treuren W, Merrill BD, Hryckowian AJ, Higginbottom SK, Le A, Cowan TM, Nolan GP, Fischbach MA, Sonnenburg JL. A gut bacterial pathway metabolizes aromatic amino acids into nine circulating metabolites. Nature. 2017;551:648–652. doi: 10.1038/nature24661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schirmer M, Smeekens SP, Vlamakis H, Jaeger M, Oosting M, Franzosa EA, Ter Horst R, Jansen T, Jacobs L, Bonder MJ, et al. Linking the human gut microbiome to inflammatory cytokine production capacity. Cell. 2016;167(1125-1136):e1128. doi: 10.1016/j.cell.2016.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Leitao-Goncalves R, Carvalho-Santos Z, Francisco AP, Fioreze GT, Anjos M, Baltazar C, Elias AP, Itskov PM, Piper MDW, Ribeiro C. Commensal bacteria and essential amino acids control food choice behavior and reproduction. PLoS Biol. 2017;15:e2000862. doi: 10.1371/journal.pbio.2000862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Velagapudi VR, Hezaveh R, Reigstad CS, Gopalacharyulu P, Yetukuri L, Islam S, Felin J, Perkins R, Boren J, Oresic M, Backhed F. The gut microbiota modulates host energy and lipid metabolism in mice. J Lipid Res. 2010;51:1101–1112. doi: 10.1194/jlr.M002774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ghazalpour A, Cespedes I, Bennett BJ, Allayee H. Expanding role of gut microbiota in lipid metabolism. Curr Opin Lipidol. 2016;27:141–147. doi: 10.1097/MOL.0000000000000278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Martinez-Guryn K, Hubert N, Frazier K, Urlass S, Musch MW, Ojeda P, Pierre JF, Miyoshi J, Sontag TJ, Cham CM, et al. Small intestine microbiota regulate host digestive and absorptive adaptive responses to dietary lipids. Cell Host Microbe. 2018;23(458-469):e455. doi: 10.1016/j.chom.2018.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Semova I, Carten JD, Stombaugh J, Mackey LC, Knight R, Farber SA, Rawls JF. Microbiota regulate intestinal absorption and metabolism of fatty acids in the zebrafish. Cell Host Microbe. 2012;12:277–288. doi: 10.1016/j.chom.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sato H, Zhang LS, Martinez K, Chang EB, Yang Q, Wang F, Howles PN, Hokari R, Miura S, Tso P. Antibiotics suppress activation of intestinal mucosal mast cells and reduce dietary lipid absorption in sprague-dawley rats. Gastroenterology. 2016;151:923–932. doi: 10.1053/j.gastro.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Araujo JR, Tazi A, Burlen-Defranoux O, Vichier-Guerre S, Nigro G, Licandro H, Demignot S, Sansonetti PJ. Fermentation products of commensal bacteria alter enterocyte lipid metabolism. Cell Host Microbe. 2020;27(358-375):e357. doi: 10.1016/j.chom.2020.01.028. [DOI] [PubMed] [Google Scholar]
- 63.Kenny DJ, Plichta DR, Shungin D, Koppel N, Hall AB, Fu B, Vasan RS, Shaw SY, Vlamakis H, Balskus EP, Xavier RJ. Cholesterol metabolism by uncultured human gut bacteria influences host cholesterol level. Cell Host Microbe. 2020;28(245-257):e246. doi: 10.1016/j.chom.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Caesar R, Tremaroli V, Kovatcheva-Datchary P, Cani PD, Backhed F. Crosstalk between gut microbiota and dietary lipids aggravates WAT inflammation through TLR signaling. Cell Metab. 2015;22:658–668. doi: 10.1016/j.cmet.2015.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.de Aguiar Vallim TQ, Tarling EJ, Edwards PA. Pleiotropic roles of bile acids in metabolism. Cell Metab. 2013;17:657–669. doi: 10.1016/j.cmet.2013.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Long SL, Gahan CGM, Joyce SA. Interactions between gut bacteria and bile in health and disease. Mol Asp Med. 2017;56:54–65. doi: 10.1016/j.mam.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 67.Jones BV, Begley M, Hill C, Gahan CG, Marchesi JR. Functional and comparative metagenomic analysis of bile salt hydrolase activity in the human gut microbiome. Proc Natl Acad Sci U S A. 2008;105:13580–13585. doi: 10.1073/pnas.0804437105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Geng W, Long SL, Chang YJ, Saxton AM, Joyce SA, Lin J. Evaluation of bile salt hydrolase inhibitor efficacy for modulating host bile profile and physiology using a chicken model system. Sci Rep. 2020;10:4941. doi: 10.1038/s41598-020-61723-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Joyce SA, MacSharry J, Casey PG, Kinsella M, Murphy EF, Shanahan F, Hill C, Gahan CG. Regulation of host weight gain and lipid metabolism by bacterial bile acid modification in the gut. Proc Natl Acad Sci U S A. 2014;111:7421–7426. doi: 10.1073/pnas.1323599111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mao K, Baptista AP, Tamoutounour S, Zhuang L, Bouladoux N, Martins AJ, Huang Y, Gerner MY, Belkaid Y, Germain RN. Innate and adaptive lymphocytes sequentially shape the gut microbiota and lipid metabolism. Nature. 2018;554:255–259. doi: 10.1038/nature25437. [DOI] [PubMed] [Google Scholar]
- 71.Wang Y, Kuang Z, Yu X, Ruhn KA, Kubo M, Hooper LV. The intestinal microbiota regulates body composition through NFIL3 and the circadian clock. Science. 2017;357:912–916. doi: 10.1126/science.aan0677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Thaiss CA, Nobs SP, Elinav E. NFIL-trating the host circadian rhythm-microbes fine-tune the epithelial clock. Cell Metab. 2017;26:699–700. doi: 10.1016/j.cmet.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 73.Chun E, Lavoie S, Fonseca-Pereira D, Bae S, Michaud M, Hoveyda HR, Fraser GL, Gallini Comeau CA, Glickman JN, Fuller MH, et al. Metabolite-sensing receptor Ffar2 regulates colonic group 3 innate lymphoid cells and gut immunity. Immunity. 2019;51(871-884):e876. doi: 10.1016/j.immuni.2019.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Spanogiannopoulos P, Bess EN, Carmody RN, Turnbaugh PJ. The microbial pharmacists within us: a metagenomic view of xenobiotic metabolism. Nat Rev Microbiol. 2016;14:273–287. doi: 10.1038/nrmicro.2016.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wilson ID, Nicholson JK. Gut microbiome interactions with drug metabolism, efficacy, and toxicity. Transl Res. 2017;179:204–222. doi: 10.1016/j.trsl.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Meinl W, Sczesny S, Brigelius-Flohe R, Blaut M, Glatt H. Impact of gut microbiota on intestinal and hepatic levels of phase 2 xenobiotic-metabolizing enzymes in the rat. Drug Metab Dispos. 2009;37:1179–1186. doi: 10.1124/dmd.108.025916. [DOI] [PubMed] [Google Scholar]
- 77.Clayton TA, Baker D, Lindon JC, Everett JR, Nicholson JK. Pharmacometabonomic identification of a significant host-microbiome metabolic interaction affecting human drug metabolism. Proc Natl Acad Sci U S A. 2009;106:14728–14733. doi: 10.1073/pnas.0904489106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Vich Vila A, Collij V, Sanna S, Sinha T, Imhann F, Bourgonje AR, Mujagic Z, Jonkers D, Masclee AAM, Fu J, et al. Impact of commonly used drugs on the composition and metabolic function of the gut microbiota. Nat Commun. 2020;11:362. doi: 10.1038/s41467-019-14177-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Maier L, Pruteanu M, Kuhn M, Zeller G, Telzerow A, Anderson EE, Brochado AR, Fernandez KC, Dose H, Mori H, et al. Extensive impact of non-antibiotic drugs on human gut bacteria. Nature. 2018;555:623–628. doi: 10.1038/nature25979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Caparros-Martin JA, Lareu RR, Ramsay JP, Peplies J, Reen FJ, Headlam HA, Ward NC, Croft KD, Newsholme P, Hughes JD, O'Gara F. Statin therapy causes gut dysbiosis in mice through a PXR-dependent mechanism. Microbiome. 2017;5:95. doi: 10.1186/s40168-017-0312-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Vieira-Silva S, Falony G, Belda E, Nielsen T, Aron-Wisnewsky J, Chakaroun R, Forslund SK, Assmann K, Valles-Colomer M, Nguyen TTD, et al. Statin therapy is associated with lower prevalence of gut microbiota dysbiosis. Nature. 2020;581:310–315. doi: 10.1038/s41586-020-2269-x. [DOI] [PubMed] [Google Scholar]
- 82.Whang A, Nagpal R, Yadav H. Bi-directional drug-microbiome interactions of anti-diabetics. EBioMedicine. 2019;39:591–602. doi: 10.1016/j.ebiom.2018.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sun L, Xie C, Wang G, Wu Y, Wu Q, Wang X, Liu J, Deng Y, Xia J, Chen B, et al. Gut microbiota and intestinal FXR mediate the clinical benefits of metformin. Nat Med. 2018;24:1919–1929. doi: 10.1038/s41591-018-0222-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wu H, Esteve E, Tremaroli V, Khan MT, Caesar R, Mannerås-Holm L, Ståhlman M, Olsson LM, Serino M, Planas-Fèlix M, et al. Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug. Nat Med. 2017;23:850–858. doi: 10.1038/nm.4345. [DOI] [PubMed] [Google Scholar]
- 85.de la Cuesta-Zuluaga J, Mueller NT, Corrales-Agudelo V, Velasquez-Mejia EP, Carmona JA, Abad JM, Escobar JS. Metformin is associated with higher relative abundance of mucin-degrading Akkermansia muciniphila and several short-chain fatty acid-producing microbiota in the gut. Diabetes Care. 2017;40:54–62. doi: 10.2337/dc16-1324. [DOI] [PubMed] [Google Scholar]
- 86.Shin NR, Lee JC, Lee HY, Kim MS, Whon TW, Lee MS, Bae JW. An increase in the Akkermansia spp. population induced by metformin treatment improves glucose homeostasis in diet-induced obese mice. Gut. 2014;63:727–735. doi: 10.1136/gutjnl-2012-303839. [DOI] [PubMed] [Google Scholar]
- 87.Jackson MA, Verdi S, Maxan ME, Shin CM, Zierer J, Bowyer RCE, Martin T, Williams FMK, Menni C, Bell JT, et al. Gut microbiota associations with common diseases and prescription medications in a population-based cohort. Nat Commun. 2018;9:2655. doi: 10.1038/s41467-018-05184-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Javdan B, Lopez JG, Chankhamjon P, Lee YJ, Hull R, Wu Q, et al. Personalized mapping of drug metabolism by the human gut microbiome. Cell. 2020;181:1661–1679.e1622. [DOI] [PMC free article] [PubMed]
- 89.Klunemann M, Andrejev S, Blasche S, Mateus A, Phapale P, Devendran S, Vappiani J, Simon B, Scott TA, Kafkia E, et al. Bioaccumulation of therapeutic drugs by human gut bacteria. Nature. 2021;597:533–538. doi: 10.1038/s41586-021-03891-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zimmermann M, Zimmermann-Kogadeeva M, Wegmann R, Goodman AL. Separating host and microbiome contributions to drug pharmacokinetics and toxicity. Science. 2019:363:eaat9931. [DOI] [PMC free article] [PubMed]
- 91.Zimmermann M, Zimmermann-Kogadeeva M, Wegmann R, Goodman AL. Mapping human microbiome drug metabolism by gut bacteria and their genes. Nature. 2019;570:462–467. doi: 10.1038/s41586-019-1291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yu EW, Gao L, Stastka P, Cheney MC, Mahabamunuge J, Torres Soto M, Ford CB, Bryant JA, Henn MR, Hohmann EL. Fecal microbiota transplantation for the improvement of metabolism in obesity: The FMT-TRIM double-blind placebo-controlled pilot trial. PLoS Med. 2020;17:e1003051. doi: 10.1371/journal.pmed.1003051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Reijnders D, Goossens GH, Hermes GD, Neis EP, van der Beek CM, Most J, Holst JJ, Lenaerts K, Kootte RS, Nieuwdorp M, et al. Effects of gut microbiota manipulation by antibiotics on host metabolism in obese humans: a randomized double-blind placebo-controlled trial. Cell Metab. 2016;24:63–74. doi: 10.1016/j.cmet.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 94.Zmora N, Soffer E, Elinav E. Transforming medicine with the microbiome. Sci Transl Med. 2019;11:eaaw1815. [DOI] [PubMed]
- 95.Dao MC, Everard A, Aron-Wisnewsky J, Sokolovska N, Prifti E, Verger EO, Kayser BD, Levenez F, Chilloux J, Hoyles L, et al. Akkermansia muciniphila and improved metabolic health during a dietary intervention in obesity: relationship with gut microbiome richness and ecology. Gut. 2016;65:426–436. doi: 10.1136/gutjnl-2014-308778. [DOI] [PubMed] [Google Scholar]
- 96.Depommier C, Everard A, Druart C, Plovier H, Van Hul M, Vieira-Silva S, Falony G, Raes J, Maiter D, Delzenne NM, et al. Supplementation with Akkermansia muciniphila in overweight and obese human volunteers: a proof-of-concept exploratory study. Nat Med. 2019;25:1096–1103. doi: 10.1038/s41591-019-0495-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yoon HS, Cho CH, Yun MS, Jang SJ, You HJ, Kim J-h, Han D, Cha KH, Moon SH, Lee K, et al. Akkermansia muciniphila secretes a glucagon-like peptide-1-inducing protein that improves glucose homeostasis and ameliorates metabolic disease in mice. Nat Microbiol. 2021;6:563–573. doi: 10.1038/s41564-021-00880-5. [DOI] [PubMed] [Google Scholar]
- 98.Allegretti JR, Kassam Z, Mullish BH, Chiang A, Carrellas M, Hurtado J, Marchesi JR, McDonald JAK, Pechlivanis A, Barker GF, et al. Effects of fecal microbiota transplantation with oral capsules in obese patients. Clin Gastroenterol Hepatol. 2020;18(855-863):e852. doi: 10.1016/j.cgh.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 99.Vrieze A, Van Nood E, Holleman F, Salojarvi J, Kootte RS, Bartelsman JF, Dallinga-Thie GM, Ackermans MT, Serlie MJ, Oozeer R, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. 2012;143(913-916):e917. doi: 10.1053/j.gastro.2012.06.031. [DOI] [PubMed] [Google Scholar]
- 100.Basolo A, Hohenadel M, Ang QY, Piaggi P, Heinitz S, Walter M, Walter P, Parrington S, Trinidad DD, von Schwartzenberg RJ, et al. Effects of underfeeding and oral vancomycin on gut microbiome and nutrient absorption in humans. Nat Med. 2020;26:589–598. doi: 10.1038/s41591-020-0801-z. [DOI] [PubMed] [Google Scholar]
- 101.Chaudhari SN, Harris DA, Aliakbarian H, Luo JN, Henke MT, Subramaniam R, Vernon AH, Tavakkoli A, Sheu EG, Devlin AS. Bariatric surgery reveals a gut-restricted TGR5 agonist with anti-diabetic effects. Nat Chem Biol. 2021;17:20–29. doi: 10.1038/s41589-020-0604-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Chaudhari SN, Luo JN, Harris DA, Aliakbarian H, Yao L, Paik D, Subramaniam R, Adhikari AA, Vernon AH, Kilic A, et al. A microbial metabolite remodels the gut-liver axis following bariatric surgery. Cell Host Microbe. 2021;29(408-424):e407. doi: 10.1016/j.chom.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Suez J, Zmora N, Segal E, Elinav E. The pros, cons, and many unknowns of probiotics. Nat Med. 2019;25:716–729. doi: 10.1038/s41591-019-0439-x. [DOI] [PubMed] [Google Scholar]
- 104.Veiga P, Suez J, Derrien M, Elinav E. Moving from probiotics to precision probiotics. Nat Microbiol. 2020;5:878–880. doi: 10.1038/s41564-020-0721-1. [DOI] [PubMed] [Google Scholar]
- 105.Rajkumar H, Mahmood N, Kumar M, Varikuti SR, Challa HR, Myakala SP. Effect of probiotic (VSL#3) and omega-3 on lipid profile, insulin sensitivity, inflammatory markers, and gut colonization in overweight adults: a randomized, controlled trial. Mediat Inflamm. 2014;2014:348959. doi: 10.1155/2014/348959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Alisi A, Bedogni G, Baviera G, Giorgio V, Porro E, Paris C, Giammaria P, Reali L, Anania F, Nobili V. Randomised clinical trial: the beneficial effects of VSL#3 in obese children with non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2014;39:1276–1285. doi: 10.1111/apt.12758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Jones RB, Alderete TL, Martin AA, Geary BA, Hwang DH, Palmer SL, Goran MI. Probiotic supplementation increases obesity with no detectable effects on liver fat or gut microbiota in obese Hispanic adolescents: a 16-week, randomized, placebo-controlled trial. Pediatric Obesity. 2018;13:705–714. doi: 10.1111/ijpo.12273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wiciński M, Gębalski J, Gołębiewski J, Malinowski B. Probiotics for the treatment of overweight and obesity in Humans-A review of clinical trials. Microorganisms. 2020;8:1148. doi: 10.3390/microorganisms8081148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Perna S, Ilyas Z, Giacosa A, Gasparri C, Peroni G, Faliva MA, Rigon C, Naso M, Riva A, Petrangolini G, et al. Is probiotic supplementation useful for the management of body weight and other anthropometric measures in adults affected by overweight and obesity with metabolic related diseases? A systematic review and meta-analysis. Nutrients. 2021;13:666. doi: 10.3390/nu13020666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Park S, Bae J-H. Probiotics for weight loss: a systematic review and meta-analysis. Nutr Res. 2015;35:566–575. doi: 10.1016/j.nutres.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 111.Mohammadi H, Ghavami A, Hadi A, Askari G, Symonds M, Miraghajani M. Effects of pro-/synbiotic supplementation on anthropometric and metabolic indices in overweight or obese children and adolescents: a systematic review and meta-analysis. Complement Ther Med. 2019;44:269–276. doi: 10.1016/j.ctim.2019.05.008. [DOI] [PubMed] [Google Scholar]
- 112.Borgeraas H, Johnson LK, Skattebu J, Hertel JK, Hjelmesæth J. Effects of probiotics on body weight, body mass index, fat mass and fat percentage in subjects with overweight or obesity: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2018;19:219–232. doi: 10.1111/obr.12626. [DOI] [PubMed] [Google Scholar]
- 113.Zhang Q, Wu Y, Fei X. Effect of probiotics on body weight and body-mass index: a systematic review and meta-analysis of randomized, controlled trials. Int J Food Sci Nutr. 2016;67:571–580. doi: 10.1080/09637486.2016.1181156. [DOI] [PubMed] [Google Scholar]
- 114.Koutnikova H, Genser B, Monteiro-Sepulveda M, Faurie J-M, Rizkalla S, Schrezenmeir J, Clément K. Impact of bacterial probiotics on obesity, diabetes and non-alcoholic fatty liver disease related variables: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2019;9:e017995. doi: 10.1136/bmjopen-2017-017995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hildebrand F, Nguyen TLA, Brinkman B, Yunta RG, Cauwe B, Vandenabeele P, Liston A, Raes J. Inflammation-associated enterotypes, host genotype, cage and inter-individual effects drive gut microbiota variation in common laboratory mice. Genome Biol. 2013;14:R4. doi: 10.1186/gb-2013-14-1-r4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Zhang X, Zhong H, Li Y, Shi Z, Ren H, Zhang Z, Zhou X, Tang S, Han X, Lin Y, et al. Sex- and age-related trajectories of the adult human gut microbiota shared across populations of different ethnicities. Nat Aging. 2021;1:87–100. doi: 10.1038/s43587-020-00014-2. [DOI] [PubMed] [Google Scholar]
- 117.David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, Ling AV, Devlin AS, Varma Y, Fischbach MA. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–563. doi: 10.1038/nature12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zmora N, Zilberman-Schapira G, Suez J, Mor U, Dori-Bachash M, Bashiardes S, Kotler E, Zur M, Regev-Lehavi D, Brik RB-Z, et al. Personalized gut mucosal colonization resistance to empiric probiotics is associated with unique host and microbiome features. Cell. 2018;174:1388–1405.e1321. doi: 10.1016/j.cell.2018.08.041. [DOI] [PubMed] [Google Scholar]
- 119.Zeevi D, Korem T, Zmora N, Israeli D, Rothschild D, Weinberger A, Ben-Yacov O, Lador D, Avnit-Sagi T, Lotan-Pompan M, et al. Personalized nutrition by prediction of glycemic responses. Cell. 2015;163:1079–1094. doi: 10.1016/j.cell.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 120.Rein M, Ben-Yacov O, Godneva A, Shilo S, Zmora N, Kolobkov D, Cohen-Dolev N, Wolf B-C, Kosower N, Lotan-Pompan M, et al. Effects of personalized diets by prediction of glycemic responses on glycemic control and metabolic health in newly diagnosed T2DM: a randomized dietary intervention pilot trial. BMC Med. 2022;20:56. doi: 10.1186/s12916-022-02254-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ben-Yacov O, Godneva A, Rein M, Shilo S, Kolobkov D, Koren N, Cohen Dolev N, Travinsky Shmul T, Wolf BC, Kosower N, et al. Personalized postprandial glucose response–targeting diet versus mediterranean diet for glycemic control in prediabetes. Diabetes Care. 2021;44:1980–1991. doi: 10.2337/dc21-0162. [DOI] [PubMed] [Google Scholar]
- 122.Delannoy-Bruno O, Desai C, Raman AS, Chen RY, Hibberd MC, Cheng J, Han N, Castillo JJ, Couture G, Lebrilla CB, et al. Evaluating microbiome-directed fibre snacks in gnotobiotic mice and humans. Nature. 2021;595:91–95. doi: 10.1038/s41586-021-03671-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Patnode ML, Beller ZW, Han ND, Cheng J, Peters SL, Terrapon N, Henrissat B, Le Gall S, Saulnier L, Hayashi DK, et al. Interspecies competition impacts targeted manipulation of human gut bacteria by fiber-derived glycans. Cell. 2019;179:59–73.e13. doi: 10.1016/j.cell.2019.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wastyk HC, Fragiadakis GK, Perelman D, Dahan D, Merrill BD, Yu FB, Topf M, Gonzalez CG, Van Treuren W, Han S, et al. Gut-microbiota-targeted diets modulate human immune status. Cell. 2021;184:4137–4153.e4114. doi: 10.1016/j.cell.2021.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Berry SE, Valdes AM, Drew DA, Asnicar F, Mazidi M, Wolf J, Capdevila J, Hadjigeorgiou G, Davies R, Al Khatib H, et al. Human postprandial responses to food and potential for precision nutrition. Nat Med. 2020;26:964–973. doi: 10.1038/s41591-020-0934-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Asnicar F, Berry SE, Valdes AM, Nguyen LH, Piccinno G, Drew DA, Leeming E, Gibson R, Le Roy C, Khatib HA, et al. Microbiome connections with host metabolism and habitual diet from 1,098 deeply phenotyped individuals. Nat Med. 2021;27:321–332. doi: 10.1038/s41591-020-01183-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bennett BJ, de Aguiar Vallim TQ, Wang Z, Shih DM, Meng Y, Gregory J, Allayee H, Lee R, Graham M, Crooke R, et al. Trimethylamine-N-oxide, a metabolite associated with atherosclerosis, exhibits complex genetic and dietary regulation. Cell Metab. 2013;17:49–60. doi: 10.1016/j.cmet.2012.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Haghikia A, Li XS, Liman TG, Bledau N, Schmidt D, Zimmermann F, Krankel N, Widera C, Sonnenschein K, Haghikia A, et al. Gut microbiota-dependent trimethylamine N-Oxide predicts risk of cardiovascular events in patients with stroke and is related to proinflammatory monocytes. Arterioscler Thromb Vasc Biol. 2018;38:2225–2235. doi: 10.1161/ATVBAHA.118.311023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Missailidis C, Hallqvist J, Qureshi AR, Barany P, Heimburger O, Lindholm B, Stenvinkel P, Bergman P. Serum trimethylamine-N-oxide is strongly related to renal function and predicts outcome in chronic kidney disease. PLoS One. 2016;11:e0141738. doi: 10.1371/journal.pone.0141738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Schiattarella GG, Sannino A, Toscano E, Giugliano G, Gargiulo G, Franzone A, Trimarco B, Esposito G, Perrino C. Gut microbe-generated metabolite trimethylamine-N-oxide as cardiovascular risk biomarker: a systematic review and dose-response meta-analysis. Eur Heart J. 2017;38:2948–2956. doi: 10.1093/eurheartj/ehx342. [DOI] [PubMed] [Google Scholar]
- 131.Tan Y, Sheng Z, Zhou P, Liu C, Zhao H, Song L, Li J, Zhou J, Chen Y, Wang L, et al. Plasma trimethylamine N-oxide as a novel biomarker for plaque rupture in patients with ST-Segment-Elevation myocardial infarction. Circ Cardiovasc Interv. 2019;12:e007281. doi: 10.1161/CIRCINTERVENTIONS.118.007281. [DOI] [PubMed] [Google Scholar]
- 132.Vogt NM, Romano KA, Darst BF, Engelman CD, Johnson SC, Carlsson CM, Asthana S, Blennow K, Zetterberg H, Bendlin BB, Rey FE. The gut microbiota-derived metabolite trimethylamine N-oxide is elevated in Alzheimer's disease. Alzheimers Res Ther. 2018;10:124. doi: 10.1186/s13195-018-0451-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wang Z, Klipfell E, Bennett BJ, Koeth R, Levison BS, Dugar B, Feldstein AE, Britt EB, Fu X, Chung YM, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011;472:57–63. doi: 10.1038/nature09922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhu W, Gregory JC, Org E, Buffa JA, Gupta N, Wang Z, Li L, Fu X, Wu Y, Mehrabian M, et al. Gut microbial metabolite TMAO enhances platelet hyperreactivity and thrombosis risk. Cell. 2016;165:111–124. doi: 10.1016/j.cell.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zhuang R, Ge X, Han L, Yu P, Gong X, Meng Q, Zhang Y, Fan H, Zheng L, Liu Z, Zhou X. Gut microbe-generated metabolite trimethylamine N-oxide and the risk of diabetes: a systematic review and dose-response meta-analysis. Obes Rev. 2019;20:883–894. doi: 10.1111/obr.12843. [DOI] [PubMed] [Google Scholar]
- 136.Roberts AB, Gu X, Buffa JA, Hurd AG, Wang Z, Zhu W, Gupta N, Skye SM, Cody DB, Levison BS, et al. Development of a gut microbe-targeted nonlethal therapeutic to inhibit thrombosis potential. Nat Med. 2018;24:1407–1417. doi: 10.1038/s41591-018-0128-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wang Z, Roberts AB, Buffa JA, Levison BS, Zhu W, Org E, Gu X, Huang Y, Zamanian-Daryoush M, Culley MK, et al. Non-lethal inhibition of gut microbial trimethylamine production for the treatment of atherosclerosis. Cell. 2015;163:1585–1595. doi: 10.1016/j.cell.2015.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Awoyemi A, Mayerhofer C, Felix AS, Hov JR, Moscavitch SD, Lappegård KT, et al. Rifaximin or saccharomyces boulardii in heart failure with reduced ejection fraction: results from the randomized GutHeart trial. eBioMedicine. 2021;70:103511. [DOI] [PMC free article] [PubMed]
- 139.Crimarco A, Springfield S, Petlura C, Streaty T, Cunanan K, Lee J, Fielding-Singh P, Carter MM, Topf MA, Wastyk HC, et al. A randomized crossover trial on the effect of plant-based compared with animal-based meat on trimethylamine-N-oxide and cardiovascular disease risk factors in generally healthy adults: Study With Appetizing Plantfood-Meat Eating Alternative Trial (SWAP-MEAT) Am J Clin Nutr. 2020;112:1188–1199. doi: 10.1093/ajcn/nqaa203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kimber C, Zhang S, Johnson C, West RE, 3rd, Prokopienko AJ, Mahnken JD, Yu AS, Hoofnagle AN, Ir D, Robertson CE, et al. Randomized, placebo-controlled trial of rifaximin therapy for lowering gut-derived cardiovascular toxins and inflammation in CKD. Kidney360. 2020;1:1206–1216. doi: 10.34067/KID.0003942020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Yang S, Li X, Yang F, Zhao R, Pan X, Liang J, et al. Gut microbiota-dependent marker TMAO in promoting cardiovascular disease: inflammation mechanism, clinical prognostic, and potential as a therapeutic target. Front Pharmacol. 2019;10. [DOI] [PMC free article] [PubMed]
- 142.Descamps HC, Herrmann B, Wiredu D, Thaiss CA. The path toward using microbial metabolites as therapies. EBioMedicine. 2019;44:747–754. doi: 10.1016/j.ebiom.2019.05.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sharpton SR, Schnabl B, Knight R, Loomba R. Current concepts, opportunities, and challenges of gut microbiome-based personalized medicine in nonalcoholic fatty liver disease. Cell Metab. 2021;33:21–32. doi: 10.1016/j.cmet.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Thaiss CA. Microbiome dynamics in obesity. Science. 2018;362:903–904. doi: 10.1126/science.aav6870. [DOI] [PubMed] [Google Scholar]
- 145.Kuang Z, Wang Y, Li Y, Ye C, Ruhn KA, Behrendt CL, Olson EN, Hooper LV. The intestinal microbiota programs diurnal rhythms in host metabolism through histone deacetylase 3. Science. 2019;365:1428–1434. doi: 10.1126/science.aaw3134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Whitt J, Woo V, Lee P, Moncivaiz J, Haberman Y, Denson L, Tso P, Alenghat T. Disruption of epithelial HDAC3 in intestine prevents diet-induced obesity in mice. Gastroenterology. 2018;155:501–513. doi: 10.1053/j.gastro.2018.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Leone V, Gibbons SM, Martinez K, Hutchison AL, Huang EY, Cham CM, Pierre JF, Heneghan AF, Nadimpalli A, Hubert N, et al. Effects of diurnal variation of gut microbes and high-fat feeding on host circadian clock function and metabolism. Cell Host Microbe. 2015;17:681–689. doi: 10.1016/j.chom.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Thaiss CA, Levy M, Elinav E. Chronobiomics: the biological clock as a new principle in host-microbial interactions. PLoS Pathog. 2015;11:e1005113. doi: 10.1371/journal.ppat.1005113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Thaiss CA, Levy M, Korem T, Dohnalova L, Shapiro H, Jaitin DA, David E, Winter DR, Gury-BenAri M, Tatirovsky E, et al. Microbiota diurnal rhythmicity programs host transcriptome oscillations. Cell. 2016;167(1495-1510):e1412. doi: 10.1016/j.cell.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 150.Thaiss CA, Zeevi D, Levy M, Segal E, Elinav E. A day in the life of the meta-organism: diurnal rhythms of the intestinal microbiome and its host. Gut Microbes. 2015;6:137–142. doi: 10.1080/19490976.2015.1016690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Thaiss CA, Zeevi D, Levy M, Zilberman-Schapira G, Suez J, Tengeler AC, Abramson L, Katz MN, Korem T, Zmora N, et al. Transkingdom control of microbiota diurnal oscillations promotes metabolic homeostasis. Cell. 2014;159:514–529. doi: 10.1016/j.cell.2014.09.048. [DOI] [PubMed] [Google Scholar]
- 152.Litichevskiy L, Thaiss CA. The oscillating gut microbiome and its effects on host circadian biology. Annual Review of Nutrition. 2022;42. [DOI] [PubMed]
- 153.Uhr GT, Dohnalova L, Thaiss CA. The dimension of time in host-microbiome interactions. mSystems. 2019;4:e00216–00218. [DOI] [PMC free article] [PubMed]
- 154.Reitmeier S, Kiessling S, Clavel T, List M, Almeida EL, Ghosh TS, Neuhaus K, Grallert H, Linseisen J, Skurk T, et al. Arrhythmic gut microbiome signatures predict risk of Type 2 diabetes. Cell Host Microbe. 2020;28(258-272):e256. doi: 10.1016/j.chom.2020.06.004. [DOI] [PubMed] [Google Scholar]
- 155.Nath K, Thaiss CA. Digitalizing the microbiome for human health. mSystems. 2019;4:e00129–00119. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.